THE HEART Introduction Size Relatively small conical organ


- Slides: 73

THE HEART
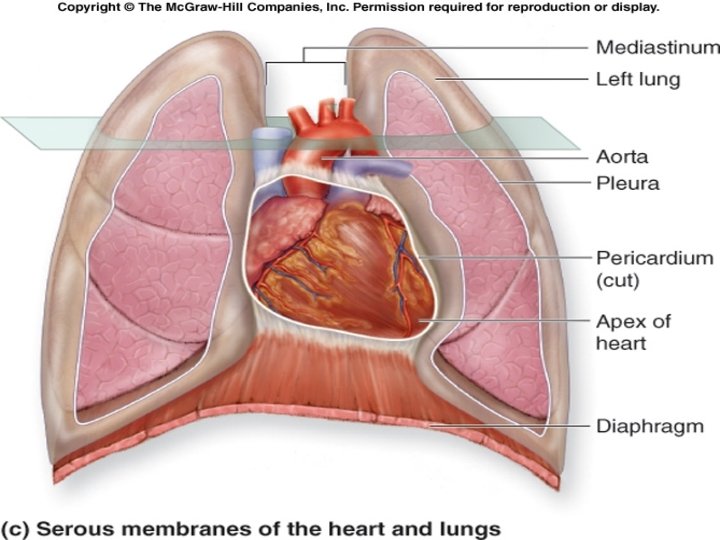
Introduction Size: Relatively small, conical organ approximately the size of a person’s clenched fist. Wt. = 250 -300 grams Dimensions: 12 x 9 cm Name: Greek (cardia) / Latin (cor) Location: left of the body midline posterior to the sternum in the middle mediastinum. ⅔’s of it lies to the left of the midsternal line
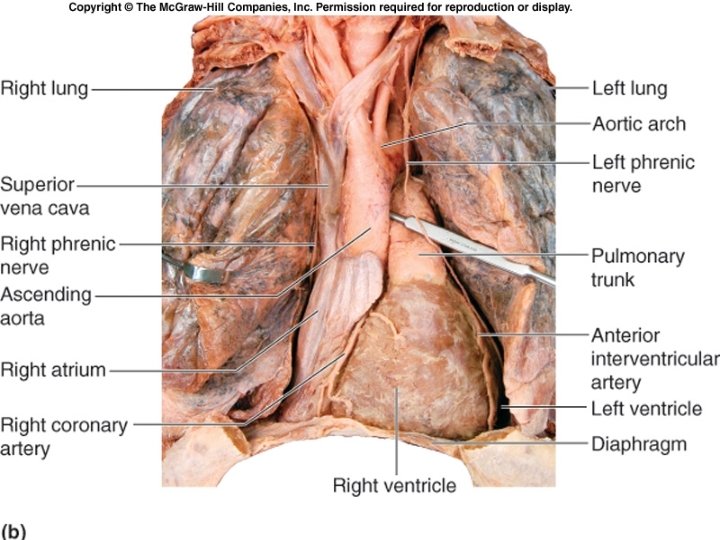
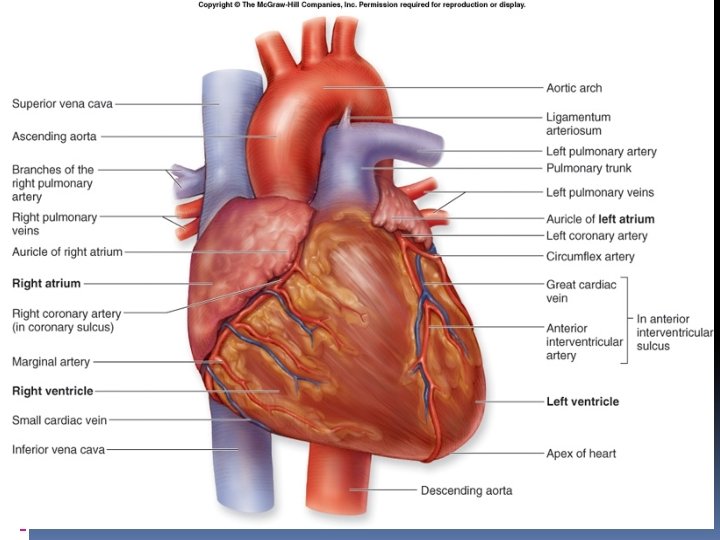
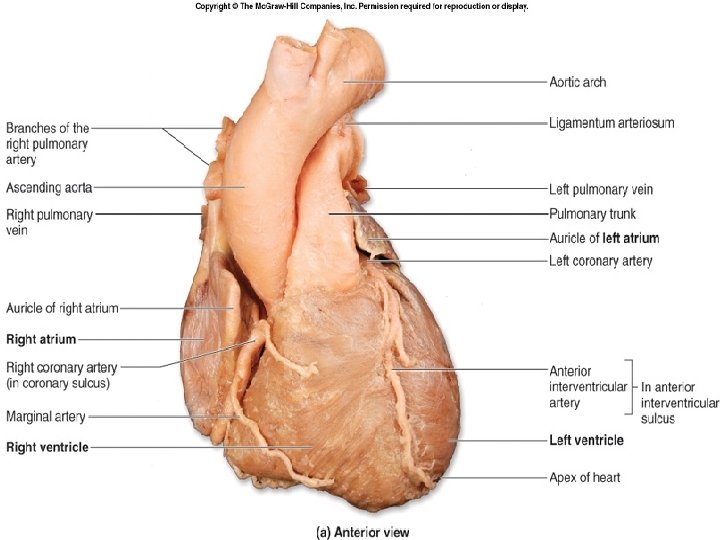
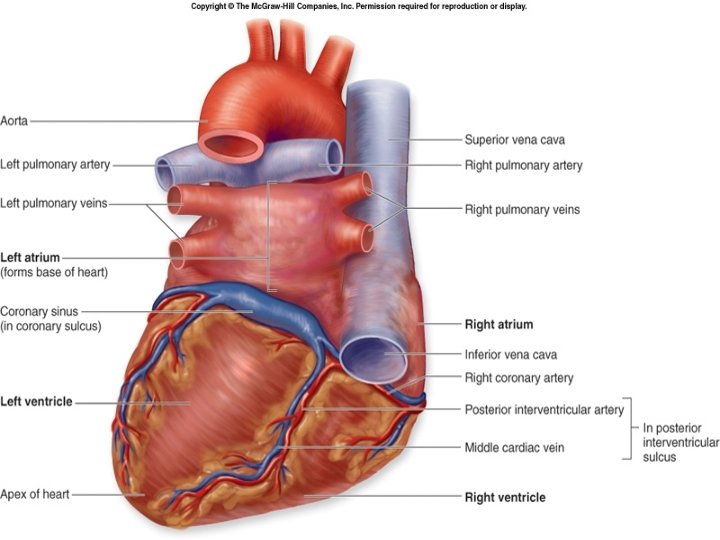
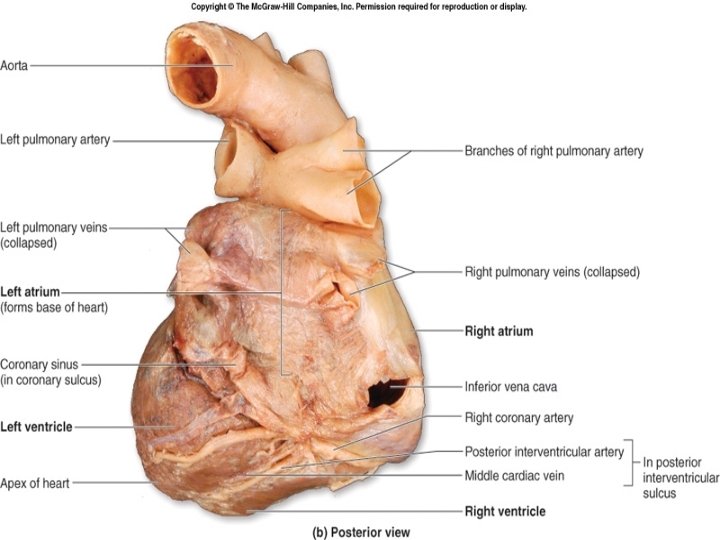
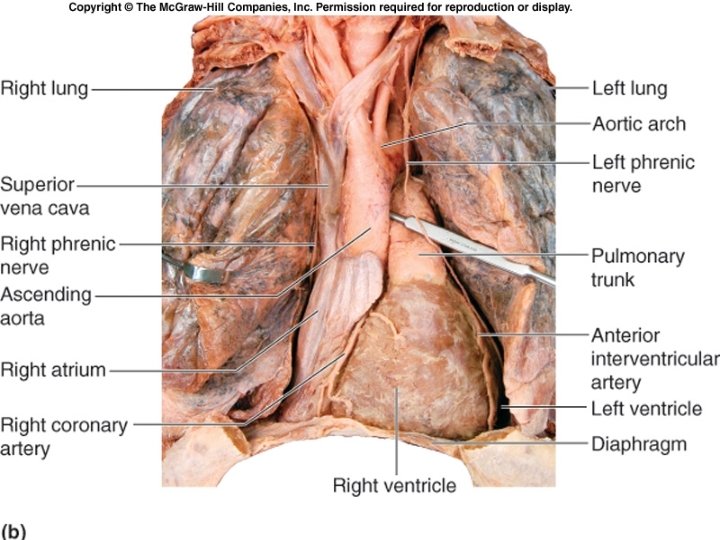
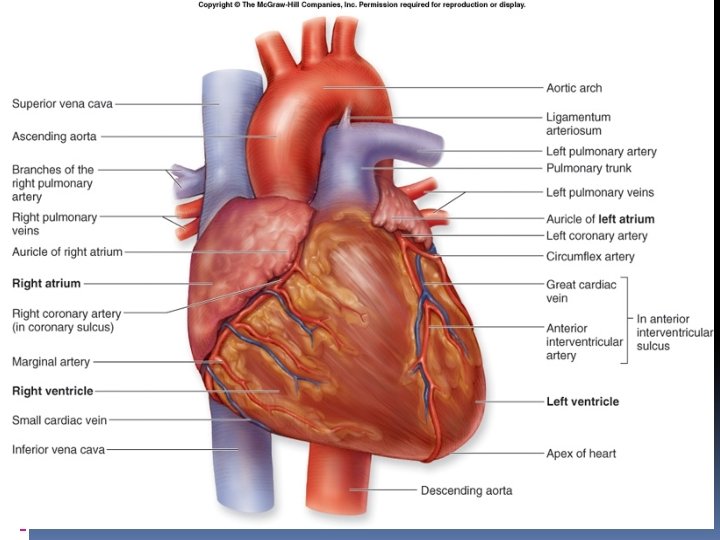
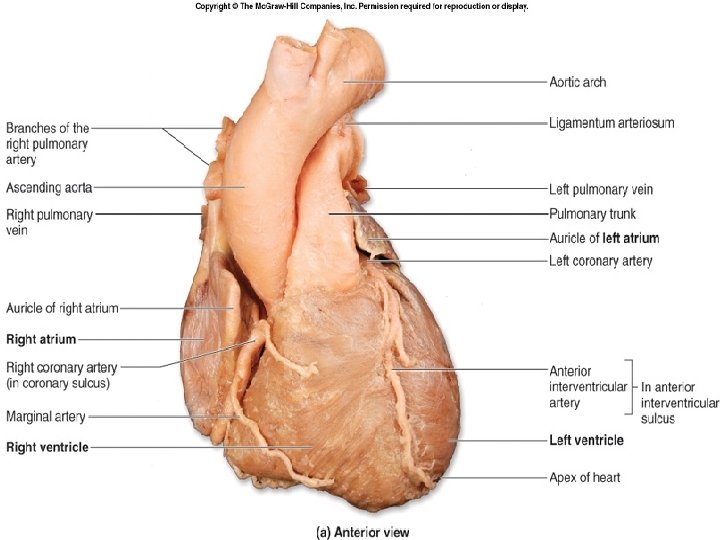
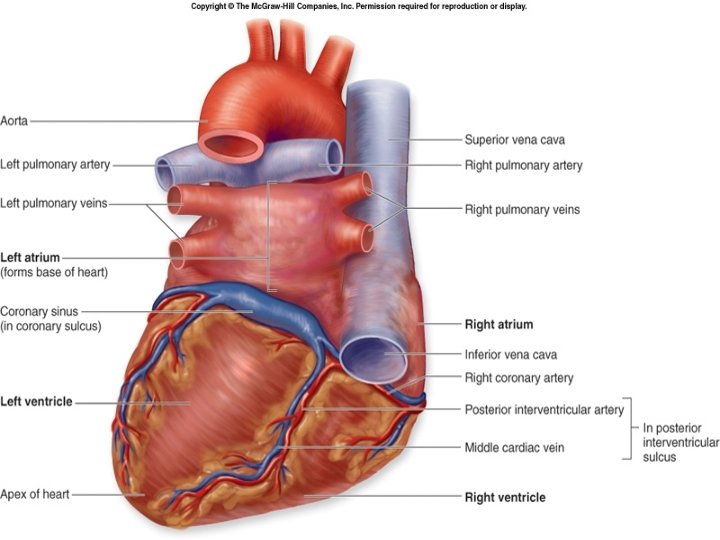
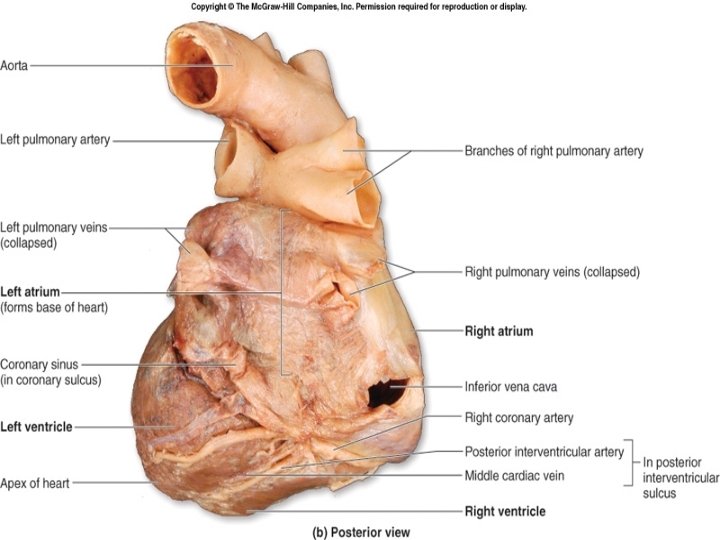
External Anatomy of the Heart Has four hollow chambers: �two smaller atria �two larger ventricles Heart is rotated such that its right side (right atrium and ventricle) is located more anteriorly, while its left side (left atrium and ventricle) is located more posteriorly. The posterosuperior surface of the heart, formed primarily by the left atrium, is called the base. Related to T 5 to T 8 vertebrae in lying position and descend by one vertebra in erect posture The apex of the heart is the most anterior and inferior portion of the left ventricle. This is the most mobile portion of the heart, and produces the "apex beat".
External Anatomy of the Heart Atria are separated from the ventricles externally by coronary sulcus (or atrioventricular sulcus) extends around the circumference of the heart. On both the anterior and posterior surfaces of the heart, the anterior interventricular sulcus and the posterior interventricular sulcus are located between the left and right ventricles. These sulci extend inferiorly from the coronary sulcus toward the heart apex.
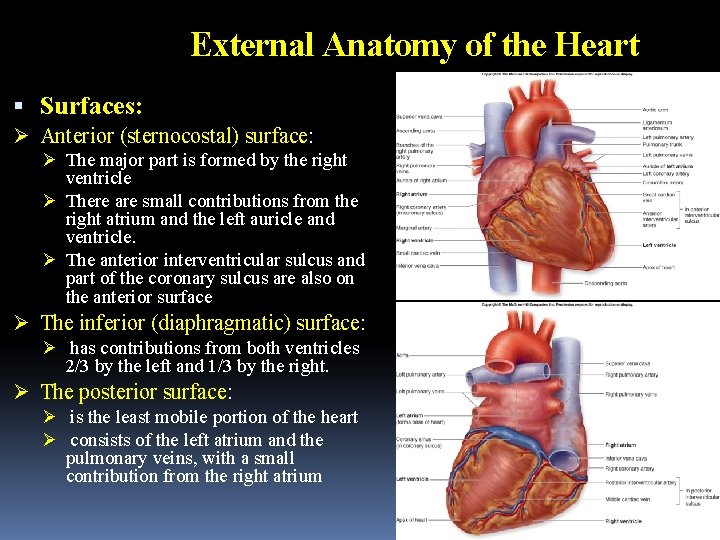
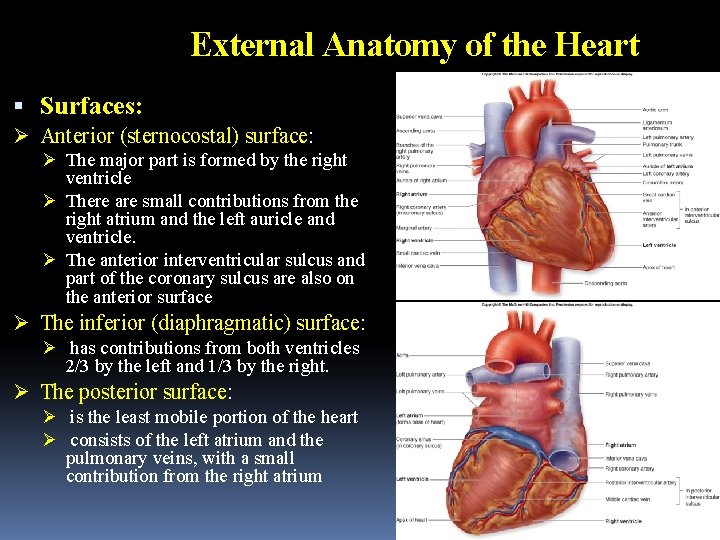
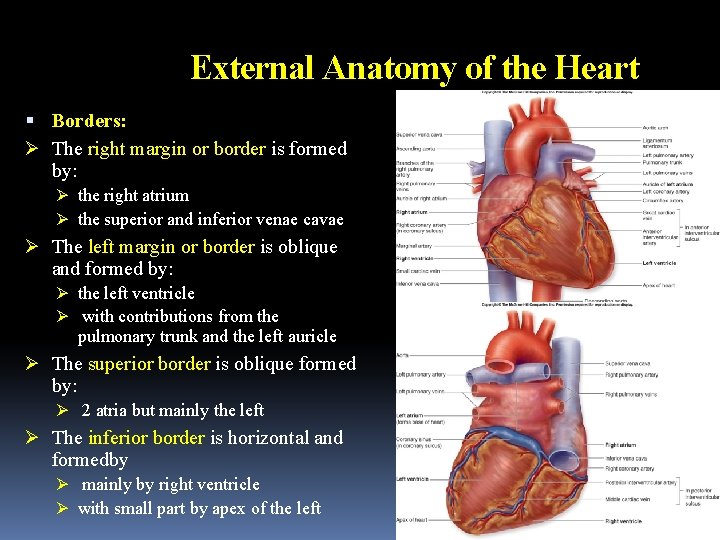
External Anatomy of the Heart Surfaces: Ø Anterior (sternocostal) surface: Ø The major part is formed by the right ventricle Ø There are small contributions from the right atrium and the left auricle and ventricle. Ø The anterior interventricular sulcus and part of the coronary sulcus are also on the anterior surface Ø The inferior (diaphragmatic) surface: Ø has contributions from both ventricles 2/3 by the left and 1/3 by the right. Ø The posterior surface: Ø is the least mobile portion of the heart Ø consists of the left atrium and the pulmonary veins, with a small contribution from the right atrium
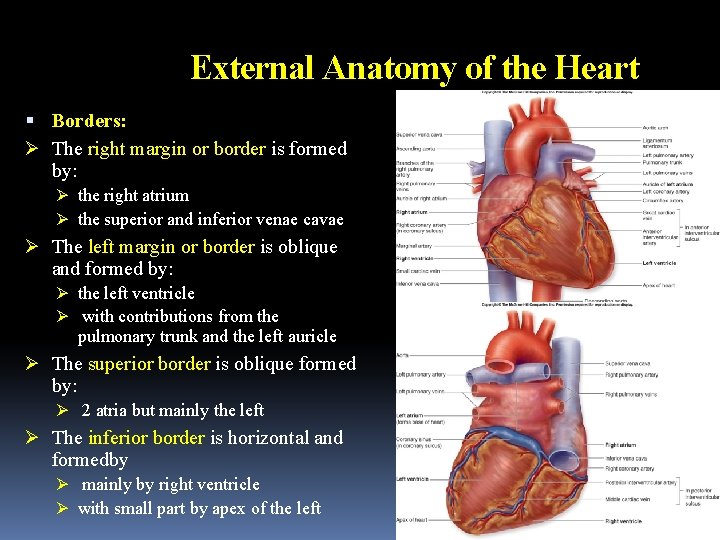
External Anatomy of the Heart Borders: Ø The right margin or border is formed by: Ø the right atrium Ø the superior and inferior venae cavae Ø The left margin or border is oblique and formed by: Ø the left ventricle Ø with contributions from the pulmonary trunk and the left auricle Ø The superior border is oblique formed by: Ø 2 atria but mainly the left Ø The inferior border is horizontal and formedby Ø mainly by right ventricle Ø with small part by apex of the left
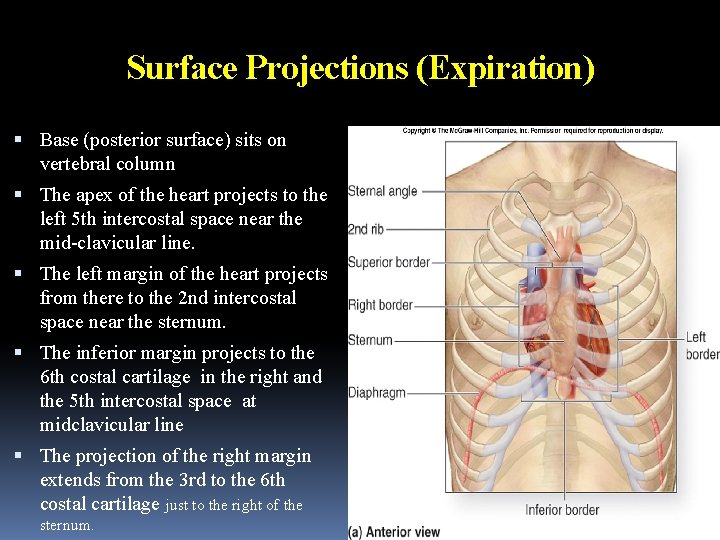
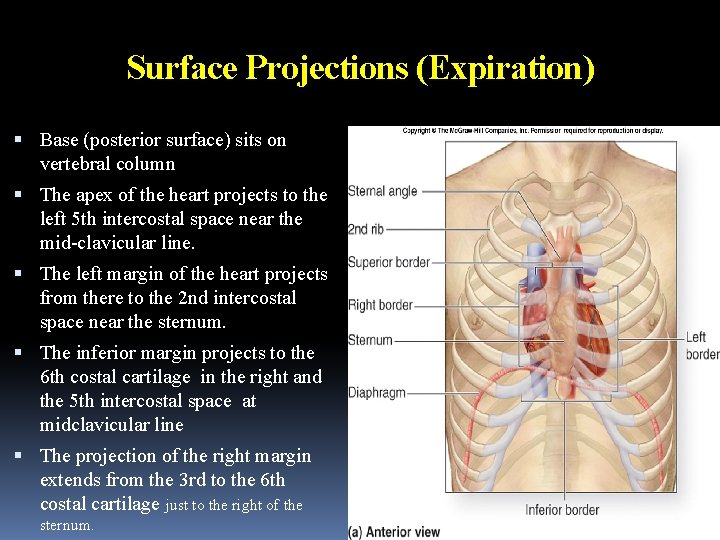
Surface Projections (Expiration) Base (posterior surface) sits on vertebral column The apex of the heart projects to the left 5 th intercostal space near the mid-clavicular line. The left margin of the heart projects from there to the 2 nd intercostal space near the sternum. The inferior margin projects to the 6 th costal cartilage in the right and the 5 th intercostal space at midclavicular line The projection of the right margin extends from the 3 rd to the 6 th costal cartilage just to the right of the sternum.
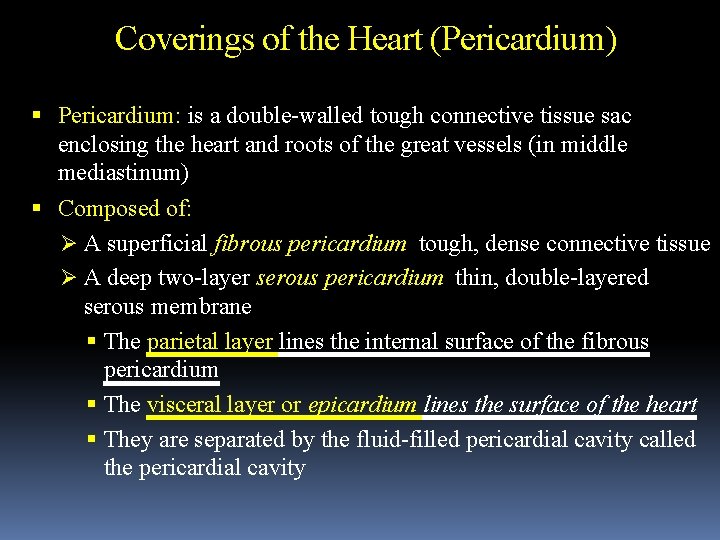
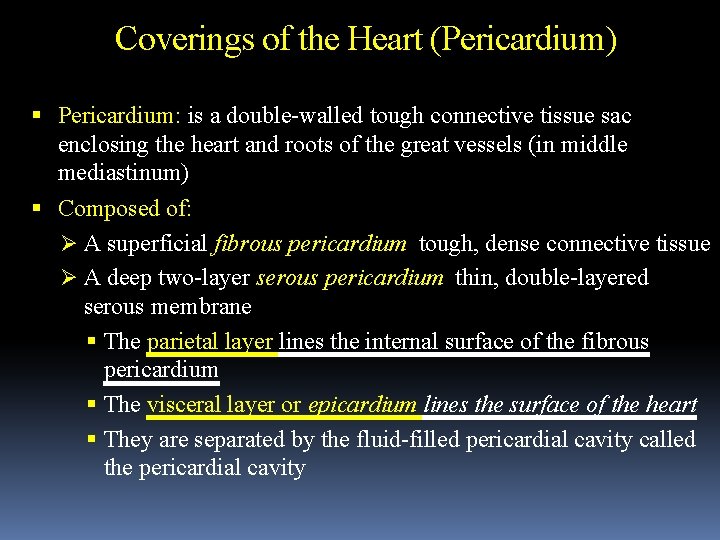
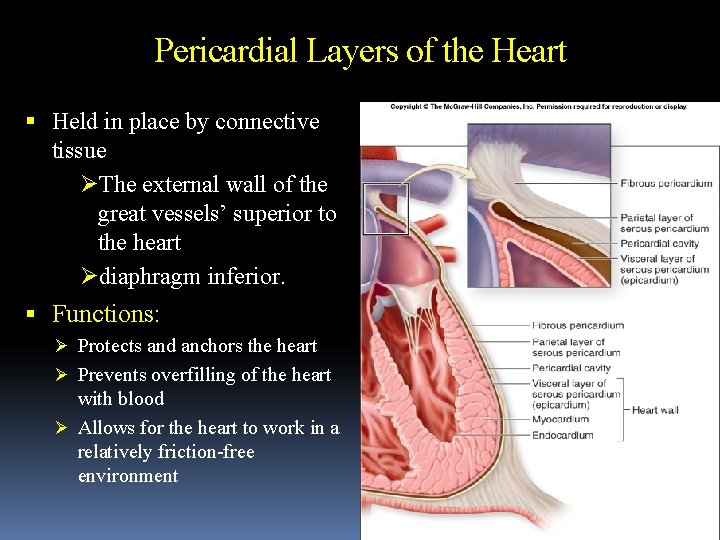
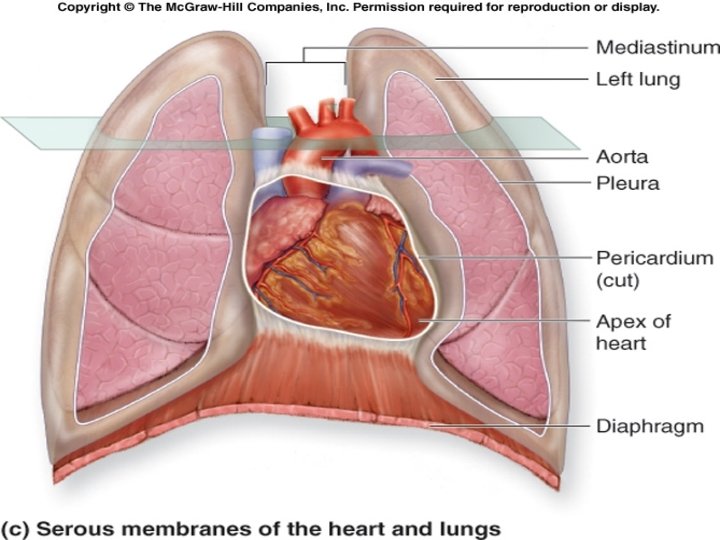
Coverings of the Heart (Pericardium) Pericardium: is a double-walled tough connective tissue sac enclosing the heart and roots of the great vessels (in middle mediastinum) Composed of: Ø A superficial fibrous pericardium tough, dense connective tissue Ø A deep two-layer serous pericardium thin, double-layered serous membrane The parietal layer lines the internal surface of the fibrous pericardium The visceral layer or epicardium lines the surface of the heart They are separated by the fluid-filled pericardial cavity called the pericardial cavity
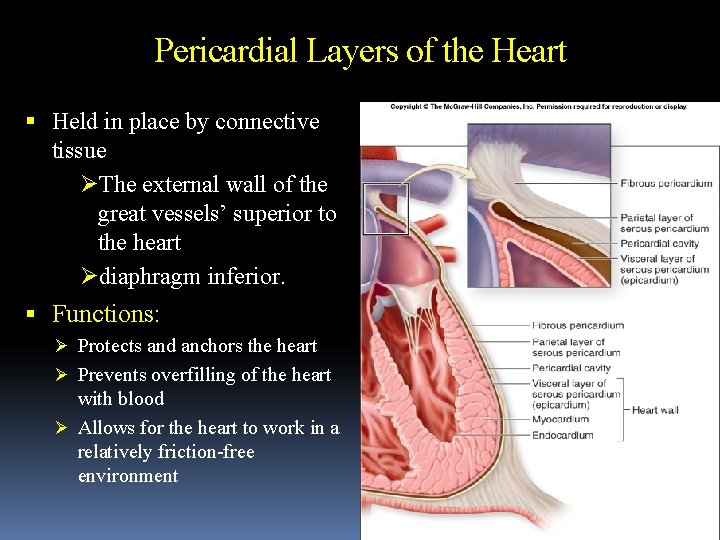
Pericardial Layers of the Heart Held in place by connective tissue ØThe external wall of the great vessels’ superior to the heart Ødiaphragm inferior. Functions: Ø Protects and anchors the heart Ø Prevents overfilling of the heart with blood Ø Allows for the heart to work in a relatively friction-free environment
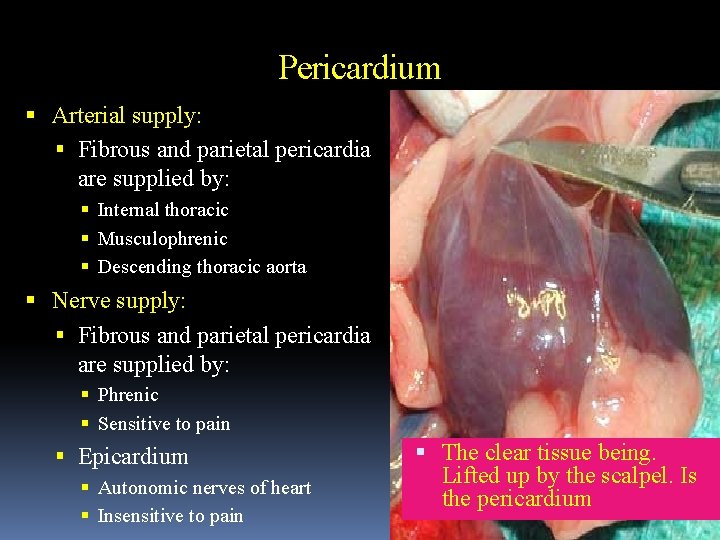
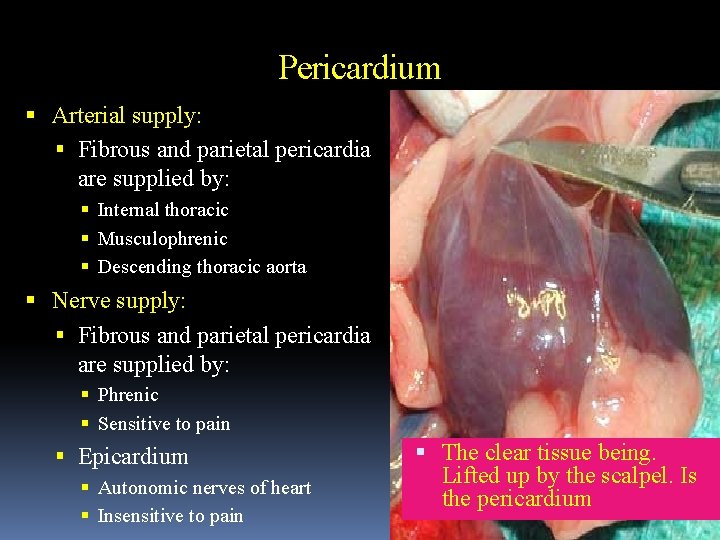
Pericardium Arterial supply: Fibrous and parietal pericardia are supplied by: Internal thoracic Musculophrenic Descending thoracic aorta Nerve supply: Fibrous and parietal pericardia are supplied by: Phrenic Sensitive to pain Epicardium Autonomic nerves of heart Insensitive to pain The clear tissue being. Lifted up by the scalpel. Is the pericardium
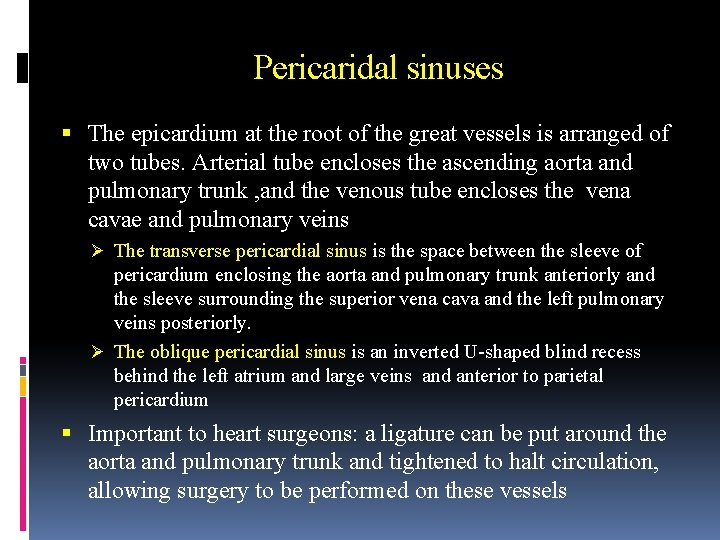
Pericaridal sinuses The epicardium at the root of the great vessels is arranged of two tubes. Arterial tube encloses the ascending aorta and pulmonary trunk , and the venous tube encloses the vena cavae and pulmonary veins Ø The transverse pericardial sinus is the space between the sleeve of pericardium enclosing the aorta and pulmonary trunk anteriorly and the sleeve surrounding the superior vena cava and the left pulmonary veins posteriorly. Ø The oblique pericardial sinus is an inverted U-shaped blind recess behind the left atrium and large veins and anterior to parietal pericardium Important to heart surgeons: a ligature can be put around the aorta and pulmonary trunk and tightened to halt circulation, allowing surgery to be performed on these vessels
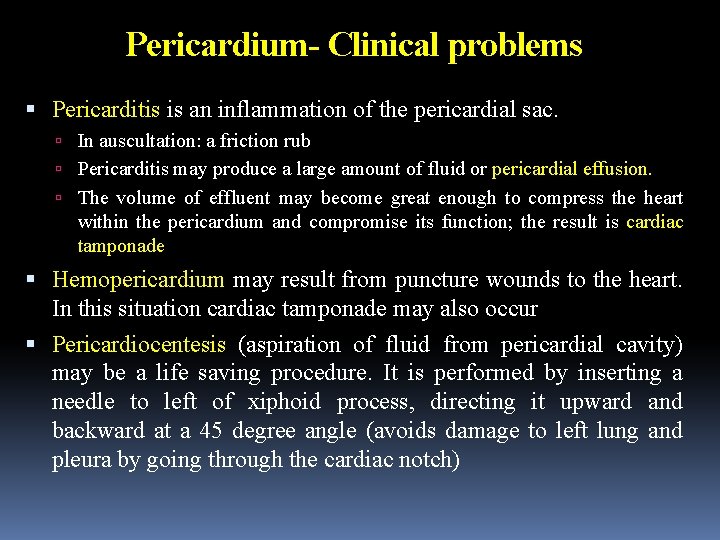
Pericardium- Clinical problems Pericarditis is an inflammation of the pericardial sac. In auscultation: a friction rub Pericarditis may produce a large amount of fluid or pericardial effusion. The volume of effluent may become great enough to compress the heart within the pericardium and compromise its function; the result is cardiac tamponade Hemopericardium may result from puncture wounds to the heart. In this situation cardiac tamponade may also occur Pericardiocentesis (aspiration of fluid from pericardial cavity) may be a life saving procedure. It is performed by inserting a needle to left of xiphoid process, directing it upward and backward at a 45 degree angle (avoids damage to left lung and pleura by going through the cardiac notch)

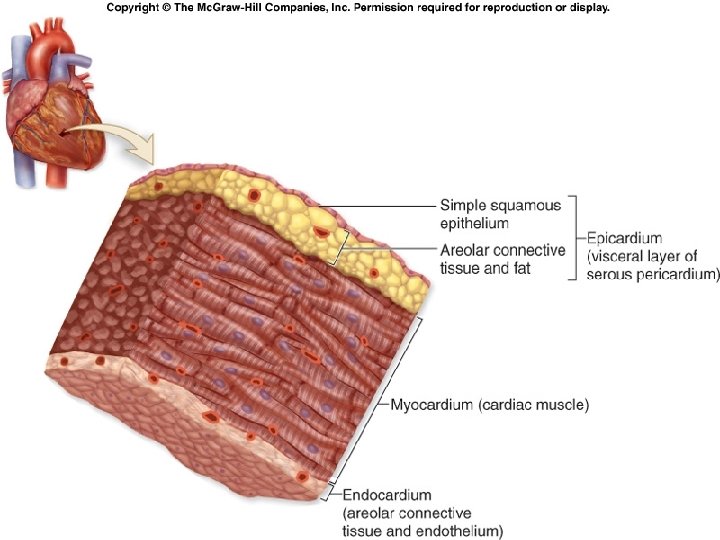
Heart Wall Structure Three distinctive layers: external epicardium middle myocardium internal endocardium Epicardium outermost heart layer also known as the visceral layer of serous pericardium. Simple squamous epithelium underlined by fat As we age, more fat is deposited in the epicardium this layer becomes thicker and more fatty.
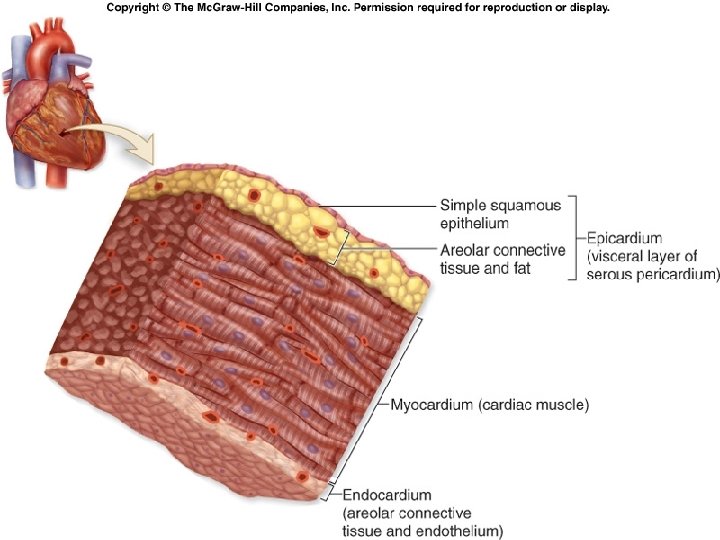
Heart Wall Structure Myocardium middle layer of the heart wall composed chiefly of cardiac muscle tissue. thickest of the three heart wall layers. lies deep to the epicardium and superficial to the endocardium Endocardium covers internal surface of the heart and the external surfaces of the heart valves thin endothelium areolar CT under the endothelium
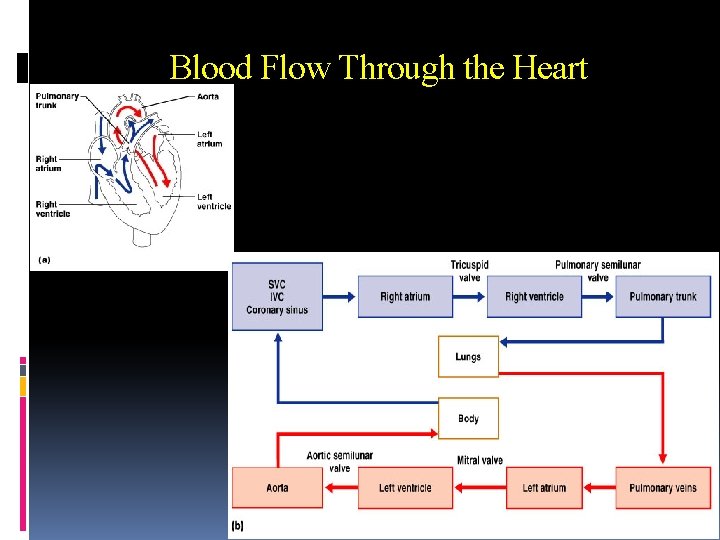
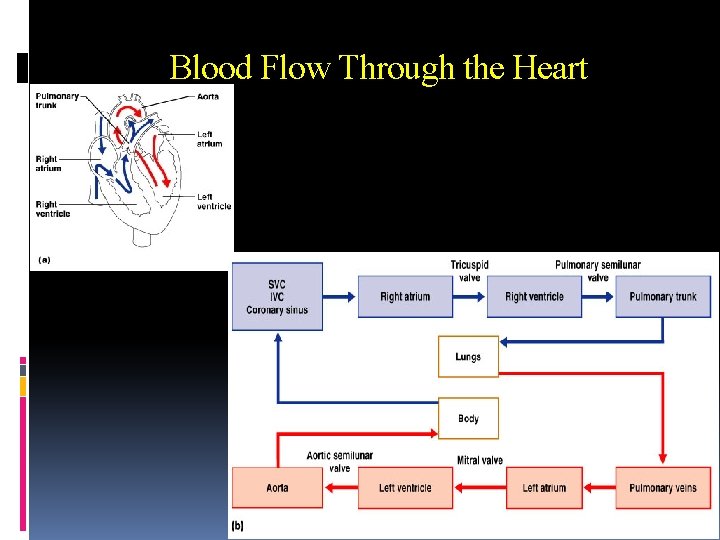
Blood Flow Through the Heart
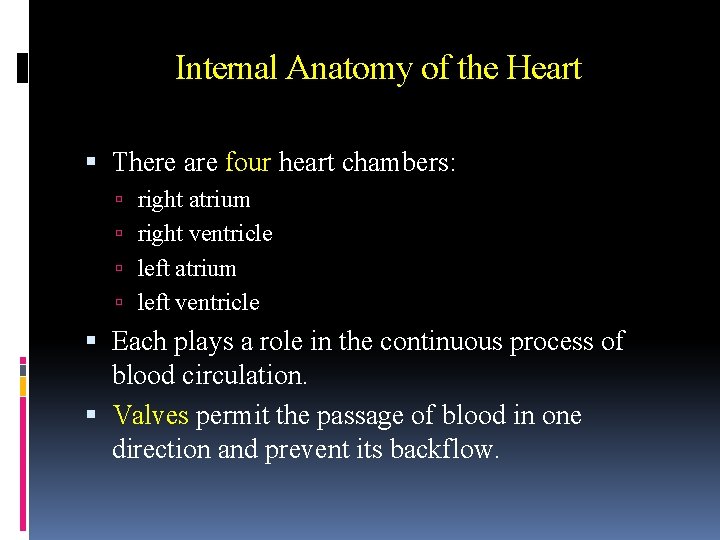
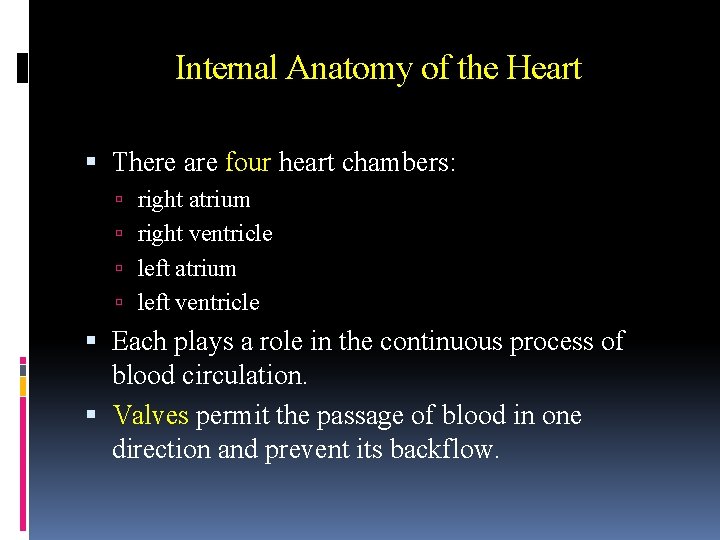
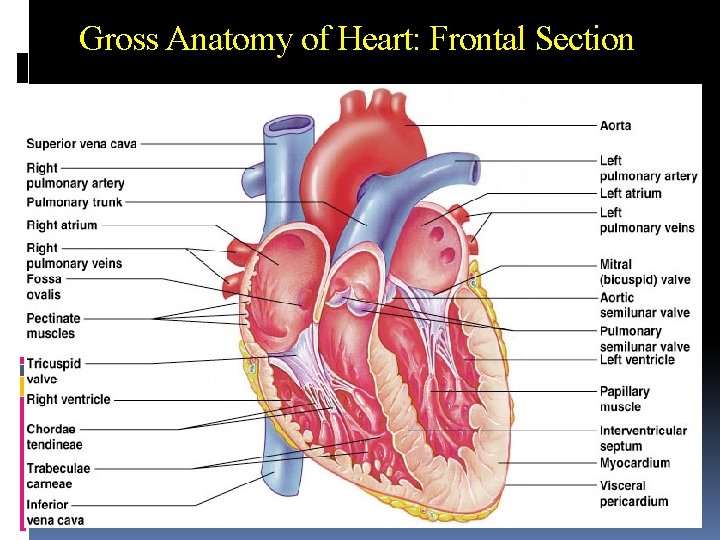
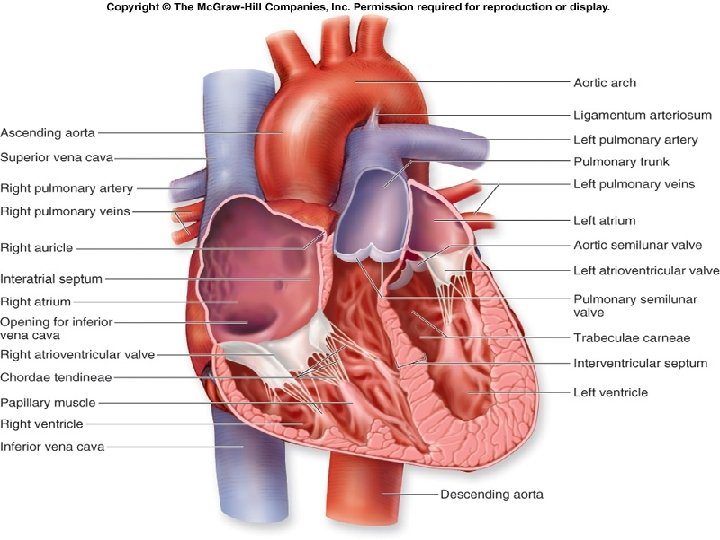
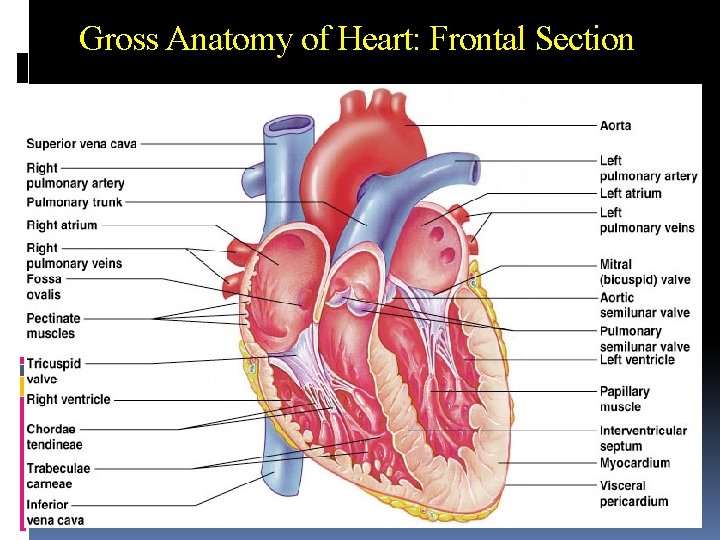
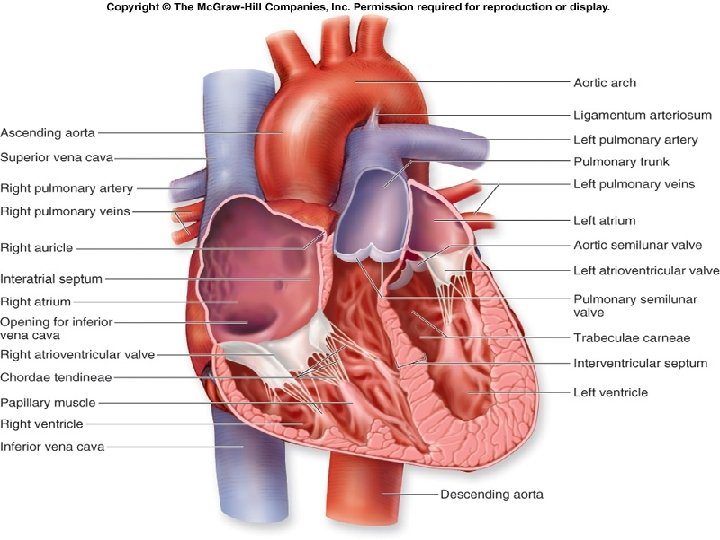
Internal Anatomy of the Heart There are four heart chambers: right atrium right ventricle left atrium left ventricle Each plays a role in the continuous process of blood circulation. Valves permit the passage of blood in one direction and prevent its backflow.
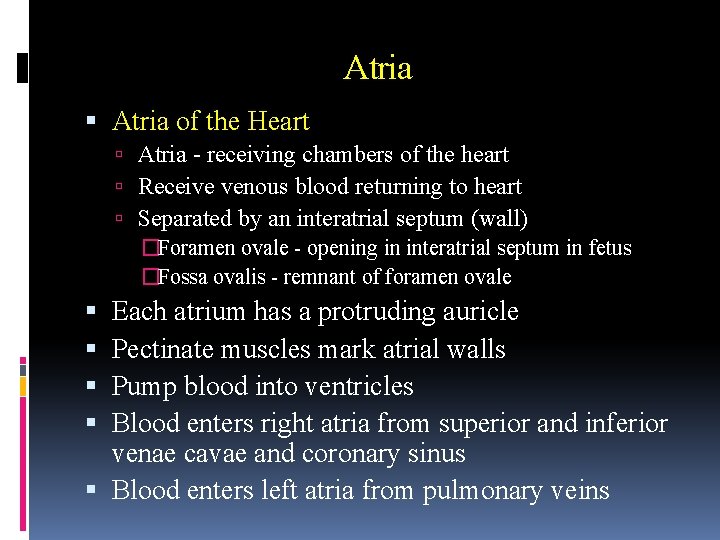
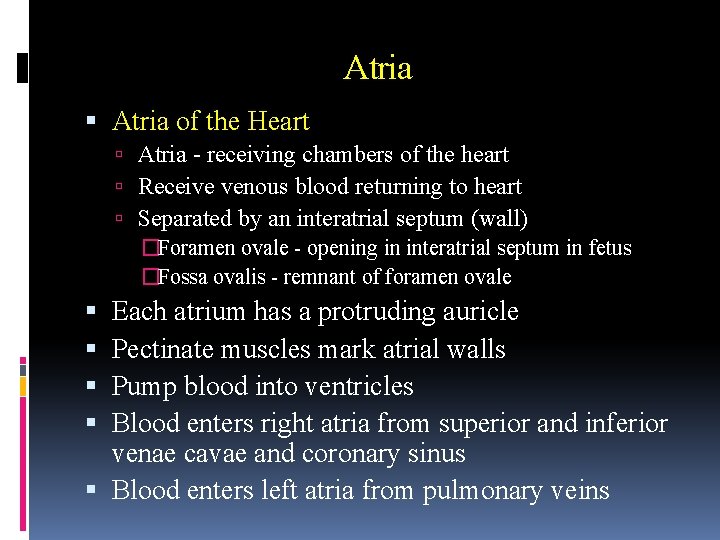
Atria of the Heart Atria - receiving chambers of the heart Receive venous blood returning to heart Separated by an interatrial septum (wall) �Foramen ovale - opening in interatrial septum in fetus �Fossa ovalis - remnant of foramen ovale Each atrium has a protruding auricle Pectinate muscles mark atrial walls Pump blood into ventricles Blood enters right atria from superior and inferior venae cavae and coronary sinus Blood enters left atria from pulmonary veins
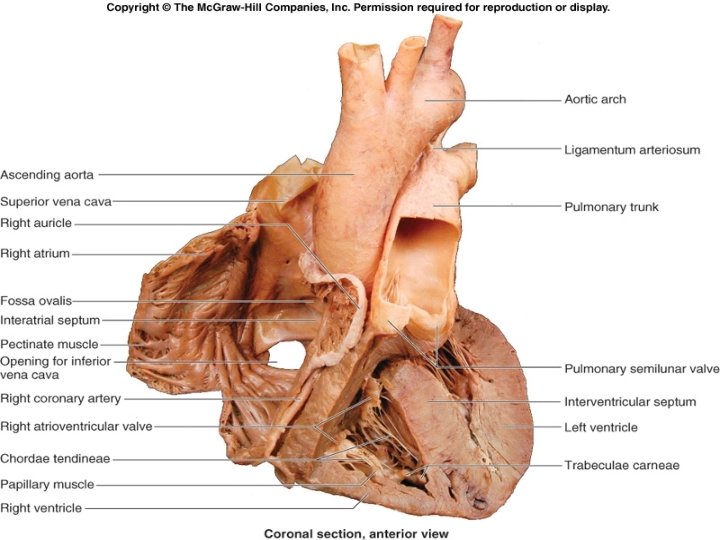
Gross Anatomy of Heart: Frontal Section
Ventricles are the discharging chambers of the heart Papillary muscles and trabeculae carneae muscles mark ventricular walls Separated by an interventricular septum Contains components of the conduction system Right ventricle pumps blood into the pulmonary trunk Left ventricle pumps blood into the aorta Thicker myocardium due to greater work load Pulmonary circulation supplied by right ventricle is a much low pressure system requiring less energy output by ventricle Systemic circulation supplied by left ventricle is a higher pressure system and thus requires more forceful contractions
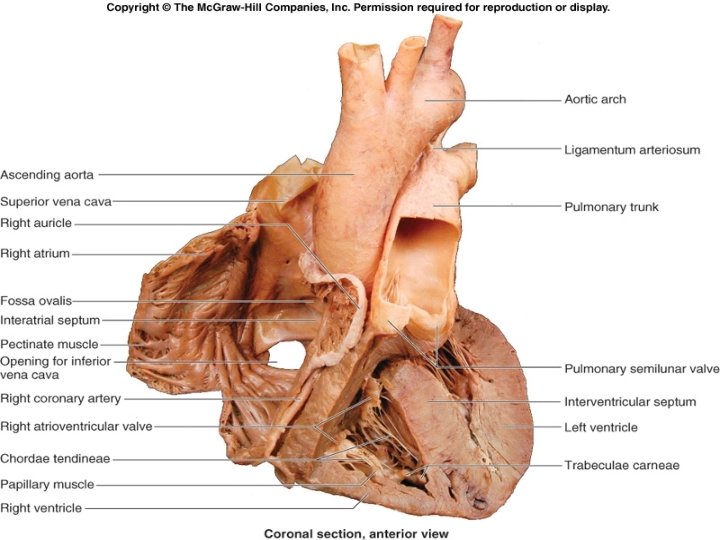
Right Atrium Consists of 2 parts. The anterior portion, including the auricle, contains pectinate muscles in its walls and contracts. The sinus venarum or smooth-walled portion, is derived from veins The boundary between the rough- and smoothwalled parts is the crista terminalis, a ridge extending between the openings of the venae cavae. The sinoatrial node is located beneath its superior part.
Right Atrium The interatrial septum forms a wall between the right and left atria. contains the opening of the coronary sinus and the remnant of the foramen ovale called the fossa ovalis Three major vessels empty into the right atrium: superior vena cava (SVC) �drains blood from the head, upper limbs, and superior regions of the trunk inferior vena cava (IVC) �drains blood from the lower limbs and trunk coronary sinus drains blood from the heart wall
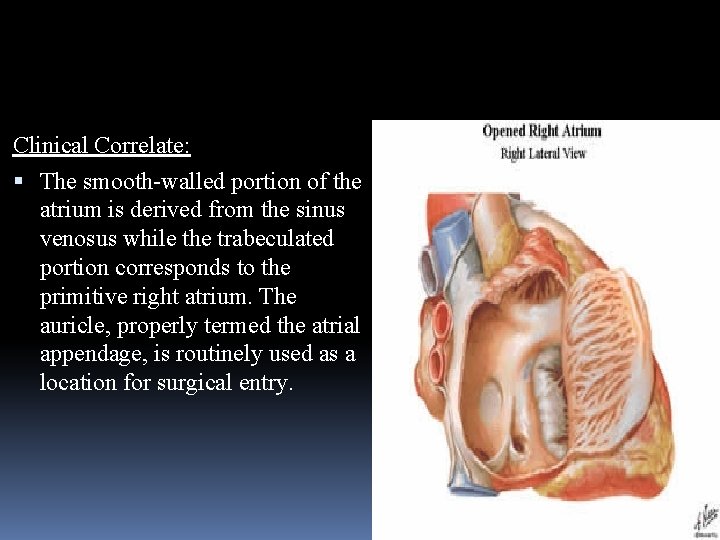
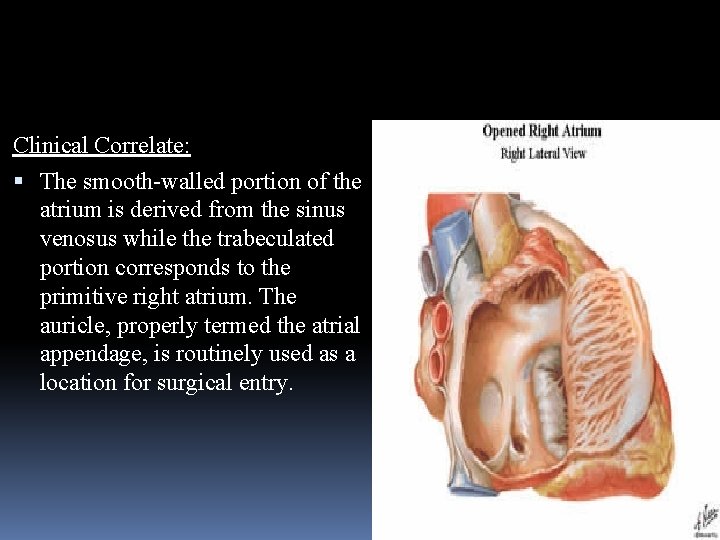
Clinical Correlate: The smooth-walled portion of the atrium is derived from the sinus venosus while the trabeculated portion corresponds to the primitive right atrium. The auricle, properly termed the atrial appendage, is routinely used as a location for surgical entry.
Right Ventricle Receives deoxygenated venous blood from the right atrium. Divided into: the muscular, inflow portion the smooth, outflow portion consisting of the infundibulum and the pulmonary trunk. The right ventricle has a thinner wall than the left, and it is C-shaped in cross-section An interventricular septum forms a wall between the right and left ventricles.
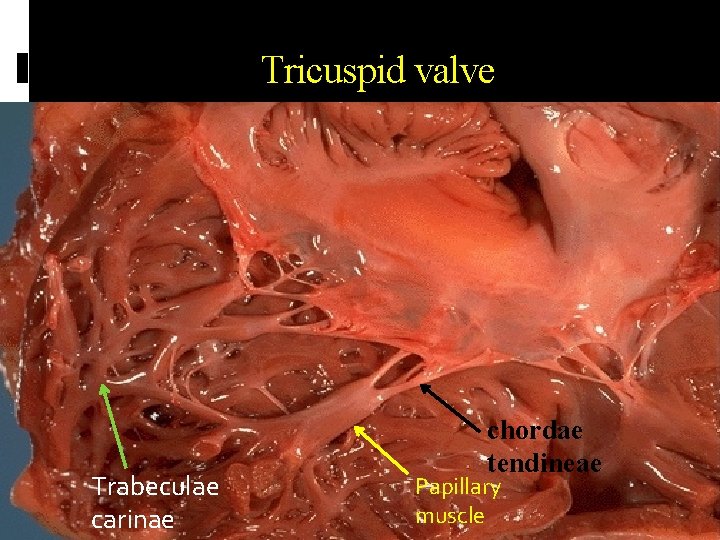
Right Ventricle The walls of the right ventricle are covered with muscles, the trabeculae carneae. One of these, the septomarginal trabeculum (moderator band), contains branches of the right AV bundle Three papillary muscles arise from the internal walls of the right ventricle as cone –shaped muscular projection and each muscle is attached to the cusps of the AV valve via the chordae tendinae which prevent everting and flipping into the atrium when contracting A large ridge, the crista supraventricularis, lies between the inflow and outflow tracts At its superior end it narrows into a smooth-walled, conical region called the conus arteriosus.
Left Atrium Once gas exchange occurs in the lungs, the oxygenated blood travels through the pulmonary veins to the left atrium. Smooth posterior wall of the left atrium contains openings for approximately four pulmonary veins. two left pulmonary veins two right pulmonary veins Has pectinate muscles along its anterior wall as well as an auricle.
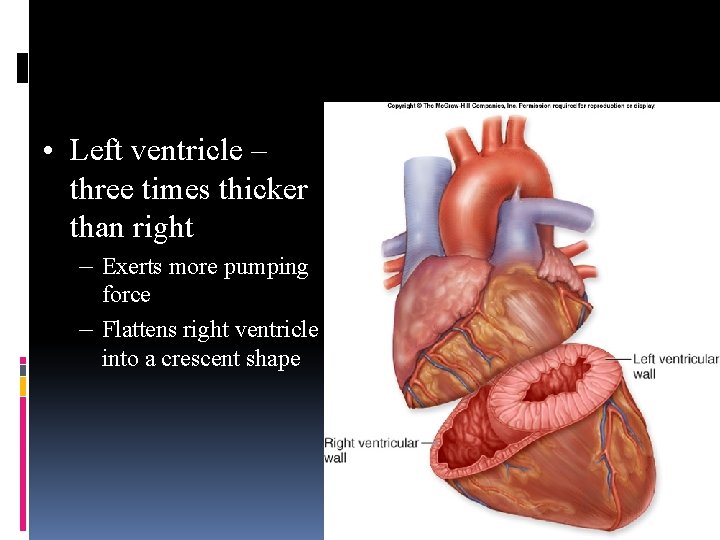
Left Ventricle Largest of the four heart chambers. It consists of: A muscular inflow portion A smooth-walled outflow portion, the aortic vestibule and the ascending aorta Muscular part of the wall is typically: Three times thicker than the right ventricular wall. is round in cross-section Requires thick walls in order to generate enough pressure to force the oxygenated blood from the lungs into the aorta and then through the entire systemic circuit. right ventricle only has to pump blood to the nearby lungs
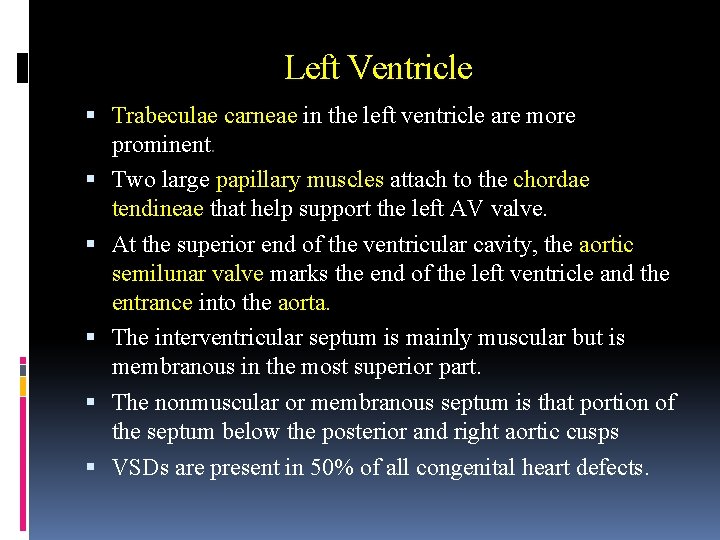
Left Ventricle Trabeculae carneae in the left ventricle are more prominent. Two large papillary muscles attach to the chordae tendineae that help support the left AV valve. At the superior end of the ventricular cavity, the aortic semilunar valve marks the end of the left ventricle and the entrance into the aorta. The interventricular septum is mainly muscular but is membranous in the most superior part. The nonmuscular or membranous septum is that portion of the septum below the posterior and right aortic cusps VSDs are present in 50% of all congenital heart defects.
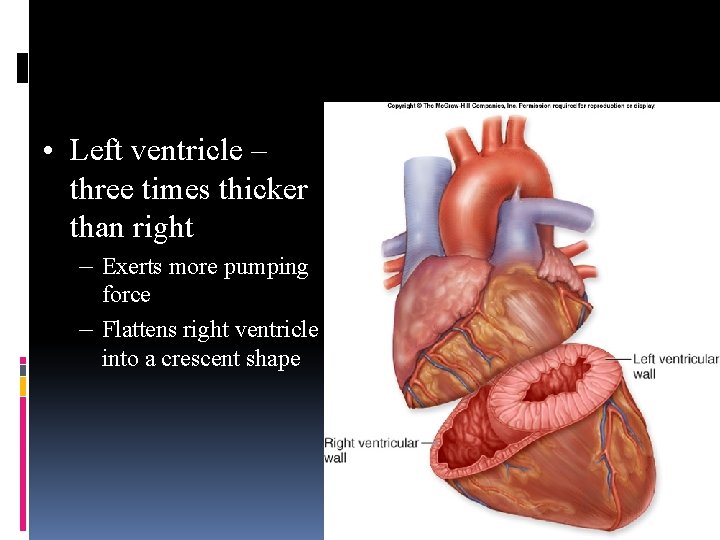
• Left ventricle – three times thicker than right – Exerts more pumping force – Flattens right ventricle into a crescent shape
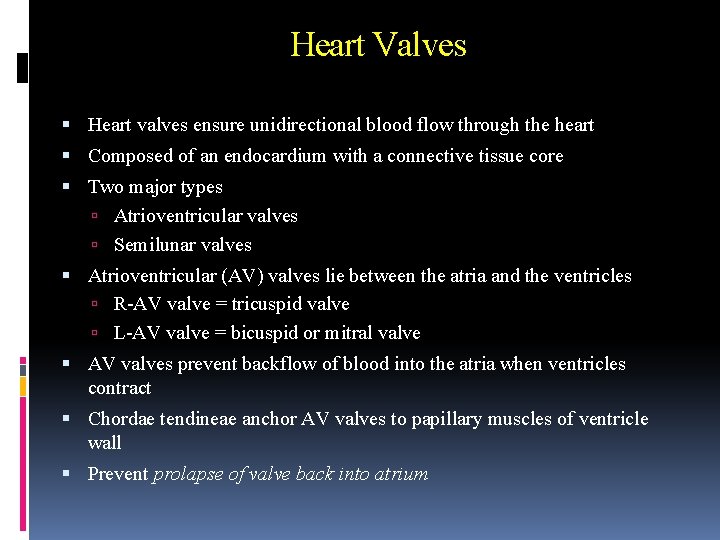
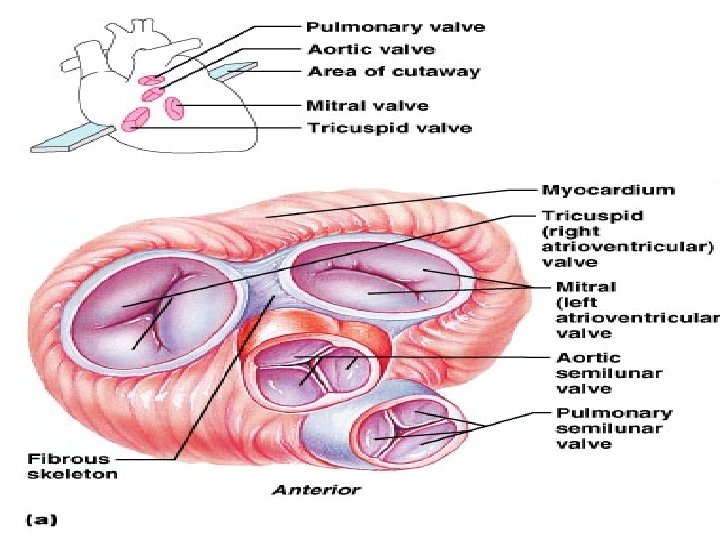
Heart Valves Heart valves ensure unidirectional blood flow through the heart Composed of an endocardium with a connective tissue core Two major types Atrioventricular valves Semilunar valves Atrioventricular (AV) valves lie between the atria and the ventricles R-AV valve = tricuspid valve L-AV valve = bicuspid or mitral valve AV valves prevent backflow of blood into the atria when ventricles contract Chordae tendineae anchor AV valves to papillary muscles of ventricle wall Prevent prolapse of valve back into atrium
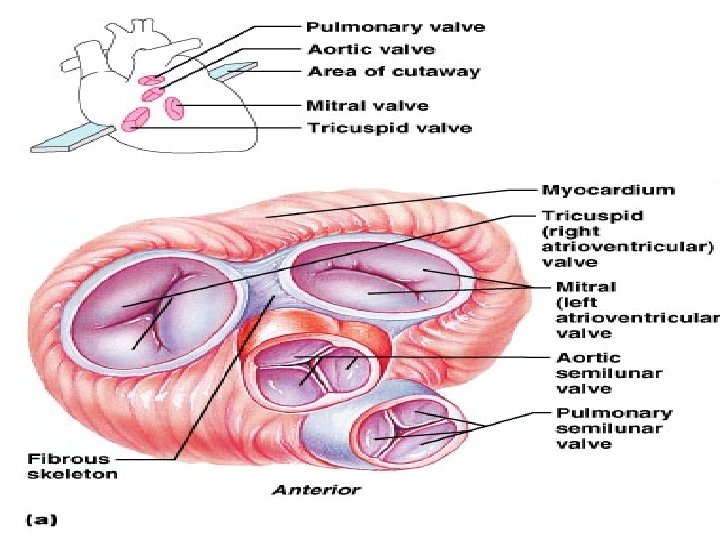
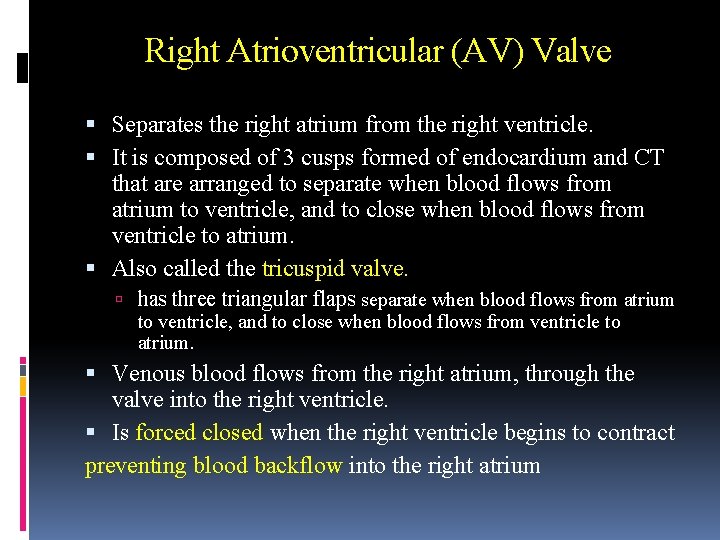
Right Atrioventricular (AV) Valve Separates the right atrium from the right ventricle. It is composed of 3 cusps formed of endocardium and CT that are arranged to separate when blood flows from atrium to ventricle, and to close when blood flows from ventricle to atrium. Also called the tricuspid valve. has three triangular flaps separate when blood flows from atrium to ventricle, and to close when blood flows from ventricle to atrium. Venous blood flows from the right atrium, through the valve into the right ventricle. Is forced closed when the right ventricle begins to contract preventing blood backflow into the right atrium
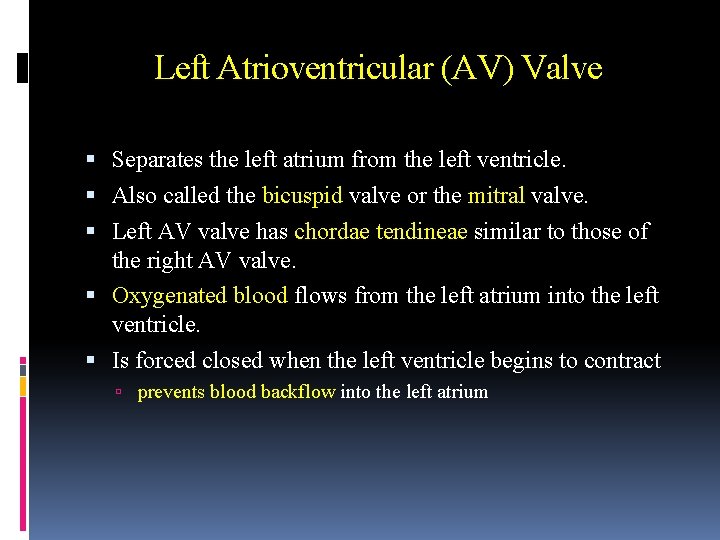
Left Atrioventricular (AV) Valve Separates the left atrium from the left ventricle. Also called the bicuspid valve or the mitral valve. Left AV valve has chordae tendineae similar to those of the right AV valve. Oxygenated blood flows from the left atrium into the left ventricle. Is forced closed when the left ventricle begins to contract prevents blood backflow into the left atrium
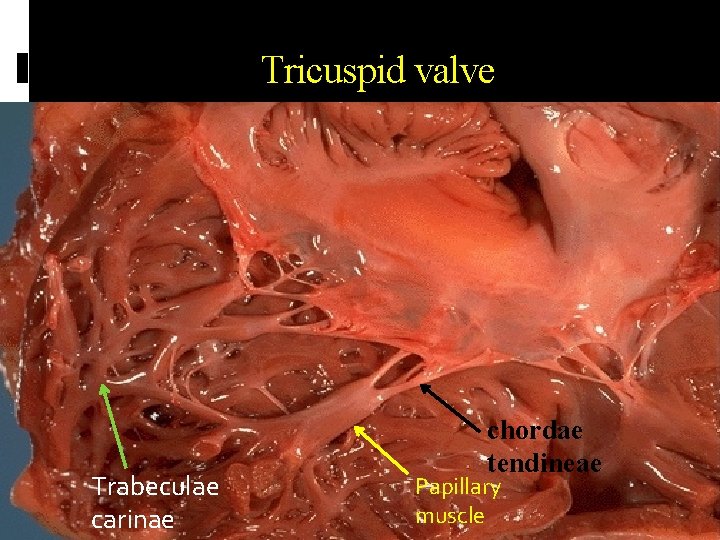
Tricuspid valve Trabeculae carinae chordae tendineae Papillary muscle
Clinical Valvular incompetence from a variety of sources results in a regurgitation or backwards flow of blood: This produces a murmur upon auscultation. Valvular stenosis, a narrowing process, may result from a fusion of valve leaflets or cusps. Atrial enlargement may accompany stenosis or regurgitation
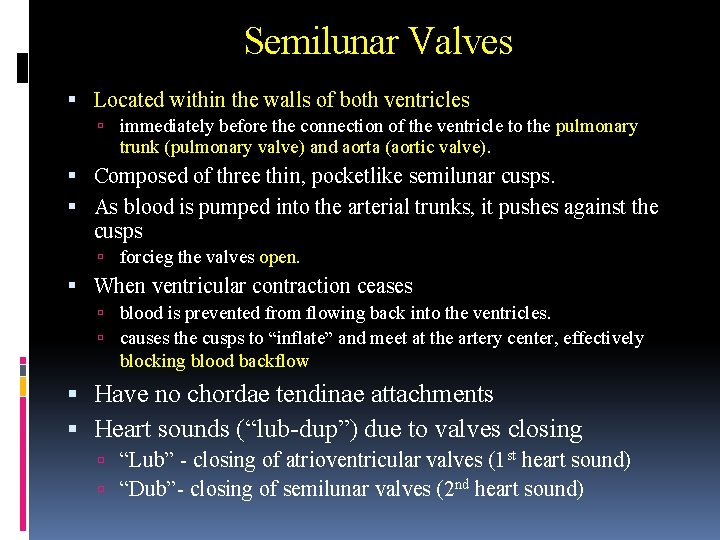
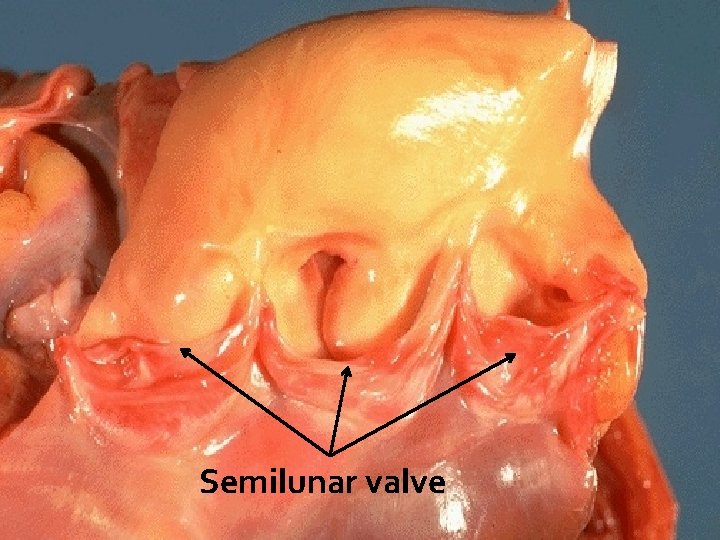
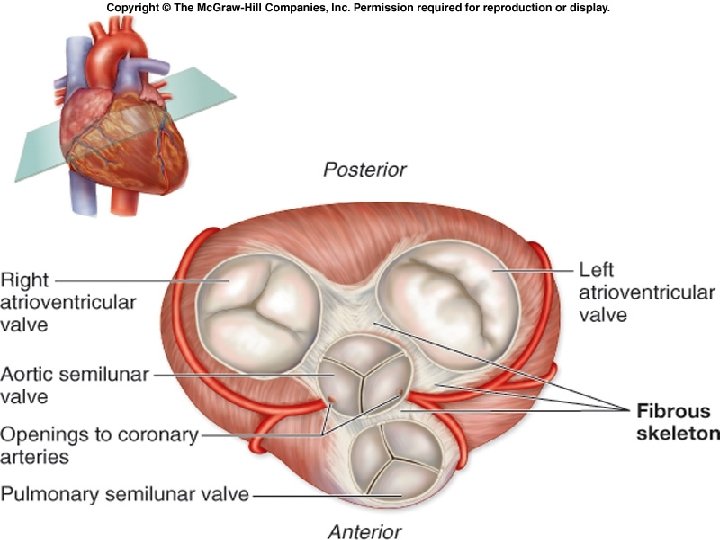
Semilunar Valves Located within the walls of both ventricles immediately before the connection of the ventricle to the pulmonary trunk (pulmonary valve) and aorta (aortic valve). Composed of three thin, pocketlike semilunar cusps. As blood is pumped into the arterial trunks, it pushes against the cusps forcieg the valves open. When ventricular contraction ceases blood is prevented from flowing back into the ventricles. causes the cusps to “inflate” and meet at the artery center, effectively blocking blood backflow Have no chordae tendinae attachments Heart sounds (“lub-dup”) due to valves closing “Lub” - closing of atrioventricular valves (1 st heart sound) “Dub”- closing of semilunar valves (2 nd heart sound)
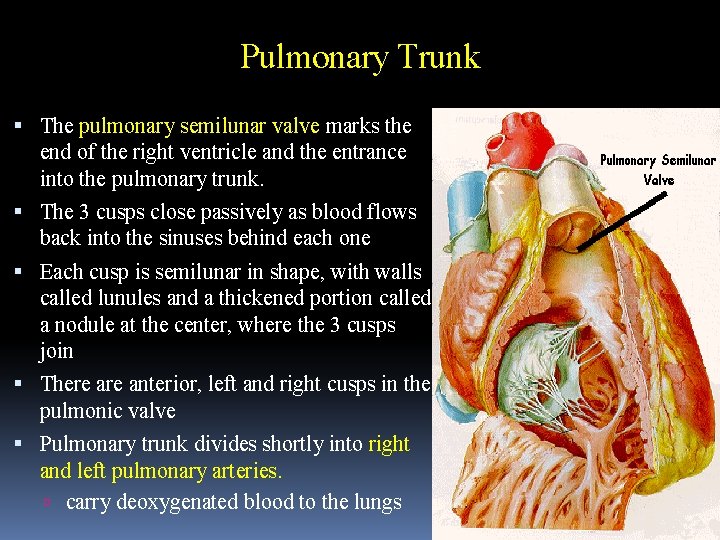
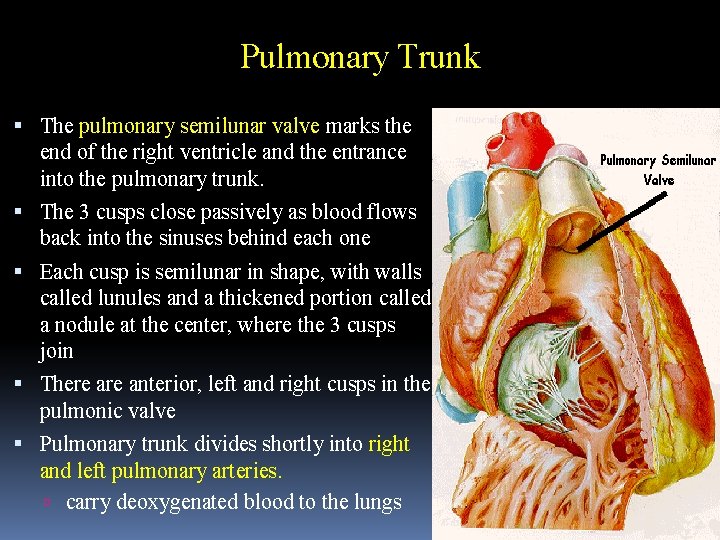
Pulmonary Trunk The pulmonary semilunar valve marks the end of the right ventricle and the entrance into the pulmonary trunk. The 3 cusps close passively as blood flows back into the sinuses behind each one Each cusp is semilunar in shape, with walls called lunules and a thickened portion called a nodule at the center, where the 3 cusps join There anterior, left and right cusps in the pulmonic valve Pulmonary trunk divides shortly into right and left pulmonary arteries. carry deoxygenated blood to the lungs
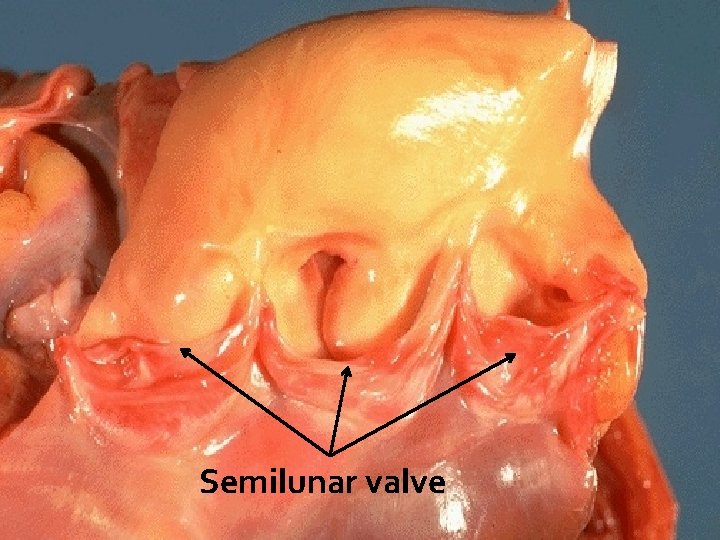
Semilunar valve
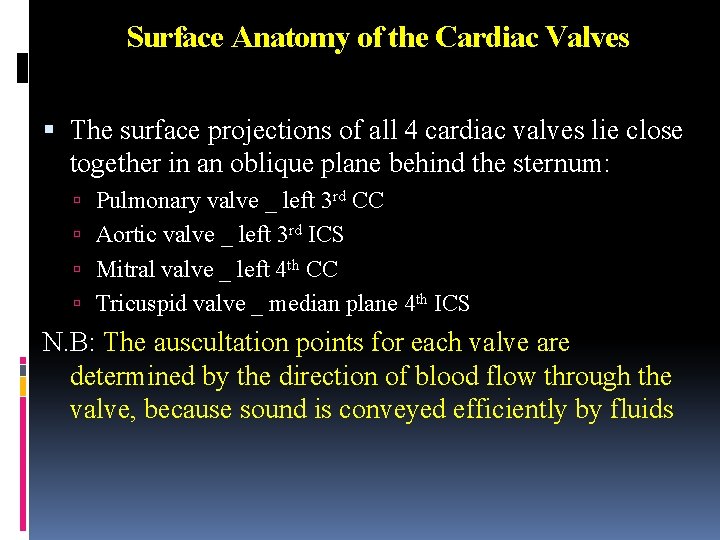
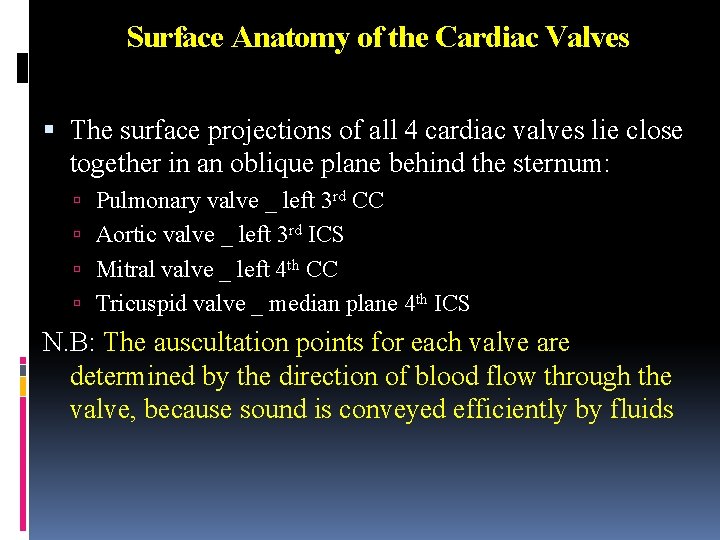
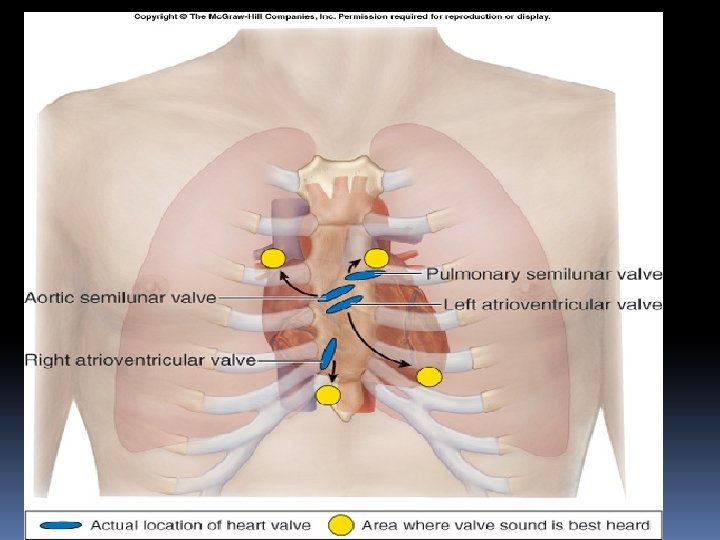
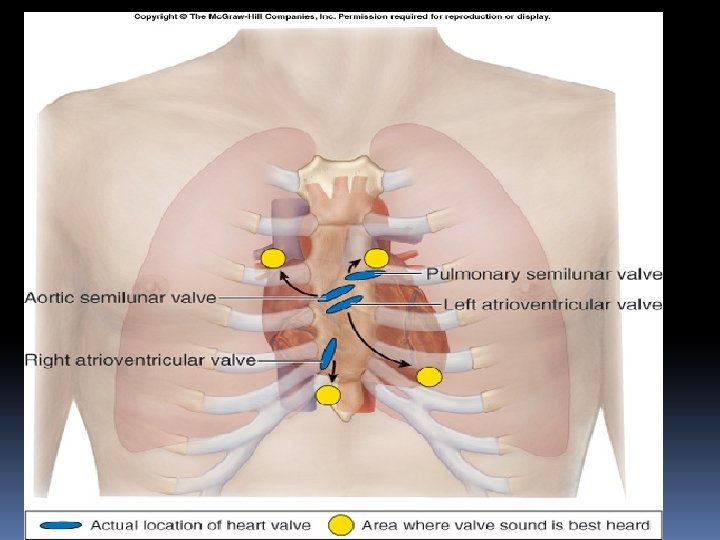
Surface Anatomy of the Cardiac Valves The surface projections of all 4 cardiac valves lie close together in an oblique plane behind the sternum: Pulmonary valve _ left 3 rd CC Aortic valve _ left 3 rd ICS Mitral valve _ left 4 th CC Tricuspid valve _ median plane 4 th ICS N. B: The auscultation points for each valve are determined by the direction of blood flow through the valve, because sound is conveyed efficiently by fluids
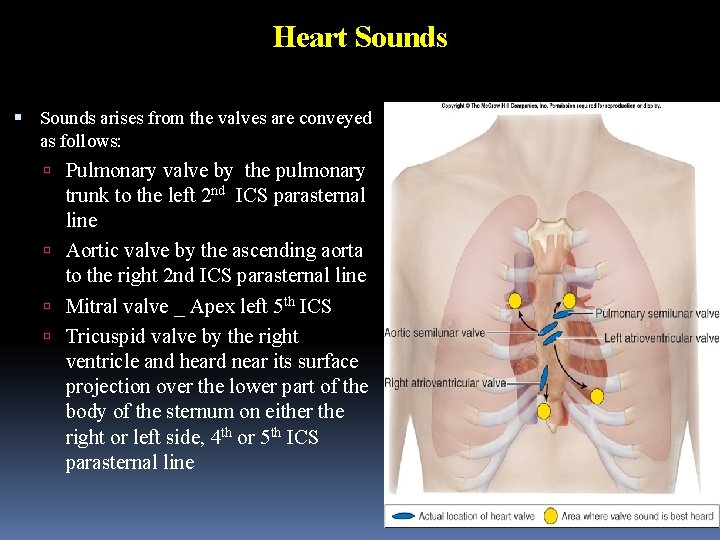
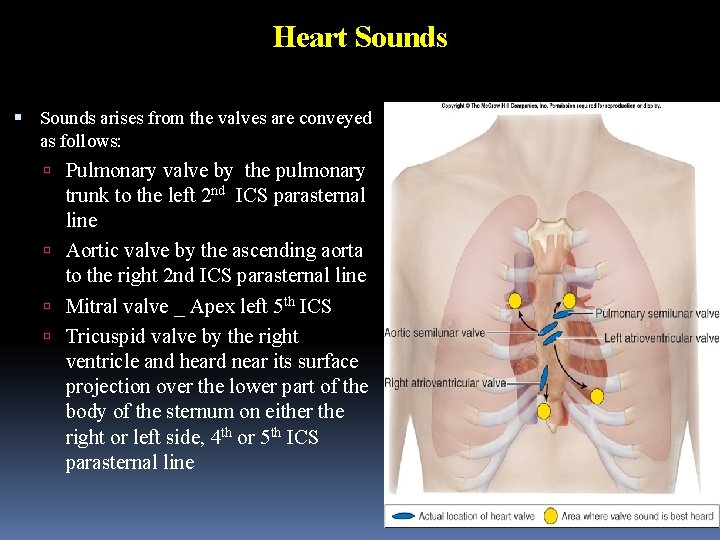
Heart Sounds arises from the valves are conveyed as follows: Pulmonary valve by the pulmonary trunk to the left 2 nd ICS parasternal line Aortic valve by the ascending aorta to the right 2 nd ICS parasternal line Mitral valve _ Apex left 5 th ICS Tricuspid valve by the right ventricle and heard near its surface projection over the lower part of the body of the sternum on either the right or left side, 4 th or 5 th ICS parasternal line
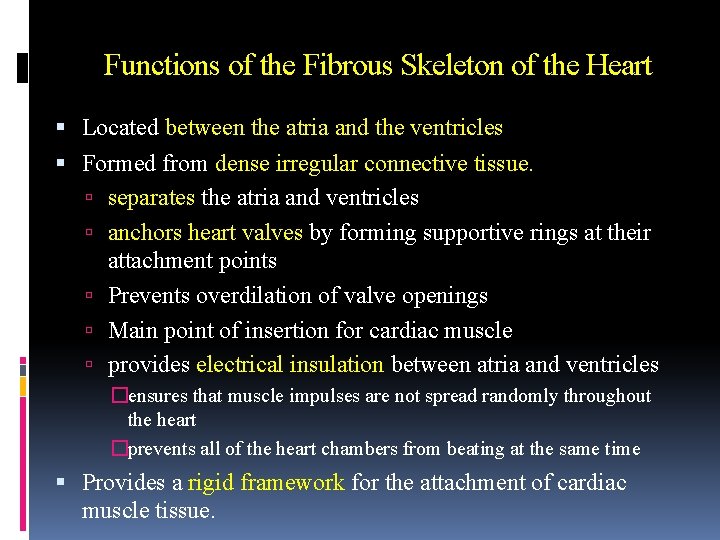
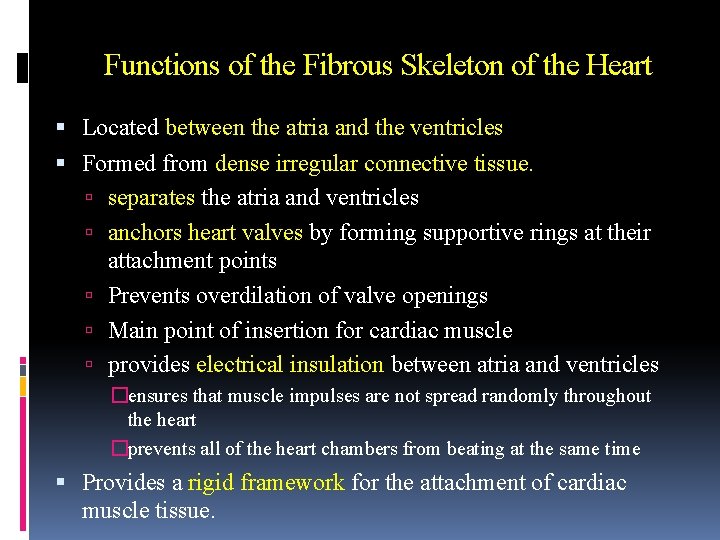
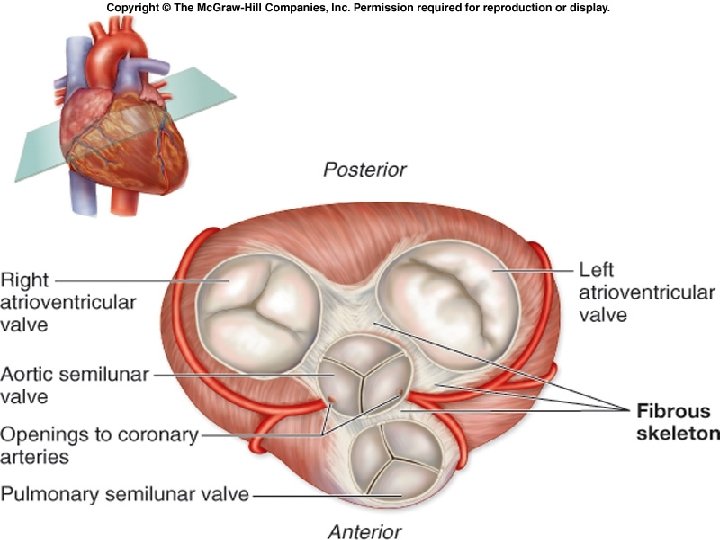
Functions of the Fibrous Skeleton of the Heart Located between the atria and the ventricles Formed from dense irregular connective tissue. separates the atria and ventricles anchors heart valves by forming supportive rings at their attachment points Prevents overdilation of valve openings Main point of insertion for cardiac muscle provides electrical insulation between atria and ventricles �ensures that muscle impulses are not spread randomly throughout the heart �prevents all of the heart chambers from beating at the same time Provides a rigid framework for the attachment of cardiac muscle tissue.
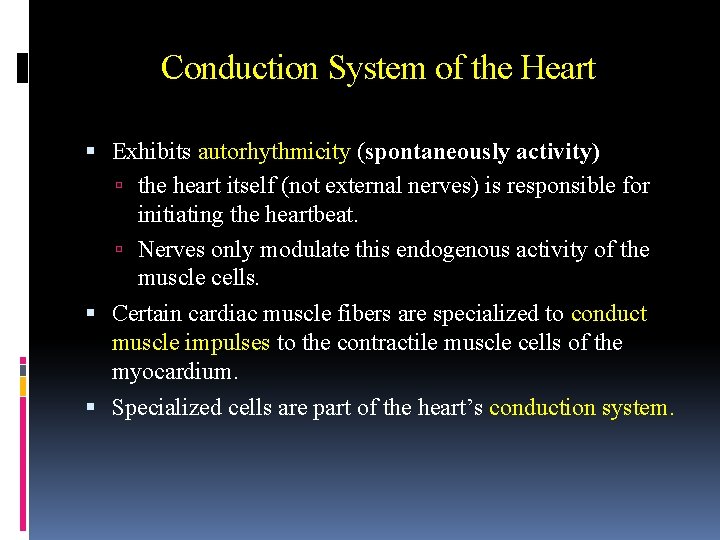
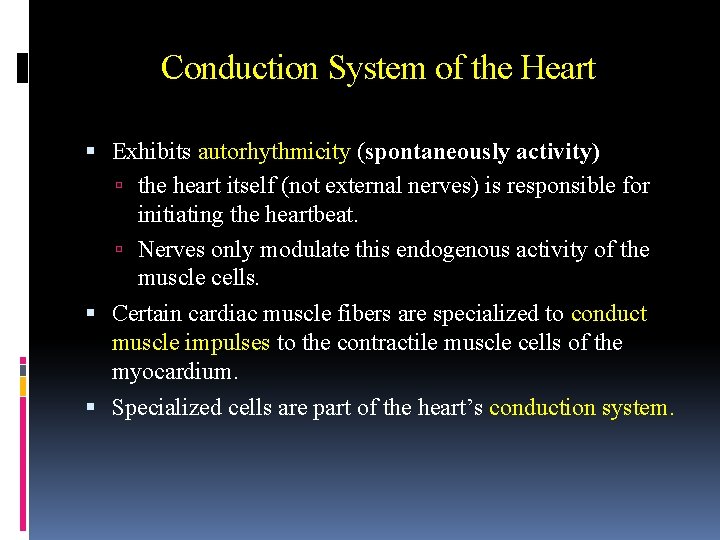
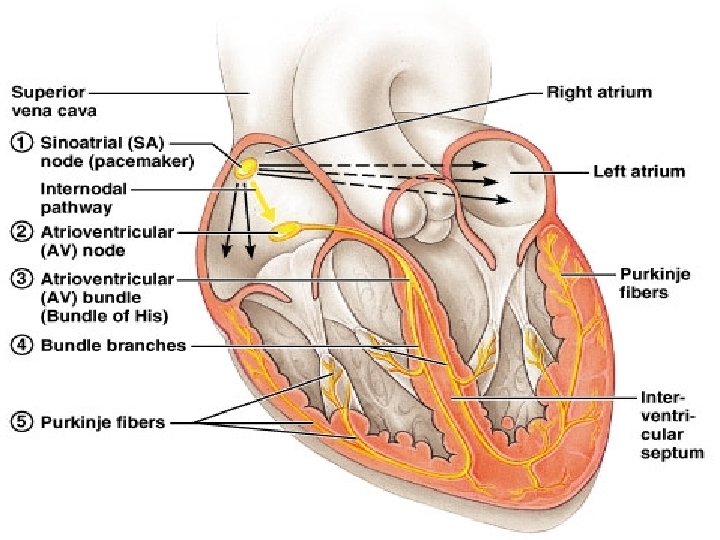
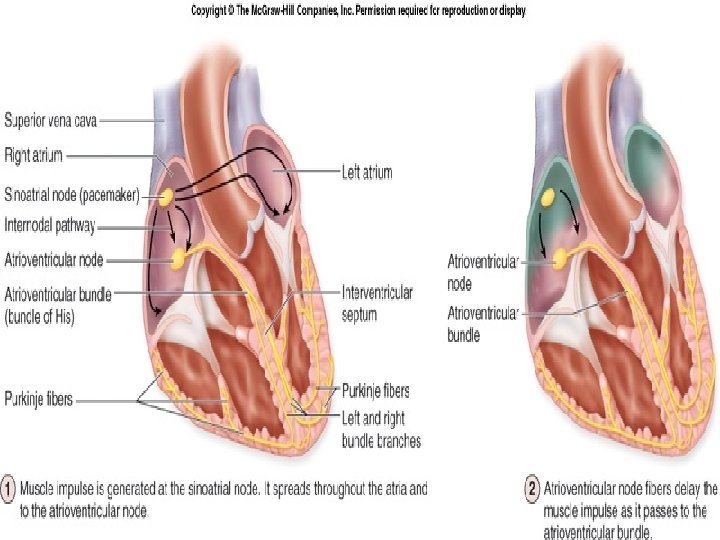
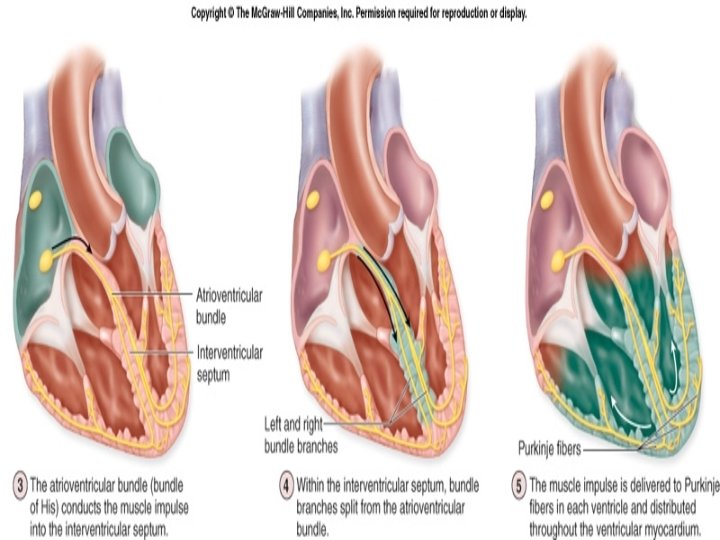
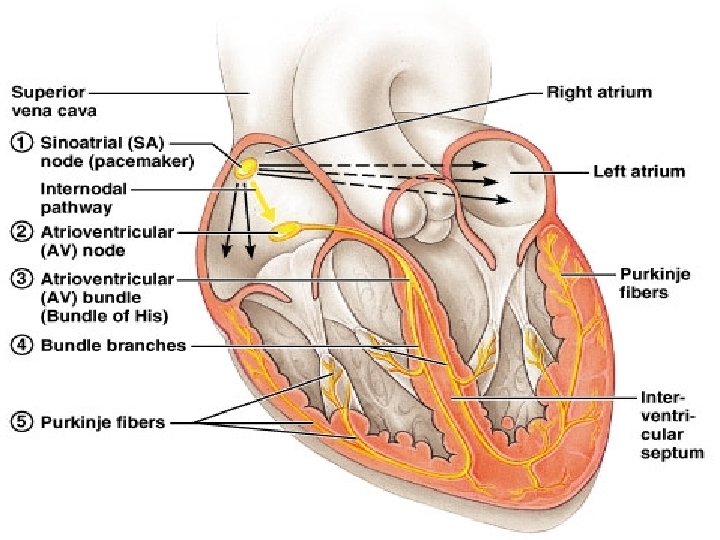
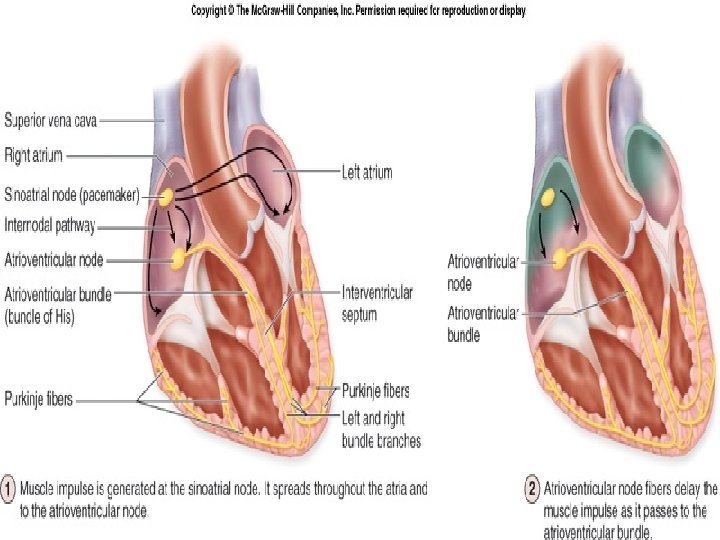
Conduction System of the Heart Exhibits autorhythmicity (spontaneously activity) the heart itself (not external nerves) is responsible for initiating the heartbeat. Nerves only modulate this endogenous activity of the muscle cells. Certain cardiac muscle fibers are specialized to conduct muscle impulses to the contractile muscle cells of the myocardium. Specialized cells are part of the heart’s conduction system.
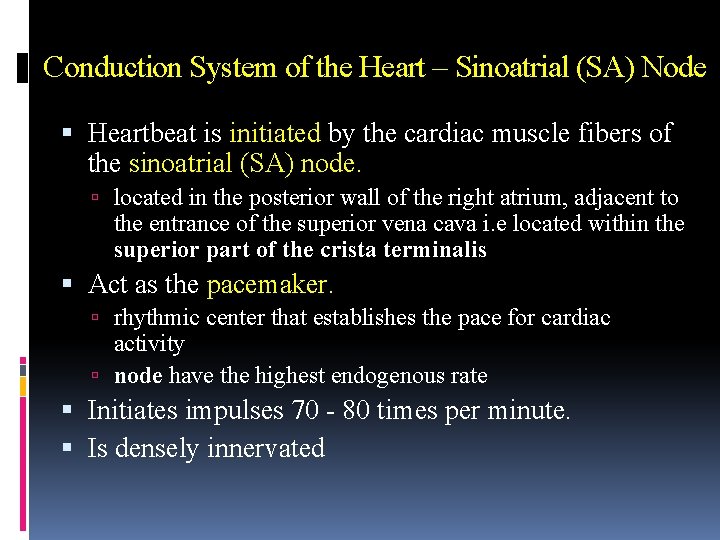
Conduction System of the Heart – Sinoatrial (SA) Node Heartbeat is initiated by the cardiac muscle fibers of the sinoatrial (SA) node. located in the posterior wall of the right atrium, adjacent to the entrance of the superior vena cava i. e located within the superior part of the crista terminalis Act as the pacemaker. rhythmic center that establishes the pace for cardiac activity node have the highest endogenous rate Initiates impulses 70 - 80 times per minute. Is densely innervated
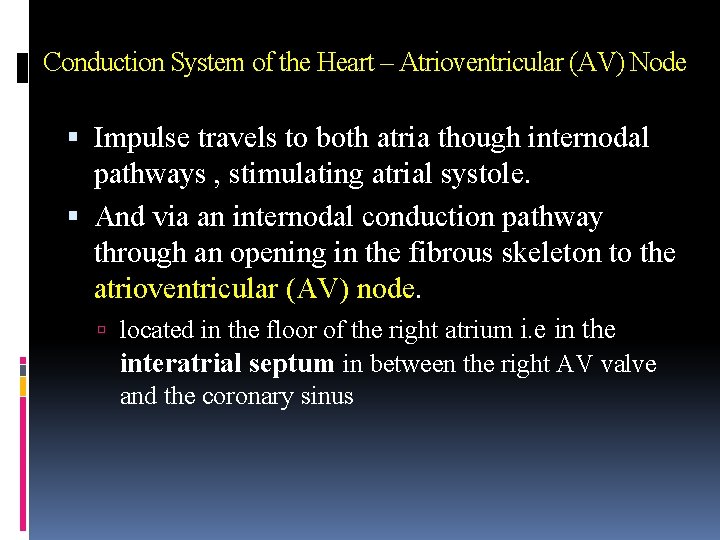
Conduction System of the Heart – Atrioventricular (AV) Node Impulse travels to both atria though internodal pathways , stimulating atrial systole. And via an internodal conduction pathway through an opening in the fibrous skeleton to the atrioventricular (AV) node. located in the floor of the right atrium i. e in the interatrial septum in between the right AV valve and the coronary sinus
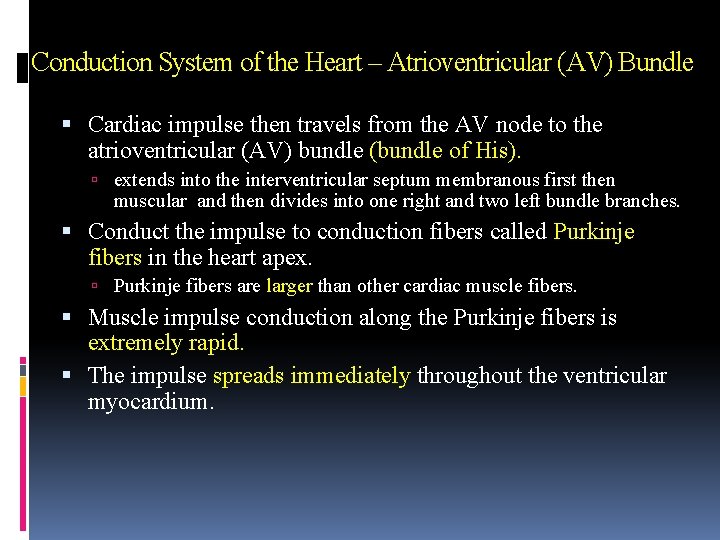
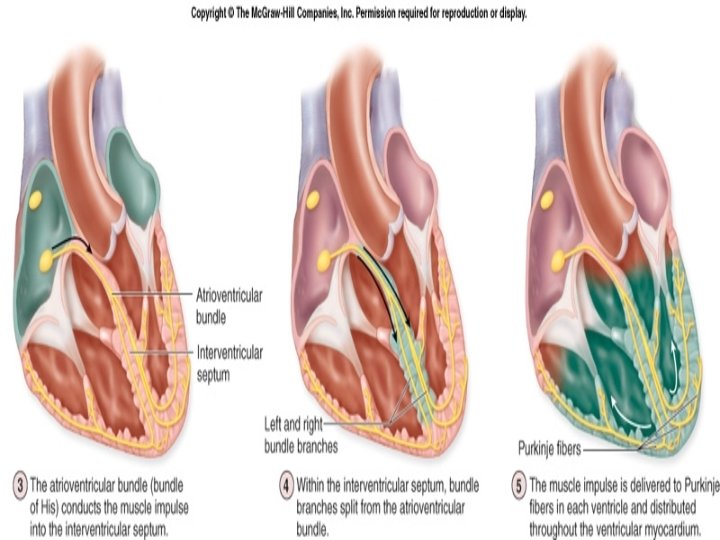
Conduction System of the Heart – Atrioventricular (AV) Bundle Cardiac impulse then travels from the AV node to the atrioventricular (AV) bundle (bundle of His). extends into the interventricular septum membranous first then muscular and then divides into one right and two left bundle branches. Conduct the impulse to conduction fibers called Purkinje fibers in the heart apex. Purkinje fibers are larger than other cardiac muscle fibers. Muscle impulse conduction along the Purkinje fibers is extremely rapid. The impulse spreads immediately throughout the ventricular myocardium.
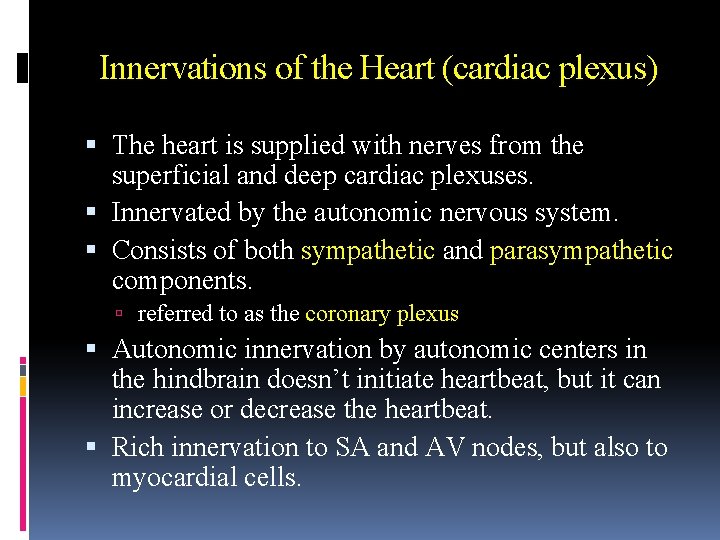
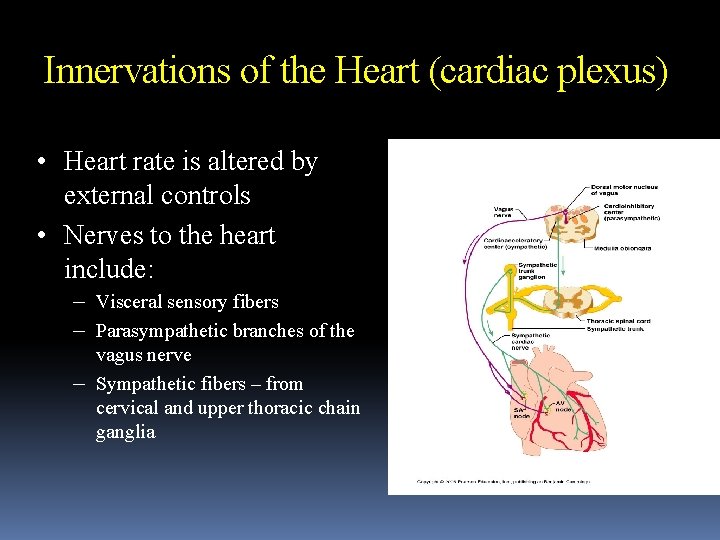
Innervations of the Heart (cardiac plexus) The heart is supplied with nerves from the superficial and deep cardiac plexuses. Innervated by the autonomic nervous system. Consists of both sympathetic and parasympathetic components. referred to as the coronary plexus Autonomic innervation by autonomic centers in the hindbrain doesn’t initiate heartbeat, but it can increase or decrease the heartbeat. Rich innervation to SA and AV nodes, but also to myocardial cells.
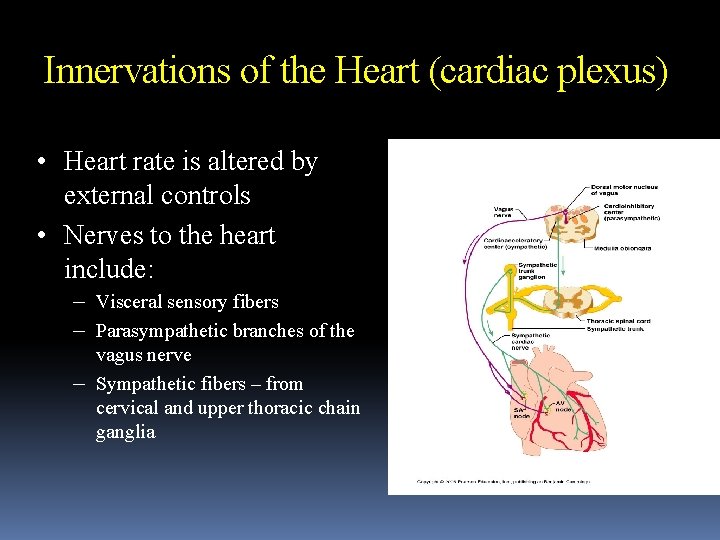
Innervations of the Heart (cardiac plexus) • Heart rate is altered by external controls • Nerves to the heart include: – Visceral sensory fibers – Parasympathetic branches of the – vagus nerve Sympathetic fibers – from cervical and upper thoracic chain ganglia
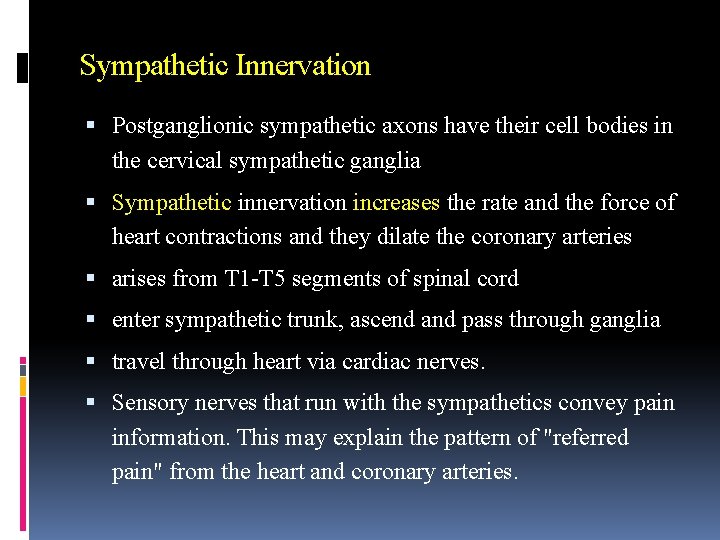
Sympathetic Innervation Postganglionic sympathetic axons have their cell bodies in the cervical sympathetic ganglia Sympathetic innervation increases the rate and the force of heart contractions and they dilate the coronary arteries arises from T 1 -T 5 segments of spinal cord enter sympathetic trunk, ascend and pass through ganglia travel through heart via cardiac nerves. Sensory nerves that run with the sympathetics convey pain information. This may explain the pattern of "referred pain" from the heart and coronary arteries.
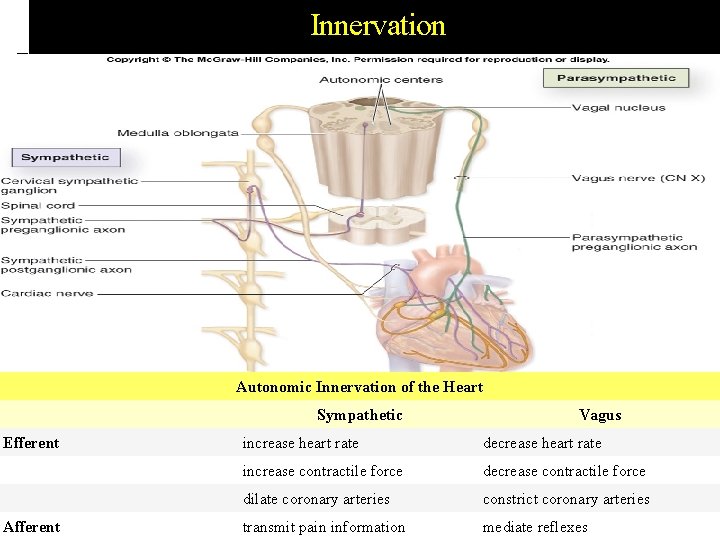
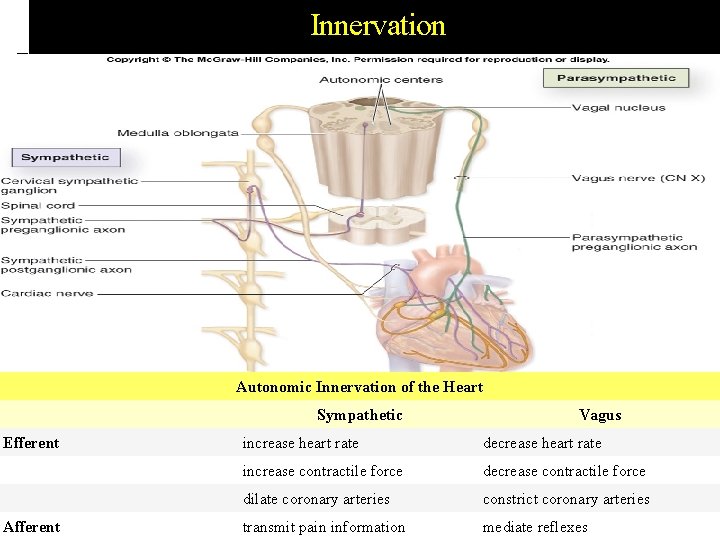
Innervation Autonomic Innervation of the Heart Efferent Afferent Sympathetic Vagus increase heart rate decrease heart rate increase contractile force decrease contractile force dilate coronary arteries constrict coronary arteries transmit pain information mediate reflexes
Parasympathetic Innervation Parasympathetic innervation decreases heart rate, but tends to have no effect on the force of contractions, except in special circumstances. And constrict the coronary arteries. comes off of the medulla oblongata via right and left vagus nerves (CN X) Sensory nerves that run with the parasympathetic convey information needed for reflexes
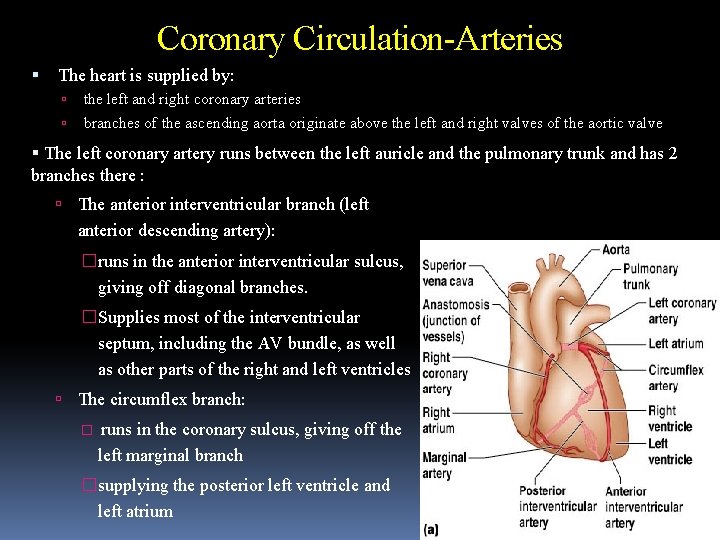
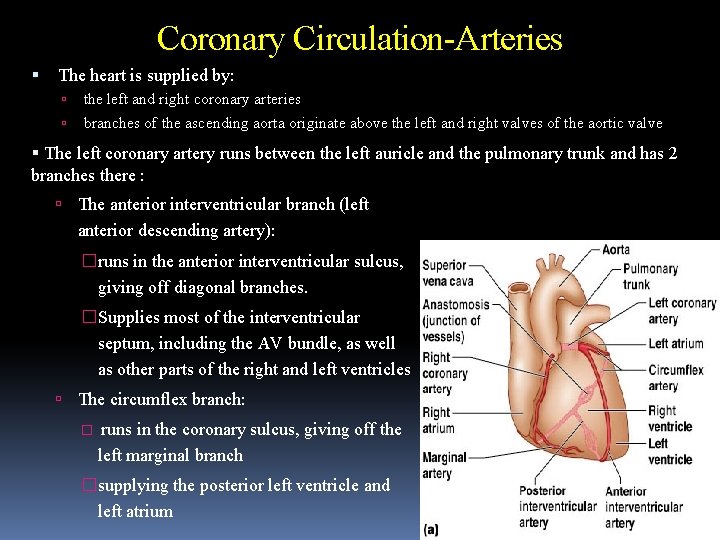
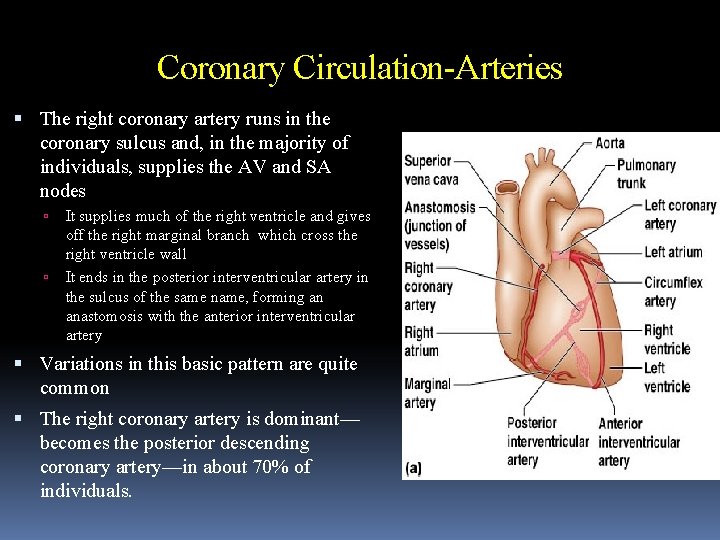
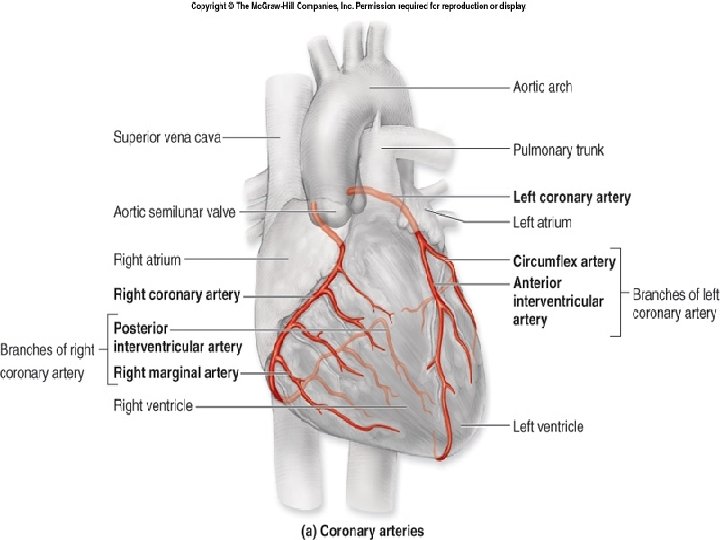
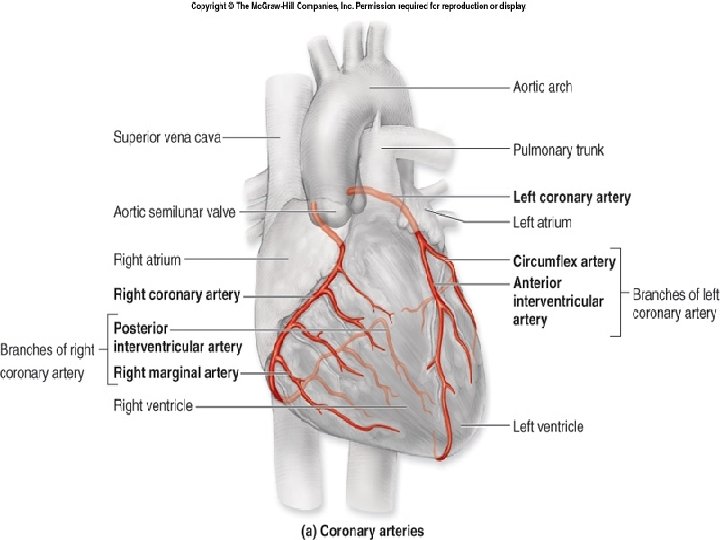
Coronary Circulation-Arteries The heart is supplied by: the left and right coronary arteries branches of the ascending aorta originate above the left and right valves of the aortic valve The left coronary artery runs between the left auricle and the pulmonary trunk and has 2 branches there : The anterior interventricular branch (left anterior descending artery): �runs in the anterior interventricular sulcus, giving off diagonal branches. �Supplies most of the interventricular septum, including the AV bundle, as well as other parts of the right and left ventricles The circumflex branch: � runs in the coronary sulcus, giving off the left marginal branch �supplying the posterior left ventricle and left atrium
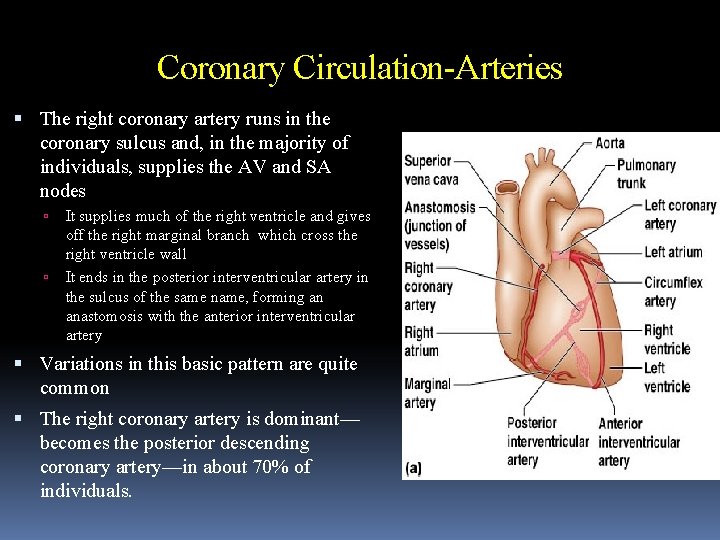
Coronary Circulation-Arteries The right coronary artery runs in the coronary sulcus and, in the majority of individuals, supplies the AV and SA nodes It supplies much of the right ventricle and gives off the right marginal branch which cross the right ventricle wall It ends in the posterior interventricular artery in the sulcus of the same name, forming an anastomosis with the anterior interventricular artery Variations in this basic pattern are quite common The right coronary artery is dominant— becomes the posterior descending coronary artery—in about 70% of individuals.
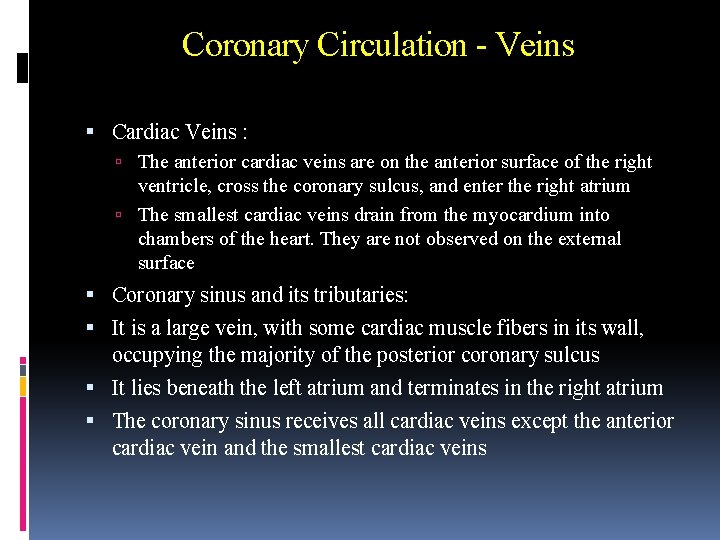
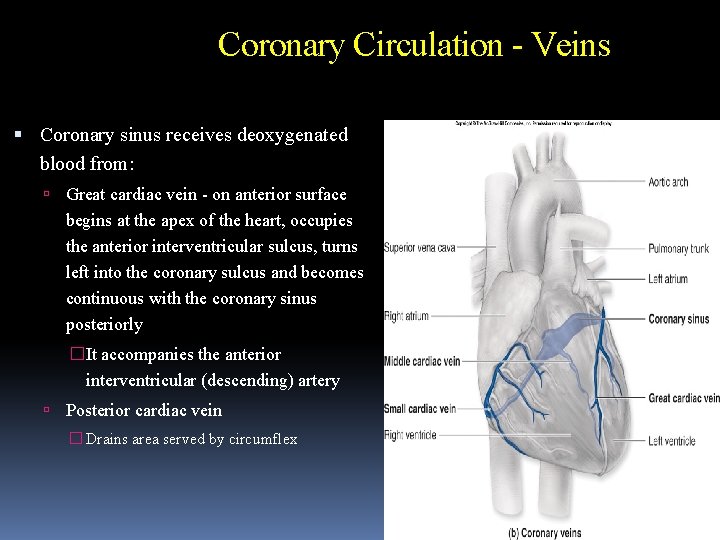
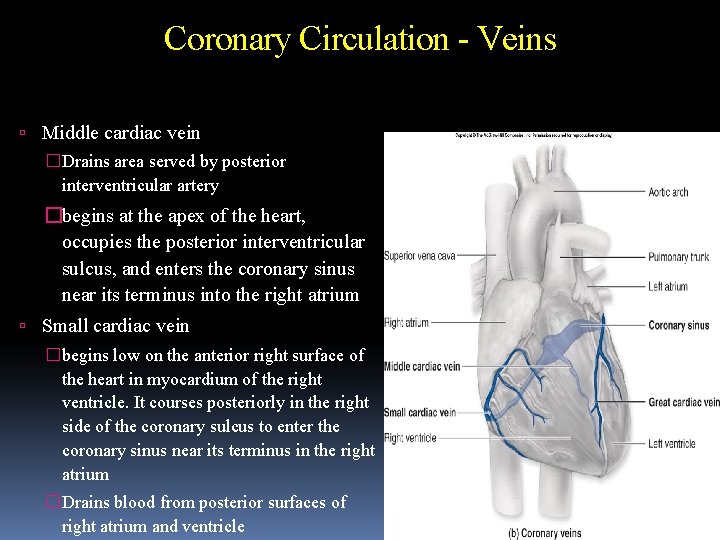
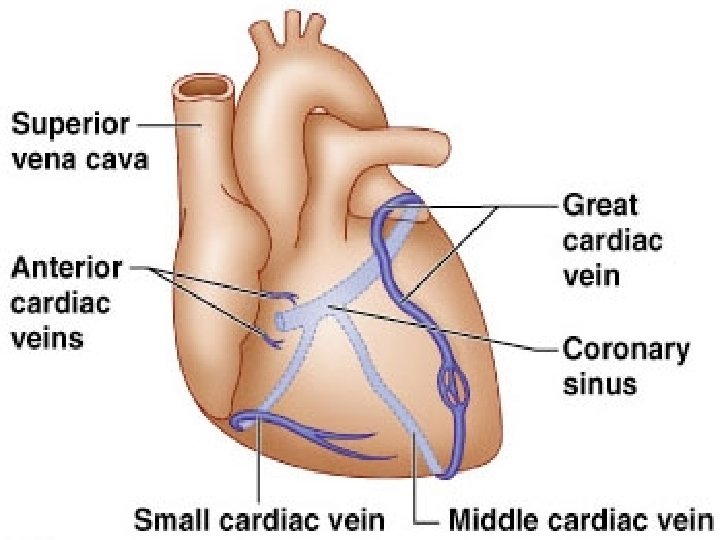
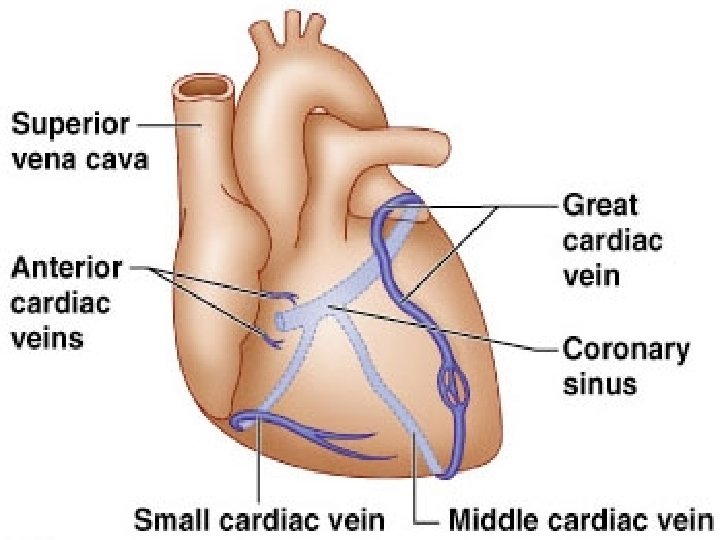
Coronary Circulation - Veins Cardiac Veins : The anterior cardiac veins are on the anterior surface of the right ventricle, cross the coronary sulcus, and enter the right atrium The smallest cardiac veins drain from the myocardium into chambers of the heart. They are not observed on the external surface Coronary sinus and its tributaries: It is a large vein, with some cardiac muscle fibers in its wall, occupying the majority of the posterior coronary sulcus It lies beneath the left atrium and terminates in the right atrium The coronary sinus receives all cardiac veins except the anterior cardiac vein and the smallest cardiac veins
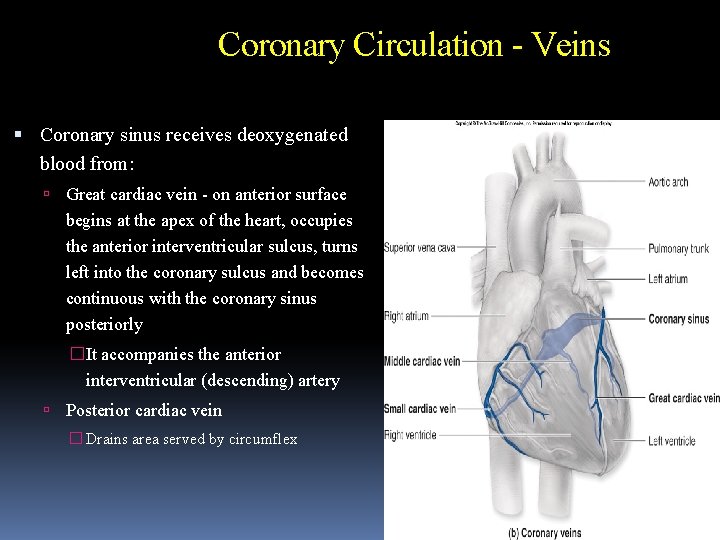
Coronary Circulation - Veins Coronary sinus receives deoxygenated blood from: Great cardiac vein - on anterior surface begins at the apex of the heart, occupies the anterior interventricular sulcus, turns left into the coronary sulcus and becomes continuous with the coronary sinus posteriorly �It accompanies the anterior interventricular (descending) artery Posterior cardiac vein � Drains area served by circumflex
Coronary Circulation - Veins Middle cardiac vein �Drains area served by posterior interventricular artery �begins at the apex of the heart, occupies the posterior interventricular sulcus, and enters the coronary sinus near its terminus into the right atrium Small cardiac vein �begins low on the anterior right surface of the heart in myocardium of the right ventricle. It courses posteriorly in the right side of the coronary sulcus to enter the coronary sinus near its terminus in the right atrium �Drains blood from posterior surfaces of right atrium and ventricle
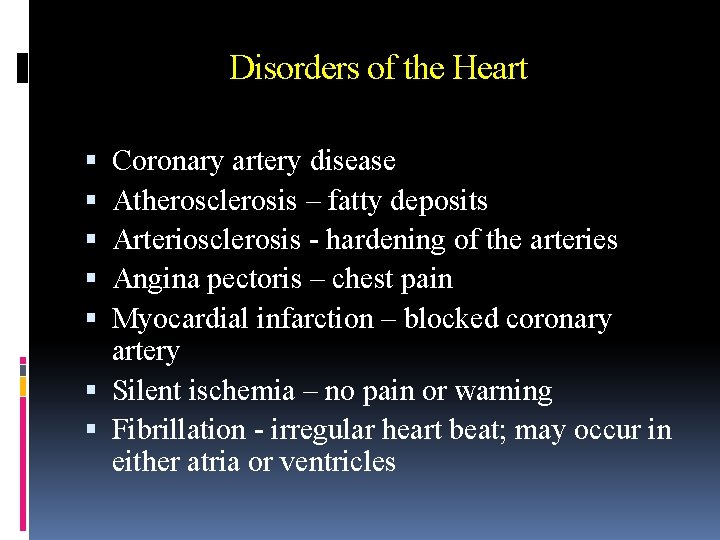
Disorders of the Heart Coronary artery disease Atherosclerosis – fatty deposits Arteriosclerosis - hardening of the arteries Angina pectoris – chest pain Myocardial infarction – blocked coronary artery Silent ischemia – no pain or warning Fibrillation - irregular heart beat; may occur in either atria or ventricles