CPR QUALITY 2015 AHA GUIDELINES UPDATE FOR CARDIOPULMONARY








- Slides: 78

CPR QUALITY 2015 AHA GUIDELINES UPDATE FOR CARDIOPULMONARY RESUSCITATION AND EMERGENCY CARDIOVASCULAR CARE : IT’S ALL ABOUT QUALITY THE GOLDILOCKS PRINCIPLE
SPEAKER DISCLOSURE Mary Fran Hazinski: Compensated consultant to the American Heart Association Emergency Cardiac Care AHA is sponsoring travel expenses for this meeting Note: Hazinski will note therapies not yet approved by the FDA for the purpose(s) cited in Guidelines (eg, therapeutic hypothermia/targeted temperature management/pediatric VT/VF drugs)
PURPOSE OF THIS WORKSHOP At the conclusion of this presentation, learners will be able to: • Discuss the evidence base for some of the changes in CPR and ECC detailed in the 2015 Guidelines Update • Describe at least one way your resuscitation practice or teaching will change as the result of information learned at this session NOTE: More information about 2015 AHA Guidelines Update for CPR and ECC presented in other ECCU sessions
CPR QUALITY 2015 AHA GUIDELINES UPDATE FOR CARDIOPULMONARY RESUSCITATION AND EMERGENCY CARDIOVASCULAR CARE : IT’S ALL ABOUT QUALITY THE GOLDILOCKS a t i c s Resu PRINCIPLE ˄ tion Also: SMALL INCREMENTAL CHANGES CAN MAKE BIG DIFFERENCES

ROBERT SOUTHEY, 1837 This is “JUST RIGHT” GOLDILOCKS images CAKRNLWX. jpg
RESUSCITATION QUALITY: THE GOLDILOCKS PRINCIPLE • We must all strive to optimize resuscitation quality elements: –Provide chest compressions of adequate rate –Provide chest compressions of adequate depth –Allow complete recoil after each compression –Minimize interruptions in compressions –Avoid excessive ventilation • More research is needed
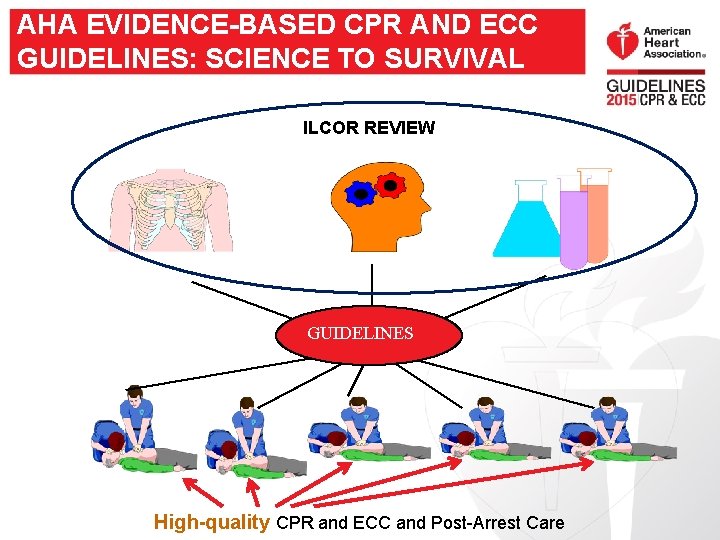
AHA EVIDENCE-BASED CPR AND ECC GUIDELINES: SCIENCE TO SURVIVAL ILCOR REVIEW GUIDELINES High-quality CPR and ECC and Post-Arrest Care
MAJOR CHANGE IN 2015 GUIDELINES PUBLICATION IN CIRCULATION • 2015 journal publication is a Guidelines Update • Includes topics addressed by ILCOR/Co. STR evidence evaluation or those addressed in response to request from training network. • Integrated 2015 AHA Guidelines for CPR and ECC is published online.

PROGRESS AND PUBLICATIONS SINCE 2010
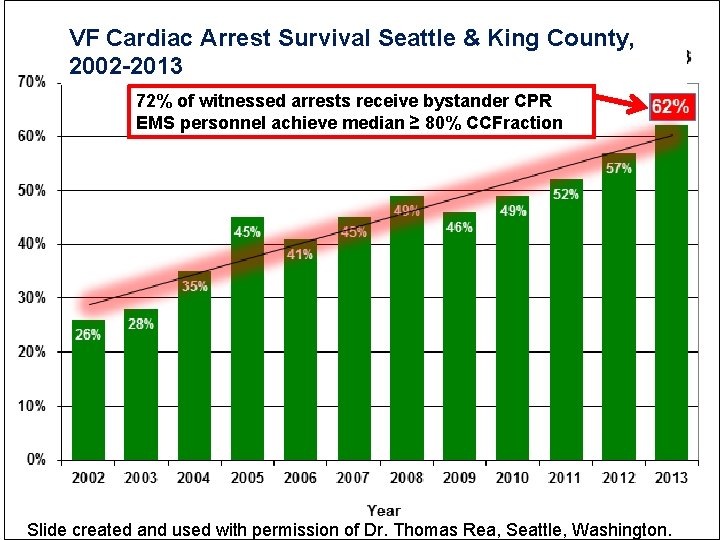
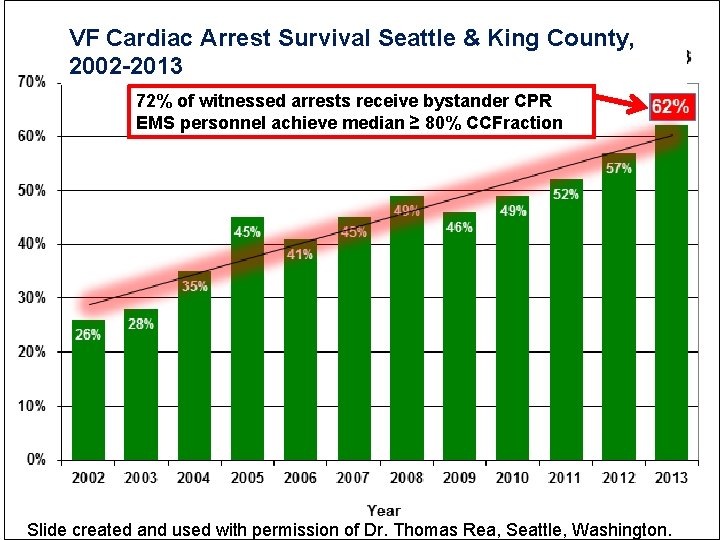
VF Cardiac Arrest Survival Seattle & King County, 2002 -2013 72% of witnessed arrests receive bystander CPR EMS personnel achieve median ≥ 80% CCFraction Slide created and used with permission of Dr. Thomas Rea, Seattle, Washington.
GOAL: CPR Quality: Improving Cardiac Resuscitation Outcomes Both Inside And Outside The Hospital A Consensus Statement from the American Heart Association Peter A. Meaney, MD, MPH, Chair; Bentley J. Bobrow, MD, FAHA, Co-Chair; Mary E. Mancini, RN, Ph. D, NE-BC, FAHA; Jim Christenson, MD; Allan R. de Caen, MD; Farhan Bhanji, MD, MSc, FAHA; Benjamin S. Abella, MD, MPhil, FAHA; Monica E. Kleinman, MD; Dana P. Edelson, MD, MS, FAHA; Robert A. Berg, MD, FAHA; Tom P. Aufderheide, MD, FAHA; Venu Menon, MD, FAHA; Marion Leary, MSN, RN; on behalf of the CPR Quality Summit Investigators Circulation 2013, TBD Circulation is published by the American Heart Association. 7272 Greenville Avenue, Dallas, TX 72514 Copyright © 2013 American Heart Association. All rights reserved. Print ISSN: 0009 -7322. Online ISSN: 15244539
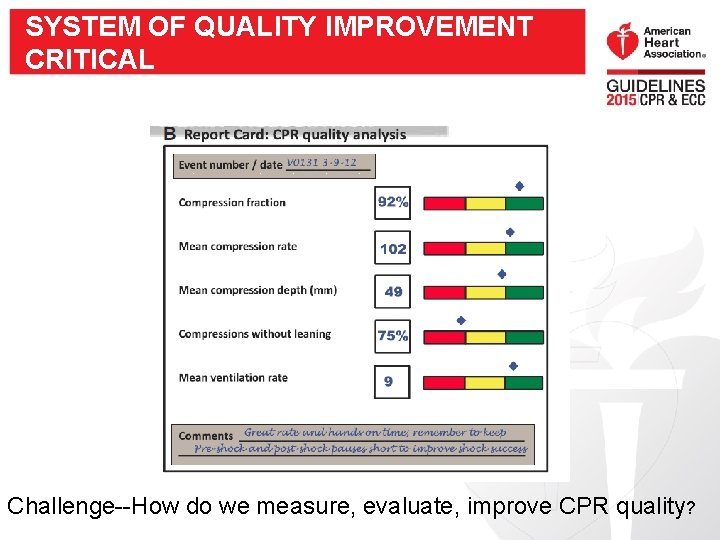
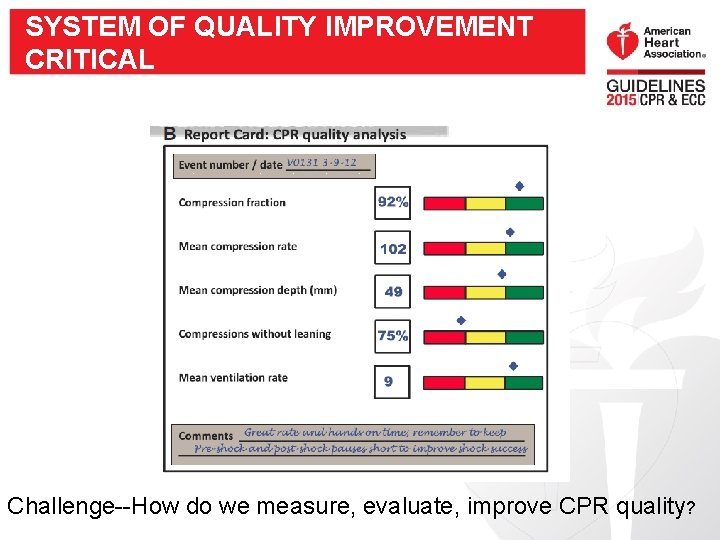
SYSTEM OF QUALITY IMPROVEMENT CRITICAL Challenge--How do we measure, evaluate, improve CPR quality?
2015 INSTITUTE OF MEDICINE REPORT n o i ss i a et n i ls M d e or e s t x ne m o fr m o T fd u A h r e e d i e

SELECTED NEW AND UPDATED RECOMMENDATIONS
SELECTED NEW AND UPDATED RECOMMENDATIONS: ADULT BLS AND CPR QUALITY More details from Ben Bobrow and Dana Edelson tomorrow
CHEST COMPRESSION RATE: UPDATED Recommendation: • Compression rate: 100120/minute (2010: at least 100/min). Why? • Absolute number of compressions delivered/minute linked with survival. • Actual compression rate often well below 100/minute. • Rates below 100/min or above 120/min adversely affect outcomes.
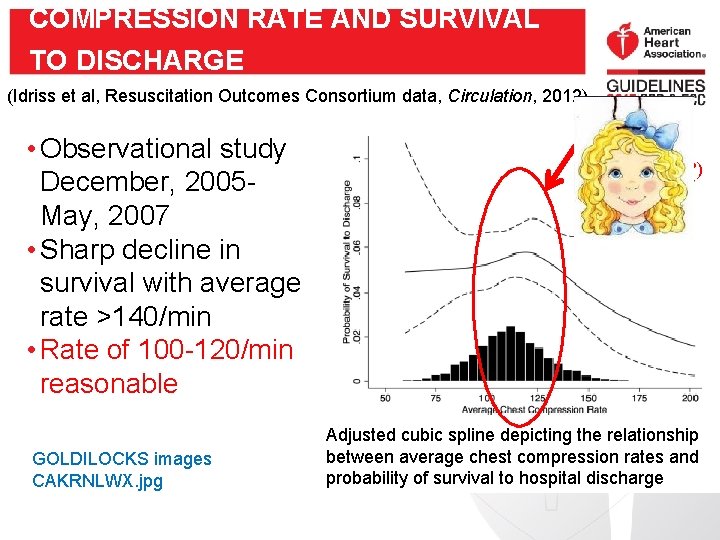
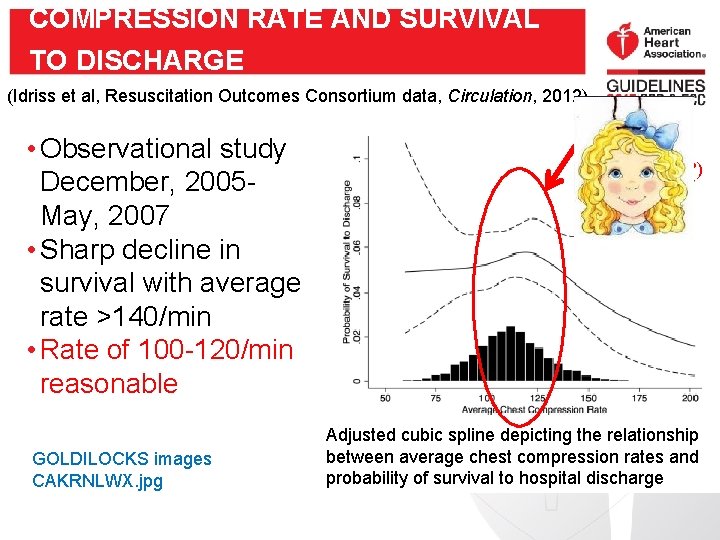
COMPRESSION RATE AND SURVIVAL TO DISCHARGE (Idriss et al, Resuscitation Outcomes Consortium data, Circulation, 2012) • Observational study December, 2005 May, 2007 • Sharp decline in survival with average rate >140/min • Rate of 100 -120/min reasonable GOLDILOCKS images CAKRNLWX. jpg Optimal rate (“sweet spot”? ) Adjusted cubic spline depicting the relationship between average chest compression rates and probability of survival to hospital discharge
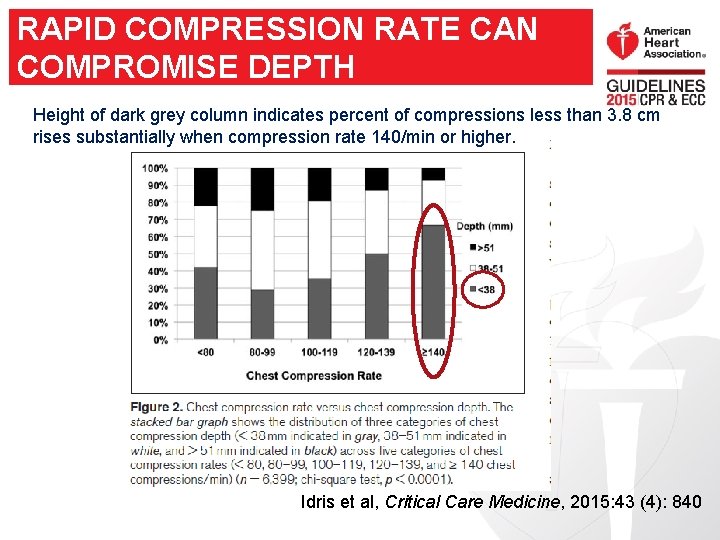
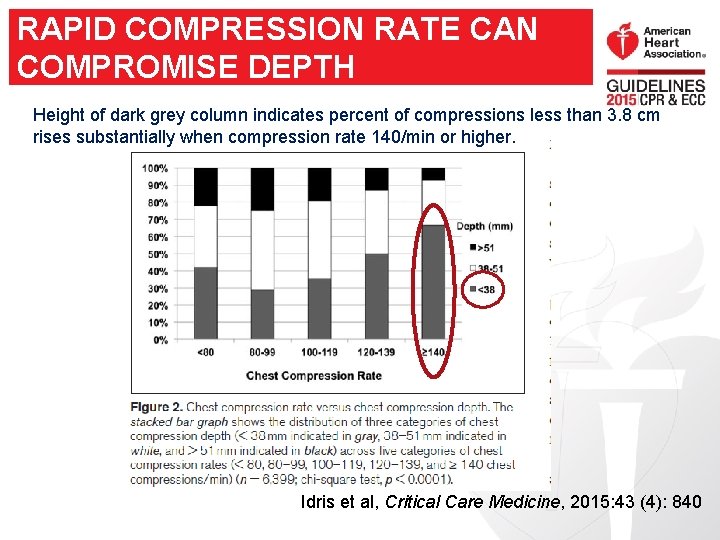
RAPID COMPRESSION RATE CAN COMPROMISE DEPTH Height of dark grey column indicates percent of compressions less than 3. 8 cm rises substantially when compression rate 140/min or higher. Idris et al, Critical Care Medicine, 2015: 43 (4): 840
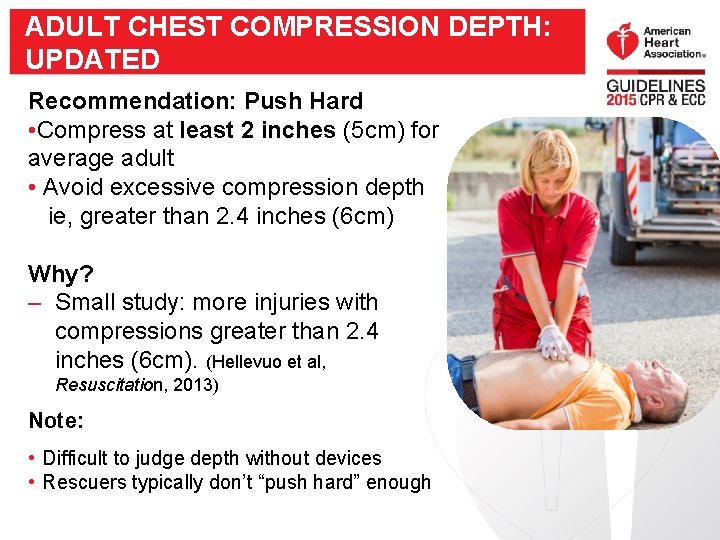
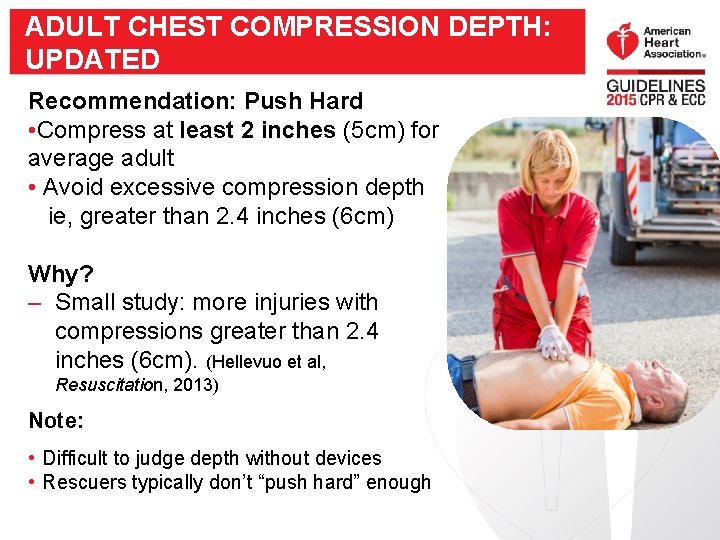
ADULT CHEST COMPRESSION DEPTH: UPDATED Recommendation: Push Hard • Compress at least 2 inches (5 cm) for average adult • Avoid excessive compression depth ie, greater than 2. 4 inches (6 cm) Why? – Small study: more injuries with compressions greater than 2. 4 inches (6 cm). (Hellevuo et al, Resuscitation, 2013) Note: • Difficult to judge depth without devices • Rescuers typically don’t “push hard” enough
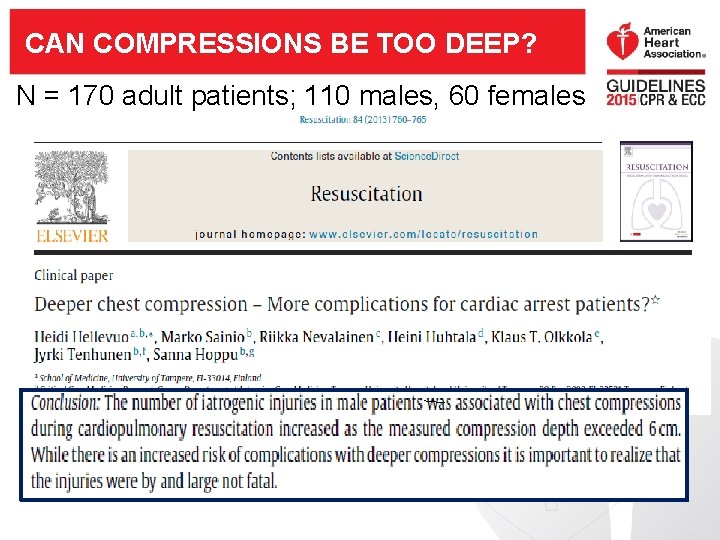
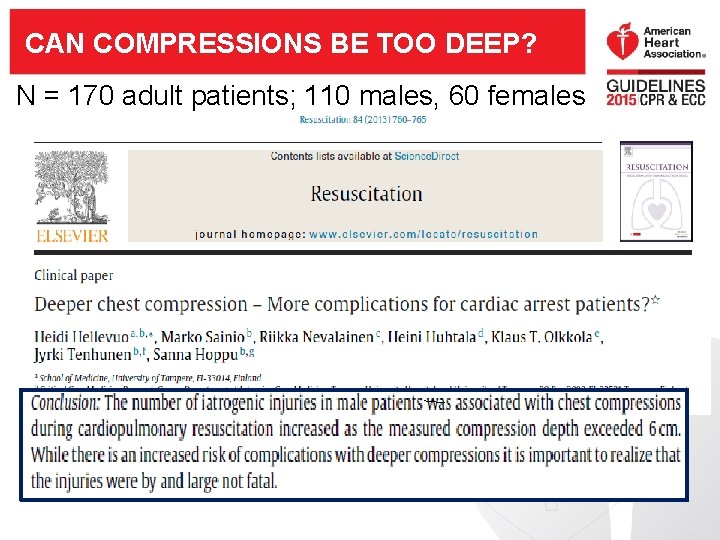
CAN COMPRESSIONS BE TOO DEEP? N = 170 adult patients; 110 males, 60 females
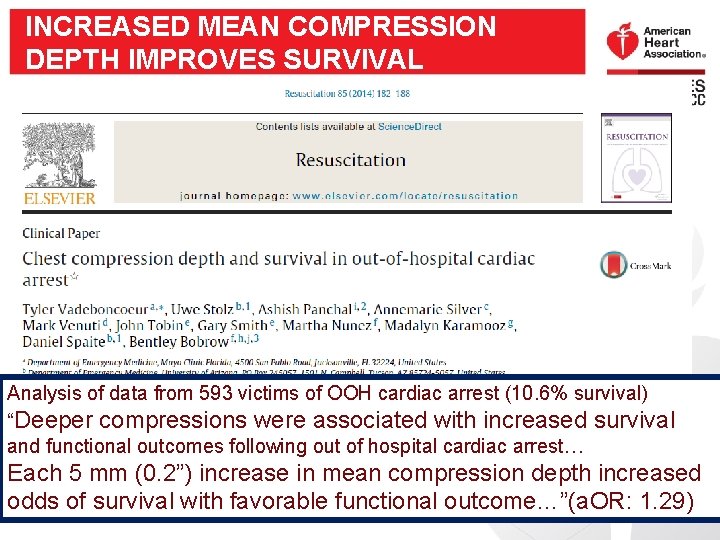
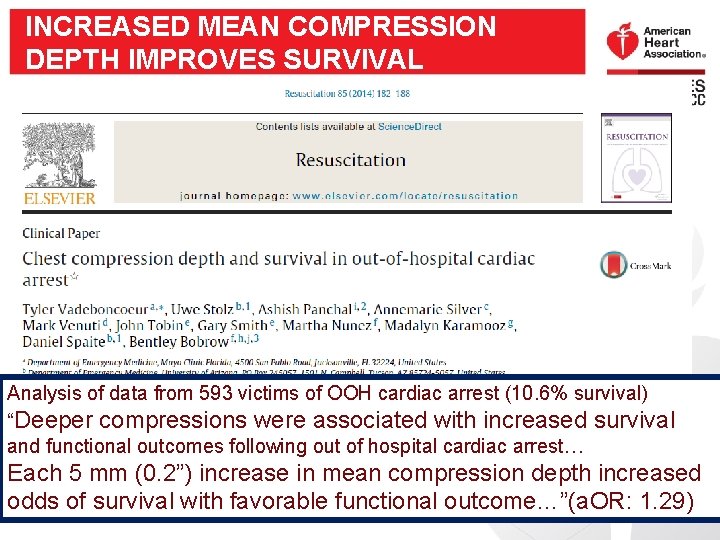
INCREASED MEAN COMPRESSION DEPTH IMPROVES SURVIVAL Analysis of data from 593 victims of OOH cardiac arrest (10. 6% survival) “Deeper compressions were associated with increased survival and functional outcomes following out of hospital cardiac arrest… Each 5 mm (0. 2”) increase in mean compression depth increased odds of survival with favorable functional outcome…”(a. OR: 1. 29)
COMPRESSION DEPTH • Adults and children beyond puberty: between 2 and 2. 4 inches (5 to 6 cm) GOLDILOCKS images CAKRNLWX. jpg • Monitoring instruments required
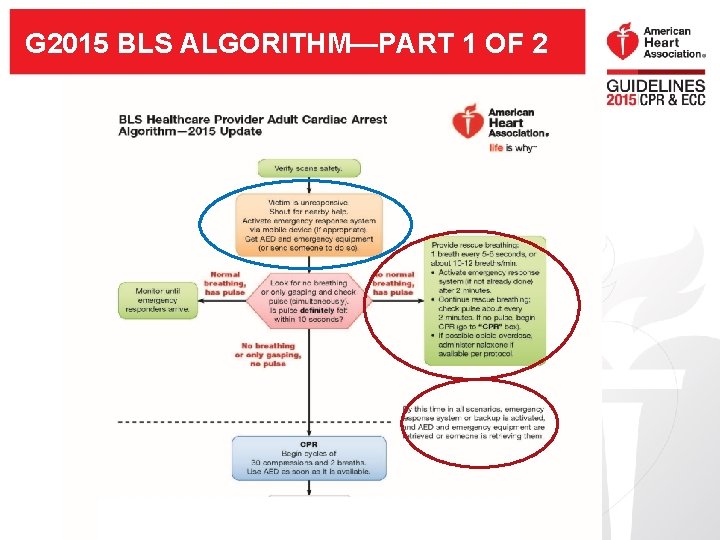
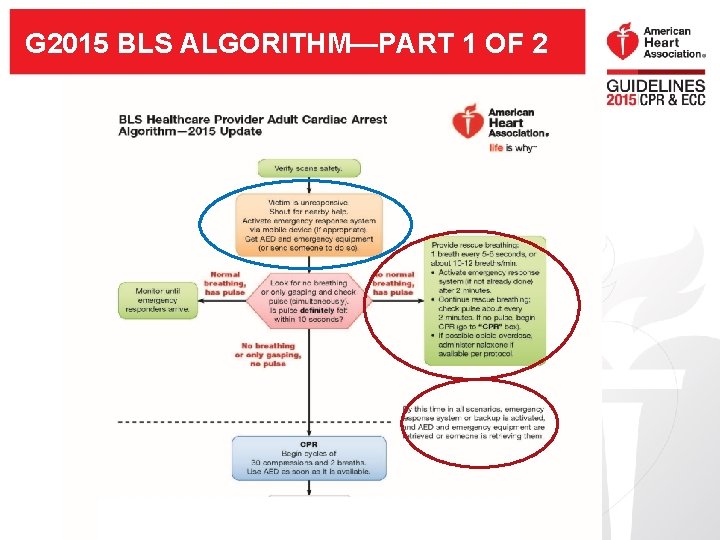
G 2015 BLS ALGORITHM—PART 1 OF 2
RESCUER CAN TAILOR SEQUENCE • Goal: To make activation and priorities “just right” for rescuer, victim, system
SELECTED NEW AND UPDATED RECOMMENDATIONS: ALTERNATIVE TECHNIQUES AND ANCILLARY DEVICES FOR CPR More details from Bob Neumar Thursday General Session
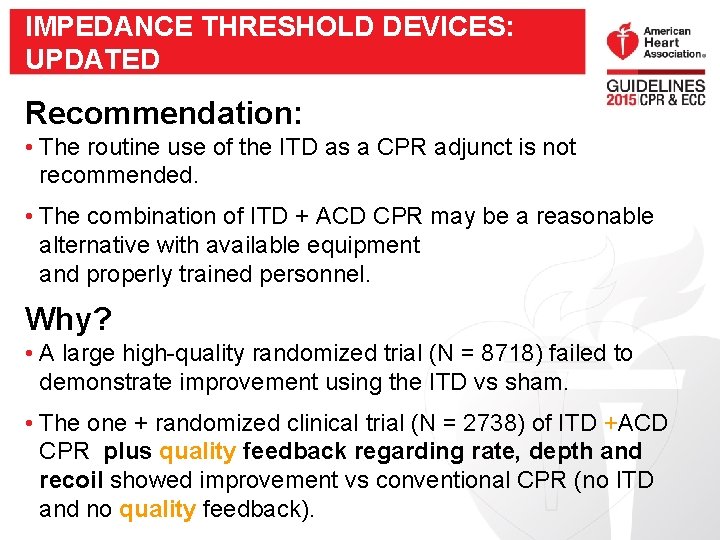
IMPEDANCE THRESHOLD DEVICES: UPDATED Recommendation: • The routine use of the ITD as a CPR adjunct is not recommended. • The combination of ITD + ACD CPR may be a reasonable alternative with available equipment and properly trained personnel. Why? • A large high-quality randomized trial (N = 8718) failed to demonstrate improvement using the ITD vs sham. • The one + randomized clinical trial (N = 2738) of ITD +ACD CPR plus quality feedback regarding rate, depth and recoil showed improvement vs conventional CPR (no ITD and no quality feedback).
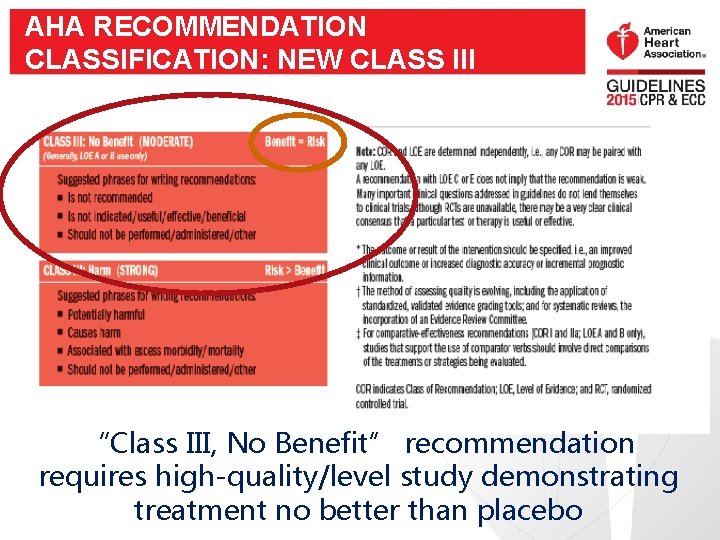
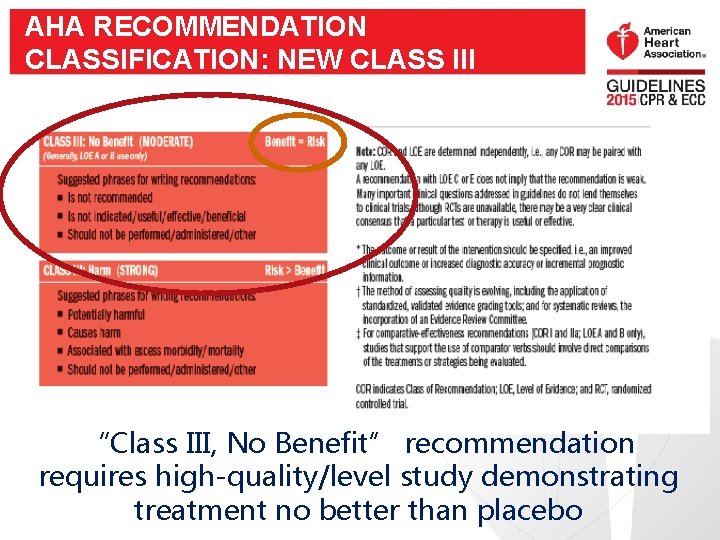
AHA RECOMMENDATION CLASSIFICATION: NEW CLASS III “Class III, No Benefit” recommendation requires high-quality/level study demonstrating treatment no better than placebo
SELECTED NEW AND UPDATED RECOMMENDATIONS: ACLS More details from Bob Neumar in plenary session Thursday
VASOPRESSORS IN CARDIAC ARREST Recommendation: • Vasopressin deleted from ACLS Cardiac Arrest Algorithm. Why? • No benefit of vasopressin + epinephrine vs epinephrine alone Recommendation • Reasonable to administer epinephrine as soon as feasible after the cardiac arrest with initial nonshockable rhythm Why? • In large observational study, better outcome (increased ROSC, survival to hospital discharge, and neurologically intact survival) associated with earlier epinephrine for cardiac arrest with nonshockable rhythms.
SELECTED NEW AND UPDATED RECOMMENDATIONS: POST-CARDIAC ARREST CARE More details from Farhan Bhanji and Allan de Caen Thursday, Concurrent Session
POST-CARDIAC ARREST ELEMENTS OF CARE: UPDATED • Emergent coronary angiography: • Should be performed after OHCA with suspected cardiac etiology and ST elevation • May be reasonable after OHCA with cardiac etiology for patients comatose but without ST elevation. • Reasonable where indicated (comatose or awake) • Targeted temperature management • Avoid and correct hypotension (systolic BP < 90 mm Hg or mean arterial pressure < 65 mm Hg)
TARGETED TEMPERATURE MANAGEMENT (TTM) • TTM recommended for patients comatose following ROSC from • TTM: select, maintain (for 24+ hours) constant temperature between 32°C and 36°C • If patient still comatose: continue TTM beyond 24 hours by actively preventing fever. • Routine prehospital cooling of patients with rapid infusion of cold IV fluids is not recommended (no benefit, possible complications)
NEW AND UPDATED RECOMMENDATIONS: ACUTE CORONARY SYNDROMES Will be presented by Karl Kern tomorrow General Session
SELECTED NEW AND UPDATED RECOMMENDATIONS: PEDIATRIC BLS More details from Vinay Nadkarni, Dianne Atkins, Wendy Simon Tomorrow (Wednesday), Concurrent Session
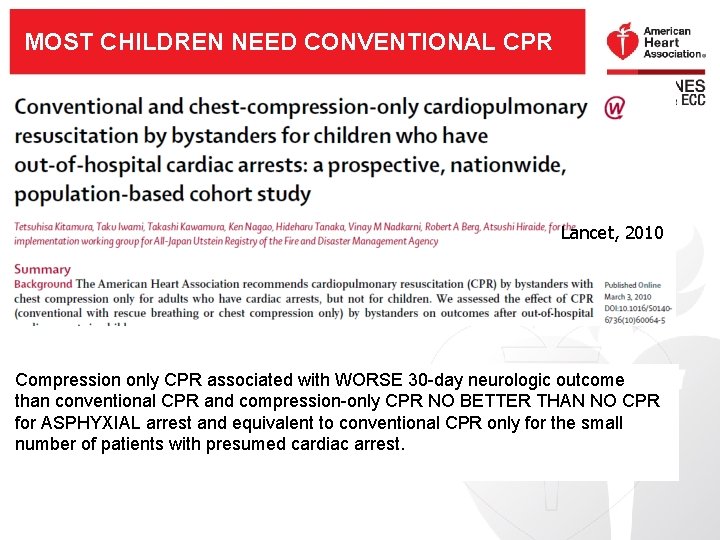
MOST CHILDREN NEED CONVENTIONAL CPR JAHA, 2014, N = 5009. aged < 18 years me o c t u gic o PR o l o r u C O y ne a N d n 0 er tha SE 3 t t R e O b no h. W t i R w P d C nly iate c o o n s o s i Ra ress P p C m y l o n on nd c o a i s R s P e r Comp ventional C on than c
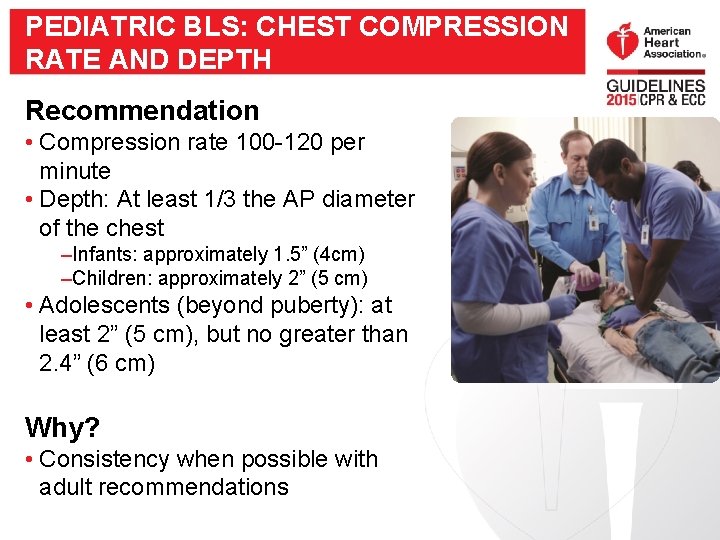
PEDIATRIC BLS: CHEST COMPRESSION RATE AND DEPTH Recommendation • Compression rate 100 -120 per minute • Depth: At least 1/3 the AP diameter of the chest –Infants: approximately 1. 5” (4 cm) –Children: approximately 2” (5 cm) • Adolescents (beyond puberty): at least 2” (5 cm), but no greater than 2. 4” (6 cm) Why? • Consistency when possible with adult recommendations
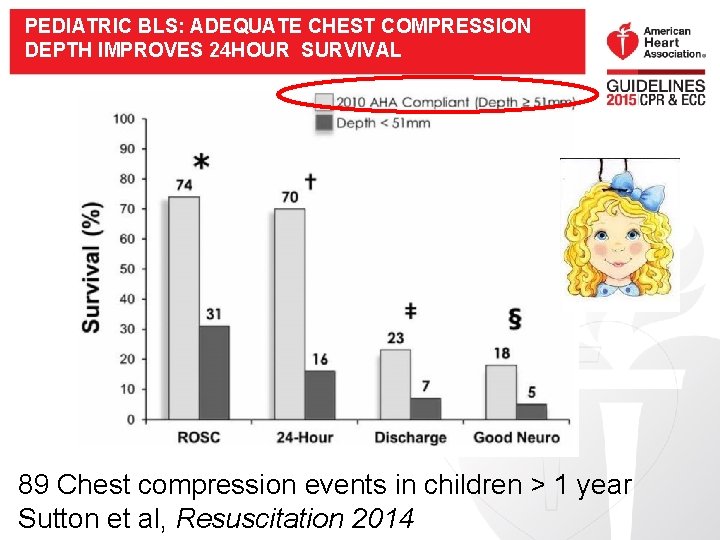
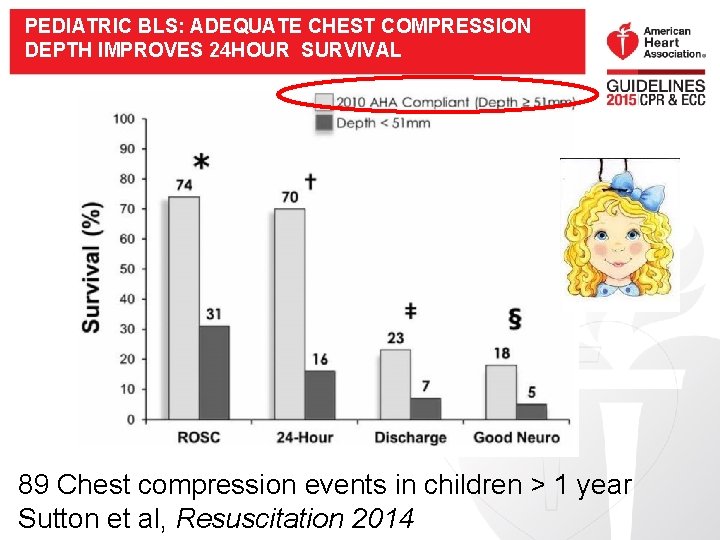
PEDIATRIC BLS: ADEQUATE CHEST COMPRESSION DEPTH IMPROVES 24 HOUR SURVIVAL 89 Chest compression events in children > 1 year Sutton et al, Resuscitation 2014

KEY NEW AND UPDATED RECOMMENDATIONS: PALS More details from Vinay Nadkarni, Dianne Atkins, Wendy Simon Tomorrow (Wednesday), Concurrent Session
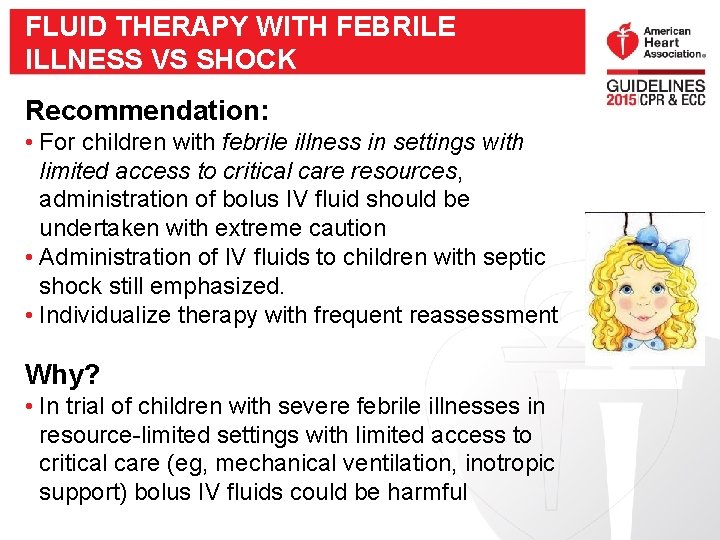
FLUID THERAPY WITH FEBRILE ILLNESS VS SHOCK Recommendation: • For children with febrile illness in settings with limited access to critical care resources, administration of bolus IV fluid should be undertaken with extreme caution • Administration of IV fluids to children with septic shock still emphasized. • Individualize therapy with frequent reassessment Why? • In trial of children with severe febrile illnesses in resource-limited settings with limited access to critical care (eg, mechanical ventilation, inotropic support) bolus IV fluids could be harmful
ATROPINE NO LONGER ROUTINE PREMEDICATION FOR EMERGENT INTUBATION Why? • No evidence to support the routine use of atropine as a premedication to prevent bradycardia during emergent intubation. • No evidence to support minimum dose of atropine for premedication • Note that recommendation for use of atropine for treatment of bradycardia is unchanged.
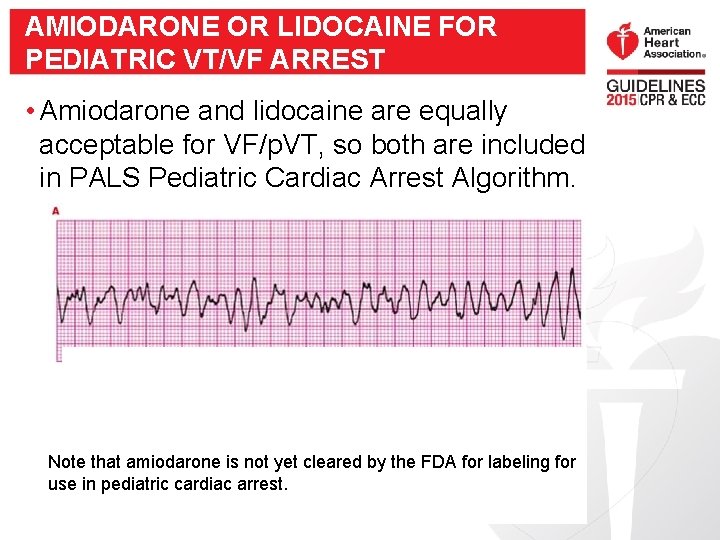
AMIODARONE OR LIDOCAINE FOR PEDIATRIC VT/VF ARREST • Amiodarone and lidocaine are equally acceptable for VF/p. VT, so both are included in PALS Pediatric Cardiac Arrest Algorithm. Note that amiodarone is not yet cleared by the FDA for labeling for use in pediatric cardiac arrest.
TARGETED TEMPERATURE MANAGEMENT IN CHILDREN Recommended • For children comatose following ROSC: -5 days normothermia (36°C - 37. 5°C) OR --2 days continuous hypothermia (32°C - 34°C), then 3 days normothermia • Prevent or aggressively treat fever during post-cardiac arrest care Why? New study published
KEY NEW AND UPDATED RECOMMENDATIONS: NEONATAL RESUSCITATION More details from Vinay Nadkarni, Dianne Atkins, Wendy Simon Tomorrow (Wednesday), Concurrent Session
ASSESSMENT OF HEART RATE AND OXYGENATION Recommendation • 3 -lead ECG more rapid and accurate than pulse oximetry to assess HR • Pulse oximetry still needed to evaluate oxygenation
UMBILICAL CORD MANAGEMENT: DELAYED CORD CLAMPING Recommendation • Delayed cord clamping after 30 seconds suggested for both term and preterm infants if resuscitation not required Why? • Beneficial effects include less intraventricular hemorrhage (IVH), higher BP and blood volume, less need for transfusion, less necrotizing enterocolitis (NEC)
INFANTS BORN THROUGH MECONIUMSTAINED AMNIOTIC FLUID: UPDATED Recommendation • When infant born through meconium-stained amniotic fluid is non-vigorous with inadequate breathing efforts, rescuers should perform routine steps of resuscitation Why? • No evidence immediate routine suctioning beneficial • Potential harm in delaying bag-mask ventilation

IMPROVING CPR QUALITY
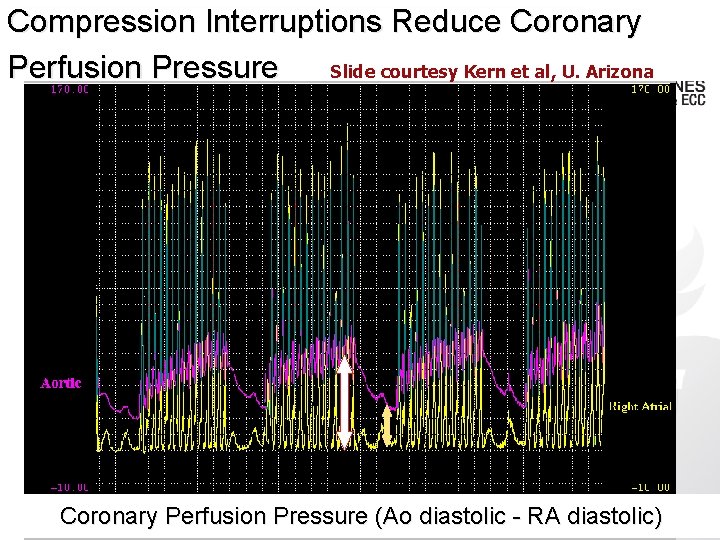
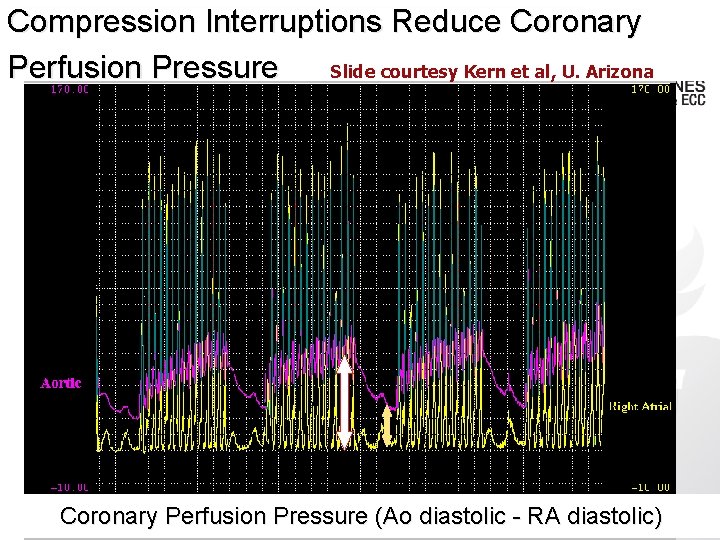
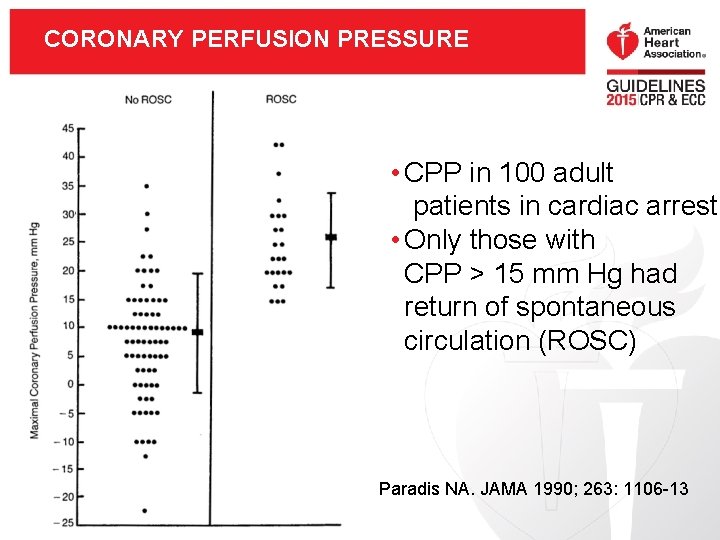
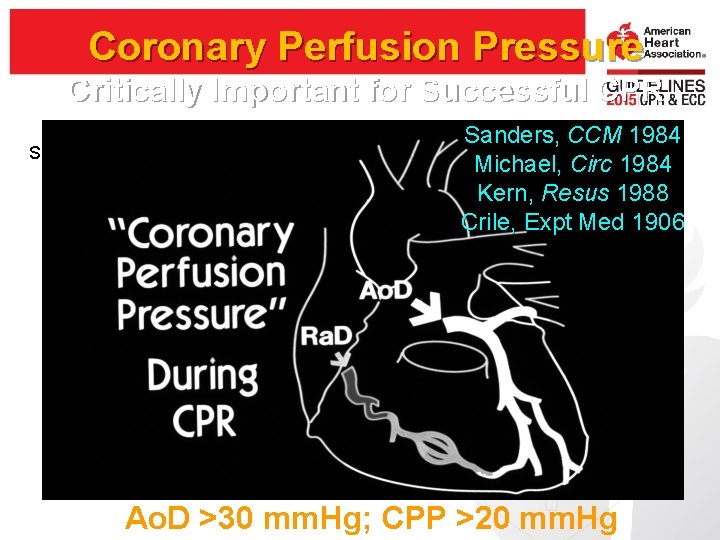
Compression Interruptions Reduce Coronary Slide courtesy Kern et al, U. Arizona Perfusion Pressure Coronary Perfusion Pressure (Ao diastolic - RA diastolic)
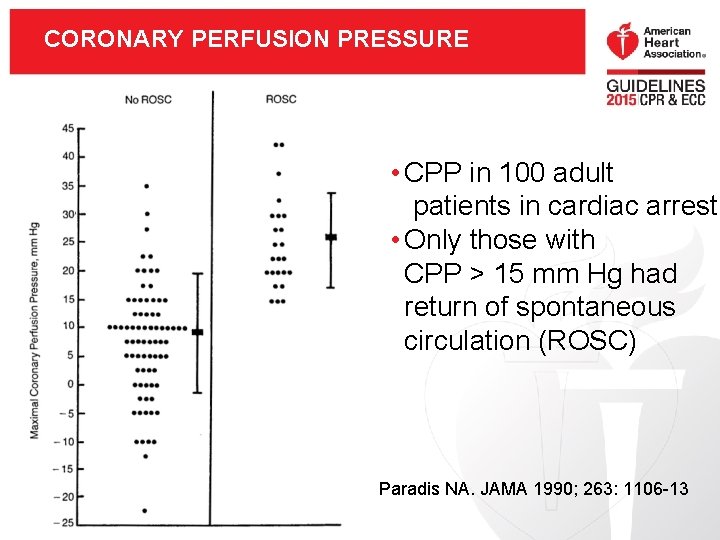
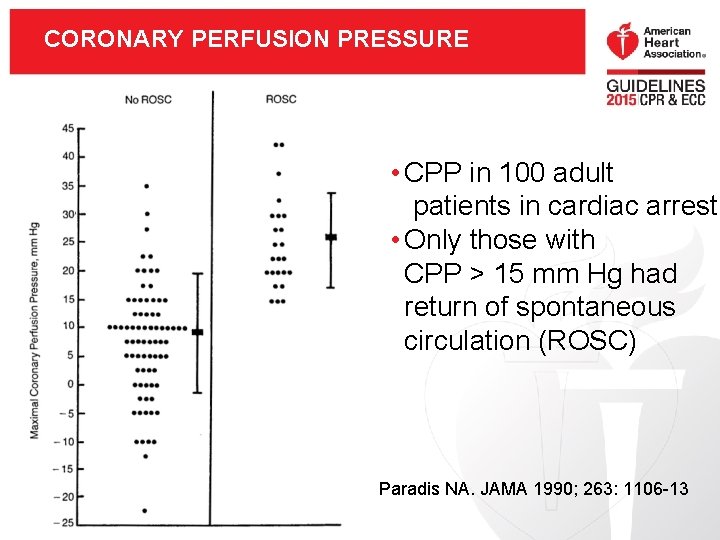
CORONARY PERFUSION PRESSURE • CPP in 100 adult patients in cardiac arrest • Only those with CPP > 15 mm Hg had return of spontaneous circulation (ROSC) Paradis NA. JAMA 1990; 263: 1106 -13
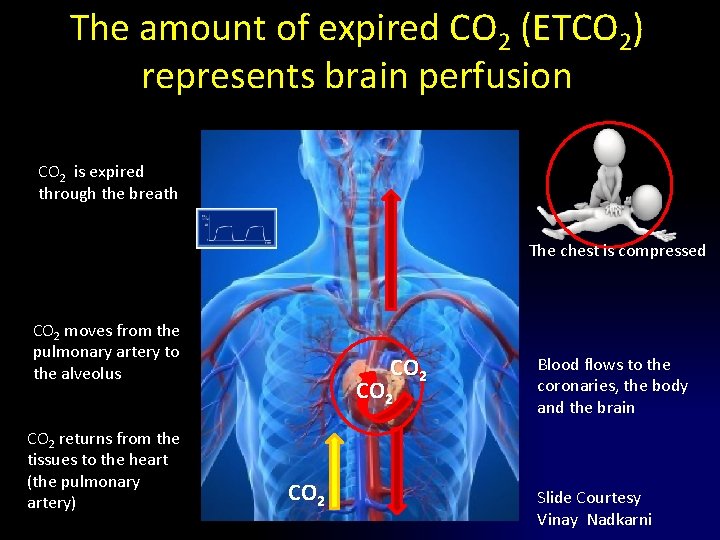
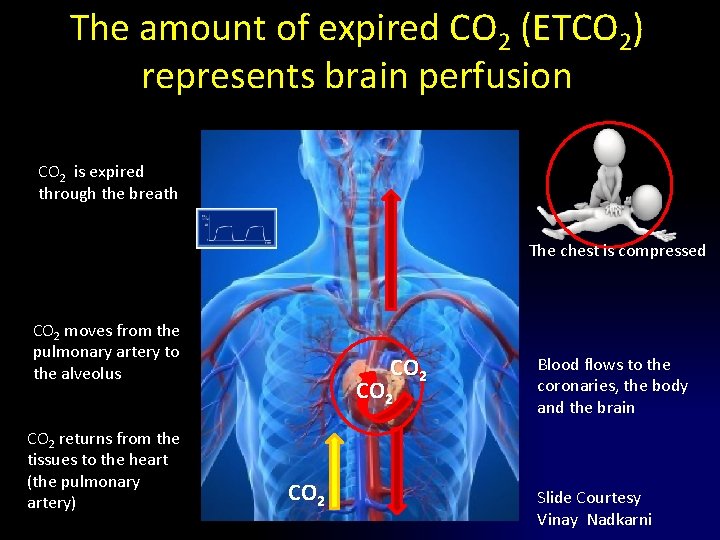
The amount of expired CO 2 (ETCO 2) represents brain perfusion CO 2 is expired through the breath The chest is compressed CO 2 moves from the pulmonary artery to the alveolus CO 2 returns from the tissues to the heart (the pulmonary artery) CO 2 Blood flows to the coronaries, the body and the brain Slide Courtesy Vinay Nadkarni
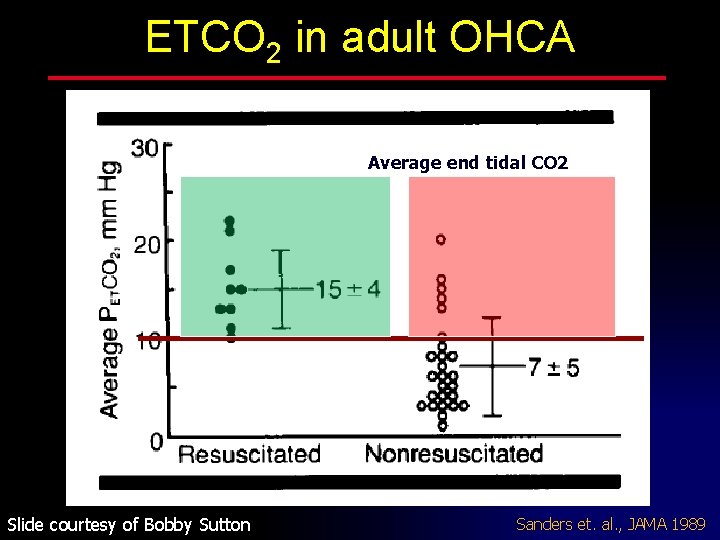
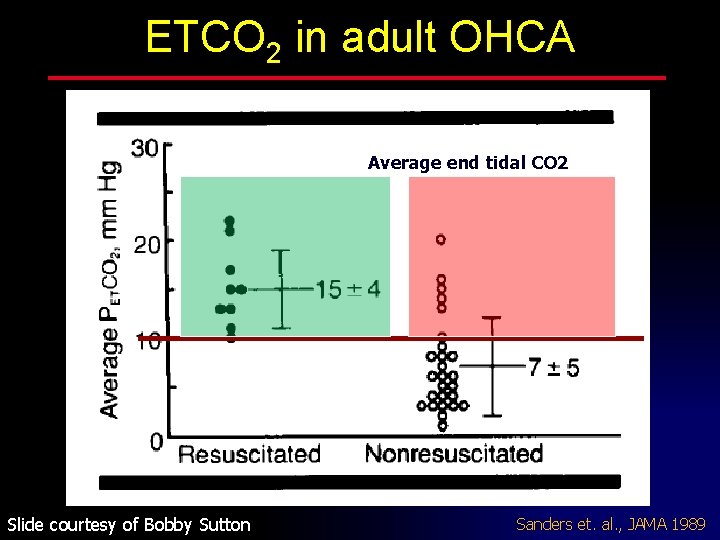
ETCO 2 in adult OHCA Average end tidal CO 2 Slide courtesy of Bobby Sutton Sanders et. al. , JAMA 1989
How do we measure CPR quality? Slides courtesy of Allan de Caen, Canada
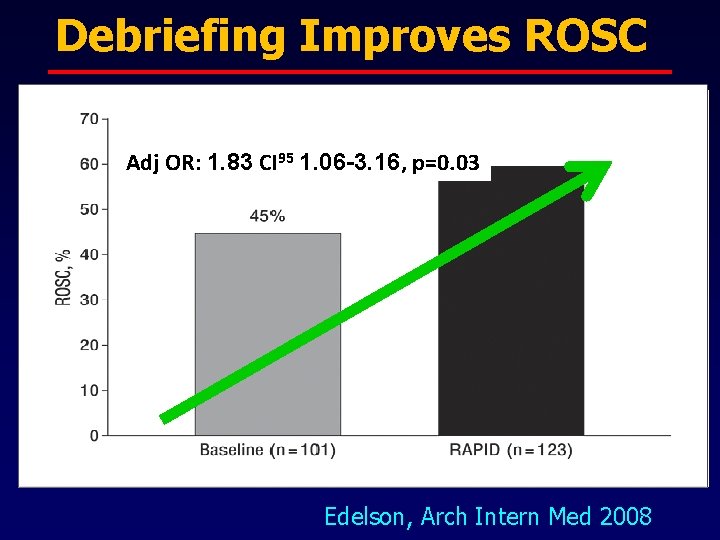
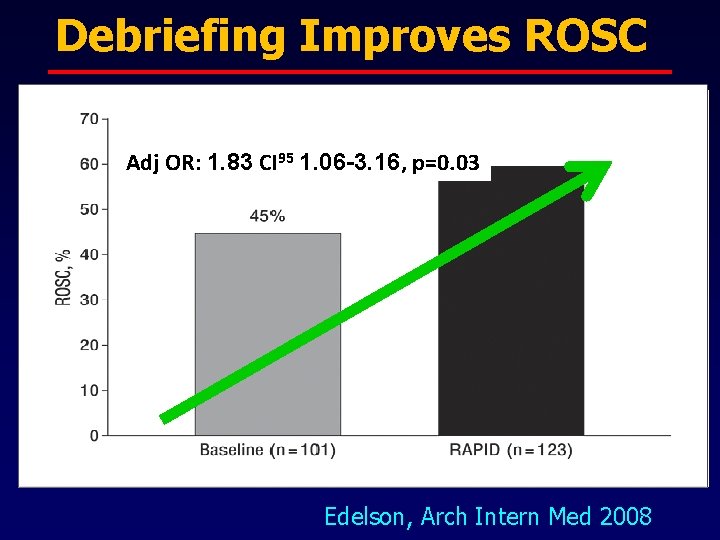
Debriefing Improves ROSC Adj OR: 1. 83 CI 95 1. 06 -3. 16, p=0. 03 Edelson, Arch Intern Med 2008
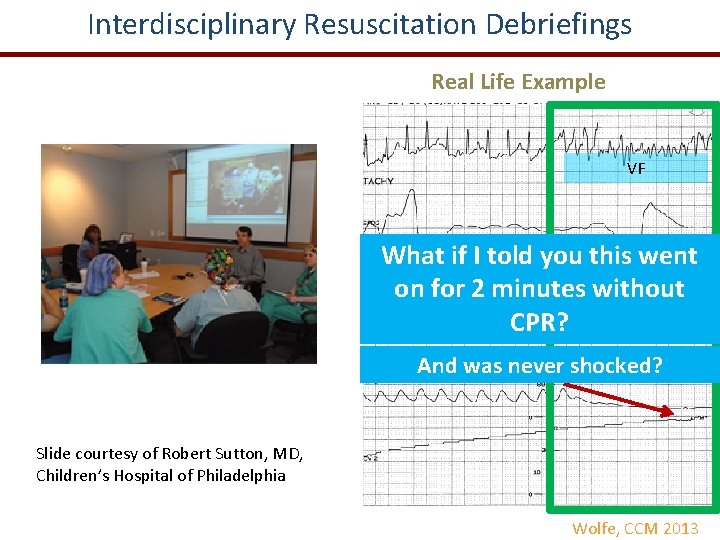
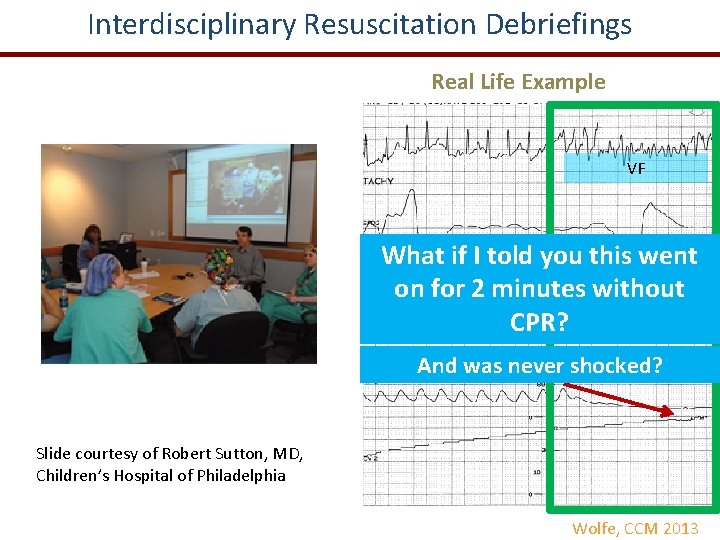
Interdisciplinary Resuscitation Debriefings • Quality of Resuscitation Real Life Example • Examples of excellence • Clinical issues - System issues • Team performance • Patient Physiology focused VF What if I told you this went on for 2 minutes without CPR? And was never shocked? Slide courtesy of Robert Sutton, MD, Children’s Hospital of Philadelphia Wolfe, CCM 2013
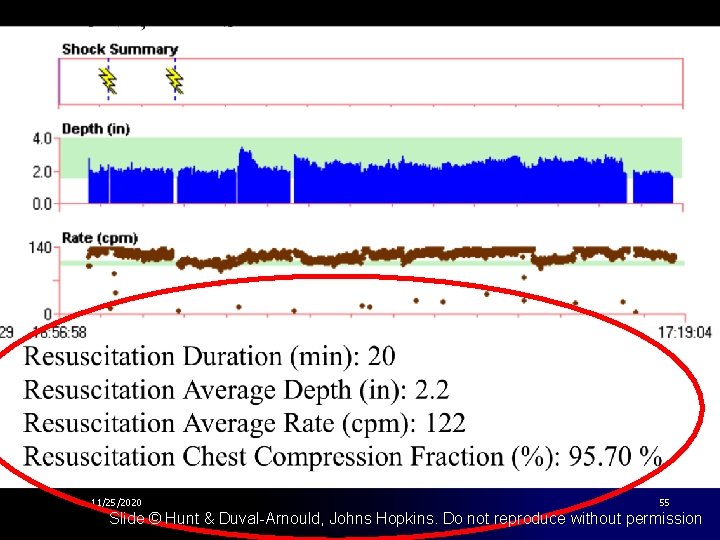
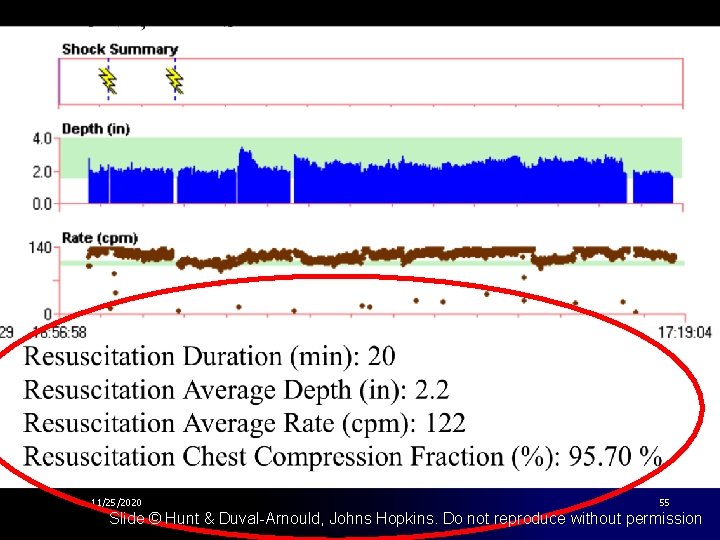
11/25/2020 55 Slide © Hunt & Duval-Arnould, Johns Hopkins. Do not reproduce without permission
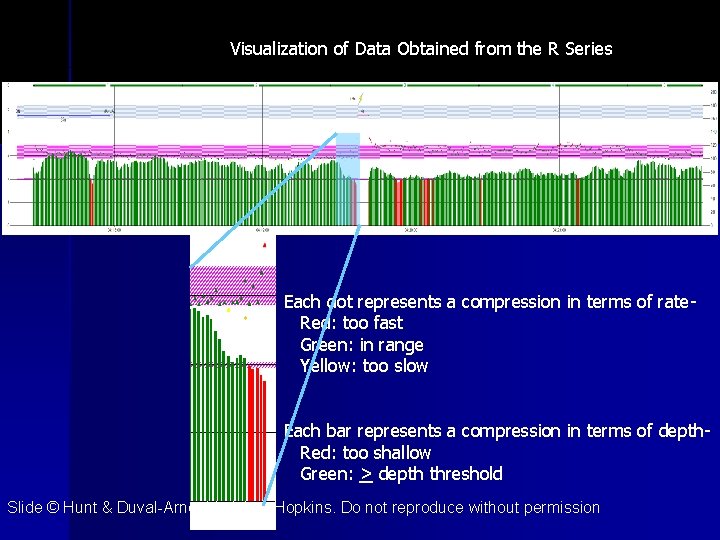
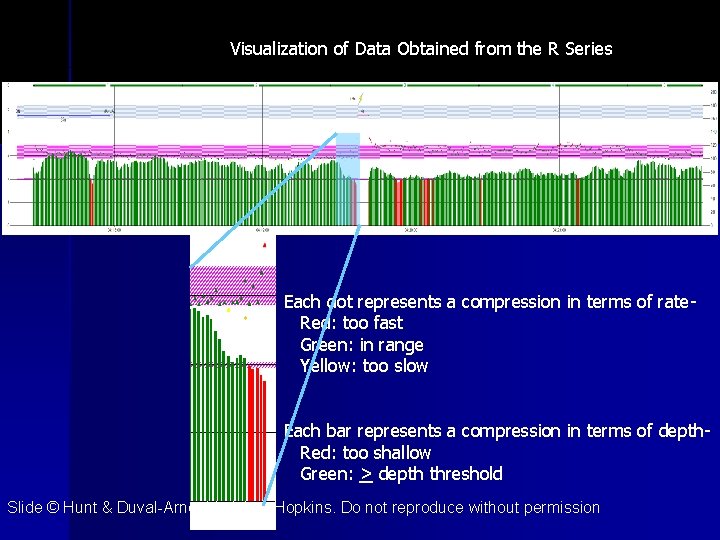
Visualization of Data Obtained from the R Series Each dot represents a compression in terms of rate Red: too fast Green: in range Yellow: too slow Each bar represents a compression in terms of depth Red: too shallow Green: > depth threshold Slide © Hunt & Duval-Arnould, Johns Hopkins. Do not reproduce without permission
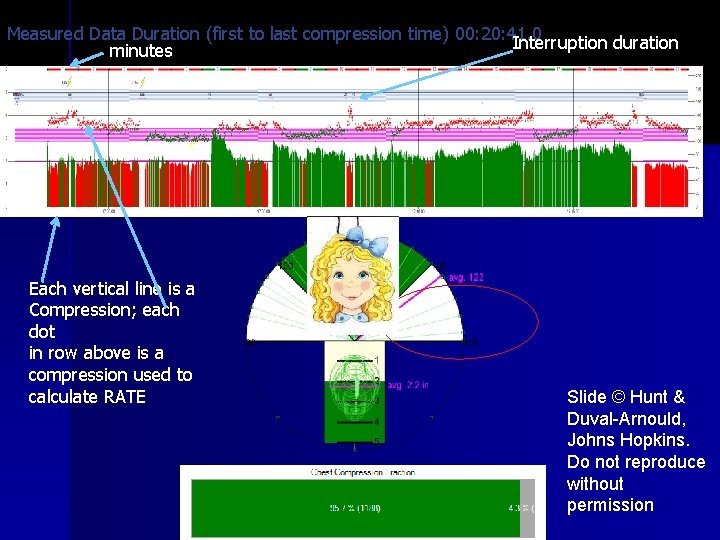
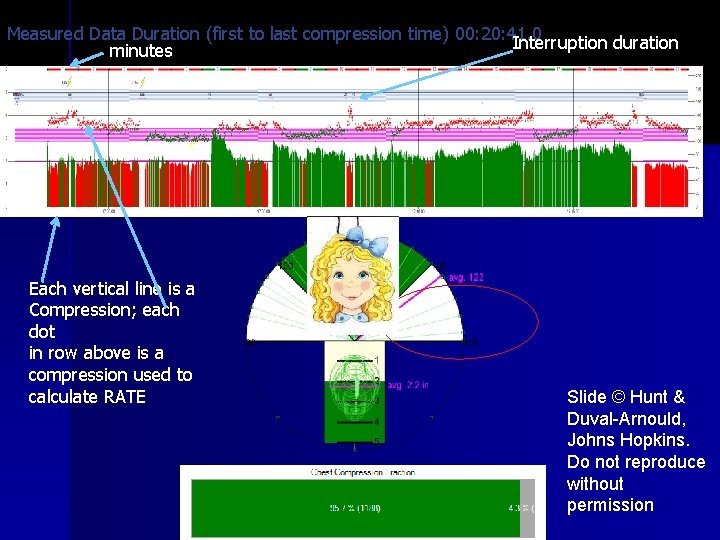
Measured Data Duration (first to last compression time) 00: 20: 41. 0 Interruption duration minutes Each vertical line is a Compression; each dot in row above is a compression used to calculate RATE Slide © Hunt & Duval-Arnould, Johns Hopkins. Do not reproduce without permission
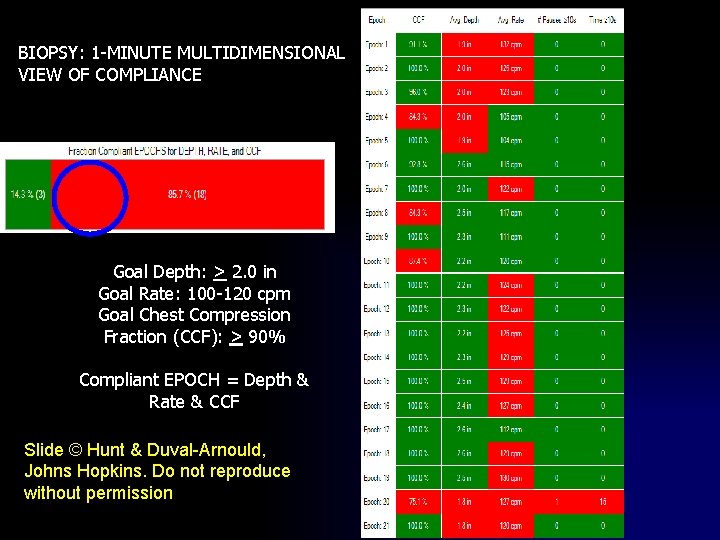
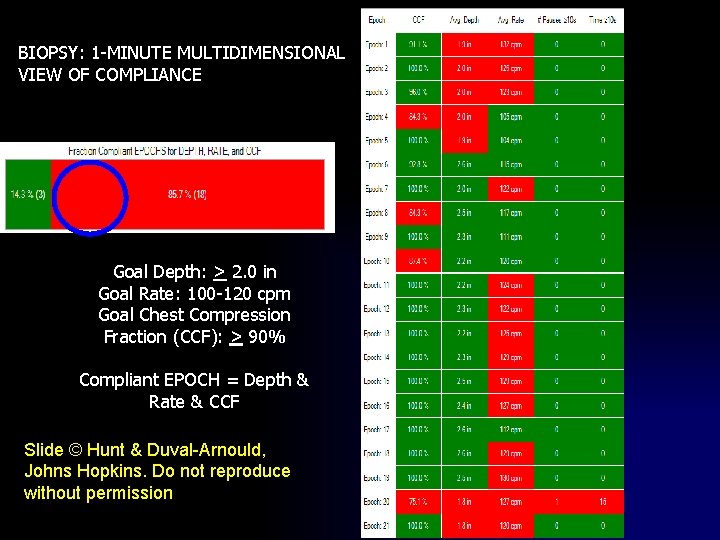
BIOPSY: 1 -MINUTE MULTIDIMENSIONAL VIEW OF COMPLIANCE Goal Depth: > 2. 0 in Goal Rate: 100 -120 cpm Goal Chest Compression Fraction (CCF): > 90% Compliant EPOCH = Depth & Rate & CCF Slide © Hunt & Duval-Arnould, Johns Hopkins. Do not reproduce without permission

Continue to drill down to details to improve performance, raise standards and save more lives!! 11/25/2020 Slide © Hunt & Duval-Arnould, Johns Hopkins. Do not 59 reproduce without permission
SUMMARY OF 2015 GUIDELINES UPDATE • We must rededicate ourselves to improving the frequency of bystander CPR and the quality of CPR and post–cardiac arrest care provided
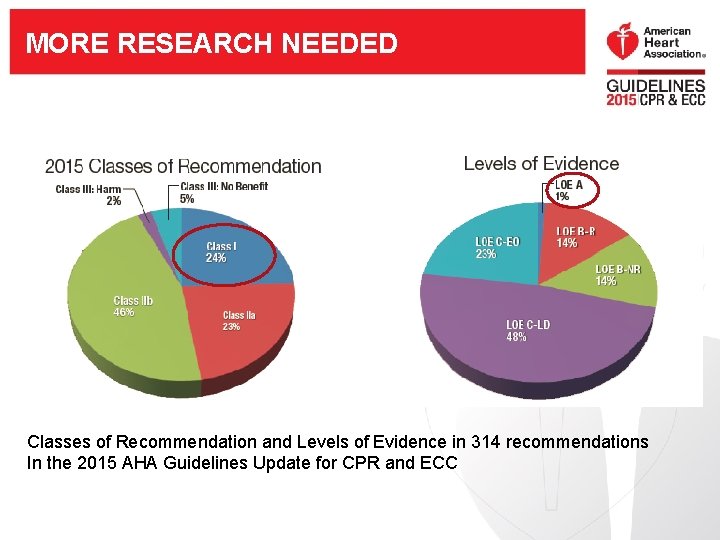
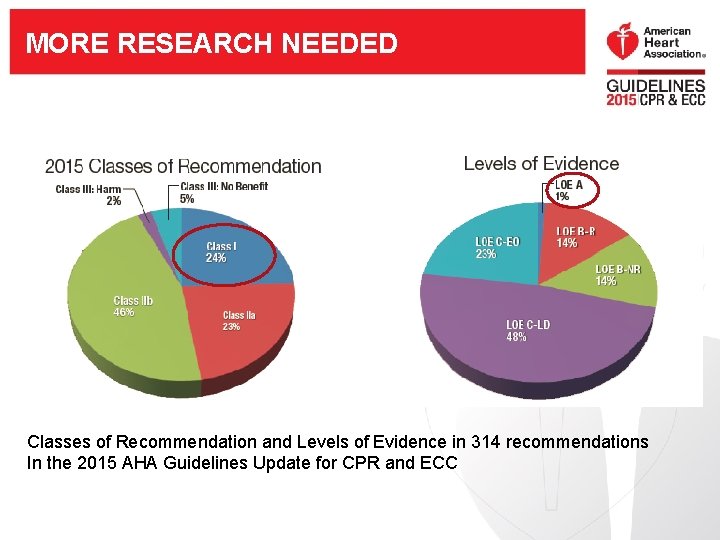
MORE RESEARCH NEEDED Classes of Recommendation and Levels of Evidence in 314 recommendations In the 2015 AHA Guidelines Update for CPR and ECC
DOWNLOAD FREE OF CHARGE To learn more about the 2015 Guidelines Update and upcoming products and information related to CPR and ECC visit www. ECCguidelines. heart. org • 2015 AHA Guidelines Update for CPR and ECC • 2015 AHA Integrated Guidelines for CPR and ECC • Highlights of the 2015 AHA Guidelines Update for CPR and ECC
QUESTIONS?
THANK YOU!
HAWTHORNE EFFECT— OBSERVATION ITSELF CREATES CHANGE • Western Electric Plant, Hawthorne NY • Studies of productivity altered performance
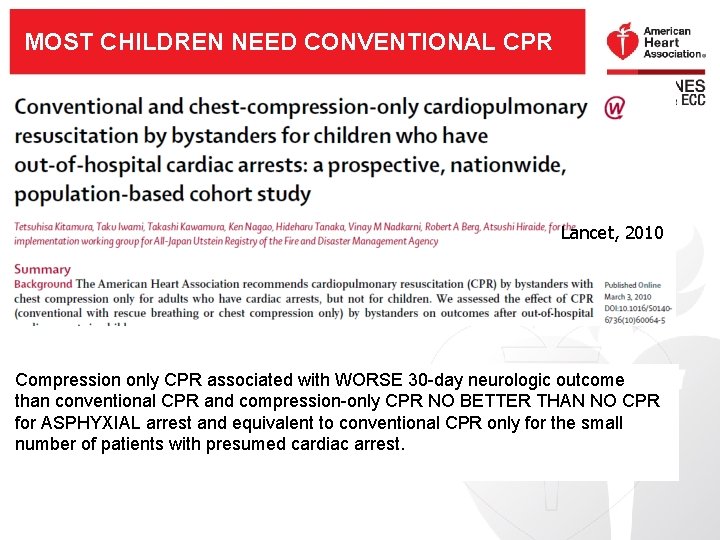
MOST CHILDREN NEED CONVENTIONAL CPR COMPRESSION ONLY FOR CHILDREN Lancet, 2010 Compression only CPR associated with WORSE 30 -day neurologic outcome than conventional CPR and compression-only CPR NO BETTER THAN NO CPR for ASPHYXIAL arrest and equivalent to conventional CPR only for the small number of patients with presumed cardiac arrest.
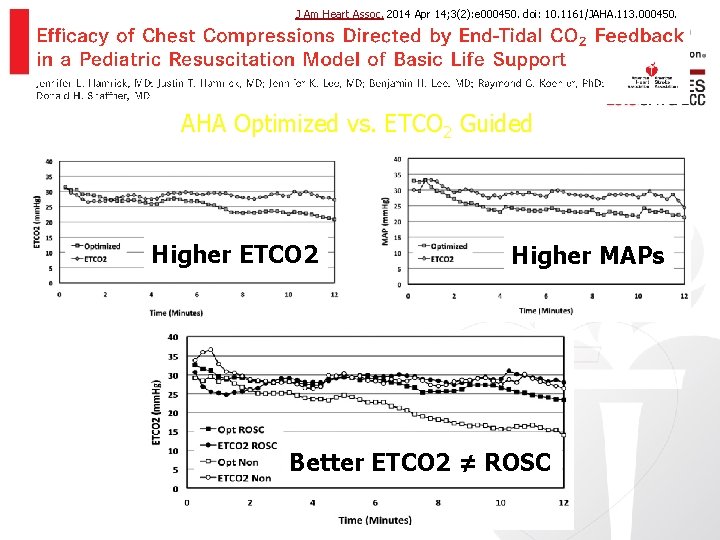
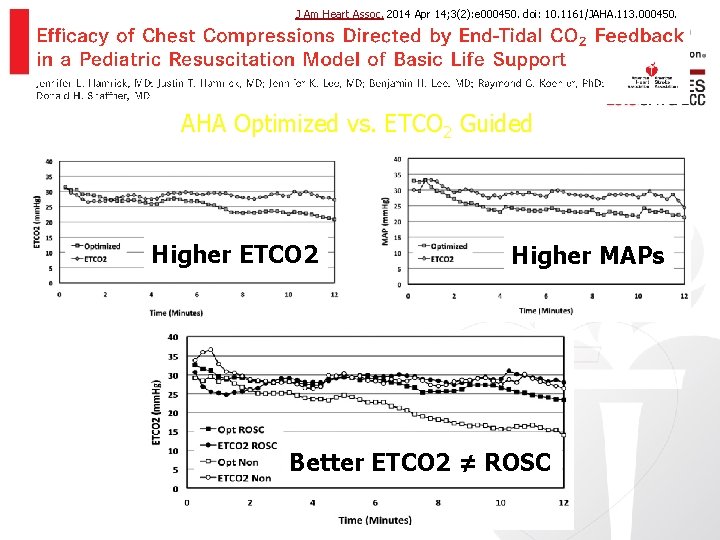
J Am Heart Assoc. 2014 Apr 14; 3(2): e 000450. doi: 10. 1161/JAHA. 113. 000450. AHA Optimized vs. ETCO 2 Guided Higher ETCO 2 Higher MAPs Better ETCO 2 ≠ ROSC
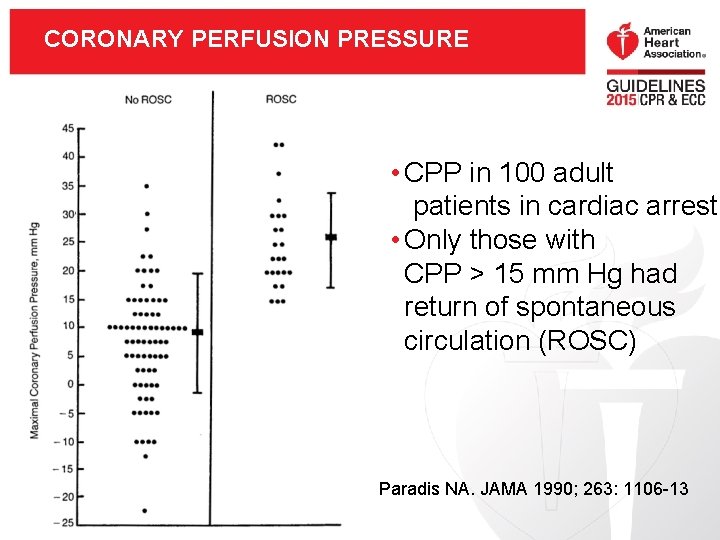
CORONARY PERFUSION PRESSURE • CPP in 100 adult patients in cardiac arrest • Only those with CPP > 15 mm Hg had return of spontaneous circulation (ROSC) Paradis NA. JAMA 1990; 263: 1106 -13

KEY NEW AND UPDATED RECOMMENDATIONS: FIRST AID
FIRST AID TOPICS (I) • Stroke assessment systems can help identify stroke signs and symptoms • Glucose tablets preferred for mild hypoglycemia, but specific candies may be useful • Open chest wound should be left open; dressings should not become occlusive • If symptoms of anaphylaxis do not resolve with an initial epinephrine autoinjector dose, second dose may be considered.
FIRST AID: CONCUSSION • As soon as possible, healthcare provider should evaluate any person with a head injury resulting in –Change in level of consciousness –Progressive development of signs or symptoms of concussion –Other causes of concern • Currently no validated tool to identify concussion available for use by first aid providers
FIRST AID TOPICS (II) • No evidence supporting the routine use of oxygen as first aid measure • Adults experiencing chest pain may chew 1 adult or 2 low dose aspirins (enteric coated or regular)
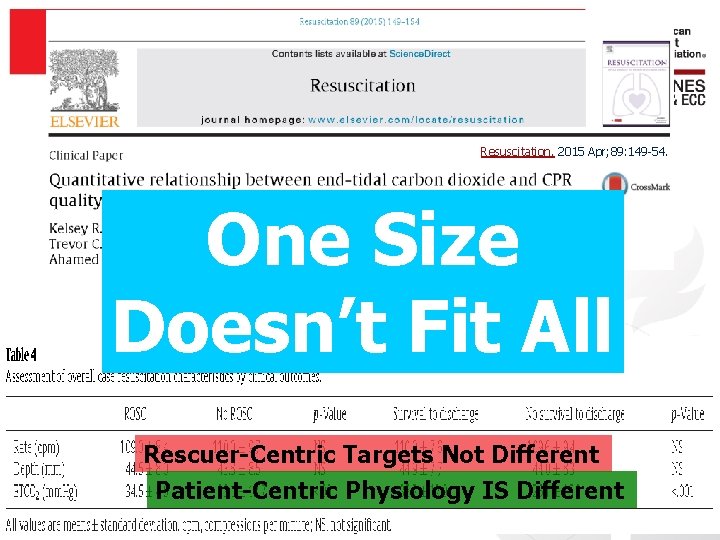
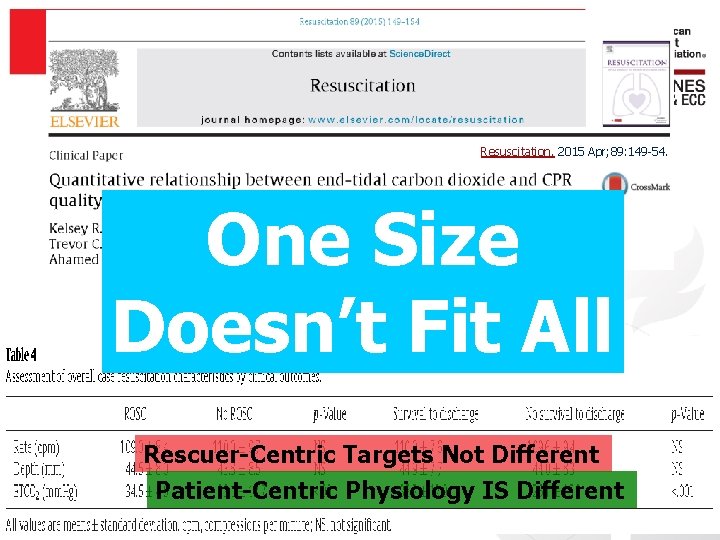
Resuscitation. 2015 Apr; 89: 149 -54. One Size Doesn’t Fit All 583 cardiac arrest events (both OHCA and IHCA) ~30, 000 chest compressions analyzed Rescuer-Centric Targets Not Different Patient-Centric Physiology IS Different
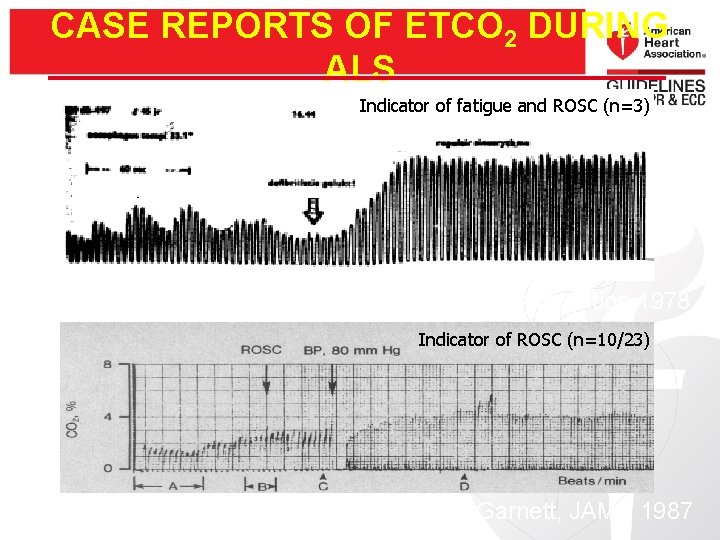
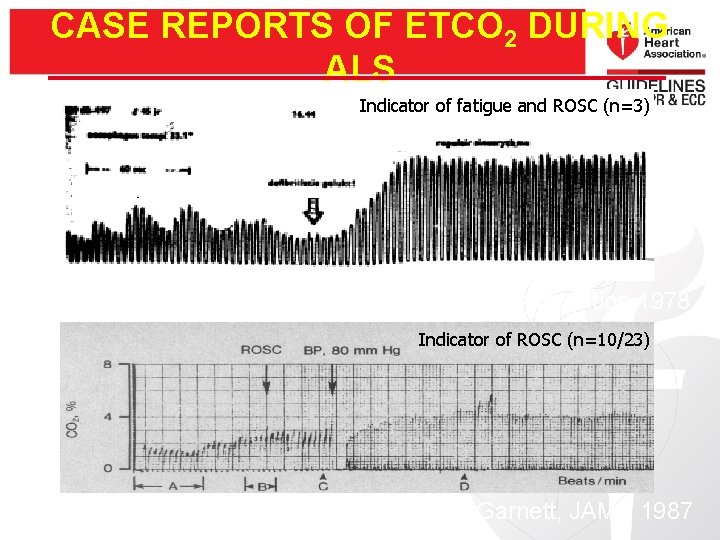
CASE REPORTS OF ETCO 2 DURING ALS Indicator of fatigue and ROSC (n=3) Kalenda, Resuscitation 1978 Indicator of ROSC (n=10/23) Slide courtesy of Bobby Sutton Garnett, JAMA 1987
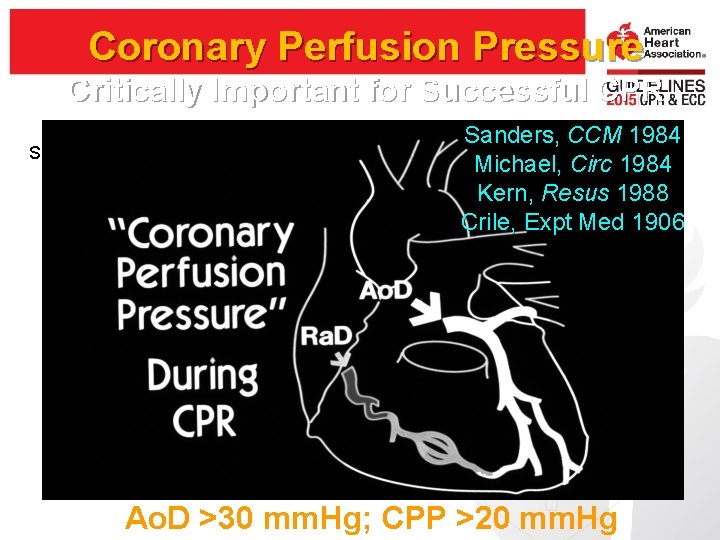
Coronary Perfusion Pressure Critically Important for Successful CPR Slide courtesy Nadkarni, Berg Sanders, CCM 1984 Michael, Circ 1984 Kern, Resus 1988 Crile, Expt Med 1906 Ao. D >30 mm. Hg; CPP >20 mm. Hg
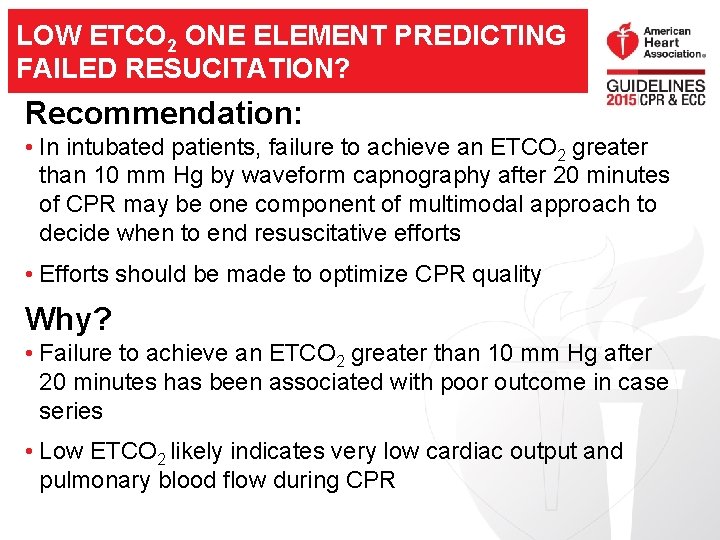
LOW ETCO 2 ONE ELEMENT PREDICTING FAILED RESUCITATION? Recommendation: • In intubated patients, failure to achieve an ETCO 2 greater than 10 mm Hg by waveform capnography after 20 minutes of CPR may be one component of multimodal approach to decide when to end resuscitative efforts • Efforts should be made to optimize CPR quality Why? • Failure to achieve an ETCO 2 greater than 10 mm Hg after 20 minutes has been associated with poor outcome in case series • Low ETCO 2 likely indicates very low cardiac output and pulmonary blood flow during CPR
ACUTE CORONARY SYNDROMES (ACS) Reperfusion Recommendations • Prehospital triage and transport to a PCI center may be preferred to prehospital fibrinolysis • Immediate transfer without fibrinolysis to a PCI center when STEMI occurs in a non. PCI capable hospital Why? • Slightly lower incidence of intracranial hemorrhage with primary PCI
TROPONINS + RISK ASSESSMENT TO IDENTIFY LOW RISK OF ACS Biomarkers Plus Risk Stratification Recommendation • High-sensitivity troponin T and troponin I levels less than 99 th percentile at 0 and 2 hours PLUS low-risk stratification may be used • Negative troponin I or T at 0 and 3 -6 hours PLUS very low risk stratification may be used Why? • High sensitivity and specificity documented