Coronary Heart Disease NUR 224 Coronary Heart Disease











- Slides: 89
Coronary Heart Disease NUR -224
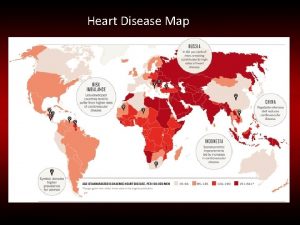
Coronary Heart Disease Affects 16 million people Causes more than 600, 000 death annually Caused by impaired blood flow to the myocardium Accumulation of atherosclerotic plaque in the coronary arteries usual cause. • May be asymptomatic or may lead to angina pectoris, acute coronary care syndrome, myocardial infarction (MI/heart attack), dysrhythmias, heart failure and even sudden death • •
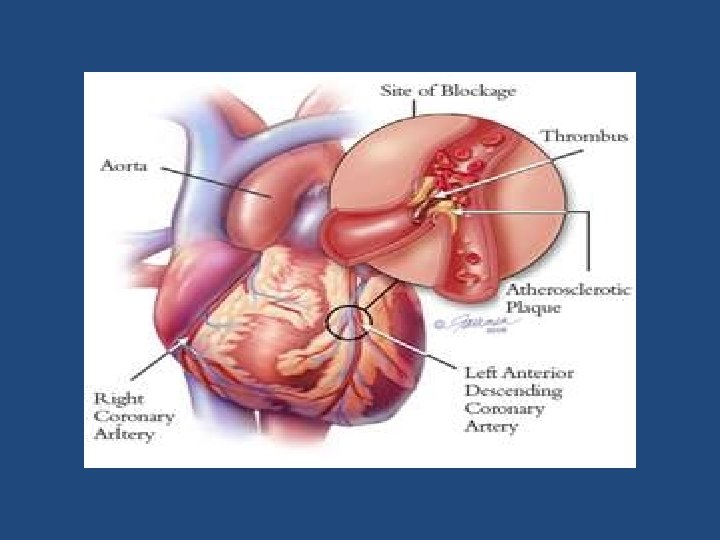
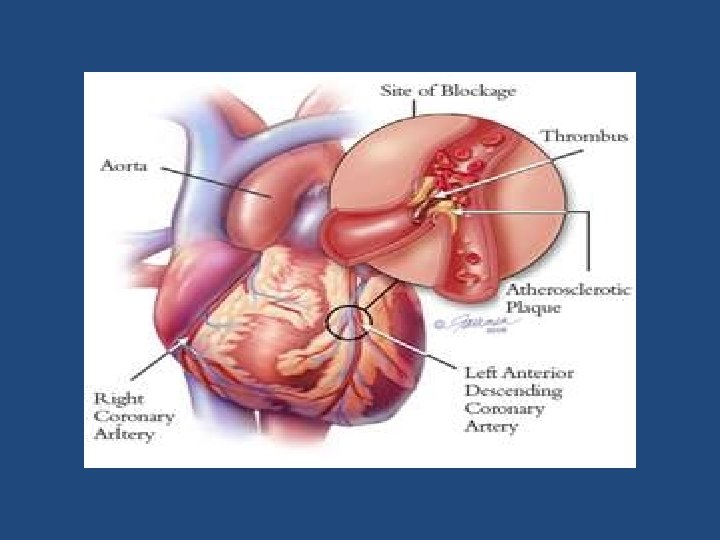
Coronary Atherosclerosis • Atherosclerosis is the abnormal accumulation of lipid deposits within arterial walls and lumen. • In coronary atherosclerosis, blockages and narrowing of the coronary vessels reduce blood flow to the myocardium.
Coronary Heart Disease Risk Factors • age (over 50) • heredity • smoking • obesity • high serum cholesterol levels • hypertension • diabetes mellitus
Angina Pectoris • Characterized by chest pain and usually precipitated by exercise and relieved by rest. • Myocardial oxygen needs are greater than partially occluded vessels can supply, myocardial cells become ischemic and shift to anaerobic metabolism • produces lactic acid that stimulates the nerve endings in the muscle pain • Pain subsides when oxygen supply meets myocardial demand.
Angina Pectoris • Chest pain reduced coronary blood flow temporary imbalance between myocardial blood supply and demand • This causes temporary/reversible myocardial ischemia. • More than 30 minutes of ischemia irreversibly damages myocardial cells (necrosis)
Types of Angina § § Stable angina Unstable angina Silent Ischemia Variant angina (Prinzmetal’s angina)
Stable Angina • Occurs with a predictable amount of activity or stress • Predictable and common • Occurs when the work of the heart is increased by physical exertion, exposure to cold, or by stress • Sensation may occur neck, jaw, shoulders • Lasts for few minutes – 5/15 minutes • Relieved by rest and/or nitrates
Unstable Angina § Occurs with increasing frequency, severity and duration § Pain is unpredictable and occurs with decreasing levels of activity or stress and may occur at rest. § Patients at risk for myocardial infarction § May not be relieved by NTG or rest
Variant Angina (Prinzmetal’s) • Atypical angina that occurs unpredictably • Caused by coronary artery spasm with/out atherosclerotic lesion • Often occurs at night
Silent Ischemia • Occurs in the absence of any subjective symptoms (asymptomatic) • Patient reports no pain • May occur with either activity or mental stress
Clinical Manifestations § § Chest pain Precipitated by an identifiable event. Classic sequence Women frequently present with atypical symptoms of angina
Angina Pain Manifestations § Chest Pain § Quality § Associated manifestations § Atypical manifestations § Precipitating factors § Relieving factors
Assessment/Diagnostic Findings o Past medical history/family history o Comprehensive description of chest pain o Presence of risk factors o Electrocardiography o Echocardiography o Cardiac stress testing o Cardiac Angiography
Medical Management § Focus on maintaining coronary blood flow and cardiac function § Measures to restore coronary blood flow (later) § Pharmacologic therapy * nitrates * beta blockers * calcium channel blockers * aspirin
Nitrates • SL NTG -> acute angina attacks (Buccal spray) • Acts within 1 -2 minutes Long acting nitroglycerin • Used to prevent attacks not treat an acute attack. • Headache, hypotension, nausea, dizziness • NTG, Nitrostat, Nitro-bid
Nitrates • Nursing Responsibilities • Patient Teaching
B –Adrenergic Blockers § Decrease myocardial contractility, HR, BP which will reduce myocardial oxygen demand § Side effects bradycardia, hypotension, wheezing, GI complaints. § Contraindicated for patient with asthma § Metoprolol (Lopressor), Atenolol(Tenormin), Carvedilol (Coreg)
Beta Blockers Nursing Responsibilities Patient Teaching
Calcium Channel Blockers • Decrease the workload of the heart • Relax blood vessels decrease BP and increase coronary perfusion • Potent coronary vasodilator • Amlodipine (Norvasc), Diltiazem(Cardizem), Felodipine (Plendil) • Used to treat Variant Angina
Aspirin • Prevent platelet aggregation/thrombus formation • Reduces the incidence of MI • 80 -325 mg of aspirin as soon as dx. is made • If patient is taking Tylenol – should continue to take aspirin • GI upset – H 2 blocker, PPI
Nursing Diagnosis • Ineffective Cardiac Tissue Perfusion • Deficient Knowledge • Risk for Ineffective Therapeutic Regimen Management

Acute Coronary Syndrome § Condition of unstable cardiac ischemia § Includes unstable angina and acute myocardial ischemia c/out significant injury of myocardial tissue § Coronary blood flow is acutely reduced, but not fully occluded. Myocardial cells are injured by the acute ischemia that results. § Most people have stenosis of one or more coronary arteries.
Acute Coronary Syndrome Cardinal manifestation § Chest pain – substernal/epigastric § Dyspnea § Diaphoresis § Pallor § Cool skin § Tachycardia § Hypotension
Acute Coronary Care Syndrome Diagnosis • ECG • Cardiac Markers *Cardiac muscle troponins (sensitive indicators of myocardial damage) * Creatine Kinase (CK) & CK-MB (specific to myocardial muscle)
Medications • Reduce myocardial ischemia • Reduce risk for blood clotting • Nitrates • Beta blockers • Antiplatelet (po/IV)
Oral Antiplatelet -Medication • • Aspirin Clopidogrel (Plavix) Ticlopidine (Ticlid) Suppress platelet aggregation, prevents the development of thrombus. • Nursing responsibilities • Patient Education
IV Antiplatelet • Tirofiban (Aggrastat) • Eptifibatide (Integrilin) • IV antiplatelets more effective than oral administered meds but the risk of bleeding is greater
Heparin Prevents the formation of new clots Reducers the occurrence of MI IV bolus/then continuous infusion Infusion based on PTT – 2 -2. 5 times the normal PTT value (25 -35 sec. ) • LMWH – Lovenox/Fragmin • All increase the risk of bleeding : bleeding precautions • •
Revascularization Procedures • Several procedures may be used to restore blood flow and oxygen to ischemic tissue. Nonsurgical techniques: • percutaneous coronary revascularization • coronary atherectomy • intracoronary stents • coronary artery bypass graft (surgical procedure may be used)
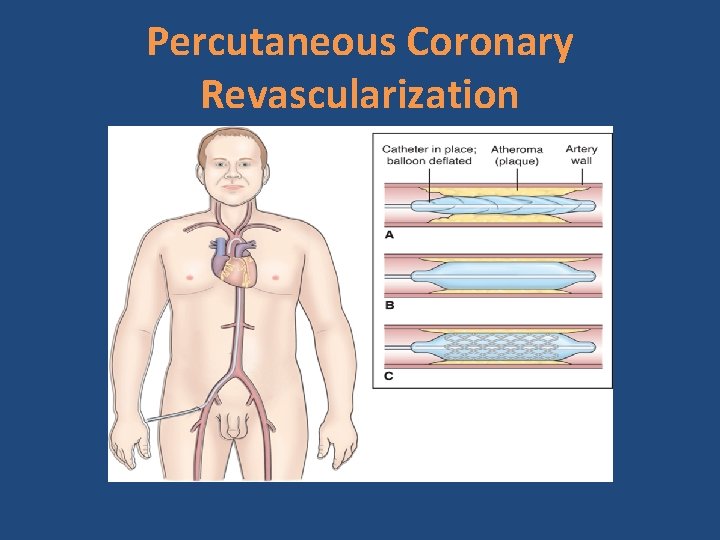
Percutaneous Coronary Revascularization Is recommended for patients: • Fail medical management • Have left main coronary artery/three vessel disease • Are not candidates for PCI • Have failed PCI with ongoing chest pain
Percutaneous Coronary Intervention Goal: open the affected artery within 90 minutes of arrival to a facility Advantages: • Alternative to surgical intervention • Performed with local anesthesia • Patient is ambulatory 24 hours after the procedure • Hospital stay shorter • Patient can return to work
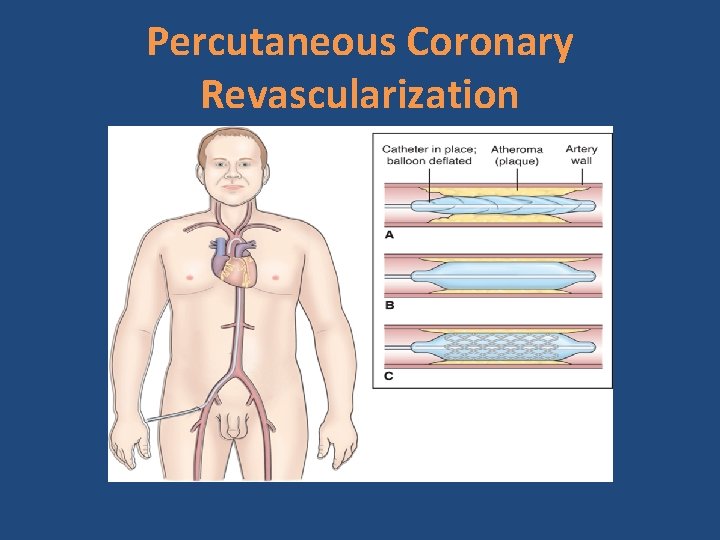
Percutaneous Coronary Revascularization • A balloon-tipped catheter is threaded over the guide wire • Balloon is inflated for about 30 sec. -2 minutes to compress the plaque against the arterial wall • The stent is then placed over a balloon catheter and expanded as the balloon is inflated • It remains in the artery when the balloon is removed.
Percutaneous Coronary Intervention Post procedure care: • Assess vital signs • Bedrest/ flat in bed • Affected leg straight • Pressure dressing applied • Monitor for bleeding/hematoma • Resume self-care activities/ambulation few hours after procedure
Percutaneous Coronary Revascularization
Atherectomy • Remove plaque from the identified lesion • Catheter shaves the plaque off vessels walls using a rotary cutting head - retaining the fragments in it compartment and removing them from the vessel. • Rotation catheter pulverize the plaque into particles small enough to pass through the coronary microcirculation.

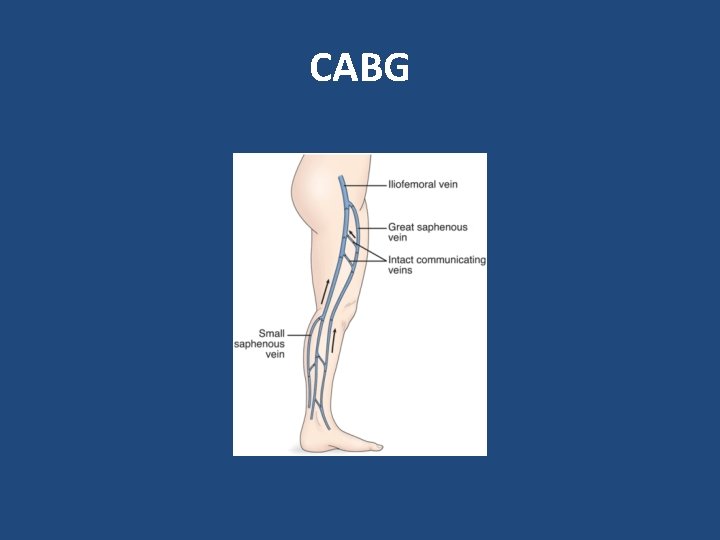
CABG • Involves using a section of a vein /artery to create a connection (bypass) between the aorta and the coronary artery beyond construction. • This allows blood to perfuse the ischemic portion of the heart. • Internal mammary artery in the chest/saphenous vein from the leg are the vessels most commonly used.
CABG Surgery Internal mammary artery – is commonly used. Remains palliative treatment and not a cure. Improves quality of life/patient outcomes Postoperative complications/mortality increase as a function of age. • Women have a higher mortality rate than men • •

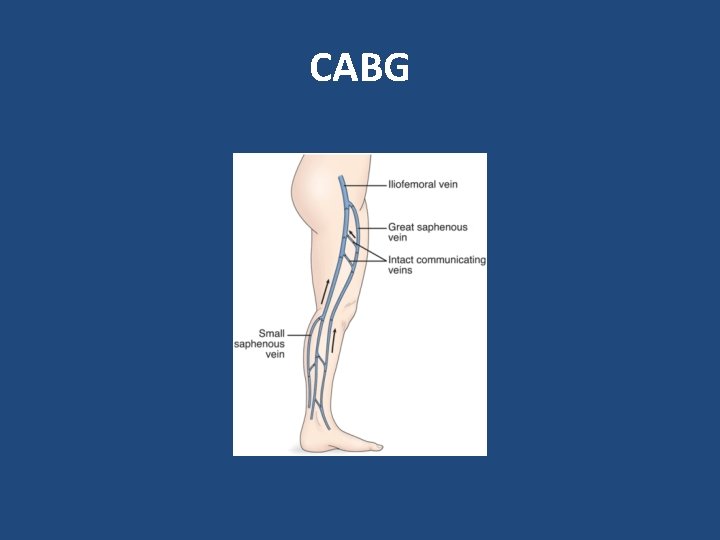
CABG
Patient teaching • Lifestyle changes and reduction of risk factors • Explore, recognize, and adapt behaviors to avoid to reduce the incidence of episodes of ischemia • Teaching regarding disease process • Cardiac rehabilitation • Stress reduction • When to seek emergency care

Myocardial Infarction • An area of the myocardium is permanently destroyed necrosis of the myocardial cells. If circulation to the affected myocardium is not promptly restored , the heart loses the ability to maintain effective cardiac output. • Life-threatening event • May lead to cardiogenic shock and death
Myocardial Infarction • Annually 785, 000 experience their first MI • Majority of deaths from MI occur during the initial period after symptoms begin: 60% within the first hour 40% prior to hospitalization • Medical treatment and training in CPR are vital to decrease deaths due to MI.
Myocardial Infarction • The area of infarction develops over minute to hours. • Cellular ischemia affects conduction and myocardial contractility • Myocardial contractility decreases, increasing the risk for dysrhythmias, subsequently reducing cardiac output, B/P, and tissue perfusion
Myocardial Infarction • When a larger artery is compromised, collateral vessels connecting smaller arteries in the coronary system dilate to maintain blood flow to the cardiac muscle. • The degree of collateral circulation determines the extent of myocardial damage. • Occlusion of coronary artery without any collateral vessels massive tissue damage and death
Clinical Manifestations • Pain – sudden and usually not associated with activity • Women/older adults atypical chest pain, elevated BP & HR initially, then ↓’es • Nausea/vomiting • Fever • Dyspnea, shortness of breath • Anxiety , sense of impending doom

Collaborative Care Goals • Relieve chest pain • Reduce the extent of myocardial damage • Maintain cardiovascular stability • Decrease cardiac workload • Prevent complications
Assessment/ Diagnostic Findings • ECG • Laboratory tests— serum cardiac biomarkers CK-MB Myoglobin Troponin CBC Echocardiogram
Laboratory Tests Serum Cardiac Markers • Are proteins released into the blood from necrotic heart muscle • They occur after cellular death indicates cardiac damage • Creatine kinase (CK-MB) and troponin are measured to diagnose an MI.
Serum Cardiac Markers Creatine kinase (CK ) • Important enzyme for cellular function • Found mainly in cardiac muscle (skeletal muscle/brain) • Begin to rise rapidly with damage to these tissues at about 4/6 hours after an MI , peak at about 12/24 hours and return to normal within 36/48 hours • CK correlates with the size of the infarction
Serum Cardiac Markers CPK-MB • Subset of CK specific to cardiac muscle • Most sensitive indicating of MI • Elevated CK –alone is not specific for MI • Elevated CPK-MB positive indicator of MI • Does not normally rise with chest pain from angina or other causes other than MI
Serum Cardiac Markers Troponin • Regulates the myocardial contractility process • Proteins released during myocardial infarction – are sensitive indicators of myocardial damage. • Necrosis of cardiac muscle, troponins are released and blood levels rise. • Is a highly cardiac specific indicator of an MI • Increases with 4 -6 hours during an acute MI, remains elevated for a long period -- 3 weeks
Serum Cardiac Markers Myoglobin • Helps transport oxygen • Found in cardiac and skeletal muscle • Levels start to increase within 1 -3 hours of symptom onset return to normal within 24 hours after onset of symptoms. • Is one of the first cardiac markers to appear after MI, it lacks cardiac specificity. • Kidneys rapidly excrete it in urine blood levels return to normal range within 24 hours.
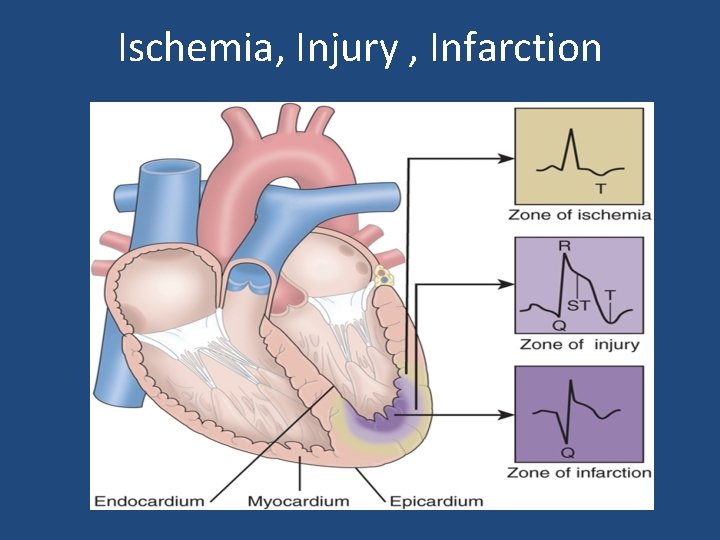
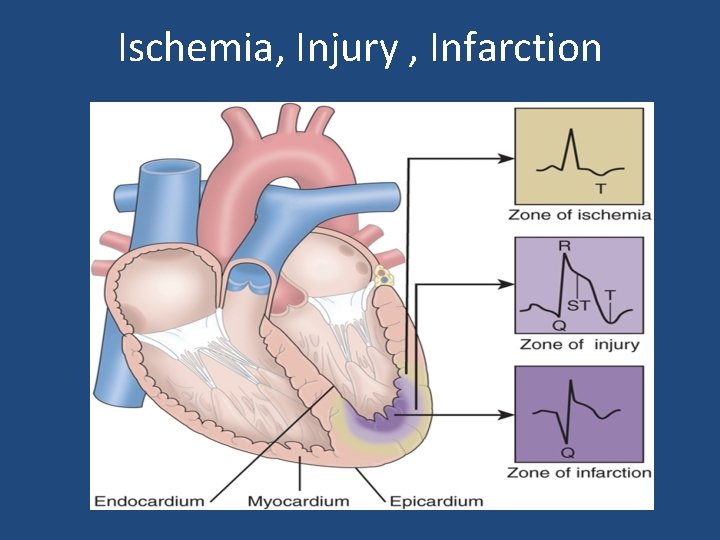
Ischemia, Injury , Infarction
COMPLICATIONS • Heart failure • Cardiogenic shock • Dysrhythmias and cardiac arrest
Interdisciplinary Care Immediate treatment goals for the MI q Relieve the chest pain q Reduce the extent of myocardial damage q Decrease the cardiac workload q Prevent complications
Treatment of Acute MI • Obtain diagnostic tests including ECG within 10 minutes of admission to the ED • Oxygen • Aspirin, nitroglycerin, morphine, beta-blockers fibrinolytic therapy • Revascularization Procedures • As indicated: IV heparin, LMWH • Bed rest
Nursing Interventions • Pain stimulates the SNS, increasing cardiac work. Pain relief is a priority. Acute Pain § Assess for verbal and nonverbal signs of pain § Administer oxygen 2 -5 L/min via nasal cannula § Promote physical and psychologic rest § Titrate IV nitroglycerin as ordered § Administer morphine by IV push for chest pain as needed
Nursing Interventions Ineffective Tissue Perfusion § Assess and document vital signs § Assess for changes in LOC § Auscultate heart and breath sounds § Monitor ECG Administer antidysrhythmic medications § Monitor oxygen saturation
Nursing Interventions Fear § Acknowledge the client’s perception of the situation § Encourage questions/ provide consistent, factual answers § Encourage self-care § Administer anti-anxiety medications as ordered § Teach non-pharmacologic methods

HEART FAILURE
Heart Failure • Complex syndrome resulting from cardiac disorders that impair the ventricles’ ability to fill and effectively pump blood • Inability of the heart to pump sufficient blood to meet the metabolic demands of the body. • 5. 7 million people in the US have heart disease. • HF is increasing in incidence and prevalence. • Primarily a disease of older adults. • HF is associated with high morbidity/mortality rates
HEART FAILURE • Heart failure develops cardiac output falls decrease in tissue perfusion. • Is a disorder of cardiac function • Hypertension and CHD are the leading causes of heart failure • The prognosis for the client with heart failure depends on the underlying cause and how effectively the precipitating factors can be treated. • Most clients with heart failure die within 8 years of the diagnosis. • Ejection fraction – provides information about the (L) ventricle during systole. Normal 55 -65%.
Pathophysiology • Decrease cardiac output activation of compensatory mechanisms neurohormonal response decrease in renal perfusion & increase vasoconstriction sodium and water retention fluid overload increase the workload of the heart

Etiology • CAD and advancing age are the primary risk factors for HF • CAD is found in more than 60% of patients • Other factors: hypertension, diabetes, cigarette smoking, obesity,
Manifestations of Heart Failure • CHD/hypertension are common causes of L-sided heart failure whereas R- heart failure caused by conditions that restrict blood flow to the lungs (acute/chronic pulmonary disease). Left sided heart failure can lead to right sided heart failure.
Classification of Heart Failure Left-sided heart failure • Most common form of HF • LV cannot pump blood effectively to the systemic circulation. Pulmonary venous pressures increase and result in pulmonary congestion with dyspnea, cough, crackles, and impaired oxygen exchange. • This increase pulmonary pressure pulmonary congestion and edema
Types of Heart Failure Manifestation of L-sided heart failure result from pulmonary congestion (backward effects) and decreased cardiac output (forward effects). § Fatigue and activity intolerance § Dizziness and syncope § Pulmonary congestion § Cyanosis § Rales/wheezing

Types of Heart Failure Right sided heart failure • Causes a back up of blood to the ( R) atrium • RV cannot eject sufficient amounts of blood into the pulmonary circulation blood backs up in the venous system. • Increase venous pressure causes abdominal organs to become congested /peripheral edema develops • This results in peripheral edema, ® upper quadrant pain, ascites, anorexia, nausea, weakness, and weight gain.

Multisystem Effects of Heart Failure v Neurologic v Respiratory v Cardiovascular v Gastrointestinal v Genitourinary v Integumentary v Metabolic
Diagnostic Studies • • • BNP levels – key diagnostic indicator of HF Serum electrolytes Liver function tests Echocardiogram Chest x-ray Electrocardiogram
Heart Failure Hemodynamics Monitoring v Used to assess cardiovascular function in the critically/unstable client and evaluate their interventions v Hemodynamic parameters heart rate, arterial blood pressure, central venous pressure, pulmonary pressure and cardiac output

Management of Heart Failure • Eliminate or reduce etiologic or contributory factors. • Reduce the workload of the heart by reducing afterload and preload. • Optimize all therapeutic regimens. • Prevent exacerbations of heart failure. • Medications are routinely prescribed for heart failure.
Medications • • • Angiotensin-converting enzyme inhibitors Angiotensin II receptor blockers Beta-blockers Diuretics Digitalis Other medications
Other Treatment q Surgery q Circulatory assistance q Cardiac transplantation q Hemodynamic Monitoring
Complications Compensatory Mechanism • Hepatomegaly/splenomegaly • Dysrhythmias • Pulmonary problems
Nursing interventions § Decreased Cardiac Output § Excess Fluid Volume § Activity Intolerance § Diet

ACUTE CORONARY SYNDROME • ACS occurs when ischemia is prolonged and not immediately reversible resulting in myocardial cell death. • The spectrum of ACS encompasses: unstable angina(UA), non-ST-segment-elevation MI (NSTEMI), ST-segment-evaluation MI (STEMI).
 Coronary heart disease
Coronary heart disease Coronary artery disease pathophysiology
Coronary artery disease pathophysiology Coronary artery disease
Coronary artery disease Coronary circulation of heart
Coronary circulation of heart Coronary groove of heart
Coronary groove of heart Crash course heart
Crash course heart Acetilena la 600-800 grade
Acetilena la 600-800 grade 224+48
224+48 Km 224
Km 224 Asw 224
Asw 224 Iso tc 224
Iso tc 224 224 meaning
224 meaning Mat 224
Mat 224 Cs 224
Cs 224 224+48
224+48 Aci224
Aci224 Uç alkin
Uç alkin 224-176
224-176 Ece224
Ece224 Cs-224 computer organization
Cs-224 computer organization Ece 224
Ece 224 224w stanford
224w stanford Binary 10110
Binary 10110 Cs 224
Cs 224 Edu224
Edu224 Oksimerkürasyon
Oksimerkürasyon Asw 224
Asw 224 Dea form 224
Dea form 224 Soc 224
Soc 224 Item 224
Item 224 Phys 224
Phys 224 Anaphora
Anaphora Km 224
Km 224 Bharathi viswanathan
Bharathi viswanathan Coronary circulatory routes
Coronary circulatory routes Dipyrimadole
Dipyrimadole Fossa ovalis
Fossa ovalis Right atrioventricular valve
Right atrioventricular valve Acute coronary syndrome
Acute coronary syndrome Coronary sinusoids
Coronary sinusoids Qfr coronary
Qfr coronary Space of disse liver
Space of disse liver Mesa coronary calcium score
Mesa coronary calcium score Classification of antianginal drugs
Classification of antianginal drugs Annulus of vieussens
Annulus of vieussens Heart wall
Heart wall Mesa coronary calcium score
Mesa coronary calcium score Unlocking of knee joint
Unlocking of knee joint What is high quality cpr
What is high quality cpr Coronary circulation
Coronary circulation Heart disease
Heart disease Anterior cardiac veins of the right ventricle
Anterior cardiac veins of the right ventricle Pk papyrus covered coronary stent system
Pk papyrus covered coronary stent system Coronary personality
Coronary personality Pulmonary trunk
Pulmonary trunk Cag spider view
Cag spider view Coronary blood flow
Coronary blood flow Coronary sulcus
Coronary sulcus Cardiac cycle animation
Cardiac cycle animation Global registry of acute coronary events
Global registry of acute coronary events Flow of coronary circulation
Flow of coronary circulation Fossa ovalis
Fossa ovalis Coronary calcium score guidelines
Coronary calcium score guidelines Pk papyrus covered coronary stent system
Pk papyrus covered coronary stent system Alle hatten die hosen voll nur bei mir liefs flüssig
Alle hatten die hosen voll nur bei mir liefs flüssig Mezonefrik kanal
Mezonefrik kanal Nur 102
Nur 102 Yoyiq burchak
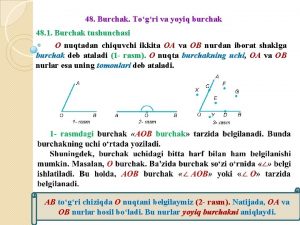
Yoyiq burchak Nur ahmad husin
Nur ahmad husin Heinz erhardt raupe
Heinz erhardt raupe Dr nur rofiah
Dr nur rofiah Iswari nur hidayati
Iswari nur hidayati Nur 680
Nur 680 Unsur jiwa
Unsur jiwa Hanif nur widhiyanti
Hanif nur widhiyanti Nur azizah umy
Nur azizah umy Hanif nur widhiyanti
Hanif nur widhiyanti Nur alia file upload
Nur alia file upload Wenn ich so liege geht's
Wenn ich so liege geht's Man kann menschen nur vor den kopf gucken
Man kann menschen nur vor den kopf gucken Makhluk sosial
Makhluk sosial Nilai dari iim
Nilai dari iim Nur endah januarti
Nur endah januarti Davetin yaygınlaşması ve sonuçları
Davetin yaygınlaşması ve sonuçları Nur muhammad taraki
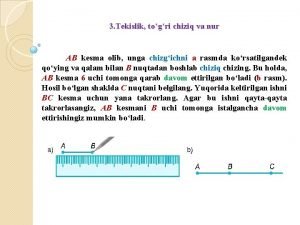
Nur muhammad taraki Kesma chizish
Kesma chizish Dr nur mohammad hadi zahalan
Dr nur mohammad hadi zahalan Nur verrückte habens eilig
Nur verrückte habens eilig Die gazelle rilke
Die gazelle rilke Struktur mikrokontroler
Struktur mikrokontroler