Coronary Circulation And Factors Affecting It Physiologic Anatomy
- Slides: 24
Coronary Circulation And Factors Affecting It
Physiologic Anatomy of the Coronary Blood Supply
• The heart has the highest oxygen consumption per tissue mass of all human organs. • The resting coronary blood flow is ∼ 250 ml/ min this represents 5% of cardiac output. • Ischaemia results when oxygen demand outstrips supply. • Blood flow to the heart occurs mainly during diastole. • Coronary blood flow is mainly determined by local oxygen demand.
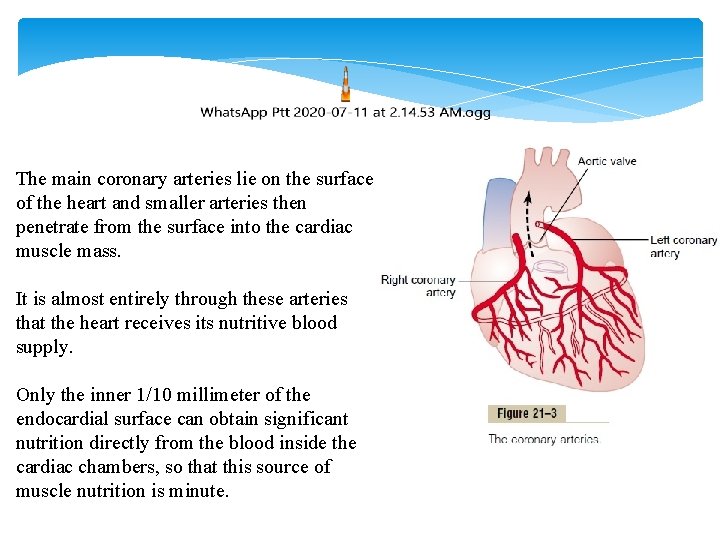
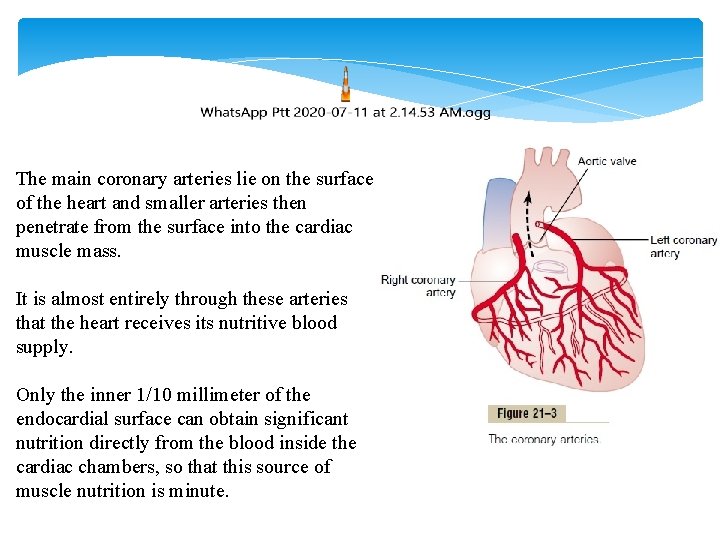
The main coronary arteries lie on the surface of the heart and smaller arteries then penetrate from the surface into the cardiac muscle mass. It is almost entirely through these arteries that the heart receives its nutritive blood supply. Only the inner 1/10 millimeter of the endocardial surface can obtain significant nutrition directly from the blood inside the cardiac chambers, so that this source of muscle nutrition is minute.
The left coronary artery supplies mainly the anterior and left lateral portions of the left ventricle, whereas the right coronary artery supplies most of the right ventricle as well as the posterior part of the left ventricle in 80 to 90 per cent of people. Most of the coronary venous blood flow from the left ventricular muscle returns to the right atrium of the heart by way of the coronary sinus—which is about 75 per cent of the total coronary blood flow. And most of the coronary venous blood from the right ventricular muscle returns through small anterior cardiac veins that flow directly into the right atrium, not by way of the coronary sinus. A very small amount of coronary venous blood also flows back into the heart through very minute thebesian veins, which empty directly into all chambers of the heart
Normal Coronary Blood Flow The resting coronary blood flow in the human being averages about 225 ml/min, which is about 4 to 5 per cent of the total cardiac output. During strenuous exercise, the heart in the young adult increases its cardiac output fourfold to seven-fold, and it pumps this blood against a higher than normal arterial pressure. Consequently, the work output of the heart under severe conditions may increase six fold to nine fold. At the same time, the coronary blood flow increases threefold to fourfold to supply the extra nutrients needed by the heart. This increase is not as much as the increase in workload which means that the ratio of energy expenditure by the heart to coronary blood flow increases.
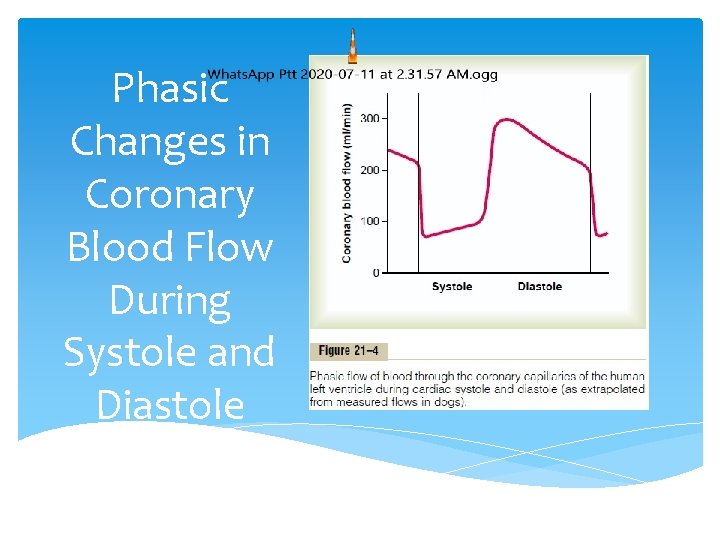
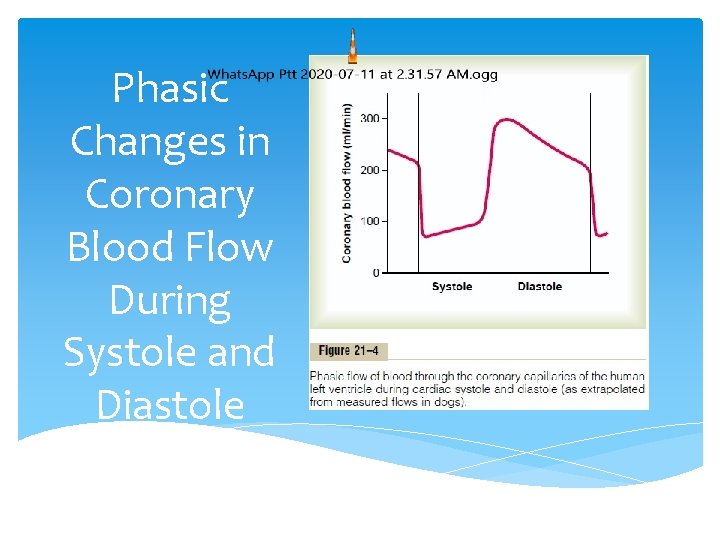
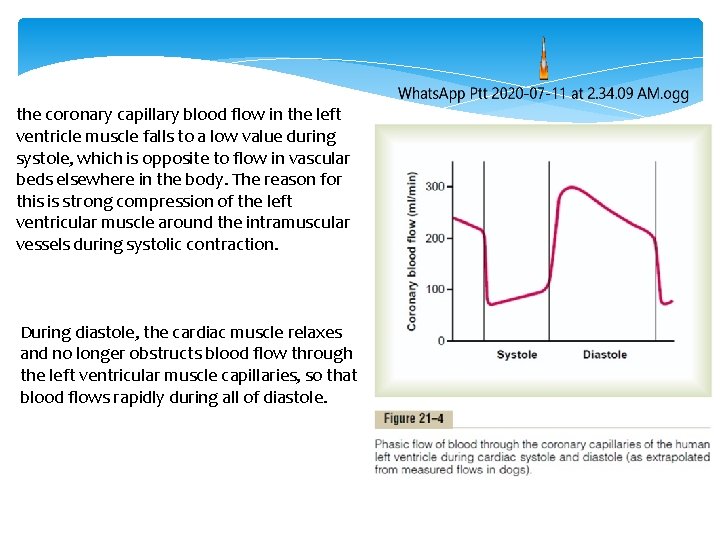
Phasic Changes in Coronary Blood Flow During Systole and Diastole
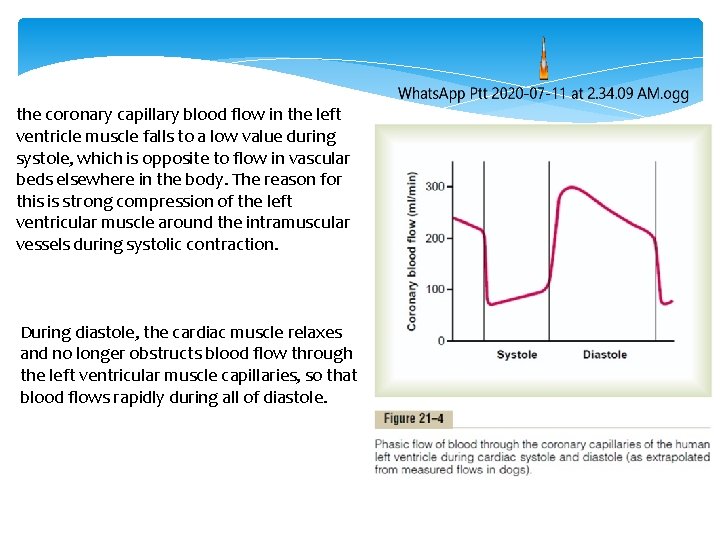
the coronary capillary blood flow in the left ventricle muscle falls to a low value during systole, which is opposite to flow in vascular beds elsewhere in the body. The reason for this is strong compression of the left ventricular muscle around the intramuscular vessels during systolic contraction. During diastole, the cardiac muscle relaxes and no longer obstructs blood flow through the left ventricular muscle capillaries, so that blood flows rapidly during all of diastole.
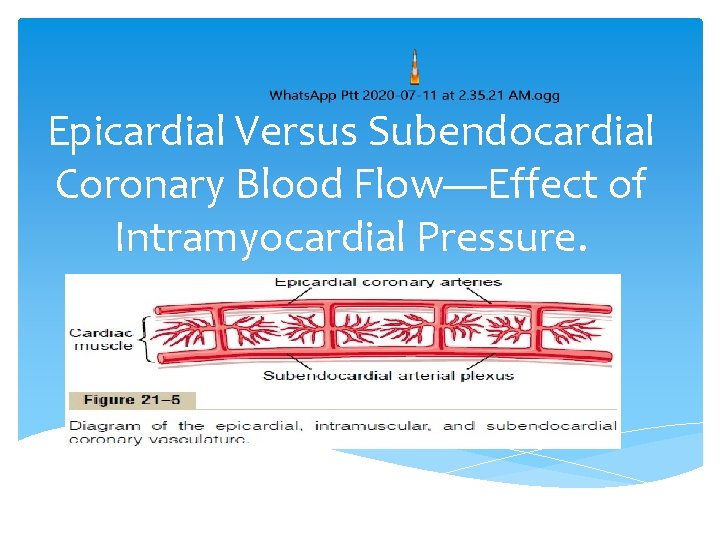
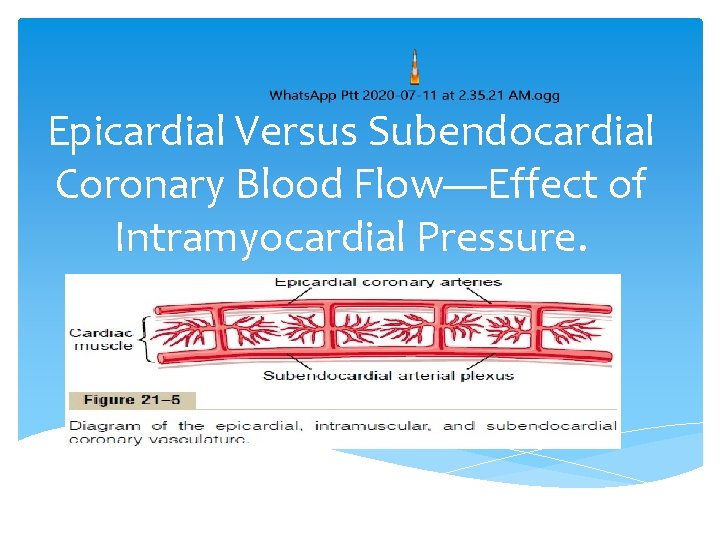
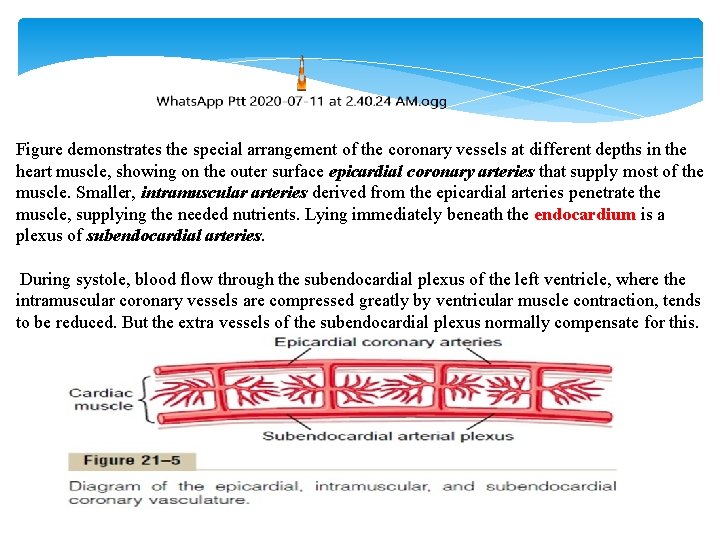
Epicardial Versus Subendocardial Coronary Blood Flow—Effect of Intramyocardial Pressure.
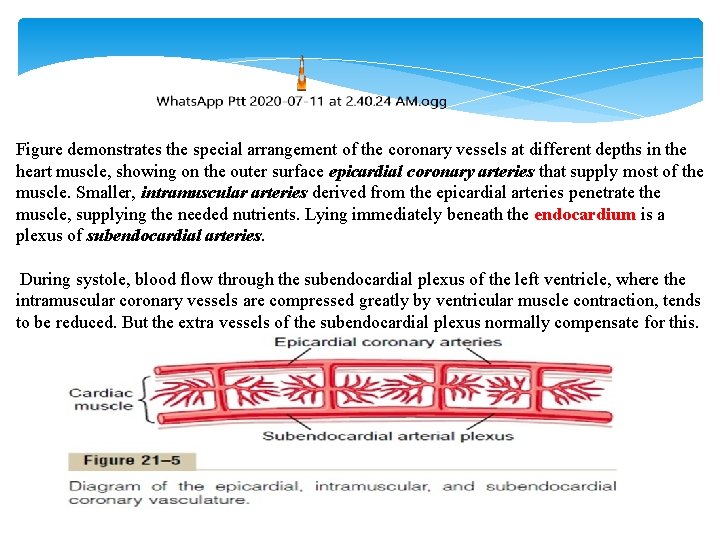
Figure demonstrates the special arrangement of the coronary vessels at different depths in the heart muscle, showing on the outer surface epicardial coronary arteries that supply most of the muscle. Smaller, intramuscular arteries derived from the epicardial arteries penetrate the muscle, supplying the needed nutrients. Lying immediately beneath the endocardium is a plexus of subendocardial arteries. During systole, blood flow through the subendocardial plexus of the left ventricle, where the intramuscular coronary vessels are compressed greatly by ventricular muscle contraction, tends to be reduced. But the extra vessels of the subendocardial plexus normally compensate for this.
Control of Coronary Blood Flow Local Muscle Metabolism Is the Primary Controller of Coronary Flow
Blood flow through the coronary system is regulated mostly by local arteriolar vasodilation in response to cardiac muscle need for nutrition. That is, whenever the vigour of cardiac contraction is increased, regardless of cause, the rate of coronary blood flow also increases. Conversely, decreased heart activity is accompanied by decreased coronary flow. This local regulation of coronary blood flow is almost identical to that occurring in many other tissues of the body, especially in the skeletal muscles all over the body.
Oxygen Demand as a Major Factor in Local Coronary Blood Flow Regulation.
Blood flow in the coronaries usually is regulated almost exactly in proportion to the need of the cardiac musculature for oxygen. Normally, about 70 per cent of the oxygen in the coronary arterial blood is removed as the blood flows through the heart muscle. Because not much oxygen is left, very little additional oxygen can be supplied to the heart musculature unless the coronary blood flow increases. Fortunately, the coronary blood flow does increase almost in direct proportion to any additional metabolic consumption of oxygen by the heart.
However, the exact means by which increased oxygen consumption causes coronary dilation has not been determined. It is speculated by many research workers that a decrease in the oxygen concentration in the heart causes vasodilator sub-stances to be released from the muscle cells and that these dilate the arterioles. A substance with great vasodilator propensity is adenosine. In the presence of very low concentrations of oxygen in the muscle cells, a large proportion of the cell’s ATP degrades to adeno-sine monophosphate; then small portions of this are further degraded and release adenosine into the tissue fluids of the heart muscle, with resultant increase in local coronary blood flow. After the adenosine causes vasodilation, much of it is reabsorbed into the cardiac cells to be reused. Adenosine is not the only vasodilator product that has been identified. Others include adenosine phosphate compounds, potassium ions, hydrogen ions, carbon dioxide, bradykinin, and, possibly, prostaglandins and nitric oxide.
Nervous Control of Coronary Blood Flow
Stimulation of the autonomic nerves to the heart can affect coronary blood flow both directly and indirectly. The direct effects result from action of the nervous transmitter substances acetylcholine from the vagus nerves and norepinephrine and epinephrine from the sympathetic nerves on the coronary vessels them-selves. The indirect effects result from secondary changes in coronary blood flow caused by increased or decreased activity of the heart.
The indirect effects, which are mostly opposite to the direct effects, play a far more important role in normal control of coronary blood flow. Thus, sympathetic stimulation, which releases norepinephrine and epinephrine, increases both heart rate and heart contractility as well as increases the rate of metabolism of the heart. In turn, the increased metabolism of the heart sets off local blood flow regulatory mechanisms for dilating the coronary vessels, and the blood flow increases approximately in proportion to the metabolic needs of the heart muscle. In contrast, vagal stimulation, with its release of acetylcholine, slows the heart and has a slight depressive effect on heart contractility. These effects in turn decrease cardiac oxygen consumption and, therefore, indirectly constrict the coronary arteries.
Direct Effects of Nervous Stimuli on the Coronary Vasculature. The distribution of parasympathetic (vagal) nerve fibers to the ventricular coronary system is not very great. However, the acetylcholine released by parasympathetic stimulation has a direct effect to dilate the coronary arteries.
There is much more extensive sympathetic innervation of the coronary vessels. the sympathetic transmitter substances norepinephrine and epinephrine can have either vascular constrictor or vascular dilator effects, depending on the presence or absence of constrictor or dilator receptors in the blood vessel walls. The constrictor receptors are called alpha receptors and the dilator receptors are called beta receptors. Both alpha and beta receptors exist in the coronary vessels.
In general, the epicardial coronary vessels have a majority of alpha receptors, whereas the intramuscular arteries may have a majority of beta receptors. Therefore, sympathetic stimulation cause slight coronary constriction or dilation, but usually constriction. In some people, the alpha vasoconstrictor effects seem to be severe, and these people can have vasospastic myocardial ischemia during periods of excess sympathetic drive, often with resultant anginal pain.
Thank you