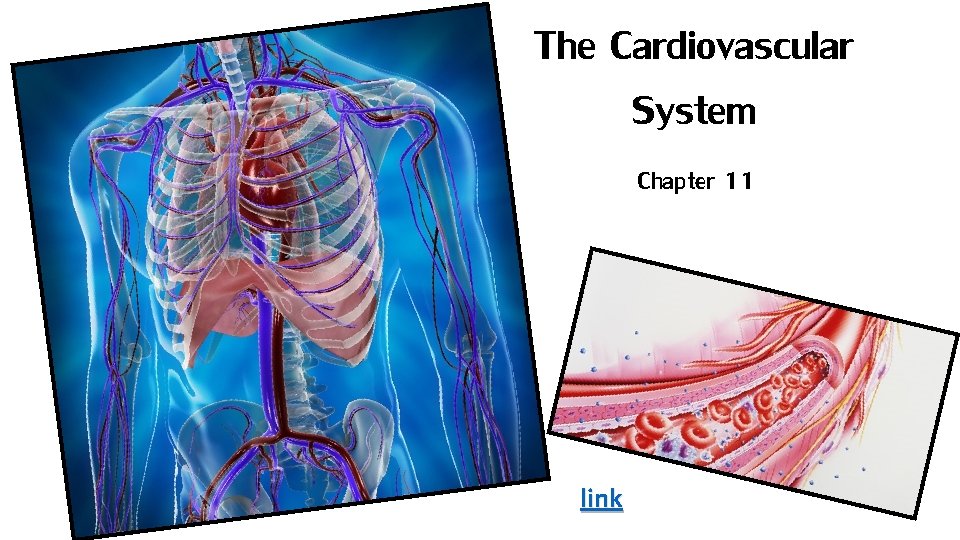
The Cardiovascular System Chapter 11 link Cardiovascular Overview


- Slides: 45
The Cardiovascular System Chapter 11 link
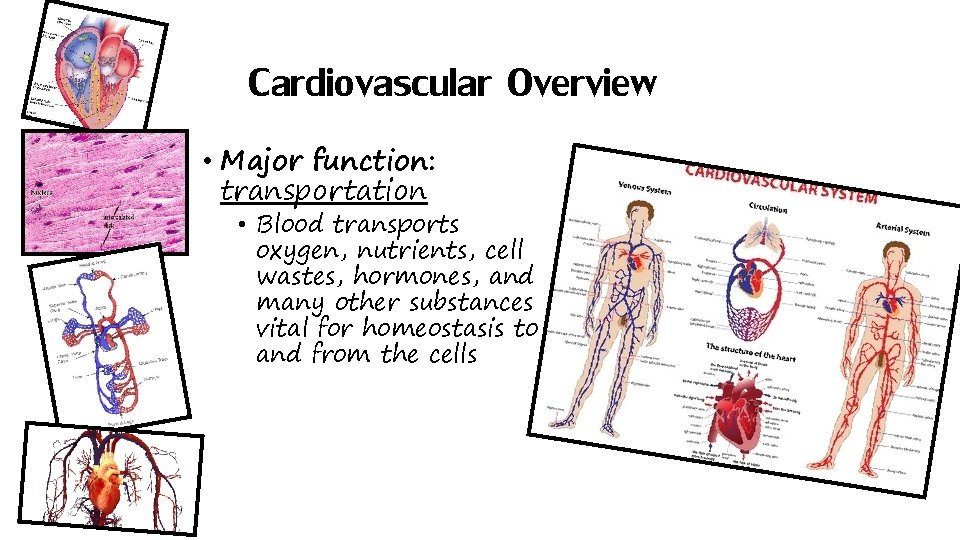
Cardiovascular Overview • Major function: transportation • Blood transports oxygen, nutrients, cell wastes, hormones, and many other substances vital for homeostasis to and from the cells
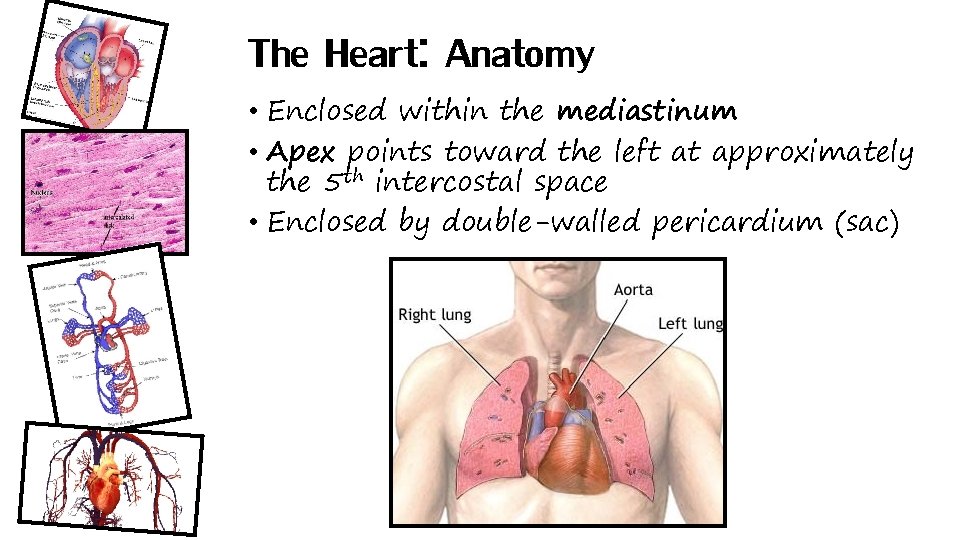
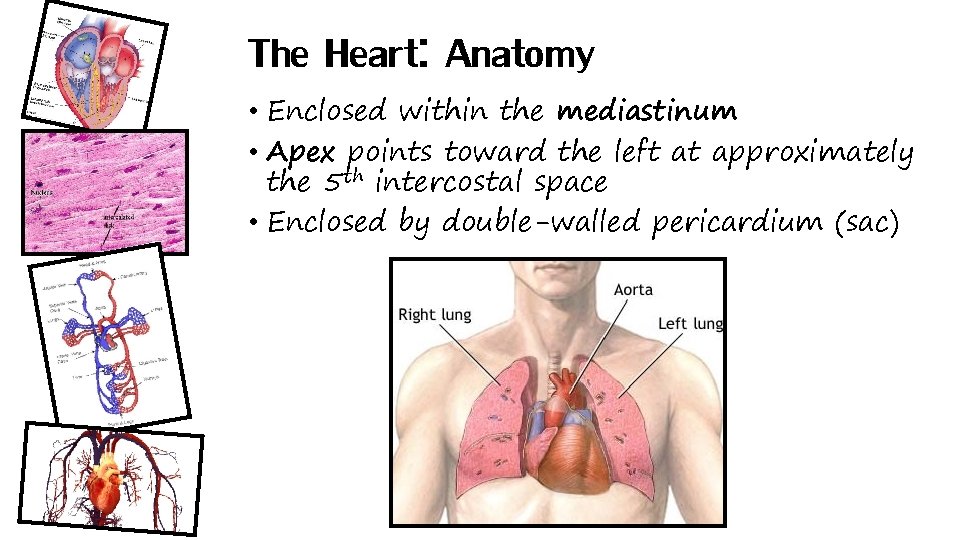
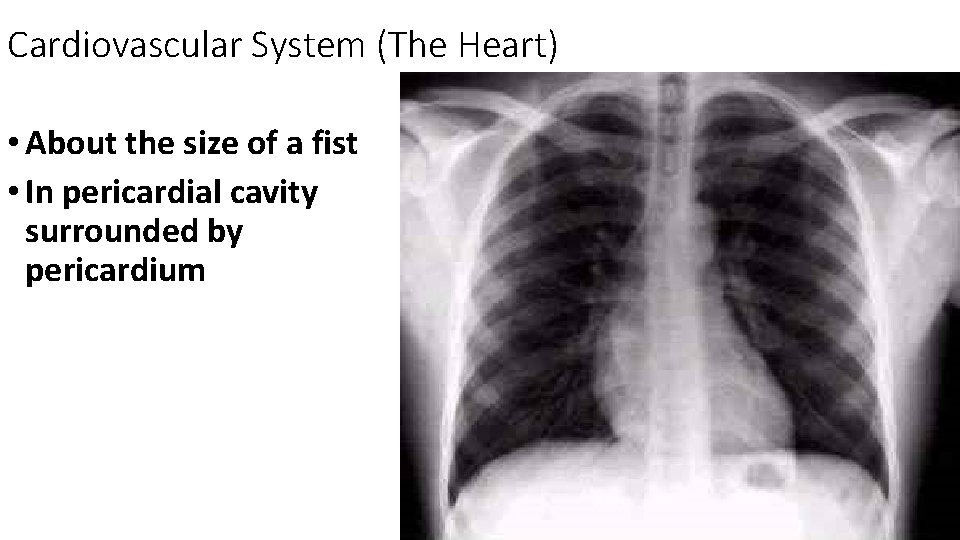
The Heart: Anatomy • Enclosed within the mediastinum • Apex points toward the left at approximately the 5 th intercostal space • Enclosed by double-walled pericardium (sac)
Cardiovascular System (The Heart) • About the size of a fist • In pericardial cavity surrounded by pericardium
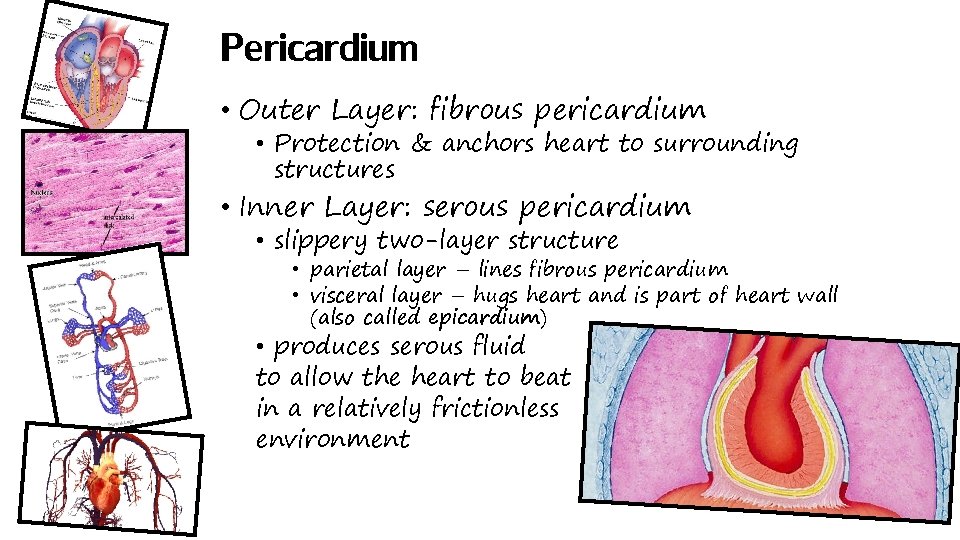
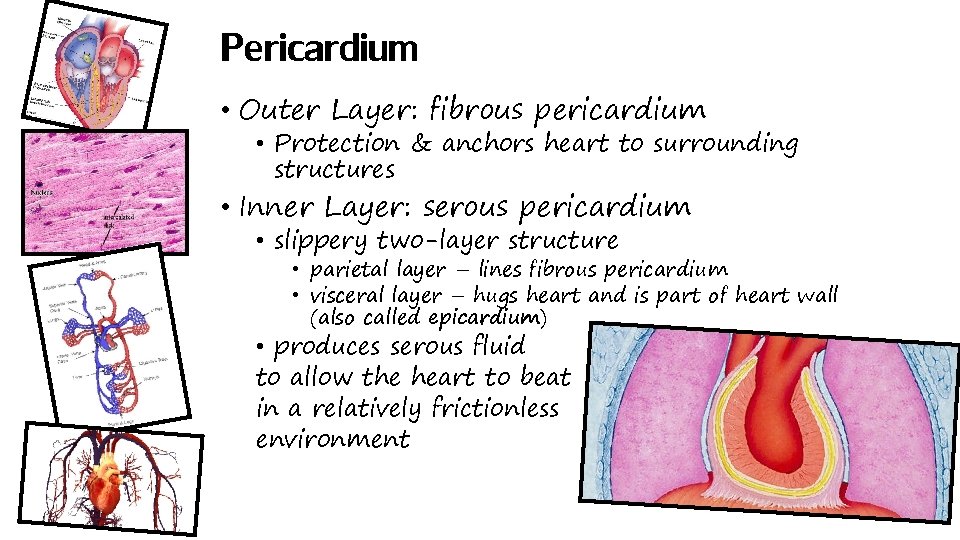
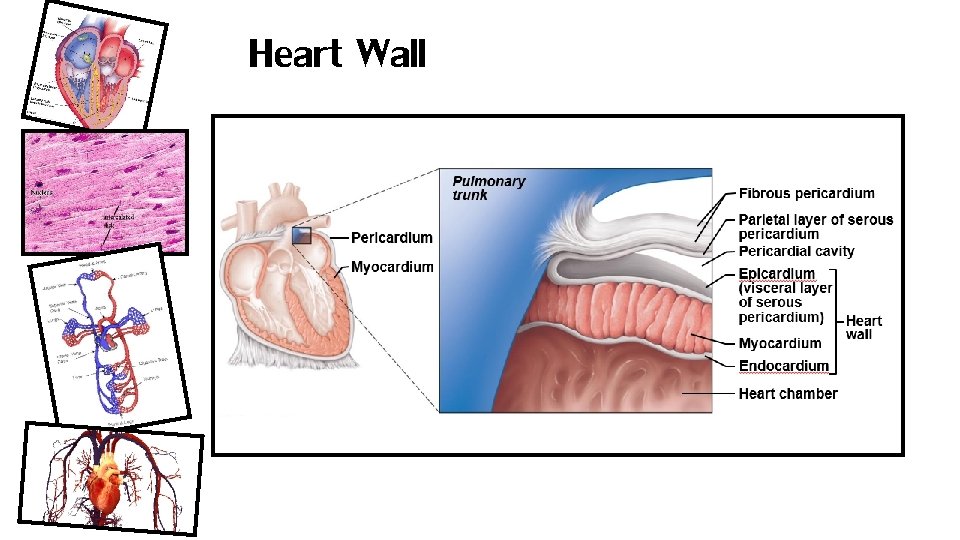
Pericardium • Outer Layer: fibrous pericardium • Protection & anchors heart to surrounding structures • Inner Layer: serous pericardium • slippery two-layer structure • parietal layer – lines fibrous pericardium • visceral layer – hugs heart and is part of heart wall (also called epicardium) • produces serous fluid to allow the heart to beat in a relatively frictionless environment
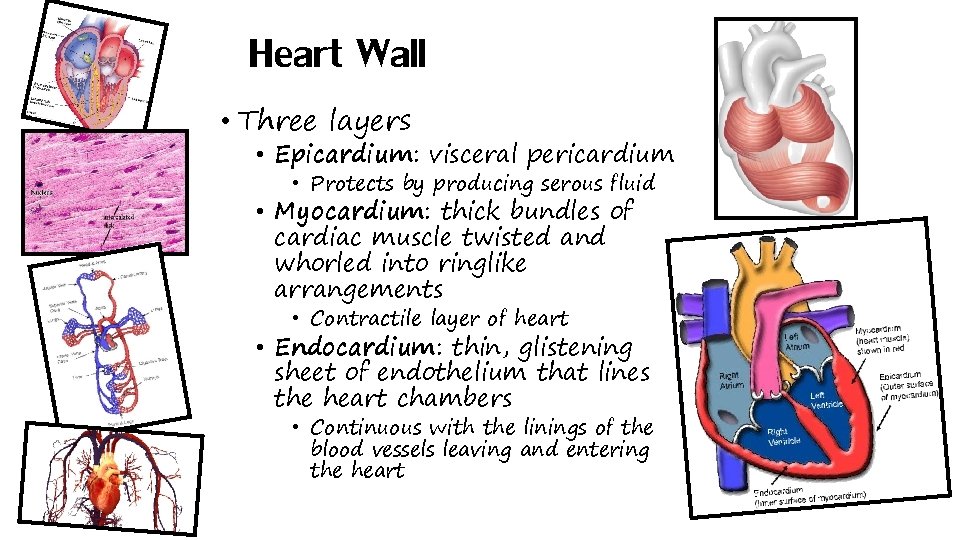
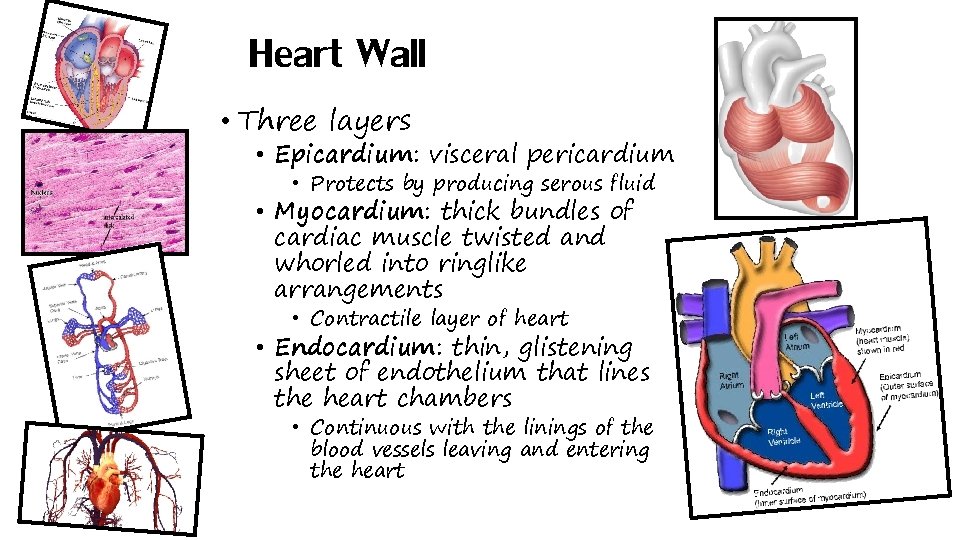
Heart Wall • Three layers • Epicardium: visceral pericardium • Protects by producing serous fluid • Myocardium: thick bundles of cardiac muscle twisted and whorled into ringlike arrangements • Contractile layer of heart • Endocardium: thin, glistening sheet of endothelium that lines the heart chambers • Continuous with the linings of the blood vessels leaving and entering the heart
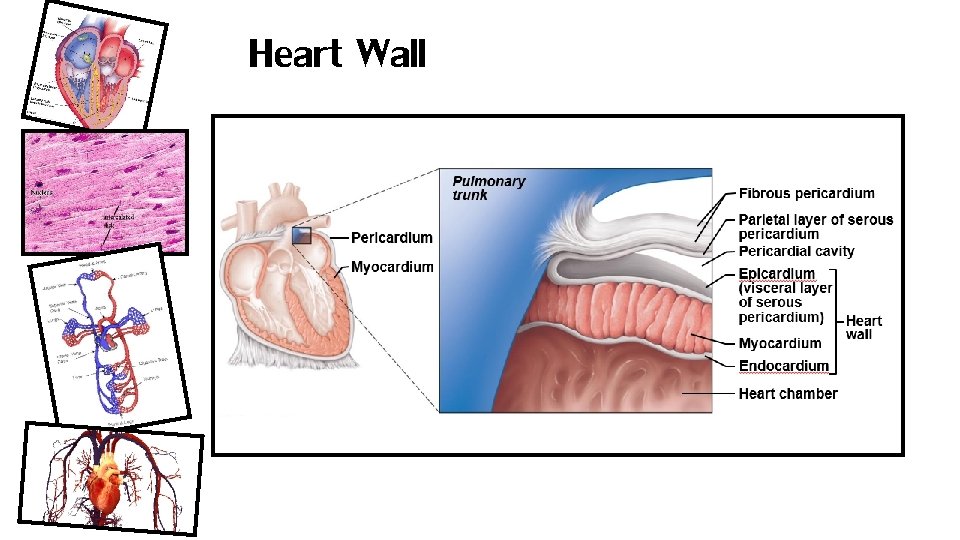
Heart Wall
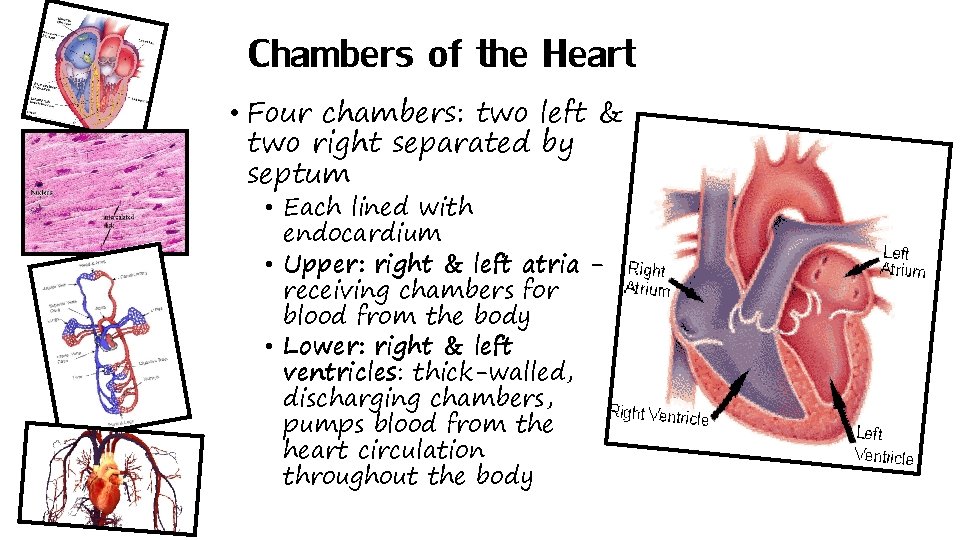
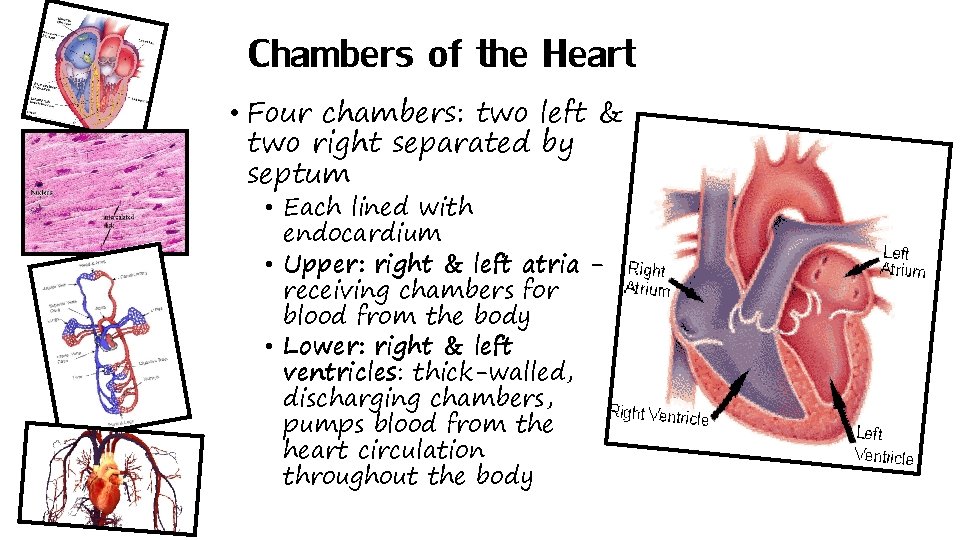
Chambers of the Heart • Four chambers: two left & two right separated by septum • Each lined with endocardium • Upper: right & left atria receiving chambers for blood from the body • Lower: right & left ventricles: thick-walled, discharging chambers, pumps blood from the heart circulation throughout the body
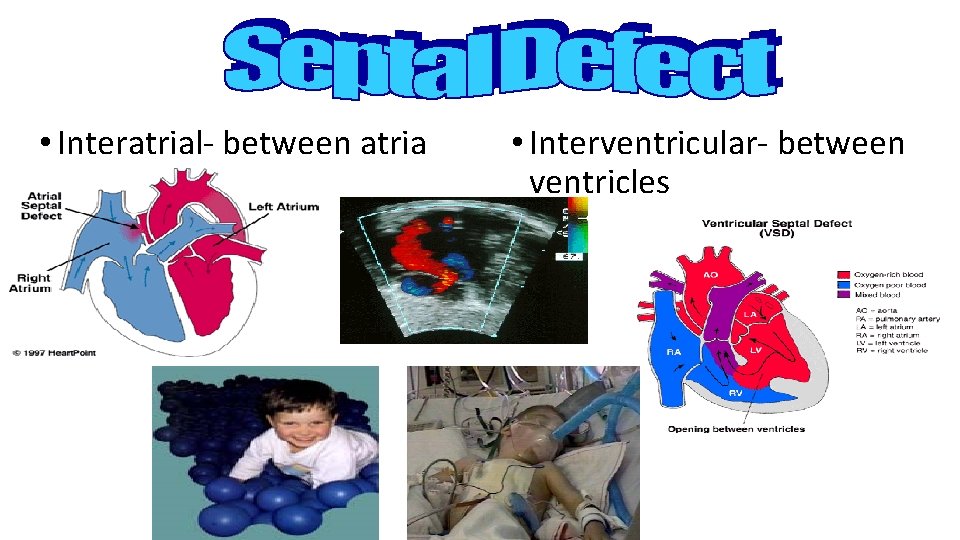
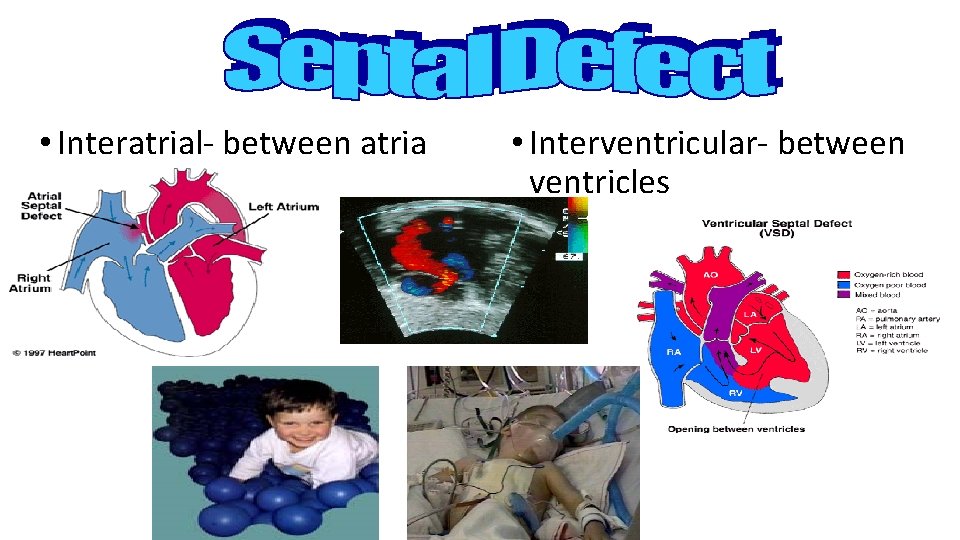
• Interatrial- between atria • Interventricular- between ventricles
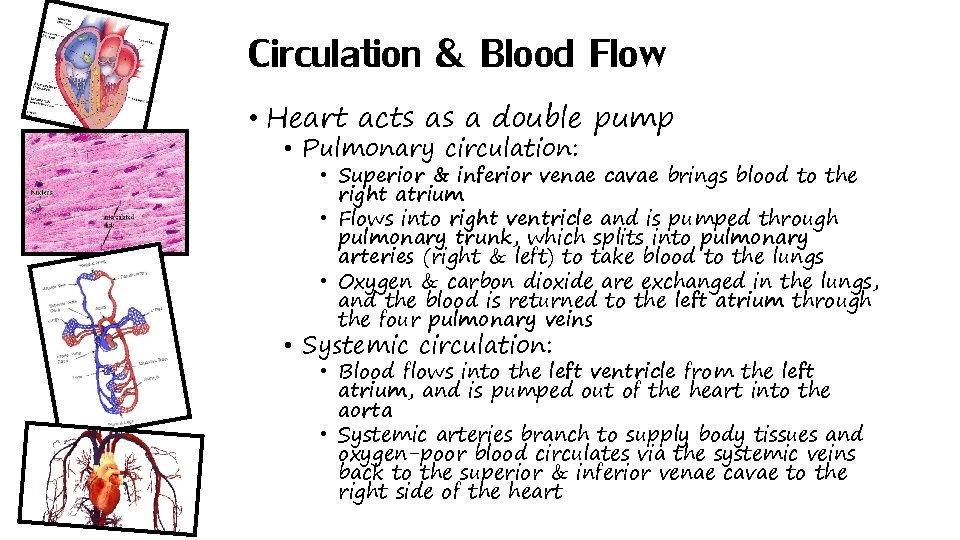
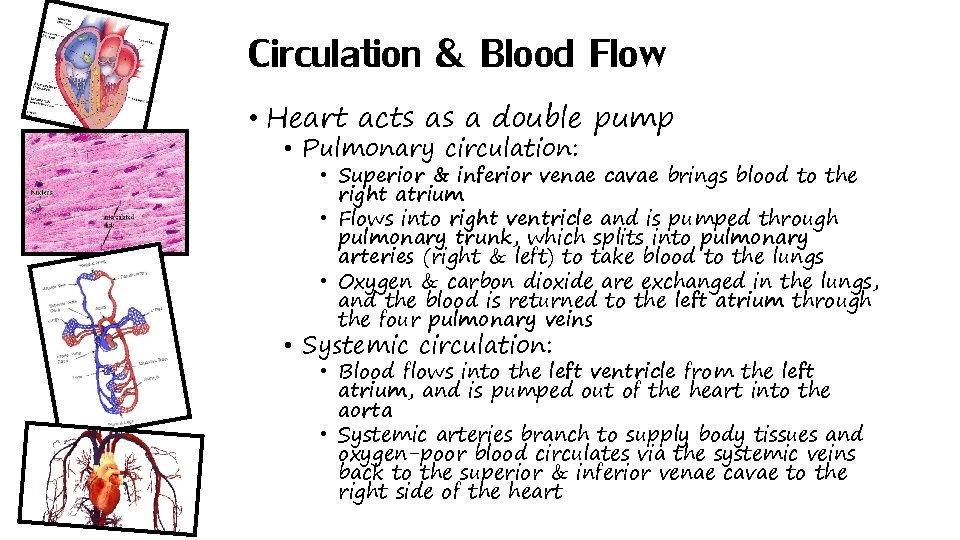
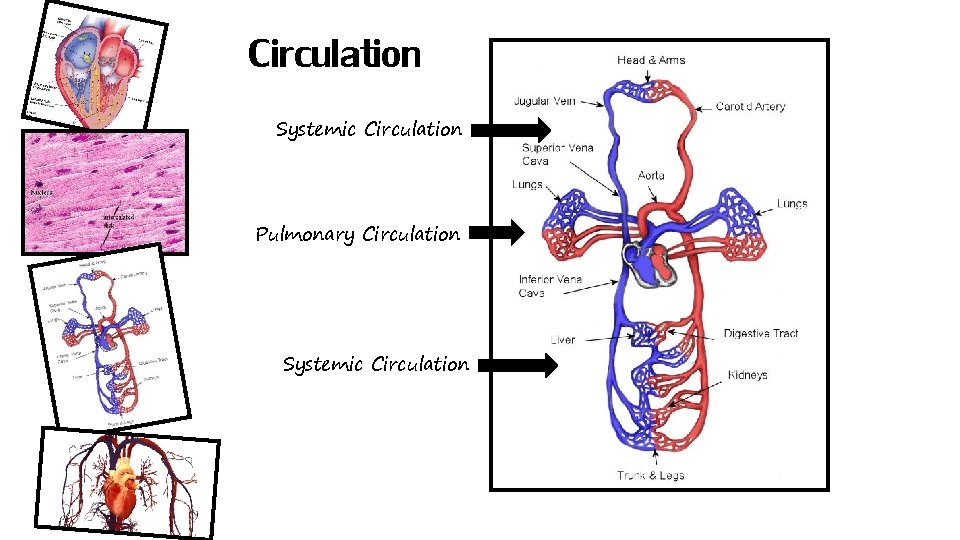
Circulation & Blood Flow • Heart acts as a double pump • Pulmonary circulation: • Superior & inferior venae cavae brings blood to the right atrium • Flows into right ventricle and is pumped through pulmonary trunk, which splits into pulmonary arteries (right & left) to take blood to the lungs • Oxygen & carbon dioxide are exchanged in the lungs, and the blood is returned to the left atrium through the four pulmonary veins • Systemic circulation: • Blood flows into the left ventricle from the left atrium, and is pumped out of the heart into the aorta • Systemic arteries branch to supply body tissues and oxygen-poor blood circulates via the systemic veins back to the superior & inferior venae cavae to the right side of the heart
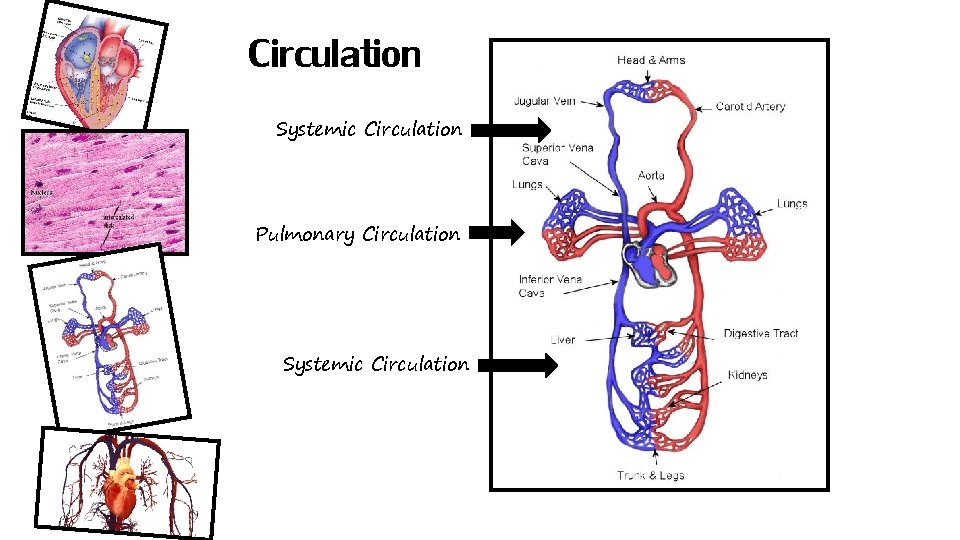
Circulation Systemic Circulation Pulmonary Circulation Systemic Circulation
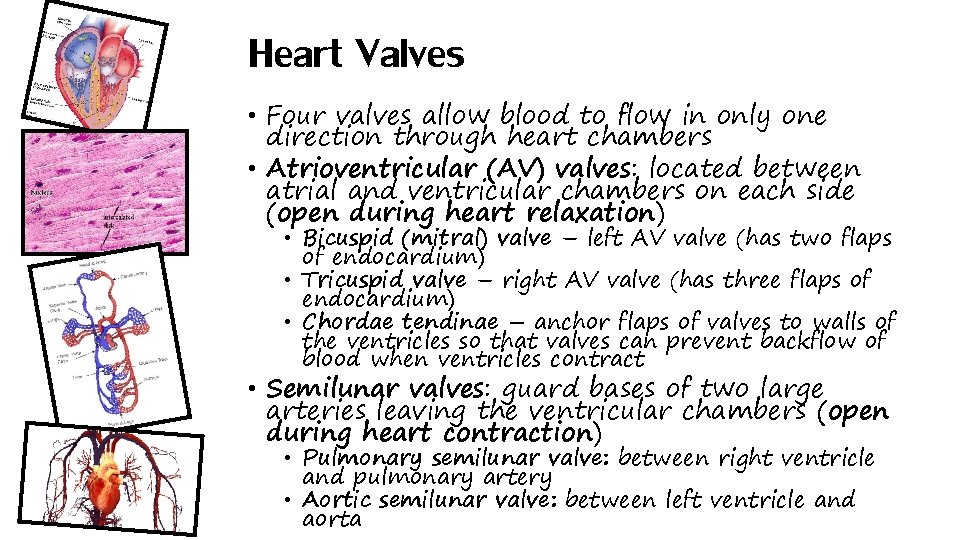
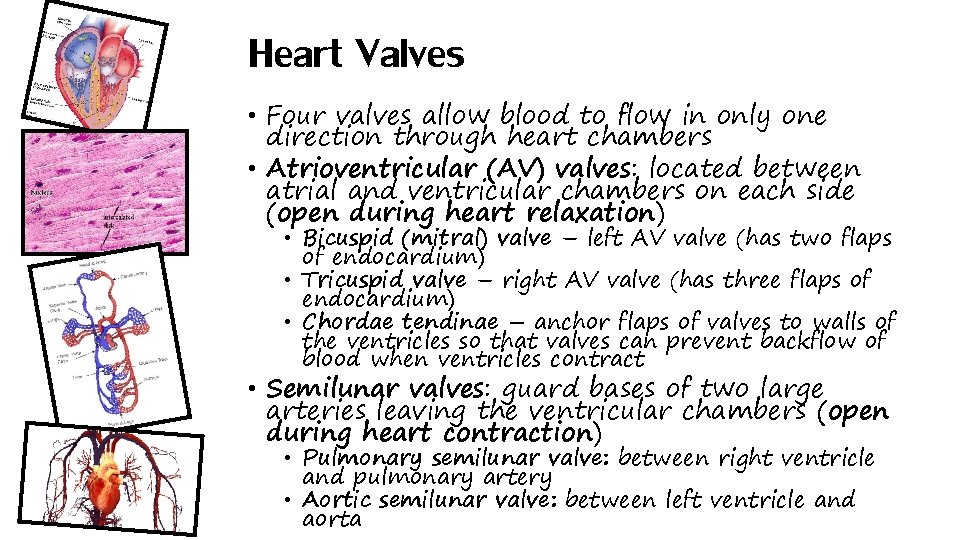
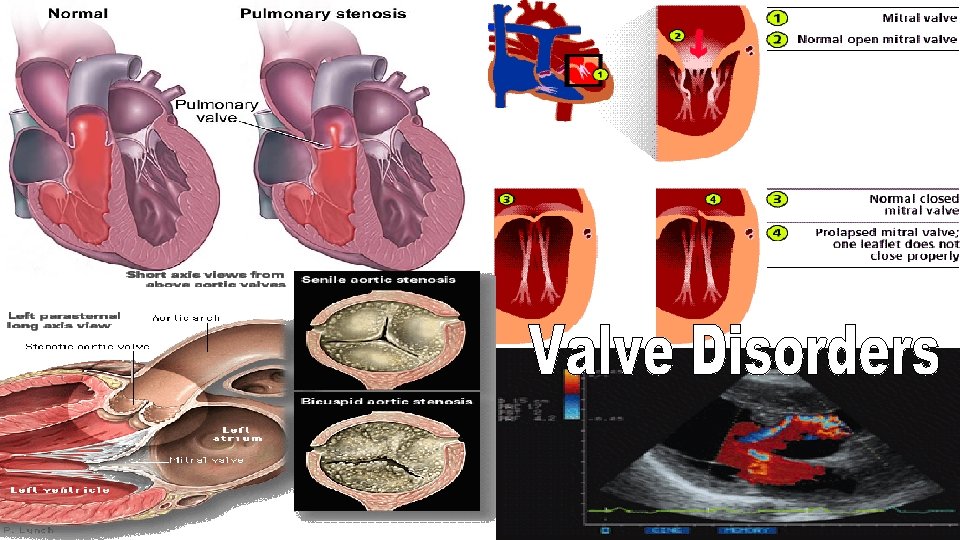
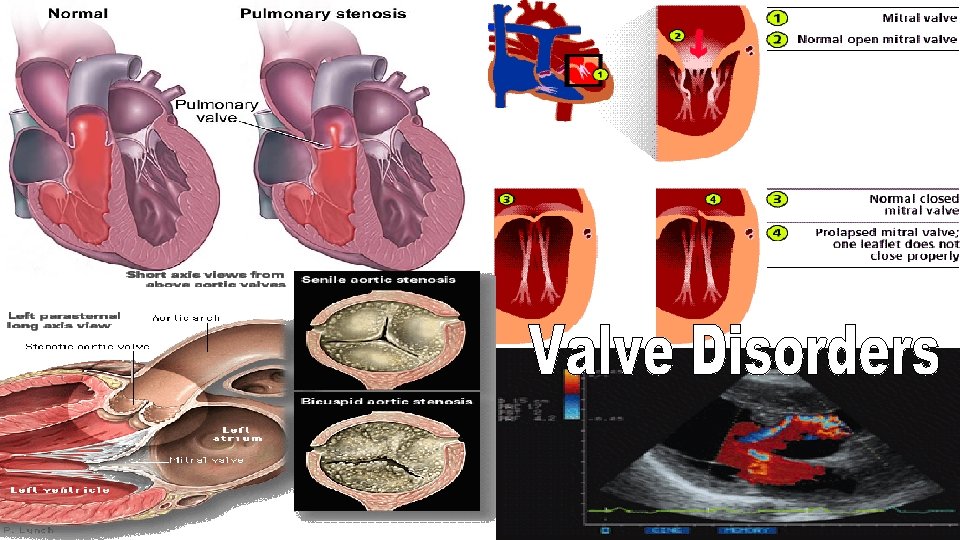
Heart Valves • Four valves allow blood to flow in only one direction through heart chambers • Atrioventricular (AV) valves: located between atrial and ventricular chambers on each side (open during heart relaxation) • Bicuspid (mitral) valve – left AV valve (has two flaps of endocardium) • Tricuspid valve – right AV valve (has three flaps of endocardium) • Chordae tendinae – anchor flaps of valves to walls of the ventricles so that valves can prevent backflow of blood when ventricles contract • Semilunar valves: guard bases of two large arteries leaving the ventricular chambers (open during heart contraction) • Pulmonary semilunar valve: between right ventricle and pulmonary artery • Aortic semilunar valve: between left ventricle and aorta

Heart Valves
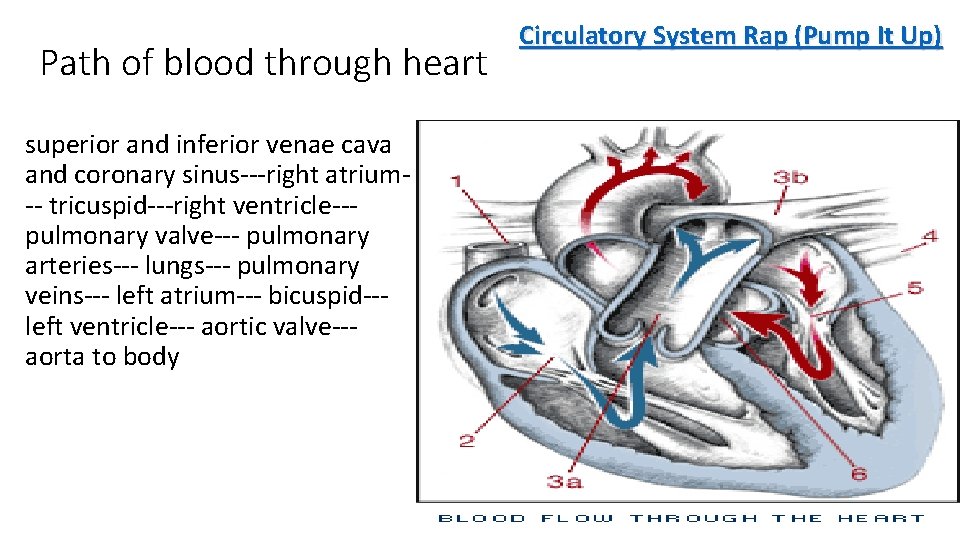
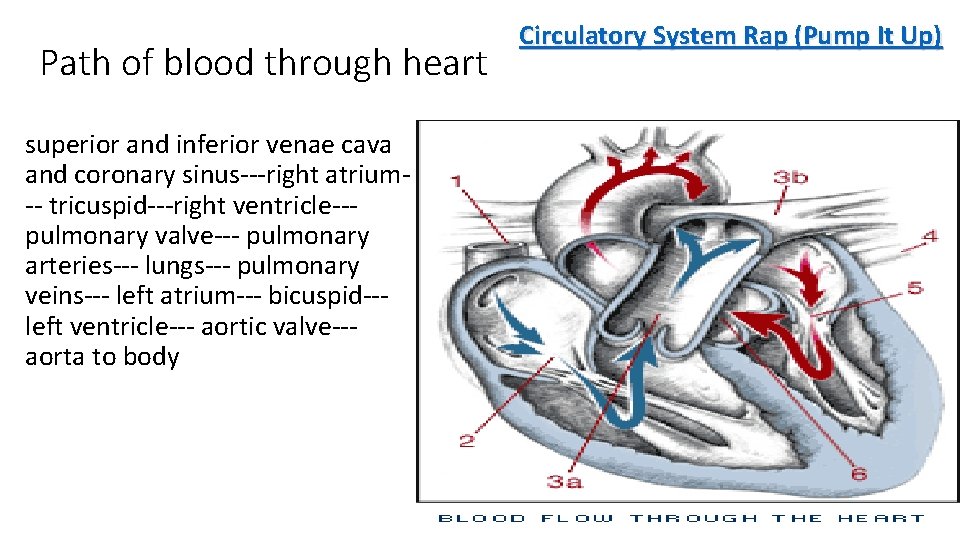
Path of blood through heart superior and inferior venae cava and coronary sinus---right atrium-- tricuspid---right ventricle--pulmonary valve--- pulmonary arteries--- lungs--- pulmonary veins--- left atrium--- bicuspid--left ventricle--- aortic valve--aorta to body Circulatory System Rap (Pump It Up)
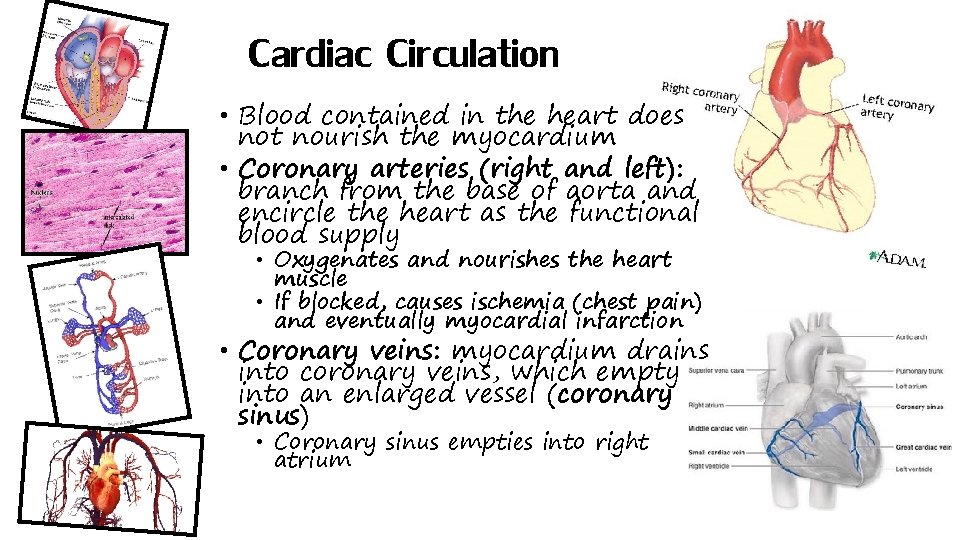
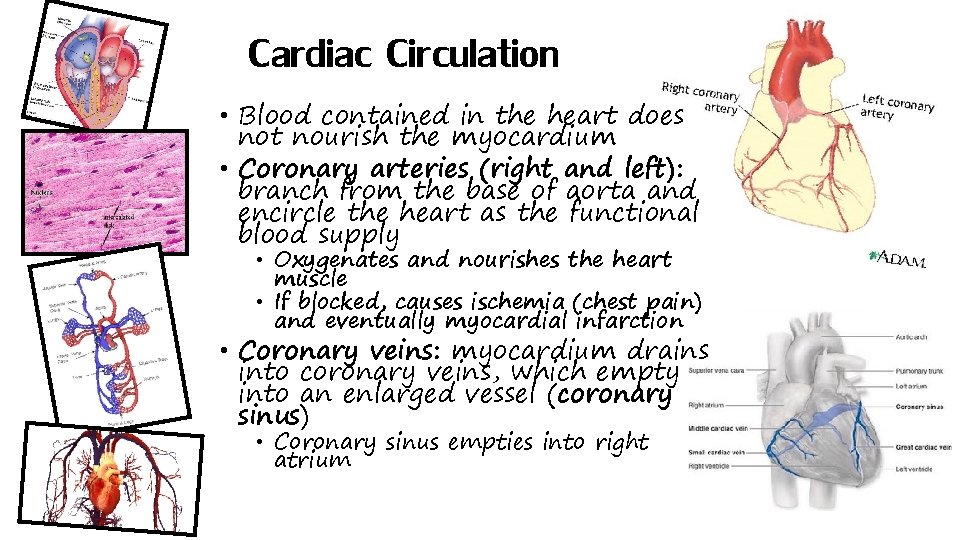
Cardiac Circulation • Blood contained in the heart does not nourish the myocardium • Coronary arteries (right and left): branch from the base of aorta and encircle the heart as the functional blood supply • Oxygenates and nourishes the heart muscle • If blocked, causes ischemia (chest pain) and eventually myocardial infarction • Coronary veins: myocardium drains into coronary veins, which empty into an enlarged vessel (coronary sinus) • Coronary sinus empties into right atrium
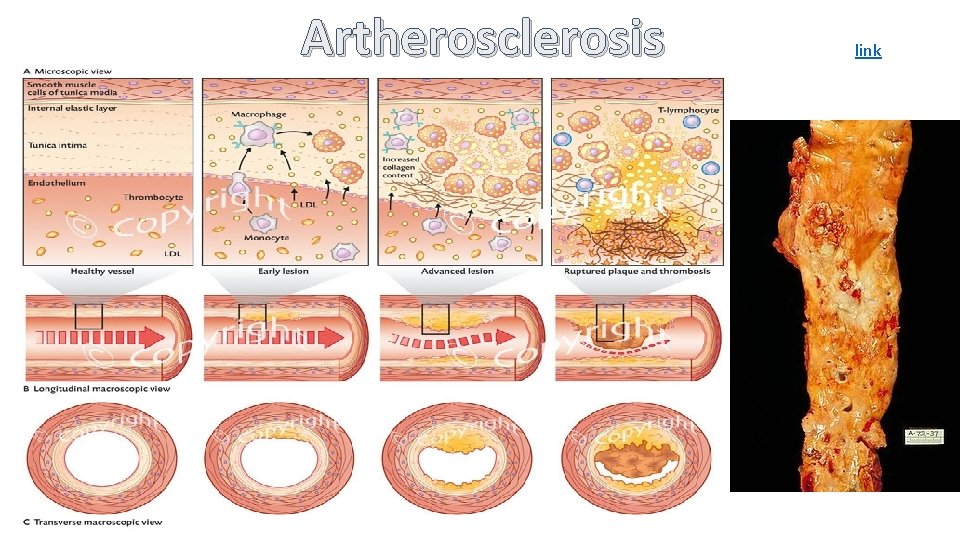
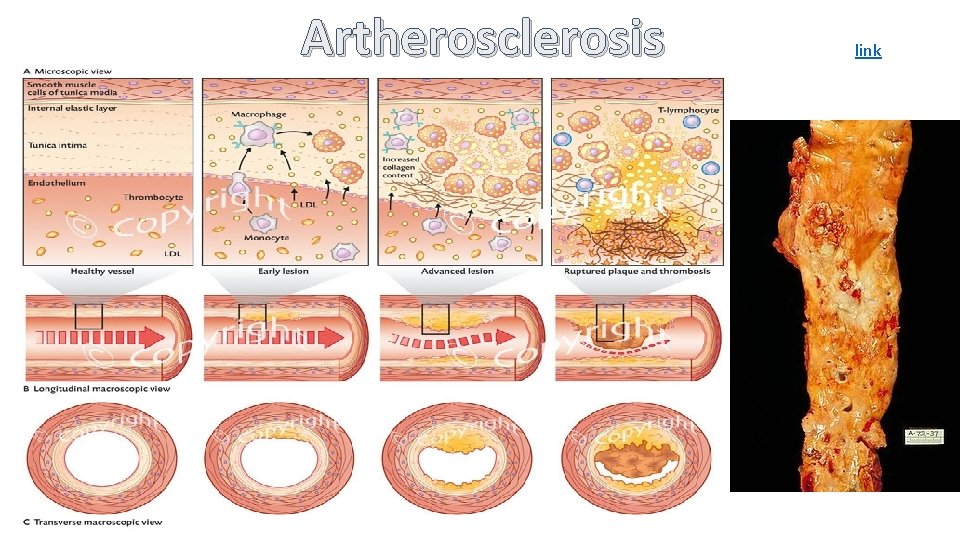
Artherosclerosis link
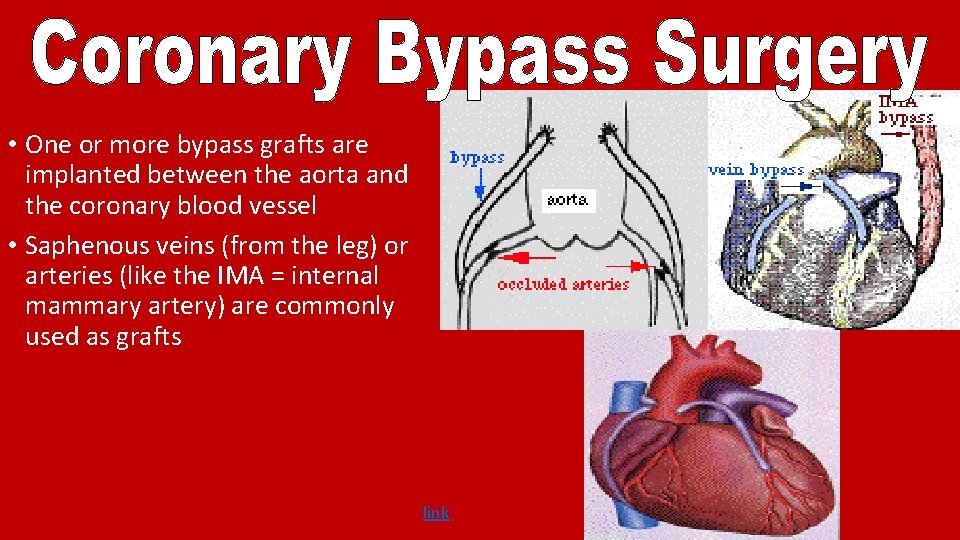
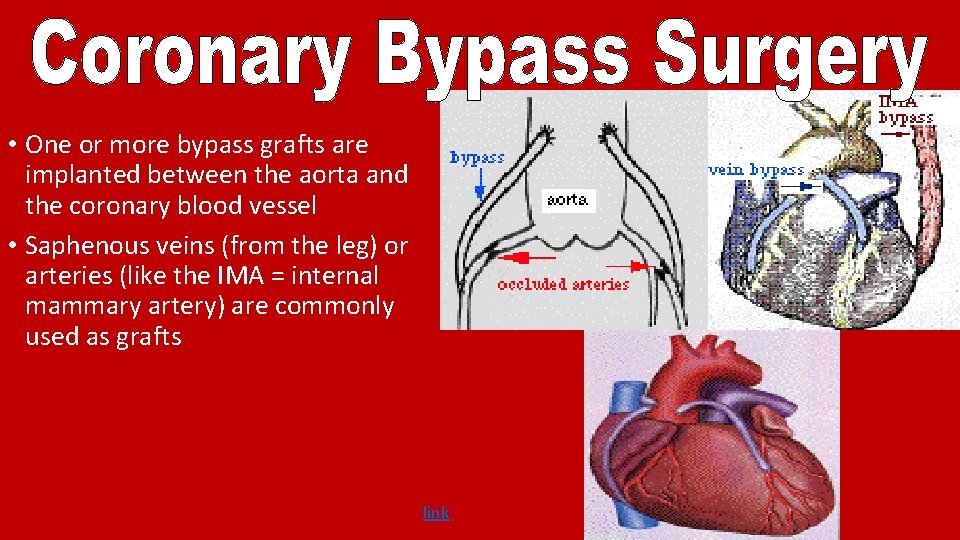
• One or more bypass grafts are implanted between the aorta and the coronary blood vessel • Saphenous veins (from the leg) or arteries (like the IMA = internal mammary artery) are commonly used as grafts link
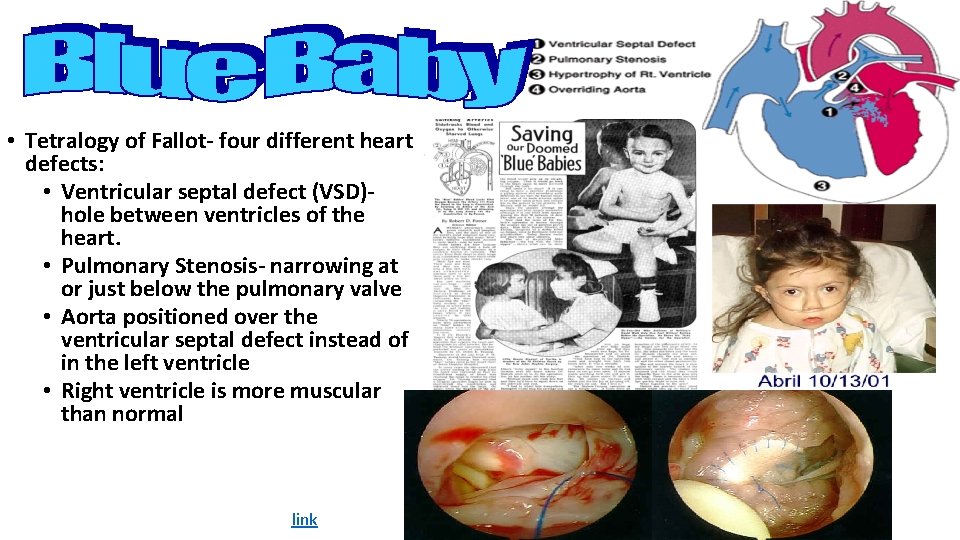
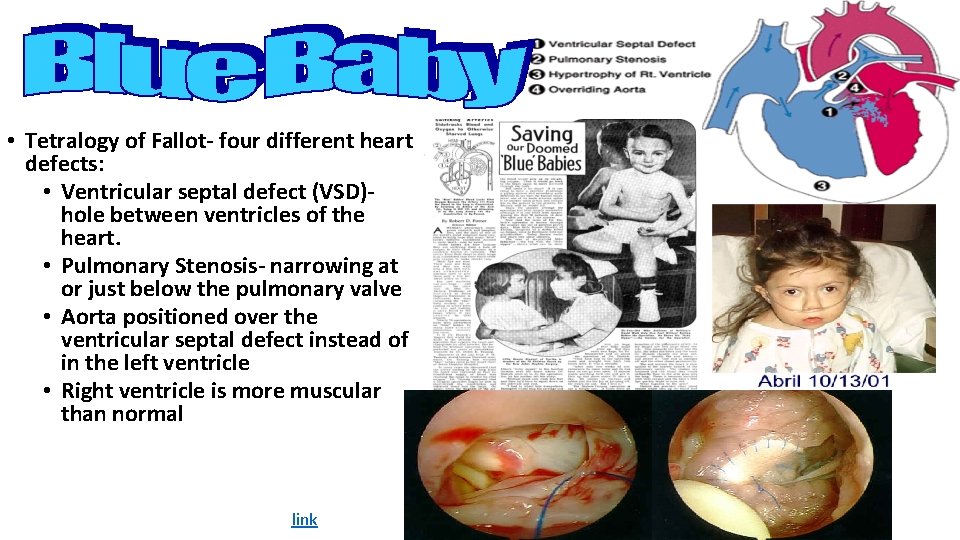
• Tetralogy of Fallot- four different heart defects: • Ventricular septal defect (VSD)hole between ventricles of the heart. • Pulmonary Stenosis- narrowing at or just below the pulmonary valve • Aorta positioned over the ventricular septal defect instead of in the left ventricle • Right ventricle is more muscular than normal link
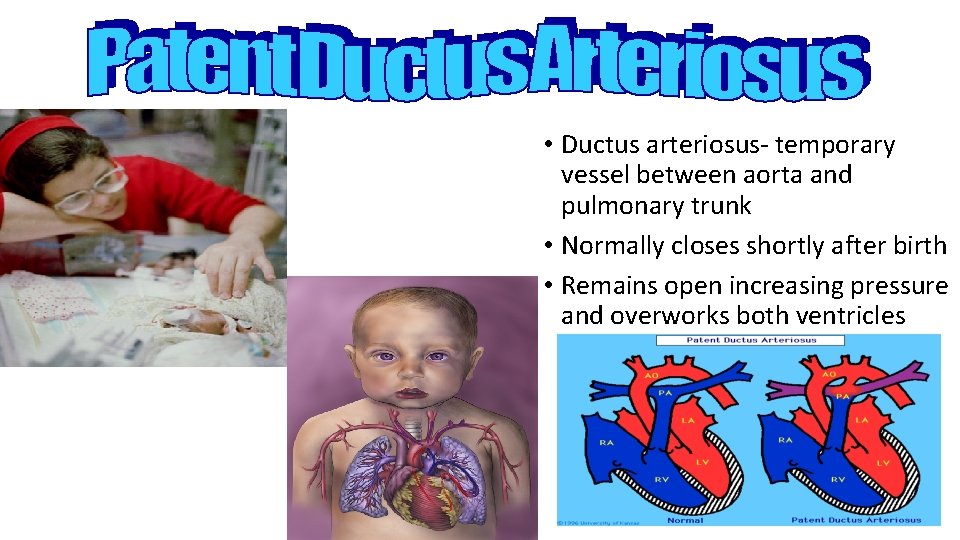
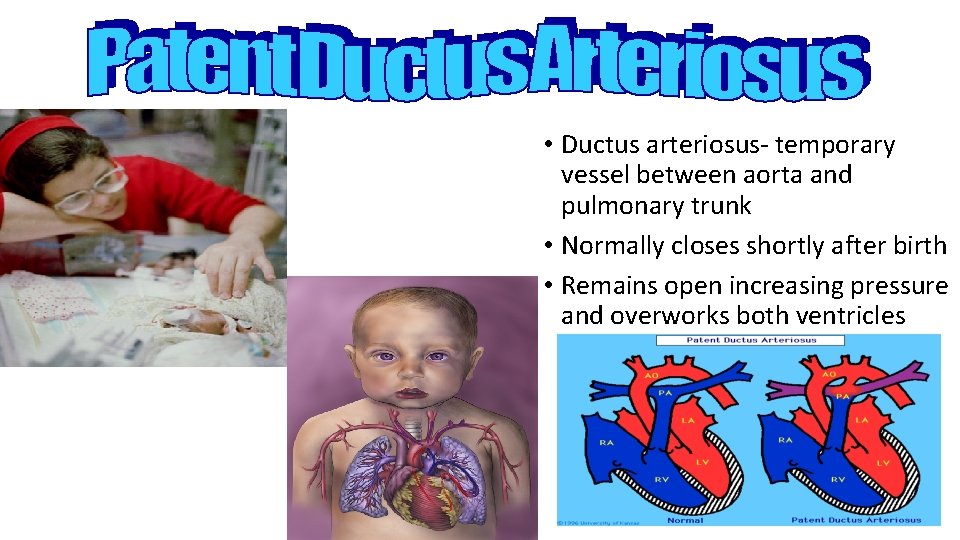
• Ductus arteriosus- temporary vessel between aorta and pulmonary trunk • Normally closes shortly after birth • Remains open increasing pressure and overworks both ventricles
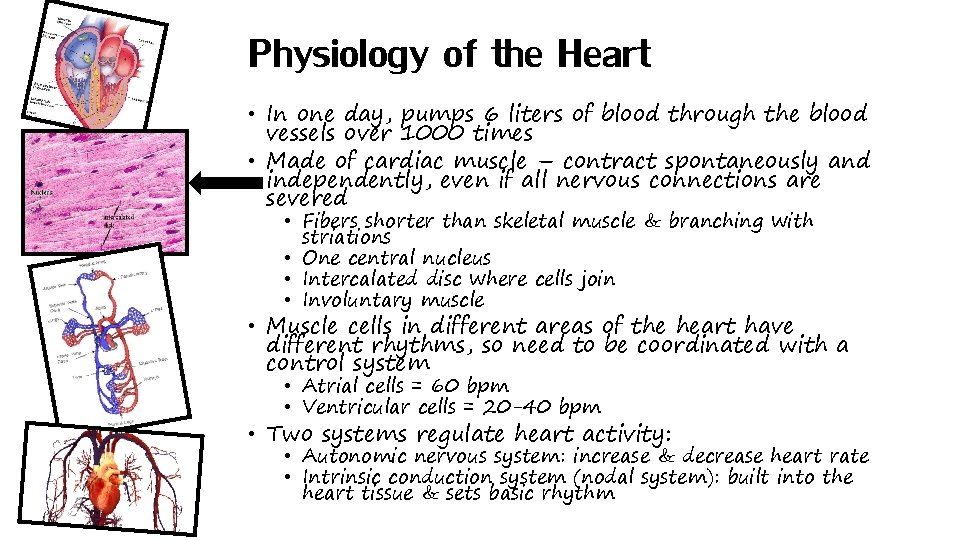
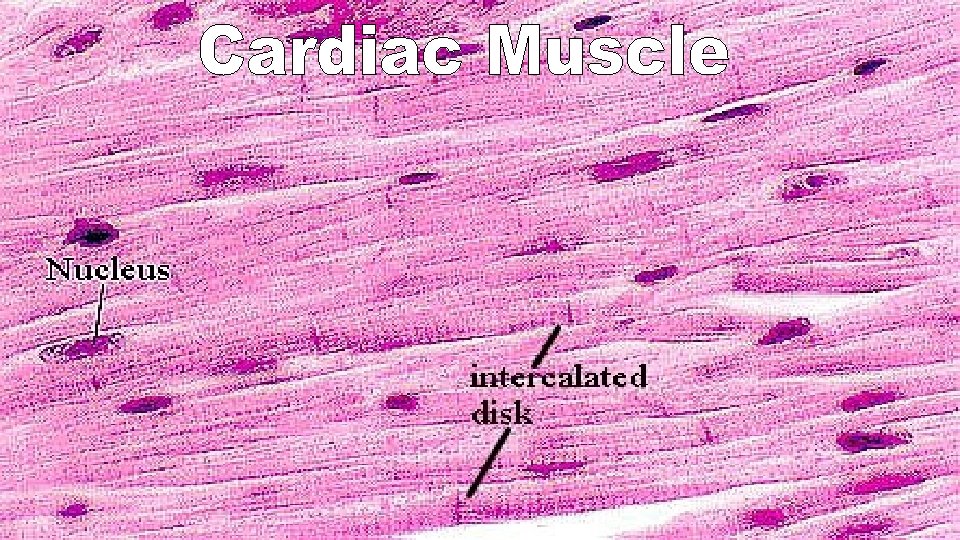
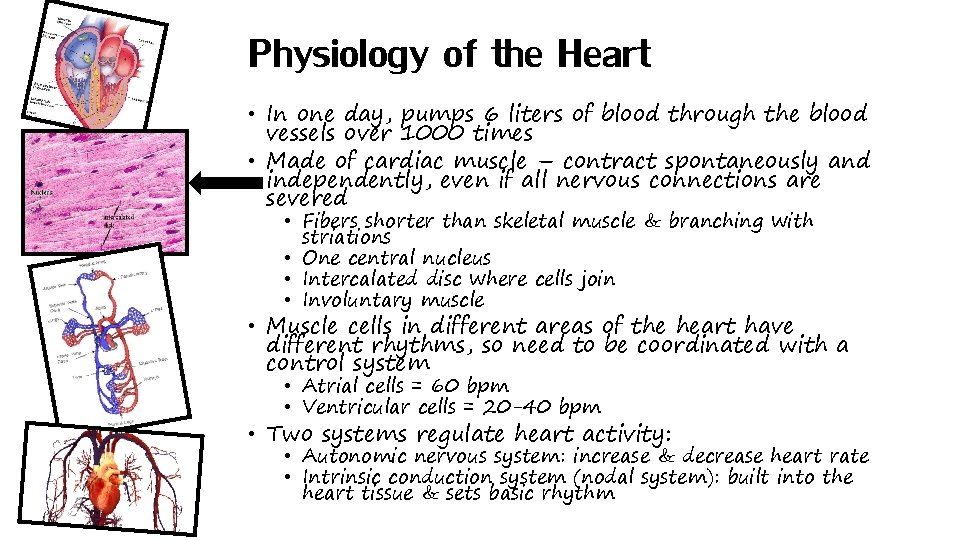
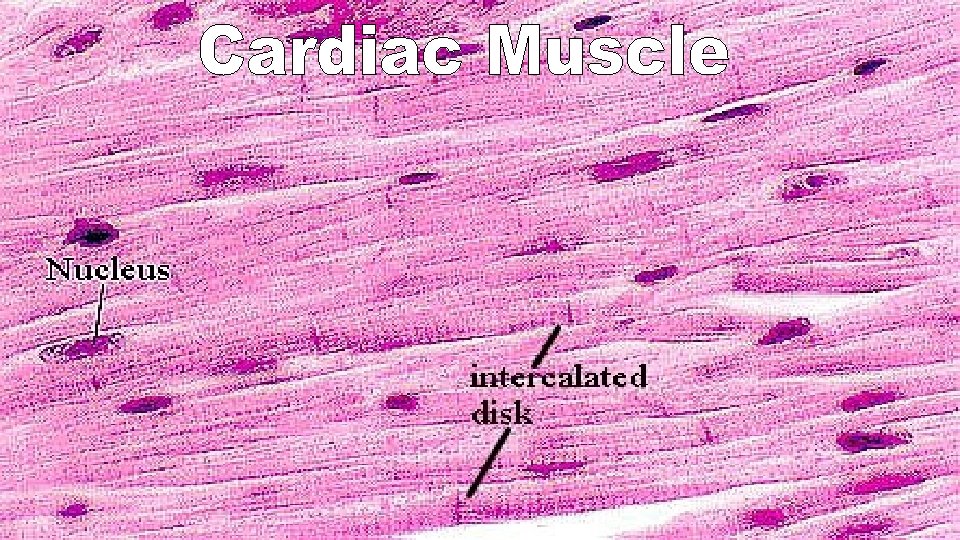
Physiology of the Heart • In one day, pumps 6 liters of blood through the blood vessels over 1000 times • Made of cardiac muscle – contract spontaneously and independently, even if all nervous connections are severed • Fibers shorter than skeletal muscle & branching with striations • One central nucleus • Intercalated disc where cells join • Involuntary muscle • Muscle cells in different areas of the heart have different rhythms, so need to be coordinated with a control system • Atrial cells = 60 bpm • Ventricular cells = 20 -40 bpm • Two systems regulate heart activity: • Autonomic nervous system: increase & decrease heart rate • Intrinsic conduction system (nodal system): built into the heart tissue & sets basic rhythm
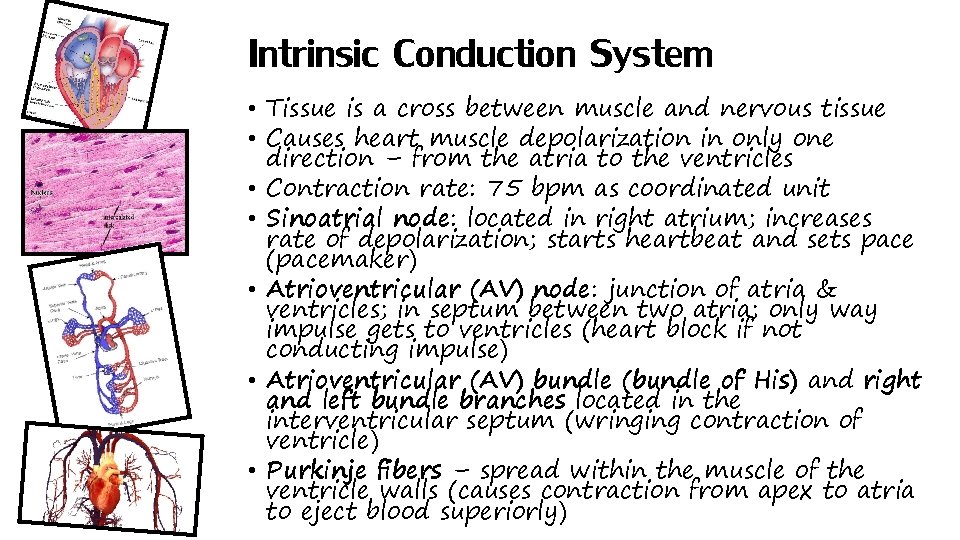
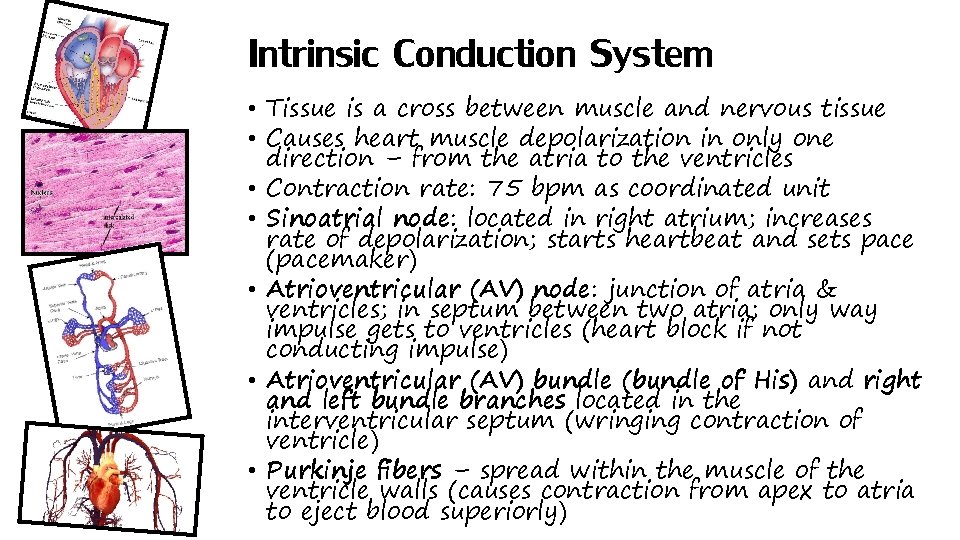
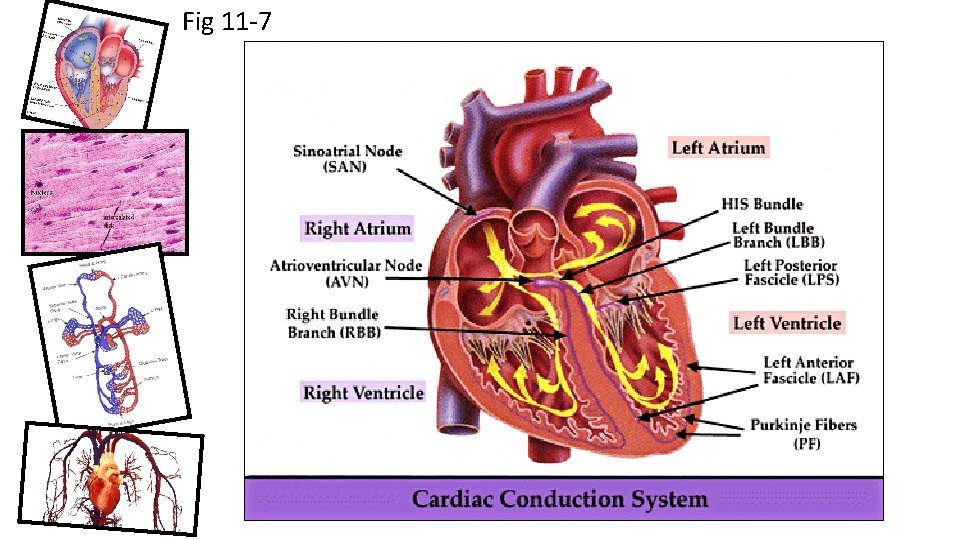
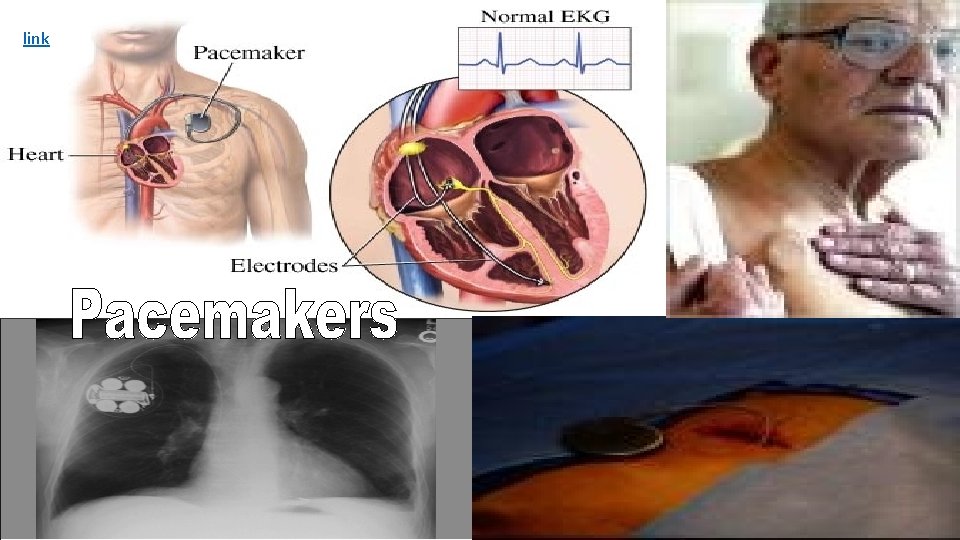
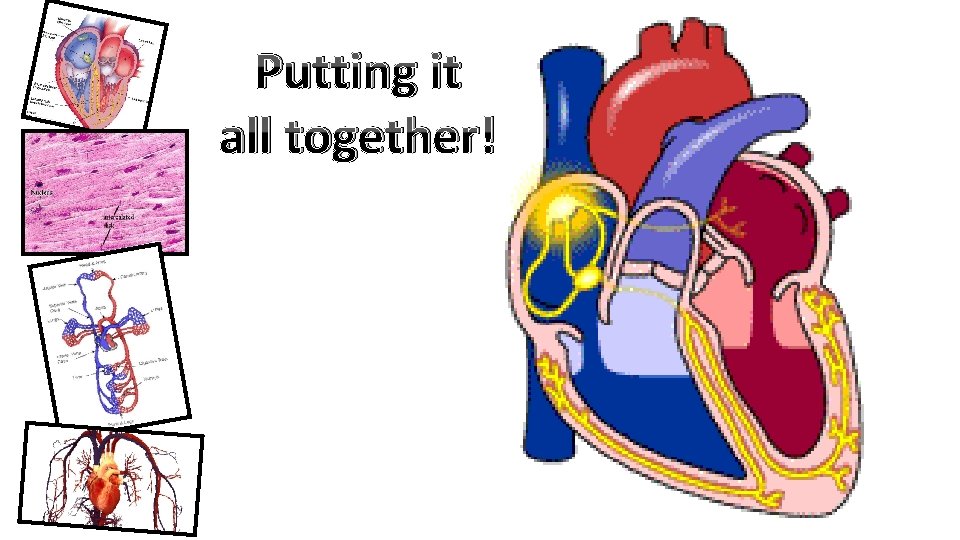
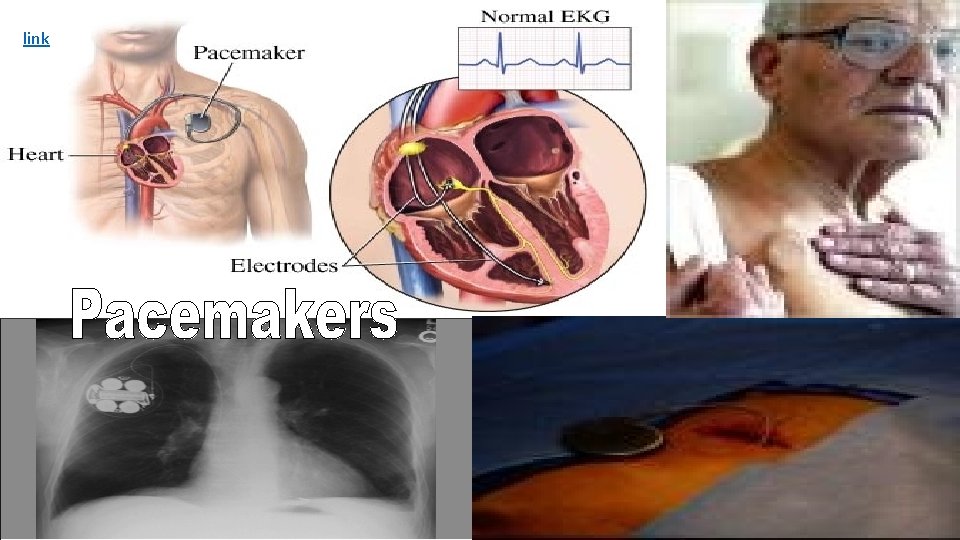
Intrinsic Conduction System • Tissue is a cross between muscle and nervous tissue • Causes heart muscle depolarization in only one direction – from the atria to the ventricles • Contraction rate: 75 bpm as coordinated unit • Sinoatrial node: located in right atrium; increases rate of depolarization; starts heartbeat and sets pace (pacemaker) • Atrioventricular (AV) node: junction of atria & ventricles; in septum between two atria; only way impulse gets to ventricles (heart block if not conducting impulse) • Atrioventricular (AV) bundle (bundle of His) and right and left bundle branches located in the interventricular septum (wringing contraction of ventricle) • Purkinje fibers – spread within the muscle of the ventricle walls (causes contraction from apex to atria to eject blood superiorly)
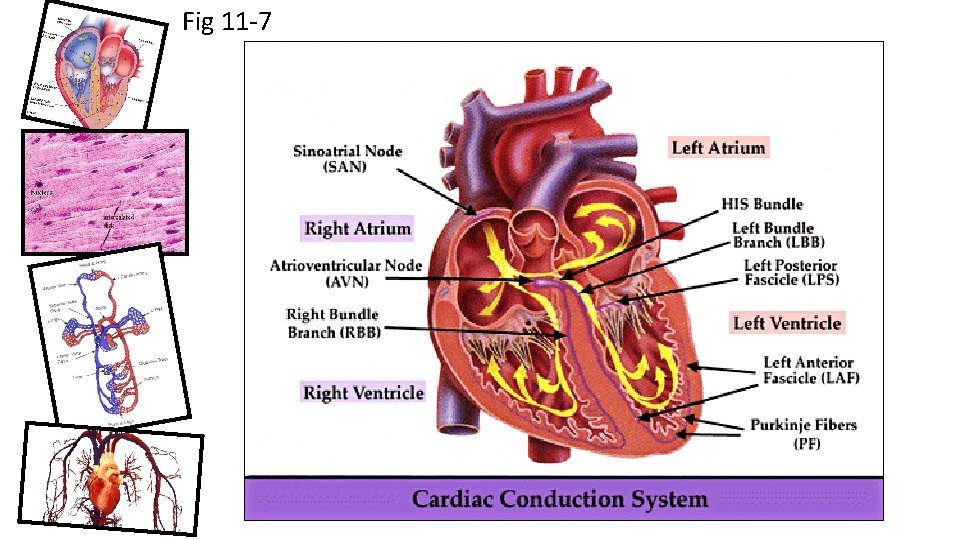
Fig 11 -7
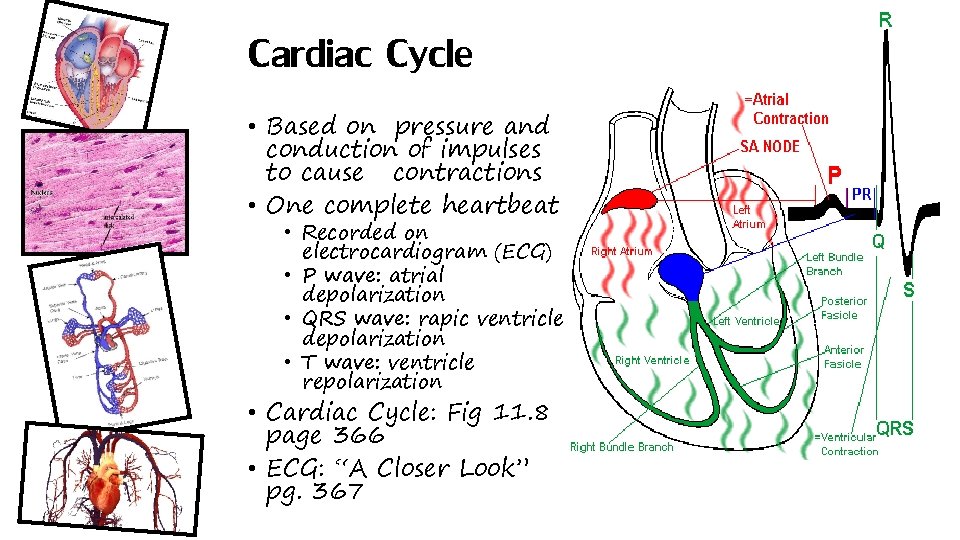
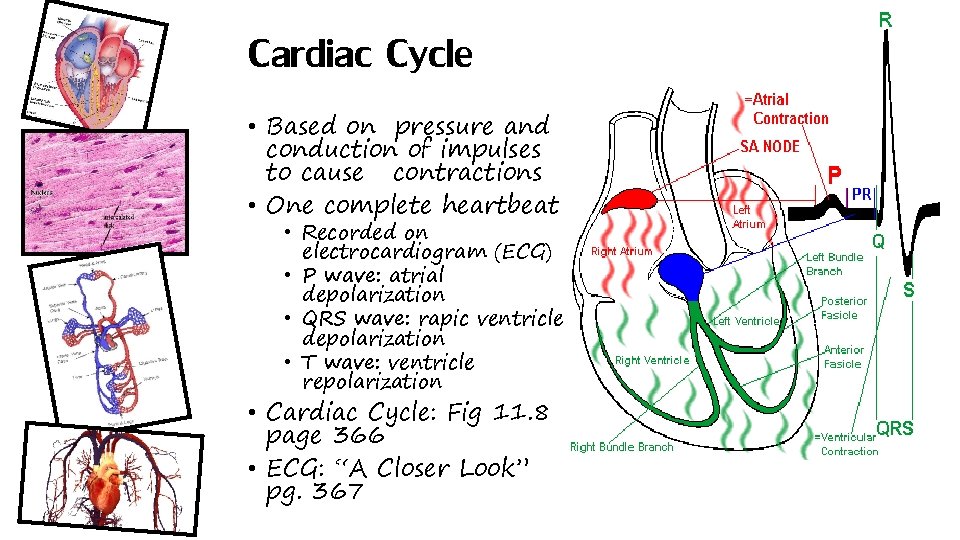
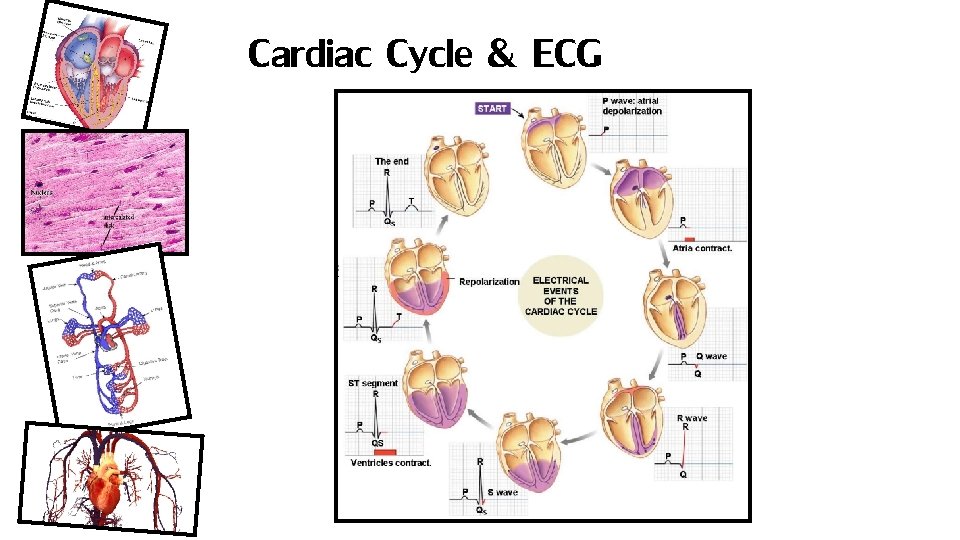
Cardiac Cycle • Based on pressure and conduction of impulses to cause contractions • One complete heartbeat • Recorded on electrocardiogram (ECG) • P wave: atrial depolarization • QRS wave: rapic ventricle depolarization • T wave: ventricle repolarization • Cardiac Cycle: Fig 11. 8 page 366 • ECG: “A Closer Look” pg. 367
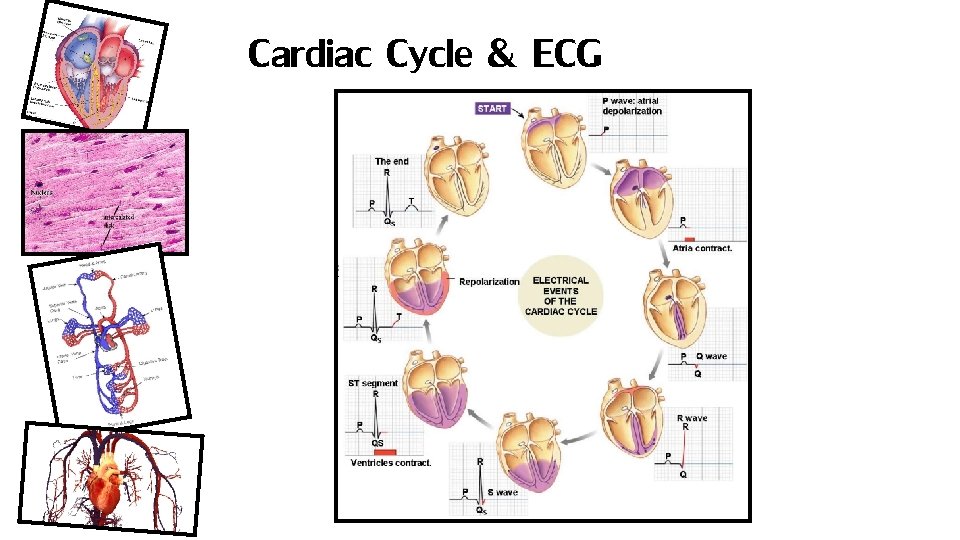
Cardiac Cycle & ECG
link
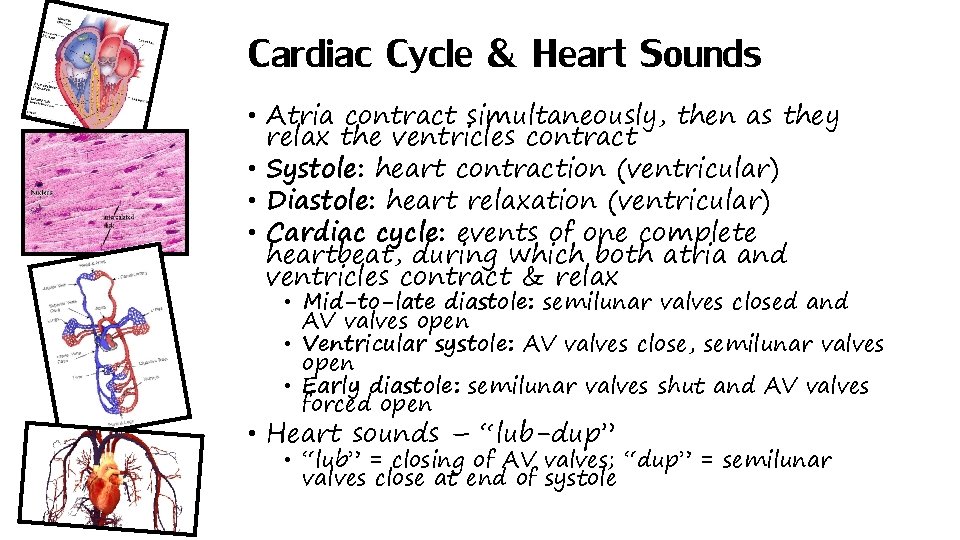
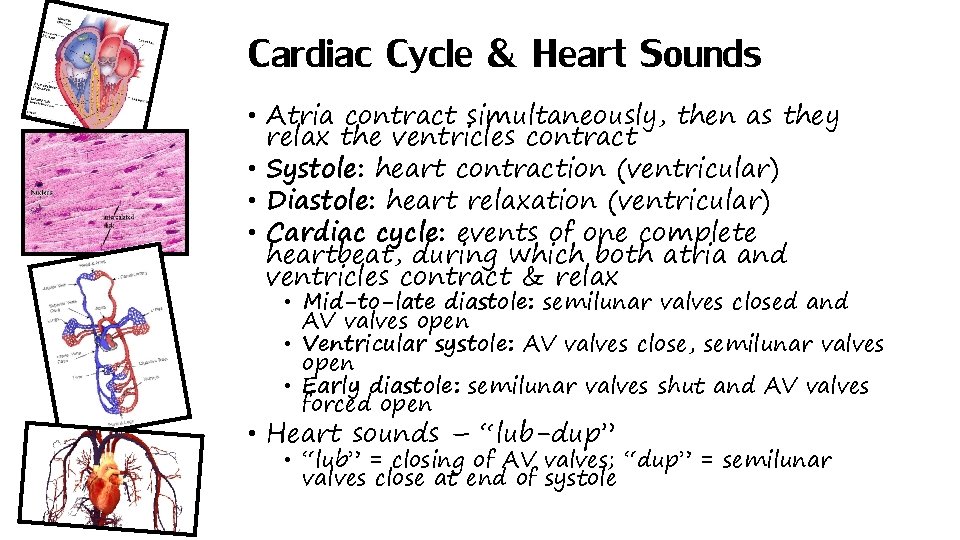
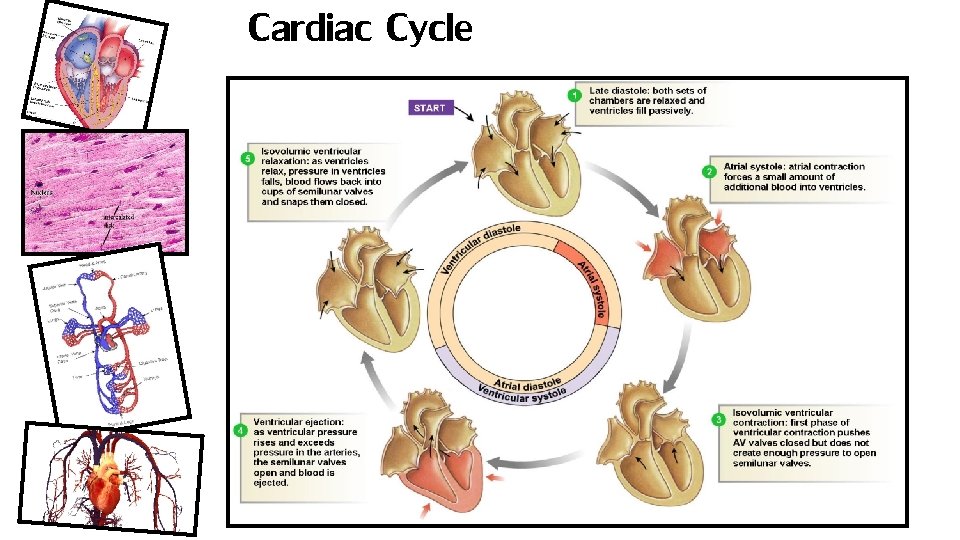
Cardiac Cycle & Heart Sounds • Atria contract simultaneously, then as they relax the ventricles contract • Systole: heart contraction (ventricular) • Diastole: heart relaxation (ventricular) • Cardiac cycle: events of one complete heartbeat, during which both atria and ventricles contract & relax • Mid-to-late diastole: semilunar valves closed and AV valves open • Ventricular systole: AV valves close, semilunar valves open • Early diastole: semilunar valves shut and AV valves forced open • Heart sounds – “lub-dup” • “lub” = closing of AV valves; “dup” = semilunar valves close at end of systole
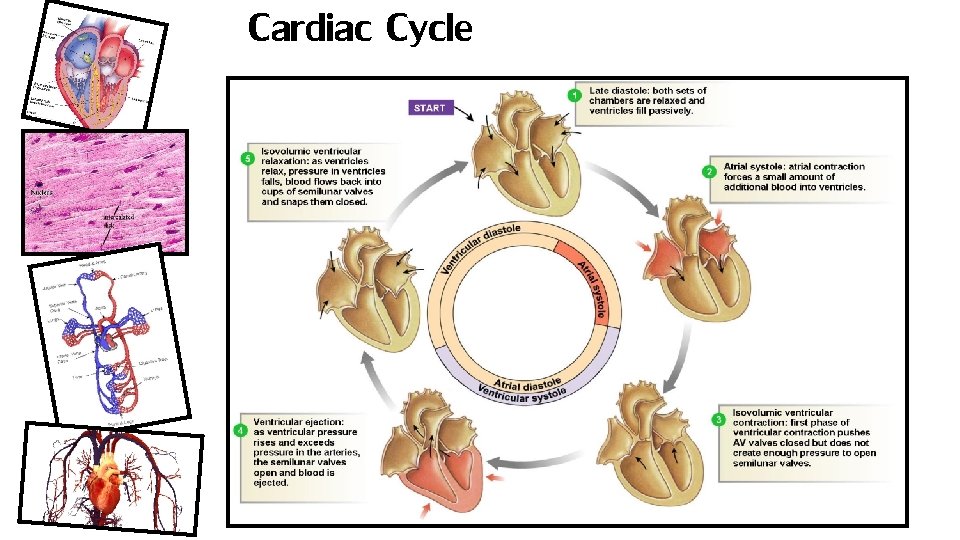
Cardiac Cycle
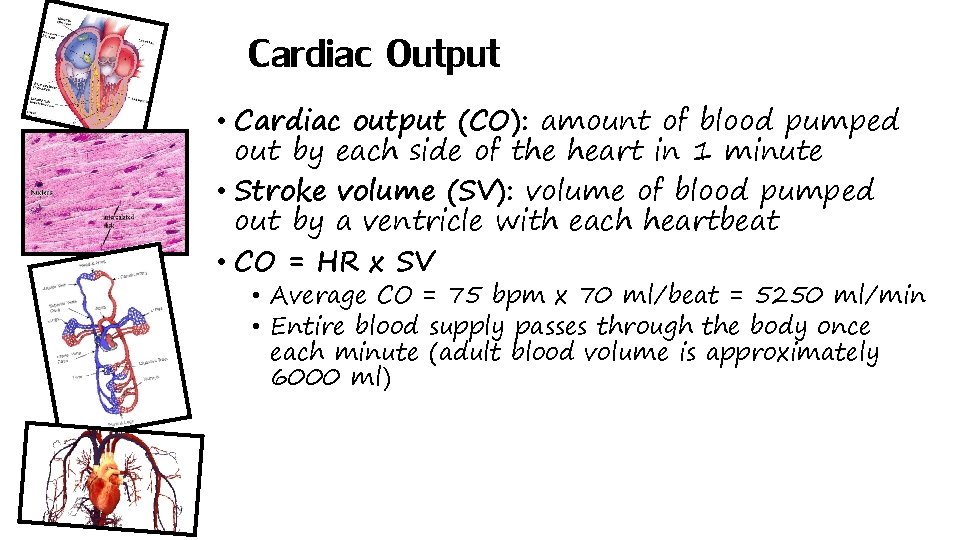
Cardiac Output • Cardiac output (CO): amount of blood pumped out by each side of the heart in 1 minute • Stroke volume (SV): volume of blood pumped out by a ventricle with each heartbeat • CO = HR x SV • Average CO = 75 bpm x 70 ml/beat = 5250 ml/min • Entire blood supply passes through the body once each minute (adult blood volume is approximately 6000 ml)
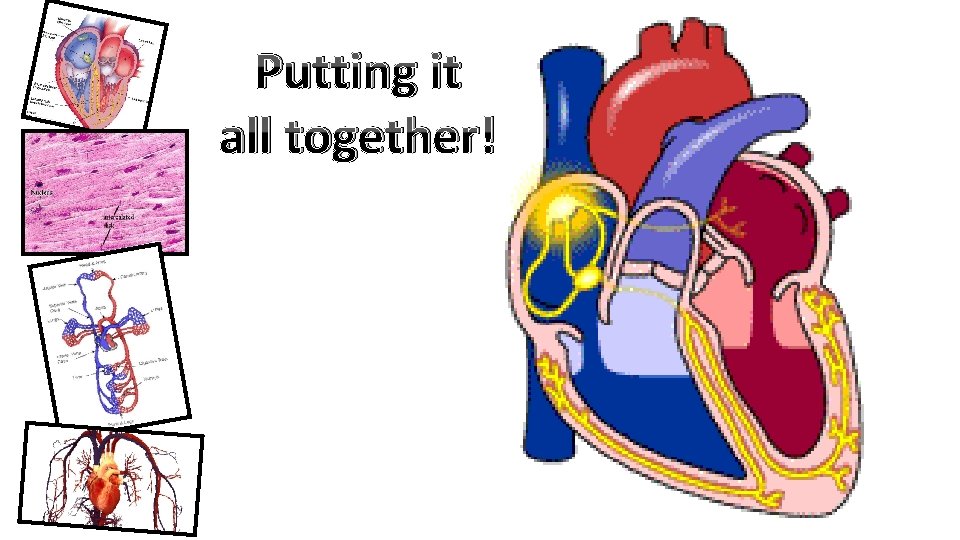
Putting it all together!
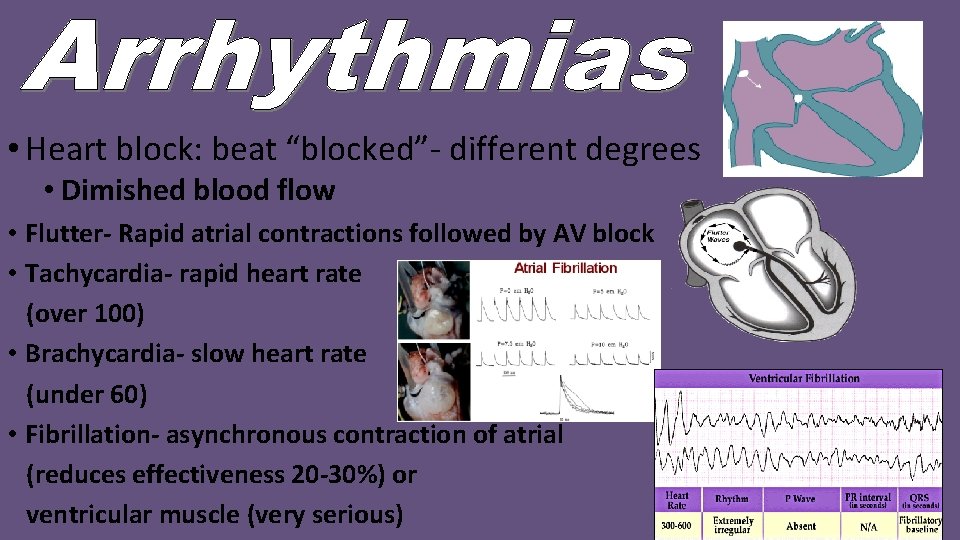
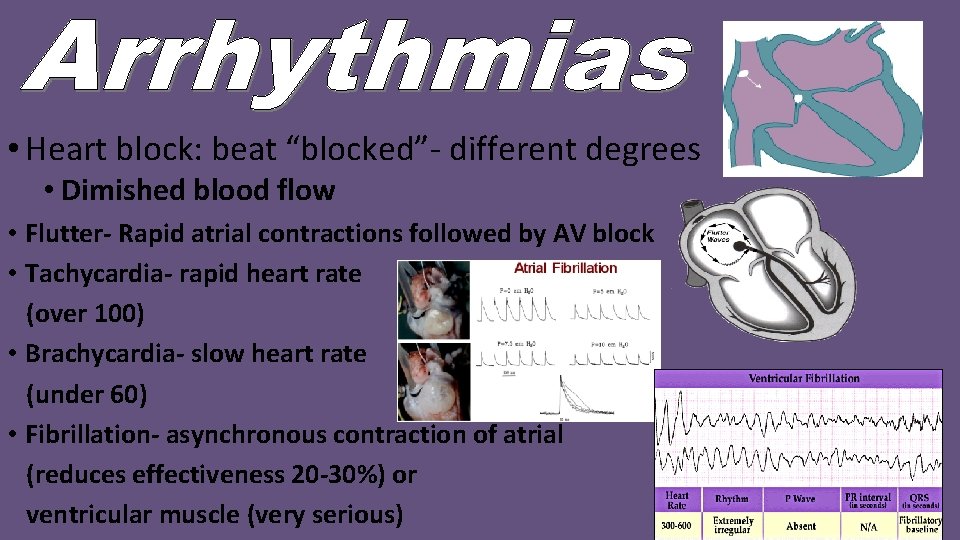
• Heart block: beat “blocked”- different degrees • Dimished blood flow • Flutter- Rapid atrial contractions followed by AV block • Tachycardia- rapid heart rate (over 100) • Brachycardia- slow heart rate (under 60) • Fibrillation- asynchronous contraction of atrial (reduces effectiveness 20 -30%) or ventricular muscle (very serious)
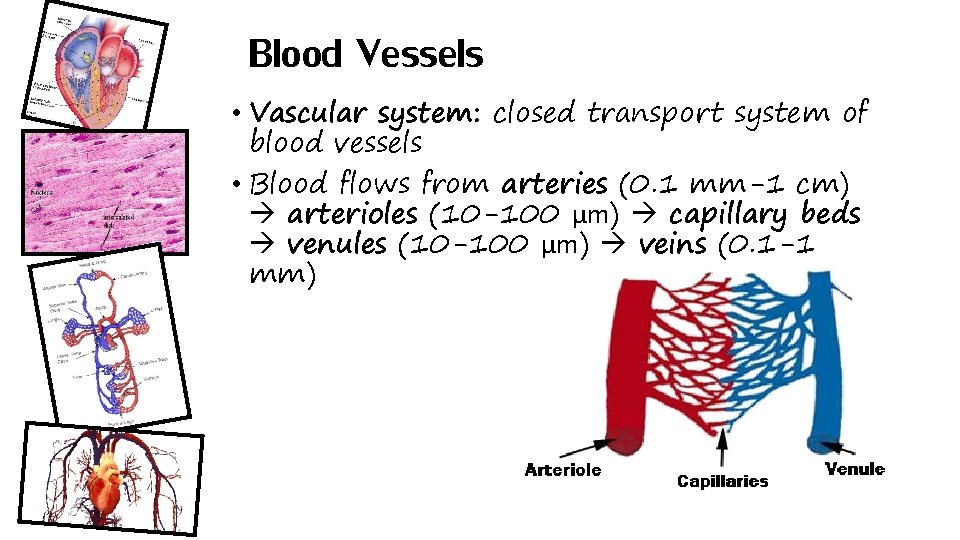
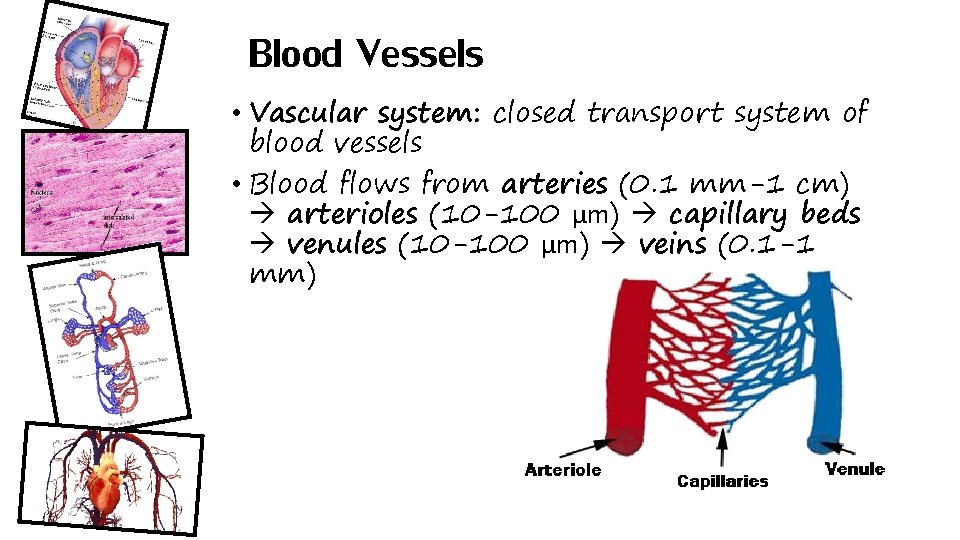
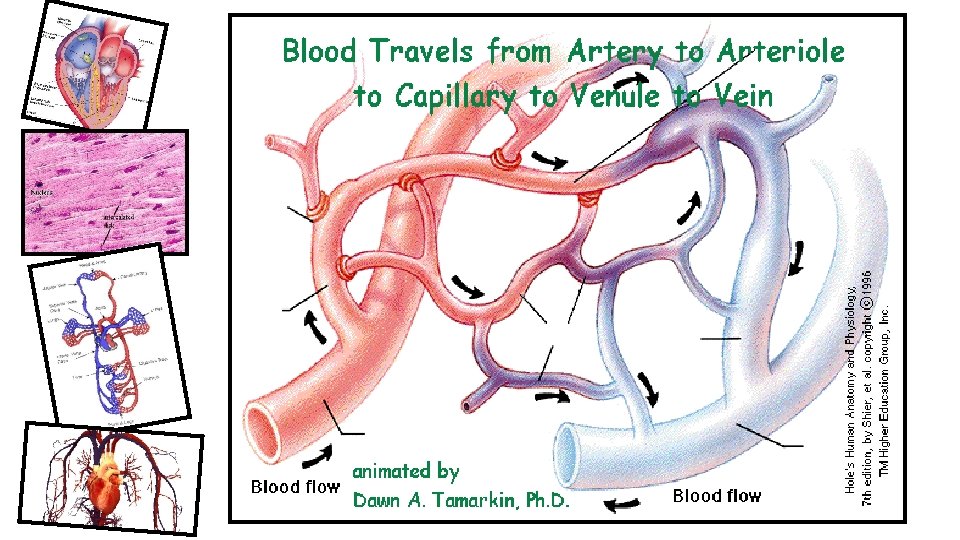
Blood Vessels • Vascular system: closed transport system of blood vessels • Blood flows from arteries (0. 1 mm-1 cm) arterioles (10 -100 µm) capillary beds venules (10 -100 µm) veins (0. 1 -1 mm)
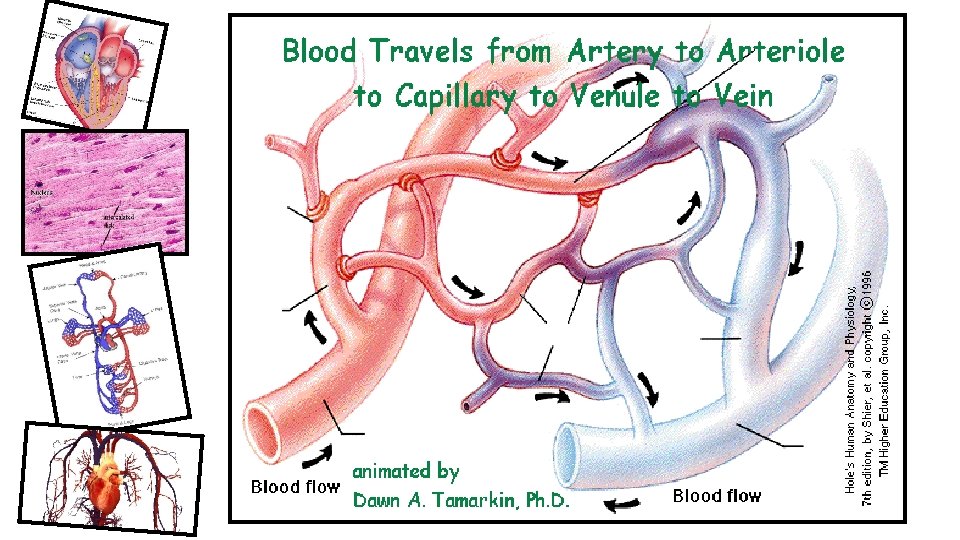
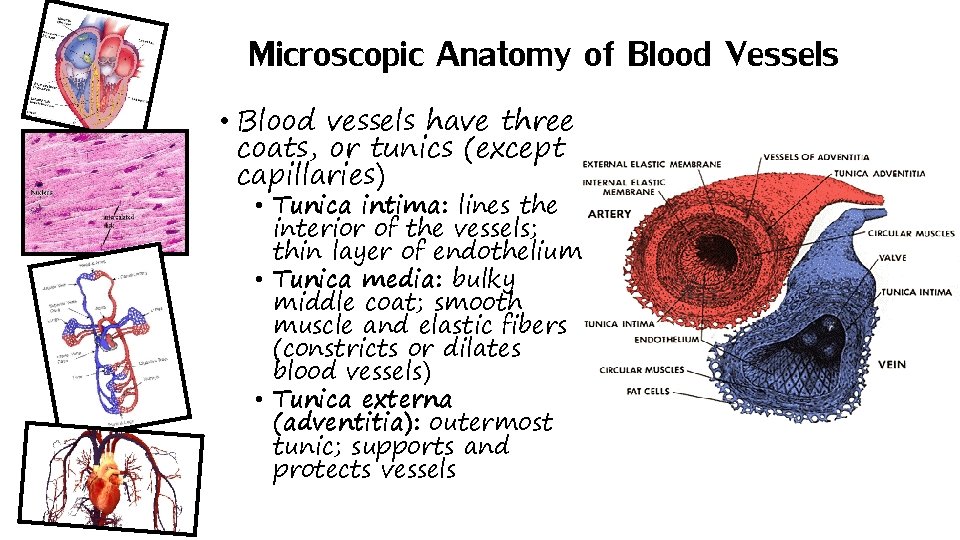
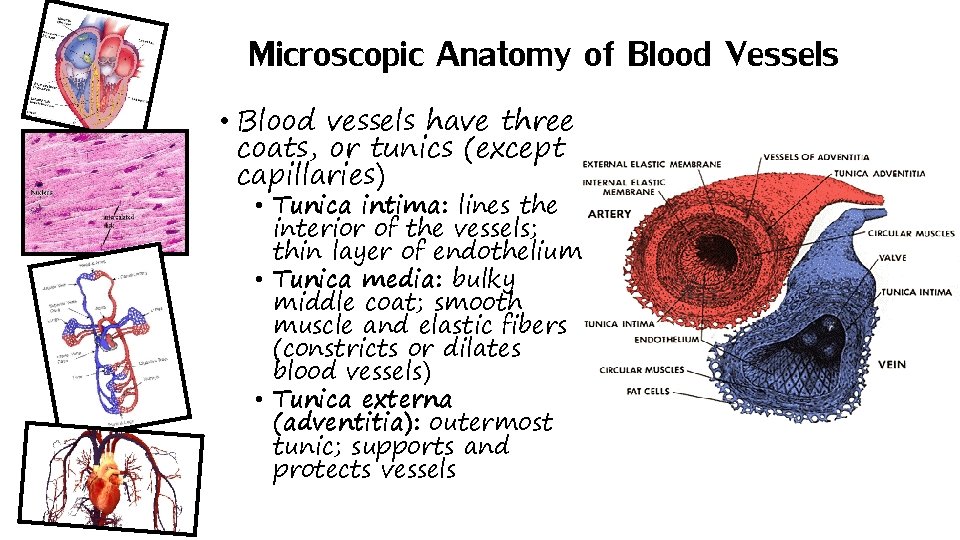
Microscopic Anatomy of Blood Vessels • Blood vessels have three coats, or tunics (except capillaries) • Tunica intima: lines the interior of the vessels; thin layer of endothelium • Tunica media: bulky middle coat; smooth muscle and elastic fibers (constricts or dilates blood vessels) • Tunica externa (adventitia): outermost tunic; supports and protects vessels
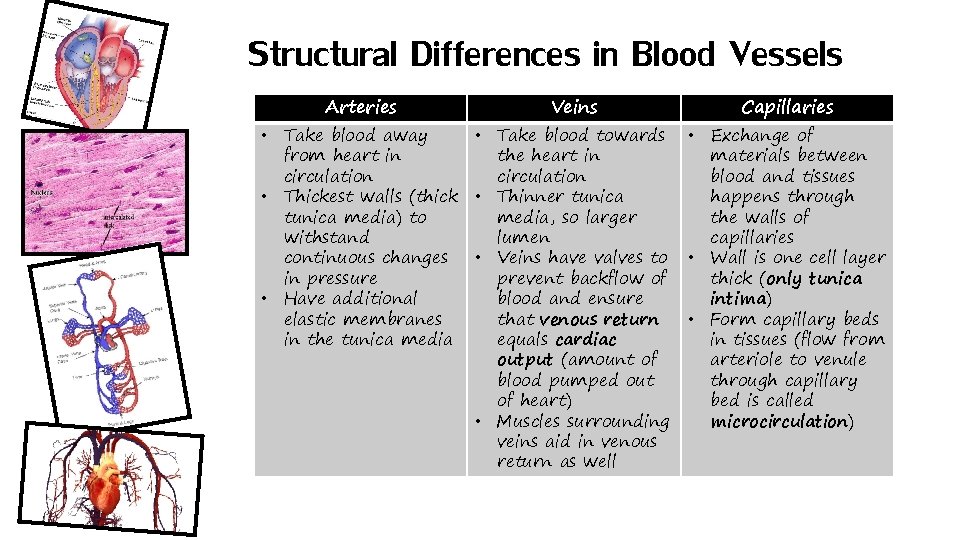
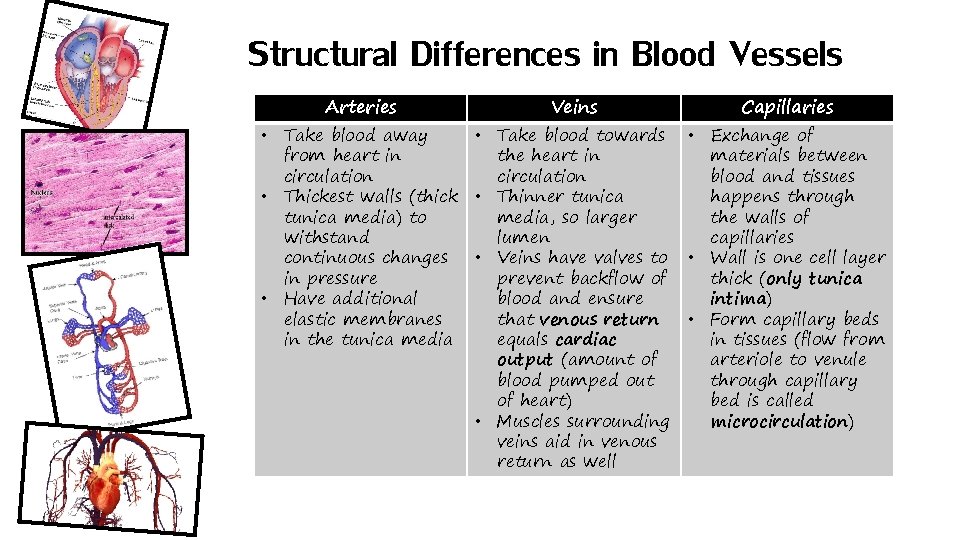
Structural Differences in Blood Vessels Arteries Veins • Take blood away • Take blood towards from heart in the heart in circulation • Thickest walls (thick • Thinner tunica media) to media, so larger withstand lumen continuous changes • Veins have valves to in pressure prevent backflow of • Have additional blood and ensure elastic membranes that venous return in the tunica media equals cardiac output (amount of blood pumped out of heart) • Muscles surrounding veins aid in venous return as well Capillaries • Exchange of materials between blood and tissues happens through the walls of capillaries • Wall is one cell layer thick (only tunica intima) • Form capillary beds in tissues (flow from arteriole to venule through capillary bed is called microcirculation)
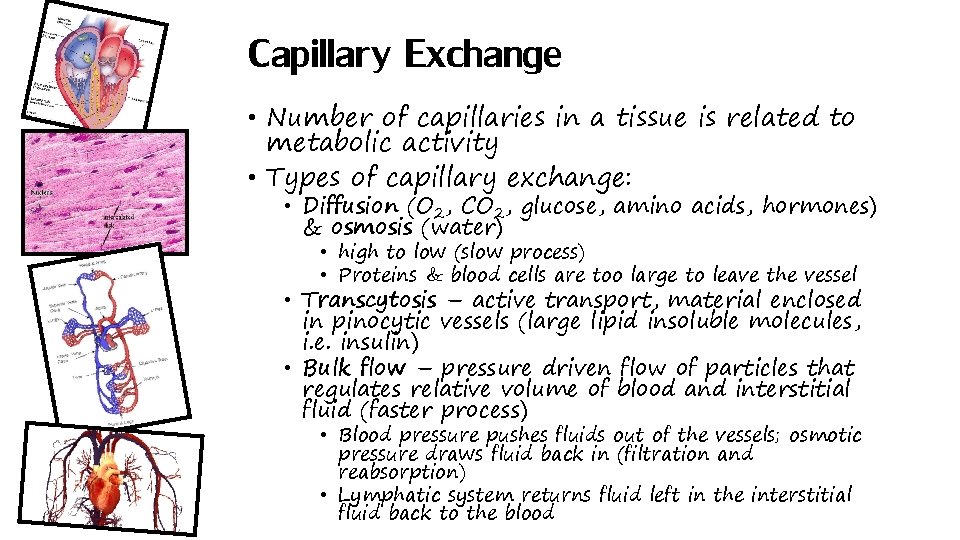
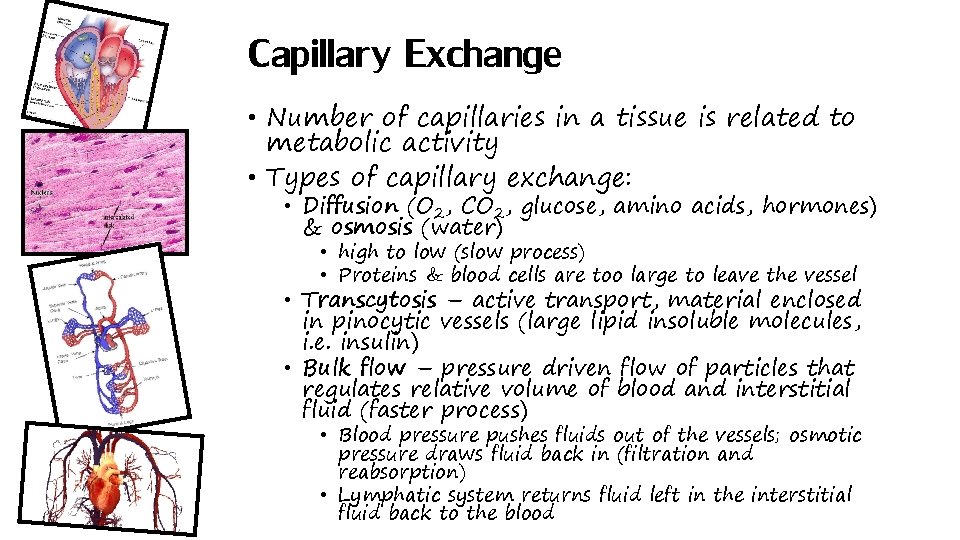
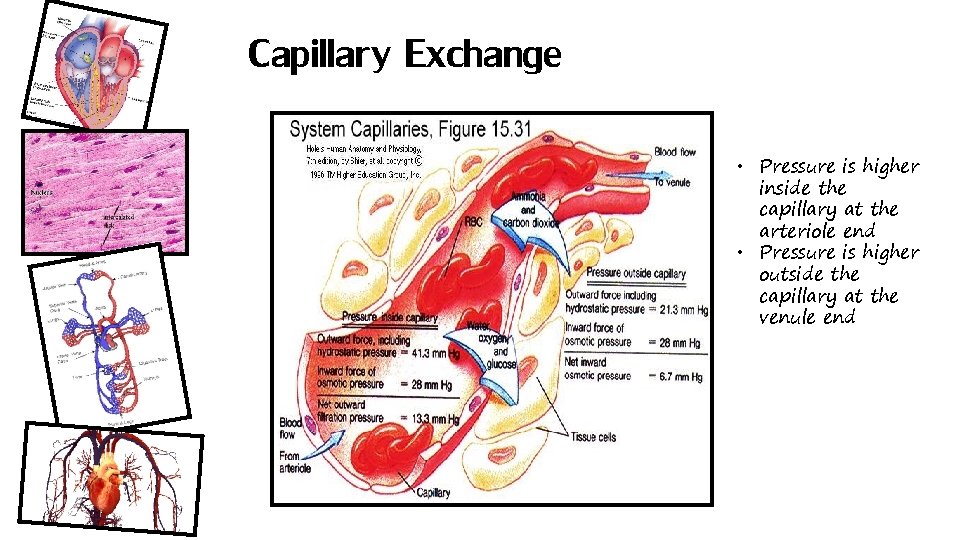
Capillary Exchange • Number of capillaries in a tissue is related to metabolic activity • Types of capillary exchange: • Diffusion (O 2, CO 2, glucose, amino acids, hormones) & osmosis (water) • high to low (slow process) • Proteins & blood cells are too large to leave the vessel • Transcytosis – active transport, material enclosed in pinocytic vessels (large lipid insoluble molecules, i. e. insulin) • Bulk flow – pressure driven flow of particles that regulates relative volume of blood and interstitial fluid (faster process) • Blood pressure pushes fluids out of the vessels; osmotic pressure draws fluid back in (filtration and reabsorption) • Lymphatic system returns fluid left in the interstitial fluid back to the blood
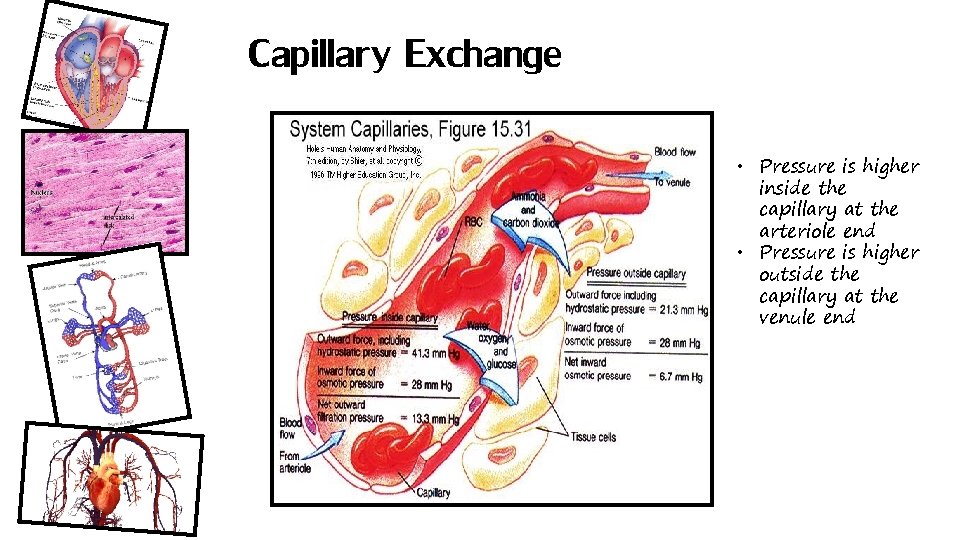
Capillary Exchange • Pressure is higher inside the capillary at the arteriole end • Pressure is higher outside the capillary at the venule end
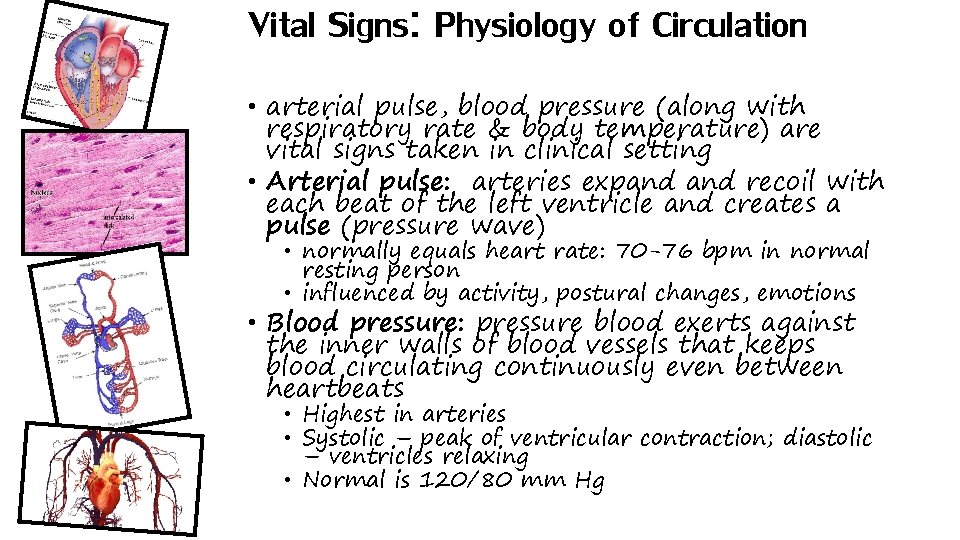
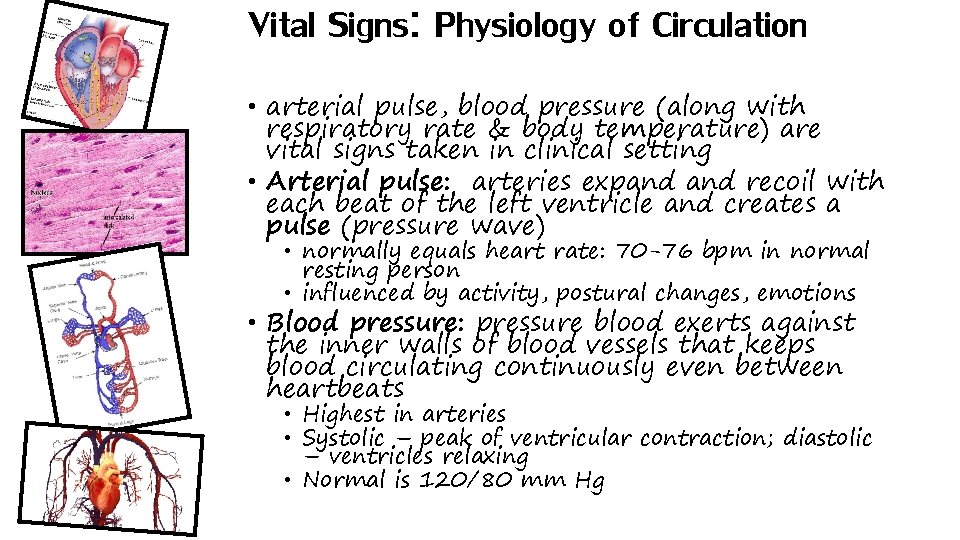
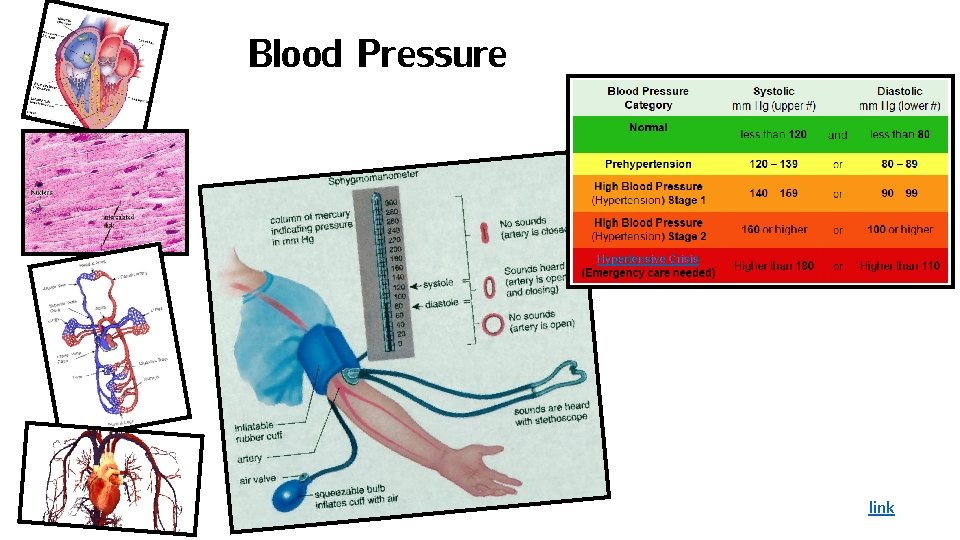
Vital Signs: Physiology of Circulation • arterial pulse, blood pressure (along with respiratory rate & body temperature) are vital signs taken in clinical setting • Arterial pulse: arteries expand recoil with each beat of the left ventricle and creates a pulse (pressure wave) • normally equals heart rate: 70 -76 bpm in normal resting person • influenced by activity, postural changes, emotions • Blood pressure: pressure blood exerts against the inner walls of blood vessels that keeps blood circulating continuously even between heartbeats • Highest in arteries • Systolic – peak of ventricular contraction; diastolic – ventricles relaxing • Normal is 120/80 mm Hg
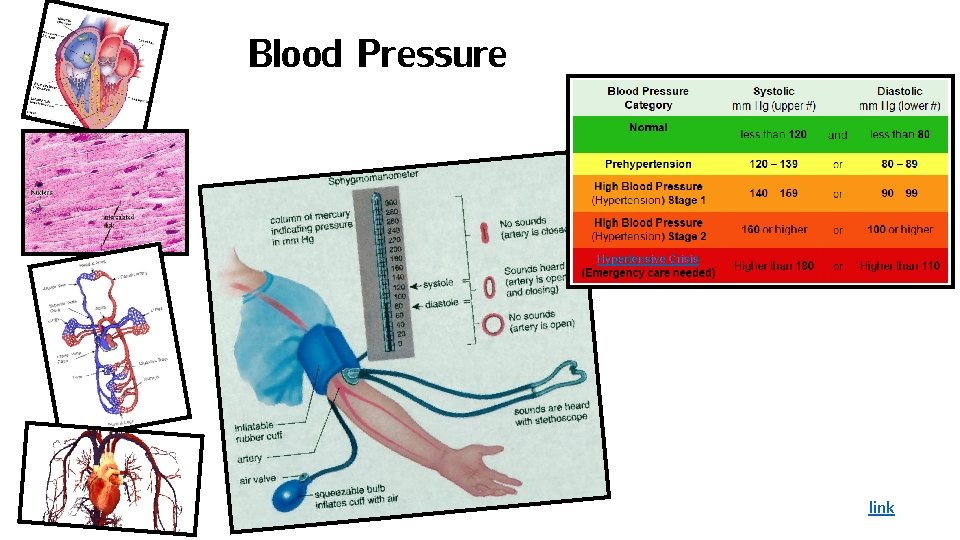
Blood Pressure link
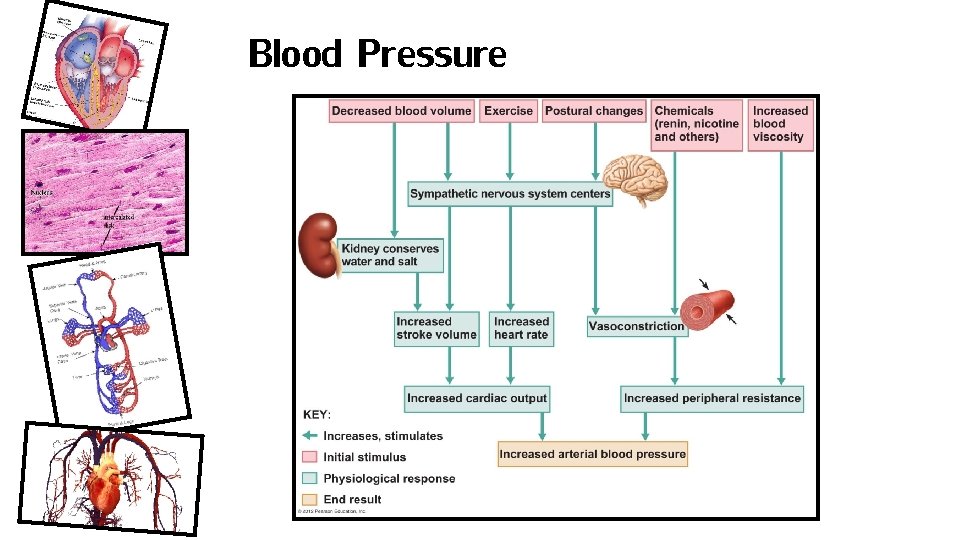
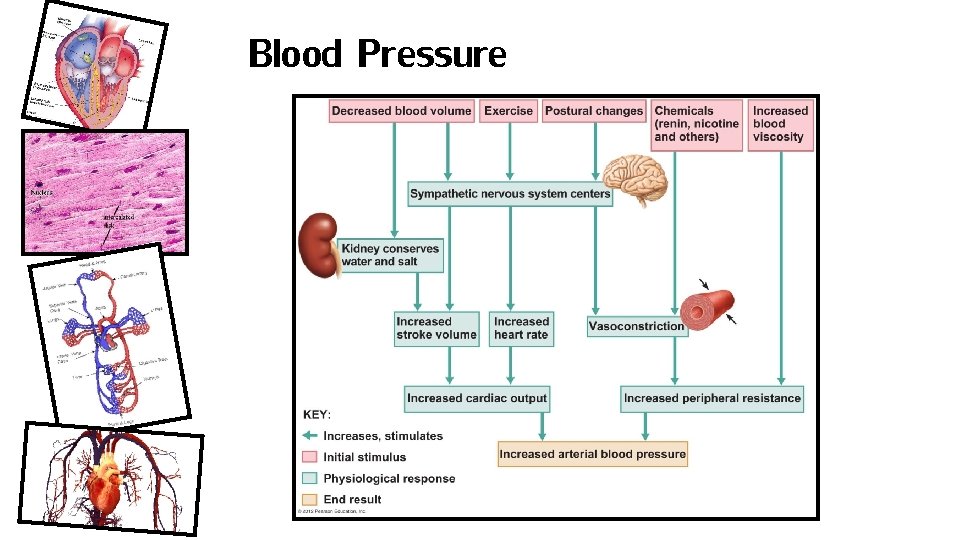
Blood Pressure
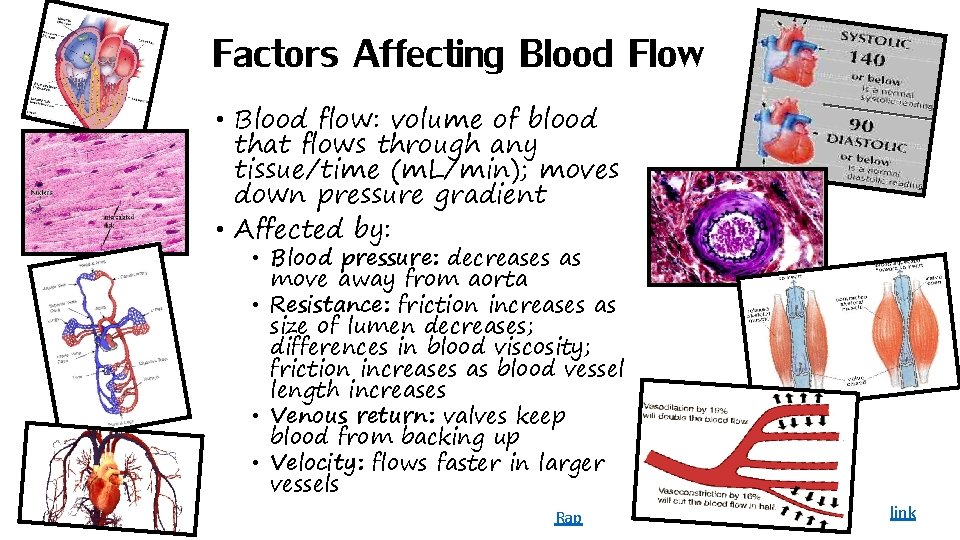
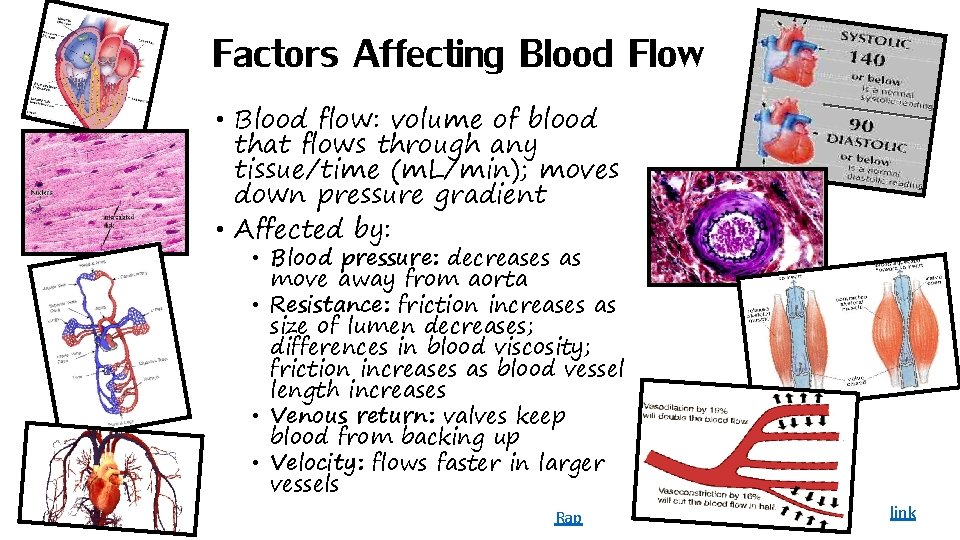
Factors Affecting Blood Flow • Blood flow: volume of blood that flows through any tissue/time (m. L/min); moves down pressure gradient • Affected by: • Blood pressure: decreases as move away from aorta • Resistance: friction increases as size of lumen decreases; differences in blood viscosity; friction increases as blood vessel length increases • Venous return: valves keep blood from backing up • Velocity: flows faster in larger vessels Rap link

link
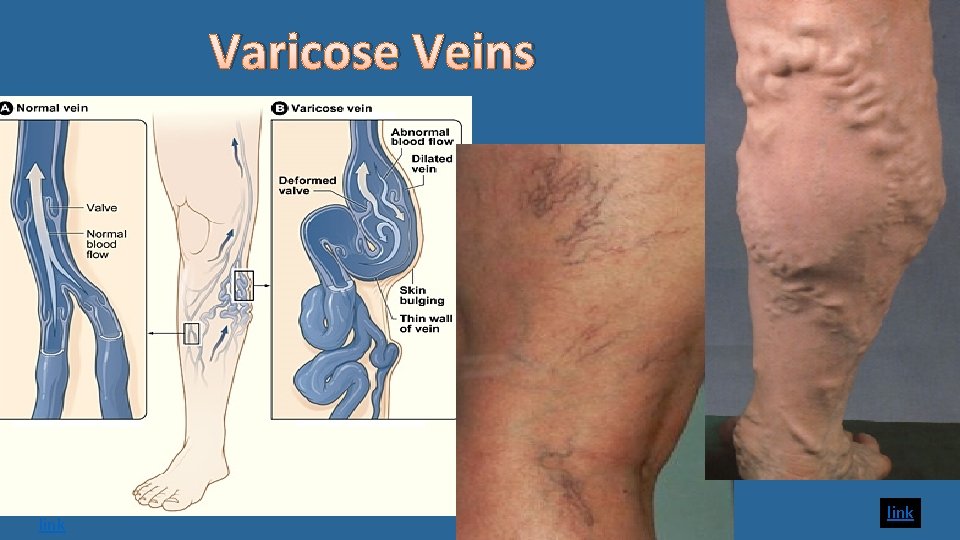
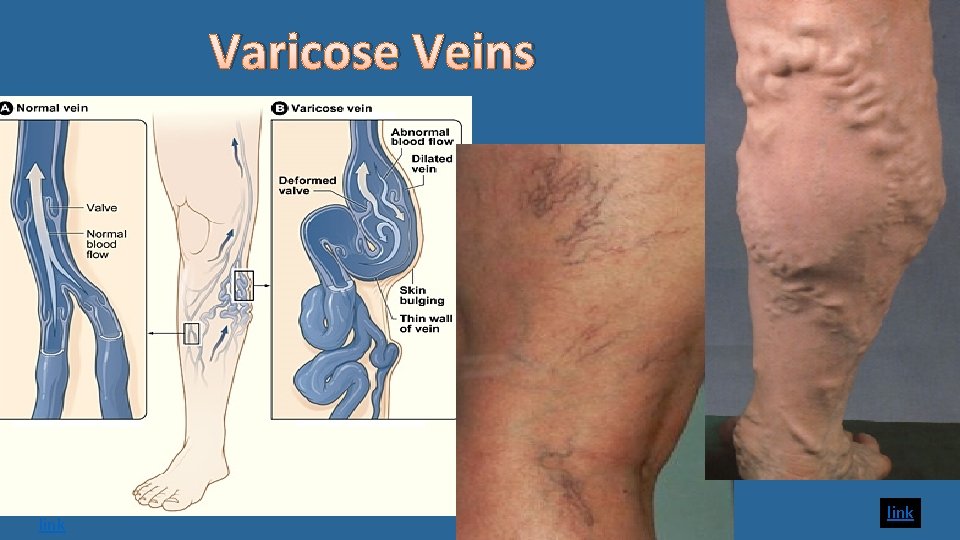
Varicose Veins link
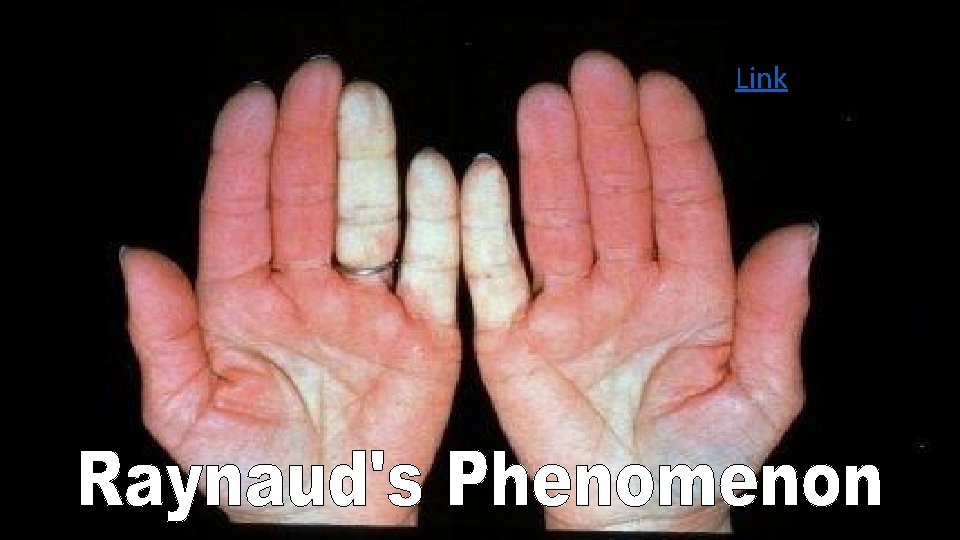
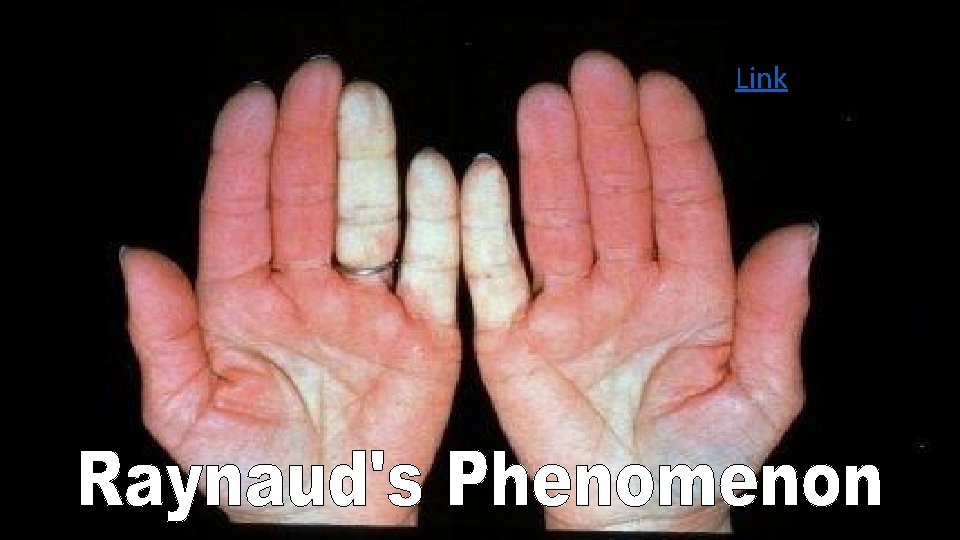
Link