Cardiovascular Disorders Congestive Heart Failure Congestive Heart Failure

- Slides: 45
Cardiovascular Disorders Congestive Heart Failure
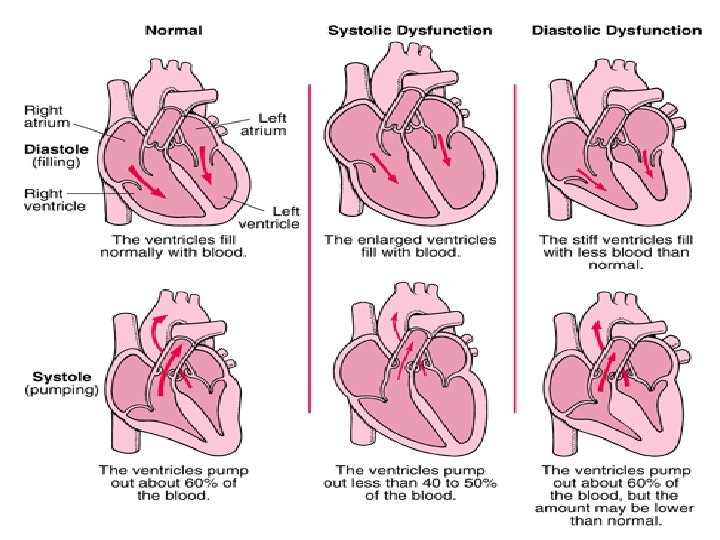
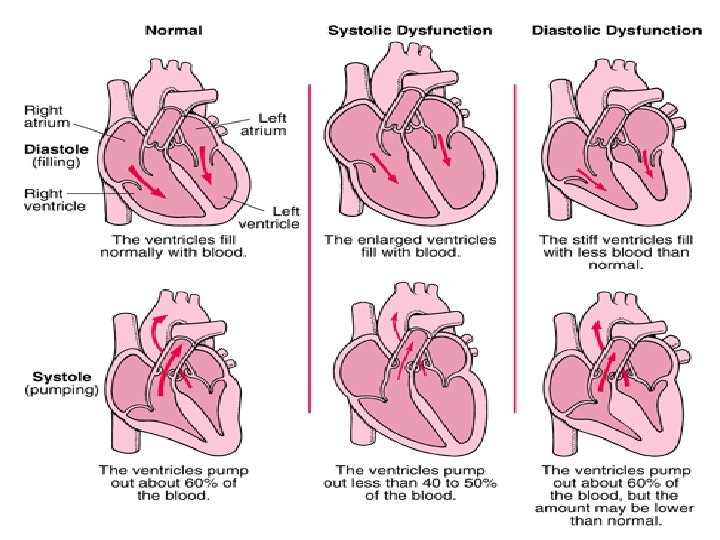
Congestive Heart Failure Definition Heart failure (HF) is a condition caused by the inability of the heart to pump sufficient blood to meet the metabolic needs of the body. Classification 1 -Systolic failure vs. Diastolic failure With systolic failure (problem in contraction): there is a decreased ejection of blood from the heart during systole. With diastolic failure (problem in the filling of ventricles), filling of the ventricles during diastole is reduced.
Congestive Heart Failure 2 - Low-output failure vs. High-output failure Low-output failure is a reduced pumping efficiency of the heart due to impair cardiac function (it includes systolic failure and diastolic failure). High-output failure, the cardiac output is normal or elevated but still cannot meet the metabolic and oxygen need of the tissues. Common causes of high-output failure include hyperthyroidism (hypermetabolism) and anaemia. Note: The term “heart failure” will refer to low-output HF in this lecture.
Congestive Heart Failure Etiology: Heart failure can be classified by the primary underlying etiology as ischemic or non-ischemic, with 70% of HF related to ischemia (Coronary artery disease). Non-ischemic etiologies include hypertension, viral illness, thyroid disease, ……. . etc.
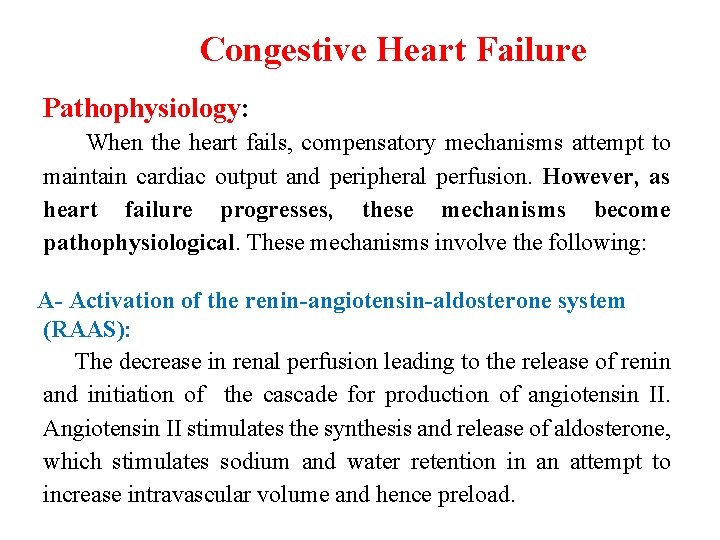
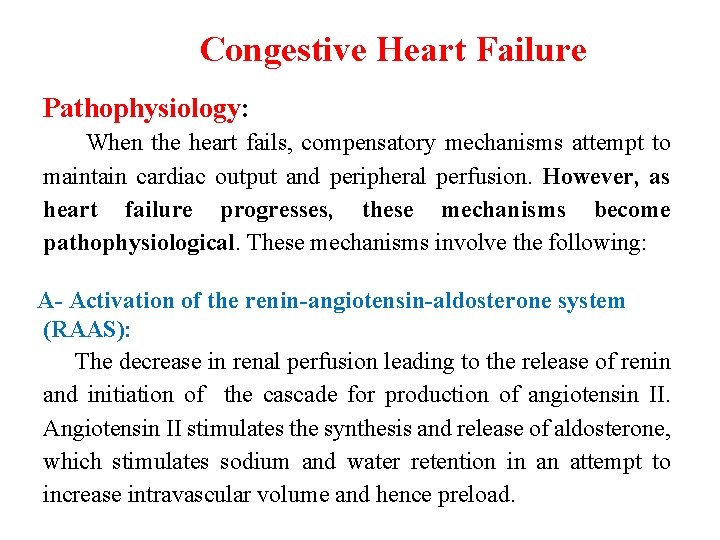
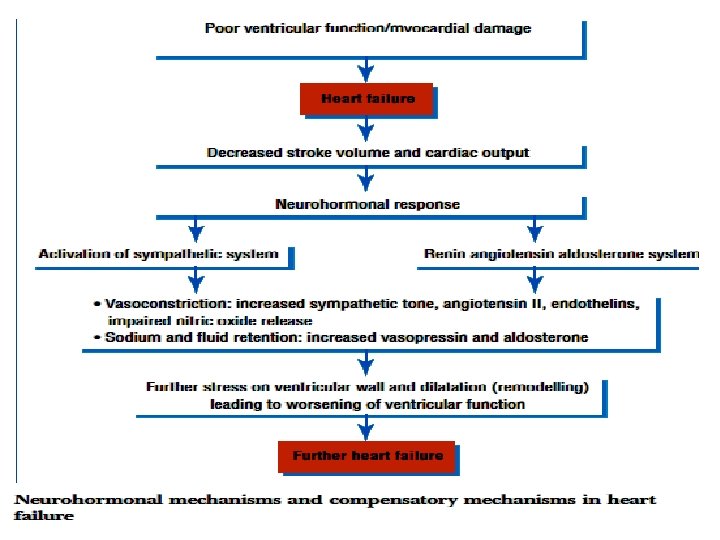
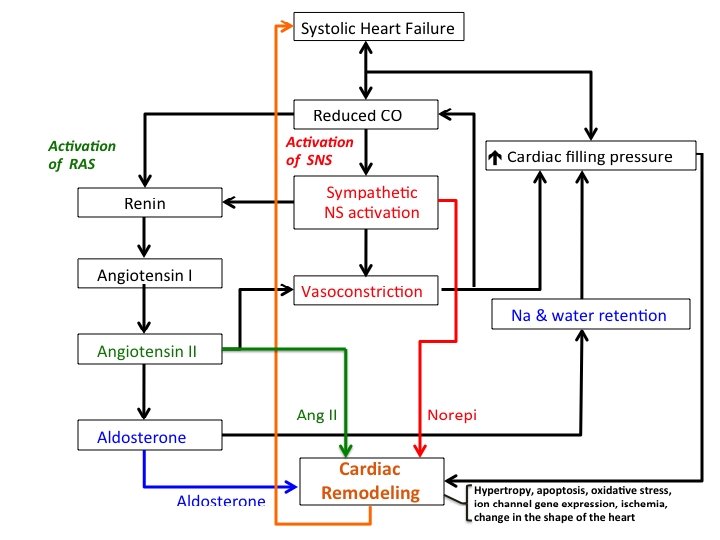
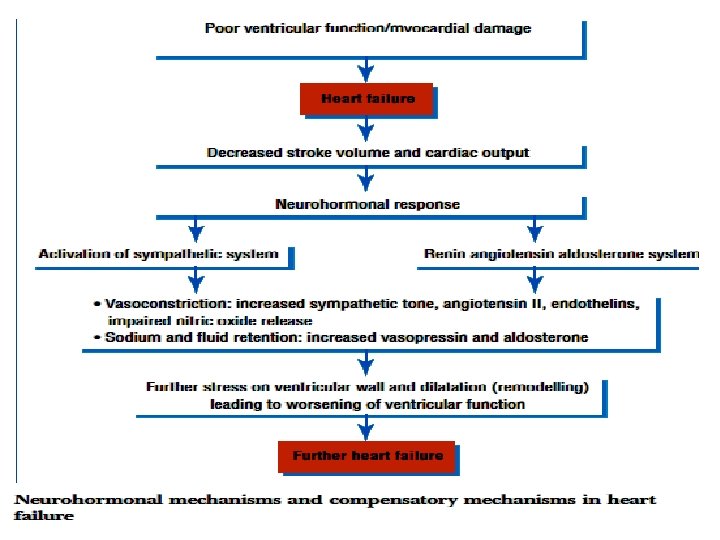
Congestive Heart Failure Pathophysiology: When the heart fails, compensatory mechanisms attempt to maintain cardiac output and peripheral perfusion. However, as heart failure progresses, these mechanisms become pathophysiological. These mechanisms involve the following: A- Activation of the renin-angiotensin-aldosterone system (RAAS): The decrease in renal perfusion leading to the release of renin and initiation of the cascade for production of angiotensin II. Angiotensin II stimulates the synthesis and release of aldosterone, which stimulates sodium and water retention in an attempt to increase intravascular volume and hence preload.
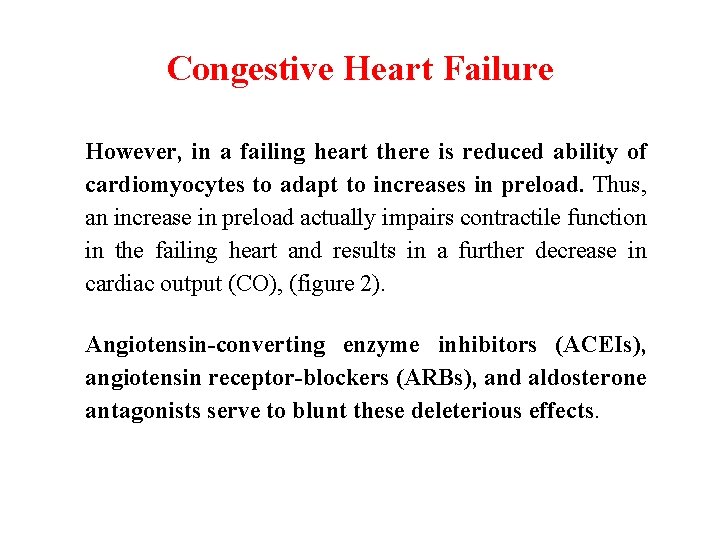
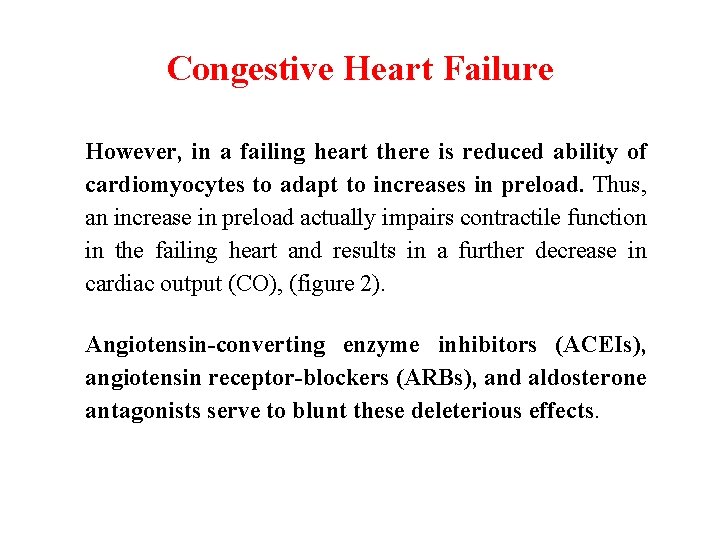
Congestive Heart Failure However, in a failing heart there is reduced ability of cardiomyocytes to adapt to increases in preload. Thus, an increase in preload actually impairs contractile function in the failing heart and results in a further decrease in cardiac output (CO), (figure 2). Angiotensin-converting enzyme inhibitors (ACEIs), angiotensin receptor-blockers (ARBs), and aldosterone antagonists serve to blunt these deleterious effects.
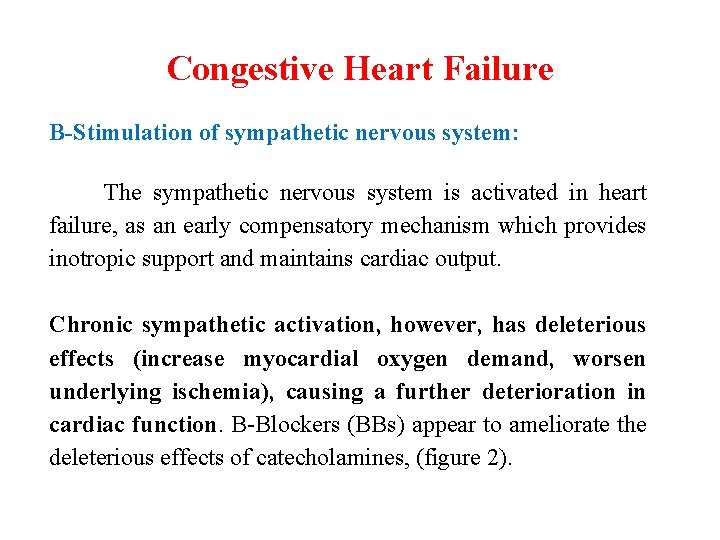
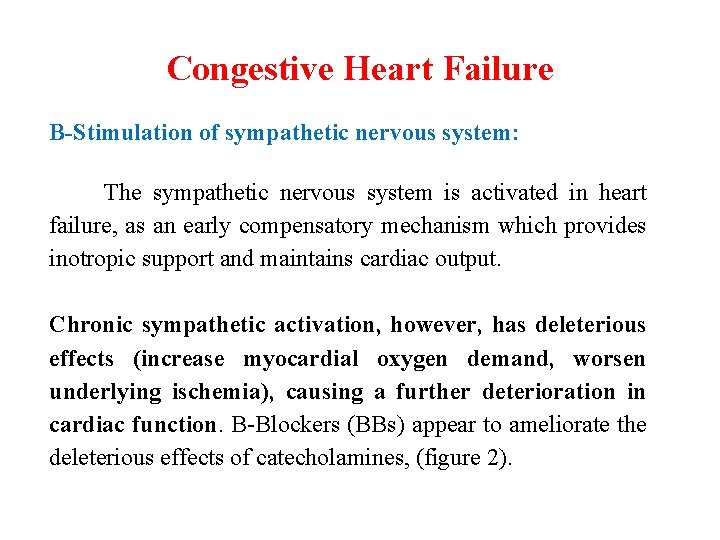
Congestive Heart Failure B-Stimulation of sympathetic nervous system: The sympathetic nervous system is activated in heart failure, as an early compensatory mechanism which provides inotropic support and maintains cardiac output. Chronic sympathetic activation, however, has deleterious effects (increase myocardial oxygen demand, worsen underlying ischemia), causing a further deterioration in cardiac function. Β-Blockers (BBs) appear to ameliorate the deleterious effects of catecholamines, (figure 2).
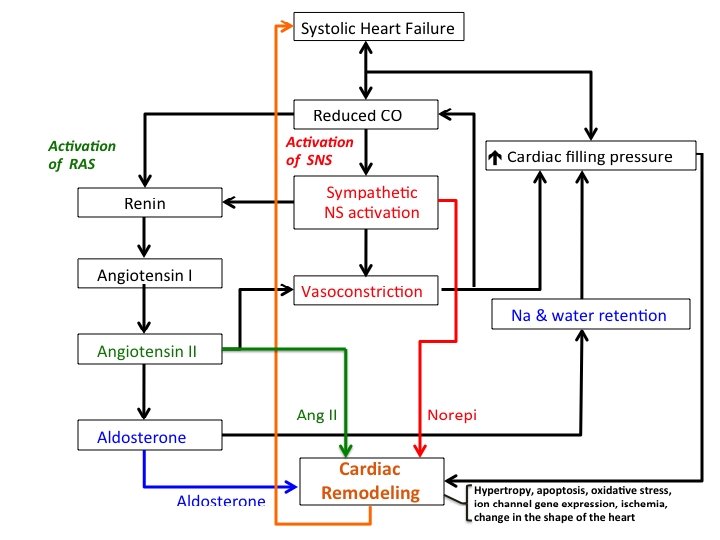
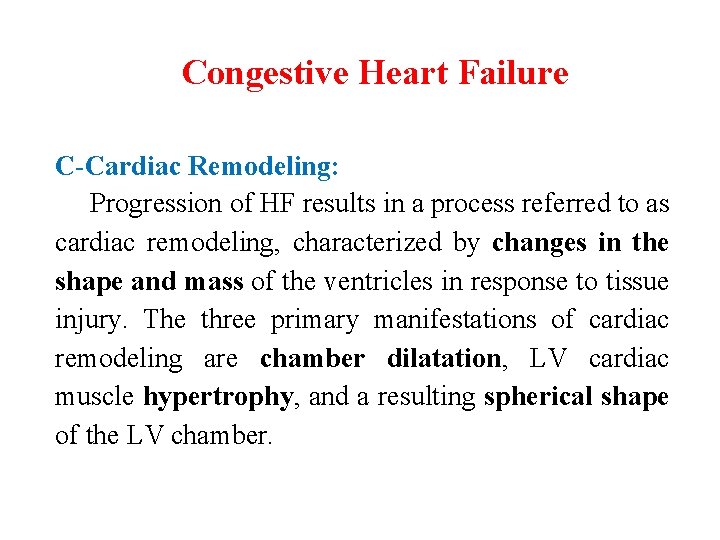
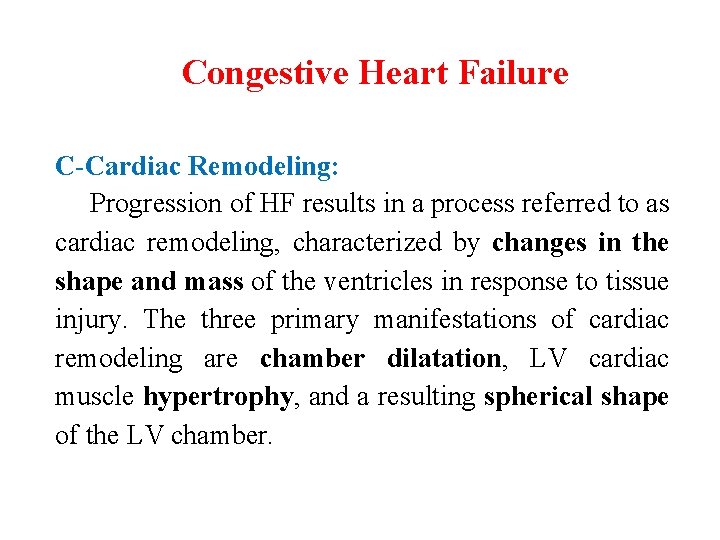
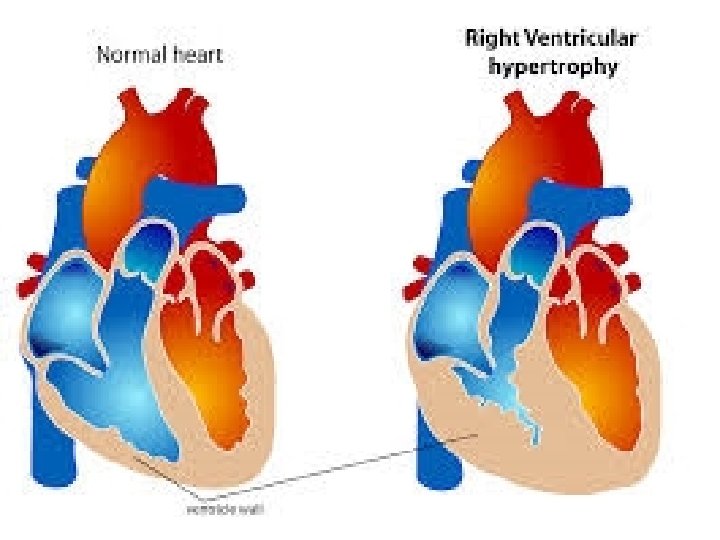
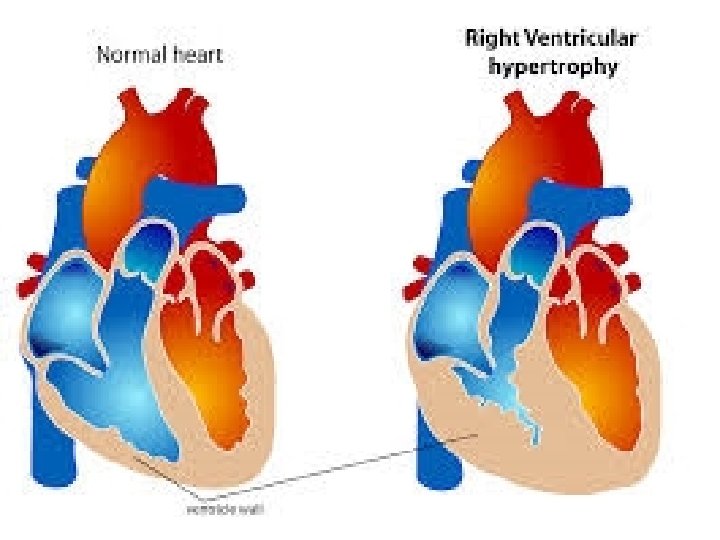
Congestive Heart Failure C-Cardiac Remodeling: Progression of HF results in a process referred to as cardiac remodeling, characterized by changes in the shape and mass of the ventricles in response to tissue injury. The three primary manifestations of cardiac remodeling are chamber dilatation, LV cardiac muscle hypertrophy, and a resulting spherical shape of the LV chamber.

Congestive Heart Failure Clinical Manifestations The resulting fluid backup (from the left ventricle into the lungs; from the right ventricle into peripheral circulation) produces the signs and symptoms of HF. A-Left-sided failure. If blood cannot be adequately pumped from the left ventricle to the peripheral circulation, the blood will backs up into the pulmonary alveoli the result is the development of pulmonary congestion and edema. Patients can experience a variety of symptoms (Dyspnea, or shortness of breath (SOB)), related to buildup of fluid in the lungs.
Congestive Heart Failure 1 -Exertional dyspnea: occurs when patients describe breathlessness induced by physical activity or a lower level of activity than previously known to cause breathlessness. Patients often state that activities such as stair climbing, carrying groceries, or walking a particular distance cause shortness of breath. 2 -Orthopnea: Orthopnea is present if a patient is unable to breathe while lying flat on a bed (i. e. , in the recumbent position). It manifests within minutes of a patient lying down and is relieved immediately when the patient sits upright. Patients can relieve orthopnea by elevating their head and shoulders with pillows.
Congestive Heart Failure 3 -Paroxysmal nocturnal dyspnea (PND) occurs when patients awaken suddenly with a feeling of breathlessness and suffocation. PND is caused by increased venous return and mobilization of interstitial fluid from the extremities, leading to alveolar edema and usually occurs within 1 to 4 hours of sleep. In contrast to orthopnea, PND is not relieved immediately by sitting upright and often takes up to 30 minutes for symptoms to Subside.
Congestive Heart Failure 4 - In cases of pulmonary edema, the most severe form of pulmonary congestion, patients may produce a pink, frothy sputum and experience extreme breathlessness and anxiety due to feelings of suffocation and drowning. If not treated aggressively, patients can become cyanotic and acidotic. 5 - “Rales” or crackling sounds that may be heard through a stethoscope as a result of fluid accumulation in the lungs.
Congestive Heart Failure B-Right-sided failure: When blood is not pumped from the right ventricle, the blood backs up throughout the body (e. g. , in the veins, liver, legs, bowels), producing systemic congestion and edema. Edema is especially noticeable in the legs (ankles edema) because gravity pulls the fluid into the lower half of the body.
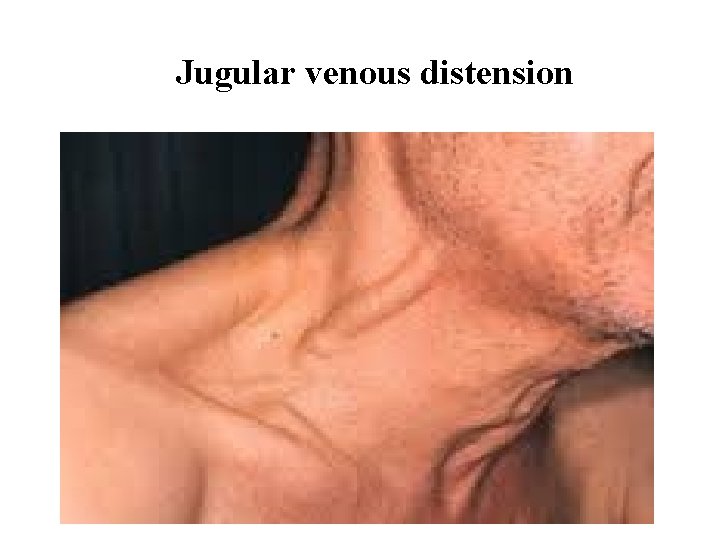
Congestive Heart Failure Abdominal congestion may cause a bloated feeling, abdominal pain, nausea, anorexia, and constipation. Often patients may have difficulty fitting into their shoes or pants due to edema. Jugular venous distension: which represent a sign of elevated pressures in the venous system Although most patients initially have left ventricular failure (LVF; pulmonary congestion), and because LVF increases the workload of the right ventricle, both ventricles eventually fail.
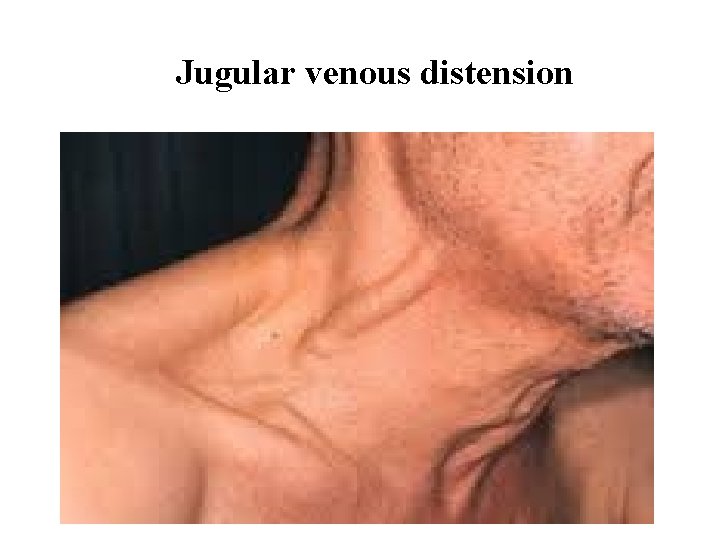
Jugular venous distension
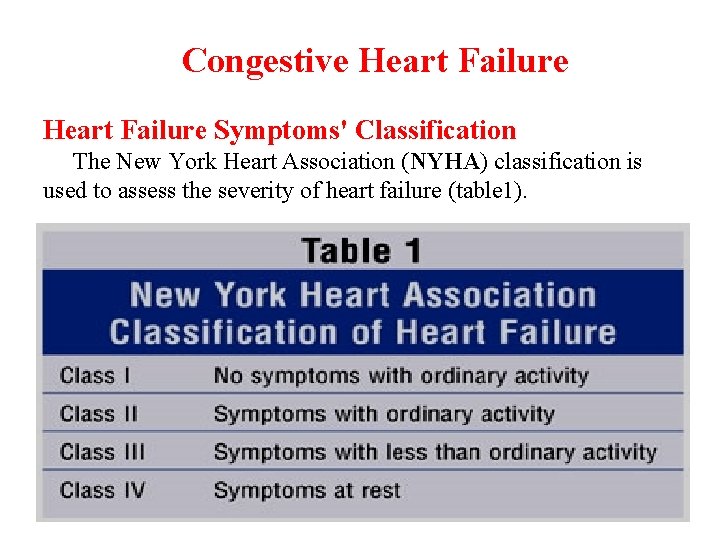
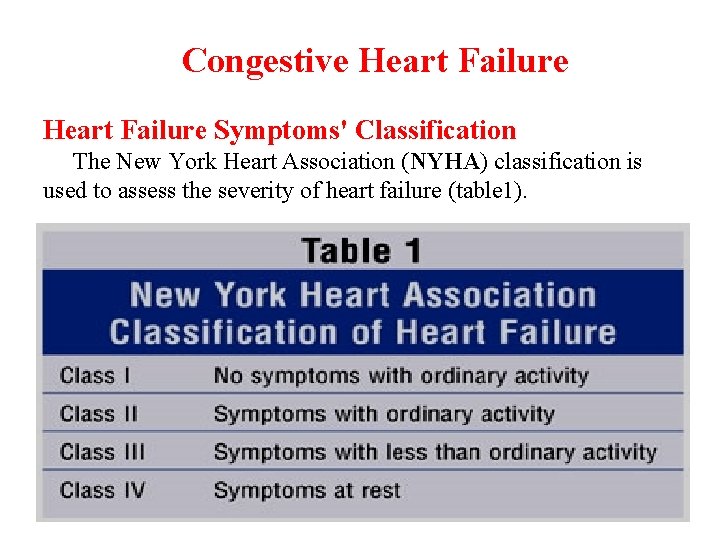
Congestive Heart Failure Symptoms' Classification The New York Heart Association (NYHA) classification is used to assess the severity of heart failure (table 1).
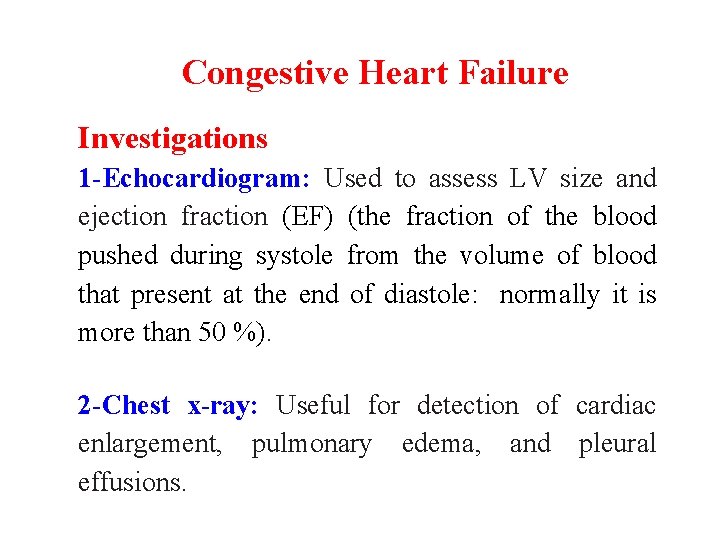
Congestive Heart Failure Investigations 1 -Echocardiogram: Used to assess LV size and ejection fraction (EF) (the fraction of the blood pushed during systole from the volume of blood that present at the end of diastole: normally it is more than 50 %). 2 -Chest x-ray: Useful for detection of cardiac enlargement, pulmonary edema, and pleural effusions.
Congestive Heart Failure 3 -Electrocardiogram (ECG): To assesses the presence of any other cardiac problems, such as arrhythmias. 4 -Blood tests: full blood to investigate anaemia, serum creatinine, urea and electrolytes to assess renal function.
Congestive Heart Failure Desired Outcome The therapeutic goals for chronic HF is to relieve or reduce symptoms, slow disease progression, and prolong survival. Treatment The first step in managing chronic HF is to determine the etiology or precipitating factors. Treatment of underlying disorders (e. g. , anemia, hyperthyroidism) may obviate the need for treating HF.
Congestive Heart Failure Non-pharmacologic Interventions Non-pharmacologic treatment involves: 1 - Dietary modifications in HF consist of sodium restriction, and sometimes fluid restriction. Patients should routinely practice moderate salt restriction (2– 2. 5 g sodium or 5– 6 g salt per day). Patients should be educated to avoid cooking with salt and to limit intake of foods with high salt content. Fluid restriction may not be necessary in many patients. When applicable, a general recommendation is to limit fluid intake from all sources to less than 2 liters per day.
Congestive Heart Failure 2 - Exercise, while discouraged when the patient is acutely decompensated, is recommended when patients are stable. The heart is a muscle that requires activity to prevent atrophy. Regular low intensity, aerobic exercise that includes walking, swimming, or riding a bike is encouraged, while heavy weight training is discouraged.
Congestive Heart Failure 3 -Modification of classic risk factors, such as tobacco and alcohol consumption, is important to minimize the potential for further aggravation of heart function.
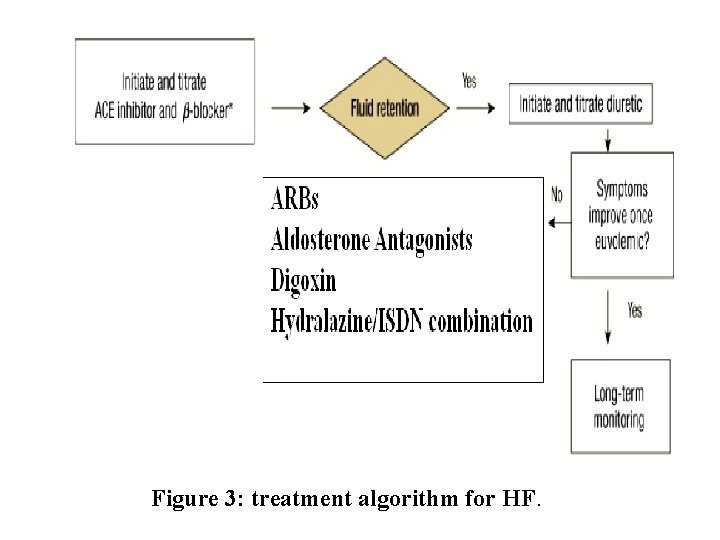
Congestive heart failure Pharmacologic Treatment A-Systolic Heart Failure Agents with proven benefits in improving symptoms, slowing disease progression, and improving survival in chronic HF, targets the neurohormonal blockade. These include ACE inhibitors, ARBs, β-adrenergic blockers, and aldosterone antagonists in select patients.
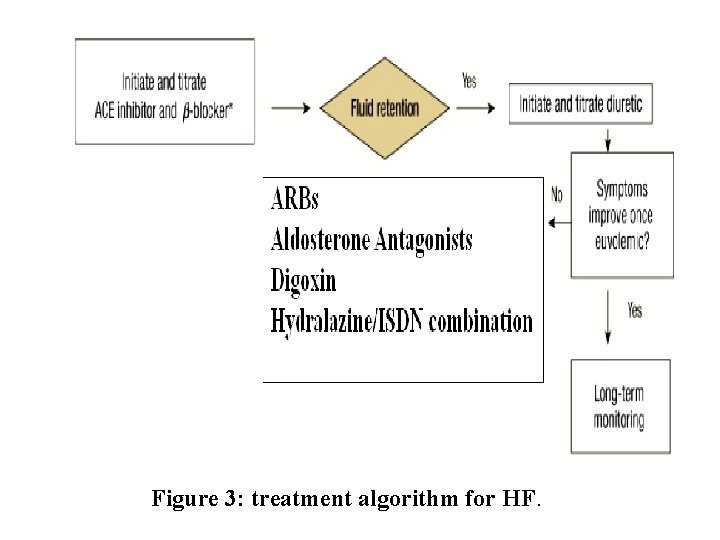
Figure 3: treatment algorithm for HF.
Congestive heart failure 1 -Angiotensin-Converting Enzyme(ACE) Inhibitors 1 - There is strong evidence that ACE inhibitors (like captopril, lisinopril, enalapril, …. . ) slow disease progression, decrease hospitalizations, and reduce mortality in patients with HF. 2 - The ACC/AHA (American college of cardiology and American heart association) guidelines state that ACE inhibitors should be prescribed to all patients with HF that
Congestive heart failure caused by left ventricular systolic dysfunction (LVSD) unless they have a contraindication to their use or have been shown to be unable to tolerate treatment with these drugs. In general, ACE inhibitors are used together with β-blockers. 3 - ACE inhibitors should be initiated at low doses, followed by increments in dose if lower doses have been well tolerated.
Congestive heart failure 2 -β-Blockers 1 - There is strong evidence that certain β-blockers slow disease progression, decrease hospitalization, and reduces mortality in patients with HF. 2 - The ACC/AHA guidelines state that β-blockers should be prescribed to all patients with stable systolic HF unless they have a contraindication to their use or are unable to tolerate the treatment.
Congestive heart failure Extended-release metoprolol succinate, carvedilol, and bisoprolol are FDA approved for use in HF. Metoprolol and bisoprolol are both partially selective β 1 -lockers, and carvedilol is a mixed α 1 - and nonselective β-blocking agent. Note: It cannot be assumed that immediate-release metoprolol (which the firm used in Iraq now) will provide benefits equivalent to Extended-release metoprolol.
Congestive heart failure 3 - β-Blockers should be initiated in stable patients who have no or minimal evidence of fluid overload, because of their negative inotropic effects. β-blockers should be started in very low doses with slow upward dose titration (in a ‘start low, go slow’ fashion) to avoid symptomatic worsening. Doses should be doubled no more often than every 2 weeks, as tolerated, until the target dose or the maximally tolerated dose is reached.
Congestive heart failure Diuretics 1 - Loop and thiazide diuretics have not been shown to improve survival in heart failure. Consequently, diuretic therapy (in addition to sodium restriction) is recommended in all patients with clinical evidence of fluid retention (peripheral and pulmonary edema). Patients who do not have fluid retention would not require diuretic therapy. 2 - Loop diuretics (furosemide, bumetanide, and torsemide) are the most widely used diuretics in HF.
Congestive heart failure Second-line therapy (Drug Therapies to Consider for Selected Patients) Those who remain symptomatic despite optimal therapy with ACEIs and BBs can be considered for the addition of a second line pharmacological agent for HF-LVSD. These second-line agents have proven efficacy when combined with first-line treatment in reducing heart failure morbidity and mortality.
Congestive heart failure It includes: 1 -Aldosterone antagonists 2 -Combined hydralazine and nitrate. 3 -ARBs. 1 -Aldosterone Antagonists 1 - There is evidence that aldosterone mediates some of the major effects of renin–angiotensin–aldosterone system activation, such as myocardial remodeling and fibrosis, as well as sodium retention and potassium loss at the distal tubules.
Congestive heart failure 2 - Currently, the aldosterone antagonists available are spironolactone and eplerenone. Both agents are inhibitors of aldosterone that produce weak diuretic effects while sparing potassium concentrations. . Eplerenone is selective for the mineralocorticoid receptor and hence does not exhibit the endocrine adverse-effect profile commonly seen with spironolactone.
Congestive heart failure 3 - Currently low-dose aldosterone antagonists (e. g. 25 mg/day spironolactone) should be added for: (1) Patients with symptoms of moderate to severe heart failure (New York Heart Association (NYHA) class III-IV) who are receiving standard therapy; and (2) Those with LV dysfunction early after MI (where heart failure occurs in the first 4 weeks after an acute myocardial infarction.
Congestive heart failure 2 -Angiotensin II Receptor Blockers (ARBs) 1 - Although some data suggest that ARBs produce equivalent mortality benefits when compared with ACE inhibitors, the ACC/AHA guidelines recommend use of ARBs only in patients who are intolerant of ACE inhibitors. Although there are currently many ARBs in the market, only candesartan and valsartan are FDAapproved for the treatment of HF and are the preferred agents, whether used alone or in combination with ACE inhibitors.
Congestive heart failure 2 - Combination therapy with an ARB and ACE inhibitor offers a theoretical advantage over either agent alone through more complete blockade of the deleterious effects of angiotensin II. However, clinical trial results indicate that the addition of an ARB to optimal HF therapy (e. g. , ACE inhibitors, β-blockers, and diuretics) offers marginal benefits at best with increased risk of adverse effects. The addition of an ARB may be considered with patients who remain symptomatic despite receiving optimal conventional therapy.
Congestive heart failure 3 -Nitrates and Hydralazine 1 - Nitrates (e. g. , ISDN) and Hydralazine are combined in the treatment of HF because of their complementary hemodynamic actions. Hydralazine is a potent arterial dilating agent that provides symptomatic relief of HF by decreasing afterload. Nitrates have venous dilating properties that decrease preload. 2 - The combination may be reasonable for patients with persistent symptoms despite optimized therapy with an ACE inhibitor (or ARB) and β-blocker. The combination is also appropriate as first-line therapy in patients unable to tolerate ACE inhibitors or ARBs.
Congestive heart failure 4 - Digoxin 1 - Digoxin does not improve survival in patients with HF but does provide symptomatic Benefits (decreases symptoms, increases exercise performance, and decreases hospital admissions secondary to HF). 2 - Current recommendations are for the addition of digoxin for patients who remain symptomatic despite an optimal HF regimen consisting of an ACE inhibitor or ARB, β-blocker, and diuretic.
Congestive heart failure 3 - Digoxin is also prescribed routinely in patients with HF and concurrent atrial Fibrillation (AF) to slow ventricular rate regardless of HF symptomology. 4 - In the absence of AF a loading dose is not indicated. Digoxin is initiated at a dose of 0. 125 to 0. 25 mg daily (depending on age, renal function, ………. ). The 0. 125 mg daily dose is adequate in the majority of patients. Routine monitoring of serum drug concentrations is not required but recommended in those with changes in renal function, suspected toxicity, or after addition or subtraction of an interacting drug.
Congestive heart failure B-Heart Failure Caused by Diastolic Dysfunction Diastolic dysfunction, an inadequacy of ventricular relaxation and impaired LV filling. Diastolic dysfunction is characterized by a normal or nearnormal LVEF (40% to 60%). For symptomatic patients, diuretics in conjunction with salt restriction are indicated initially to relieve congestive symptoms. Thereafter, β-adrenergic blockers, calcium channel blockers (e. g. , verapamil), or ACE inhibitors, and ARBs, may be beneficial.
Congestive heart failure Note : Unlike in systolic HF, nondihydropyridine calcium channel blockers (diltiazem and verapamil) may be useful in heart failure caused by diastolic dysfunction.