TETRALOGY OF FALLOT TOF Mary Beth Sanders BSN
TETRALOGY OF FALLOT (TOF) Mary Beth Sanders BSN & Laura Durbin BSN East Carolina University College of Nursing, Greenville, North Carolina
Incidence and Risk • occurs in 3 of every 10, 000 live births. • most common cause of cyanotic cardiac disease in patients beyond the neonatal age • accounts for up to one-tenth of all congenital cardiac lesions • There a number of state-based programs monitoring CHDs among newborns and young children, but currently no population-based tracking system exists to look at this growing population of older children and adults with heart defects. • It is the least diagnosed CHD during the prenatal period. • Factors that increase the risk for this condition during pregnancy include: Alcoholism in the mother Diabetes Mother who is over 40 years old Poor nutrition during pregnancy Rubella or other viral illnesses during pregnancy • Maternal intake of retinoic acid in 1 st trimester • • • Associated conditions • trisomies 21, 18, 13 • microdeletions of chromosome 22 • Di. George Syndrome. • 3% risk of recurrence in a family
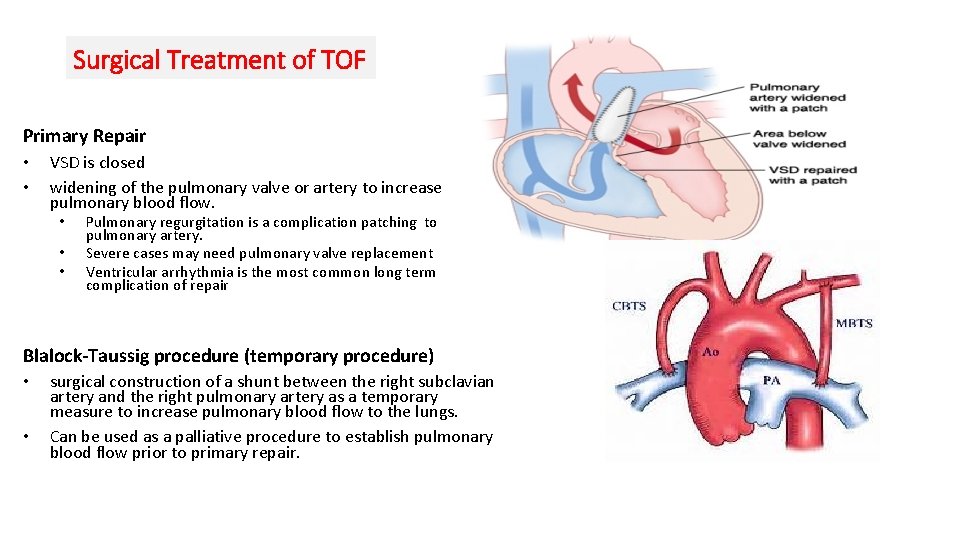
Surgical Treatment of TOF Primary Repair • • VSD is closed widening of the pulmonary valve or artery to increase pulmonary blood flow. • • • Pulmonary regurgitation is a complication patching to pulmonary artery. Severe cases may need pulmonary valve replacement Ventricular arrhythmia is the most common long term complication of repair Blalock-Taussig procedure (temporary procedure) • • surgical construction of a shunt between the right subclavian artery and the right pulmonary artery as a temporary measure to increase pulmonary blood flow to the lungs. Can be used as a palliative procedure to establish pulmonary blood flow prior to primary repair.
Prostaglandin E (PGE) • Stabilizes infants with severe cyanosis by reopening or maintaining the ductus arteriosus • In most infants, the ductus will reopen within 30 minutes to 2 hours after starting PGE 1 • Administered as a continuous IV infusion at 0. 05 -0. 2 ug/kg/min. • Side effects include • • Refractory hypotension from vasodilation Apnea Hyperthermia/ Flushing Seizures • Pharmacology • Prostaglandins are long chain unsaturated fatty acids produced by the action of the enzyme clooxygenase and are classified into groups E, D, A, F & B • PGE is also produced in the kidney in response to decreased renal blood flow prevents vasoconstriction and renal ischemia • PGE vasodilates all arterioles, inhibits platelet aggregation, and stimulates uterine and intestinal smooth muscles.
Physiology of TOF Four Different Defects In TOF • large ventral septal defect: An opening between the 2 bottom chambers of the heart. • Pulmonary valve stenosis or atresia: Pulmonary blood flow obstruction. This is due to a narrowing at the pulmonary valve or the pulmonary arteries. • Right ventricular hypertrophy: Caused by the heart working harder to pump blood through the body because of the narrow pulmonary valve. Overriding aorta: The aorta overrides the ventral septal defect.
Tetralogy of Fallot Pink TOF Blue TOF • Mild outflow tract obstruction • Severe outflow tract obstruction is present. • Blood is shunted from left to right. • Blood is able to enter the pulmonary system thus, it is oxygenated. • Infant is “pink”. • Infants and children can experience TET spells. • Surgical repair is between 18 months and 3 years old. • Blood is shunted from right to left. • Pulmonary blood flow is dependent upon R to L shunting through the PDA. • Infant will require PGE until surgical repair is undertaken.
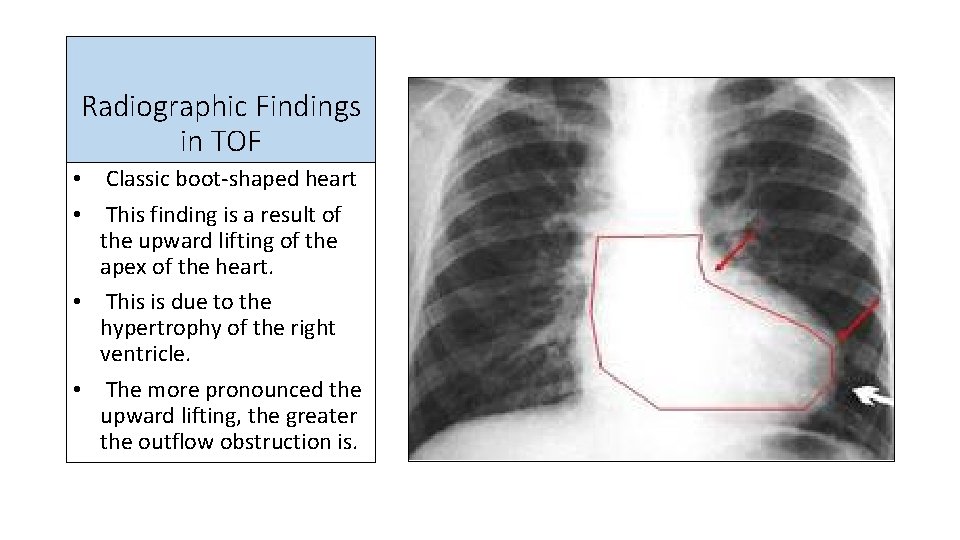
Radiographic Findings in TOF • Classic boot-shaped heart • This finding is a result of the upward lifting of the apex of the heart. • This is due to the hypertrophy of the right ventricle. • The more pronounced the upward lifting, the greater the outflow obstruction is.
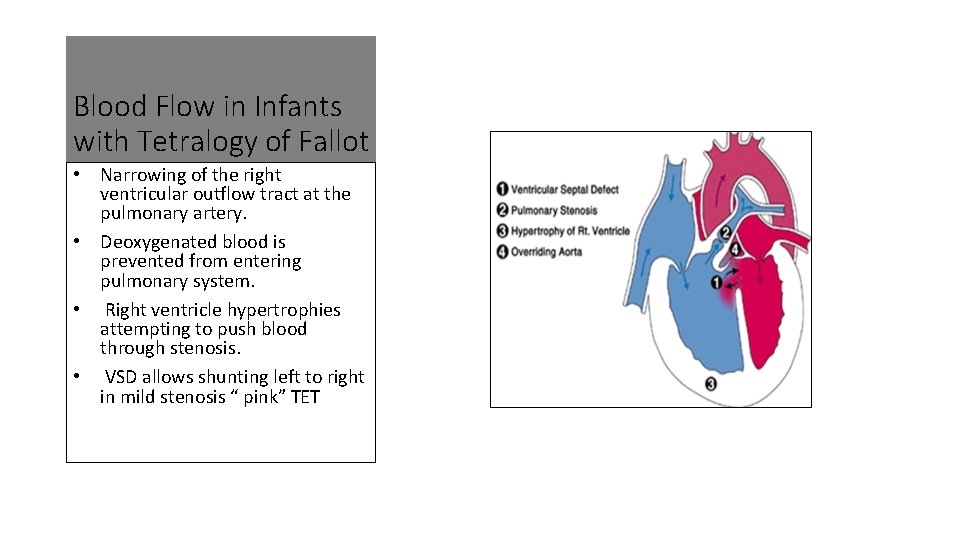
Blood Flow in Infants with Tetralogy of Fallot • Narrowing of the right ventricular outflow tract at the pulmonary artery. • Deoxygenated blood is prevented from entering pulmonary system. • Right ventricle hypertrophies attempting to push blood through stenosis. • VSD allows shunting left to right in mild stenosis “ pink” TET
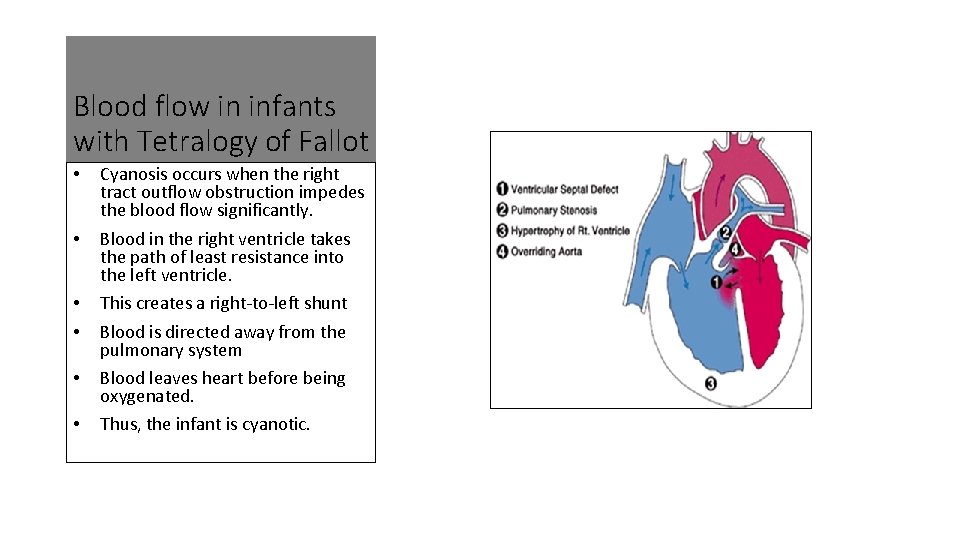
Blood flow in infants with Tetralogy of Fallot • • • Cyanosis occurs when the right tract outflow obstruction impedes the blood flow significantly. Blood in the right ventricle takes the path of least resistance into the left ventricle. This creates a right-to-left shunt Blood is directed away from the pulmonary system Blood leaves heart before being oxygenated. Thus, the infant is cyanotic.
References • Bailliard, F. , & Anderson, R. H. (2009, January 13). Tetralogy of Fallot. Orpanet journal of rare diseases, 4. http: //dx. doi. org/10. 1186/1750 -1172 -4 -2 • Buck, M. L. (2000). Alprostadil (pge 1) for maintaining ductal patency. Pediatric Pharmacotherapy, 6. Retrieved from http: //www. medscape. com/viewarticle/410907_2 • Ferguson, E. C. , Krishnamurthy, R. , & Oldham, S. A. (2007). Classic imaging signs of congenital cardiovascular abnormalities. Radio. Graphics, 27, 1323 -1334. http: //dx. doi. org/10. 1148/rg. 275065148 • Ismail, S. R. , Kabbani, M. S. , Najm, H. K. , Abusuliman, R. M. , & Elbarbary, M. (2010, April ). Early outcome of tetralogy of fallot repair in the current era of management. J Saudi Heart Association, 22(2), 55 -59. http: //dx. doi. org/10. 1016/j. jsha. 2010. 02. 006 • Quek, S. C. , & Lee, C. N. (2010). The modified blalock-taussig shunt revisited. Cardiology in the Young, 208 -209. http: //dx. doi. org/10. 1017/S 1047951109991041
References • Martínez, J. , Gómez, O. , Bennasar, M. , Olivella, A. , Crispi, F. , Puerto, B. , & Gratacós, E. (2010). The 'question mark' sign as a new ultrasound marker of tetralogy of Fallot in the fetus. Ultrasound In Obstetrics & Gynecology, 36(5), 556 -560. doi: 10. 1002/uog. 7614 • Westmoreland, D. (1999). Critical congenital cardiac defects in the newborn. Journal Of Perinatal & Neonatal Nursing, 12(4), 67 -87.
References • Scholz, T. D. , & Reinking, B. E. (2012). Congenital heart disease. In Avery’s diseases of the newborn (9 th ed. , pp. 762 -768). Phildelphia, PA: Elsevier • U. S. National Library of Medicine website. (2011). http: //www. ncbi. nlm. nih. gov/pubmedhealth/PMH 0002534/ • Westmoreland, D. (1999). Critical congenital cardiac defects in the newborn. Journal Of Perinatal & Neonatal Nursing, 12(4), 67 -87.
- Slides: 12