Radiation Protection RAD 101 Unit 4 Protection of
- Slides: 49
Radiation Protection RAD 101 Unit 4 Protection of the Patient and Technologist During Diagnostic Radiography
Objectives • Explain the need for effective communication between the radiographer and the patient. • Explain the significance of adequate immobilization of the patient during a radiographic exposure. • Describe the various beam-limiting devices and identify the device which best confines the radiographic beam. • Explain the function of x-ray beam filtration in diagnostic radiology. • State the reason for using gonadal shielding during radiologic examinations and identify the types of shields used. • Discuss the need for using appropriate exposure factors for all radiologic procedures. • Explain how the use of IR combinations reduces radiographic exposure for the patient. • Discuss the value of good radiographic processing techniques in reducing radiographic exposure for the patient. • State the reason for reducing the number of repeat radiographs. • Explain how patient exposure can be reduced during fluoroscopic procedures
Equipment Design for Radiation Protection Chapter 11
Equipment Design • Control Panel – Must be behind protective barrier w/ window – Must indicate condition of exposure and have light or audible x-ray indicator • Tube housing – Must be lead lined metal (protective tube housing) • Protects from off-focus or leakage radiation • Leakage can not exceed 100 m. R/hr at a distance of 1 meter when operating at the highest voltage • Table – Uniform thickness – Radiolucent- absorbs only minimal amount of radiation- commonly carbon fiber • SID – Must have a means of measurement from anode focal spot to IR – Distance must be accurate to 2% of SID – Centering must be accurate to 1% of SID
Beam Limiting Devices • Devices that limit the x-ray beam before it enters the patient • Benefits – – Amount of tissue irradiated is less Dose received is less Amount of scatter radiation produced in the body is less Image quality is improved • Types – Aperture diaphragm – fixed and variable – Cone/cylinders – Collimator
Aperture Diaphragm • Lead square with a fixed circular opening-fixed • Placed below ( under) the tube • Restricts the beam dimensions to a given size Pg 236
Cones/Cylinders • Fixed aperture device consisting of an extended metal structure – Cone – flared metal tube – Cylinder- straight tube , more restricting- • Longer cylinders are more restricting • Slide into attachment under tube housing • Uses: – Dental, detail , sinuses, spot L-spine
Collimators • “Variable aperture or variable rectangular” • Most versatile • More control over beam limitation • 2 sets of shutters • 1 st set reduces off focus radiation from the primary beam- located below tube window – Off focus- radiation in tube that results from electrons hitting areas other that the focal spot) • 2 nd Set- 2 pairs; each pair can be independently adjusted- located below the light source and mirror • Most machines have PBL- positive beam limitations – but can be reduce further • NCRP requires light field to be accurate to no more than 2% of the SID – 40” x 2%=. 8 “ of light showing around cassette
Filtration • The process of eliminating undesirable low-energy x-ray photons by the insertion of absorbing materials into the primary beam • Effects of filtration – Increase quality of the beam because boo penetrating x-rays are left- Beam gets “hardened”- removes low energy – Decreased quantity of x-rays- by absorbing some low energy beams- fewer overall beams are left – Reduces patient dose- especially to skin and superficial tissue • 2 types – Inherent – Added
Inherent filtration • Result of tube and housing composition • Glass envelope surrounding tube • Oil that surrounds tube ( oil helps in heat dissipation) • Glass window- most of inherent comes from here • Typical x-ray tube may have total inherent filtration of. 5 -1. 0 mm Al equivalent
Added Filtration • Any filtration occurring outside the tube and housing and before the IR • The collimators themselves are considered added filtration – avg 1. 0 mm. Al eq. • Sheets of Al also added after tube window • Al is considered standard filtering material – All filtration is expressed in Al equivalences • Inherent + Added = total filtration • Operating levels require certain amts of filtration per NCRP #102 • When filtration is increased, technical factors must be increased to maintain same density on film • Although exposure needs to be increased to pt, there is still a greater decrease in overall exposure to pt with filtration
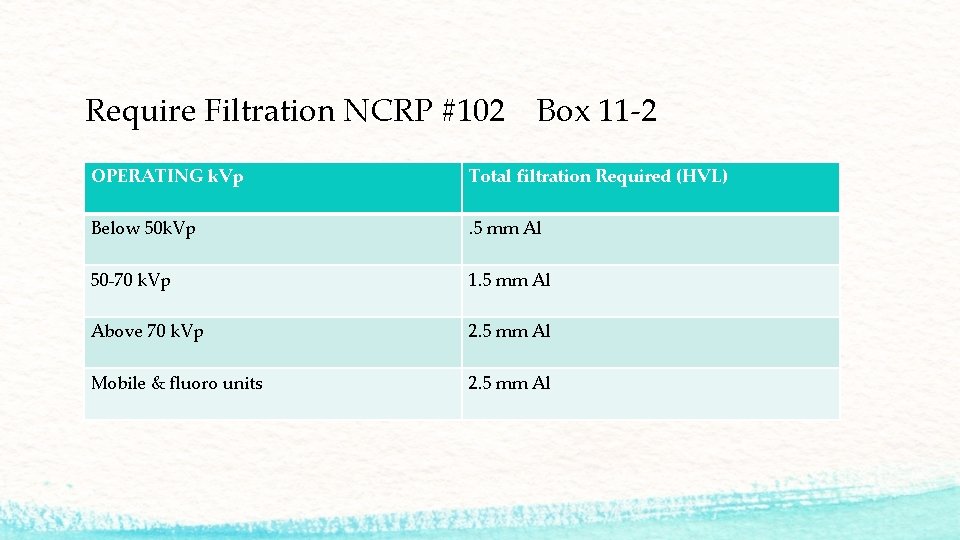
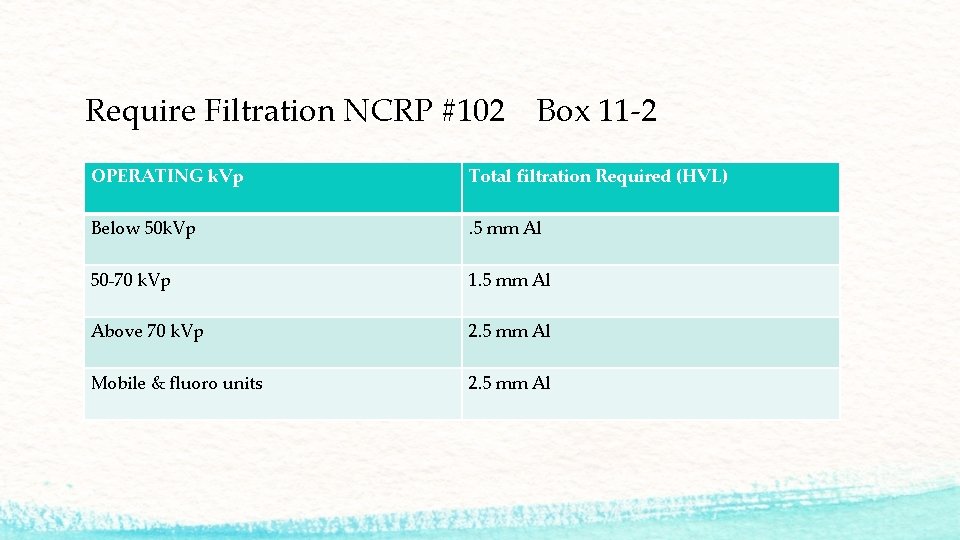
Require Filtration NCRP #102 Box 11 -2 OPERATING k. Vp Total filtration Required (HVL) Below 50 k. Vp . 5 mm Al 50 -70 k. Vp 1. 5 mm Al Above 70 k. Vp 2. 5 mm Al Mobile & fluoro units 2. 5 mm Al
Half Value Layer - HVL • The amount ( thickness) of an absorber ( Al) required to decrease the intensity of the primary beam by ½ (50%) of its original value • Expressed in terms of Al equivalent • Physicist measures beam quality • Shielding devices use HVL • TVL- amount of shielding required to reduce the radiation intensity to one-tenth its original value
http: //o. quizlet. com/RUQPb. YCy 7 J 8 zw. Da. Ucy. N. GA_m. jpg Compensating Filters • Placed outside under collimators • Designed to solve a problem of unequal subject densities • Adds an absorber to compensate for unequal absorption with the subject • Result – overall absorption of primary beam will be more equal and even densites on radiograph ( one end won’t be black and other underexposed) • Made of aluminum, leaded plastic or plastic ( acrylic) • Types – Wedge – bone and joint – T-spine, feet – Trough ( bilateral wedge) CXR-PA http: //o. quizlet. com/zi. B 0 q. Nlw 6 LZl. WDVCa. LGRKA_m. png
Reproducibility/ Linearity • Reproducibility – Consistent output in radiation intensity for identical generator setting from one exposure to the next – Any combo of k. Vp, m. A and time – Variance of 5% or less • Linearity – Consistent output of radiation intensity at any selected k. Vp setting when generator setting are changed from m. A/time combo to another – Cannot exceed 10%
Image Receptors • Film Screen – – intensifying screens – convert x-ray energy to visible light- screens have phosphors ( crystals) that luminesce(give off visible light) when struck by x-rays – Screen-Speed- how fast a screen is capable of converting x-rays to light – Slow screens need more radiation to produce same density- higher pt dose but better detail • CR- computed radiography – Photostimulable phosphor plate- aprox equal to 200 speed screen film – Dose creep- results from practice of overexposing patients to create good images and avoid repeat images • DR- digital radiography – Latent image is formed by x-ray photons on a radiation detector- electronic latent image – Matrix size and pixel size determine image detail – Reduction in repeats reduce overall patient dose
Grids • Devices that remove scattered x-ray photons that emerge from the patient before the scatter reaches the film • Improves contrast and visibility of detail- image quality • Placed between the patient and IR • Pt dose will increase because bore technique is necessary • Used when thickness of part is >10 cm • Made of alternating strips of lead and aluminum or plastic • Come in varying grid ratios- the higher the grid ratio the more grid lines-better absorption of scatter- higher patient dose
Dose Reduction for Mobile X-Ray ( portable) • Mobile radiography requires SSD of at least 30 cm (12 inches) • Recheck your positioning • Check previous radiographs for exposure factors, SID and body habitus – useful for CXR • Use high k. Vp technique ( gives a wider margin for exposure error and reduces dose) • Shield pt • Collimate • Warn personnel and family to reduce their dose- have family leave room
Dose Reduction during Fluoro X-ray exam is performed and demonstrates dynamic, or active, motion of selected anatomy- real time (Regular x-ray is considered static images ) • Use intermittent rather than continuous beam on • Dead-man switch for foot pedal must be equipped- fluoro only when switch is depressed • Collimate • Filtration of 2. 5 mm. AL required • Exposure rate cannot exceed 10 R/min • 5 minute reset timer- audible
Dose Reduction during Fluoro • Bucky slot shielding device of at least. 25 mm. Pb is required • Protective curtain min. 25 mm lead • Stationary Fixed Fluoro SSD no less that 38 cm ( 15 inches) • Mobile fluoro (c-arm) requires SSD of at least 30 cm (12 inches) • Cannot operate in parked position • Primary protective barrier must be 2 mm. Pb equivalent • Lower exposure factors for peds • Fluoroscopically Guided Positioning (FGP) – Practice of using fluoro to determine exact location of the central ray before taking a radiographic exposure – ASRT says “ unethical practice that increases patient dose”
Management of Patient Dose Chapter 12
Effective Communication • “ The holistic approach” the use of verbal messages and body language to communicate with your patient • Advantages: – Reduces patient anxiety – Creates better tech/patient relationship- trust and caring – Increases chance of completing exams and reduce repeats • Consists of : – – – Clear concise instructions Give patient time to ask questions and answer truthfully Listen and offer empathy Respond according to ethical guidelines Don’t overemphasize pain ( may cause more anziety)
Immobilization • Sometimes needed based on patient and exam being performed • Reduces motion • 2 types of motion – Voluntary- patient controlled • Age • Breathing • Fear – Involuntary- body systems • Muscle spasms • Chills • Tremors • Shortened exposure time while maintaining m. As ( high m. A , low seconds) • Good instructions
Protective Shielding • Devices made of lead or lead impregnated materials that will adequately attenuate ionizing radiation • Should reduce or eliminate radiation doses that can cause biological damage • Areas that should be shielded – Eyes – Breasts – Reproductive organs • Types of shields – Gonadal • Flat, shadow, shaped, clear – Specific area shielding • Breast, thyroid
Gonadal Shielding • Used to protect reproductive organs when organs are within 5 cm of the beam • Used unless it will compromise the exam (pelvic, abdominal ) • Females receive 3 x the exposure to reproductive organs than males during exams of the pelvic region • Female dose- can be reduced by up to 50% with contact shield – placed 2. 5 cm medial to ASIS • Male dose- can be reduced by up to 90 -95% with contact shield- placed below symphysis pubis
Types of Gonadal Shielding • Flat contact shields – – Lead strips Placed directly over patient’s reproductive organs Best when used in AP or PA recumbent position Under the patient during fluoro • Shadow shields – – – Made of radiopaque material Suspend from above the tube collimator box Hang over patient and shadow area to be shielded- gonad and breast Can’t use during fluoro Can use during sterile procedures Reduce patient embarrassment
Types of Gonadal Shielding Cont’d • Shaped Contact shields – 1 mm of lead and are contoured to enclose male reproductive organs – Can be used with disposable or washable briefs – Can be used for recumbent or nonrecumbent positions- AP, oblique, and lateral – not for use with PA projections- only covers anterior and lateral – Can be used for fluoro exams – Have patient place when changing for exam • Clear Lead Shields – Transparent lead acrylic impregnated with approx. 30% lead by weight – Can be gonad and breast shielding for scoliosis exams
Specific Area Shielding • Used for radiosensitive organs and tissues – Thyroid – Breast ( or PA positioning can reduce dose) – Eyes • Can be contact, shadow or clear plastic http: //www. eakoh. com/X-rays/thyroid. jpg http: //www. alimed. com/_resources/images/product/_cache/920338_280 x 280. jpg http: //corearmor. com/cav 02/wp-content/uploads/2012/09/attenurad-ct-eye-shield. png
Technical Exposure Factors • Essential to ensure a diagnostic image with minimal patient dose • Images must have: – – Sufficient density (brightness) to display structures Good contrast to differentiate structures Maximum special resolution( detail) and minimal distortion Low quantum noise or mottle – results from insufficient technique
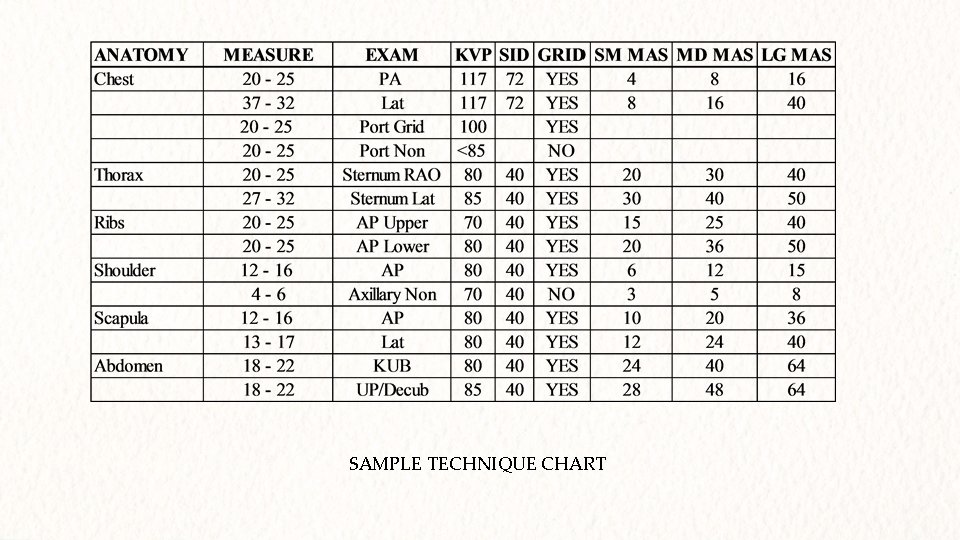
Technique Charts • Used when AEC ( automatic exposure control) is not used • Standardized set of techniques based on equipment and patient size • Departments establish own protocols • Ensures consistency • Minimizes errors if used correctly
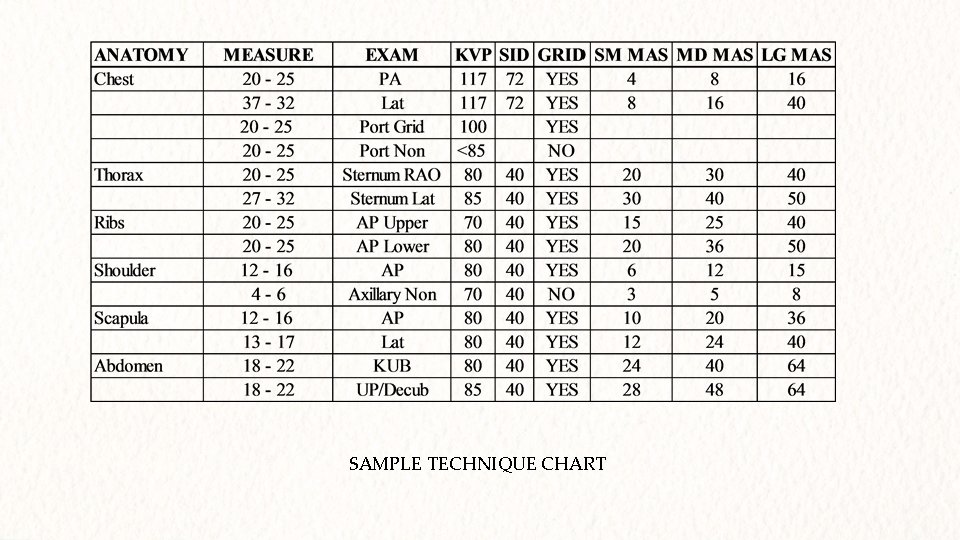
SAMPLE TECHNIQUE CHART
Exposure Factor • Typically high k. Vp and low m. As will reduce dose • Increasing k. Vp by 15% and reducing m. As ( ½) will reduce radiation exposure • Select the highest practical k. Vp within optimal range for the position and part along with sufficient m. As that will produce and optimal radiograph
Radiographic Processing • Of main concern with film-screen imaging • Correct processing promotes archival quality • Inadequate processing will produce poor films leading to repeats and extra exposures • Digital Imaging- also concern on post-processing – Artifacts – Software problems
Quality Control Program/ Repeat Analysis Program • Ensures standardization in processing in film and digital • Regular monitoring and maintenance of processor and image display • Types of QC – Acceptance testing – Calibration – PM schedule • Repeat analysis program – Repeats and reasons for repeats are evaluated – Increases awareness about quality of images – In-service if consistent problems arise
The Pregnant Patient • Screen all women of child bearing age – Some hospitals have specific ages outlined • Ask LMP – NCRP- Elective exams should be completed in the first few days after the onset of menses to minimize possible radiation of an embryo. - “Ten day rule” ICRP for woman of reproductive age. States that "whenever possible, one should confine the radiological examination of the lower abdomen and pelvis to the 10 -day interval following the onset of menstruation. ” - Consideration for replacing with 28 day rule. Pt is considered not pregnant until a menstrual period is skipped then they are until proven otherwise. • Shield is recommended if the ovaries and uterus are less than 5 cm from edge • Some facilities will require HCG
Figuring Fetal Dose • List in as much detail about the x-ray exam – – – – – Projections Number of views Film size Technique SID Shielding used? Patient thickness Fluoro time Number Spot films taken • Report information to RSO or Medical Physicist- they will determine Eq. D
Management of Tech Dose Chapter 13
The Patient as a Beam Emitter • During the exam- the patient becomes a source of radiation for the tech- scattered radiation because of Compton interaction • Greatest occupational hazard • Lowest scatter area is at 900 to the patient • Ways of reducing – – – Beam limiting devices –PBL Filtration- (primarily benefits pt) Protective apparel Technical factors Cardinal principles Structure of dept
Protective Apparel • Lead aprons, gloves and shielded barriers • Protect from secondary ( scatter and leakage) • Standard apron thickness. 5 mm lead equivalent at 100 k. Vp reduces by 75% • . 25 mm is minimum (mammo) 1 mm is maximum ( rare because of weight) • Lead should be hung on racks or draped over a bar- never folded or crunched • Must be inspected yearly for integrity ( use high k. Vp to reduce dose) • Thyroid shields-. 5 mm lead • Glasses. 35 mm lead • Gloves. 25 mm lead
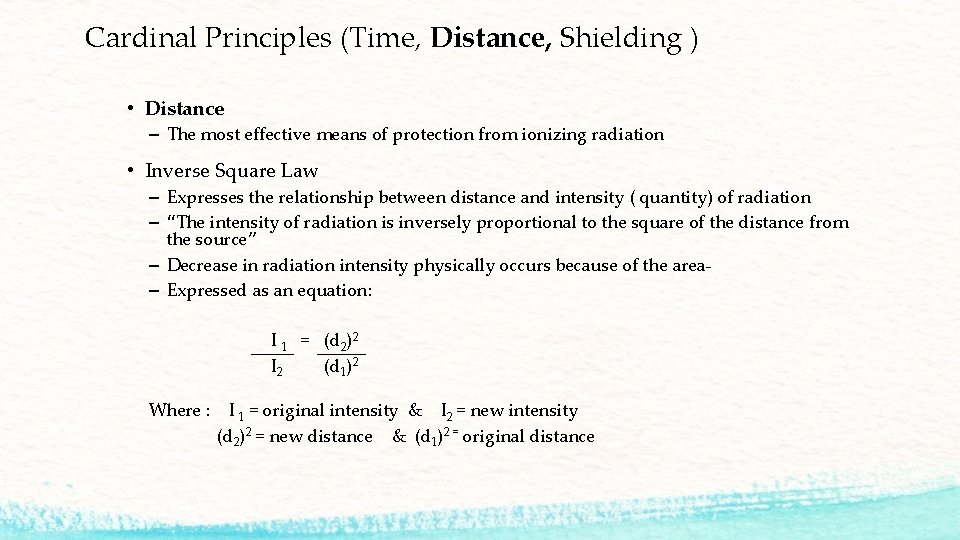
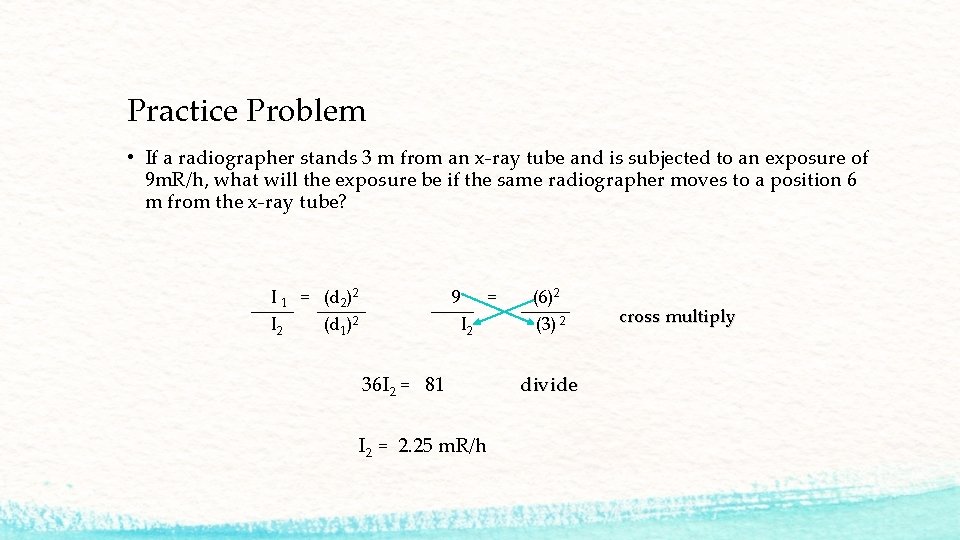
Cardinal Principles (Time, Distance, Shielding ) • Distance – The most effective means of protection from ionizing radiation • Inverse Square Law – Expresses the relationship between distance and intensity ( quantity) of radiation – “The intensity of radiation is inversely proportional to the square of the distance from the source” – Decrease in radiation intensity physically occurs because of the area– Expressed as an equation: I 1 = (d 2)2 I 2 (d 1)2 Where : I 1 = original intensity & I 2 = new intensity (d 2)2 = new distance & (d 1)2 = original distance
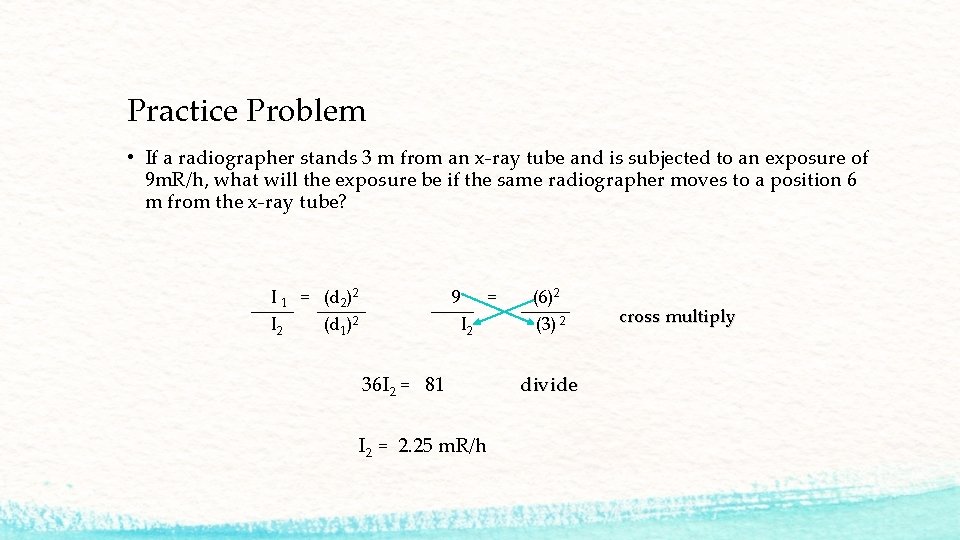
Practice Problem • If a radiographer stands 3 m from an x-ray tube and is subjected to an exposure of 9 m. R/h, what will the exposure be if the same radiographer moves to a position 6 m from the x-ray tube? I 1 = (d 2)2 9 = (6)2 I 2 (d 1)2 I 2 (3) 2 cross multiply 36 I 2 = 81 divide I 2 = 2. 25 m. R/h
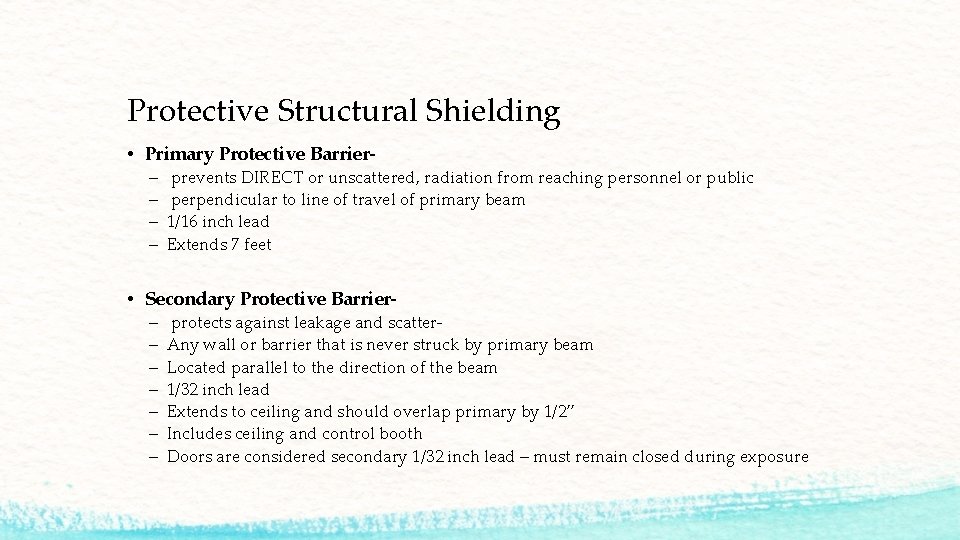
Protective Structural Shielding • Primary Protective Barrier– – prevents DIRECT or unscattered, radiation from reaching personnel or public perpendicular to line of travel of primary beam 1/16 inch lead Extends 7 feet • Secondary Protective Barrier– – – – protects against leakage and scatter. Any wall or barrier that is never struck by primary beam Located parallel to the direction of the beam 1/32 inch lead Extends to ceiling and should overlap primary by 1/2” Includes ceiling and control booth Doors are considered secondary 1/32 inch lead – must remain closed during exposure
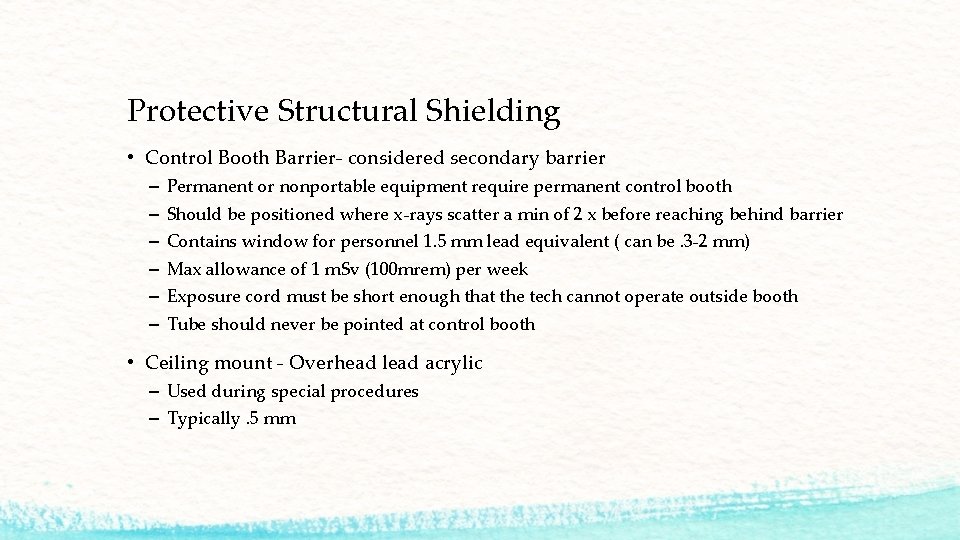
Protective Structural Shielding • Control Booth Barrier- considered secondary barrier – – – Permanent or nonportable equipment require permanent control booth Should be positioned where x-rays scatter a min of 2 x before reaching behind barrier Contains window for personnel 1. 5 mm lead equivalent ( can be. 3 -2 mm) Max allowance of 1 m. Sv (100 mrem) per week Exposure cord must be short enough that the tech cannot operate outside booth Tube should never be pointed at control booth • Ceiling mount - Overhead lead acrylic – Used during special procedures – Typically. 5 mm
Workload • Used to determine barrier shield requirements • Since x-ray units do not have constant on-time a formula is used to determine approx. amount of radiation “output-weighted time” • Expressed in m. As per week or m. A-min per week • Workload (W)= m. A x time x days per week x #pts x #img per pt
Use Factor & Occupancy Factor If no one will ever be present beyond an existing wall- no additional shielding is needed ( courtyard) • Use Factor- the factor that represent the portion of beam-on time that the x-ray beam is directed at a primary barrier during the week ( table 13 -2 pg 328) • Occupancy Factor- use to modify shielding based on the fraction of the work week during which the space beyond the barrier is occupied (table 13 -3 p 329) • Controlled area- used only by x-ray personnel – 1 m. Sv (100 mrem) • Uncontrolled area- general public – hallway, stairwell – Weekly max dose 20 microsieverts ( 2 mrem)
Caution Signs Posted signs warning for radiation “Catution” and radiation symbol : Must be magenta, purple or black on a yellow background Must read: “Radiation Area” “High Radiation Area” “Very High Radiation Area” Departments usually have “If you think you are pregnant please tell the technologist”
Where to stand during exams • Fluoro – Stand as far away from the patient as practical or behind radiologist – Book recommends control booth…. . Usually not practical • Portable – Cord must be 6 foot – 90 degrees to beam • C-arm – As far as achievable – use of foot pedal for exposure helps – Position image intensifier as close to patient as possible ( decreases scatter) – If possible place tube under table and image intensifier over table
Holding Patients • DO NOT stand in primary beam to restrain patient • Use mechanical holding devices first : tape, Pigg-O-Stat • Use nonoccupational persons second– family / parent / ancillary staff/ nursing • Order – – Male relative Female relative Nonradiology personnel Radiology personnel • Always provide lead • Pregnant women are never to hold patients • Rotate human holder Resources: Radiation Protection in Medical Radiography by Mary Alice Statkeiwicz Sherrer, Paula Visconti, E. Russell Ritenour and Kelli Welch Haynes. 6 th and 7 th Edition. Elsevier online. Essentials of Radiographic Physics and Imaging. James N. Johnston and Terri L Fauber. 1 st Edition. Elsevier Online.
This workforce solution was funded by a grant awarded by the U. S. Department of Labor's Employment and Training Administration. The solution was created by the grantee and does not necessarily reflect the official position of the U. S. Department of Labor. The Department of Labor makes no guarantees, warranties, or assurances of any kind, express or implied, with respect to such information, including any information on linked sites and including, but not limited to, accuracy of the information or its completeness, timeliness, usefulness, adequacy, continued availability, or ownership.