Chest Pain MIShock Victor Politi M D FACP

































- Slides: 74

Chest Pain/ MI/Shock Victor Politi, M. D. , FACP Medical Director SVCMC PA program
n Approximately 1 million hospitalized patients each year have MI as a principal diagnosis n Approximately 200, 000 - 300, 000 people in US die from MI’s each year

MI Risk Factors n n n n n Smoking HTN High fat diet High LDL Diabetes Stress Inactivity Male gender Age/Heredity – Elevated homocysteine and C-reactive protein levels
A patient presents with chest pain n What do you do?


Stable angina, unstable angina, ACI, AMI n An indistinguishable spectrum – beginning with stable lumen-restricting coronary artery plaques – results in plaque fissuring – initiates platelet adhesion & fibrin plugs w/overlying but non-occlusive thrombus – results in plaque disruption, occlusive thrombus composed of fibrin, platelets & erythrocytes
n Most heart attacks are caused by the build up of atherosclerotic plaque inside the arterial wall - which can trigger the formation of a thrombus
Frequency of “Silent” AMIs n n n Framingham Study: largest long term prospective study of cardiovascular disease Cohort of 5, 127 participants 708 (13%) suffered AMI 213 (30%) were not recognized during AMI Only 1/2 demonstrated classic AMI S/Sxs allowing identification of AMI in retrospect
Classic Presentation Retrosternal, epigastric chest pain or tightness n SOB n Diaphoresis n Nausea, vomiting n Levine’s sign n
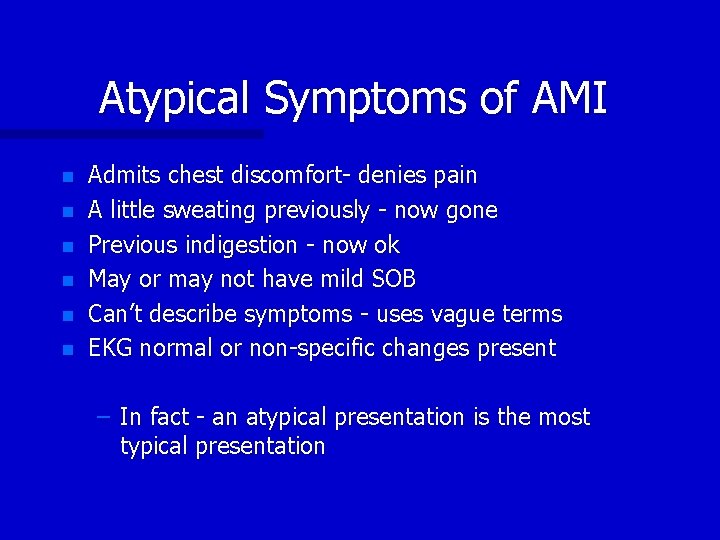
Atypical Symptoms of AMI n n n Admits chest discomfort- denies pain A little sweating previously - now gone Previous indigestion - now ok May or may not have mild SOB Can’t describe symptoms - uses vague terms EKG normal or non-specific changes present – In fact - an atypical presentation is the most typical presentation
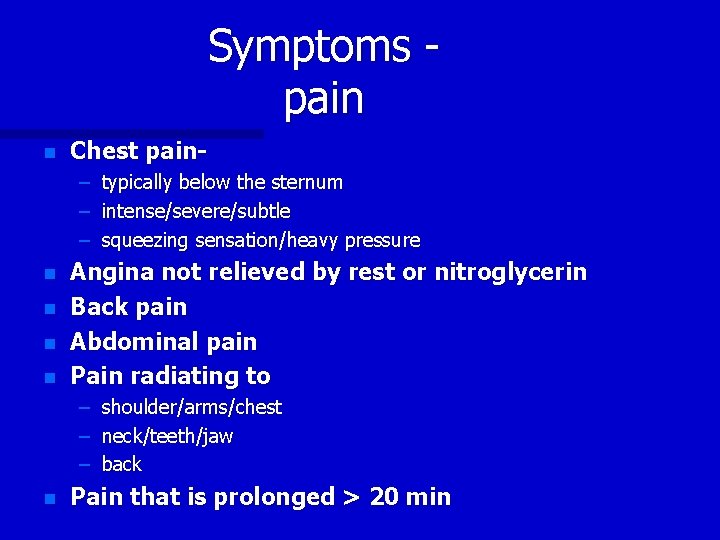
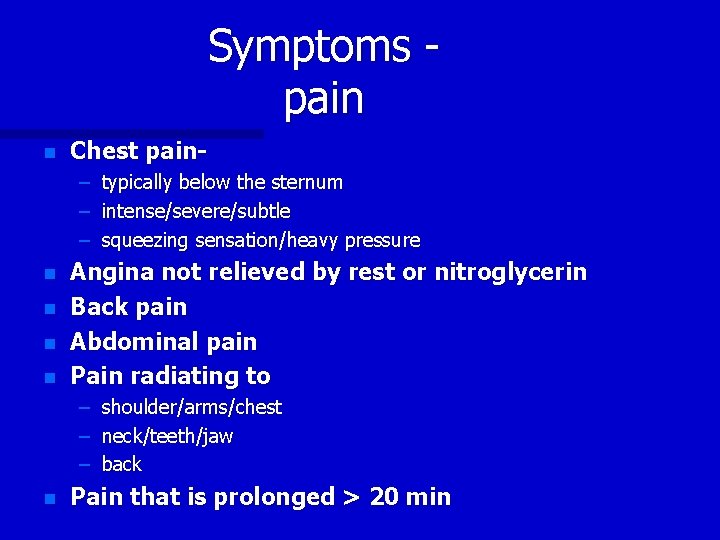
Symptoms pain n Chest pain– typically below the sternum – intense/severe/subtle – squeezing sensation/heavy pressure n n Angina not relieved by rest or nitroglycerin Back pain Abdominal pain Pain radiating to – – – n shoulder/arms/chest neck/teeth/jaw back Pain that is prolonged > 20 min
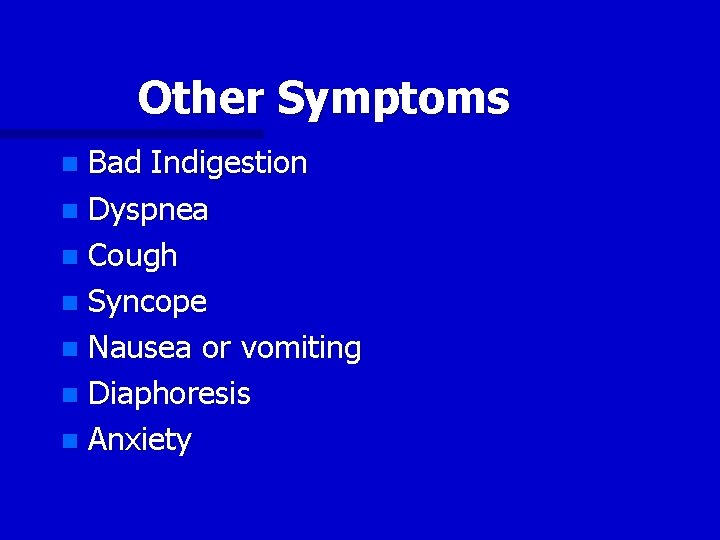
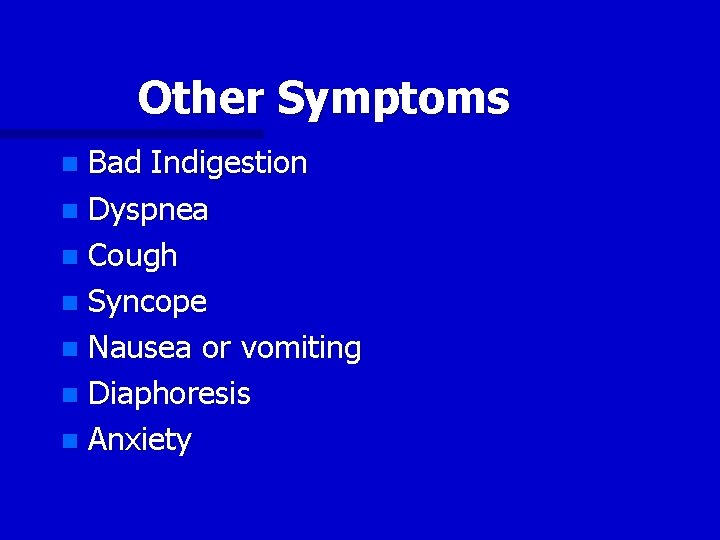
Other Symptoms Bad Indigestion n Dyspnea n Cough n Syncope n Nausea or vomiting n Diaphoresis n Anxiety n
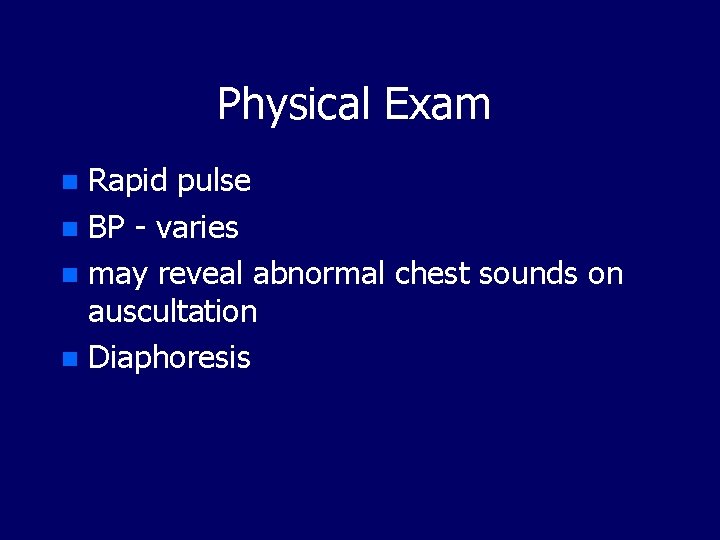
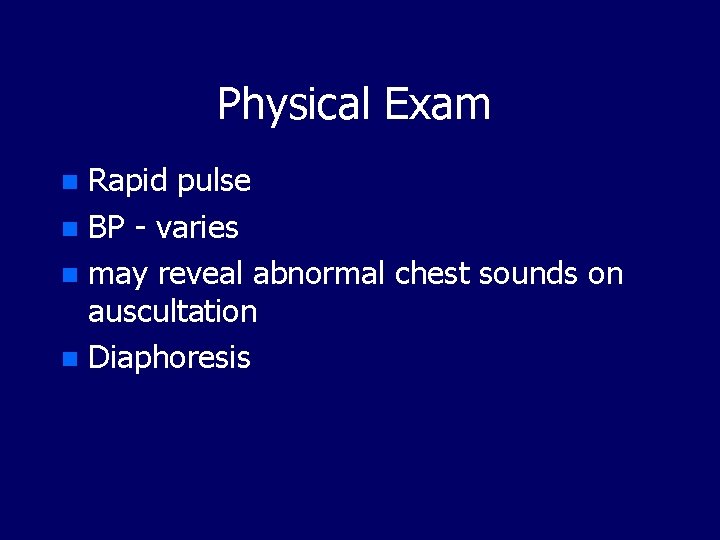
Physical Exam Rapid pulse n BP - varies n may reveal abnormal chest sounds on auscultation n Diaphoresis n
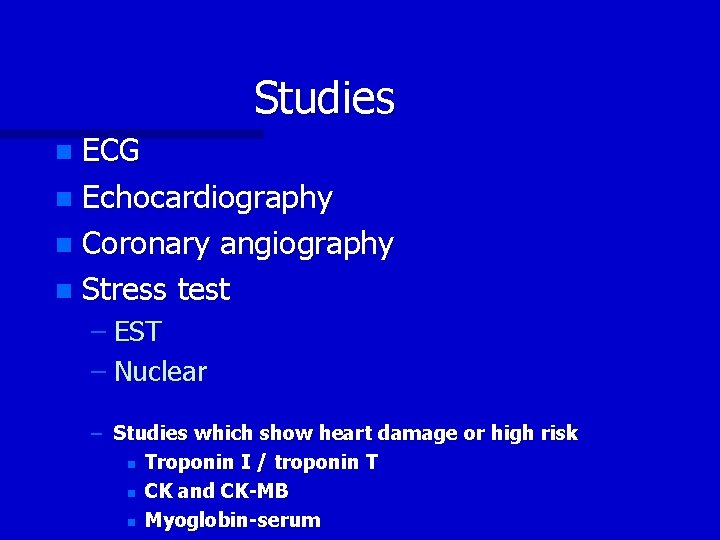
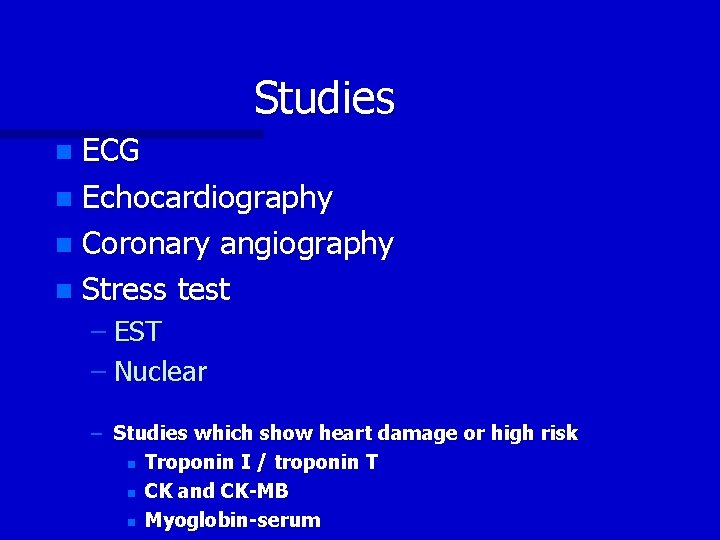
Studies ECG n Echocardiography n Coronary angiography n Stress test n – EST – Nuclear – Studies which show heart damage or high risk n Troponin I / troponin T n CK and CK-MB n Myoglobin-serum
Additional Lab Tests CBC n 6 n Pt/Ptt n Chest x-ray n
What is first in your work-up? 12 lead ECG n Is it useful ? n
A “normal” ECG Studies show that as many as 15% of ECGs are completely normal and 60% of ECGs are normal or show nonspecific changes even in the presence of an evolving AMI n When are ECGs useful ? n
Treatment Continuous ECG n Continuous BP n IV - fluids/meds n oxygen n Pulse ox n Blood work n urinary catheter - to monitor fluid status n
ASA
Aspirin 40% relative reduction in mortality n What’s the right dose? n Probably the single most important thing we can do n Irreversible - inhibit platelet aggregation n
Aspirin -Contraindications ASA Allergy n GI bleed n Bleeding disorder n

Nitrates When should nitrates be given? n Who should receive nitrates? n Who should not receive nitrates? n Dose n – SL NTG – Spray – Paste – IV
Morphine MSO 4 Does morphine reduce pain? Yes n Does morphine reduce mortality/morbidity? NO n n Morphine vs NTG
Glycoprotein IIB/IIA Inhibitors Utilized in ACISs without AMI n Action is to “de-couple” platelets n Three FDA-approved n – Integrillin - eptifibatide – Aggrestat - tirobifan hydrochloride – Repro-abciximab
Heparin n When should heparin be given? Who should receive heparin? What is the right way to give heparin? – n n n Is there a wrong way to give heparin? Other forms of heparin, anticoagulants? Therapeutic monitoring Oral anticoagulation – Warfarin – Coumadin
Low-molecular weight heparin Enoxaparin dosed 1 mg/kg SQ Q 12 hr n No PTT monitoring necessary n – potential of fewer labs drawn, run n No IV necessary – fewer IV starts, no pumps, outpatient treatment n Fragmin
The ESSENCE Trial n n Efficacy & safety of SQ Enoxaparin in non-Qwave coronary events Significant relative risk reductions (RRR) & cost savings compared to unfractionated heparin >15% relative risk reduction in incidence of death, AMI, recurrent angina & combined triple endpoints n 10% relative risk reduction in CABG n 21% relative risk reduction in PTCA n n Decreased resource utilization resulting in cost savings exceeding $1000 per patient
Beta-blocker IVP When should beta blockers be given? n Who should receive beta blockers? n Who should not receive beta blockers? n What is the right dosing regimen? n Primary, secondary benefits? n B 1 -B 2 Blocker n
Ace Inhibitors Studies show decreased mortality if given in first few days after AMI n Benefit due to effects on myocardium remodeling n long term benefits show increased EF and decreased incidence of CHF n
Cholesterol Lowering Agents n Current thinking; the lower the total and LDL cholesterol - the better ! n Many types available -currently the statins seem to show the best reduction
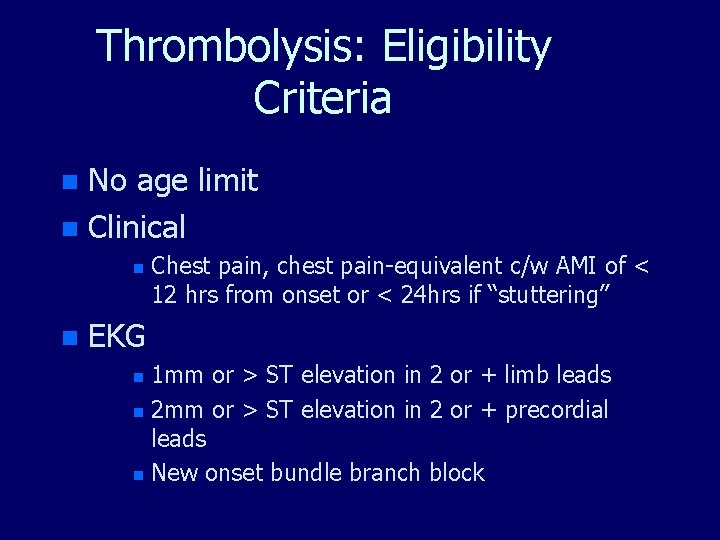
Thrombolysis: Eligibility Criteria No age limit n Clinical n n n Chest pain, chest pain-equivalent c/w AMI of < 12 hrs from onset or < 24 hrs if “stuttering” EKG 1 mm or > ST elevation in 2 or + limb leads n 2 mm or > ST elevation in 2 or + precordial leads n New onset bundle branch block n
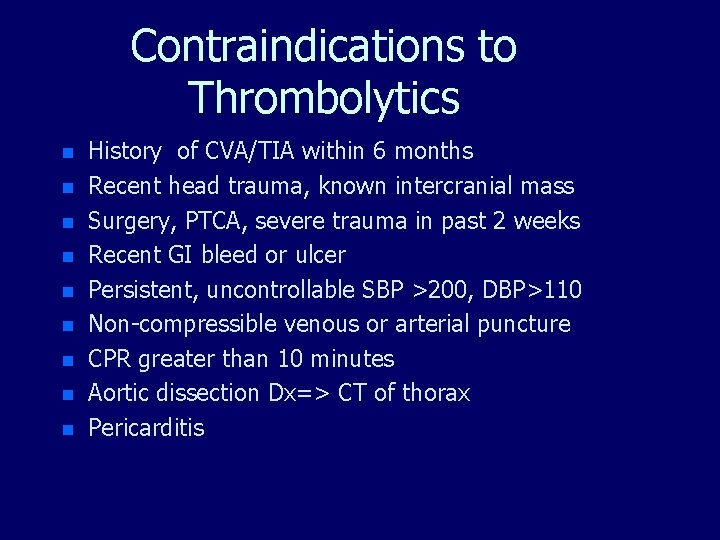
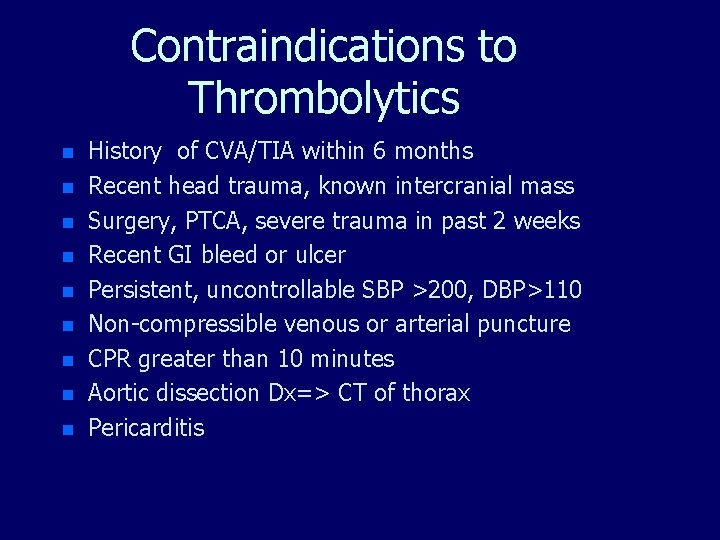
Contraindications to Thrombolytics n n n n n History of CVA/TIA within 6 months Recent head trauma, known intercranial mass Surgery, PTCA, severe trauma in past 2 weeks Recent GI bleed or ulcer Persistent, uncontrollable SBP >200, DBP>110 Non-compressible venous or arterial puncture CPR greater than 10 minutes Aortic dissection Dx=> CT of thorax Pericarditis
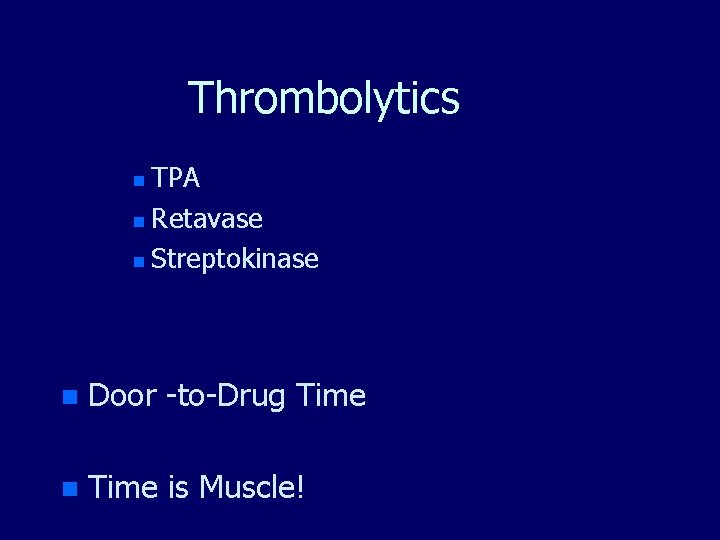
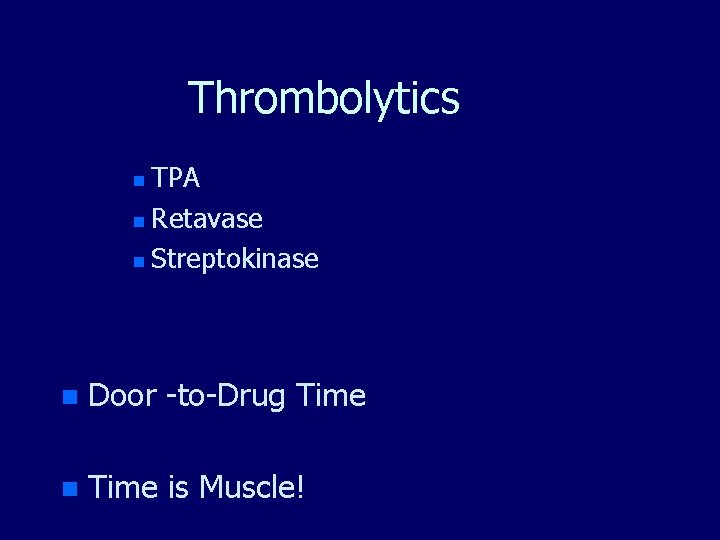
Thrombolytics TPA n Retavase n Streptokinase n n Door -to-Drug Time n Time is Muscle!
Goal of Treatment Stabilize patient n Stop the progression of heart attack n – prevent further heart damage n Reduce demands on heart – so it can heal n Prevent complications
Other cardiac conditions
Bradycardia Systolic rate < 60 n Symptomatic n Atropine n Isopril n Pacemaker n What medications has the patient taken? n

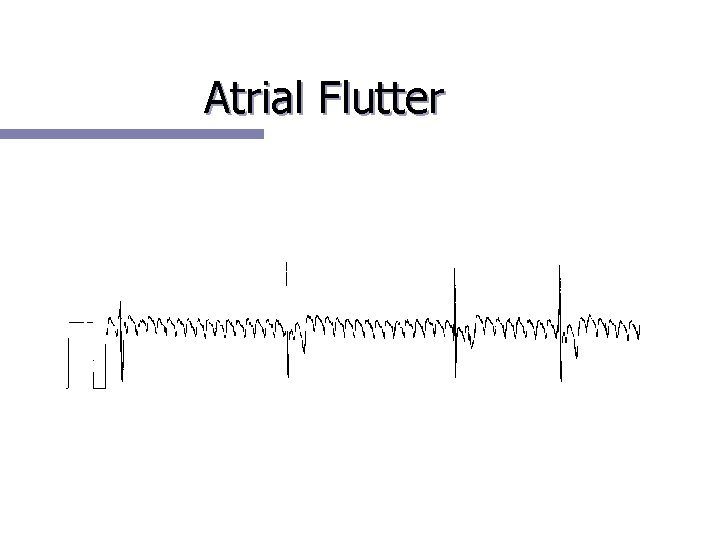
Atrial Arrythmia A Fib n A flutter n SVT n PAC n

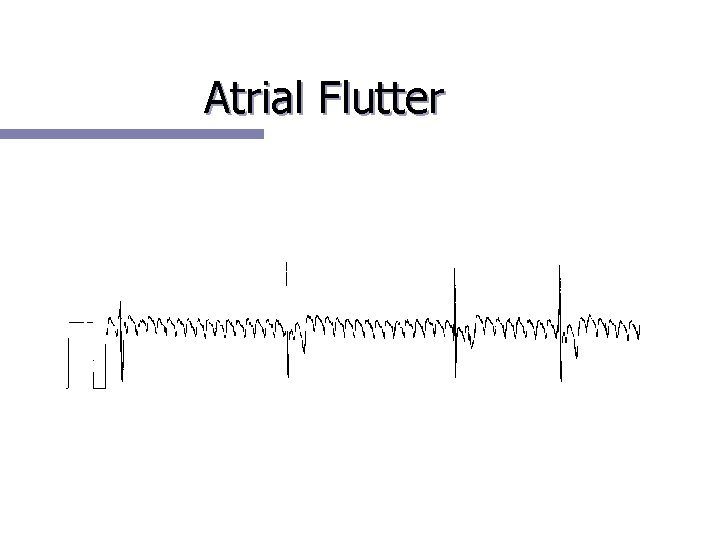
Atrial Flutter
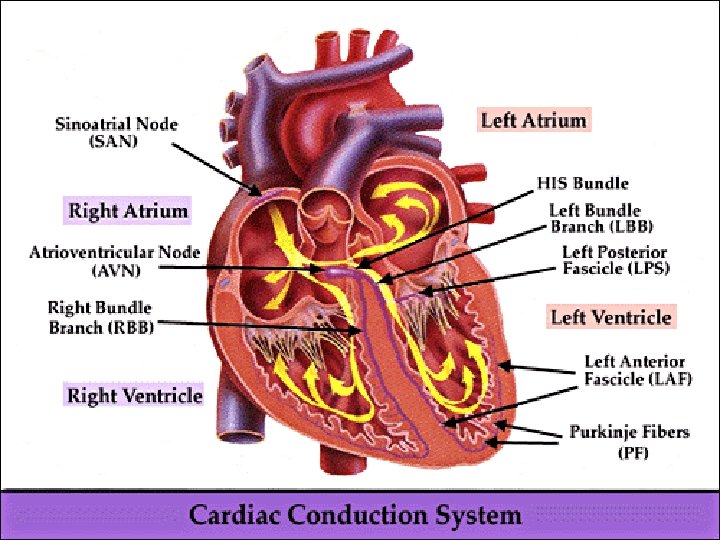
AV Blocks 1 st degree AVB n 2 nd degree AVB n – Type 1 – Type 2 n 3 rd degree AVB

Ventricular Arrythmias PVC n V Tach n V Fib n Torsades n Ventricular escape beat n
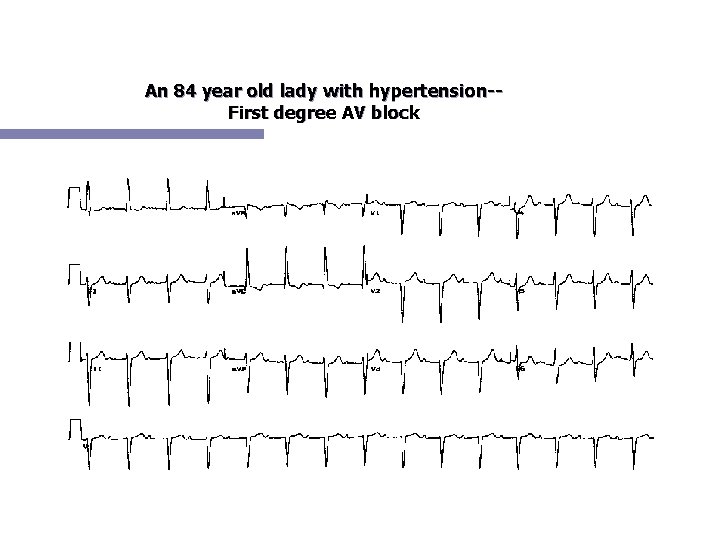
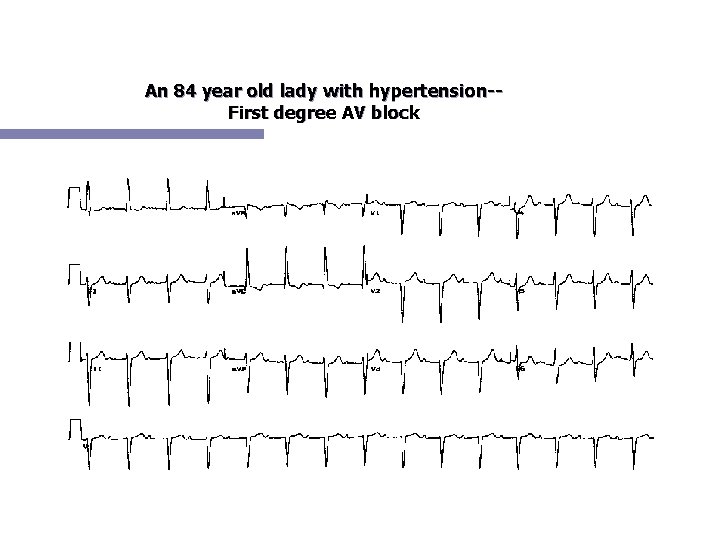
An 84 year old lady with hypertension-First degree AV block
Cardiogenic Shock Symptomatic blood pressure <90 systolic n due to low cardiac output n Goal of treatment - increase perfusion to vital organs n Treatment options include Dopamine/Dobutamine/Levophed/ balloon pump (aortic counterpulsation) n
Cardiac Tamponade n Hypotension caused by reduction of cardiac output secondary to inability of the ventricle to provide adequate stroke volume due to fluid in the pericardial sac

























Questions ? ? ?
 Victor politi
Victor politi Victor politi
Victor politi Victor politi
Victor politi Iga nephropathy vs psgn
Iga nephropathy vs psgn Rachel politi
Rachel politi Causes chest pain
Causes chest pain Typical chest pain
Typical chest pain 50 shades of chest pain
50 shades of chest pain Chest pain in pediatrics
Chest pain in pediatrics Retrosternal chest pain
Retrosternal chest pain örebro musculoskeletal pain screening questionnaire
örebro musculoskeletal pain screening questionnaire Stabbing pain in chest
Stabbing pain in chest Chest pain triage
Chest pain triage Care plan on angina pectoris
Care plan on angina pectoris Visceral referral patterns
Visceral referral patterns Typical chest pain
Typical chest pain Petmac chest pain
Petmac chest pain Martian pain
Martian pain Tender breast sign of pregnancy
Tender breast sign of pregnancy Period cramps vs early pregnancy cramps
Period cramps vs early pregnancy cramps Wormhost chest worm locations
Wormhost chest worm locations Lordotic chest x ray
Lordotic chest x ray Egophony
Egophony Posterior thorax
Posterior thorax The scarlet letter chapter 23
The scarlet letter chapter 23 Stem stature index
Stem stature index Thymus baby chest x ray
Thymus baby chest x ray Vertical
Vertical Sitting duck heart truncus arteriosus
Sitting duck heart truncus arteriosus Latent tb chest x ray
Latent tb chest x ray Chest indrawing
Chest indrawing Bronchopneumonia
Bronchopneumonia Chest assessment
Chest assessment Trigonum lumbale petit
Trigonum lumbale petit Mitral stenosis chest x ray
Mitral stenosis chest x ray Water seal drainage
Water seal drainage Tactile fremitus increased
Tactile fremitus increased Umbliculus
Umbliculus Chest x ray tutorial
Chest x ray tutorial Bilateral chest tubes
Bilateral chest tubes Barrel chest
Barrel chest Chest lateral decubitus position
Chest lateral decubitus position Rash on upper chest and back
Rash on upper chest and back Boney spine
Boney spine Nursing position for patients
Nursing position for patients Painted chest from the tomb of tutankhamun
Painted chest from the tomb of tutankhamun Urticaria classification
Urticaria classification Dextocardia
Dextocardia Head body head body gif
Head body head body gif Clin chest med
Clin chest med Where's your chest located
Where's your chest located Chest tube parts
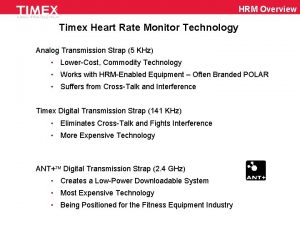
Chest tube parts Timex digital heart rate monitor
Timex digital heart rate monitor Normal diaphragmatic excursion
Normal diaphragmatic excursion Chest x ray lateral view positioning
Chest x ray lateral view positioning Egg on a string heart
Egg on a string heart Knee chest position
Knee chest position Pigeon chest
Pigeon chest Heart sounds on chest
Heart sounds on chest Barrel chested meaning
Barrel chested meaning Basic life support
Basic life support Ap and transverse diameter
Ap and transverse diameter Chest area name
Chest area name Mid clavicular line
Mid clavicular line Atheromatous thoracic aorta
Atheromatous thoracic aorta Deep chest muscles
Deep chest muscles Azgos vein
Azgos vein How to measure ap diameter of chest
How to measure ap diameter of chest Chest and back muscles
Chest and back muscles Ellis curve
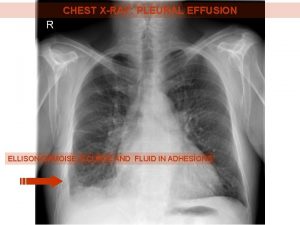
Ellis curve Pleural biopsy
Pleural biopsy Opposite of lateral
Opposite of lateral Open chest wound first aid
Open chest wound first aid Ilo classification of chest radiograph
Ilo classification of chest radiograph Chest compressions
Chest compressions