Nursing Transition NUR 2013 Selected Respiratory Disorders COPD

- Slides: 120
Nursing Transition NUR 2013 Selected Respiratory Disorders: COPD, Asthma, Pneumonia, and Pulmonary Tuberculosis
Unit II Objectives By the end of this lecture the student should be able to Demonstrate knowledge of pathophysiology of clients experiencing COPD, Asthma, TB, GERD, and PUD Nursing interventions, treatment modalities including pharmacological therapy of clients experiencing COPD, Asthma, TB, GERD, and PUD Nutritional needs of clients experiencing COPD, Asthma, TB, GERD, and PUD
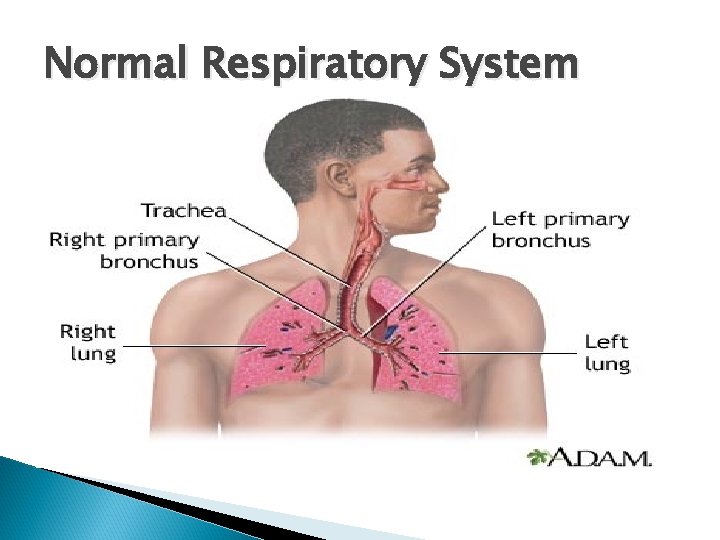
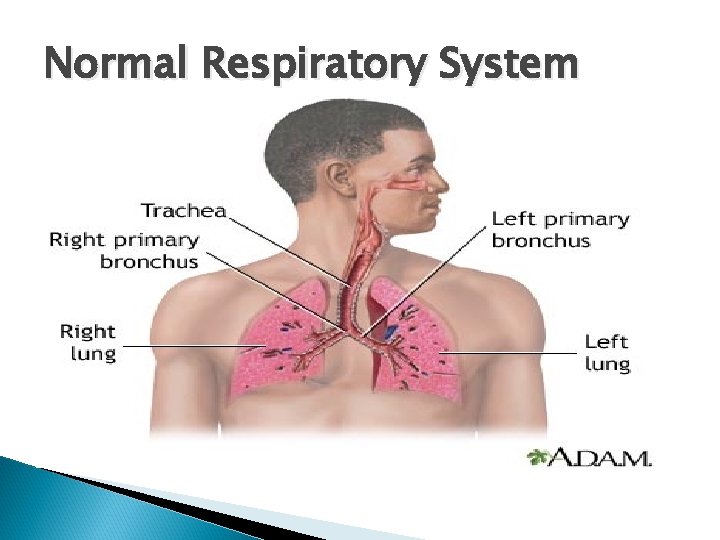
Normal Respiratory System
A&P of Lungs Upper airway includes nasopharynx, oraophyarnx, laryngopharynx. The function is to warm, filter, and humidfy inspired air Lower airway includes trachea, bronchioles, and alveoli. The function is prevention of aspiration, location of vocal cords, passage way for air, gas exchange Lungs are prefused by bronchial arteries small amt. of blood to lungs. Pulmonary arteries bring the entire cardiac output to the right ventricle to the aveoli for gas exchange
Key Terms Ventilation is the process of moving air into the lungs and distribution of air within the lungs to gas exchange units Airway reisitance is determined by the diameter of the airway. Lung compliance the lungs expandibility & ease of lung inflations The mechanicas of breathing include airway resistance, lung compliance, opposing lungs forces(elastic recoil vs chest wall expansion. )
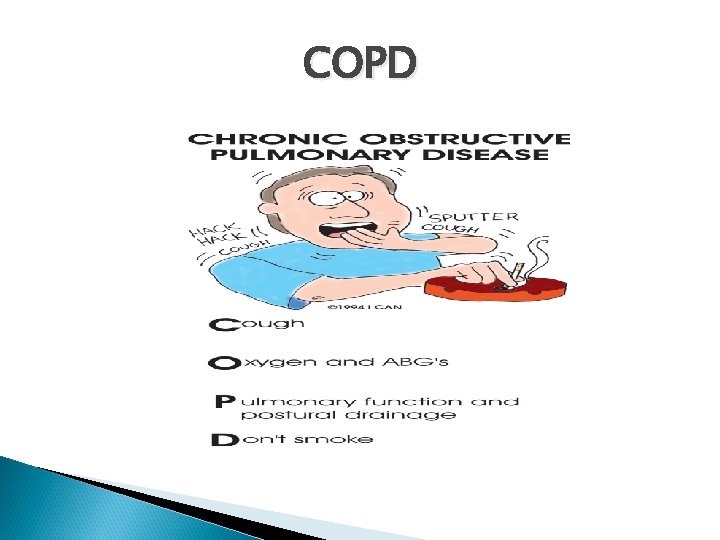
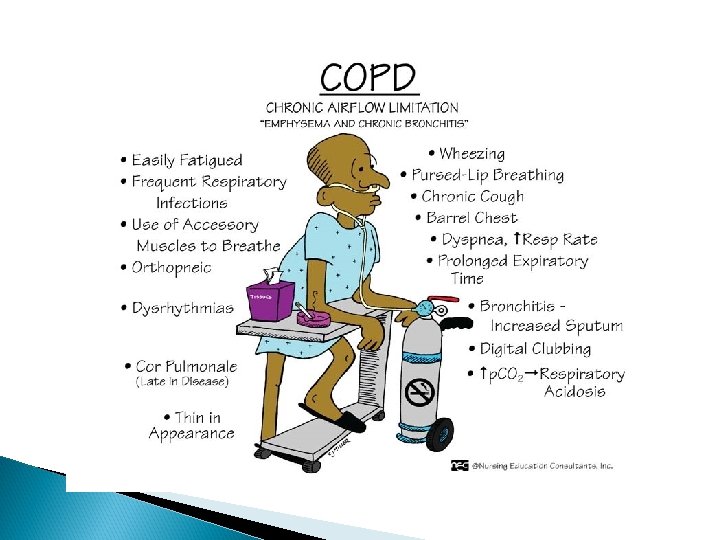
COPD Chronic Obstructive Pulmonary Disease A disease state characterized by airflow limitation that is not full reversible (GOLD). COPD is the currently is 4 th leading cause of death and the 12 th leading cause of disability. COPD includes diseases that cause airflow obstruction (emphysema, chronic bronchitis) or a combination of these disorders. Asthma is now considered a separate disorder but can coexist with COPD.
Chronic Obstructive Pulmonary Disease (COPD) Chronic Bronchitis > chronic productive cough X 3 mo in 2 consecutive yrs Emphysema > abnormal enlargement & destruction of alveoli walls
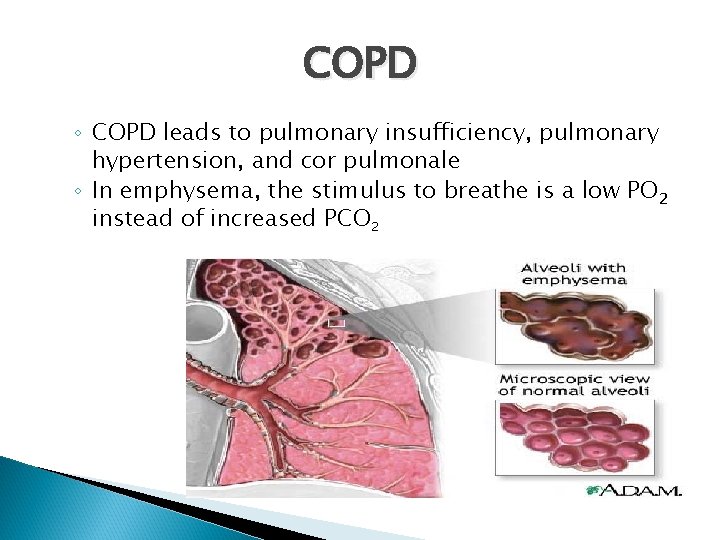
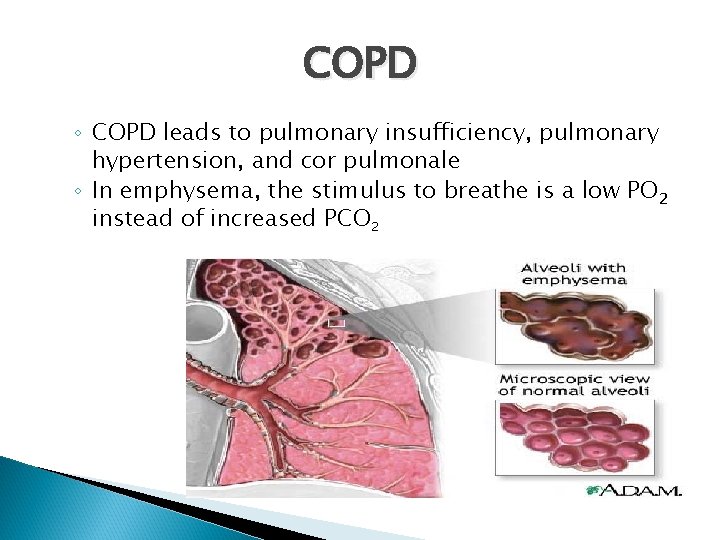
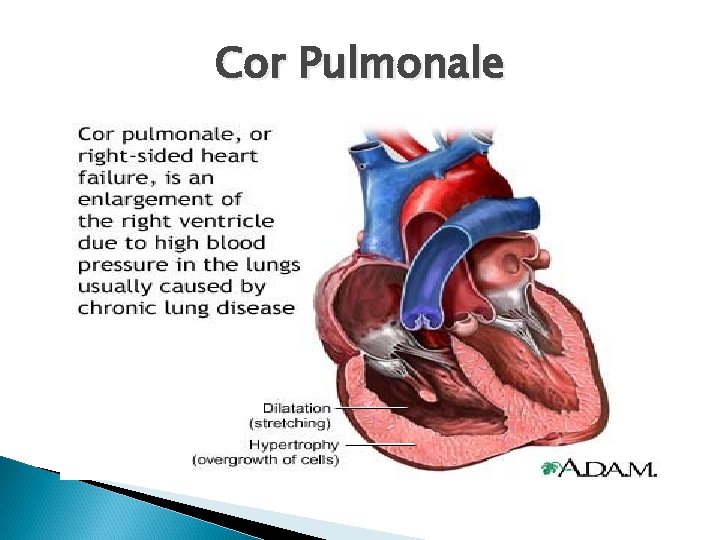
COPD ◦ COPD leads to pulmonary insufficiency, pulmonary hypertension, and cor pulmonale ◦ In emphysema, the stimulus to breathe is a low PO 2 instead of increased PCO 2
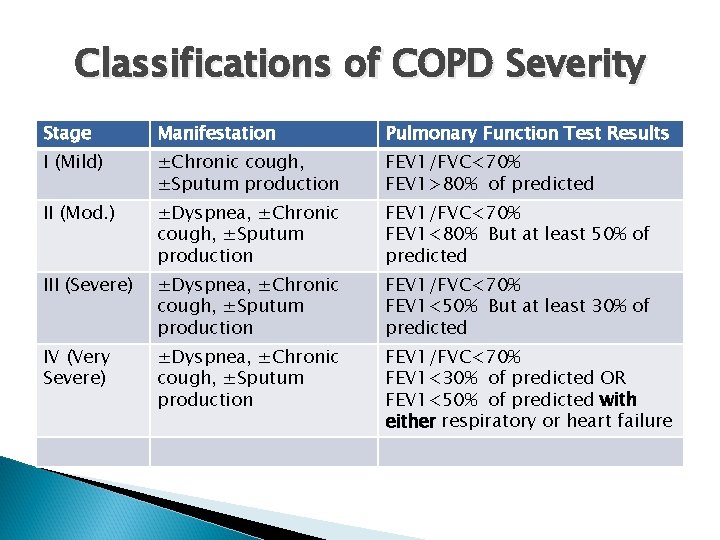
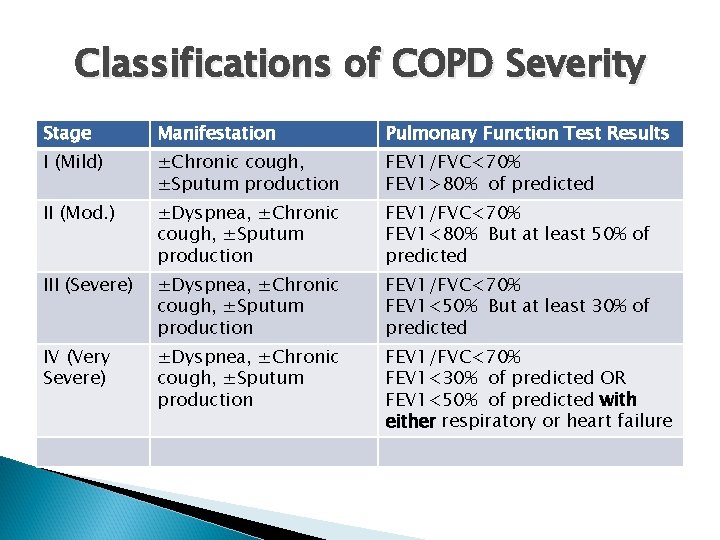
Classifications of COPD Severity Stage Manifestation Pulmonary Function Test Results I (Mild) ±Chronic cough, ±Sputum production FEV 1/FVC<70% FEV 1>80% of predicted II (Mod. ) ±Dyspnea, ±Chronic cough, ±Sputum production FEV 1/FVC<70% FEV 1<80% But at least 50% of predicted III (Severe) ±Dyspnea, ±Chronic cough, ±Sputum production FEV 1/FVC<70% FEV 1<50% But at least 30% of predicted IV (Very Severe) ±Dyspnea, ±Chronic cough, ±Sputum production FEV 1/FVC<70% FEV 1<30% of predicted OR FEV 1<50% of predicted with either respiratory or heart failure
COPD A fifth category--Stage 0: At Risk--that appeared in the 2001 report is no longer included as a stage of COPD, as there is incomplete evidence that the individuals who meet the definition of “At Risk” (chronic cough and sputum production, normal spirometry) necessarily progress on to Stage I: Mild COPD.
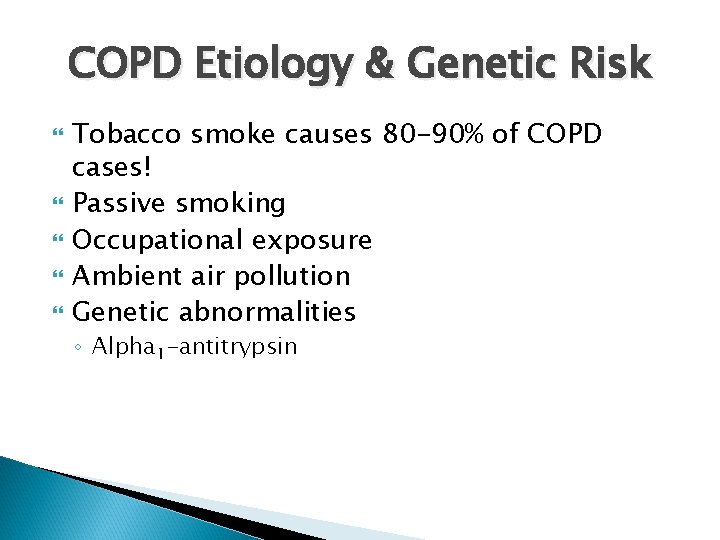
COPD Etiology & Genetic Risk Tobacco smoke causes 80 -90% of COPD cases! Passive smoking Occupational exposure Ambient air pollution Genetic abnormalities ◦ Alpha 1 -antitrypsin
Cultural Considerations Higher among African-Americans. Blue collar workers, and less educated people in the US Highest among Northern Plains American Indians/Native Americans and Alaskan Natives Decrease overall for men and women, but decrease less for women than men
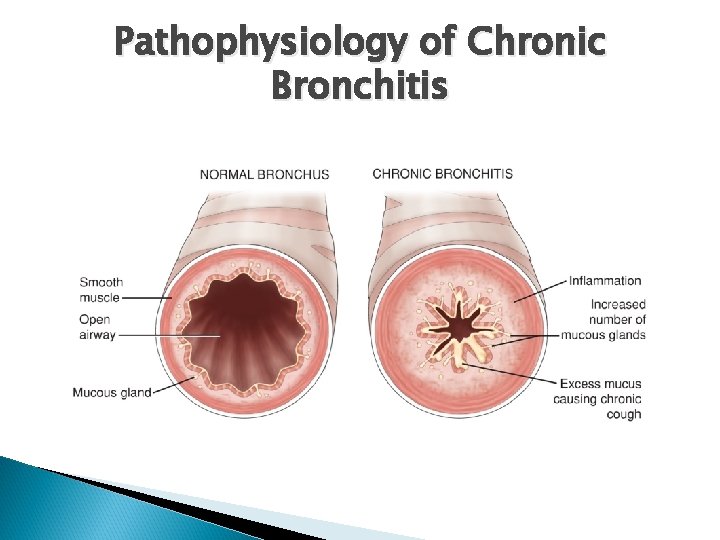
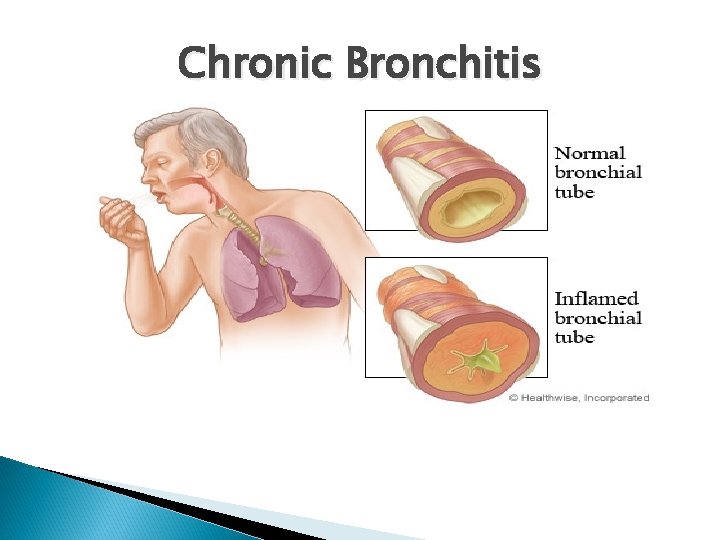
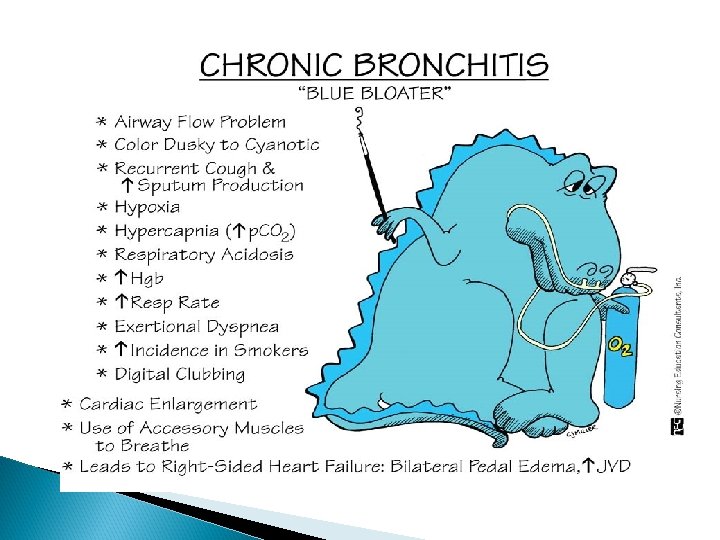
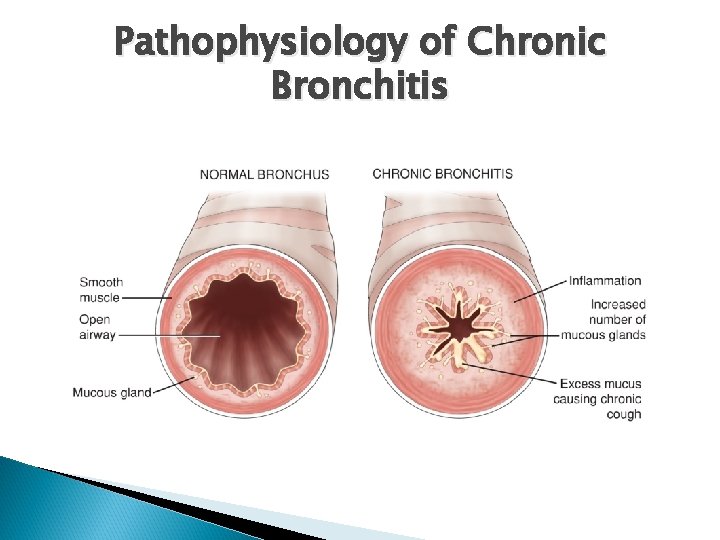
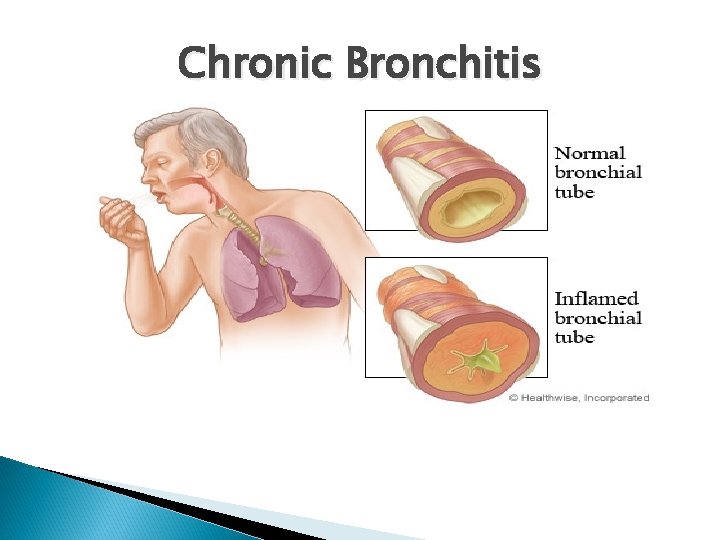
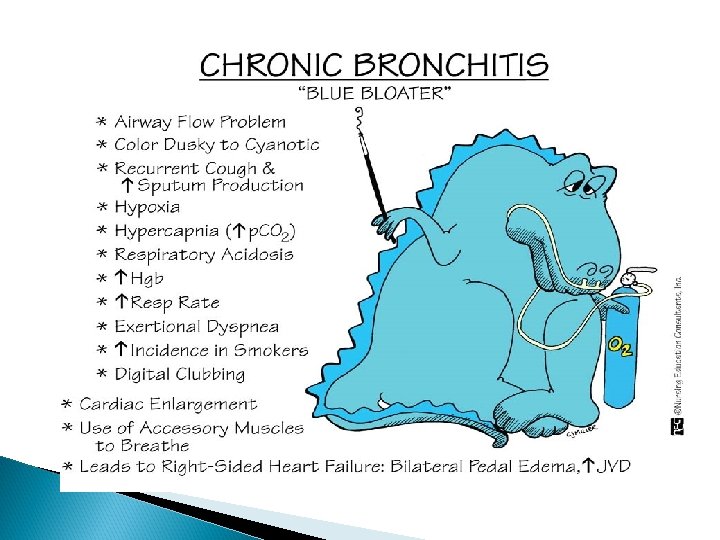
Chronic Bronchitis The presence of a cough and sputum production for at least 3 months in each of 2 consecutive years. Irritation of airways results in inflammation and hypersecretion of mucous. Mucous-secreting glands and goblet cells increase in number.
Chronic Bronchitis Ciliary function is reduced, bronchial walls thicken, bronchial airways narrow, and mucous may plug airways. Alveoli become damaged, fibrosed, and alveolar macrophage function diminishes. The patient is more susceptible to respiratory infections
Chronic Bronchitis Chronic bronchitis causes ↑in the number and size of mucous glands→ produce large amount of thick mucus ↑ bronchial wall thickness (2 X the normal thickness)→ impair airflow Block small airway and narrows large ones Small airways are affected before large ones get involved
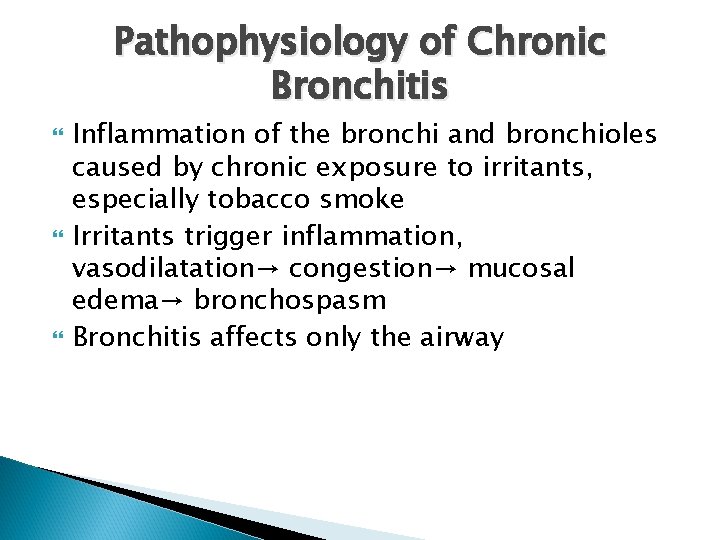
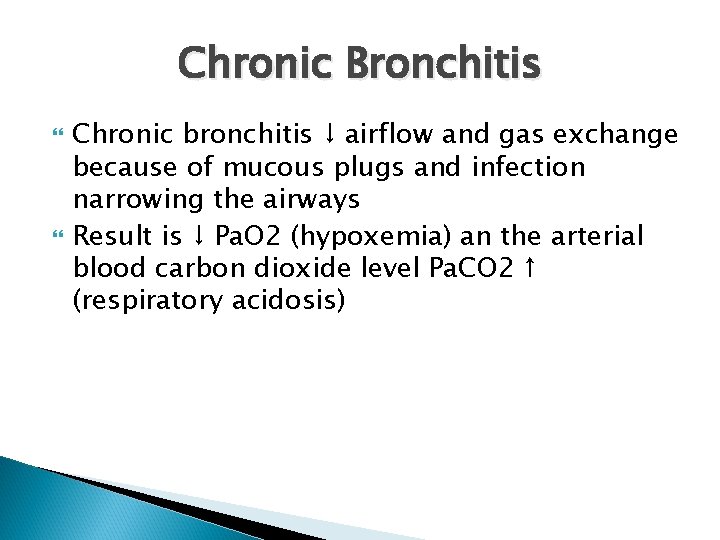
Pathophysiology of Chronic Bronchitis Inflammation of the bronchi and bronchioles caused by chronic exposure to irritants, especially tobacco smoke Irritants trigger inflammation, vasodilatation→ congestion→ mucosal edema→ bronchospasm Bronchitis affects only the airway
Chronic Bronchitis Chronic bronchitis ↓ airflow and gas exchange because of mucous plugs and infection narrowing the airways Result is ↓ Pa. O 2 (hypoxemia) an the arterial blood carbon dioxide level Pa. CO 2 ↑ (respiratory acidosis)
Pathophysiology of Chronic Bronchitis
Chronic Bronchitis
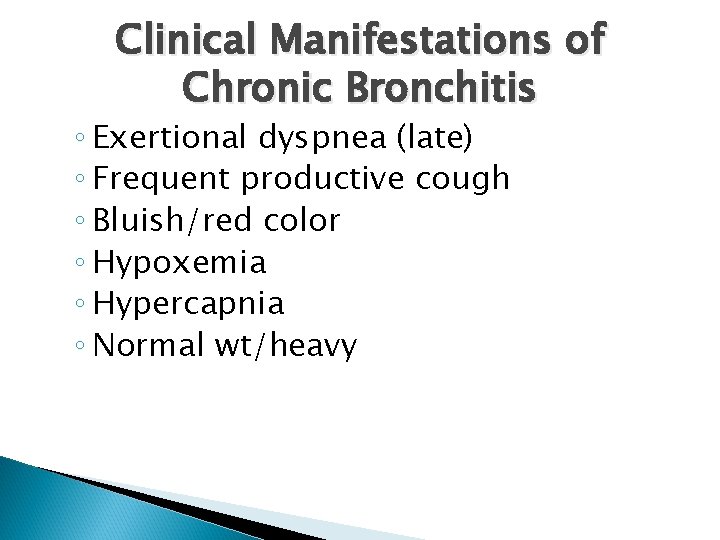
Clinical Manifestations of Chronic Bronchitis ◦ Exertional dyspnea (late) ◦ Frequent productive cough ◦ Bluish/red color ◦ Hypoxemia ◦ Hypercapnia ◦ Normal wt/heavy
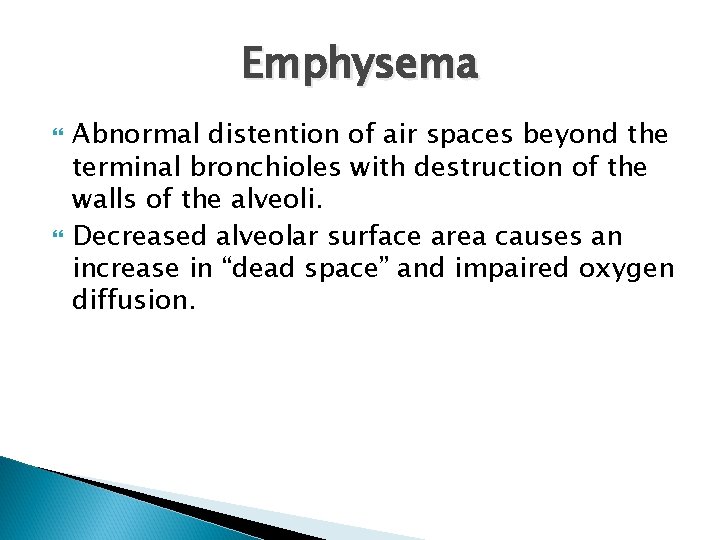
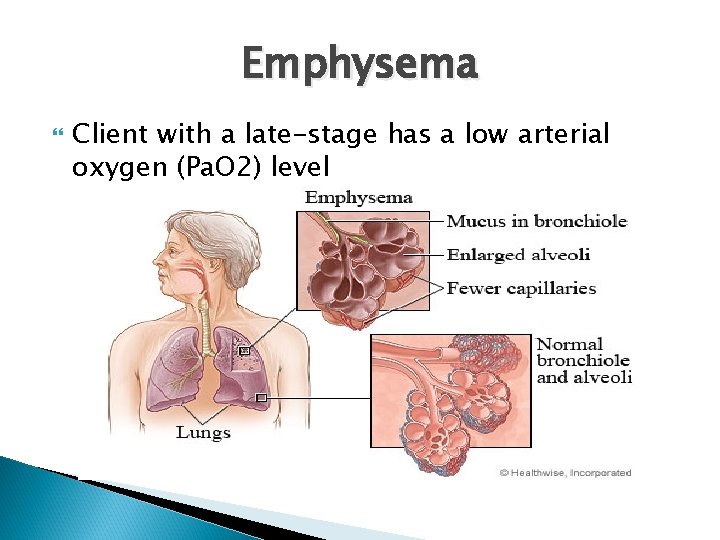
Emphysema Abnormal distention of air spaces beyond the terminal bronchioles with destruction of the walls of the alveoli. Decreased alveolar surface area causes an increase in “dead space” and impaired oxygen diffusion.
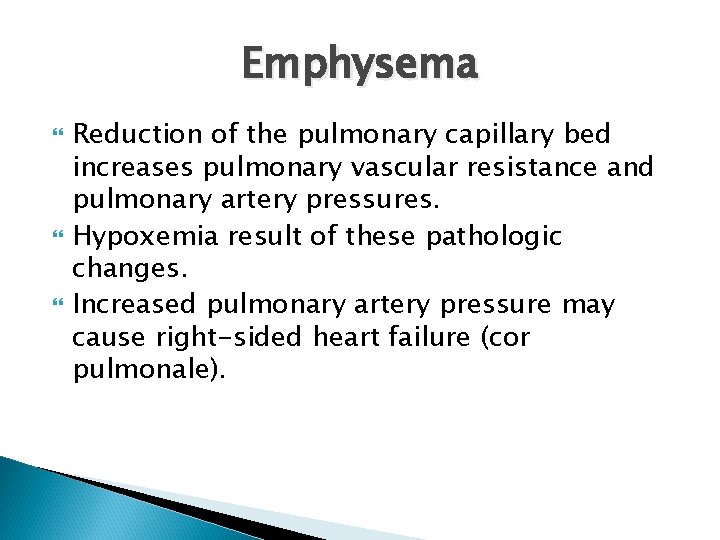
Emphysema Reduction of the pulmonary capillary bed increases pulmonary vascular resistance and pulmonary artery pressures. Hypoxemia result of these pathologic changes. Increased pulmonary artery pressure may cause right-sided heart failure (cor pulmonale).
Pathophysiology of Emphysema →hyperinflation , destruction , collapse alveoli →Centrilobular/panlobular
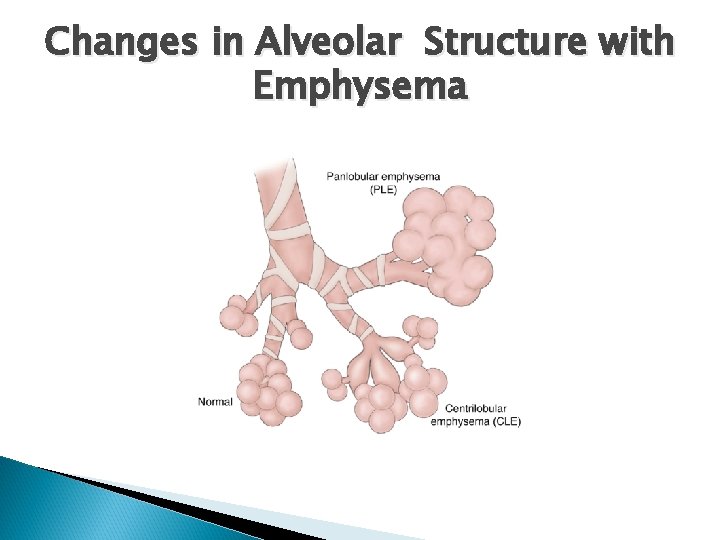
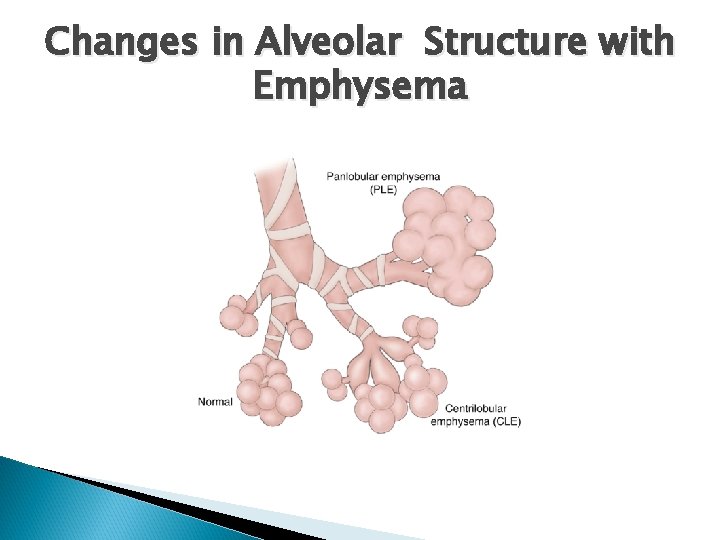
Changes in Alveolar Structure with Emphysema
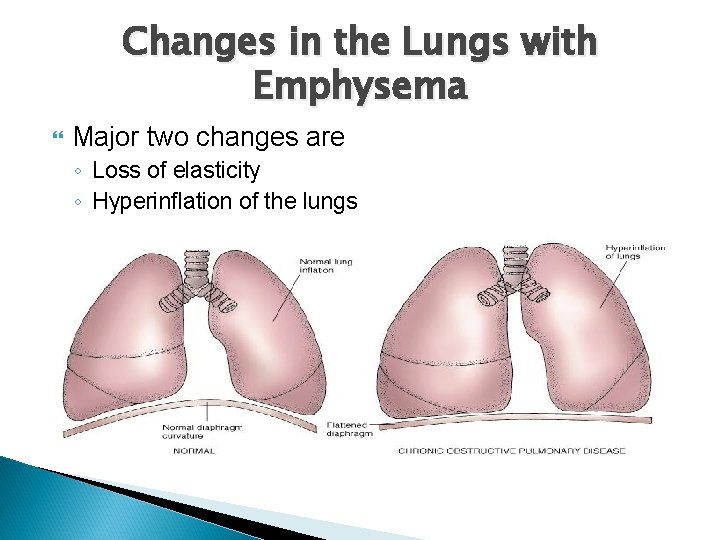
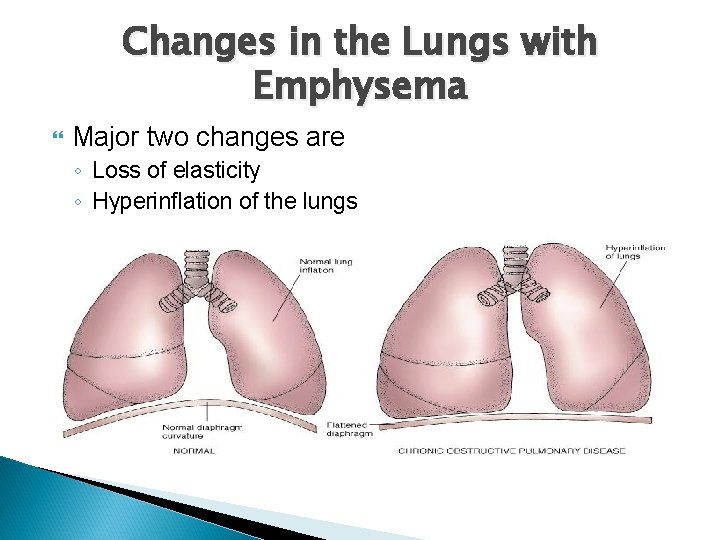
Changes in the Lungs with Emphysema Major two changes are ◦ Loss of elasticity ◦ Hyperinflation of the lungs
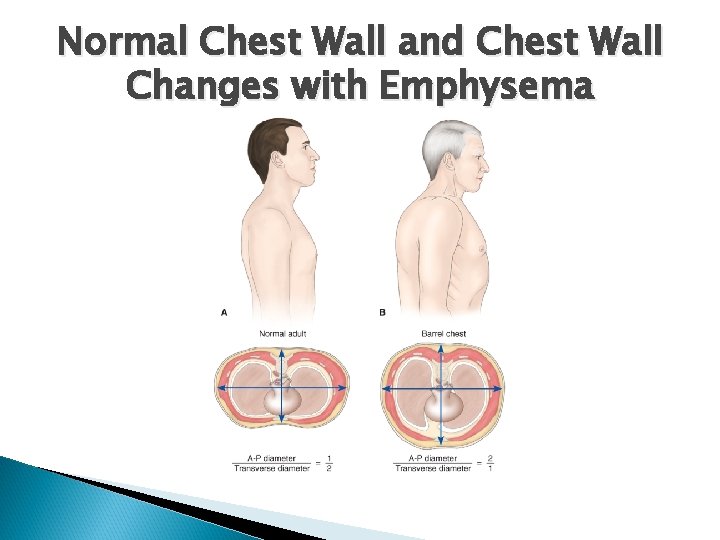
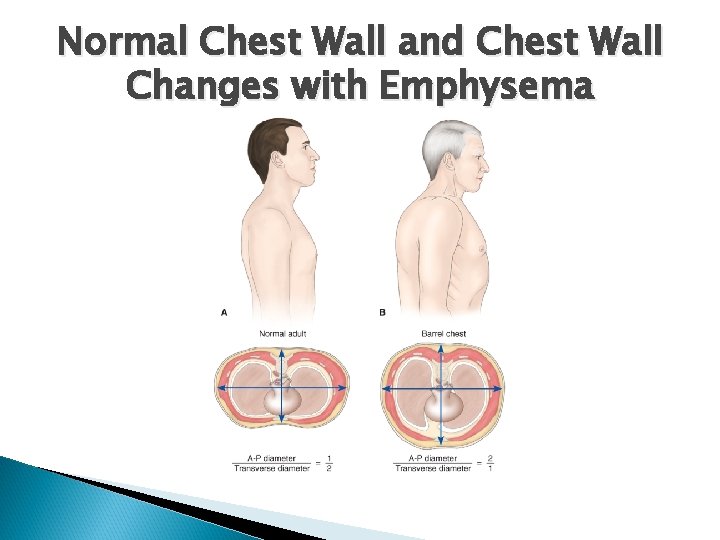
Normal Chest Wall and Chest Wall Changes with Emphysema
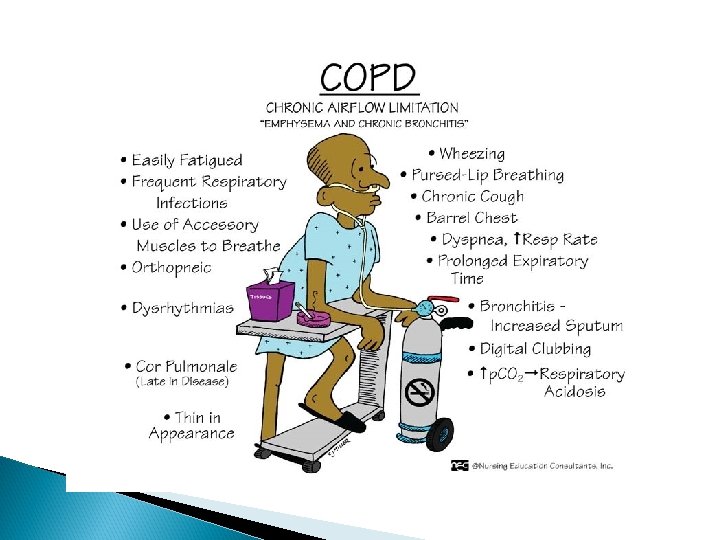
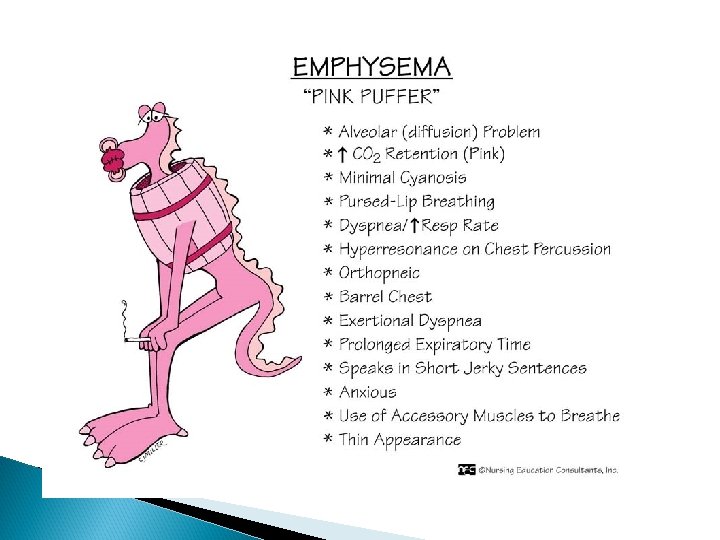
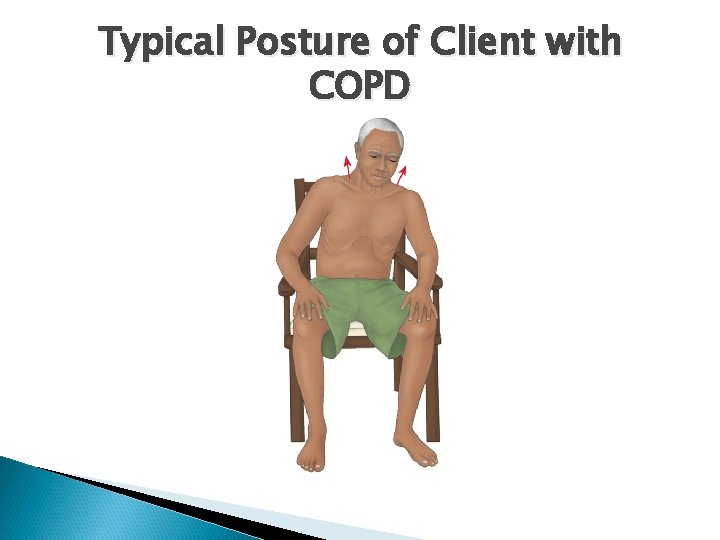
◦ ◦ ◦ ◦ Clinical Manifestations of Emphysema Dyspnea Exertion/rest Min. nonproductive Barrel chest Hypoxemia Hypercapina (late) Underweight (↑ BMR/ ↑ work breathing)
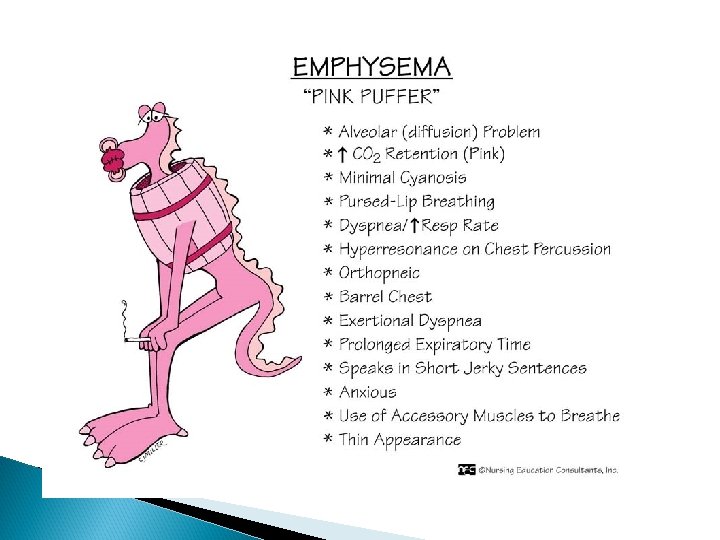
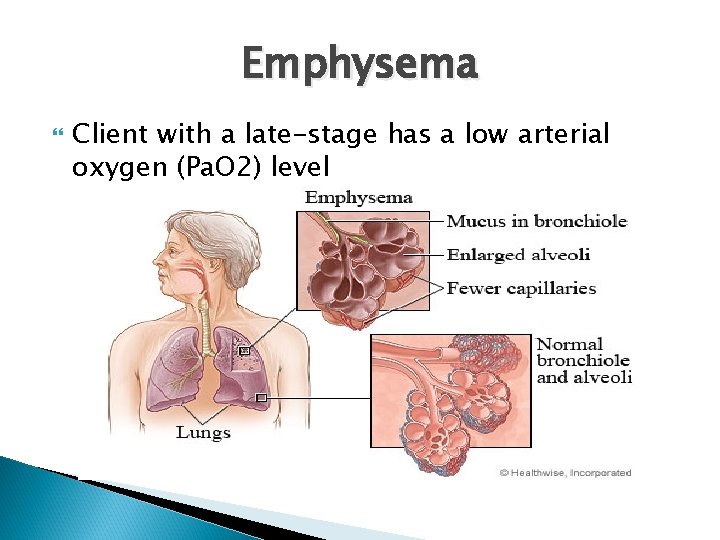
Emphysema Client with a late-stage has a low arterial oxygen (Pa. O 2) level
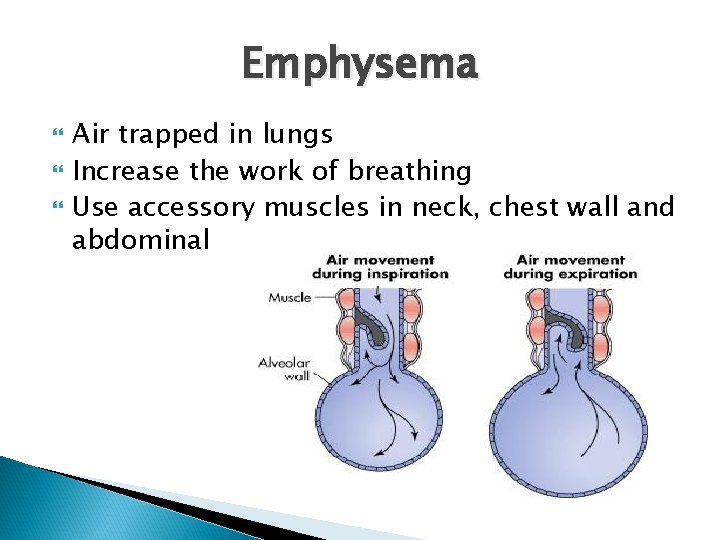
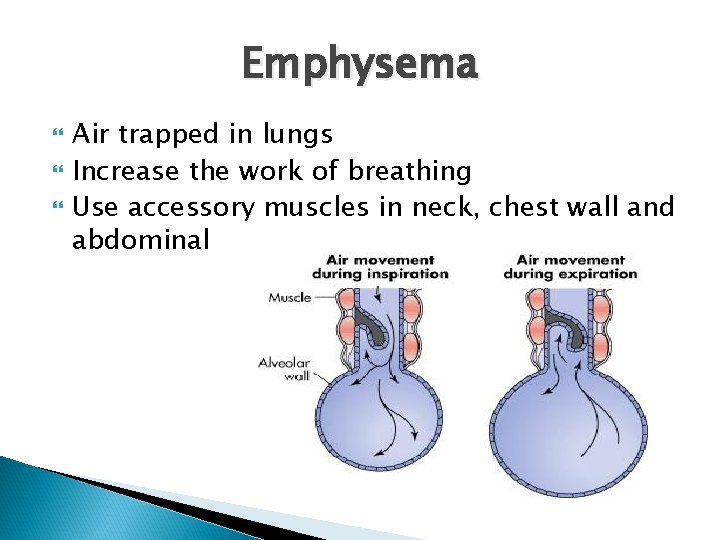
Emphysema Air trapped in lungs Increase the work of breathing Use accessory muscles in neck, chest wall and abdominal
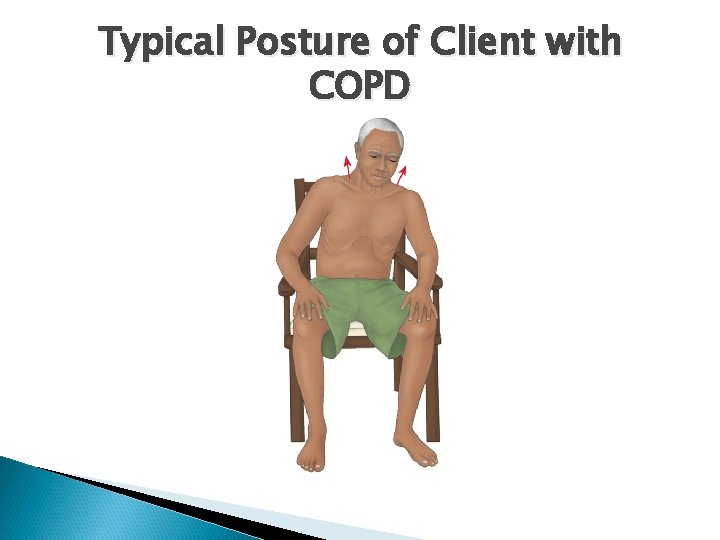
Typical Posture of Client with COPD
Emphysema Gas exchange is affected Often inhalation starts before exhalation is completed, resulting in uncoordinated pattern of breathing Air hunger Client ↑ respiration rate. CO 2 is produced faster than can be eliminated resulting in → CO 2 retention and chronic respiratory acidosis
Emphysema Classifications Panlobular Centrilobular Each type can occur along or in combination in the same lung
Panlobular (panacinar) Panlobular emphysema (PLE) has destruction of the entire alveolus uniformly Diffuse and more severe in the lower lung area
Centrilobular (centriacinar) Occur in the bronchioles Allow spaces to develop as tissue walls breakdown Often seen in longstanding cigarette smokers
ALpha 1 -Antitrypsin Deficiency (AAT) Enzyme made by the liver and is normally present in the lungs Purpose is to regulate other enzymes (protease) that are present to break down inhaled pollutants and microorganisms AAT prevent the protease from working on lung structures AAT is dependent on the inheritance of a pair of normal gene alleles About 100, 000 American have this deficiency
Complications of COPD affects the delivery of oxygen to all tissue Complication of COPD can lead to organ anoxia and tissue death Major problems are: ◦ ◦ Hypoxemia and acidosis Respiratory infections Cardiac failure Cardiac dysrhythmias
Hypoxemia and Acidosis ↓ gas exchange ↓ oxygenation ↑ carbon dioxide→ hypoxemia and acidosis Most tissue have decreased function Hypoxemia refers to deficient blood oxygen Hypoxia refers to decrease in tissue oxygenation
Respiratory Infection from ↑ mucous and poor oxygenation Acute respiratory infections make COPD worse by ↑ inflammation and mucus production and induce more bronchospasm
Complications of COPD Acute exac. of chronic bronchitis due to impaired mucocillary system Acute respiratory failure from acute URI & indiscriminate use of sedatives/narcotics Peptic Ulcer/GERD> meds / stress of disease Pneumonia
Complications of COPD Cor pulmonale or right-sided hart failure Key features of Cor Pulmonale ◦ ◦ ◦ ◦ ◦ Hypoxia & hypoxemia Increasing dyspnea Enlarged & tender liver Warm , cyanotic extremities with bounding pulse Fatigue Cyanotic lips Right ventricle enlargement (hypertrophy) Distended neck veins weakness
Complications of COPD Key features of Cor Pulmonale ◦ ◦ ◦ Lower sternal or epigastric pulsation GI disturbance such as N/V Dependent edema Metabolic and respiratory acidosis Pulmonary hypertension
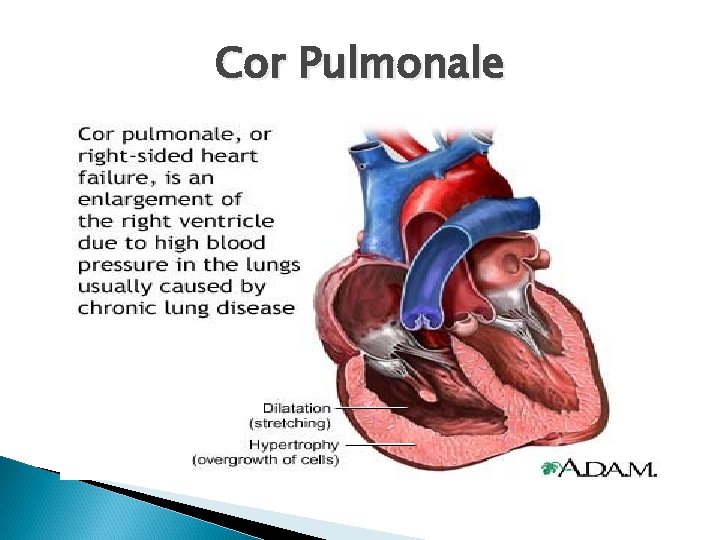
Cor Pulmonale
Health Prevention/Promotion Smoking cessation Pneumonia/influenza vaccines Avoidance of environmental irritants/triggers, extreme in temp, crowds peak URI season & prompt Tx URI
Management COPD History Physical assessment Psychological assessment Laboratory assessment Radiographic assessment Other diagnostic assessments
Management of COPD Assessment History ◦ Risk factors Consider age Gender Occupational history Ethnic cultural background Current problem Weight and diet
Physical Assessment/Clinical Manifestations General appearance ◦ ◦ ◦ Weight in proportion to height Posture Mobility Muscle mass Overall hygiene
Physical Assessment/Clinical Manifestations Respiratory changes ◦ Assess breathing rate and pattern ◦ Assess degree of dyspnea ◦ palpate chest for tenderness and abnormal retractions ◦ Examine chest for presence of “barrel chest” ◦ Assess for cyanosis, delayed capillary refill and clubbing of the fingers

Physical Assessment/Clinical Manifestations Cardiac changes ◦ Assess heart rate & rhythm ◦ Check for swelling of feet and ankles (dependent edema) ◦ Examine nail beds and oral mucous membranes ◦ Pallor or frank cyanosis
Psychosocial Assessment Reduced socialization ◦ ◦ ◦ Annoying coughs Excessive sputum Dyspnea Exposure to irritants may reduce hobbies Economic status Work, family, social and sexual roles affected
Diagnostic Assessment ABGs Sputum cultures WBC HGB & HCT Serum electrolytes CXR PFT Pulse oximetry ECG
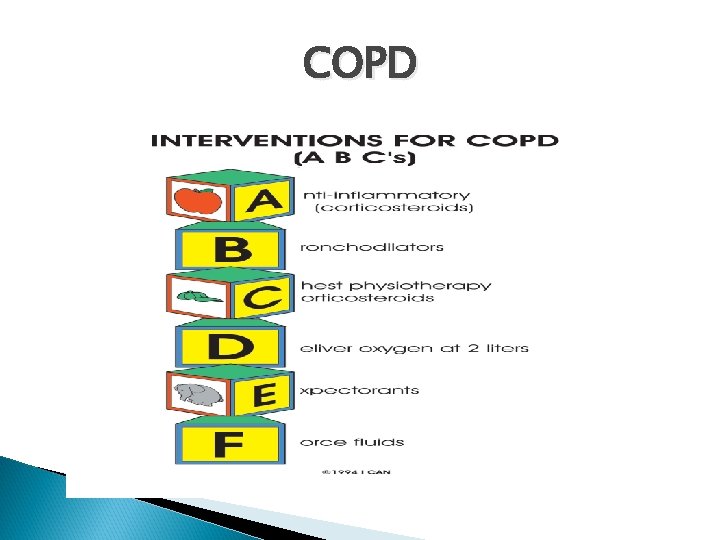
Management of COPD Oxygen therapy Drug therapy Respiratory therapy Exercise training Surgical intervention Nutrition Anxiety Activity intolerance
Management of COPD Oxygen therapy ◦ Use to treat hypoxemia. COPD pt are CO 2 retainers ◦ Their drive to breath is stimulated by hypoxia ◦ Always use humidity & titrate O 2 to lowest effective concentration usually 1 to 2 liters
Management of COPD Drug Therapy Bronchodilators- decrease airway resistant & hyperinflation of lung resulting in decreased dyspnea & ˄FEV. Used as maintenance therapy ◦ Inhaled anticholingerics (atrovent most effective also used in combination B 2 agonist (combivent) ◦ B 2 agonist (albuterol) ◦ Long acting B 2 agonist (theophylline)
Management of COPD Drug Therapy (cont. ) Corticosteroids used frequent in exac. that don’t respond to bronchodilators/ bronchospasm/asthma Mucolytic prescribed for pt with thick tenacious mucous secretions ◦ Neb with NS or agents such as mucomyst or mucosil ◦ Guiafenesin is a systemic mucolytic taken orally
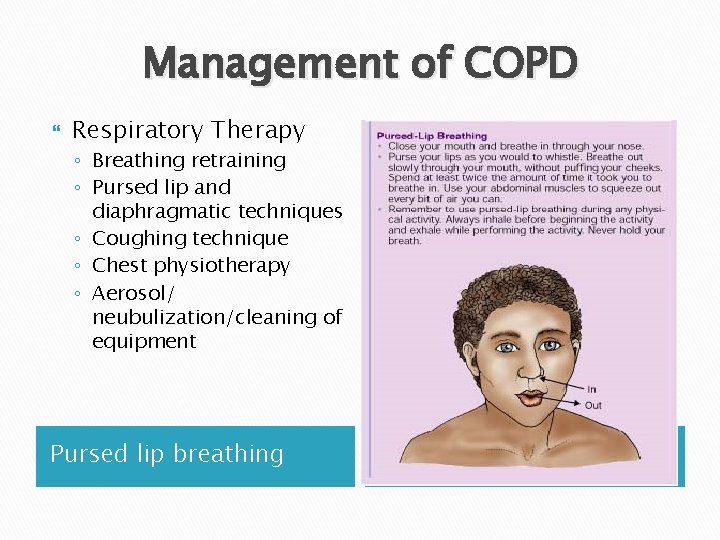
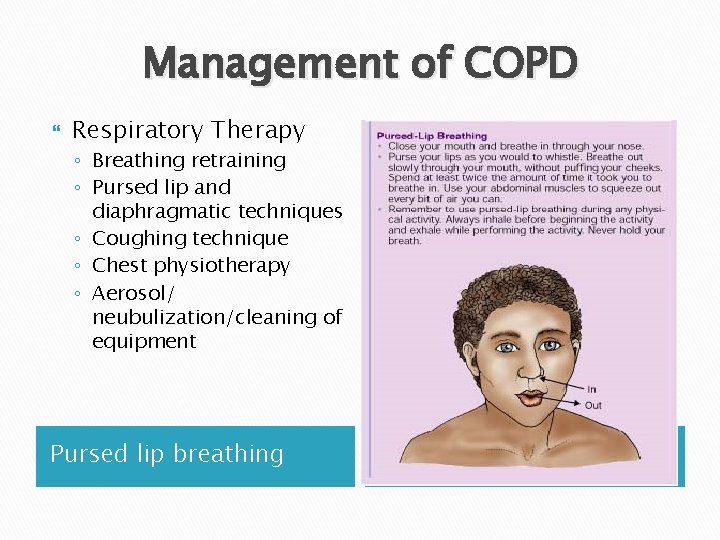
Management of COPD Respiratory Therapy ◦ Breathing retraining ◦ Pursed lip and diaphragmatic techniques ◦ Coughing technique ◦ Chest physiotherapy ◦ Aerosol/ neubulization/cleaning of equipment Pursed lip breathing
Management of COPD Exercise training ◦ Walk 15 -20 min/day. Guideline to avoid over exerting if SOB return to normal level 5 min after rest ◦ Use bronchodilator before exercise and 5 min after stopping activity
Management of COPD Surgical management ◦ Lung transplantation ◦ Lung reduction Preoperative ◦ Selection process requires several criteria Post care ◦ Close monitoring for respiratory problems
Management of COPD Nutrition ◦ Monitor pt weight ◦ Foods easy to chew and non gas forming ◦ High caloric & high protein diet divided in to 5 -6 meals /day ◦ Rest and bronchodilators before and after meals ◦ Avoid drinking fluids before and during meals ◦ Avoid milk, chocolate when symptomatic ◦ Fluid intake 3 liters/day between meals ◦ Mouth care before meals ◦ Assist with feeding when tire easy
Management of COPD Activity intolerance Encourage pt to pace activities Provide as much self-care as possible Instruct not to rush through morning activities Assess pt response to activities (skin color, vital signs, etc. ) ◦ Provide supplemental oxygen during high energy activities as necessary ◦ ◦
Management of COPD Anxiety ◦ Develop written plan that states exactly what to do if symptoms flare ◦ Stress the use of pursed lip and diaphragmatic breathing technique ◦ Friends, family and support group ◦ Professional counseling id necessary
Current Evidence –Based Practices Early identifications with spirometry Individualize the management of stable COPD Education Pharmacotherapy Exercise exacerbations
Current Evidence –Based Practice Referral to registered dietitian for COPD pts Restrict sodium to <2000 mg/day Consume folate in the form of food and/or a combination of B 6, B 12 and supplementation Drink 48 -64 oz of fluid daily Consume RDA for antioxidants A, C and E, and adequate intake of omega-3 fatty acids
Community Based Care Home care management ◦ Oxygen, equipment at home ◦ Financial concerns (disability benefits) Health teaching ◦ Knowledgeable of disease process ◦ Drug therapy, manifestation of infection and avoidance of irritants Health care resources ◦ Support group (American Lung Association) ◦ Smoking cessation ◦ Meals on wheels
Nursing Process: The Care of Patients with COPD- Assessment Health history Inspection and examination findings Review of diagnostic tests
Nursing Process: The Care of Patients with COPD- Diagnoses Impaired gas exchange Impaired airway clearance Ineffective breathing pattern Activity intolerance Deficient knowledge Ineffective coping
Nursing Diagnosis for COPD Ineffective airway clearance R/T exp airflow obstruction /ineffective cough Impaired gas exchange R/T alveolar hypoventilation Imbalanced nutrition: less than R/T poor appetite/fatigue/SOB/sputum production Disturbed sleep pattern R/T dyspnea/depression/abnormal ABG Risk for infection R/T ineffective airway clearance/lack of knowledge regarding infectious process
Nursing Process: The Care of Patients with COPD- Planning Smoking cessation Improved activity tolerance Maximal self-management Improved coping ability Adherence to therapeutic regimen and home care Absence of complications
Collaborative Problems Respiratory insufficiency or failure Atelectasis Pulmonary infection Pneumonia Pneumothorax Pulmonary hypertension
Improving Gas Exchange Proper administration of bronchodilators and corticosteroids Reduction of pulmonary irritants Directed coughing, “huff” coughing Chest physiotherapy Breathing exercises to reduce air trapping ◦ diaphragmatic breathing ◦ pursed lip breathing Use of supplemental oxygen
Improving Activity Tolerance Focus on rehabilitation activities to improve ADLs and promote independence. Pacing of activities Exercise training Walking aides Utilization of a collaborative approach
Other Interventions Set realistic goals Avoid extreme temperatures Enhancement of coping strategies Monitor for and management of potential complications
COPD
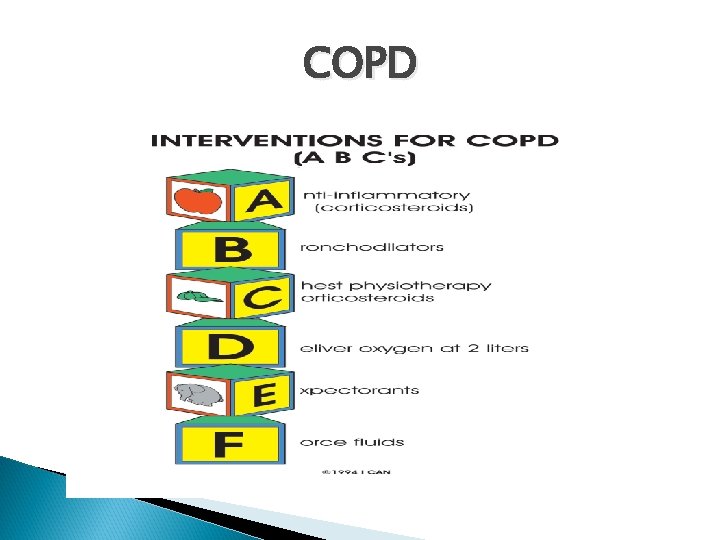
COPD
Client Teaching Disease process Medications Procedures When and how to seek help Prevention of infections Avoidance of irritants; indoor and outdoor pollution, and occupational exposure Lifestyle changes, including cessation of smoking
COPD Summary Overall goal for management Return/maintain baseline resp. function Ability to perform ADL Relief of dyspnea Suffer no or delay complications Knowledge and ability to implement long-term treatment plan ◦ Overall improvement in quality of life ◦ ◦ ◦
Asthma A chronic inflammatory disease of the airways that causes hyperresponsiveness, mucosal edema, and mucous production. Inflammation leads to cough, chest tightness, wheezing, and dyspnea. The most common chronic disease of childhood. Can occur at any age. Allergy is the strongest predisposing factor.
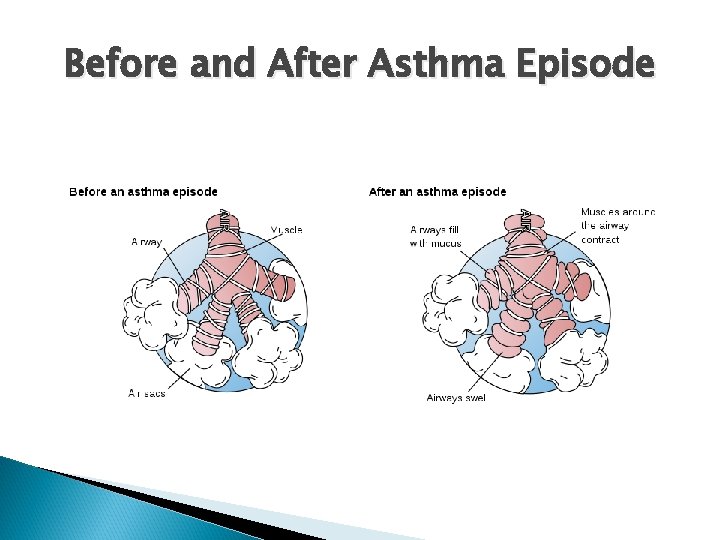
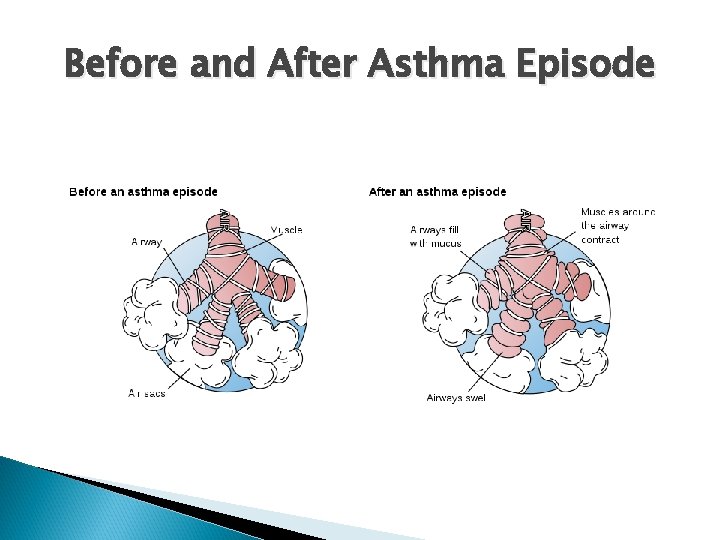
Before and After Asthma Episode
Pathophysiology of Asthma Hyperresponsiveness to a trigger which cause muscosal edema in the bronchi and mucus production the stagnated muscus in the bronchi cause inflammation causing bronchoconstriction Chronic asthma Acute asthma is caused by triggers that stimulate beta-adrenergic receptors in the bronchi which cause bronchoconstriction
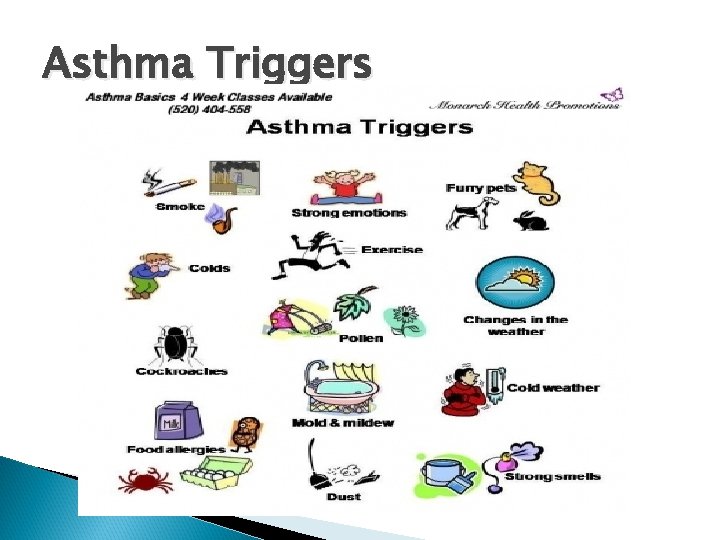
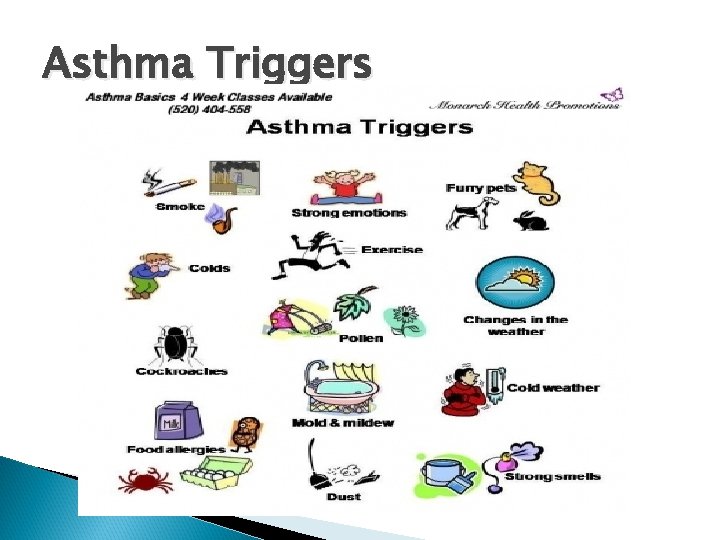
Asthma Triggers
Clinical Manifestation of Asthma Cough Dyspnea Wheezing Chest tightness Exacerbation progression ◦ ◦ Diaphoresis Tachycardia Wide pulse pressure Hypoxemia (late sign of poor oxygenation)
Assessment and Diagnostic Findings Family and environmental history Cormobidity conditions (GERD) Other possible allergic reactions Sputum Blood tests (WBC, Ie. G, ABGs) Pulmonary function test ◦ Spirometer(preferred test) ◦ Peak flow(not reliable for kids <5 yrs old) Nursing alert: Normal Pa. CO 2 during an asthma attack may be a signal of impending respiratory failure
Use of Peak Flow Meter Peak flow meter is small hand held device used to measure amount of air flow out of the lung Meter records flow as a number also known as Peak Expiratory Flow (PEF) Use of a peak flow meter helps to determine how well controlled a person’s asthma is and can help indicate when an attack may happen
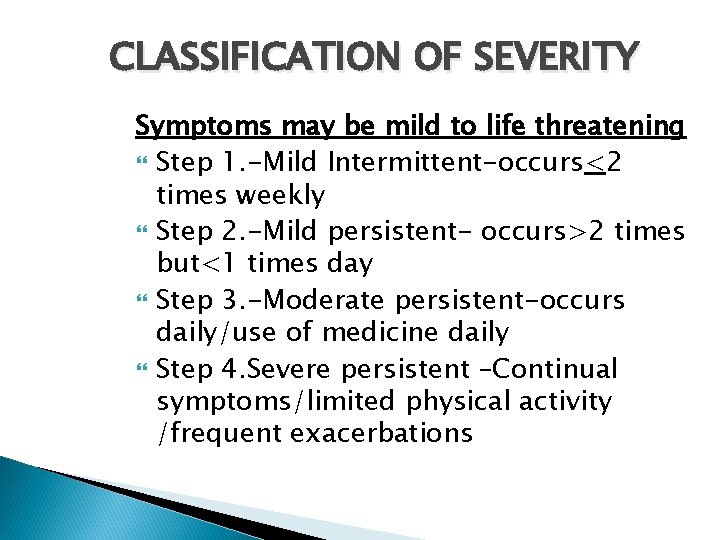
CLASSIFICATION OF SEVERITY Symptoms may be mild to life threatening Step 1. -Mild Intermittent-occurs<2 times weekly Step 2. -Mild persistent- occurs>2 times but<1 times day Step 3. -Moderate persistent-occurs daily/use of medicine daily Step 4. Severe persistent –Continual symptoms/limited physical activity /frequent exacerbations
Asthma Preventions Complications Medical Management ◦ ◦ Pharmacologic Therapy Quick relief medications Long acting controlling medications Peak flow monitoring
Medications Used for Asthma Quick-relief medications ◦ Beta 2 -adrenergic agonists ◦ Anticholinergics Long-acting medications ◦ Corticosteroids ◦ Long acting beta 2 -adrenergic agonists ◦ Leukotriene modifiers
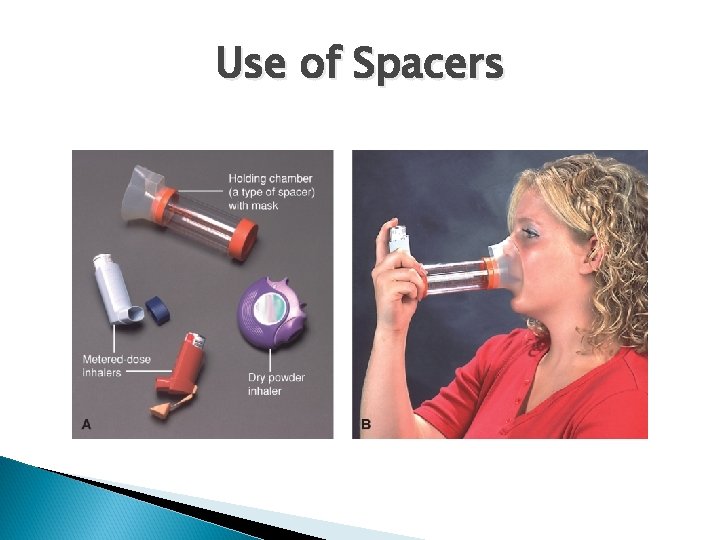
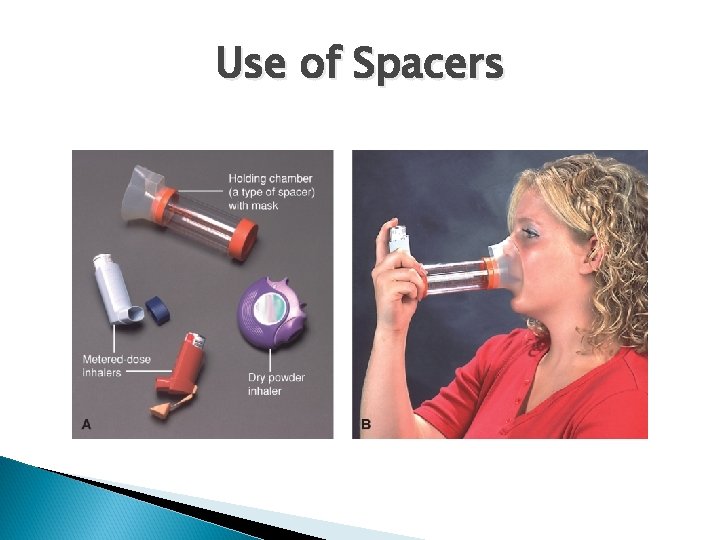
Use of Spacers
Nursing Management Assessment ◦ ◦ ◦ Assess respiratory status History Identify medication Administrating prescribed medications Administrating fluids Promoting home and community-based care
Asthma
Client Teaching The nature of asthma as a chronic inflammatory disease Definition of inflammation and bronchoconstriction Purpose and action for each medication Identification of triggers and how to avoid them Proper inhalation techniques How to perform peak flow monitoring How to implement an action plan When and how to seek assistance
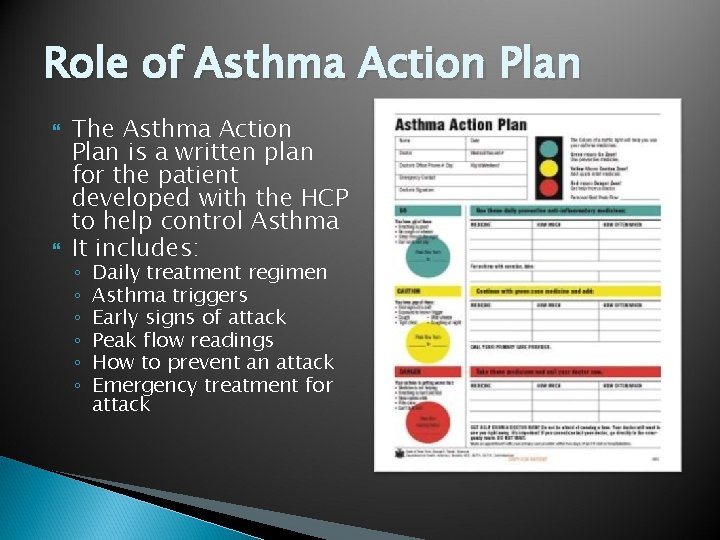
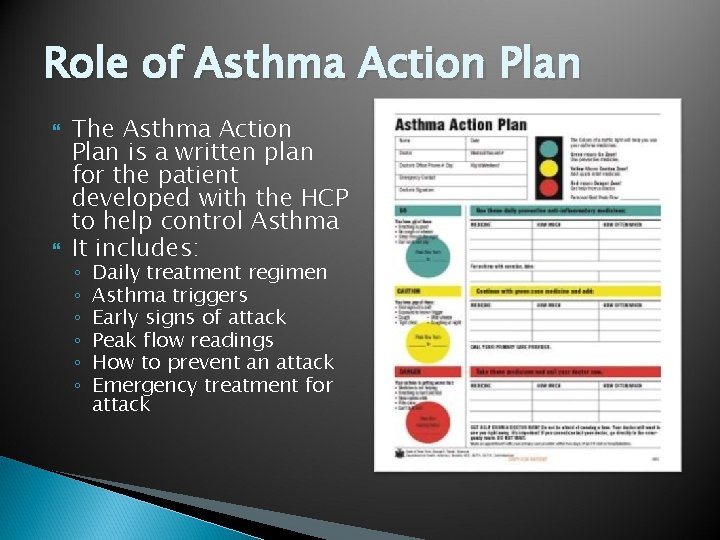
Role of Asthma Action Plan The Asthma Action Plan is a written plan for the patient developed with the HCP to help control Asthma It includes: ◦ ◦ ◦ Daily treatment regimen Asthma triggers Early signs of attack Peak flow readings How to prevent an attack Emergency treatment for attack
Asthma Summary Pathophysiology Clinical Manifestation Assessment and Diagnostic findings Preventions Complications Medical Management Nursing Management Client Teaching
Pulmonary Tuberculosis Infectious disease affecting the lung parenchyma Other parts of the body: meninges, kidneys, bones, and lymph nodes
Pathophysiology of TB Infected with mycobacteria organism via airborne through airway to the alveoli. Immune system activate which engulfs the organism and cause the accumulation of exduate in the alveoli within 2 to 10 weeks after exposure. This tissue of live and dead bacilli forms a protective wall and become necrotic and later become calcified and form a collagenous scar. Common site is the apical or posterior segment of the upper lobe or the superior segment of the lower lobe of the lung
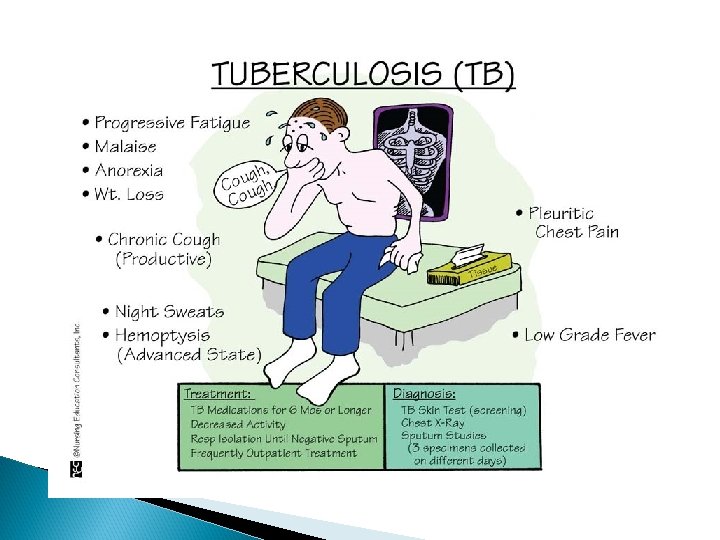
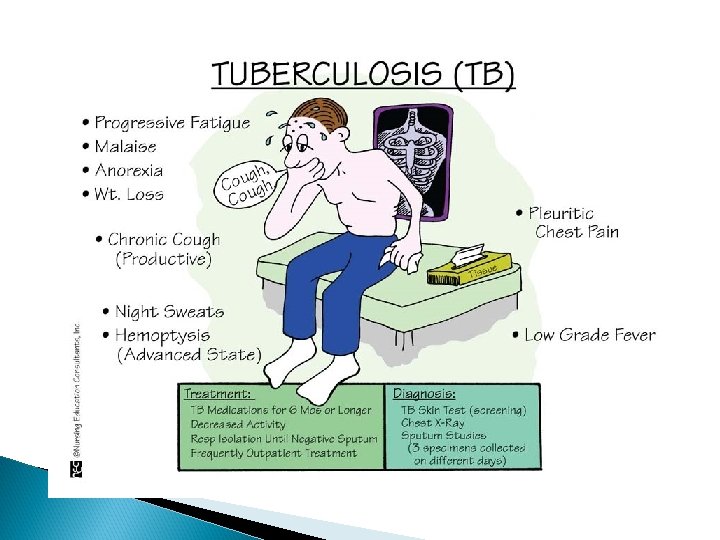
Clinical Manifestation Low grade fever Cough night sweats Hemoptysis Anorexia Weight loss Present for weeks or months
Assessment and Diagnostic Findings History Physical exam Tuberculin skin test Chest Xray Sputum culture Quanti. FERON-TB Gold Test
Classifications of TB Page 569 Class o- no exposure; no infection Class 1 - exposure no infection Class 2 - latent infection; no disease (positive PPD, no clinical evidence of active RB Class 3 - disease; clinically active Class 4 - disease; not clinically active Class 5 - suspect disease; diagnosis pending
TB Gerontology Consideration Medical Management ◦ Pharmacologic therapy Nursing Management ◦ ◦ Promoting airway clearance Advocating adherence to treatment regimen Promoting activity and adequate nutrition Preventing spread of TB infection
Tuberculosis R RIFAMPIN I ISONIAZID S STREPTOMYCIN E ETHAMBUTOL
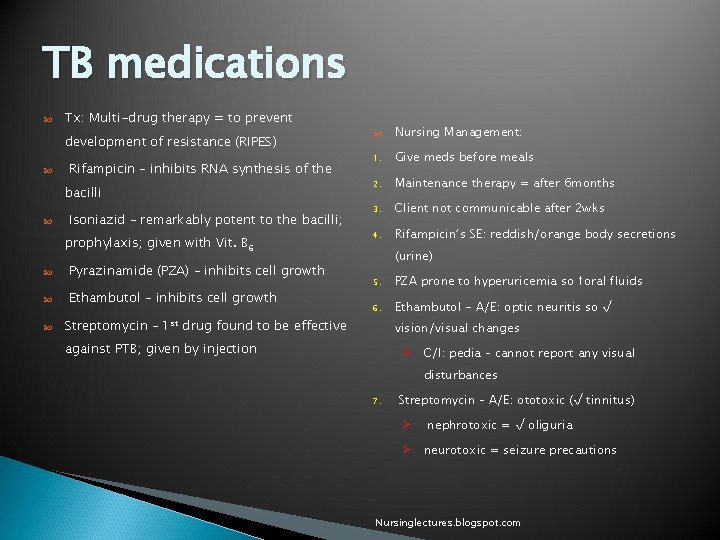
TB medications Tx: Multi-drug therapy = to prevent development of resistance (RIPES) Rifampicin – inhibits RNA synthesis of the bacilli Isoniazid – remarkably potent to the bacilli; prophylaxis; given with Vit. B 6 Pyrazinamide (PZA) – inhibits cell growth Ethambutol – inhibits cell growth Nursing Management: 1. Give meds before meals 2. Maintenance therapy = after 6 months 3. Client not communicable after 2 wks 4. Rifampicin’s SE: reddish/orange body secretions (urine) 5. PZA prone to hyperuricemia so ↑oral fluids 6. Ethambutol - A/E: optic neuritis so √ Streptomycin – 1 st drug found to be effective vision/visual changes against PTB; given by injection Ø C/I: pedia – cannot report any visual disturbances 7. Streptomycin – A/E: ototoxic (√ tinnitus) Ø nephrotoxic = √ oliguria Ø neurotoxic = seizure precautions Nursinglectures. blogspot. com
TB Infection Control Airbone isolation Negative Pressure Room N 95 masks Keep door closed at all times Transport patient with masks
Criteria to be considered Noninfectious 3 consecutive negative sputum smears Their symptoms have improved, and They are adhering to an adequate treatment regimen for at least two weeks.
TB Summary Pathophysiology Clinical Manifestation Assessment and diagnostic findings Classifications Gerontology consideration Medical management Nursing management
Respiratory Infections Acute tracheobronchitis Pneumonia ◦ ◦ Community-acquired pneumonia Hospital-acquired pneumonia Pneumonia in immunocompromised host Aspiration pneumonia
Diagnostic Tests Chest x-ray Sputum examination
Medical Treatment of Pneumonia Supportive treatment includes fluids, oxygen for hypoxia, antipyretics, antitussives, decongestants, antihistamines Administration of antibiotic therapy determined by gram-stain results If etiologic agent is not identified, utilize empiric antibiotic therapy Antibiotics not indicated for viral infections but are used for secondary bacterial infection
Nursing Process: Care of the Patient with Pneumonia Diagnoses Ineffective airway clearance Activity intolerance Risk for fluid volume deficient Imbalanced nutrition Deficient knowledge
Collaborative Problems Continuing symptoms after initiation of therapy Shock Respiratory failure Atelectasis Pleural effusion Confusion Superinfection
Nursing Process: Care of the Patient with Pneumonia - Planning Improved airway clearance Maintenance of proper fluid volume Maintenance of adequate nutrition Patient understanding of treatment, prevention Absence of complications
Improving Airway Clearance Encourage hydration; 2 to 3 L a day, unless contraindicated Humidification may be used to loosen secretions ◦ By face mask or with oxygen Coughing techniques Chest physiotherapy Position changes Oxygen therapy administered to meet patient needs
Other Interventions Promoting rest ◦ Encourage rest, avoidance of overexertion ◦ Positioning to promote rest, breathing (Semi-Fowler’s) Promoting fluid intake ◦ Encourage fluid intake to at least 2 L a day Maintaining nutrition ◦ Provide nutritionally enriched foods, fluids Patient teaching
Evidenced Based Core Measures for Pneumonia Oxygenation assessment with ABG or pulse oximetry within 24 hour prior to or after hospital arrival Pneumococcal vaccine Blood cultures within 24 hours prior to or 24 hours after hospital arrival Adult smoking cessation advice/counseling(including prescriptions for patches/gum/meds/handouts/video Initial Antibiotic with 4 -6 hr of hospital arrival Influenza vaccination discharged during October and March
Aspiration Risk factors Pathophysiology Prevention: ◦ Elevate HOB ◦ Turn patient to side when vomiting ◦ Prevention of stimulation of gag reflex with suctioning or other procedures ◦ Assessment, proper administration of tube feeding ◦ Rehabilitation therapy for swallowing
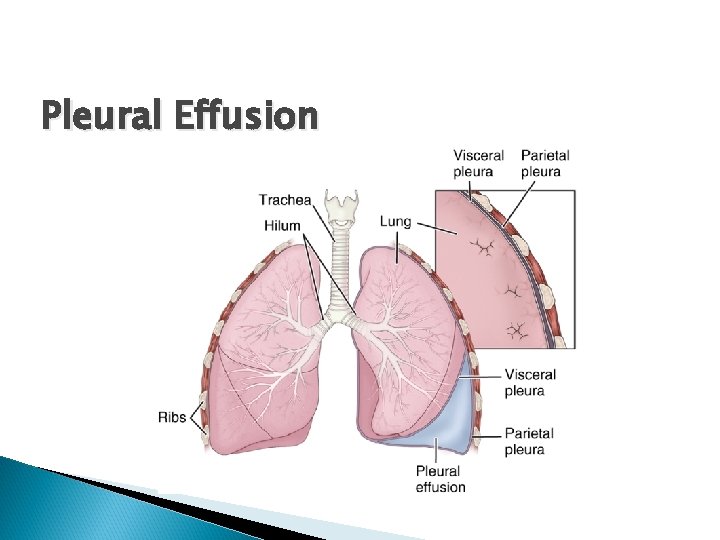
Pleural Conditions Pleurisy: inflammation of both layers of pleurae ◦ Inflamed surfaces rub together with respirations, cause sharp pain intensified with inspiration Pleural effusion: collection fluid in pleural space usually secondary to another disease process ◦ Large effusions impair lung expansion, cause dyspnea
Pleural Conditions (cont’d) Empyema: accumulation of thick, purulent fluid in pleural space. ◦ Patient usually acutely ill; fluid, fibrin development, loculation impair lung expansion ◦ Resolution is a prolonged process
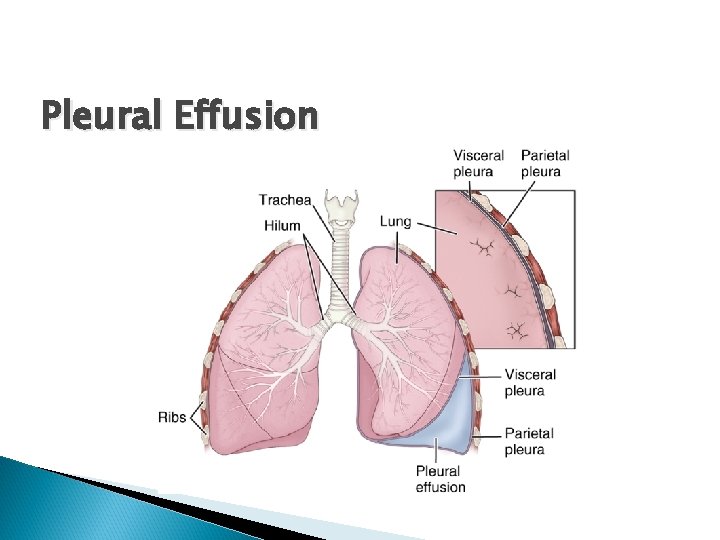
Pleural Effusion
Causative Factors for Pulmonary Disease Cigarette smoking Air pollution