Some Respiratory Presentations in Kids David Williams Wheezy


- Slides: 56
Some Respiratory Presentations in Kids David Williams
Wheezy Child Bronchiolitis Croup
Wheezing Child
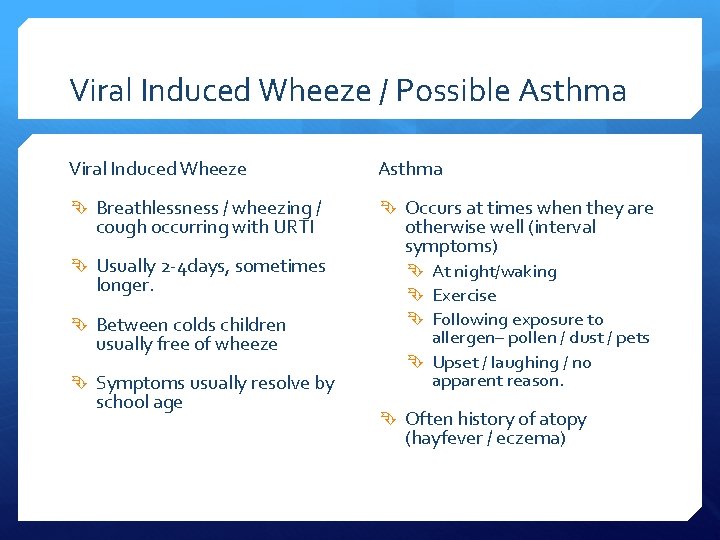
Viral Induced Wheeze / Possible Asthma Viral Induced Wheeze Asthma Breathlessness / wheezing / Occurs at times when they are cough occurring with URTI Usually 2 -4 days, sometimes longer. Between colds children usually free of wheeze Symptoms usually resolve by school age otherwise well (interval symptoms) At night/waking Exercise Following exposure to allergen– pollen / dust / pets Upset / laughing / no apparent reason. Often history of atopy (hayfever / eczema)
Viral Induced Wheeze / Exacerbation of Asthma – Initial Assessment Degree of Agitation / Consciousness - behavioral change/agitation can be signs of hypoxia

Viral Induced Wheeze / Exacerbation of Asthma – Initial Assessment Signs of Exhaustion (inability to complete sentences) Signs of cyanosis (lips / extremities) Use of accessory muscles at rest
Viral Induced Wheeze / Exacerbation of Asthma – Initial Assessment Examine Chest Record Resp Rate Pulse BP
Viral Induced Wheeze / Exacerbation of Asthma – Initial Assessment Record Peak Flow (if old enough) use best of three compare to best (if last two years) or predicted
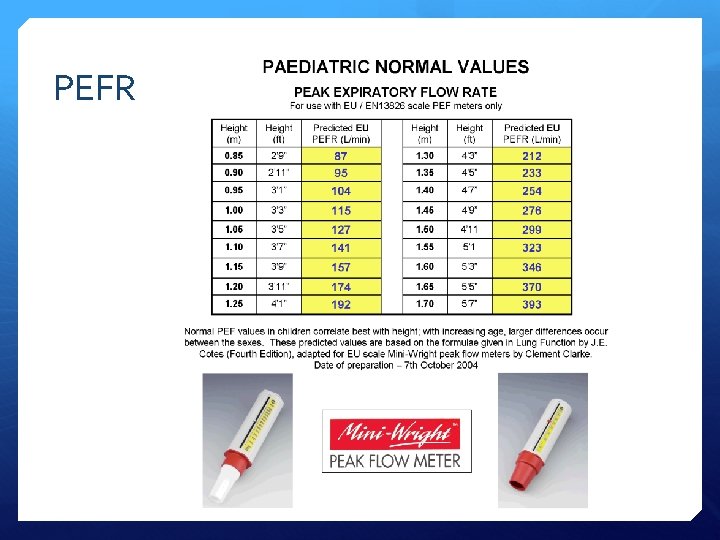
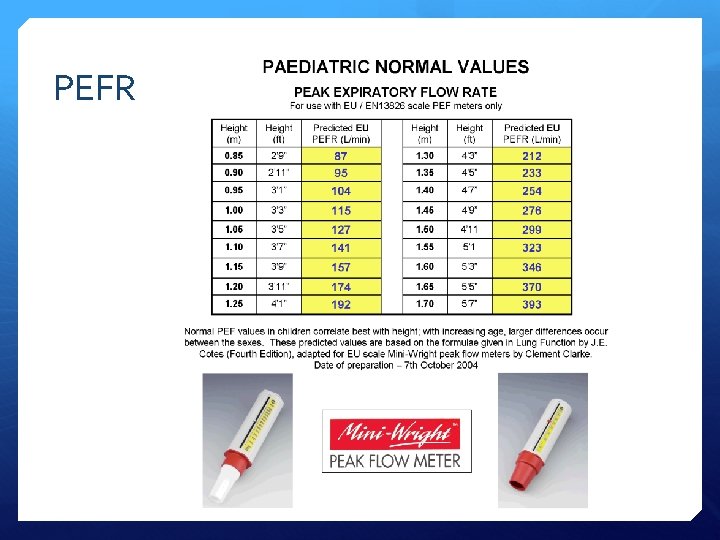
PEFR
Viral Induced Wheeze / Exacerbation of Asthma – Assessment Grade of severity Life Threatening Acute Severe Moderate
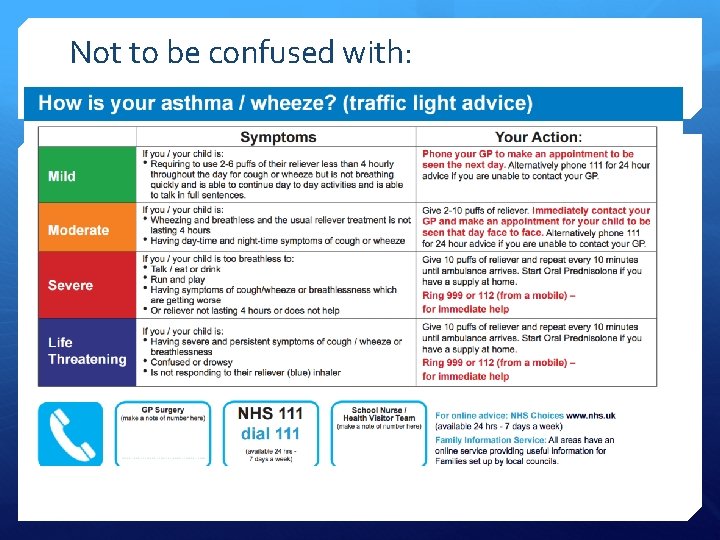
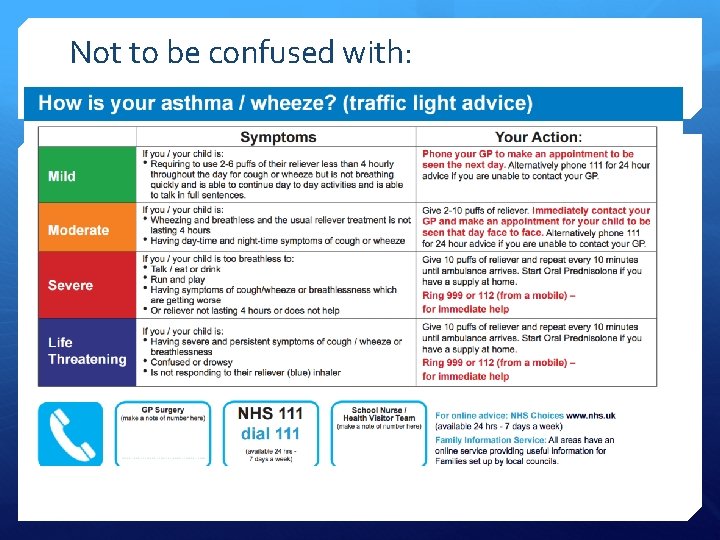
Not to be confused with:
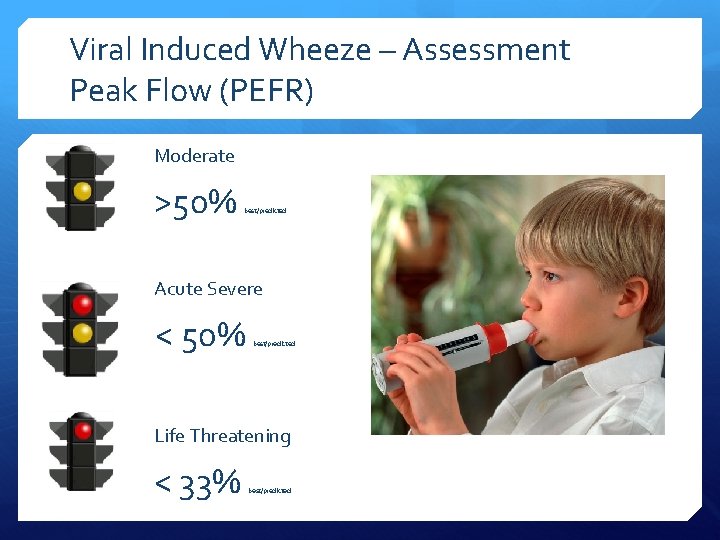
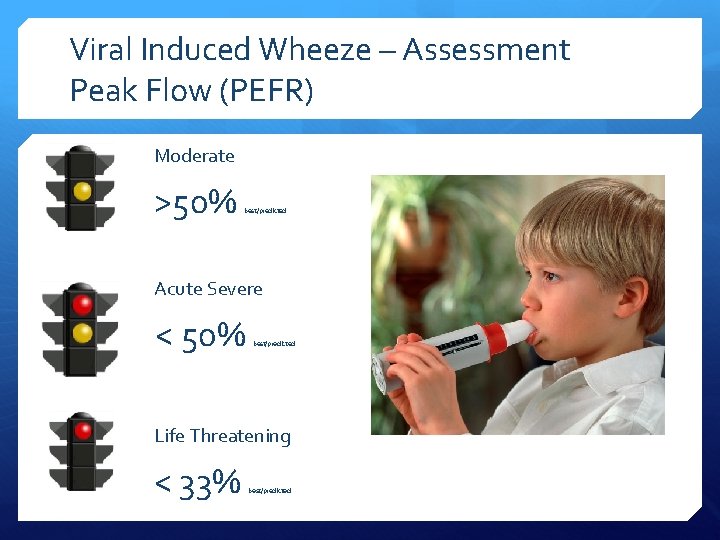
Viral Induced Wheeze – Assessment Peak Flow (PEFR) Moderate >50% best/predicted Acute Severe < 50% best/predicted Life Threatening < 33% best/predicted
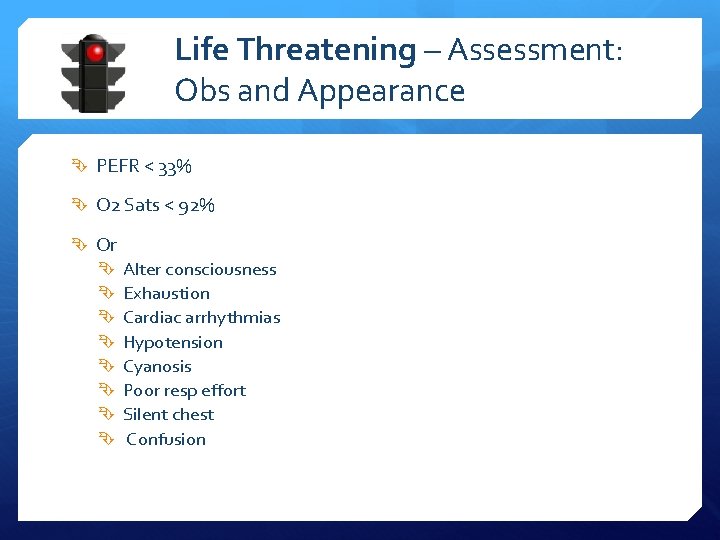
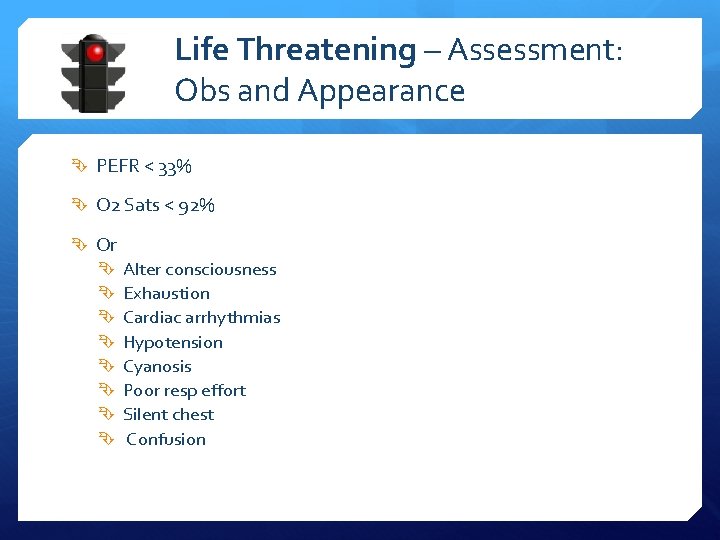
Life Threatening – Assessment: Obs and Appearance PEFR < 33% O 2 Sats < 92% Or Alter consciousness Exhaustion Cardiac arrhythmias Hypotension Cyanosis Poor resp effort Silent chest Confusion
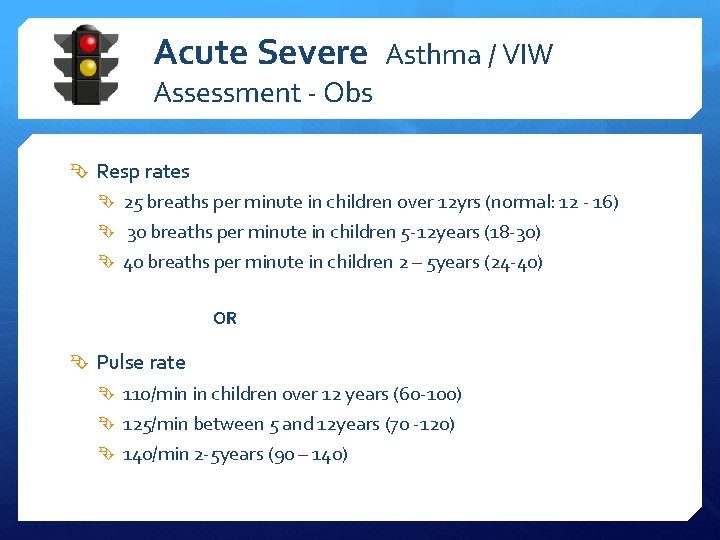
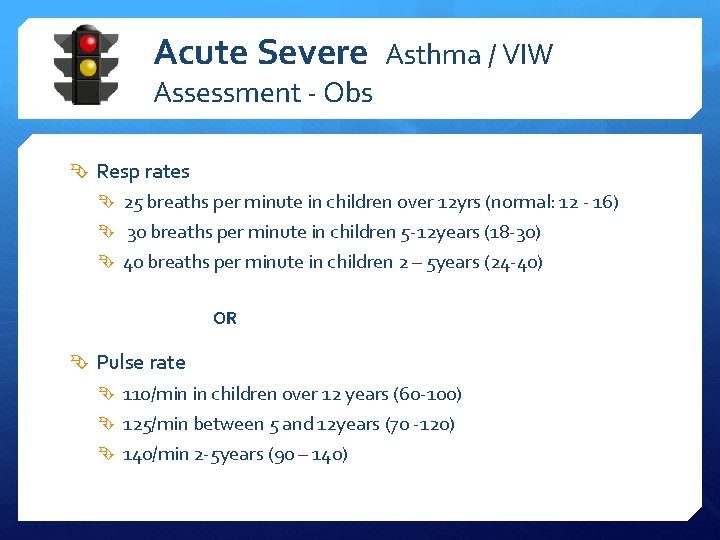
Acute Severe Asthma / VIW Assessment - Obs Resp rates 25 breaths per minute in children over 12 yrs (normal: 12 - 16) 30 breaths per minute in children 5 -12 years (18 -30) 40 breaths per minute in children 2 – 5 years (24 -40) OR Pulse rate 110/min in children over 12 years (60 -100) 125/min between 5 and 12 years (70 -120) 140/min 2 -5 years (90 – 140)
Moderate VIW / Exacerbation of Asthma Moderate PEFR > 50% best/predicted Normal speech No acute severe or life threatening features
Viral Induced Wheeze / Possible Asthma – When to Admit All life-threatening Any severe attack where symptoms don’t settle after initial treatment Any moderate attack with worsening symptoms despite treatment and/or have had previous near-fatal attack
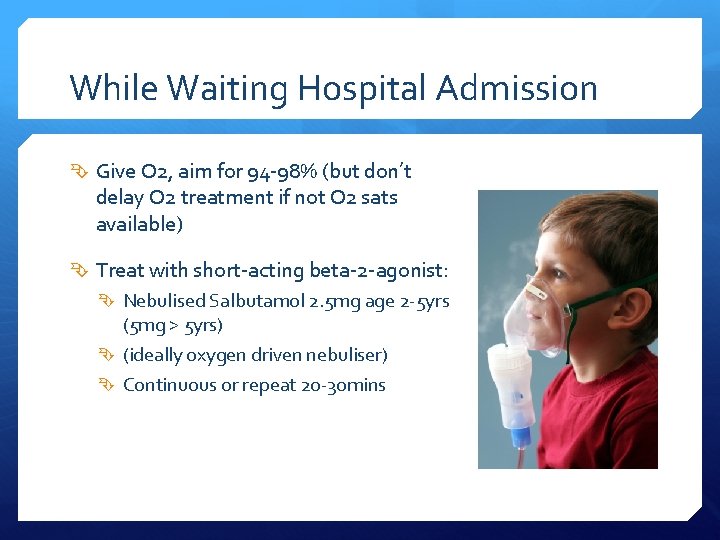
While Waiting Hospital Admission Give O 2, aim for 94 -98% (but don’t delay O 2 treatment if not O 2 sats available) Treat with short-acting beta-2 -agonist: Nebulised Salbutamol 2. 5 mg age 2 -5 yrs (5 mg > 5 yrs) (ideally oxygen driven nebuliser) Continuous or repeat 20 -30 mins
While Waiting Hospital Admission If nebs not available MDI with large-volume spacer (and mask for small kids) 1 puff every 30 -60 seconds (5 tidal breaths per puff) 10 puffs – if response poor – repeat – and switch to neb when available Monitor peak flow and Sats
Treatment when admission not required Salbutamol: 1 Puff every 30 -60 seconds up to 10 puffs via large volume spacer. (One puff at a time with 5 tidal breaths) Repeat every 10 -20 minutes according to response If good response prescribe salbutamol & spacer to be used at home as required. If history of asthma or asthma is suspected prescribe a short course of prednisolone Antibiotics where bacterial infection is suspected – usually five day.
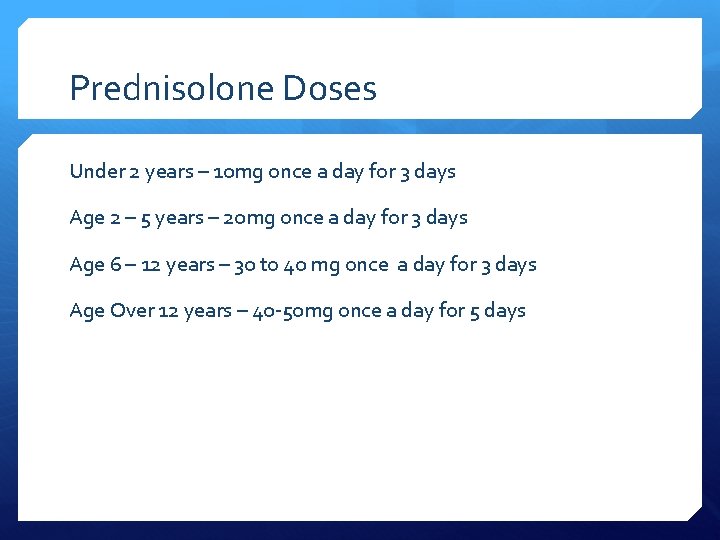
Prednisolone Doses Under 2 years – 10 mg once a day for 3 days Age 2 – 5 years – 20 mg once a day for 3 days Age 6 – 12 years – 30 to 40 mg once a day for 3 days Age Over 12 years – 40 -50 mg once a day for 5 days
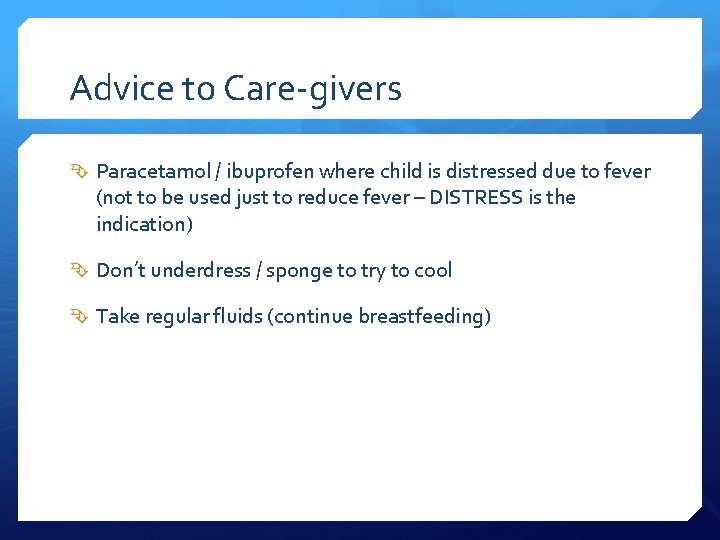
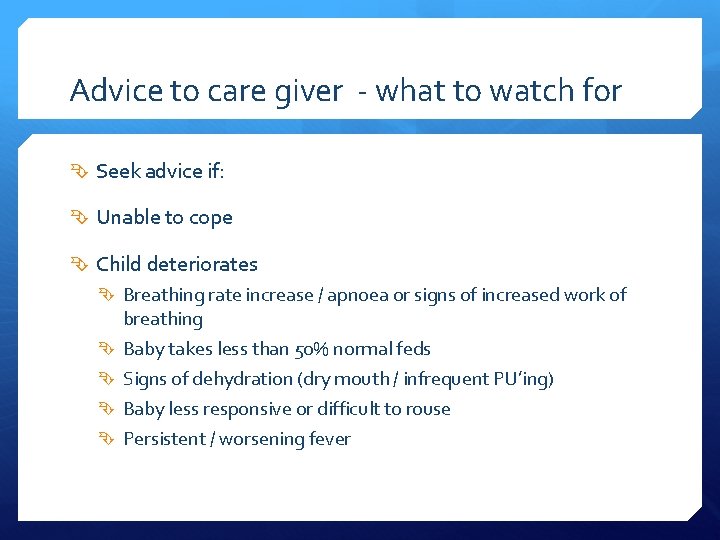
Advice to Care-givers Paracetamol / ibuprofen where child is distressed due to fever (not to be used just to reduce fever – DISTRESS is the indication) Don’t underdress / sponge to try to cool Take regular fluids (continue breastfeeding)
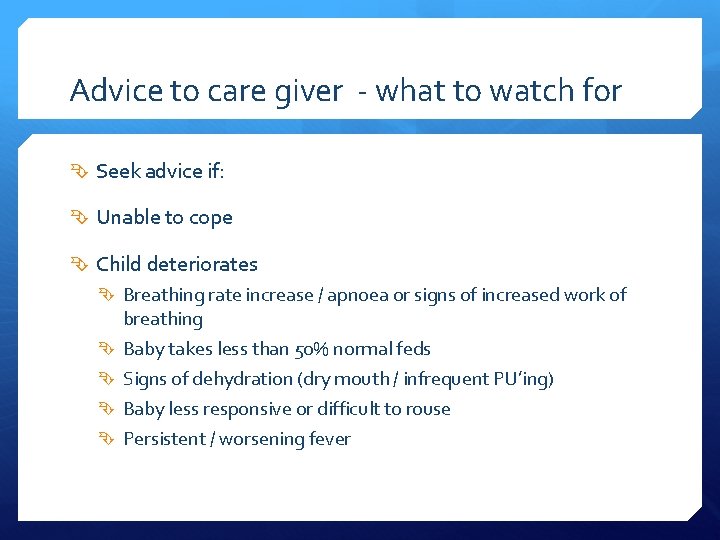
Advice to care giver - what to watch for Seek advice if: Unable to cope Child deteriorates Breathing rate increase / apnoea or signs of increased work of breathing Baby takes less than 50% normal feds Signs of dehydration (dry mouth / infrequent PU’ing) Baby less responsive or difficult to rouse Persistent / worsening fever
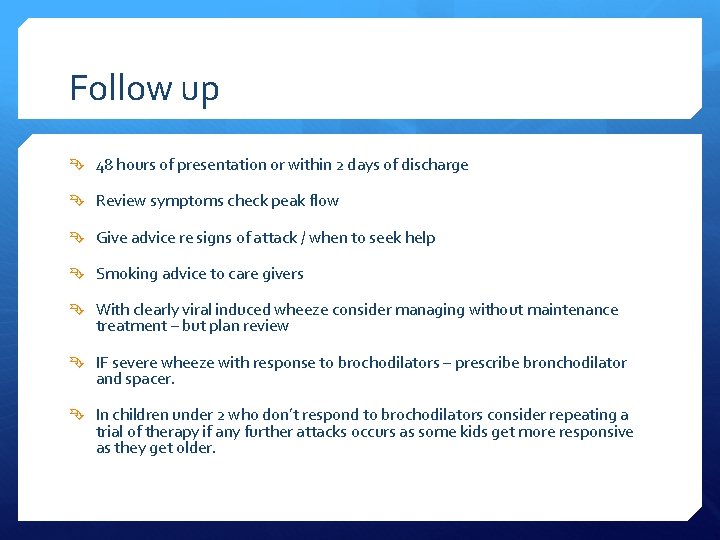
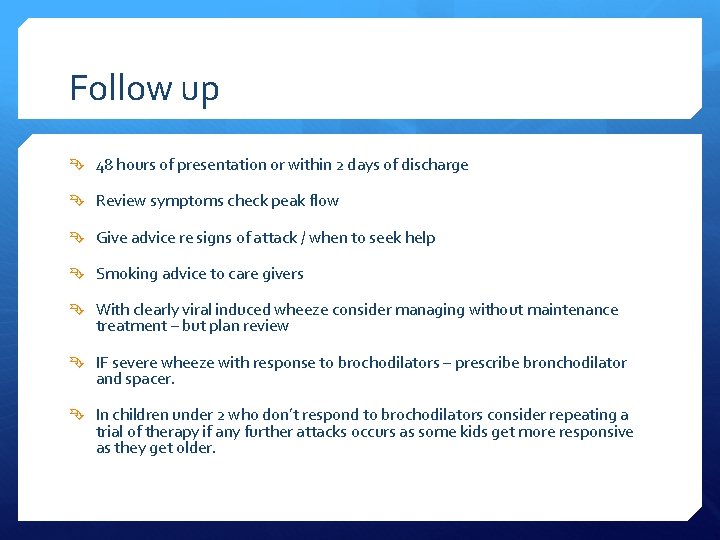
Follow up 48 hours of presentation or within 2 days of discharge Review symptoms check peak flow Give advice re signs of attack / when to seek help Smoking advice to care givers With clearly viral induced wheeze consider managing without maintenance treatment – but plan review IF severe wheeze with response to brochodilators – prescribe bronchodilator and spacer. In children under 2 who don’t respond to brochodilators consider repeating a trial of therapy if any further attacks occurs as some kids get more responsive as they get older.
Bronchiolitis
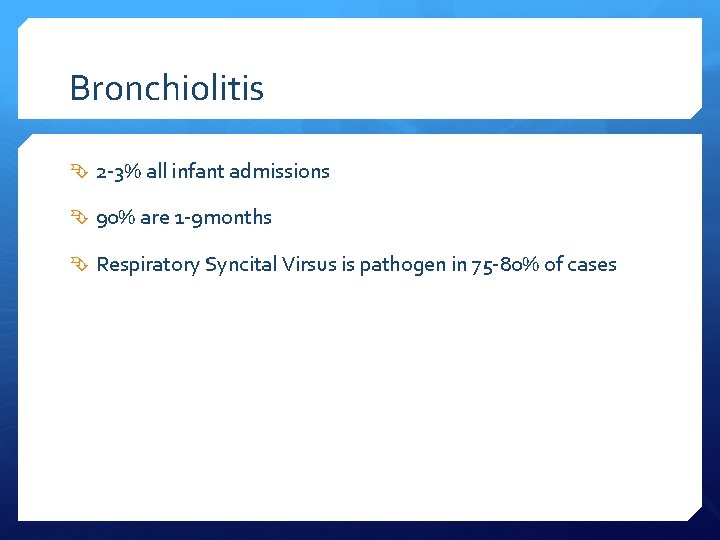
Bronchiolitis 2 -3% all infant admissions 90% are 1 -9 months Respiratory Syncital Virsus is pathogen in 75 -80% of cases
Bronchiolitis – Clinical Coryzal Symptoms initially then Dry Cough and breathlessness Often (not always) wheeze Feeding difficulty with increasing dyspnoea Recurrent apnoea is serious complication Examination findings: Sharp dry cough Tachypnoea Subcostal recession
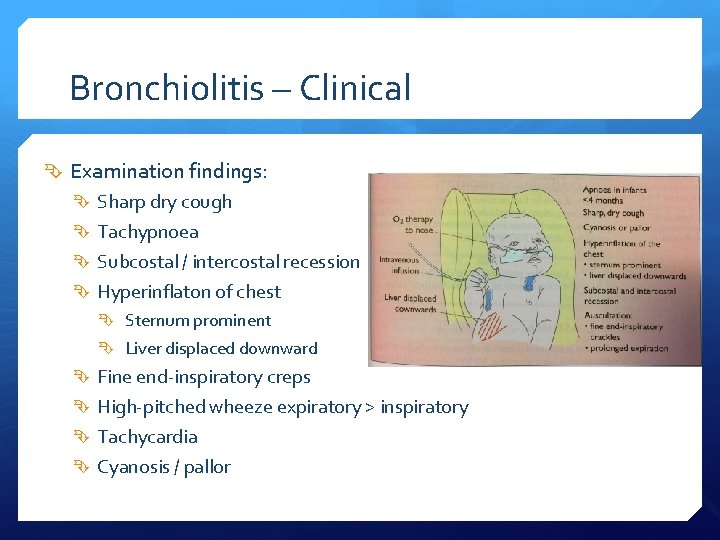
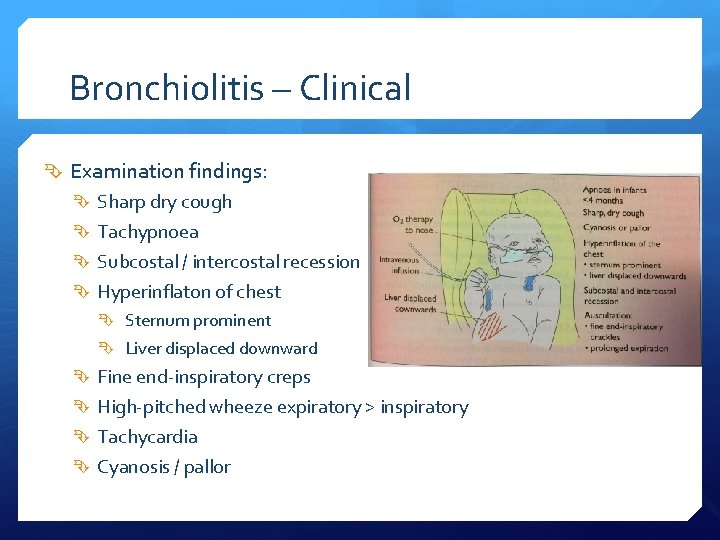
Bronchiolitis – Clinical Examination findings: Sharp dry cough Tachypnoea Subcostal / intercostal recession Hyperinflaton of chest Sternum prominent Liver displaced downward Fine end-inspiratory creps High-pitched wheeze expiratory > inspiratory Tachycardia Cyanosis / pallor
Bronchiolitis - Assessment Agitation / consciousness Signs of exhastion / cyanosis / accessory muscles Examine chest / Resp rate / pulse / bp Oxygen saturations Hydration status Cap refil / skin turgor / mucousal membranes / ascertain urine output

Bronchiolitis -999 immediate transfer Apnoea – observed or reported Child looks seriously unwell Severe respiratory distress Grunting Marked chest recession Respiratory rate > 70 breaths/min Central cyanosis O 2 Sats < 92% on air
Impending Respiratory Failure Impending respiratory failure is indicated by: Decreased respiratory effort Recurrent apnoea Failure to maintain adequate o 2 sats despite o 2 supplementation
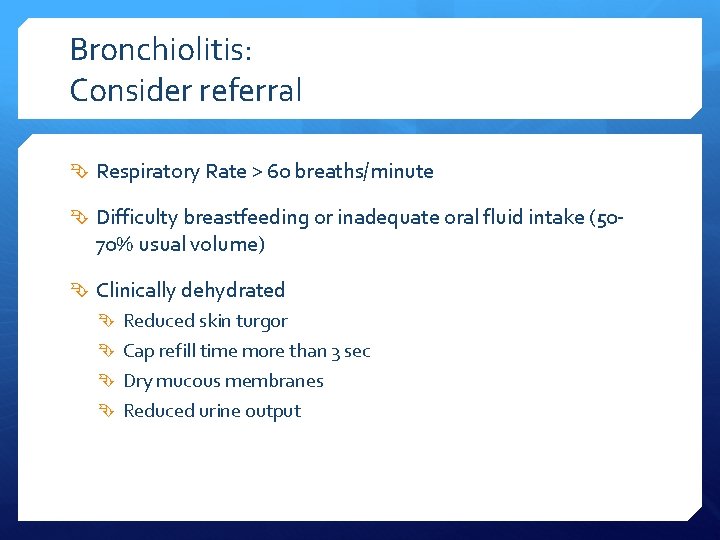
Bronchiolitis: Consider referral Respiratory Rate > 60 breaths/minute Difficulty breastfeeding or inadequate oral fluid intake (50 - 70% usual volume) Clinically dehydrated Reduced skin turgor Cap refill time more than 3 sec Dry mucous membranes Reduced urine output
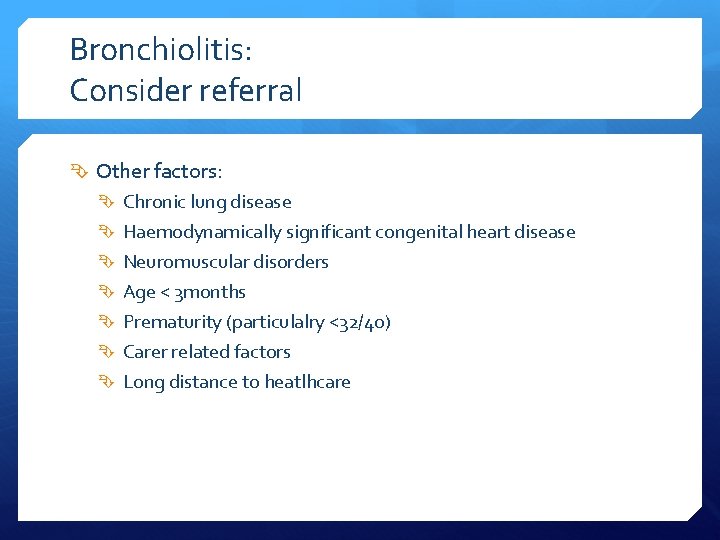
Bronchiolitis: Consider referral Other factors: Chronic lung disease Haemodynamically significant congenital heart disease Neuromuscular disorders Age < 3 months Prematurity (particulalry <32/40) Carer related factors Long distance to heatlhcare
Bronchiolitis While awaiting transfer to hospital • Give O 2 supplementation if o 2 sats are less than 92%
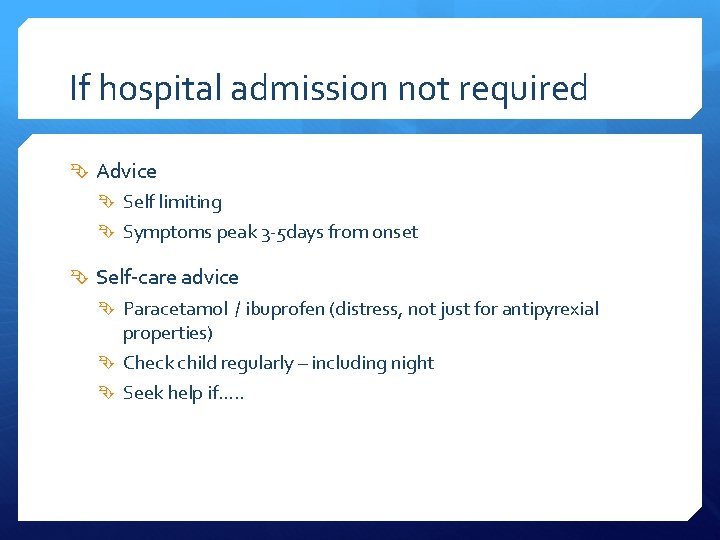
If hospital admission not required Advice Self limiting Symptoms peak 3 -5 days from onset Self-care advice Paracetamol / ibuprofen (distress, not just for antipyrexial properties) Check child regularly – including night Seek help if…. .
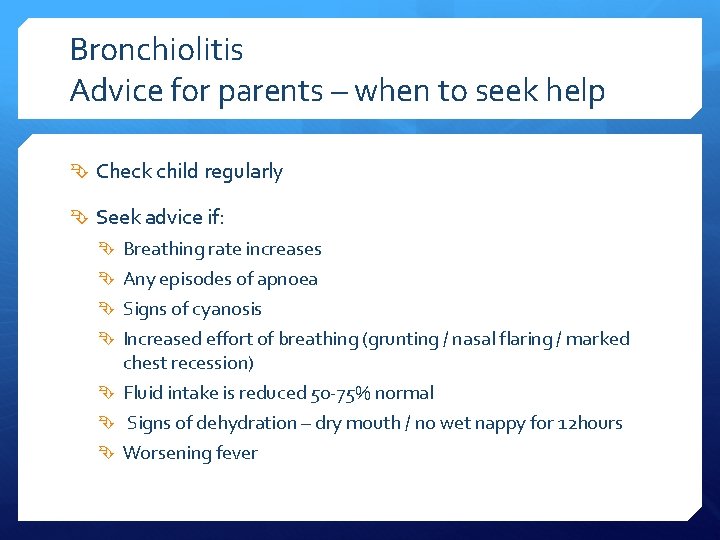
Bronchiolitis Advice for parents – when to seek help Check child regularly Seek advice if: Breathing rate increases Any episodes of apnoea Signs of cyanosis Increased effort of breathing (grunting / nasal flaring / marked chest recession) Fluid intake is reduced 50 -75% normal Signs of dehydration – dry mouth / no wet nappy for 12 hours Worsening fever
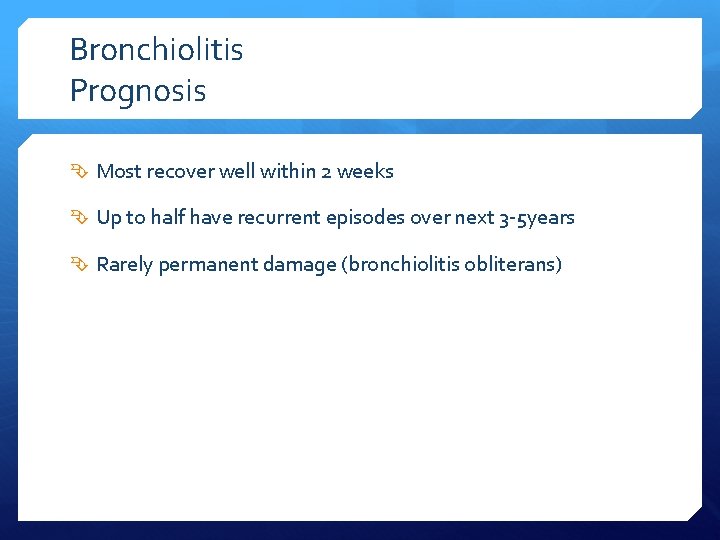
Bronchiolitis Prognosis Most recover well within 2 weeks Up to half have recurrent episodes over next 3 -5 years Rarely permanent damage (bronchiolitis obliterans)
Bronchiolitis Advice / Follow up Advise against smoking Decide whether follow up is necessary
Croup
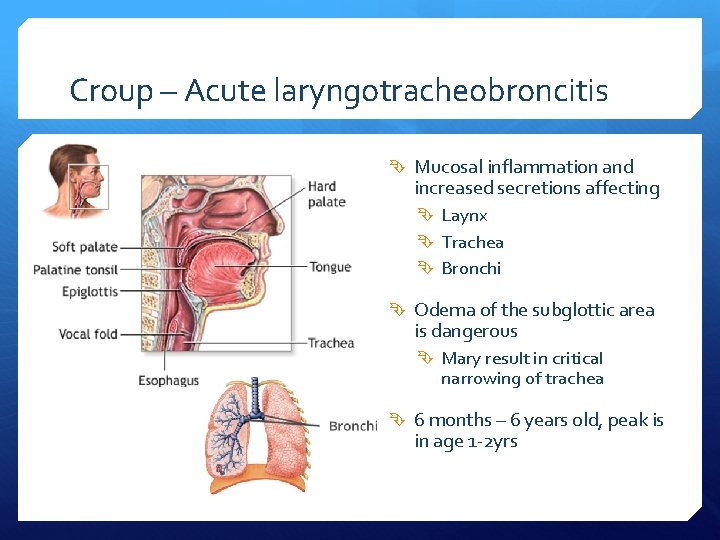
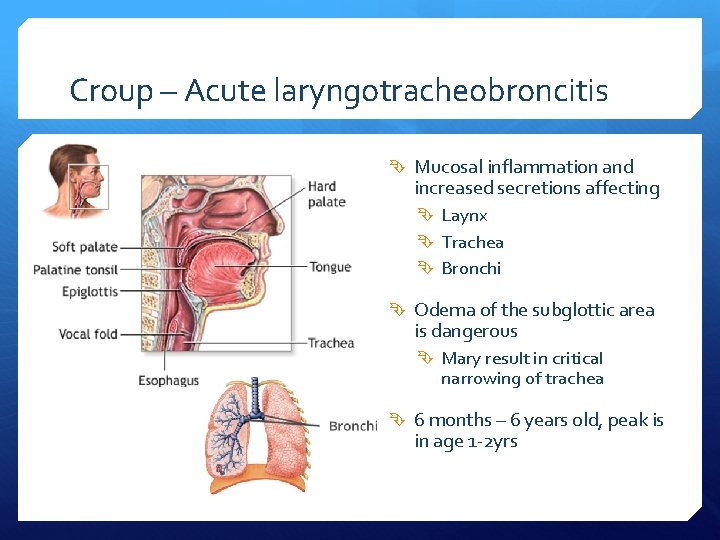
Croup – Acute laryngotracheobroncitis Mucosal inflammation and increased secretions affecting Laynx Trachea Bronchi Odema of the subglottic area is dangerous Mary result in critical narrowing of trachea 6 months – 6 years old, peak is in age 1 -2 yrs
Croup Mild fever Hoarse voice Barking cough Stridor
Croup – Assessment Mild Moderate Severe NB: Impending respiratory failure may develop regardless of the severity of the symptoms!!
Croup - Assessment Mild: Occasional barking cough No audible stridor at rest No or mild suprasternal/intercostal recession Child is happy and eats / drinks / plays
Croup - Assessment Moderate Frequent barking cough and easily audible stridor at rest Suprasternal and sternal wall retraction at rest No or little distress/agitation Child can be placated and is intersted in surroundings
Croup - Assessment Severe Frequent barking cough Prominent inspiratory (occasionaly expiratory) stridor at rest Mark sternal recession Significant distress agitation Or lethargy or restlessness (hypoxaemia) Tachycardia occurs with more sever obstructin symptoms and hypoxaemia
Croup – beware! Impending respiratory failure may develop regardless of the severity of the symptoms. I If there is any of the following – they override other signs: Change in mental state (lethargy / listlessnesss / decrease level of consciousness) Pallor Dusky appearance Tachycardia
With Impending respiratory failure breathing may be laboured a barking cough may not be prominent stridor at rest may be hard to hear Chest wall recession may not be marked A child who appears to be deterioration but whose stridor appears to be improving has worsening airway obstruction and is at high risk of complete obstruction
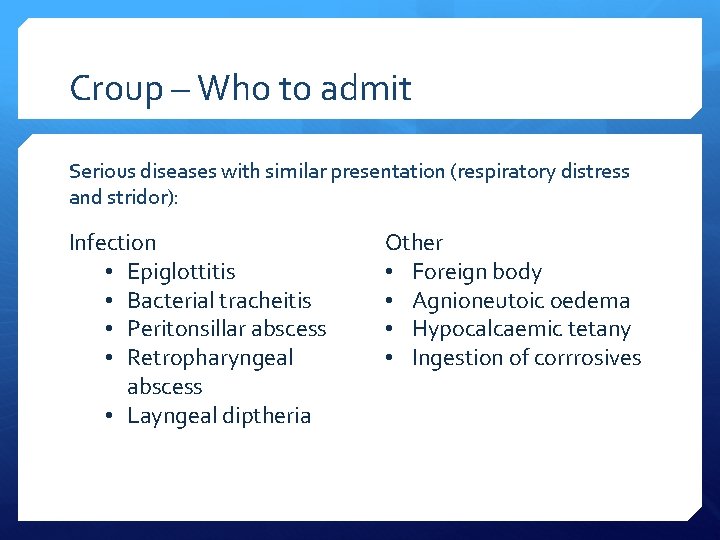
Croup – Who to admit Serious diseases with similar presentation (respiratory distress and stridor): Infection • Epiglottitis • Bacterial tracheitis • Peritonsillar abscess • Retropharyngeal abscess • Layngeal diptheria Other • Foreign body • Agnioneutoic oedema • Hypocalcaemic tetany • Ingestion of corrrosives
Croup – who to admit Moderate croup Severe croup Impending respiratory failure
Croup – Who to admit Also consider admission in children with history of Severe obstruction Previous serious croup Known structural upper airway abnormalities Laryngomalacia / tracheomalacia / vascular ring / Down’s
Croup - Also admit: Less than 6 months infant Immunocompromised Inadequate fluid intake / refusing liquids Poor response to treatment Uncertain diagnosis
Croup - Also admit: Others: Significant parental anxiety late evening or night presentation Home long distance away No transport
Treatment Dexamethasone 0. 15 mg / kg orally 1. 5 mg – 2 mg for 12 -15 months 2 – 3 mg for 3 -4 years or Oral prednisolone 1 -2 mg / kg Second dose if symptoms are still present next day
Croup - Advice for Parents Explain: Croup is self limiting Symptoms usually resolve in 48 hours (may last 1 week) Usually followed by URTI Use paracetamol to control pain / fever Don’t under/over dress child with fever Don’t tepid sponge Don’t give antipyretics with sole aim of reducing temp
Croup - Advice for Parents Ensure adequate fluid intake Do not advise humidified air (steam) ✕
Croup See child within a few hours (face to face or by phone) Advice to seek urgent medical review if: Progression milt to moderate (development of intermittent stridor at rest / increased effort) Child becomes toxic (pale / very high fever / tachycardic) – as child may have alternative diagnosis Call 999 if: Child become cyanosied Unusually sleepy Struggling to breath
Croup – Advice to parents Cough medicine Decongestants Beta-agnosist Antibiotics – croup is usually viral DON’T WORK!!