RESPIRATORY SYSTEM RESPIRATORY FUNCTIONS MECHANICS OF RESPIRATORY SYSTEM


![LUNG VOLUMES INSPIRATORY RESERVE VOLUME maximal inspiratory level [l ] IRV ~2. 5 end LUNG VOLUMES INSPIRATORY RESERVE VOLUME maximal inspiratory level [l ] IRV ~2. 5 end](https://slidetodoc.com/presentation_image_h2/7717f57ff690341ee7038bd3f32aee8e/image-10.jpg)




- Slides: 33
RESPIRATORY SYSTEM RESPIRATORY FUNCTIONS MECHANICS OF RESPIRATORY SYSTEM GAS TRANSPORT Author of presentation: doc. MUDr. Milena Šimurdová, CSc. STOMATOLOGY
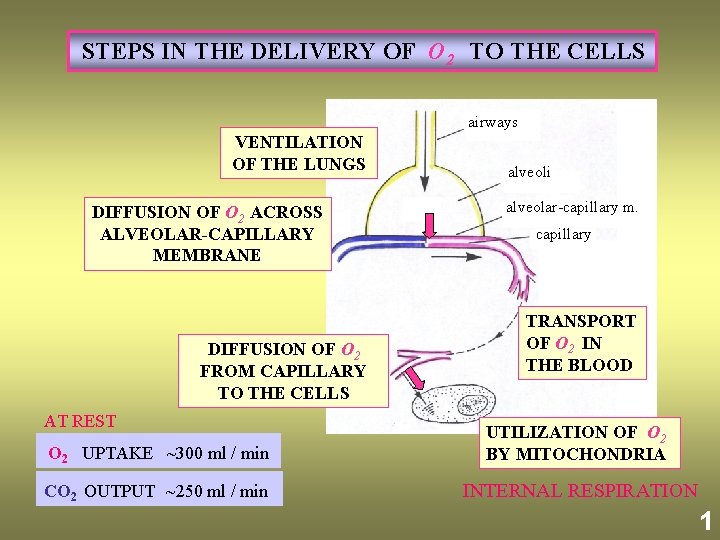
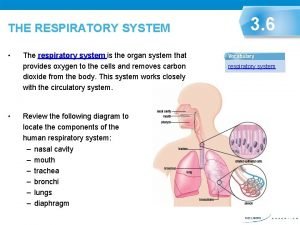
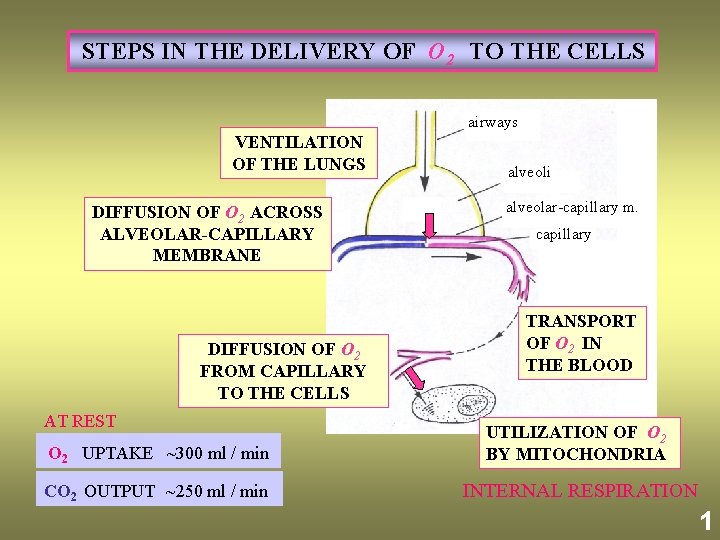
STEPS IN THE DELIVERY OF O 2 TO THE CELLS airways VENTILATION OF THE LUNGS DIFFUSION OF O 2 ACROSS ALVEOLAR-CAPILLARY MEMBRANE DIFFUSION OF O 2 FROM CAPILLARY TO THE CELLS AT REST alveoli alveolar-capillary m. capillary TRANSPORT OF O 2 IN THE BLOOD O 2 UPTAKE ~300 ml / min UTILIZATION OF O 2 BY MITOCHONDRIA CO 2 OUTPUT ~250 ml / min INTERNAL RESPIRATION 1

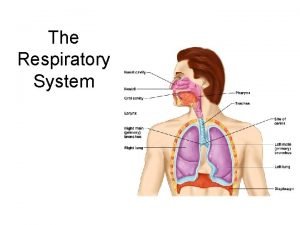
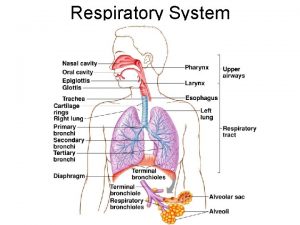
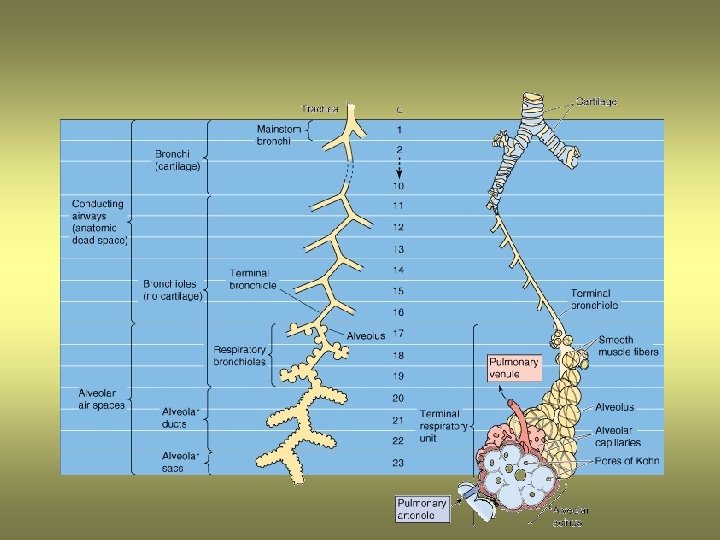
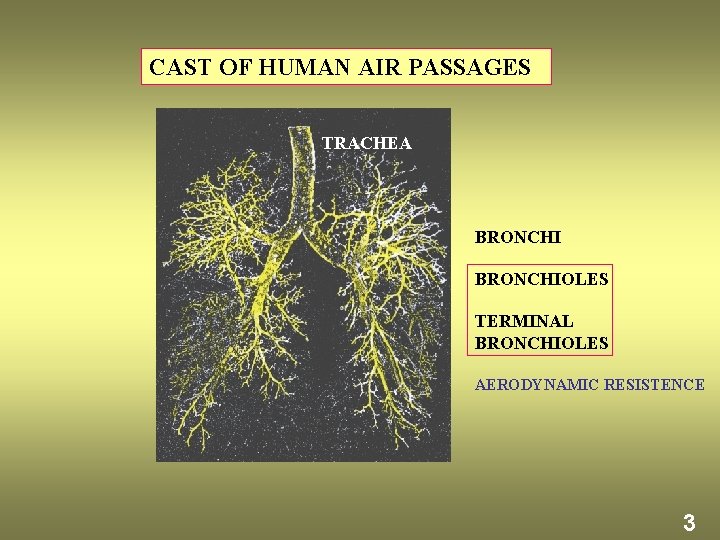
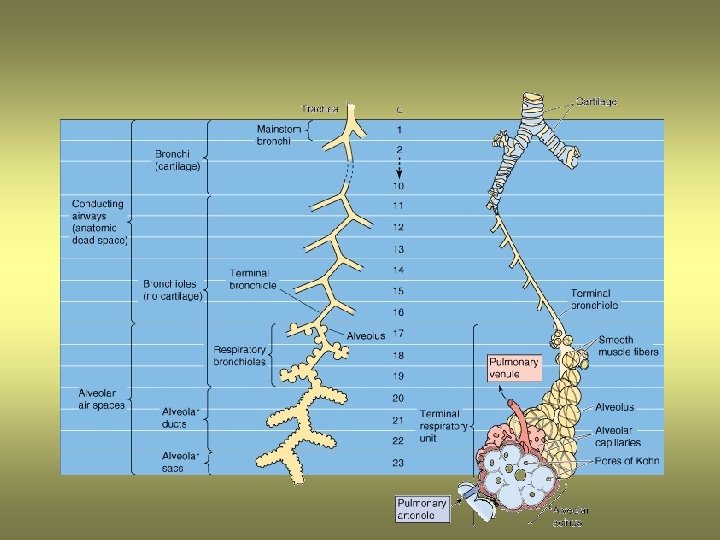
AIR PASSAGES ANATOMICAL DEAD SPACE –CONDUCTING ZONE NASAL PASSAGES PHARYNX Other physiological functions: LARYNX air is warmed, cleaned and takes up water vapour respiratory reflex responses to the irritants TRACHEA speech and singing (function of larynx) BRONCHIOLES TERMINAL BRONCHIOLES RESPIRATORY ZONE (GAS EXCHANGE) Total alveolar area ~100 m 2 2
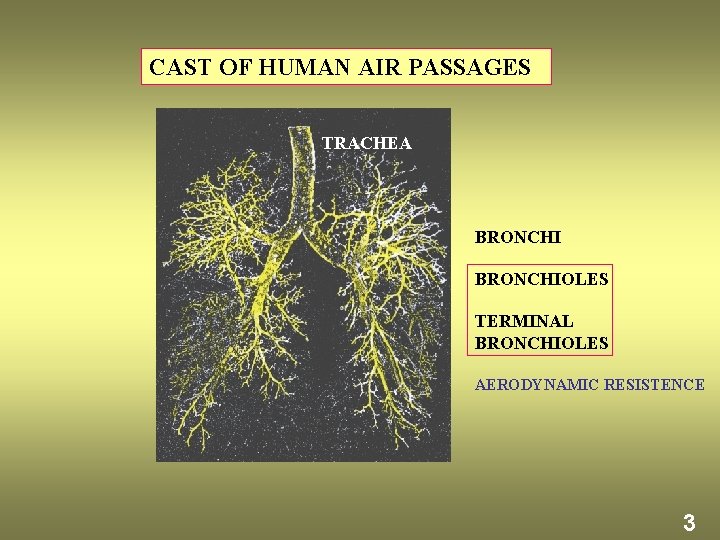
CAST OF HUMAN AIR PASSAGES TRACHEA BRONCHIOLES TERMINAL BRONCHIOLES AERODYNAMIC RESISTENCE 3
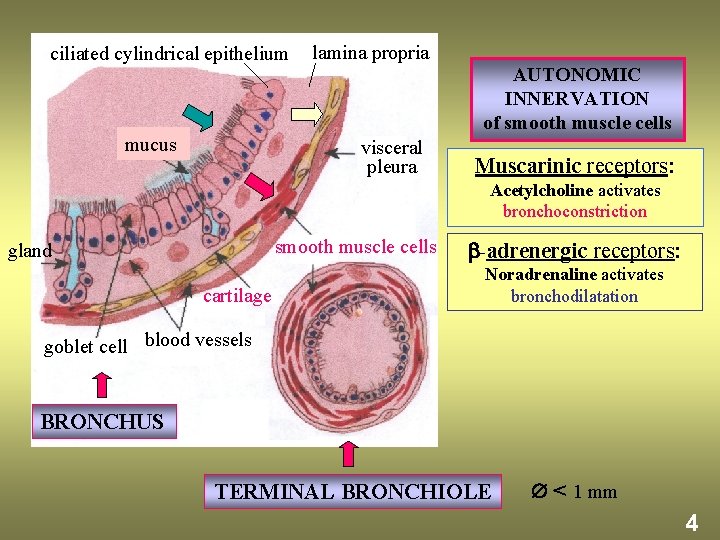
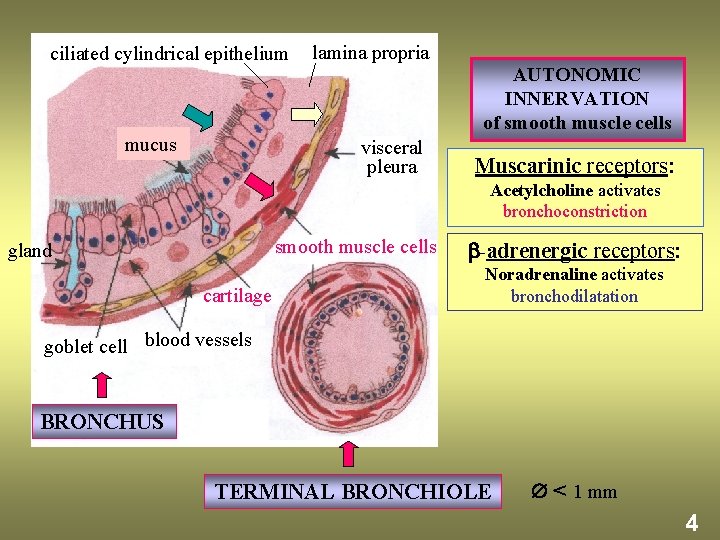
ciliated cylindrical epithelium mucus lamina propria AUTONOMIC INNERVATION of smooth muscle cells visceral pleura Muscarinic receptors: Acetylcholine activates bronchoconstriction smooth muscle cells gland cartilage -adrenergic receptors: Noradrenaline activates bronchodilatation goblet cell blood vessels BRONCHUS TERMINAL BRONCHIOLE < 1 mm 4

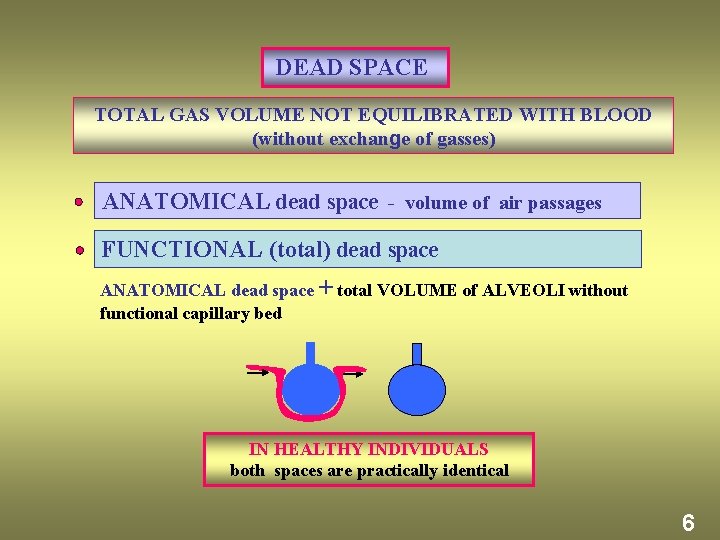
VT tidal volume VT = VA + VD ~ 500 ml VA part of tidal volume entering alveoli ~ 350 ml VD part of tidal volume remaining in the dead space ~ 150 ml f = 12/min ∙ V = VT x f PULMONARY MINUTE VENTILATION 6 l/min · VA = VA x f ALVEOLAR VENTILATION 4. 2 l/min · VD = VD x f DEAD SPACE VENTILATION 1. 8 l/min 5
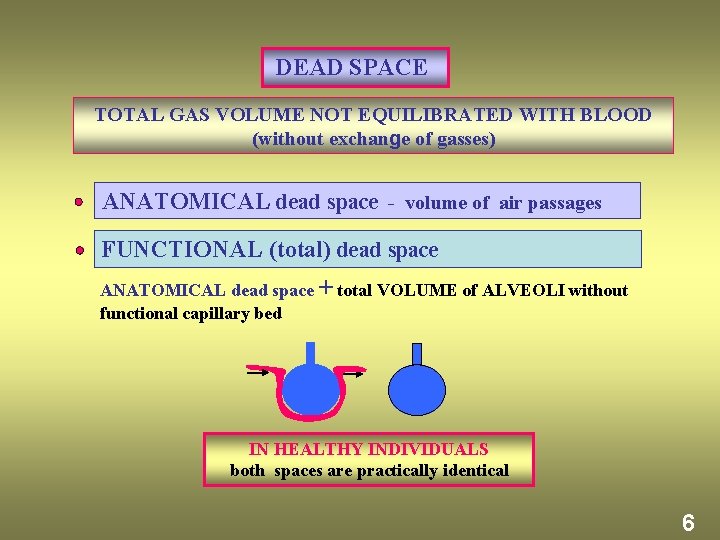
DEAD SPACE TOTAL GAS VOLUME NOT EQUILIBRATED WITH BLOOD (without exchange of gasses) ANATOMICAL dead space - volume of air passages FUNCTIONAL (total) dead space ANATOMICAL dead space + total VOLUME of ALVEOLI without functional capillary bed IN HEALTHY INDIVIDUALS both spaces are practically identical 6
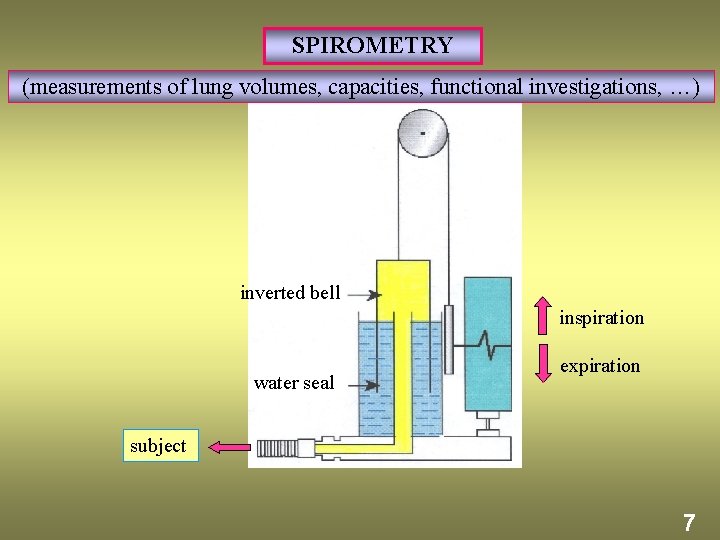
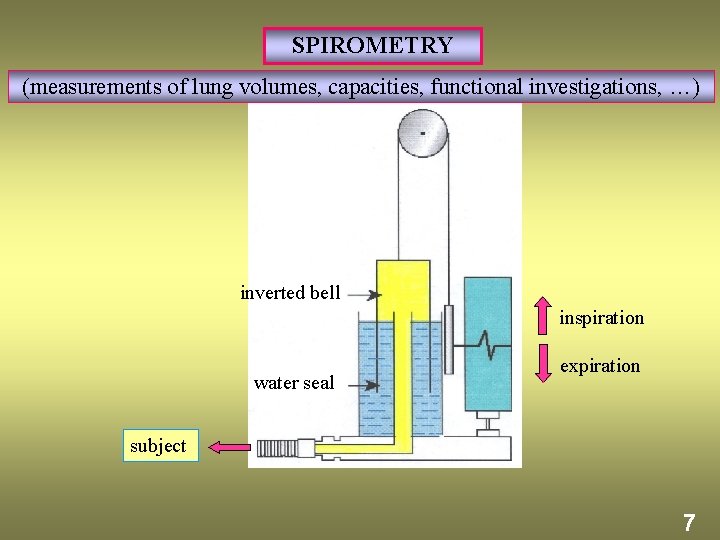
SPIROMETRY (measurements of lung volumes, capacities, functional investigations, …) inverted bell inspiration water seal expiration subject 7
![LUNG VOLUMES INSPIRATORY RESERVE VOLUME maximal inspiratory level l IRV 2 5 end LUNG VOLUMES INSPIRATORY RESERVE VOLUME maximal inspiratory level [l ] IRV ~2. 5 end](https://slidetodoc.com/presentation_image_h2/7717f57ff690341ee7038bd3f32aee8e/image-10.jpg)
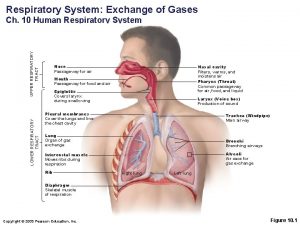
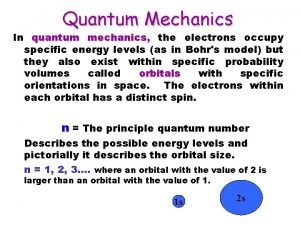
LUNG VOLUMES INSPIRATORY RESERVE VOLUME maximal inspiratory level [l ] IRV ~2. 5 end of quiet inspiration TIDAL VOLUME VT EXPIRATORY RESERVE VOLUME ERV He RV ~1. 7 maximal expiratory level ~1. 3 RESIDUAL VOLUME RV DILUTION METHOD end of quiet expiration Principle of method: 1 Maximal expiration, 2 Repeated inspiration from and expiration into a reservoir (known volume Vr) with inert gas He (known concentration ci) Equilibration of the air in the residual volume and reservoir He ci reservoir (Vr) 3 Calculation of residual volume RV from the initial and final He concentrations in reservoir (ci , cf). RV He cf reservoir (V) 8
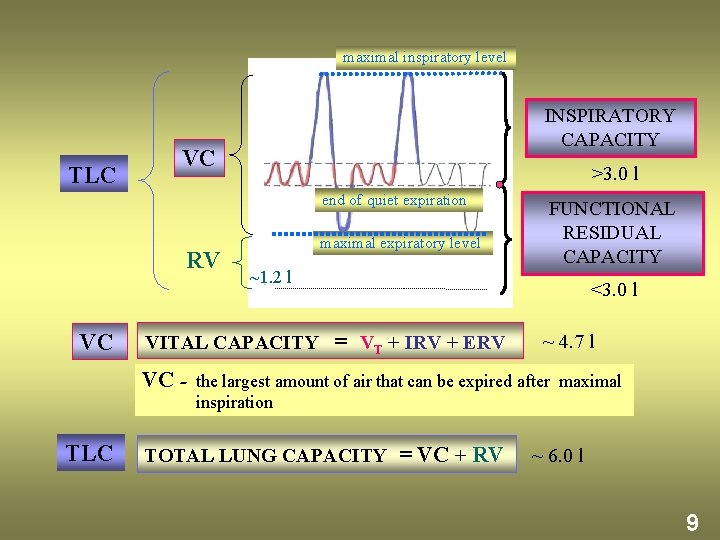
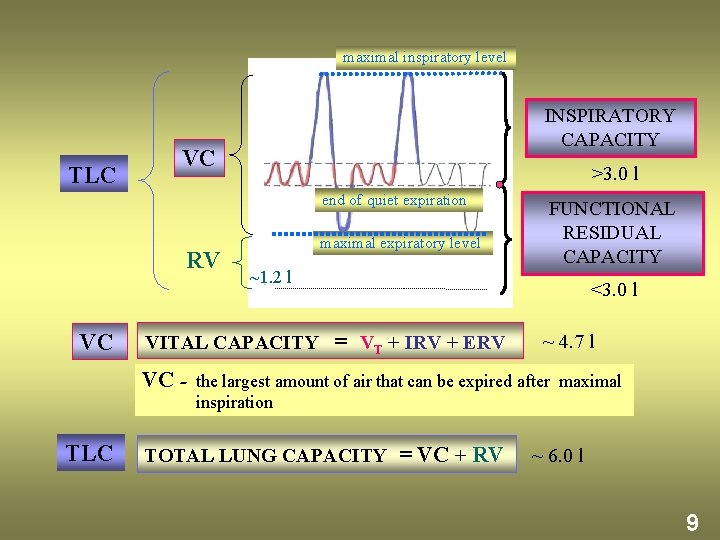
maximal inspiratory level TLC INSPIRATORY CAPACITY VC >3. 0 l end of quiet expiration RV VC maximal expiratory level ~1. 2 l VITAL CAPACITY FUNCTIONAL RESIDUAL CAPACITY <3. 0 l = VT + IRV + ERV ~ 4. 7 l VC - the largest amount of air that can be expired after maximal inspiration TLC TOTAL LUNG CAPACITY = VC + RV ~ 6. 0 l 9
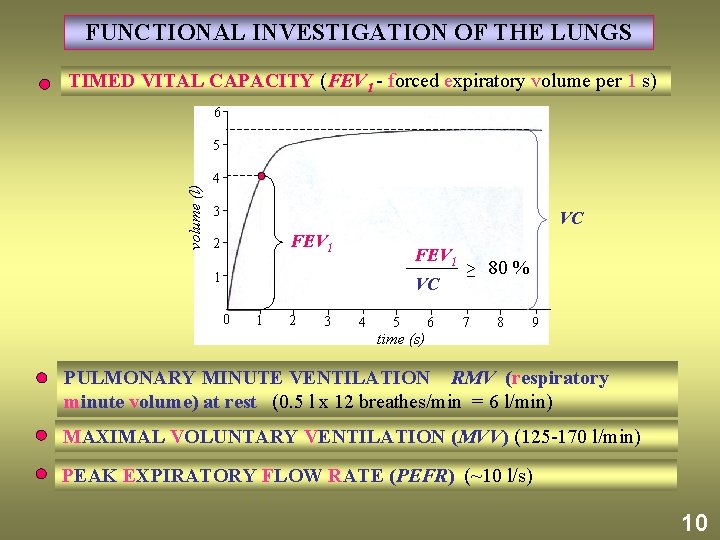
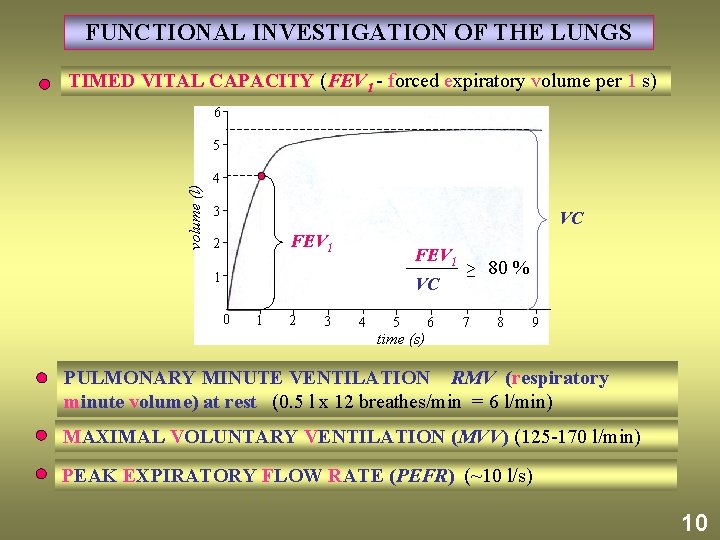
FUNCTIONAL INVESTIGATION OF THE LUNGS TIMED VITAL CAPACITY (FEV 1 - forced expiratory volume per 1 s) 6 volume (l) 5 4 3 VC FEV 1 2 FEV 1 1 VC 0 1 2 3 4 5 time (s) 6 ≥ 80 % 7 8 9 PULMONARY MINUTE VENTILATION RMV (respiratory minute volume) at rest (0. 5 l x 12 breathes/min = 6 l/min) MAXIMAL VOLUNTARY VENTILATION (MVV) (125 -170 l/min) PEAK EXPIRATORY FLOW RATE (PEFR) (~10 l/s) 10
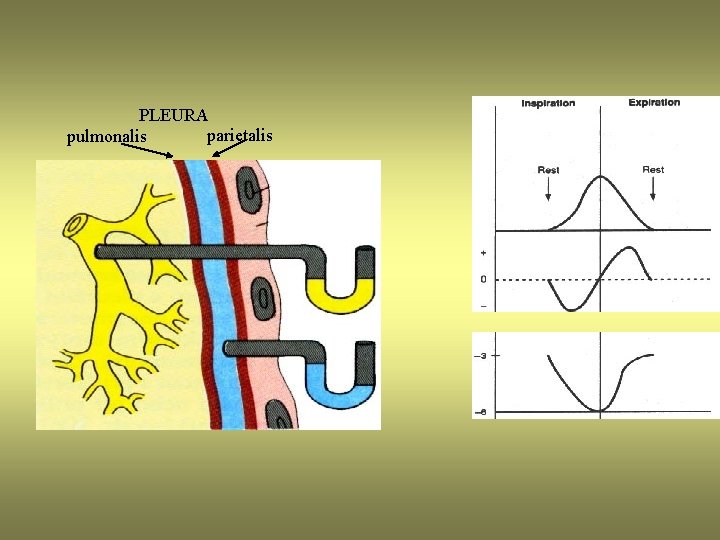
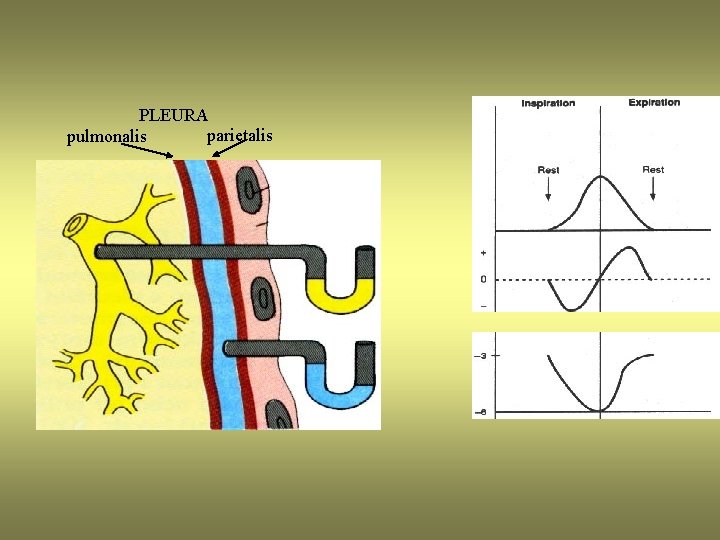
PLEURA parietalis pulmonalis
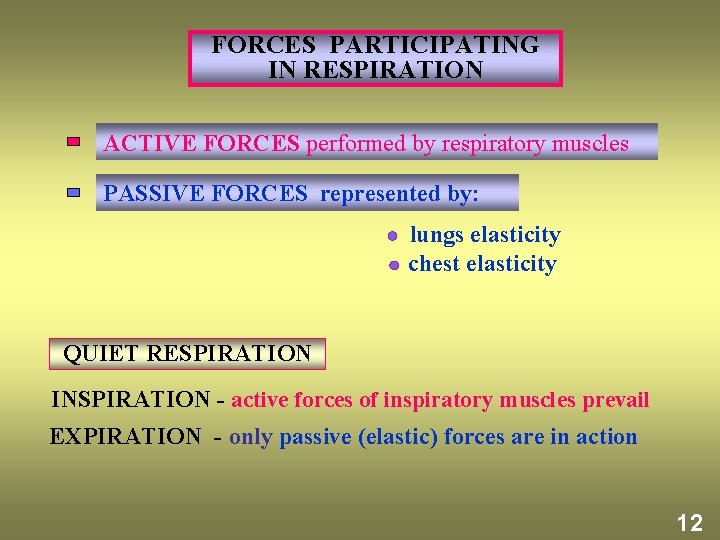
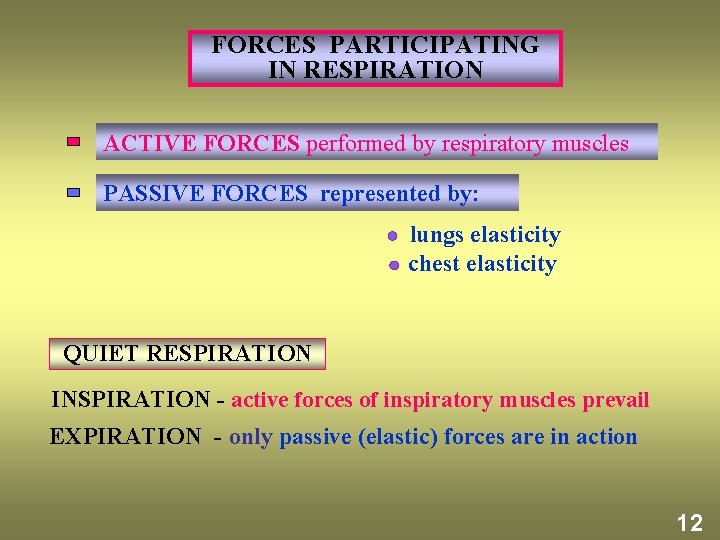
FORCES PARTICIPATING IN RESPIRATION ACTIVE FORCES performed by respiratory muscles PASSIVE FORCES represented by: lungs elasticity chest elasticity QUIET RESPIRATION INSPIRATION - active forces of inspiratory muscles prevail EXPIRATION - only passive (elastic) forces are in action 12

RESPIRATORY MUSCLES accessory muscles external intercostals internal intercostals INSPIRATORY EXPIRATORY diaphragm abdominal muscles 13
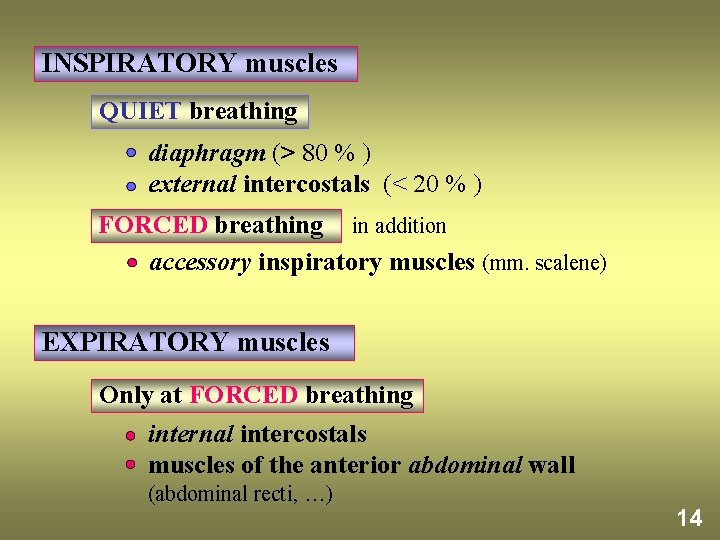
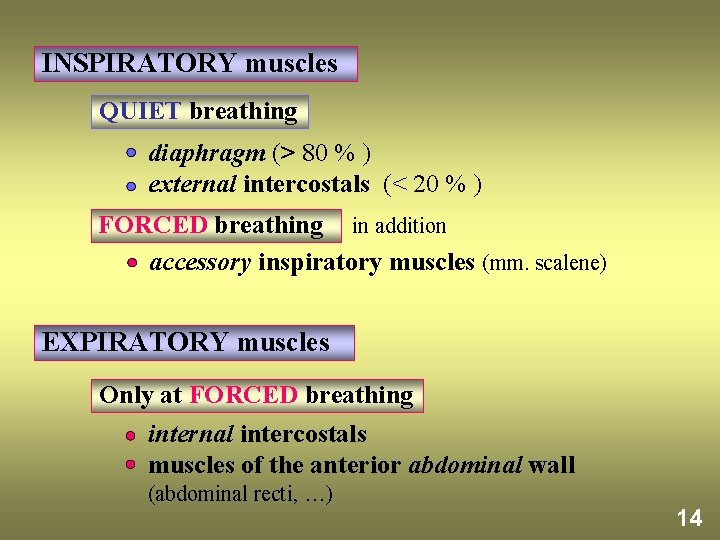
INSPIRATORY muscles QUIET breathing diaphragm (> 80 % ) external intercostals (< 20 % ) FORCED breathing in addition accessory inspiratory muscles (mm. scalene) EXPIRATORY muscles Only at FORCED breathing internal intercostals muscles of the anterior abdominal wall (abdominal recti, …) 14
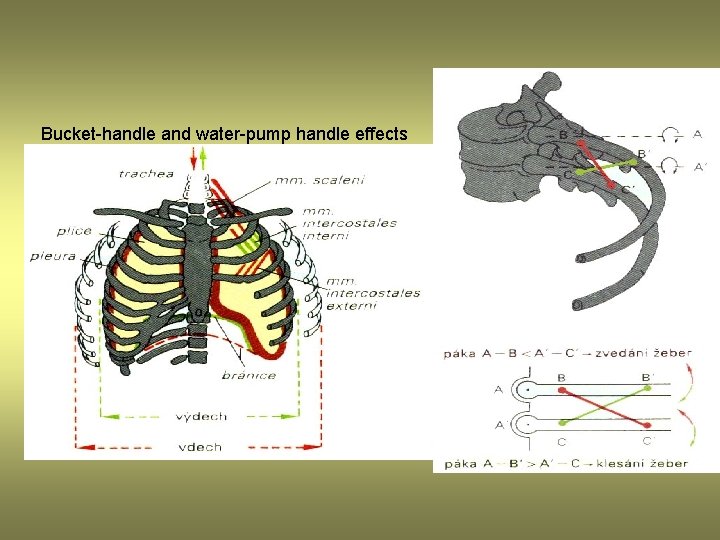
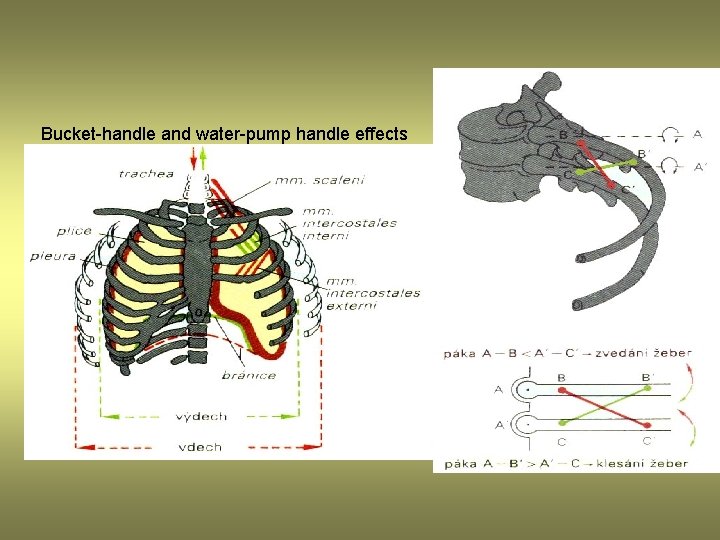
Bucket-handle and water-pump handle effects

LAW OF LAPLACE spherical structures r 2 T P= r P T P pressure r radius T surface tension ? P 1 P 2 P 1 > P 2 PATHOLOGY COLLAPSE OF ALVEOLI - ATELECTASIS EXPANSION OF ALVEOLI 16
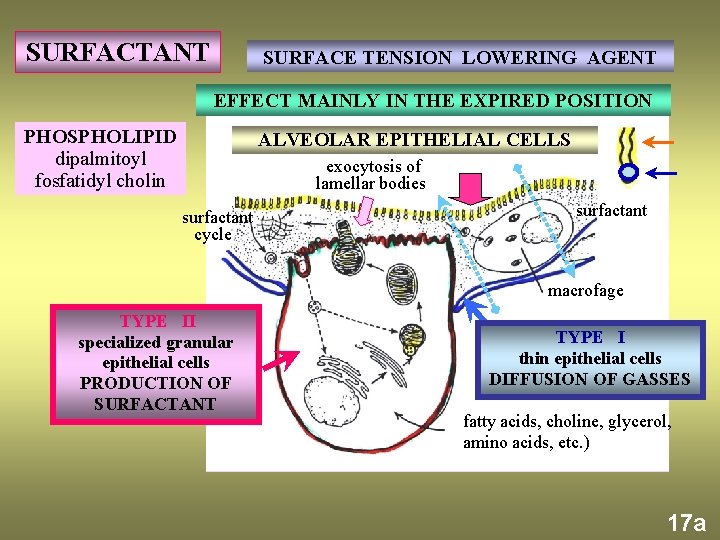
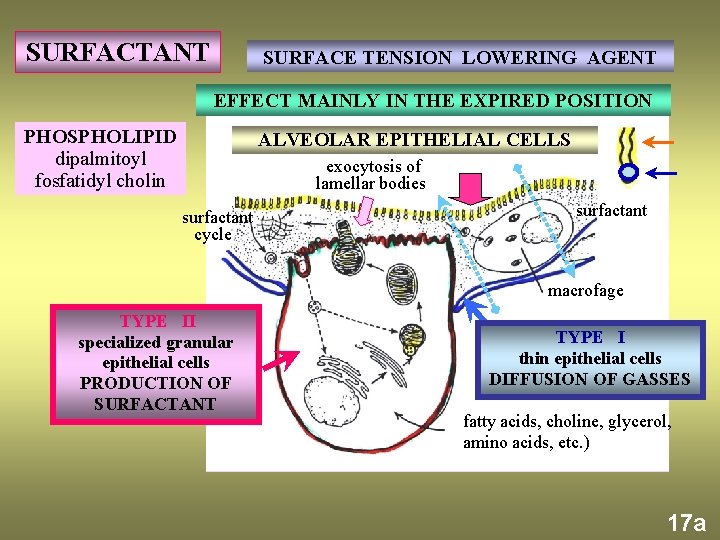
SURFACTANT SURFACE TENSION LOWERING AGENT EFFECT MAINLY IN THE EXPIRED POSITION PHOSPHOLIPID dipalmitoyl fosfatidyl cholin ALVEOLAR EPITHELIAL CELLS exocytosis of lamellar bodies surfactant cycle surfactant macrofage TYPE II specialized granular epithelial cells PRODUCTION OF SURFACTANT TYPE I thin epithelial cells DIFFUSION OF GASSES fatty acids, choline, glycerol, amino acids, etc. ) 17 a
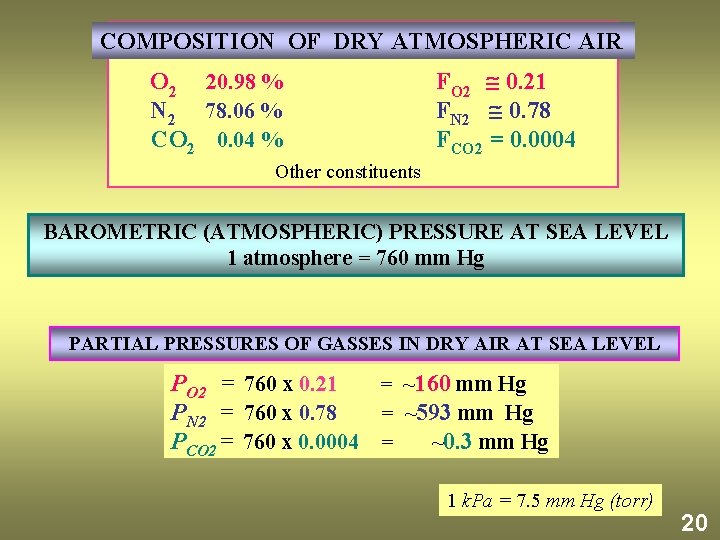
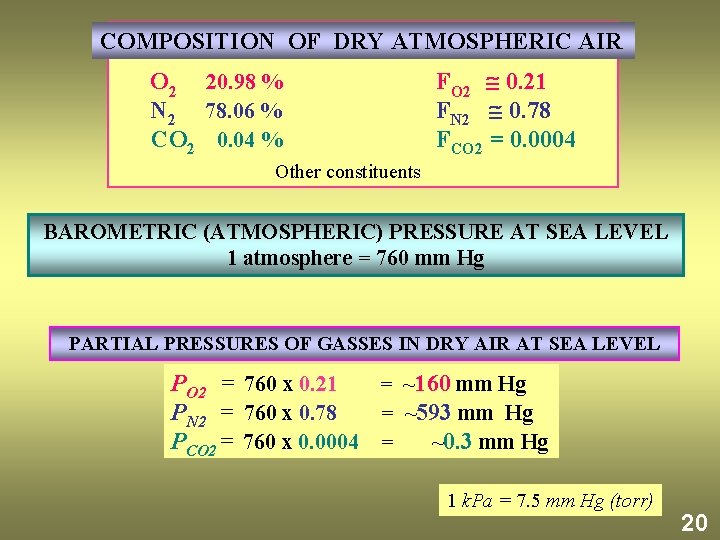
COMPOSITION OF DRY ATMOSPHERIC AIR O 2 20. 98 % N 2 78. 06 % CO 2 0. 04 % FO 2 0. 21 FN 2 0. 78 FCO 2 = 0. 0004 Other constituents BAROMETRIC (ATMOSPHERIC) PRESSURE AT SEA LEVEL 1 atmosphere = 760 mm Hg PARTIAL PRESSURES OF GASSES IN DRY AIR AT SEA LEVEL PO 2 = 760 x 0. 21 = ~160 mm Hg PN 2 = 760 x 0. 78 = ~593 mm Hg PCO 2 = 760 x 0. 0004 = ~0. 3 mm Hg 1 k. Pa = 7. 5 mm Hg (torr) 20
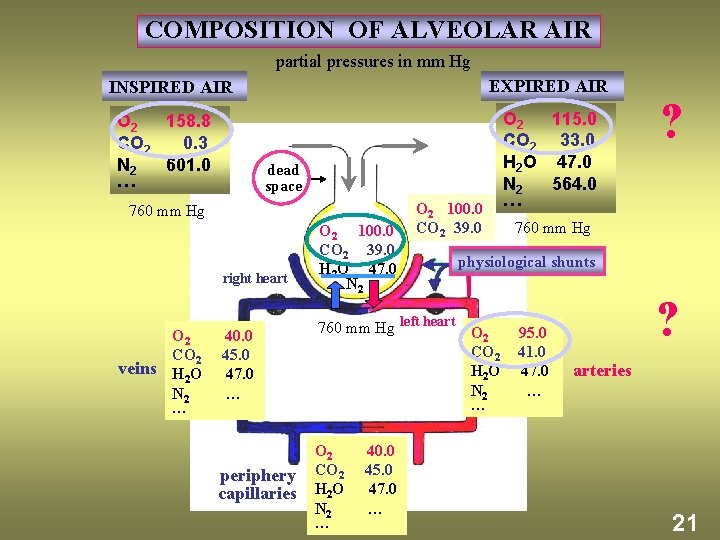
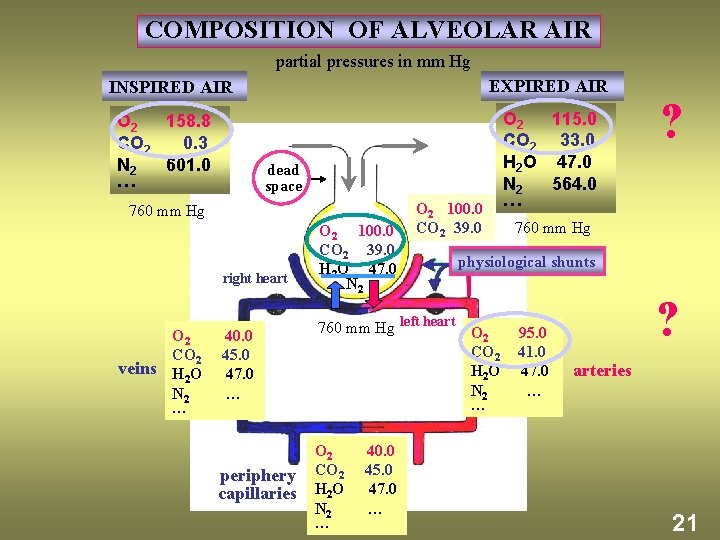
COMPOSITION OF ALVEOLAR AIR partial pressures in mm Hg EXPIRED AIR INSPIRED AIR O 2 158. 8 CO 2 0. 3 N 2 601. 0 … dead space 760 mm Hg right heart O 2 CO 2 veins H O 2 N 2 … O 2 100. 0 CO 2 39. 0 H 2 O 47. 0 N 2 O 2 100. 0 CO 2 39. 0 ? 760 mm Hg physiological shunts 40. 0 45. 0 47. 0 … 760 mm Hg left heart O 2 CO 2 H 2 O N 2 … periphery capillaries O 2 CO 2 H 2 O N 2 … 40. 0 45. 0 47. 0 … O 2 115. 0 CO 2 33. 0 H 2 O 47. 0 N 2 564. 0 … 95. 0 41. 0 47. 0 … ? arteries 21

ALVEOLAR-CAPILLARY (RESPIRATORY) MEMBRANE DIFFUSION OF GASES alveolar epithelial cell nucleus RED BLOOD CELL ALVEOLAR AIR PO 2 = 100 PCO 2 = 39 (mm Hg) O 2 CO 2 ALVEOLAR-CAPILLARY (RESPIRATORY) MEMBRANE interstitial space O 2 Hb Hb. O 2 capillary endothelial cell nucleus PULMONARY CAPILLARY diameter about 5 µm CO 2 ~1 µm 0. 75 s time interval of erythrocyte contact with respiratory membrane at rest 23
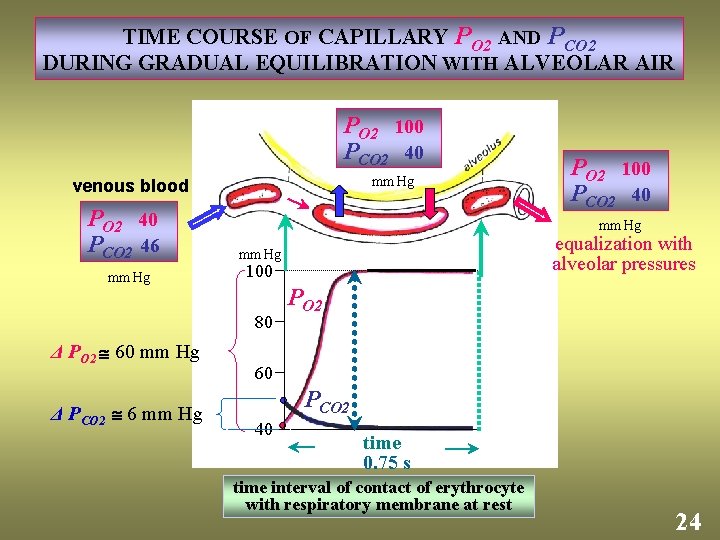
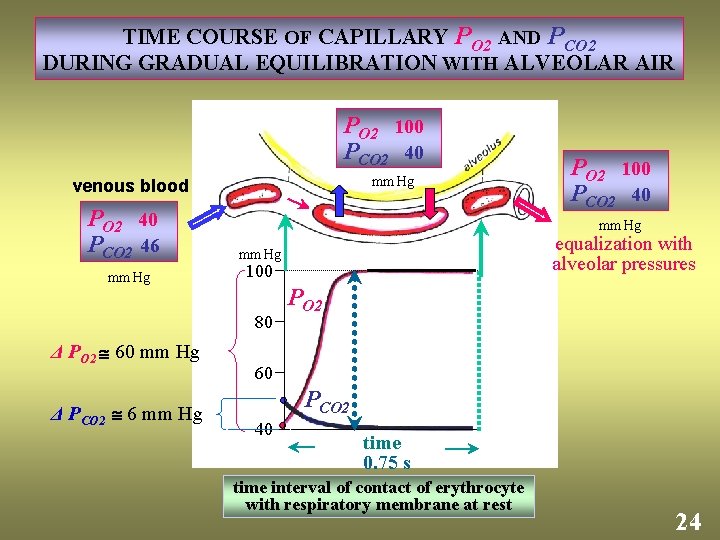
TIME COURSE OF CAPILLARY PO 2 AND PCO 2 DURING GRADUAL EQUILIBRATION WITH ALVEOLAR AIR PO 2 100 PCO 2 40 mm Hg venous blood PO 2 40 PCO 2 46 mm Hg Δ PCO 2 6 mm Hg equalization with alveolar pressures mm Hg 100 80 Δ PO 2 60 mm Hg PO 2 100 PCO 2 40 PO 2 60 PCO 2 40 time 0. 75 s time interval of contact of erythrocyte with respiratory membrane at rest 24
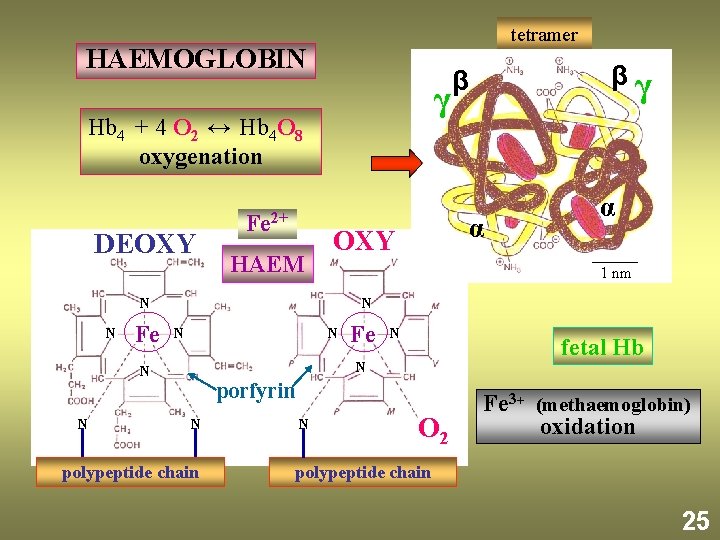
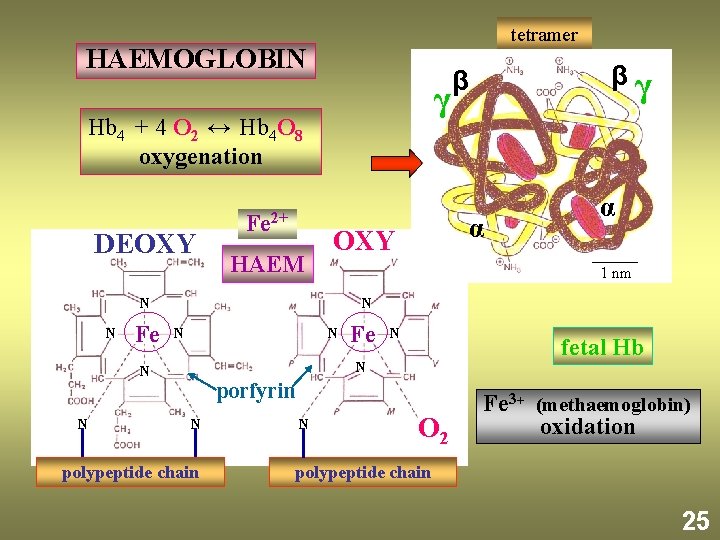
tetramer HAEMOGLOBIN γ Hb 4 + 4 O 2 ↔ Hb 4 O 8 oxygenation DEOXY Fe 2+ HAEM Fe α 1 nm N N N Fe N fetal Hb N N N α OXY N N βγ β porfyrin N polypeptide chain N O 2 Fe 3+ (methaemoglobin) oxidation polypeptide chain 25
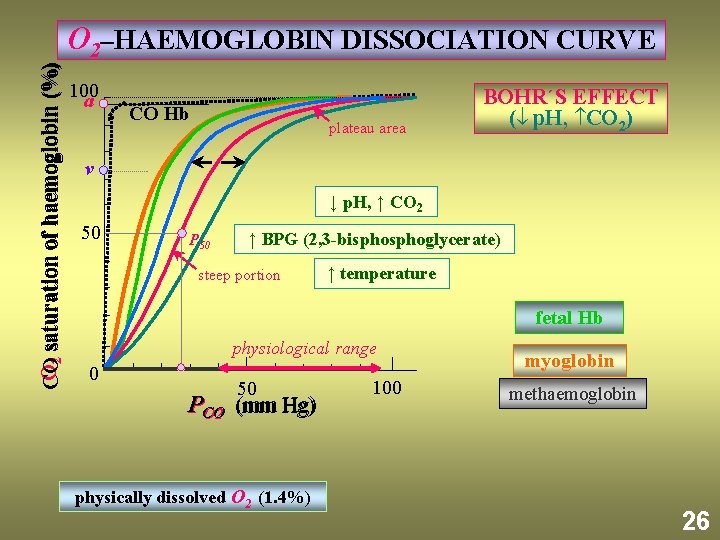
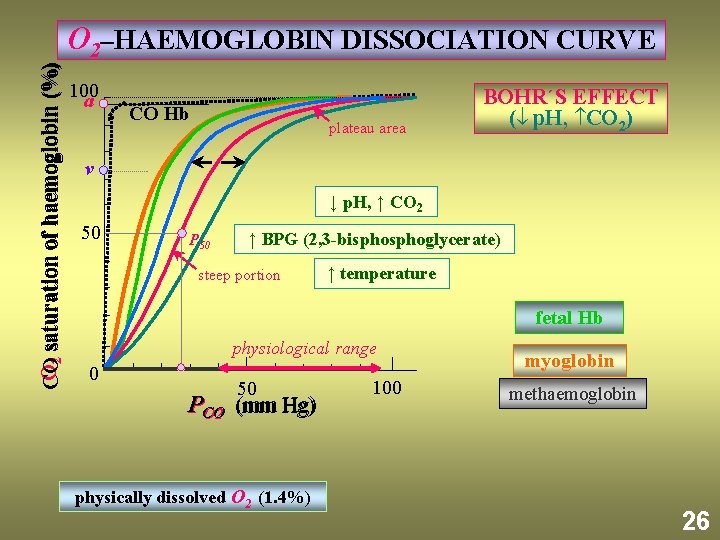
O 2 saturation of haemoglobin (%) CO O 2–HAEMOGLOBIN DISSOCIATION CURVE 100 a CO Hb plateau area BOHR´S EFFECT ( p. H, CO 2) v ↓ p. H, ↑ CO 2 50 P 50 ↑ BPG (2, 3 -bisphoglycerate) steep portion ↑ temperature fetal Hb physiological range 0 50 PCO O 2 (mm Hg) physically dissolved O 2 (1. 4%) 100 myoglobin methaemoglobin 26
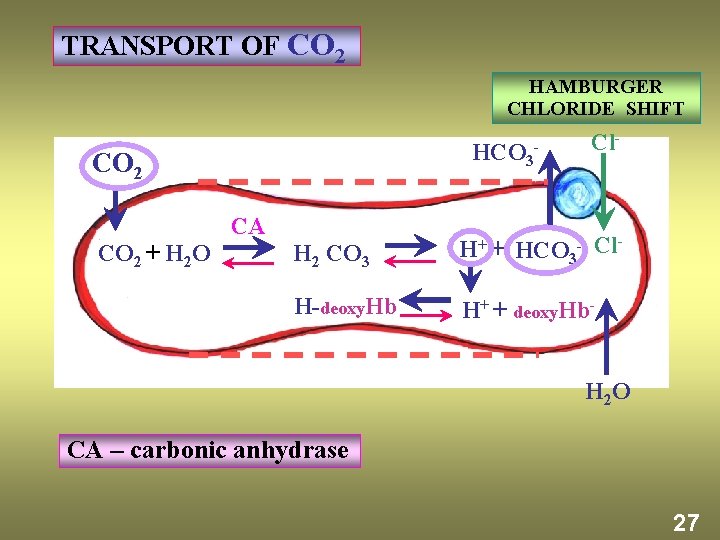
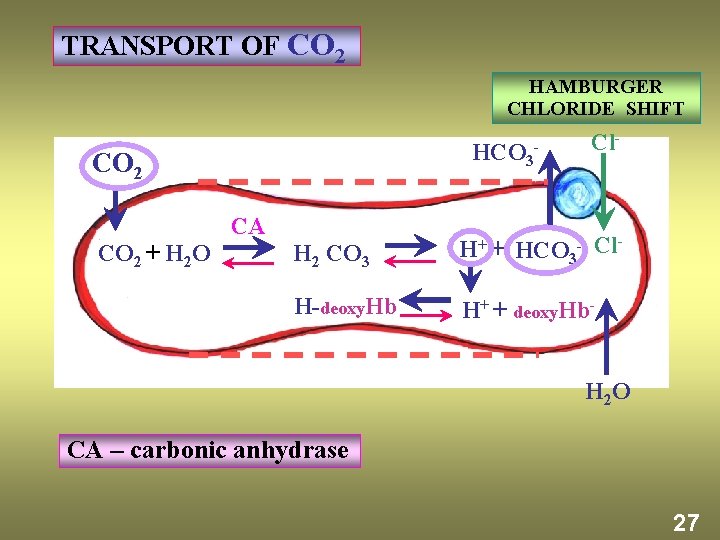
TRANSPORT OF CO 2 HAMBURGER CHLORIDE SHIFT HCO 3 - CO 2 + H 2 O CA Cl- H 2 CO 3 H+ + HCO 3 - Cl- H-deoxy. Hb H+ + deoxy. Hb. H 2 O CA – carbonic anhydrase 27
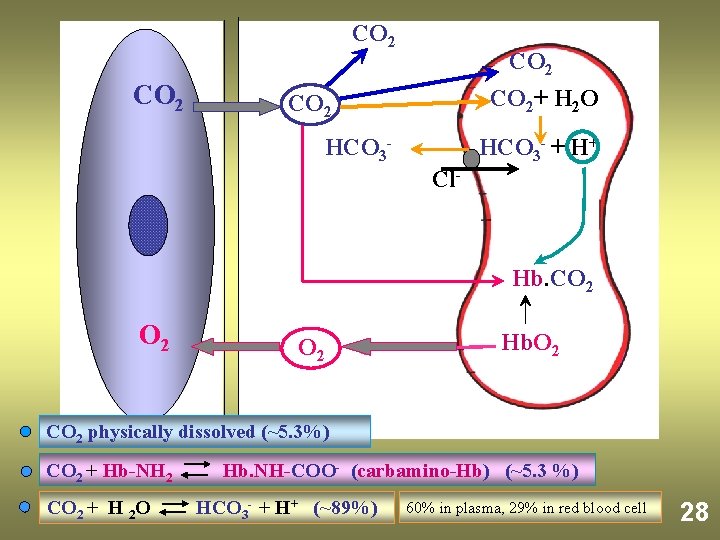
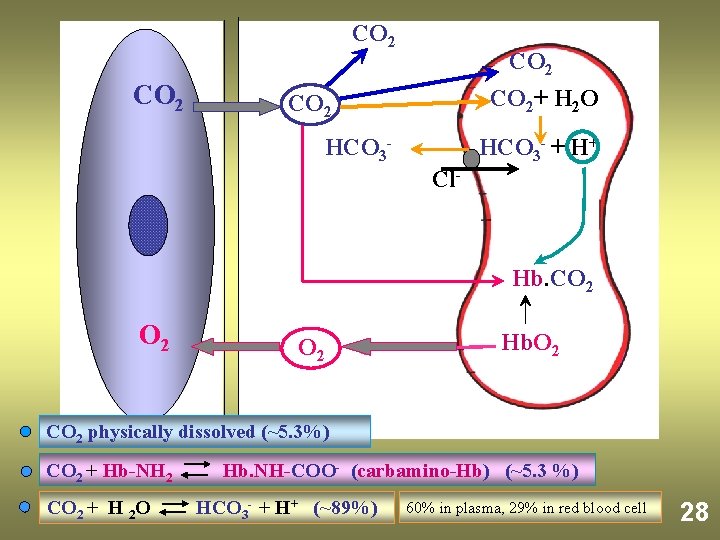
CO 2 CO 2+ H 2 O CO 2 HCO 3 - + H+ Cl- Hb. CO 2 O 2 Hb. O 2 CO 2 physically dissolved (~5. 3%) CO 2 + Hb-NH 2 CO 2 + H 2 O Hb. NH-COO- (carbamino-Hb) (~5. 3 %) HCO 3 - + H+ (~89%) 60% in plasma, 29% in red blood cell 28
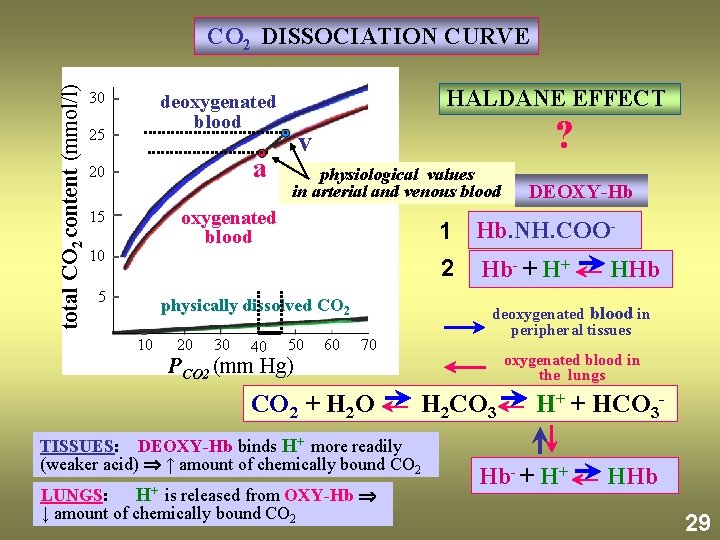
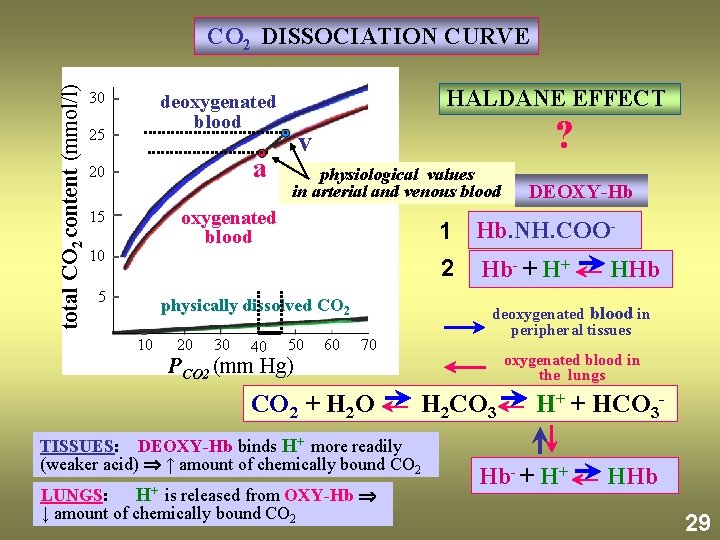
total CO 2 content (mmol/l) CO 2 DISSOCIATION CURVE 30 HALDANE EFFECT deoxygenated blood 25 a 20 ? v physiological values in arterial and venous blood oxygenated blood 15 10 1 Hb. NH. COO 2 5 physically dissolved CO 2 10 20 30 40 50 60 Hb- + H+ 70 CO 2 + H 2 O oxygenated blood in the lungs H 2 CO 3 TISSUES: DEOXY-Hb binds H+ more readily (weaker acid) ↑ amount of chemically bound CO 2 LUNGS: is released from OXY-Hb ↓ amount of chemically bound CO 2 HHb deoxygenated blood in peripheral tissues PCO 2 (mm Hg) H+ DEOXY-Hb H+ + HCO 3 - Hb- + H+ HHb 29

TIME COURSE OF PRESSURES AT QUIET RESPIRATION P. V = const INSPIRATION PA < PATM EXPIRATION PA > PATM VT [l] time +1 [mm Hg] PA -1 PPL -3 measured curve PA ALVEOLAR (INTRAPULMONARY, LUNG) PPL INTRAPLEURAL (INTRATHORACIC) ? [mm Hg] theoretical -6 curve ? 11
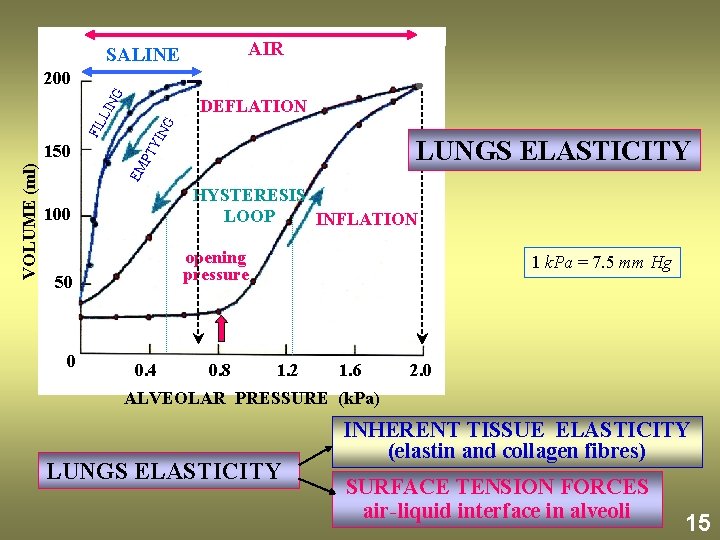
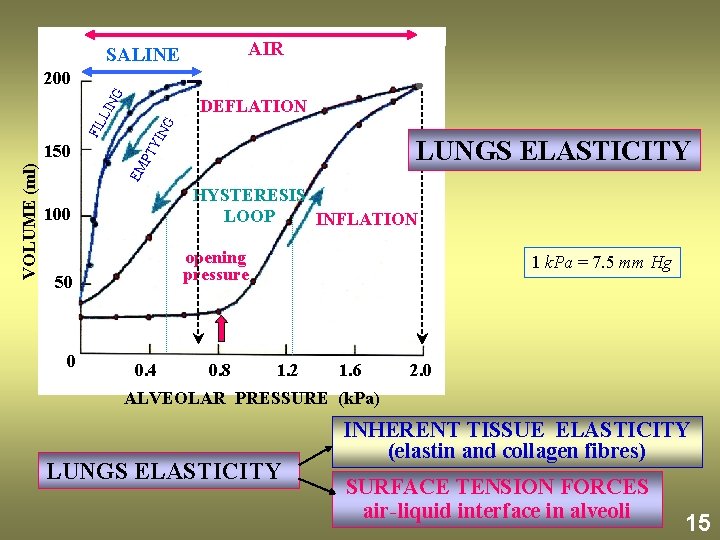
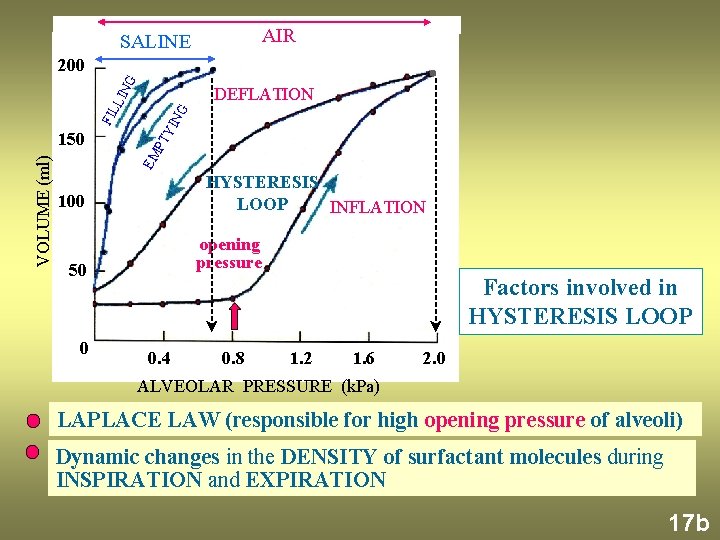
AIR SALINE G 200 NG LUNGS ELASTICITY EM VOLUME (ml) 150 PT YI FIL LIN DEFLATION HYSTERESIS LOOP INFLATION 100 opening pressure 50 0 0. 4 0. 8 1 k. Pa = 7. 5 mm Hg 1. 2 1. 6 2. 0 ALVEOLAR PRESSURE (k. Pa) LUNGS ELASTICITY INHERENT TISSUE ELASTICITY (elastin and collagen fibres) SURFACE TENSION FORCES air-liquid interface in alveoli 15
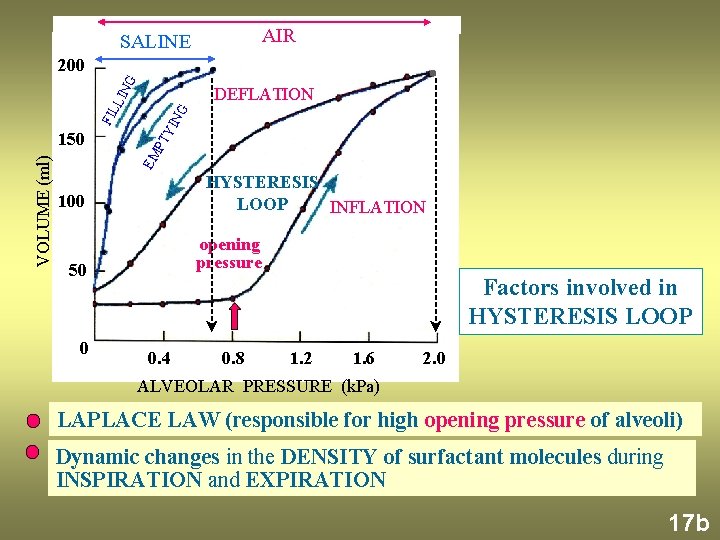
AIR SALINE G 200 NG EM VOLUME (ml) 150 PT YI FIL LIN DEFLATION HYSTERESIS LOOP INFLATION 100 opening pressure 50 0 Factors involved in HYSTERESIS LOOP 0. 4 0. 8 1. 2 1. 6 2. 0 ALVEOLAR PRESSURE (k. Pa) LAPLACE LAW (responsible for high opening pressure of alveoli) Dynamic changes in the DENSITY of surfactant molecules during INSPIRATION and EXPIRATION 17 b
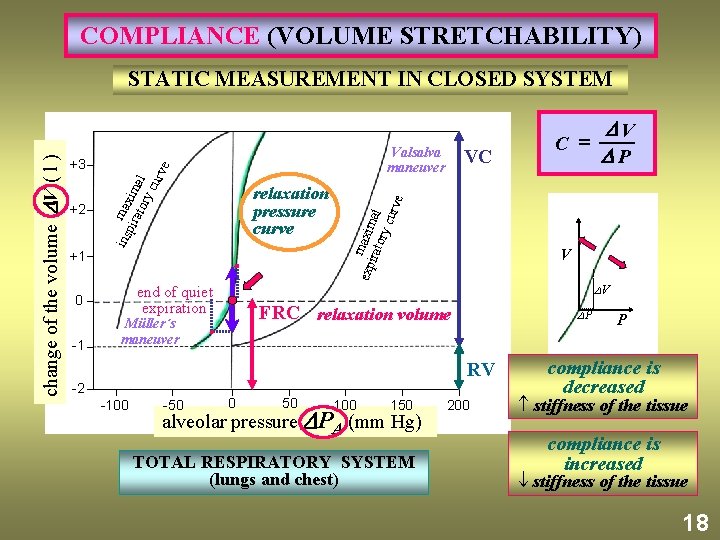
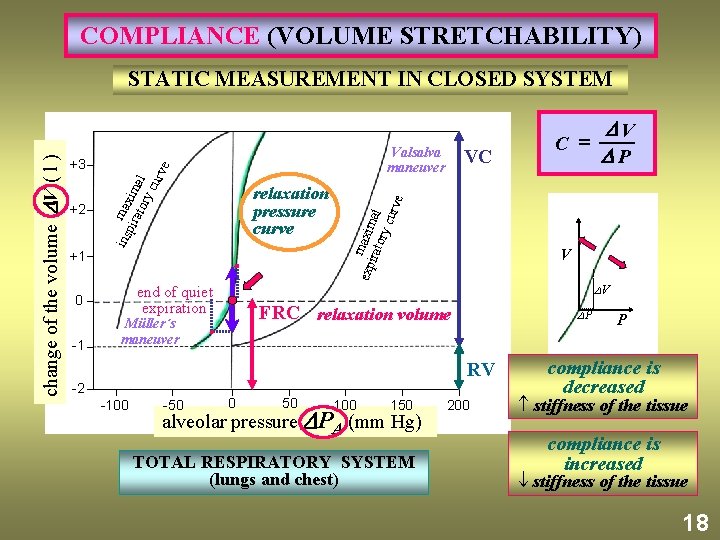
COMPLIANCE (VOLUME STRETCHABILITY) relaxation pressure curve +1 end of quiet expiration 0 -1 VC V P RV -2 -100 -50 0 50 V P V FRC relaxation volume Müller´s maneuver C = e +2 Valsalva maneuver exp maxim irat ory al curv +3 ins max pir im ato al ry cur ve change of the volume V ( l ) STATIC MEASUREMENT IN CLOSED SYSTEM 100 150 alveolar pressure PA (mm Hg) TOTAL RESPIRATORY SYSTEM (lungs and chest) 200 P compliance is decreased stiffness of the tissue compliance is increased stiffness of the tissue 18
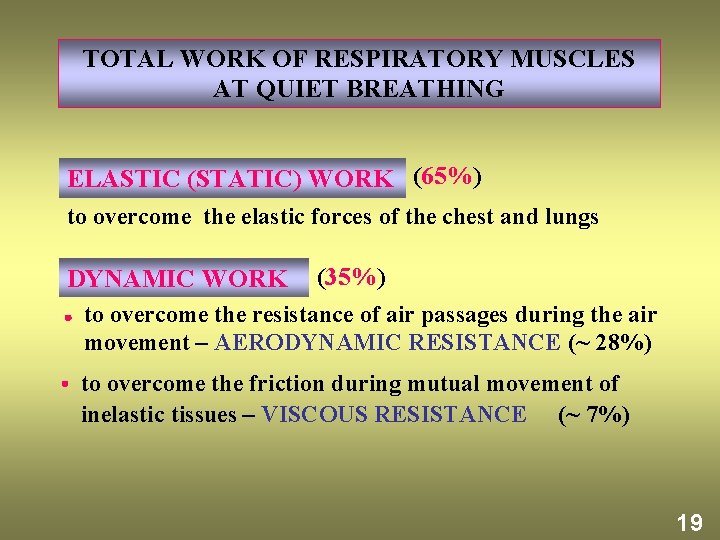
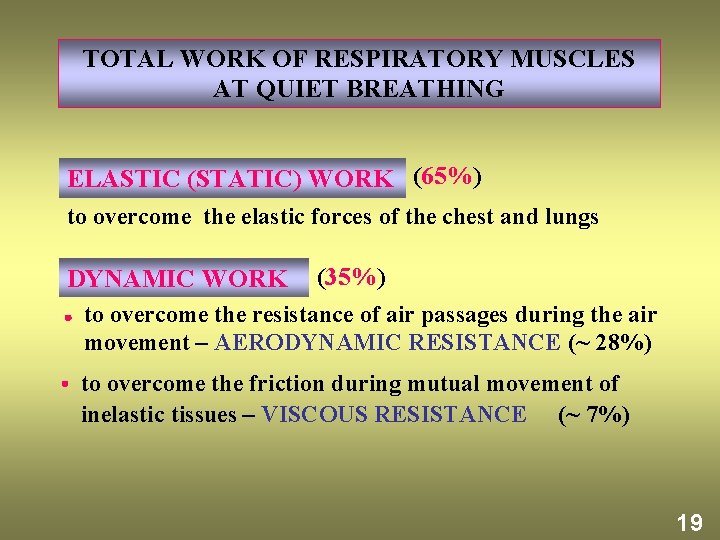
TOTAL WORK OF RESPIRATORY MUSCLES AT QUIET BREATHING ELASTIC (STATIC) WORK (65%) to overcome the elastic forces of the chest and lungs DYNAMIC WORK (35%) to overcome the resistance of air passages during the air movement – AERODYNAMIC RESISTANCE (~ 28%) to overcome the friction during mutual movement of inelastic tissues – VISCOUS RESISTANCE (~ 7%) 19
 Respiratory zone of the respiratory system
Respiratory zone of the respiratory system Inspiration anatomy and physiology
Inspiration anatomy and physiology Respiratory digestive and circulatory system
Respiratory digestive and circulatory system Tiny air sacs at the end of the bronchioles
Tiny air sacs at the end of the bronchioles Circulatory system and respiratory system work together
Circulatory system and respiratory system work together Absolute value functions as piecewise functions
Absolute value functions as piecewise functions Evaluating functions and operations on functions
Evaluating functions and operations on functions Evaluating functions and operations on functions
Evaluating functions and operations on functions Statics chapter 2 solutions
Statics chapter 2 solutions Force system in mechanics
Force system in mechanics Bozeman respiratory system
Bozeman respiratory system Unit 9 respiratory system
Unit 9 respiratory system Diagnostic test of respiratory system
Diagnostic test of respiratory system What is the respiratory system
What is the respiratory system Respiratory system larynx
Respiratory system larynx Respiratory system coloring page
Respiratory system coloring page Respiratory system purpose
Respiratory system purpose Respiratory system conclusion
Respiratory system conclusion Respiratory system jobs
Respiratory system jobs Chapter 7:10 respitory system
Chapter 7:10 respitory system Respiratory tree divisions
Respiratory tree divisions Respiratory perfusion
Respiratory perfusion Interesting facts about respiratory system
Interesting facts about respiratory system How to draw the respiratory system
How to draw the respiratory system What is the major function of the respiratory system
What is the major function of the respiratory system Respiratory system diagram unlabeled
Respiratory system diagram unlabeled Respiratory system vocabulary
Respiratory system vocabulary Gas diffusion
Gas diffusion How the respiratory system maintains homeostasis
How the respiratory system maintains homeostasis Respiratory zone and conducting zone
Respiratory zone and conducting zone History taking respiratory system
History taking respiratory system Upper and lower respiratory system
Upper and lower respiratory system Chapter 15 lesson 2 the respiratory system answer key
Chapter 15 lesson 2 the respiratory system answer key Diagnostic test of respiratory system
Diagnostic test of respiratory system