Wheezy Infant Prof Dr Reha Cengizlier 30 10




- Slides: 27
Wheezy Infant Prof. Dr. Reha Cengizlier 30. 10. 2014
The most common causes of infantile wheezing are viral respiratory infections and asthma
Wheezing phenotypes Young children have been grouped into three wheezing phenotypes : ◦ Transient (onset ≤ 3 yr of age, then resolving) ◦ Persistent (onset ≤ 3 yr of age and then persisting) ◦ Late onset (onset of wheeze between 3 -6 yr )
Frequency -20% of all children will have had at least one wheezing illness by 1 yr of age -33% by 3 yr of age -50% by 6 yr Less than 15% of children are subsequently diagnosed with asthma Asthma is the most common disease of childhood and confers a significant degree of morbidity, thereby demanding early evaluation and management in the predisposed persistently wheezing infant
Risk factors The presence of atopy in the host development of lower respiratory tract infections; Are the two most important independent risk factors for the development of persistent wheezing and asthma
Risk factors The atopic state can influence lower airway response to viral infections, whereas viral infections may influence the development of allergy Infection with RSV is the cause of the majority of lower respiratory tract illnesses with wheezing during the first 3 yr of life and may increase the risk of allergic sensitization later in childhood
Clinical findings Respiratory distress and breathing difficulty The location of wheezing (unilateral, suggestive of a foreign body or bronchomalacia, or bilateral, suggestive of a more generalized process) Wheezing and crackles (suggestive of an interstitial lung component including infection, bronchopulmonary dysplasia [BPD], or pulmonary edema with congestive heart disease)
Laboratory findings Most infants with a single episode of wheezing will not require a chest radiograph, other than to confirm positive additional findings and/or to alleviate parental anxieties Any child with recurrent episodes of wheezing or congenital anomalies should have anteroposterior and lateral radiographic views taken to ascertain the presence of hyperinflation and/or structural abnormalities Suspicion of structural abnormalities may warrant additional imaging studies such as a CT or MRI and/or direct visualization using laryngobronchoscopy
Laboratory findings The patient with an atopic family history and/or physical findings include allergy tests Infant pulmonary function testing very rarely necessary to assess decreased lung function
Treatment The treatment of infantile wheeze should be based on the underlying etiology For viral-induced wheezing, management involves the use of supplemental oxygen to treat hypoxemia and a trial of bronchodilators Systemic corticosteroids are not indicated for the treatment of acute viral bronchiolitis, and the role of inhaled corticosteroids used acutely remains controversial
Prognosis The majority (60%) of children with early-onset wheezing will stop wheezing A minority (15%) are at significant risk for persistent asthma
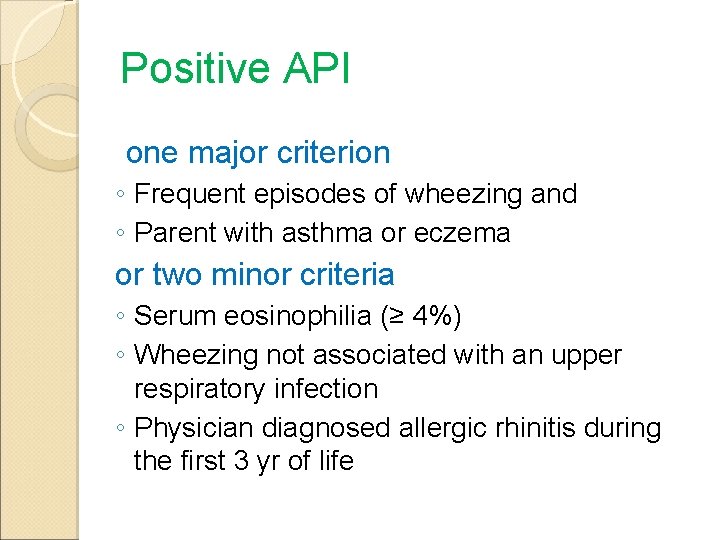
Prognosis Based on the Tucson Children's Respiratory Study's asthma predictive index (API), young children with frequent wheezing episodes may be identified who are potentially at increased risk for the development of persistent asthma Positive API:
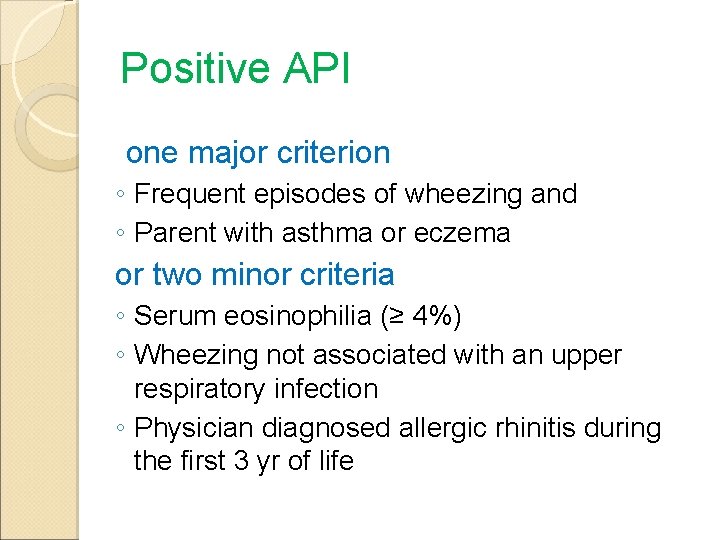
Positive API one major criterion ◦ Frequent episodes of wheezing and ◦ Parent with asthma or eczema or two minor criteria ◦ Serum eosinophilia (≥ 4%) ◦ Wheezing not associated with an upper respiratory infection ◦ Physician diagnosed allergic rhinitis during the first 3 yr of life
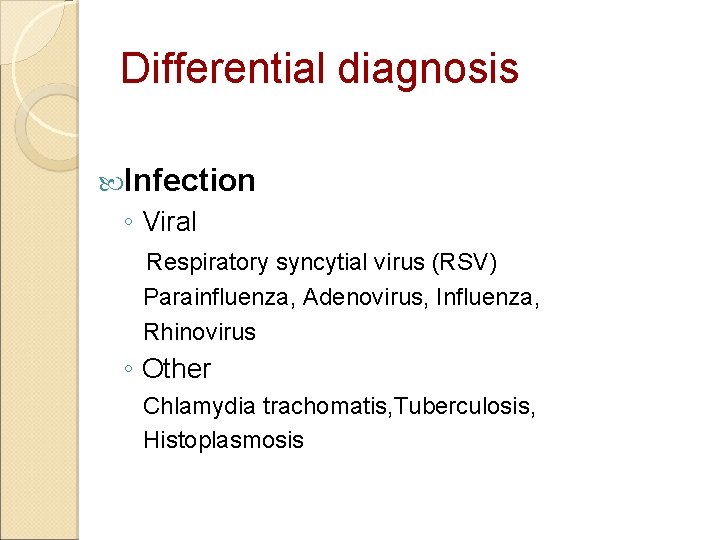
Differential diagnosis Infection ◦ Viral Respiratory syncytial virus (RSV) Parainfluenza, Adenovirus, Influenza, Rhinovirus ◦ Other Chlamydia trachomatis, Tuberculosis, Histoplasmosis
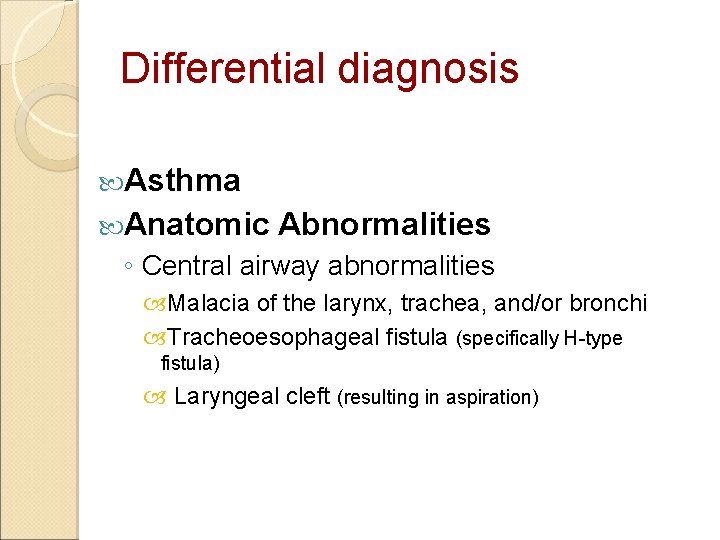
Differential diagnosis Asthma Anatomic Abnormalities ◦ Central airway abnormalities Malacia of the larynx, trachea, and/or bronchi Tracheoesophageal fistula (specifically H-type fistula) Laryngeal cleft (resulting in aspiration)
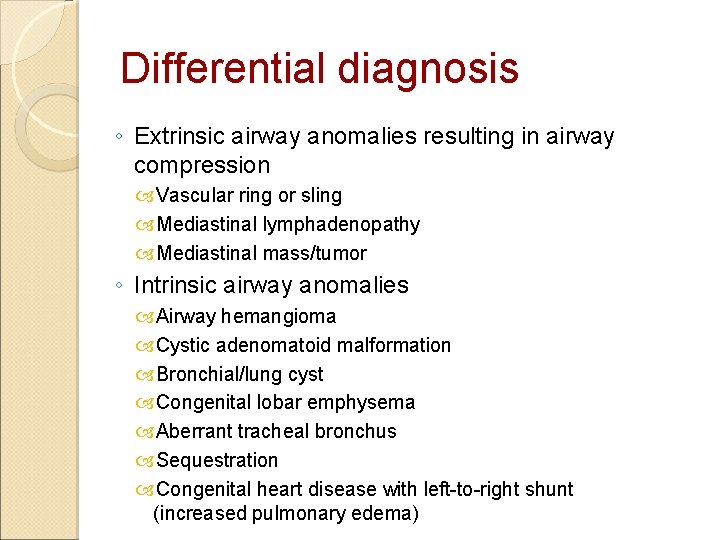
Differential diagnosis ◦ Extrinsic airway anomalies resulting in airway compression Vascular ring or sling Mediastinal lymphadenopathy Mediastinal mass/tumor ◦ Intrinsic airway anomalies Airway hemangioma Cystic adenomatoid malformation Bronchial/lung cyst Congenital lobar emphysema Aberrant tracheal bronchus Sequestration Congenital heart disease with left-to-right shunt (increased pulmonary edema)
Differential diagnosis Inherited ◦ Cystic fibrosis ◦ Immunodeficiency states ◦ Ig. A deficiency ◦ B-cell deficiencies ◦ Primary ciliary dyskinesia ◦ Neonatal AIDS ◦ Bronchiectasis
Differential diagnosis Bronchopulmonary Dysplasia Aspiration Syndromes Gastroesophageal reflux disease Pharyngeal/swallow dysfunction Interstitial Lung Disease, including Bronchiolitis Obliterans Foreign Body
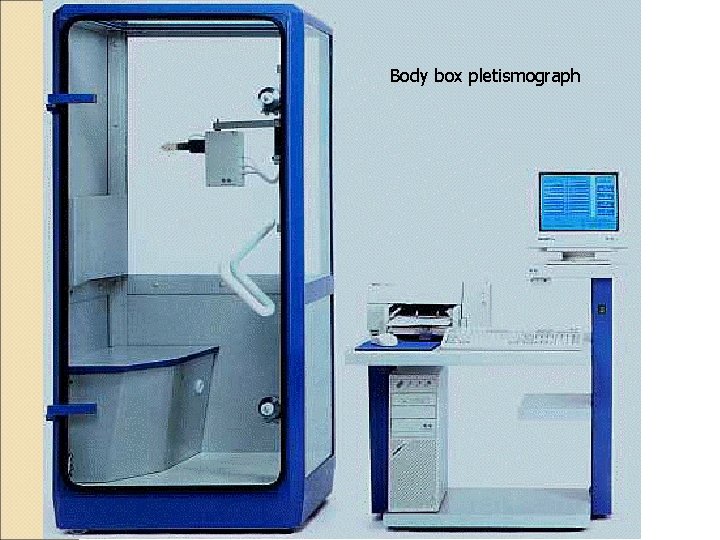
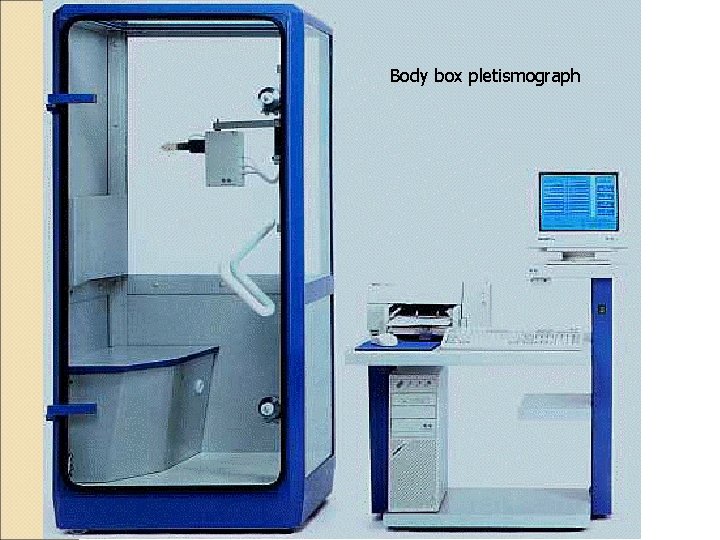
Body box pletismograph
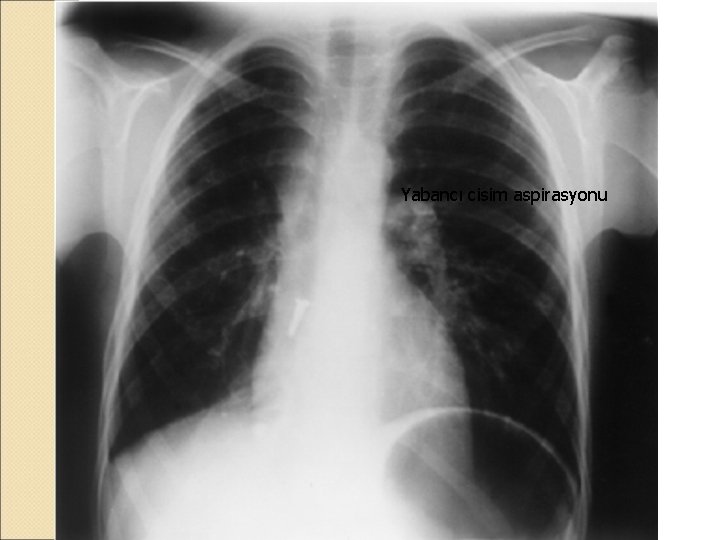
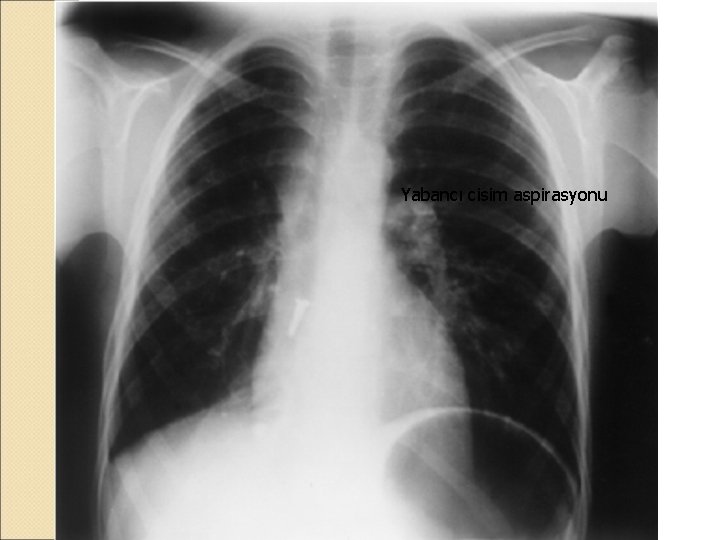
Yabancı cisim aspirasyonu
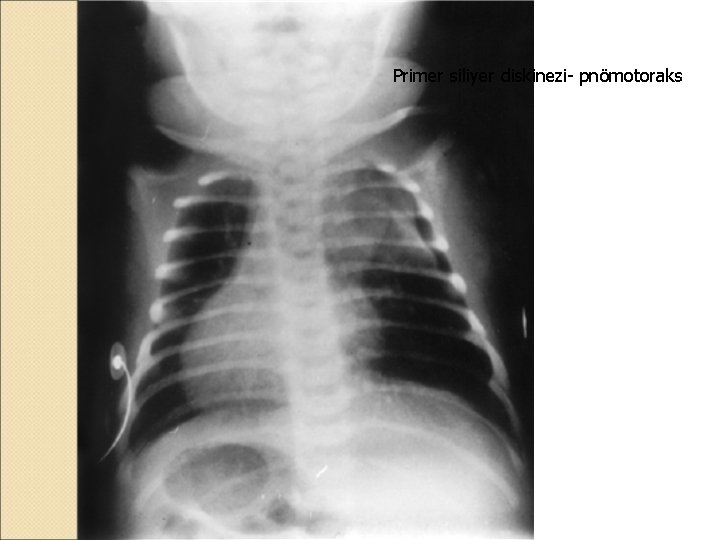
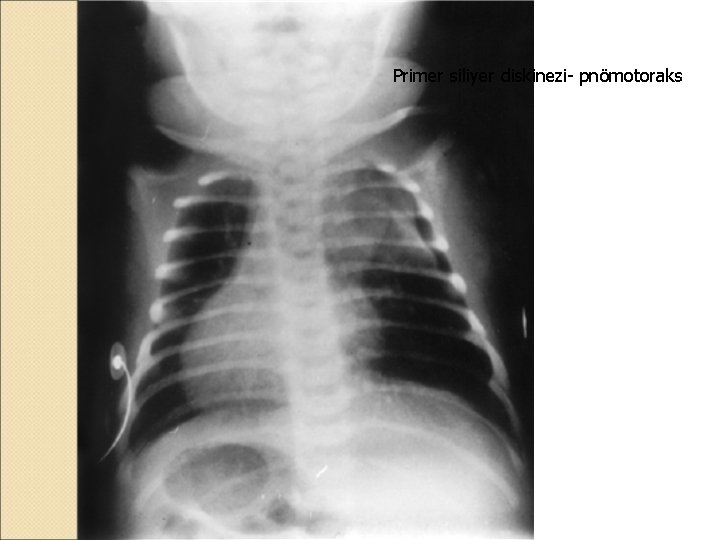
Primer siliyer diskinezi- pnömotoraks
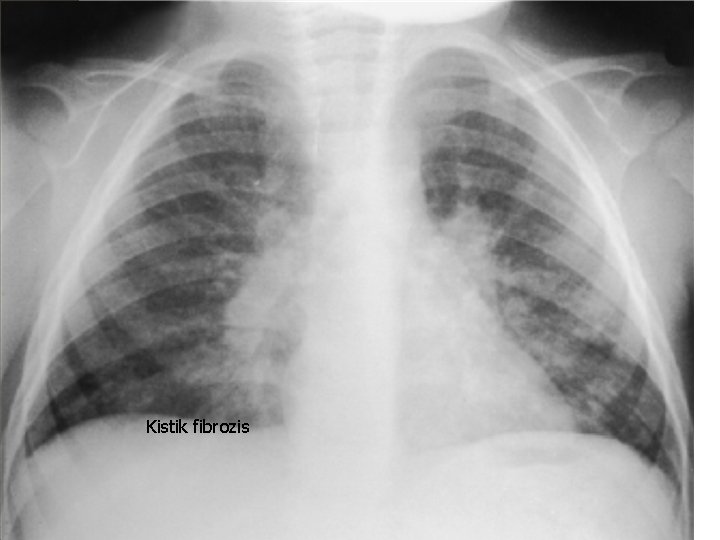
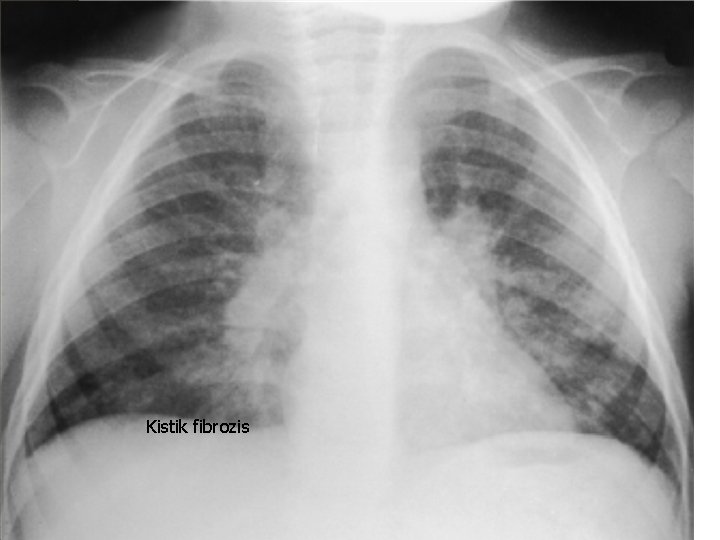
Kistik fibrozis
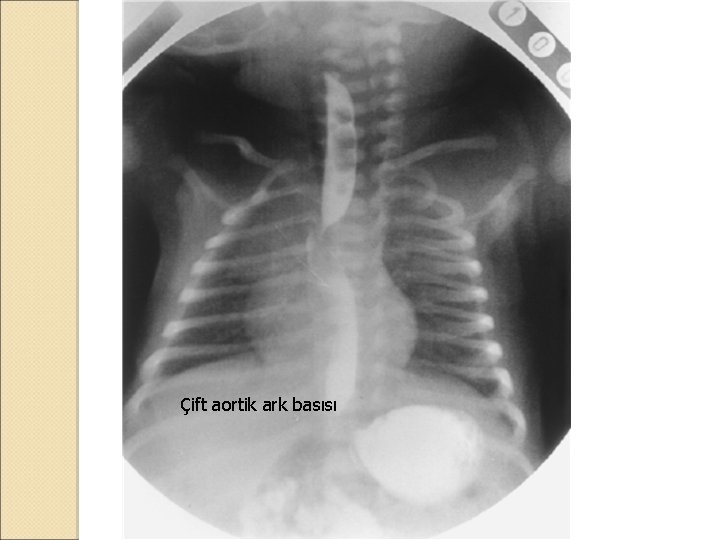
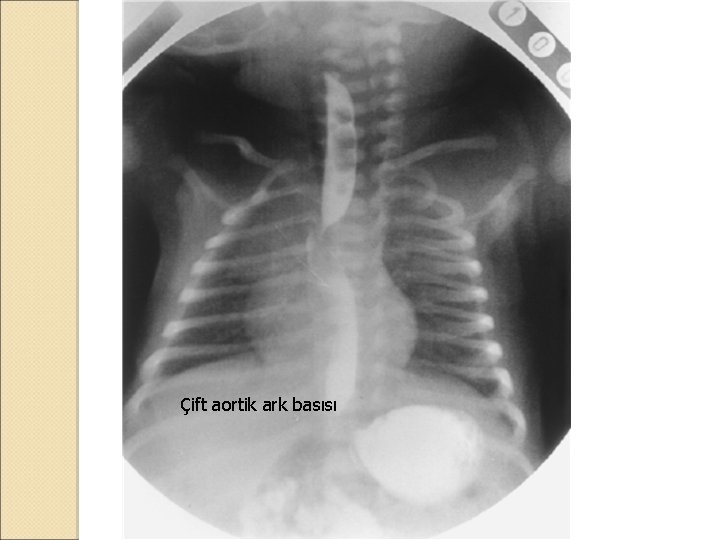
Çift aortik ark basısı




 Dr reha
Dr reha Its not easy being wheezy
Its not easy being wheezy Debian 7 wheezy
Debian 7 wheezy Reha groten würselen
Reha groten würselen Schulische reha
Schulische reha Www.aws-rehab.at
Www.aws-rehab.at Zar bielefeld
Zar bielefeld Annela valdi
Annela valdi Geriatrie neuruppin
Geriatrie neuruppin Reha tözün
Reha tözün Infant epiglottis anatomy
Infant epiglottis anatomy Infant-industry argument
Infant-industry argument Kenmore park infant and nursery school
Kenmore park infant and nursery school For sale baby shoes never worn short story
For sale baby shoes never worn short story Phoenix infant academy
Phoenix infant academy Femoral pulse infant
Femoral pulse infant Denis browne bar
Denis browne bar Infant industries apush
Infant industries apush Saguaro infant care and preschool
Saguaro infant care and preschool Infant hip
Infant hip Infant reflexes chart
Infant reflexes chart Crvs institute panel
Crvs institute panel Flacc pain scale ages
Flacc pain scale ages Infant industry
Infant industry Social impulses foster infant language
Social impulses foster infant language High quality cpr infant
High quality cpr infant Ap human geography unit 2
Ap human geography unit 2 Infants display a wide range of emotional expressions
Infants display a wide range of emotional expressions