Case Study Heart Chief Complaint 68 yearold man













- Slides: 162
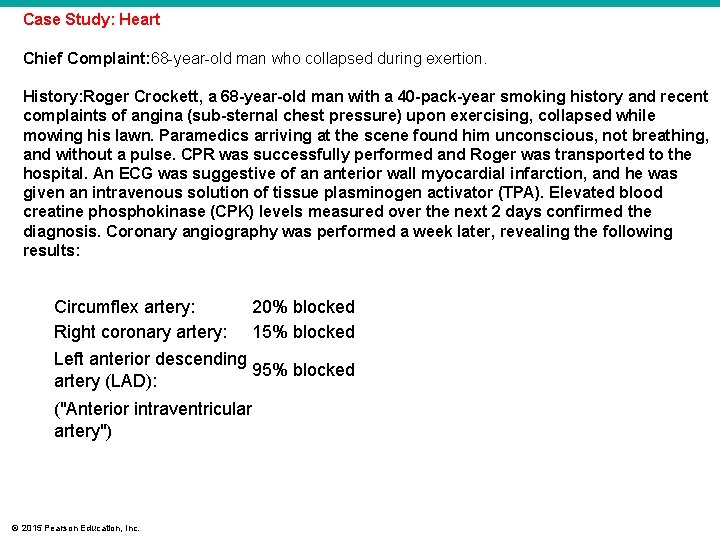
Case Study: Heart Chief Complaint: 68 -year-old man who collapsed during exertion. History: Roger Crockett, a 68 -year-old man with a 40 -pack-year smoking history and recent complaints of angina (sub-sternal chest pressure) upon exercising, collapsed while mowing his lawn. Paramedics arriving at the scene found him unconscious, not breathing, and without a pulse. CPR was successfully performed and Roger was transported to the hospital. An ECG was suggestive of an anterior wall myocardial infarction, and he was given an intravenous solution of tissue plasminogen activator (TPA). Elevated blood creatine phosphokinase (CPK) levels measured over the next 2 days confirmed the diagnosis. Coronary angiography was performed a week later, revealing the following results: Circumflex artery: 20% blocked Right coronary artery: 15% blocked Left anterior descending 95% blocked artery (LAD): ("Anterior intraventricular artery") © 2015 Pearson Education, Inc.
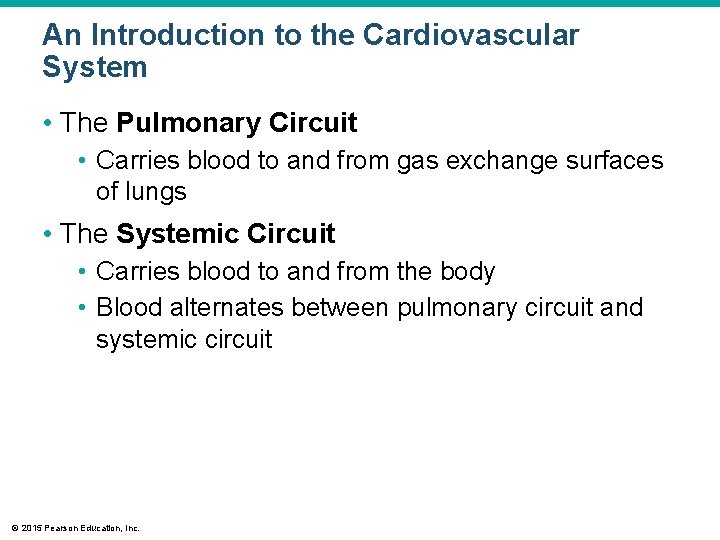
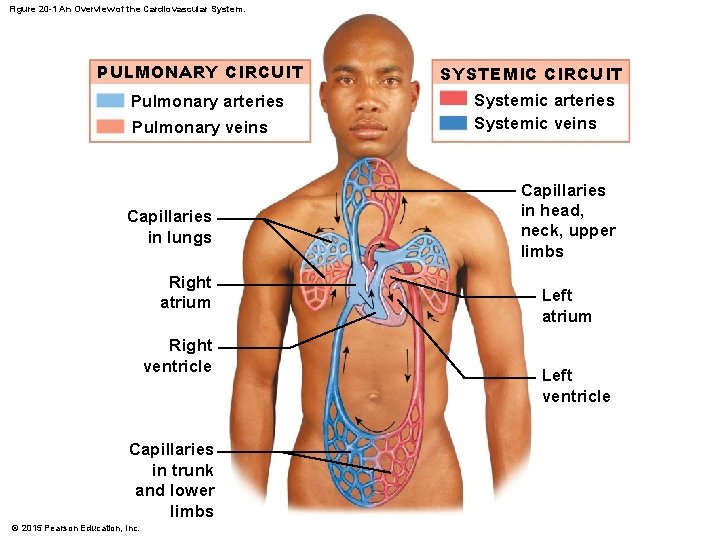
An Introduction to the Cardiovascular System • The Pulmonary Circuit • Carries blood to and from gas exchange surfaces of lungs • The Systemic Circuit • Carries blood to and from the body • Blood alternates between pulmonary circuit and systemic circuit © 2015 Pearson Education, Inc.
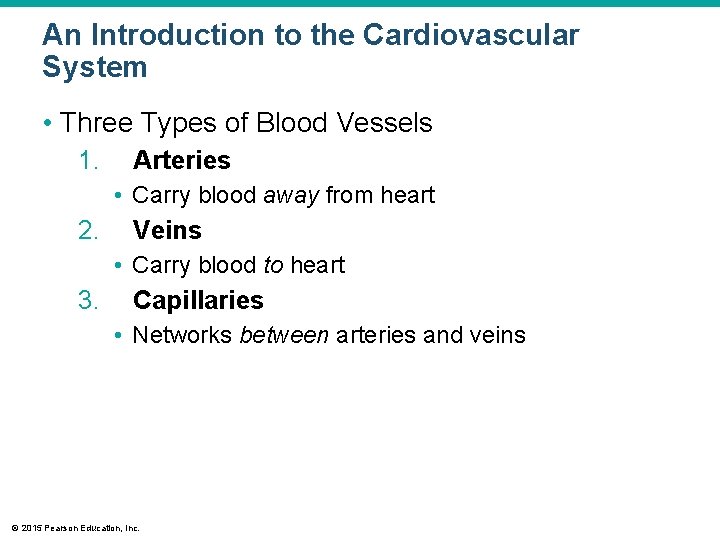
An Introduction to the Cardiovascular System • Three Types of Blood Vessels 1. Arteries • Carry blood away from heart 2. Veins • Carry blood to heart 3. Capillaries • Networks between arteries and veins © 2015 Pearson Education, Inc.
An Introduction to the Cardiovascular System • Capillaries • Also called exchange vessels • Exchange materials between blood and tissues • Materials include dissolved gases, nutrients, waste products © 2015 Pearson Education, Inc.
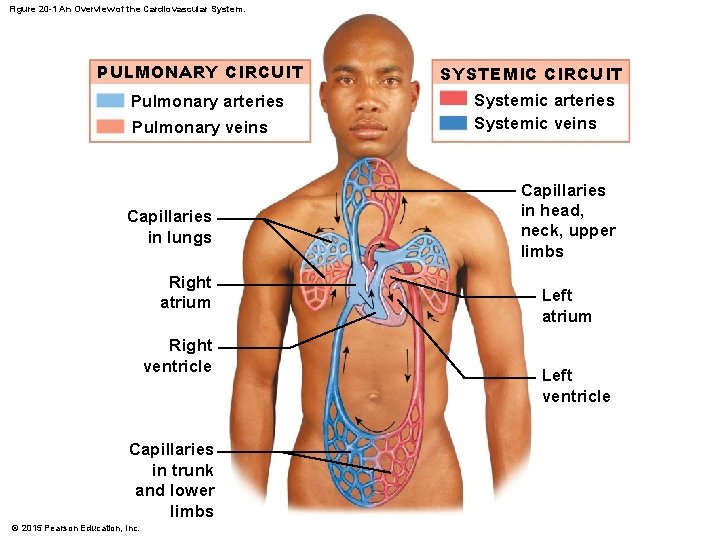
Figure 20 -1 An Overview of the Cardiovascular System. PULMONARY CIRCUIT Pulmonary arteries Pulmonary veins Capillaries in lungs Right atrium Right ventricle Capillaries in trunk and lower limbs © 2015 Pearson Education, Inc. SYSTEMIC CIRCUIT Systemic arteries Systemic veins Capillaries in head, neck, upper limbs Left atrium Left ventricle
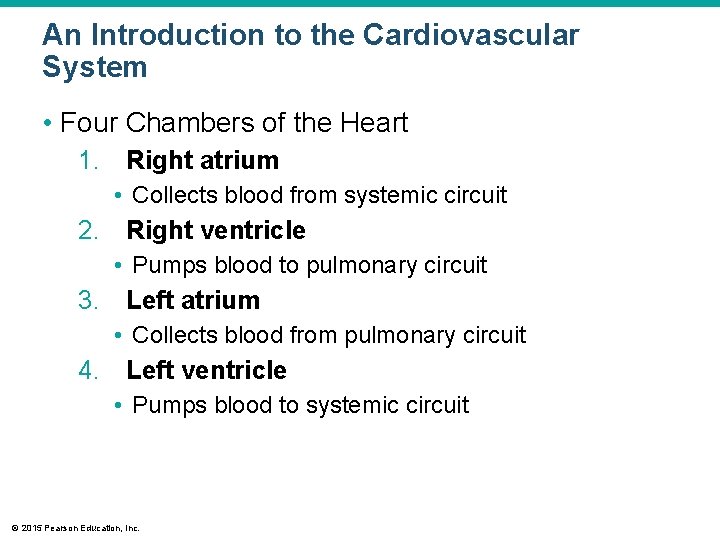
An Introduction to the Cardiovascular System • Four Chambers of the Heart 1. Right atrium • Collects blood from systemic circuit 2. Right ventricle • Pumps blood to pulmonary circuit 3. Left atrium • Collects blood from pulmonary circuit 4. Left ventricle • Pumps blood to systemic circuit © 2015 Pearson Education, Inc.
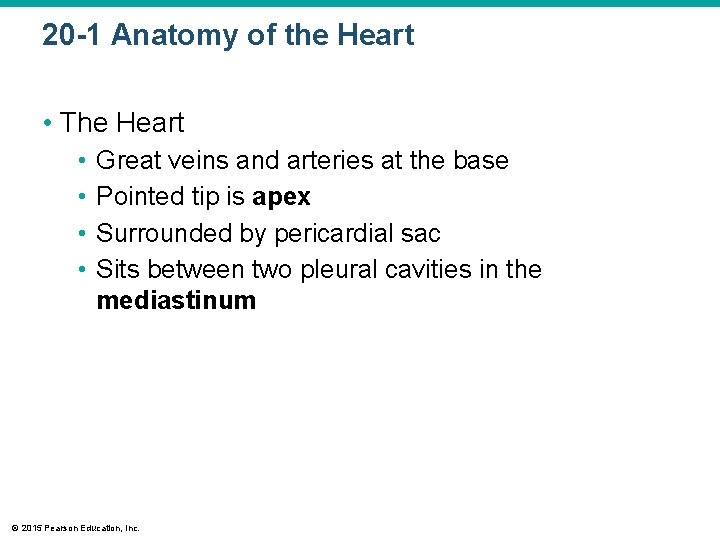
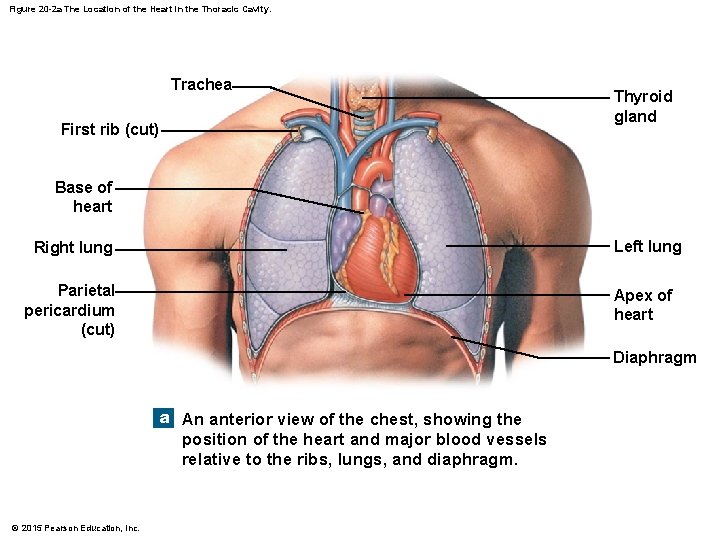
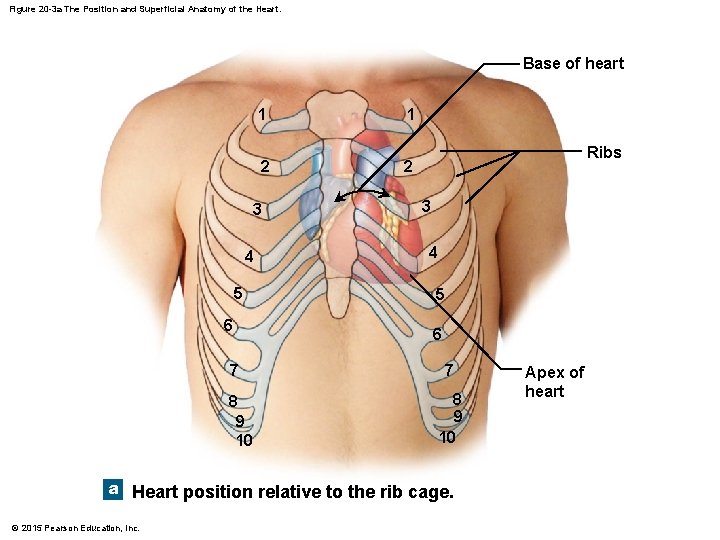
20 -1 Anatomy of the Heart • The Heart • • Great veins and arteries at the base Pointed tip is apex Surrounded by pericardial sac Sits between two pleural cavities in the mediastinum © 2015 Pearson Education, Inc.
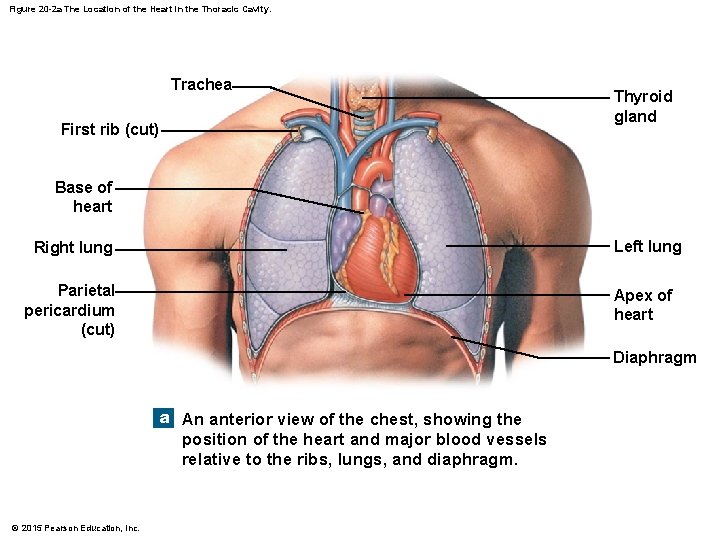
Figure 20 -2 a The Location of the Heart in the Thoracic Cavity. Trachea First rib (cut) Thyroid gland Base of heart Right lung Left lung Parietal pericardium (cut) Apex of heart Diaphragm a An anterior view of the chest, showing the position of the heart and major blood vessels relative to the ribs, lungs, and diaphragm. © 2015 Pearson Education, Inc.
20 -1 Anatomy of the Heart • The Pericardium • Double lining of the pericardial cavity • Visceral pericardium • Inner layer of pericardium • Parietal pericardium • Outer layer • Forms inner layer of pericardial sac © 2015 Pearson Education, Inc.
20 -1 Anatomy of the Heart • The Pericardium • Pericardial cavity • Is between parietal and visceral layers • Contains pericardial fluid • Pericardial sac • Fibrous tissue • Surrounds and stabilizes heart © 2015 Pearson Education, Inc.
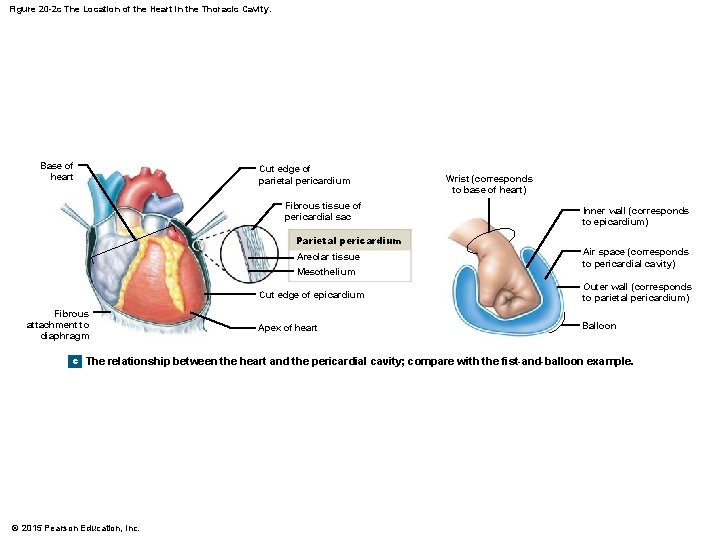
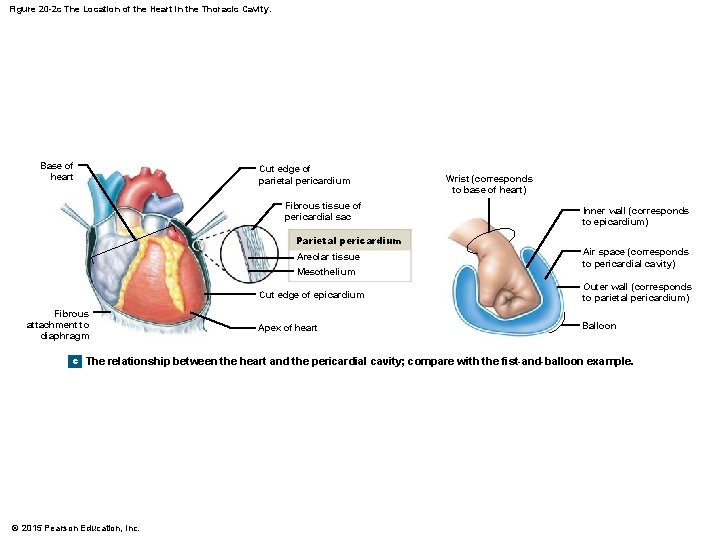
Figure 20 -2 c The Location of the Heart in the Thoracic Cavity. Base of heart Cut edge of parietal pericardium Fibrous tissue of pericardial sac Parietal pericardium Areolar tissue Mesothelium Fibrous attachment to diaphragm Wrist (corresponds to base of heart) Inner wall (corresponds to epicardium) Air space (corresponds to pericardial cavity) Cut edge of epicardium Outer wall (corresponds to parietal pericardium) Apex of heart Balloon c The relationship between the heart and the pericardial cavity; compare with the fist-and-balloon example. © 2015 Pearson Education, Inc.
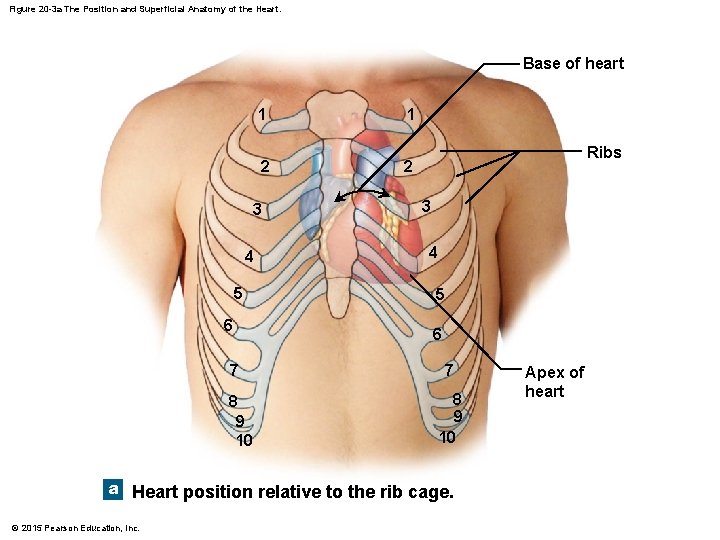
Figure 20 -3 a The Position and Superficial Anatomy of the Heart. Base of heart 1 2 3 4 5 6 7 8 9 10 1 Ribs 2 3 4 5 6 7 8 9 10 a Heart position relative to the rib cage. © 2015 Pearson Education, Inc. Apex of heart
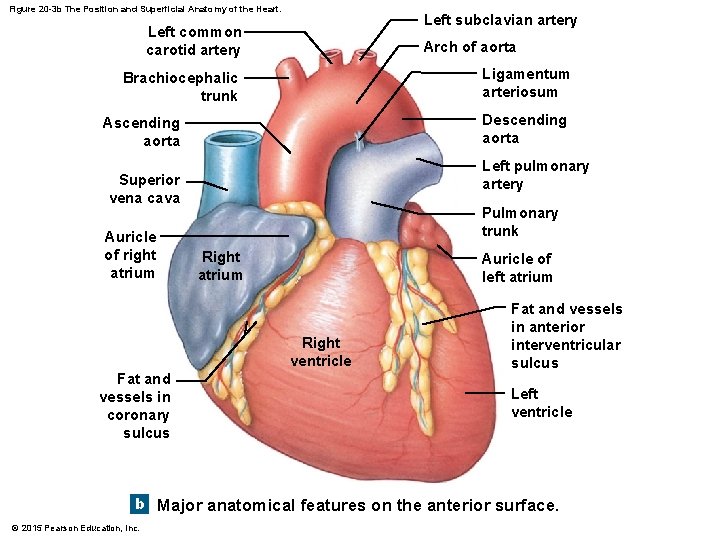
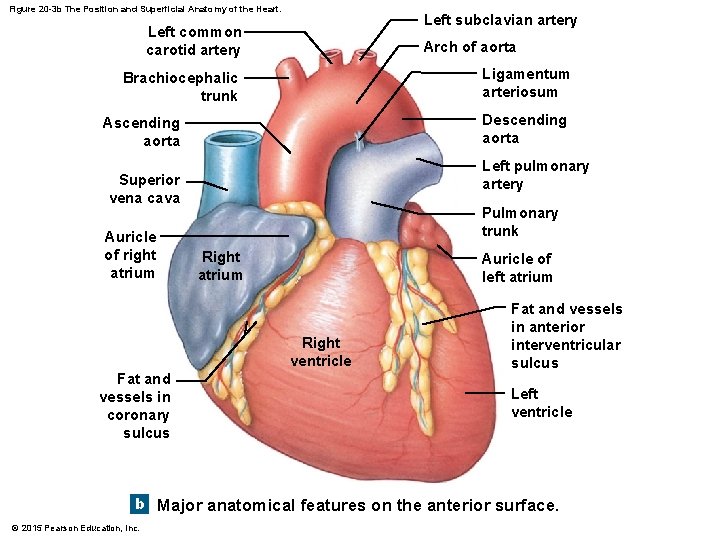
Figure 20 -3 b The Position and Superficial Anatomy of the Heart. Left subclavian artery Left common carotid artery Arch of aorta Ligamentum arteriosum Brachiocephalic trunk Descending aorta Ascending aorta Left pulmonary artery Superior vena cava Auricle of right atrium Pulmonary trunk Right atrium Auricle of left atrium Right ventricle Fat and vessels in coronary sulcus Fat and vessels in anterior interventricular sulcus Left ventricle b Major anatomical features on the anterior surface. © 2015 Pearson Education, Inc.
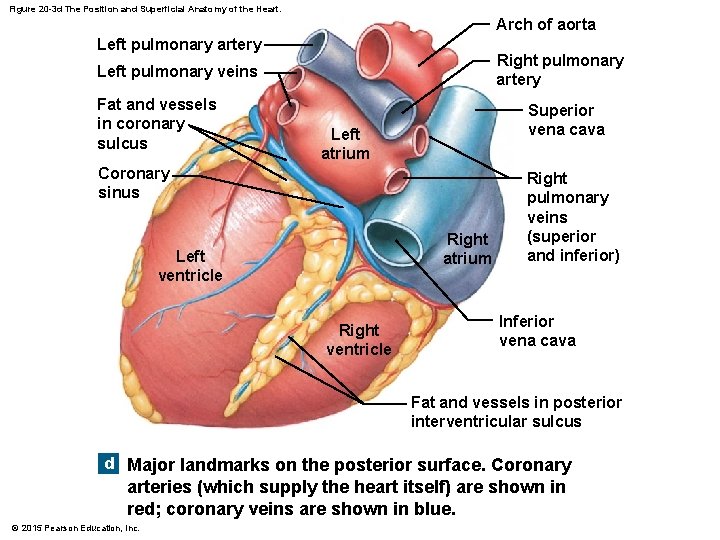
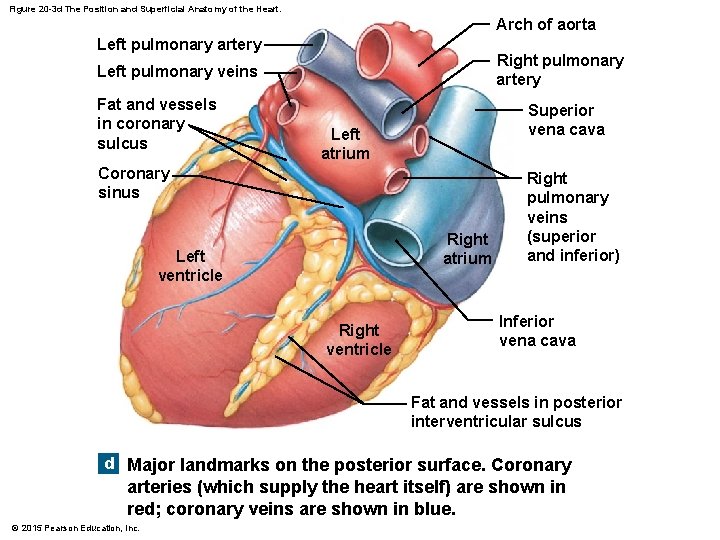
Figure 20 -3 d The Position and Superficial Anatomy of the Heart. Arch of aorta Left pulmonary artery Right pulmonary artery Left pulmonary veins Fat and vessels in coronary sulcus Superior vena cava Left atrium Coronary sinus Right atrium Left ventricle Right pulmonary veins (superior and inferior) Inferior vena cava Fat and vessels in posterior interventricular sulcus d Major landmarks on the posterior surface. Coronary arteries (which supply the heart itself) are shown in red; coronary veins are shown in blue. © 2015 Pearson Education, Inc.
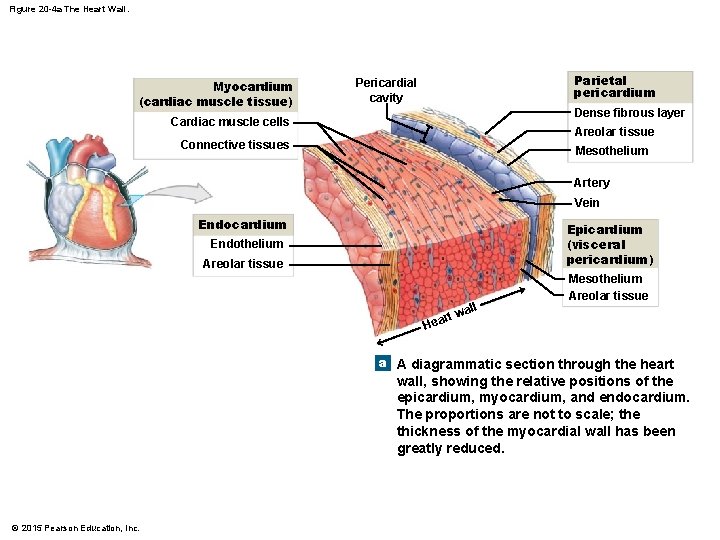
20 -1 Anatomy of the Heart • The Heart Wall 1. Epicardium 2. Myocardium 3. Endocardium © 2015 Pearson Education, Inc.
20 -1 Anatomy of the Heart • Epicardium (Outer Layer) • Visceral pericardium • Covers the heart © 2015 Pearson Education, Inc.
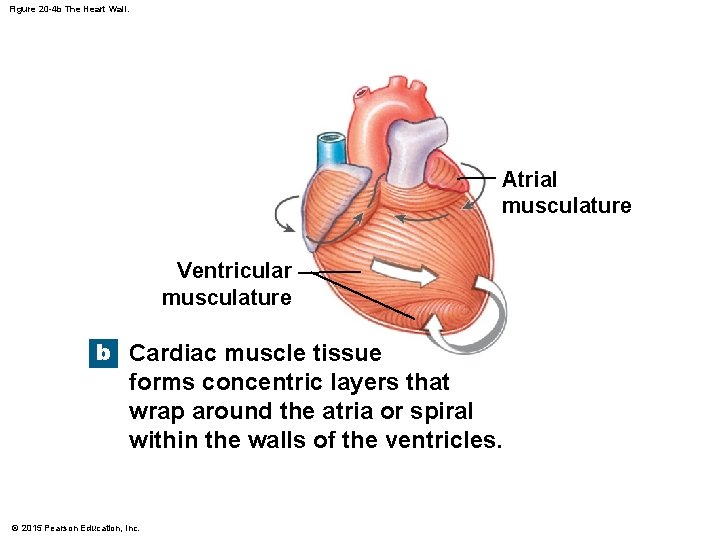
20 -1 Anatomy of the Heart • Myocardium (Middle Layer) • • Muscular wall of the heart Concentric layers of cardiac muscle tissue Atrial myocardium wraps around great vessels Two divisions of ventricular myocardium • Endocardium (Inner Layer) • Simple squamous epithelium © 2015 Pearson Education, Inc.
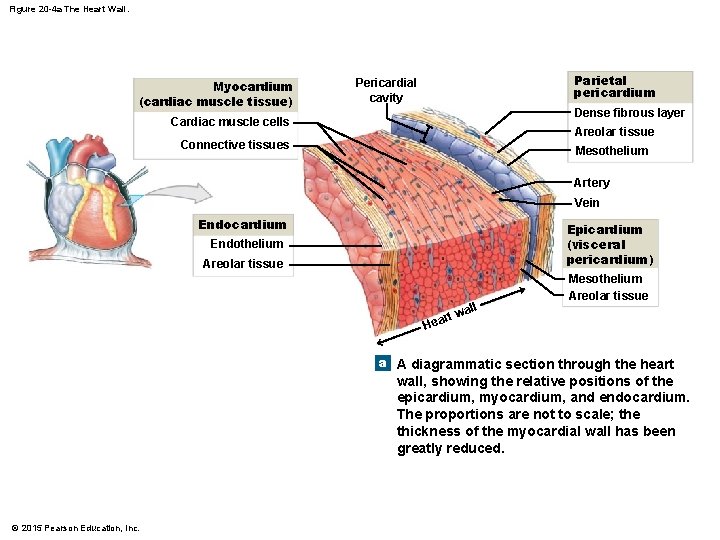
Figure 20 -4 a The Heart Wall. Myocardium (cardiac muscle tissue) Parietal pericardium Pericardial cavity Dense fibrous layer Cardiac muscle cells Areolar tissue Connective tissues Mesothelium Artery Vein Endocardium Endothelium Epicardium (visceral pericardium) Areolar tissue all Mesothelium Areolar tissue rt w Hea a A diagrammatic section through the heart wall, showing the relative positions of the epicardium, myocardium, and endocardium. The proportions are not to scale; the thickness of the myocardial wall has been greatly reduced. © 2015 Pearson Education, Inc.
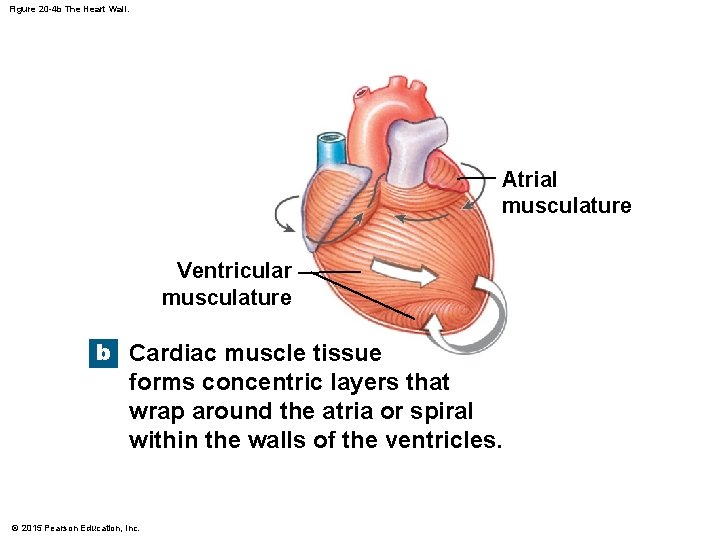
Figure 20 -4 b The Heart Wall. Atrial musculature Ventricular musculature b Cardiac muscle tissue forms concentric layers that wrap around the atria or spiral within the walls of the ventricles. © 2015 Pearson Education, Inc.
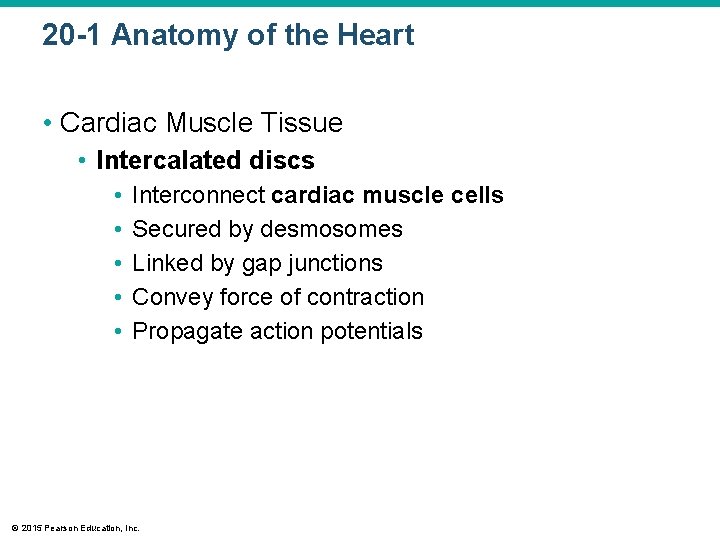
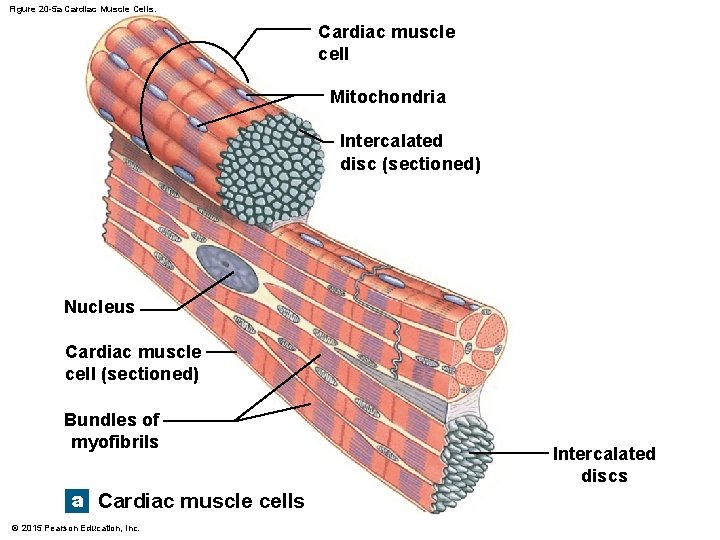
20 -1 Anatomy of the Heart • Cardiac Muscle Tissue • Intercalated discs • • • Interconnect cardiac muscle cells Secured by desmosomes Linked by gap junctions Convey force of contraction Propagate action potentials © 2015 Pearson Education, Inc.
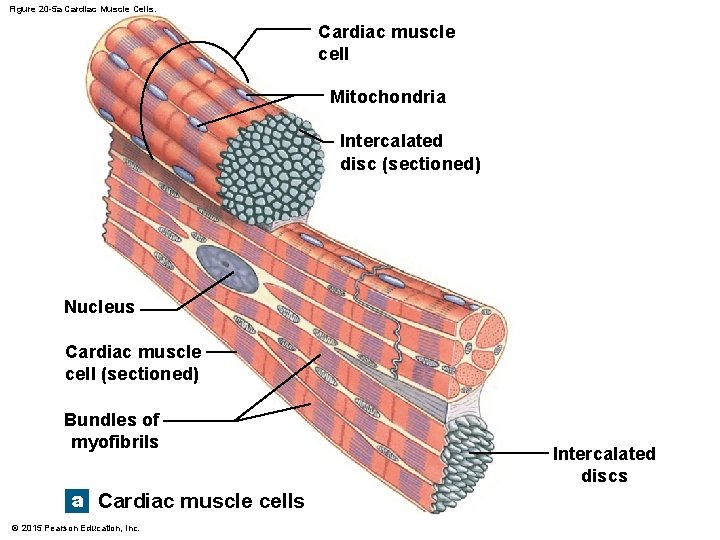
Figure 20 -5 a Cardiac Muscle Cells. Cardiac muscle cell Mitochondria Intercalated disc (sectioned) Nucleus Cardiac muscle cell (sectioned) Bundles of myofibrils a Cardiac muscle cells © 2015 Pearson Education, Inc. Intercalated discs
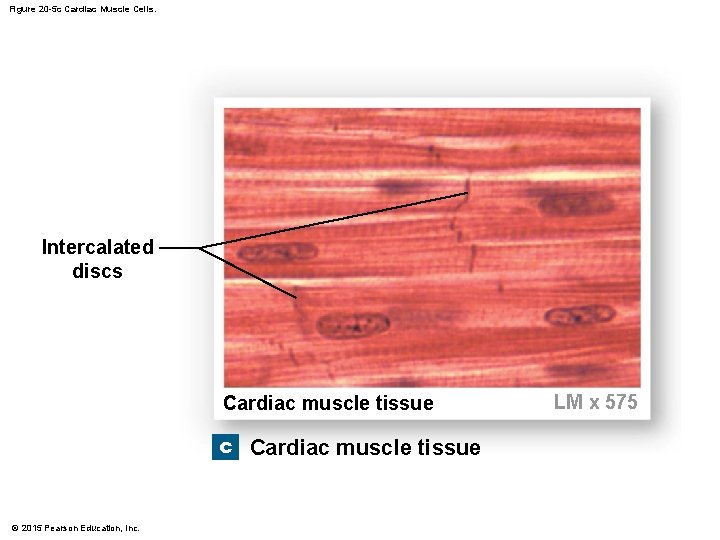
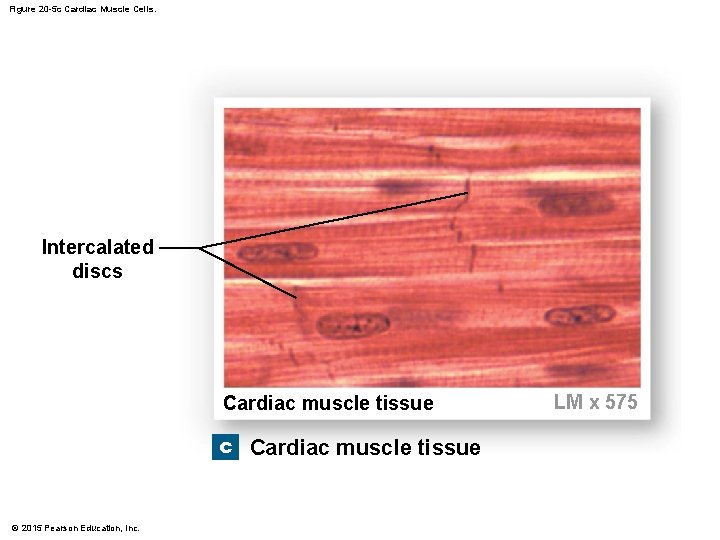
Figure 20 -5 c Cardiac Muscle Cells. Intercalated discs Cardiac muscle tissue c Cardiac muscle tissue © 2015 Pearson Education, Inc. LM x 575
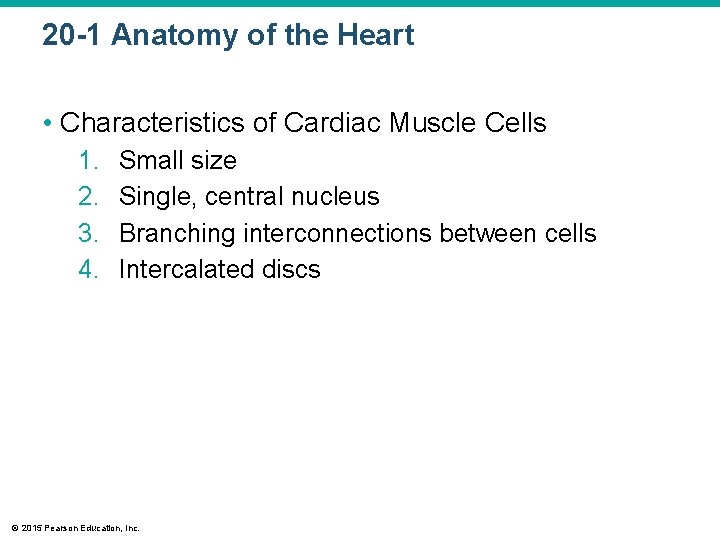
20 -1 Anatomy of the Heart • Characteristics of Cardiac Muscle Cells 1. 2. 3. 4. Small size Single, central nucleus Branching interconnections between cells Intercalated discs © 2015 Pearson Education, Inc.
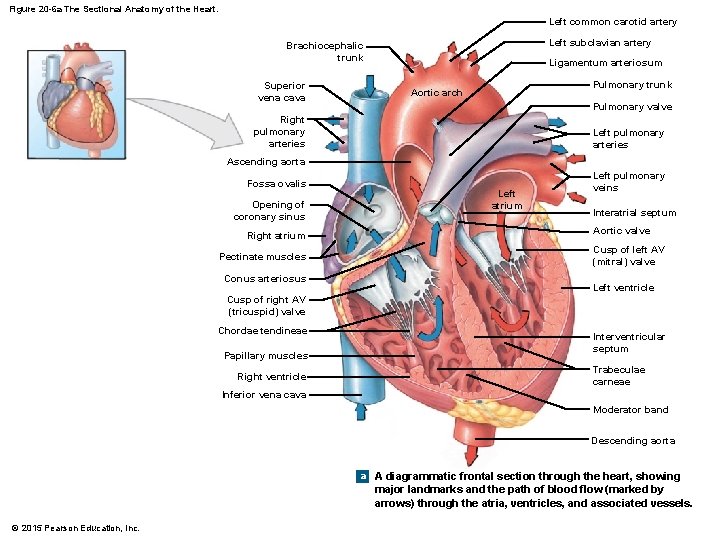
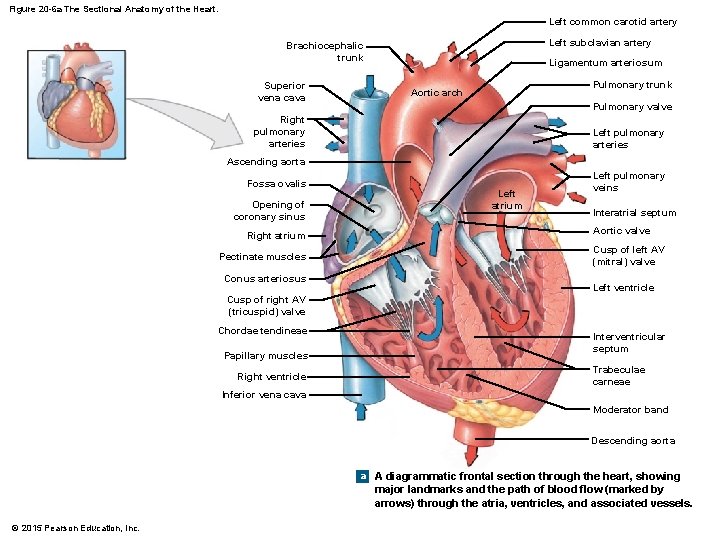
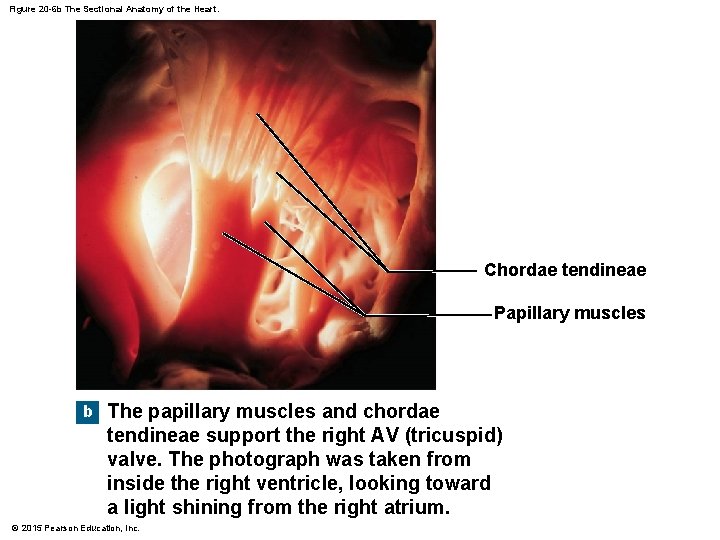
Figure 20 -6 a The Sectional Anatomy of the Heart. Left common carotid artery Left subclavian artery Brachiocephalic trunk Superior vena cava Ligamentum arteriosum Pulmonary trunk Aortic arch Pulmonary valve Right pulmonary arteries Left pulmonary arteries Ascending aorta Fossa ovalis Opening of coronary sinus Right atrium Pectinate muscles Conus arteriosus Left atrium Left pulmonary veins Interatrial septum Aortic valve Cusp of left AV (mitral) valve Left ventricle Cusp of right AV (tricuspid) valve Chordae tendineae Papillary muscles Right ventricle Interventricular septum Trabeculae carneae Inferior vena cava Moderator band Descending aorta a A diagrammatic frontal section through the heart, showing major landmarks and the path of blood flow (marked by arrows) through the atria, ventricles, and associated vessels. © 2015 Pearson Education, Inc.
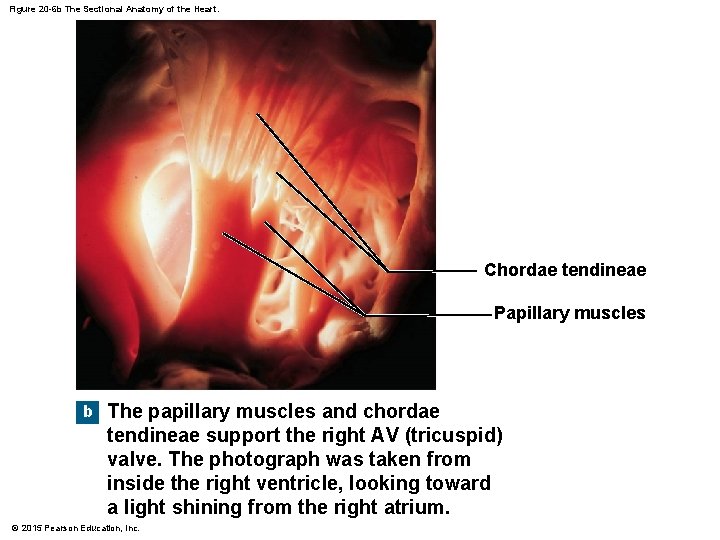
Figure 20 -6 b The Sectional Anatomy of the Heart. Chordae tendineae Papillary muscles b The papillary muscles and chordae tendineae support the right AV (tricuspid) valve. The photograph was taken from inside the right ventricle, looking toward a light shining from the right atrium. © 2015 Pearson Education, Inc.
20 -1 Anatomy of the Heart • The Pulmonary Circuit • Conus arteriosus (superior end of right ventricle) leads to pulmonary trunk • Pulmonary trunk divides into left and right pulmonary arteries • Blood flows from right ventricle to pulmonary trunk through pulmonary valve • Pulmonary valve has three semilunar cusps © 2015 Pearson Education, Inc.
20 -1 Anatomy of the Heart • The Left Atrium • Blood gathers into left and right pulmonary veins • Pulmonary veins deliver to left atrium • Blood from left atrium passes to left ventricle through left atrioventricular (AV) valve • A two-cusped bicuspid valve or mitral valve © 2015 Pearson Education, Inc.
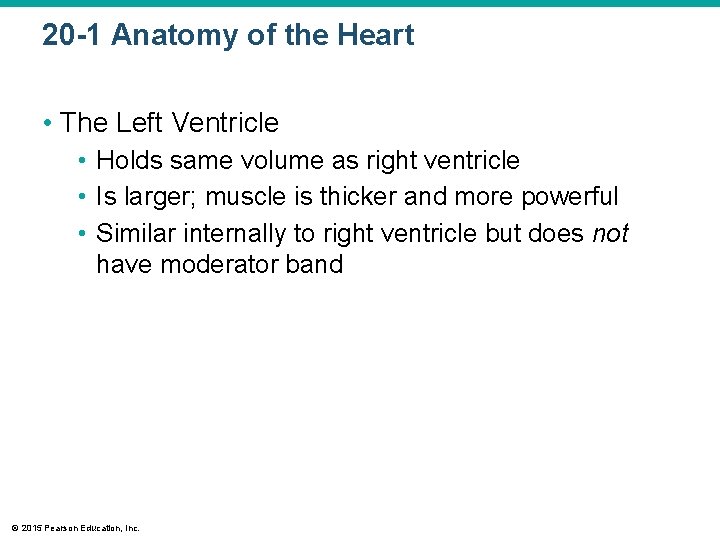
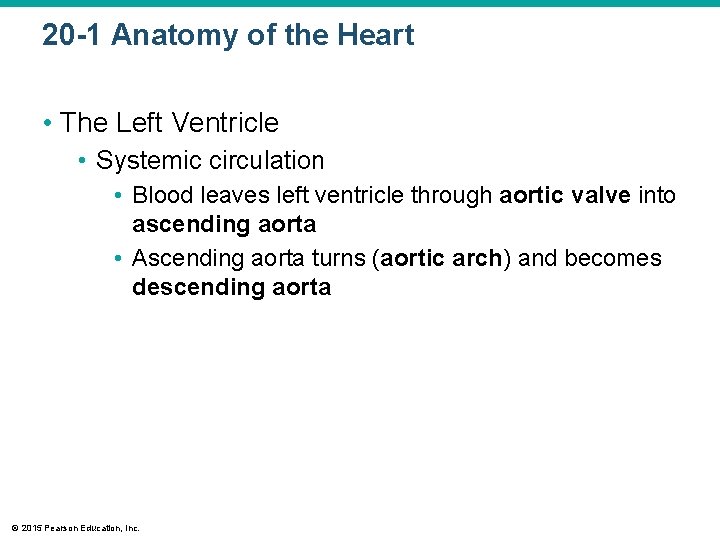
20 -1 Anatomy of the Heart • The Left Ventricle • Holds same volume as right ventricle • Is larger; muscle is thicker and more powerful • Similar internally to right ventricle but does not have moderator band © 2015 Pearson Education, Inc.
20 -1 Anatomy of the Heart • The Left Ventricle • Systemic circulation • Blood leaves left ventricle through aortic valve into ascending aorta • Ascending aorta turns (aortic arch) and becomes descending aorta © 2015 Pearson Education, Inc.
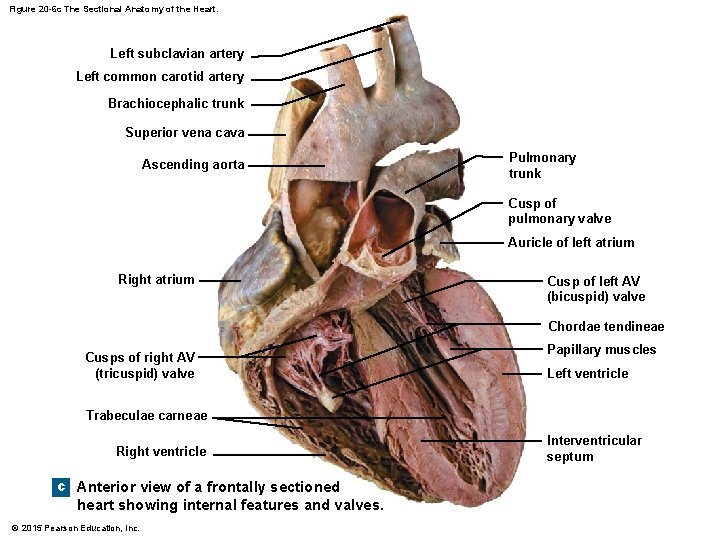
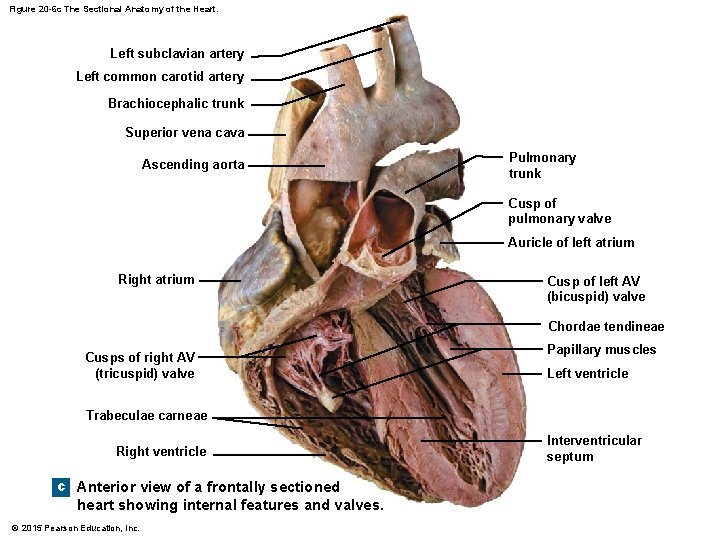
Figure 20 -6 c The Sectional Anatomy of the Heart. Left subclavian artery Left common carotid artery Brachiocephalic trunk Superior vena cava Ascending aorta Pulmonary trunk Cusp of pulmonary valve Auricle of left atrium Right atrium Cusp of left AV (bicuspid) valve Chordae tendineae Cusps of right AV (tricuspid) valve Papillary muscles Left ventricle Trabeculae carneae Right ventricle c Anterior view of a frontally sectioned heart showing internal features and valves. © 2015 Pearson Education, Inc. Interventricular septum
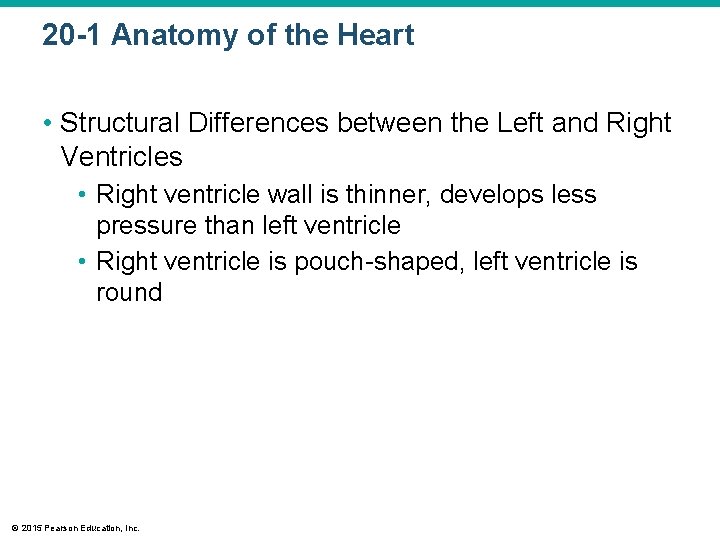
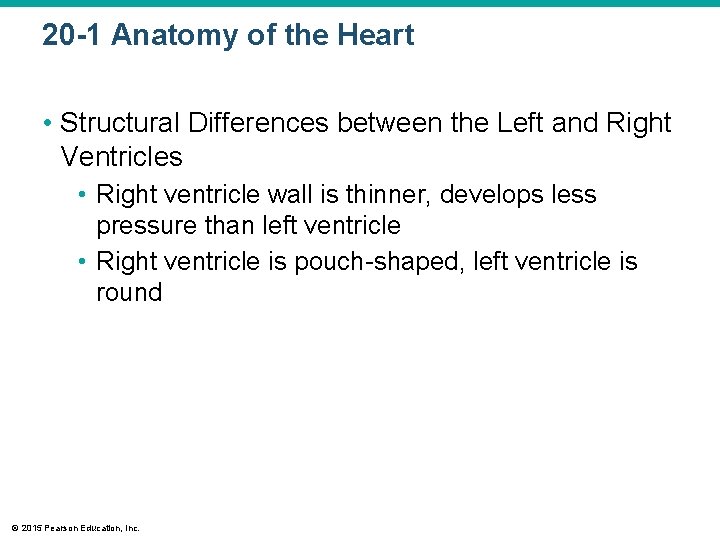
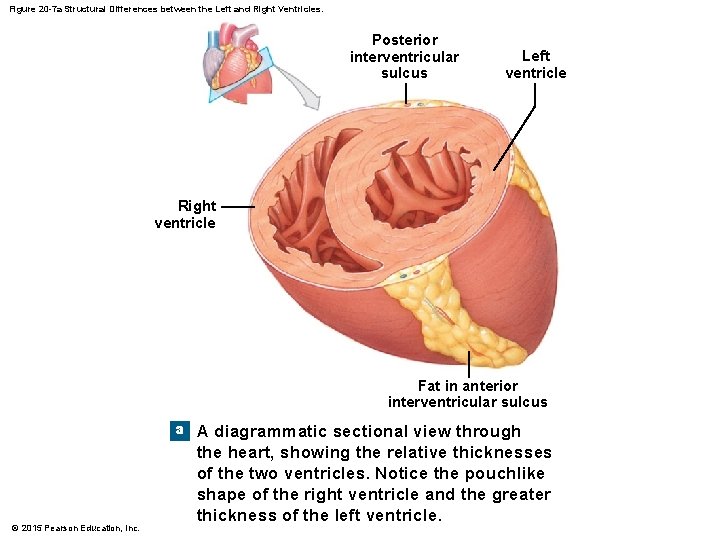
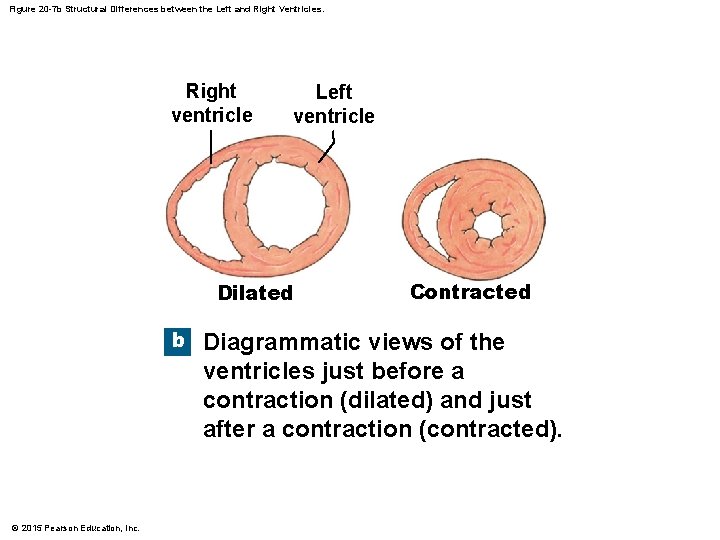
20 -1 Anatomy of the Heart • Structural Differences between the Left and Right Ventricles • Right ventricle wall is thinner, develops less pressure than left ventricle • Right ventricle is pouch-shaped, left ventricle is round © 2015 Pearson Education, Inc.
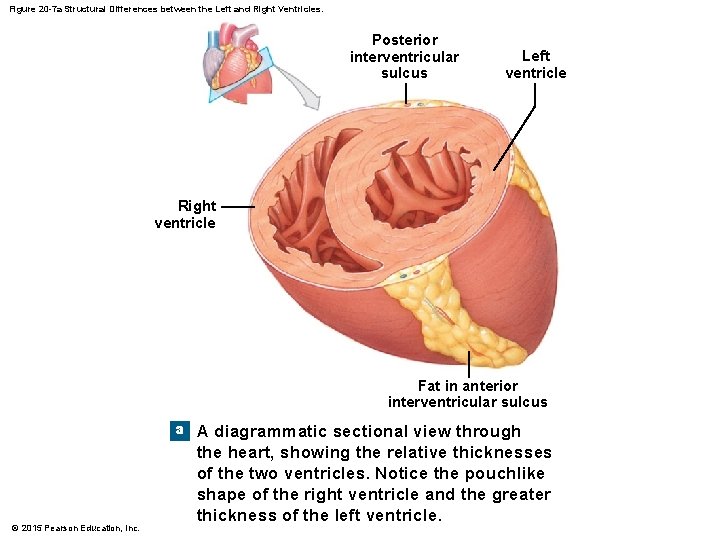
Figure 20 -7 a Structural Differences between the Left and Right Ventricles. Posterior interventricular sulcus Left ventricle Right ventricle Fat in anterior interventricular sulcus a © 2015 Pearson Education, Inc. A diagrammatic sectional view through the heart, showing the relative thicknesses of the two ventricles. Notice the pouchlike shape of the right ventricle and the greater thickness of the left ventricle.
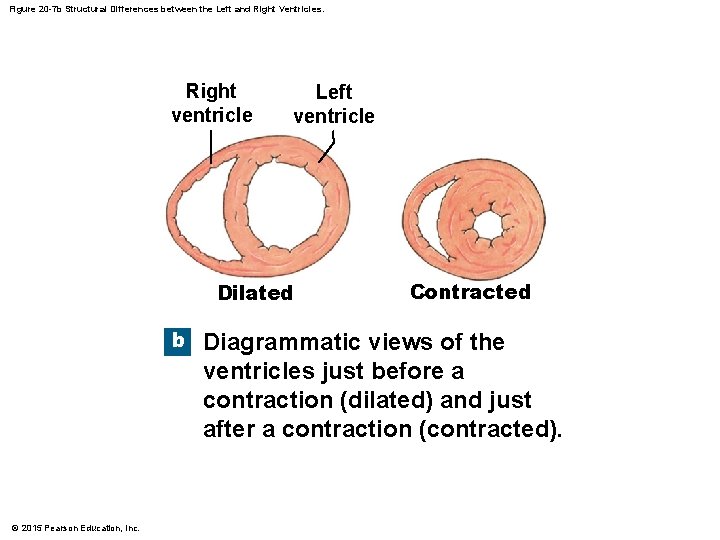
Figure 20 -7 b Structural Differences between the Left and Right Ventricles. Right ventricle Left ventricle Dilated b © 2015 Pearson Education, Inc. Contracted Diagrammatic views of the ventricles just before a contraction (dilated) and just after a contraction (contracted).
20 -1 Anatomy of the Heart • The Heart Valves • Two pairs of one-way valves prevent backflow during contraction • Atrioventricular (AV) valves • Between atria and ventricles • Blood pressure closes valve cusps during ventricular contraction • Papillary muscles tense chordae tendineae to prevent valves from swinging into atria © 2015 Pearson Education, Inc.
20 -1 Anatomy of the Heart • The Heart Valves • Semilunar valves • Pulmonary and aortic tricuspid valves • Prevent backflow from pulmonary trunk and aorta into ventricles • Have no muscular support • Three cusps support like tripod © 2015 Pearson Education, Inc.
20 -1 Anatomy of the Heart • Aortic Sinuses • At base of ascending aorta • Sacs that prevent valve cusps from sticking to aorta • Origin of right and left coronary arteries © 2015 Pearson Education, Inc.
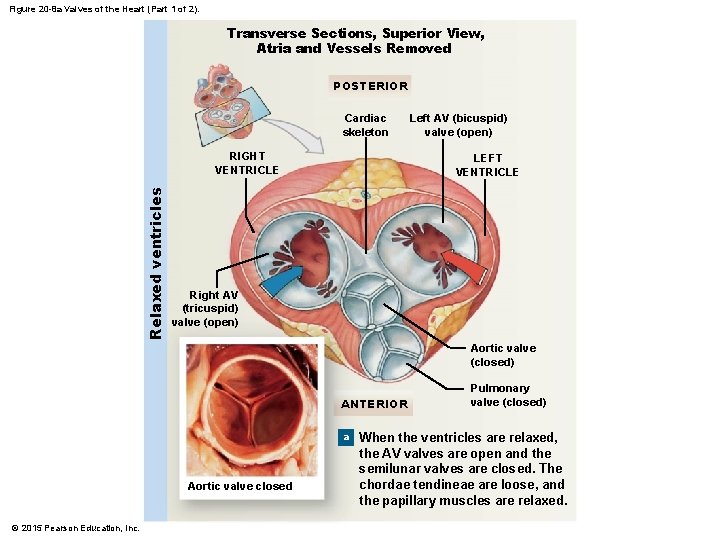
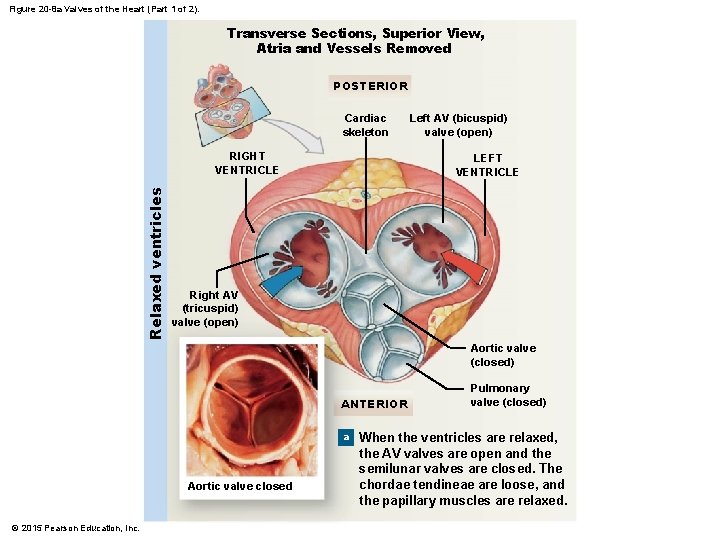
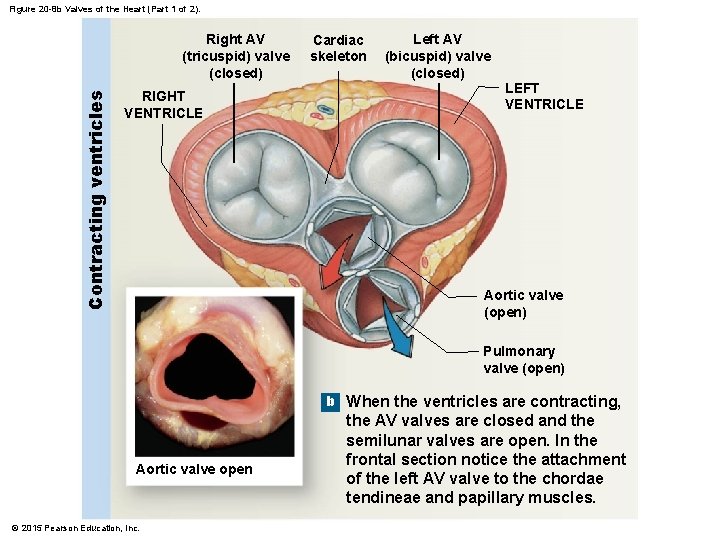
Figure 20 -8 a Valves of the Heart (Part 1 of 2). Transverse Sections, Superior View, Atria and Vessels Removed POSTERIOR Cardiac skeleton Relaxed ventricles RIGHT VENTRICLE Left AV (bicuspid) valve (open) LEFT VENTRICLE Right AV (tricuspid) valve (open) Aortic valve (closed) ANTERIOR a Aortic valve closed © 2015 Pearson Education, Inc. Pulmonary valve (closed) When the ventricles are relaxed, the AV valves are open and the semilunar valves are closed. The chordae tendineae are loose, and the papillary muscles are relaxed.
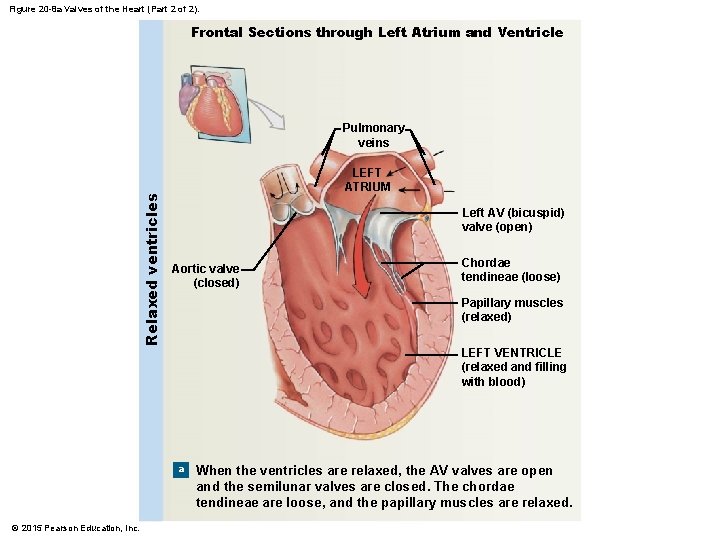
Figure 20 -8 a Valves of the Heart (Part 2 of 2). Frontal Sections through Left Atrium and Ventricle Relaxed ventricles Pulmonary veins LEFT ATRIUM Left AV (bicuspid) valve (open) Aortic valve (closed) Chordae tendineae (loose) Papillary muscles (relaxed) LEFT VENTRICLE (relaxed and filling with blood) a © 2015 Pearson Education, Inc. When the ventricles are relaxed, the AV valves are open and the semilunar valves are closed. The chordae tendineae are loose, and the papillary muscles are relaxed.
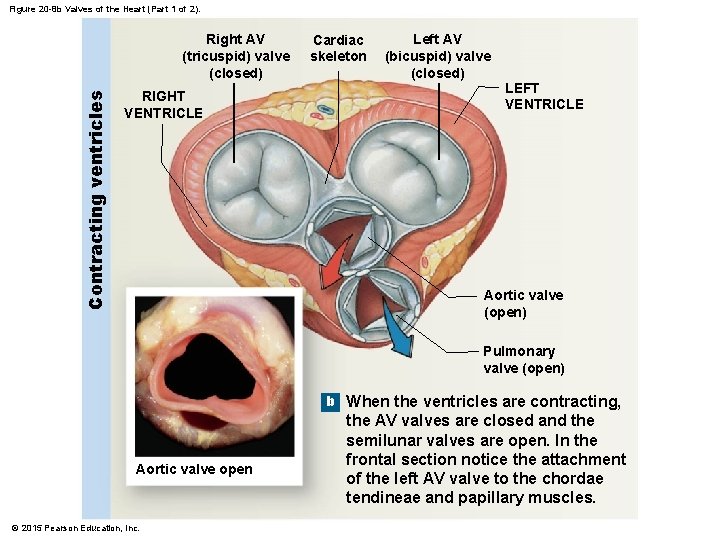
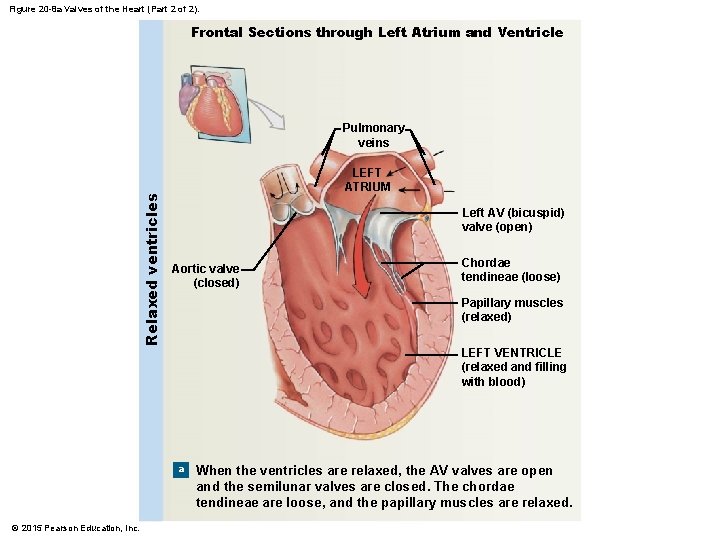
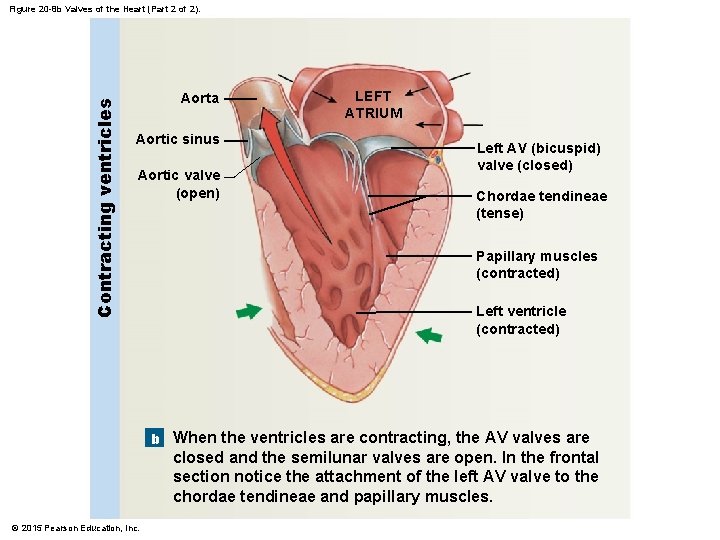
Figure 20 -8 b Valves of the Heart (Part 1 of 2). Contracting ventricles Right AV (tricuspid) valve (closed) RIGHT VENTRICLE Cardiac skeleton Left AV (bicuspid) valve (closed) LEFT VENTRICLE Aortic valve (open) Pulmonary valve (open) b When the ventricles are contracting, Aortic valve open © 2015 Pearson Education, Inc. the AV valves are closed and the semilunar valves are open. In the frontal section notice the attachment of the left AV valve to the chordae tendineae and papillary muscles.
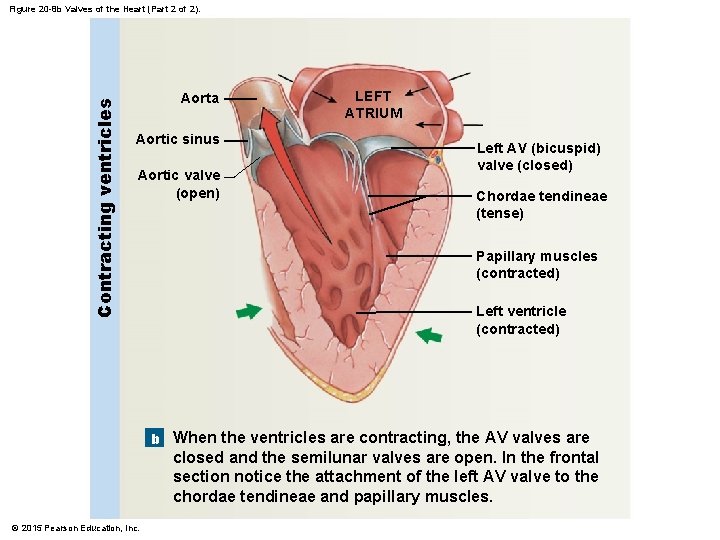
Contracting ventricles Figure 20 -8 b Valves of the Heart (Part 2 of 2). Aorta Aortic sinus Aortic valve (open) LEFT ATRIUM Left AV (bicuspid) valve (closed) Chordae tendineae (tense) Papillary muscles (contracted) Left ventricle (contracted) b When the ventricles are contracting, the AV valves are closed and the semilunar valves are open. In the frontal section notice the attachment of the left AV valve to the chordae tendineae and papillary muscles. © 2015 Pearson Education, Inc.
20 -1 Anatomy of the Heart • Connective Tissues and the Cardiac Skeleton • Connective tissue fibers 1. 2. 3. 4. © 2015 Pearson Education, Inc. Physically support cardiac muscle fibers Distribute forces of contraction Add strength and prevent overexpansion of heart Provide elasticity that helps return heart to original size and shape after contraction

20 -1 Anatomy of the Heart • The Cardiac Skeleton • Four bands around heart valves and bases of pulmonary trunk and aorta • Stabilize valves • Electrically insulate ventricular cells from atrial cells © 2015 Pearson Education, Inc.

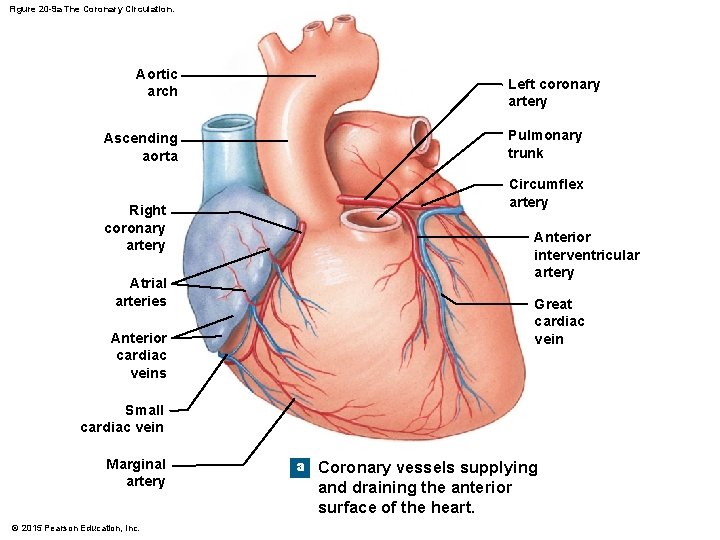
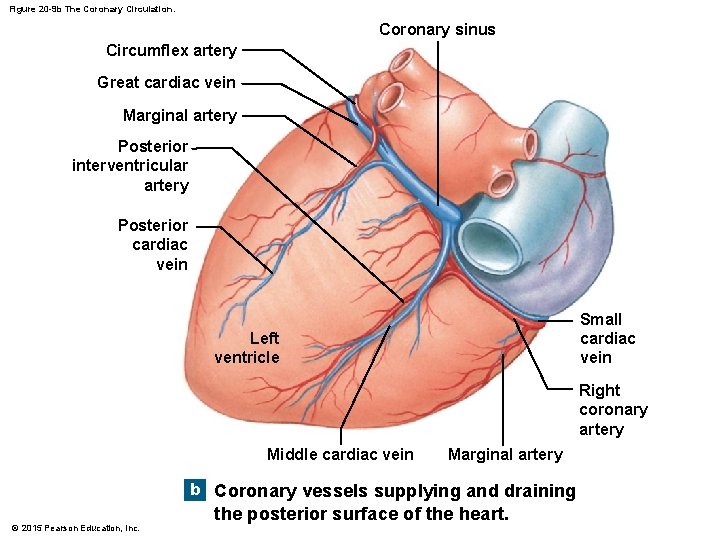
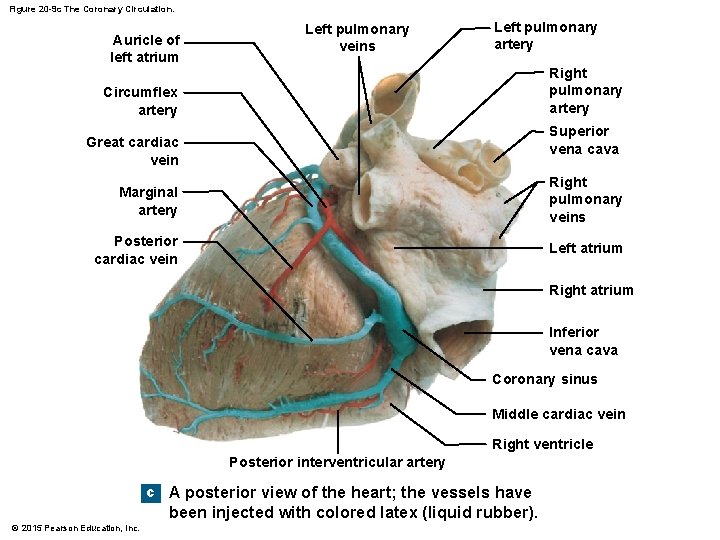
20 -1 Anatomy of the Heart • The Blood Supply to the Heart • = Coronary circulation • Supplies blood to muscle tissue of heart • Coronary arteries and cardiac veins © 2015 Pearson Education, Inc.
20 -1 Anatomy of the Heart • The Coronary Arteries • Left and right • Originate at aortic sinuses • High blood pressure, elastic rebound forces blood through coronary arteries between contractions © 2015 Pearson Education, Inc.
20 -1 Anatomy of the Heart • Right Coronary Artery • Supplies blood to: • • • Right atrium Portions of both ventricles Cells of sinoatrial (SA) and atrioventricular nodes Marginal arteries (surface of right ventricle) Posterior interventricular artery © 2015 Pearson Education, Inc.
20 -1 Anatomy of the Heart • Left Coronary Artery • Supplies blood to: • Left ventricle • Left atrium • Interventricular septum © 2015 Pearson Education, Inc.
20 -1 Anatomy of the Heart • Two Main Branches of Left Coronary Artery 1. Circumflex artery 2. Anterior interventricular artery • Arterial Anastomoses • Interconnect anterior and posterior interventricular arteries • Stabilize blood supply to cardiac muscle © 2015 Pearson Education, Inc.
20 -1 Anatomy of the Heart • The Cardiac Veins • Great cardiac vein • Drains blood from area of anterior interventricular artery into coronary sinus • Anterior cardiac veins • Empty into right atrium • Posterior cardiac vein, middle cardiac vein, and small cardiac vein • Empty into great cardiac vein or coronary sinus © 2015 Pearson Education, Inc.
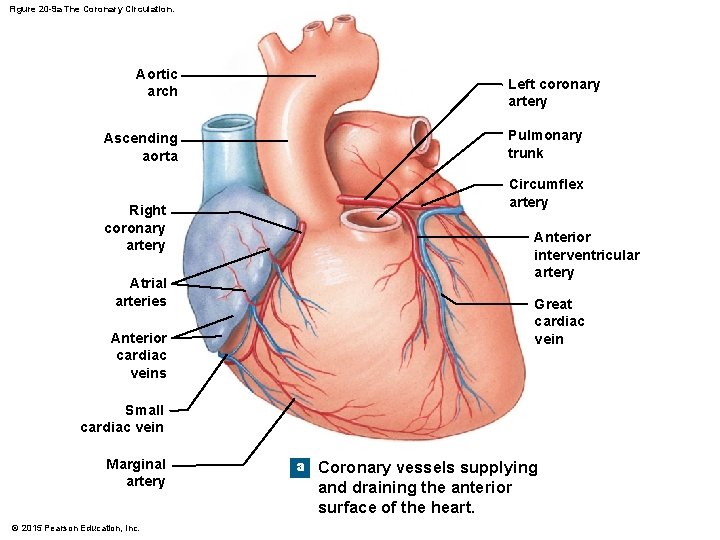
Figure 20 -9 a The Coronary Circulation. Aortic arch Ascending aorta Right coronary artery Left coronary artery Pulmonary trunk Circumflex artery Anterior interventricular artery Atrial arteries Great cardiac vein Anterior cardiac veins Small cardiac vein Marginal artery © 2015 Pearson Education, Inc. a Coronary vessels supplying and draining the anterior surface of the heart.
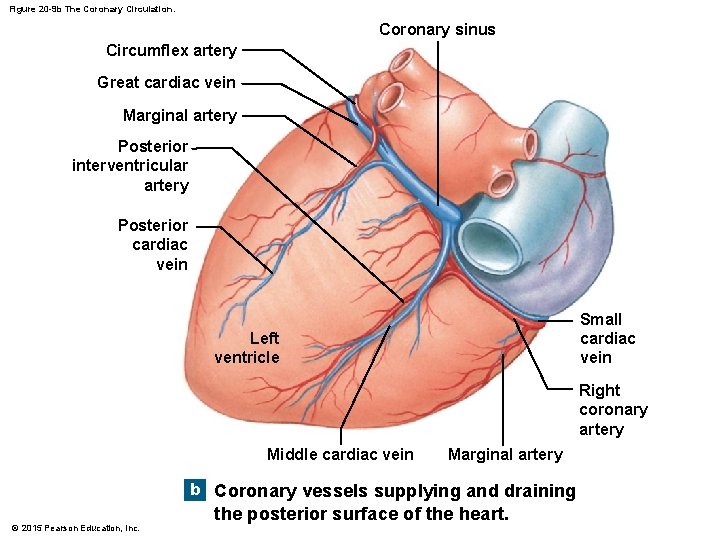
Figure 20 -9 b The Coronary Circulation. Coronary sinus Circumflex artery Great cardiac vein Marginal artery Posterior interventricular artery Posterior cardiac vein Small cardiac vein Left ventricle Right coronary artery Middle cardiac vein Marginal artery b Coronary vessels supplying and draining © 2015 Pearson Education, Inc. the posterior surface of the heart.
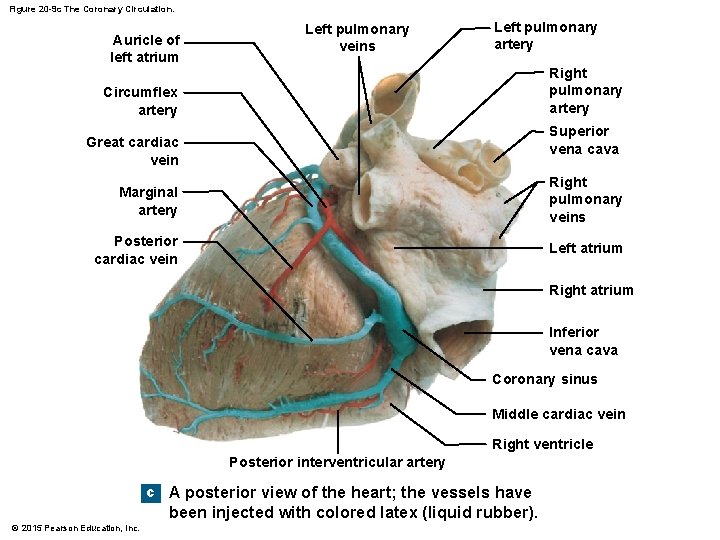
Figure 20 -9 c The Coronary Circulation. Auricle of left atrium Left pulmonary veins Left pulmonary artery Right pulmonary artery Circumflex artery Superior vena cava Great cardiac vein Marginal artery Right pulmonary veins Posterior cardiac vein Left atrium Right atrium Inferior vena cava Coronary sinus Middle cardiac vein Right ventricle Posterior interventricular artery c A posterior view of the heart; the vessels have been injected with colored latex (liquid rubber). © 2015 Pearson Education, Inc.
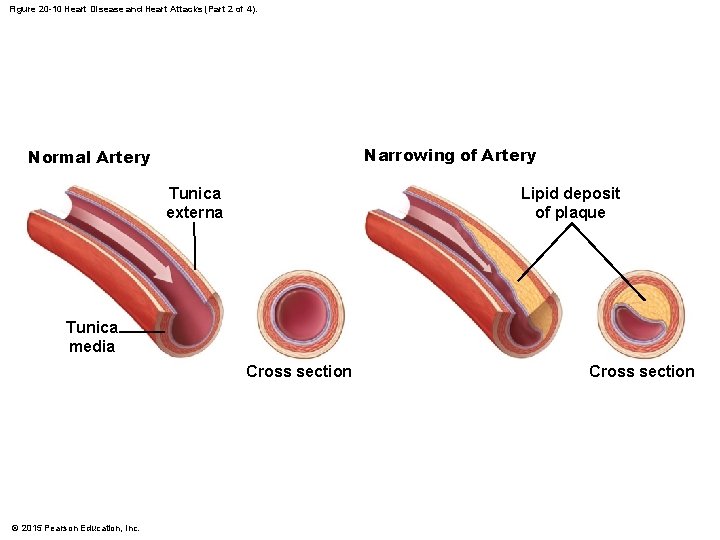
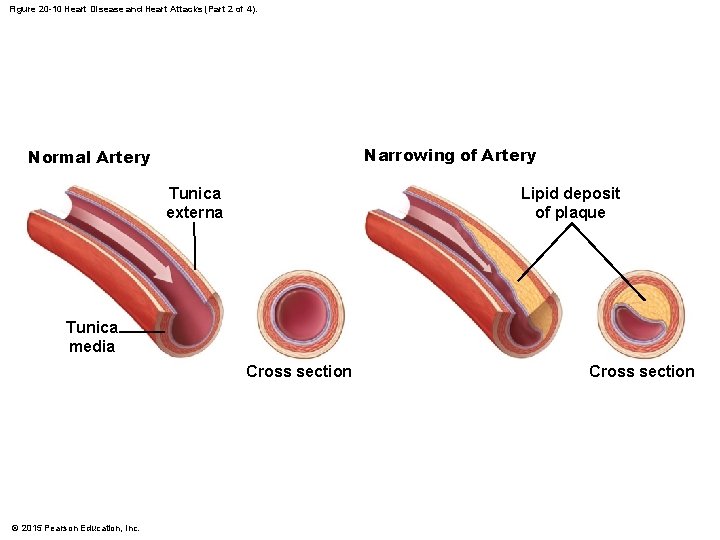
Figure 20 -10 Heart Disease and Heart Attacks (Part 2 of 4). Narrowing of Artery Normal Artery Tunica externa Lipid deposit of plaque Tunica media Cross section © 2015 Pearson Education, Inc. Cross section
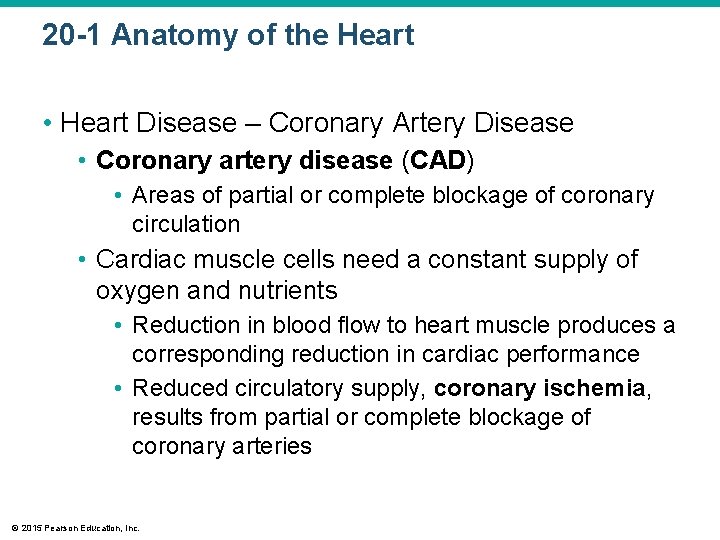
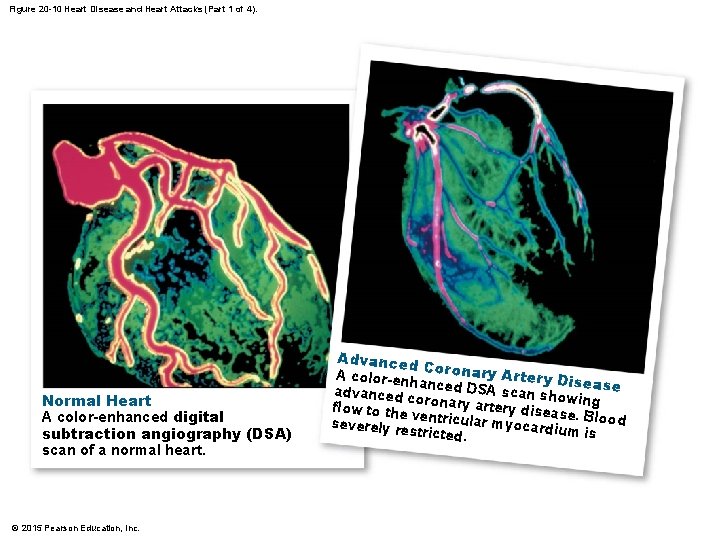
20 -1 Anatomy of the Heart • Heart Disease – Coronary Artery Disease • Coronary artery disease (CAD) • Areas of partial or complete blockage of coronary circulation • Cardiac muscle cells need a constant supply of oxygen and nutrients • Reduction in blood flow to heart muscle produces a corresponding reduction in cardiac performance • Reduced circulatory supply, coronary ischemia, results from partial or complete blockage of coronary arteries © 2015 Pearson Education, Inc.
20 -1 Anatomy of the Heart • Heart Disease – Coronary Artery Disease • Usual cause is formation of a fatty deposit, or atherosclerotic plaque, in the wall of a coronary vessel • The plaque, or an associated thrombus (clot), then narrows the passageway and reduces blood flow • Spasms in smooth muscles of vessel wall can further decrease or stop blood flow • One of the first symptoms of CAD is commonly angina pectoris © 2015 Pearson Education, Inc.
20 -1 Anatomy of the Heart • Heart Disease – Coronary Artery Disease • Angina pectoris • In its most common form, a temporary ischemia develops when the workload of the heart increases • Although the individual may feel comfortable at rest, exertion or emotional stress can produce a sensation of pressure, chest constriction, and pain that may radiate from the sternal area to the arms, back, and neck © 2015 Pearson Education, Inc.
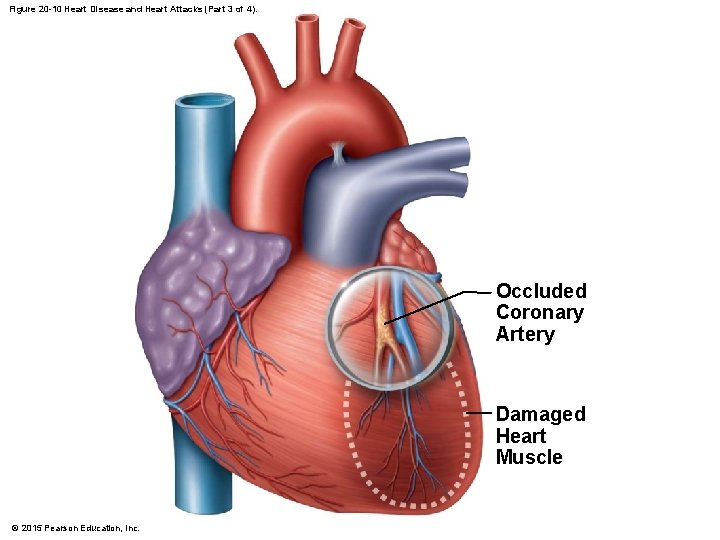
20 -1 Anatomy of the Heart • Heart Disease – Coronary Artery Disease • Myocardial infarction (MI), or heart attack • Part of the coronary circulation becomes blocked, and cardiac muscle cells die from lack of oxygen • The death of affected tissue creates a nonfunctional area known as an infarct • Heart attacks most commonly result from severe coronary artery disease (CAD) © 2015 Pearson Education, Inc.

20 -1 Anatomy of the Heart • Heart Disease – Coronary Artery Disease • Myocardial infarction (MI), or heart attack • Consequences depend on the site and nature of the circulatory blockage • If it occurs near the start of one of the coronary arteries: • The damage will be widespread and the heart may stop beating • If the blockage involves one of the smaller arterial branches: • The individual may survive the immediate crisis but may have many complications such as reduced contractility and cardiac arrhythmias © 2015 Pearson Education, Inc.
20 -1 Anatomy of the Heart • Heart Disease – Coronary Artery Disease • Myocardial infarction (MI), or heart attack • A crisis often develops as a result of thrombus formation at a plaque (the most common cause of an MI), a condition called coronary thrombosis • A vessel already narrowed by plaque formation may also become blocked by a sudden spasm in the smooth muscles of the vascular wall • Individuals having an MI experience intense pain, similar to that felt in angina, but persisting even at rest © 2015 Pearson Education, Inc.
20 -1 Anatomy of the Heart • Heart Disease – Coronary Artery Disease • Myocardial infarction (MI), or heart attack • Pain does not always accompany a heart attack; therefore, the condition may go undiagnosed and may not be treated before a fatal MI occurs • A myocardial infarction can usually be diagnosed with an ECG and blood studies • Damaged myocardial cells release enzymes into the circulation, and these elevated enzymes can be measured in diagnostic blood tests • The enzymes include: • Cardiac troponin T, • Cardiac troponin I, • A special form of creatinine phosphokinase, CK-MB © 2015 Pearson Education, Inc.
20 -1 Anatomy of the Heart • Heart Disease – Coronary Artery Disease • Treatment of CAD and myocardial infarction • About 25 percent of MI patients die before obtaining medical assistance • 65 percent of MI deaths among those under age 50 occur within an hour after the initial infarction © 2015 Pearson Education, Inc.
20 -1 Anatomy of the Heart • Heart Disease – Coronary Artery Disease • Treatment of CAD and myocardial infarction • Risk factor modification • Stop smoking • High blood pressure treatment • Dietary modification to lower cholesterol and promote weight loss • Stress reduction • Increased physical activity (where appropriate) © 2015 Pearson Education, Inc.
20 -1 Anatomy of the Heart • Heart Disease – Coronary Artery Disease • Treatment of CAD and myocardial infarction • Drug treatment • Drugs that reduce coagulation and therefore the risk of thrombosis, such as aspirin and coumadin • Drugs that block sympathetic stimulation (propranolol or metoprolol) • Drugs that cause vasodilation, such as nitroglycerin • Drugs that block calcium movement into the cardiac and vascular smooth muscle cells (calcium channel blockers) • In a myocardial infarction, drugs to relieve pain, fibrinolytic agents to help dissolve clots, and oxygen © 2015 Pearson Education, Inc.
20 -1 Anatomy of the Heart • Heart Disease – Coronary Artery Disease • Treatment of CAD and myocardial infarction • Noninvasive surgery • Atherectomy • Blockage by a single, soft plaque may be reduced with the aid of a long, slender catheter inserted into a coronary artery to the plaque © 2015 Pearson Education, Inc.
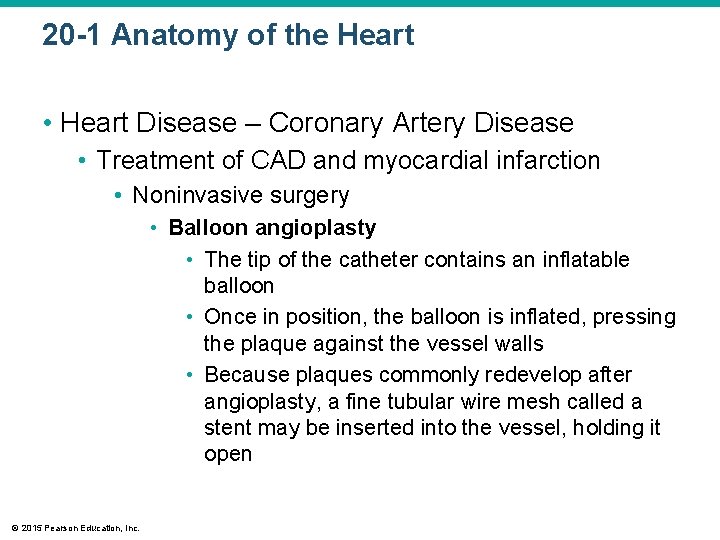
20 -1 Anatomy of the Heart • Heart Disease – Coronary Artery Disease • Treatment of CAD and myocardial infarction • Noninvasive surgery • Balloon angioplasty • The tip of the catheter contains an inflatable balloon • Once in position, the balloon is inflated, pressing the plaque against the vessel walls • Because plaques commonly redevelop after angioplasty, a fine tubular wire mesh called a stent may be inserted into the vessel, holding it open © 2015 Pearson Education, Inc.
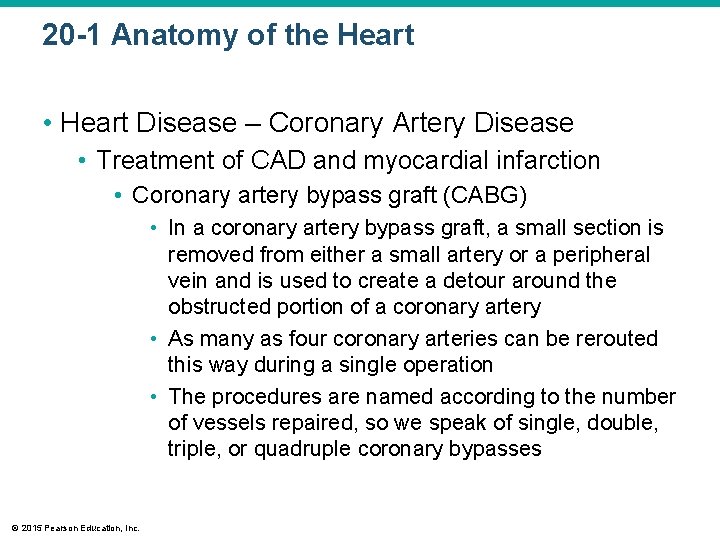
20 -1 Anatomy of the Heart • Heart Disease – Coronary Artery Disease • Treatment of CAD and myocardial infarction • Coronary artery bypass graft (CABG) • In a coronary artery bypass graft, a small section is removed from either a small artery or a peripheral vein and is used to create a detour around the obstructed portion of a coronary artery • As many as four coronary arteries can be rerouted this way during a single operation • The procedures are named according to the number of vessels repaired, so we speak of single, double, triple, or quadruple coronary bypasses © 2015 Pearson Education, Inc.
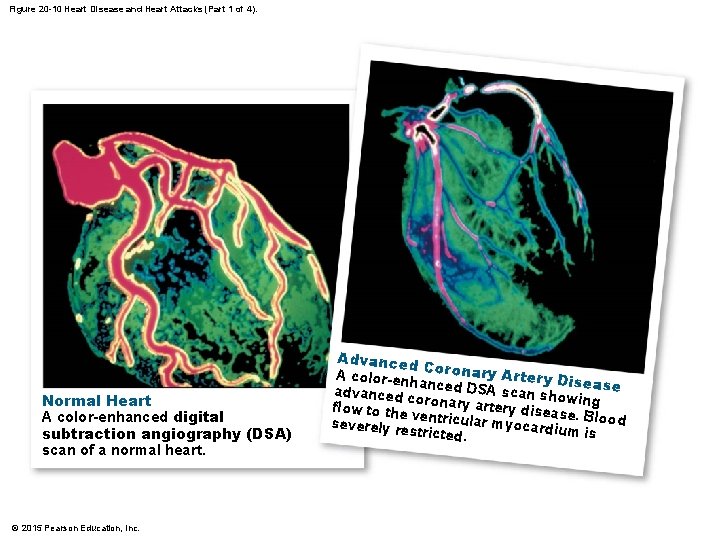
Figure 20 -10 Heart Disease and Heart Attacks (Part 1 of 4). Normal Heart A color-enhanced digital subtraction angiography (DSA) scan of a normal heart. © 2015 Pearson Education, Inc. Advanced Coronary A color-en hanced DS Artery Disease A advanced c oronary ar scan showing te flow to the ventricular ry disease. Blood severely re myocardiu m is stricted.
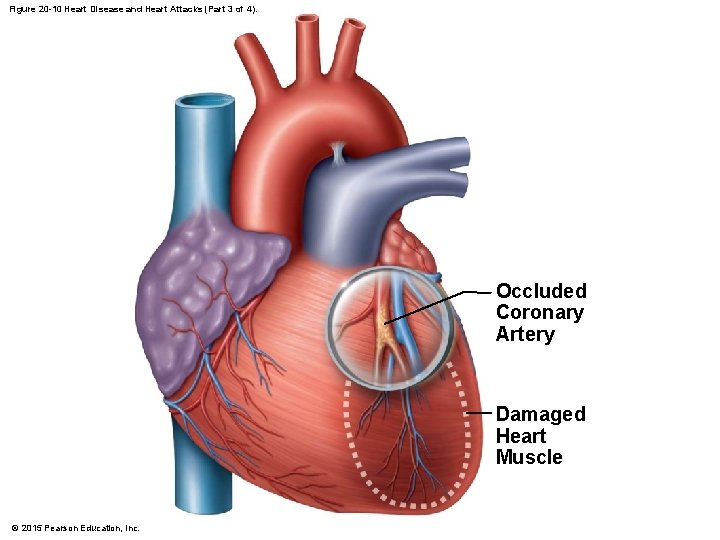
Figure 20 -10 Heart Disease and Heart Attacks (Part 3 of 4). Occluded Coronary Artery Damaged Heart Muscle © 2015 Pearson Education, Inc.
20 -2 The Conducting System • Heartbeat • A single contraction of the heart • The entire heart contracts in series • First the atria • Then the ventricles © 2015 Pearson Education, Inc.
20 -2 The Conducting System • Cardiac Physiology • Two types of cardiac muscle cells 1. Conducting system • Controls and coordinates heartbeat 2. Contractile cells • Produce contractions that propel blood © 2015 Pearson Education, Inc.
20 -2 The Conducting System • The Cardiac Cycle • Begins with action potential at SA node • Transmitted through conducting system • Produces action potentials in cardiac muscle cells (contractile cells) • Electrocardiogram (ECG or EKG) • Electrical events in the cardiac cycle can be recorded on an electrocardiogram © 2015 Pearson Education, Inc.
20 -2 The Conducting System • A system of specialized cardiac muscle cells • Initiates and distributes electrical impulses that stimulate contraction • Automaticity • Cardiac muscle tissue contracts automatically © 2015 Pearson Education, Inc.
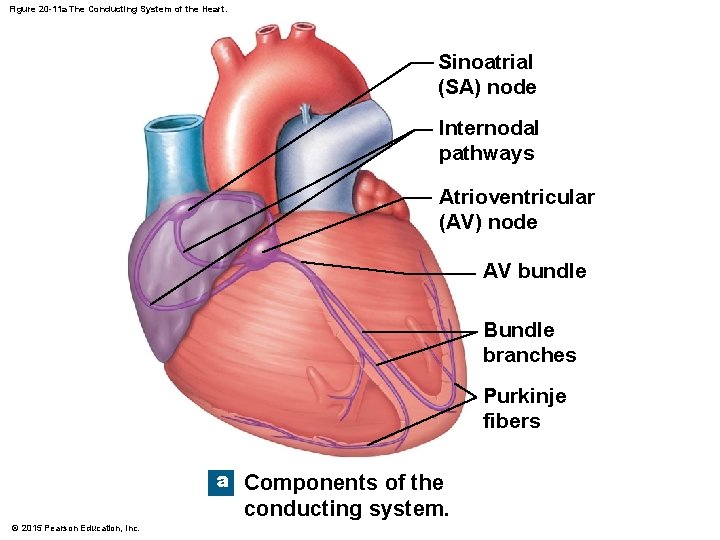
20 -2 The Conducting System • Structures of the Conducting System • Sinoatrial (SA) node – wall of right atrium • Atrioventricular (AV) node – junction between atria and ventricles • Conducting cells – throughout myocardium © 2015 Pearson Education, Inc.
20 -2 The Conducting System • Conducting Cells • Interconnect SA and AV nodes • Distribute stimulus through myocardium • In the atria • Internodal pathways • In the ventricles • AV bundle and the bundle branches © 2015 Pearson Education, Inc.
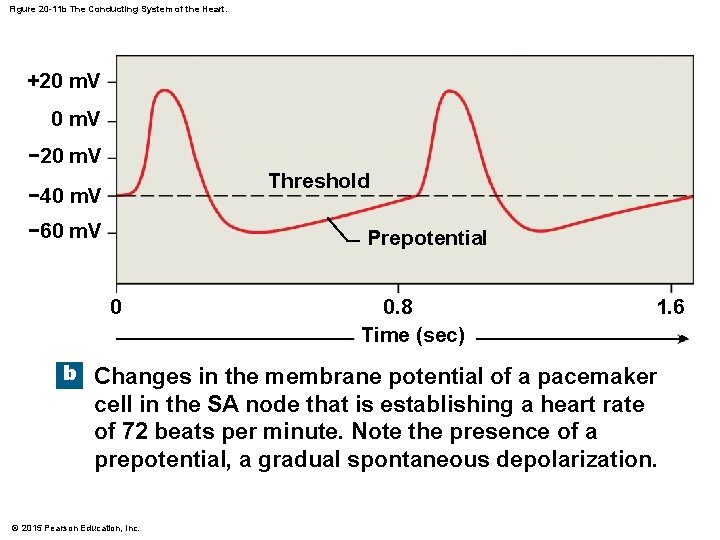
20 -2 The Conducting System • Prepotential • Also called pacemaker potential • Resting potential of conducting cells • Gradually depolarizes toward threshold • SA node depolarizes first, establishing heart rate © 2015 Pearson Education, Inc.
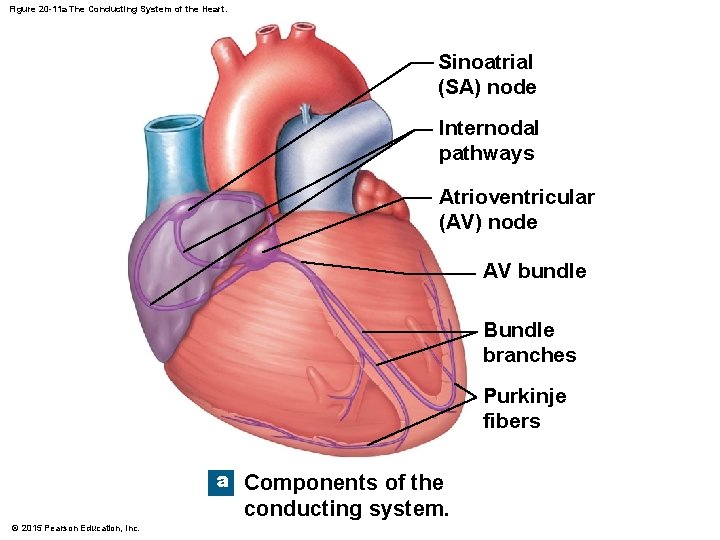
Figure 20 -11 a The Conducting System of the Heart. Sinoatrial (SA) node Internodal pathways Atrioventricular (AV) node AV bundle Bundle branches Purkinje fibers a Components of the conducting system. © 2015 Pearson Education, Inc.
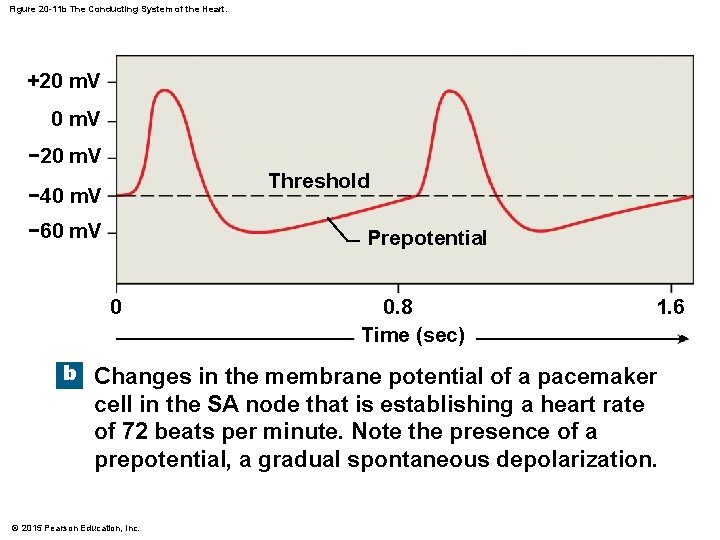
Figure 20 -11 b The Conducting System of the Heart. +20 m. V − 20 m. V Threshold − 40 m. V − 60 m. V Prepotential 0 0. 8 Time (sec) 1. 6 b Changes in the membrane potential of a pacemaker cell in the SA node that is establishing a heart rate of 72 beats per minute. Note the presence of a prepotential, a gradual spontaneous depolarization. © 2015 Pearson Education, Inc.
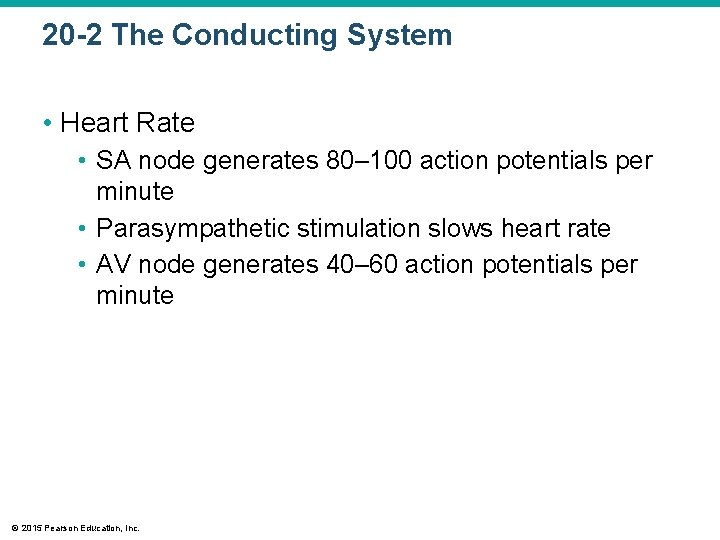
20 -2 The Conducting System • Heart Rate • SA node generates 80– 100 action potentials per minute • Parasympathetic stimulation slows heart rate • AV node generates 40– 60 action potentials per minute © 2015 Pearson Education, Inc.
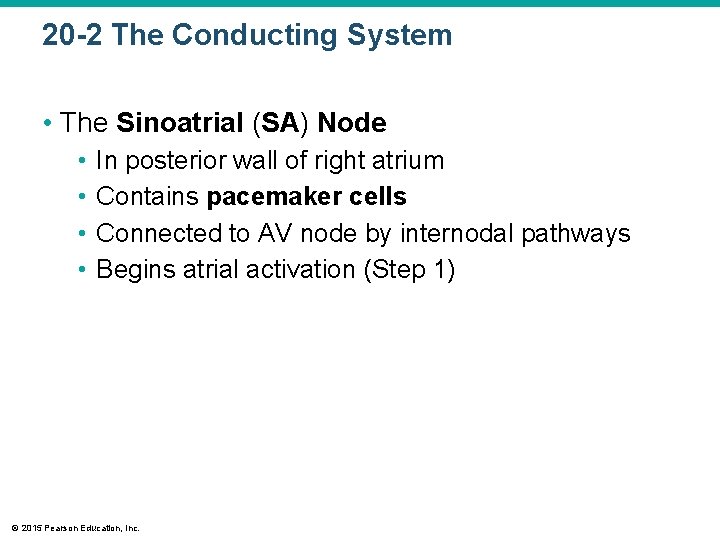
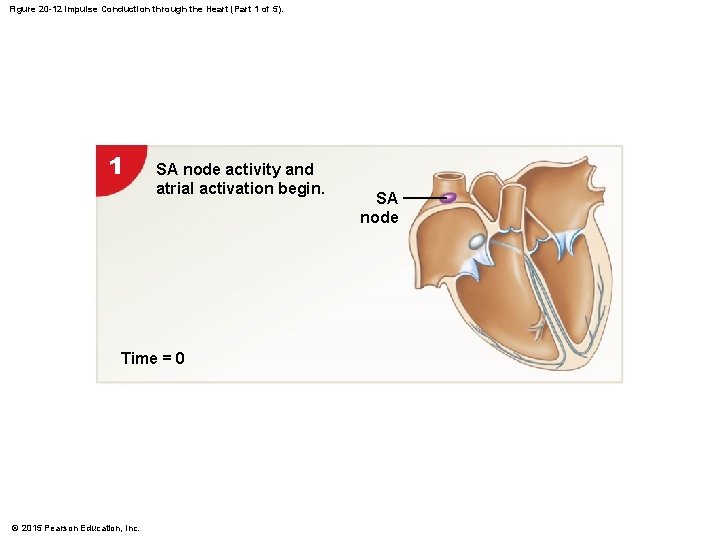
20 -2 The Conducting System • The Sinoatrial (SA) Node • • In posterior wall of right atrium Contains pacemaker cells Connected to AV node by internodal pathways Begins atrial activation (Step 1) © 2015 Pearson Education, Inc.
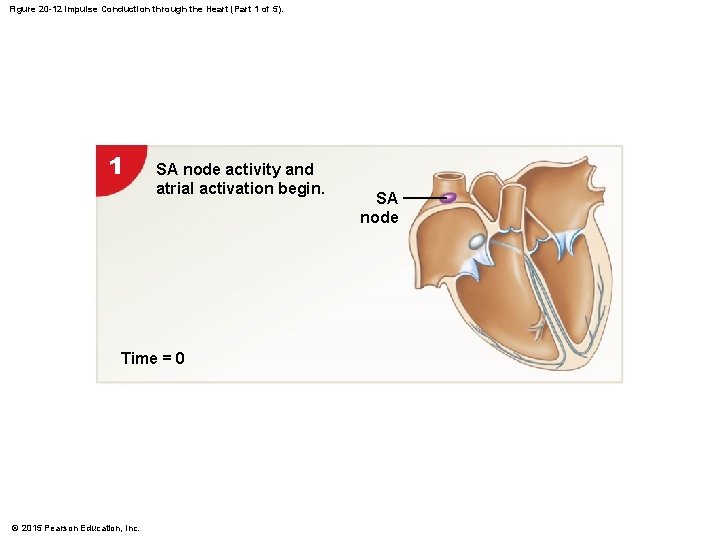
Figure 20 -12 Impulse Conduction through the Heart (Part 1 of 5). 1 SA node activity and atrial activation begin. Time = 0 © 2015 Pearson Education, Inc. SA node
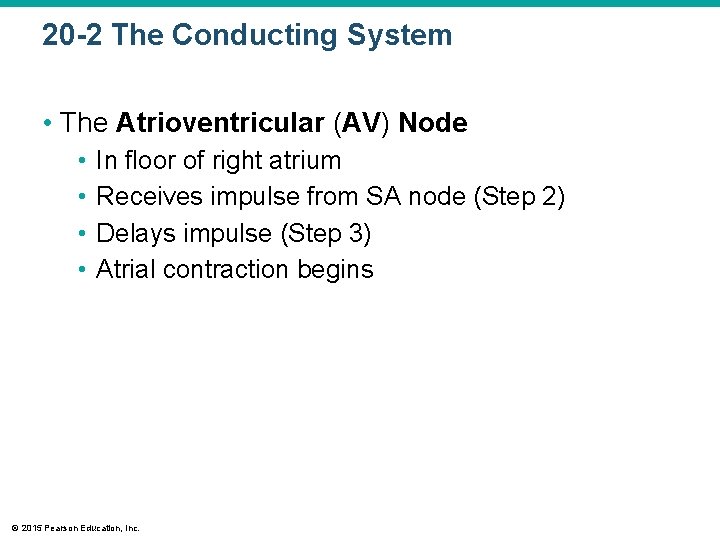
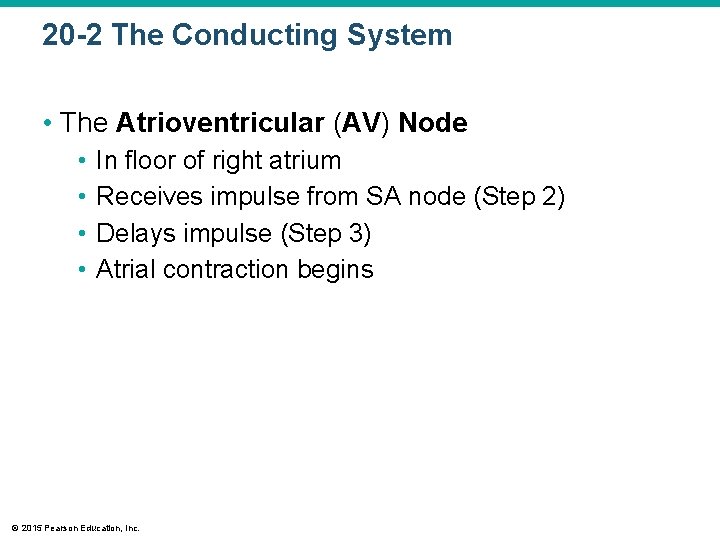
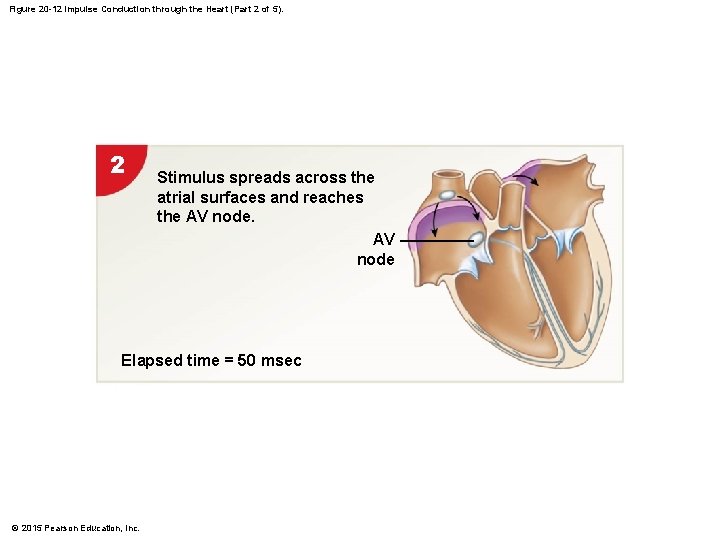
20 -2 The Conducting System • The Atrioventricular (AV) Node • • In floor of right atrium Receives impulse from SA node (Step 2) Delays impulse (Step 3) Atrial contraction begins © 2015 Pearson Education, Inc.
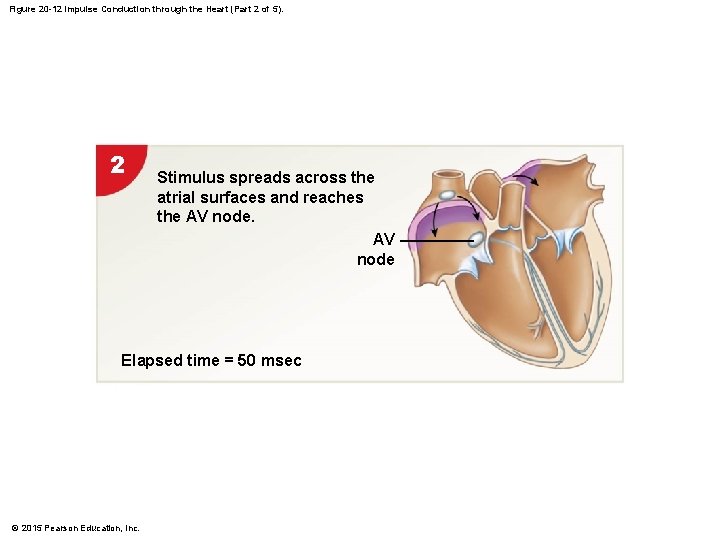
Figure 20 -12 Impulse Conduction through the Heart (Part 2 of 5). 2 Stimulus spreads across the atrial surfaces and reaches the AV node Elapsed time = 50 msec © 2015 Pearson Education, Inc.

Figure 20 -12 Impulse Conduction through the Heart (Part 3 of 5). 3 There is a 100 -msec delay at the AV node. Atrial contraction begins. AV bundle Bundle branches Elapsed time = 150 msec © 2015 Pearson Education, Inc.

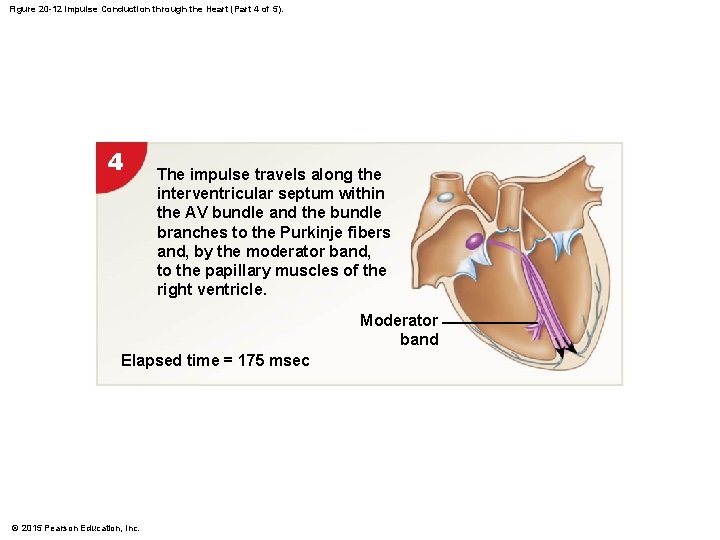
20 -2 The Conducting System • The AV Bundle • In the septum • Carries impulse to left and right bundle branches • Which conduct to Purkinje fibers (Step 4) • And to the moderator band • Which conducts to papillary muscles © 2015 Pearson Education, Inc.
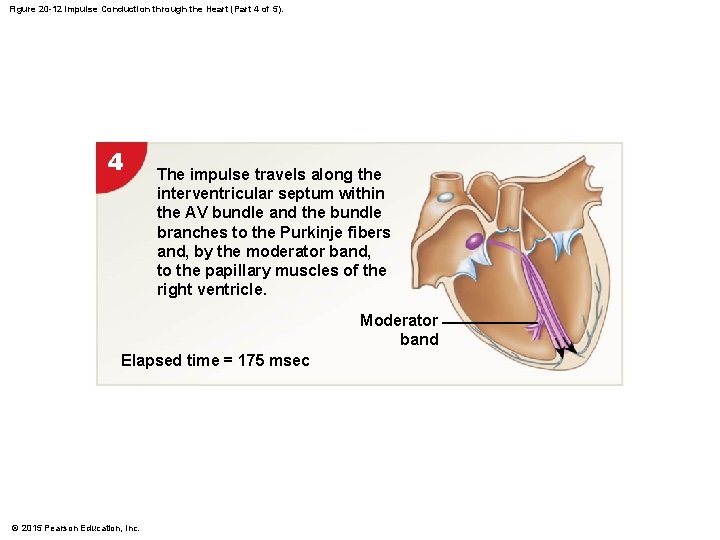
Figure 20 -12 Impulse Conduction through the Heart (Part 4 of 5). 4 The impulse travels along the interventricular septum within the AV bundle and the bundle branches to the Purkinje fibers and, by the moderator band, to the papillary muscles of the right ventricle. Moderator band Elapsed time = 175 msec © 2015 Pearson Education, Inc.
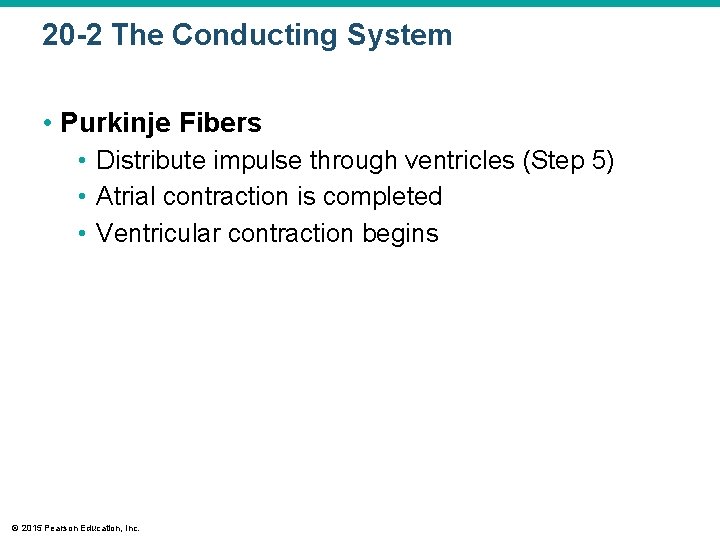
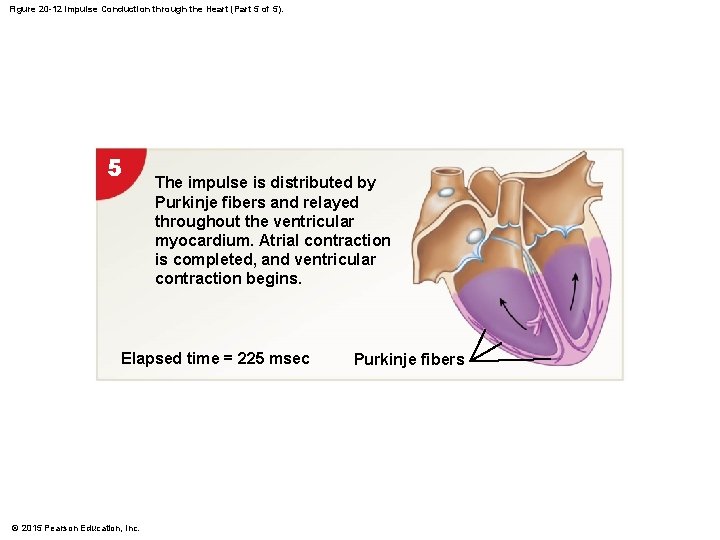
20 -2 The Conducting System • Purkinje Fibers • Distribute impulse through ventricles (Step 5) • Atrial contraction is completed • Ventricular contraction begins © 2015 Pearson Education, Inc.
Figure 20 -12 Impulse Conduction through the Heart (Part 5 of 5). 5 The impulse is distributed by Purkinje fibers and relayed throughout the ventricular myocardium. Atrial contraction is completed, and ventricular contraction begins. Elapsed time = 225 msec © 2015 Pearson Education, Inc. Purkinje fibers
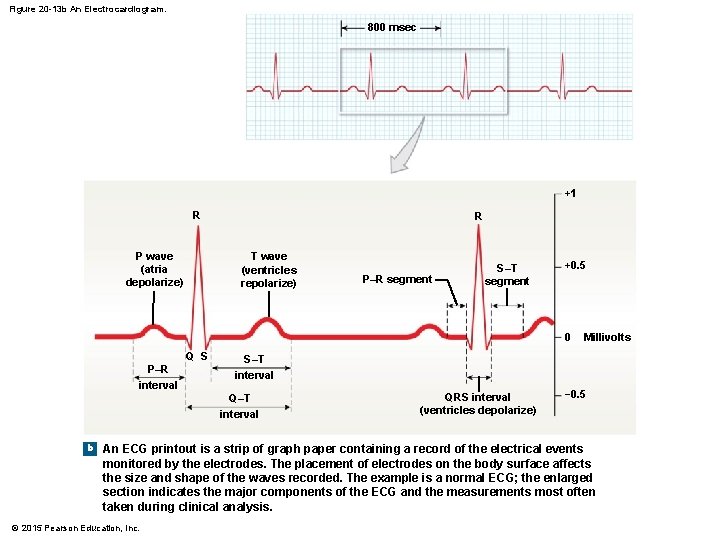
20 -2 The Conducting System • Abnormal Pacemaker Function • Bradycardia – abnormally slow heart rate • Tachycardia – abnormally fast heart rate • Ectopic pacemaker • • Abnormal cells Generate high rate of action potentials Bypass conducting system Disrupt ventricular contractions © 2015 Pearson Education, Inc.
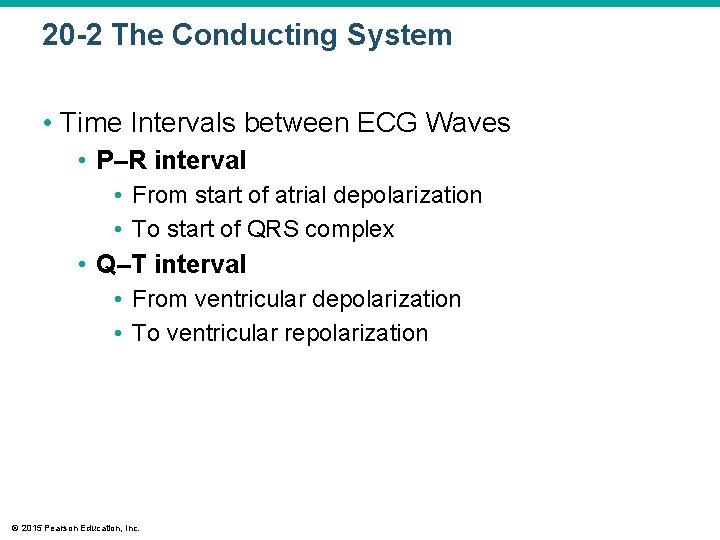
20 -2 The Conducting System • The Electrocardiogram (ECG or EKG) • A recording of electrical events in the heart • Obtained by electrodes at specific body locations • Abnormal patterns diagnose damage © 2015 Pearson Education, Inc.
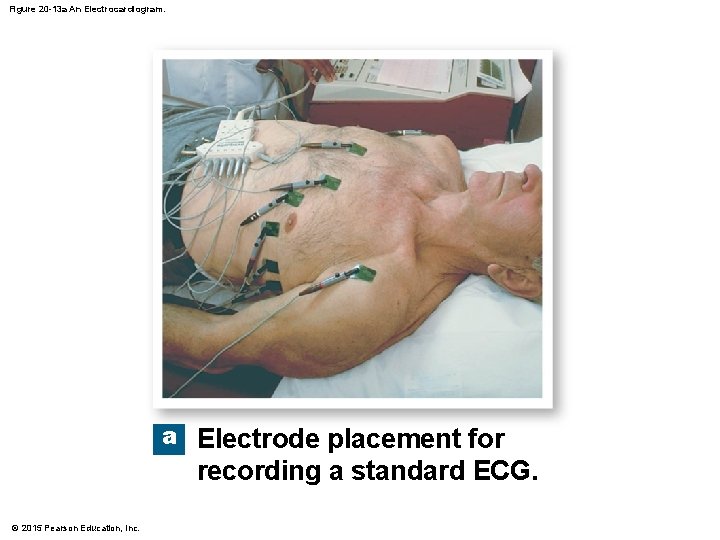
20 -2 The Conducting System • Features of an ECG • P wave • Atria depolarize • QRS complex • Ventricles depolarize • T wave • Ventricles repolarize © 2015 Pearson Education, Inc.
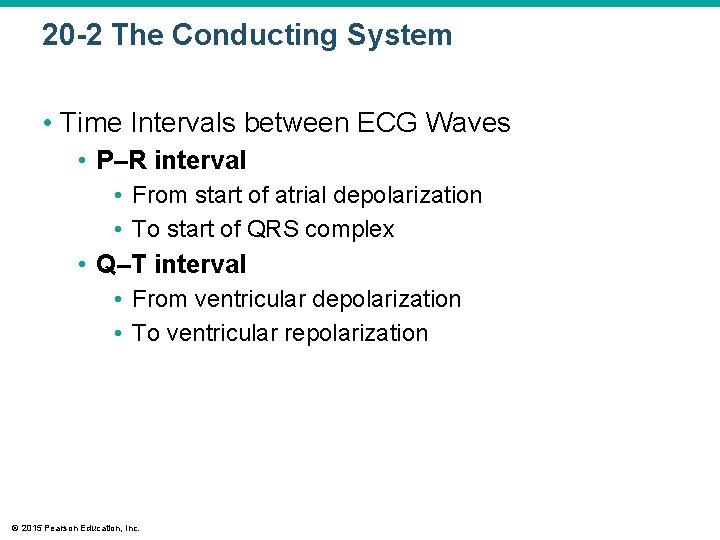
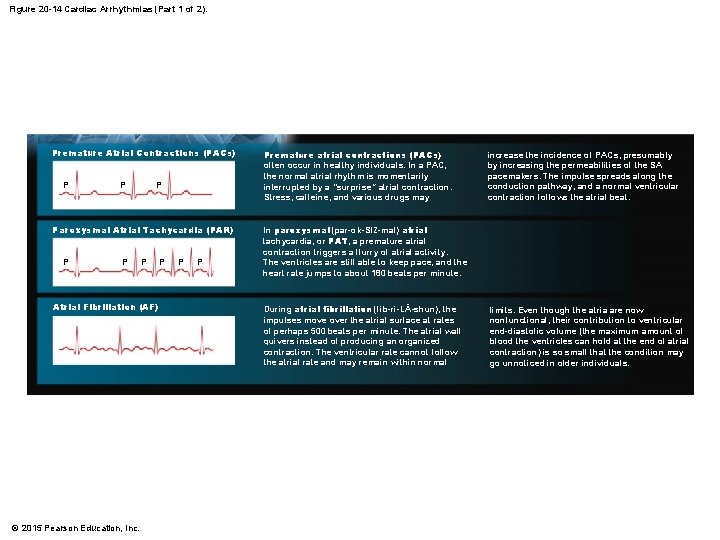
20 -2 The Conducting System • Time Intervals between ECG Waves • P–R interval • From start of atrial depolarization • To start of QRS complex • Q–T interval • From ventricular depolarization • To ventricular repolarization © 2015 Pearson Education, Inc.
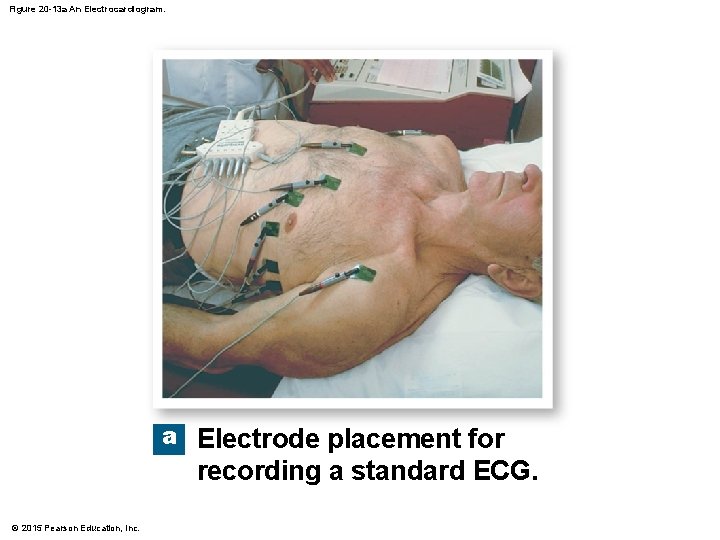
Figure 20 -13 a An Electrocardiogram. a Electrode placement for recording a standard ECG. © 2015 Pearson Education, Inc.
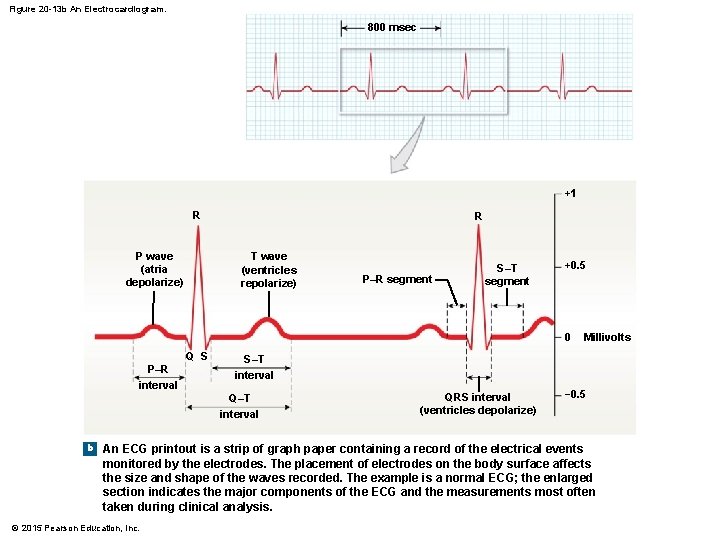
Figure 20 -13 b An Electrocardiogram. 800 msec +1 R P wave (atria depolarize) R T wave (ventricles repolarize) P–R segment S–T segment +0. 5 0 Q S P–R interval S–T interval Q–T interval b Millivolts QRS interval (ventricles depolarize) − 0. 5 An ECG printout is a strip of graph paper containing a record of the electrical events monitored by the electrodes. The placement of electrodes on the body surface affects the size and shape of the waves recorded. The example is a normal ECG; the enlarged section indicates the major components of the ECG and the measurements most often taken during clinical analysis. © 2015 Pearson Education, Inc.
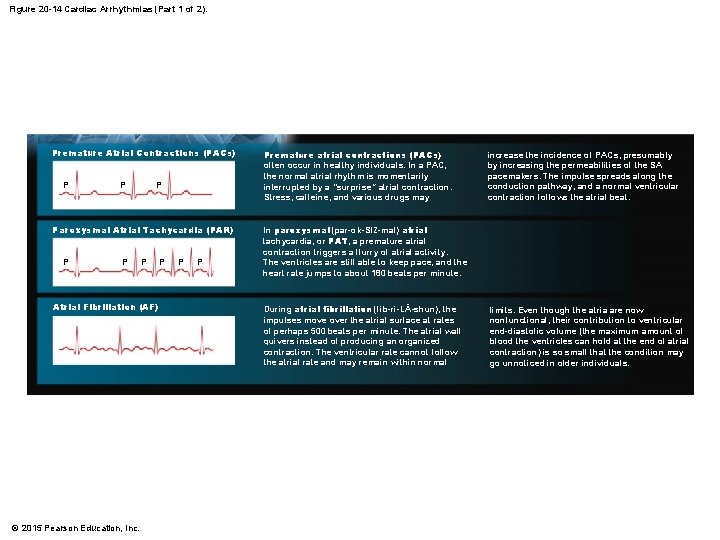
Figure 20 -14 Cardiac Arrhythmias (Part 1 of 2). Premature Atrial Contractions (PACs) P Paroxysmal Atrial Tachycardia (PAR) P P P Atrial Fibrillation (AF) © 2015 Pearson Education, Inc. P Premature atrial contractions (PACs) often occur in healthy individuals. In a PAC, the normal atrial rhythm is momentarily interrupted by a “surprise” atrial contraction. Stress, caffeine, and various drugs may increase the incidence of PACs, presumably by increasing the permeabilities of the SA pacemakers. The impulse spreads along the conduction pathway, and a normal ventricular contraction follows the atrial beat. In paroxysmal (par-ok-SIZ-mal) atrial tachycardia, or PAT, a premature atrial contraction triggers a flurry of atrial activity. The ventricles are still able to keep pace, and the heart rate jumps to about 180 beats per minute. During atrial fibrillation (fib-ri-LĀ-shun), the impulses move over the atrial surface at rates of perhaps 500 beats per minute. The atrial wall quivers instead of producing an organized contraction. The ventricular rate cannot follow the atrial rate and may remain within normal limits. Even though the atria are now nonfunctional, their contribution to ventricular end-diastolic volume (the maximum amount of blood the ventricles can hold at the end of atrial contraction) is so small that the condition may go unnoticed in older individuals.
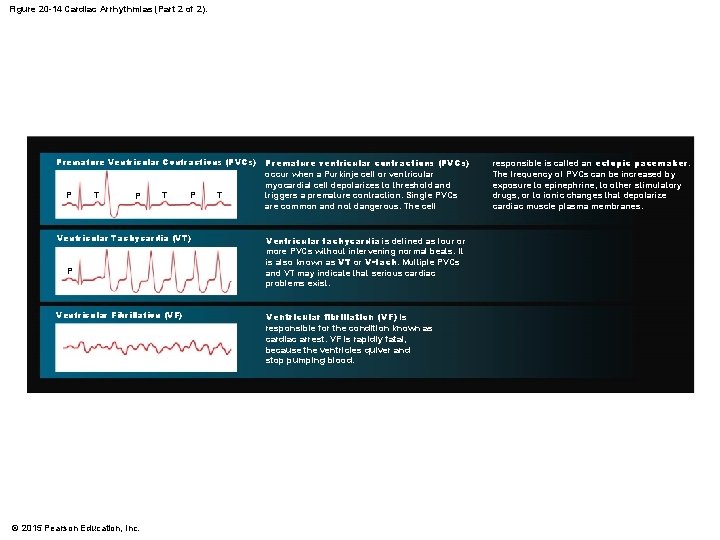
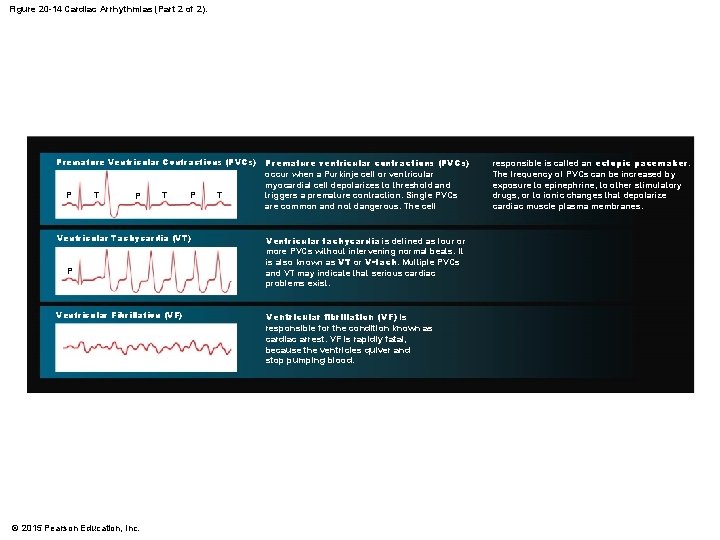
Figure 20 -14 Cardiac Arrhythmias (Part 2 of 2). Premature Ventricular Contractions (PVCs) P T P Ventricular Tachycardia (VT) P Ventricular Fibrillation (VF) © 2015 Pearson Education, Inc. T Premature ventricular contractions (PVCs) occur when a Purkinje cell or ventricular myocardial cell depolarizes to threshold and triggers a premature contraction. Single PVCs are common and not dangerous. The cell Ventricular tachycardia is defined as four or more PVCs without intervening normal beats. It is also known as VT or V-tach. Multiple PVCs and VT may indicate that serious cardiac problems exist. Ventricular fibrillation (VF) is responsible for the condition known as cardiac arrest. VF is rapidly fatal, because the ventricles quiver and stop pumping blood. responsible is called an ectopic pacemaker. The frequency of PVCs can be increased by exposure to epinephrine, to other stimulatory drugs, or to ionic changes that depolarize cardiac muscle plasma membranes.
20 -2 The Conducting System • Contractile Cells • Purkinje fibers distribute the stimulus to the contractile cells, which make up most of the muscle cells in the heart • Resting potential • Of a ventricular cell about – 90 m. V • Of an atrial cell about – 80 m. V © 2015 Pearson Education, Inc.
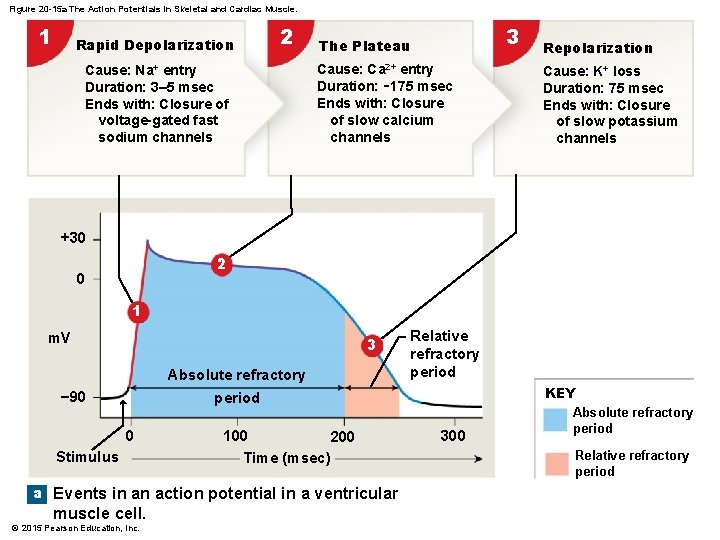
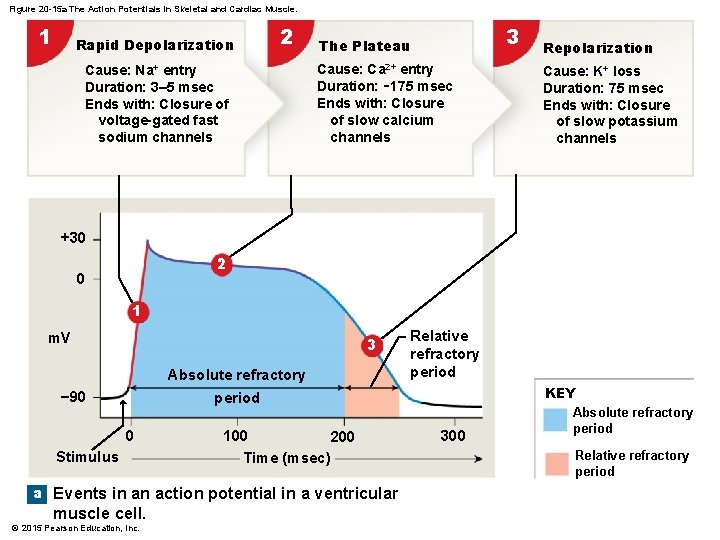
Figure 20 -15 a The Action Potentials in Skeletal and Cardiac Muscle. 1 Rapid Depolarization 2 Cause: Na+ entry Duration: 3– 5 msec Ends with: Closure of voltage-gated fast sodium channels 3 The Plateau Cause: Ca 2+ entry Duration: ∼ 175 msec Ends with: Closure of slow calcium channels Repolarization Cause: K+ loss Duration: 75 msec Ends with: Closure of slow potassium channels +30 2 0 1 m. V 3 Absolute refractory − 90 Relative refractory period KEY period 0 Stimulus 100 200 Time (msec) a Events in an action potential in a ventricular muscle cell. © 2015 Pearson Education, Inc. 300 Absolute refractory period Relative refractory period
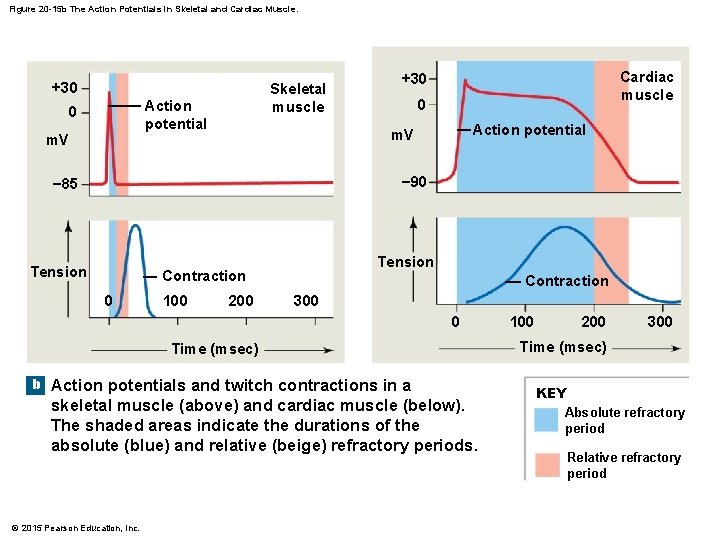
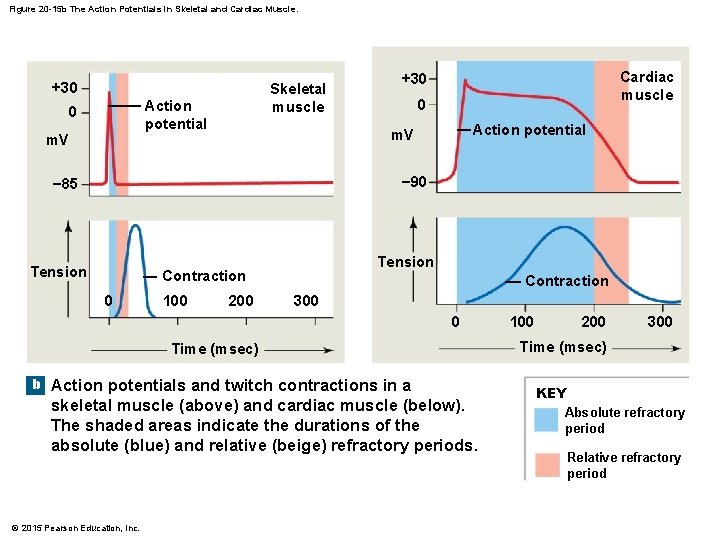
Figure 20 -15 b The Action Potentials in Skeletal and Cardiac Muscle. +30 Skeletal muscle Action potential 0 m. V Cardiac muscle +30 0 Action potential m. V − 90 − 85 Tension Contraction 0 100 200 Contraction 300 0 Time (msec) b Action potentials and twitch contractions in a skeletal muscle (above) and cardiac muscle (below). The shaded areas indicate the durations of the absolute (blue) and relative (beige) refractory periods. © 2015 Pearson Education, Inc. 100 200 300 Time (msec) KEY Absolute refractory period Relative refractory period
20 -2 The Conducting System • Refractory Period • Absolute refractory period • Long • Cardiac muscle cells cannot respond • Relative refractory period • Short • Response depends on degree of stimulus © 2015 Pearson Education, Inc.
20 -2 The Conducting System • Timing of Refractory Periods • Length of cardiac action potential in ventricular cell • 250– 300 msec • 30 times longer than skeletal muscle fiber • Long refractory period prevents summation and tetany © 2015 Pearson Education, Inc.
20 -2 The Conducting System • The Role of Calcium Ions in Cardiac Contractions • Contraction of a cardiac muscle cell • Is produced by an increase in calcium ion concentration around myofibrils © 2015 Pearson Education, Inc.
20 -2 The Conducting System • The Role of Calcium Ions in Cardiac Contractions 1. 20 percent of calcium ions required for a contraction • Calcium ions enter plasma membrane during plateau phase 2. Arrival of extracellular Ca 2+ • Triggers release of calcium ion reserves from sarcoplasmic reticulum (SR) © 2015 Pearson Education, Inc.

20 -2 The Conducting System • The Role of Calcium Ions in Cardiac Contractions • As slow calcium channels close • Intracellular Ca 2+ is absorbed by the SR • Or pumped out of cell • Cardiac muscle tissue • Very sensitive to extracellular Ca 2+ concentrations © 2015 Pearson Education, Inc.
20 -2 The Conducting System • The Energy for Cardiac Contractions • Aerobic energy of heart • From mitochondrial breakdown of fatty acids and glucose • Oxygen from circulating hemoglobin • Cardiac muscles store oxygen in myoglobin © 2015 Pearson Education, Inc.
20 -3 The Cardiac Cycle • The Cardiac Cycle • Is the period between the start of one heartbeat and the beginning of the next • Includes both contraction and relaxation © 2015 Pearson Education, Inc.
20 -3 The Cardiac Cycle • Two Phases of the Cardiac Cycle • Within any one chamber 1. Systole (contraction) 2. Diastole (relaxation) © 2015 Pearson Education, Inc.

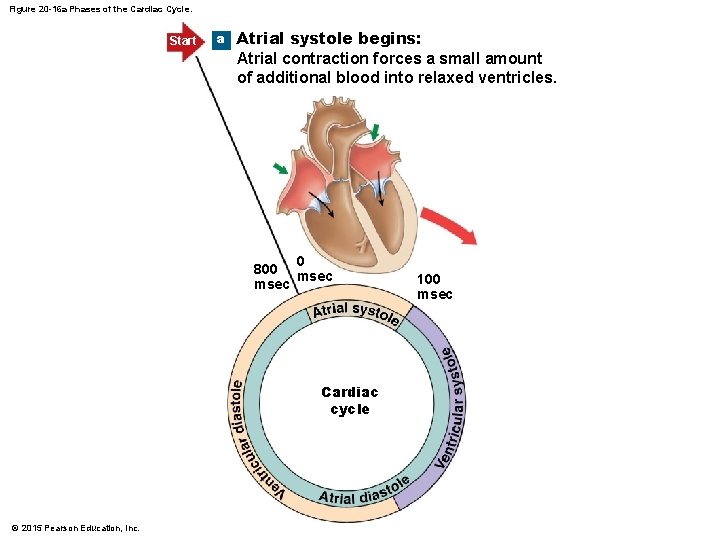
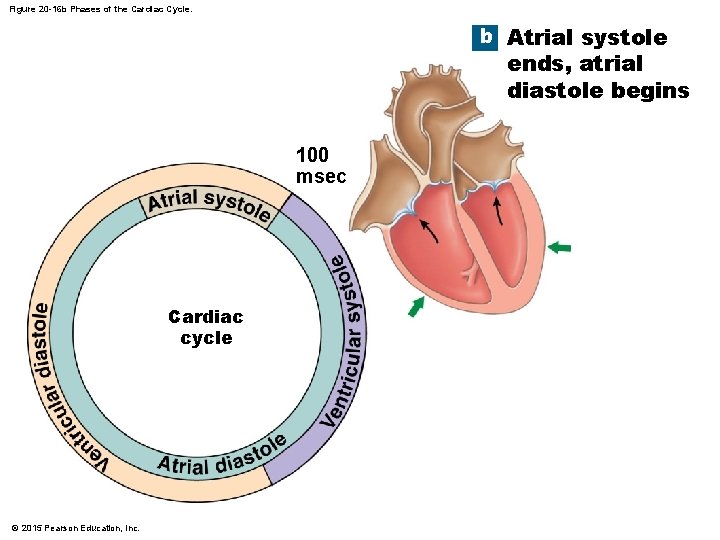
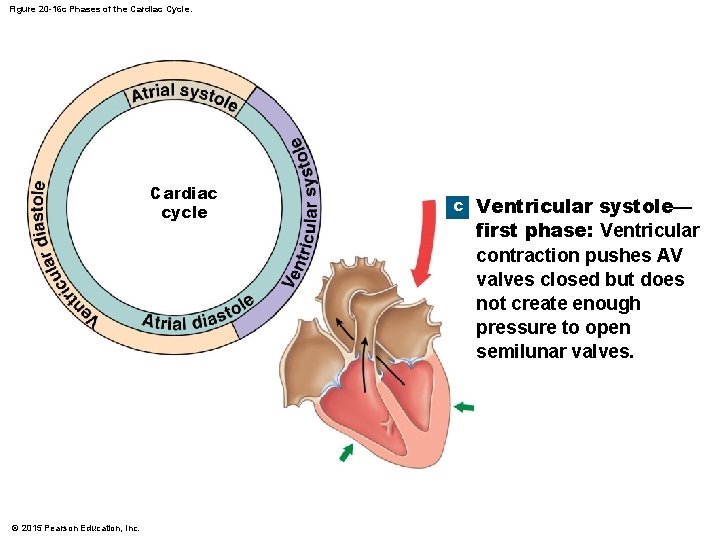
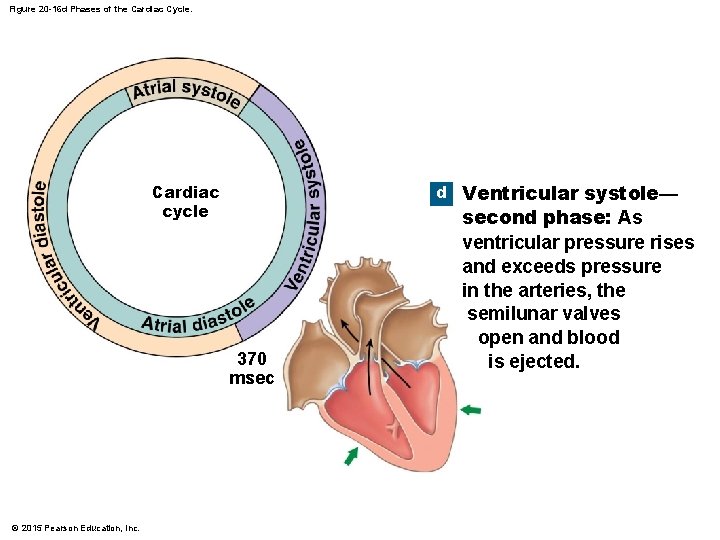
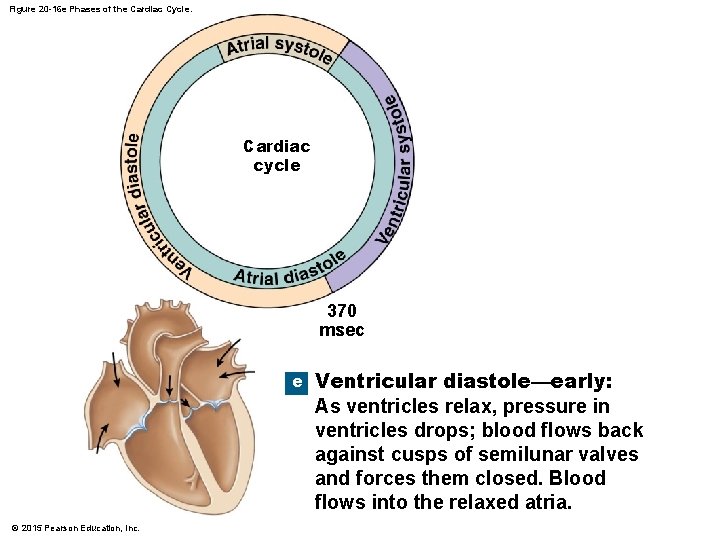
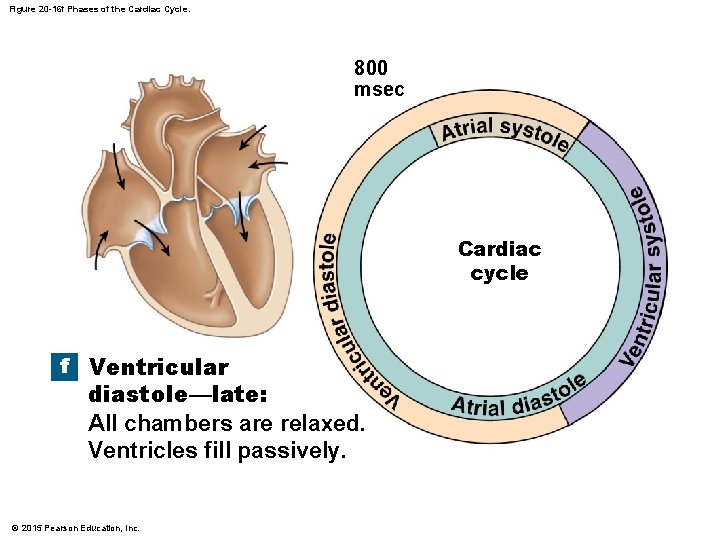
Figure 20 -16 Phases of the Cardiac Cycle. Start a Atrial systole begins: Atrial contraction forces a small amount of additional blood into relaxed ventricles. b Atrial systole ends, atrial diastole begins 0 800 msec f Ventricular 100 msec Cardiac cycle c Ventricular systole— diastole—late: All chambers are relaxed. Ventricles fill passively. 370 msec first phase: Ventricular contraction pushes AV valves closed but does not create enough pressure to open semilunar valves. d Ventricular systole— e Ventricular diastole—early: As ventricles relax, pressure in ventricles drops; blood flows back against cusps of semilunar valves and forces them closed. Blood flows into the relaxed atria. © 2015 Pearson Education, Inc. second phase: As ventricular pressure rises and exceeds pressure in the arteries, the semilunar valves open and blood is ejected.
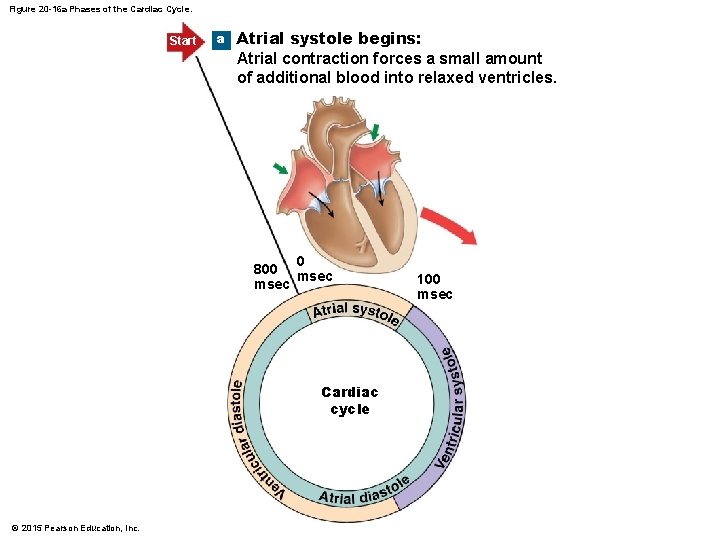
Figure 20 -16 a Phases of the Cardiac Cycle. Start a Atrial systole begins: Atrial contraction forces a small amount of additional blood into relaxed ventricles. 0 800 msec Cardiac cycle © 2015 Pearson Education, Inc. 100 msec
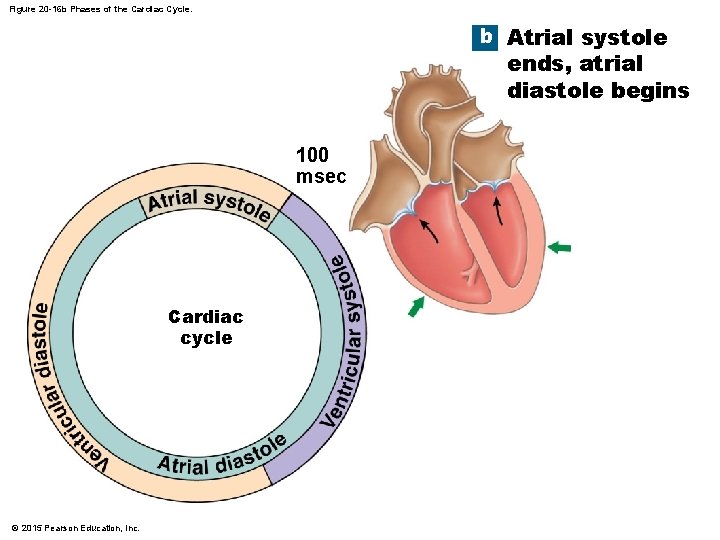
Figure 20 -16 b Phases of the Cardiac Cycle. b Atrial systole ends, atrial diastole begins 100 msec Cardiac cycle © 2015 Pearson Education, Inc.
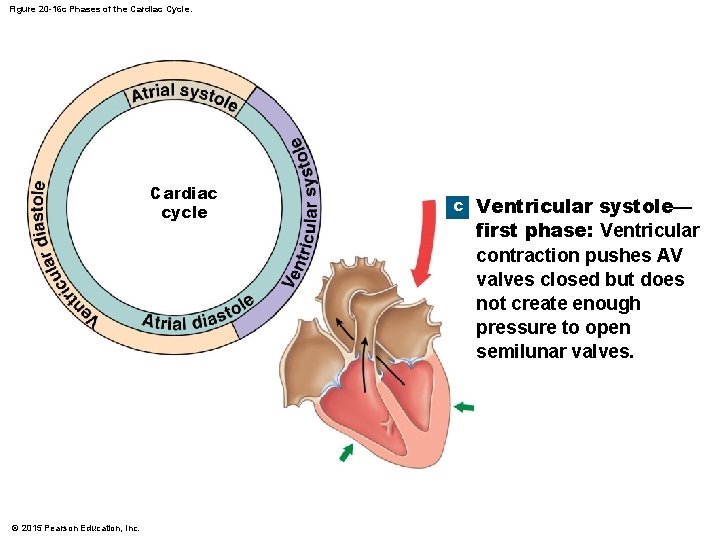
Figure 20 -16 c Phases of the Cardiac Cycle. Cardiac cycle © 2015 Pearson Education, Inc. c Ventricular systole— first phase: Ventricular contraction pushes AV valves closed but does not create enough pressure to open semilunar valves.
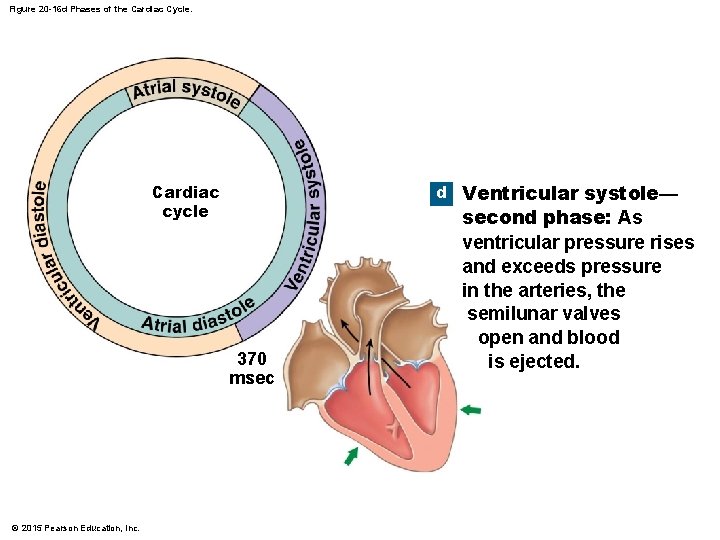
Figure 20 -16 d Phases of the Cardiac Cycle. d Ventricular systole— Cardiac cycle 370 msec © 2015 Pearson Education, Inc. second phase: As ventricular pressure rises and exceeds pressure in the arteries, the semilunar valves open and blood is ejected.
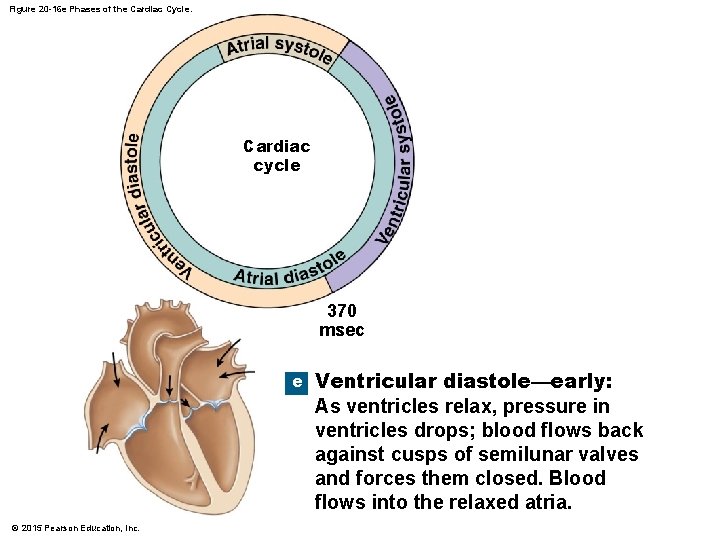
Figure 20 -16 e Phases of the Cardiac Cycle. Cardiac cycle 370 msec e © 2015 Pearson Education, Inc. Ventricular diastole—early: As ventricles relax, pressure in ventricles drops; blood flows back against cusps of semilunar valves and forces them closed. Blood flows into the relaxed atria.
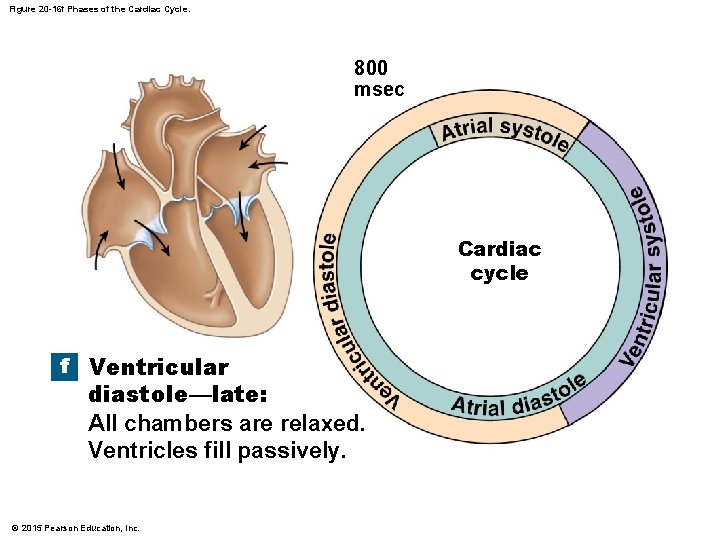
Figure 20 -16 f Phases of the Cardiac Cycle. 800 msec Cardiac cycle f Ventricular diastole—late: All chambers are relaxed. Ventricles fill passively. © 2015 Pearson Education, Inc.
20 -3 The Cardiac Cycle • Blood Pressure • In any chamber • Rises during systole • Falls during diastole • Blood flows from high to low pressure • Controlled by timing of contractions • Directed by one-way valves © 2015 Pearson Education, Inc.
20 -3 The Cardiac Cycle • Cardiac Cycle and Heart Rate • At 75 beats per minute (bpm) • Cardiac cycle lasts about 800 msec • When heart rate increases • All phases of cardiac cycle shorten, particularly diastole © 2015 Pearson Education, Inc.
20 -3 The Cardiac Cycle • Phases of the Cardiac Cycle • • Atrial systole Atrial diastole Ventricular systole Ventricular diastole © 2015 Pearson Education, Inc.
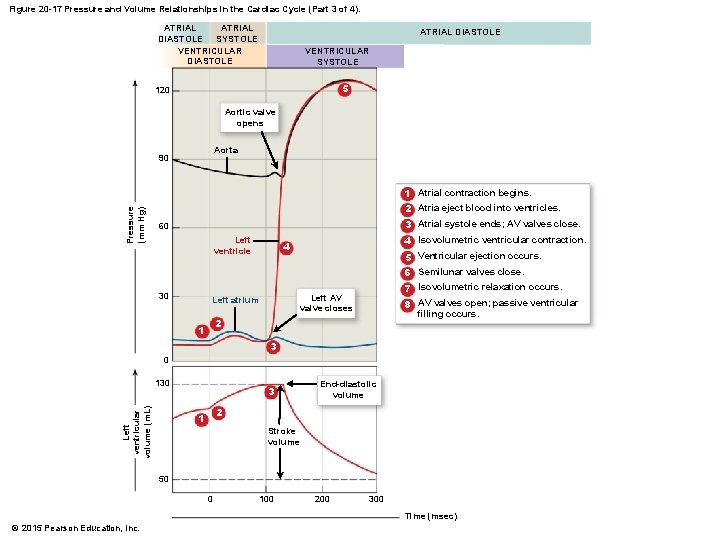
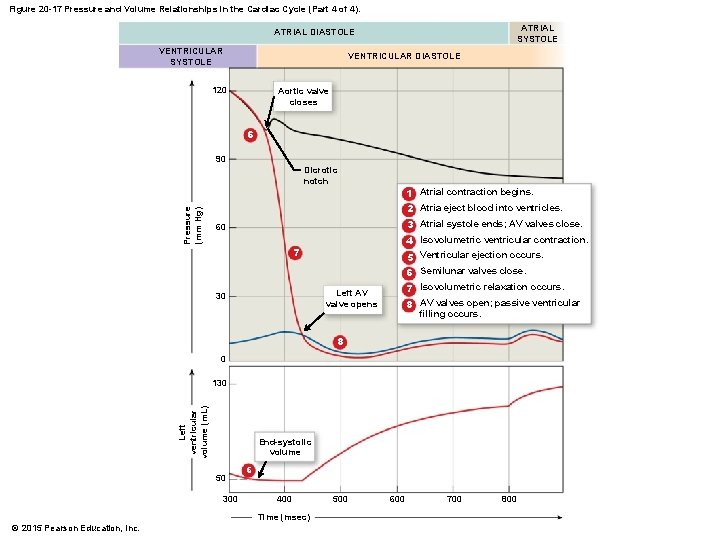
20 -3 The Cardiac Cycle • Atrial Systole 1. Atrial systole • Atrial contraction begins • Right and left AV valves are open 2. Atria eject blood into ventricles • Filling ventricles 3. Atrial systole ends • AV valves close • Ventricles contain maximum blood volume • Known as end-diastolic volume (EDV) © 2015 Pearson Education, Inc.
20 -3 The Cardiac Cycle • Ventricular Systole 4. Ventricles contract and build pressure • AV valves close causing isovolumetric contraction 5. Ventricular ejection • Ventricular pressure exceeds vessel pressure opening the semilunar valves and allowing blood to leave the ventricle • Amount of blood ejected is called the stroke volume (SV) © 2015 Pearson Education, Inc.
20 -3 The Cardiac Cycle • Ventricular Systole 6. Ventricular pressure falls • Semilunar valves close • Ventricles contain end-systolic volume (ESV), about 40 percent of end-diastolic volume © 2015 Pearson Education, Inc.
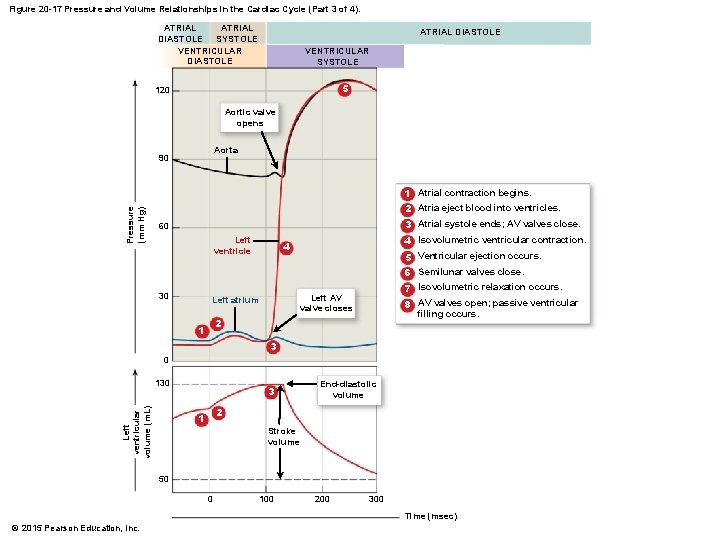
Figure 20 -17 Pressure and Volume Relationships in the Cardiac Cycle (Part 3 of 4). ATRIAL DIASTOLE SYSTOLE VENTRICULAR DIASTOLE ATRIAL DIASTOLE VENTRICULAR SYSTOLE 5 120 Aortic valve opens Aorta 90 Pressure (mm Hg) 1 Atrial contraction begins. 2 Atria eject blood into ventricles. 3 Atrial systole ends; AV valves close. 60 Left ventricle 4 Isovolumetric ventricular contraction. 4 5 Ventricular ejection occurs. 6 Semilunar valves close. 30 7 Isovolumetric relaxation occurs. Left AV valve closes Left atrium 8 AV valves open; passive ventricular filling occurs. 2 1 3 0 Left ventricular volume (m. L) 130 3 End-diastolic volume 2 1 Stroke volume 50 0 100 200 300 Time (msec) © 2015 Pearson Education, Inc.
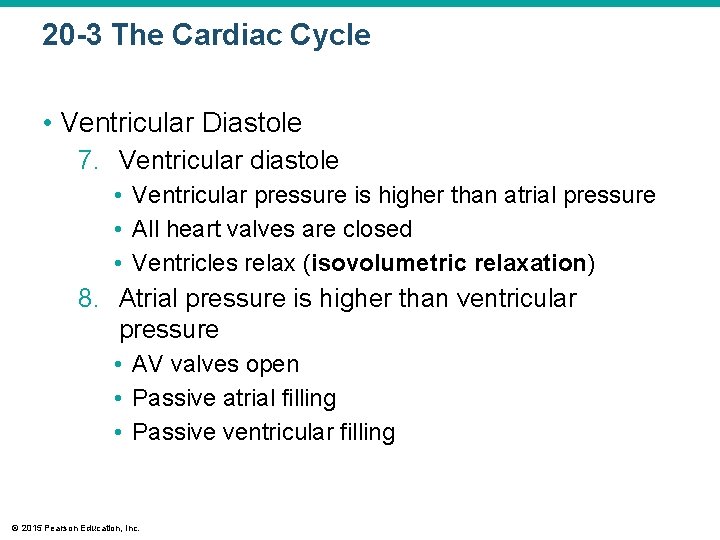
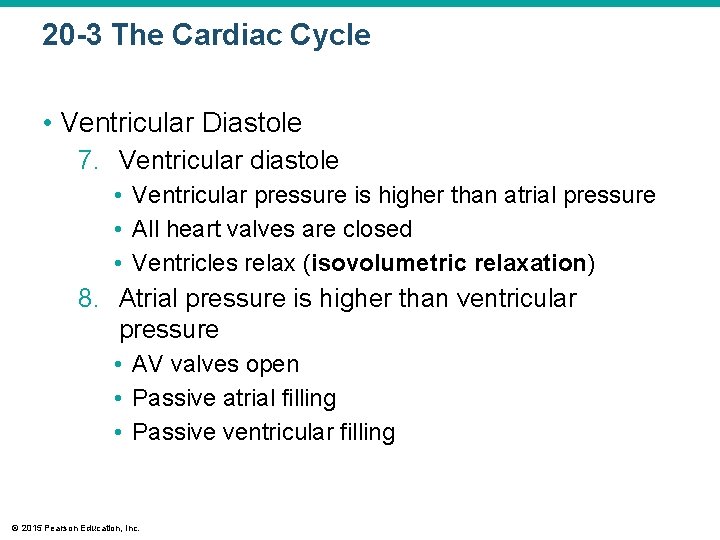
20 -3 The Cardiac Cycle • Ventricular Diastole 7. Ventricular diastole • Ventricular pressure is higher than atrial pressure • All heart valves are closed • Ventricles relax (isovolumetric relaxation) 8. Atrial pressure is higher than ventricular pressure • AV valves open • Passive atrial filling • Passive ventricular filling © 2015 Pearson Education, Inc.
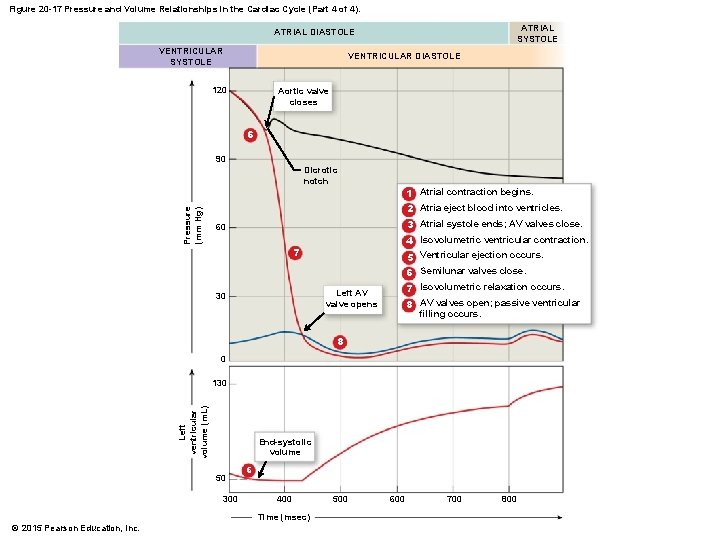
Figure 20 -17 Pressure and Volume Relationships in the Cardiac Cycle (Part 4 of 4). ATRIAL SYSTOLE ATRIAL DIASTOLE VENTRICULAR SYSTOLE VENTRICULAR DIASTOLE 120 Aortic valve closes 6 90 Pressure (mm Hg) Dicrotic notch 1 Atrial contraction begins. 2 Atria eject blood into ventricles. 3 Atrial systole ends; AV valves close. 60 4 Isovolumetric ventricular contraction. 7 5 Ventricular ejection occurs. 6 Semilunar valves close. 7 Isovolumetric relaxation occurs. Left AV valve opens 30 8 AV valves open; passive ventricular filling occurs. 8 0 Left ventricular volume (m. L) 130 End-systolic volume 50 300 6 400 Time (msec) © 2015 Pearson Education, Inc. 500 600 700 800
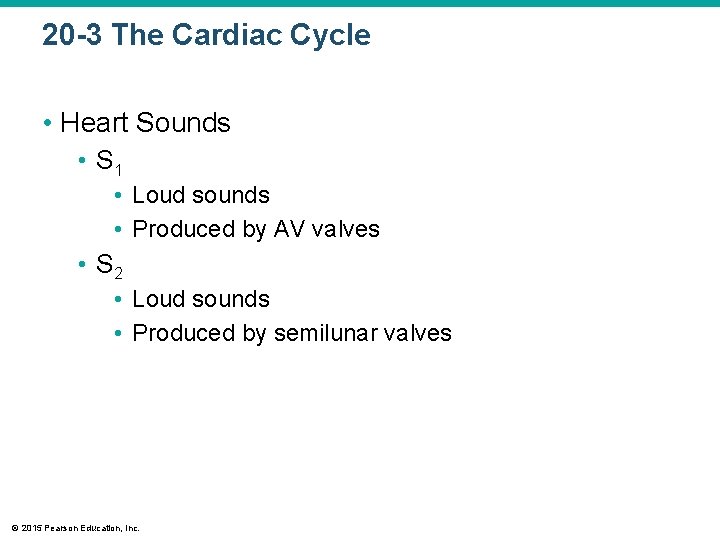
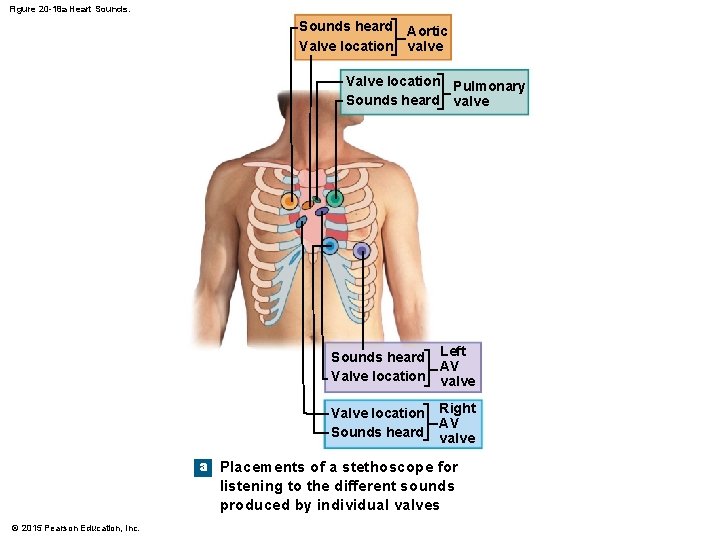
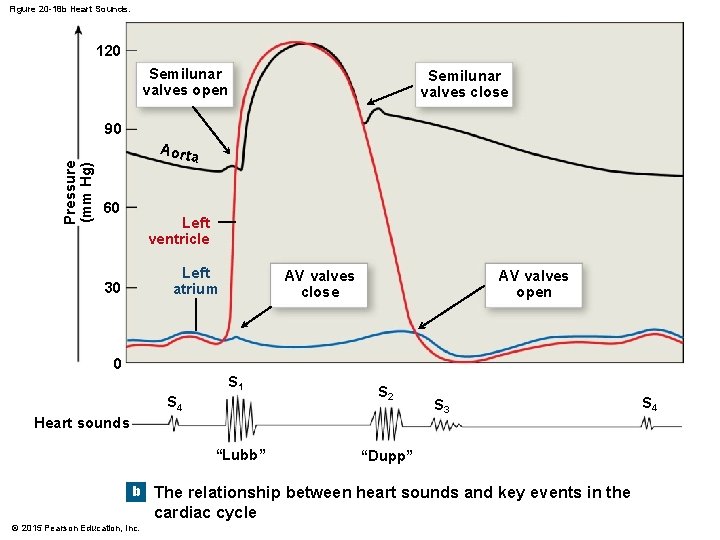
20 -3 The Cardiac Cycle • Heart Sounds • S 1 • Loud sounds • Produced by AV valves • S 2 • Loud sounds • Produced by semilunar valves © 2015 Pearson Education, Inc.
20 -3 The Cardiac Cycle • S 3, S 4 • Soft sounds • Blood flow into ventricles and atrial contraction • Heart Murmur • Sounds produced by regurgitation through valves © 2015 Pearson Education, Inc.
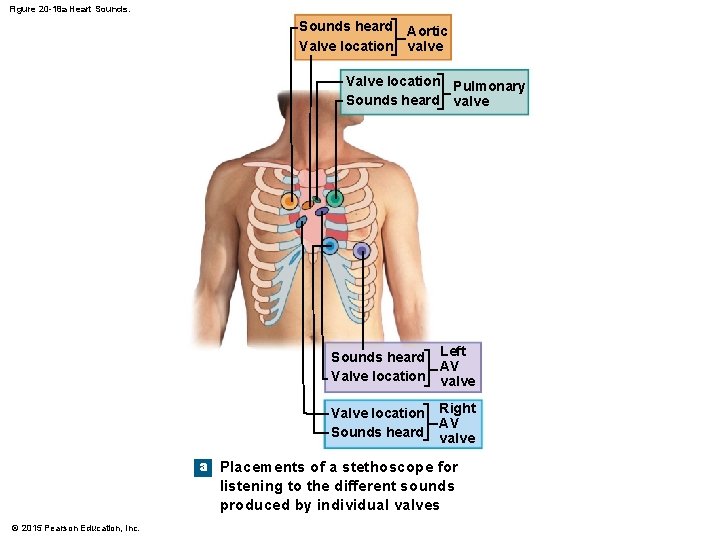
Figure 20 -18 a Heart Sounds heard Aortic Valve location valve Valve location Pulmonary Sounds heard valve Sounds heard Valve location Left AV valve Valve location Sounds heard Right AV valve a Placements of a stethoscope for listening to the different sounds produced by individual valves © 2015 Pearson Education, Inc.
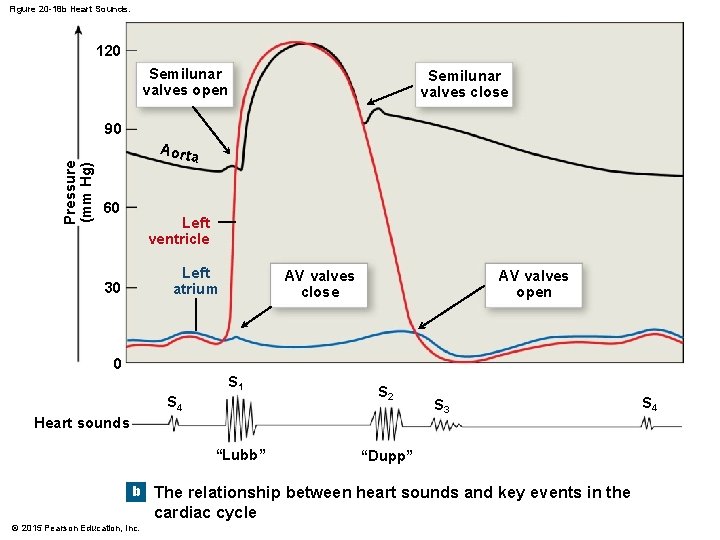
Figure 20 -18 b Heart Sounds. 120 Semilunar valves open Semilunar valves close Pressure (mm Hg) 90 Aorta 60 Left ventricle Left atrium 30 AV valves close AV valves open 0 S 1 S 4 S 2 Heart sounds “Lubb” S 3 “Dupp” b The relationship between heart sounds and key events in the cardiac cycle © 2015 Pearson Education, Inc. S 4

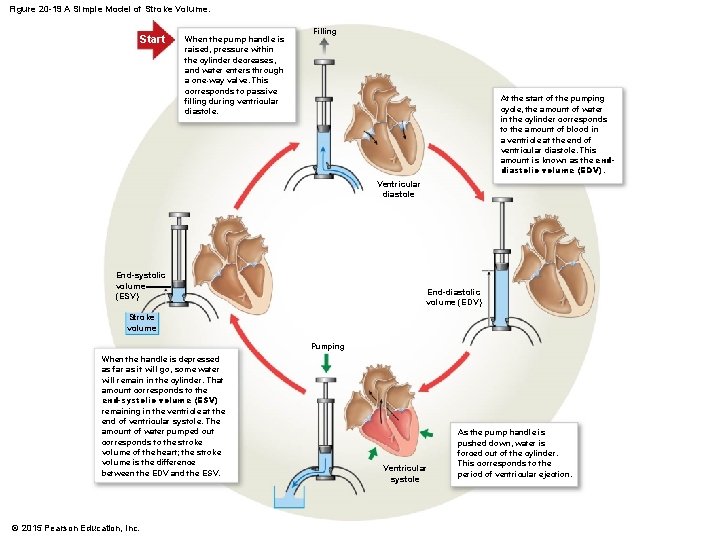
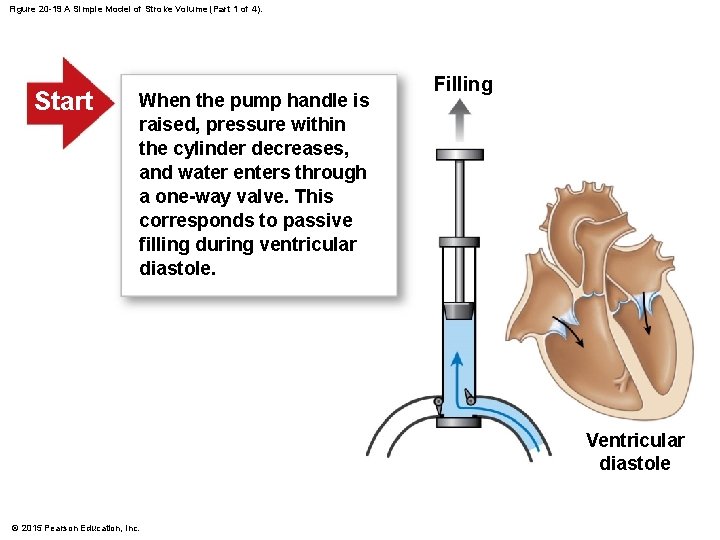
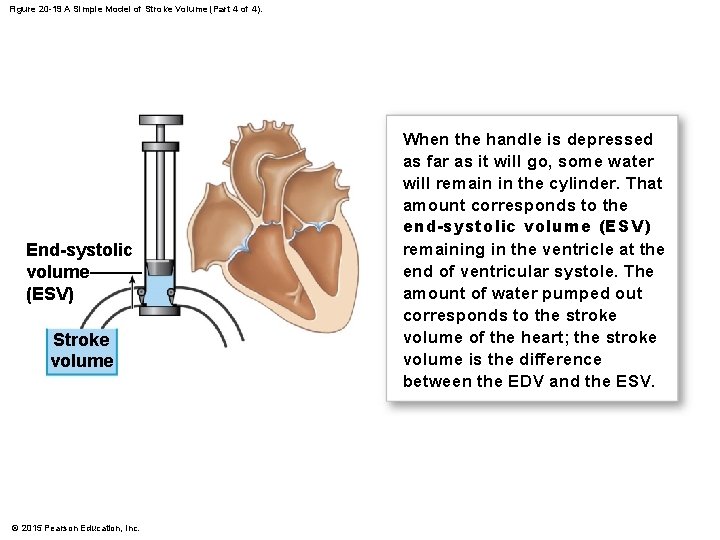
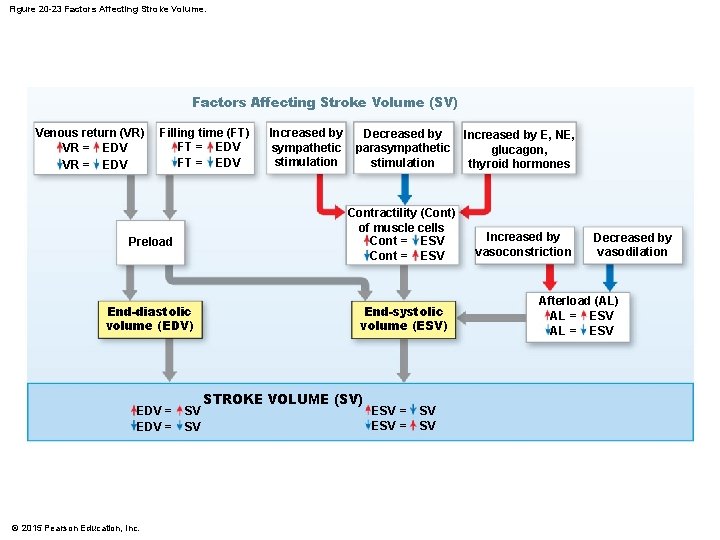
20 -4 Cardiodynamics • The movement and force generated by cardiac contractions • End-diastolic volume (EDV) • End-systolic volume (ESV) • Stroke volume (SV) • SV = EDV – ESV • Ejection fraction • The percentage of EDV represented by SV © 2015 Pearson Education, Inc.
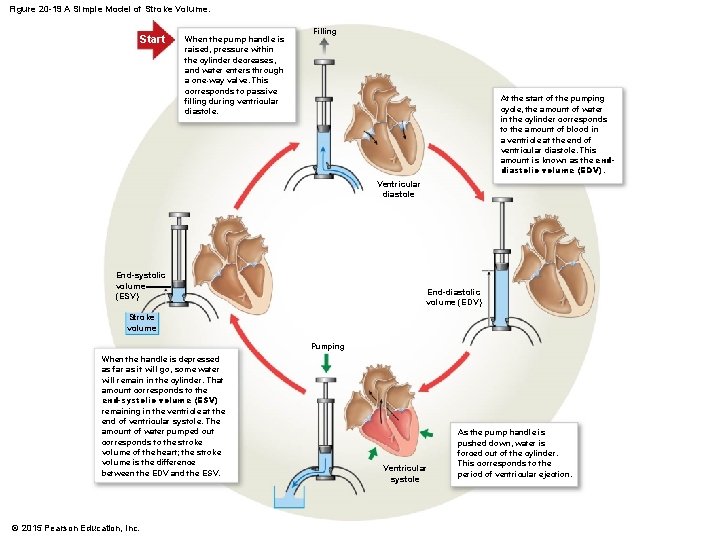
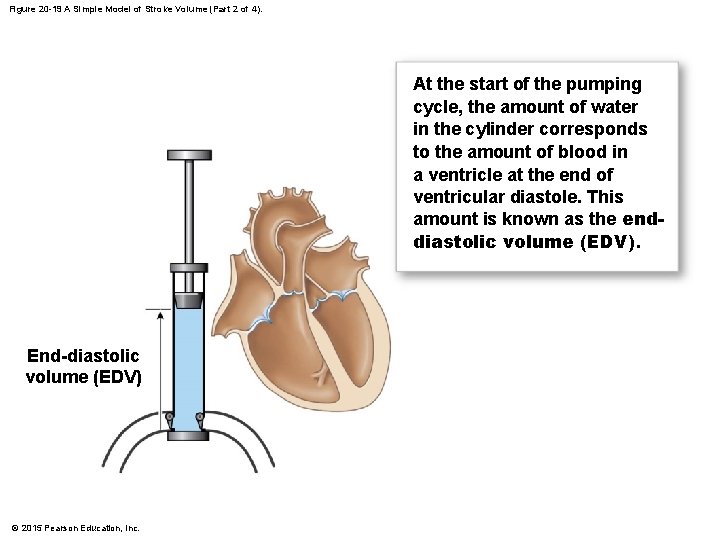
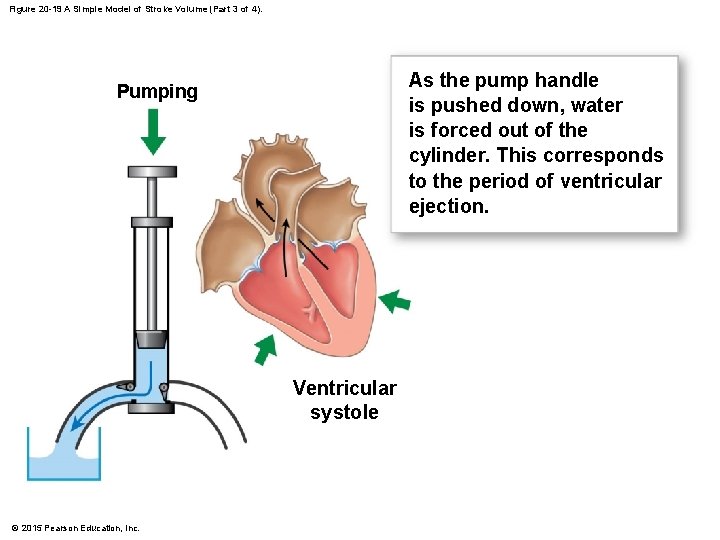
Figure 20 -19 A Simple Model of Stroke Volume. Start When the pump handle is raised, pressure within the cylinder decreases, and water enters through a one-way valve. This corresponds to passive filling during ventricular diastole. Filling At the start of the pumping cycle, the amount of water in the cylinder corresponds to the amount of blood in a ventricle at the end of ventricular diastole. This amount is known as the enddiastolic volume (EDV). Ventricular diastole End-systolic volume (ESV) End-diastolic volume (EDV) Stroke volume Pumping When the handle is depressed as far as it will go, some water will remain in the cylinder. That amount corresponds to the end-systolic volume (ESV) remaining in the ventricle at the end of ventricular systole. The amount of water pumped out corresponds to the stroke volume of the heart; the stroke volume is the difference between the EDV and the ESV. © 2015 Pearson Education, Inc. Ventricular systole As the pump handle is pushed down, water is forced out of the cylinder. This corresponds to the period of ventricular ejection.
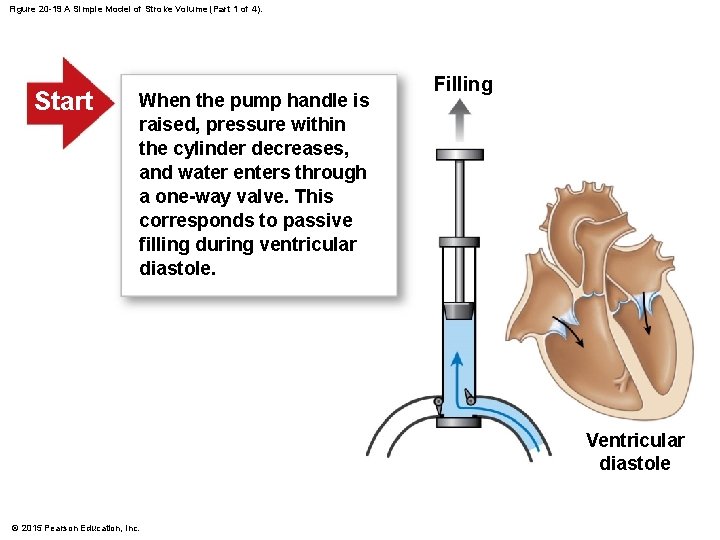
Figure 20 -19 A Simple Model of Stroke Volume (Part 1 of 4). Start When the pump handle is raised, pressure within the cylinder decreases, and water enters through a one-way valve. This corresponds to passive filling during ventricular diastole. Filling Ventricular diastole © 2015 Pearson Education, Inc.
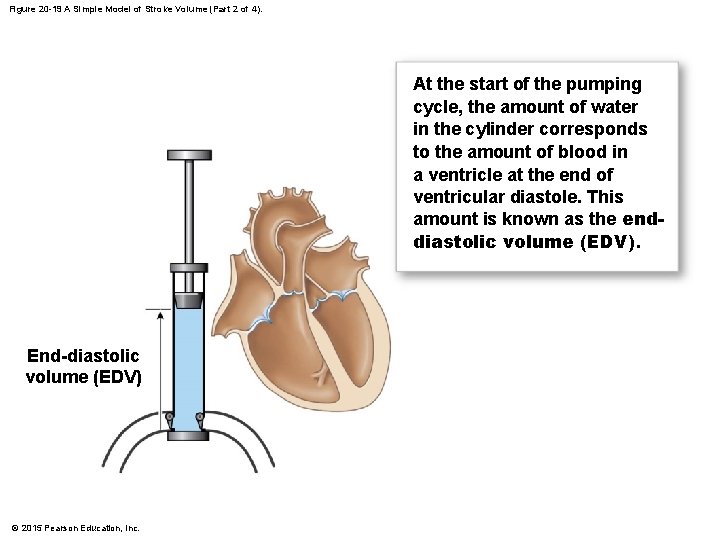
Figure 20 -19 A Simple Model of Stroke Volume (Part 2 of 4). At the start of the pumping cycle, the amount of water in the cylinder corresponds to the amount of blood in a ventricle at the end of ventricular diastole. This amount is known as the enddiastolic volume (EDV). End-diastolic volume (EDV) © 2015 Pearson Education, Inc.
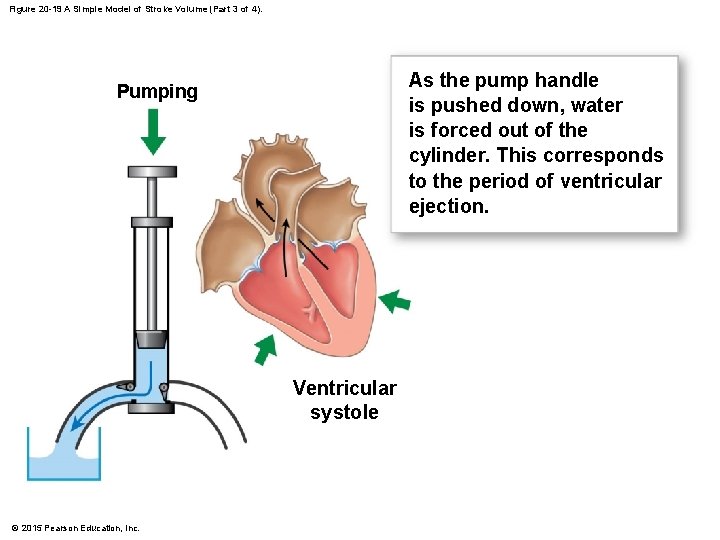
Figure 20 -19 A Simple Model of Stroke Volume (Part 3 of 4). As the pump handle is pushed down, water is forced out of the cylinder. This corresponds to the period of ventricular ejection. Pumping Ventricular systole © 2015 Pearson Education, Inc.
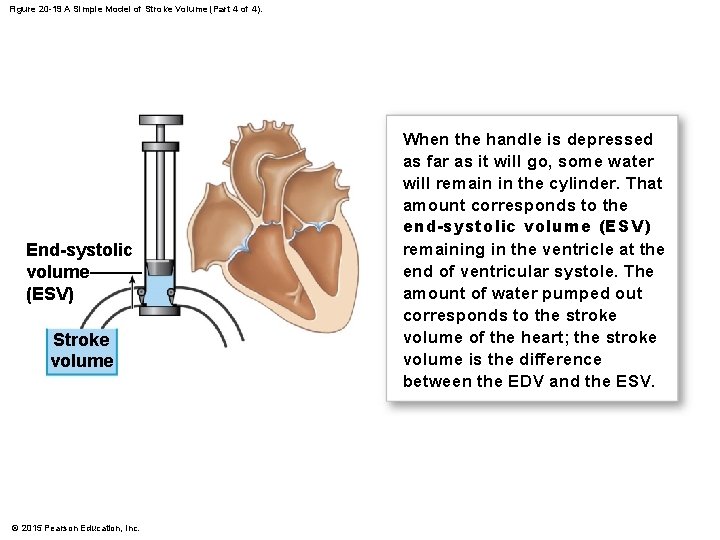
Figure 20 -19 A Simple Model of Stroke Volume (Part 4 of 4). End-systolic volume (ESV) Stroke volume © 2015 Pearson Education, Inc. When the handle is depressed as far as it will go, some water will remain in the cylinder. That amount corresponds to the end-systolic volume (ESV) remaining in the ventricle at the end of ventricular systole. The amount of water pumped out corresponds to the stroke volume of the heart; the stroke volume is the difference between the EDV and the ESV.
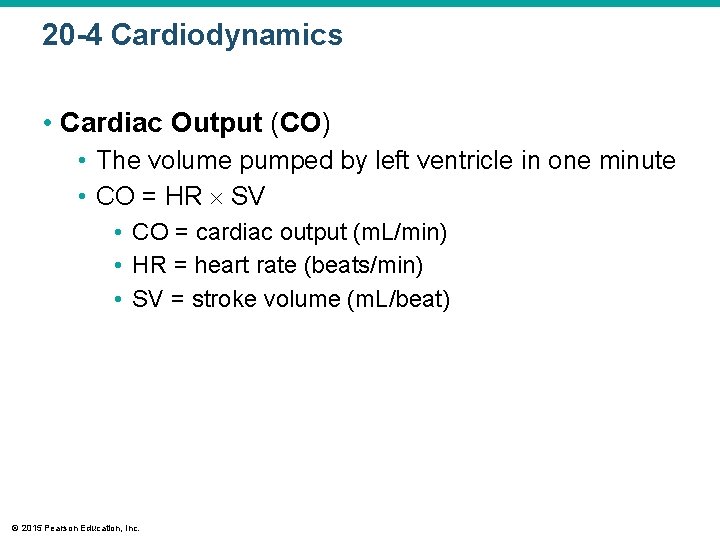
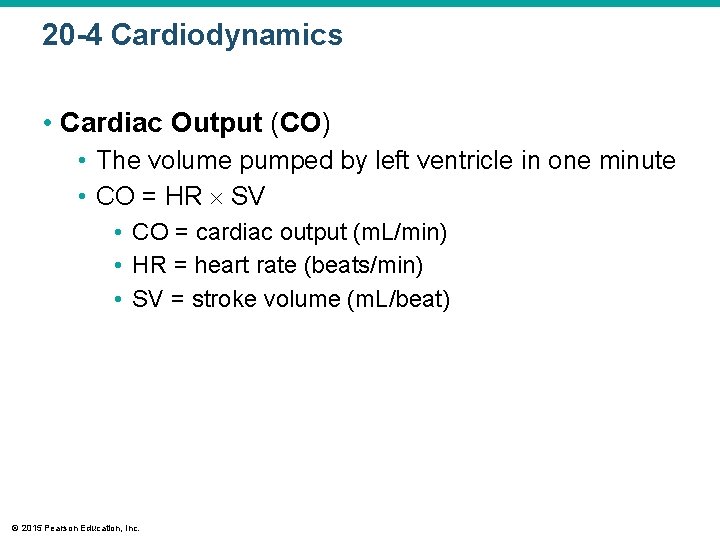
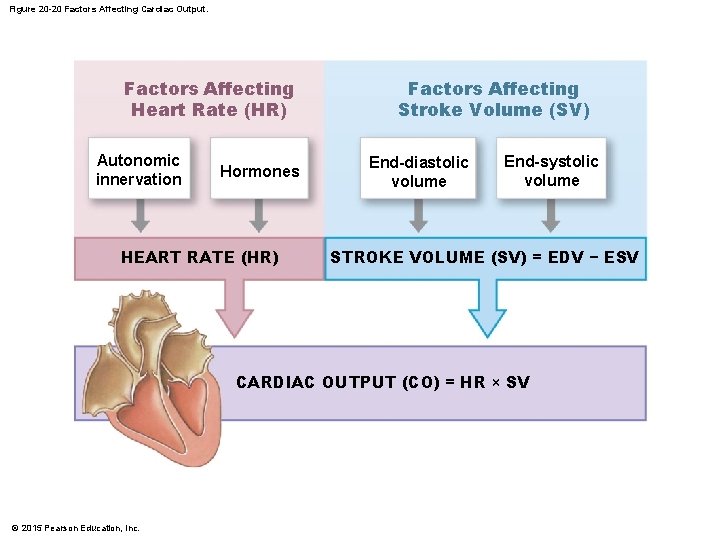
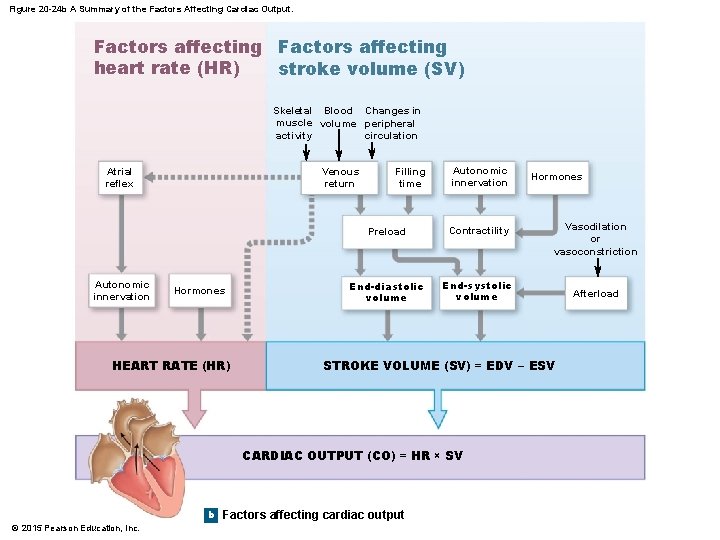
20 -4 Cardiodynamics • Cardiac Output (CO) • The volume pumped by left ventricle in one minute • CO = HR SV • CO = cardiac output (m. L/min) • HR = heart rate (beats/min) • SV = stroke volume (m. L/beat) © 2015 Pearson Education, Inc.
20 -4 Cardiodynamics • Factors Affecting Cardiac Output • Cardiac output • Adjusted by changes in heart rate or stroke volume • Heart rate • Adjusted by autonomic nervous system or hormones • Stroke volume • Adjusted by changing EDV or ESV © 2015 Pearson Education, Inc.
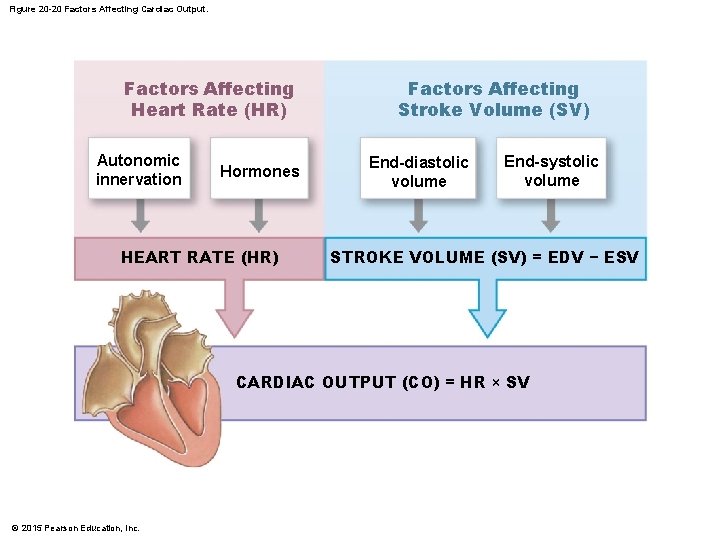
Figure 20 -20 Factors Affecting Cardiac Output. Factors Affecting Heart Rate (HR) Autonomic innervation Hormones HEART RATE (HR) Factors Affecting Stroke Volume (SV) End-diastolic volume End-systolic volume STROKE VOLUME (SV) = EDV − ESV CARDIAC OUTPUT (CO) = HR × SV © 2015 Pearson Education, Inc.

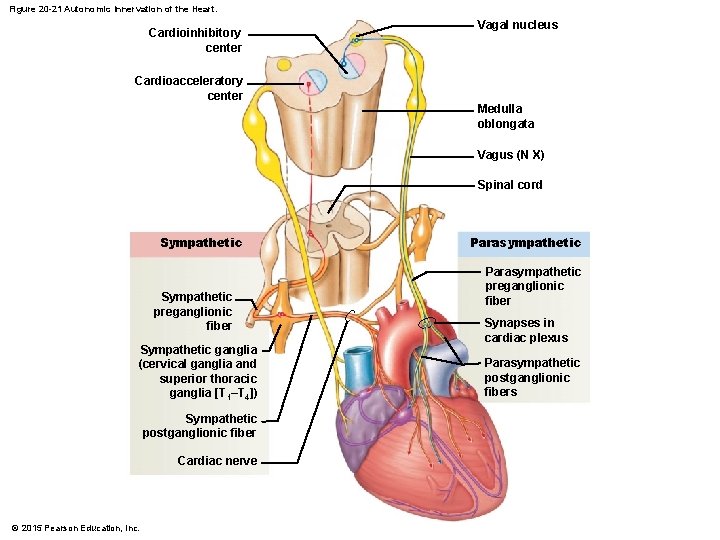
20 -4 Cardiodynamics • Autonomic Innervation • Cardiac plexuses innervate heart • Vagus nerves (N X) carry parasympathetic preganglionic fibers to small ganglia in cardiac plexus • Cardiac centers of medulla oblongata • Cardioacceleratory center controls sympathetic neurons (increases heart rate) • Cardioinhibitory center controls parasympathetic neurons (slows heart rate) © 2015 Pearson Education, Inc.
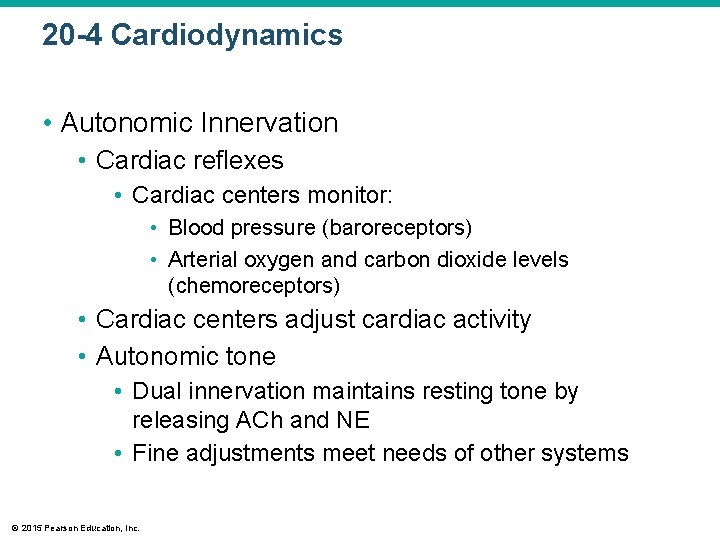
20 -4 Cardiodynamics • Autonomic Innervation • Cardiac reflexes • Cardiac centers monitor: • Blood pressure (baroreceptors) • Arterial oxygen and carbon dioxide levels (chemoreceptors) • Cardiac centers adjust cardiac activity • Autonomic tone • Dual innervation maintains resting tone by releasing ACh and NE • Fine adjustments meet needs of other systems © 2015 Pearson Education, Inc.
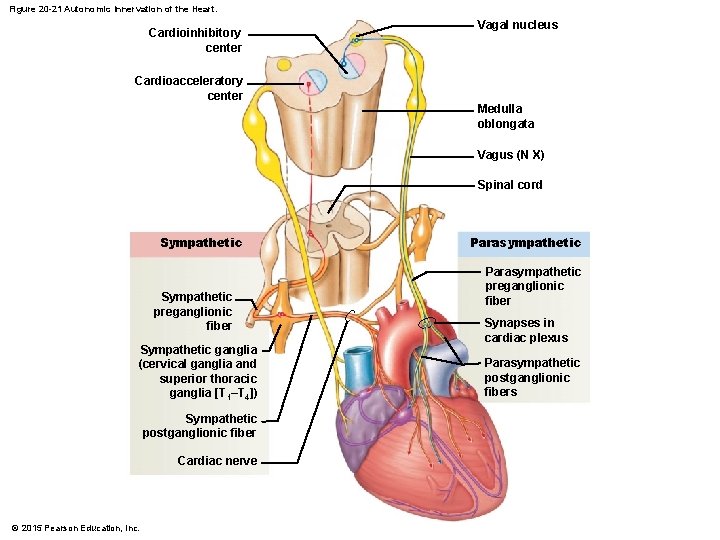
Figure 20 -21 Autonomic Innervation of the Heart. Cardioinhibitory center Vagal nucleus Cardioacceleratory center Medulla oblongata Vagus (N X) Spinal cord Sympathetic preganglionic fiber Sympathetic ganglia (cervical ganglia and superior thoracic ganglia [T 1–T 4]) Sympathetic postganglionic fiber Cardiac nerve © 2015 Pearson Education, Inc. Parasympathetic preganglionic fiber Synapses in cardiac plexus Parasympathetic postganglionic fibers
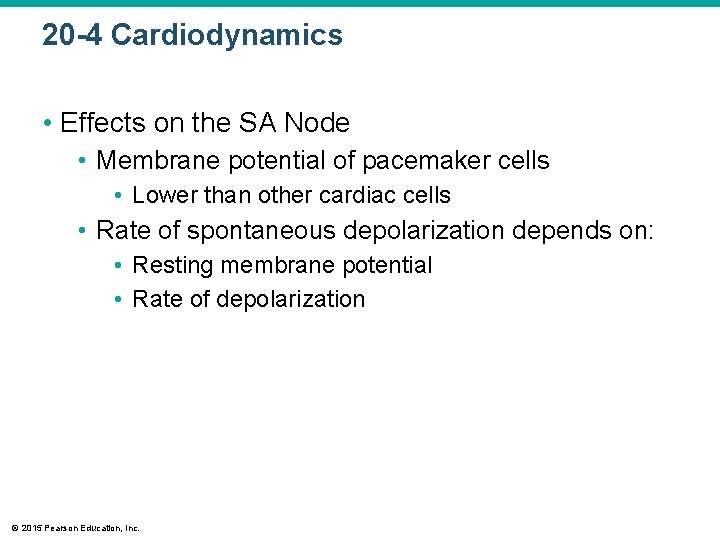
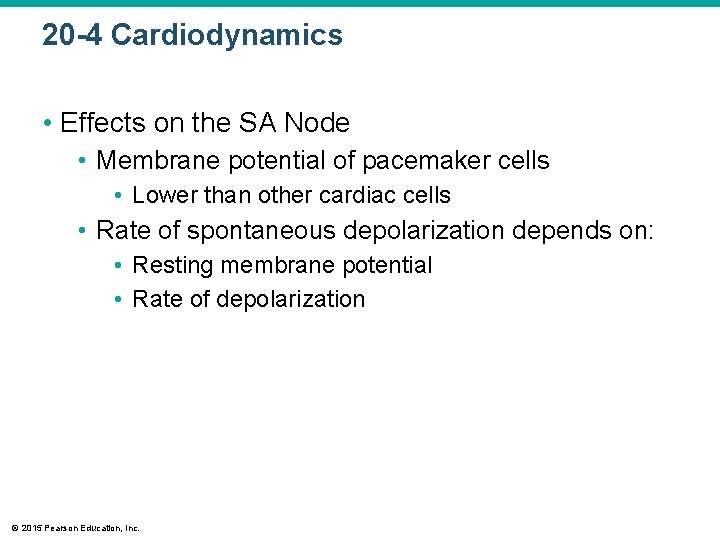
20 -4 Cardiodynamics • Effects on the SA Node • Membrane potential of pacemaker cells • Lower than other cardiac cells • Rate of spontaneous depolarization depends on: • Resting membrane potential • Rate of depolarization © 2015 Pearson Education, Inc.
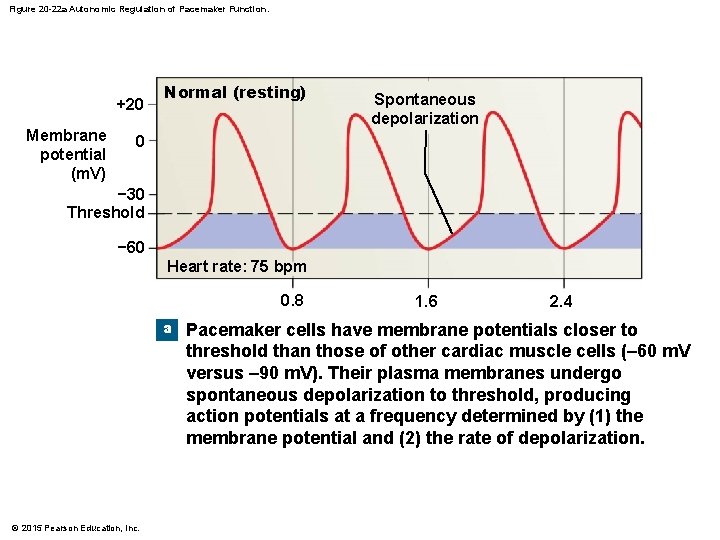
Figure 20 -22 a Autonomic Regulation of Pacemaker Function. +20 Membrane potential (m. V) Normal (resting) Spontaneous depolarization 0 − 30 Threshold − 60 Heart rate: 75 bpm 0. 8 a © 2015 Pearson Education, Inc. 1. 6 2. 4 Pacemaker cells have membrane potentials closer to threshold than those of other cardiac muscle cells (– 60 m. V versus – 90 m. V). Their plasma membranes undergo spontaneous depolarization to threshold, producing action potentials at a frequency determined by (1) the membrane potential and (2) the rate of depolarization.
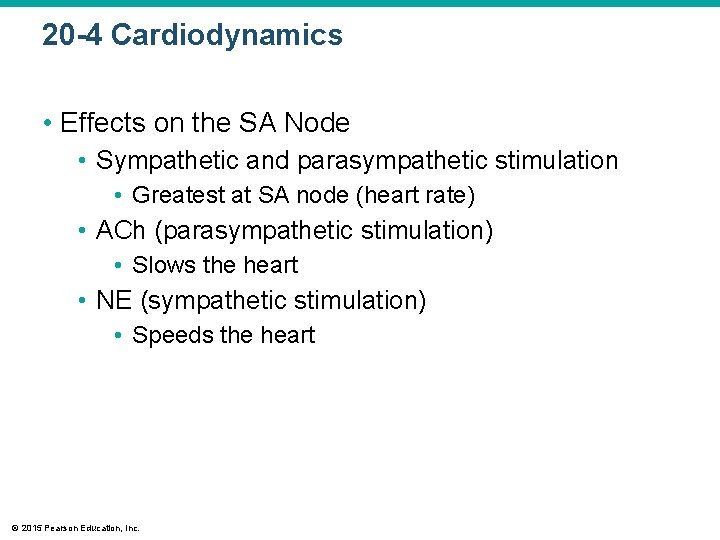
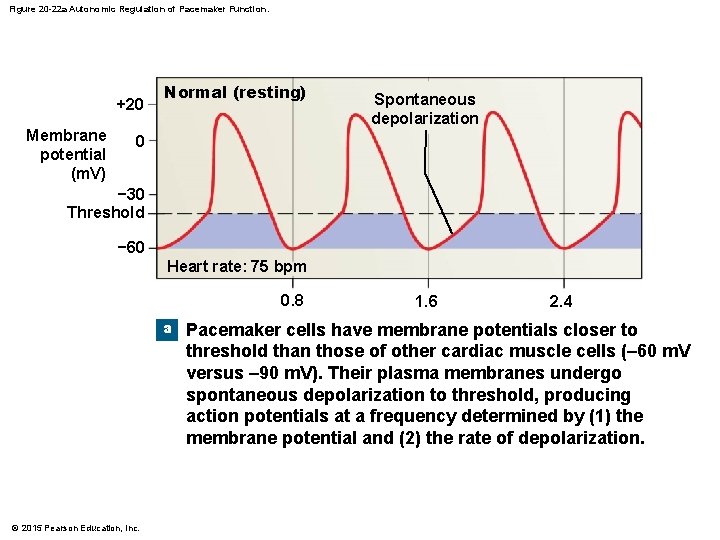
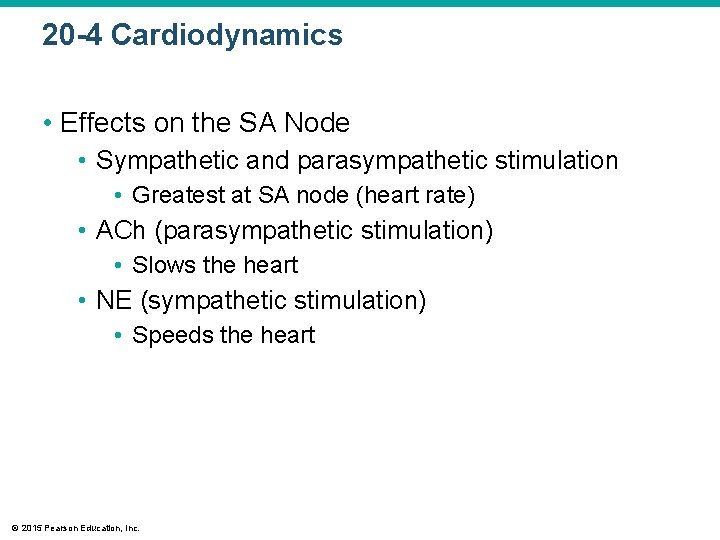
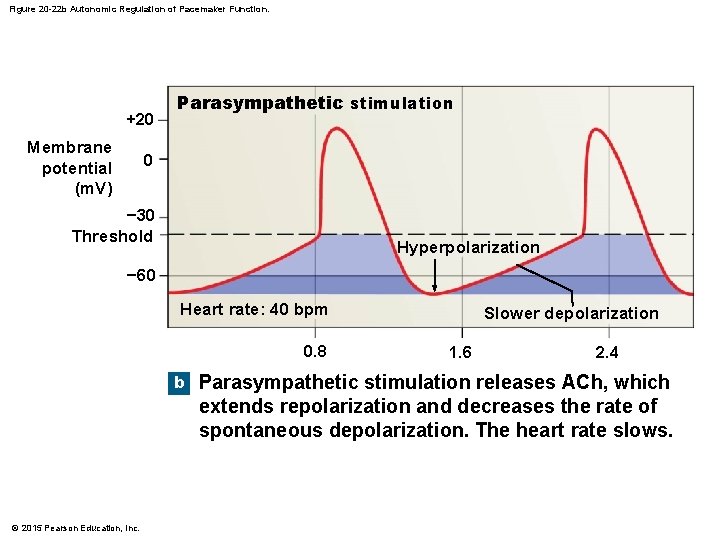
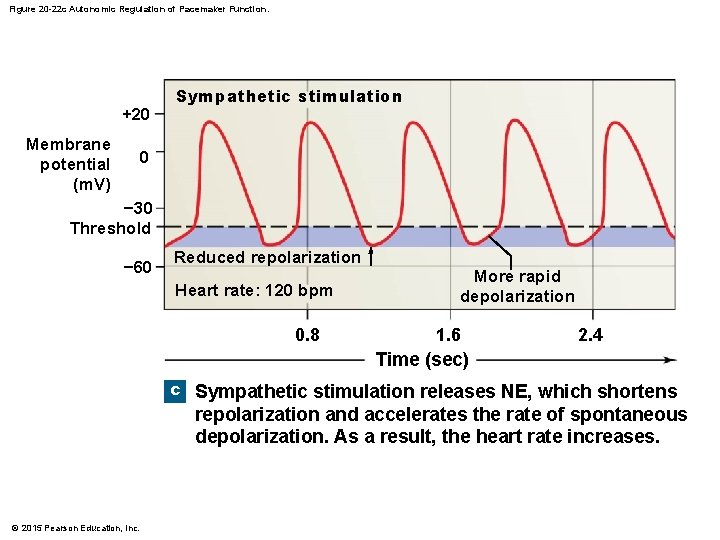
20 -4 Cardiodynamics • Effects on the SA Node • Sympathetic and parasympathetic stimulation • Greatest at SA node (heart rate) • ACh (parasympathetic stimulation) • Slows the heart • NE (sympathetic stimulation) • Speeds the heart © 2015 Pearson Education, Inc.
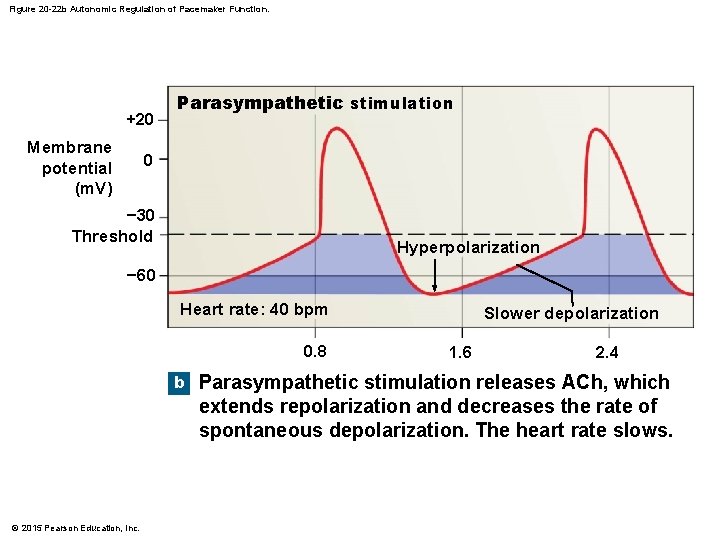
Figure 20 -22 b Autonomic Regulation of Pacemaker Function. +20 Membrane potential (m. V) Parasympathetic stimulation 0 − 30 Threshold Hyperpolarization − 60 Heart rate: 40 bpm 0. 8 b © 2015 Pearson Education, Inc. Slower depolarization 1. 6 2. 4 Parasympathetic stimulation releases ACh, which extends repolarization and decreases the rate of spontaneous depolarization. The heart rate slows.
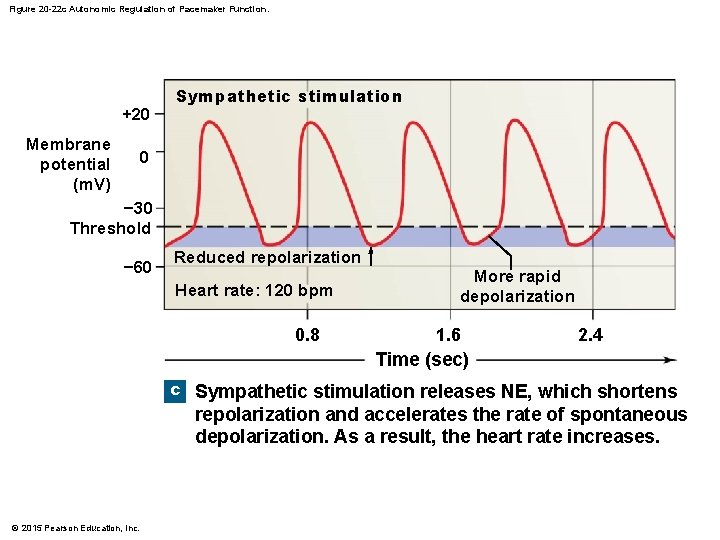
Figure 20 -22 c Autonomic Regulation of Pacemaker Function. +20 Membrane potential (m. V) Sympathetic stimulation 0 − 30 Threshold − 60 Reduced repolarization Heart rate: 120 bpm 0. 8 More rapid depolarization 1. 6 2. 4 Time (sec) c Sympathetic stimulation releases NE, which shortens repolarization and accelerates the rate of spontaneous depolarization. As a result, the heart rate increases. © 2015 Pearson Education, Inc.
20 -4 Cardiodynamics • Atrial Reflex • Also called Bainbridge reflex • Adjusts heart rate in response to venous return • Stretch receptors in right atrium • Trigger increase in heart rate • Through increased sympathetic activity © 2015 Pearson Education, Inc.
20 -4 Cardiodynamics • Hormonal Effects on Heart Rate • Increase heart rate (by sympathetic stimulation of SA node) • Epinephrine (E) • Norepinephrine (NE) • Thyroid hormone © 2015 Pearson Education, Inc.
20 -4 Cardiodynamics • Factors Affecting the Stroke Volume • The EDV – amount of blood a ventricle contains at the end of diastole • Filling time • Duration of ventricular diastole • Venous return • Rate of blood flow during ventricular diastole © 2015 Pearson Education, Inc.
20 -4 Cardiodynamics • Preload • The degree of ventricular stretching during ventricular diastole • Directly proportional to EDV • Affects ability of muscle cells to produce tension © 2015 Pearson Education, Inc.
20 -4 Cardiodynamics • The EDV and Stroke Volume • At rest • EDV is low • Myocardium stretches less • Stroke volume is low • With exercise • EDV increases • Myocardium stretches more • Stroke volume increases © 2015 Pearson Education, Inc.
20 -4 Cardiodynamics • The Frank–Starling Principle • As EDV increases, stroke volume increases • Physical Limits • Ventricular expansion is limited by: • Myocardial connective tissue • The cardiac (fibrous) skeleton • The pericardial sac © 2015 Pearson Education, Inc.
20 -4 Cardiodynamics • End-Systolic Volume (ESV) • Is the amount of blood that remains in the ventricle at the end of ventricular systole © 2015 Pearson Education, Inc.

20 -4 Cardiodynamics • Three Factors That Affect ESV 1. Preload • Ventricular stretching during diastole 2. Contractility • Force produced during contraction, at a given preload 3. Afterload • Tension the ventricle produces to open the semilunar valve and eject blood © 2015 Pearson Education, Inc.
20 -4 Cardiodynamics • Contractility • Is affected by: • Autonomic activity • Hormones © 2015 Pearson Education, Inc.
20 -4 Cardiodynamics • Effects of Autonomic Activity on Contractility • Sympathetic stimulation • NE released by postganglionic fibers of cardiac nerves • Epinephrine and NE released by adrenal medullae • Causes ventricles to contract with more force • Increases ejection fraction and decreases ESV © 2015 Pearson Education, Inc.

20 -4 Cardiodynamics • Effects of Autonomic Activity on Contractility • Parasympathetic activity • Acetylcholine released by vagus nerves • Reduces force of cardiac contractions © 2015 Pearson Education, Inc.
20 -4 Cardiodynamics • Hormones • Many hormones affect heart contraction • Pharmaceutical drugs mimic hormone actions • Stimulate or block beta receptors • Affect calcium ions (e. g. , calcium channel blockers) © 2015 Pearson Education, Inc.
20 -4 Cardiodynamics • Afterload • Is increased by any factor that restricts arterial blood flow • As afterload increases, stroke volume decreases © 2015 Pearson Education, Inc.
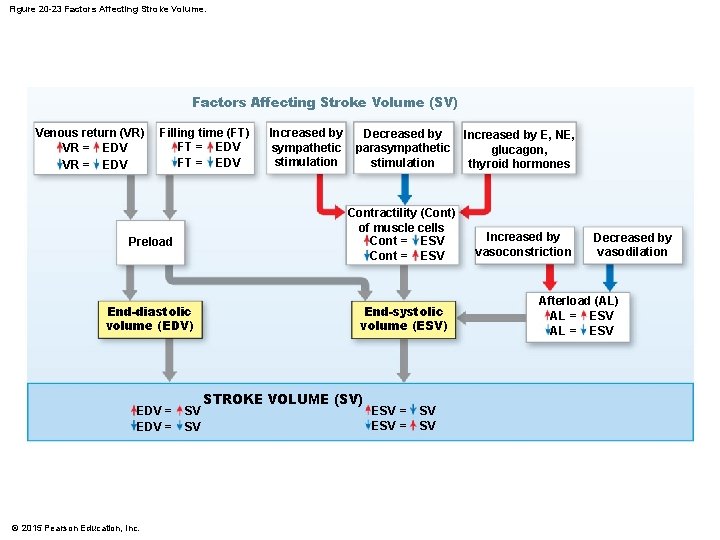
Figure 20 -23 Factors Affecting Stroke Volume (SV) Venous return (VR) VR = EDV Filling time (FT) FT = EDV End-diastolic volume (EDV) © 2015 Pearson Education, Inc. Decreased by parasympathetic stimulation Contractility (Cont) of muscle cells Cont = ESV Preload EDV = Increased by sympathetic stimulation SV SV End-systolic volume (ESV) STROKE VOLUME (SV) ESV = SV SV Increased by E, NE, glucagon, thyroid hormones Increased by vasoconstriction Decreased by vasodilation Afterload (AL) AL = ESV
20 -4 Cardiodynamics • Summary: The Control of Cardiac Output • Heart rate control factors • Autonomic nervous system • Sympathetic and parasympathetic • Circulating hormones • Venous return and stretch receptors © 2015 Pearson Education, Inc.
20 -4 Cardiodynamics • Summary: The Control of Cardiac Output • Stroke volume control factors • EDV • Filling time and rate of venous return • ESV • Preload, contractility, afterload © 2015 Pearson Education, Inc.

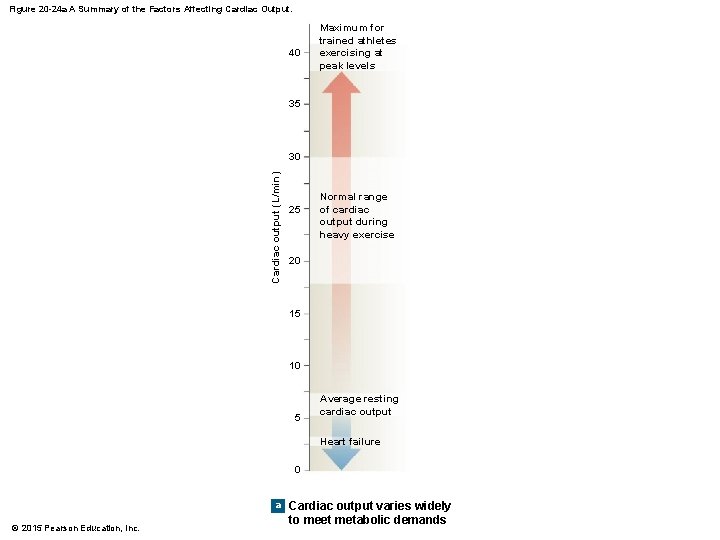
20 -4 Cardiodynamics • Cardiac Reserve • The difference between resting and maximal cardiac outputs © 2015 Pearson Education, Inc.

20 -4 Cardiodynamics • The Heart and Cardiovascular System • Cardiovascular regulation • Ensures adequate circulation to body tissues • Cardiovascular centers • Control heart and peripheral blood vessels • Cardiovascular system responds to: • Changing activity patterns • Circulatory emergencies © 2015 Pearson Education, Inc.
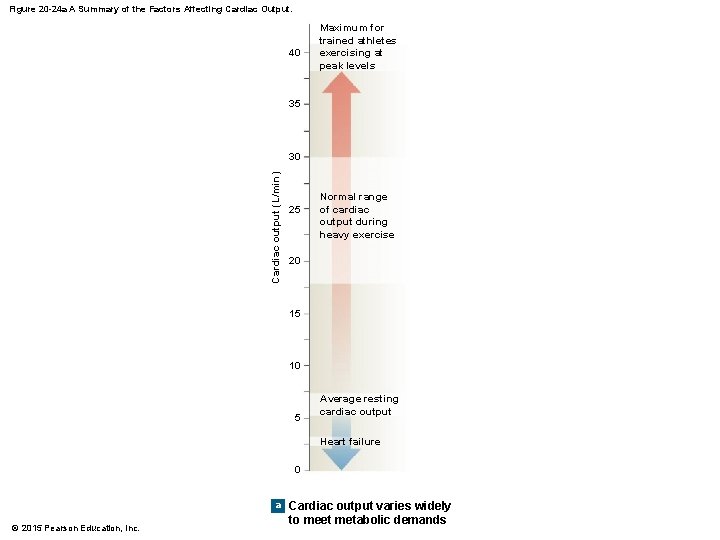
Figure 20 -24 a A Summary of the Factors Affecting Cardiac Output. 40 Maximum for trained athletes exercising at peak levels 35 Cardiac output (L/min) 30 25 Normal range of cardiac output during heavy exercise 20 15 10 5 Average resting cardiac output Heart failure 0 a © 2015 Pearson Education, Inc. Cardiac output varies widely to meet metabolic demands
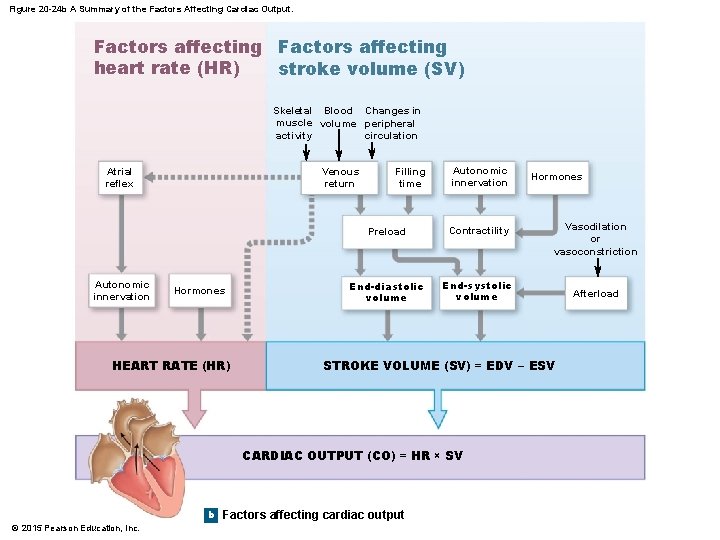
Figure 20 -24 b A Summary of the Factors Affecting Cardiac Output. Factors affecting heart rate (HR) stroke volume (SV) Skeletal Blood Changes in muscle volume peripheral activity circulation Atrial reflex Autonomic innervation Venous return Hormones HEART RATE (HR) Filling time Autonomic innervation Preload Contractility End-diastolic volume End-systolic volume b Vasodilation or vasoconstriction STROKE VOLUME (SV) = EDV − ESV CARDIAC OUTPUT (CO) = HR × SV © 2015 Pearson Education, Inc. Hormones Factors affecting cardiac output Afterload