Pharmacological Management of Atrial and Ventricular Arrhythmias Monica

- Slides: 97
Pharmacological Management of Atrial and Ventricular Arrhythmias Monica Knapp, ARNP Acute Care Nurse Practitioner Teaching Associate, Electrophysiology University of Washington School of Medicine Seattle, WA Pharmacology 515 - November 8, 2011
Objectives • Review cardiac electrophysiology • Outline ACLS Guidelines for bradycardias and tachycardias • Discuss pharmacological agents used in the management of atrial and ventricular arrhythmias – mechanism of action, indications, dosing, adverse reactions, monitoring • Case studies
Cardiac Electrophysiology: Cardiac Automaticity • Cardiac Automaticity: result of spontaneous and repetitive depolarization of pacemaker cells. In turn, this leads to generation of action potentials • Action Potential (AP): time change in electrical voltage across traveling across a cardiac cell membrane during cell depolarization & repolarization • Depolarization: changes in concentrations of charged particles between the inside and outside of the cell that ultimately result in contraction • Resting Membrane Potential: result of a difference in the concentration of cations (+) and anions (-) between the inside of the cell and the outside of the cell; RMP is -90 m. V. – Inside cell is K+ rich; outside is Na+ rich. – At rest, cell membrane is permeable to K+ only so it can leak out
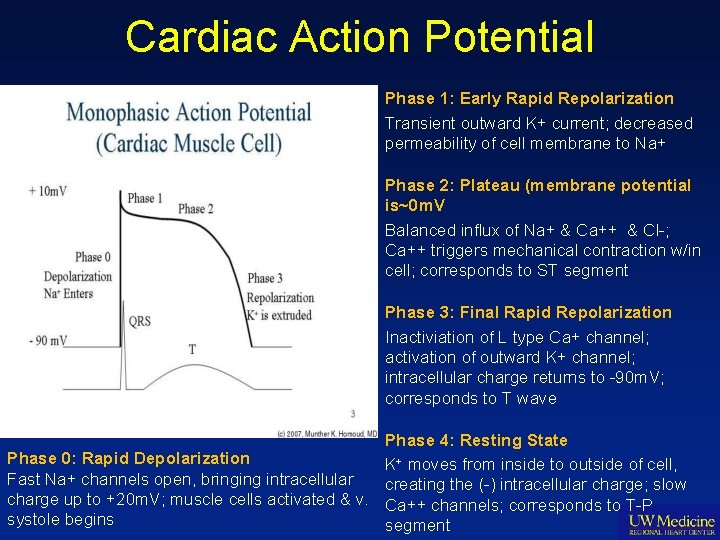
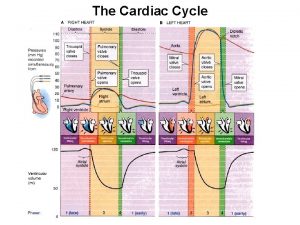
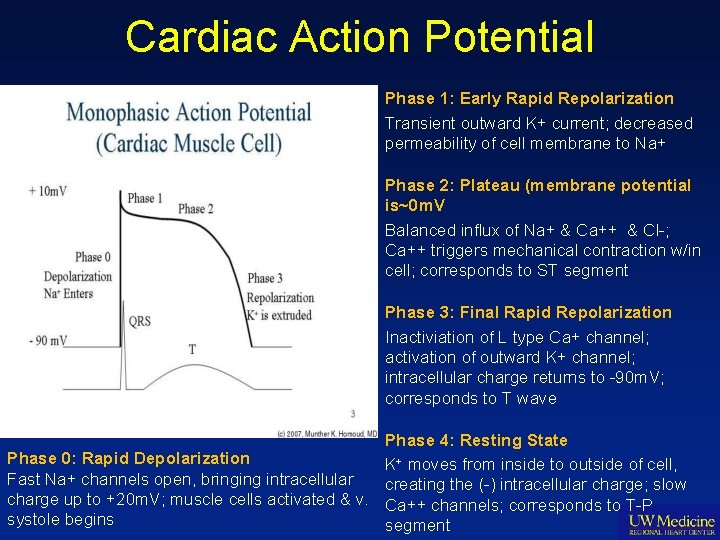
Cardiac Action Potential Phase 1: Early Rapid Repolarization Transient outward K+ current; decreased permeability of cell membrane to Na+ Phase 2: Plateau (membrane potential is~0 m. V Balanced influx of Na+ & Ca++ & Cl-; Ca++ triggers mechanical contraction w/in cell; corresponds to ST segment Phase 3: Final Rapid Repolarization Inactiviation of L type Ca+ channel; activation of outward K+ channel; intracellular charge returns to -90 m. V; corresponds to T wave Phase 4: Resting State Phase 0: Rapid Depolarization K+ moves from inside to outside of cell, Fast Na+ channels open, bringing intracellular creating the (-) intracellular charge; slow charge up to +20 m. V; muscle cells activated & v. Ca++ channels; corresponds to T-P systole begins segment
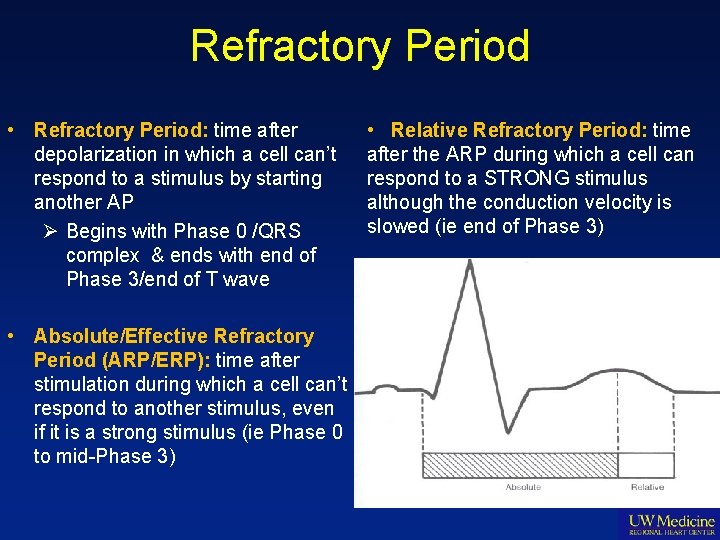
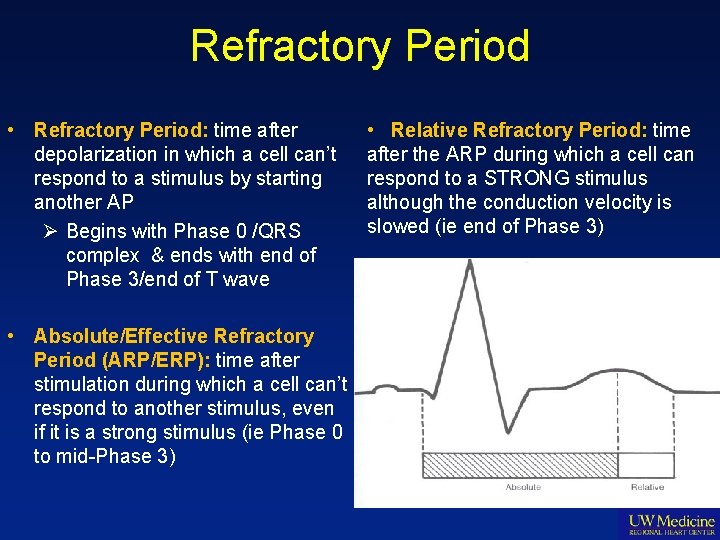
Refractory Period • Refractory Period: time after depolarization in which a cell can’t respond to a stimulus by starting another AP Ø Begins with Phase 0 /QRS complex & ends with end of Phase 3/end of T wave • Absolute/Effective Refractory Period (ARP/ERP): time after stimulation during which a cell can’t respond to another stimulus, even if it is a strong stimulus (ie Phase 0 to mid-Phase 3) • Relative Refractory Period: time after the ARP during which a cell can respond to a STRONG stimulus although the conduction velocity is slowed (ie end of Phase 3)
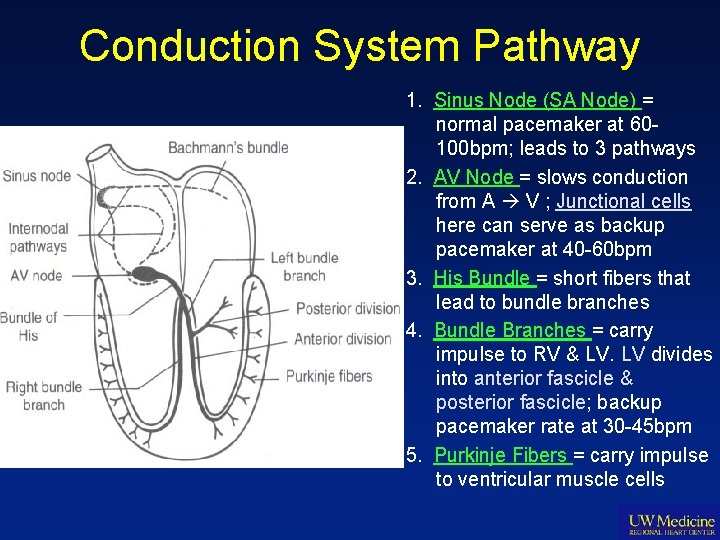
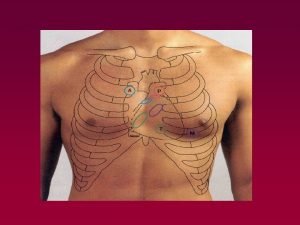
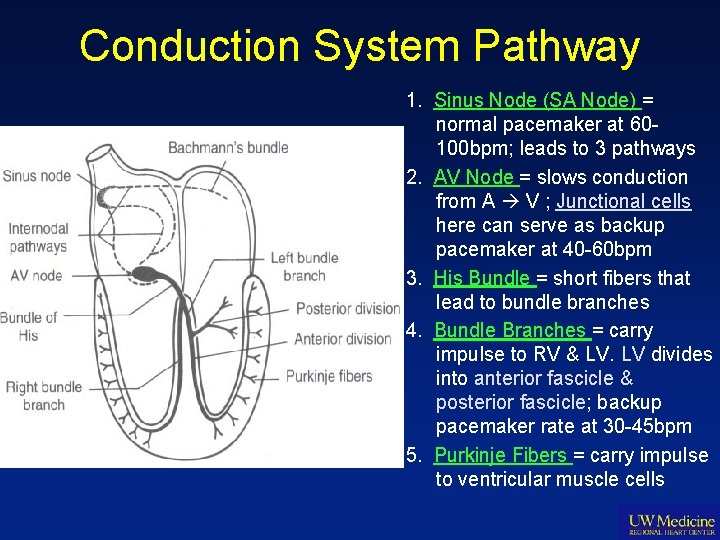
Conduction System Pathway 1. Sinus Node (SA Node) = normal pacemaker at 60100 bpm; leads to 3 pathways 2. AV Node = slows conduction from A V ; Junctional cells here can serve as backup pacemaker at 40 -60 bpm 3. His Bundle = short fibers that lead to bundle branches 4. Bundle Branches = carry impulse to RV & LV. LV divides into anterior fascicle & posterior fascicle; backup pacemaker rate at 30 -45 bpm 5. Purkinje Fibers = carry impulse to ventricular muscle cells
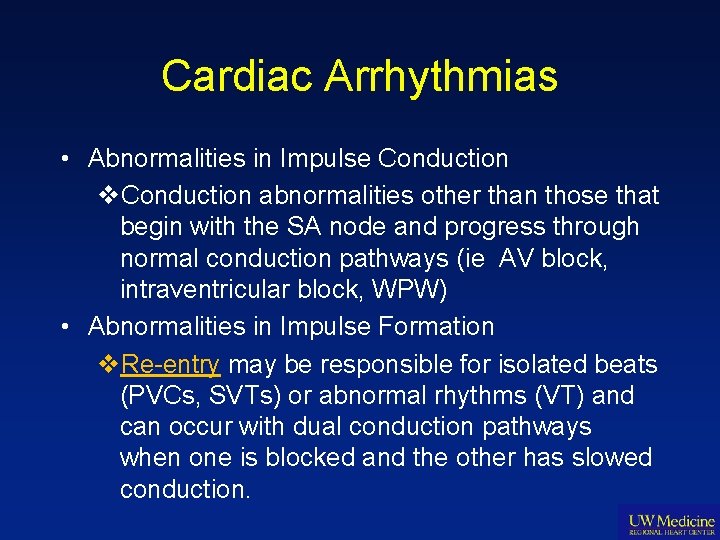
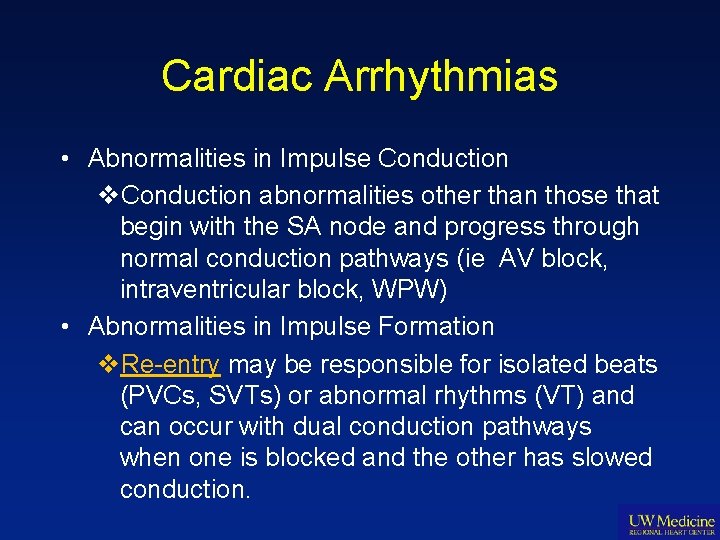
Cardiac Arrhythmias • Abnormalities in Impulse Conduction v. Conduction abnormalities other than those that begin with the SA node and progress through normal conduction pathways (ie AV block, intraventricular block, WPW) • Abnormalities in Impulse Formation v. Re-entry may be responsible for isolated beats (PVCs, SVTs) or abnormal rhythms (VT) and can occur with dual conduction pathways when one is blocked and the other has slowed conduction.
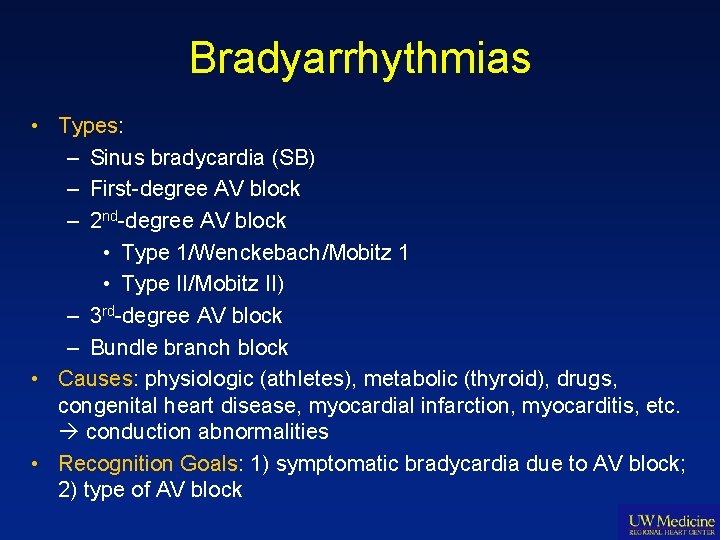
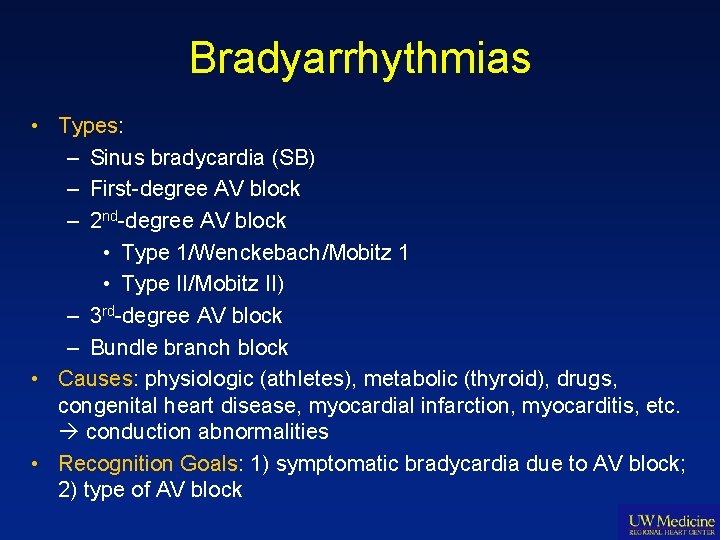
Bradyarrhythmias • Types: – Sinus bradycardia (SB) – First-degree AV block – 2 nd-degree AV block • Type 1/Wenckebach/Mobitz 1 • Type II/Mobitz II) – 3 rd-degree AV block – Bundle branch block • Causes: physiologic (athletes), metabolic (thyroid), drugs, congenital heart disease, myocardial infarction, myocarditis, etc. conduction abnormalities • Recognition Goals: 1) symptomatic bradycardia due to AV block; 2) type of AV block
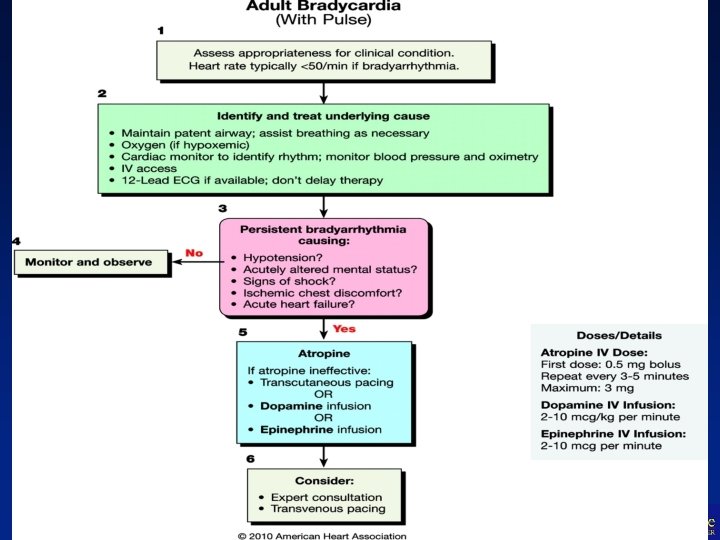
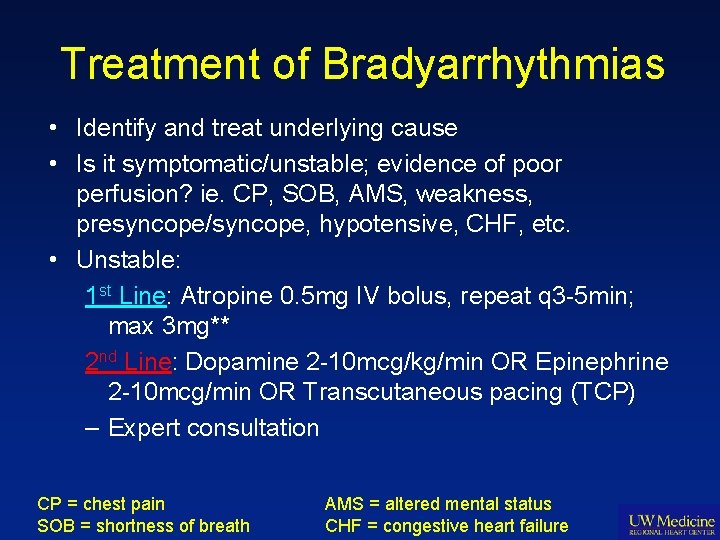
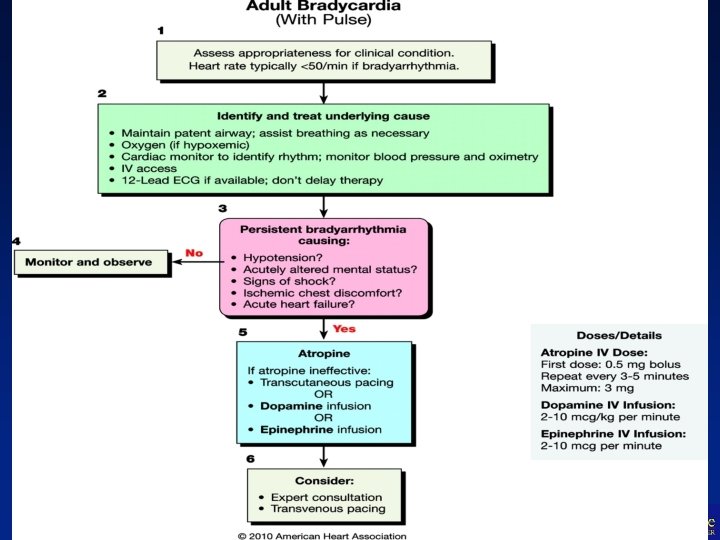
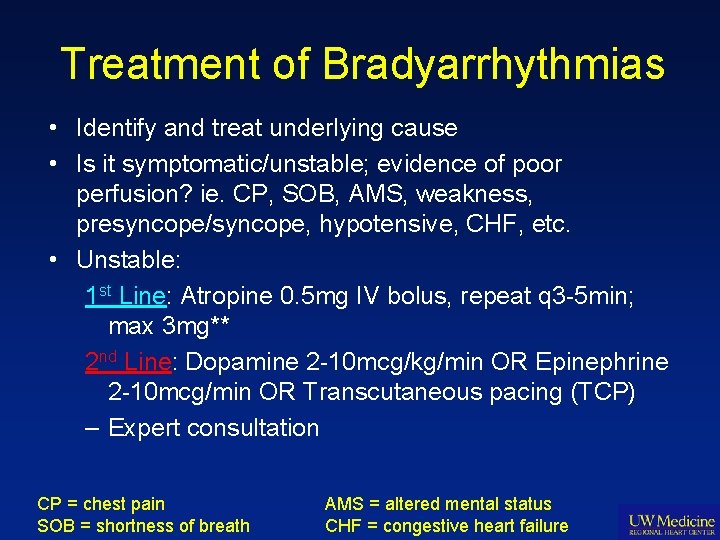
Treatment of Bradyarrhythmias • Identify and treat underlying cause • Is it symptomatic/unstable; evidence of poor perfusion? ie. CP, SOB, AMS, weakness, presyncope/syncope, hypotensive, CHF, etc. • Unstable: 1 st Line: Atropine 0. 5 mg IV bolus, repeat q 3 -5 min; max 3 mg** 2 nd Line: Dopamine 2 -10 mcg/kg/min OR Epinephrine 2 -10 mcg/min OR Transcutaneous pacing (TCP) – Expert consultation CP = chest pain SOB = shortness of breath AMS = altered mental status CHF = congestive heart failure
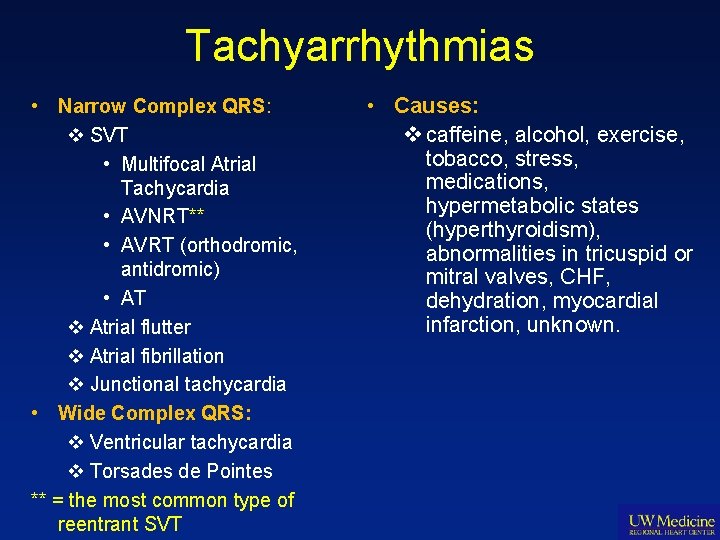
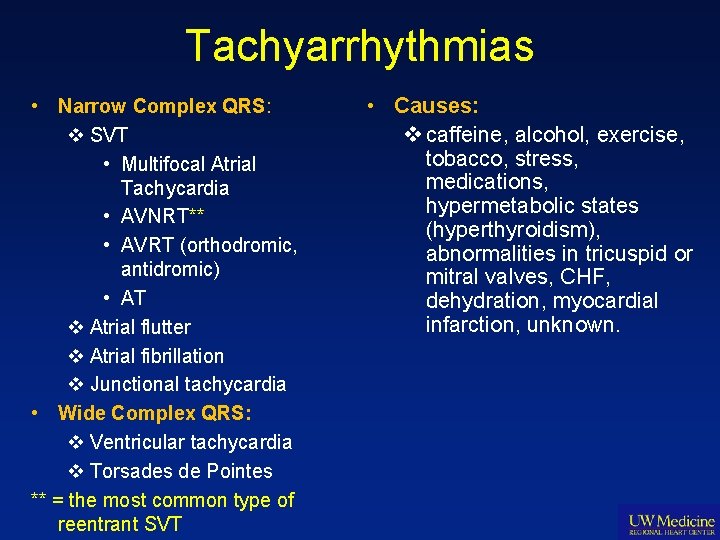
Tachyarrhythmias • Narrow Complex QRS: v SVT • Multifocal Atrial Tachycardia • AVNRT** • AVRT (orthodromic, antidromic) • AT v Atrial flutter v Atrial fibrillation v Junctional tachycardia • Wide Complex QRS: v Ventricular tachycardia v Torsades de Pointes ** = the most common type of reentrant SVT • Causes: v caffeine, alcohol, exercise, tobacco, stress, medications, hypermetabolic states (hyperthyroidism), abnormalities in tricuspid or mitral valves, CHF, dehydration, myocardial infarction, unknown.
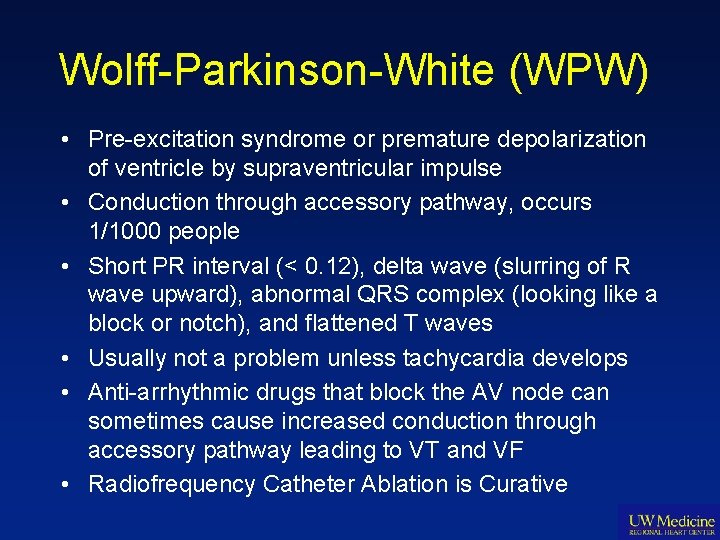
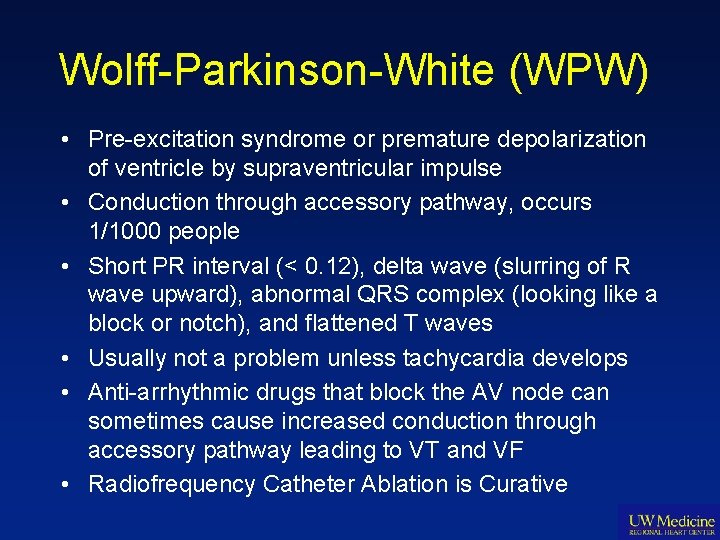
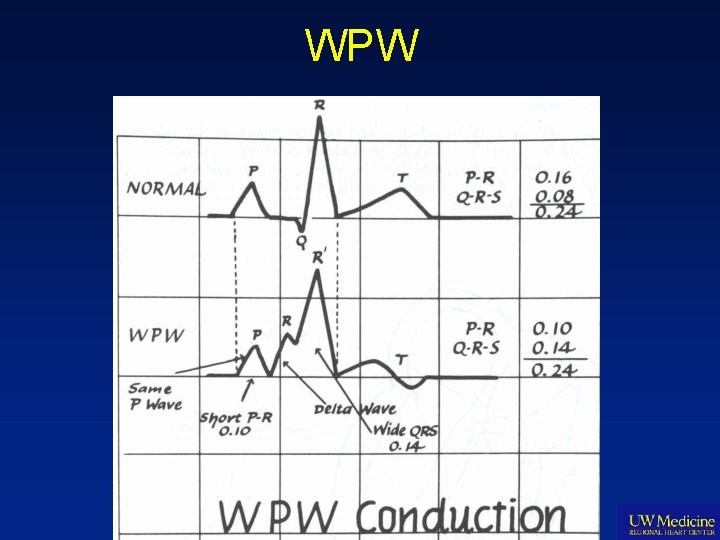
Wolff-Parkinson-White (WPW) • Pre-excitation syndrome or premature depolarization of ventricle by supraventricular impulse • Conduction through accessory pathway, occurs 1/1000 people • Short PR interval (< 0. 12), delta wave (slurring of R wave upward), abnormal QRS complex (looking like a block or notch), and flattened T waves • Usually not a problem unless tachycardia develops • Anti-arrhythmic drugs that block the AV node can sometimes cause increased conduction through accessory pathway leading to VT and VF • Radiofrequency Catheter Ablation is Curative
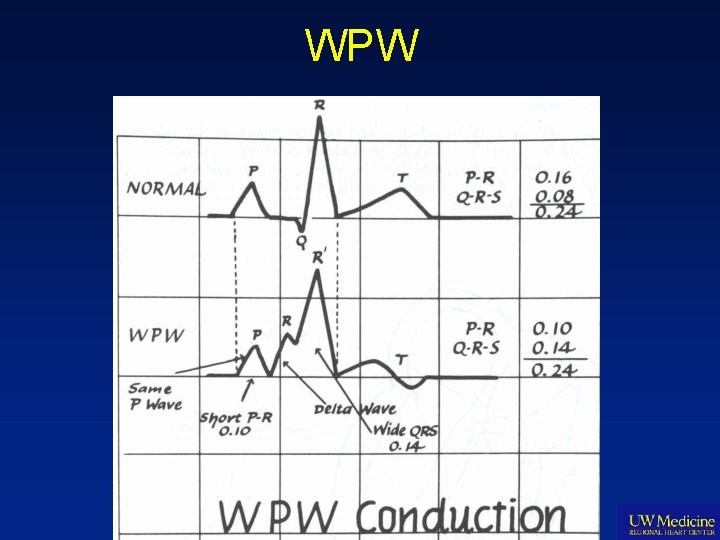
WPW
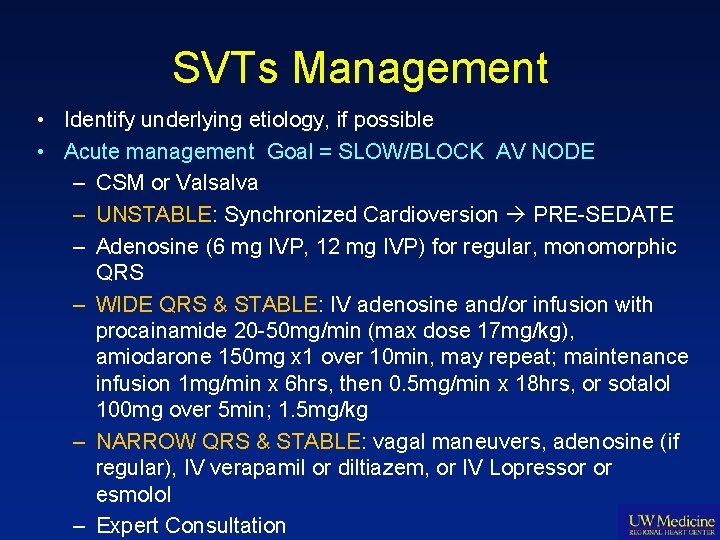
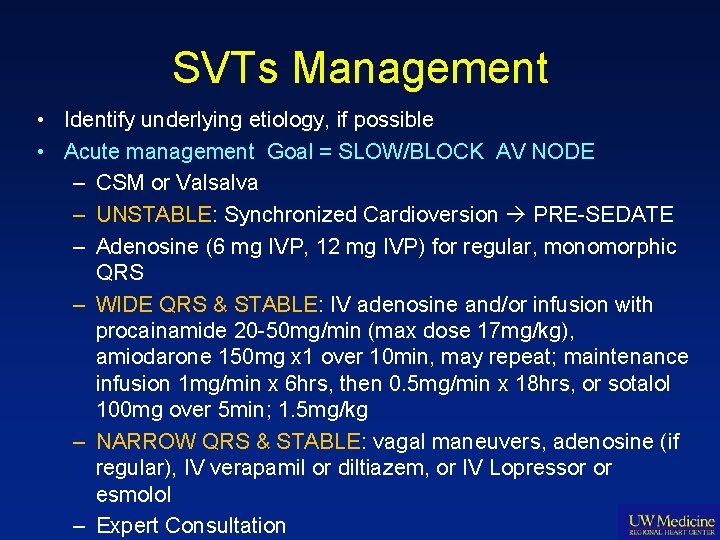
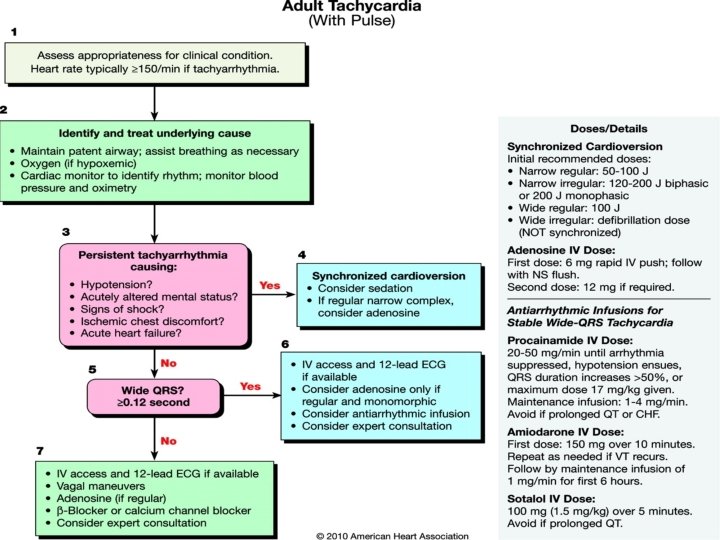
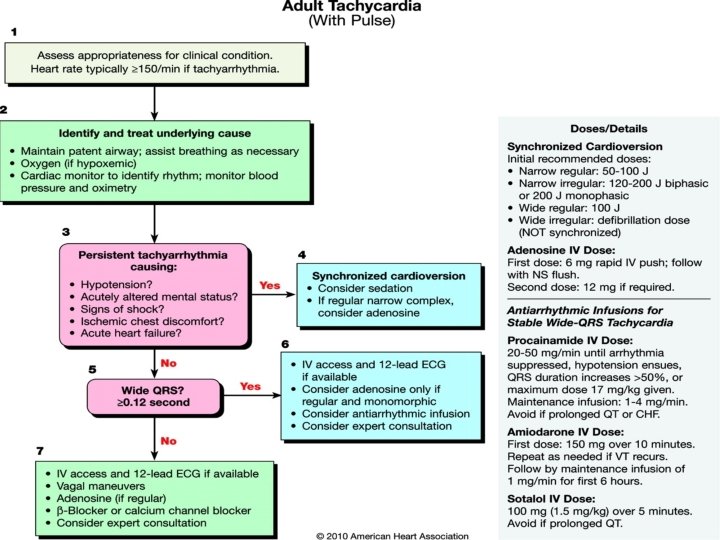
SVTs Management • Identify underlying etiology, if possible • Acute management Goal = SLOW/BLOCK AV NODE – CSM or Valsalva – UNSTABLE: Synchronized Cardioversion PRE-SEDATE – Adenosine (6 mg IVP, 12 mg IVP) for regular, monomorphic QRS – WIDE QRS & STABLE: IV adenosine and/or infusion with procainamide 20 -50 mg/min (max dose 17 mg/kg), amiodarone 150 mg x 1 over 10 min, may repeat; maintenance infusion 1 mg/min x 6 hrs, then 0. 5 mg/min x 18 hrs, or sotalol 100 mg over 5 min; 1. 5 mg/kg – NARROW QRS & STABLE: vagal maneuvers, adenosine (if regular), IV verapamil or diltiazem, or IV Lopressor or esmolol – Expert Consultation
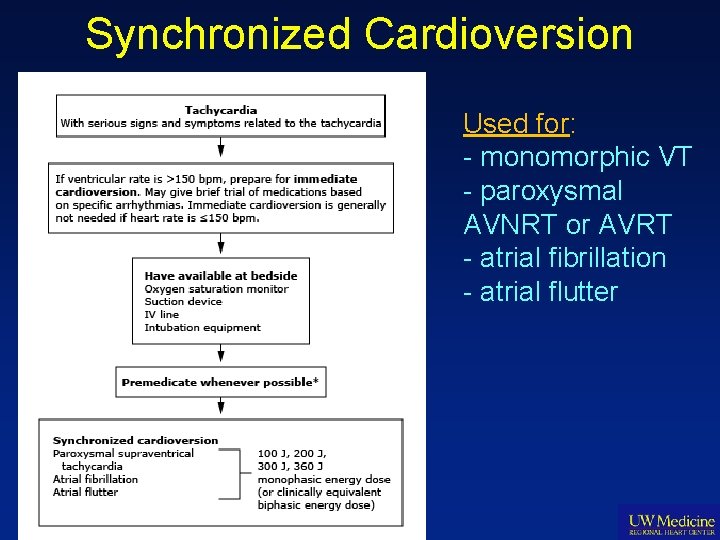
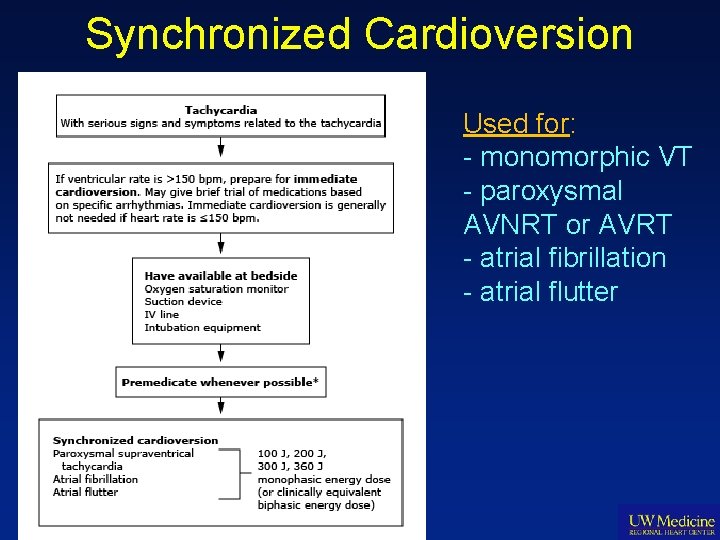
Synchronized Cardioversion Used for: - monomorphic VT - paroxysmal AVNRT or AVRT - atrial fibrillation - atrial flutter
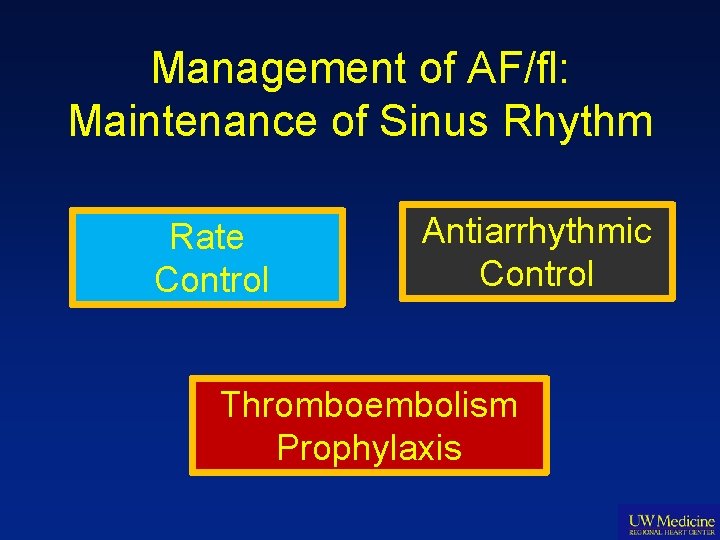
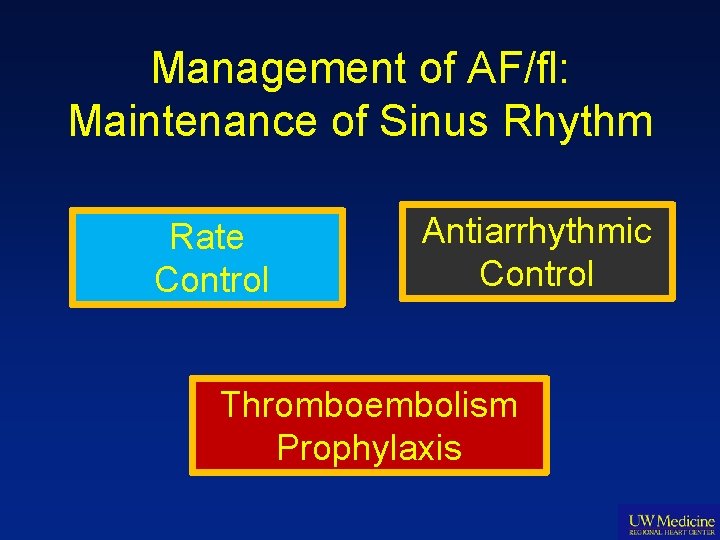
Management of AF/fl: Maintenance of Sinus Rhythm Rate Control Antiarrhythmic Control Thromboembolism Prophylaxis
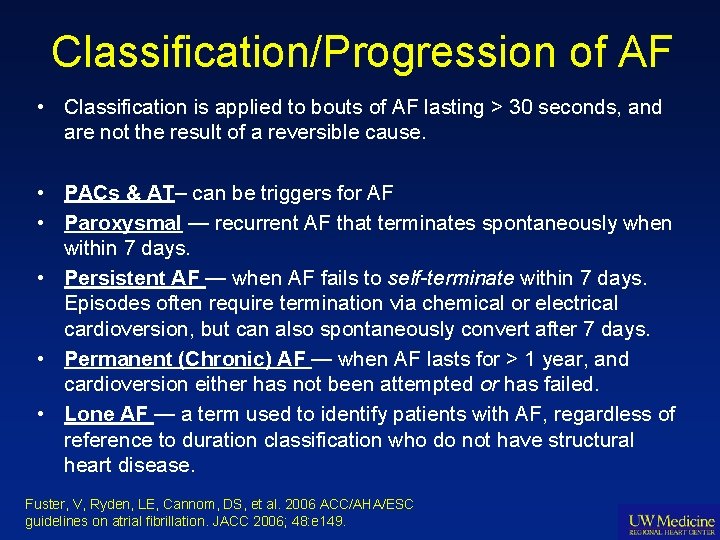
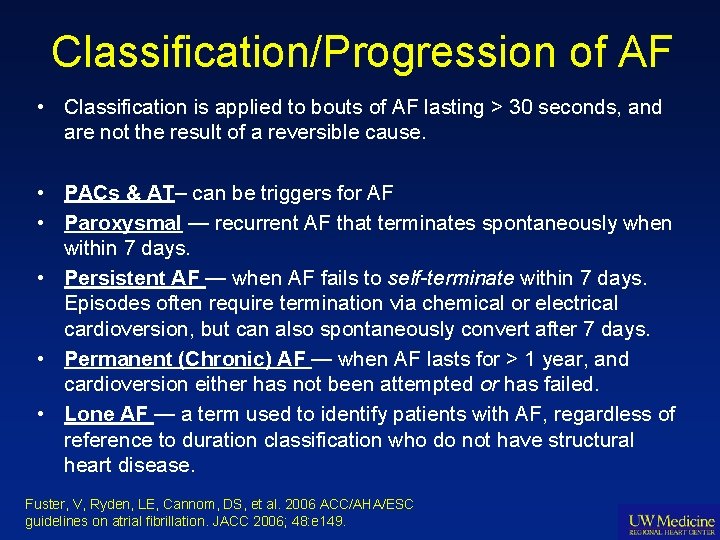
Classification/Progression of AF • Classification is applied to bouts of AF lasting > 30 seconds, and are not the result of a reversible cause. • PACs & AT– can be triggers for AF • Paroxysmal — recurrent AF that terminates spontaneously when within 7 days. • Persistent AF — when AF fails to self-terminate within 7 days. Episodes often require termination via chemical or electrical cardioversion, but can also spontaneously convert after 7 days. • Permanent (Chronic) AF — when AF lasts for > 1 year, and cardioversion either has not been attempted or has failed. • Lone AF — a term used to identify patients with AF, regardless of reference to duration classification who do not have structural heart disease. Fuster, V, Ryden, LE, Cannom, DS, et al. 2006 ACC/AHA/ESC guidelines on atrial fibrillation. JACC 2006; 48: e 149.
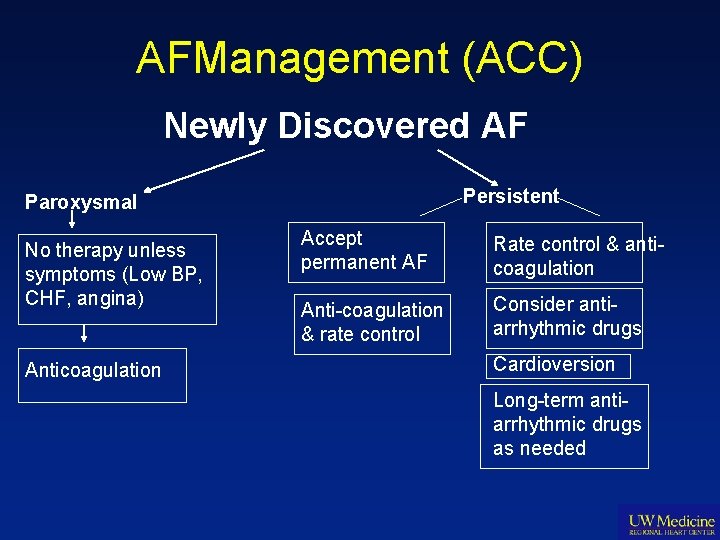
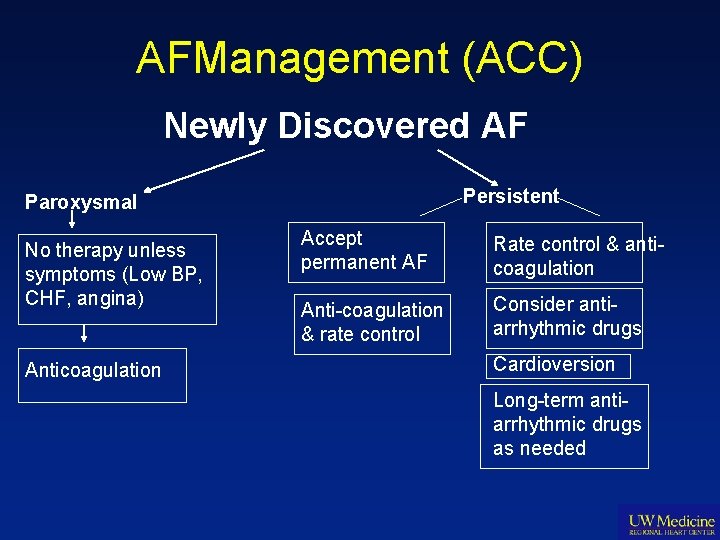
AFManagement (ACC) Newly Discovered AF Persistent Paroxysmal No therapy unless symptoms (Low BP, CHF, angina) Anticoagulation Accept permanent AF Rate control & anticoagulation Anti-coagulation & rate control Consider antiarrhythmic drugs Cardioversion Long-term antiarrhythmic drugs as needed
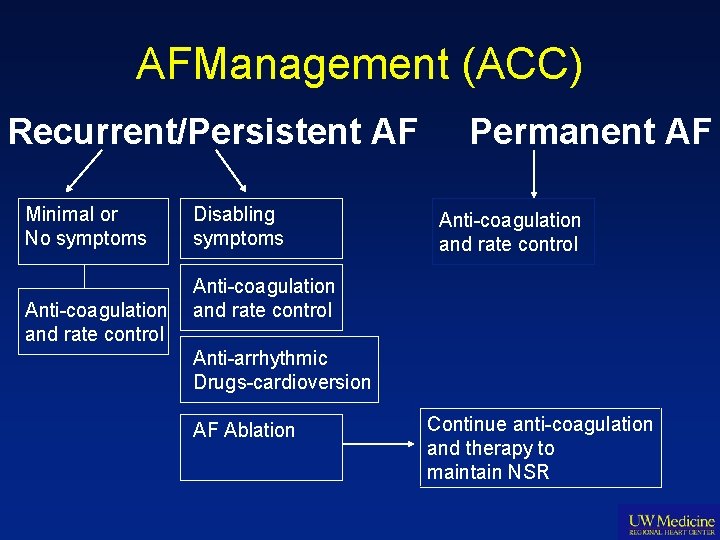
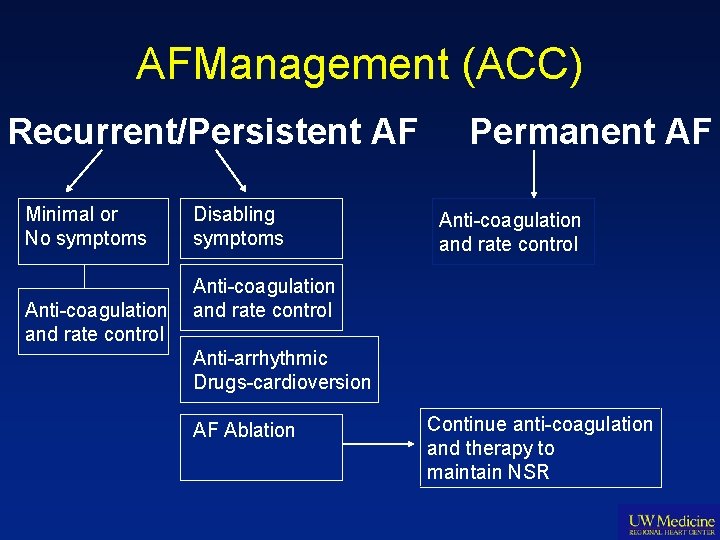
AFManagement (ACC) Recurrent/Persistent AF Minimal or No symptoms Anti-coagulation and rate control Disabling symptoms Permanent AF Anti-coagulation and rate control Anti-arrhythmic Drugs-cardioversion AF Ablation Continue anti-coagulation and therapy to maintain NSR
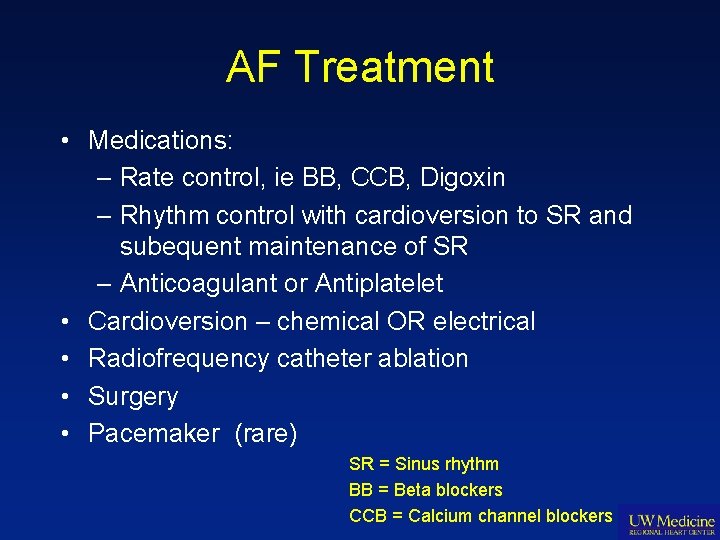
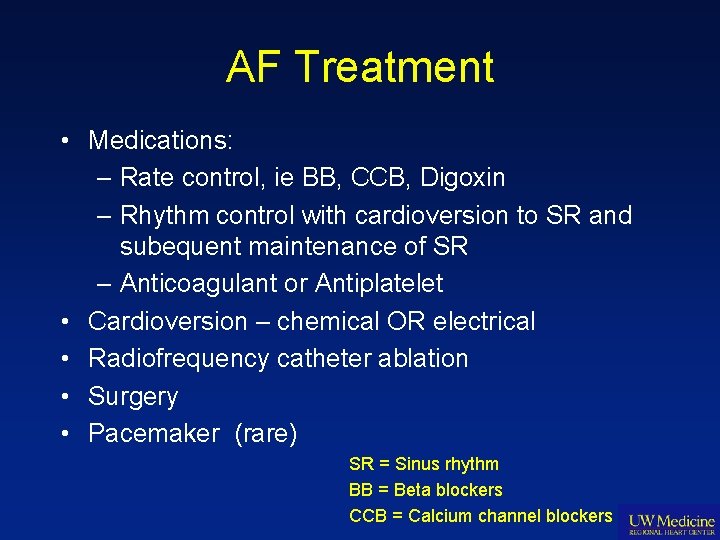
AF Treatment • Medications: – Rate control, ie BB, CCB, Digoxin – Rhythm control with cardioversion to SR and subequent maintenance of SR – Anticoagulant or Antiplatelet • Cardioversion – chemical OR electrical • Radiofrequency catheter ablation • Surgery • Pacemaker (rare) SR = Sinus rhythm BB = Beta blockers CCB = Calcium channel blockers
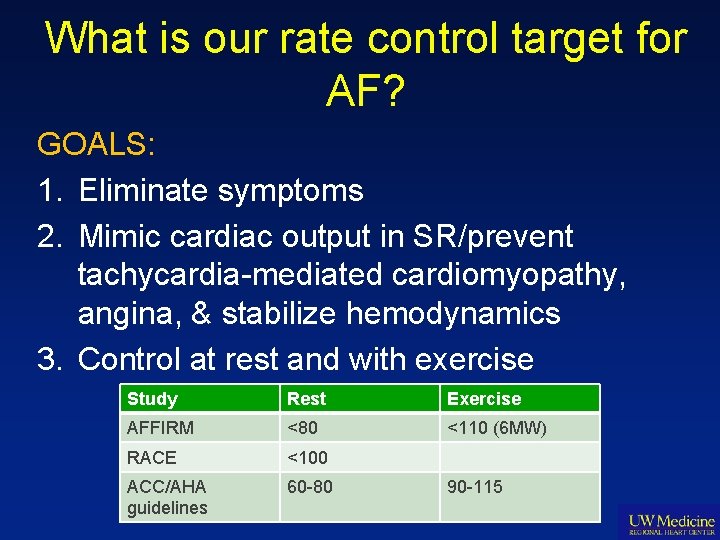
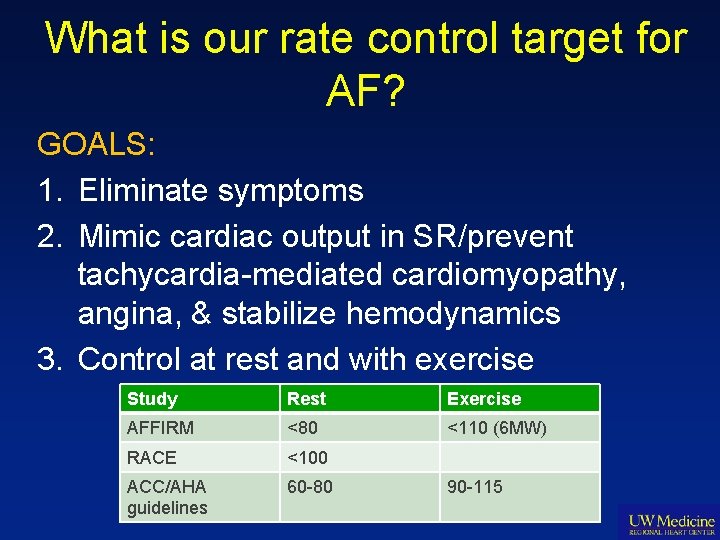
What is our rate control target for AF? GOALS: 1. Eliminate symptoms 2. Mimic cardiac output in SR/prevent tachycardia-mediated cardiomyopathy, angina, & stabilize hemodynamics 3. Control at rest and with exercise Study Rest Exercise AFFIRM <80 <110 (6 MW) RACE <100 ACC/AHA guidelines 60 -80 90 -115
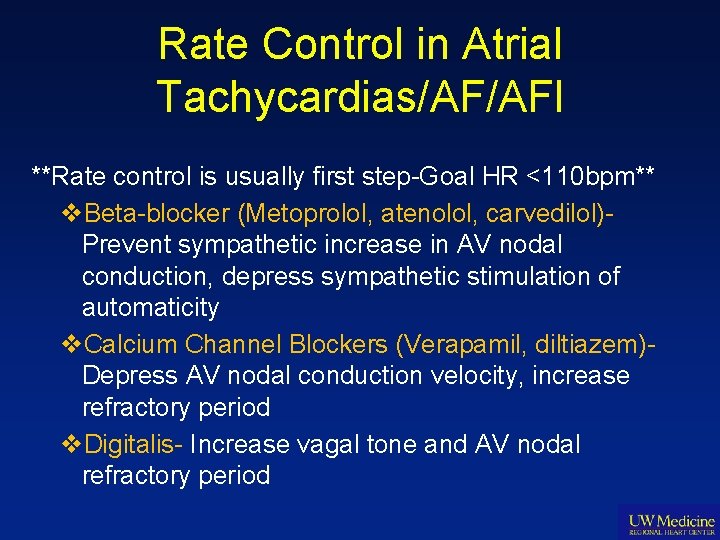
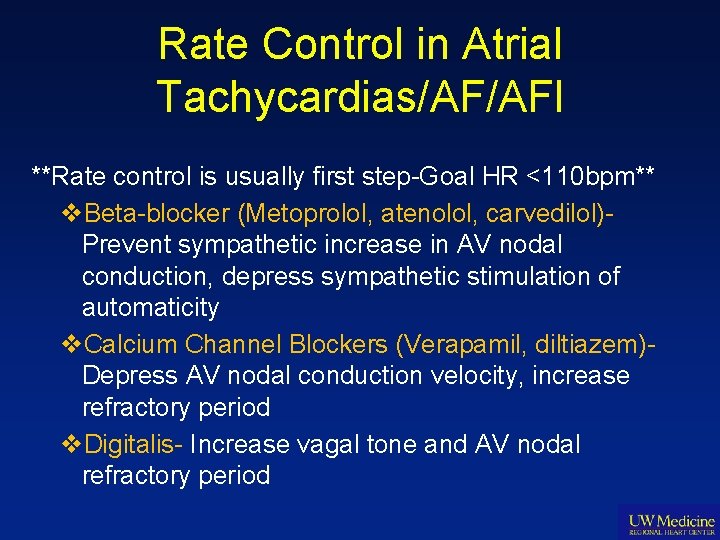
Rate Control in Atrial Tachycardias/AF/AFl **Rate control is usually first step-Goal HR <110 bpm** v. Beta-blocker (Metoprolol, atenolol, carvedilol)Prevent sympathetic increase in AV nodal conduction, depress sympathetic stimulation of automaticity v. Calcium Channel Blockers (Verapamil, diltiazem)Depress AV nodal conduction velocity, increase refractory period v. Digitalis- Increase vagal tone and AV nodal refractory period
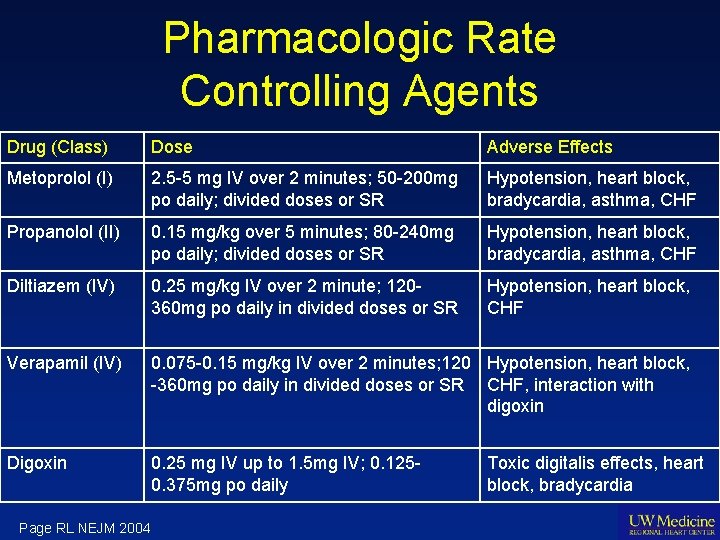
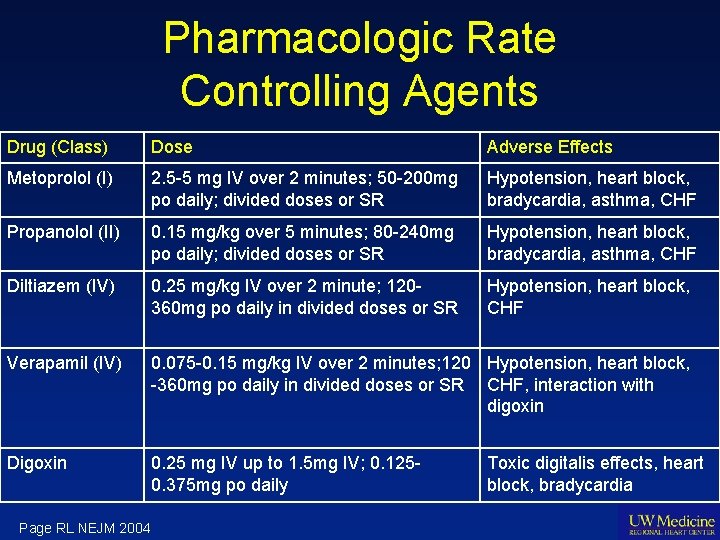
Pharmacologic Rate Controlling Agents Drug (Class) Dose Adverse Effects Metoprolol (I) 2. 5 -5 mg IV over 2 minutes; 50 -200 mg po daily; divided doses or SR Hypotension, heart block, bradycardia, asthma, CHF Propanolol (II) 0. 15 mg/kg over 5 minutes; 80 -240 mg po daily; divided doses or SR Hypotension, heart block, bradycardia, asthma, CHF Diltiazem (IV) 0. 25 mg/kg IV over 2 minute; 120360 mg po daily in divided doses or SR Hypotension, heart block, CHF Verapamil (IV) 0. 075 -0. 15 mg/kg IV over 2 minutes; 120 Hypotension, heart block, -360 mg po daily in divided doses or SR CHF, interaction with digoxin Digoxin 0. 25 mg IV up to 1. 5 mg IV; 0. 1250. 375 mg po daily Page RL NEJM 2004 Toxic digitalis effects, heart block, bradycardia
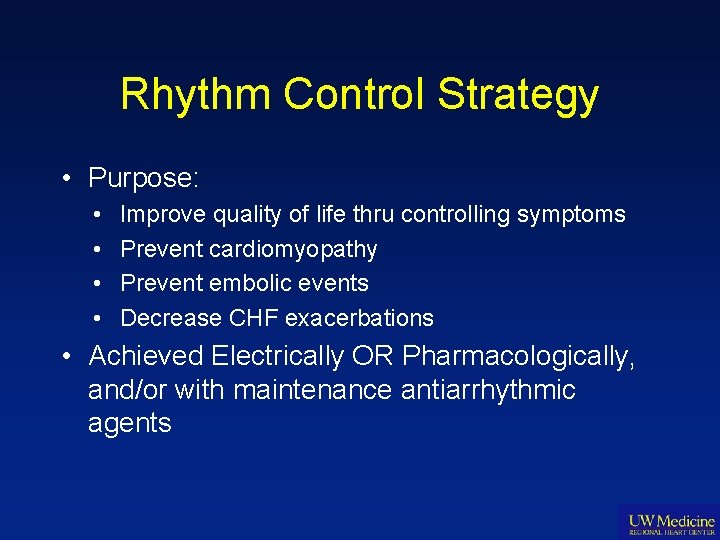
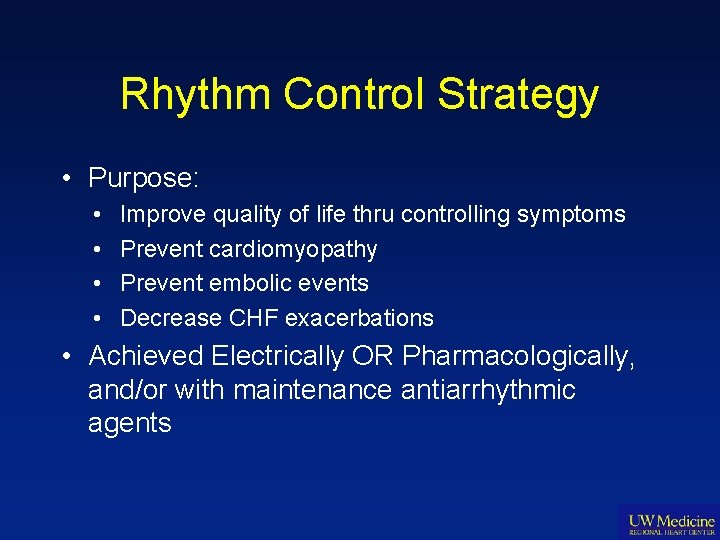
Rhythm Control Strategy • Purpose: • • Improve quality of life thru controlling symptoms Prevent cardiomyopathy Prevent embolic events Decrease CHF exacerbations • Achieved Electrically OR Pharmacologically, and/or with maintenance antiarrhythmic agents
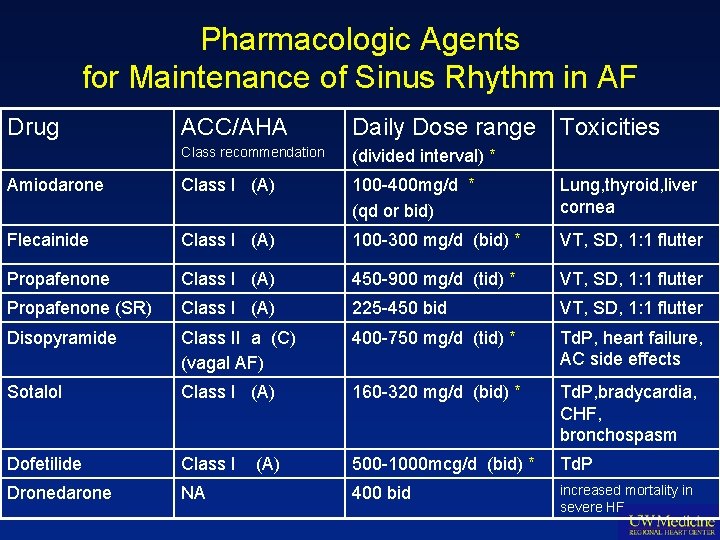
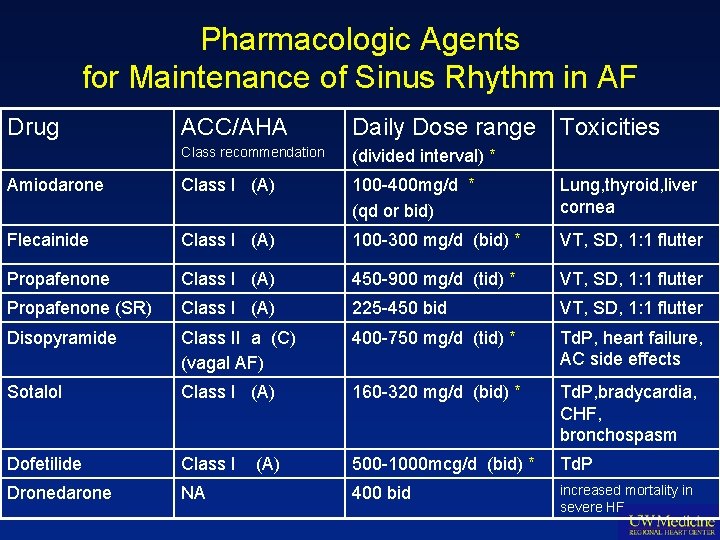
Pharmacologic Agents for Maintenance of Sinus Rhythm in AF Drug ACC/AHA Daily Dose range Class recommendation (divided interval) * Amiodarone Class I (A) 100 -400 mg/d * (qd or bid) Lung, thyroid, liver cornea Flecainide Class I (A) 100 -300 mg/d (bid) * VT, SD, 1: 1 flutter Propafenone Class I (A) 450 -900 mg/d (tid) * VT, SD, 1: 1 flutter Propafenone (SR) Class I (A) 225 -450 bid VT, SD, 1: 1 flutter Disopyramide Class II a (C) (vagal AF) 400 -750 mg/d (tid) * Td. P, heart failure, AC side effects Sotalol Class I (A) 160 -320 mg/d (bid) * Td. P, bradycardia, CHF, bronchospasm Dofetilide Class I 500 -1000 mcg/d (bid) * Td. P Dronedarone NA 400 bid increased mortality in severe HF (A) Toxicities
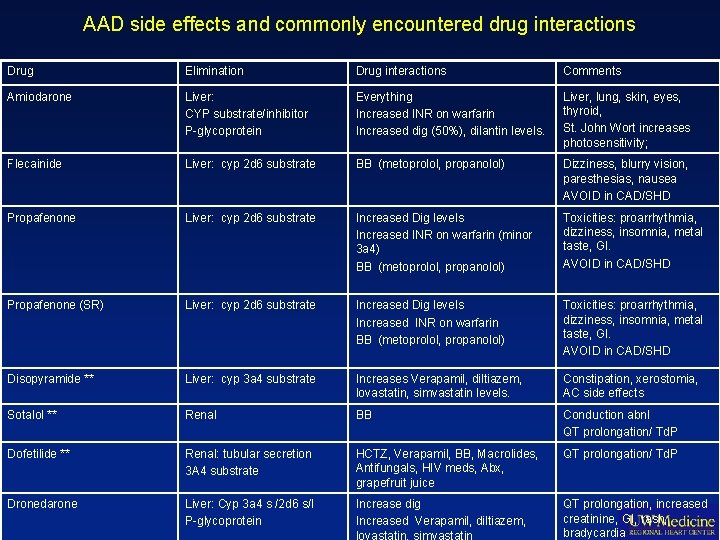
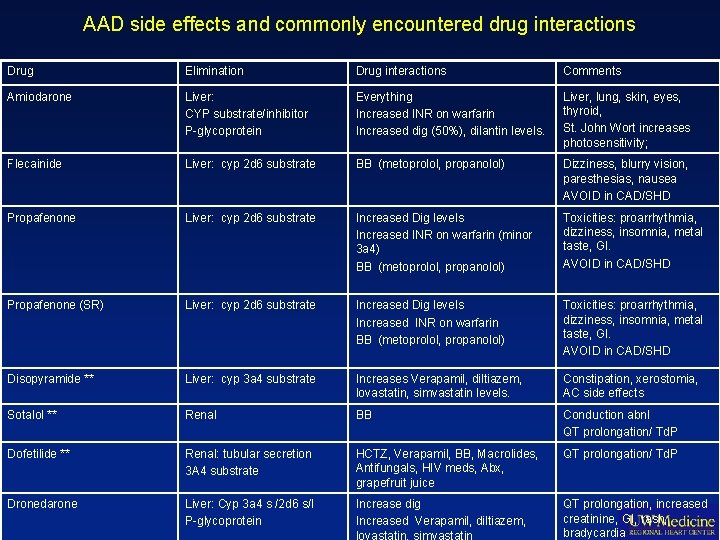
AAD side effects and commonly encountered drug interactions Drug Elimination Drug interactions Comments Amiodarone Liver: CYP substrate/inhibitor P-glycoprotein Everything Increased INR on warfarin Increased dig (50%), dilantin levels. Liver, lung, skin, eyes, thyroid, St. John Wort increases photosensitivity; Flecainide Liver: cyp 2 d 6 substrate BB (metoprolol, propanolol) Dizziness, blurry vision, paresthesias, nausea AVOID in CAD/SHD Propafenone Liver: cyp 2 d 6 substrate Increased Dig levels Increased INR on warfarin (minor 3 a 4) BB (metoprolol, propanolol) Toxicities: proarrhythmia, dizziness, insomnia, metal taste, GI. AVOID in CAD/SHD Propafenone (SR) Liver: cyp 2 d 6 substrate Increased Dig levels Increased INR on warfarin BB (metoprolol, propanolol) Toxicities: proarrhythmia, dizziness, insomnia, metal taste, GI. AVOID in CAD/SHD Disopyramide ** Liver: cyp 3 a 4 substrate Increases Verapamil, diltiazem, lovastatin, simvastatin levels. Constipation, xerostomia, AC side effects Sotalol ** Renal BB Conduction abnl QT prolongation/ Td. P Dofetilide ** Renal: tubular secretion 3 A 4 substrate HCTZ, Verapamil, BB, Macrolides, Antifungals, HIV meds, Abx, grapefruit juice QT prolongation/ Td. P Dronedarone Liver: Cyp 3 a 4 s /2 d 6 s/I P-glycoprotein Increase dig Increased Verapamil, diltiazem, lovastatin, simvastatin QT prolongation, increased creatinine, GI, rash, bradycardia
Options for Pharmacologic Cardioversion…
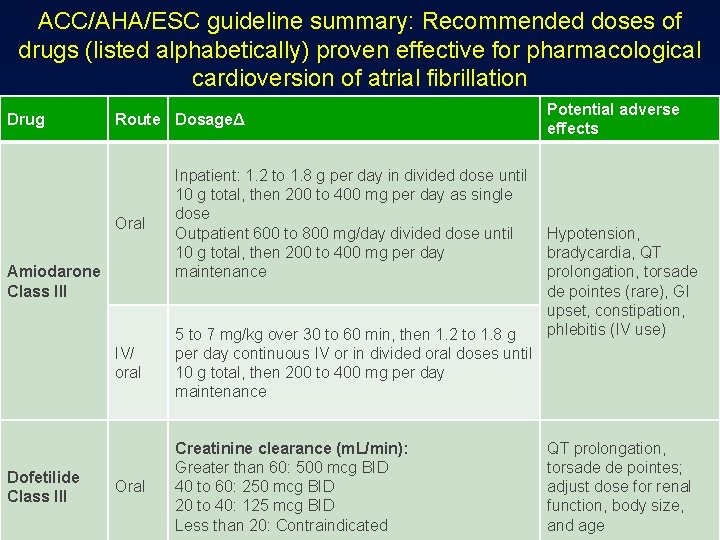
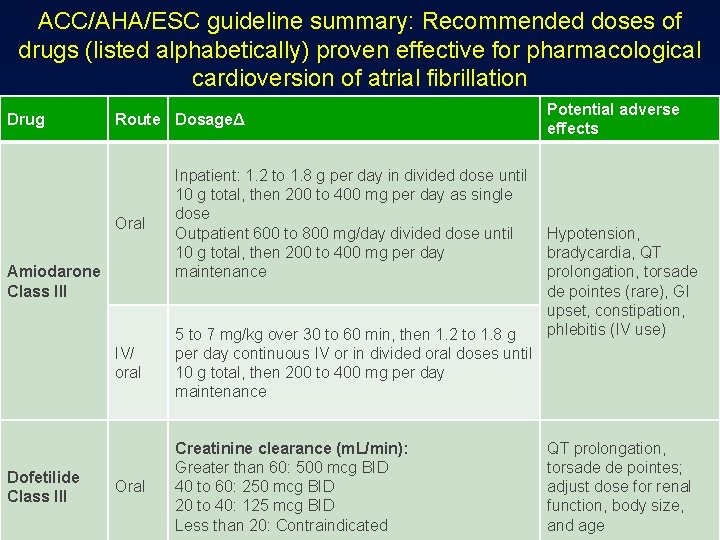
ACC/AHA/ESC guideline summary: Recommended doses of drugs (listed alphabetically) proven effective for pharmacological cardioversion of atrial fibrillation Drug Route DosageΔ Oral Inpatient: 1. 2 to 1. 8 g per day in divided dose until 10 g total, then 200 to 400 mg per day as single dose Outpatient 600 to 800 mg/day divided dose until 10 g total, then 200 to 400 mg per day maintenance IV/ oral 5 to 7 mg/kg over 30 to 60 min, then 1. 2 to 1. 8 g per day continuous IV or in divided oral doses until 10 g total, then 200 to 400 mg per day maintenance Oral Creatinine clearance (m. L/min): Greater than 60: 500 mcg BID 40 to 60: 250 mcg BID 20 to 40: 125 mcg BID Less than 20: Contraindicated Amiodarone Class III Dofetilide Class III Potential adverse effects Hypotension, bradycardia, QT prolongation, torsade de pointes (rare), GI upset, constipation, phlebitis (IV use) QT prolongation, torsade de pointes; adjust dose for renal function, body size, and age
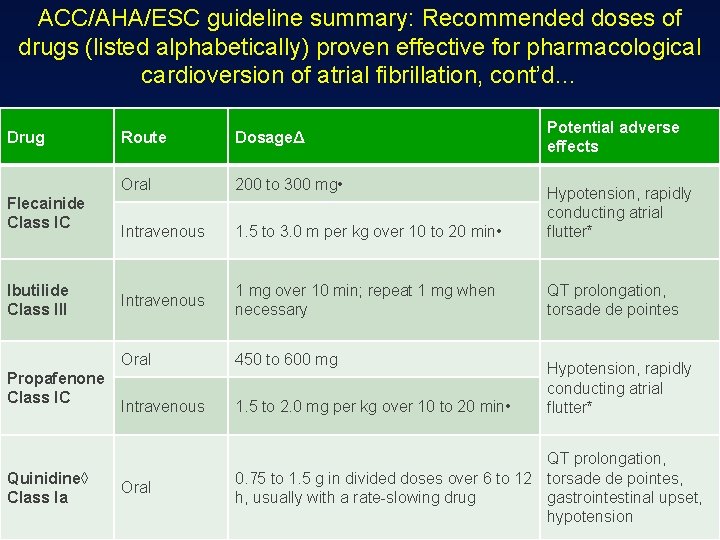
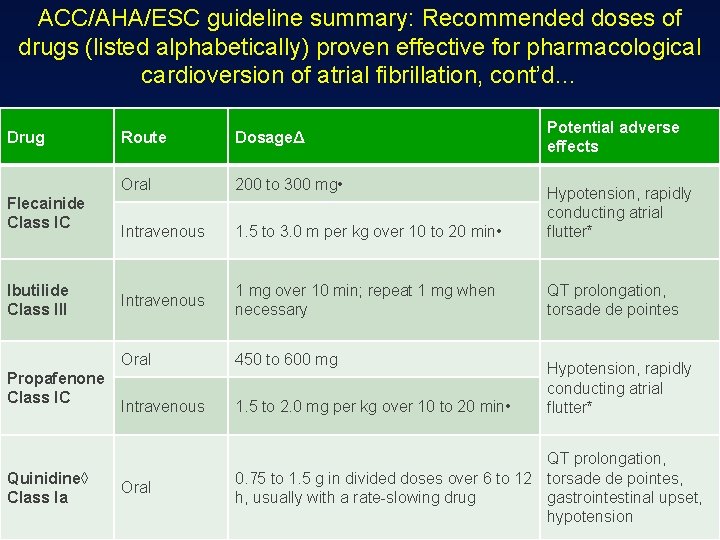
ACC/AHA/ESC guideline summary: Recommended doses of drugs (listed alphabetically) proven effective for pharmacological cardioversion of atrial fibrillation, cont’d… Drug Flecainide Class IC Ibutilide Class III Propafenone Class IC Quinidine◊ Class Ia Potential adverse effects Route DosageΔ Oral 200 to 300 mg • Intravenous 1. 5 to 3. 0 m per kg over 10 to 20 min • Hypotension, rapidly conducting atrial flutter* Intravenous 1 mg over 10 min; repeat 1 mg when necessary QT prolongation, torsade de pointes Oral 450 to 600 mg Intravenous 1. 5 to 2. 0 mg per kg over 10 to 20 min • Oral QT prolongation, 0. 75 to 1. 5 g in divided doses over 6 to 12 torsade de pointes, h, usually with a rate-slowing drug gastrointestinal upset, hypotension Hypotension, rapidly conducting atrial flutter*

Considerations for Antithrombotic Treatment Strategy…
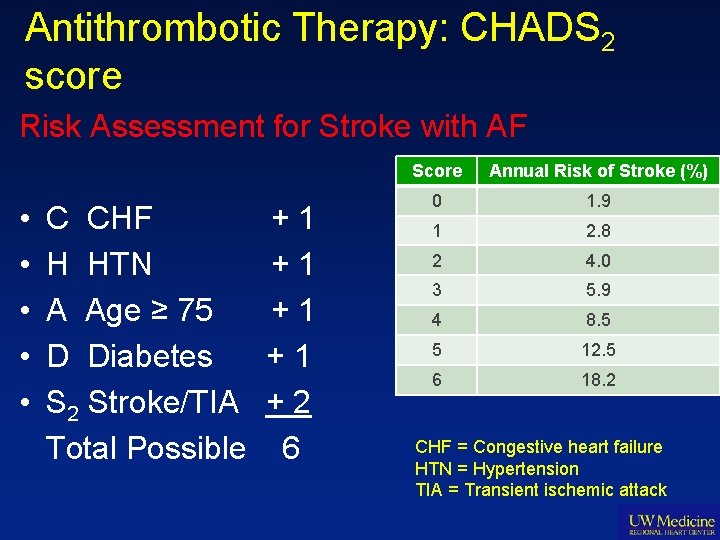
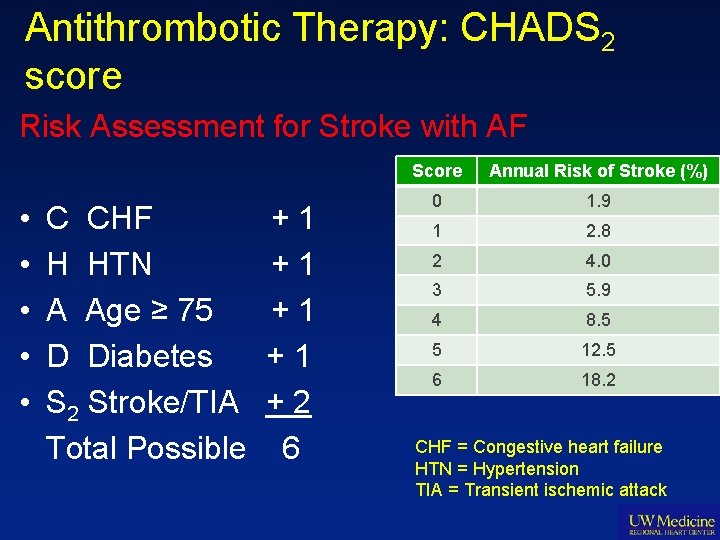
Antithrombotic Therapy: CHADS 2 score Risk Assessment for Stroke with AF • • • C CHF H HTN A Age ≥ 75 D Diabetes S 2 Stroke/TIA Total Possible +1 +1 +2 6 Score Annual Risk of Stroke (%) 0 1. 9 1 2. 8 2 4. 0 3 5. 9 4 8. 5 5 12. 5 6 18. 2 CHF = Congestive heart failure HTN = Hypertension TIA = Transient ischemic attack
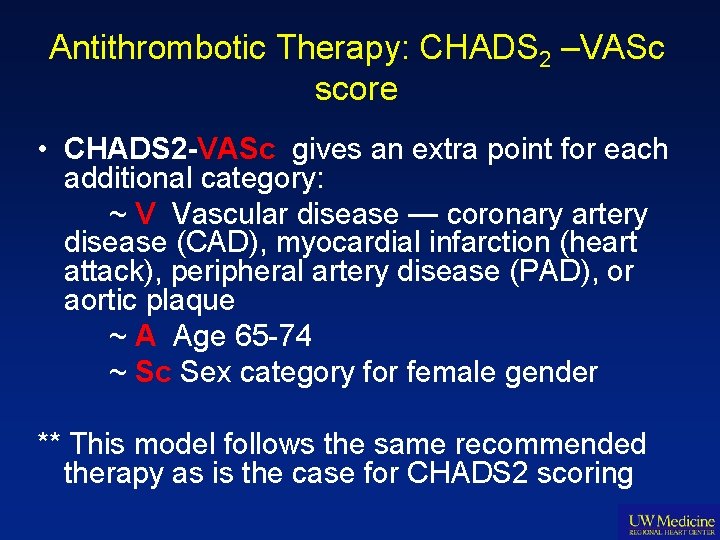
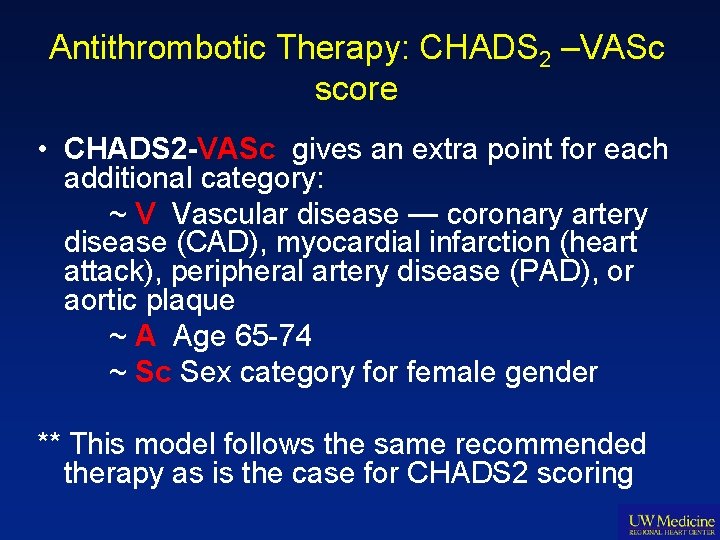
Antithrombotic Therapy: CHADS 2 –VASc score • CHADS 2 -VASc gives an extra point for each additional category: ~ V Vascular disease — coronary artery disease (CAD), myocardial infarction (heart attack), peripheral artery disease (PAD), or aortic plaque ~ A Age 65 -74 ~ Sc Sex category for female gender ** This model follows the same recommended therapy as is the case for CHADS 2 scoring
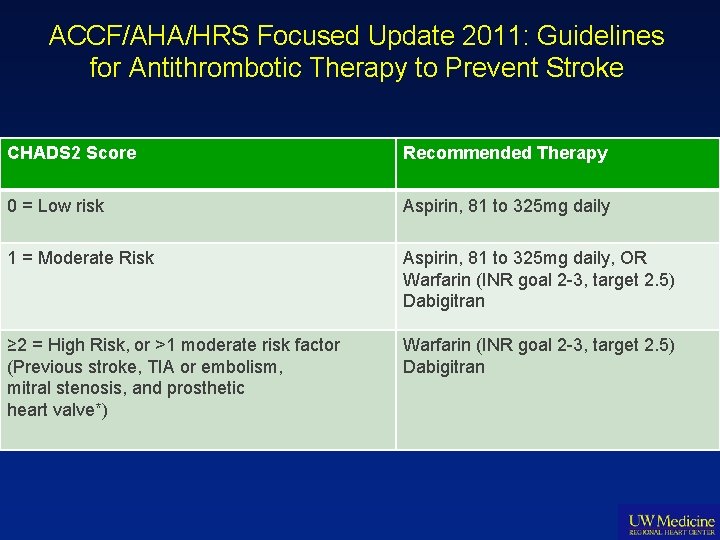
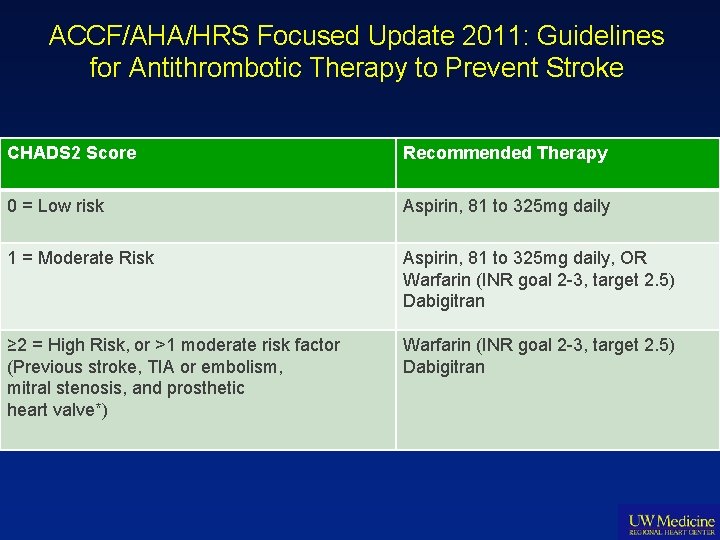
ACCF/AHA/HRS Focused Update 2011: Guidelines for Antithrombotic Therapy to Prevent Stroke CHADS 2 Score Recommended Therapy 0 = Low risk Aspirin, 81 to 325 mg daily 1 = Moderate Risk Aspirin, 81 to 325 mg daily, OR Warfarin (INR goal 2 -3, target 2. 5) Dabigitran ≥ 2 = High Risk, or >1 moderate risk factor (Previous stroke, TIA or embolism, mitral stenosis, and prosthetic heart valve*) Warfarin (INR goal 2 -3, target 2. 5) Dabigitran
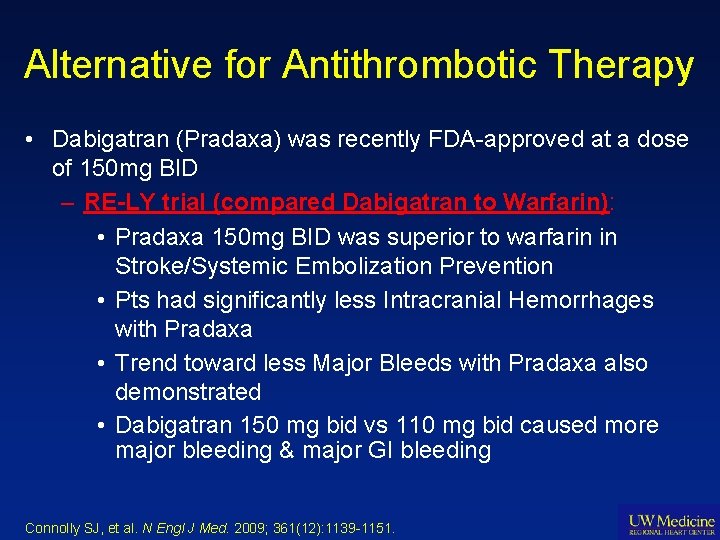
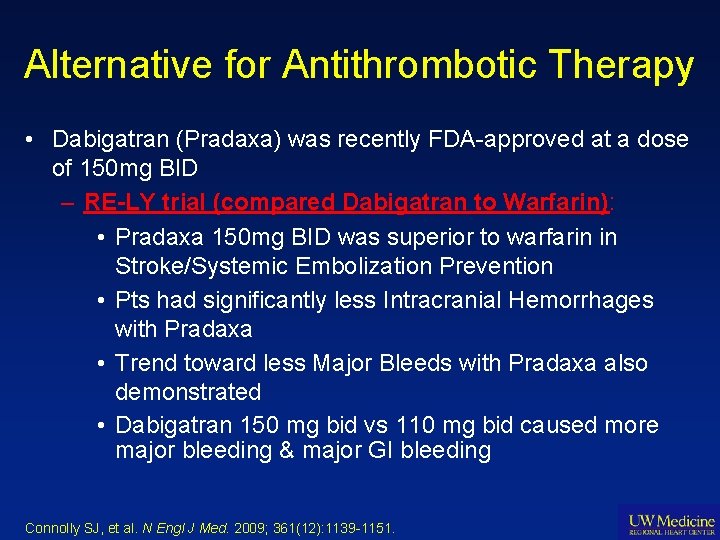
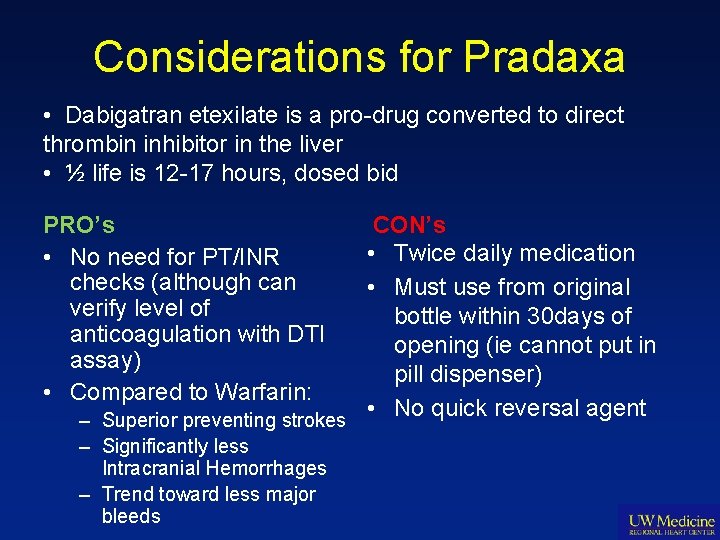
Alternative for Antithrombotic Therapy • Dabigatran (Pradaxa) was recently FDA-approved at a dose of 150 mg BID – RE-LY trial (compared Dabigatran to Warfarin): • Pradaxa 150 mg BID was superior to warfarin in Stroke/Systemic Embolization Prevention • Pts had significantly less Intracranial Hemorrhages with Pradaxa • Trend toward less Major Bleeds with Pradaxa also demonstrated • Dabigatran 150 mg bid vs 110 mg bid caused more major bleeding & major GI bleeding Connolly SJ, et al. N Engl J Med. 2009; 361(12): 1139 -1151.
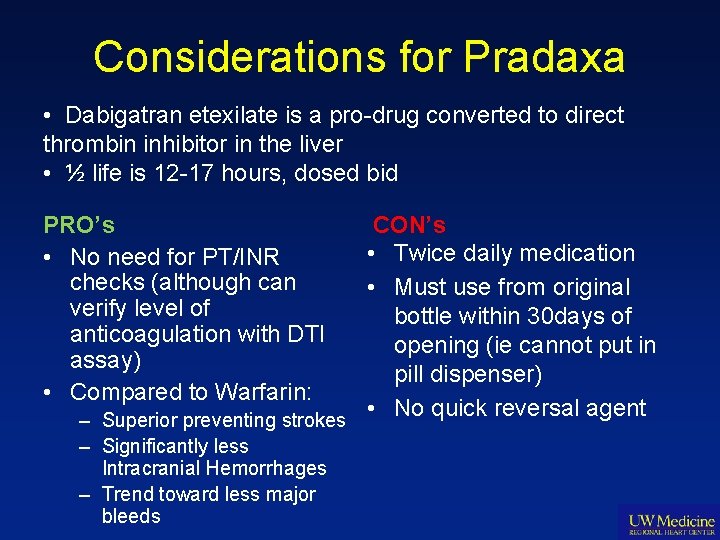
Considerations for Pradaxa • Dabigatran etexilate is a pro-drug converted to direct thrombin inhibitor in the liver • ½ life is 12 -17 hours, dosed bid PRO’s • No need for PT/INR checks (although can verify level of anticoagulation with DTI assay) • Compared to Warfarin: CON’s • Twice daily medication • Must use from original bottle within 30 days of opening (ie cannot put in pill dispenser) • No quick reversal agent – Superior preventing strokes – Significantly less Intracranial Hemorrhages – Trend toward less major bleeds
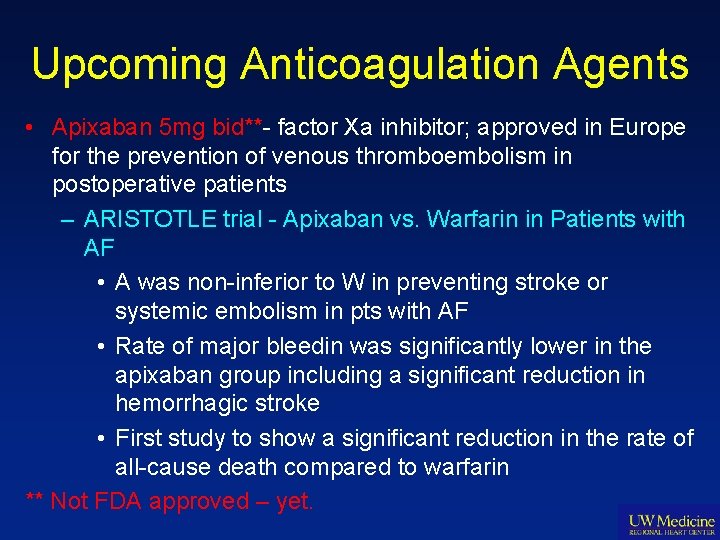
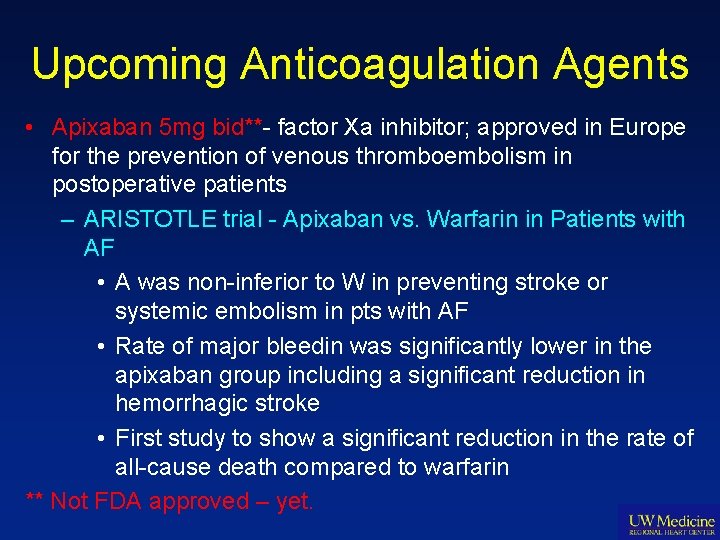
Upcoming Anticoagulation Agents • Apixaban 5 mg bid**- factor Xa inhibitor; approved in Europe for the prevention of venous thromboembolism in postoperative patients – ARISTOTLE trial - Apixaban vs. Warfarin in Patients with AF • A was non-inferior to W in preventing stroke or systemic embolism in pts with AF • Rate of major bleedin was significantly lower in the apixaban group including a significant reduction in hemorrhagic stroke • First study to show a significant reduction in the rate of all-cause death compared to warfarin ** Not FDA approved – yet.
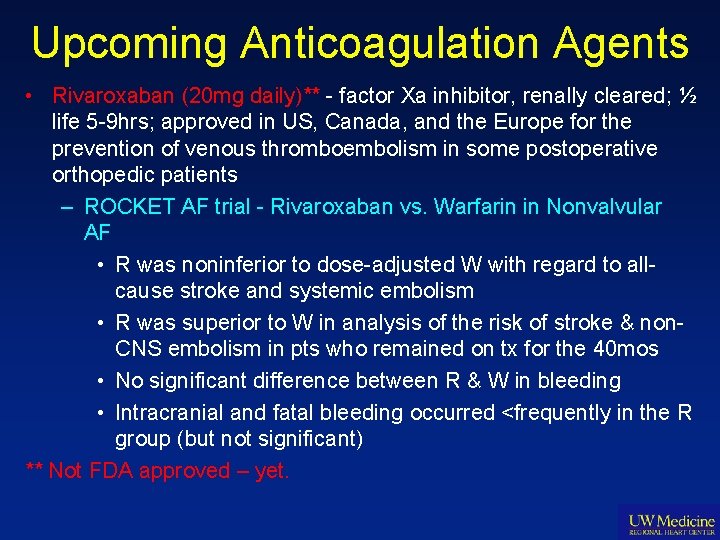
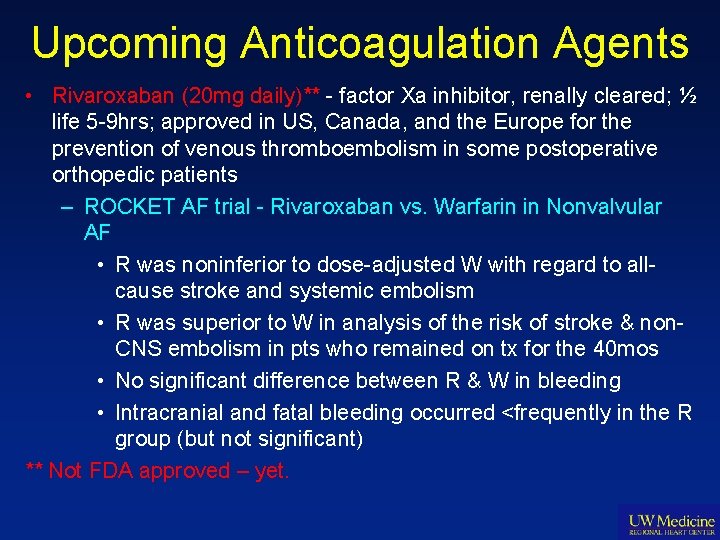
Upcoming Anticoagulation Agents • Rivaroxaban (20 mg daily)** - factor Xa inhibitor, renally cleared; ½ life 5 -9 hrs; approved in US, Canada, and the Europe for the prevention of venous thromboembolism in some postoperative orthopedic patients – ROCKET AF trial - Rivaroxaban vs. Warfarin in Nonvalvular AF • R was noninferior to dose-adjusted W with regard to allcause stroke and systemic embolism • R was superior to W in analysis of the risk of stroke & non. CNS embolism in pts who remained on tx for the 40 mos • No significant difference between R & W in bleeding • Intracranial and fatal bleeding occurred <frequently in the R group (but not significant) ** Not FDA approved – yet.
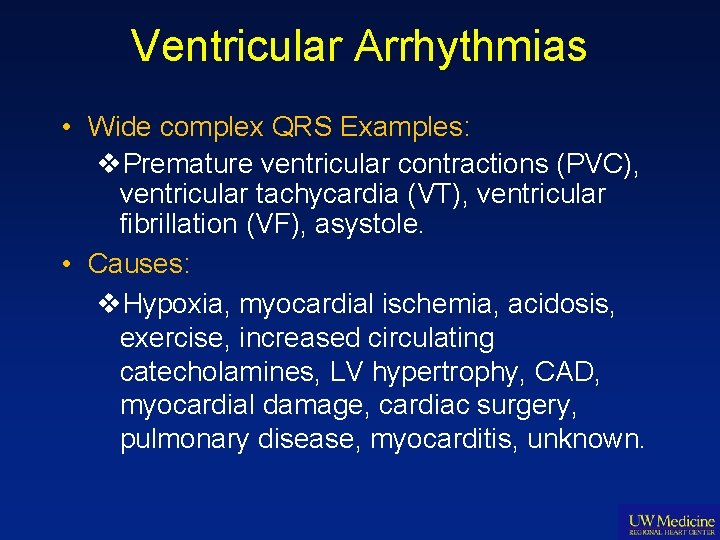
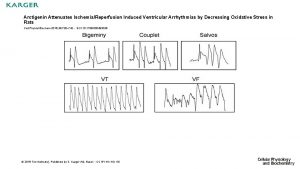
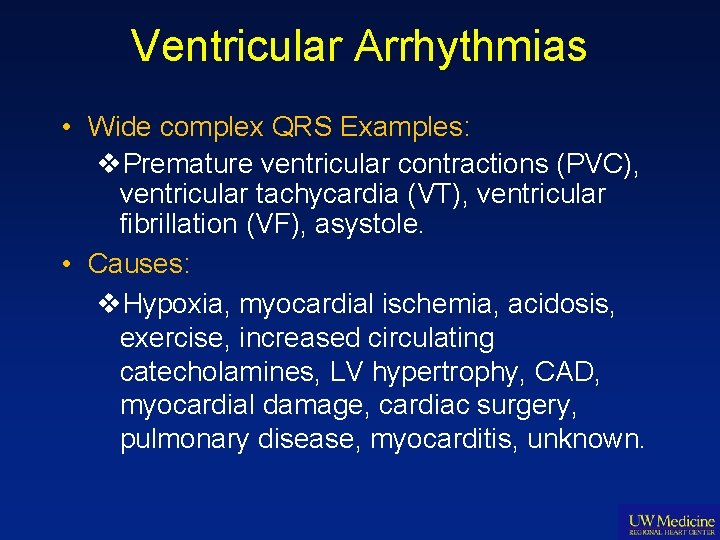
Ventricular Arrhythmias • Wide complex QRS Examples: v. Premature ventricular contractions (PVC), ventricular tachycardia (VT), ventricular fibrillation (VF), asystole. • Causes: v. Hypoxia, myocardial ischemia, acidosis, exercise, increased circulating catecholamines, LV hypertrophy, CAD, myocardial damage, cardiac surgery, pulmonary disease, myocarditis, unknown.
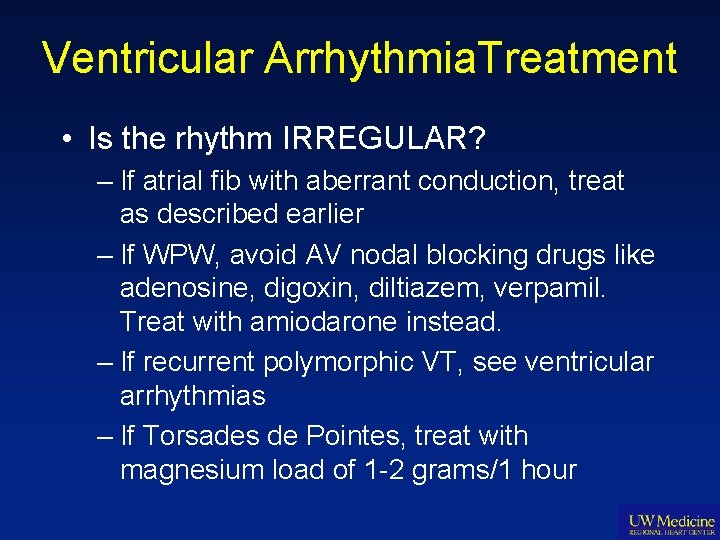
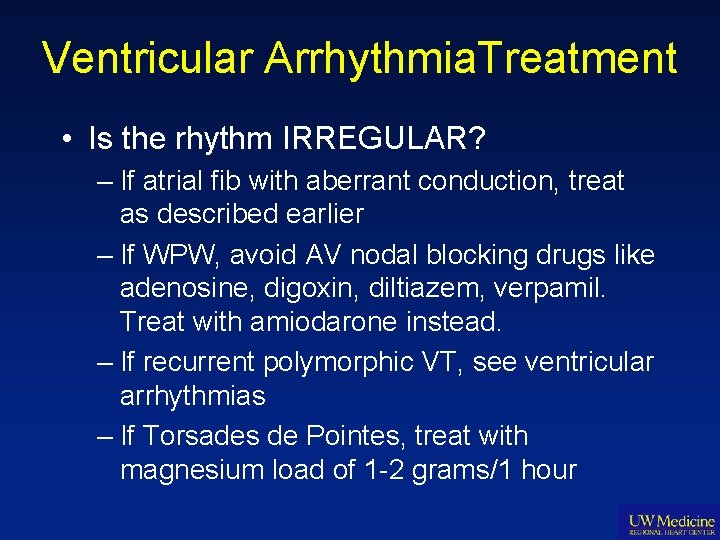
Ventricular Arrhythmia. Treatment • Is the rhythm IRREGULAR? – If atrial fib with aberrant conduction, treat as described earlier – If WPW, avoid AV nodal blocking drugs like adenosine, digoxin, diltiazem, verpamil. Treat with amiodarone instead. – If recurrent polymorphic VT, see ventricular arrhythmias – If Torsades de Pointes, treat with magnesium load of 1 -2 grams/1 hour
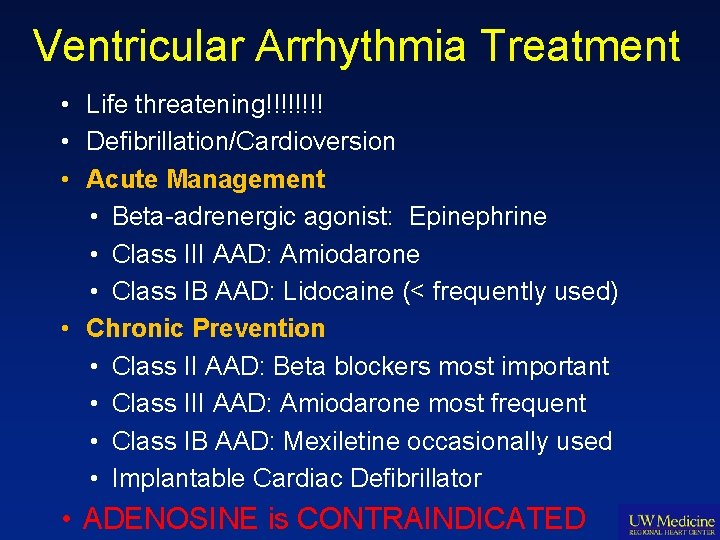
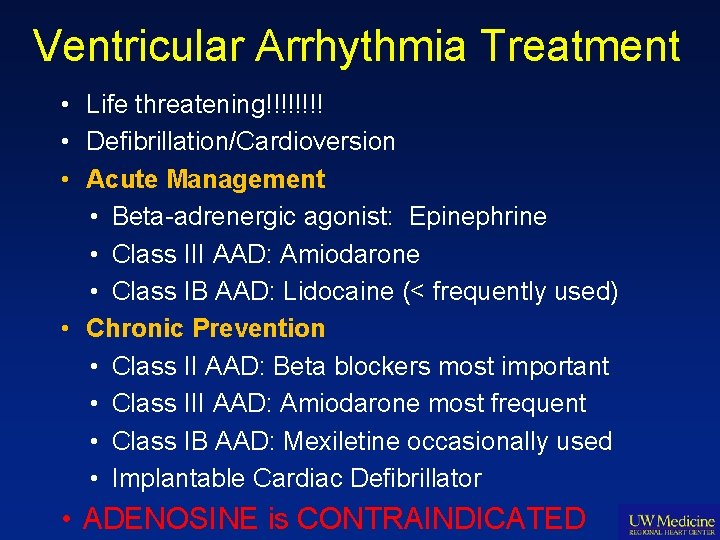
Ventricular Arrhythmia Treatment • Life threatening!!!! • Defibrillation/Cardioversion • Acute Management • Beta-adrenergic agonist: Epinephrine • Class III AAD: Amiodarone • Class IB AAD: Lidocaine (< frequently used) • Chronic Prevention • Class II AAD: Beta blockers most important • Class III AAD: Amiodarone most frequent • Class IB AAD: Mexiletine occasionally used • Implantable Cardiac Defibrillator • ADENOSINE is CONTRAINDICATED
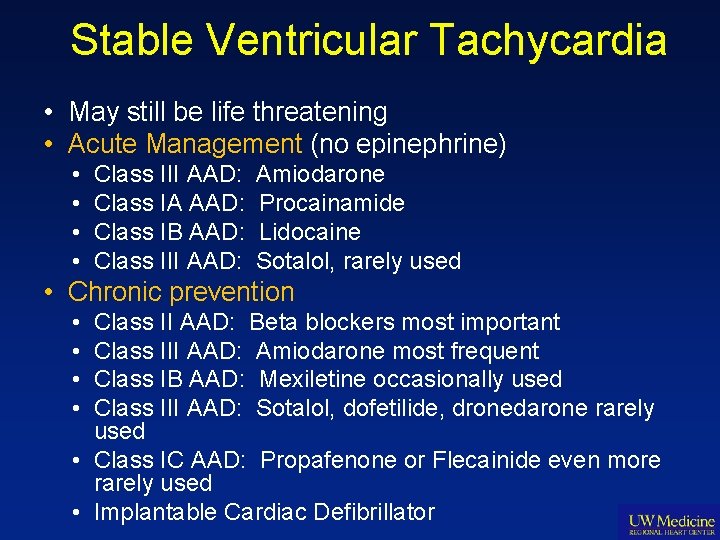
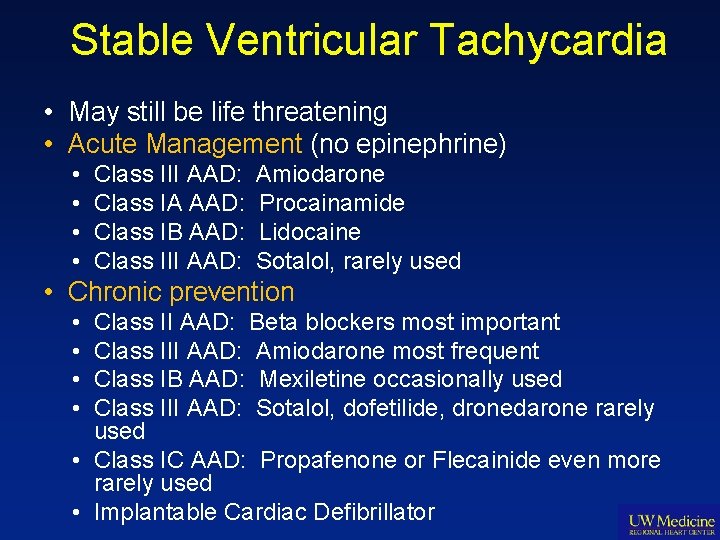
Stable Ventricular Tachycardia • May still be life threatening • Acute Management (no epinephrine) • • Class III AAD: Class IA AAD: Class IB AAD: Class III AAD: Amiodarone Procainamide Lidocaine Sotalol, rarely used • Chronic prevention • • Class II AAD: Beta blockers most important Class III AAD: Amiodarone most frequent Class IB AAD: Mexiletine occasionally used Class III AAD: Sotalol, dofetilide, dronedarone rarely used • Class IC AAD: Propafenone or Flecainide even more rarely used • Implantable Cardiac Defibrillator
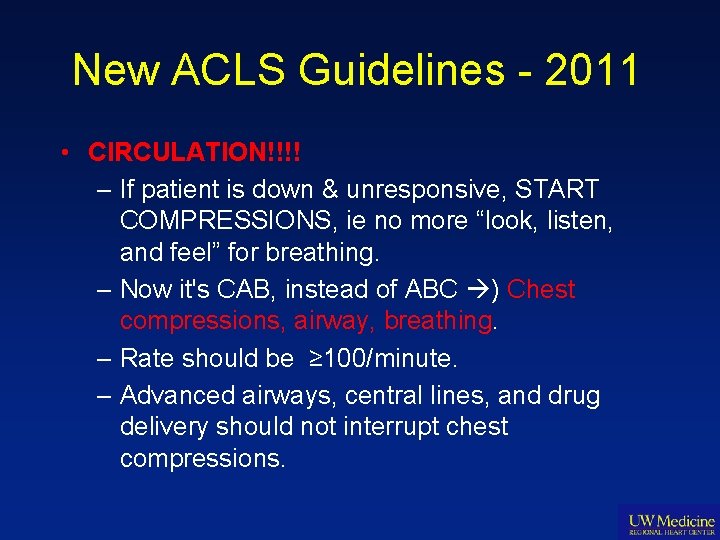
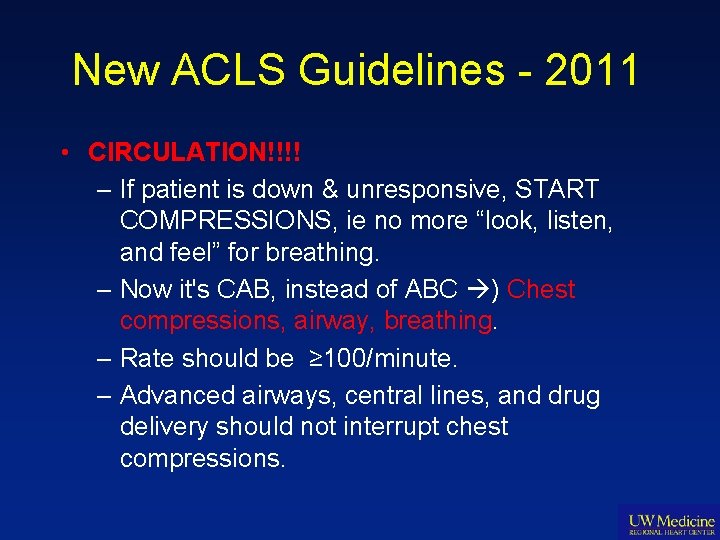
New ACLS Guidelines - 2011 • CIRCULATION!!!! – If patient is down & unresponsive, START COMPRESSIONS, ie no more “look, listen, and feel” for breathing. – Now it's CAB, instead of ABC ) Chest compressions, airway, breathing. – Rate should be ≥ 100/minute. – Advanced airways, central lines, and drug delivery should not interrupt chest compressions.
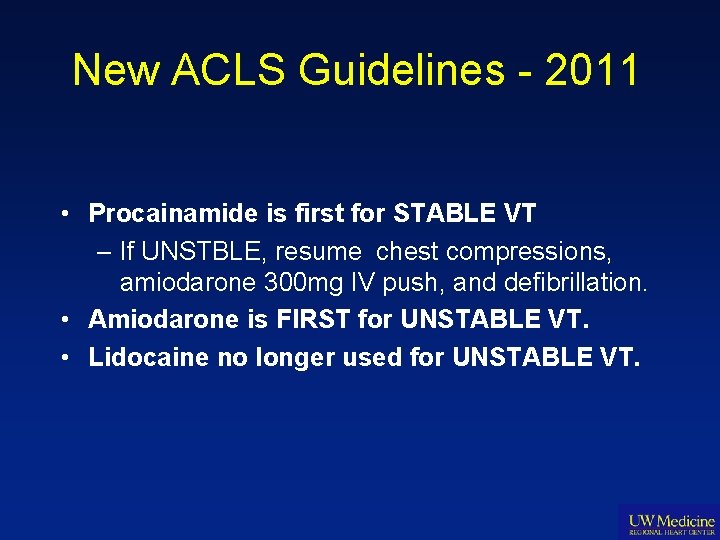
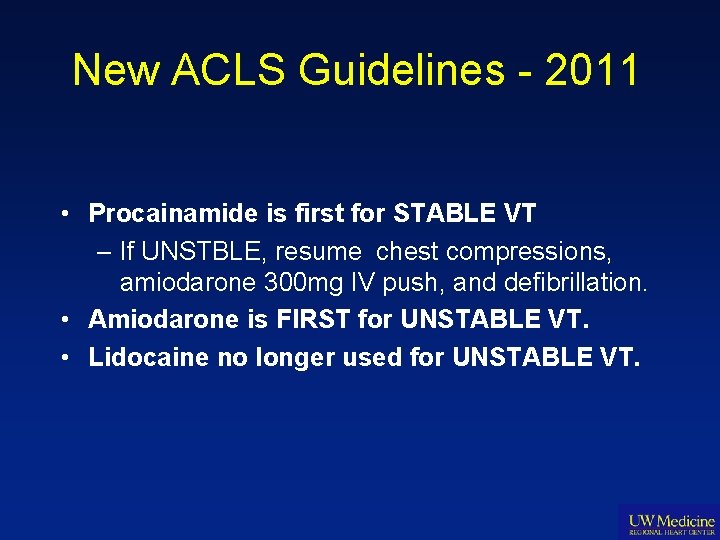
New ACLS Guidelines - 2011 • Procainamide is first for STABLE VT – If UNSTBLE, resume chest compressions, amiodarone 300 mg IV push, and defibrillation. • Amiodarone is FIRST for UNSTABLE VT. • Lidocaine no longer used for UNSTABLE VT.
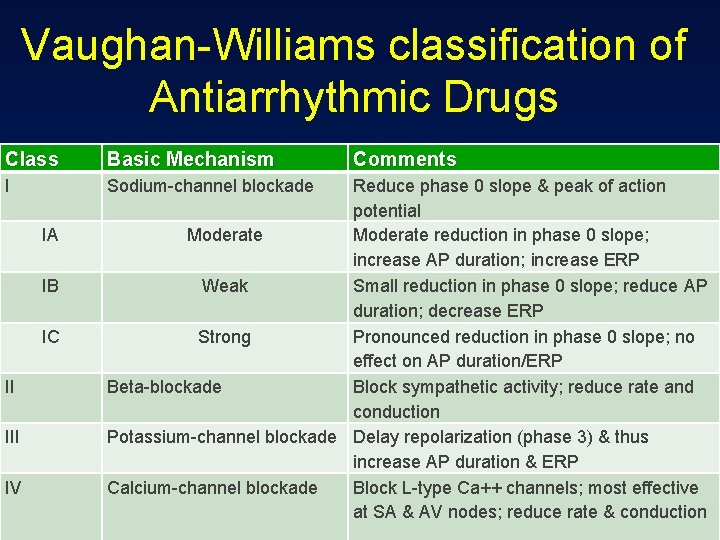
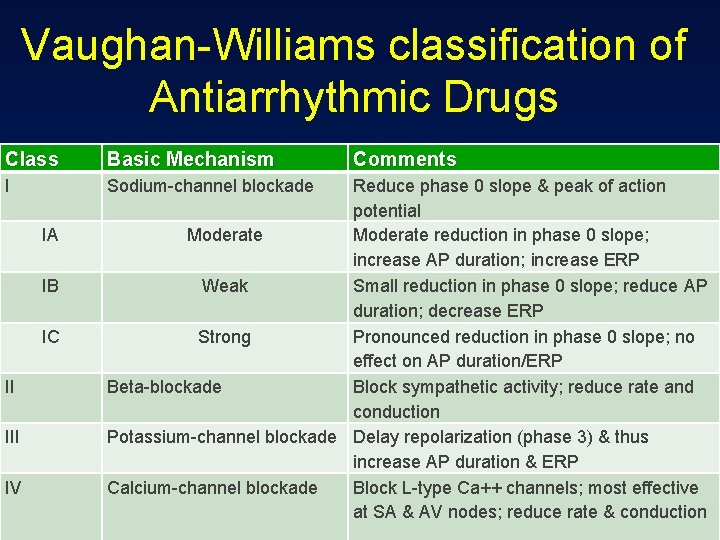
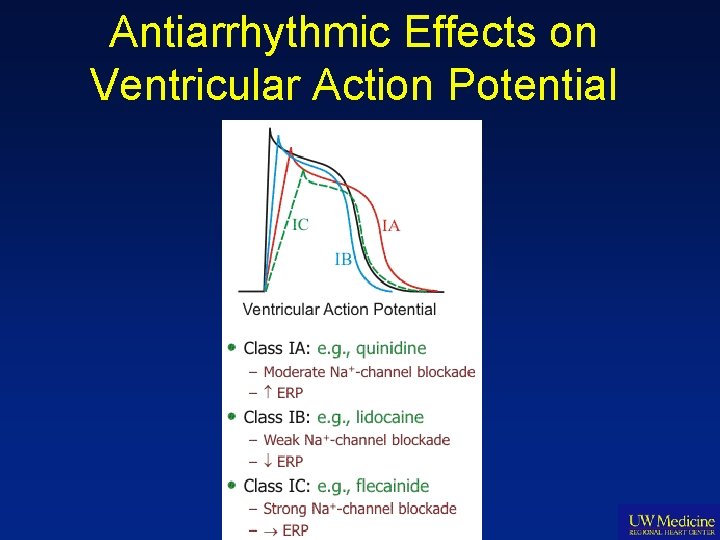
Vaughan-Williams classification of Antiarrhythmic Drugs Class Basic Mechanism I Sodium-channel blockade IA IB IC II IV Comments Reduce phase 0 slope & peak of action potential Moderate reduction in phase 0 slope; increase AP duration; increase ERP Weak Small reduction in phase 0 slope; reduce AP duration; decrease ERP Strong Pronounced reduction in phase 0 slope; no effect on AP duration/ERP Beta-blockade Block sympathetic activity; reduce rate and conduction Potassium-channel blockade Delay repolarization (phase 3) & thus increase AP duration & ERP Calcium-channel blockade Block L-type Ca++ channels; most effective at SA & AV nodes; reduce rate & conduction
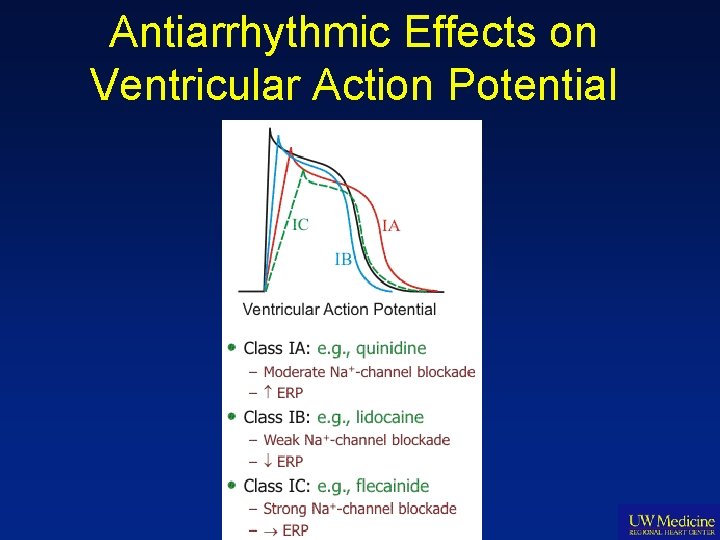
Antiarrhythmic Effects on Ventricular Action Potential
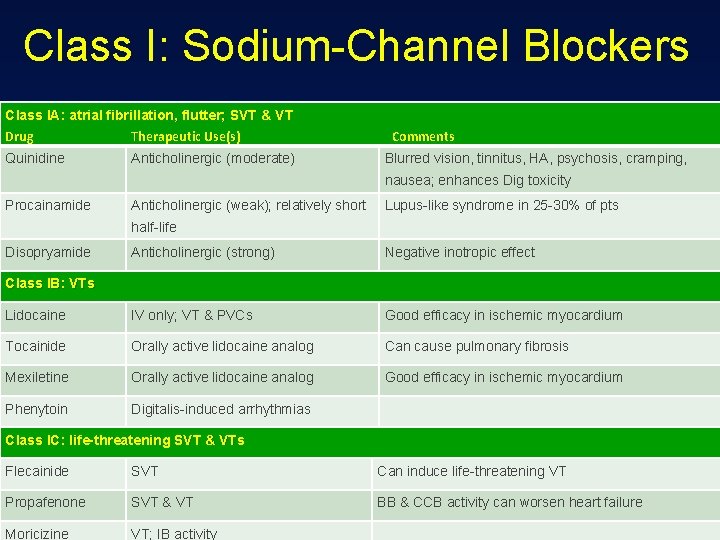
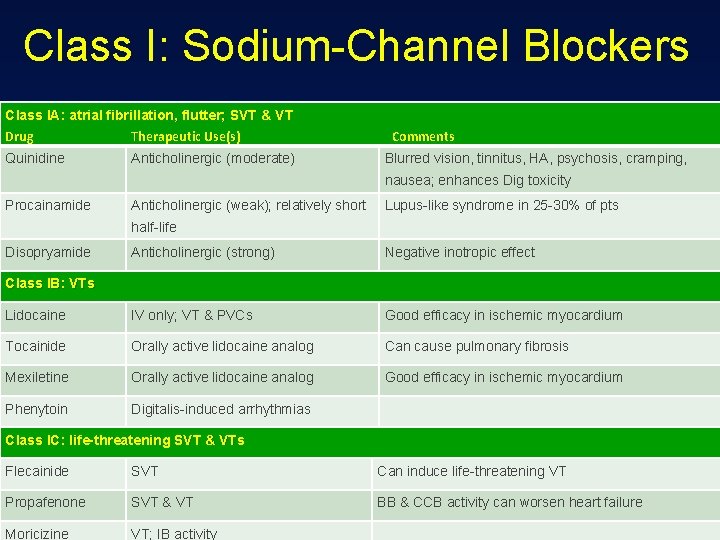
Class I: Sodium-Channel Blockers Class IA: atrial fibrillation, flutter; SVT & VT Drug Therapeutic Use(s) Quinidine Anticholinergic (moderate) Comments Blurred vision, tinnitus, HA, psychosis, cramping, nausea; enhances Dig toxicity Procainamide Anticholinergic (weak); relatively short Lupus-like syndrome in 25 -30% of pts half-life Disopryamide Anticholinergic (strong) Negative inotropic effect Lidocaine IV only; VT & PVCs Good efficacy in ischemic myocardium Tocainide Orally active lidocaine analog Can cause pulmonary fibrosis Mexiletine Orally active lidocaine analog Good efficacy in ischemic myocardium Phenytoin Digitalis-induced arrhythmias Class IB: VTs Class IC: life-threatening SVT & VTs Flecainide SVT Can induce life-threatening VT Propafenone SVT & VT BB & CCB activity can worsen heart failure Moricizine VT; IB activity
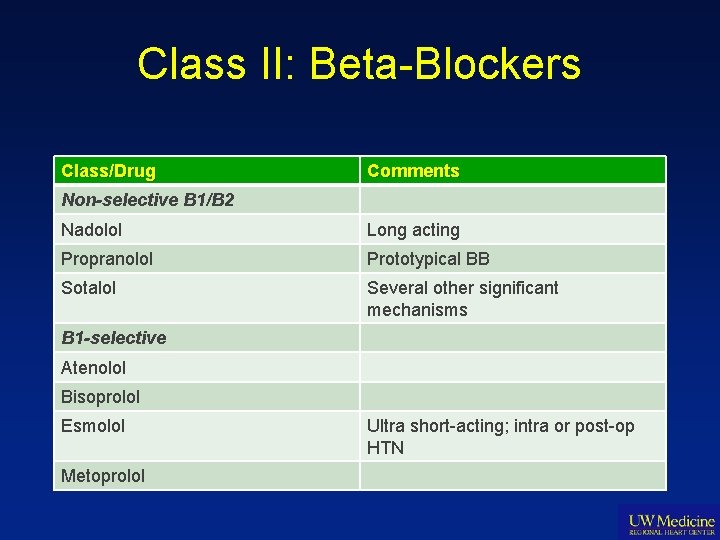
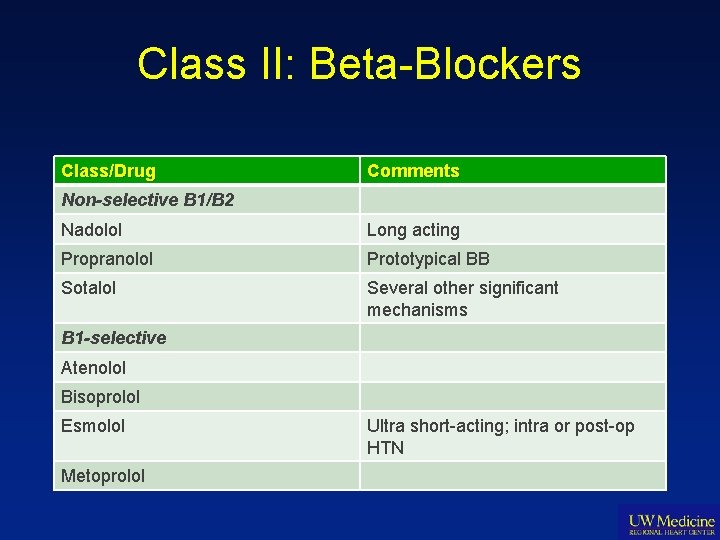
Class II: Beta-Blockers Class/Drug Comments Non-selective B 1/B 2 Nadolol Long acting Propranolol Prototypical BB Sotalol Several other significant mechanisms B 1 -selective Atenolol Bisoprolol Esmolol Metoprolol Ultra short-acting; intra or post-op HTN
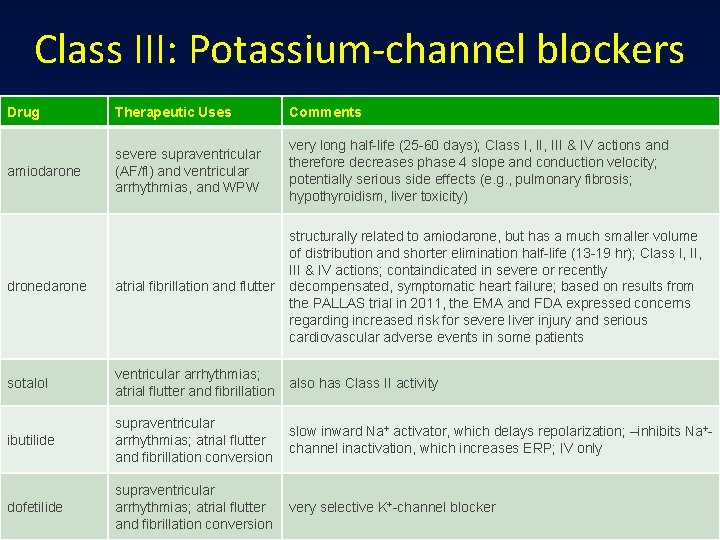
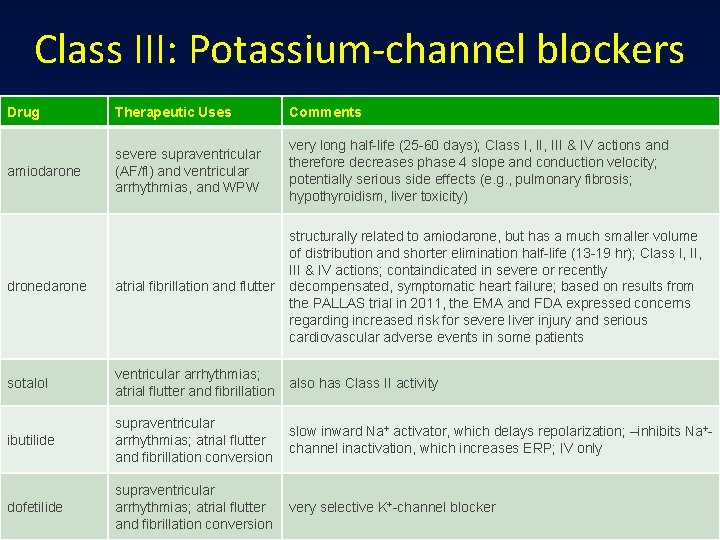
Class III: Potassium-channel blockers Drug Therapeutic Uses Comments amiodarone severe supraventricular (AF/fl) and ventricular arrhythmias, and WPW very long half-life (25 -60 days); Class I, III & IV actions and therefore decreases phase 4 slope and conduction velocity; potentially serious side effects (e. g. , pulmonary fibrosis; hypothyroidism, liver toxicity) dronedarone atrial fibrillation and flutter structurally related to amiodarone, but has a much smaller volume of distribution and shorter elimination half-life (13 -19 hr); Class I, III & IV actions; containdicated in severe or recently decompensated, symptomatic heart failure; based on results from the PALLAS trial in 2011, the EMA and FDA expressed concerns regarding increased risk for severe liver injury and serious cardiovascular adverse events in some patients sotalol ventricular arrhythmias; atrial flutter and fibrillation also has Class II activity ibutilide supraventricular arrhythmias; atrial flutter and fibrillation conversion slow inward Na+ activator, which delays repolarization; –inhibits Na+channel inactivation, which increases ERP; IV only dofetilide supraventricular arrhythmias; atrial flutter and fibrillation conversion very selective K+-channel blocker
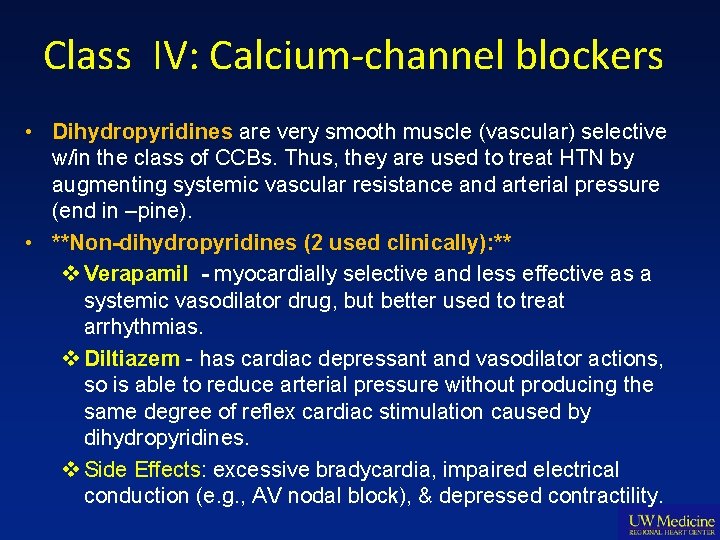
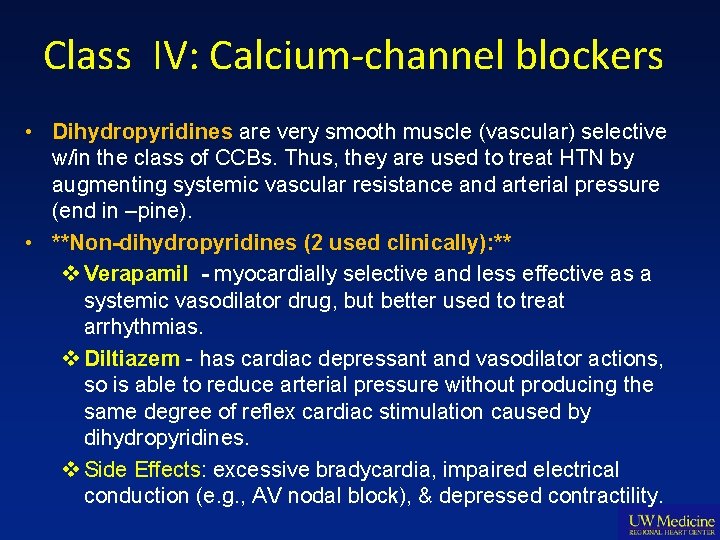
Class IV: Calcium-channel blockers • Dihydropyridines are very smooth muscle (vascular) selective w/in the class of CCBs. Thus, they are used to treat HTN by augmenting systemic vascular resistance and arterial pressure (end in –pine). • **Non-dihydropyridines (2 used clinically): ** v Verapamil - myocardially selective and less effective as a systemic vasodilator drug, but better used to treat arrhythmias. v Diltiazem - has cardiac depressant and vasodilator actions, so is able to reduce arterial pressure without producing the same degree of reflex cardiac stimulation caused by dihydropyridines. v Side Effects: excessive bradycardia, impaired electrical conduction (e. g. , AV nodal block), & depressed contractility.
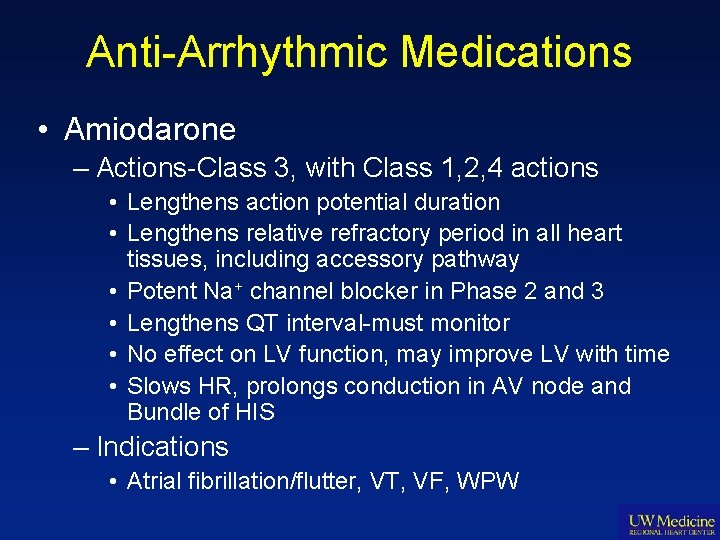
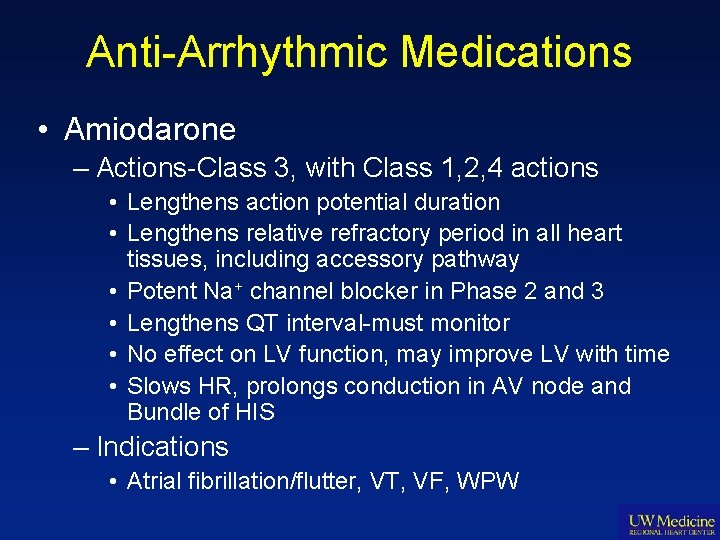
Anti-Arrhythmic Medications • Amiodarone – Actions-Class 3, with Class 1, 2, 4 actions • Lengthens action potential duration • Lengthens relative refractory period in all heart tissues, including accessory pathway • Potent Na+ channel blocker in Phase 2 and 3 • Lengthens QT interval-must monitor • No effect on LV function, may improve LV with time • Slows HR, prolongs conduction in AV node and Bundle of HIS – Indications • Atrial fibrillation/flutter, VT, VF, WPW
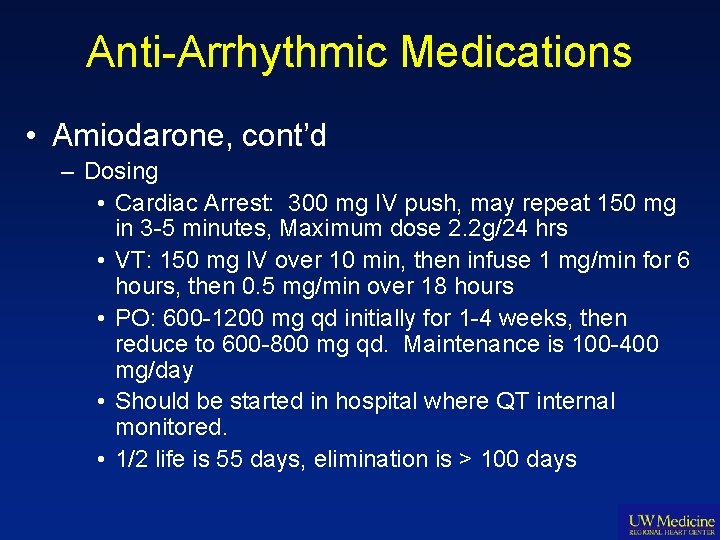
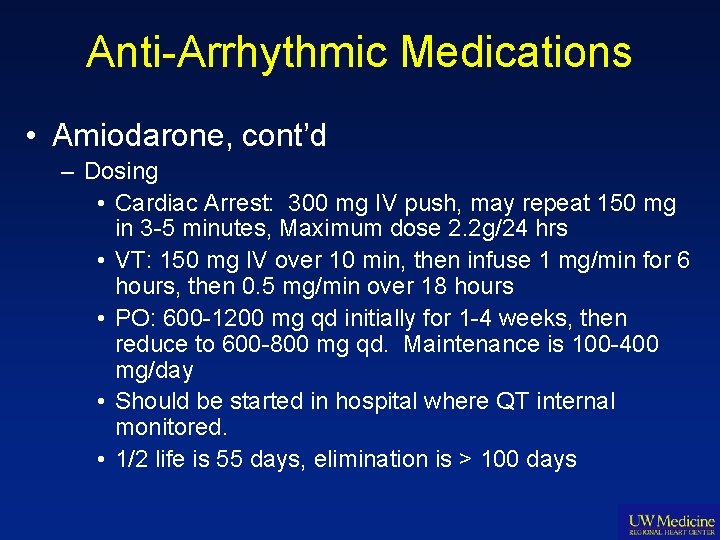
Anti-Arrhythmic Medications • Amiodarone, cont’d – Dosing • Cardiac Arrest: 300 mg IV push, may repeat 150 mg in 3 -5 minutes, Maximum dose 2. 2 g/24 hrs • VT: 150 mg IV over 10 min, then infuse 1 mg/min for 6 hours, then 0. 5 mg/min over 18 hours • PO: 600 -1200 mg qd initially for 1 -4 weeks, then reduce to 600 -800 mg qd. Maintenance is 100 -400 mg/day • Should be started in hospital where QT internal monitored. • 1/2 life is 55 days, elimination is > 100 days
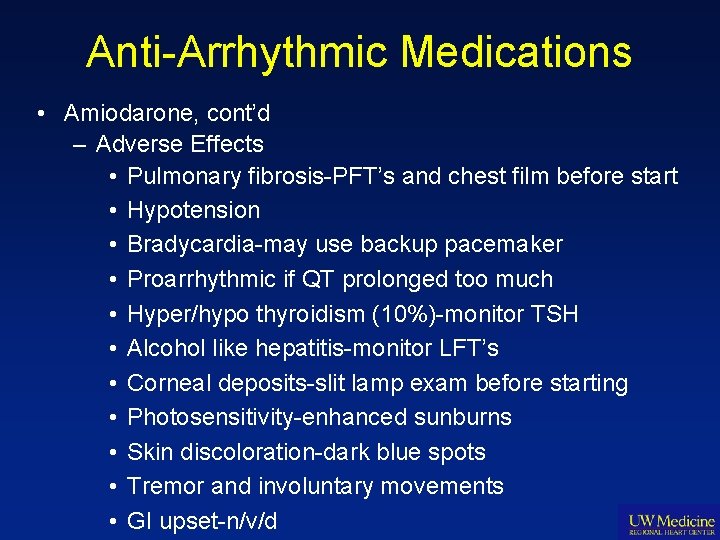
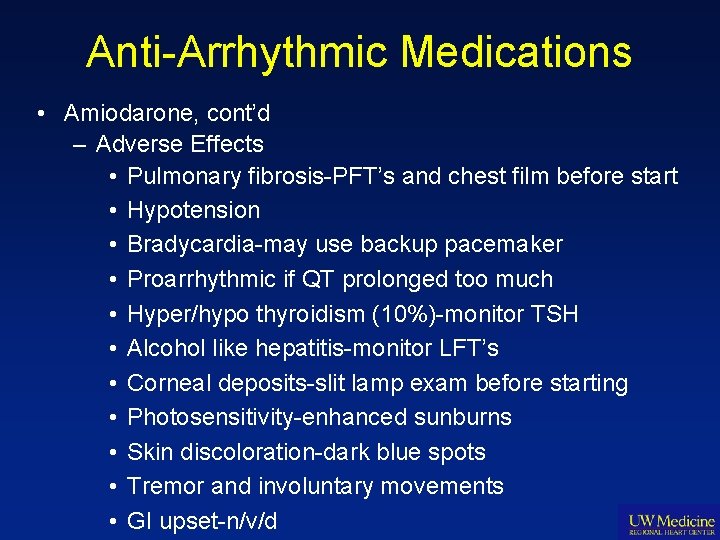
Anti-Arrhythmic Medications • Amiodarone, cont’d – Adverse Effects • Pulmonary fibrosis-PFT’s and chest film before start • Hypotension • Bradycardia-may use backup pacemaker • Proarrhythmic if QT prolonged too much • Hyper/hypo thyroidism (10%)-monitor TSH • Alcohol like hepatitis-monitor LFT’s • Corneal deposits-slit lamp exam before starting • Photosensitivity-enhanced sunburns • Skin discoloration-dark blue spots • Tremor and involuntary movements • GI upset-n/v/d
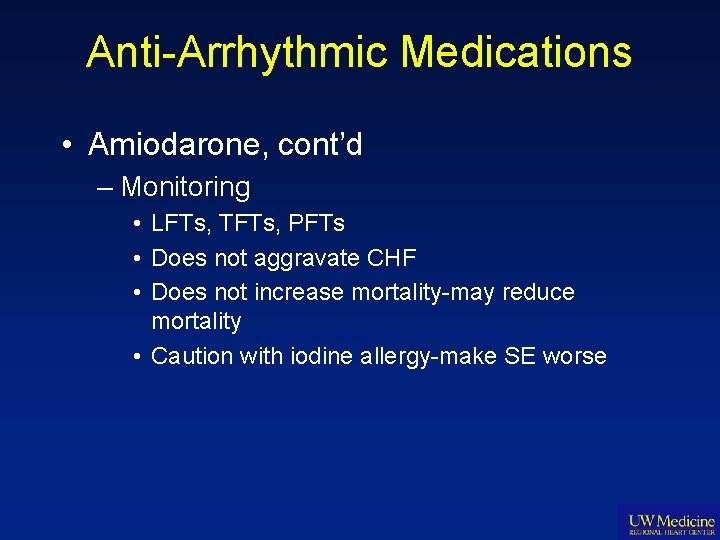
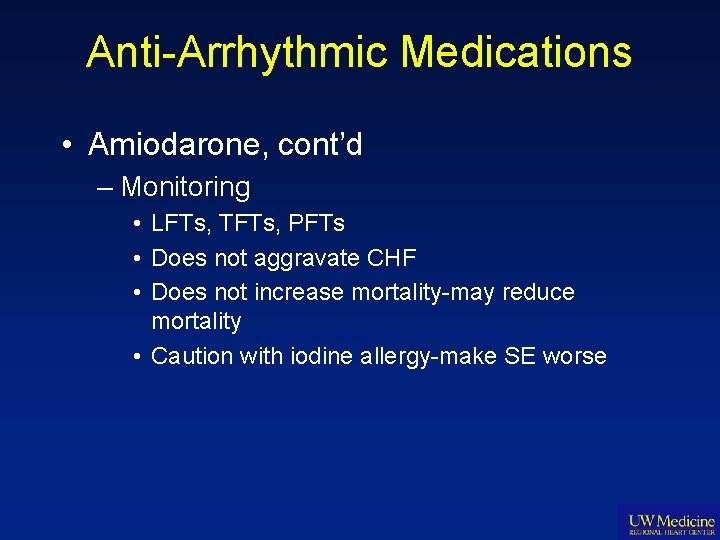
Anti-Arrhythmic Medications • Amiodarone, cont’d – Monitoring • LFTs, TFTs, PFTs • Does not aggravate CHF • Does not increase mortality-may reduce mortality • Caution with iodine allergy-make SE worse
Anti-Arrhythmic Medications • Dronedarone – Non-iodized derivative of amiodarone developed to avoid major SE seen with amiodarone – FDA approved to maintain NSR in AFib in 2009 – Oral form available only in the US
Anti-Arrhythmic Medications • Dronedarone – Action: Class 3, with Class 1, 2 4 properties • Inhibits potassium currents, sodium currents as well as Ca currents • Anti-adrenergic properties similar to beta blockers – Indications: FDA approved for maintaining NSR after cardioversion from a fib • More effective than amiodarone in preventing reperfusion arrhythmias in ischemia – Dosing: 400 mg bid orally**, no other forms available in US-half life 48 hours, steady state in 57 days • Tested at 1200 qd and 1600 qd but these doses associated with more SE
Anti-Arrhythmic Medications • Dronedarone – Adverse Effects • Torsades de pointes reported in dogs only, not in humans • No thyroid, ocular, or pulmonary toxicity reported in humans • 2 case reports/400, 000 prescriptions filled to date of fulminant liver failure in elderly females liver txp • Excessive deaths in those with recent HF exacerbation and reduced LVH-black box warning • More long term testing needed to determine safety • No data for use in ventricular arrhythmias • Expensive $267/month or 60 tabs
Anti-Arrhythmic Medications • Beta Blockers (Atenolol, Metoprolol, Esmolol) – Actions-Class 2 • Depresses Phase 4 depolarization • Blocks AV node conduction and prevents arrhythmias mediated through SNS • Increases VF threshold • Reduces HR, BP, myocardial contractility, myocardial O 2 consumption, cardiac mortality in setting of acute MI
Anti-Arrhythmic Medications • Beta Blockers, cont’d – Indications • Atrial fibrillation/flutter, VT, VF • Reduces incidence of VF in acute MI • Prevents sudden cardiac arrest in acute MI – Dosing • Atenolol and Metoprolol: 5 mg IV every 5 min, repeat x 3 • PO: 12. 5 -50 mg po qd and metoprolol 50 -100 mg bid • 1/2 life is 6 -9 hrs for atenolol and 3 -4 hrs metoprolol 59
Anti-Arrhythmic Medications • Beta Blockers, cont’d – Adverse Effects • • Reduces HR, BP, sensitivity to hypoglycemia in DM Reduces EF in low LV function Sexual dysfunction Bronchospasm in asthmatics and COPD • Carvedilol: A 1, B 2 activity, ½ life 4 -8 hours, titrated dosing schedule. – Start 3. 125 mg x 1 week, 3. 125 mg bid week 2 -3, 6. 25 mg bid week 4 -5, 12. 5 mg bid week 6 -7, 25 mg week 8 -9, then 50 mg bid.
Anti-Arrhythmic Medications • Beta Blocker: Sotalol – Actions-Class 2 and 3 • Class 2 properties are non-selective beta blockade • Class 3 properties are increasing action potential duration, slows SA node cycle length, and increases AV node conduction time – Indications • Atrial fibrillation/flutter, VT, VF, SVT (not in US) • Maintains NSR in a fib • Suppresses inducible ventricular arrhythmias in EPS
Anti-Arrhythmic Medications • Sotalol cont’d • May precipitate Torsades in those with low K+ or Mg++, not used for chronic a fib because other BB work just as well • Similar to amiodarone with ventricular arrhythmias • Used after cardioversion from a fib • Used as alternative to amiodarone in setting of new or recent ischemia – Dosing • PO: 40 -80 mg bid initial, then 240 -320 mg bid • IV Sotalol not available in US • 1/2 life 10 -20 hours
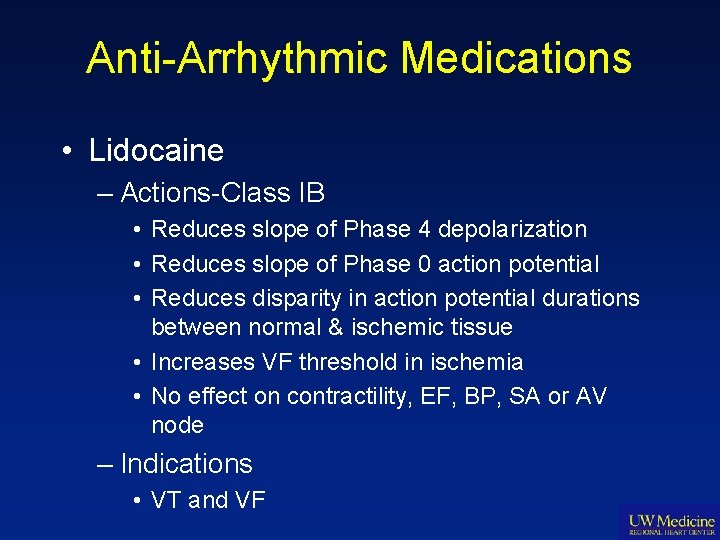
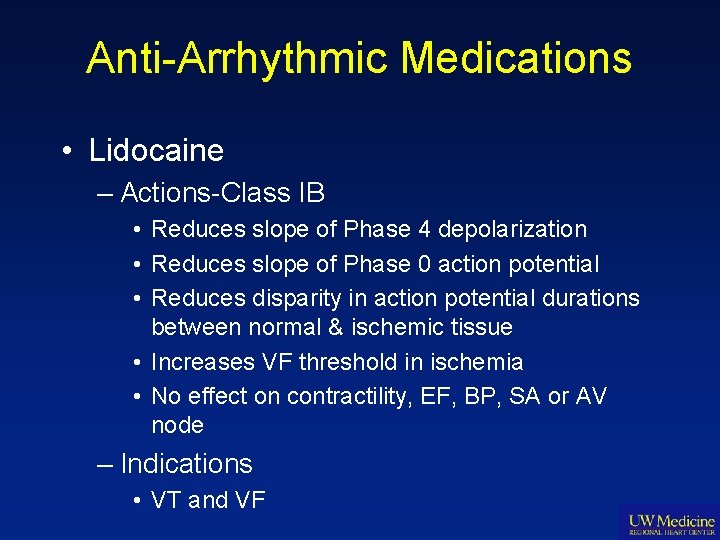
Anti-Arrhythmic Medications • Lidocaine – Actions-Class IB • Reduces slope of Phase 4 depolarization • Reduces slope of Phase 0 action potential • Reduces disparity in action potential durations between normal & ischemic tissue • Increases VF threshold in ischemia • No effect on contractility, EF, BP, SA or AV node – Indications • VT and VF
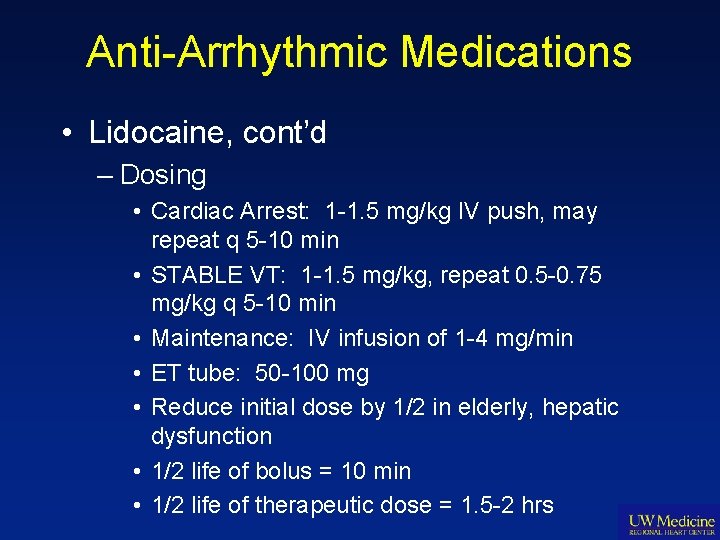
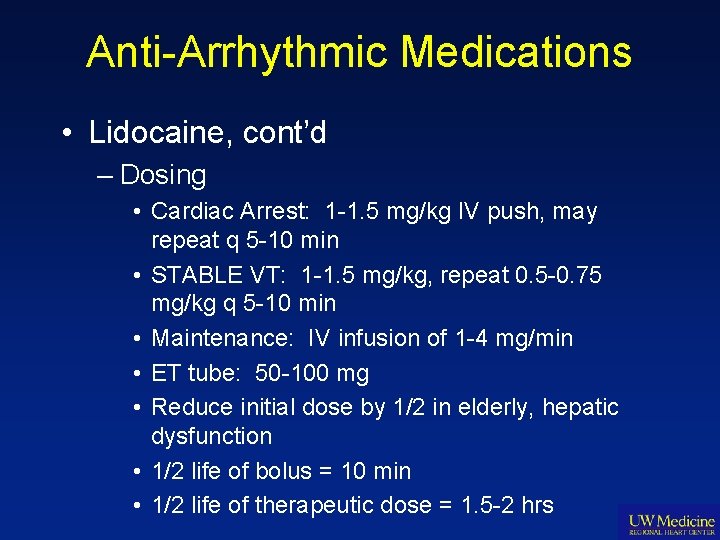
Anti-Arrhythmic Medications • Lidocaine, cont’d – Dosing • Cardiac Arrest: 1 -1. 5 mg/kg IV push, may repeat q 5 -10 min • STABLE VT: 1 -1. 5 mg/kg, repeat 0. 5 -0. 75 mg/kg q 5 -10 min • Maintenance: IV infusion of 1 -4 mg/min • ET tube: 50 -100 mg • Reduce initial dose by 1/2 in elderly, hepatic dysfunction • 1/2 life of bolus = 10 min • 1/2 life of therapeutic dose = 1. 5 -2 hrs
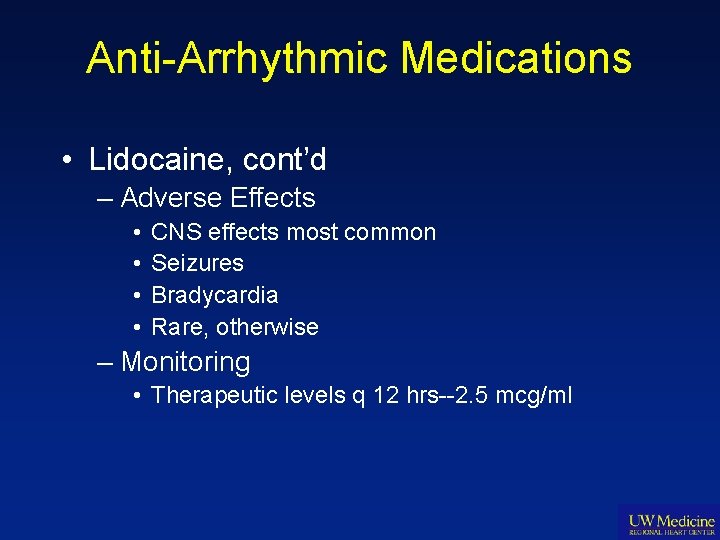
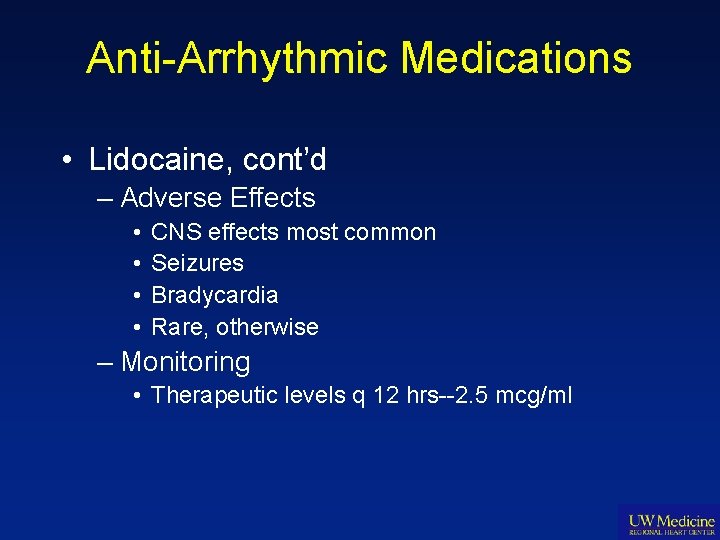
Anti-Arrhythmic Medications • Lidocaine, cont’d – Adverse Effects • • CNS effects most common Seizures Bradycardia Rare, otherwise – Monitoring • Therapeutic levels q 12 hrs--2. 5 mcg/ml
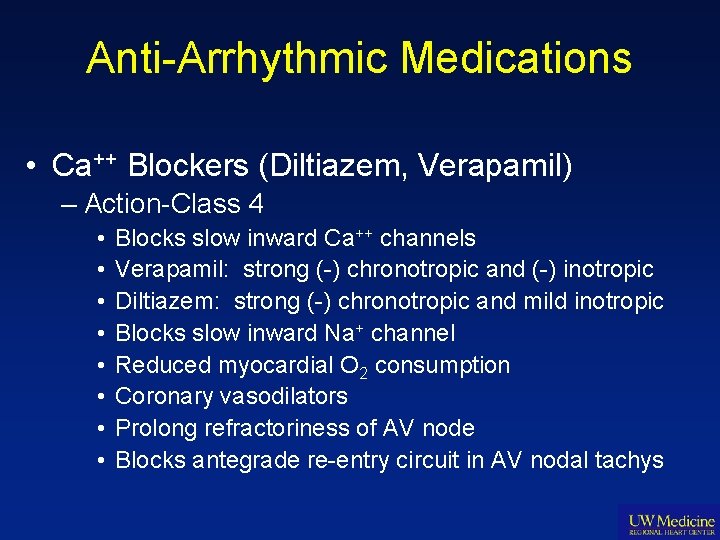
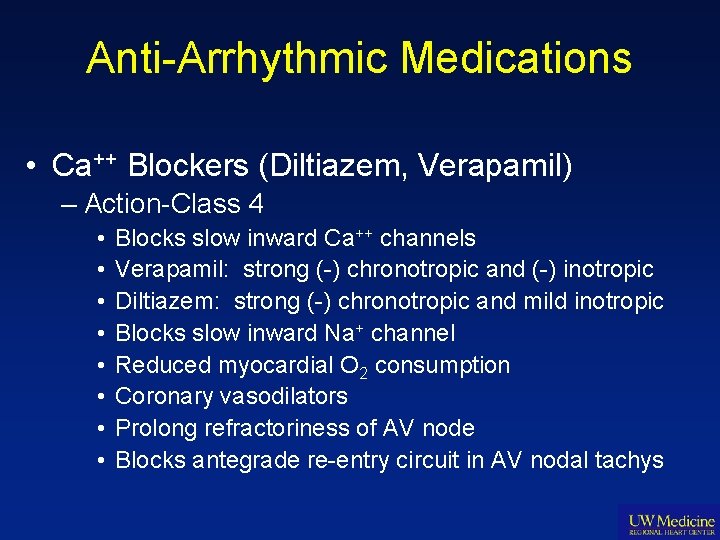
Anti-Arrhythmic Medications • Ca++ Blockers (Diltiazem, Verapamil) – Action-Class 4 • • Blocks slow inward Ca++ channels Verapamil: strong (-) chronotropic and (-) inotropic Diltiazem: strong (-) chronotropic and mild inotropic Blocks slow inward Na+ channel Reduced myocardial O 2 consumption Coronary vasodilators Prolong refractoriness of AV node Blocks antegrade re-entry circuit in AV nodal tachys
Anti-Arrhythmic Medications • Ca++ Blockers, cont’d – Indications • Verapamil: acute and preventive SVT, do NOT use in WPW-causes VF • Diltiazem: SVT and rapid ventricular response in afib/flutter, minimal effect in WPW, no effect on EF • Ischemia related tachycardias
Anti-Arrhythmic Medications • Ca++ Blockers, cont’d – Dosing • Diltiazem: IV only for arrhythmias, acute rate control is 15 -20 mg IV over 2 min. PO dosing for anti-anginal effects only • Infuse 5 -15 mg/hr, titrate to HR • 1/2 life is 4 -50 hrs • Verapamil: IV infusion 2. 5 -5 mg IV over 2 min, may give 5 -10 mg over 15 -30 min • Maximum dose is 20 mg • 1/2 life is 3 -7 hrs • PO: 80 -120 mg bid • Therapeutic IV level is 80 -400 mcg/ml
Anti-Arrhythmic Medications • Ca++ Blockers, cont’d – Adverse Effects • Diltiazem has very few • Reduces HR and BP • Verapamil causes reduced LV function, used with caution in AV node dysfunction-can cause heart block • Severe constipation with Verapamil – Monitoring • Verapamil is best anti-arrhythmic of the Ca++ blockers • Diltiazem is the best anti-anginal • Nifedipine, amlodipine, felodipine are best anti- HTNs
Anti-Arrhythmic Medications • Procainamide (Pronestyl) – Actions Class IA • • Suppresses Phase 4 deploarization Reduces automaticity in all pacemaker cells in heart Slows conduction in AV node Slows conduction in accessory pathway in WPW – Indications • VT when Lidocaine fails, VF • WPW – Dosing • VT/VF: 20 mg/min IV infusion or 17 mg/kg max.
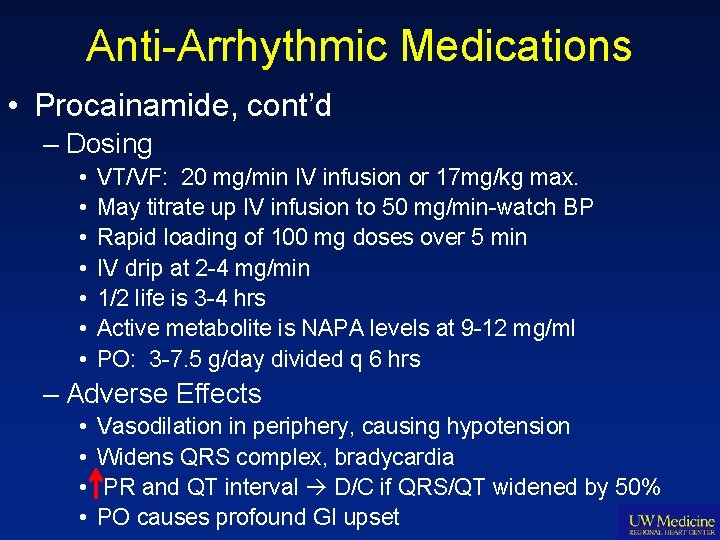
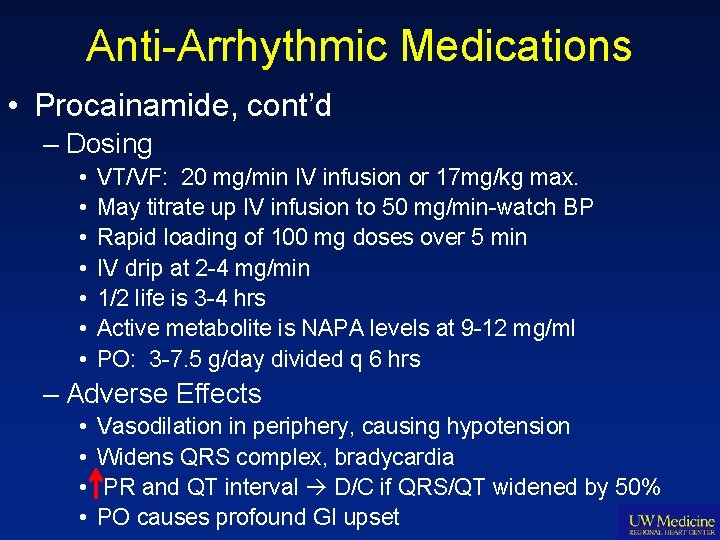
Anti-Arrhythmic Medications • Procainamide, cont’d – Dosing • • VT/VF: 20 mg/min IV infusion or 17 mg/kg max. May titrate up IV infusion to 50 mg/min-watch BP Rapid loading of 100 mg doses over 5 min IV drip at 2 -4 mg/min 1/2 life is 3 -4 hrs Active metabolite is NAPA levels at 9 -12 mg/ml PO: 3 -7. 5 g/day divided q 6 hrs – Adverse Effects • • Vasodilation in periphery, causing hypotension Widens QRS complex, bradycardia PR and QT interval D/C if QRS/QT widened by 50% PO causes profound GI upset
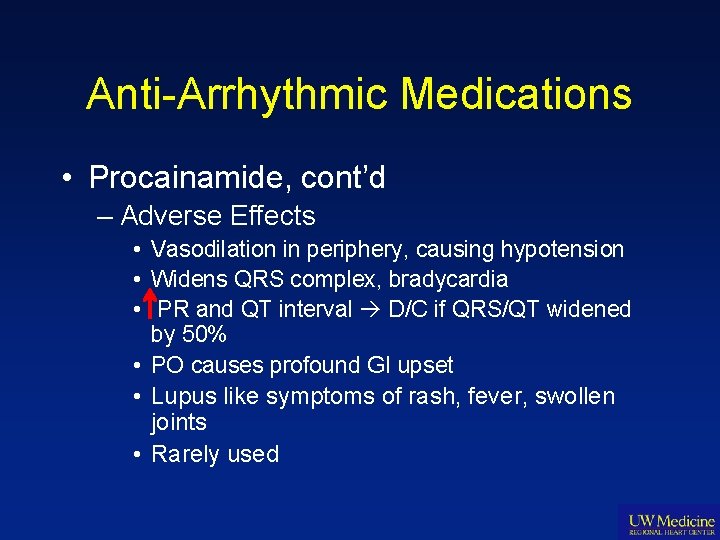
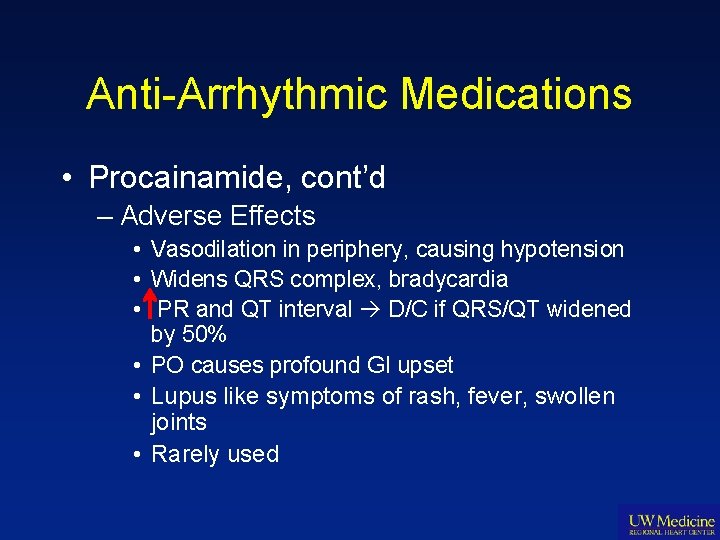
Anti-Arrhythmic Medications • Procainamide, cont’d – Adverse Effects • Vasodilation in periphery, causing hypotension • Widens QRS complex, bradycardia • PR and QT interval D/C if QRS/QT widened by 50% • PO causes profound GI upset • Lupus like symptoms of rash, fever, swollen joints • Rarely used
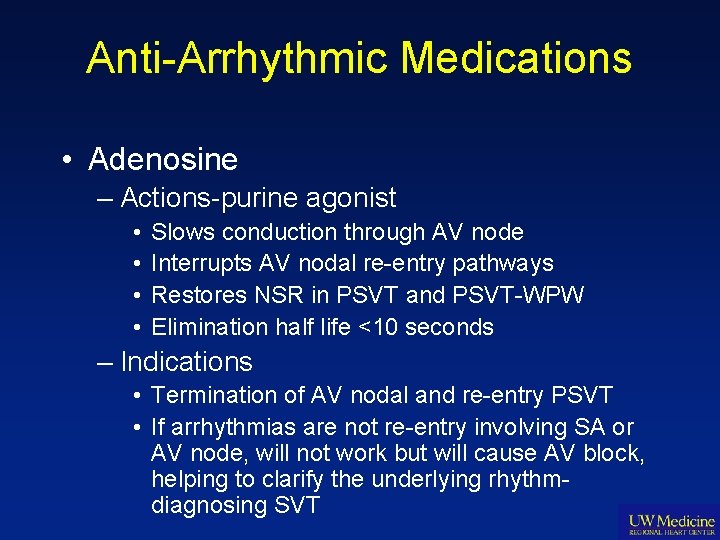
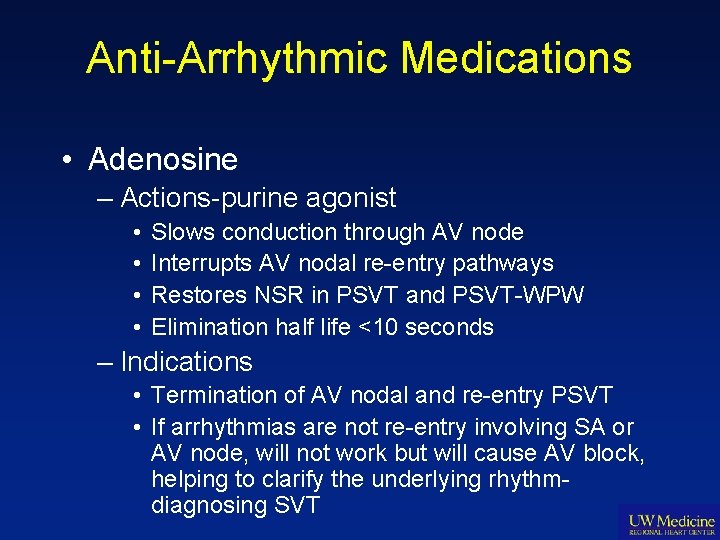
Anti-Arrhythmic Medications • Adenosine – Actions-purine agonist • • Slows conduction through AV node Interrupts AV nodal re-entry pathways Restores NSR in PSVT and PSVT-WPW Elimination half life <10 seconds – Indications • Termination of AV nodal and re-entry PSVT • If arrhythmias are not re-entry involving SA or AV node, will not work but will cause AV block, helping to clarify the underlying rhythmdiagnosing SVT
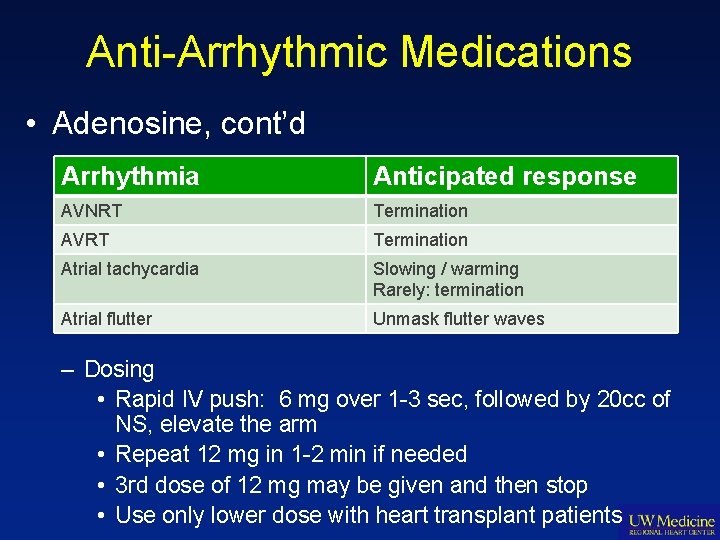
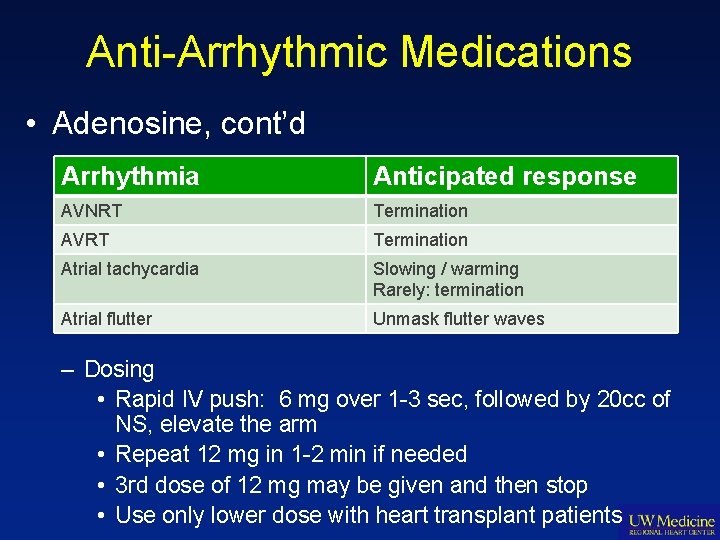
Anti-Arrhythmic Medications • Adenosine, cont’d Arrhythmia Anticipated response AVNRT Termination AVRT Termination Atrial tachycardia Slowing / warming Rarely: termination Atrial flutter Unmask flutter waves – Dosing • Rapid IV push: 6 mg over 1 -3 sec, followed by 20 cc of NS, elevate the arm • Repeat 12 mg in 1 -2 min if needed • 3 rd dose of 12 mg may be given and then stop • Use only lower dose with heart transplant patients
Anti-Arrhythmic Medications • Adenosine, cont’d – Adverse Effects • Flushing, dyspnea, chest pain over a few seconds • Acute AV block may last a few seconds • Torsades de pointes may occur in those susceptible to bradycardia dependent arrhythmias – Caution in: • WPW with AFib • Severe bronchospastic pulmonary disease • Heart transplantation
Anti-Arrhythmic Medications • Digoxin – Actions-cardiac glycoside • Controls ventricular response in A fib/flutter • (+) inotropic in CHF to improve LV function by inhibition of Na-K-ATPase, increasing intracellular Ca++, and increasing contractility • Reduced conduction through SA and AV node
Anti-Arrhythmic Medications • Digoxin, cont’d – Indications • Controls ventricular rate in A fib/flutter • Converts PSVT to NSR • Can use emergently if no DC cardioversion needed-can cause asystole if shocked – Dosing • IV: 0. 5 -1 mg in divided doses over 3 -4 hours, effects seen in 5 -30 min • 1/2 life is 36 -48 hrs • PO: load 0. 5 -1 mg in divided doses over 6 -8 hrs, then 0. 125 -0. 25 mg po qd • Therapeutic level is 0. 8 -1. 2 mcg/L
Anti-Arrhythmic Medications • Digoxin, cont’d – Adverse Effects • Digoxin toxicity: 7 -20% of cases, more common with low K+, low Mg++, or high Ca++, causes all kinds of arrhythmias, n/v, bradycardia, AV block • Digoxin has liver metabolism • Digitoxin-renal metabolism, not used anymore • Do not use with WPW • Do not cardiovert dig toxic patient • Many drug interactions
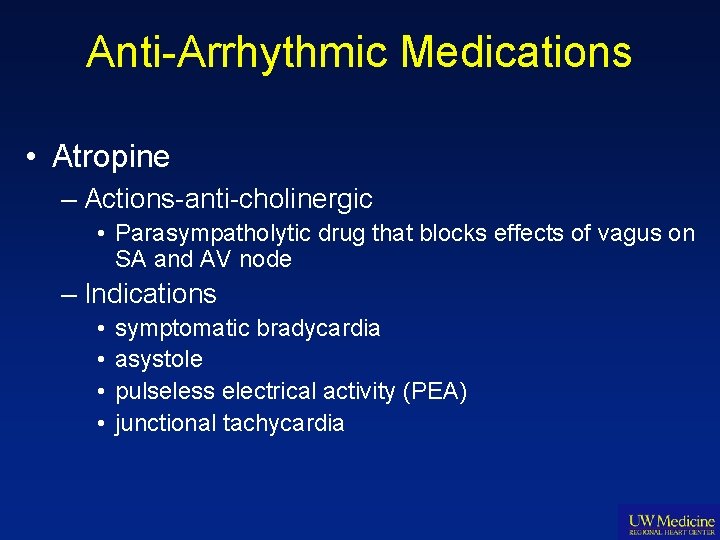
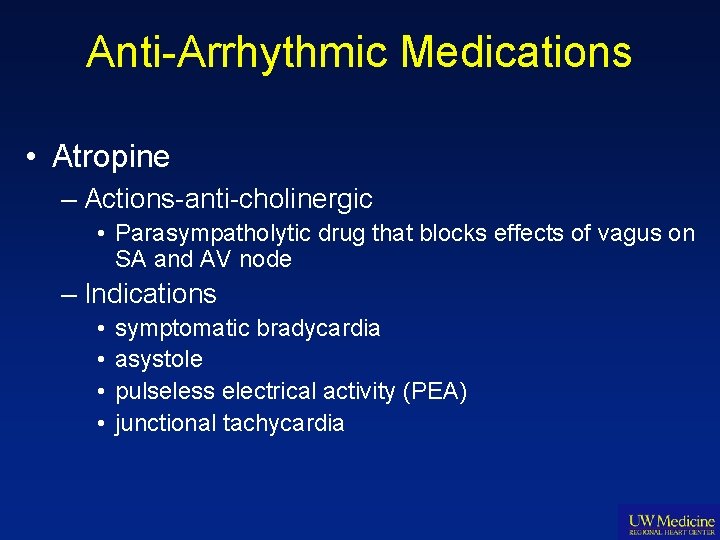
Anti-Arrhythmic Medications • Atropine – Actions-anti-cholinergic • Parasympatholytic drug that blocks effects of vagus on SA and AV node – Indications • • symptomatic bradycardia asystole pulseless electrical activity (PEA) junctional tachycardia
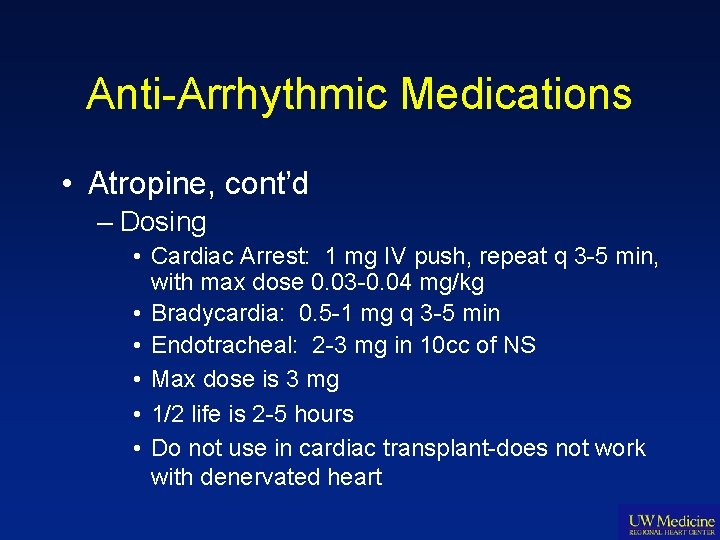
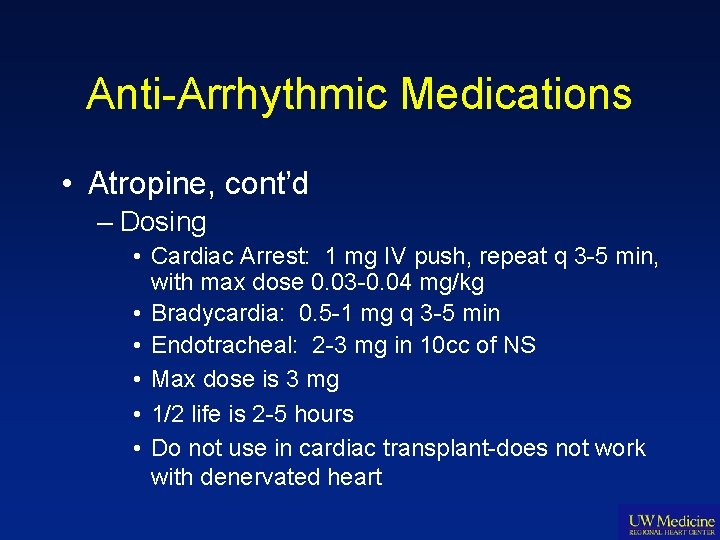
Anti-Arrhythmic Medications • Atropine, cont’d – Dosing • Cardiac Arrest: 1 mg IV push, repeat q 3 -5 min, with max dose 0. 03 -0. 04 mg/kg • Bradycardia: 0. 5 -1 mg q 3 -5 min • Endotracheal: 2 -3 mg in 10 cc of NS • Max dose is 3 mg • 1/2 life is 2 -5 hours • Do not use in cardiac transplant-does not work with denervated heart
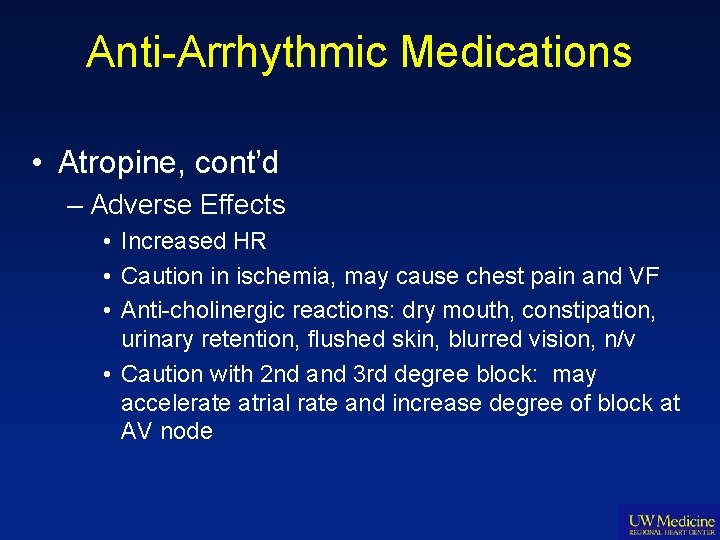
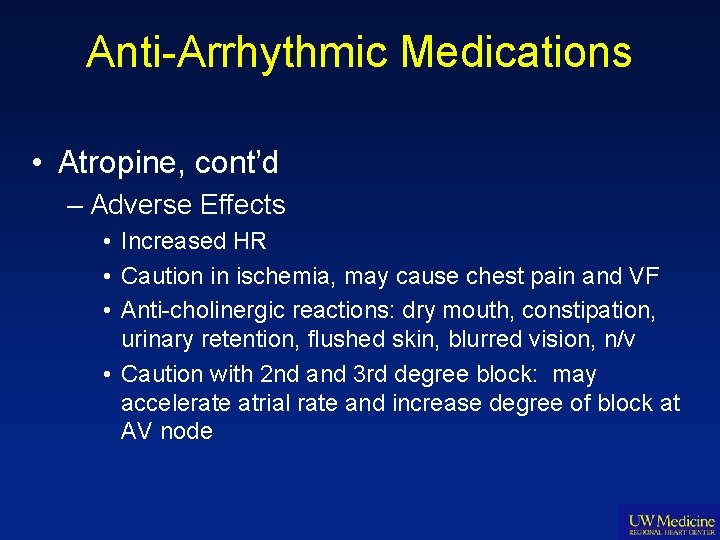
Anti-Arrhythmic Medications • Atropine, cont’d – Adverse Effects • Increased HR • Caution in ischemia, may cause chest pain and VF • Anti-cholinergic reactions: dry mouth, constipation, urinary retention, flushed skin, blurred vision, n/v • Caution with 2 nd and 3 rd degree block: may accelerate atrial rate and increase degree of block at AV node
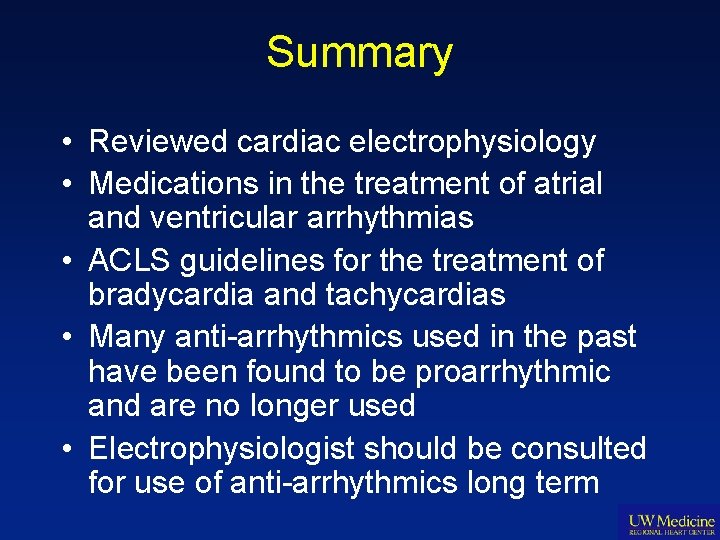
Summary • Reviewed cardiac electrophysiology • Medications in the treatment of atrial and ventricular arrhythmias • ACLS guidelines for the treatment of bradycardia and tachycardias • Many anti-arrhythmics used in the past have been found to be proarrhythmic and are no longer used • Electrophysiologist should be consulted for use of anti-arrhythmics long term
CASE STUDIES…
Case Study-A fib In 2007, a 62 yr old male presented to an ER with palpitations & irregular rhythm. He was found to be in AF. Subsequently, he was treated with metoprolol, followed by diltiazem. but experienced intolerable SE. Thereafter, he tried propafenone but had frequent breakthrough of AF. In 2010, he developed exertional CP. An angiogram demonstrated 70% RCA stenosis so he had a DES placed. He’s now seeking EP referral for management of AF. PMH: 1) PAF. 2) CAD s/p DES x 3 in 6/2010. EF 55%, normal LV & LA size. CHADS 2 = 0. MEDS: Diltiazem, Ranitidine, Plavix, ASA, Fish Oil, Lipitor. EKG: NSR with left anterior fascicular block and vent. rate 88 bpm. RX: Discontinued Propafenone (1 c). Replaced with dronedarone (Multaq) 400 mg BID. Continued ASA (& Plavix).
Case Study-A fib 3 months later…in clinic reported horrible SE with dronedarone + recurrent paroxysmal AF episodes (now in AF about 40% of the time). Desires more “aggressive” approach to treatment. • RX: AF ablation with pulmonary vein isolation 9/2010. Treated post-op ≥ 3 mos w/ oral amiodarone load (baseline testing performed prior to initiation) & warfarin (referred to ACC and kept on ASA + Plavix given that DES placed < 1 year prior to this). 1 month post-ablation… 10/2010 +recurrence of AF >24 hrs. Underwent DCCV. No medication changes made. 3 months post-ablation… 12/2010 in clinic reported no more AF bouts. EKG demonstrated NSR. • RX: Discontinued amiodarone. Continued warfarin. Scheduled event monitor x 21 days beginning 6 weeks later. No AF events seen. Rate well-controlled.
Case Study-A fib 6 months post-ablation…Event monitor showed several AF episodes w/o RVR, lasting up to 16 hrs. Also Atrial Flutter seen w/ symptoms. • RX: EP study. Ablation of cavotricuspid isthmus & mitral annulus. Bidirectional block still in all 4 pulmonary veins. Post-op treated again with amiodarone and continued warfarin x 3 months post-2 nd ablation…no AF/fl recurrence. • RX: Discontinued amio; 21 day event monitor ~6 wks later…NO AF. 12 months post-2 nd ablation…No AF/fl. On Aspirin EC 325 mg daily w/o Plavix. No AADs. Energy & QOL signficantly improved. • RX: Event monitor q 6 mos until 2 years, then after this, annually.
Case Study-A fib • Atrial fibrillation – Consider ablation procedures in highly symptomatic patients with recurrence – Difficult to treat, often comes back, even after an AF ablation which may need to be repleated, usually not before 3 months post-op – Recommended long-term use of anti-coagulation, esp. if CHADS 2 score is ≥ 1 – Can precipitate ischemia in patients with CAD with rapid ventricular response – EF can improve with > time in NSR
Case Study-VT 73 yr old w male with dilated cardiomyopathy, EF = 30%. VT since 1992, previously treated with Amiodarone; stopped due to cerebellar ataxia. Had sustained VT in 2000, received ICD. Had ICD shocks in 2000, 2001, 2002 x 3. Then started sotalol 120 mg bid. Also has paroxysmal AF with cardioversion in 2000. Angiogram in 2003 with 60% LAD, Circ < 50%. NYHA Class 2. In NSR. MEDS: lisinopril, lasix, digoxin, ASA, sotalol 120 mg bid, carvedilol 6. 25 bid, simvastatin, KCl, omeprazole, Diltiazem 30 mg tid. ICD interrogation: NSVT 8 x in last month, no shocks. Rate 250 bpm. ATP was added to ICD programming. 3 days later, presented to ER & admitted with rigors, tingling, feeling of impending syncope. EKG shows V-paced rhythm in 60’s with underlying AF. He received no ICD shocks, but ICD at ERI. ICD interrogation also revealed 4 episodes of NSVT x 8 beats, rates 300 msec, self-terminating. ICD replaced the next day.
Case Study-VT NSVT was symptomatic, poorly controlled with sotalol. Pt not an amiodarone candidate, with low EF and CAD. Begin carvedilol titration up to 25 mg bid. VT resolved. Sotalol was continued at 120 mg bid. Pt was stable on carvedilol and sotalol 120 mg bid x 6 months. He then experienced VT storm where the ICD shocked him 12 x in 30 minutes. He was started on mexilitene 400 mg tid and dofetilide 500 mg bid, both seemed to stop the VT (sotalol d/c’d). He refused VT ablation several times. Subsequent ICD interrogations, showed VT at rates 100 -120 bpm. He insisted that he not receive any further ICD shocks. His ICD was turned off in June 2007. He suffered VF cardiac arrest in September and died.
Case Study-VT • Ventricular Tachycardia – Often recurrent and difficult to treat in cardiomyopathy – ICD therapy assists in diagnosis and treatment – Many medications previously found for VT now are no longer used – Consider VT ablation therapy for recurrent symptomatic VT or multiple ICD shocks
References • Special Thanks to: – Cindy Dougherty, ARNP, Ph. D – Dr. Jordan Prutkin – Dr. Robert Rho
References • Fuster, V, Ryden, LE, Cannom, DS, et al. 2006 ACC/AHA/ESC guidelines on atrial fibrillation. JACC 2006; 48: e 149. • AHA. Handbook of emergency cardiovascular care for health care providers. Dallas, TX: AHA, 2005. • Gregoratos G, Epstein AE, Hayes DL et al. ACC/AHA/NASPE 2002 Guideline Update for implantation of cardiac pacemakers and antiarrhythmia devices: Summary article. Circulation 2002; 106: 2145 -61. • 2005 AHA Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2005; 112(24): IV 1 -211.
References • Epstein AE, Di. Marco JP, et al. ACC/AHA/ HRS 2008 Guidelines for device based therapy of cardiac rhythm abnormalities. JACC, 2008; 51: e 1 -e 62. • Goldberger JJ, Cain ME, Hohnloser SH, et al. AHA/ACC/HRS scientific statement on noninvasive risk stratification techniques for identifying patients at risk for sudden cardiac death. Circulation, 2008; 118: 1497 -1518. • Serfimovski N, Burke P, Khawaja O. Usefulness of dofetilide for the prevention of atrial tachyarrhythmias (atrial fibrillation or flutter) after coronary artery bypass grafting. AJC, 2008; 101: 1574 -79.
References • ACC/AHA 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. JACC, 2006; 48: 1064 -1108. • Roy et al. Vernakalant hydrochloride for the rapid conversion of a fib. Circulation, 2008; 117: 1518 -1525, • ACTIVE Investigators. Effect of clopidrogrel added to ASA in patients with a fib. NEJM, 2009; 360: 2066 -2078.
References • 2011 ACCF/AHA/HRS Focused Update on the Management of Patients With Atrial Fibrillation (Updating the 2006 Guideline) : A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circ, 2011; 123: 104 -123. • Sinz, E & Navarro, K. (Eds. ). (2011). AHA Advanced Cardiovascular Life Support Provider Manual. United States: AHA.
References • Connolly SJ, et al. RE-LY Steering Committee and Investigators. Dabigatran Versus Warfarin in Patients With Atrial Fibrillation. N Engl J Med. 2009; 361(12): 1139 -1151. • Van Gelder IC, et al. A comparison of rate control and rhythm control in patients with recurrent persistent atrial fibrillation. N Engl J Med. 2002; 347: 1834. • Wyse DG, et al. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med. 2002; 347: 1825.
THANK YOU Monica Knapp, ARNP VM: 206 -598 -8185 Pager: 206 -540 -6735 email: miknapp@uw. edu
 Hypertension
Hypertension Stage 1 hypertension
Stage 1 hypertension Classification of crude drugs with examples
Classification of crude drugs with examples Pharmacological and parenteral therapies
Pharmacological and parenteral therapies Copd step up
Copd step up Paul ehrlich
Paul ehrlich The pharmacological basis of therapeutics
The pharmacological basis of therapeutics Endocrine axis
Endocrine axis The pharmacological basis of therapeutics
The pharmacological basis of therapeutics Nursing management of atrial septal defect
Nursing management of atrial septal defect Drenaj ventriculo-peritoneal
Drenaj ventriculo-peritoneal H's and t's
H's and t's Failure to capture vs failure to sense ecg
Failure to capture vs failure to sense ecg What is it
What is it Inotrop batmotrop cronotrop dromotrop
Inotrop batmotrop cronotrop dromotrop Ventricular escape rhythm
Ventricular escape rhythm Ventricular shunting
Ventricular shunting Hipertrofia ventricular
Hipertrofia ventricular Tratamiento de taquicardia sinusal
Tratamiento de taquicardia sinusal Taquicardia ventricular polimorfa
Taquicardia ventricular polimorfa Normal pulmonary artery pressure
Normal pulmonary artery pressure Ventricular standstill
Ventricular standstill Left anterior fascicular block
Left anterior fascicular block Muscle contracts
Muscle contracts Fine vs coarse ventricular fibrillation
Fine vs coarse ventricular fibrillation Taquicardia ventricular polimorfa
Taquicardia ventricular polimorfa Taquicardia supraventricular
Taquicardia supraventricular Criterios de reperfusion
Criterios de reperfusion Pjc rhythm
Pjc rhythm Acls vt
Acls vt Ventricular bigeminy ecg
Ventricular bigeminy ecg Fibrilacion ventricular
Fibrilacion ventricular Ventricular system
Ventricular system Taquicardia ventricular monomórfica
Taquicardia ventricular monomórfica Autor de la imagen
Autor de la imagen Cartilago cricoides
Cartilago cricoides Desfribilador
Desfribilador Signs of increased intracranial pressure
Signs of increased intracranial pressure Interpretacion de electrocardiograma
Interpretacion de electrocardiograma Left ventricular hypertrophy
Left ventricular hypertrophy Y
Y Ventricular wall aneurysm
Ventricular wall aneurysm Electrical conduction system of the heart
Electrical conduction system of the heart Antihypertensive drugs
Antihypertensive drugs Lupus fotos
Lupus fotos Frequencia cardiaca pediatria
Frequencia cardiaca pediatria Heart tube
Heart tube Peptídeo natriurético atrial
Peptídeo natriurético atrial Lvh criteria cornell
Lvh criteria cornell Cardiversion
Cardiversion Atrial fibrilasi perki
Atrial fibrilasi perki Svt no p waves
Svt no p waves Peptídeo natriurético atrial
Peptídeo natriurético atrial Fisinopril
Fisinopril Wandering atrial pacemaker rhythm
Wandering atrial pacemaker rhythm Wandering atrial pacemaker criteria
Wandering atrial pacemaker criteria Atrial standstill
Atrial standstill Right atrial enlargement ecg
Right atrial enlargement ecg Atrial depolarization
Atrial depolarization Atrial systole
Atrial systole Right atrial abnormality ecg
Right atrial abnormality ecg Atriclip mri safety
Atriclip mri safety Batimento de escape atrial
Batimento de escape atrial Tubular secretion in nephron
Tubular secretion in nephron Sinal de sodi pallares
Sinal de sodi pallares Atrial diastole
Atrial diastole Simple cardiac cycle flow chart
Simple cardiac cycle flow chart Atrial natriuretic peptide
Atrial natriuretic peptide 7 phases of cardiac cycle
7 phases of cardiac cycle Atrial fiberation
Atrial fiberation Na+ equilibrium potential
Na+ equilibrium potential Pathway hiperkalemia
Pathway hiperkalemia Pathway hiperkalemia
Pathway hiperkalemia Atrial repolarization
Atrial repolarization Coarctatie de aorta definitie
Coarctatie de aorta definitie Block xoang nhĩ là gì
Block xoang nhĩ là gì Atrial systole
Atrial systole Atrial repolarization
Atrial repolarization Atrial systole
Atrial systole Atrial septal defect
Atrial septal defect Leitura de eletrocardiograma
Leitura de eletrocardiograma Right atrial appendage
Right atrial appendage Cpt code for left atrial appendage ligation with atriclip
Cpt code for left atrial appendage ligation with atriclip Medical ppt blogspot
Medical ppt blogspot Endocrine parts
Endocrine parts Ccs afib guidelines
Ccs afib guidelines Terapia clark monica
Terapia clark monica Monica bassili
Monica bassili Mona mawari
Mona mawari Logo colegio agustiniano cristo rey
Logo colegio agustiniano cristo rey Santa monica california
Santa monica california Monica menniti
Monica menniti Monica toca
Monica toca Sociologia della devianza unimc
Sociologia della devianza unimc Monica morgado
Monica morgado Monica white physical therapy
Monica white physical therapy Scenico in inglese
Scenico in inglese Monica selesh
Monica selesh