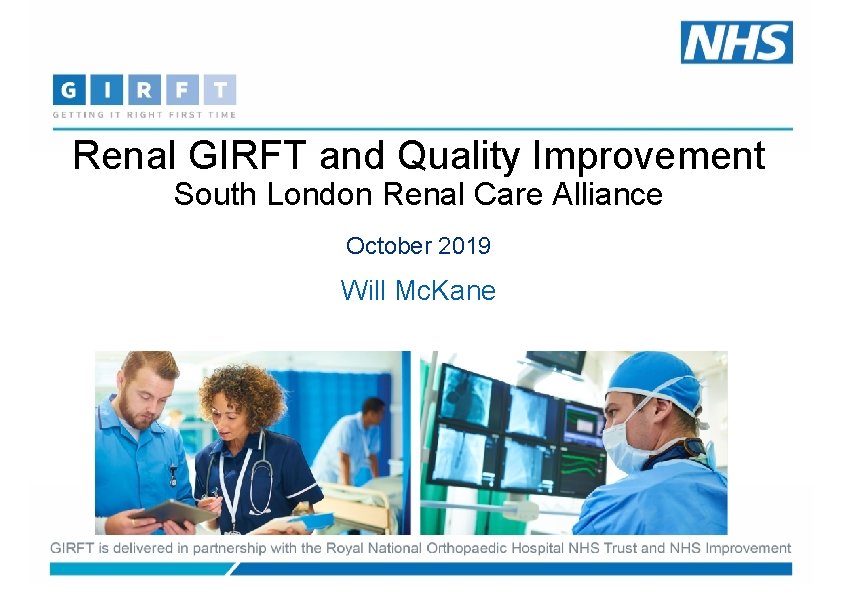
Renal GIRFT and Quality Improvement South London Renal
- Slides: 31
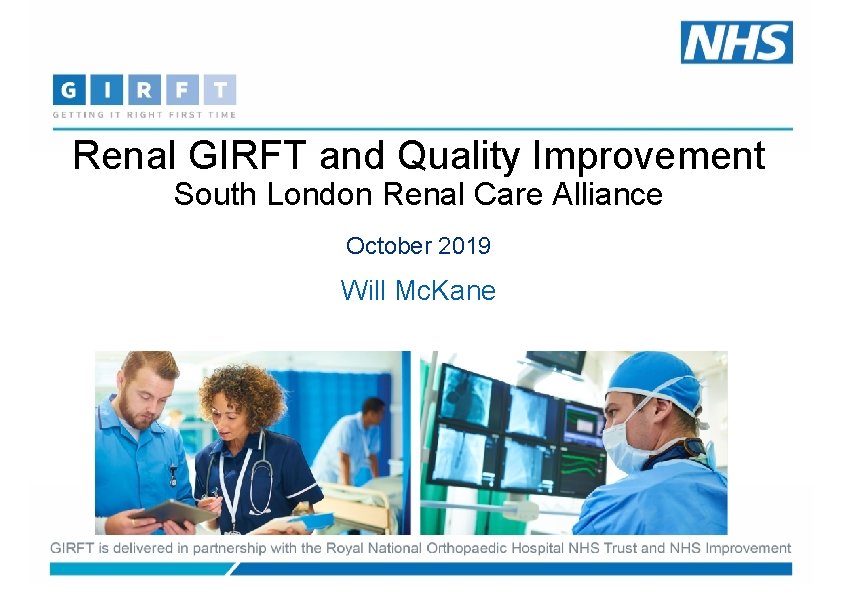
Renal GIRFT and Quality Improvement South London Renal Care Alliance October 2019 Will Mc. Kane
Getting it Right First Time (GIRFT) A clinically led programme across 40 specialties: Aims • Reduce unwarranted variation, • Improve the quality of patient outcomes • Deliver operational productivity improvements Cross Cutting themes: CC, OP, Pathology. . 2
Where are we? • 52 visits complete • Paid a price in terms of timeliness of reports • Excellent clinical engagement • Less consistent senior executive engagement • Working on National Report • February 2020 • Co-badged with RA/BRS/RCP
Emerging themes • Data • The “predictable three” • Vascular Access • Access to Transplantation • Home therapies • Prevalence • PD Access and peritonitis • Staffing • AKI requiring nephrology input • Infection • Hospitalisation • Medicines management • Procurement
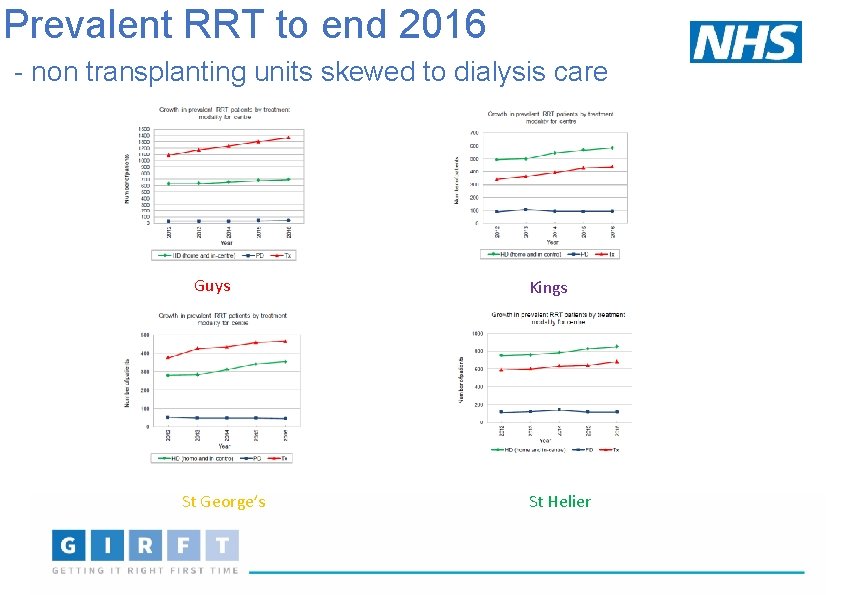
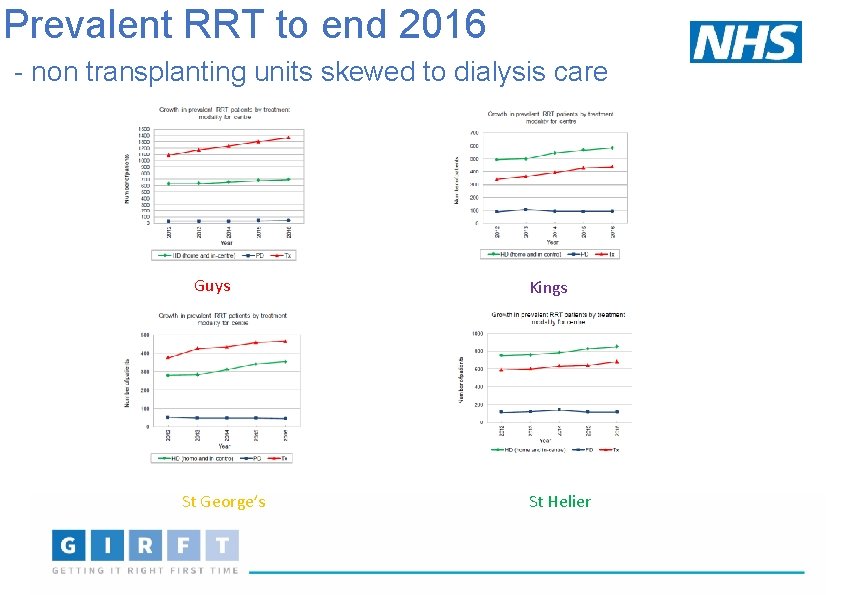
Prevalent RRT to end 2016 - non transplanting units skewed to dialysis care Guys St George’s Kings St Helier
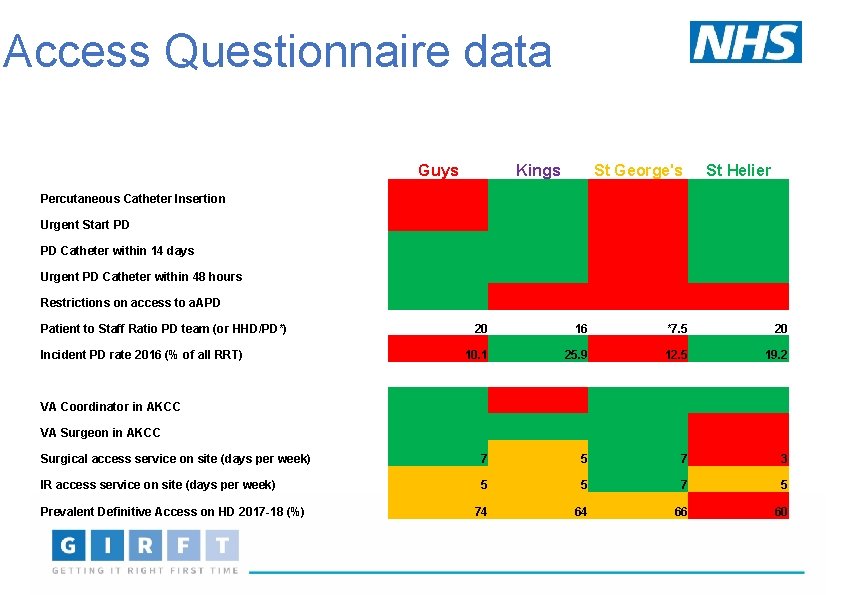
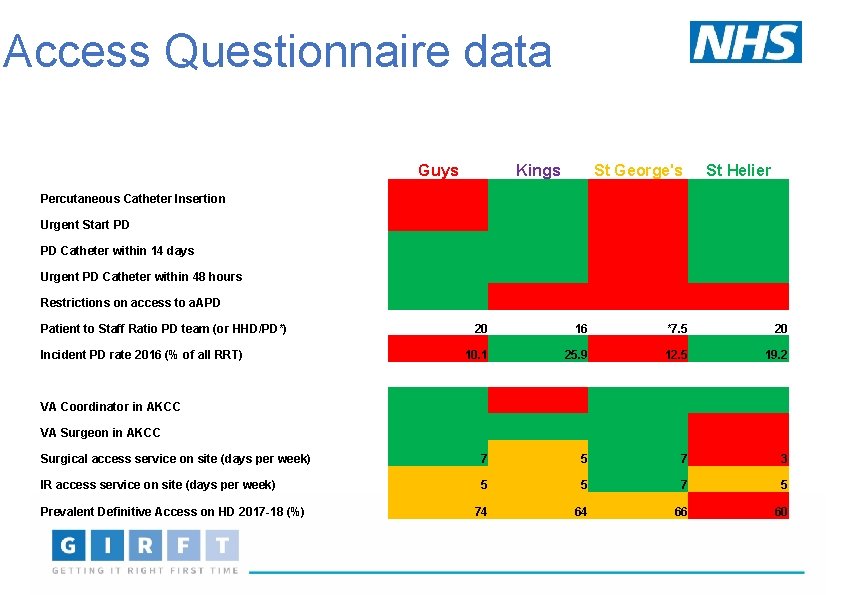
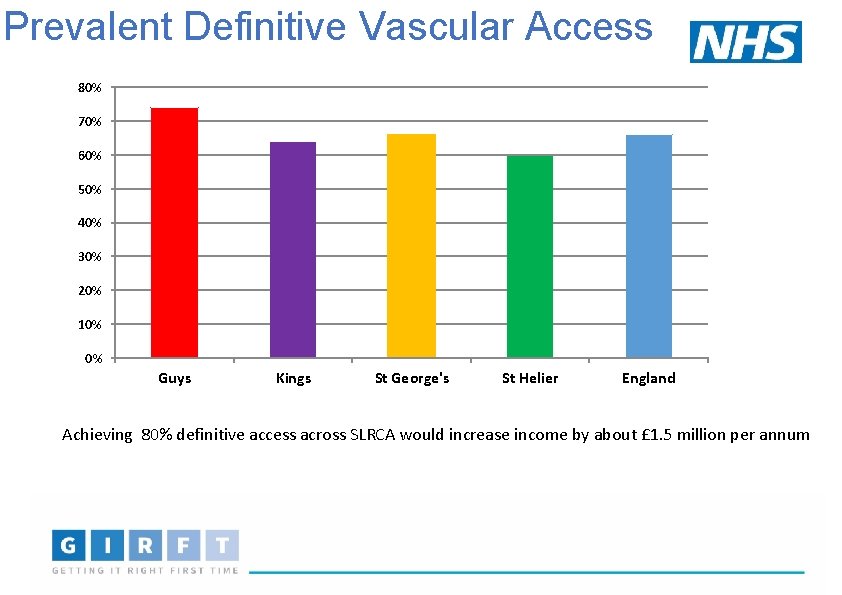
Access Questionnaire data Guys Kings St George's St Helier Percutaneous Catheter Insertion Urgent Start PD Catheter within 14 days Urgent PD Catheter within 48 hours Restrictions on access to a. APD Patient to Staff Ratio PD team (or HHD/PD*) Incident PD rate 2016 (% of all RRT) 20 16 *7. 5 20 10. 1 25. 9 12. 5 19. 2 VA Coordinator in AKCC VA Surgeon in AKCC Surgical access service on site (days per week) 7 5 7 3 IR access service on site (days per week) 5 5 74 64 66 60 Prevalent Definitive Access on HD 2017 -18 (%)
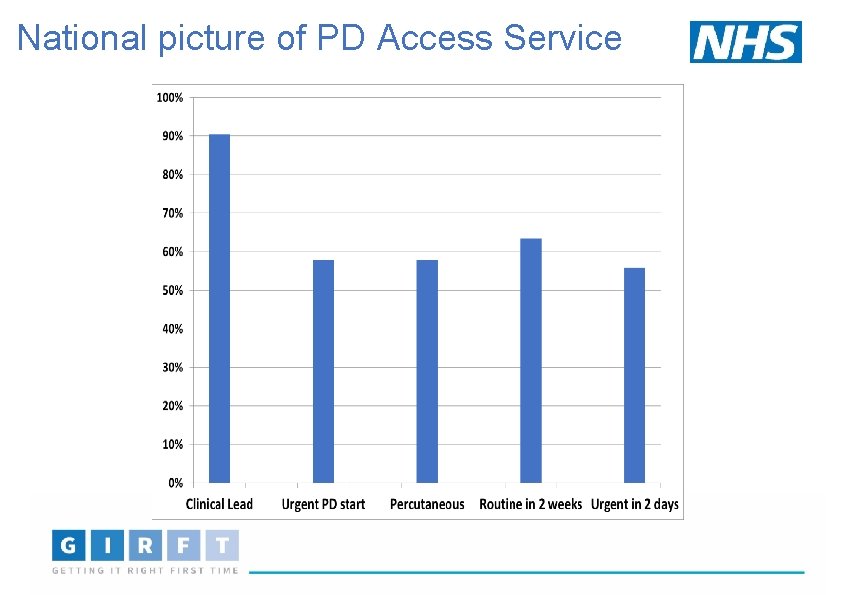
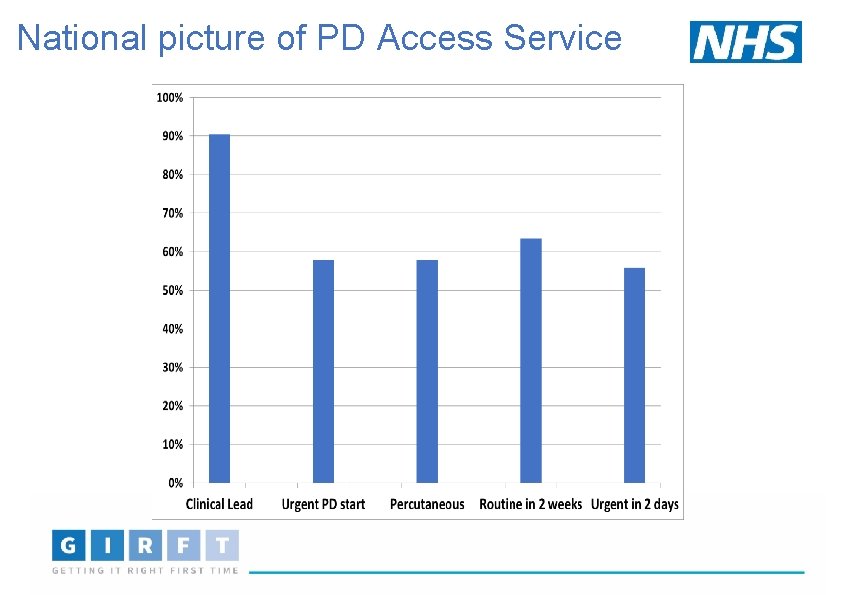
National picture of PD Access Service
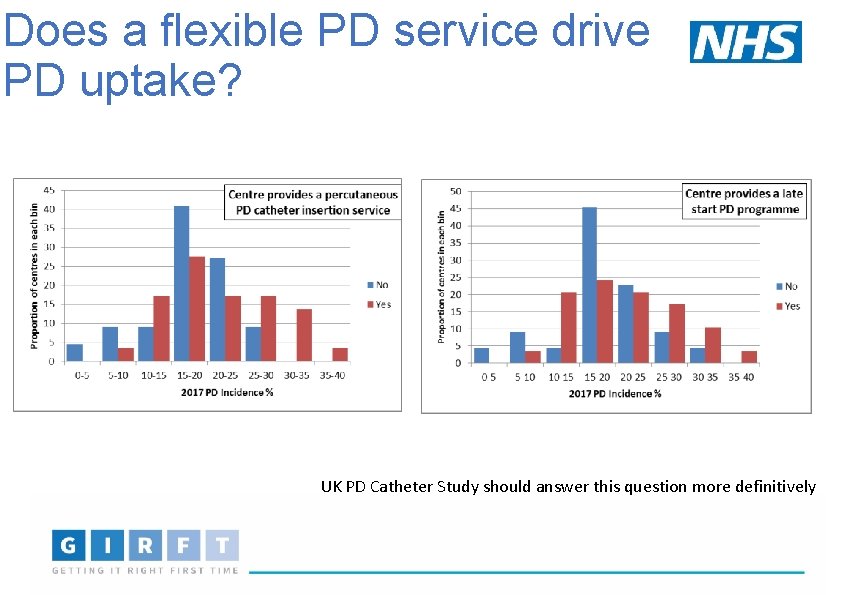
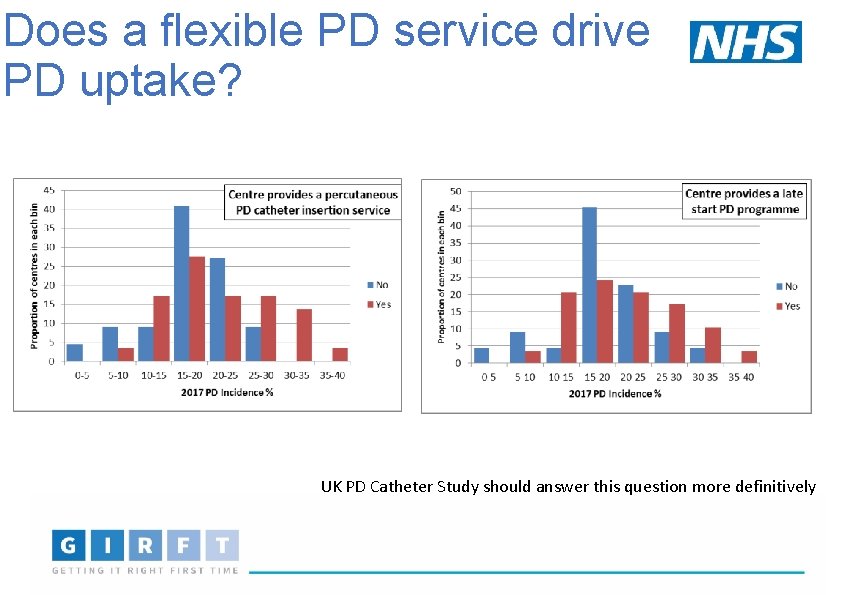
Does a flexible PD service drive PD uptake? UK PD Catheter Study should answer this question more definitively
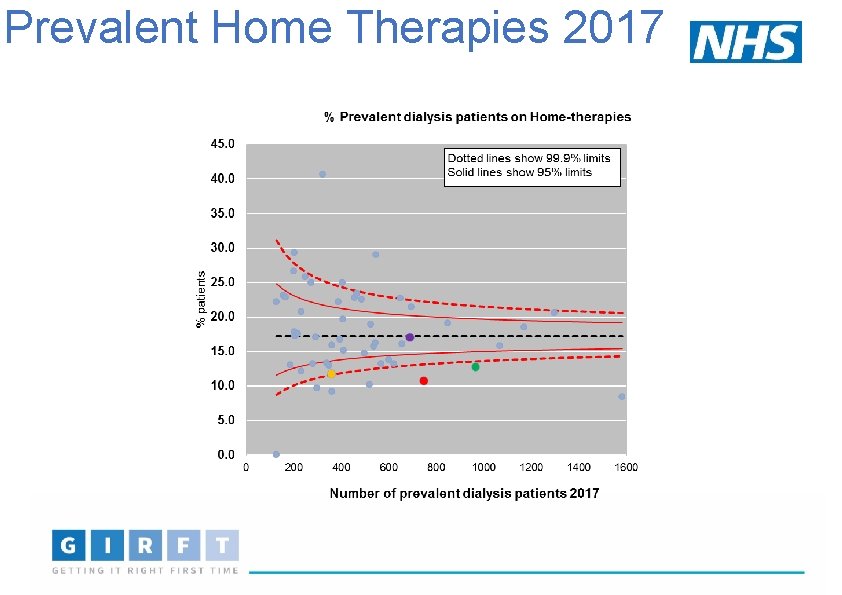
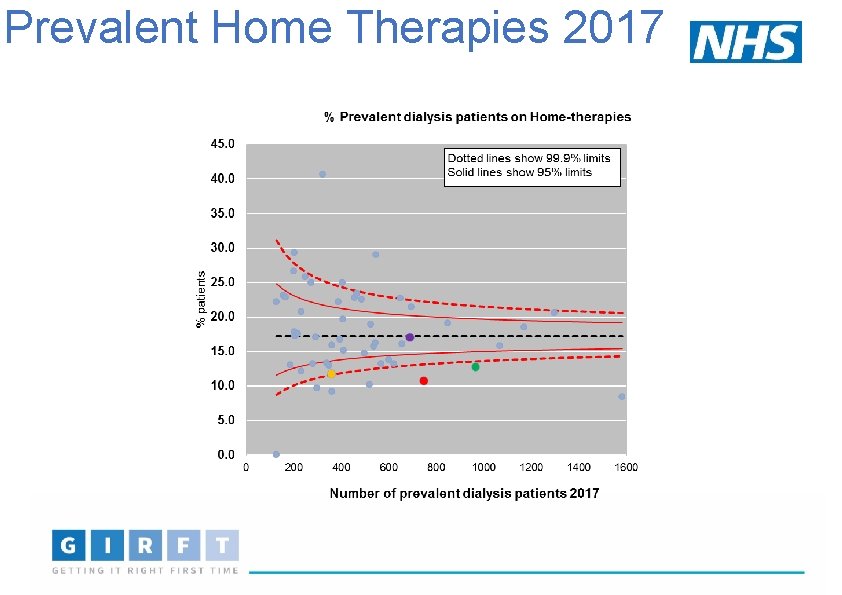
Prevalent Home Therapies 2017
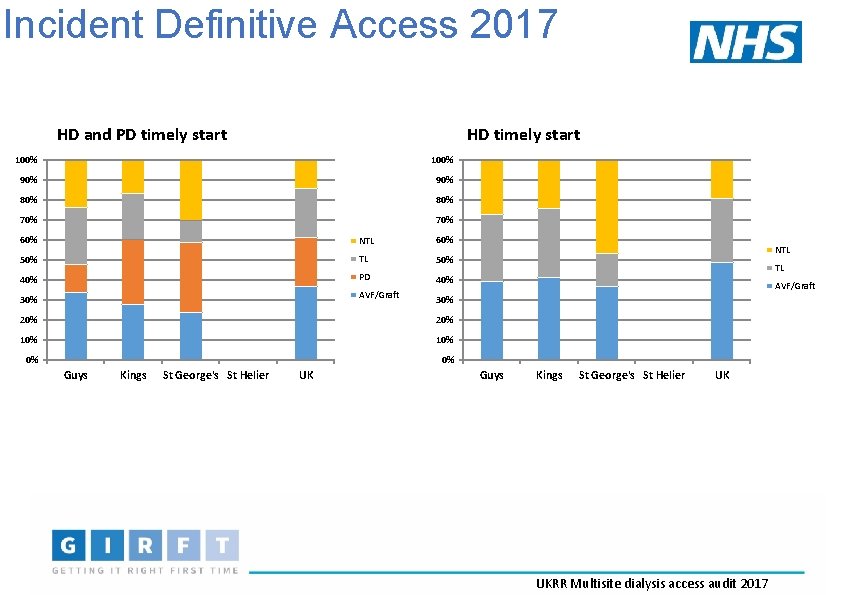
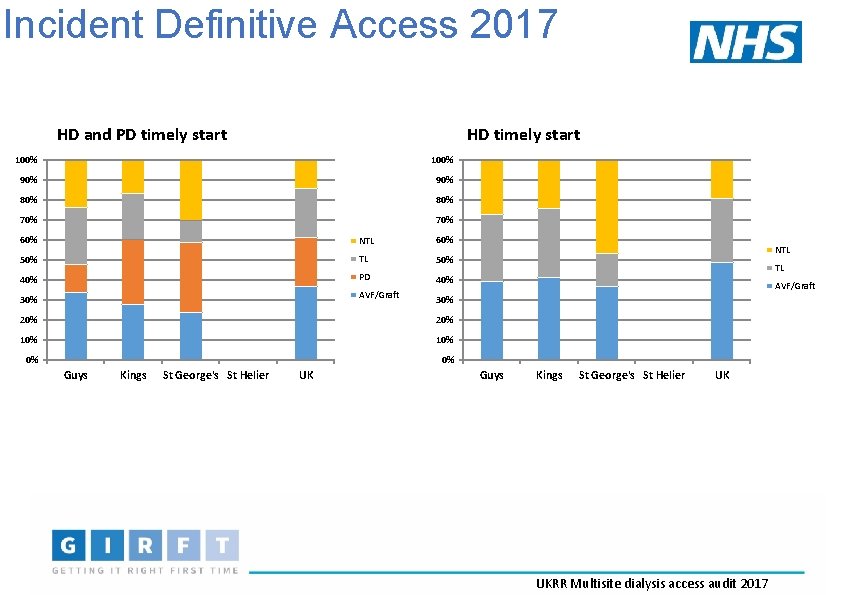
Incident Definitive Access 2017 HD and PD timely start HD timely start 100% 90% 80% 70% 60% NTL 60% 50% TL 50% 40% PD 40% AVF/Graft 30% 20% 10% 0% 0% Kings St George's St Helier UK TL AVF/Graft 30% 20% Guys NTL Guys Kings St George's St Helier UK UKRR Multisite dialysis access audit 2017
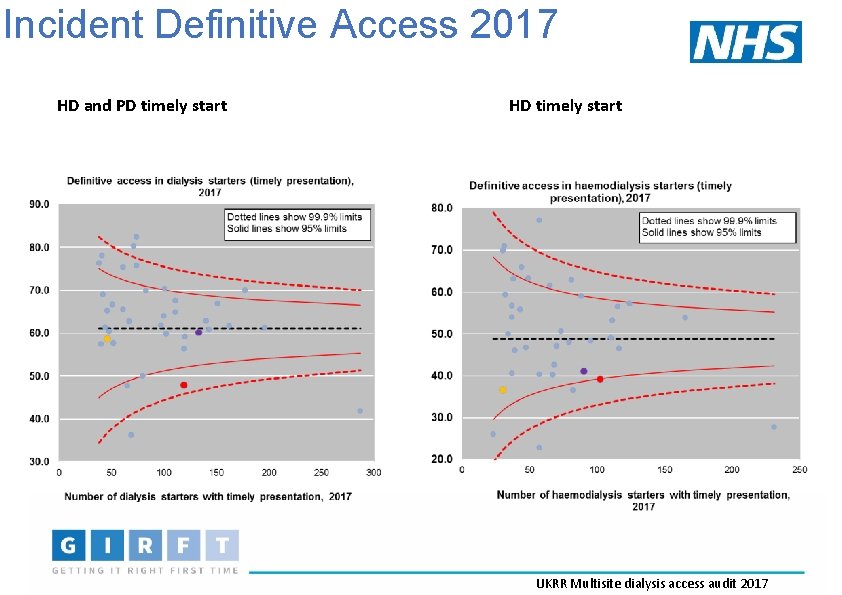
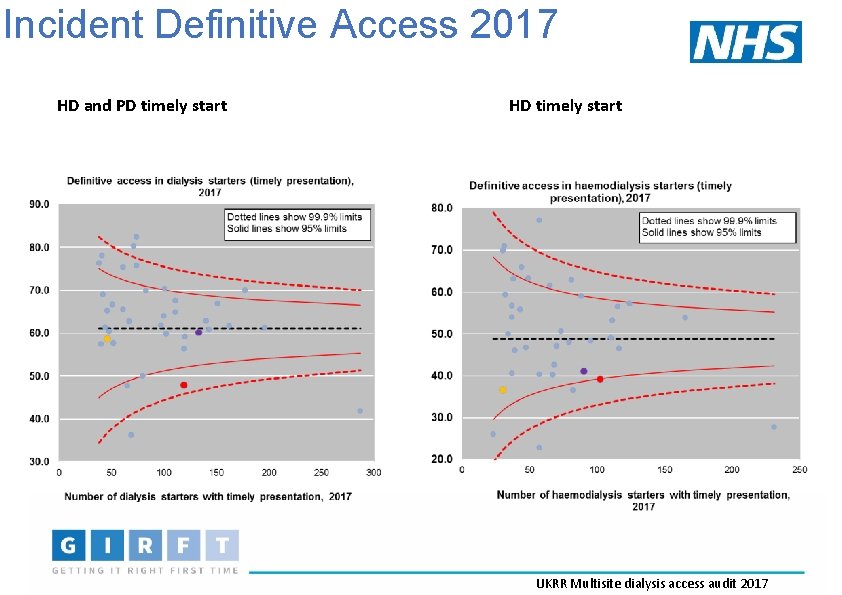
Incident Definitive Access 2017 HD and PD timely start HD timely start UKRR Multisite dialysis access audit 2017
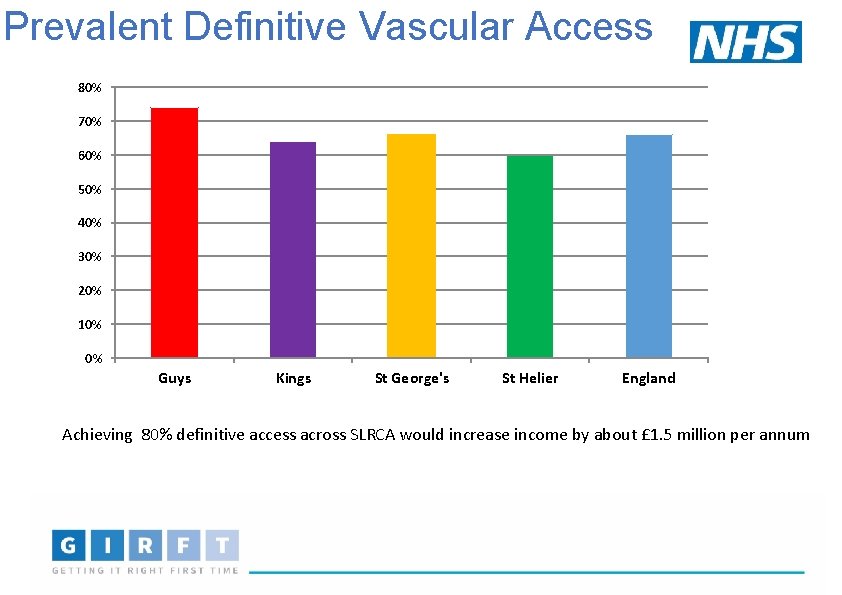
Prevalent Definitive Vascular Access 80% 70% 60% 50% 40% 30% 20% 10% 0% Guys Kings St George's St Helier England Achieving 80% definitive access across SLRCA would increase income by about £ 1. 5 million per annum
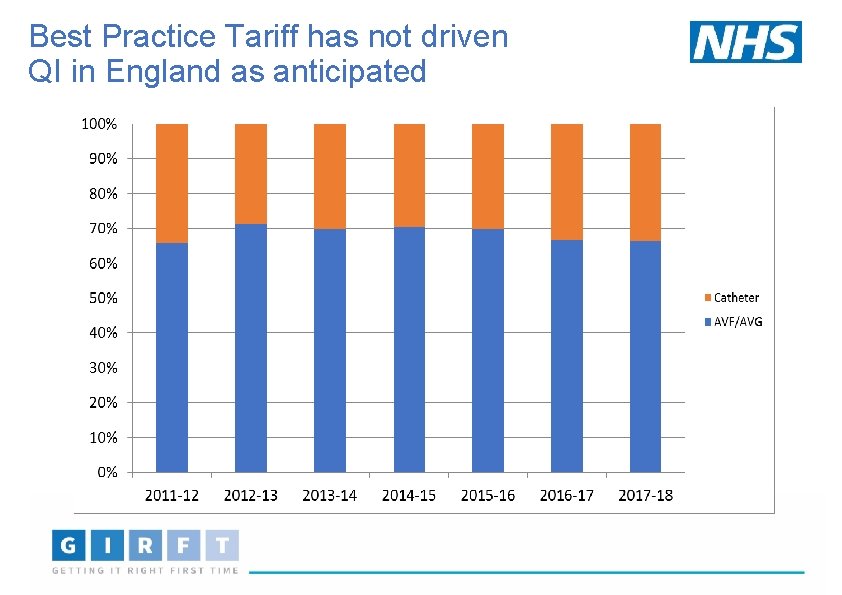
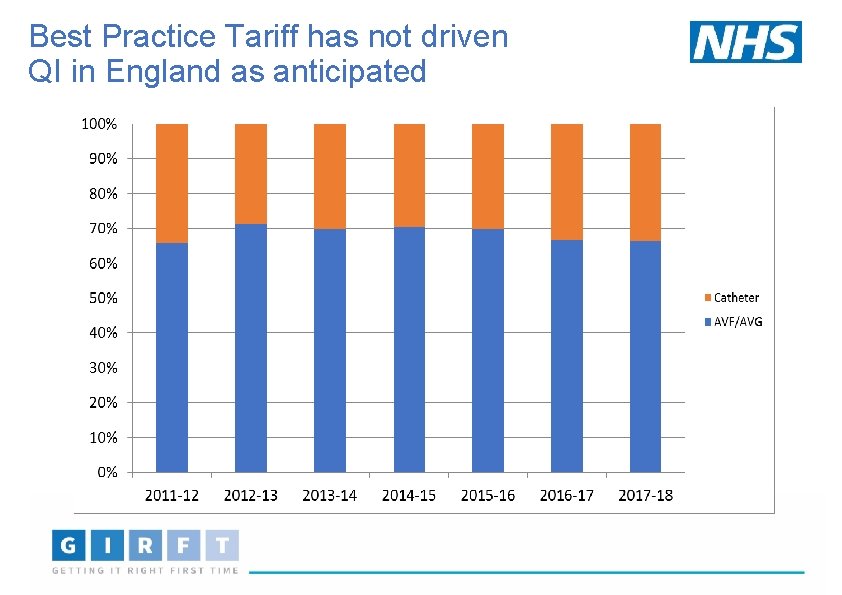
Best Practice Tariff has not driven QI in England as anticipated
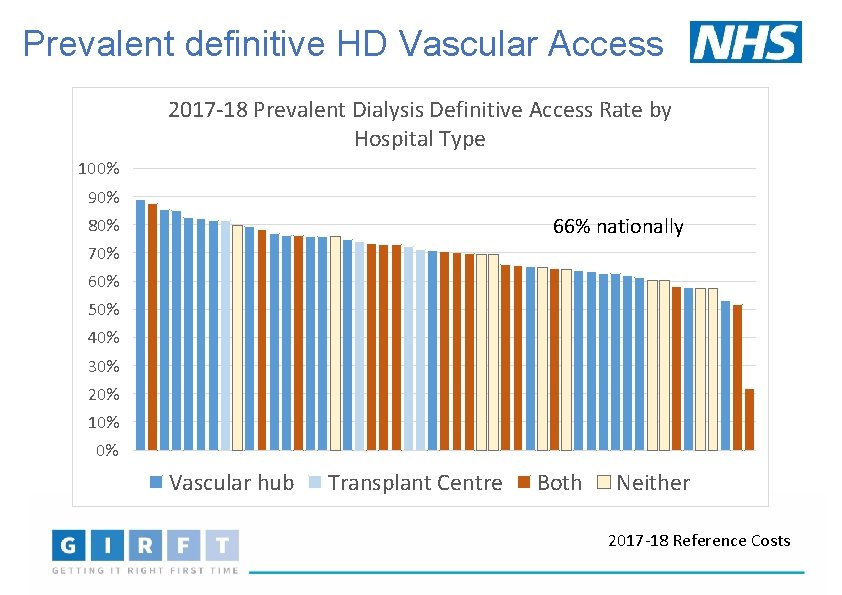
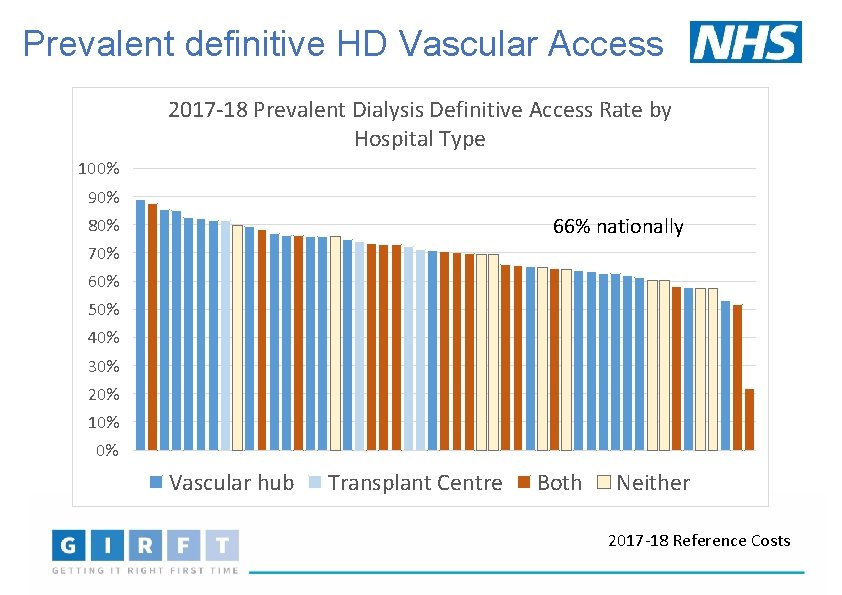
Prevalent definitive HD Vascular Access 2017 -18 Prevalent Dialysis Definitive Access Rate by Hospital Type 100% 90% 66% nationally 80% 70% 60% 50% 40% 30% 20% 10% 0% Vascular hub Transplant Centre Both Neither 2017 -18 Reference Costs
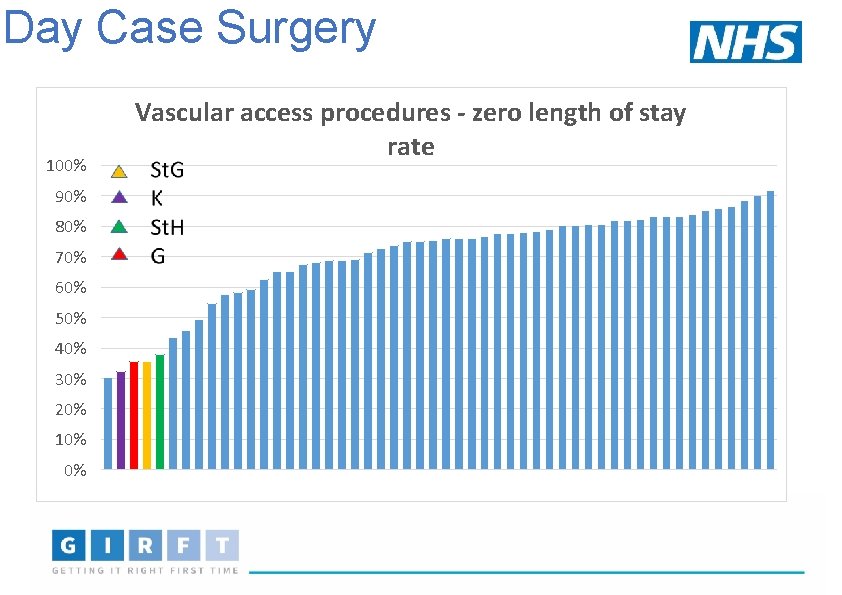
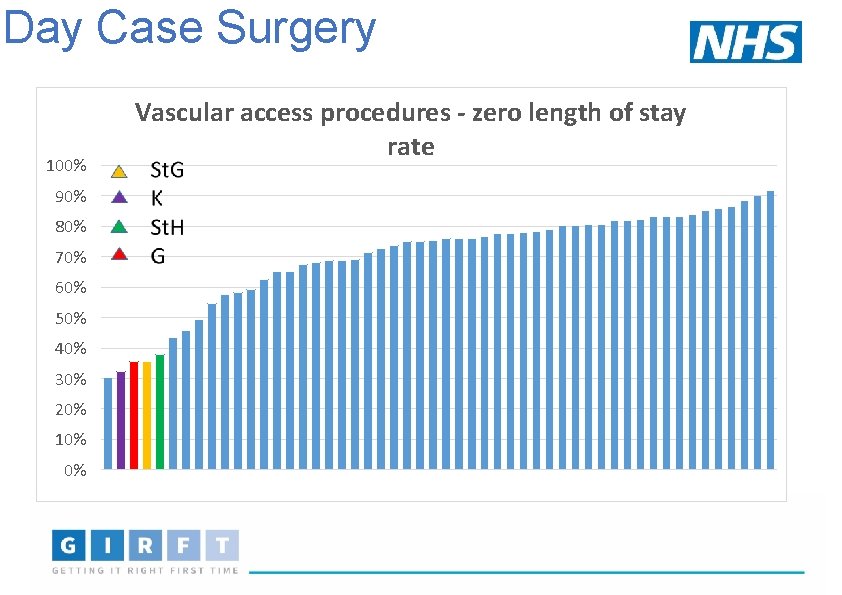
Day Case Surgery 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% Vascular access procedures - zero length of stay rate
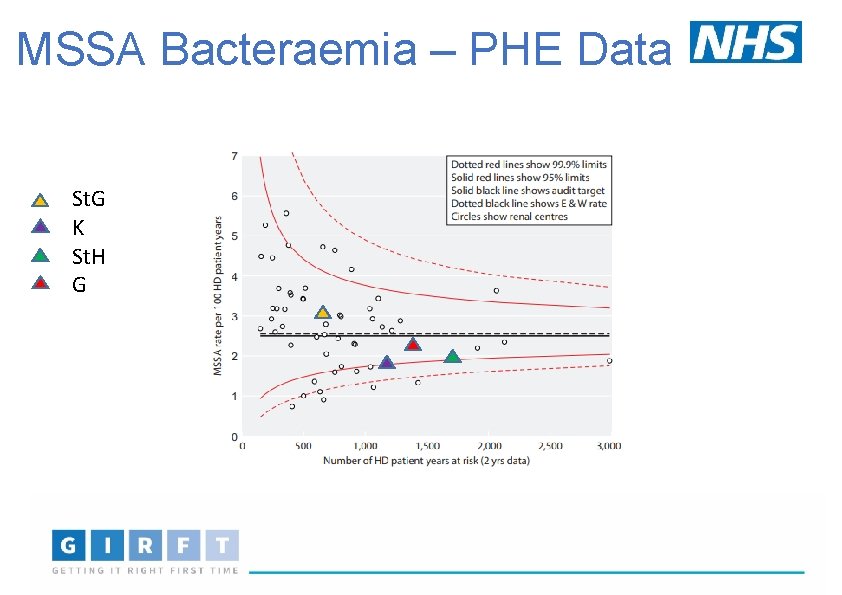
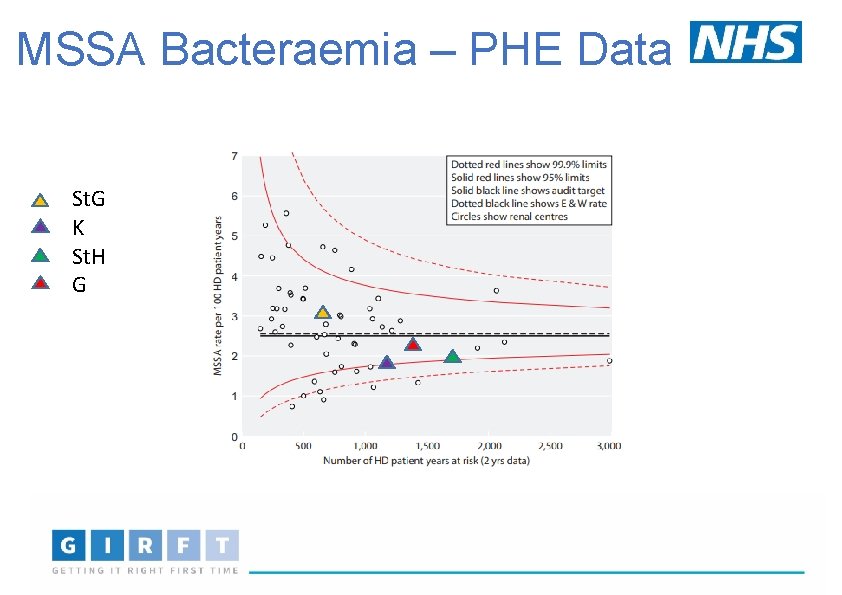
MSSA Bacteraemia – PHE Data St. G K St. H G
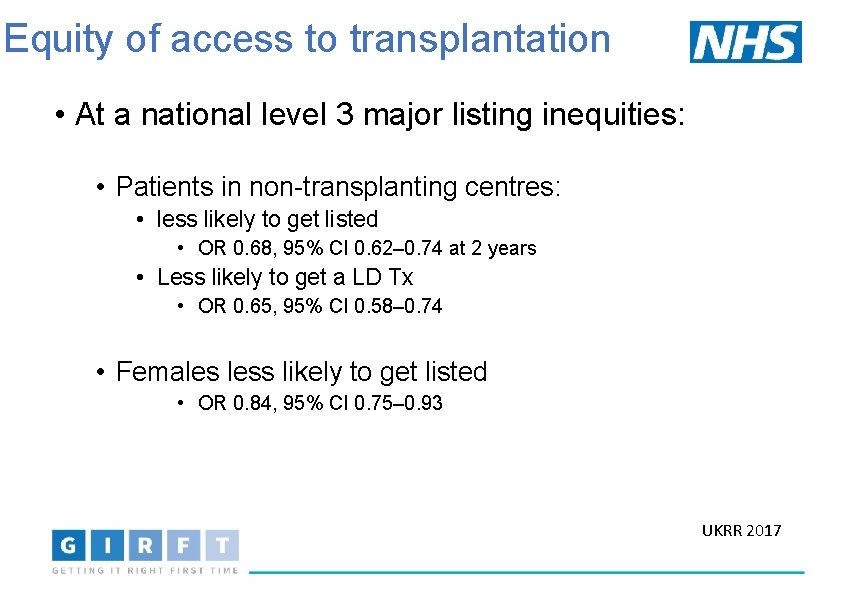
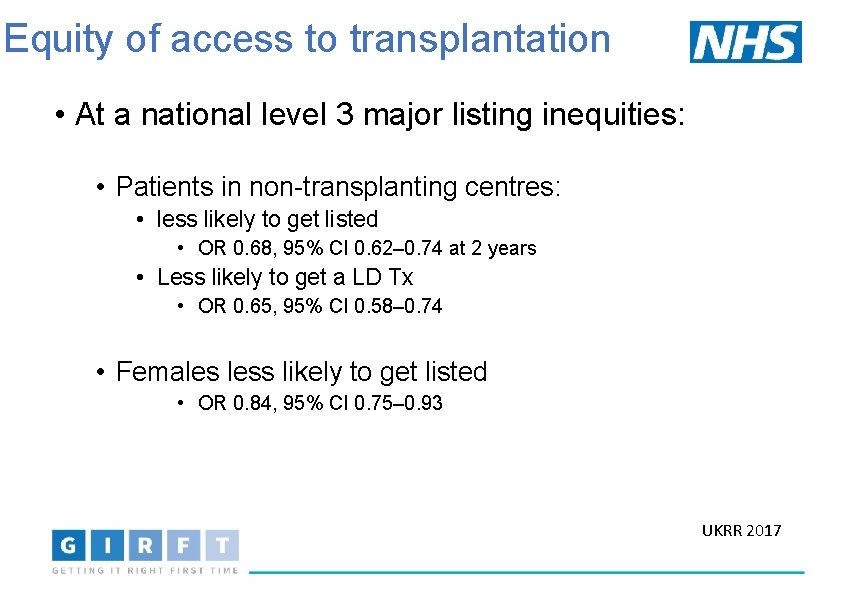
Equity of access to transplantation • At a national level 3 major listing inequities: • Patients in non-transplanting centres: • less likely to get listed • OR 0. 68, 95% CI 0. 62– 0. 74 at 2 years • Less likely to get a LD Tx • OR 0. 65, 95% CI 0. 58– 0. 74 • Females less likely to get listed • OR 0. 84, 95% CI 0. 75– 0. 93 UKRR 2017
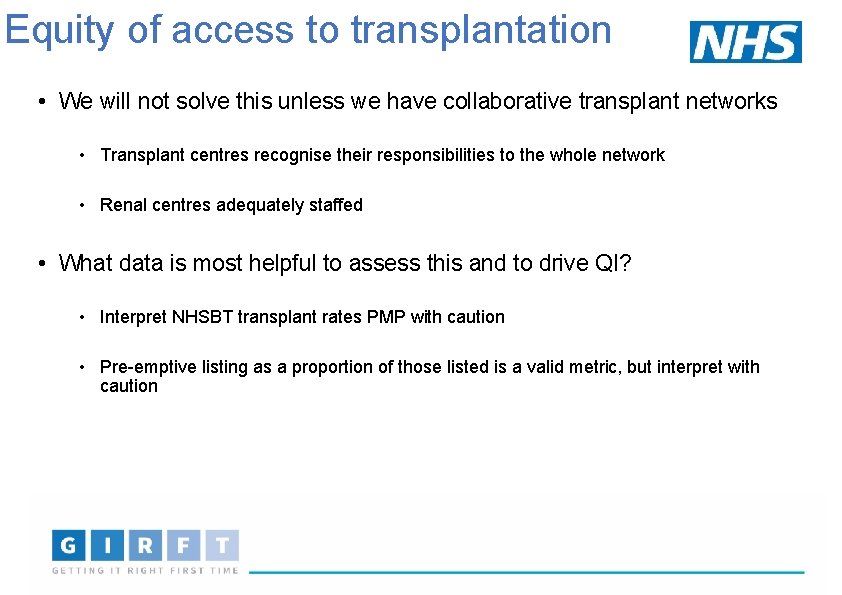
Equity of access to transplantation • We will not solve this unless we have collaborative transplant networks • Transplant centres recognise their responsibilities to the whole network • Renal centres adequately staffed • What data is most helpful to assess this and to drive QI? • Interpret NHSBT transplant rates PMP with caution • Pre-emptive listing as a proportion of those listed is a valid metric, but interpret with caution
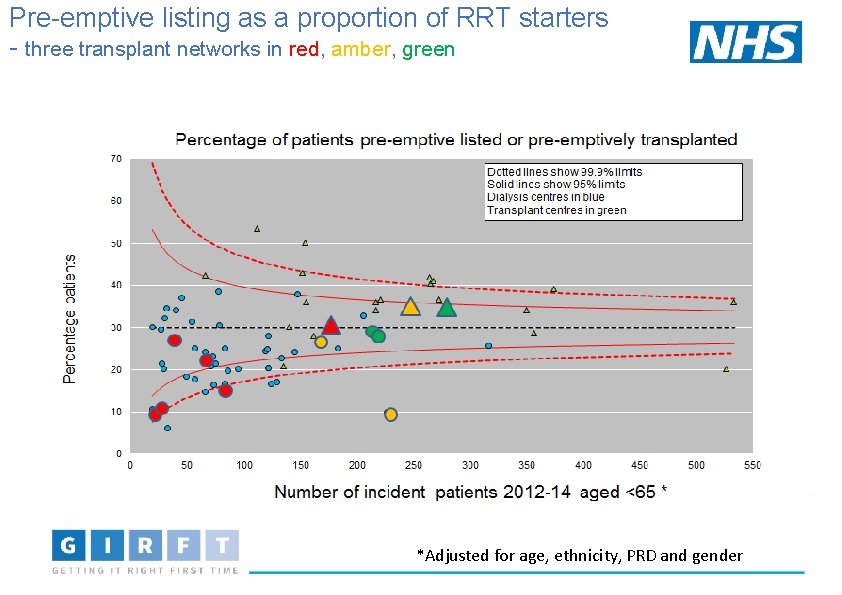
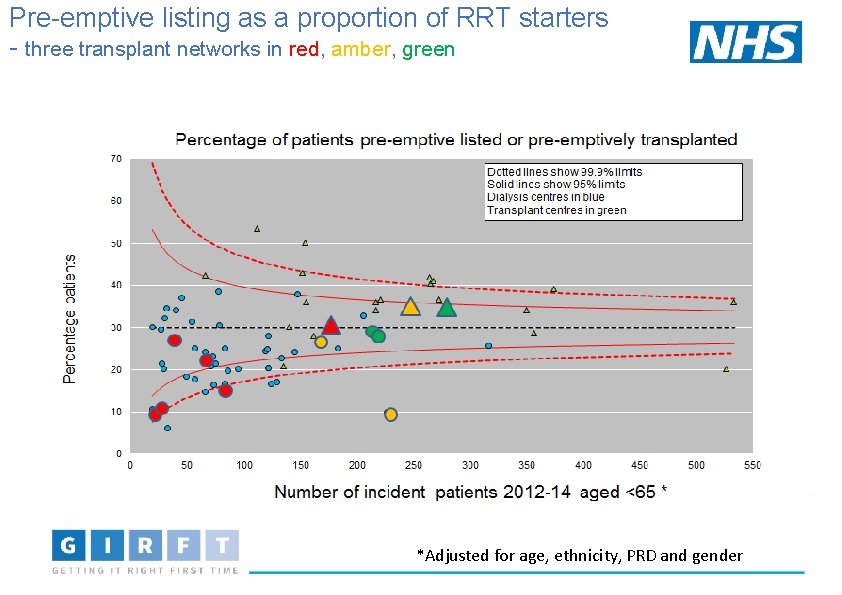
Pre-emptive listing as a proportion of RRT starters - three transplant networks in red, amber, green *Adjusted for age, ethnicity, PRD and gender
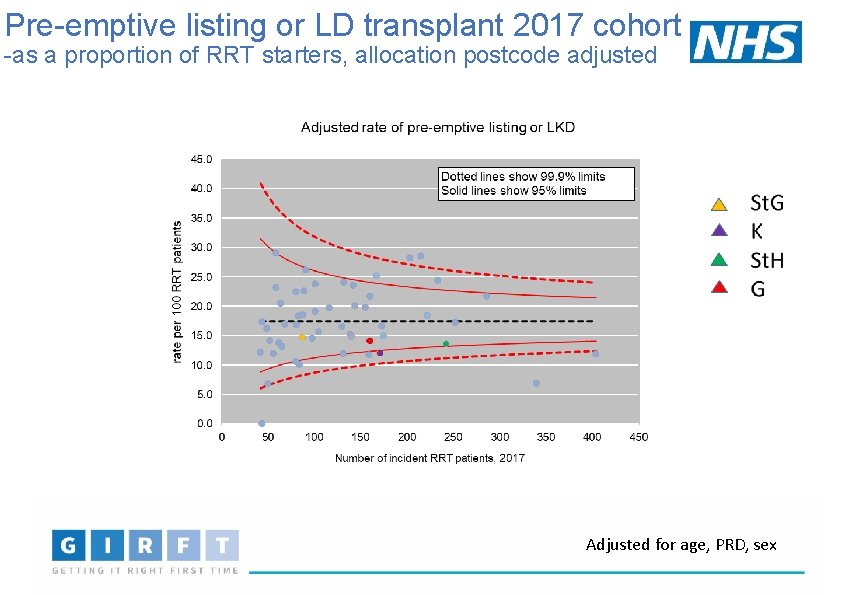
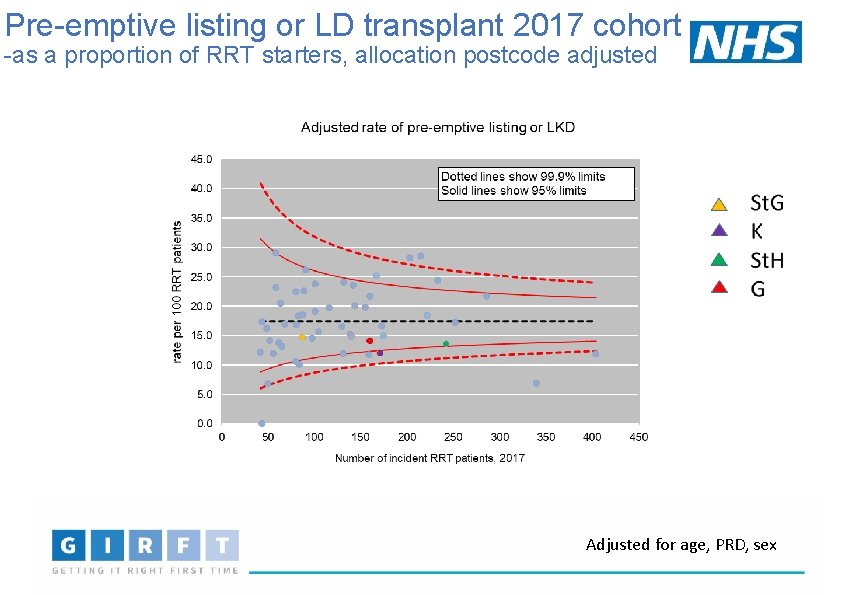
Pre-emptive listing or LD transplant 2017 cohort -as a proportion of RRT starters, allocation postcode adjusted Adjusted for age, PRD, sex
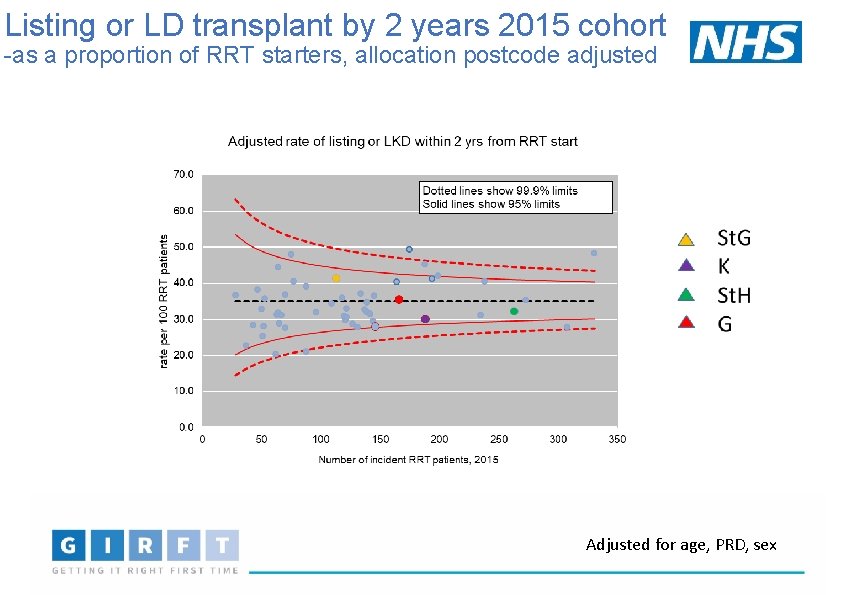
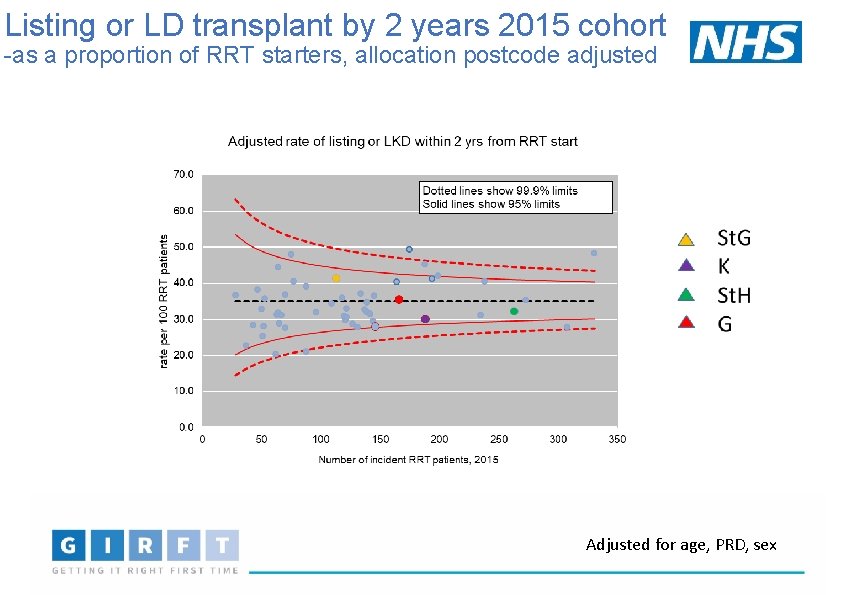
Listing or LD transplant by 2 years 2015 cohort -as a proportion of RRT starters, allocation postcode adjusted Adjusted for age, PRD, sex
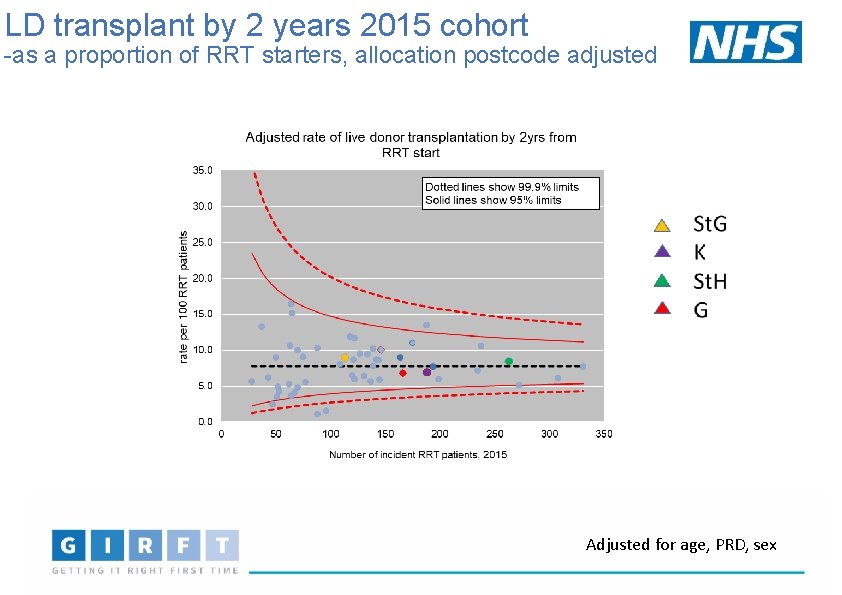
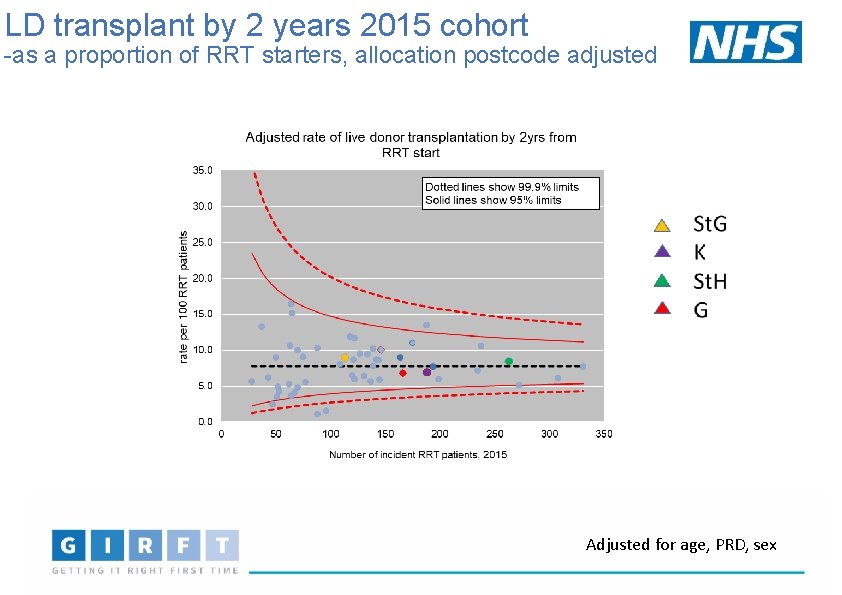
LD transplant by 2 years 2015 cohort -as a proportion of RRT starters, allocation postcode adjusted Adjusted for age, PRD, sex
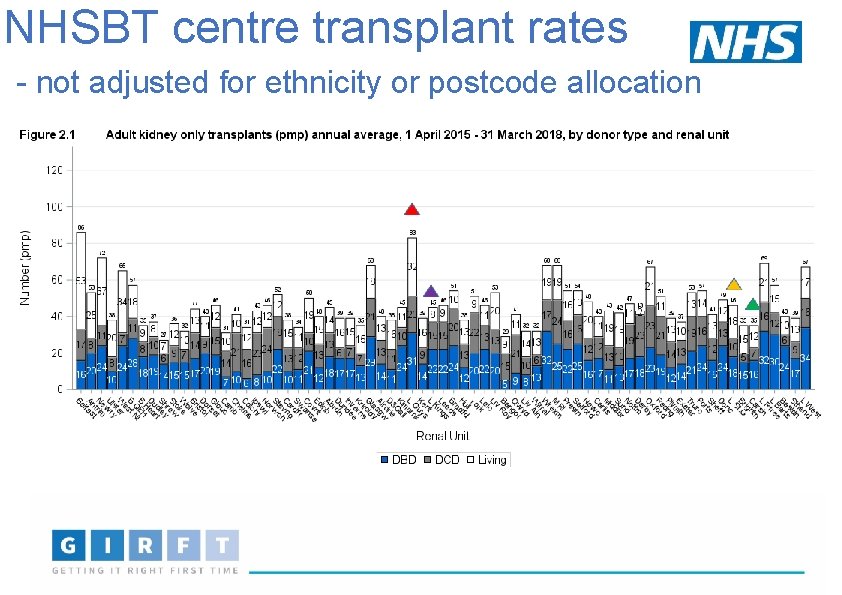
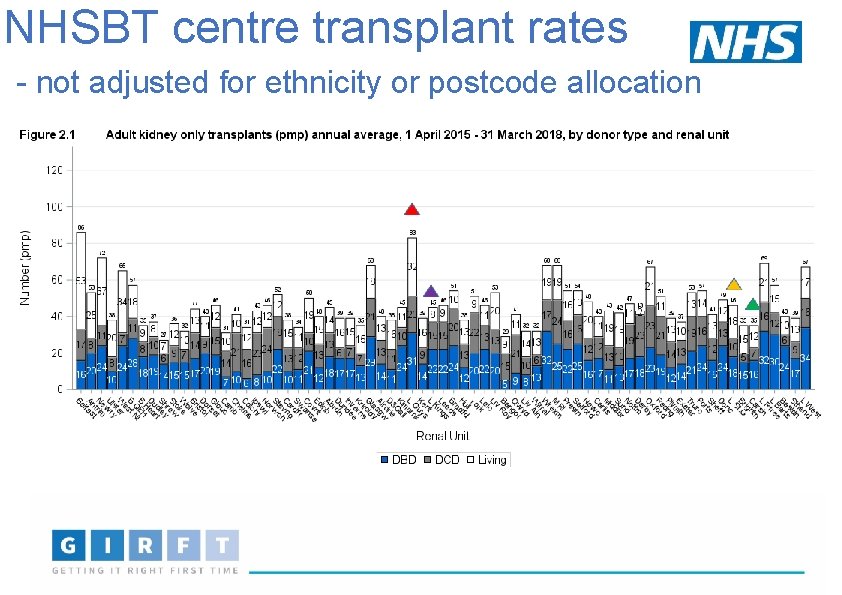
NHSBT centre transplant rates - not adjusted for ethnicity or postcode allocation
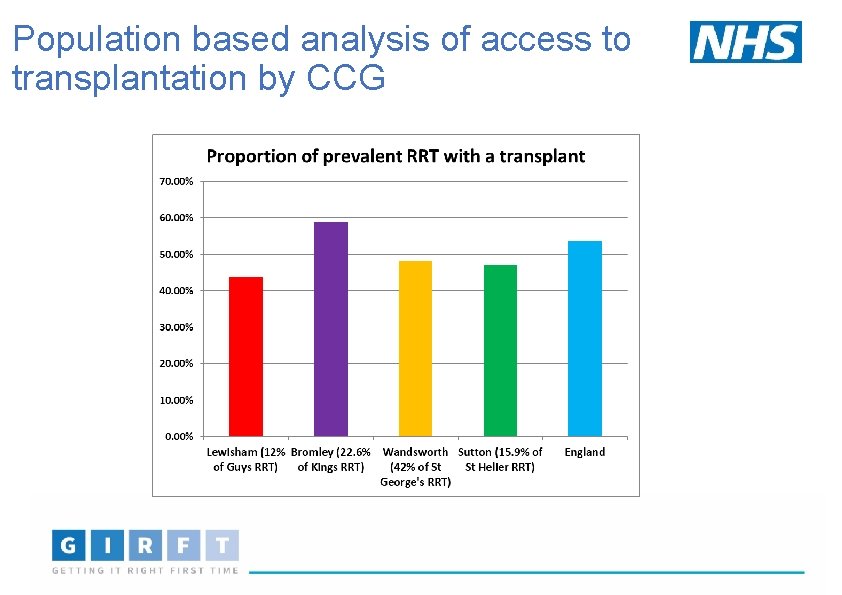
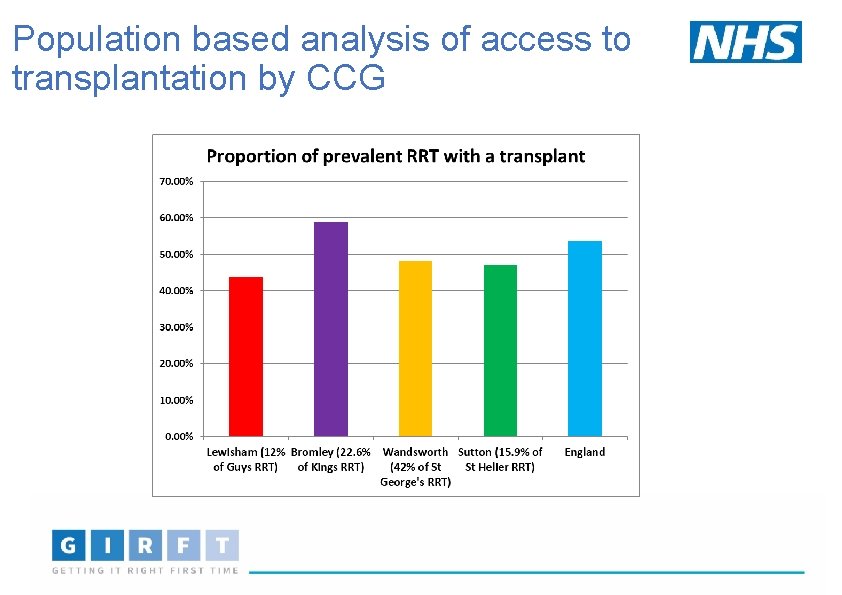
Population based analysis of access to transplantation by CCG
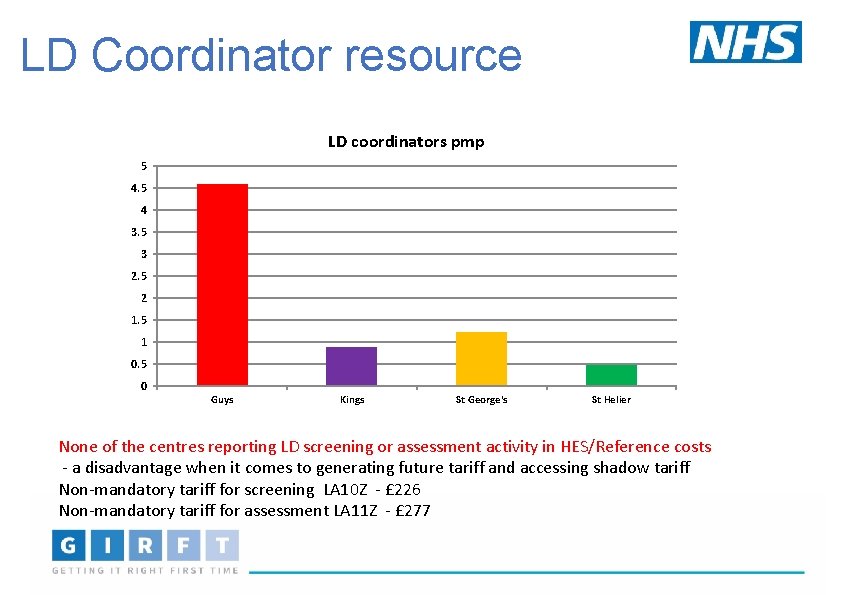
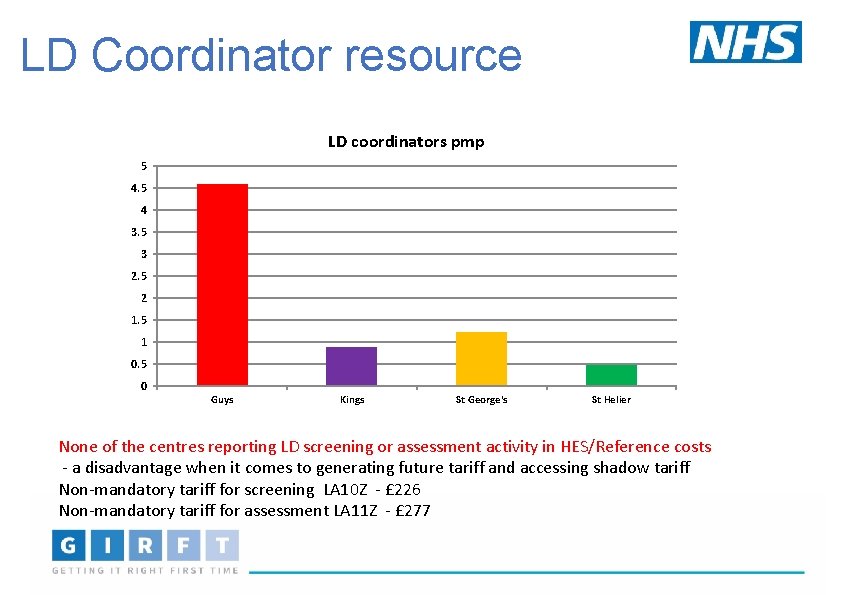
LD Coordinator resource LD coordinators pmp 5 4 3. 5 3 2. 5 2 1. 5 1 0. 5 0 Guys Kings St George's St Helier None of the centres reporting LD screening or assessment activity in HES/Reference costs - a disadvantage when it comes to generating future tariff and accessing shadow tariff Non-mandatory tariff for screening LA 10 Z - £ 226 Non-mandatory tariff for assessment LA 11 Z - £ 277
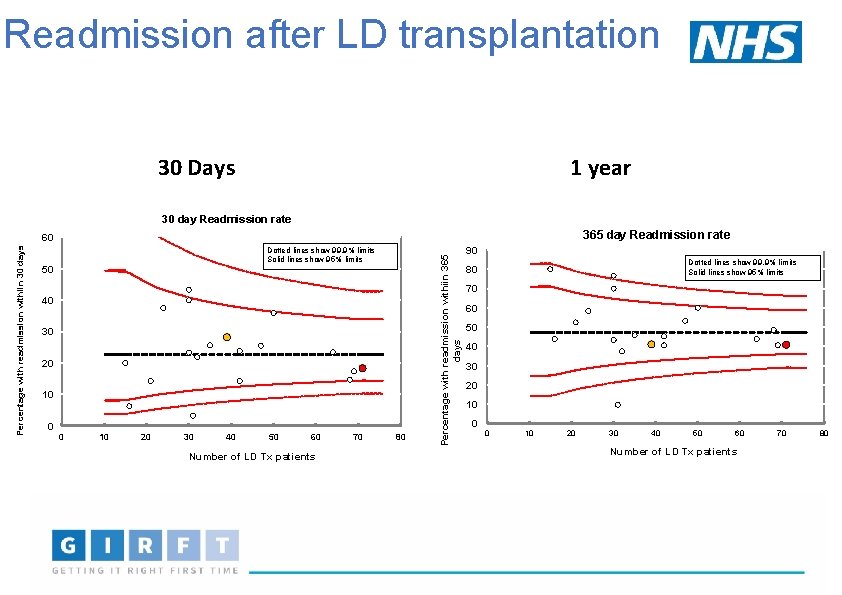
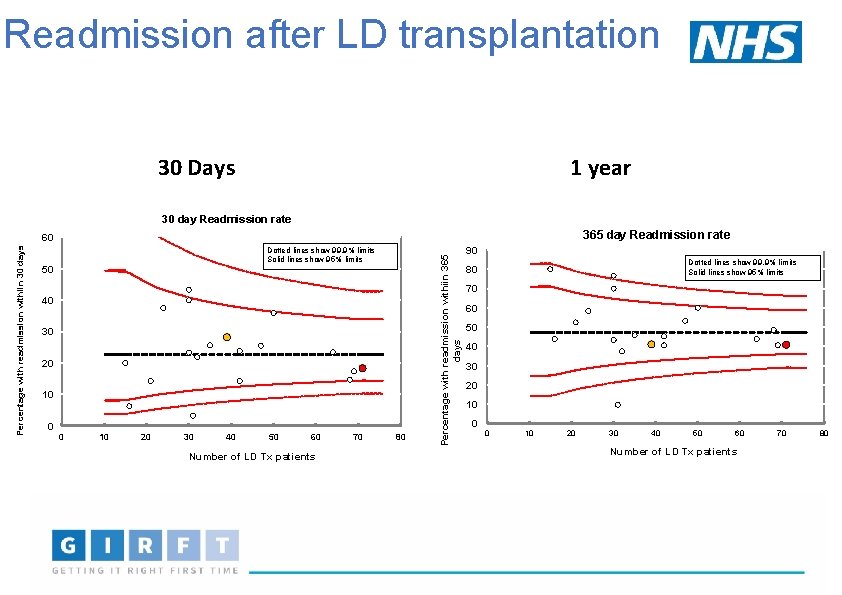
Readmission after LD transplantation 1 year 30 Days 30 day Readmission rate 365 day Readmission rate Dotted lines show 99. 9% limits Solid lines show 95% limits 50 40 30 20 10 0 0 10 20 30 40 50 60 Number of LD Tx patients 70 80 Percentage with readmission withiin 365 days Percentage with readmission withiin 30 days 60 90 Dotted lines show 99. 9% limits Solid lines show 95% limits 80 70 60 50 40 30 20 10 0 0 10 20 30 40 50 60 Number of LD Tx patients 70 80
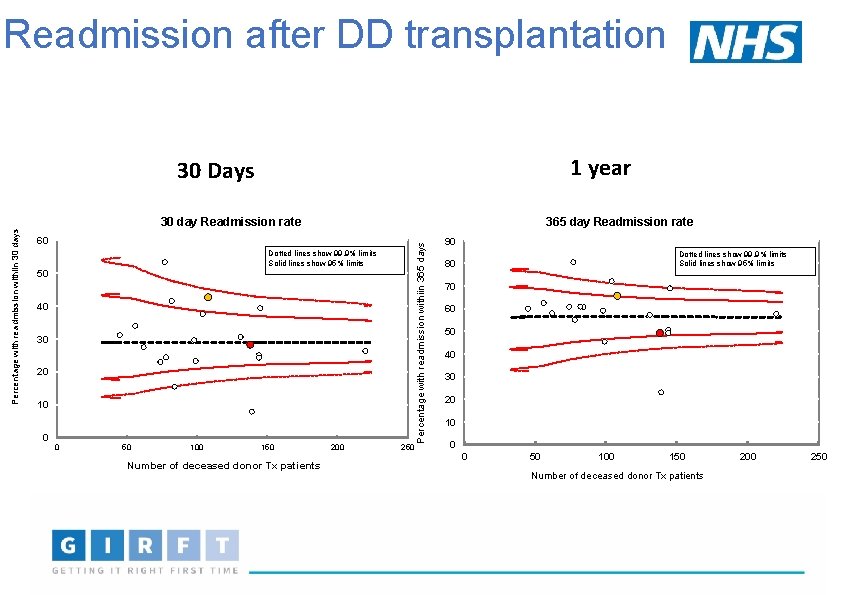
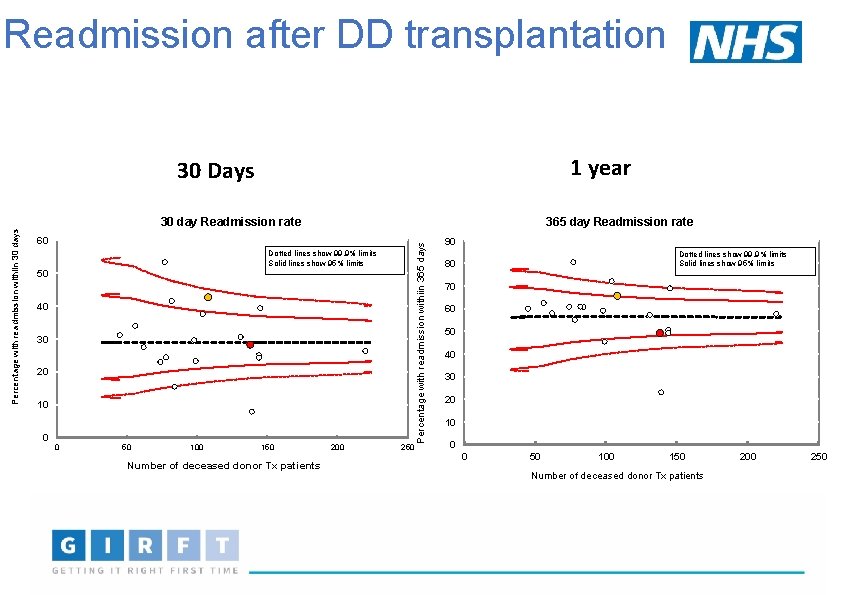
Readmission after DD transplantation 1 year 30 Days 365 day Readmission rate 60 Dotted lines show 99. 9% limits Solid lines show 95% limits 50 40 30 20 10 0 0 50 100 150 Number of deceased donor Tx patients 200 250 Percentage with readmission withiin 365 days Percentage with readmission withiin 30 days 30 day Readmission rate 90 Dotted lines show 99. 9% limits Solid lines show 95% limits 80 70 60 50 40 30 20 10 0 0 50 100 150 Number of deceased donor Tx patients 200 250
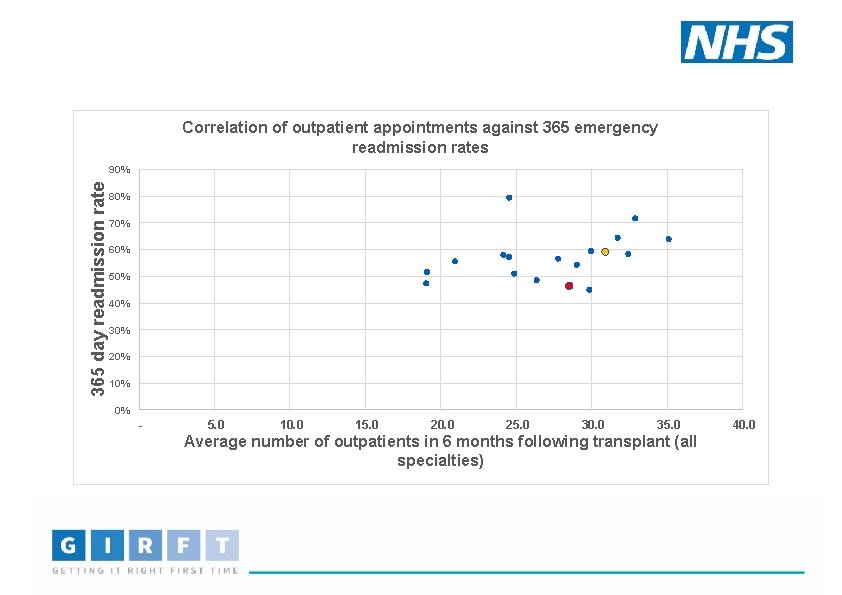
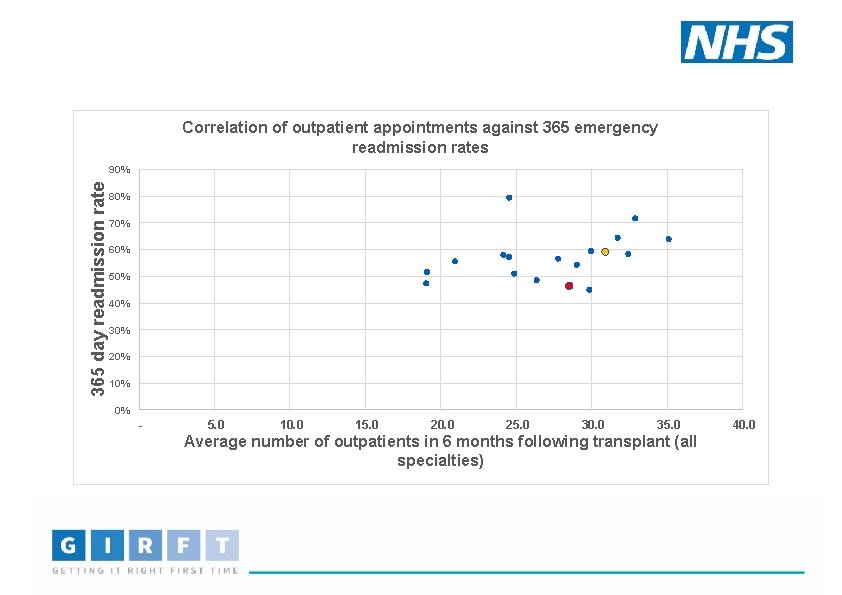
Correlation of outpatient appointments against 365 emergency readmission rates 365 day readmission rate 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% - 5. 0 10. 0 15. 0 20. 0 25. 0 30. 0 35. 0 Average number of outpatients in 6 months following transplant (all specialties) 40. 0
What next? • GIRFT data has set the scene • Variation • • Workforce On site access surgery and IR Infrastructure for PD Day case surgery • Evidence of improved equity in access to transplantation • Work in progress • Transplant First • Areas where a coordinated network approach could help • Making sure that patients have equal access to the resources within South London • May require • • Some changes in working practices Innovative models of care delivery for dialysis access
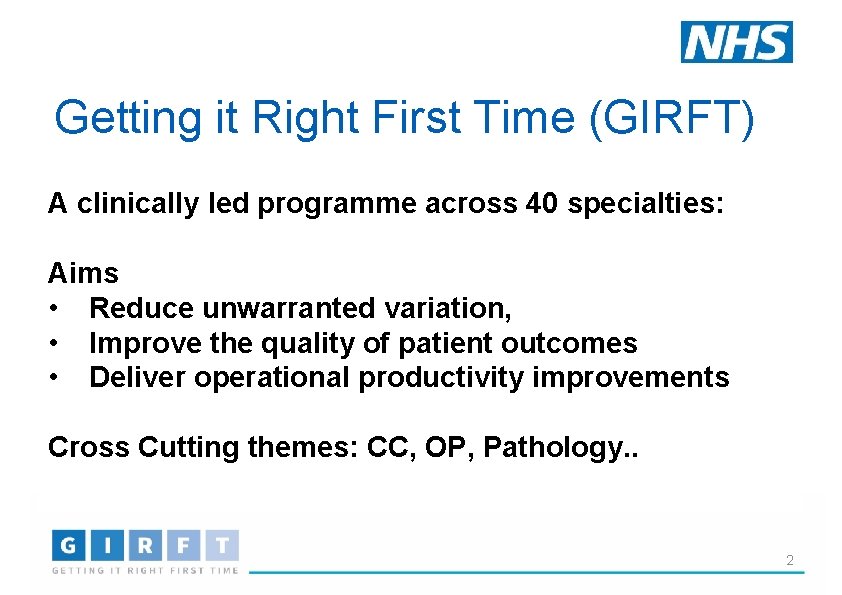
Renal Co-Leads and core project team 30
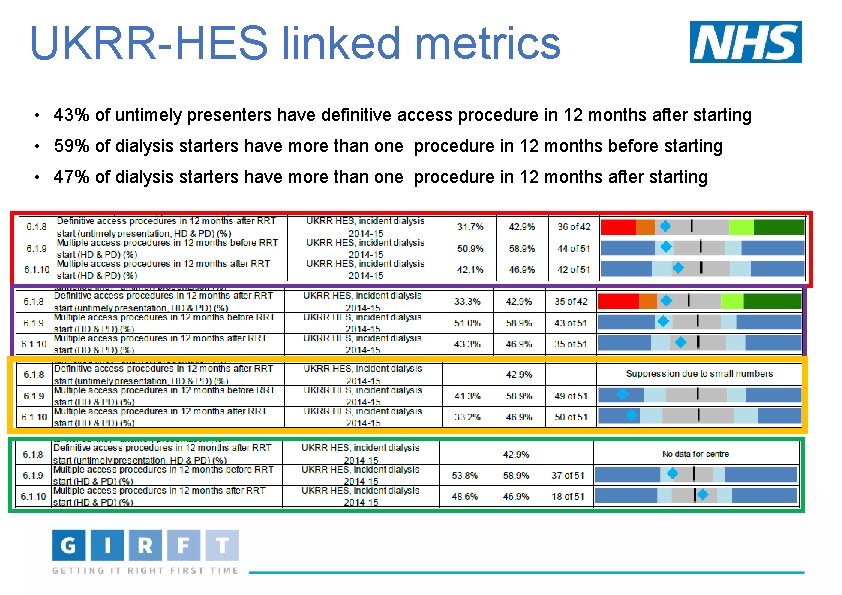
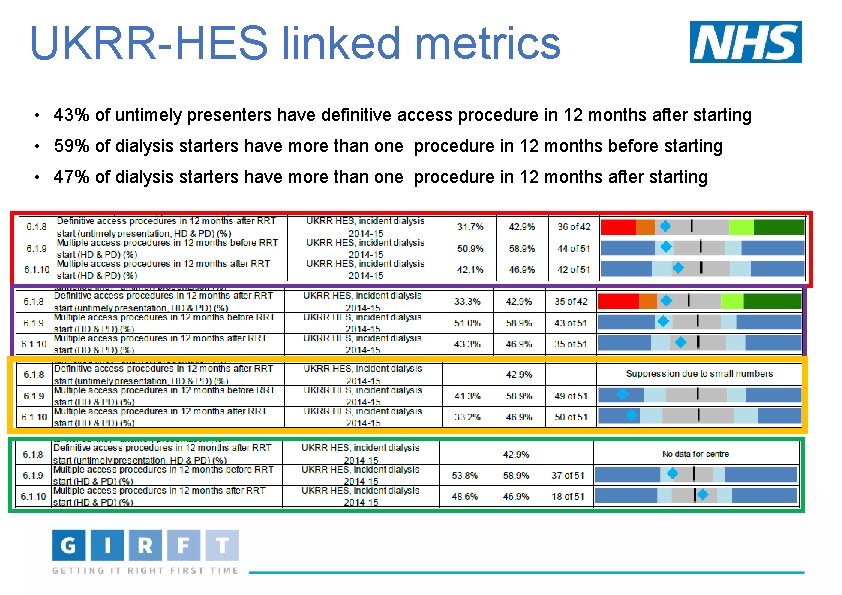
UKRR-HES linked metrics • 43% of untimely presenters have definitive access procedure in 12 months after starting • 59% of dialysis starters have more than one procedure in 12 months before starting • 47% of dialysis starters have more than one procedure in 12 months after starting
 Girft renal
Girft renal Res extra commercium
Res extra commercium Sindrome nefrótica
Sindrome nefrótica Quality assurance model in nursing management
Quality assurance model in nursing management Quality improvement vs quality assurance
Quality improvement vs quality assurance Renal corpuscle
Renal corpuscle South west london health and care partnership
South west london health and care partnership Orthopaedic services east london
Orthopaedic services east london Rape crisis south london
Rape crisis south london Ymca london south west
Ymca london south west South east london stp
South east london stp Quality improvement vs research
Quality improvement vs research Qsen patient-centered care examples
Qsen patient-centered care examples Quality improvement paradigm
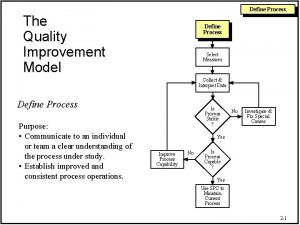
Quality improvement paradigm Define continuous quality improvement
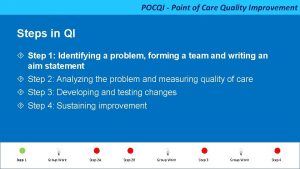
Define continuous quality improvement Point of care quality improvement
Point of care quality improvement Define continuous quality improvement
Define continuous quality improvement Efmd quality improvement system
Efmd quality improvement system Indiana perinatal quality improvement collaborative
Indiana perinatal quality improvement collaborative Continuous quality improvement program planning worksheet
Continuous quality improvement program planning worksheet Tea quality improvement
Tea quality improvement Xerox problem solving process
Xerox problem solving process Sus qi
Sus qi Cotinuous
Cotinuous Quality improvement
Quality improvement Juran 10 steps to quality improvement
Juran 10 steps to quality improvement Swot analysis quality improvement
Swot analysis quality improvement Malnutrition quality improvement initiative
Malnutrition quality improvement initiative Quality improvement
Quality improvement Data driven quality
Data driven quality Rapid cycle quality improvement
Rapid cycle quality improvement Crosby quality is free
Crosby quality is free