Quality Improvement Decision Support for Quality Improvement Lecture

- Slides: 22
Quality Improvement Decision Support for Quality Improvement Lecture b This material (Comp 12 Unit 5) was developed by Johns Hopkins University, funded by the Department of Health and Human Services, Office of the National Coordinator for Health Information Technology under Award Number IU 24 OC 000013. This material was updated in 2016 by Johns Hopkins University under Award Number 90 WT 0005. This work is licensed under the Creative Commons Attribution-Non. Commercial-Share. Alike 4. 0 International License. To view a copy of this license, visit http: //creativecommons. org/licenses/by-nc-sa/4. 0/
Decision Support for Quality Improvement Learning Objective — Lecture b • Analyze the benefits and shortfalls of alerts and clinical reminders. 2
Reminders and Alerts • “… the burden of reminders and alerts must not be too high … or alert fatigue may cause clinicians to override both important and unimportant alerts, in a manner that compromises the desired safety effect of integrating decision support into CPOE” (Van der Sijs, et al. , 2006). 3
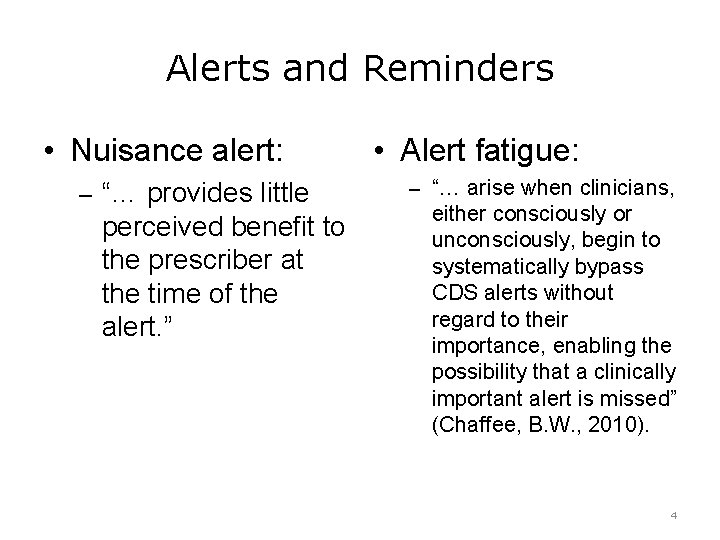
Alerts and Reminders • Nuisance alert: – “… provides little perceived benefit to the prescriber at the time of the alert. ” • Alert fatigue: – “… arise when clinicians, either consciously or unconsciously, begin to systematically bypass CDS alerts without regard to their importance, enabling the possibility that a clinically important alert is missed” (Chaffee, B. W. , 2010). 4
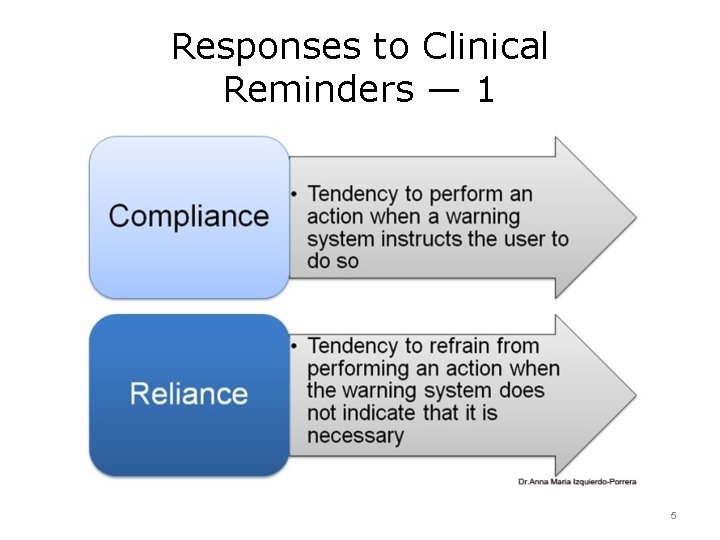
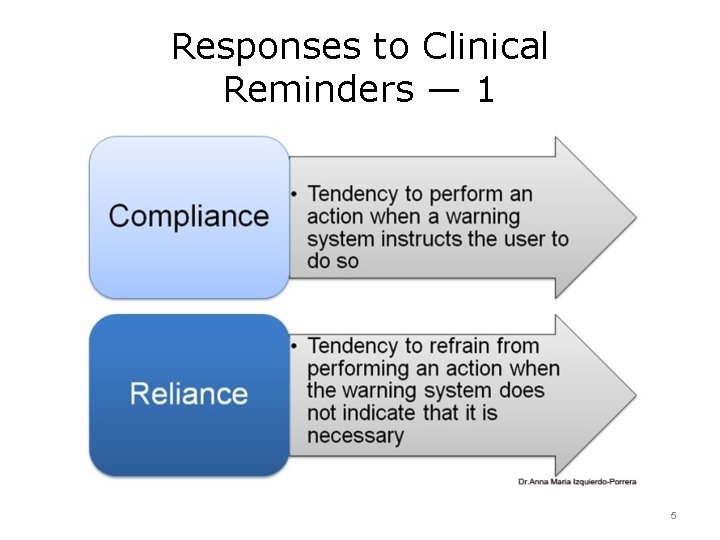
Responses to Clinical Reminders — 1 5
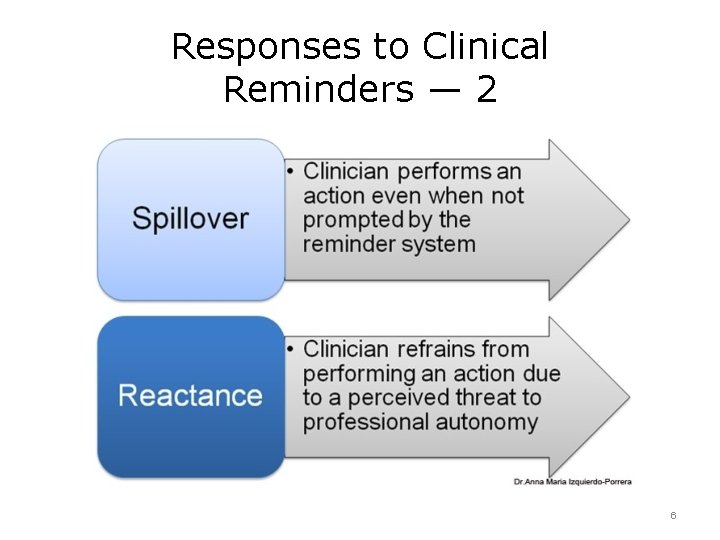
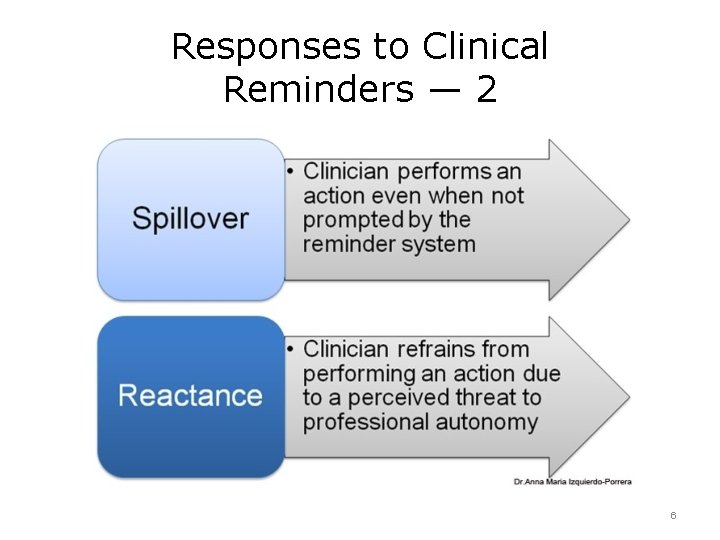
Responses to Clinical Reminders — 2 6
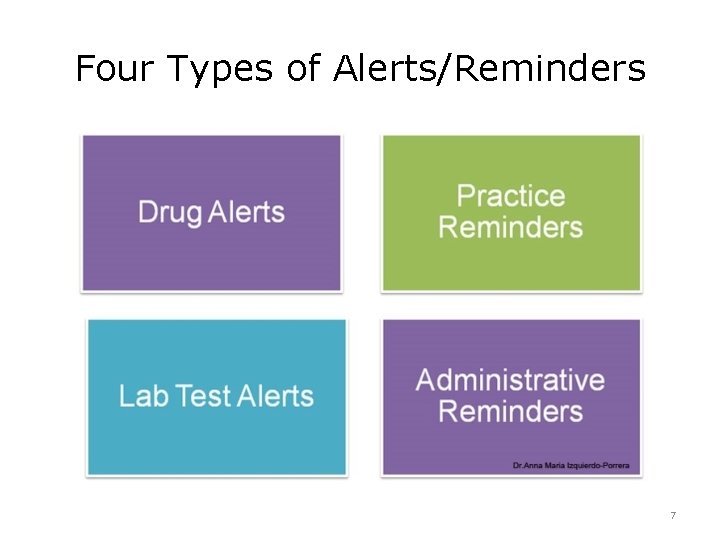
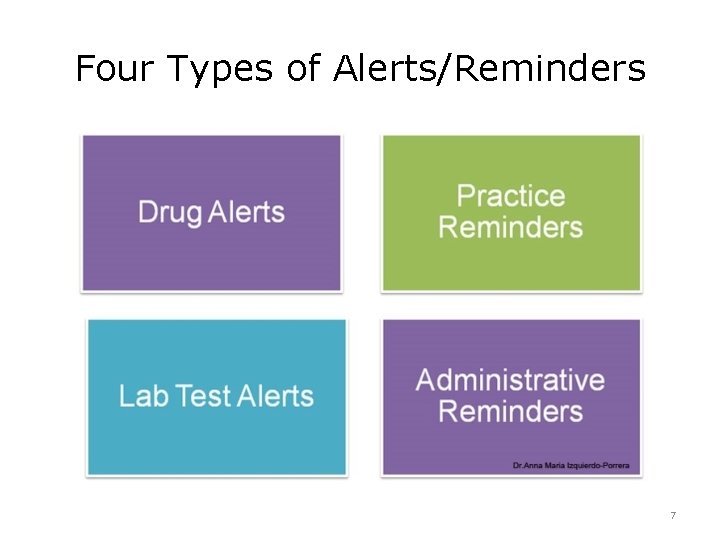
Four Types of Alerts/Reminders 7
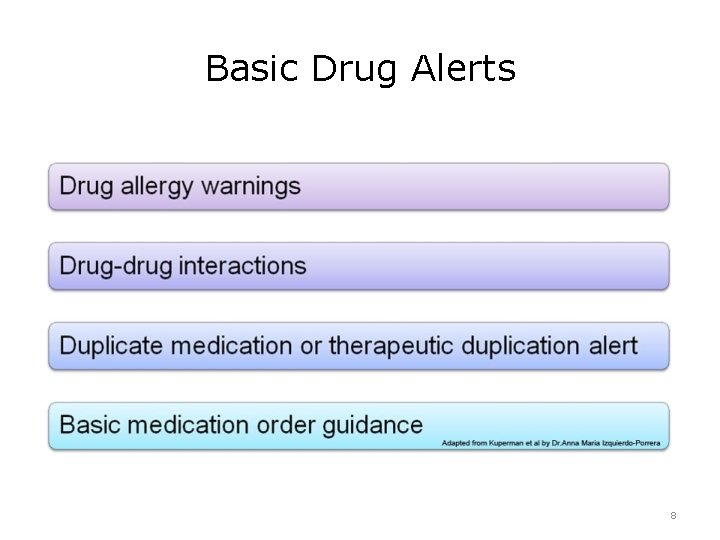
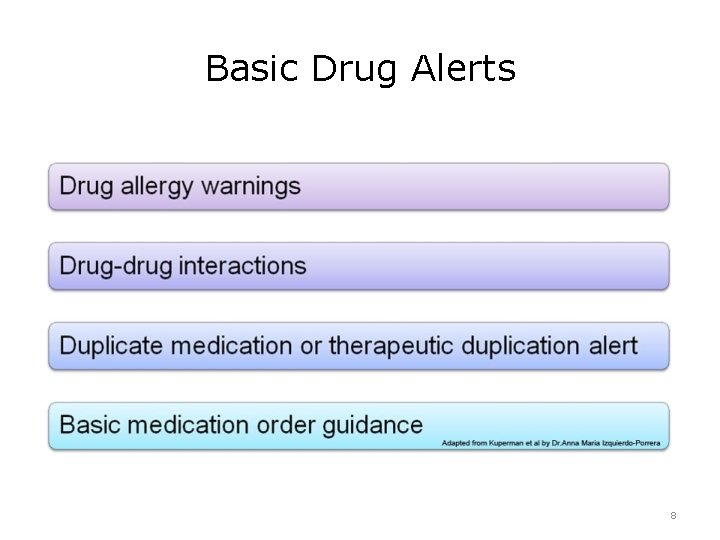
Basic Drug Alerts 8

Advanced Drug Alerts 9
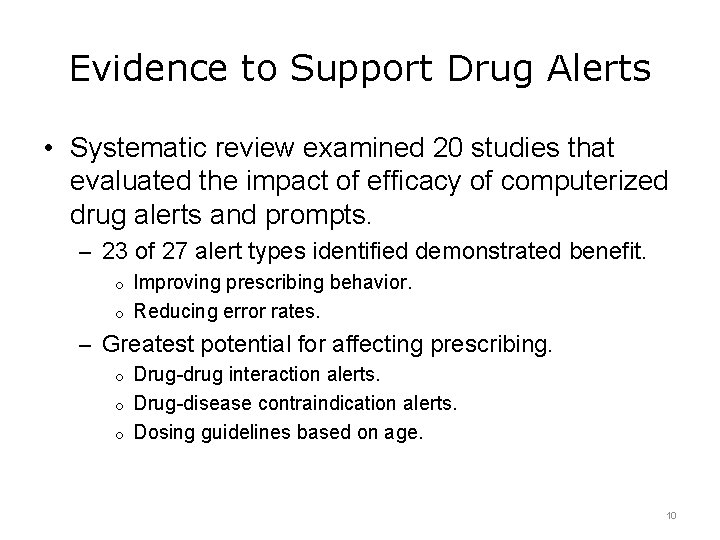
Evidence to Support Drug Alerts • Systematic review examined 20 studies that evaluated the impact of efficacy of computerized drug alerts and prompts. – 23 of 27 alert types identified demonstrated benefit. o Improving prescribing behavior. o Reducing error rates. – Greatest potential for affecting prescribing. o Drug-drug interaction alerts. o Drug-disease contraindication alerts. o Dosing guidelines based on age. 10
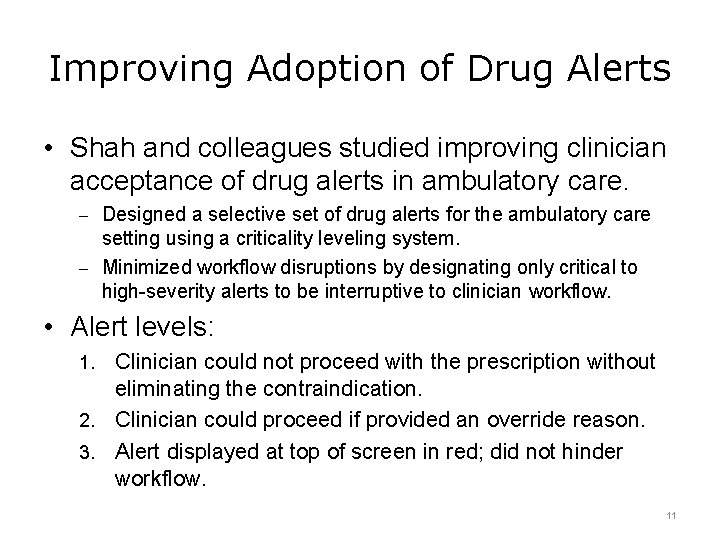
Improving Adoption of Drug Alerts • Shah and colleagues studied improving clinician acceptance of drug alerts in ambulatory care. – Designed a selective set of drug alerts for the ambulatory care setting using a criticality leveling system. – Minimized workflow disruptions by designating only critical to high-severity alerts to be interruptive to clinician workflow. • Alert levels: Clinician could not proceed with the prescription without eliminating the contraindication. 2. Clinician could proceed if provided an override reason. 3. Alert displayed at top of screen in red; did not hinder workflow. 1. 11
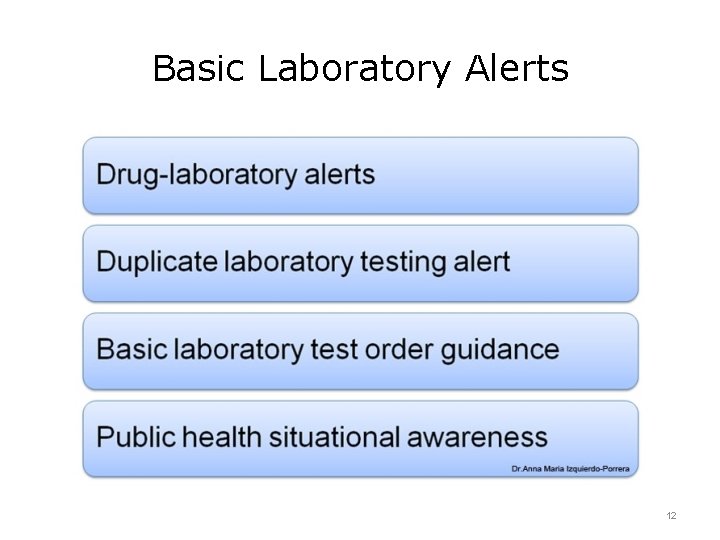
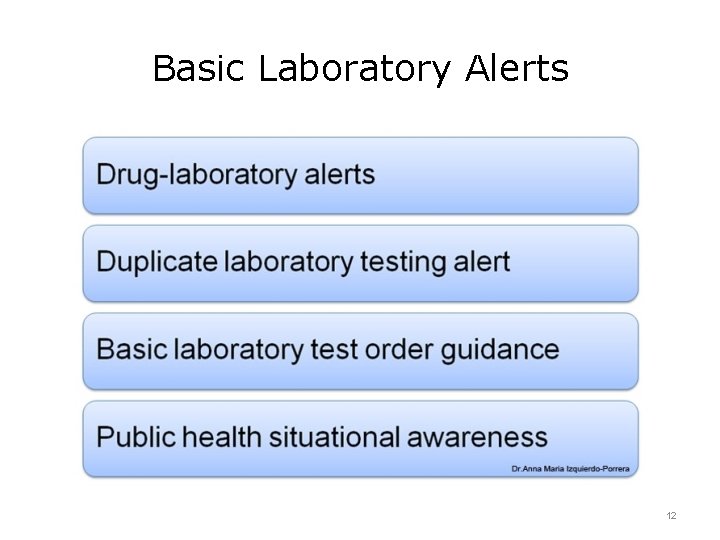
Basic Laboratory Alerts 12
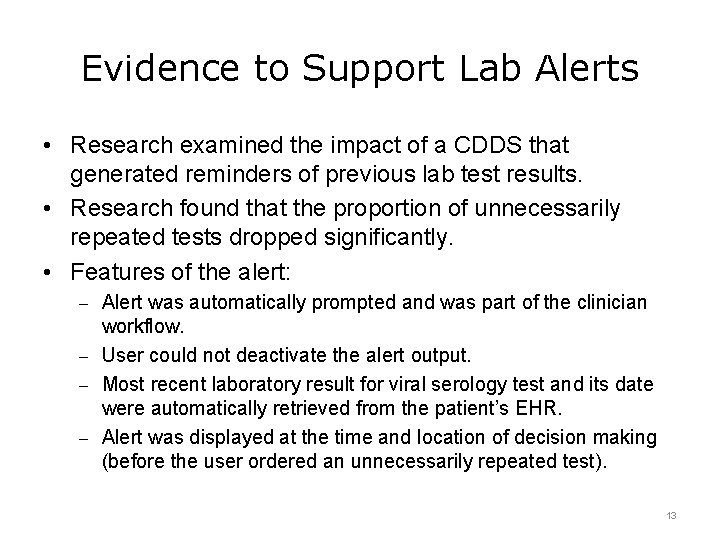
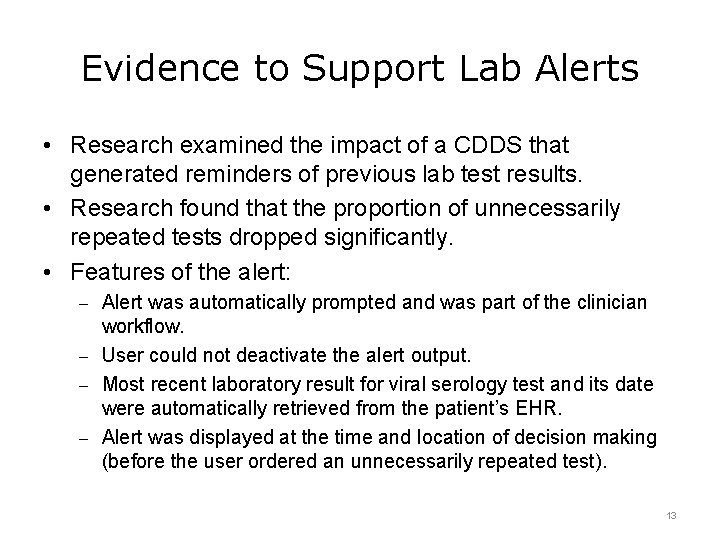
Evidence to Support Lab Alerts • Research examined the impact of a CDDS that generated reminders of previous lab test results. • Research found that the proportion of unnecessarily repeated tests dropped significantly. • Features of the alert: – Alert was automatically prompted and was part of the clinician workflow. – User could not deactivate the alert output. – Most recent laboratory result for viral serology test and its date were automatically retrieved from the patient’s EHR. – Alert was displayed at the time and location of decision making (before the user ordered an unnecessarily repeated test). 13
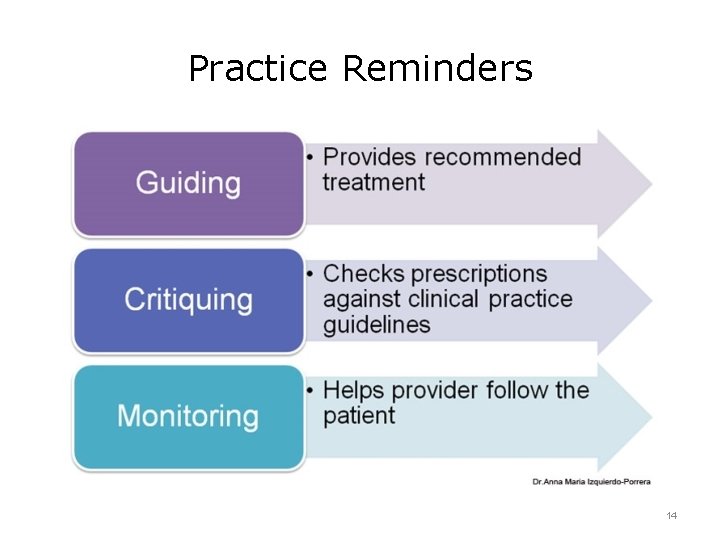
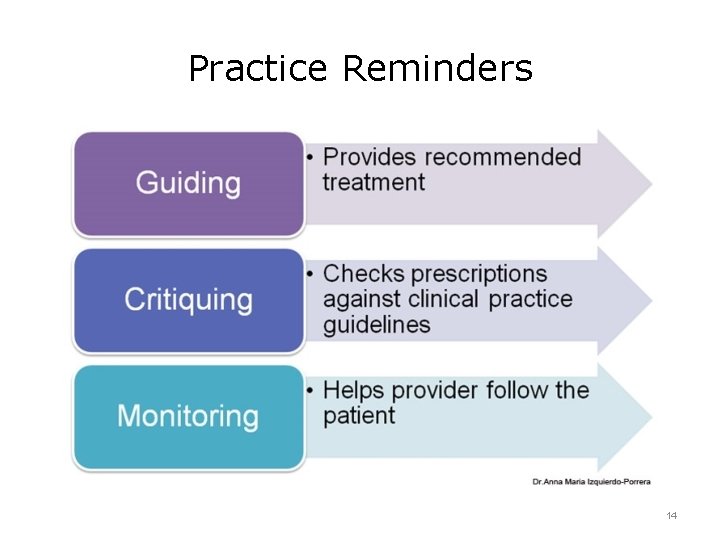
Practice Reminders 14
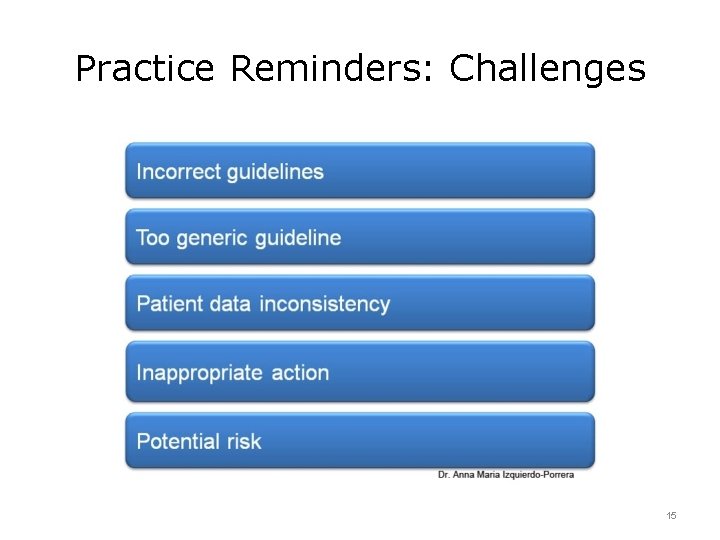
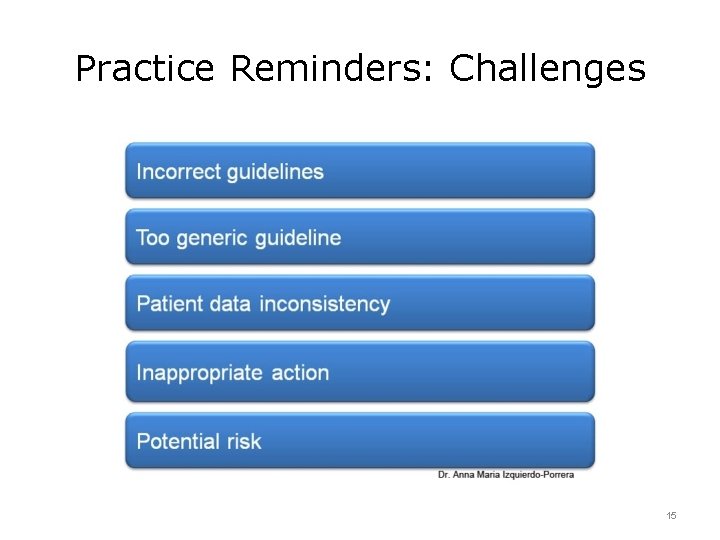
Practice Reminders: Challenges 15
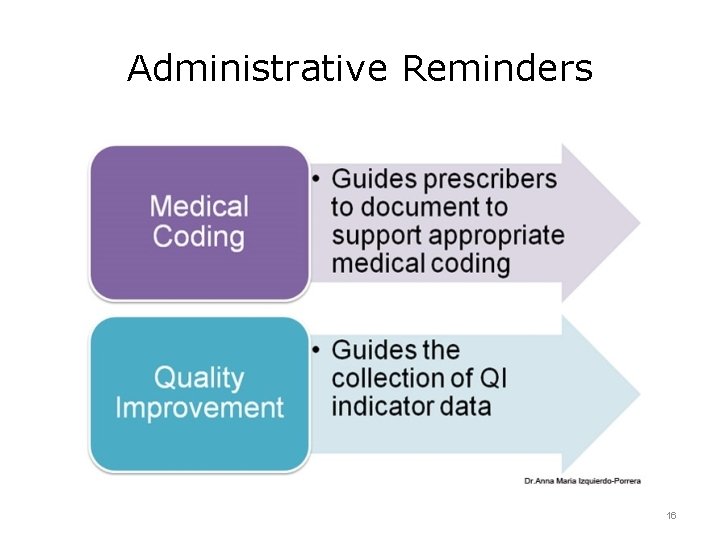
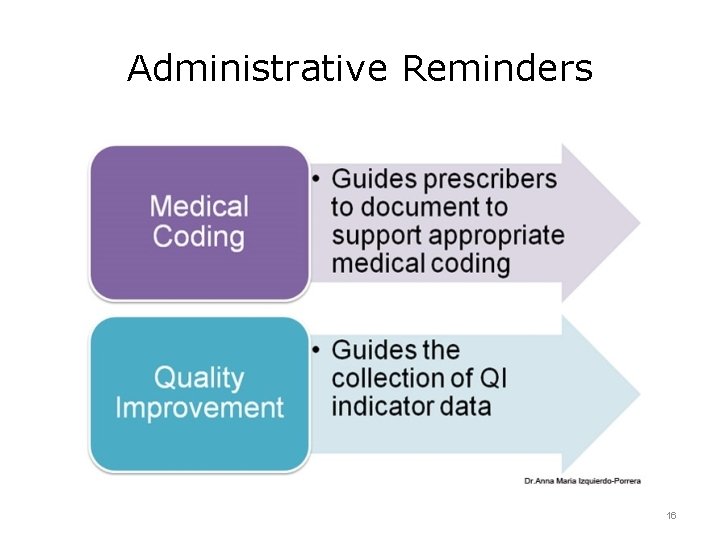
Administrative Reminders 16
Decision Support for Quality Improvement Summary — Lecture b • Alerts/reminders have the potential to improve patient safety. • Alert types include drug and lab test alerts, practice reminders, and administrative reminders. • Nuisance alerts provide little perceived benefit to the prescriber at the time of the alert, causing clinician frustration and alert fatigue. • Successful alerts are specific, sensitive, clear, and concise, and support clinical workflow, allowing for safe, efficient responses. 17
Decision Support for Quality Improvement References — Lecture b — 1 References Chaffee, B. W. (2010). Future of clinical decision support in computerized prescriber order entry. American Journal of Health System Pharmacists. 67: 932– 935. De Clercq, P. A. , Blom, J. A. , Hasman, A. , Korsten, H. H. M. (1999). A strategy for developing practice guidelines for the ICU using automated knowledge acquisition techniques. Journal of Clinical Monitoring. 15: 109– 117. Kuperman, G. J. , Bobb, A. , Payne, T. H. , et al. (2007). Medication-related clinical decisionsupport in computerized provider order entry systems: a review. Journal of the American Medical Informatics Association. 14(1): 29– 40. Lami, J. B. , Ebrahiminia , V. , Riou C. , et al. (2010). How to translate therapeutic recommendations in clinical practice guidelines into rules for critiquing physician prescriptions. Methods and application to five guidelines. BMC Medical Informatics and Decision Making. 10: 31. Metzger, J. , Macdonald, K. (2002). Clinical decision support for the independent physician practice. Health Reports, California Health Care Foundation. Nies, J. , Colombet, I. , Zapleta, l. E. , et al. (2010). Effects of automated alerts on unnecessarily repeated serology tests in cardiovascular surgery department: a time series analysis. BMC Health Services Research. 10: 70. 18
Decision Support for Quality Improvement References — Lecture b — 2 References Porter, S. (2010). Primary care associations release joint principles for accountable care organizations. Available from: http: //www. aafp. org/online/en/home/publications/news-now/professionalissues/20101118 acojointprinciples. html Schedlbauer, A. , Prasad, V, Mulvaney, C, et al. (2009). What evidence supports the use of computerized alerts and prompts to improve clinicians’ prescribing behavior? Journal of the American Medical Informatics Association. 16(4): 531– 8. Shah, N. R. , Seger, A. C. , Seger, D. L. , et al. (2006). Improving Acceptance of Computerized Prescribing Alerts in Ambulatory Care. Journal of the American Medical Informatics Association 2006; 13(1): 5– 11. Teich, J. M. , Merchia, P. R. , Schmiz, J. L. , et al. (2000). Effects of computerized physician order entry on prescribing practices. Arch Intern Med. 160 (18): 2471– 7. Van Der Sijs, H. , Aarts, J. , Vulto, A. , Berg, M. (2006). Overriding of drug safety alerts in computerized physician order entry. Journal of the American Medical Informatics Association. 13(2), 138– 147. Vashitz, G. , Meyer, J. , Parmet, Y. , Peleq, R. , et al. (2009). Defining and measuring physicians' responses to clinical reminders. Journal of Biomedical Informatics. 42(2): 317– 26. 19
Decision Support for Quality Improvement References — Lecture b — 3 References Zanetti, G. , Flanagan, H. L. Cohn, L. H. et al. (2003). Improvement of intraoperative antibiotic prophylaxis in prolonged cardiac surgery by automated alerts in the operating room, Infect Control Hosp Epidemiol 24(1): 13– 16. Images Slide 5: Responses to Clinical Reminders — 1. Adapted by Dr. Anna Maria Izquierdo. Porrera from Vashitz, G. , Meyer J, Parmet, Y, et al. (2009). Defining and measuring physicians’ responses to clinical reminders. Journal of Biomedical Informatics 42(2): 317 -26. Epub 2008 Oct 26. Slide 6: Responses to Clinical Reminders — 2. Adapted by Dr. Anna Maria Izquierdo. Porrera from Vashitz, G. , Meyer J, Parmet, Y, et al. (2009). Defining and measuring physicians’ responses to clinical reminders. Journal of Biomedical Informatics 42(2): 317 -26. Epub 2008 Oct 26. Slide 7: Four Types of Alerts/Reminders. Dr. Anna Maria Izquierdo-Porrera. 20
Decision Support for Quality Improvement References — Lecture b — 4 Images Slide 8: Basic Drug Alerts. Adapted by Dr. Anna Maria Izquierdo-Porrera from Kuperman, G. J. , Bobb, A. , Payne, T. H. , et al. (2007). Medication-related clinical decision-support in computerized provider order entry systems: a review. Journal of the American Medical Informatics Association 14(1): 29 -40. Slide 9: Advanced Drug Alerts. Dr. Anna Maria Izquierdo-Porrera. Slide 12: Basic Laboratory Alerts. Dr. Anna Maria Izquierdo-Porrera. Slide 14: Practice Reminders. Adapted by Dr. Anna Maria Izquierdo-Porrera from Lami, J. B. , Ebrahiminia, V. , Riou, C. , et al. (2010). How to translate therapeutic recommendations in clinical practice guidelines into rules for critiquing physician prescriptions. Methods and application to five guidelines. BMC Medical Informatics and Decision Making. 10: 31. Slide 15: Practice Reminders: Challenges. Dr. Anna Maria Izquierdo-Porrera. Slide 16: Administrative Reminders. Dr. Anna Maria Izquierdo-Porrera. 21
Quality Improvement Decision Support for Quality Improvement This material (Comp 12 Unit 5) was developed by Johns Hopkins University, funded by the Department of Health and Human Services, Office of the National Coordinator for Health Information Technology under Award Number IU 24 OC 000013. This material was updated in 2016 by Johns Hopkins University under Award Number 90 WT 0005. 22