Sustainability in Quality Improvement Sus QI training materials

Sustainability in Quality Improvement (Sus. QI) training materials, developed by the Centre for Sustainable Healthcare with grant funding from North Bristol NHS Trust. QUALITY IMPROVEMENT: CREATIVELY DESIGNING SUSTAINABLE SERVICES RCOT Annual Conference 08. 06. 2017 Ben Whittaker (Occupational Therapy Programme Lead, CSH) Camilla Cox (Occupational Therapist, Eating Disorders Service, BEHMHT) CENTRE for SUSTAINABLE HEALTHCARE
AIMS 1. Recognise sustainability as a domain of quality in healthcare and discuss its relationship to other domains. 2. Review the environmental, social and economic inputs to a given health system, and identify relevant carbon hotspots. 3. Apply the principles of sustainable clinical practice in the design of a QI intervention. 4. Consider ways of evaluating environmental, social and economic impacts. CENTRE for SUSTAINABLE HEALTHCARE
WHAT IS QUALITY IMPROVEMENT? “Designing and redesigning work processes and systems that deliver health care with better outcomes and lower cost, wherever this can be achieved. ” The Kings Fund (2016) WFOT Quality Indicators project – developing set of indicators for OTs CENTRE for SUSTAINABLE HEALTHCARE
Turn to the person next to you and say: • Hello • Something about how you understand quality improvement and quality indicators are being used within your service or setting. CENTRE for SUSTAINABLE HEALTHCARE
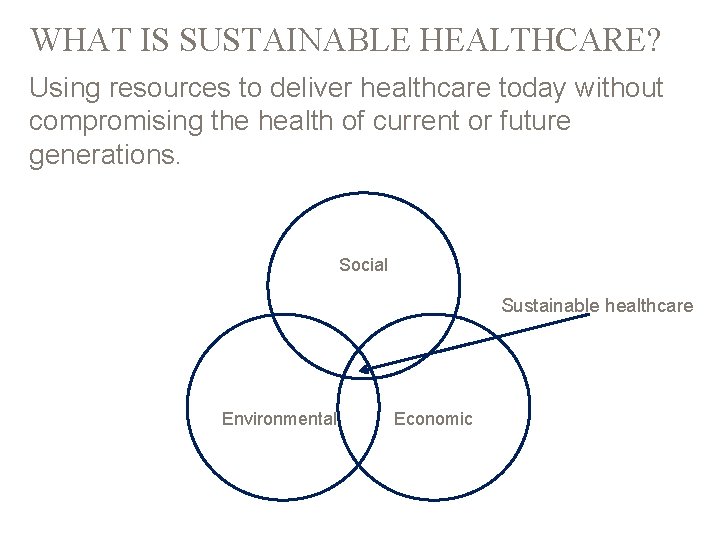
WHAT IS SUSTAINABLE HEALTHCARE? Using resources to deliver healthcare today without compromising the health of current or future generations. Social Sustainable healthcare Environmental Economic

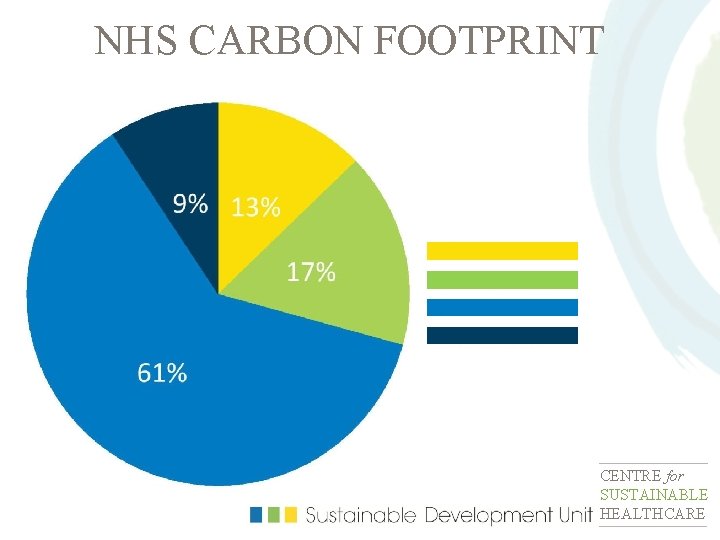
NHS CARBON FOOTPRINT CENTRE for SUSTAINABLE HEALTHCARE
Clinical Estates CENTRE for SUSTAINABLE HEALTHCARE

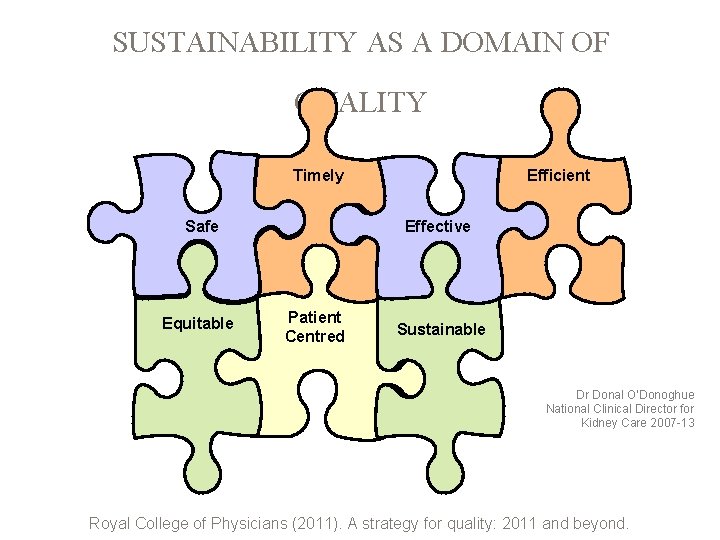
SUSTAINABILITY AS A DOMAIN OF QUALITY Timely Safe Equitable Efficient Effective Patient Centred Sustainable Dr Donal O’Donoghue National Clinical Director for Kidney Care 2007 -13 Royal College of Physicians (2011). A strategy for quality: 2011 and beyond.
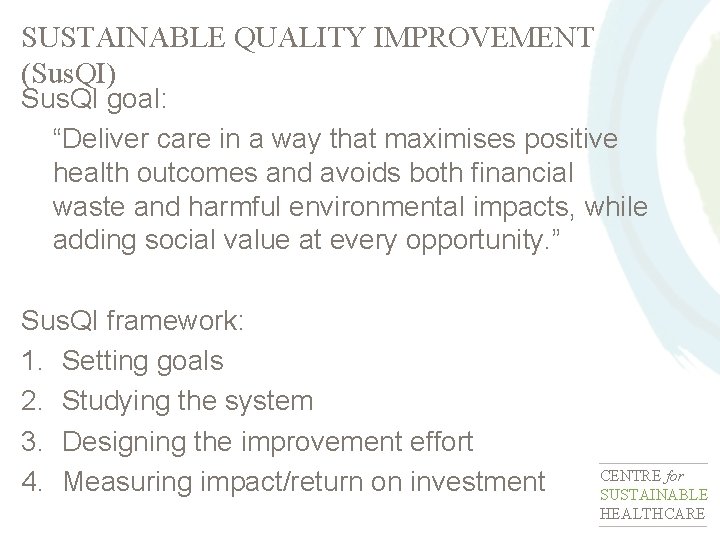
SUSTAINABLE QUALITY IMPROVEMENT (Sus. QI) Sus. QI goal: “Deliver care in a way that maximises positive health outcomes and avoids both financial waste and harmful environmental impacts, while adding social value at every opportunity. ” Sus. QI framework: 1. Setting goals 2. Studying the system 3. Designing the improvement effort 4. Measuring impact/return on investment CENTRE for SUSTAINABLE HEALTHCARE
1. SETTING QI GOALS Including sustainability within your project aims (how will this affect engagement with colleagues and wider stakeholders? ) CENTRE for SUSTAINABLE HEALTHCARE
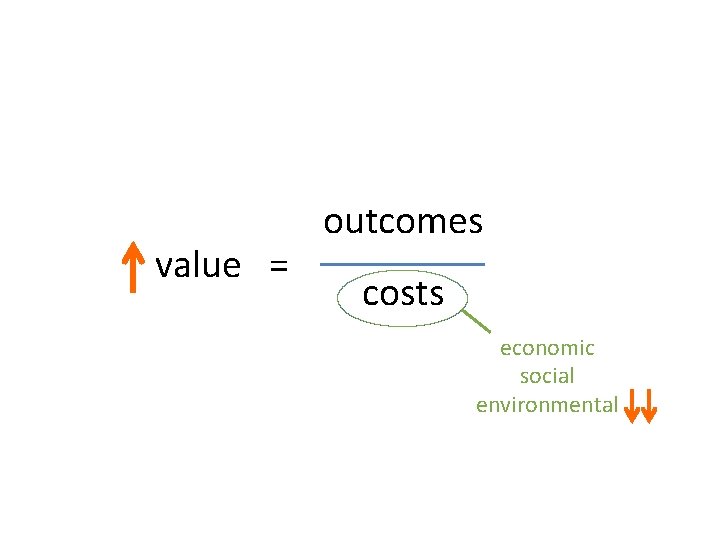
value = outcomes costs economic social environmental
2. STUDYING THE SYSTEM Understanding social and environmental resource use and impacts CENTRE for SUSTAINABLE HEALTHCARE
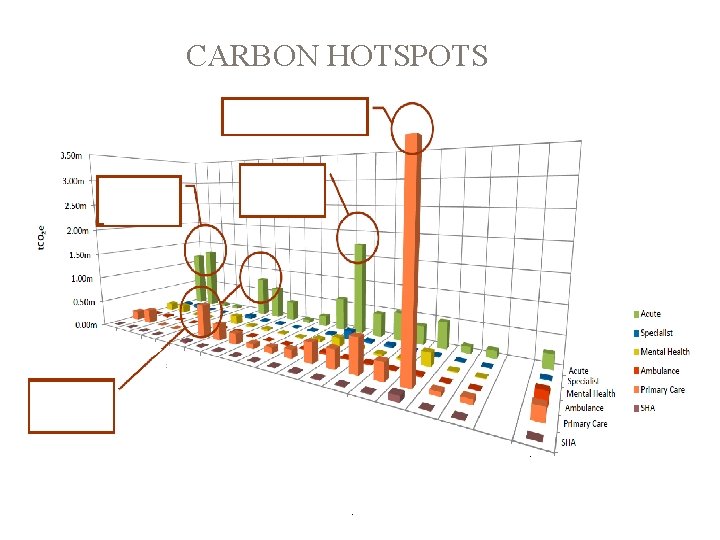
CARBON HOTSPOTS
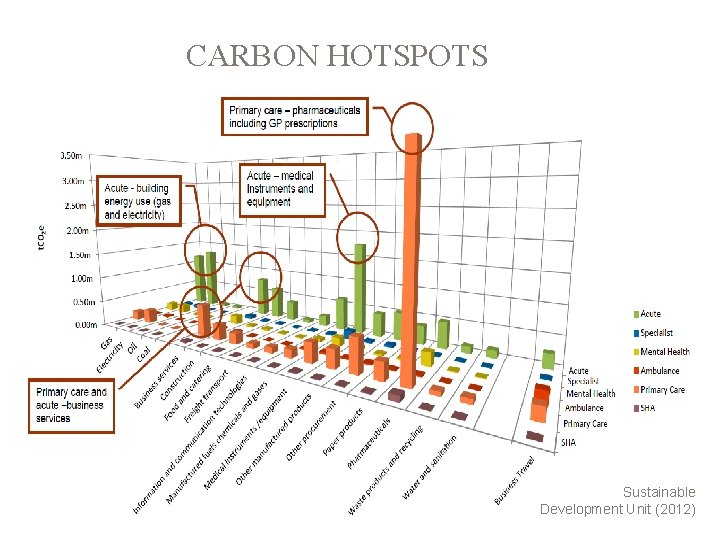
CARBON HOTSPOTS Sustainable Development Unit (2012)

SOCIAL IMPACTS… ON WHOM? �� Patient �� Staff �� Carers �� Dependants �� Local community �� Distant communities (e. g. supply chain workers) CENTRE for SUSTAINABLE HEALTHCARE
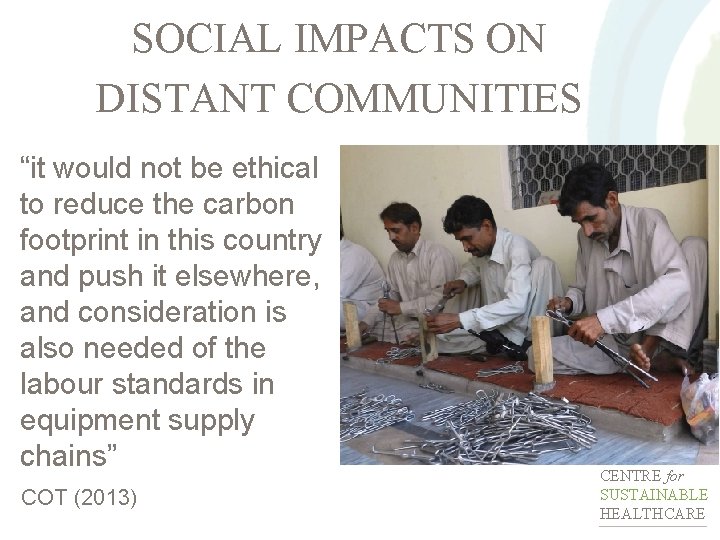
SOCIAL IMPACTS ON DISTANT COMMUNITIES “it would not be ethical to reduce the carbon footprint in this country and push it elsewhere, and consideration is also needed of the labour standards in equipment supply chains” COT (2013) CENTRE for SUSTAINABLE HEALTHCARE
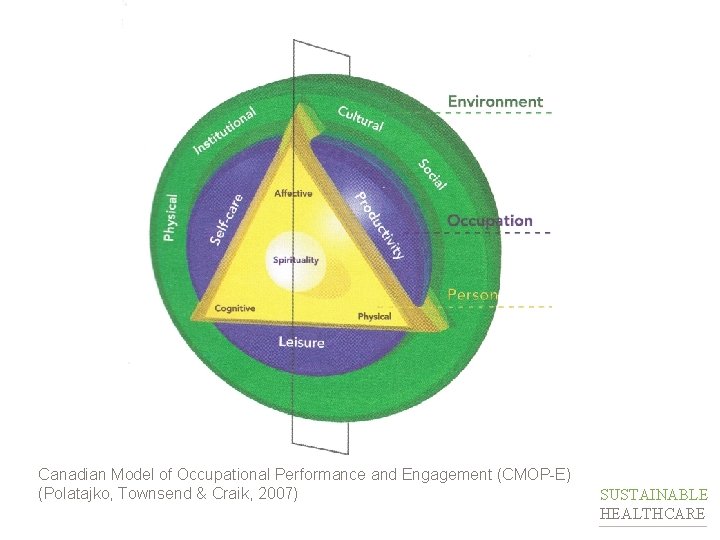
Canadian Model of Occupational Performance and Engagement (CMOP-E) (Polatajko, Townsend & Craik, 2007) CENTRE for SUSTAINABLE HEALTHCARE
3. DESIGNING YOUR QI INTERVENTION Applying the principles of sustainable clinical practice CENTRE for SUSTAINABLE HEALTHCARE
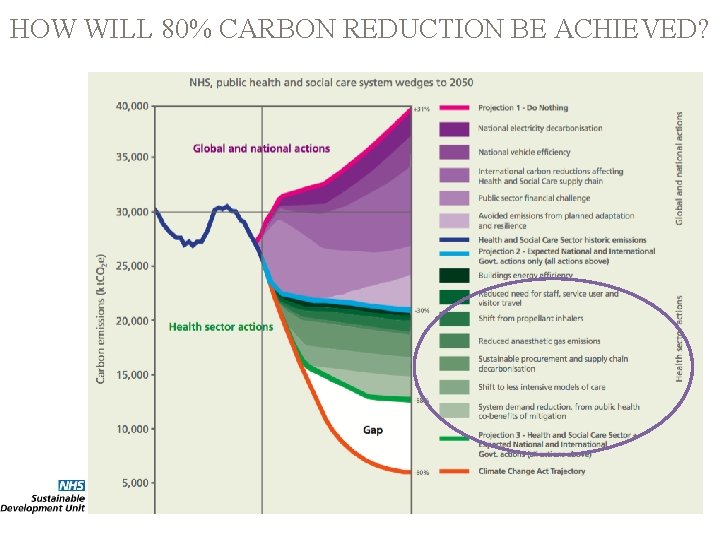
HOW WILL 80% CARBON REDUCTION BE ACHIEVED?
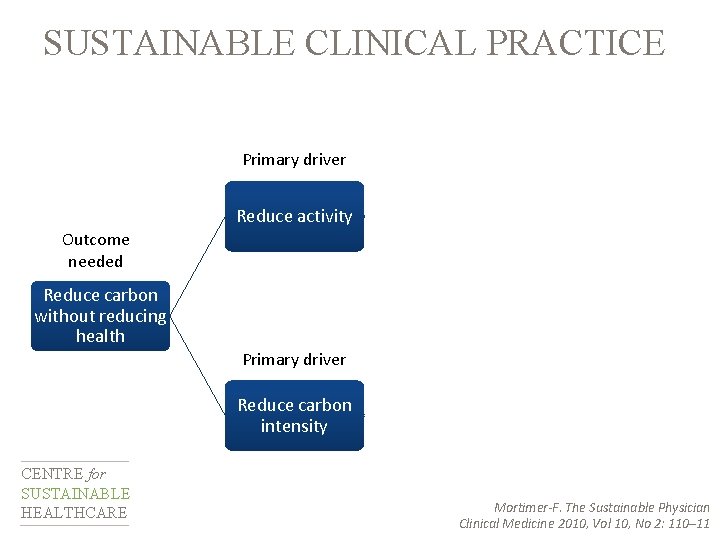
SUSTAINABLE CLINICAL PRACTICE Secondary drivers Prevention Primary driver Reduce activity Self care Outcome needed Reduce carbon without reducing health Lean pathways Primary driver Reduce carbon intensity CENTRE for SUSTAINABLE HEALTHCARE Low carbon alternatives Sustainable estates Mortimer-F. The Sustainable Physician Clinical Medicine 2010, Vol 10, No 2: 110– 11
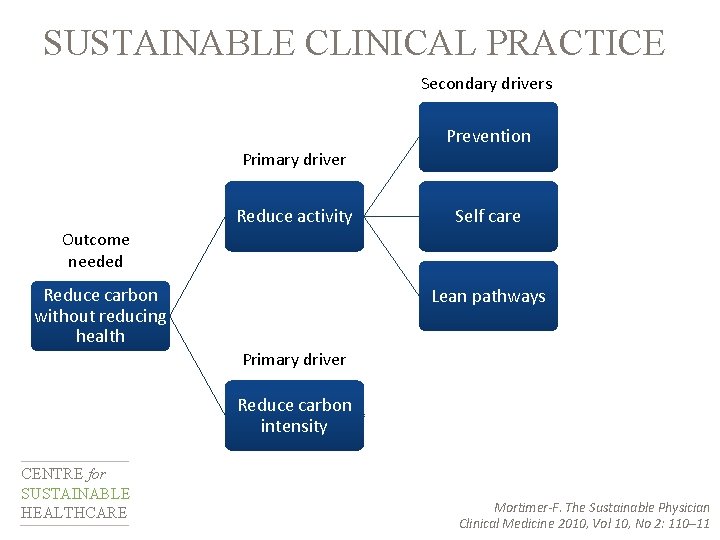
SUSTAINABLE CLINICAL PRACTICE Secondary drivers Prevention Primary driver Reduce activity Self care Outcome needed Reduce carbon without reducing health Lean pathways Primary driver Reduce carbon intensity CENTRE for SUSTAINABLE HEALTHCARE Low carbon alternatives Sustainable estates Mortimer-F. The Sustainable Physician Clinical Medicine 2010, Vol 10, No 2: 110– 11

SUSTAINABLE CLINICAL PRACTICE Secondary drivers Prevention Primary driver Reduce activity Self care Outcome needed Reduce carbon without reducing health Lean pathways Primary driver Reduce carbon intensity CENTRE for SUSTAINABLE HEALTHCARE Sustainable clinical practice Low carbon alternatives Sustainable estates Infrastructure & process Mortimer-F. The Sustainable Physician Clinical Medicine 2010, Vol 10, No 2: 110– 11
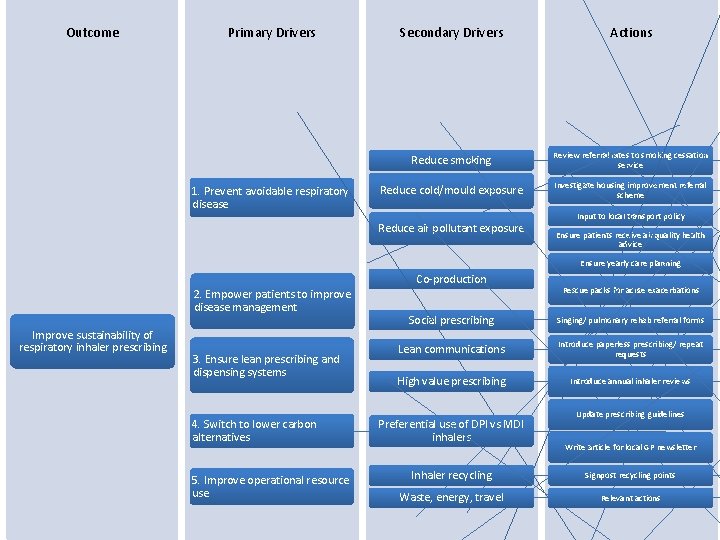
Outcome Primary Drivers 1. Prevent avoidable respiratory disease Secondary Drivers Actions Reduce smoking Review referral rates to smoking cessation service Reduce cold/mould exposure Investigate housing improvement referral scheme Reduce air pollutant exposure Input to local transport policy Ensure patients receive air quality health advice Ensure yearly care planning Co-production 2. Empower patients to improve disease management Improve sustainability of respiratory inhaler prescribing 3. Ensure lean prescribing and dispensing systems 4. Switch to lower carbon alternatives 5. Improve operational resource use Rescue packs for acute exacerbations Social prescribing Singing/ pulmonary rehab referral forms Lean communications Introduce paperless prescribing/ repeat requests High value prescribing Introduce annual inhaler reviews Preferential use of DPI vs MDI inhalers Update prescribing guidelines Write article for local GP newsletter Inhaler recycling Signpost recycling points Waste, energy, travel Relevant actions
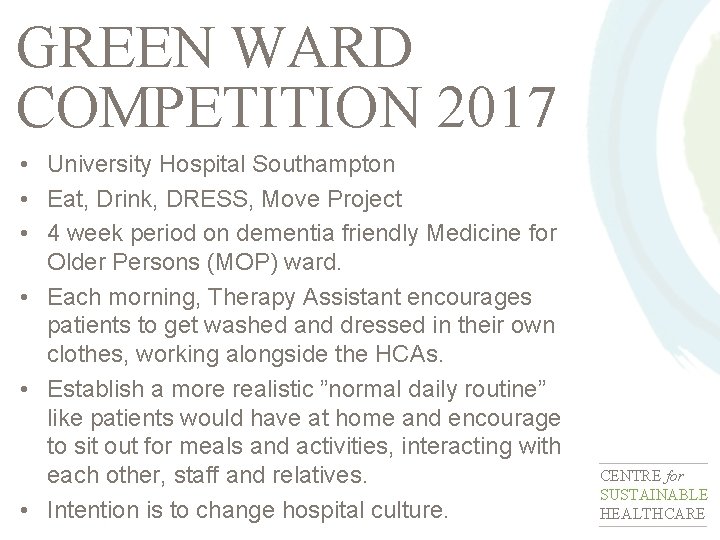
GREEN WARD COMPETITION 2017 • University Hospital Southampton • Eat, Drink, DRESS, Move Project • 4 week period on dementia friendly Medicine for Older Persons (MOP) ward. • Each morning, Therapy Assistant encourages patients to get washed and dressed in their own clothes, working alongside the HCAs. • Establish a more realistic ”normal daily routine” like patients would have at home and encourage to sit out for meals and activities, interacting with each other, staff and relatives. • Intention is to change hospital culture. CENTRE for SUSTAINABLE HEALTHCARE
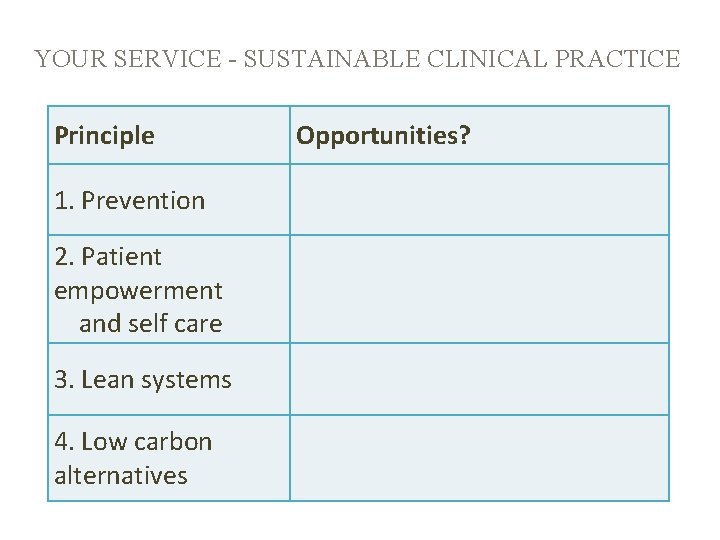
YOUR SERVICE - SUSTAINABLE CLINICAL PRACTICE Principle 1. Prevention 2. Patient empowerment and self care 3. Lean systems 4. Low carbon alternatives Opportunities?
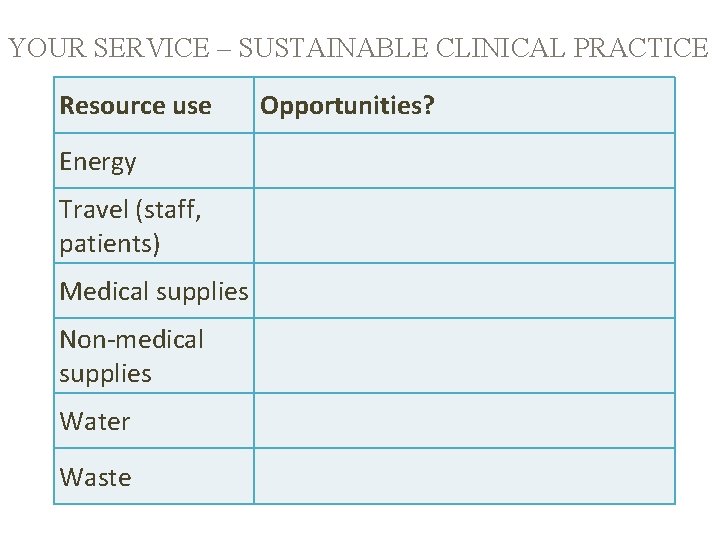
YOUR SERVICE – SUSTAINABLE CLINICAL PRACTICE Resource use Energy Travel (staff, patients) Medical supplies Non-medical supplies Water Waste Opportunities?

4. MEASURING ENVIRONMENTAL AND SOCIAL COSTS/IMPACTS CENTRE for SUSTAINABLE HEALTHCARE
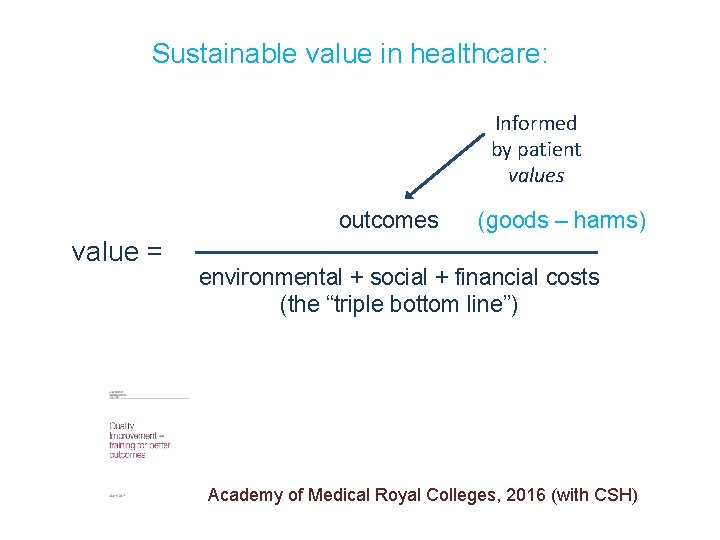
Sustainable value in healthcare: Informed by patient values outcomes value = (goods – harms) environmental + social + financial costs (the “triple bottom line”) Academy of Medical Royal Colleges, 2016 (with CSH)
ENVIRONMENTAL COSTS Carbon footprint - the sum of greenhouse gas emissions released in relation to an organisation, product or service, expressed as carbon dioxide equivalents (CO 2 e). CENTRE for SUSTAINABLE HEALTHCARE
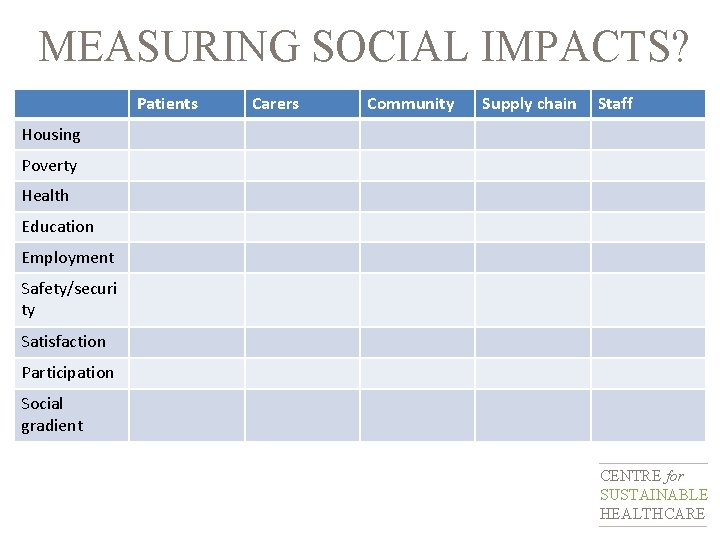
MEASURING SOCIAL IMPACTS? Patients Carers Community Supply chain Staff Housing Poverty Health Education Employment Safety/securi ty Satisfaction Participation Social gradient CENTRE for SUSTAINABLE HEALTHCARE
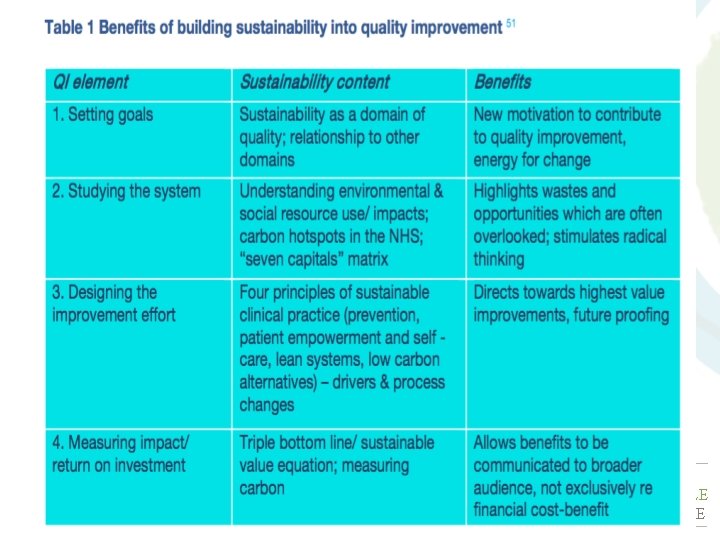
Sustainable QI CENTRE for SUSTAINABLE HEALTHCARE
“We need to develop a health and care system that is financially, socially and environmentally sustainable; that does not simply mean that we must make the best use of resources; it also means that we must improve both the quality of life and quality of care, experienced by all users of health and care services. ” Stephen Dorrell (SDU 2014) CENTRE for SUSTAINABLE HEALTHCARE
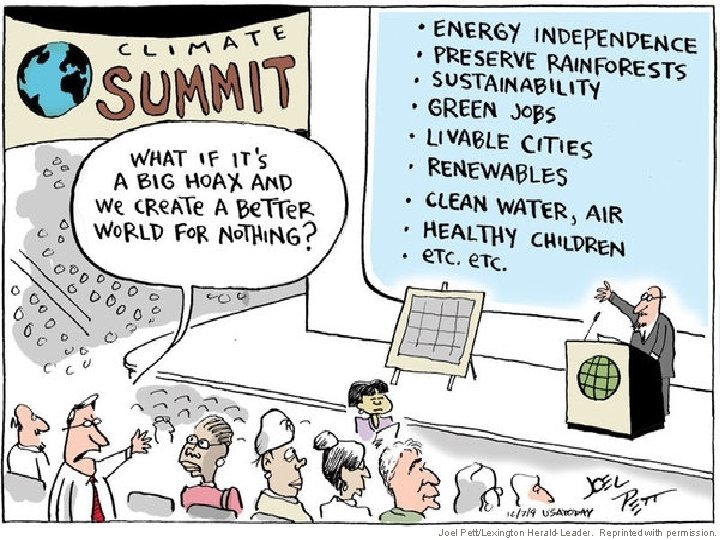
CENTRE for SUSTAINABLE HEALTHCARE Joel Pett/Lexington Herald-Leader. Reprinted with permission.

REFERENCES • Mortimer F (2010) The sustainable physician. Clinical Medicine, 10(2), 110 -111 • Mortimer F (2013) Transforming models of care: Sustainable clinical practice. Clean. Med Europe, Oxford, 18. 09. 2013. Available at: http: //cleanmedeurope. org/speakers/plenary-speakers-slides Accessed on: 12. 03. 2014 • Montgomery H (2009) The Time for Action is Now. Available at: www. climateandhealth. org/getinformed/ Accessed on: 11. 12. 2010 • NHS Sustainable Development Unit (2009) Saving Carbon, Improving Health: NHS Carbon Reduction Strategy for England. Cambridge: NHS Sustainable Development Unit • NHS Sustainable Development Unit (2012). NHS England Carbon Footprint. Cambridge: NHS Sustainable Development Unit • Pett J (2010) “What if it’s a big hoax and we create a better world…? ” editorial cartoon. USA Today, 07. 12. 2009, A. 8 • UCL Lancet Commission (2009) Managing the health effects of climate change. The Lancet, 373(9676), 1693 -1733 • WCED (1987) Our Common Future: Brundtland Report. Oxford: Oxford University Press. Available at: worldinbalance. net/pdf/1987 -brundtland. pdf Accessed on: 06. 12. 2009 CENTRE for SUSTAINABLE HEALTHCARE
REFERENCES • Atkinson, S. et al (2010). Defining Quality and Quality Improvement. Clin Med. 10(6), 537 -539 • COT (2013) Briefing paper on sustainable development. London: COT • COT (2017). Saving Money, Improving Lives. Available at: www. cotimprovinglives. com [Accessed: 22. 01. 2017] • Kings Fund (2016). Improving quality in the English NHS. London: Kings Fund. • Mortimer F (2010) The sustainable physician. Clinical Medicine, 10(2), 110 -111 • Mortimer F (2013) Transforming models of care: Sustainable clinical practice. Clean. Med Europe, Oxford, 18. 09. 2013. Available at: http: //cleanmedeurope. org/speakers/plenary-speakers-slides Accessed on: 12. 03. 2014 • Mortimer F (2017) Sustainability in Quality Improvement. February 2017 presentation. • Mortimer F, Isherwood J, Vaux E, Pearce M, Kenward C & Wilkinson A (in press). Sustainability in Quality Improvement: Redefining Value. CENTRE for SUSTAINABLE HEALTHCARE

REFERENCES • Pett J (2010) “What if it’s a big hoax and we create a better world…? ” editorial cartoon. USA Today, 07. 12. 2009, A. 8 • Polatajko HJ, Townsend EA & Craik J (2007) Canadian Model of Occupational Performance and Engagement (CMOP-E). In: Townsend EA & Polatajko HJ (2007) Enabling Occupation II: Advancing an Occupational Therapy Vision for Health, Well-being & Justice through Occupation. Ottawa, ON: CAOT ACE • Royal College of Physicians (2011). A strategy for quality: 2011 and beyond. London: Royal College of Physicians. • Sustainable Development Unit (2012) Goods and Services Carbon Hotspots. • Sustainable Development Unit (2014) Sustainable, Resilient, Healthy People & Places: A Sustainable Development Strategy for the NHS, Public Health and Social Care System. Cambridge: SDU. Available at: http: //www. sduhealth. org. uk/policystrategy/engagement-resources. aspx Accessed on: 09. 02. 2015 • UCL Lancet Commission (2009) Managing the health effects of climate change. The Lancet, 373(9676), 1693 -1733 • WCED (1987) Our Common Future: Brundtland Report. Oxford: Oxford University Press. Available at: worldinbalance. net/pdf/1987 brundtland. pdf Accessed on: 06. 12. 2009 CENTRE for SUSTAINABLE HEALTHCARE

WEBSITES www. carbonaddict. org www. climateandhealthalliance. org www. theclimateconnection. org www. nhsforest. org www. networks. sustainablehealthcare. org. uk www. sap. sustainablehealthcare. org. uk www. sd-commission. org. uk www. sduhealth. org. uk www. sustainabilityforhealth. org www. un. org/sustainabledevelopment-goals/ www. wfot. org CENTRE for SUSTAINABLE HEALTHCARE

ben. whittaker@sustainablehealthcare. org. uk
- Slides: 40