Quality Improvement Decision Support for Quality Improvement Lecture
- Slides: 20
Quality Improvement Decision Support for Quality Improvement Lecture a This material (Comp 12 Unit 5) was developed by Johns Hopkins University, funded by the Department of Health and Human Services, Office of the National Coordinator for Health Information Technology under Award Number IU 24 OC 000013. This material was updated in 2016 by Johns Hopkins University under Award Number 90 WT 0005. This work is licensed under the Creative Commons Attribution-Non. Commercial-Share. Alike 4. 0 International License. To view a copy of this license, visit http: //creativecommons. org/licenses/by-nc-sa/4. 0/
Decision Support for Quality Improvement Learning Objectives — Lecture a • Define decision support, its importance, and why it is difficult to implement. • Compare decision support tools that help improve quality. 2
Clinical Decision Support Definitions • Clinical Decision Support (CDS): “a process for enhancing health-related decisions and actions with pertinent, organized clinical knowledge and patient information to improve health and healthcare delivery” (Improving outcomes with clinical decision support: an implementer’s guide. Second Edition. HIMSS, 2011). • Clinical Decision Support Systems (CDSS): “active knowledge systems which use two or more items of patient data to generate case-specific advice” (Wyatt, J. and Spiegelhalter, D. , 1991). 3
Examples of CDS • Hospital example: appropriate dosing of antibiotics. • Primary care example: compliance with preventive recommendations. 4
CDS Five Rights Model 1. 2. 3. 4. 5. The right information. To the right person. In the right CDS intervention format. Through the right channel. At the right time in workflow. 5
Types of CDS — 1 • Relevant data displays. • Smart documentation forms. • Order facilitators (order sets, order consequents, order modifiers). • Extended-time guideline and protocol followers. • Targeted reference, including contextually relevant medical references or info buttons. • Reactive alerts. 6
Types of CDS — 2 • Task assistants for tasks such as drug dosing and acknowledging laboratory results. • Diagnostic suggestions. • Patient summaries for clinician hand-offs. • Procedure refreshers, training, and reminders. • Performance dashboards with prompts for areas needing attention. • Tracking and management systems that facilitate task prioritization and whole-service management. 7
CDS Systems: Effects on Medication Safety • CDSS, combined with CPOE, can improve medication safety and reduce medication-related expenditures: – Introduces automation at the time of ordering. – Increases legibility. – Assures that the order is safe and compliant with guidelines. • Seidling and colleagues (2010) created a comprehensive software algorithm that extracted relevant patient information (age, renal function, co-medications) and adjusted upper-dose limits to these patient characteristics. – This highly specific algorithm-based CDSS significantly improved electronic prescription quality and reduced prescription of excessive doses. 8
CDS Systems: Are They Being Used? • Despite potential usefulness, lack of widespread acceptance. • Myths – “Diagnosis is the dominant decision-making issue in medicine. ” – “Clinicians will use knowledge-based systems if the programs can be shown to function at the level of experts. ” – “Clinicians will use stand-alone decision-support tools” (Edward [Ted] E. Shortliffe, Conference on Medical Thinking, University College, London, June 23, 2006). 9
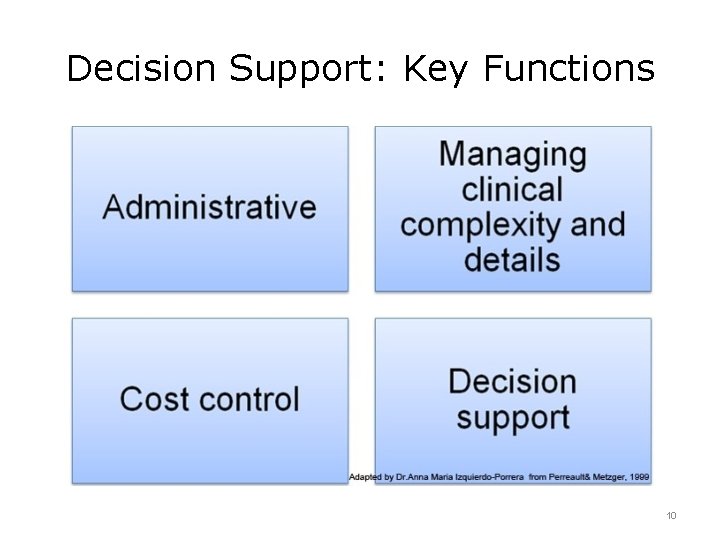
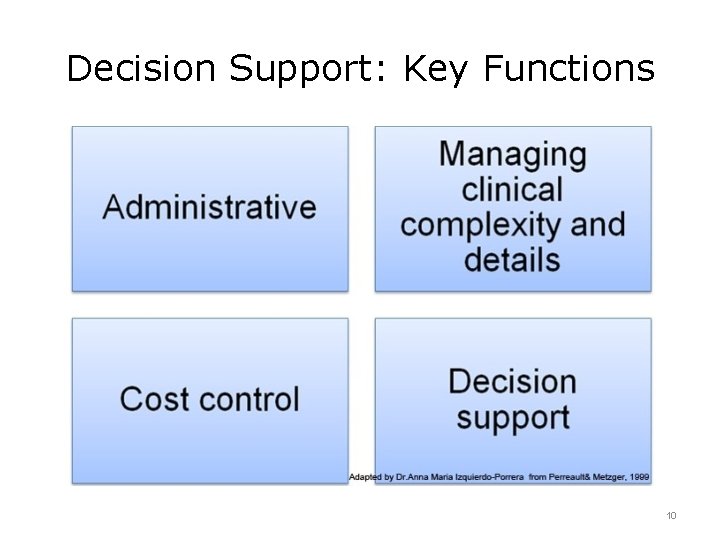
Decision Support: Key Functions 10
Decision Support: Administrative Function • Supports clinical coding and documentation. • Example: authorization of procedures and referrals. • “Choosing diagnosis codes is a nonintuitive operation for the practitioner. Mistakes are frequent with severe consequences on healthcare evaluation and funding” (Peters, 2005). 11
Decision Support: Complexity Management Function • Assists with the details of managing clinical complexity. • Examples: – Keeping patients on research and chemotherapy protocols. – Tracking orders. – Referral follow-up. – Preventive care. 12
Decision Support: Cost Control Function • Supports control of costs. • Examples: – Monitoring medication orders. – Avoiding duplicate or unnecessary tests. 13
Decision Support: Decision Support Function • Supports clinical diagnosis and treatment plan processes and promotes use of best practices. • Examples: – Condition-specific clinical practice guidelines. – Population-based management. – Clinical calculation. – Disease registries and patient tracking tools. – Summary screens. – Order sets (Metzger, J. and Macdonald, K. , 2002). 14
Unintended Consequences of CDS • Content: – Elimination or changing of roles of clinicians and staff. – Currency of CDS content. – Wrong or misleading CDS content. • Presentation: – Rigidity of systems. – Alert fatigue. – Sources of potential error. 15
Decision Support for Quality Improvement Summary — Lecture a • CDSS integrate a medical knowledge base, patient data, and an inference engine to generate carespecific advice. • Despite potential usefulness, there has not been widespread clinician acceptance of CDSS. • The design of useful CDS must include: right information, right person, right CDS intervention format, right channel, and right time in workflow. • Key functions of CDSS are: administrative, managing clinical complexity/details, cost control, and decision support. 16
Decision Support for Quality Improvement References — Lecture a — 1 References Ash, J. S. , Sittig, D. F. , Campbell, E. M, et al. (2007). Some unintended consequences of clinical decision support systems. AMIA 2007 Symposium Proceedings. 11: 26– 30. Bates, D. Clinical Decision Support Workshop, ONC, August 25– 26, 2009. Chaffee, B. W. (2010). Future of clinical decision support in computerized prescriber order entry. American Journal of Health System Pharmacists. 67: 932– 935. De Clercq, P. A. , Blom, J. A. , Hasman, A. , Korsten, H. H. M. (1999). A strategy for developing practice guidelines for the ICU using automated knowledge acquisition techniques. Journal of Clinical Monitoring. 15: 109– 117. Handler, J, A. , Feied, C. F. , Coonan , K. , et al. (2004). Computerized physician order entry and online decision support. Academy of Emergency Medicine. 11(11): 1135– 1141. Kawamoto, K. , Houlihan, C. A. , Balas, E. A. , Lobach, D. F. (2005). Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. BMJ. 330(7494): 765. Kuperman, G. J. , Bobb, A. , Payne, T. H. , et al. (2007). Medication-related clinical decisionsupport in computerized provider order entry systems: a review. Journal of the American Medical Informatics Association. 14(1), 29– 40. 17
Decision Support for Quality Improvement References — Lecture a — 2 References Metzger, J. and Macdonald, K. (2002). Clinical decision support for the independent physician practice. Health Reports, California Health Care Foundation. Moxey, A. , Robertson, J. , Newby, D. , Hains, I. , et al. (2001). Computerized clinical decision support for prescribing: provision does not guarantee uptake. Journal of the American Medical Informatics Association. 17: 25– 33. Osheroff , J. A. (2009). Improving medication use and outcomes with clinical decision support: a step-by-step guide. Chicago, IL: The Healthcare Information and Management Systems Society. Peters, J. and Le Cornu, R. (2005). Beyond Communities of Practice: Learning Circles for Transformational School Leadership, Chapter 6 in P. Carden and T. Stehlik (eds. ) Beyond Communities of Practice, Queensland, Post Pressed. Seidling , H. M. , Schmitt, S. P. W. , Bruckner , T. , et al. (2010 April 27). Patient-specific electronic decision support reduces prescription of excessive doses. Quality and Safety in Health Care. Shortliffe, E. E. (2006 June 23). Conference on Medical Thinking, University College, London. 18
Decision Support for Quality Improvement References — Lecture a — 3 References Wyatt, J. , Spiegelhalter, D. (1991). Field trials of medical decision-aids: potential problems and solutions. Proceedings of the Annual Symposium on Computer Application in Medical Care. 3– 7. Images Slide 10: Decision Support: Key Functions. Adapted from Perreault and Metzer, 1999, by Dr. Anna Maria Izquierdo-Porrera. 19
Quality Improvement Decision Support for Quality Improvement This material (Comp 12 Unit 5) was developed by Johns Hopkins University, funded by the Department of Health and Human Services, Office of the National Coordinator for Health Information Technology under Award Number IU 24 OC 000013. This material was updated in 2016 by Johns Hopkins University under Award Number 90 WT 0005. 20