NITMED TUTORIALS INC ACUTE RENAL FAILURE Acute Renal













- Slides: 89
NITMED TUTORIALS INC
ACUTE RENAL FAILURE
Acute Renal Failure Definition ◦ The loss of renal function (measured as GFR) over hours to days ◦ Expressed clinically as the retention of nitrogenous waste products in the blood
Acute Renal Failure Definitions ◦ Azotemia - the accumulation of nitrogenous wastes ◦ Uremia - symptomatic renal failure ◦ Oliguria - urine output < 400 -500 m. L/24 hours ◦ Anuria - urine output < 100 m. L/24 hours
Functions of the Renal System Maintenance of fluid balance: ◦ The kidneys maintain the fluid balance in the body by regulating the amount and makeup of fluid inside and outside (mainly) the cells. ◦ The kidneys are continuously exchanging water, (plus sodium, potassium, chloride, and other ions across their cell membranes. ) Two hormones play a key role in the kidney’s ability to maintain fluid balance in the body
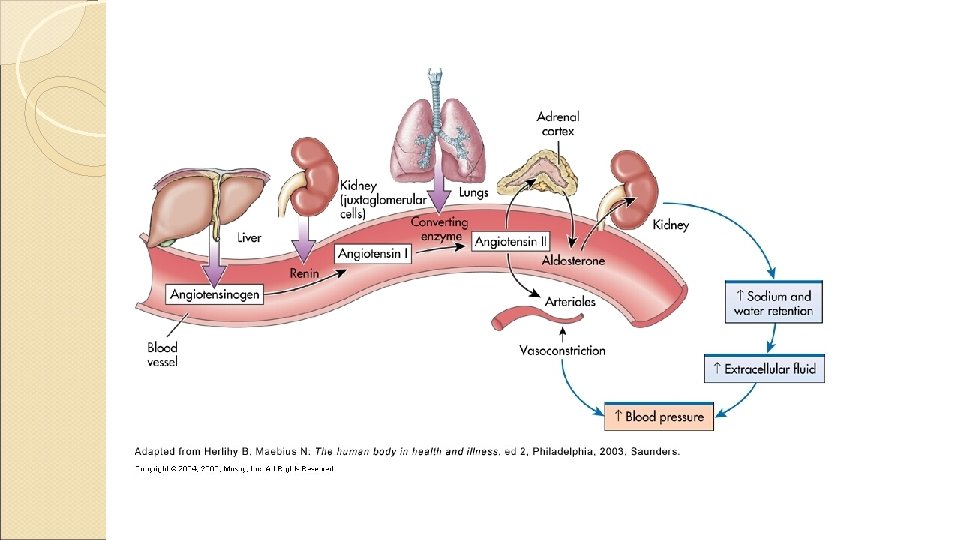
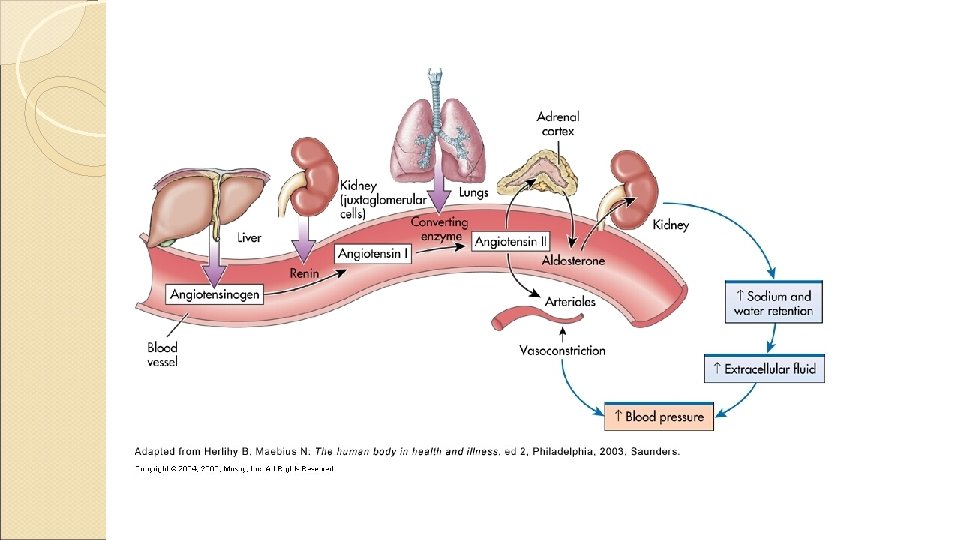
Functions of the Renal System 1. ADH: controls the collecting tubules permeability to water according to the osmoreceptor’s ability to sense high concentration of solute in the plasma. (In other words when the plasma is concentrated, ADH is secreted to hold on to more water. When the plasma is dilute, ADH is not secreted so the permeability to water changes in the collecting tubules, and water is released. ) 2. Aldosterone: regulates water reabsorption in the distal tubules by increasing sodium reabsorption and therefore water reabsorption when released from the adrenal cortex. (It is released as the final response in the renin angiotensin aldosterone system. ) The presence of Aldosterone also helps increase the excretion of potassium. NB: when this fails fluid retention occurs
Functions of the Renal System The regulation of acid-base balance: The kidneys regulate acid base balance by: Excreting just enough hydrogen ions to keep the ph of the blood in the normal range. Manufacturing bicarbonate (a base) as needed to maintain ph between 7. 357. 45. When the kidneys fail: Metabolic acidosis results. Patients may develop Kussmaul respirations
Functions of the Renal System Maintenance of electrolyte balance: The kidneys function to regulate electrolyte concentrations. When the kidneys fail, electrolyte levels are not maintained: K+, Na, Phosphate, Ca+ Potassium: Hypokalemia may occur… with vomiting or excessive diarrhea in early renal failure when uremic toxins begin to circulate. in the diuretic phase of acute renal failure as the kidney is unable to conserve water and electrolytes. ………………. ARRYTHMIAS, NAUSEA, and LETHARGY occur. Hyperkalemia occurs with…. . decreased renal excretion of potassium both in the oliguric phase of acute renal failure and in end stage renal disease. Hyperkalemia could lead to life threatening ARRYTHMIAS!!
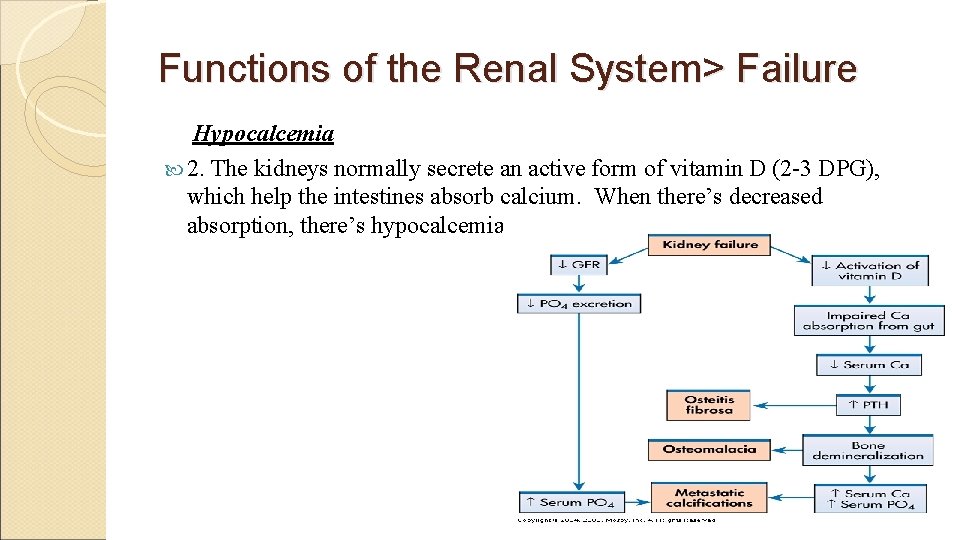
Functions of the Renal System> Failure Sodium: Hyponatremia also occurs in the diuretic phase of acute renal failure when the kidneys cannot conserve sodium or water. MUSCLE WEAKNESS, CONFUSION, and ABDOMINAL CRAMPING occur. Hypernatremia occurs with decreased renal excretion of sodium. This will occur in the end stages of renal disease and the person will be on a sodium-restricted diet. ……DRY MUCOUS MEMBRANES, and OLIGURIA occurs. Calcium: Hypocalcemia occurs for two reasons: 1. A hyperphosphatemia occurs because of a decreased excretion of phosphate. There is an inverse relationship between phosphate and Calcium, so a hypocalcemia occurs. ( These electrolytes are regulated by the parathyroid gland, so when the phosphate level rises out of control due to the kidneys inability to excrete it, the parathyroid hormone (from the gland) is over secreted and starts to get Calcium from the bones, due to a depletion in the serum) OSTEOPOROSIS, OSTEODYSTROPHY (bone disease), AND TETANY occurs.
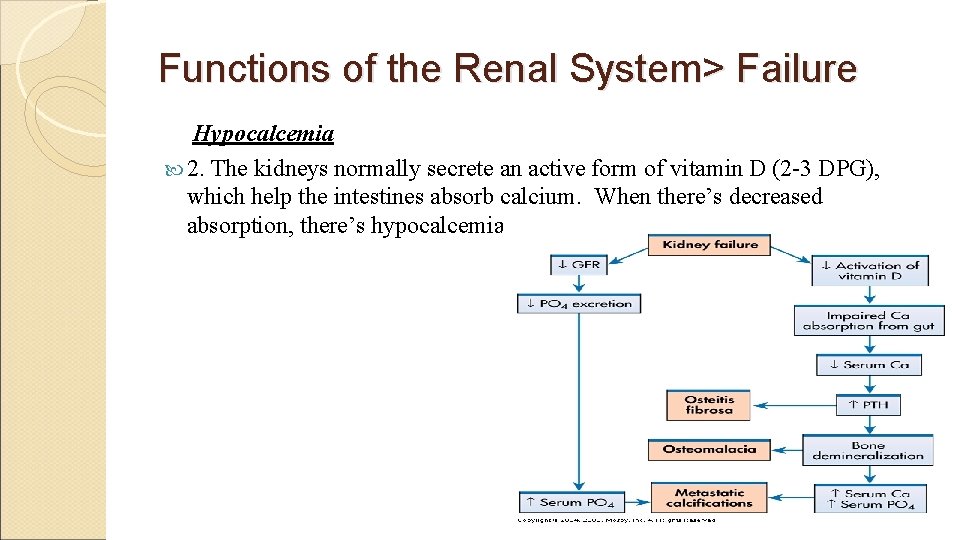
Functions of the Renal System> Failure Hypocalcemia 2. The kidneys normally secrete an active form of vitamin D (2 -3 DPG), which help the intestines absorb calcium. When there’s decreased absorption, there’s hypocalcemia.
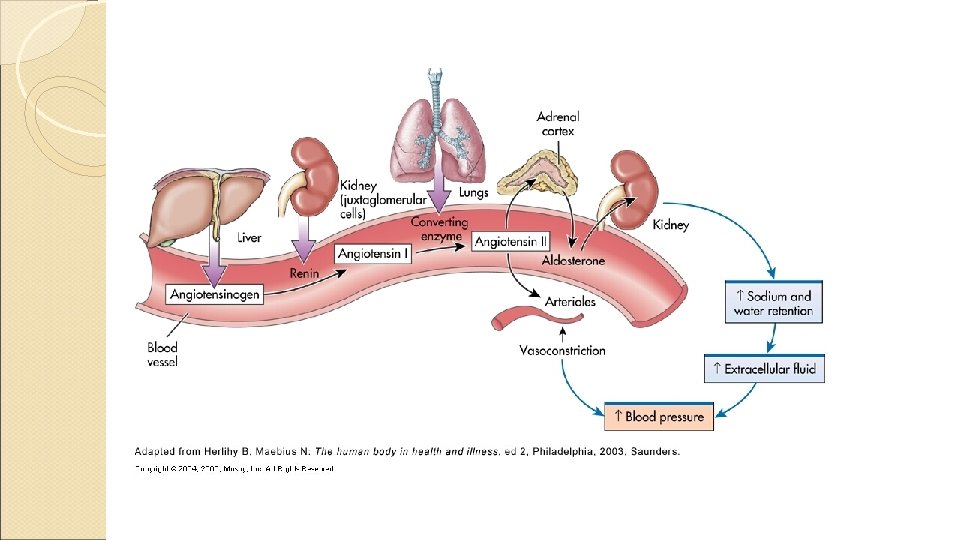
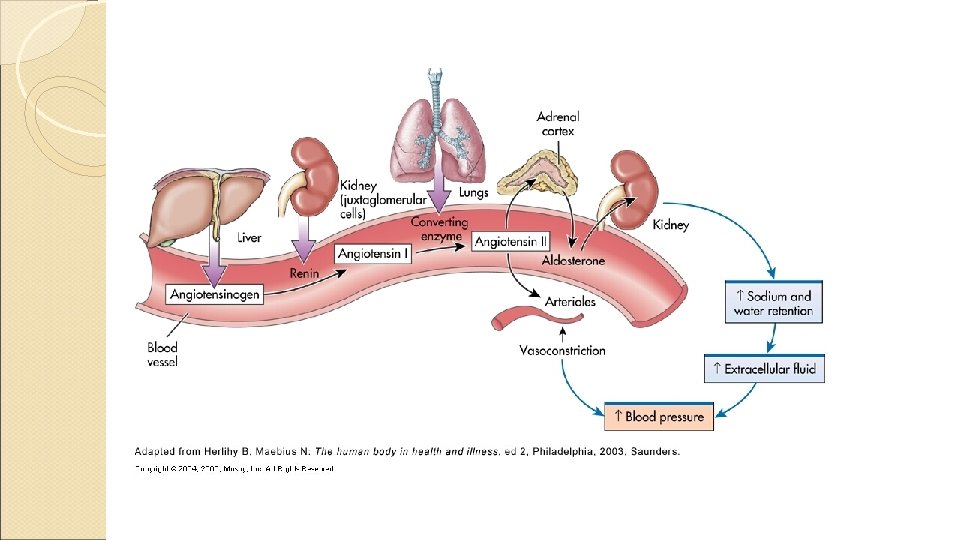
Functions of the Renal System Maintenance of blood pressure: The kidneys help regulate blood pressure by producing and secreting the enzyme renin in response to an actual or perceived decline in extra cellular fluid volume. (Angiotensinogen) turns Renin into angiotensin I which is converted into angiotensin II (by an enzyme), the most potent vasoconstrictor in the body. Angiotensin II raises arterial blood pressure by…
RENIN… 1. Increasing peripheral vasoconstriction 2. Stimulating Aldosterone secretion Aldosterone promotes the reabsorption of sodium and water to correct the fluid deficit and/or inadequate blood flow (renal ischemia)

Functions of the Renal System> Failure When the kidneys fail: Patients are often HYPERTENSIVE.

Functions of the Renal System The collection and elimination of metabolic waste such as urea and creatinine: The kidney’s job is to excrete the waste products of metabolism. Urea is a byproduct of protein metabolism. It is not as adequate an indicator of renal disease as elevated creatinine levels are because urea (BUN) levels elevate with an increased protein intake, trauma, dehydration etc. . Serum creatinine levels are an accurate indicator of renal function/dysfunction. The urinary excretion should equal the amount produced by the body (by skeletal muscle catabolism).

Functions of the Renal System> Failure When the kidneys fail: The patient suffers from an overload of these circulating uremic toxins. All body systems may be affected. the CNS is affected by the uremic toxins. Drowsiness, poor memory, inability to concentrate, seizures, and even come may result. GI distress may result such as nausea, vomiting, abdominal distension, diarrh and constipation.
Functions of the Renal System The secretion of erythropoietin: ◦ The kidneys secrete erythropoietin when the oxygen supply in the tissue blood drops. This hormone prompts the bone marrow to produce more RBCs. ◦ When the kidneys fail: The patient becomes anemic. (Remember also they are anemic due to the increased destruction of RBCs & PLTS by the uremic toxins, and even due to their bleeding tendency secondary to their low PLTS. )
Functions of the Renal System> Failure Pericarditis may result as pericardium is inflamed due to the buildup of these uremic wastes. A pericardial friction rub and pain may result. Pruritis may result as the excretory function of the skin attempts to excrete the waste products. A uremic frost may be notable on skin and collect on eyebrows. Skin may become a pale yellowish color, as urochrome pigments are present. Anemia and thrombocytopenia occur because the uremic toxins destroy RBCs and PLTS.
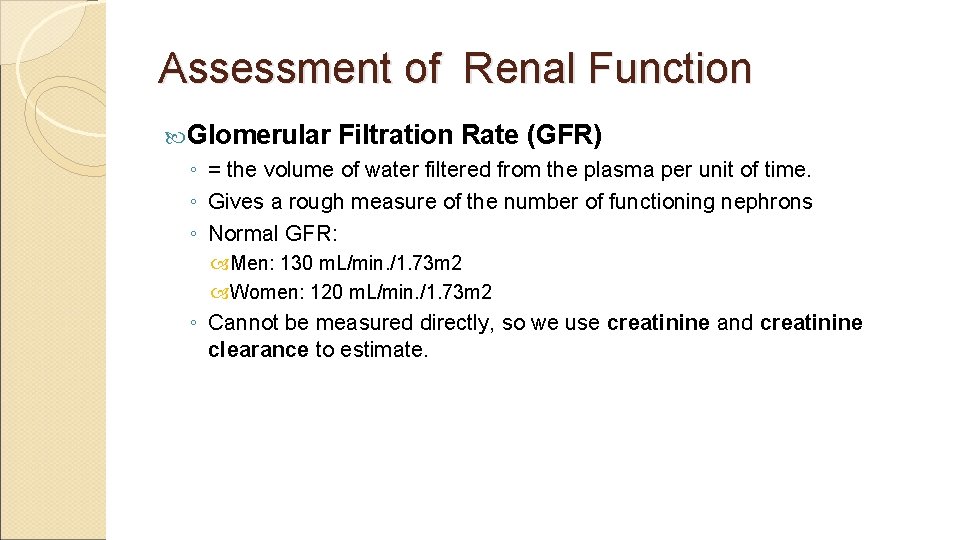
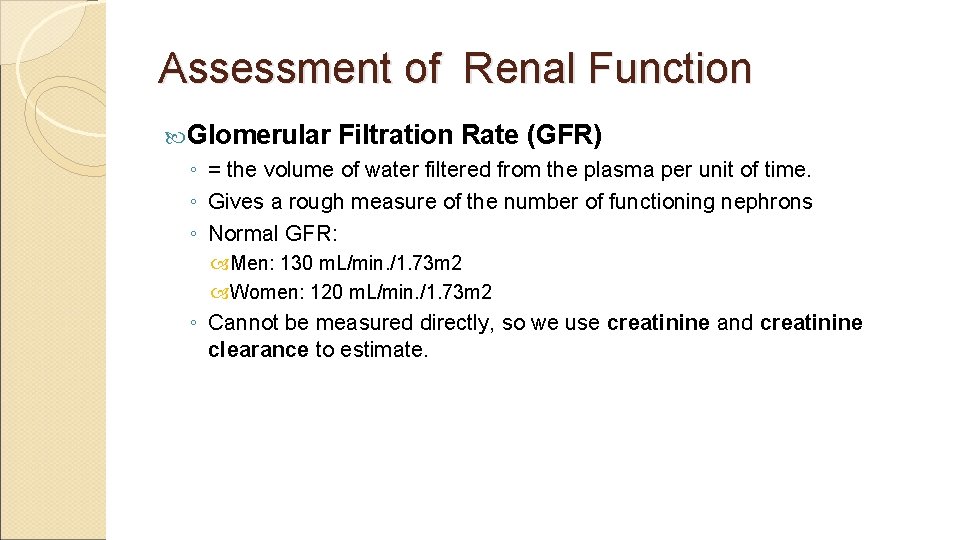
Assessment of Renal Function Glomerular Filtration Rate (GFR) ◦ = the volume of water filtered from the plasma per unit of time. ◦ Gives a rough measure of the number of functioning nephrons ◦ Normal GFR: Men: 130 m. L/min. /1. 73 m 2 Women: 120 m. L/min. /1. 73 m 2 ◦ Cannot be measured directly, so we use creatinine and creatinine clearance to estimate.

Assessment of Renal Function (cont. ) Creatinine ◦ A naturally occurring amino acid, predominately found in skeletal muscle ◦ Freely filtered in the glomerulus, excreted by the kidney and readily measured in the plasma ◦ As plasma creatinine increases, the GFR exponentially decreases. ◦ Limitations to estimate GFR: Patients with decrease in muscle mass, liver disease, malnutrition, advanced age, may have low/normal creatinine despite underlying kidney disease 15 -20% of creatinine in the bloodstream is not filtered in glomerulus, but secreted by renal tubules (giving overestimation of GFR) Medications may artificially elevate creatinine: Trimethroprim (Bactrim) Cimetidine

Assessment of Renal Function (cont. ) Creatinine Clearance ◦ Best way to estimate GFR ◦ GFR = (creatinine clearance) x (body surface area in m 2/1. 73) ◦ Ways to measure: 24 -hour urine creatinine: Creatinine clearance = (Ucr x Uvol)/ plasma Cr Cockcroft-Gault Equation: (140 - age) x lean body weight [kg] Cr. Cl (m. L/min) = ———————— x 0. 85 if Cr [mg/d. L] x 72 female Limitations: Based on white men with non-diabetes kidney disease Modification of Diet in Renal Disease (MDRD) Equation: GFR (m. L/min. /1. 73 m 2) = 186 X (SCr)-1. 154 X (Age)-0. 203 X (0. 742 if female) X (1. 210 if African-American )
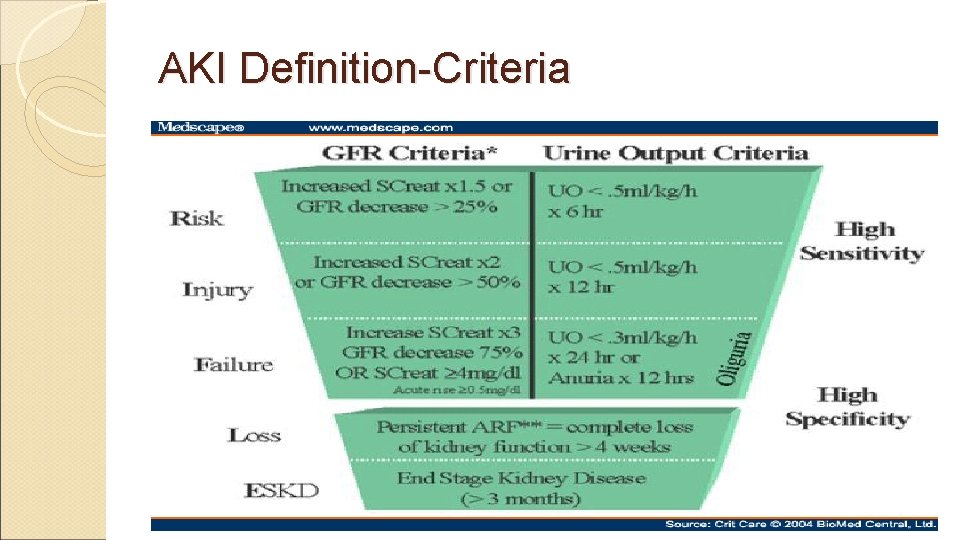
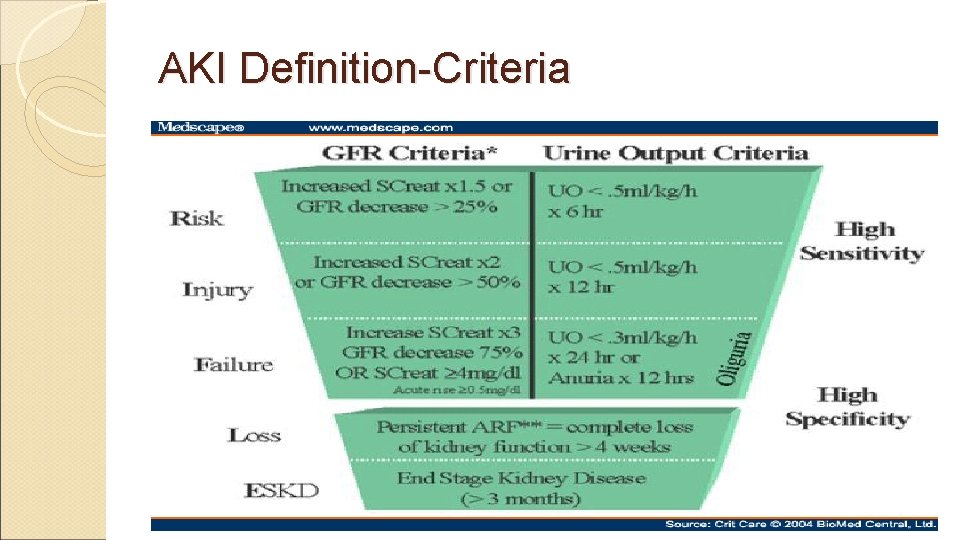
AKI Definition-Criteria

RIFLE criteria for diagnosis of AKI based on The “Acute Dialysis Quality Initiative” Increase in SCr Urine output Risk of renal injury 0. 3 mg/dl increase < 0. 5 ml/kg/hr for > 6 h Injury to the kidney 2 X baseline < 0. 5 ml/kg/hr for >12 h Failure of kidney function 3 X baseline OR Anuria for >12 h > 0. 5 mg/dl increase if SCr >=4 mg/dl Loss of kidney function End-stage disease Persistent renal failure for > 4 weeks Persistent renal failure for > 3 months Am J Kidney Dis. 2005 Dec; 46(6): 1038 -48
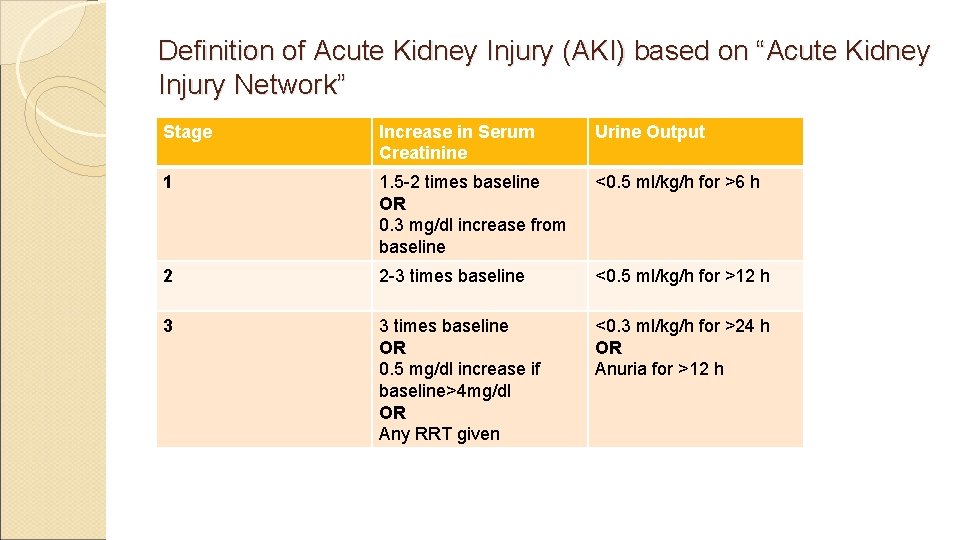
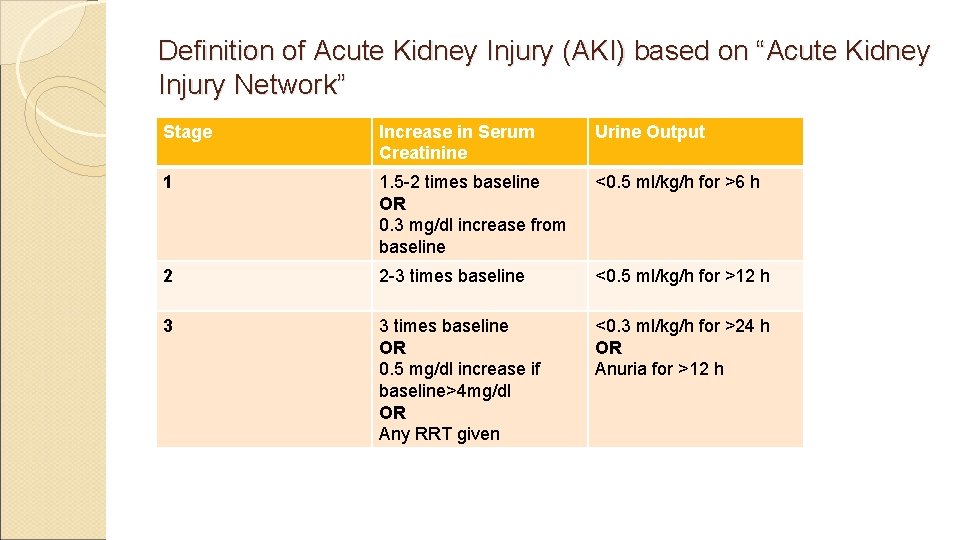
Definition of Acute Kidney Injury (AKI) based on “Acute Kidney Injury Network” Stage Increase in Serum Creatinine Urine Output 1 1. 5 -2 times baseline OR 0. 3 mg/dl increase from baseline <0. 5 ml/kg/h for >6 h 2 2 -3 times baseline <0. 5 ml/kg/h for >12 h 3 3 times baseline OR 0. 5 mg/dl increase if baseline>4 mg/dl OR Any RRT given <0. 3 ml/kg/h for >24 h OR Anuria for >12 h
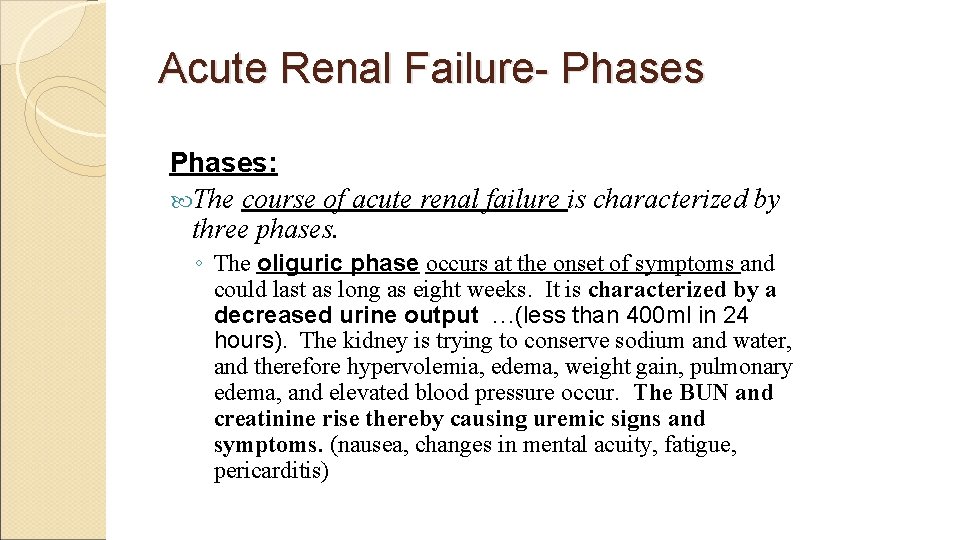
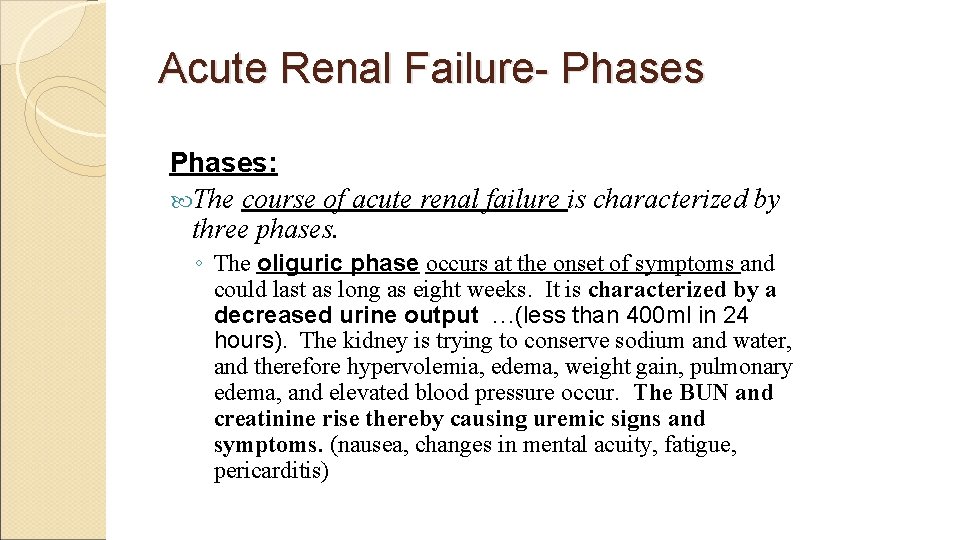
Acute Renal Failure- Phases: The course of acute renal failure is characterized by three phases. ◦ The oliguric phase occurs at the onset of symptoms and could last as long as eight weeks. It is characterized by a decreased urine output …(less than 400 ml in 24 hours). The kidney is trying to conserve sodium and water, and therefore hypervolemia, edema, weight gain, pulmonary edema, and elevated blood pressure occur. The BUN and creatinine rise thereby causing uremic signs and symptoms. (nausea, changes in mental acuity, fatigue, pericarditis)
Acute Renal Failure- Phases diuretic phase is marked by urine output that can range from 1 -5 L/day. The kidney has lost its ability to conserve water. Hypovolemia, (fluid) weight loss, hypokalemia, hyponatremia all can result. The BUN and creatinine begin to level out. May last 7 -14 days. The
Acute Renal Failure- Phases recovery phase is reached when the BUN and creatinine have returned to normal. This phase can last from 3 -12 months. The

Acute Renal Failure- Diagnostic Findings: Laboratory data and other assessments reveal the following: . . . (In the oliguric phase) 1. Decreased or absent urinary output 2. Increased BUN, creatinine, sodium, potassium, chloride 3. Decreased calcium (high phos), bicarbonate (acidosis), H/H (anemic) 4. Metabolic acidosis
Causes of ARF Pre-renal = ◦ vomiting, diarrhea, poor fluid intake, fever, use of diuretics, and heart failure ◦ cardiac failure, liver dysfunction, or septic shock Intrinsic ◦ Interstitial nephritis, acute glomerulonephritis, tubular necrosis, ischemia, toxins Post-renal = ◦ prostatic hypertrophy, cancer of the prostate or cervix, or retroperitoneal disorders ◦ neurogenic bladder ◦ bilateral renal calculi, papillary necrosis, coagulated blood, bladder carcinoma, and fungus

Symptoms of ARF Decrease urine output (70%) Edema, esp. lower extremity Mental changes Heart failure Nausea, vomiting Pruritus Anemia Tachypenic Cool, pale, moist skin
Hyperkalemia Symptoms Weakness Lethargy Muscle cramps Paresthesias Dysrhythmias

Hyperkalemia Treatment Calcium gluconate (carbonate) Sodium Bicarbonate Insulin/glucose Diuretics (Furosemid) Albuterol Hemodialysis
Prerenal Acute Renal Failure Volume Depletion Decreased effective blood volume ◦ congestive heart failure ◦ cirrhosis ◦ nephrotic syndrome ◦ sepsis Renal vasoconstriction ◦ hepatorenal syndrome ◦ hypercalcemia ◦ nonsteroidal anti-inflammatory drugs
Prerenal Acute Renal Failure: Clinical Presentation History ◦ volume loss (e. g. , diarrhea, acute blood loss) ◦ heart disease ◦ liver disease ◦ evidence of infection ◦ diuretic use ◦ thirst ◦ orthostatic symptoms
Prerenal Acute Renal Failure: Clinical Presentation Physical Examination ◦ Blood pressure and pulse ◦ Orthostatic changes in blood pressure ◦ Skin turgor ◦ Dryness of mucous membranes and axillae ◦ Neck veins ◦ Cardiopulmonary exam ◦ Peripheral edema
Prerenal Acute Renal Failure: Clinical Presentation BUN: Creatinine ratio ◦ > 20: 1 Urine indices ◦ Oliguria usually < 500 m. L/24 hours; but may be non-oliguric ◦ Elevated urine concentration UOsm > 700 mmol/L specific gravity > 1. 020 ◦ Evidence of high renal sodium avidity UNa < 20 mmol/L FENa < 0. 01 ◦ Inactive urine sediment
Fractional Excretion of Sodium Etiologies of a fractional excretion of sodium <0. 01 ◦ normal renal function ◦ prerenal azotemia ◦ hepatorenal syndrome ◦ early obstructive uropathy ◦ contrast nephropathy ◦ rhabdomyolysis ◦ acute glomerulonephritis
Treatment of Prerenal Acute Renal Failure Correction of volume deficits Discontinuation of antagonizing medications ◦ NSAIDs/COX-2 inhibitors ◦ Diuretics Optimization of cardiac function
Postrenal Acute Renal Failure Urinary tract obstruction ◦ level of obstruction upper tract (ureters) lower tract (bladder outlet or urethra) ◦ degree of obstruction partial complete
Pathophysiology of Renal Failure in Obstructive Uropathy Early ◦ Increased intratubular pressure ◦ Initial increase followed by decrease in renal plasma flow Late ◦ Normal intratubular pressure ◦ Marked decrease in renal plasma flow
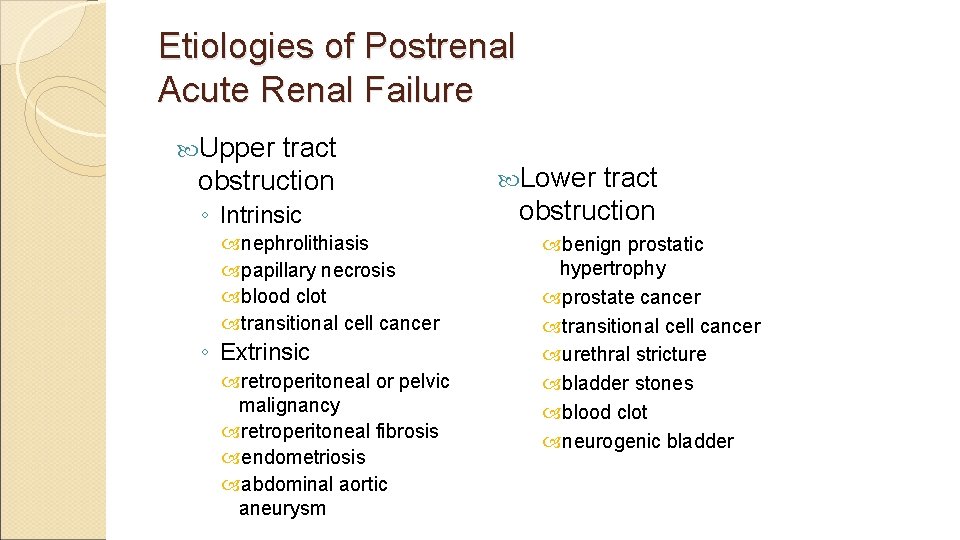
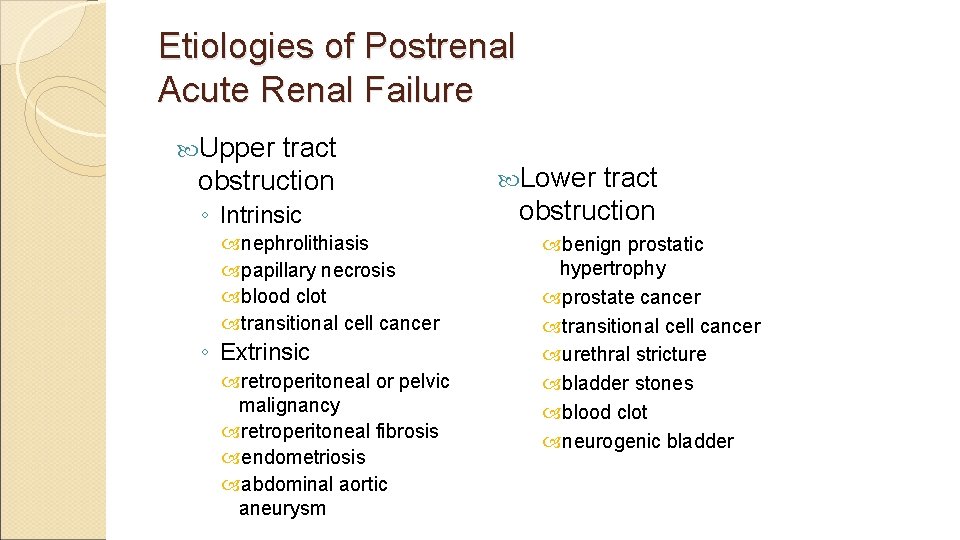
Etiologies of Postrenal Acute Renal Failure Upper tract obstruction ◦ Intrinsic nephrolithiasis papillary necrosis blood clot transitional cell cancer ◦ Extrinsic retroperitoneal or pelvic malignancy retroperitoneal fibrosis endometriosis abdominal aortic aneurysm Lower tract obstruction benign prostatic hypertrophy prostate cancer transitional cell cancer urethral stricture bladder stones blood clot neurogenic bladder
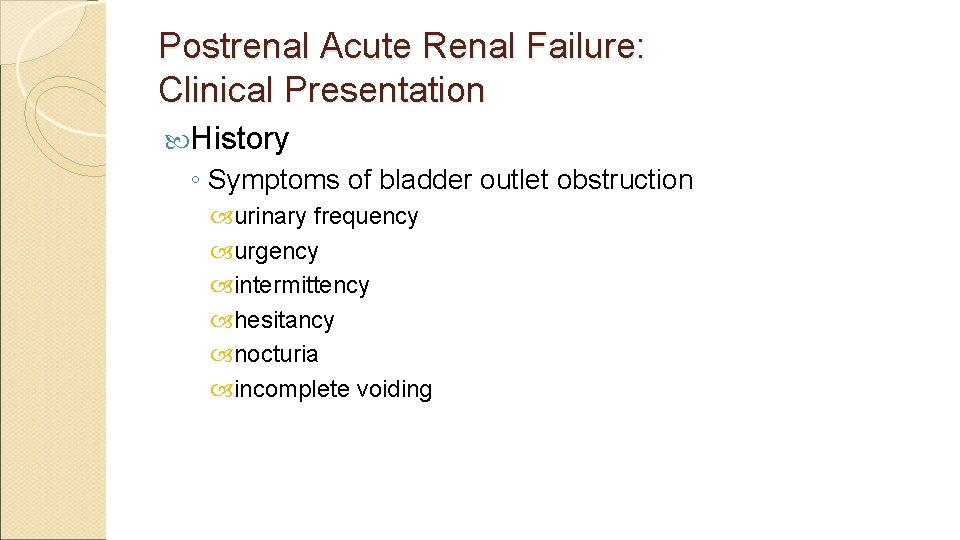
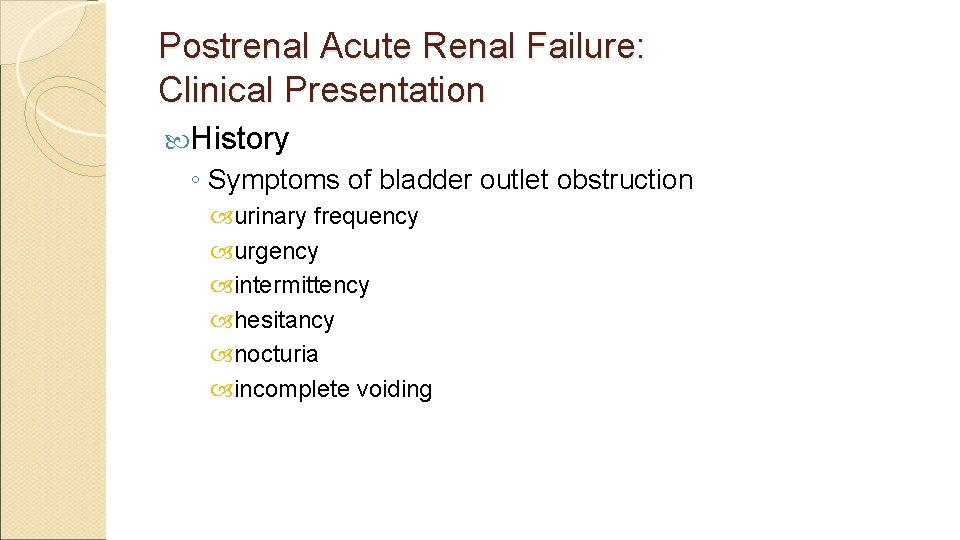
Postrenal Acute Renal Failure: Clinical Presentation History ◦ Symptoms of bladder outlet obstruction urinary frequency urgency intermittency hesitancy nocturia incomplete voiding

Postrenal Acute Renal Failure: Clinical Presentation History ◦ Changes in urine volume anuria polyuria fluctuating urine volume ◦ Flank pain ◦ Hematuria ◦ History of pelvic malignancy
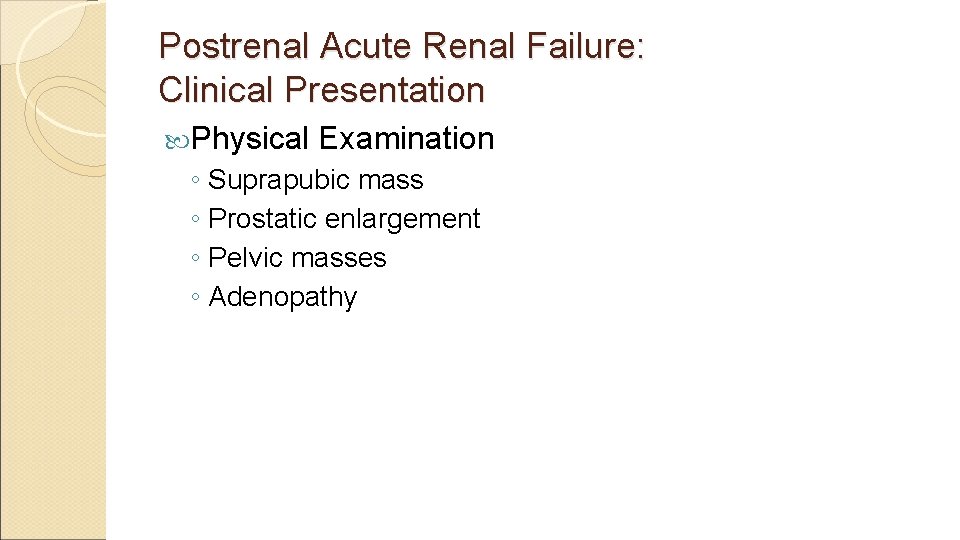
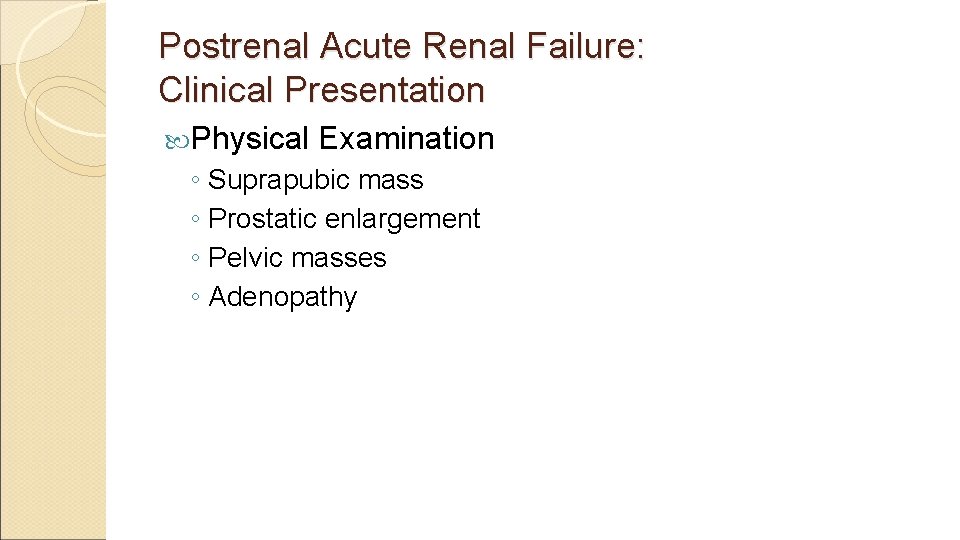
Postrenal Acute Renal Failure: Clinical Presentation Physical Examination ◦ Suprapubic mass ◦ Prostatic enlargement ◦ Pelvic masses ◦ Adenopathy
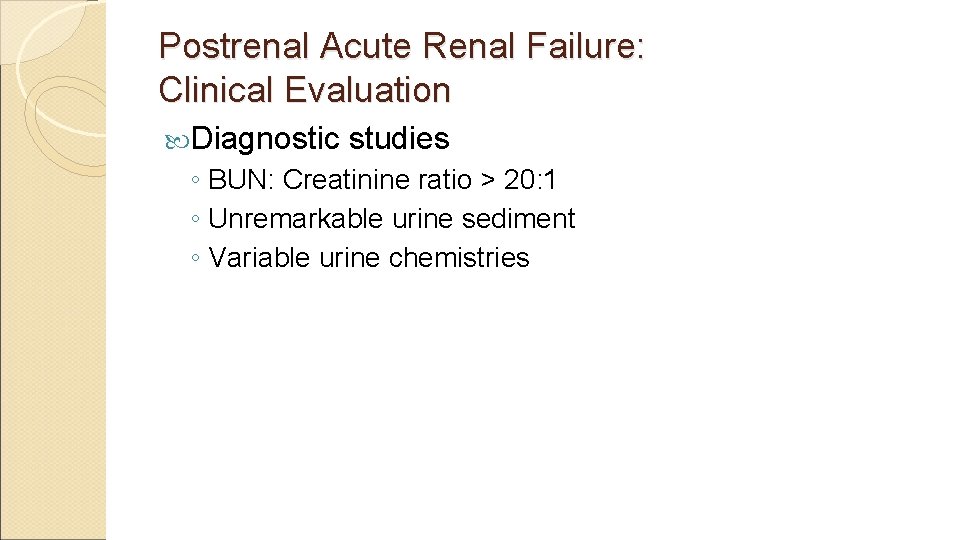
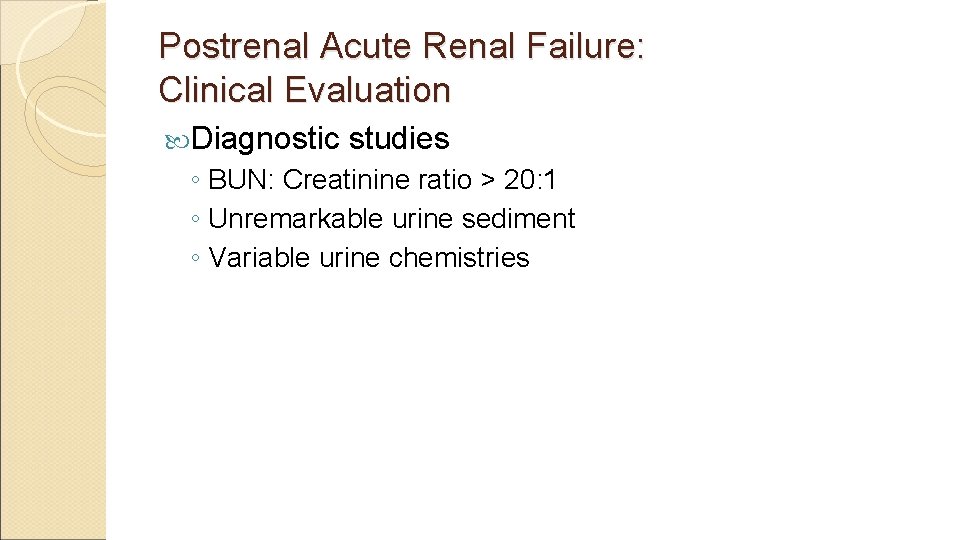
Postrenal Acute Renal Failure: Clinical Evaluation Diagnostic studies ◦ BUN: Creatinine ratio > 20: 1 ◦ Unremarkable urine sediment ◦ Variable urine chemistries
Postrenal Acute Renal Failure: Clinical Evaluation Diagnostic studies ◦ Post-void residual bladder volume > 100 m. L consistent with voiding dysfunction ◦ Radiologic studies Ultrasound CT scan Nuclear medicine Retrograde pyelography Antegrade nephrostograms
Treatment of Postrenal Acute Renal Failure Relief of obstruction ◦ Lower tract obstruction bladder catheter ◦ Upper tract obstruction ureteral stents percutaneous nephrostomies Recovery of renal function dependent upon duration of obstruction Risk of post-obstructive diuresis
Intrinsic Acute Renal Failure Acute tubular necrosis (ATN) Acute interstitial nephritis (AIN) Acute glomerulonephritis (AGN) Acute vascular syndromes Intratubular obstruction
Acute Tubular Necrosis Ischemic prolonged prerenal azotemia hypotension hypovolemic shock cardiopulmonary arrest cardiopulmonary bypass Sepsis Nephrotoxic ◦ drug-induced radiocontrast agents aminoglycosides amphotericin B cisplatinum acetaminophen ◦ pigment nephropathy hemoglobin myoglobin
Pathophysiology of Acute Tubular Necrosis Mechanisms of decreased renal function ◦ Vasoconstriction ◦ Tubular obstruction by sloughed debris ◦ Backleak of glomerular filtrate across denuded tubular basement membrane
Acute Tubular Necrosis: Clinical Presentation History ◦ Acute illness ◦ Exposure to nephrotoxins ◦ Episodes of hypotension Physical examination ◦ Hemodynamic status ◦ Volume status ◦ Features of associated illness Laboratory data ◦ BUN: Creatinine ratio < 10: 1 ◦ Evidence of toxin exposure
Acute Tubular Necrosis: Clinical Presentation Urine indices ◦ Urine volume may be oliguric or non-oliguric ◦ Isosthenuric urine concentration UOsm 300 mmol/L specific gravity 1. 010 ◦ Evidence of renal sodium wasting UNa > 40 mmol/L FENa > 0. 02 ◦ Urine sediment tubular epithelial cells granular casts
Acute Tubular Necrosis: Treatment Supportive therapy No specific pharmacologic treatments Acute dialysis for: ◦ volume overload ◦ metabolic acidosis ◦ hyperkalemia ◦ uremic syndrome pericarditis encephalopathy ◦ azotemia
Prognosis of Acute Tubular Necrosis Mortality dependent upon comorbid conditions ◦ overall mortality ~ 50% Recovery of renal function seen in ~ 90% of patients who survive - although not necessarily back to prior baseline renal function
Acute Interstitial Nephritis Acute renal failure due to lymphocytic infiltration of the interstitium Classic triad of ◦ fever ◦ rash ◦ eosinophilia
Acute Interstitial Nephritis Drug-induced ◦ penicillins ◦ cephalosporins ◦ sulfonamides ◦ rifampin ◦ phenytoin ◦ furosemide ◦ NSAIDs Malignancy Idiopathic Infection-related ◦ bacterial ◦ viral ◦ rickettsial ◦ tuberculosis Systemic diseases ◦ SLE ◦ sarcoidosis ◦ Sjögren’s syndrome ◦ tubulointerstitial nephritis and uveitis
Acute Interstitial Nephritis: Clinical Presentation History ◦ preceding illness or drug exposure Physical examination ◦ fever ◦ rash Laboratory Findings ◦ eosinophilia
Acute Interstitial Nephritis: Clinical Presentation Urine findings ◦ non-nephrotic protinuria ◦ hematuria ◦ pyuria ◦ WBC casts ◦ eosinophiluria
Acute Interstitial Nephritis: Treatment Discontinue offending drug Treat underlying infection Treat systemic illness Glucocorticoid therapy may be used in patients who fail to respond to more conservative therapy
Acute Glomerulonephritis Nephritic presentation ◦ proteinuria may be in nephrotic range (> 3 g/day) ◦ hematuria ◦ RBC casts Diagnosis usually requires renal biopsy
Acute Glomerulonephritis Etiologies ◦ poststreptococcal glomerulonephritis ◦ postinfectious glomerulonephritis ◦ endocarditis-associated glomerulonephritis ◦ systemic vasculitis ◦ thrombotic microangiopathy hemolytic-uremic syndrome thrombotic thrombocytopenic purpura ◦ rapidly progressive glomerulonephritis
Acute Vascular Syndromes Renal artery thromboembolism Renal artery dissection Renal vein thrombosis Atheroembolic disease
Intratubular Obstruction Intratubular crystal deposition ◦ tumor lysis syndrome acute urate nephropathy ◦ ethylene glycol toxicity calcium oxylate deposition Intratubular protein deposition ◦ multiple myeloma -Bence-Jones protein deposition
Differential Diagnosis of Acute Renal Failure Prerenal ARF Postrenal ARF Intrinsic ARF ◦ acute tubular necrosis ◦ acute interstitial nephritis ◦ acute glomerulonephritis ◦ acute vascular syndromes ◦ intratubular obstruction
Clinical Assesment History: ◦ Cancer? ◦ Recent Infections? ◦ Blood in urine? ◦ Change in urine output? ◦ Flank Pain? ◦ Recent bleeding? ◦ Dehydration? Diarrhea? Nausea? Vomiting? ◦ Blurred vision? Elevated BP at home? Elevated sugars?
Clinical Assessment (cont. ) Family History: Cancers? Polycystic kidney disease? Meds: ◦ Any non-compliance with diabetic or hypertensive meds? ◦ Any recent antibiotic use? ◦ Any NSAID use?
Clinical Assessment– Physical exam Vital Signs: Elevated BP: Concern for malignant hypertension Low BP: Concern for hypotension/hypoperfusion (acute tubular necrosis) Neuro: Confusion: hypercalcemia, uremia, malignant hypertension, infection, malignancy HEENT: Dry mucus membranes: Concern for dehydration (pre-renal) Abd: Ascites: Concern for liver disease (hepatorenal syndrome), or nephrotic syndrome Ext: Edema: Concern for nephrotic syndrome Skin: Tight skin, sclerodactyly – Sclerodermal renal crisis Malar rash - Lupus
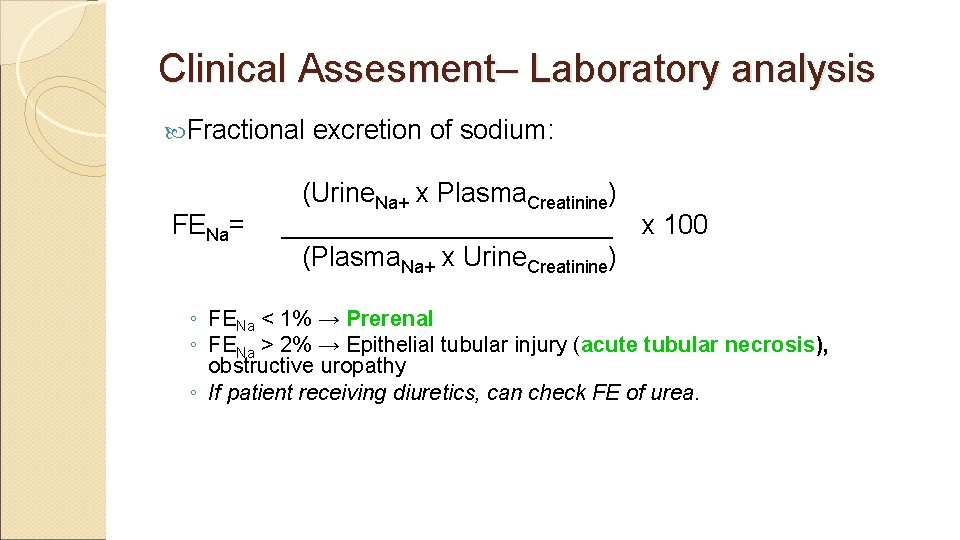
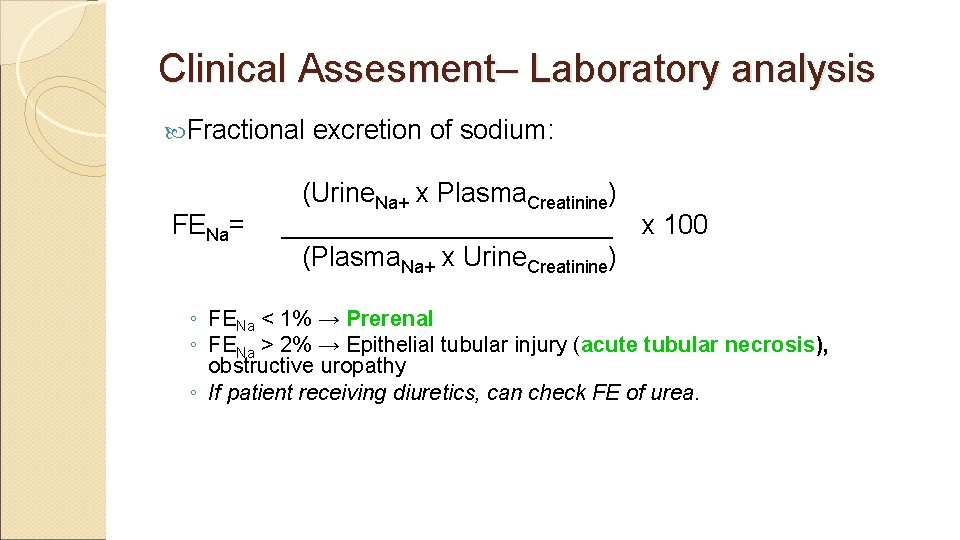
Clinical Assesment– Laboratory analysis Fractional excretion of sodium: (Urine. Na+ x Plasma. Creatinine) FENa= ___________ x 100 (Plasma. Na+ x Urine. Creatinine) ◦ FENa < 1% → Prerenal ◦ FENa > 2% → Epithelial tubular injury (acute tubular necrosis), obstructive uropathy ◦ If patient receiving diuretics, can check FE of urea.
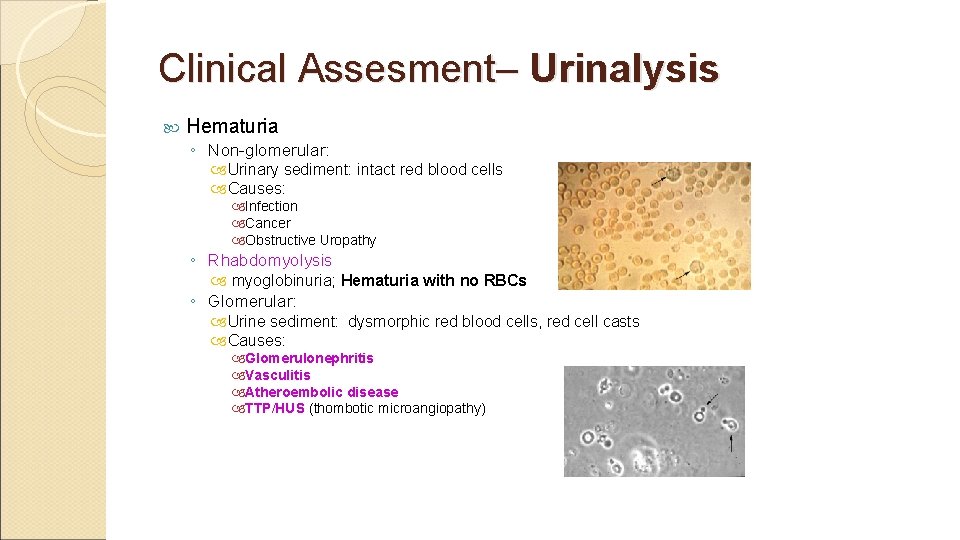
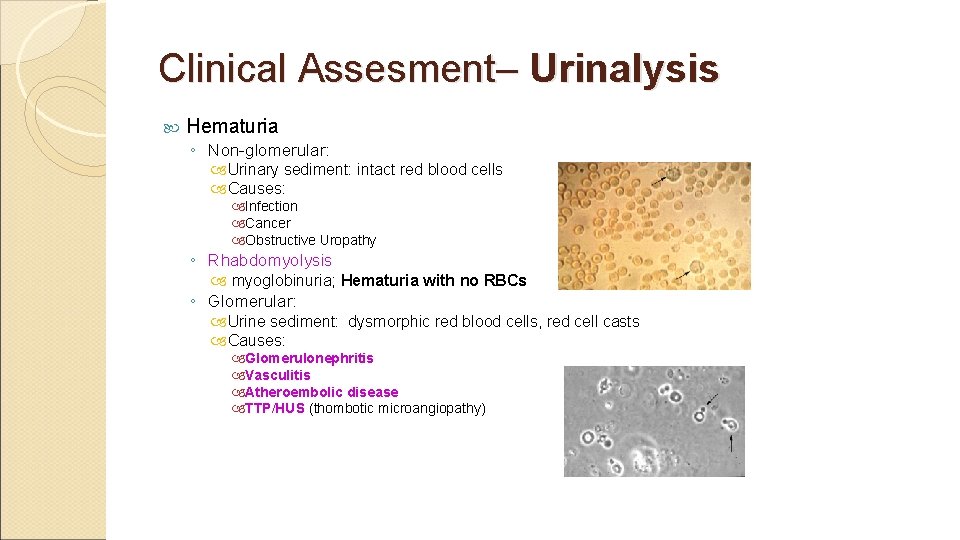
Clinical Assesment– Urinalysis Hematuria ◦ Non-glomerular: Urinary sediment: intact red blood cells Causes: Infection Cancer Obstructive Uropathy ◦ Rhabdomyolysis myoglobinuria; Hematuria with no RBCs ◦ Glomerular: Urine sediment: dysmorphic red blood cells, red cell casts Causes: Glomerulonephritis Vasculitis Atheroembolic disease TTP/HUS (thombotic microangiopathy)
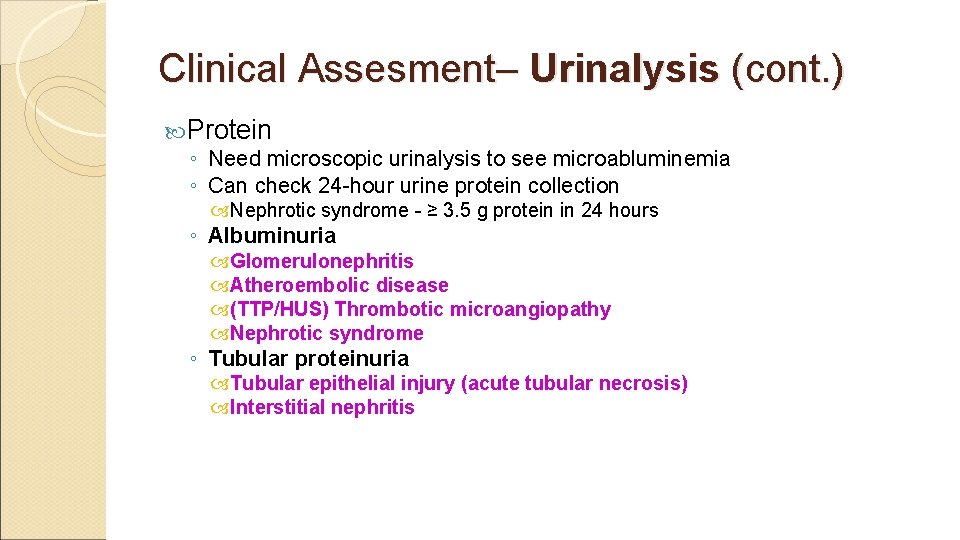
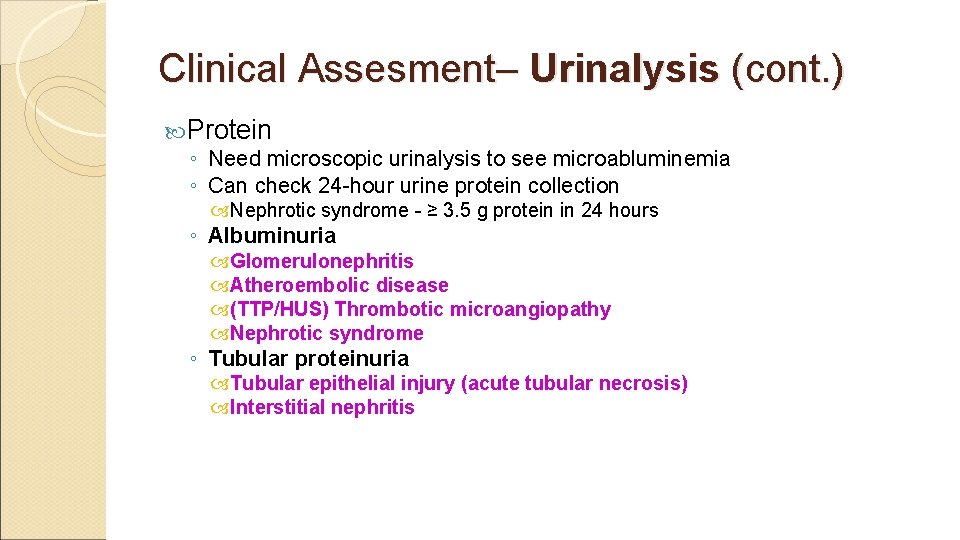
Clinical Assesment– Urinalysis (cont. ) Protein ◦ Need microscopic urinalysis to see microabluminemia ◦ Can check 24 -hour urine protein collection Nephrotic syndrome - ≥ 3. 5 g protein in 24 hours ◦ Albuminuria Glomerulonephritis Atheroembolic disease (TTP/HUS) Thrombotic microangiopathy Nephrotic syndrome ◦ Tubular proteinuria Tubular epithelial injury (acute tubular necrosis) Interstitial nephritis

Clinical Assesment-- Radiology Renal Ultrasound ◦ Look for signs of hydronephrosis as sign of obstructive uropathy.
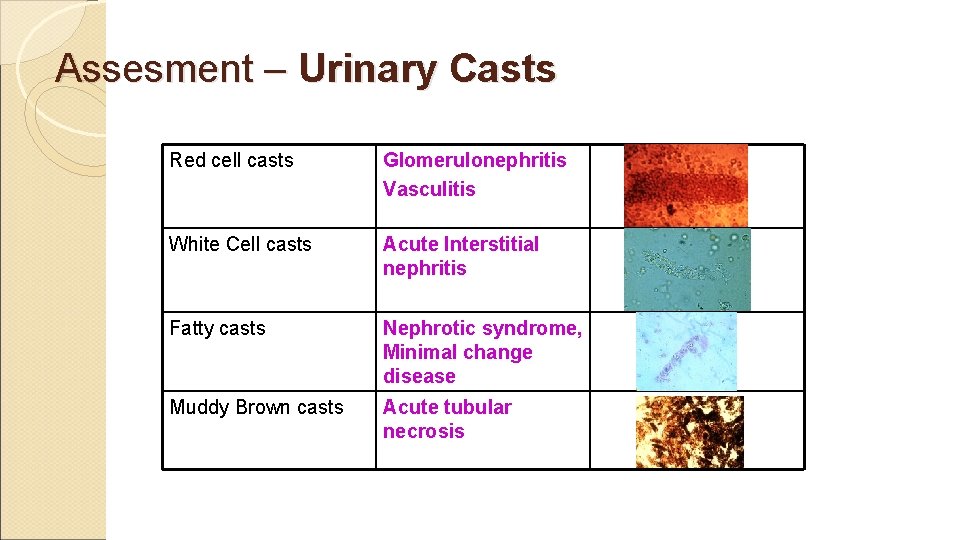
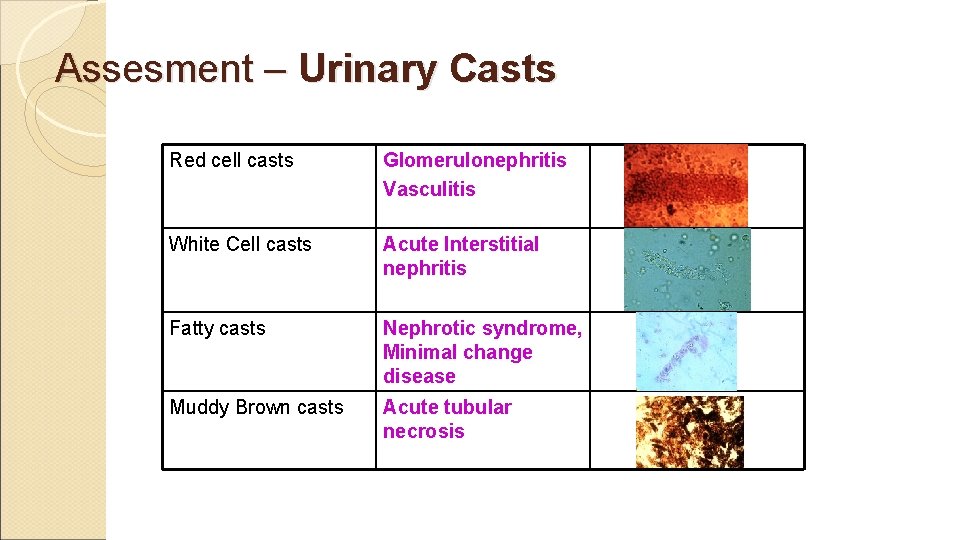
Assesment – Urinary Casts Red cell casts Glomerulonephritis Vasculitis White Cell casts Acute Interstitial nephritis Fatty casts Nephrotic syndrome, Minimal change disease Muddy Brown casts Acute tubular necrosis
Assesment– Renal Biopsy If unable to discover cause of renal disease, renal biopsy may be warranted. Renal biopsy frequently performed in patient’s with history of renal transplant with worsening renal function.
Treatment of Acute Renal Failure Treat underlying cause Blood pressure Infections Stop inciting medications Nephrostomy tubes/ureteral stents if obstruction Treat scleroderma renal crisis with ACE inhibitor Hydration Diuresis (Lasix) Dialysis Renal Transplant
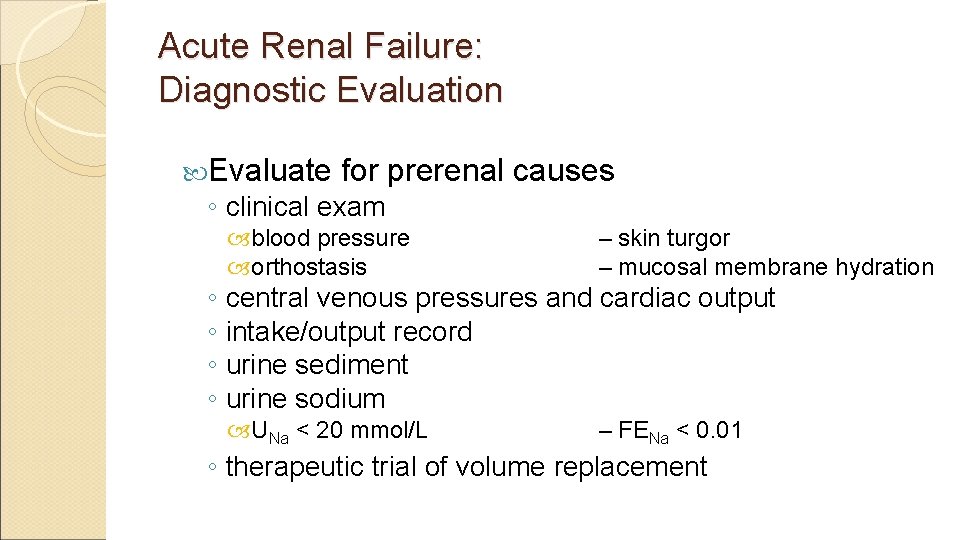
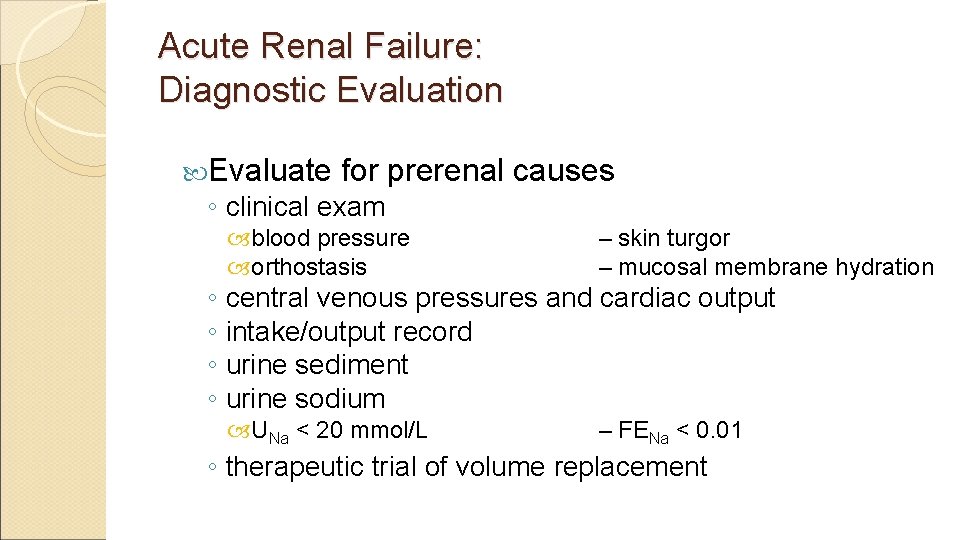
Acute Renal Failure: Diagnostic Evaluation Evaluate for prerenal causes ◦ clinical exam blood pressure orthostasis – skin turgor – mucosal membrane hydration UNa < 20 mmol/L – FENa < 0. 01 ◦ central venous pressures and cardiac output ◦ intake/output record ◦ urine sediment ◦ urine sodium ◦ therapeutic trial of volume replacement
Acute Renal Failure: Diagnostic Evaluation Evaluate for postrenal causes ◦ bladder catheterization ◦ renal ultrasound

Acute Renal Failure: Diagnostic Evaluation for intrinsic ARF ◦ clinical history medications hypotension – radiocontrast agents – sepsis crystals paraproteins – cells – casts ◦ physical exam ◦ urinalysis
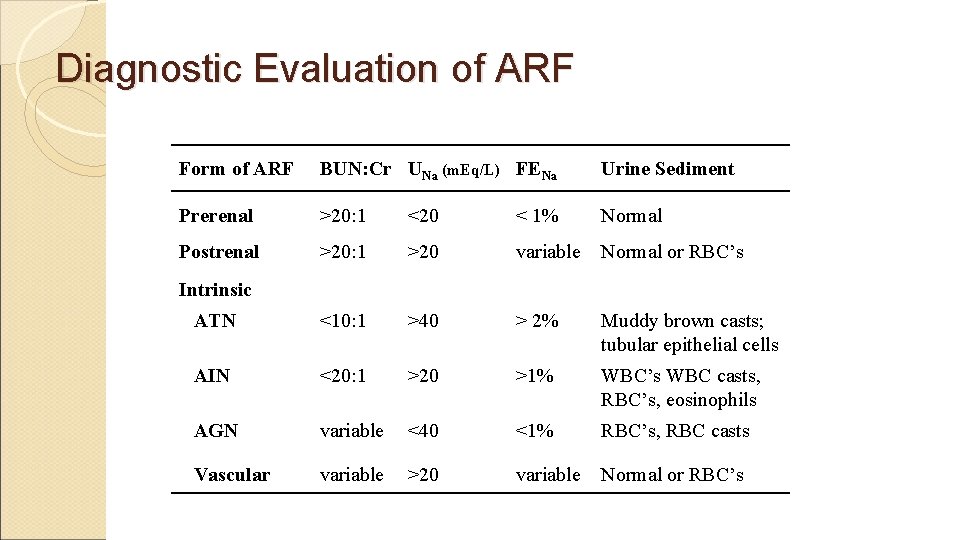
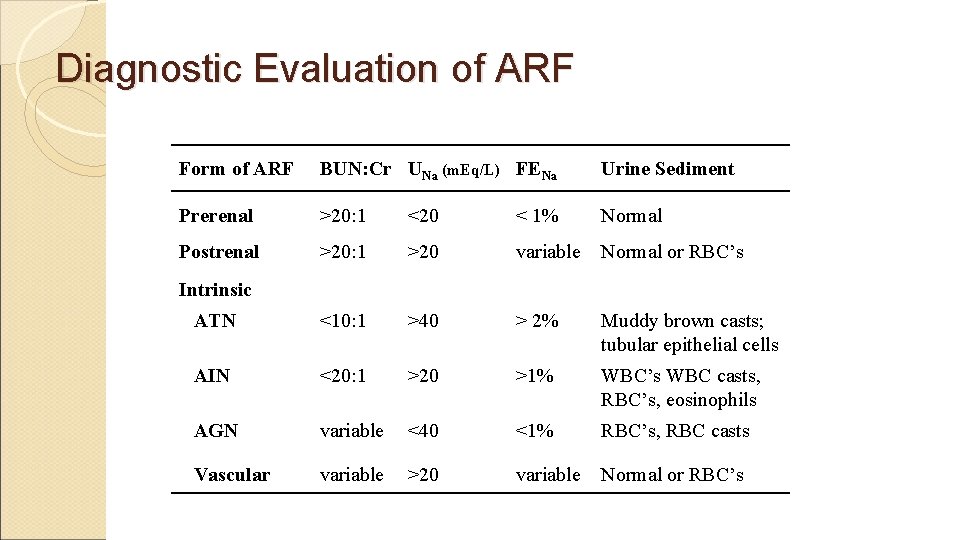
Diagnostic Evaluation of ARF Form of ARF BUN: Cr UNa (m. Eq/L) FENa Urine Sediment Prerenal >20: 1 <20 < 1% Normal Postrenal >20: 1 >20 variable Normal or RBC’s ATN <10: 1 >40 > 2% Muddy brown casts; tubular epithelial cells AIN <20: 1 >20 >1% WBC’s WBC casts, RBC’s, eosinophils AGN variable <40 <1% RBC’s, RBC casts Vascular variable >20 variable Normal or RBC’s Intrinsic

Acute Renal Failure: Management Prerenal ARF ◦ volume repletion ◦ inotropic support ◦ discontinue diuretics Postrenal ARF ◦ bladder catheterization ◦ percutaneous nephrostomy or ureteral stents ◦ fluid management during post-obstructive diuresis
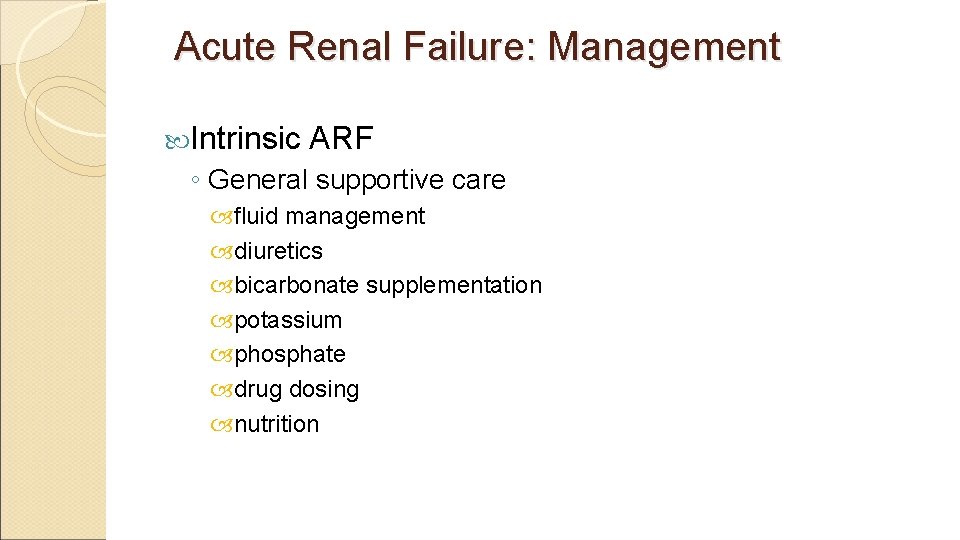
Acute Renal Failure: Management Intrinsic ARF ◦ General supportive care fluid management diuretics bicarbonate supplementation potassium phosphate drug dosing nutrition
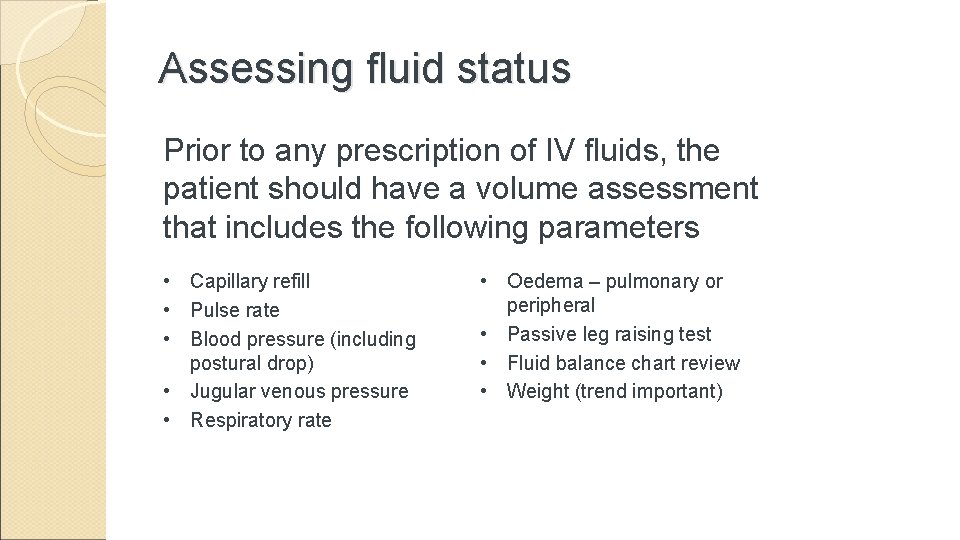
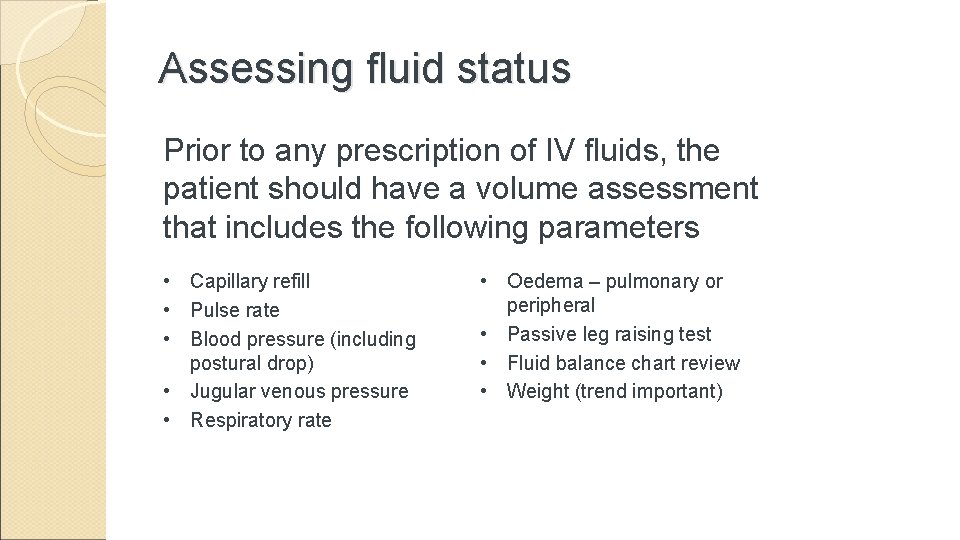
Assessing fluid status Prior to any prescription of IV fluids, the patient should have a volume assessment that includes the following parameters • Capillary refill • Pulse rate • Blood pressure (including postural drop) • Jugular venous pressure • Respiratory rate • Oedema – pulmonary or peripheral • Passive leg raising test • Fluid balance chart review • Weight (trend important)
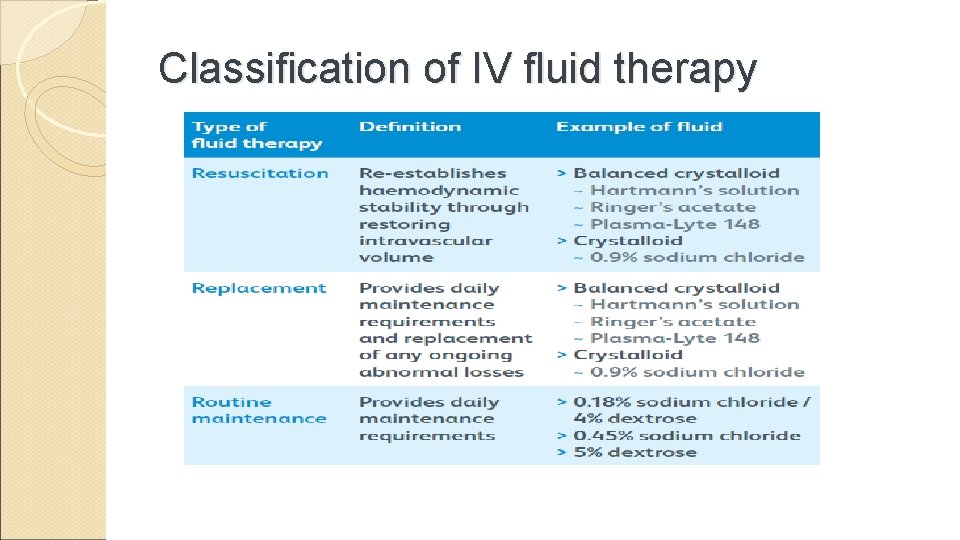
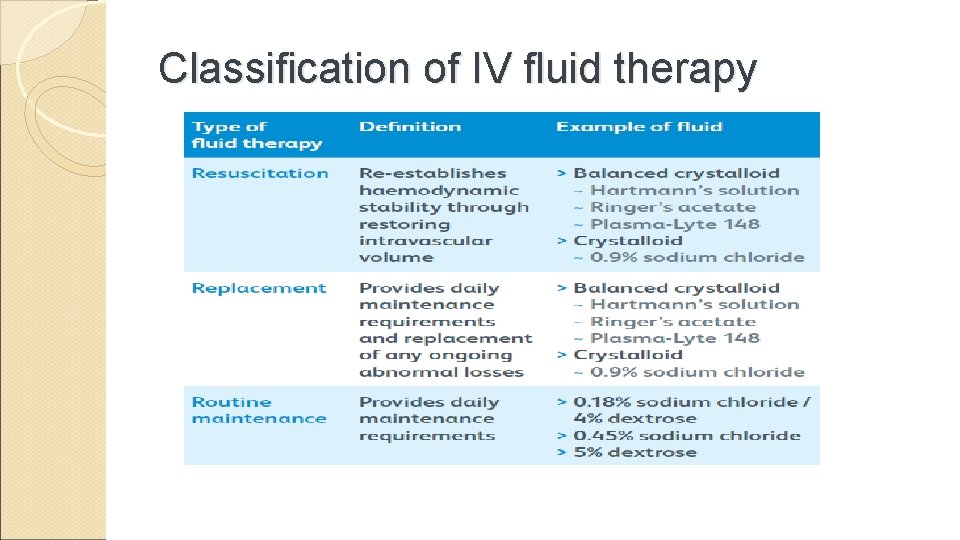
Classification of IV fluid therapy
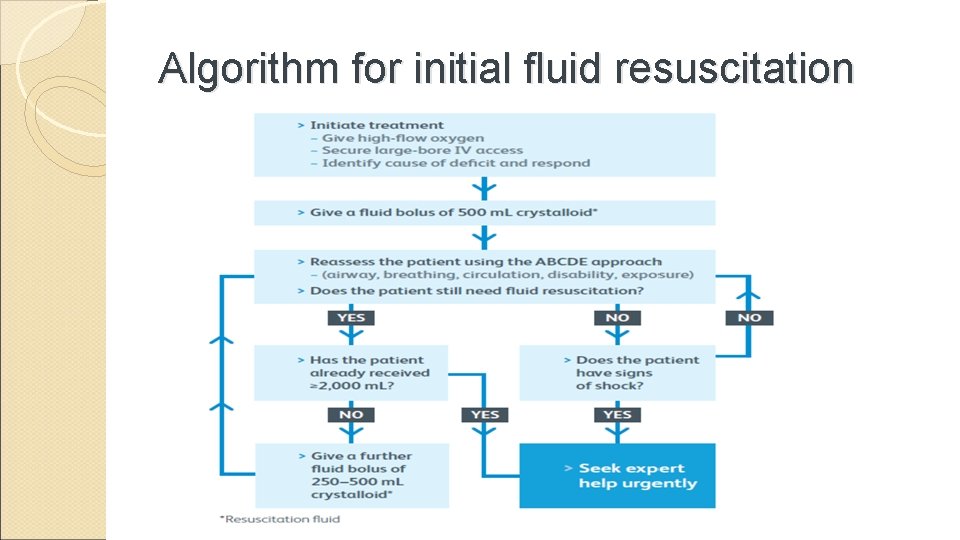
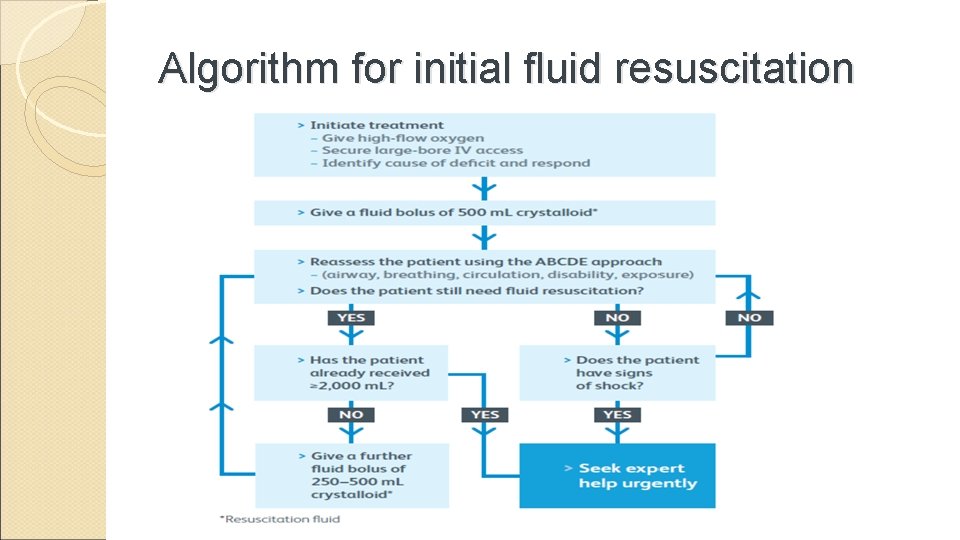
Algorithm for initial fluid resuscitation
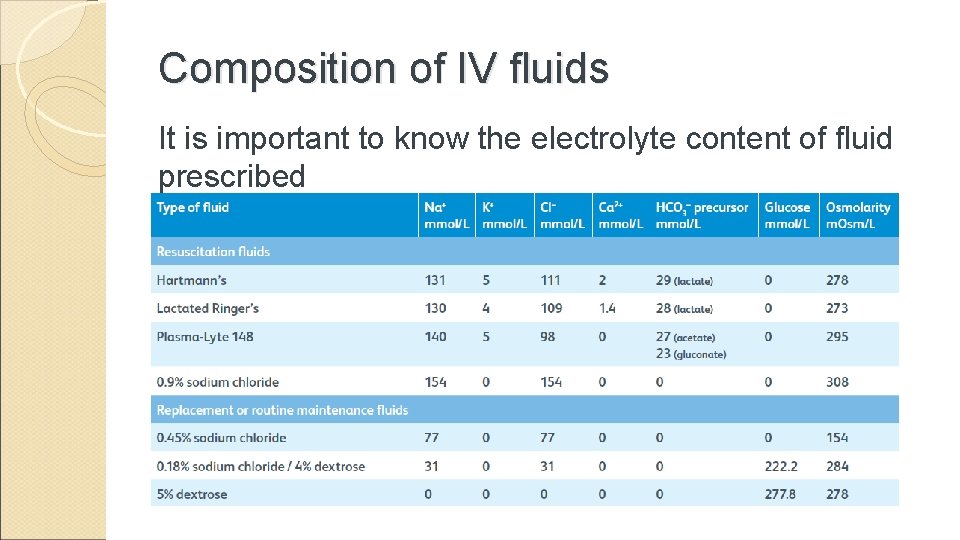
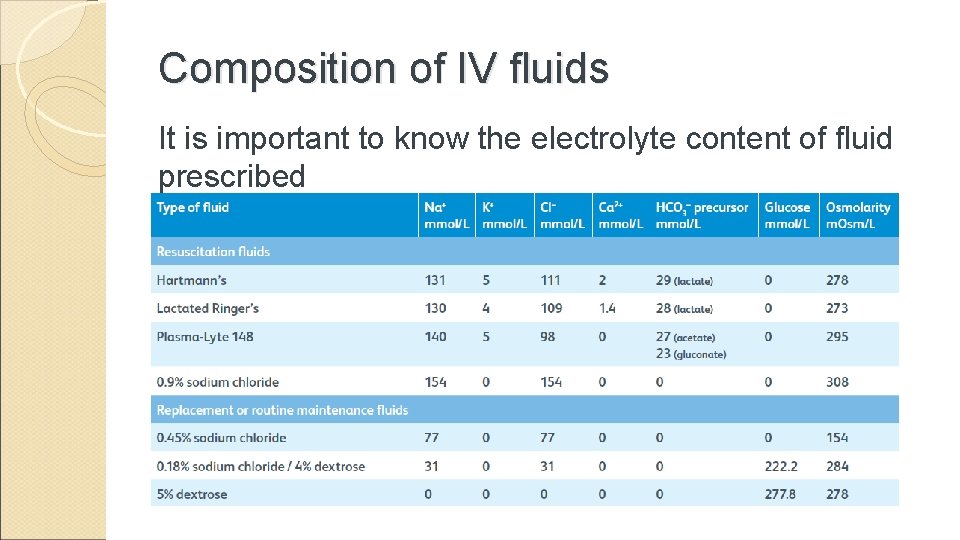
Composition of IV fluids It is important to know the electrolyte content of fluid prescribed
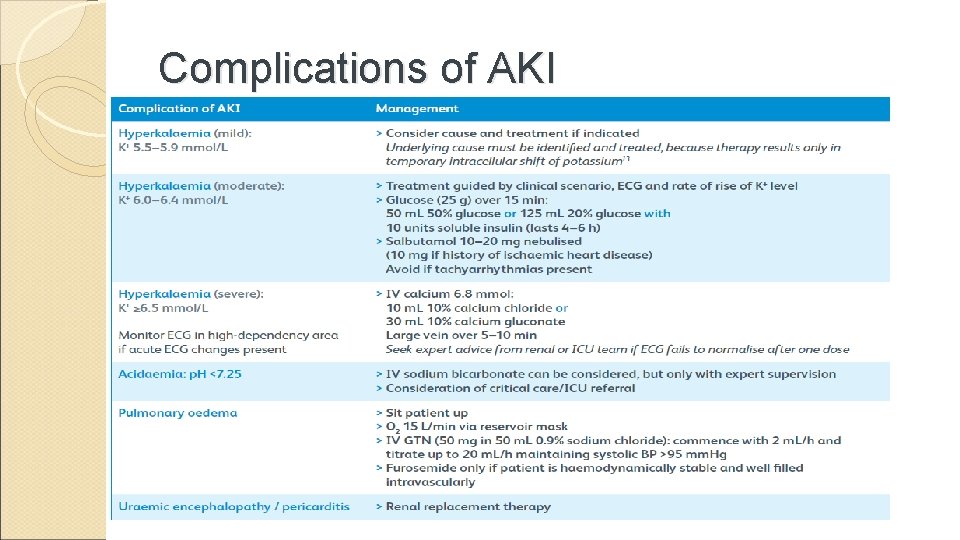
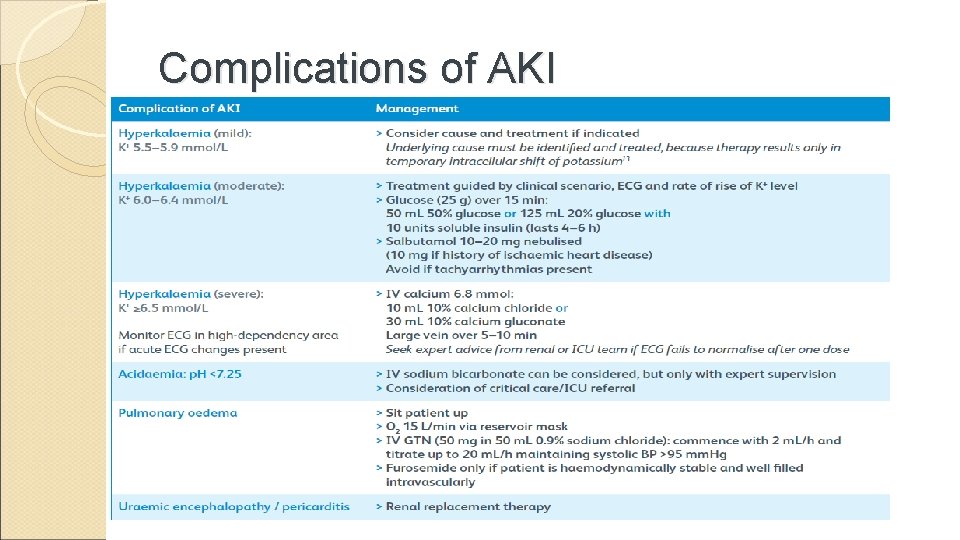
Complications of AKI
Referring to a nephrologist • Management of AKI should be discussed with a nephrologist as soon as possible, and within 24 h of detection when one or more of the following is present – A possible diagnosis that may necessitate specialist treatment (eg vasculitis, glomerulonephritis, tubulointerstitial nephritis or myeloma) – AKI with no clear cause – Inadequate response to treatment – Complications associated with AKI – AKI stage 3 – A renal transplant – Chronic kidney disease (CKD) stage 4 or 5
Indications for Hemodialysis Refractory fluid overload Hyperkalemia (plasma potassium concentration >6. 5 meq/L) or rapidly rising potassium levels Metabolic acidosis (p. H less than 7. 1) Azotemia (BUN greater than 80 to 100 mg/d. L [29 to 36 mmol/L]) Signs of uremia, such as pericarditis, neuropathy, or an otherwise unexplained decline in mental status Severe dysnatremias (sodium concentration greater than 155 meq/L or less than 120 meq/L) Hyperthermia Overdose with a dialyzable drug/toxin
CONCLUSION AKI is an irreversible decline in renal function xterised by increased blood nitrogenous waste. Most causes are pre-renal of which fluid depletion accounts for over 70% Prompt detection and treatment are key to management