Urine Formation by the Kidneys I Glomerular Filtration
Urine Formation by the Kidneys: I. Glomerular Filtration, Renal Blood Flow and Their Control Yanal A Shafagoj. MD, Ph. D 1
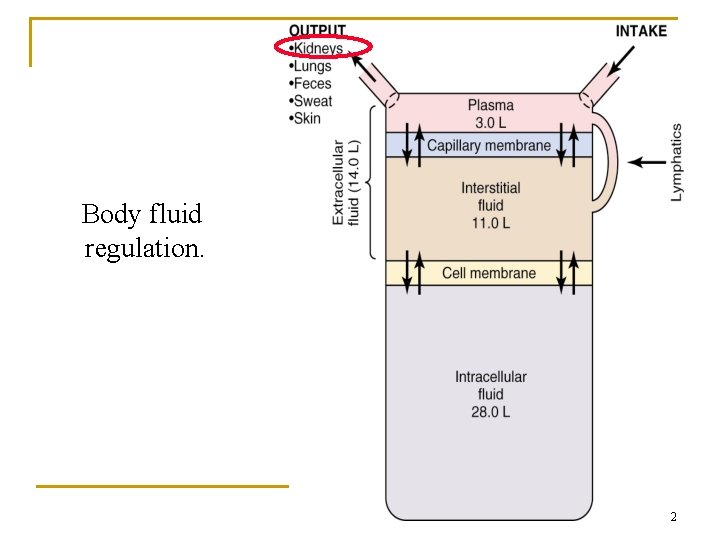
Body fluid regulation. 2
Summary of Kidney Functions • Excretion of metabolic waste products urea, creatinine, bilirubin, hydrogen • Excretion of foreign chemicals: drugs, toxins, pesticides, food additives • Secretion, metabolism, and excretion of hormones - renal erythropoetic factor (erythropoietin) - 1, 25 dihydroxycholecalciferol (Vitamin D) - renin Hormones metabolized and excreted by the kidney - Most peptide hormones (e. g. insulin, angiotensin II, etc • Regulation of acid-base balance • Gluconeogenesis: glucose synthesis from amino acids • Control of arterial pressure • Regulation of water & electrolyte excretion 3
Excretion of Metabolic Waste Products • Urea (from protein metabolism) • Uric acid (from nucleic acid metabolism) • Creatinine (from muscle metabolism) • Bilirubin (from hemoglobin metabolism) 4
Excretion of Foreign Chemicals • Pesticides • Food additives • Toxins • Drugs 5
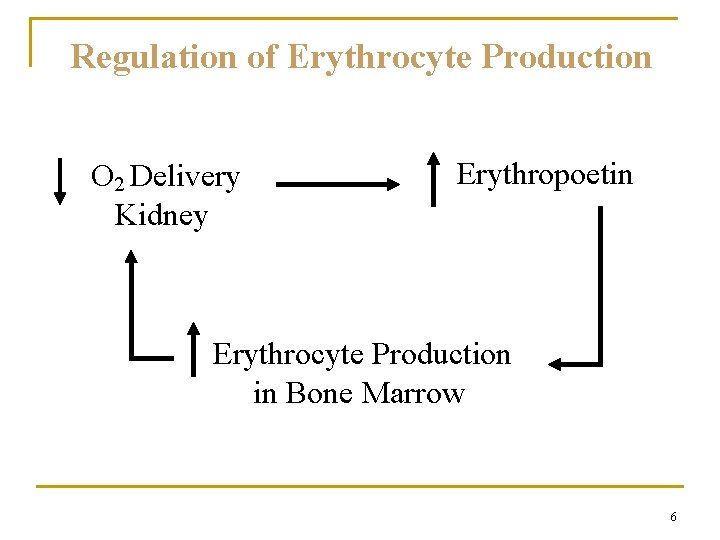
Regulation of Erythrocyte Production O 2 Delivery Kidney Erythropoetin Erythrocyte Production in Bone Marrow 6
Regulation of Vitamin D Activity • Kidney produces active form of vitamin D (1, 25 dihydroxy vitamin D 3 ) • Vitamin D 3 is important in calcium and phosphate metabolism 7
Regulation of Acid-Base Balance • Excrete acids (kidneys are the only means of excreting non-volatile acids) • Regulate body fluid buffers (e. g. Bicarbonate) 8
Glucose Synthesis Gluconeogenesis: kidneys synthesize glucose from precursors (e. g. , amino acids) during prolonged fasting 9
Regulation of Arterial Pressure Endocrine Organ • renin-angiotensin system • prostaglandins • kallikrein-kinin system Control of Extracellular Fluid Volume 10
Regulation of Water and Electrolyte Balances • Sodium and Water • Potassium • Hydrogen Ions • Calcium, Phosphate, Magnesium 11
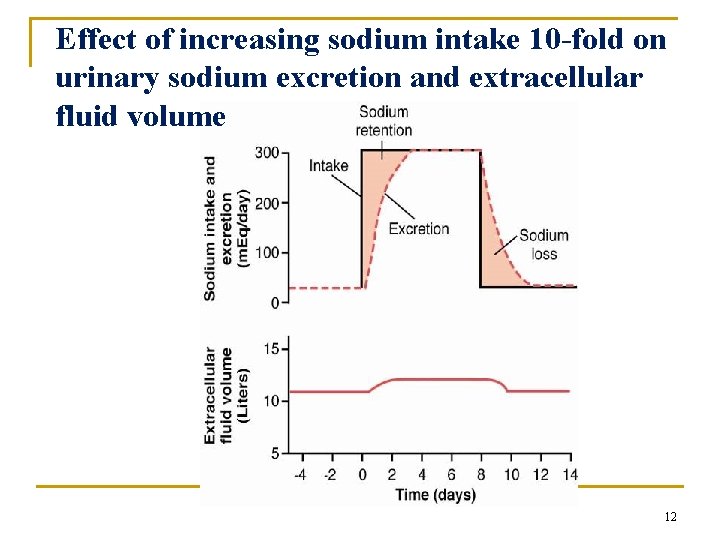
Effect of increasing sodium intake 10 -fold on urinary sodium excretion and extracellular fluid volume 12
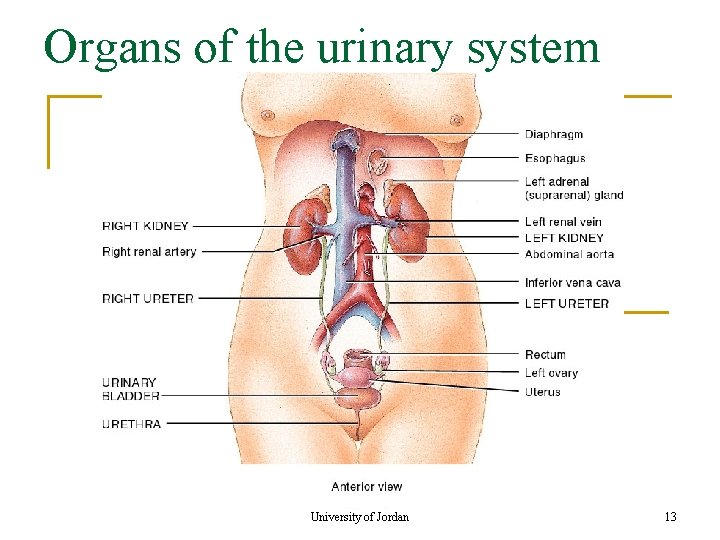
Organs of the urinary system University of Jordan 13
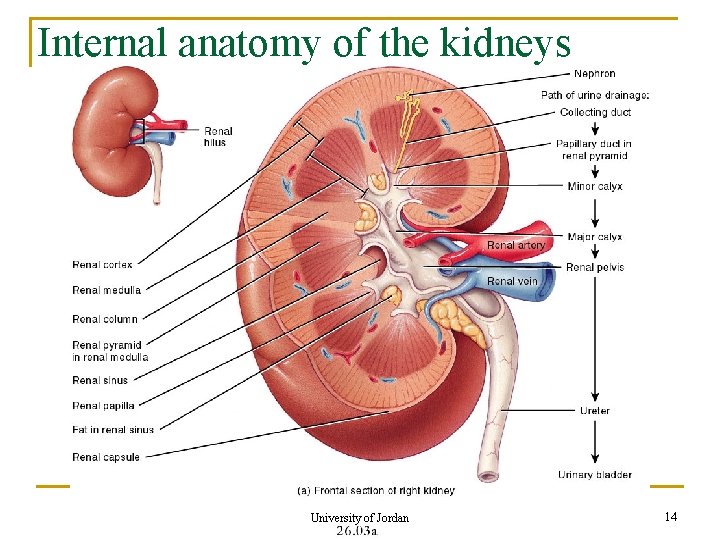
Internal anatomy of the kidneys University of Jordan 14
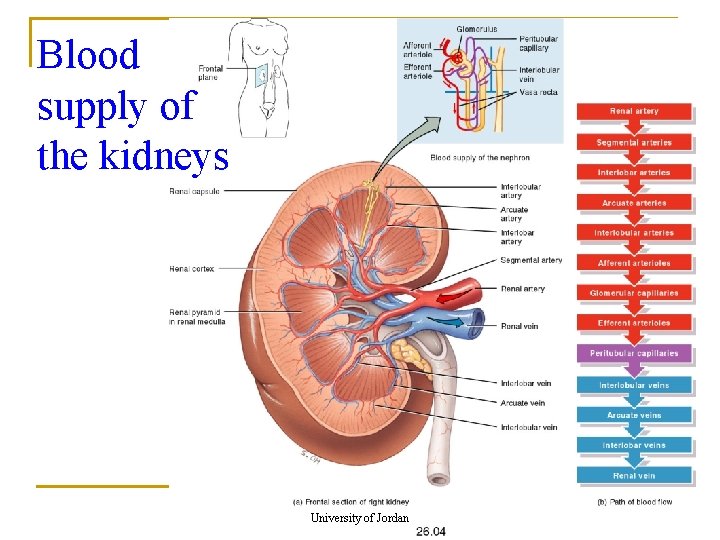
Blood supply of the kidneys University of Jordan 15
n n The kidney weighs 113 -170 gm. Renal artery arises as the fifth branch of the abdominal aorta. The renal artery arises from the aorta at the level of the second lumber vertebra. Because the aorta is to the left of the midline, the right renal artery is longer. The inferior vena cava lies to the right midline making the left renal vein two times longer than the right renal vein. For this reason it is better to take the donor left kidney (short artery, long vein) & place it in the right pelvis of the recipient. Multiple arteries & veins can supply the kidney. 16
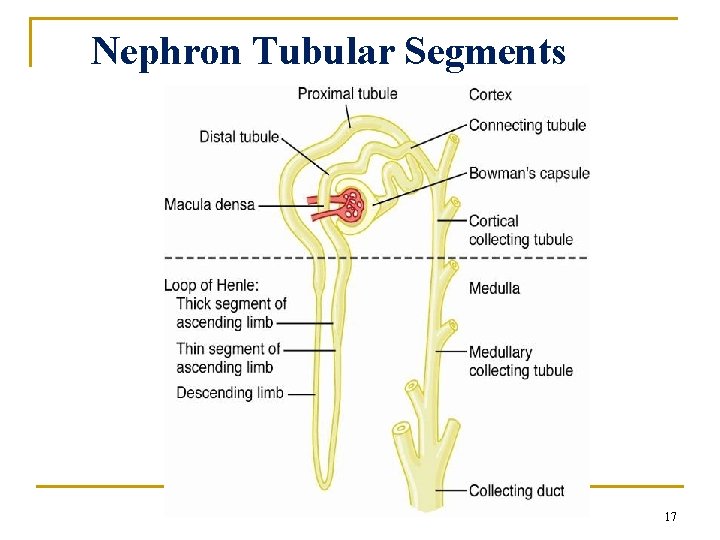
Nephron Tubular Segments 17
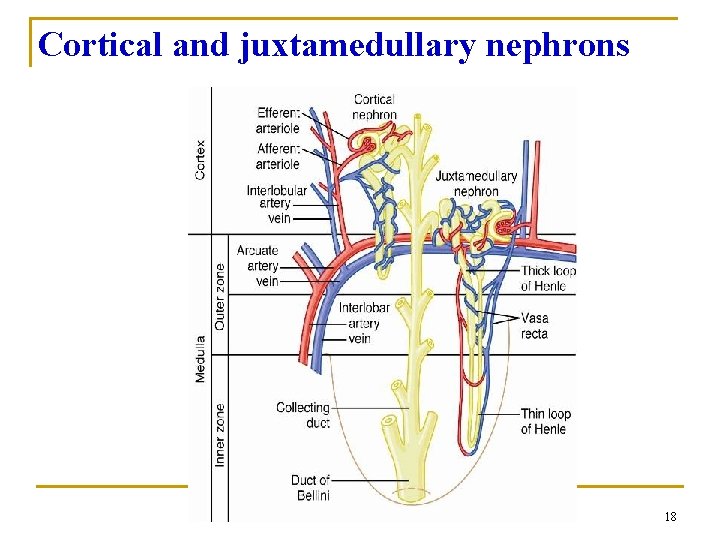
Cortical and juxtamedullary nephrons 18
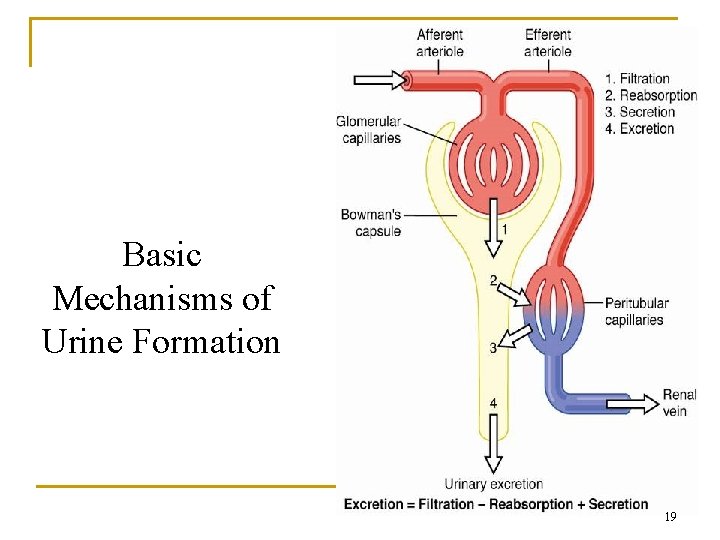
Basic Mechanisms of Urine Formation 19
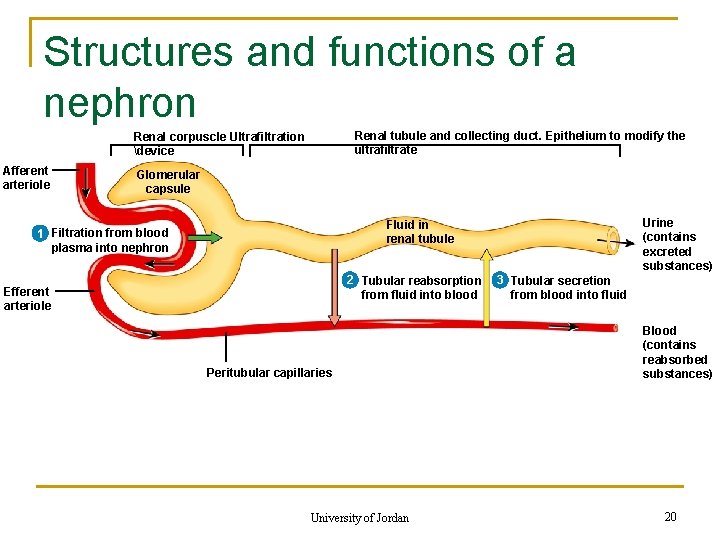
Structures and functions of a nephron Renal tubule and collecting duct. Epithelium to modify the ultrafiltrate Renal corpuscle Ultrafiltration device Afferent arteriole Glomerular capsule Urine (contains excreted substances) Fluid in renal tubule 1 Filtration from blood plasma into nephron 2 Tubular reabsorption from fluid into blood Efferent arteriole Peritubular capillaries University of Jordan 3 Tubular secretion from blood into fluid Blood (contains reabsorbed substances) 20
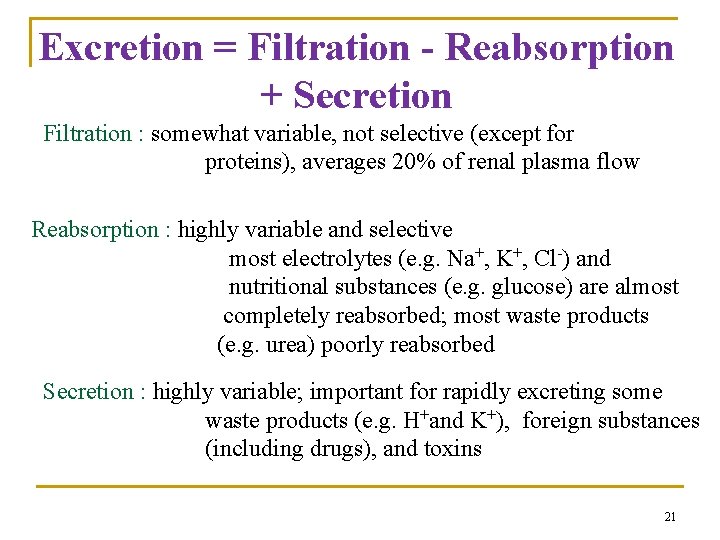
Excretion = Filtration - Reabsorption + Secretion Filtration : somewhat variable, not selective (except for proteins), averages 20% of renal plasma flow Reabsorption : highly variable and selective most electrolytes (e. g. Na+, K+, Cl-) and nutritional substances (e. g. glucose) are almost completely reabsorbed; most waste products (e. g. urea) poorly reabsorbed Secretion : highly variable; important for rapidly excreting some waste products (e. g. H+and K+), foreign substances (including drugs), and toxins 21
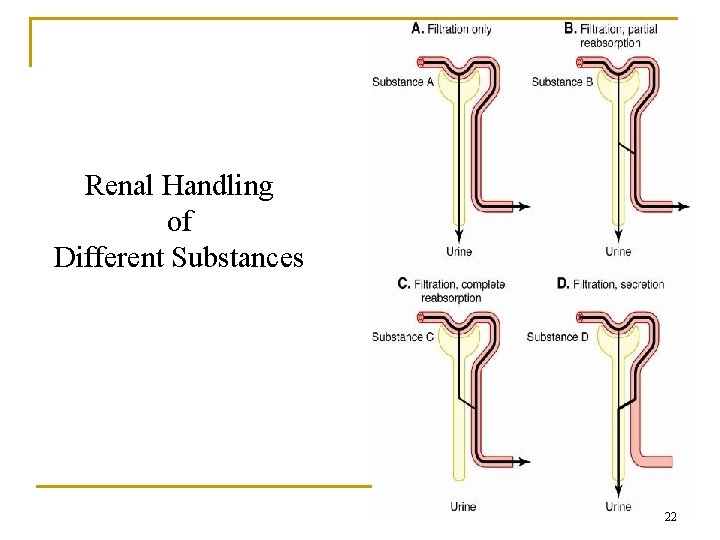
Renal Handling of Different Substances 22
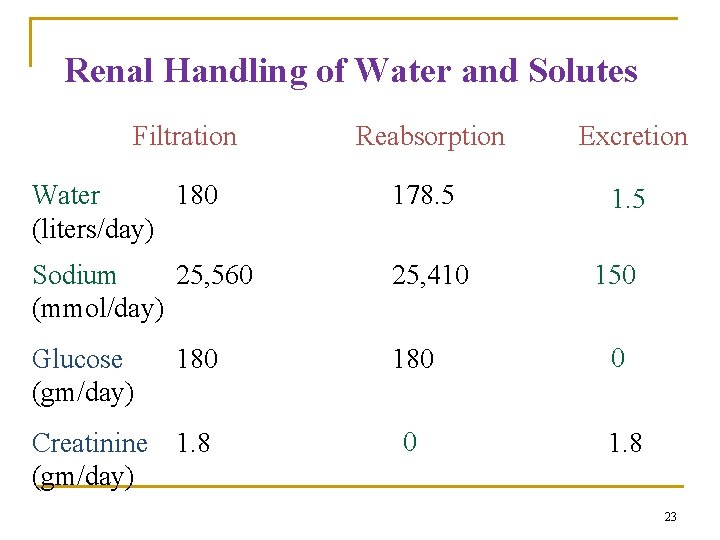
Renal Handling of Water and Solutes Filtration Reabsorption Excretion Water 180 (liters/day) 178. 5 1. 5 Sodium 25, 560 (mmol/day) 25, 410 Glucose (gm/day) 180 0 0 1. 8 180 Creatinine 1. 8 (gm/day) 150 23
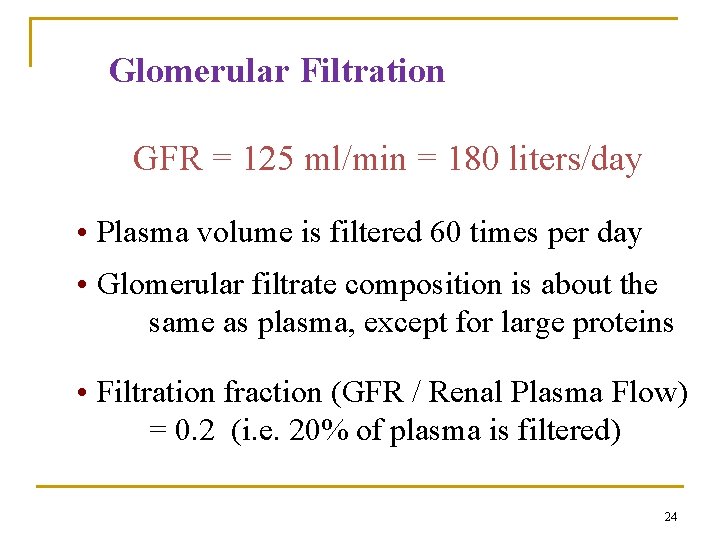
Glomerular Filtration GFR = 125 ml/min = 180 liters/day • Plasma volume is filtered 60 times per day • Glomerular filtrate composition is about the same as plasma, except for large proteins • Filtration fraction (GFR / Renal Plasma Flow) = 0. 2 (i. e. 20% of plasma is filtered) 24
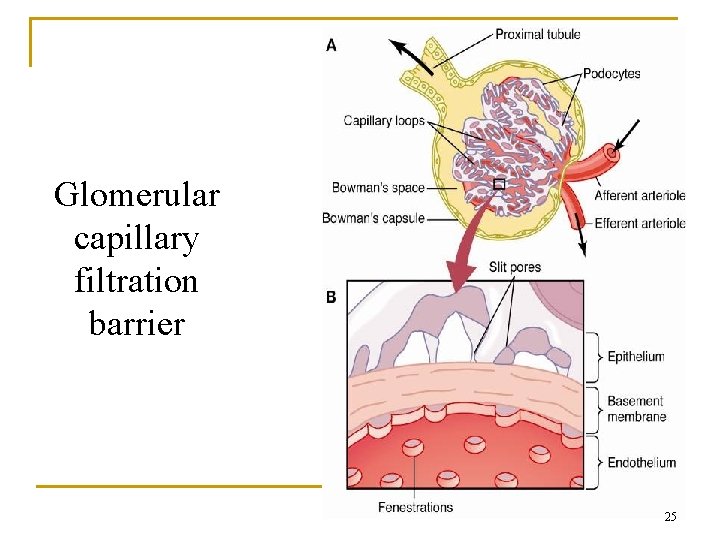
Glomerular capillary filtration barrier 25
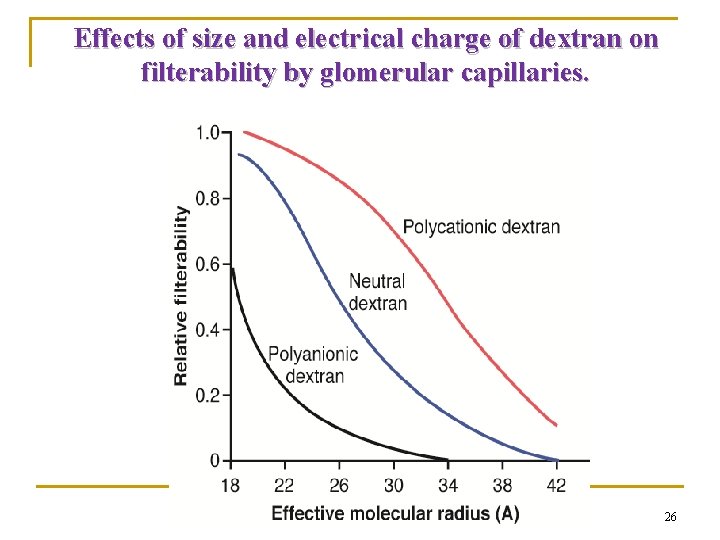
Effects of size and electrical charge of dextran on filterability by glomerular capillaries. 26
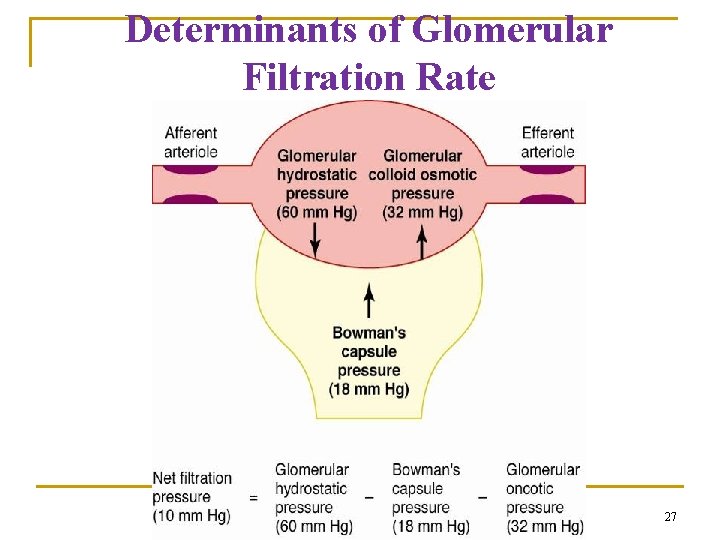
Determinants of Glomerular Filtration Rate 27
Determinants of Glomerular Filtration Rate Normal Values: GFR = 125 ml/min Net Filt. Press = 10 mm. Hg Kf = 12. 5 ml/min per mm. Hg, or 4. 2 ml/min per mm. Hg/ 100 gm (400 x greater than in many tissues) 28
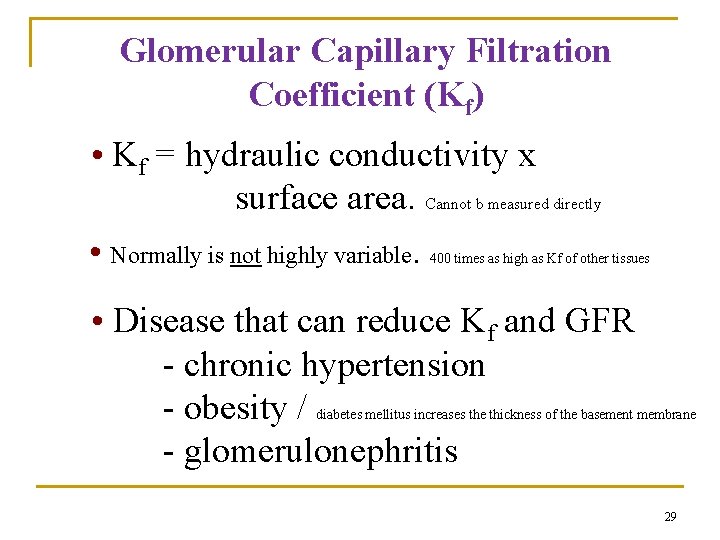
Glomerular Capillary Filtration Coefficient (Kf) • Kf = hydraulic conductivity x surface area. Cannot b measured directly • Normally is not highly variable. 400 times as high as Kf of other tissues • Disease that can reduce Kf and GFR - chronic hypertension - obesity / - glomerulonephritis diabetes mellitus increases the thickness of the basement membrane 29
Bowman’s Capsule hydrostatic Pressure (PB) • Normally changes as a function of GFR, not a physiological regulator of GFR • Tubular Obstruction kidney stones tubular necrosis • Urinary tract obstruction Prostate hypertrophy/cancer 30
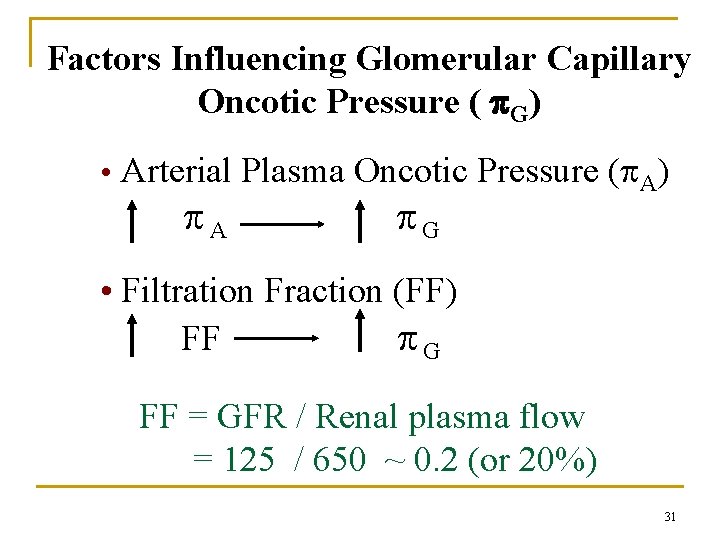
Factors Influencing Glomerular Capillary Oncotic Pressure ( G) • Arterial Plasma Oncotic Pressure ( A) A G • Filtration Fraction (FF) FF G FF = GFR / Renal plasma flow = 125 / 650 ~ 0. 2 (or 20%) 31
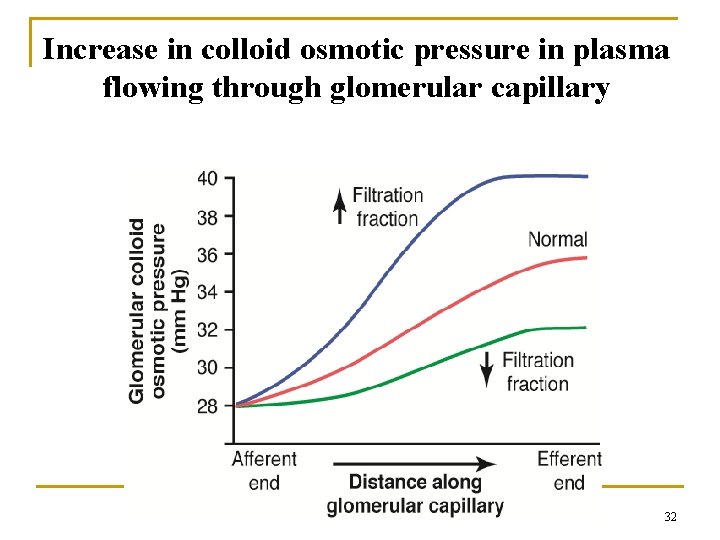
Increase in colloid osmotic pressure in plasma flowing through glomerular capillary 32
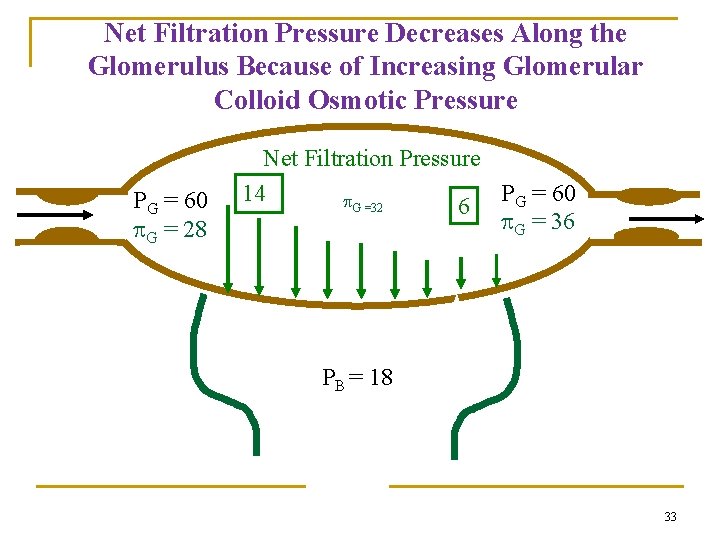
Net Filtration Pressure Decreases Along the Glomerulus Because of Increasing Glomerular Colloid Osmotic Pressure PG = 60 G = 28 Net Filtration Pressure PG = 60 14 G =32 6 G = 36 PB = 18 33
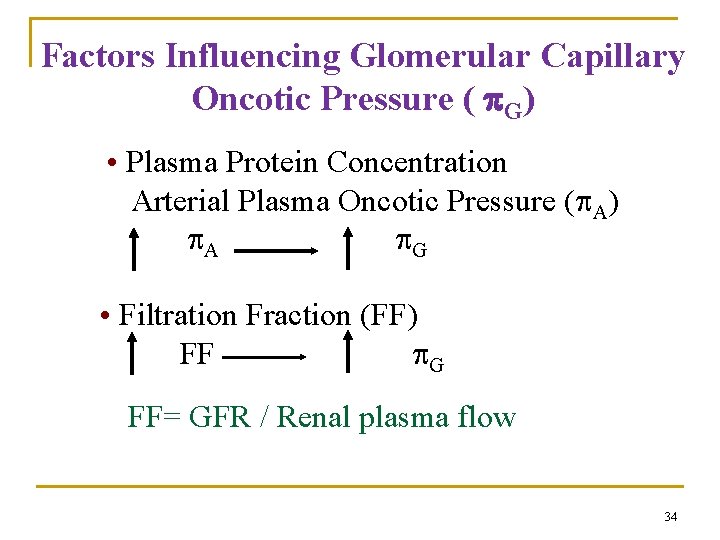
Factors Influencing Glomerular Capillary Oncotic Pressure ( G) • Plasma Protein Concentration Arterial Plasma Oncotic Pressure ( A) A G • Filtration Fraction (FF) FF G FF= GFR / Renal plasma flow 34
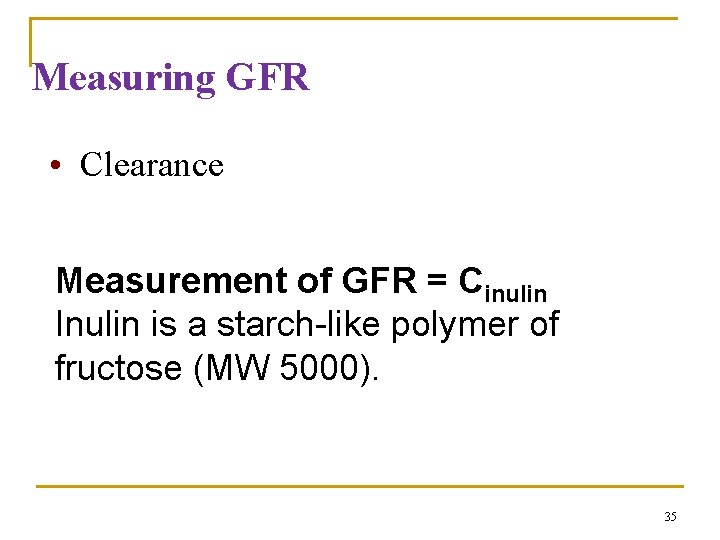
Measuring GFR • Clearance Measurement of GFR = Cinulin Inulin is a starch-like polymer of fructose (MW 5000). 35
36
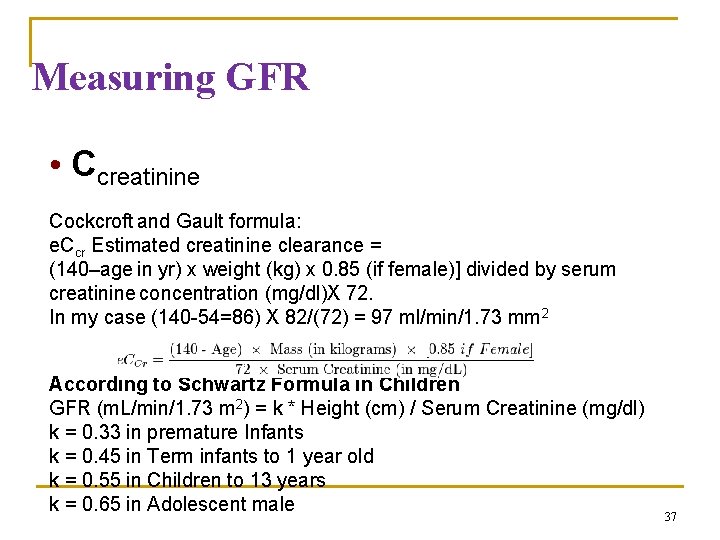
Measuring GFR • Ccreatinine Cockcroft and Gault formula: e. Ccr Estimated creatinine clearance = (140–age in yr) x weight (kg) x 0. 85 (if female)] divided by serum creatinine concentration (mg/dl)X 72. In my case (140 -54=86) X 82/(72) = 97 ml/min/1. 73 mm 2 According to Schwartz Formula in Children GFR (m. L/min/1. 73 m 2) = k * Height (cm) / Serum Creatinine (mg/dl) k = 0. 33 in premature Infants k = 0. 45 in Term infants to 1 year old k = 0. 55 in Children to 13 years k = 0. 65 in Adolescent male 37
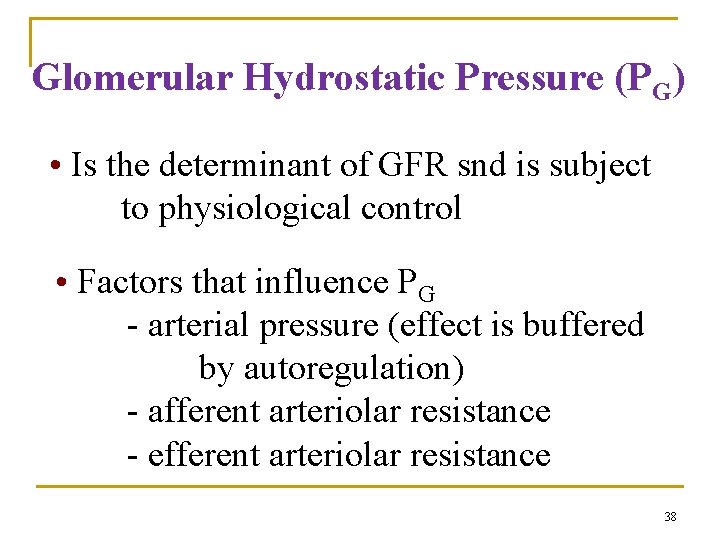
Glomerular Hydrostatic Pressure (PG) • Is the determinant of GFR snd is subject to physiological control • Factors that influence PG - arterial pressure (effect is buffered by autoregulation) - afferent arteriolar resistance - efferent arteriolar resistance 38
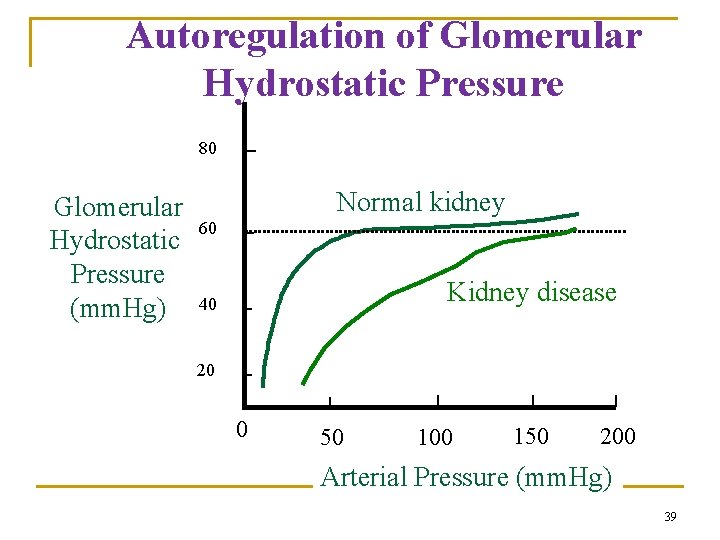
Autoregulation of Glomerular Hydrostatic Pressure 80 Glomerular Hydrostatic Pressure (mm. Hg) Normal kidney 60 Kidney disease 40 20 0 50 100 150 200 Arterial Pressure (mm. Hg) 39
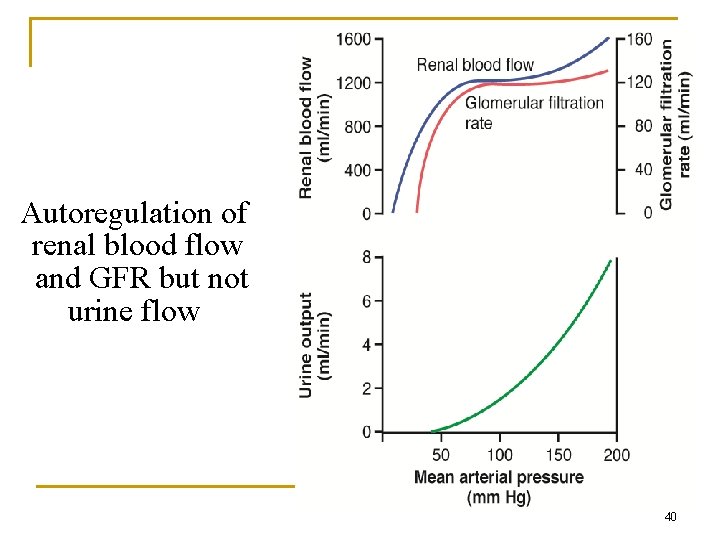
Autoregulation of renal blood flow and GFR but not urine flow 40
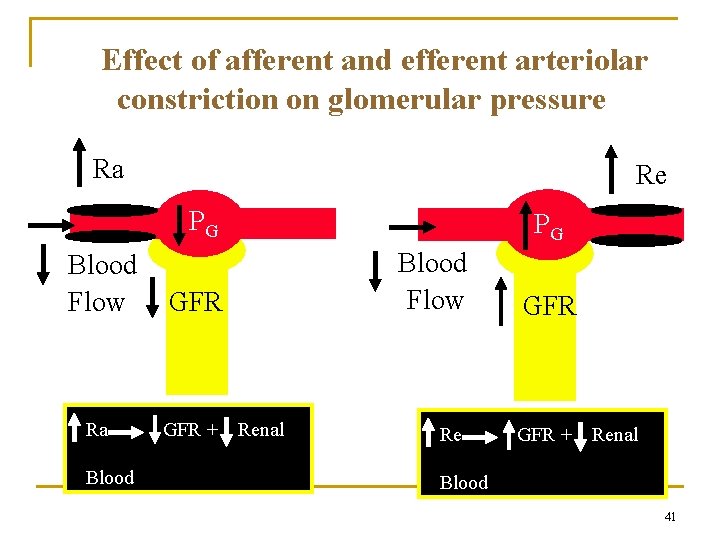
Effect of afferent and efferent arteriolar constriction on glomerular pressure Ra Re PG Blood Flow GFR Ra GFR + Blood Flow PG Renal Blood Flow GFR Re GFR + Renal Blood Flow 41
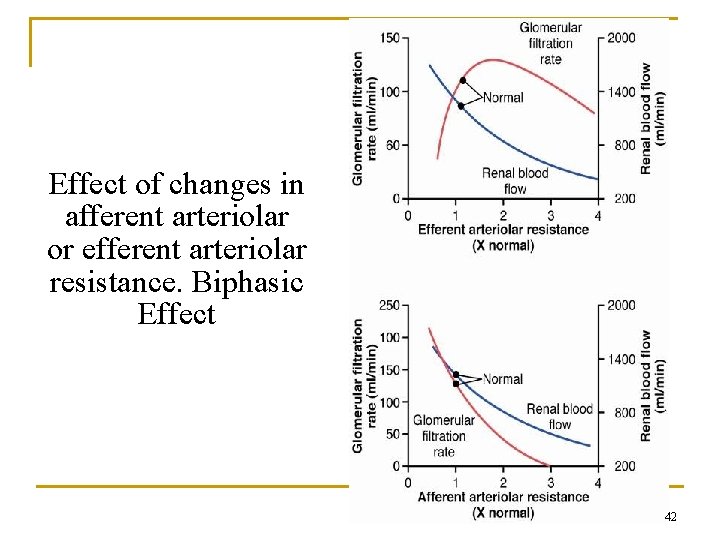
Effect of changes in afferent arteriolar or efferent arteriolar resistance. Biphasic Effect 42
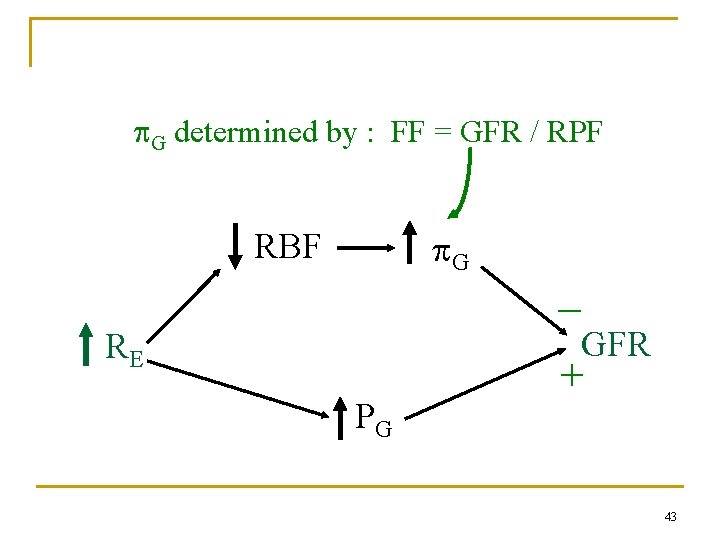
G determined by : FF = GFR / RPF G RBF _ GFR RE PG + 43
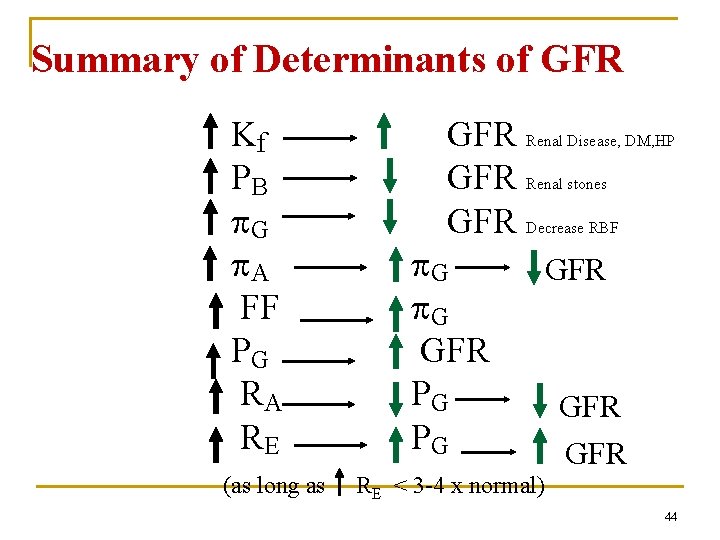
Summary of Determinants of GFR Kf PB G A FF PG RA RE (as long as GFR Renal Disease, DM, HP GFR Renal stones GFR Decrease RBF G G GFR PG PG GFR GFR RE < 3 -4 x normal) 44
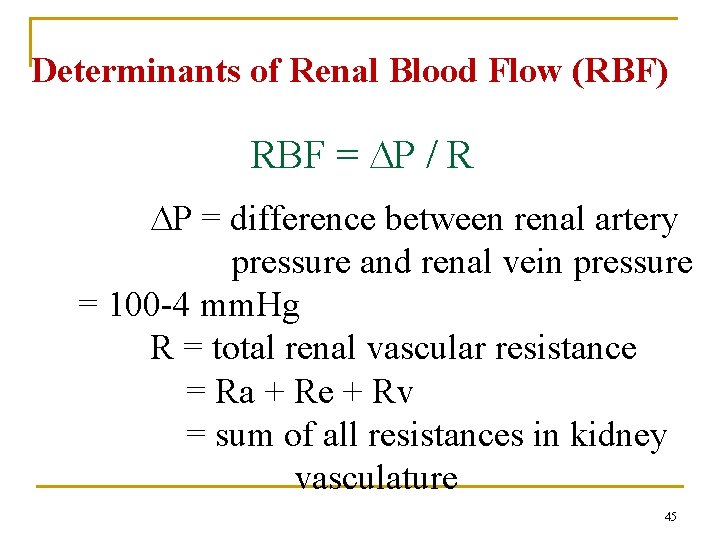
Determinants of Renal Blood Flow (RBF) RBF = P / R P = difference between renal artery pressure and renal vein pressure = 100 -4 mm. Hg R = total renal vascular resistance = Ra + Re + Rv = sum of all resistances in kidney vasculature 45
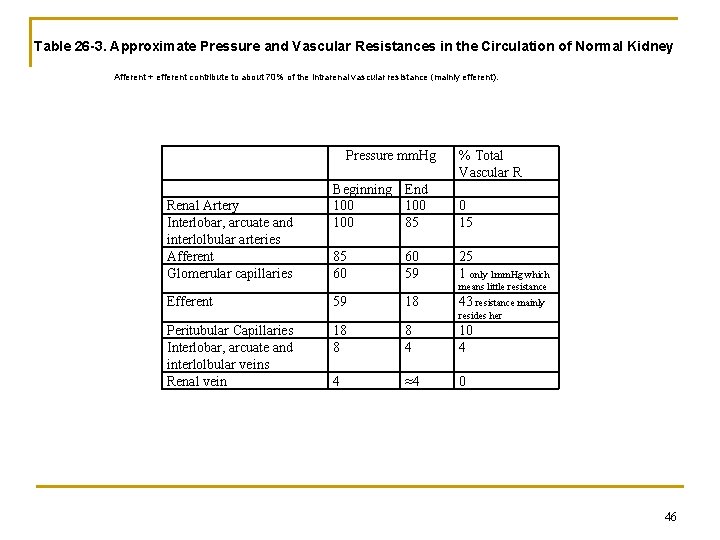
Table 26 -3. Approximate Pressure and Vascular Resistances in the Circulation of Normal Kidney Afferent + efferent contribute to about 70% of the intrarenal vascular resistance (mainly efferent). Pressure mm. Hg Renal Artery Interlobar, arcuate and interlolbular arteries Afferent Glomerular capillaries % Total Vascular R Beginning End 100 100 85 0 15 85 60 25 1 only 1 mm. Hg which 60 59 means little resistance Efferent 59 18 43 resistance mainly resides her Peritubular Capillaries Interlobar, arcuate and interlolbular veins Renal vein 18 8 8 4 10 4 4 ≈4 0 46
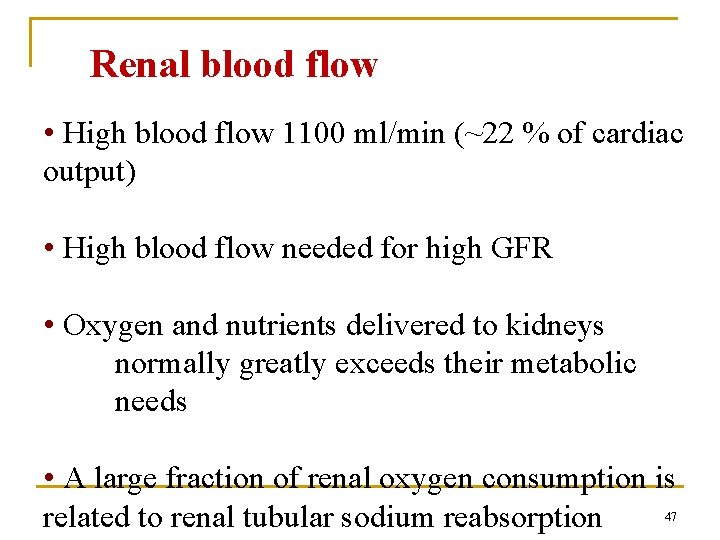
Renal blood flow • High blood flow 1100 ml/min (~22 % of cardiac output) • High blood flow needed for high GFR • Oxygen and nutrients delivered to kidneys normally greatly exceeds their metabolic needs • A large fraction of renal oxygen consumption is related to renal tubular sodium reabsorption 47
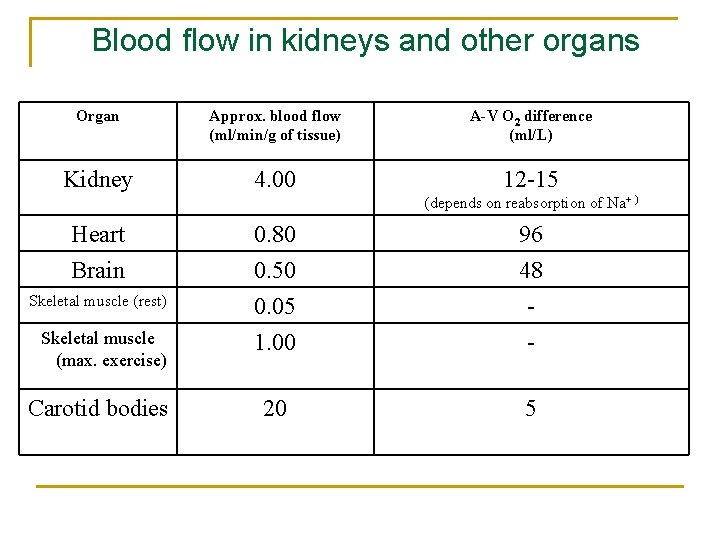
Blood flow in kidneys and other organs Organ Approx. blood flow (ml/min/g of tissue) A-V O 2 difference (ml/L) Kidney 4. 00 12 -15 (depends on reabsorption of Na+ ) Heart 0. 80 96 Brain 0. 50 48 Skeletal muscle (rest) 0. 05 - Skeletal muscle (max. exercise) 1. 00 - 20 5 Carotid bodies
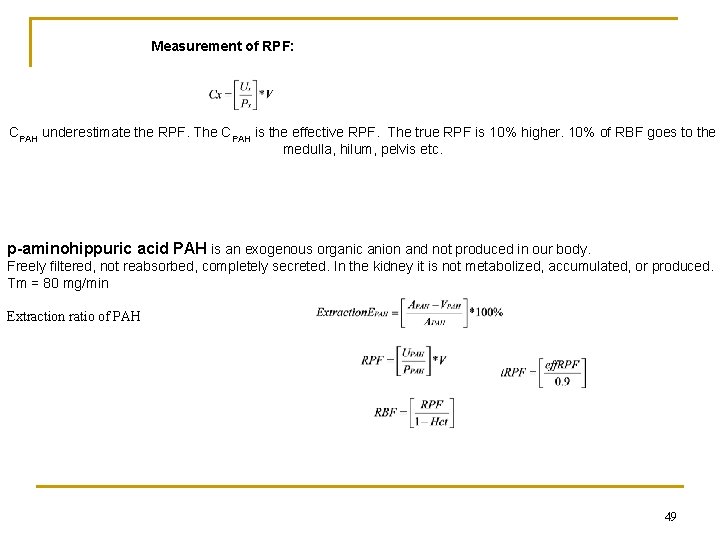
Measurement of RPF: CPAH underestimate the RPF. The CPAH is the effective RPF. The true RPF is 10% higher. 10% of RBF goes to the medulla, hilum, pelvis etc. p-aminohippuric acid PAH is an exogenous organic anion and not produced in our body. Freely filtered, not reabsorbed, completely secreted. In the kidney it is not metabolized, accumulated, or produced. Tm = 80 mg/min Extraction ratio of PAH 49
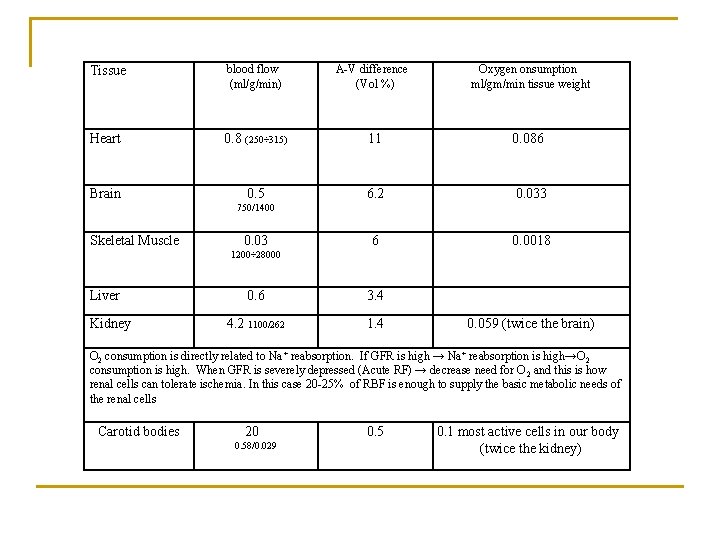
Tissue blood flow (ml/g/min) A-V difference (Vol %) Oxygen onsumption ml/gm/min tissue weight Heart 0. 8 (250÷ 315) 11 0. 086 0. 5 6. 2 0. 033 6 0. 0018 Brain 750/1400 Skeletal Muscle 0. 03 1200÷ 28000 Liver Kidney 0. 6 3. 4 4. 2 1100/262 1. 4 0. 059 (twice the brain) O 2 consumption is directly related to Na + reabsorption. If GFR is high → Na+ reabsorption is high→O 2 consumption is high. When GFR is severely depressed (Acute RF) → decrease need for O 2 and this is how renal cells can tolerate ischemia. In this case 20 -25% of RBF is enough to supply the basic metabolic needs of the renal cells Carotid bodies 20 0. 58/0. 029 0. 5 0. 1 most active cells in our body (twice the kidney)
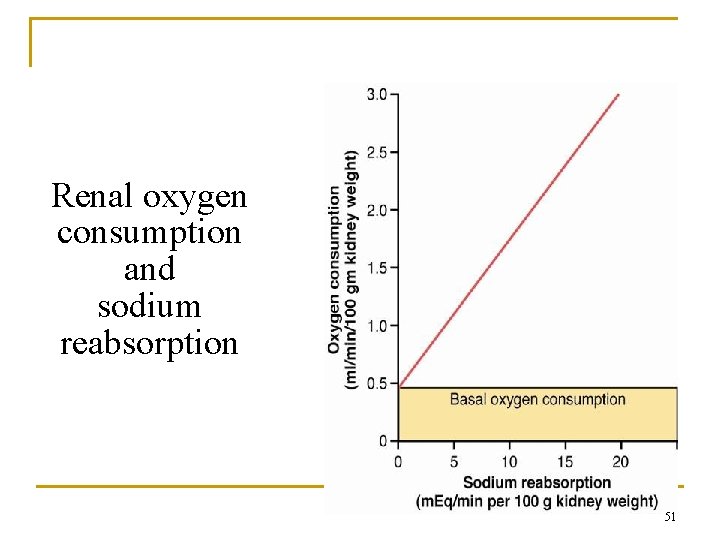
Renal oxygen consumption and sodium reabsorption 51
Control of GFR and renal blood flow • Neurohumoral • Local (Intrinsic) 52
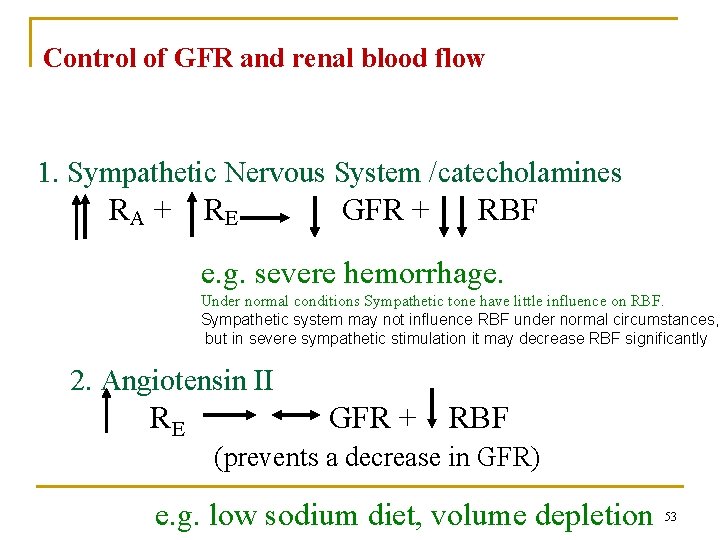
Control of GFR and renal blood flow 1. Sympathetic Nervous System /catecholamines RA + R E GFR + RBF e. g. severe hemorrhage. Under normal conditions Sympathetic tone have little influence on RBF. Sympathetic system may not influence RBF under normal circumstances, but in severe sympathetic stimulation it may decrease RBF significantly 2. Angiotensin II RE GFR + RBF (prevents a decrease in GFR) e. g. low sodium diet, volume depletion 53
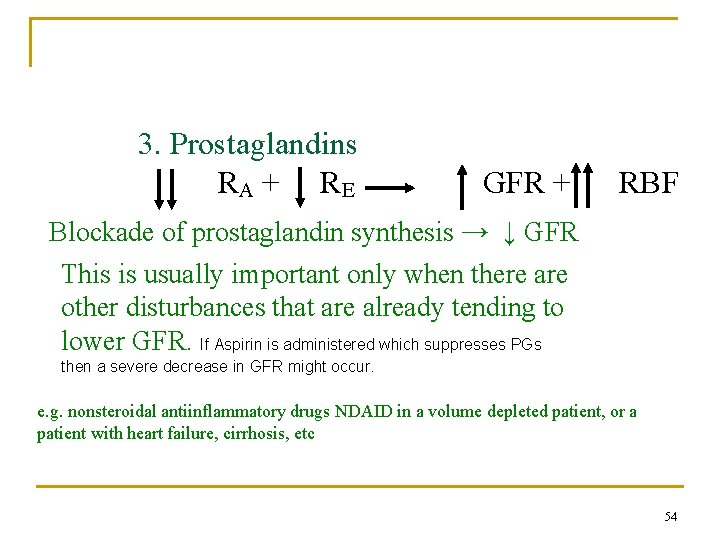
Control of GFR and renal blood flow 3. Prostaglandins RA + R E GFR + RBF Blockade of prostaglandin synthesis → ↓ GFR This is usually important only when there are other disturbances that are already tending to lower GFR. If Aspirin is administered which suppresses PGs then a severe decrease in GFR might occur. e. g. nonsteroidal antiinflammatory drugs NDAID in a volume depleted patient, or a patient with heart failure, cirrhosis, etc 54
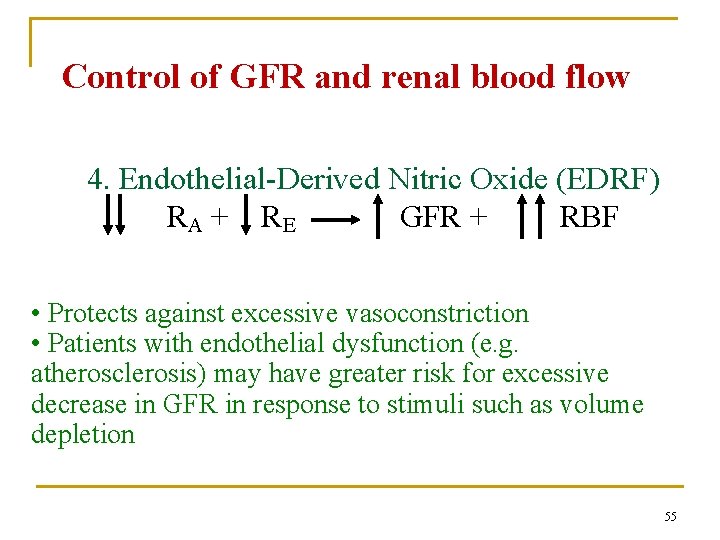
Control of GFR and renal blood flow 4. Endothelial-Derived Nitric Oxide (EDRF) RA + R E GFR + RBF • Protects against excessive vasoconstriction • Patients with endothelial dysfunction (e. g. atherosclerosis) may have greater risk for excessive decrease in GFR in response to stimuli such as volume depletion 55
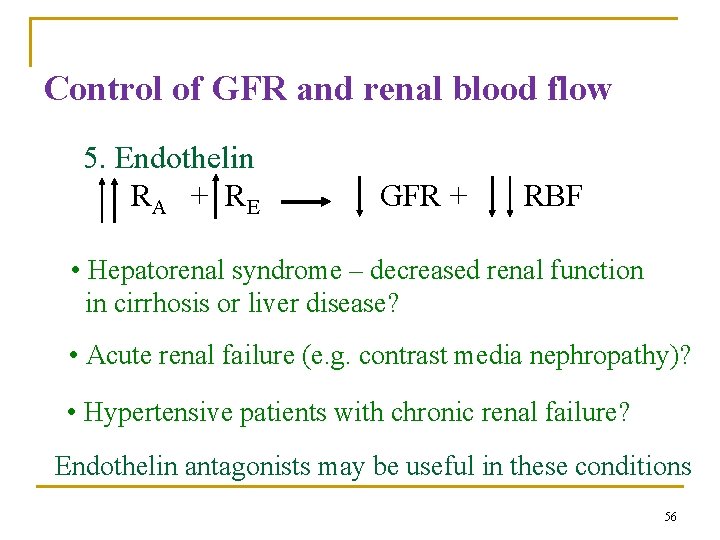
Control of GFR and renal blood flow 5. Endothelin RA + R E GFR + RBF • Hepatorenal syndrome – decreased renal function in cirrhosis or liver disease? • Acute renal failure (e. g. contrast media nephropathy)? • Hypertensive patients with chronic renal failure? Endothelin antagonists may be useful in these conditions 56
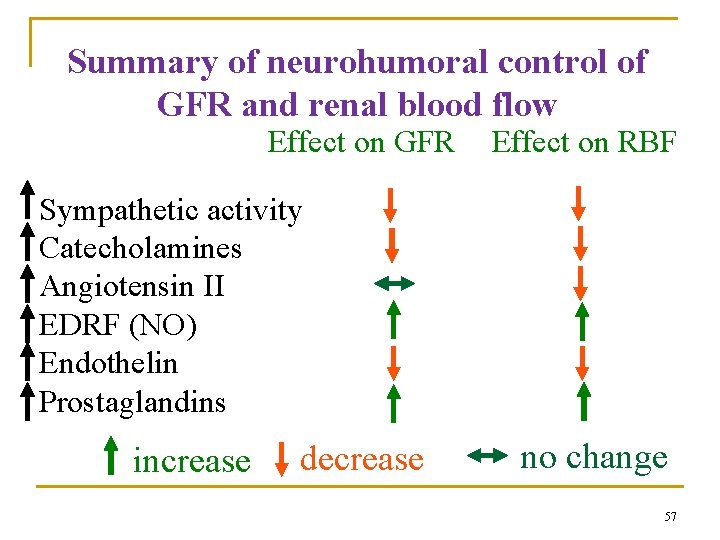
Summary of neurohumoral control of GFR and renal blood flow Effect on GFR Effect on RBF Sympathetic activity Catecholamines Angiotensin II EDRF (NO) Endothelin Prostaglandins increase decrease no change 57
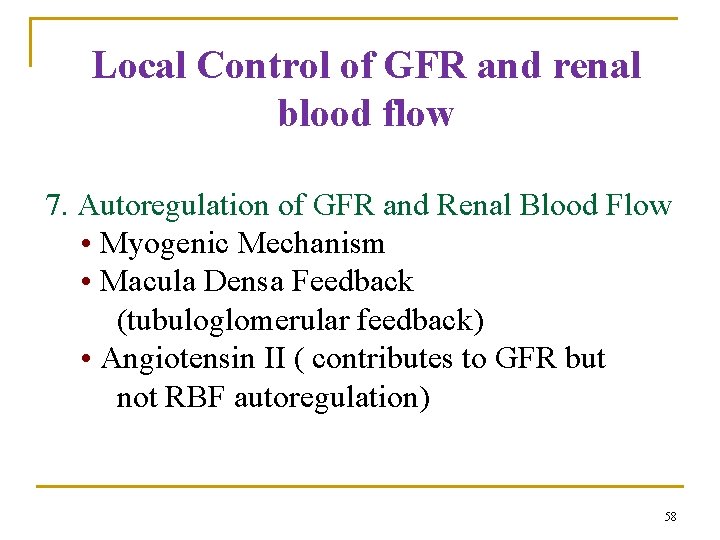
Local Control of GFR and renal blood flow 7. Autoregulation of GFR and Renal Blood Flow • Myogenic Mechanism • Macula Densa Feedback (tubuloglomerular feedback) • Angiotensin II ( contributes to GFR but not RBF autoregulation) 58
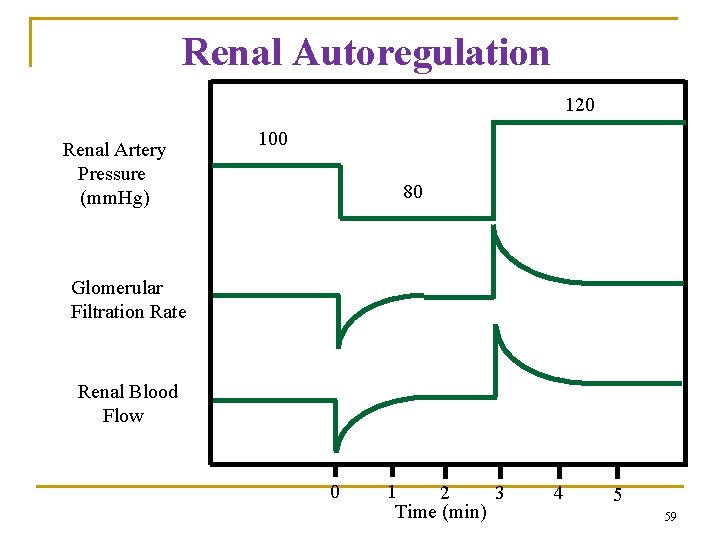
Renal Autoregulation 120 Renal Artery Pressure (mm. Hg) 100 80 Glomerular Filtration Rate Renal Blood Flow 0 1 2 3 Time (min) 4 5 59
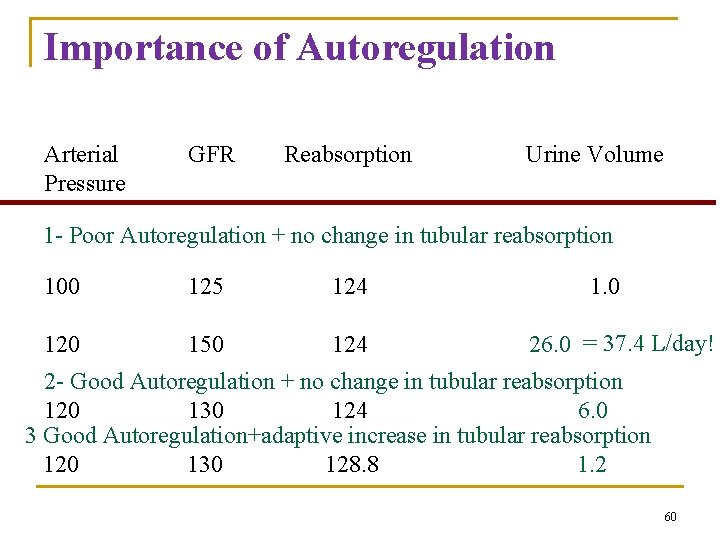
Importance of Autoregulation Arterial Pressure GFR Reabsorption Urine Volume 1 - Poor Autoregulation + no change in tubular reabsorption 100 125 124 120 150 124 1. 0 26. 0 = 37. 4 L/day! 2 - Good Autoregulation + no change in tubular reabsorption 120 130 124 6. 0 3 Good Autoregulation+adaptive increase in tubular reabsorption 120 130 128. 8 1. 2 60
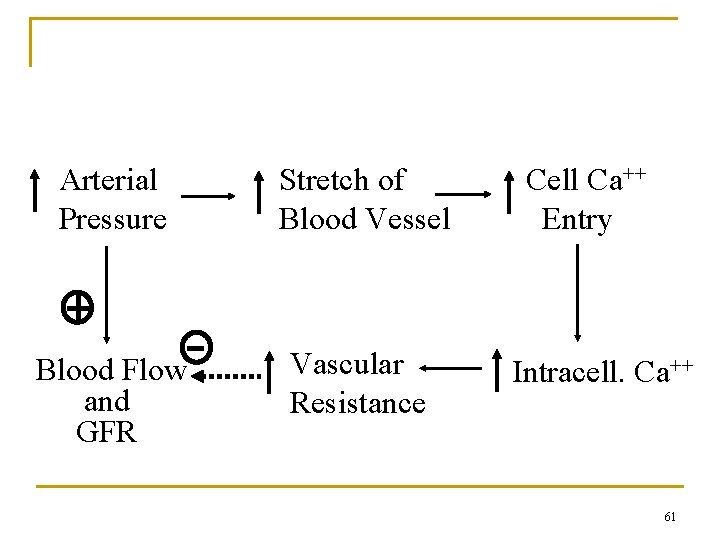
Myogenic Mechanism Arterial Pressure Stretch of Blood Vessel Blood Flow and GFR Vascular Resistance Cell Ca++ Entry Intracell. Ca++ 61
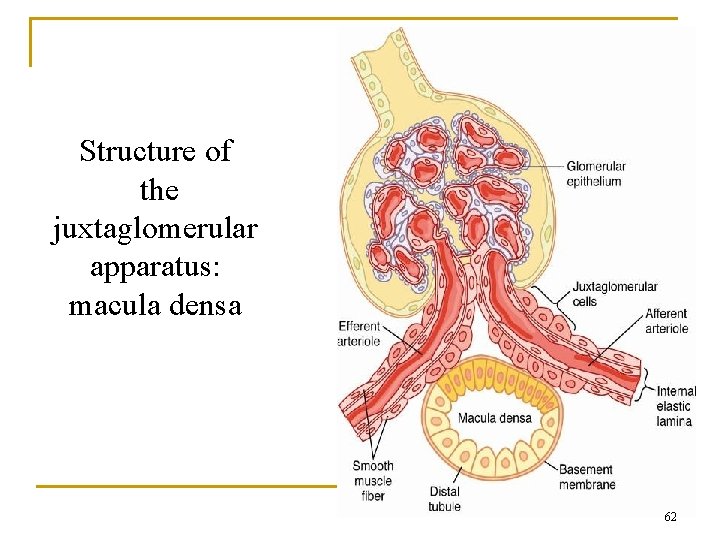
Structure of the juxtaglomerular apparatus: macula densa 62
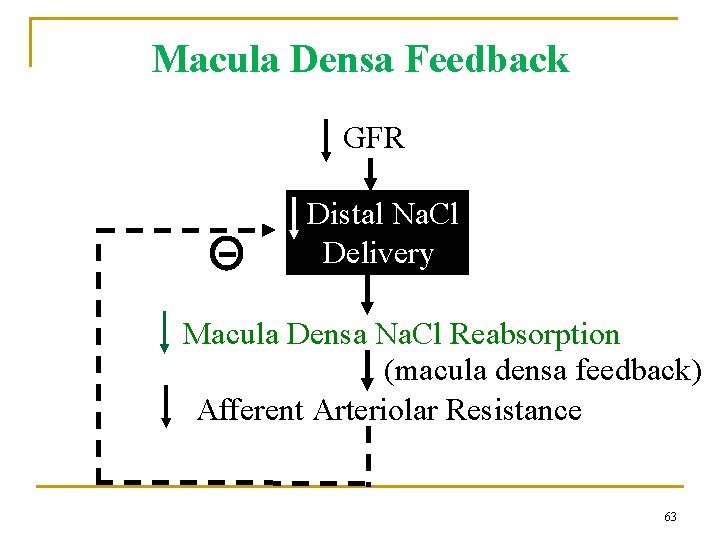
Macula Densa Feedback GFR Distal Na. Cl Delivery Macula Densa Na. Cl Reabsorption (macula densa feedback) Afferent Arteriolar Resistance 63
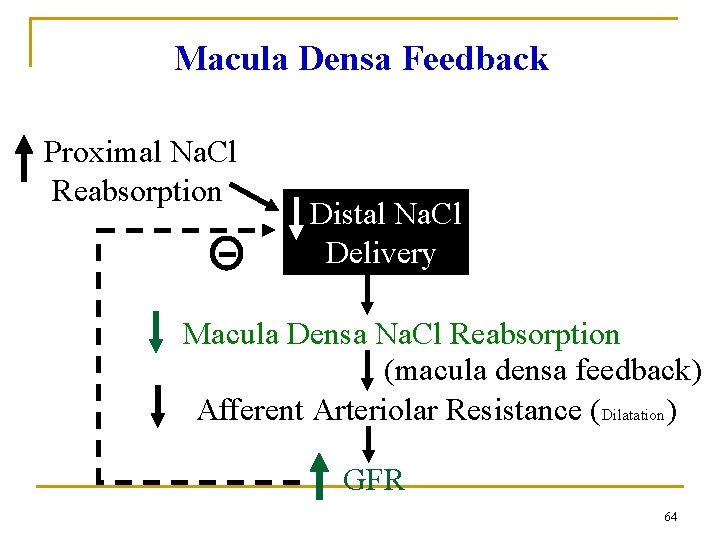
Macula Densa Feedback Proximal Na. Cl Reabsorption Distal Na. Cl Delivery Macula Densa Na. Cl Reabsorption (macula densa feedback) Afferent Arteriolar Resistance (Dilatation) GFR 64
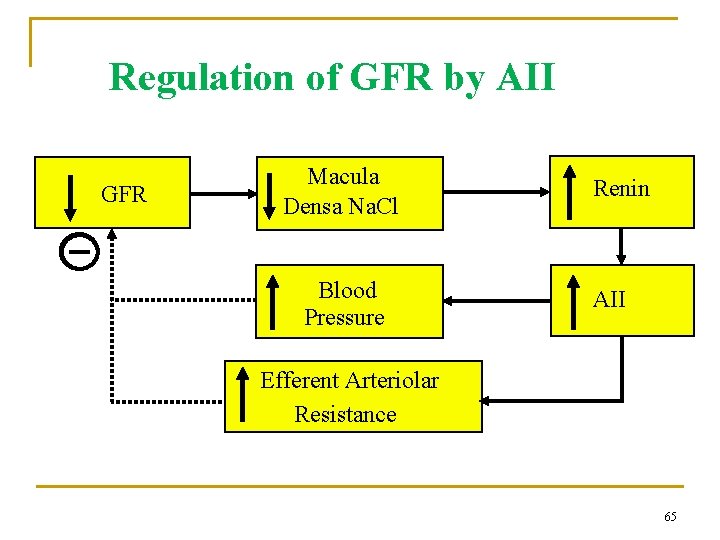
Regulation of GFR by AII GFR Macula Densa Na. Cl Blood Pressure Renin AII Efferent Arteriolar Resistance 65
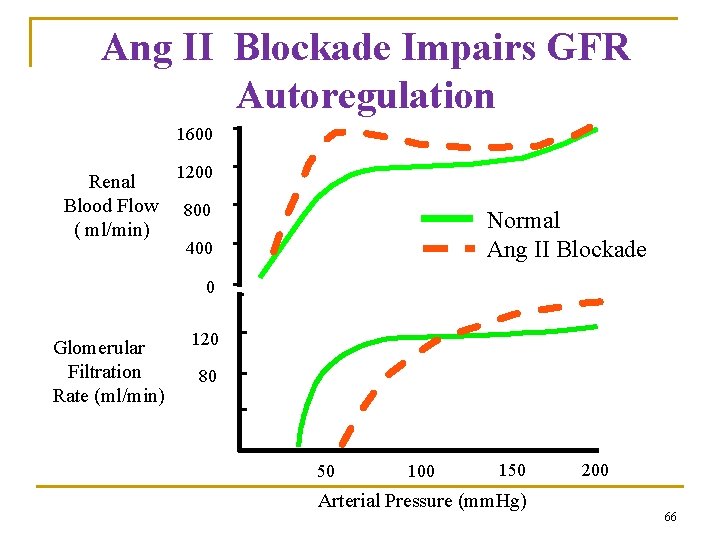
Ang II Blockade Impairs GFR Autoregulation 1600 Renal Blood Flow ( ml/min) 1200 800 Normal Ang II Blockade 400 0 Glomerular Filtration Rate (ml/min) 120 80 40 0 0 50 100 150 Arterial Pressure (mm. Hg) 200 66
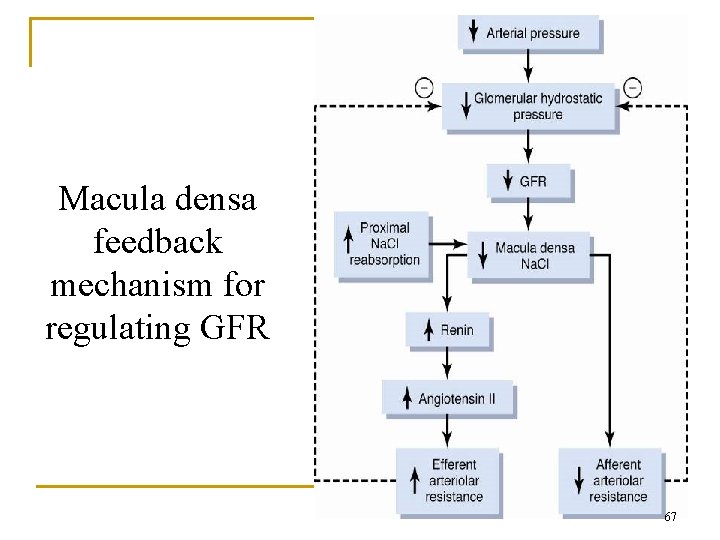
Macula densa feedback mechanism for regulating GFR 67
Other Factors That Influence GFR • Fever, pyrogens: increase GFR • Glucorticoids: increase GFR • Aging: decreases GFR 10% / decade after 40 yrs • Hyperglycemia: increases GFR (diabetes mellitus) • Dietary protein: high protein increases GFR low protein decreases GFR 68
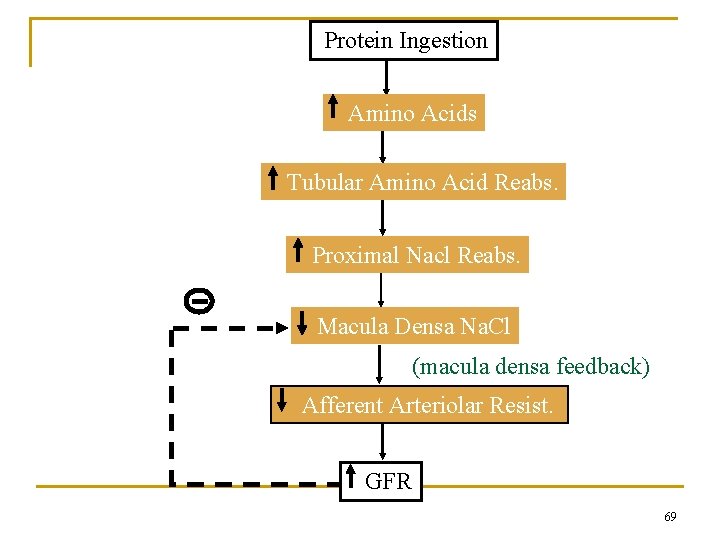
Protein Ingestion Amino Acids Tubular Amino Acid Reabs. Proximal Nacl Reabs. Macula Densa Na. Cl (macula densa feedback) Afferent Arteriolar Resist. GFR 69
- Slides: 69