Secondary Hyperparathyroidism in Chronic Kidney Disease 20091113 R
- Slides: 20
Secondary Hyperparathyroidism in Chronic Kidney Disease 2009/11/13 신장내과 R 3 이완수
Definition • Secondary hyperparathyroidism ? – Excessive secretion of parathyroid hormone (PTH) by the parathyroid glands in response to hypocalcemia, hyperphsophatemia – Associated hypertrophy of the glands – Especially seen in chronic kidey disease – Also result from malabsorption • Chronic pancreatitis • Small bowel disease
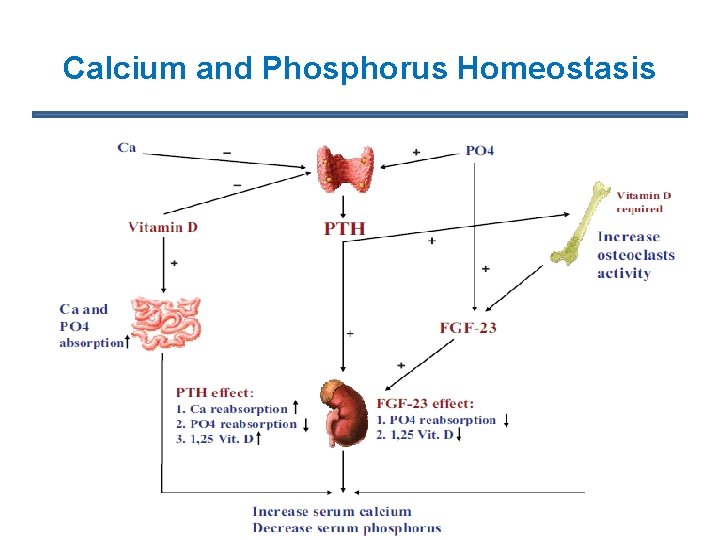
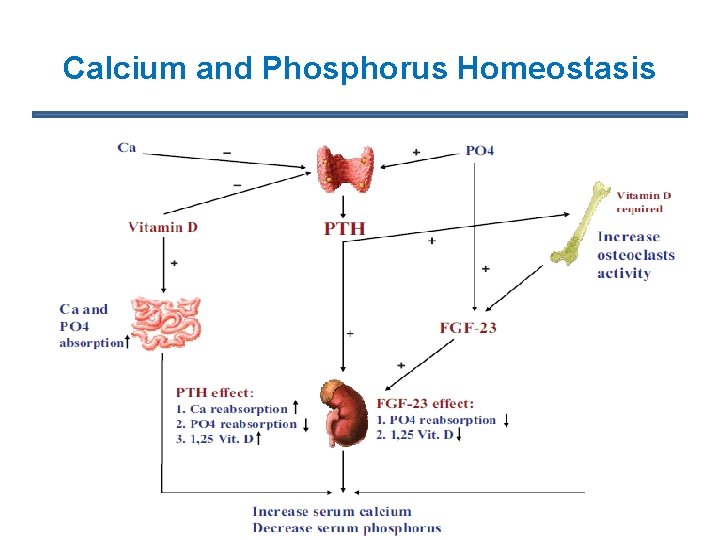
Calcium and Phosphorus Homeostasis
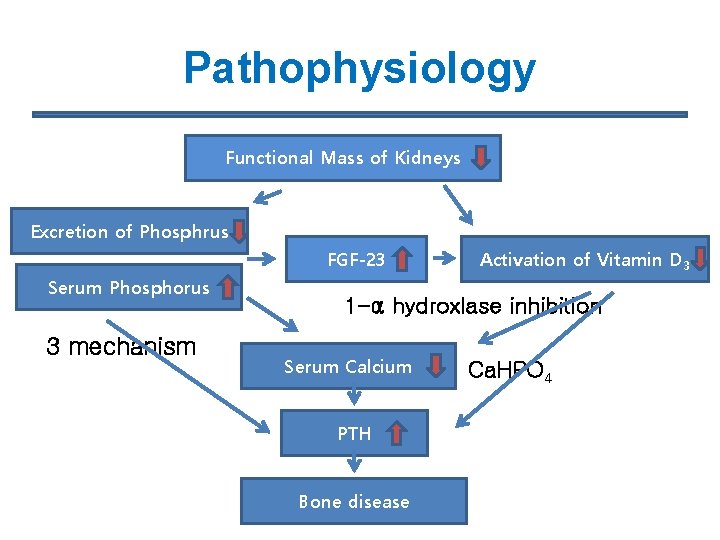
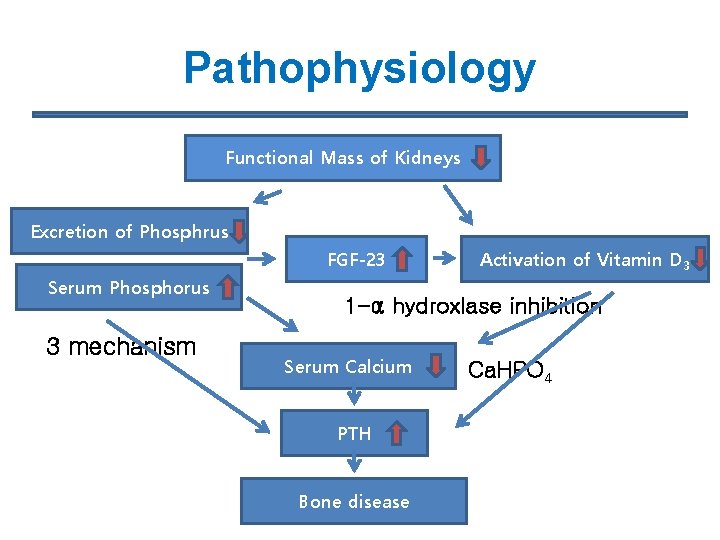
Pathophysiology Functional Mass of Kidneys Excretion of Phosphrus FGF-23 Serum Phosphorus 3 mechanism Activation of Vitamin D 3 1 -α hydroxlase inhibition Serum Calcium PTH Bone disease Ca. HPO 4
Parathyoid Hormone (PTH) • most important regulator of calcium metabolism • secreted by the chief cells of the parathyroid glands in response to hypocalcemia and hyperphosphatemia • half-life (2 to 4 minutes) before being degraded to various inactive fragments “intact” PTH assay is widely used to estimate active PTH level
Parathyoid Hormone (PTH) ① Bone stimulates the “osteoclasts” and causes “bone resorption” P ↑ , Ca ↑ ② Kidney stimulates the “ 1 -α hydroxylase” activity in the kidney “ 1, 25 dihydroxyvitamin D” production ↑ increases the reabsorption of calcium in the distal renal tubules Ca ↑ decrease the reabsorption of phosphorus in the proximal renal tubules P↓ ③ Intestine indirectly increases intestinal calcium and phosphorus absorption P ↑ , Ca ↑
Vitamin D • Essential factor in the regulation of calcium and phosphorus balance • Synthesized in the skin but is also present in the diet • Along with PTH, vitamin D is a required factor in the bone resorption process • Increases the reabsorption of urinary calcium and phosphorus in the renal tubules ( P ↑ , Ca ↑) • Through the vitamin D receptors it has a direct effect on the parathyroid glands to “suppress PTH secretion”
Fibroblasts Growth Factor-23 • New protein with “phosphaturic activity” • secreted by osteocytes • now considered to be the most important factor for regulation of phosphorus homeostasis • Through the “Klotho receptor” it acts mainly on the kidney to increase phosphorus clearance • inhibits the 1 - α hydoxylase activity, causing a low 1, 25 dihydroxyvitamin D level • Hyperphosphatemia is the principal stimulator for FGF-23
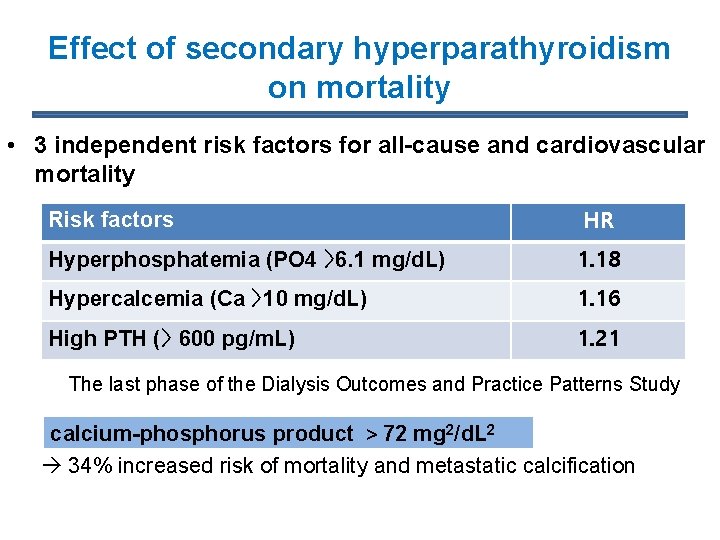
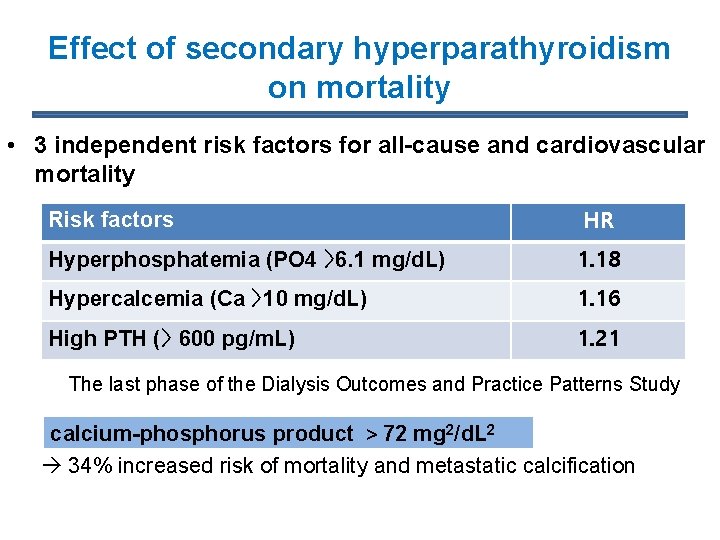
Effect of secondary hyperparathyroidism on mortality • 3 independent risk factors for all-cause and cardiovascular mortality Risk factors HR Hyperphosphatemia (PO 4 〉6. 1 mg/d. L) 1. 18 Hypercalcemia (Ca 〉10 mg/d. L) 1. 16 High PTH (〉 600 pg/m. L) 1. 21 The last phase of the Dialysis Outcomes and Practice Patterns Study calcium-phosphorus product > 72 mg 2/d. L 2 34% increased risk of mortality and metastatic calcification
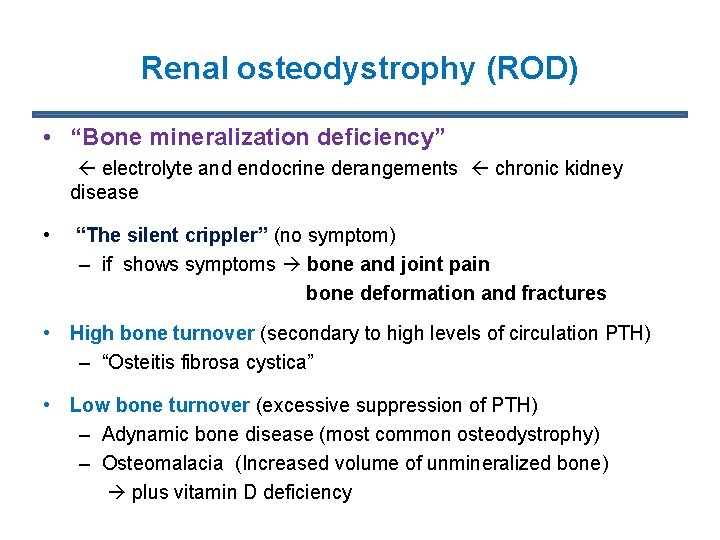
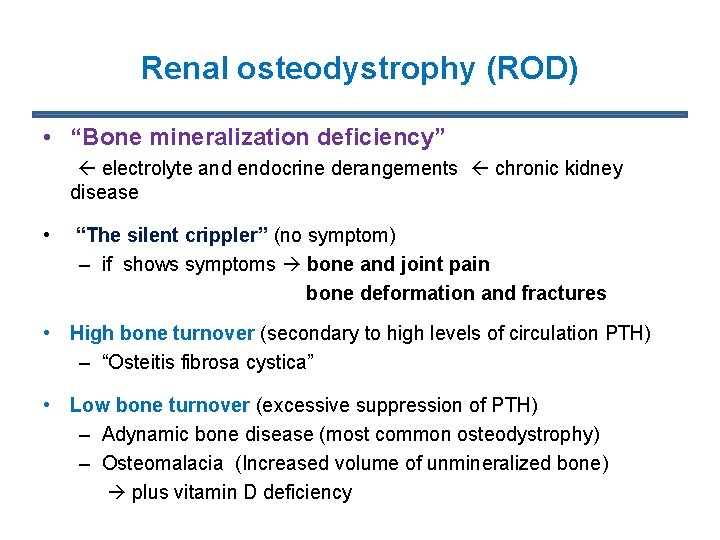
Renal osteodystrophy (ROD) • “Bone mineralization deficiency” electrolyte and endocrine derangements chronic kidney disease • “The silent crippler” (no symptom) – if shows symptoms bone and joint pain bone deformation and fractures • High bone turnover (secondary to high levels of circulation PTH) – “Osteitis fibrosa cystica” • Low bone turnover (excessive suppression of PTH) – Adynamic bone disease (most common osteodystrophy) – Osteomalacia (Increased volume of unmineralized bone) plus vitamin D deficiency
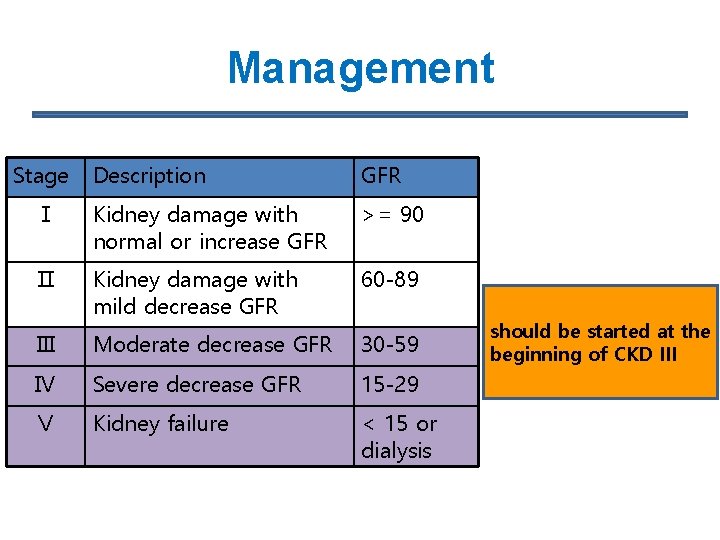
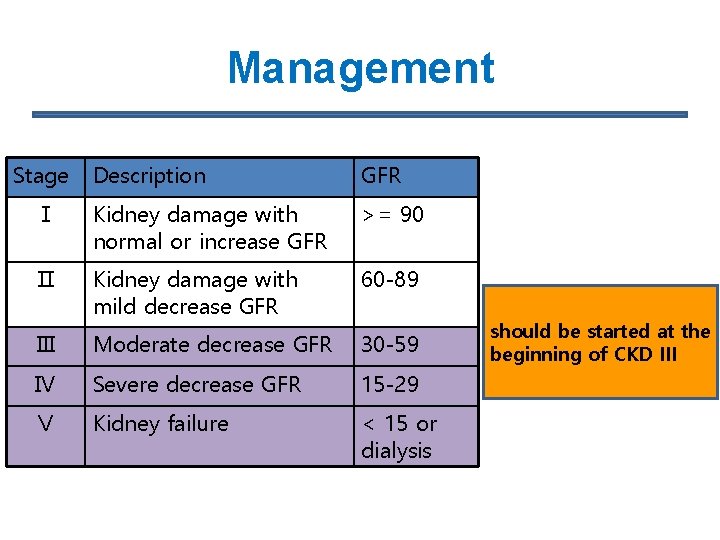
Management Stage Description GFR Ⅰ Kidney damage with normal or increase GFR >= 90 Ⅱ Kidney damage with mild decrease GFR 60 -89 Ⅲ Moderate decrease GFR 30 -59 Ⅳ Severe decrease GFR 15 -29 Ⅴ Kidney failure < 15 or dialysis should be. PTH started at the beginning of CKD III P
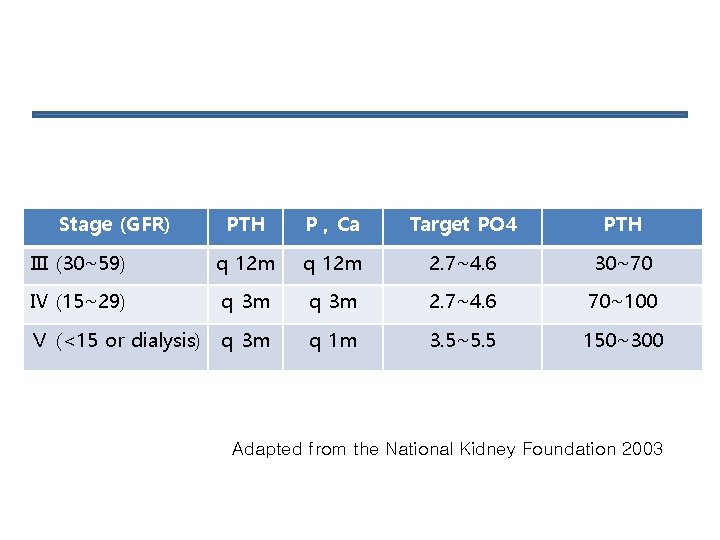
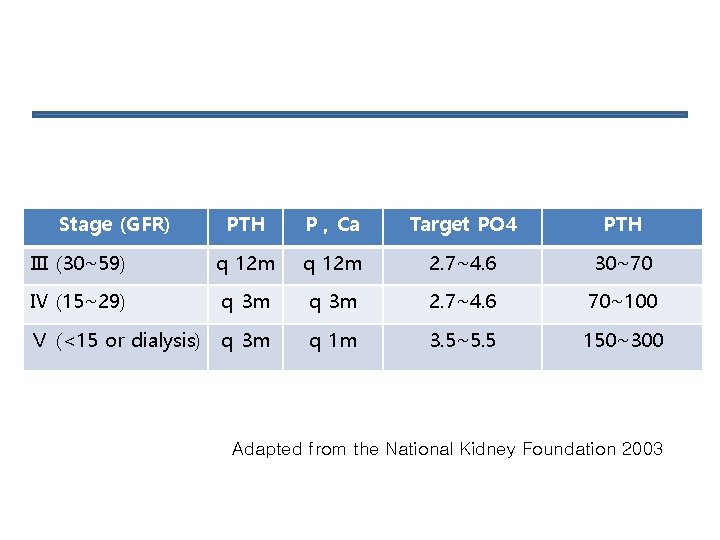
Stage (GFR) PTH P , Ca Target PO 4 PTH Ⅲ (30~59) q 12 m 2. 7~4. 6 30~70 Ⅳ (15~29) q 3 m 2. 7~4. 6 70~100 Ⅴ (<15 or dialysis) q 3 m q 1 m 3. 5~5. 5 150~300 Adapted from the National Kidney Foundation 2003
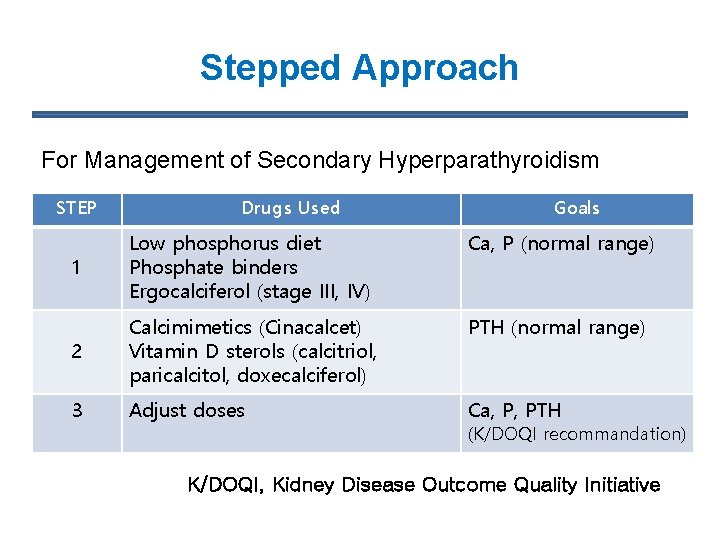
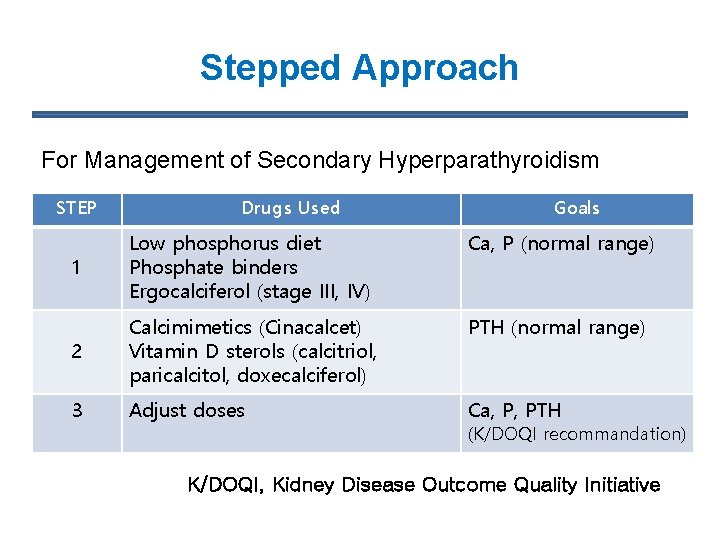
Stepped Approach For Management of Secondary Hyperparathyroidism STEP Drugs Used Goals 1 Low phosphorus diet Phosphate binders Ergocalciferol (stage III, IV) Ca, P (normal range) 2 Calcimimetics (Cinacalcet) Vitamin D sterols (calcitriol, paricalcitol, doxecalciferol) PTH (normal range) 3 Adjust doses Ca, P, PTH (K/DOQI recommandation) K/DOQI, Kidney Disease Outcome Quality Initiative
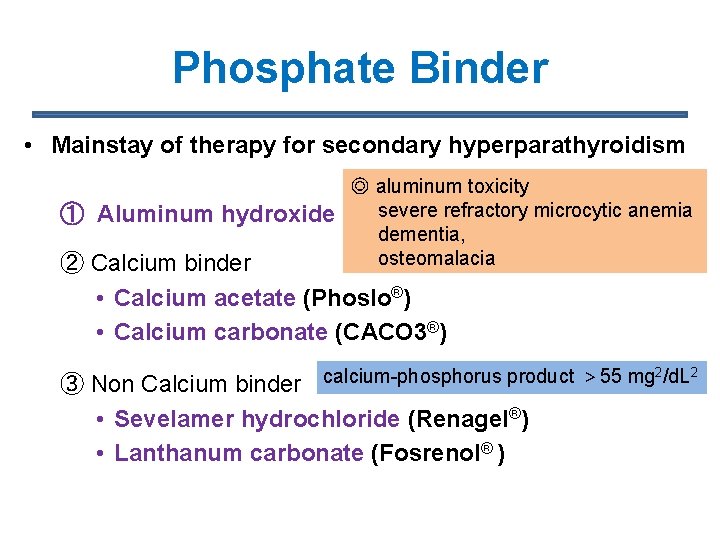
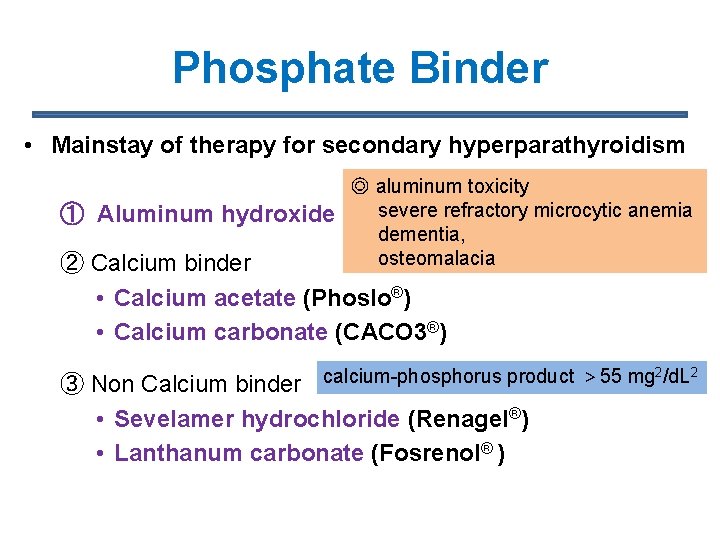
Phosphate Binder • Mainstay of therapy for secondary hyperparathyroidism ① Aluminum hydroxide ◎ aluminum toxicity severe refractory microcytic anemia dementia, osteomalacia ② Calcium binder • Calcium acetate (Phoslo®) • Calcium carbonate (CACO 3®) 2 2 ③ Non Calcium binder calcium-phosphorus product > 55 mg /d. L • Sevelamer hydrochloride (Renagel®) • Lanthanum carbonate (Fosrenol® )
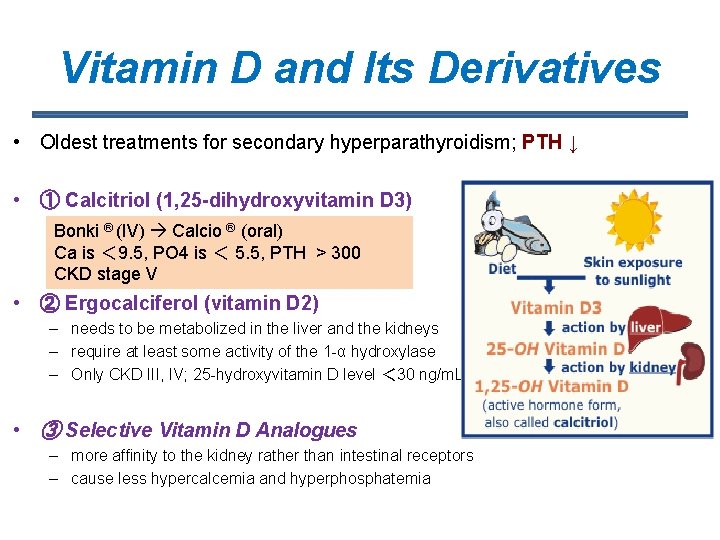
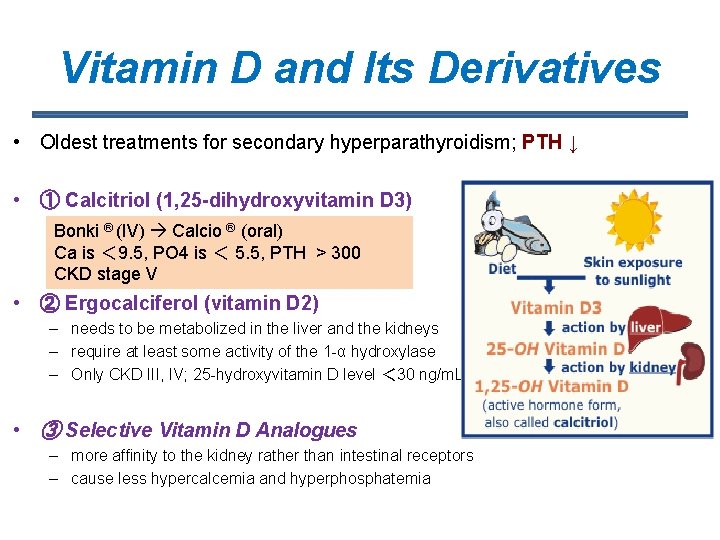
Vitamin D and Its Derivatives • Oldest treatments for secondary hyperparathyroidism; PTH ↓ • ① Calcitriol (1, 25 -dihydroxyvitamin D 3) –Bonki natural form of. Calcio vitamin®D(oral) ® (IV) –Ca. IVisadministration is more effective < 9. 5, PO 4 is < 5. 5, PTH > 300 CKD stage V • ② Ergocalciferol (vitamin D 2) – needs to be metabolized in the liver and the kidneys – require at least some activity of the 1 -α hydroxylase – Only CKD III, IV; 25 -hydroxyvitamin D level < 30 ng/m. L • ③ Selective Vitamin D Analogues – more affinity to the kidney rather than intestinal receptors – cause less hypercalcemia and hyperphosphatemia
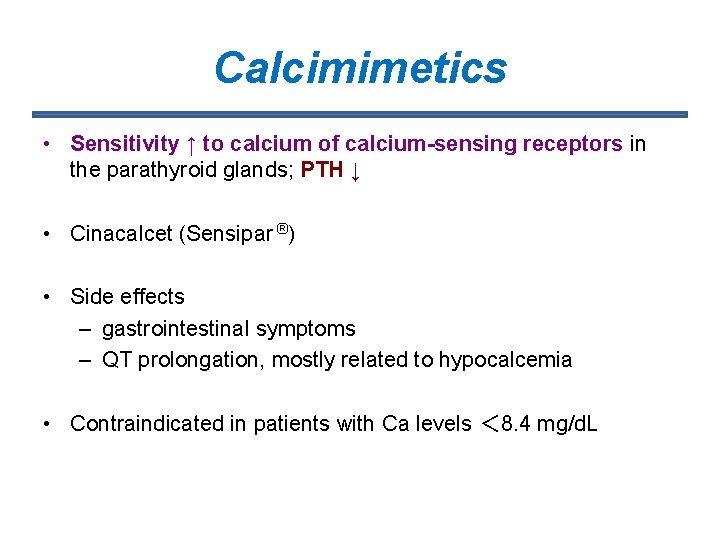
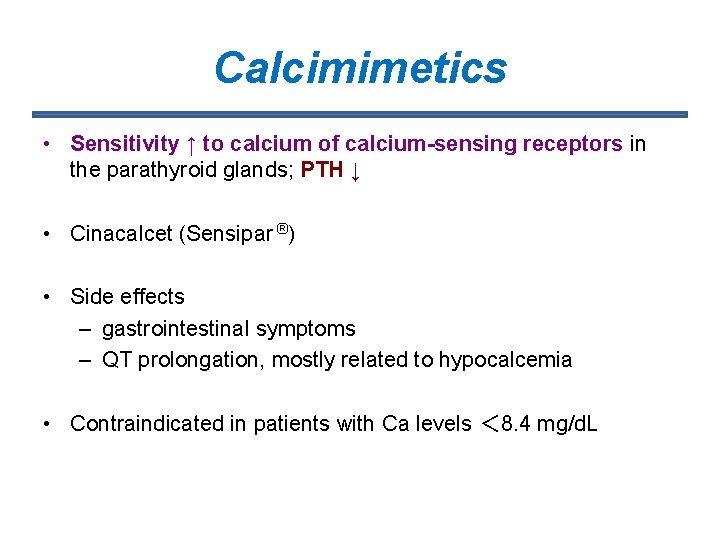
Calcimimetics • Sensitivity ↑ to calcium of calcium-sensing receptors in the parathyroid glands; PTH ↓ • Cinacalcet (Sensipar ®) • Side effects – gastrointestinal symptoms – QT prolongation, mostly related to hypocalcemia • Contraindicated in patients with Ca levels < 8. 4 mg/d. L
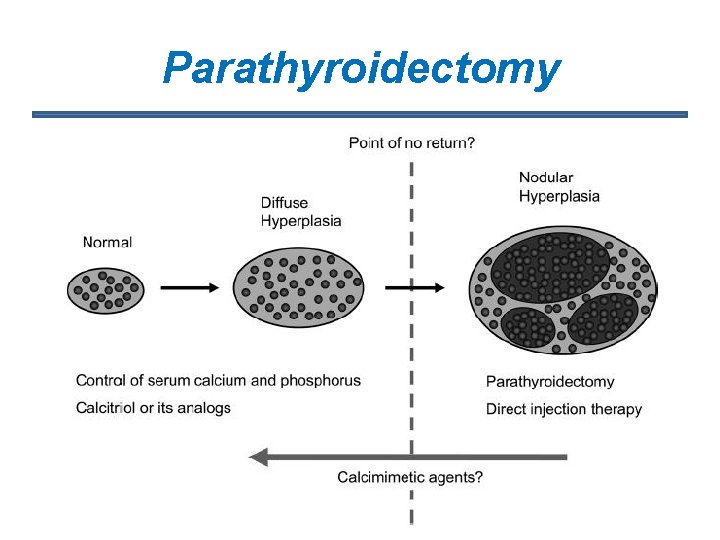
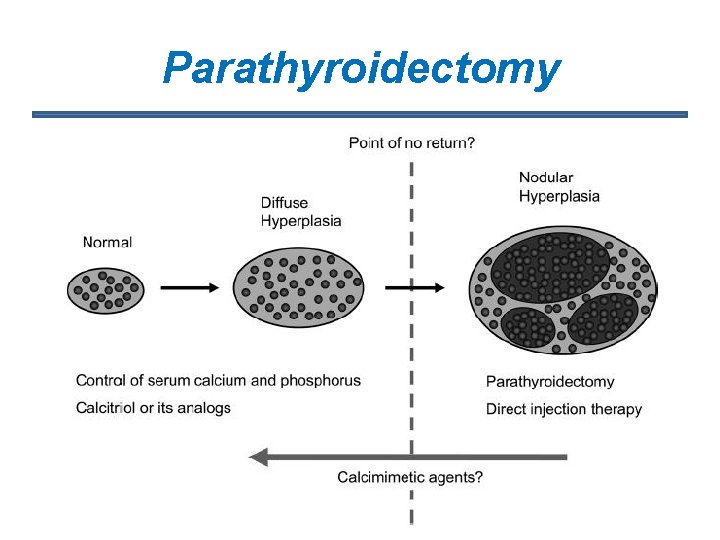
Parathyroidectomy
Parathyroidectomy • only used when all medical therapy is unsuccessful • Strong indications for surgery – Extraskeletal calcification, – Calciphylaxis – Debilitating bone disease – Refractory pruritus – severe hypercalcemia – PTH levels > 800 pg/m. L • Lack of osteoclastic activity “hungry-bone syndrome” – Hypocalcemia (Tetany)
Percutaneous ethanol injection (PEI) • High-risk parathyroidectomy patients are good candidates for PEIT • ① Indications – (i) i. PTH ≥ 400 pg/ml – (ii) Osteitis fibrosa or high-turnover bone – (iii) Enlarged parathyroid glands detectable by sono – (iv) Resistant to medical therapy – (v) Parathyroid glands should be ≥ 1 cm in length, ≥ 0. 5 cm 3 in estimated volume If three or more glands are enlarged by this amount PEIT will be ineffective in the long term – (vi) Patients who have given informed consent to undergo PEIT Guidline for PEI of parathyroid gland, Nephrology Dialysis Transplantation 2003
Percutaneous ethanol injection (PEI) • ② Exclusion criteria – (i) Enlarged parathyroid gland located where sono-guided puncture is impossible – (ii) Paralysis of the recurrent laryngeal nerve on the opposite side – (iii) Operation on the neck region for thyroid carcinoma, etc. is scheduled – (iv) Institutions without the equipment required or without skilled operators
 Ersd
Ersd Nih scale
Nih scale Approach to hyperparathyroidism
Approach to hyperparathyroidism Albumin kidney disease
Albumin kidney disease Nemo ckd
Nemo ckd Albumin kidney disease
Albumin kidney disease Sighns of kidney disease
Sighns of kidney disease Symptomatic polycystic kidney disease
Symptomatic polycystic kidney disease Resonium por
Resonium por Stages of cirrosis
Stages of cirrosis Stigmata of chronic liver disease
Stigmata of chronic liver disease Kate lorig stanford
Kate lorig stanford Nonalcoholic fatty liver disease
Nonalcoholic fatty liver disease Chronic disease
Chronic disease Jewish chronic disease study
Jewish chronic disease study Chronic care model wagner
Chronic care model wagner Copd disease
Copd disease Cld chronic liver disease
Cld chronic liver disease Chronic disease
Chronic disease Chronic granulomatous disease
Chronic granulomatous disease Chronic rheumatic heart disease
Chronic rheumatic heart disease