RENAL DISEASE CHRONIC RENAL FAILURE Pathophysiology of Disease

- Slides: 16
RENAL DISEASE: CHRONIC RENAL FAILURE Pathophysiology of Disease: Chapter 16 (394 -398) Jack De. Ruiter, Ph. D Department of Pharmacal Sciences April, 2000
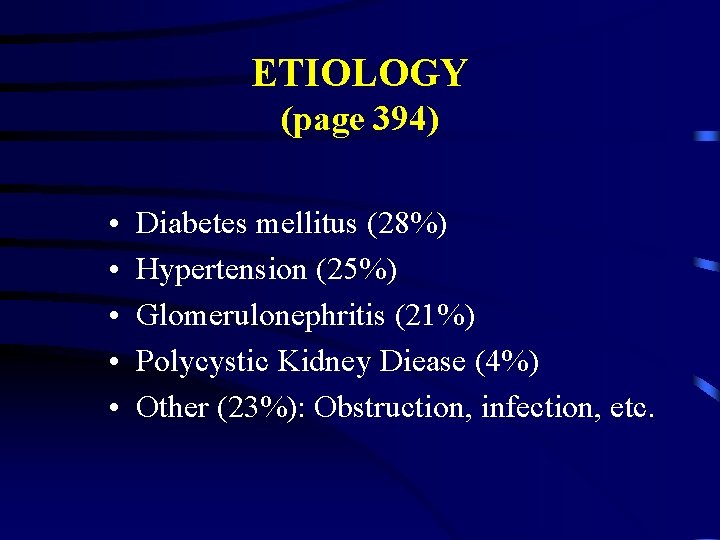
ETIOLOGY (page 394) • • • Diabetes mellitus (28%) Hypertension (25%) Glomerulonephritis (21%) Polycystic Kidney Diease (4%) Other (23%): Obstruction, infection, etc.

Pathology and Pathogenesis (page 395) • Chronic vs Acute renal failure pathogenesis: – Acute: tubular cell death and regeneration (reversible) – Chronic: Irreversible nephron loss • Glomerular Hyperfiltration: – Compensatory mechanism with increased nephron GFR: – Pre-disposition to glomerular sclerosis • Azotemia at 30 -35% GFR • Uremia: <20% normal excretory capacity
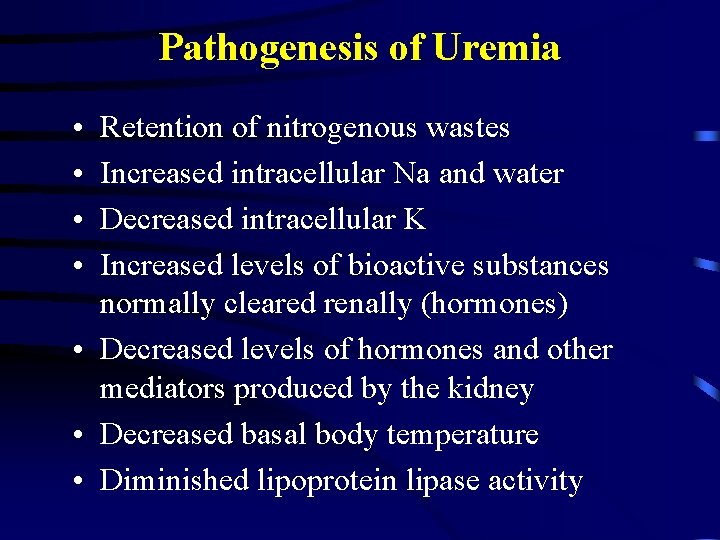
Pathogenesis of Uremia • • Retention of nitrogenous wastes Increased intracellular Na and water Decreased intracellular K Increased levels of bioactive substances normally cleared renally (hormones) • Decreased levels of hormones and other mediators produced by the kidney • Decreased basal body temperature • Diminished lipoprotein lipase activity
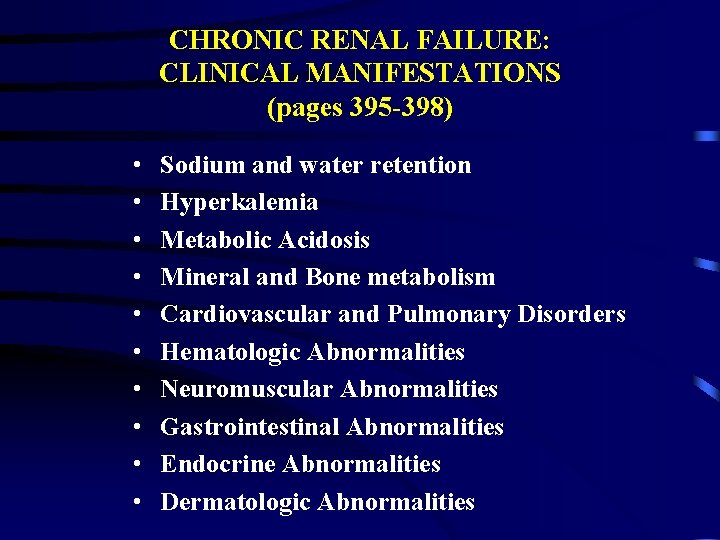
CHRONIC RENAL FAILURE: CLINICAL MANIFESTATIONS (pages 395 -398) • • • Sodium and water retention Hyperkalemia Metabolic Acidosis Mineral and Bone metabolism Cardiovascular and Pulmonary Disorders Hematologic Abnormalities Neuromuscular Abnormalities Gastrointestinal Abnormalities Endocrine Abnormalities Dermatologic Abnormalities
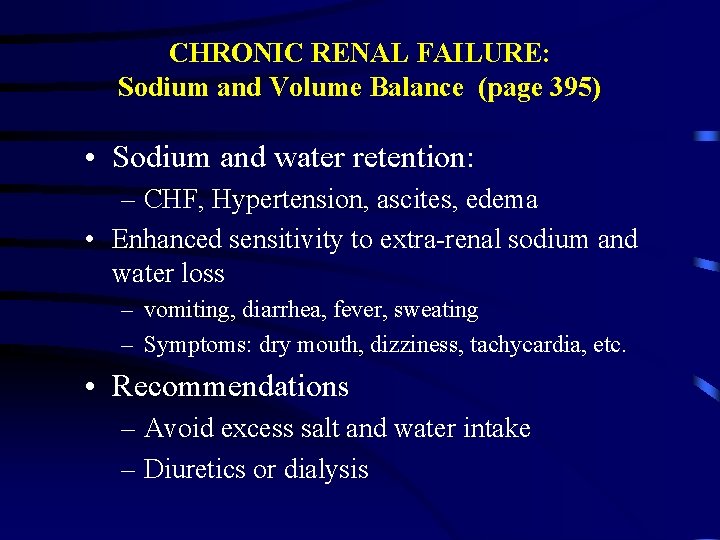
CHRONIC RENAL FAILURE: Sodium and Volume Balance (page 395) • Sodium and water retention: – CHF, Hypertension, ascites, edema • Enhanced sensitivity to extra-renal sodium and water loss – vomiting, diarrhea, fever, sweating – Symptoms: dry mouth, dizziness, tachycardia, etc. • Recommendations – Avoid excess salt and water intake – Diuretics or dialysis
CHRONIC RENAL FAILURE: Potassium Balance (pages 395 -396) • Hyperkalemia (GFR below 5 m. L/min) – GFRs >5 m. L/min: compensatory aldosteronemediated K transport in the DCT – K-sparing diuretics, ACEis, beta-blockers impair Aldosterone-mediated actions – Exacerbation of hyperkalenia: • Exogenous factors: K-rich diet, etc. • Endogenous factors: infection, trauma, etc.
CHRONIC RENAL FAILURE: Potassium Balance and Diabetes (page 396) • Diabetics (major cause of CRF): – Hyporeninemic hypoaldosteronism – Lack of renin - decreased angiotensin II impaired aldosterone secretion - loss of compensation for low GFr
CHRONIC RENAL FAILURE: Metabolic Acidosis (page 396) Decreased acid excretion and ability to maintain physiologic buffering capacity: • GFR > 20 m. L/min: transient moderate acidosis • Treat with oral sodium bicarbonate • Increased susceptibility to acidosis
CHRONIC RENAL FAILURE: Mineral and Bone (page 396 -397) Bone disease (Figure 16 -6) from: • Decreased Ca absorption from the gut • Over-production of PTH • Altered Vitamin D metabolism • Chronic metabolic acidosis
CHRONIC RENAL FAILURE: Cardiovascular and Pulmonary Abnormalities (page 397) • Volume and salt overload – CHF and pulmonary edema – Hypertension • Hyperreninemia: Hypertension • Pericarditis: Remic toxin accumulation • Accelerated atherosclerosis: linked to factors above and metabolic abnormalities (Ca alterations, hyperlipidemia)
CHRONIC RENAL FAILURE: Hematological Abnormalities (page 397) • Anemia: lack of erythropoietin production • Bone marrow suppression: – uremic poisons: leukocyte suppression - infection – bone marrow fibrosis: elevated PTH an aluminum toxicity from dialysis • Increased bruising, blood loss (surgery) and hemorrhage • Lab Abnormalities: Prolonged bleeding time, abnormal platelet aggregation
CHRONIC RENAL FAILURE: Neuromuscular Abnormalites (page 397) • CNS Abnormalities: – Mild-Moderate: Sleep disorders, impaired concentration and memory, irritability – Severe: Asterixis, myoclonus, stupor, seizures and coma • Peripheral neuropathies: – “restless legs” syndrome • Hemodialysis-related neuropathies
CHRONIC RENAL FAILURE: Gastrointestinal Abnormalities (page 397) • Peptic Ulcer disease: Secondary hyperparathyrodism? • Uremic gastroenteritis: mucosal alterations • Uremic Fetor: bad breath (ammonia) • Non-Specific abnormalities: – anorexia, nausea, vomiting, diverticulosis, hiccoughs
CHRONIC RENAL FAILURE: Endocrine Abnormalities (page 398) • Insulin: Prolonged half-life due to reduced clearance (metabolism) • Amenorrhea and pregnancy failure: low estrogen levels • Impotence, oligospermia and geminal cell dysplasia: Low testosterone levels
CHRONIC RENAL FAILURE: Dermatologic Abnormalities (page 398) • Pallor: anemia • Skin color changes: accumulation of pigments • Ecchymoses and hematomas: clotting abnormalities • Pruritus and Excoriations: Ca deposits from secondary hyperparathyroidism
 Earthy look in chronic renal failure
Earthy look in chronic renal failure Res extra commercium
Res extra commercium Ira pré renal renal e pós renal
Ira pré renal renal e pós renal Renal vein thrombosis pathophysiology
Renal vein thrombosis pathophysiology Acute vs chronic heart failure
Acute vs chronic heart failure Failure to sense pacemaker
Failure to sense pacemaker Moderately ductile fracture
Moderately ductile fracture Ventricular escape rhythm
Ventricular escape rhythm Renal failure
Renal failure Urinalysis
Urinalysis Acute glomerulonephritis pathophysiology
Acute glomerulonephritis pathophysiology Mitral stenosis severity
Mitral stenosis severity Coronary artery disease pathophysiology
Coronary artery disease pathophysiology Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Pathophysiology of ischemic heart disease
Pathophysiology of ischemic heart disease Pathophysiology of hirschsprung disease
Pathophysiology of hirschsprung disease Nursing assessment for congestive heart failure
Nursing assessment for congestive heart failure