Malignant Neoplasms of the Oral Cavity a m

- Slides: 94
Malignant Neoplasms of the Oral Cavity a m i r 1 3 5 @ m g m a i l. c o 1
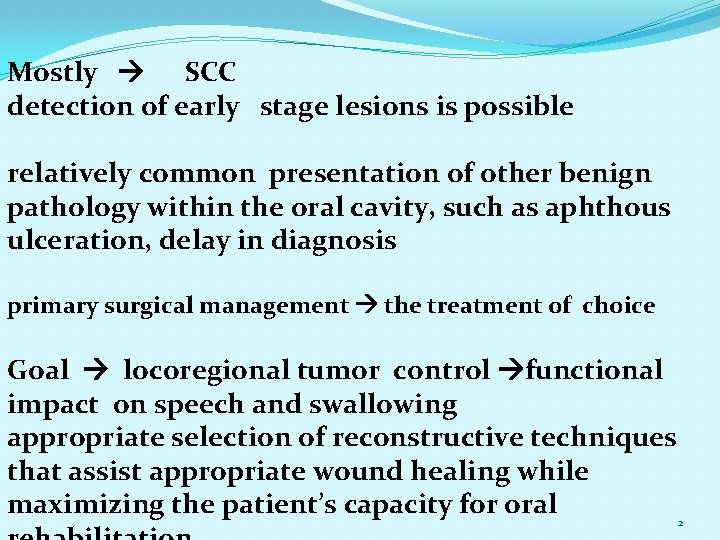
Mostly SCC detection of early stage lesions is possible relatively common presentation of other benign pathology within the oral cavity, such as aphthous ulceration, delay in diagnosis primary surgical management the treatment of choice Goal locoregional tumor control functional impact on speech and swallowing appropriate selection of reconstructive techniques that assist appropriate wound healing while maximizing the patient’s capacity for oral 2
prevalence of smoking in the United States decreased from 42% in 1965 to 19% in 2010. Tobacco and alcohol consumption the most common preventable risk factors relation synergistic, with alcohol serving as a promoter for the carcinogenic effects of tobacco. Smoking 1. 9 -fold risk to males and a 3 fold risk to females for development of head and neck SCC. risk directly proportional to the years spent smoking and the number of cigarettes smoked per day Alcohol alone a 1. 7 -fold risk to males who drink one to two drinks per day compared with nondrinkers. This risk rises to more than threefold for heavy drinkers. Individuals who both smoke (two packs per day) and drink (four units of alcohol per day) are 35 times more likely to develop cancer when compared with controls. 9% of U. S. adults meet the criteria for an alcohol-use disorder. 3
rate of death from any cause among current smokers was three times that of those who had never smoked (ages 25 to 79 years) neoplastic, vascular, respiratory, and other smoking-related causes Smoking cessation before the age of 40 90% decreased risk smoking rates have declined, the rate of death from chronic obstructive pulmonary disease continues to increase length of time smoking cessation prior to surgery (shortterm vs. long-term) longer better Freedman study 450000 men and women , smoking habit Montero in 25 year smoking & drinking decline oral tongue the most subsite , men over 60 Smokers tumors of the larynx, hypopharynx, and floor of the mouth The time to first cigarette (TTFC), considered a distinct nicotine-dependence phenotype, is an indicator of risk Pharyngeal , FOM , palate cancer quit smoking and relapse after cessation Head & neck cancer &smoke more regional metastasis and extracapsular 4 spread
Smoking and habitual use of alcohol have also been associated with CDKN 2 B gene methylation , more mutation and chromosomal changes, , TP 53 mutation Former smokers, defined as those individuals who had quit more than 10 years earlier, demonstrate a genetic profile more consistent with nonsmokers A recent review of the Surveillance, Epidemiology, and End Results database of 71, 446 cases of oral cavity and pharyngeal cancer (1975 through 2008) showed an increasing rate of oral tongue cancer of unknown etiology in young patients; this was seen in females more often than in males and in individuals 25 to 44 years of age who were nonsmokers negative for human papillomavirus (HPV). In the same time frame, a decrease in total incidence of all cases of oral cavity and pharyngeal cancer was seen and was considered to reflect reductions in rates of smoking and habitual use of alcohol. World Health Organization International Agency for Research on Cancer has concluded that evidence is sufficient to state that smokeless tobacco causes oral and pancreatic cancer in humans 5
Betel nut (including its derivatives, such as betel quid) the fourth most abused substance estimated 10% of the world population Various other substances, such as tobacco, are added in the chewed product. Surprisingly, the addition of tobacco does not significantly increase the carcinogenicity of the product beyond the already well-established risk seen with habitual use of betel nut. Oral submucosal fibrosis (OSF) is a chronic inflammatory reaction associated with the habitual use of betel nut and betel quid and typically presents as a burning sensation in the oral buccal mucosa that manifests with trismus on examination. A dose-response relationship occurs with habitual use, and the rate of malignant transformation has been reported to be greater than 5% reverse smoking 47 times hard palate carcinoma 6
Environmental ultraviolet light exposure lip cancer the vermilion border of the lower lip Pipe smoking associated with the development of lip carcinoma. Mechanical irritation, thermal injury, and chemical exposure are suspected to be etiologic factors in the development of lip cancer in pipe-smoking patients. Fanconi anemia Dental restorations compounds Plummer-Vinson syndrome (achlorhydria, iron deficiency anemia, and mucosal atrophy of the mouth, pharynx, and esophagus), chronic infection with syphilis, long-term immunosuppression, and HIV infection SCC at a younger age (mean 31. 7 years) with poorly differentiated tumor and stage III/IV disease. elevated risk for the development of cancers of the oral cavity/pharynx, tongue, anus, liver, larynx, lung/bronchus, 7 and penis and also Hodgkin lymphoma
MOLECULAR BIOLOGY Tumor development loss of multiple signaling mechanisms that regulate the control of cell growth HPV an epitheliotropic virus oral cavity SCC The overall incidence of oral HPV infection in the United States, based on 2009/2010 survey data, was 6. 9% in men and women aged 14 to 69 years Oral HPV 16 infection was 1. 0% Prevalence of oral HPV was significantly higher in men and was linked to the number of sexual partners in the patient history and the number of cigarettes smoked per day HPV oncoproteins E 6 and E 7 have the ability to bind and degrade tumor suppressor gene products of TP 53 and RB 1, respectively This binding can impair the capacity of the cell cycle to arrest for the repair of DNA damage and results in an accumulation of genetic changes that can facilitate malignant Transformation The incidence of HPV in oral tongue carcinoma has been reported to be less than 2% The role of HPV in carcinogenesis and the effect on prognosis are far different with oral cancer than with oropharyngeal carcinoma For nonoropharyngeal carcinomas, no significant data are available to suggest that a survival advantage or improved prognosis can be experienced at other head and neck primary sites found to be HPV positive 8
• Sirtuin-3 is overexpressed in oral SCC in vitro and in vivo. Downregulation inhibits growth and induces apoptosis while increasing tumor sensitivity to radiation therapy and cisplatin in vitro. Sirtuin-3 is considered to have a novel role as a promoter of cell proliferation and survival in oral SCC and may represent a potential site for targeted therapy • Levels of remodeling and spacing factor 1 (RSF-1), a subunit of a chromatin remodeling complex, are significantly elevated in the setting of oral SCC and correlate with angiolymphatic invasion, tumor recurrence, and compromised OS. RSF-1 knockdown decreased cellular proliferation and induced apoptosis; RSF-1 overexpression is believed to contribute to the aggressiveness of oral cancer and to also potentiate chemotherapy and radiation resistance • MTBP is an MDM 2 binding protein that can alter p 53/MDM 2 homeostasis, and it correlates with Ki-67 expression; it likely has both oncogenic and tumor-suppressing properties. Vlatkovic generated and validated an antibody to MTBP and utilized it to evaluate 198 head and neck SCCa samples. They revealed that the biomarker combination of p 53 positivity and low MDM 2 levels was significantly associated with reduced OS. In patients with this phenotype, the authors also found that loss of MTBP expression was significantly associated with markedly reduced OS • Micro. RNA-137 plays an essential role in cell cycle control at the G 1/S phase checkpoint aberrant micro. RNA-137 promoter methylation in 16. 4% (11/67) of head and neck SCC specimens (oral cavity, 4; oropharynx, 5; larynx, 2). This finding was seen more frequently in individuals who ate fewer daily servings of fruit and vegetables and was significantly associated with a lower OS rate • reduced secretory leukocyte protease inhibitor RNA levels in oral SCC compared with normal epithelium. Secretory leukocyte protease inihibitor is an inhibitor of plasminogen activation and macrophage matrix-degrading metalloproteinases, and it is considered 9 to have a protective role in the prevention of local tumor invasion and metastasis of oral carcinoma
• Hyaluronan/CD 44 -mediated signaling has been proposed to have a role in the promotion of tumor progression and chemoresistance. The leukemia-associated Rhoguanine nucleotide exchange factor associates with CD 44 and endothelial growth factor receptor (EGFR) to create intracellular cross talk with the Ras, Rho. A, and phosphatidylinositol 3 -kinase (PI 3 K) pathways, which can result in cell growth, migration, and tumor survival. The secretion of matrix metalloproteinases is also regulated by hyaluronan/CD 44 mediated pathways • In a study of whole-exome sequencing, Agrawal and associates identified six gene mutations—TP 53, CDKN 2 A, PIK 3 CA, HRAS, FBXW 7, and NOTCH 1—in multiple specimens that were associated with the development of head and neck SCC. Findings from this study suggested that NOTCH 1 functions as an important tumor suppressor gene in head and neck SCC 10
• Overexpression of mutant TP 53 has been associated with carcinogenesis at multiple sites. Point mutations in TP 53 have been reported in up to 45% of head and neck carcinomas. assessment of specimens on the basis of p 53 staining to guide the need for further treatment TP 53 mutation is a key event in the malignant transformation of more than 50% of head and neck SCCs in smokers • The Akt receptor has been correlated with the histologic progression of oral premalignant lesions to carcinoma phosphorylated Akt, when highly expressed, is associated with recurrence and shorter DFS independent of a patient’s overall staging Intracellular adhesion molecule 5 (ICAM-5, telecephalin) expression is associated with perineural invasion with head and neck carcinoma. When normal oral mucosal specimens were examined, none demonstrated detectable ICAM-5 levels, whereas 64% of matched primary SCC specimens showed expression ICAM-5 expression was decreased when a PI 3 K inhibitor was utilized, which supports the likely interaction of ICAM-5 in the PI 3 K/Akt pathway signaling 11
EPIDEMIOLOGY Oral cavity malignancies (excluding those of the lip) 14% of all head and neck cancers • National Cancer Data Base from 1985 through 1996, patients diagnosed with an oral cavity cancer had a mean age at presentation of 64 years with a male predominance (60%) SCC represented the majority of lesions (86. 3%), adenocarcinoma (5. 9%), verrucous carcinoma (2. 0%), lymphoma (1. 5%), Kaposi sarcoma (1. 5%) At the time of diagnosis, 55% of patients had early-stage lesions (stages I and II) Patients younger than 35 years of age were more likely to present with oral tongue SCC than were older patients (76. 1% vs. 33%) patients younger than age 35 were less likely to present with a floor-of-mouth SCC (10. 5% vs. 35. 9%) Of note, the National Cancer Data Base findings did not reveal a poorer overall prognosis for those patients diagnosed at a younger age. In fact, younger patients demonstrated a better 5 -year survival (63. 7%) than older, stage-matched patients (51% for those 36 to 65 12 years of age vs. 47. 6% for those >65 years)
Blacks and lower-income patients more frequently presented with advanced-stage lesions 5 -year survival was found to be worse for males, blacks, and patients older than 65 years Adenocarcinoma more frequently in women and was typically diagnosed on the hard palate After adjustment for age, race, gender, smoking, alcohol use, primary site, socioeconomic status, treatment, and cancer stage, uninsured patients and those receiving Medicaid or Medicare disability insurance coverage (<65 years) are at increased risk of death after diagnosis of SCC compared with patients who have private insurance. Medicaid and uninsured patients were also significantly more likely to present with an advanced-stage tumor at diagnosis and to present with at least one positive lymph node compared with patients who had private insurance. oral tongue carcinoma in patients younger than 40 years of age increased 60% from 1973 to 1984 and has since stabilized During this same time frame, the incidence of carcinoma at all other oral cavity subsites remained constant or decreased This rise was primarily related to patients born during the years 1938 to 1948, and the 5 year determinant survival of these patients was better than that for older individuals 13
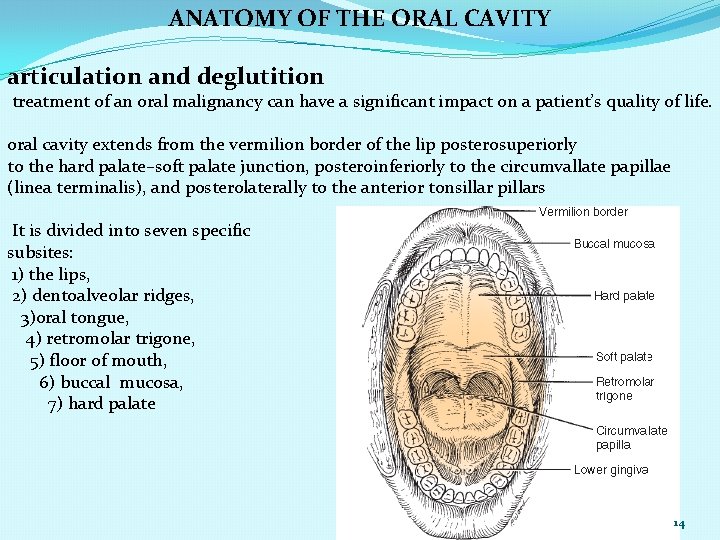
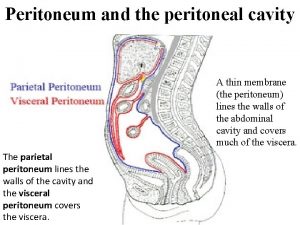
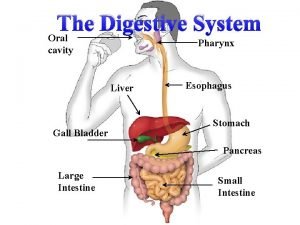
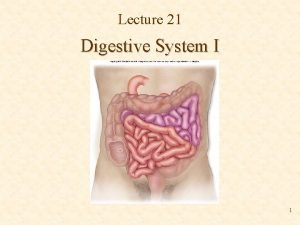
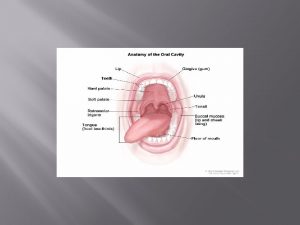
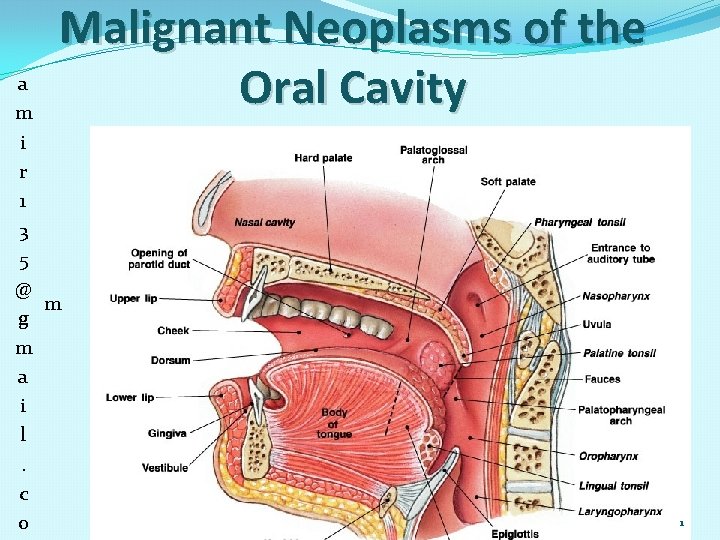
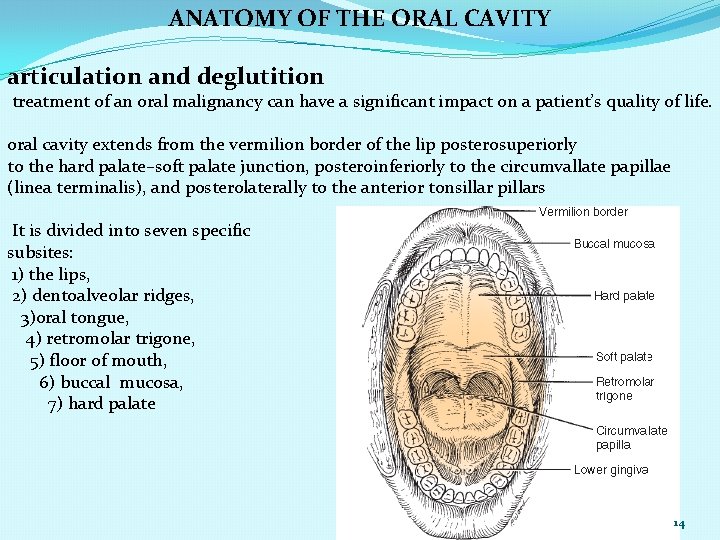
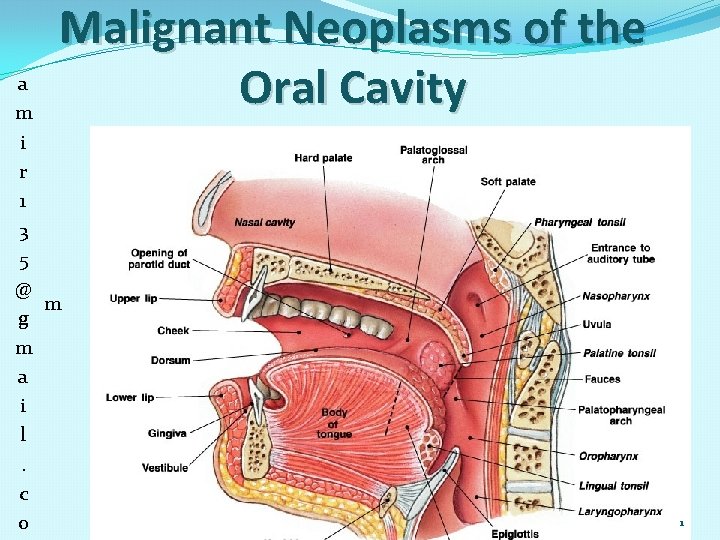
ANATOMY OF THE ORAL CAVITY articulation and deglutition treatment of an oral malignancy can have a significant impact on a patient’s quality of life. oral cavity extends from the vermilion border of the lip posterosuperiorly to the hard palate–soft palate junction, posteroinferiorly to the circumvallate papillae (linea terminalis), and posterolaterally to the anterior tonsillar pillars It is divided into seven specific subsites: 1) the lips, 2) dentoalveolar ridges, 3)oral tongue, 4) retromolar trigone, 5) floor of mouth, 6) buccal mucosa, 7) hard palate 14
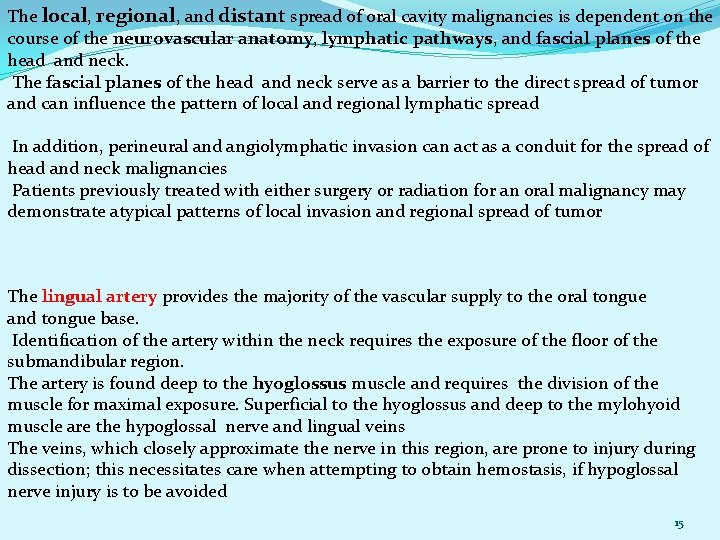
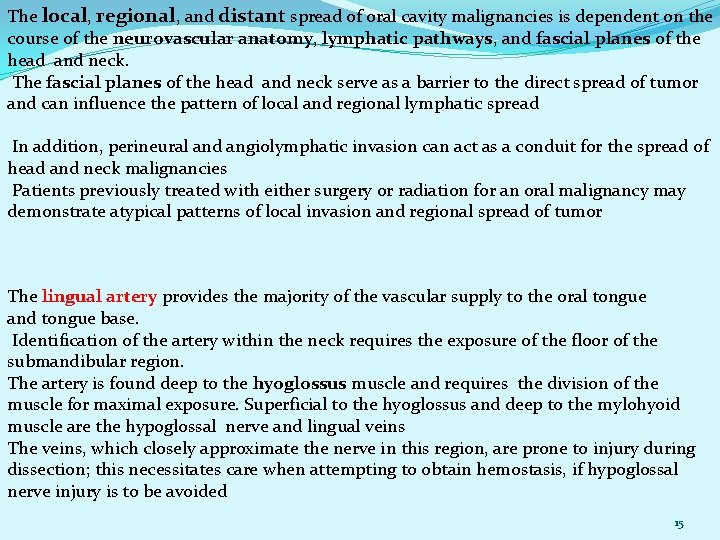
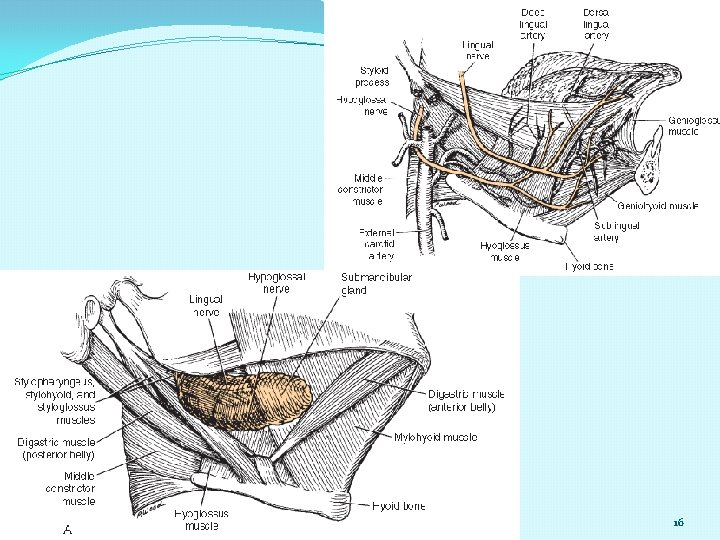
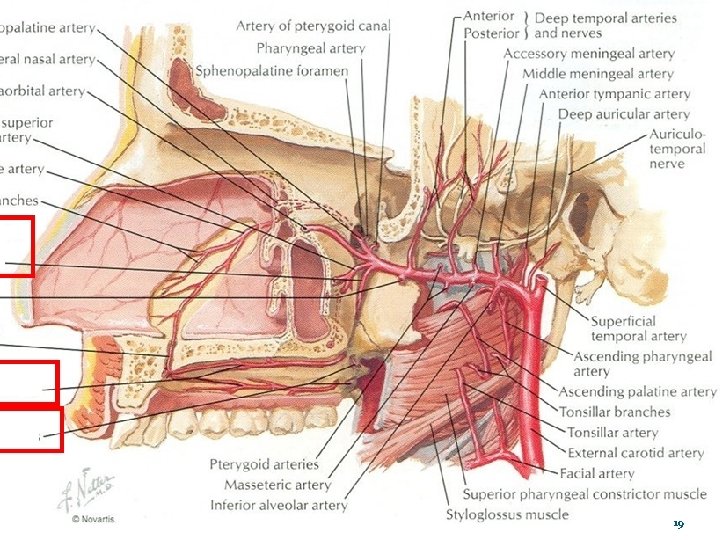
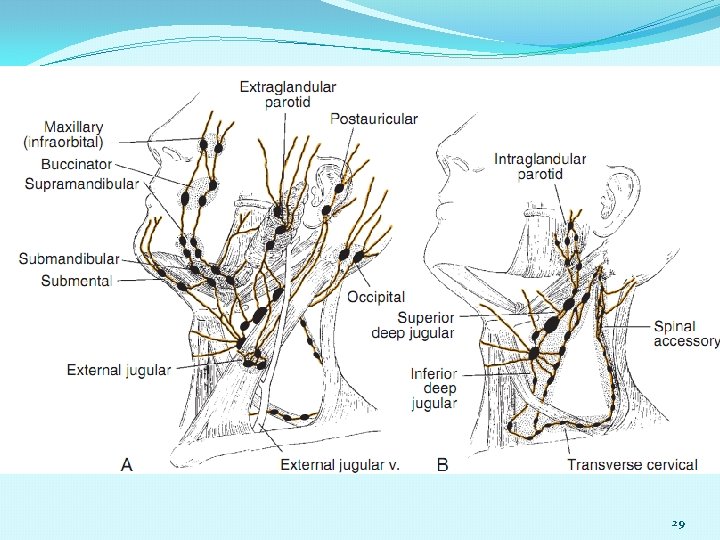
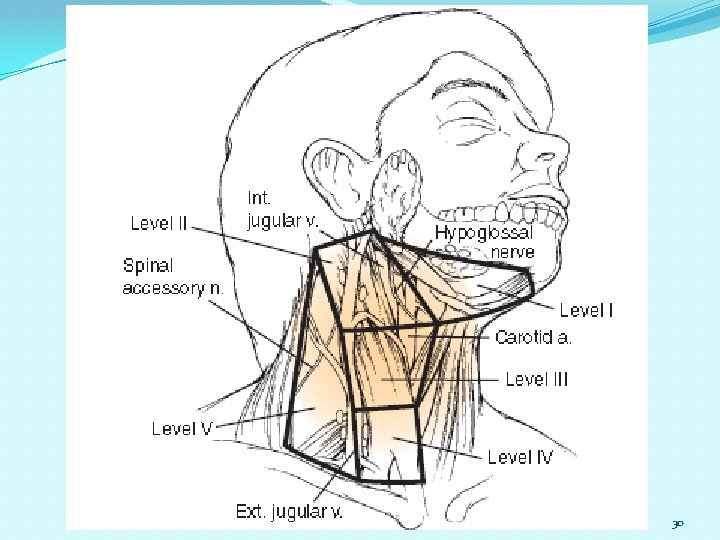
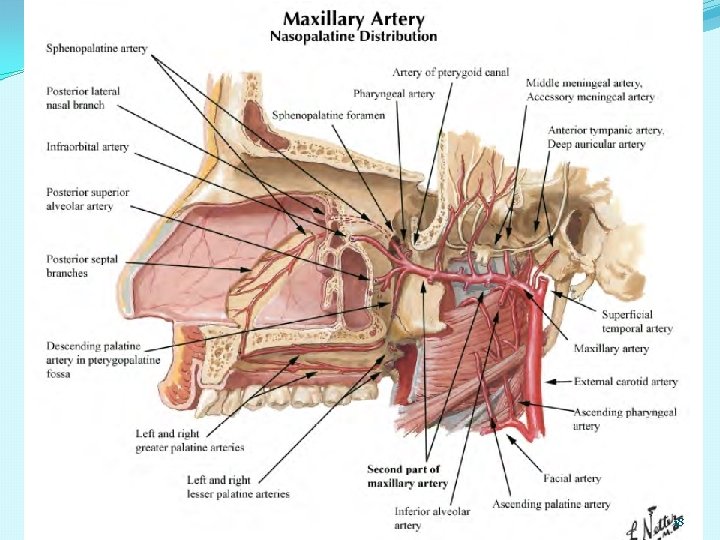
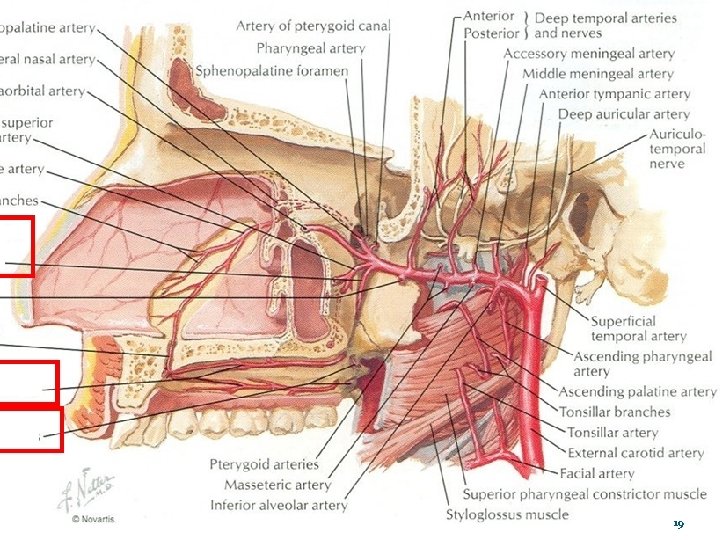
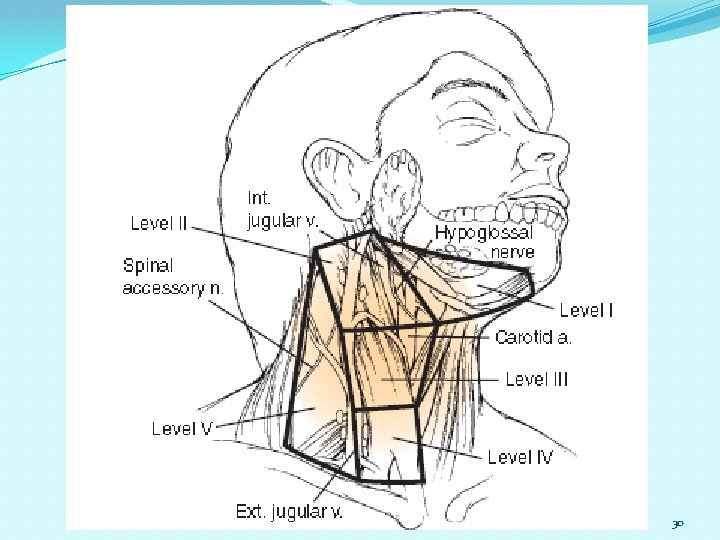
The local, regional, and distant spread of oral cavity malignancies is dependent on the course of the neurovascular anatomy, lymphatic pathways, and fascial planes of the head and neck. The fascial planes of the head and neck serve as a barrier to the direct spread of tumor and can influence the pattern of local and regional lymphatic spread In addition, perineural and angiolymphatic invasion can act as a conduit for the spread of head and neck malignancies Patients previously treated with either surgery or radiation for an oral malignancy may demonstrate atypical patterns of local invasion and regional spread of tumor The lingual artery provides the majority of the vascular supply to the oral tongue and tongue base. Identification of the artery within the neck requires the exposure of the floor of the submandibular region. The artery is found deep to the hyoglossus muscle and requires the division of the muscle for maximal exposure. Superficial to the hyoglossus and deep to the mylohyoid muscle are the hypoglossal nerve and lingual veins The veins, which closely approximate the nerve in this region, are prone to injury during dissection; this necessitates care when attempting to obtain hemostasis, if hypoglossal nerve injury is to be avoided 15
16
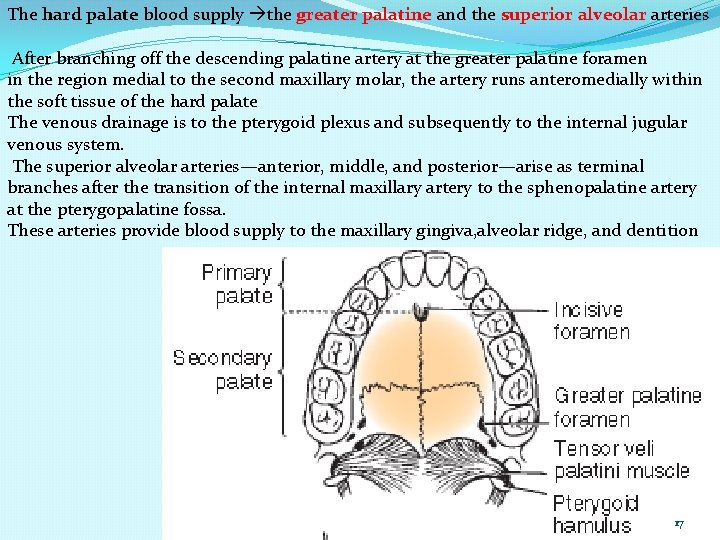
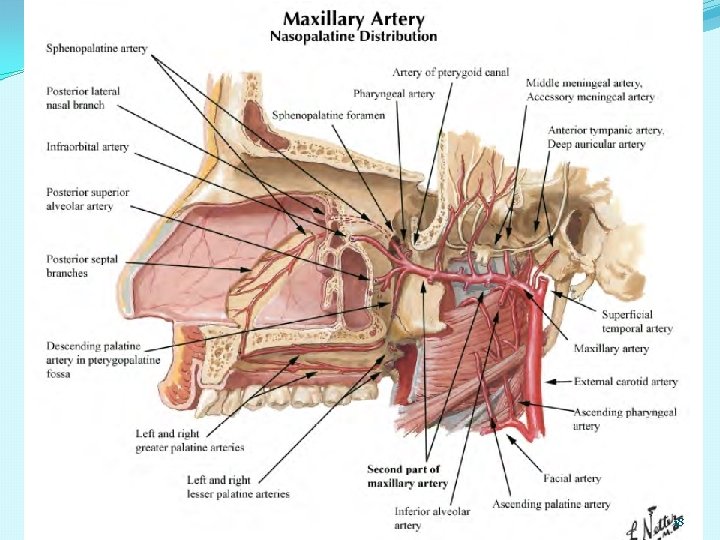
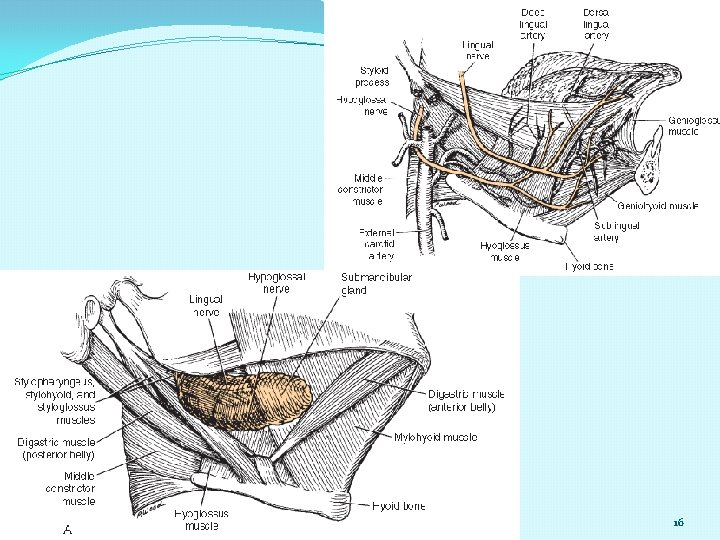
The hard palate blood supply the greater palatine and the superior alveolar arteries After branching off the descending palatine artery at the greater palatine foramen in the region medial to the second maxillary molar, the artery runs anteromedially within the soft tissue of the hard palate The venous drainage is to the pterygoid plexus and subsequently to the internal jugular venous system. The superior alveolar arteries—anterior, middle, and posterior—arise as terminal branches after the transition of the internal maxillary artery to the sphenopalatine artery at the pterygopalatine fossa. These arteries provide blood supply to the maxillary gingiva, alveolar ridge, and dentition 17
18
19
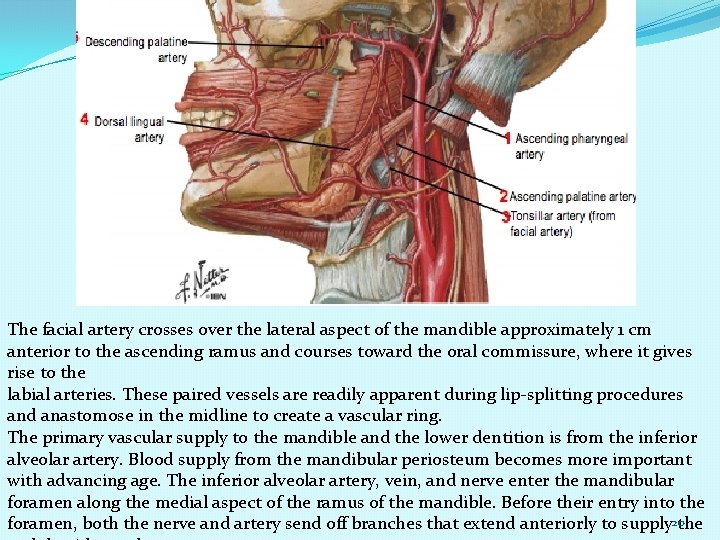
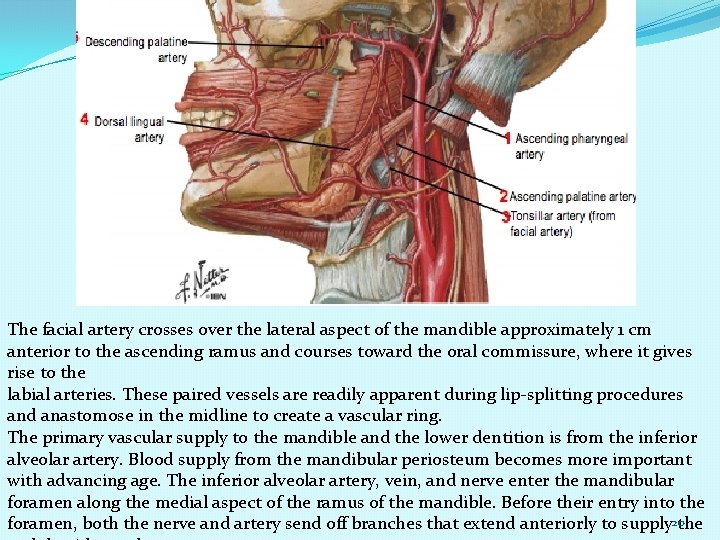
The facial artery crosses over the lateral aspect of the mandible approximately 1 cm anterior to the ascending ramus and courses toward the oral commissure, where it gives rise to the labial arteries. These paired vessels are readily apparent during lip-splitting procedures and anastomose in the midline to create a vascular ring. The primary vascular supply to the mandible and the lower dentition is from the inferior alveolar artery. Blood supply from the mandibular periosteum becomes more important with advancing age. The inferior alveolar artery, vein, and nerve enter the mandibular foramen along the medial aspect of the ramus of the mandible. Before their entry into the foramen, both the nerve and artery send off branches that extend anteriorly to supply 20 the
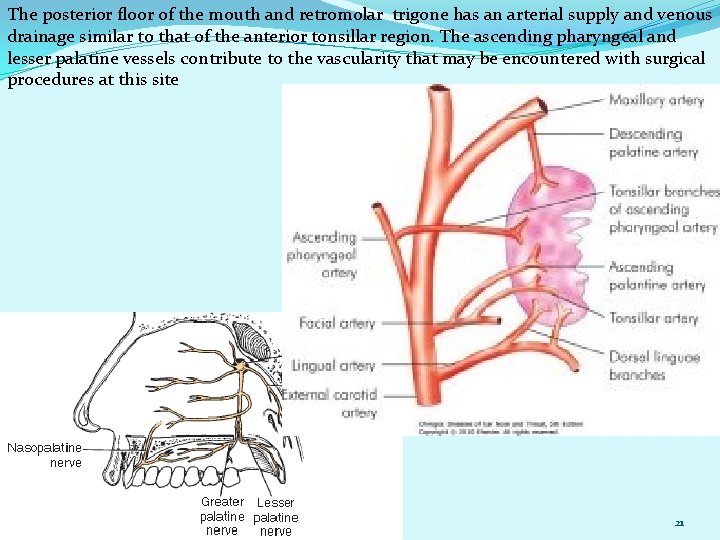
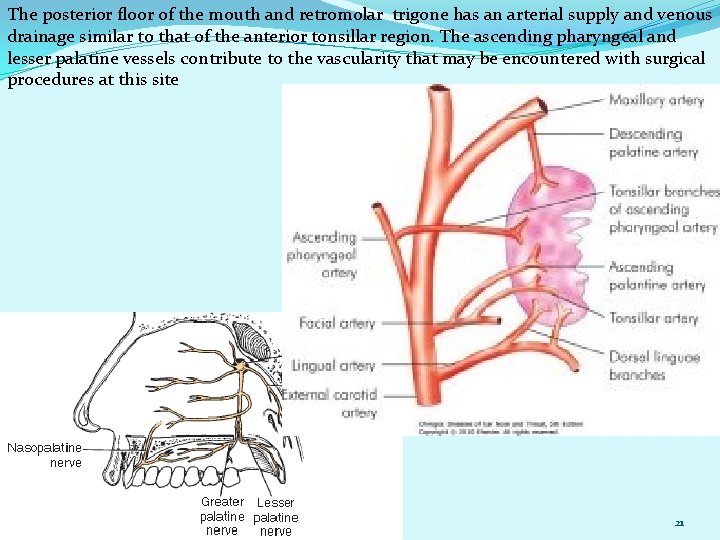
The posterior floor of the mouth and retromolar trigone has an arterial supply and venous drainage similar to that of the anterior tonsillar region. The ascending pharyngeal and lesser palatine vessels contribute to the vascularity that may be encountered with surgical procedures at this site 21
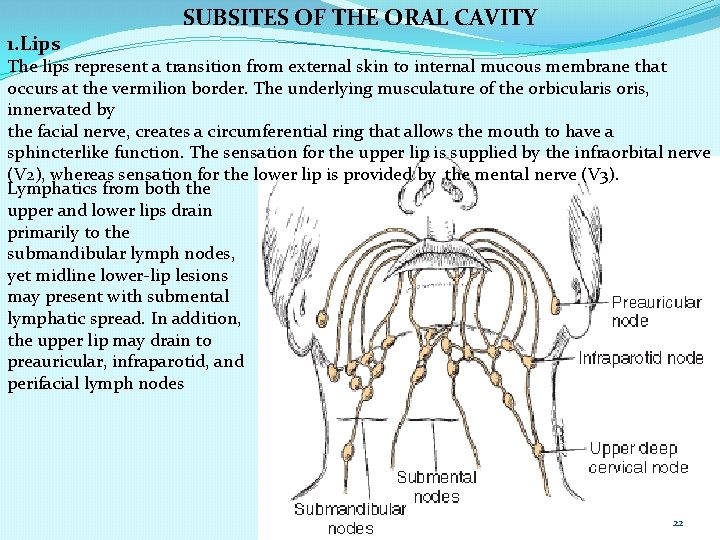
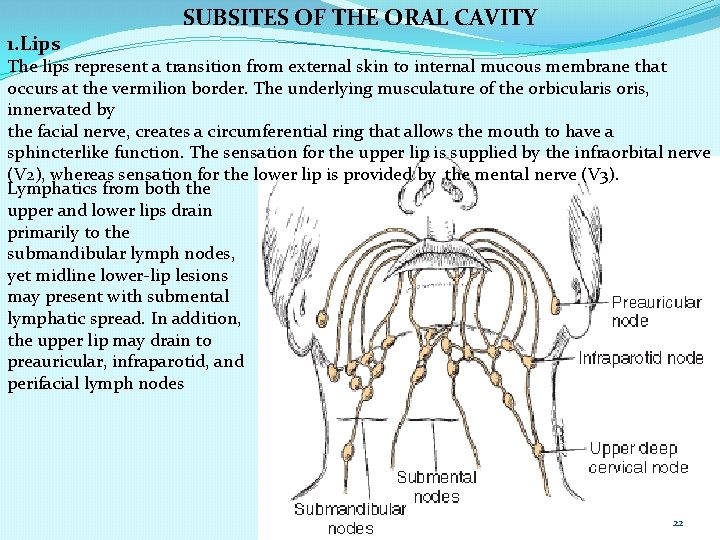
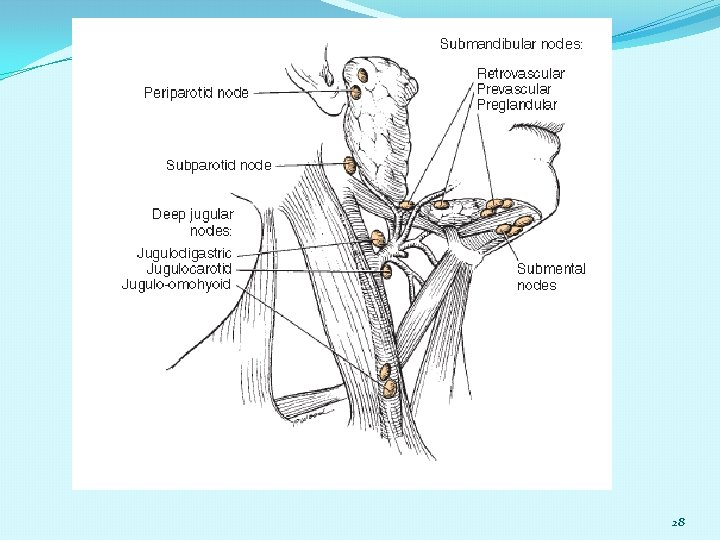
1. Lips SUBSITES OF THE ORAL CAVITY The lips represent a transition from external skin to internal mucous membrane that occurs at the vermilion border. The underlying musculature of the orbicularis oris, innervated by the facial nerve, creates a circumferential ring that allows the mouth to have a sphincterlike function. The sensation for the upper lip is supplied by the infraorbital nerve (V 2), whereas sensation for the lower lip is provided by the mental nerve (V 3). Lymphatics from both the upper and lower lips drain primarily to the submandibular lymph nodes, yet midline lower-lip lesions may present with submental lymphatic spread. In addition, the upper lip may drain to preauricular, infraparotid, and perifacial lymph nodes 22
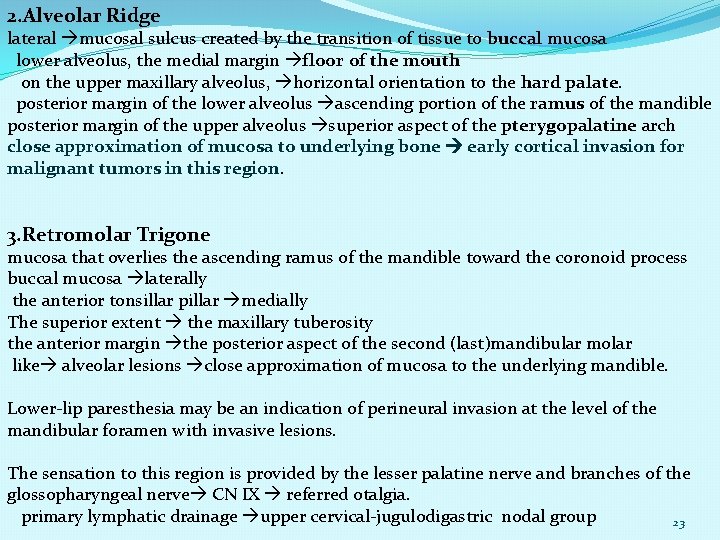
2. Alveolar Ridge lateral mucosal sulcus created by the transition of tissue to buccal mucosa lower alveolus, the medial margin floor of the mouth on the upper maxillary alveolus, horizontal orientation to the hard palate. posterior margin of the lower alveolus ascending portion of the ramus of the mandible posterior margin of the upper alveolus superior aspect of the pterygopalatine arch close approximation of mucosa to underlying bone early cortical invasion for malignant tumors in this region. 3. Retromolar Trigone mucosa that overlies the ascending ramus of the mandible toward the coronoid process buccal mucosa laterally the anterior tonsillar pillar medially The superior extent the maxillary tuberosity the anterior margin the posterior aspect of the second (last)mandibular molar like alveolar lesions close approximation of mucosa to the underlying mandible. Lower-lip paresthesia may be an indication of perineural invasion at the level of the mandibular foramen with invasive lesions. The sensation to this region is provided by the lesser palatine nerve and branches of the glossopharyngeal nerve CN IX referred otalgia. primary lymphatic drainage upper cervical-jugulodigastric nodal group 23
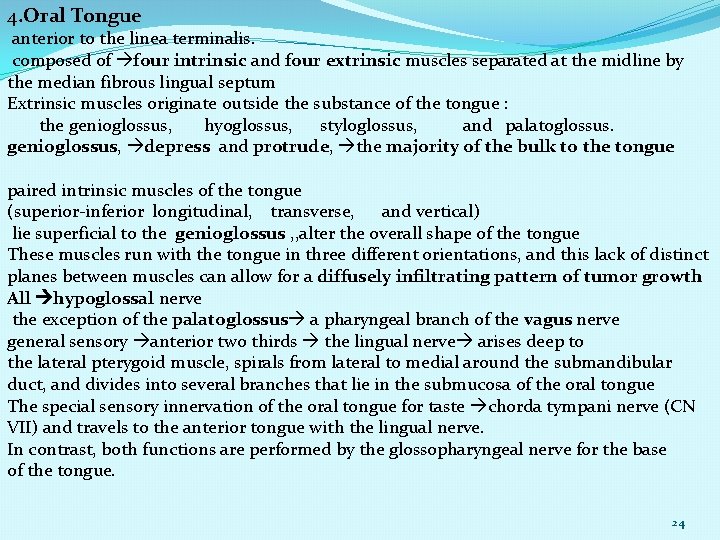
4. Oral Tongue anterior to the linea terminalis. composed of four intrinsic and four extrinsic muscles separated at the midline by the median fibrous lingual septum Extrinsic muscles originate outside the substance of the tongue : the genioglossus, hyoglossus, styloglossus, and palatoglossus. genioglossus, depress and protrude, the majority of the bulk to the tongue paired intrinsic muscles of the tongue (superior-inferior longitudinal, transverse, and vertical) lie superficial to the genioglossus , , alter the overall shape of the tongue These muscles run with the tongue in three different orientations, and this lack of distinct planes between muscles can allow for a diffusely infiltrating pattern of tumor growth All hypoglossal nerve the exception of the palatoglossus a pharyngeal branch of the vagus nerve general sensory anterior two thirds the lingual nerve arises deep to the lateral pterygoid muscle, spirals from lateral to medial around the submandibular duct, and divides into several branches that lie in the submucosa of the oral tongue The special sensory innervation of the oral tongue for taste chorda tympani nerve (CN VII) and travels to the anterior tongue with the lingual nerve. In contrast, both functions are performed by the glossopharyngeal nerve for the base of the tongue. 24
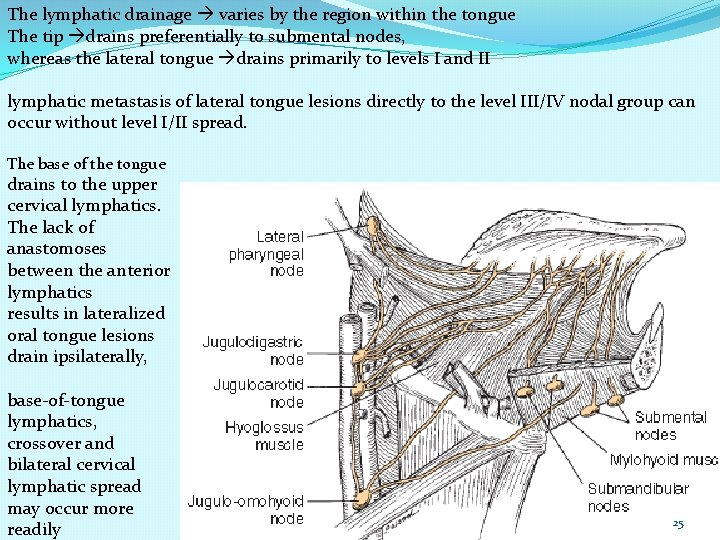
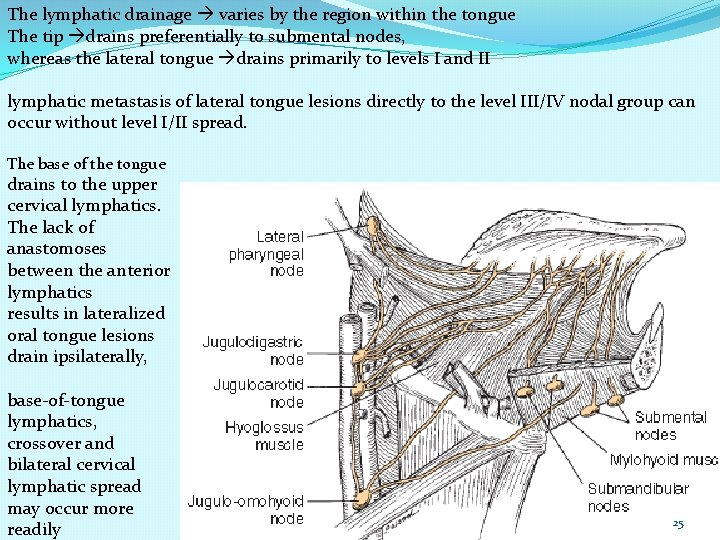
The lymphatic drainage varies by the region within the tongue The tip drains preferentially to submental nodes, whereas the lateral tongue drains primarily to levels I and II lymphatic metastasis of lateral tongue lesions directly to the level III/IV nodal group can occur without level I/II spread. The base of the tongue drains to the upper cervical lymphatics. The lack of anastomoses between the anterior lymphatics results in lateralized oral tongue lesions drain ipsilaterally, base-of-tongue lymphatics, crossover and bilateral cervical lymphatic spread may occur more readily 25
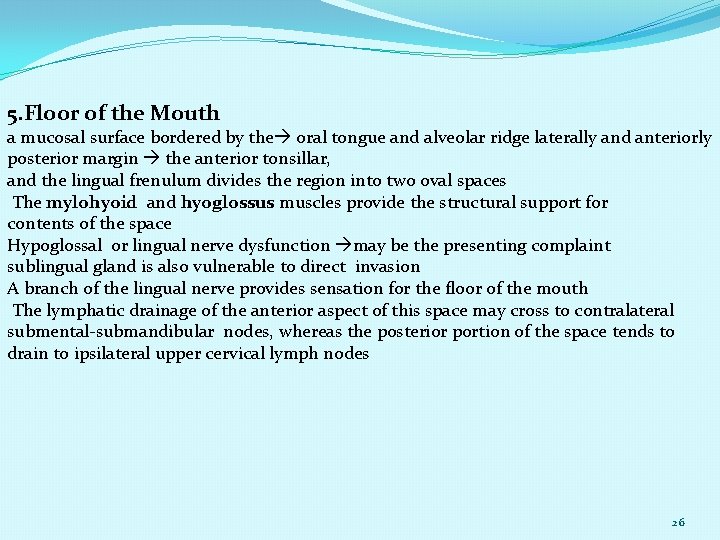
5. Floor of the Mouth a mucosal surface bordered by the oral tongue and alveolar ridge laterally and anteriorly posterior margin the anterior tonsillar, and the lingual frenulum divides the region into two oval spaces The mylohyoid and hyoglossus muscles provide the structural support for contents of the space Hypoglossal or lingual nerve dysfunction may be the presenting complaint sublingual gland is also vulnerable to direct invasion A branch of the lingual nerve provides sensation for the floor of the mouth The lymphatic drainage of the anterior aspect of this space may cross to contralateral submental-submandibular nodes, whereas the posterior portion of the space tends to drain to ipsilateral upper cervical lymph nodes 26
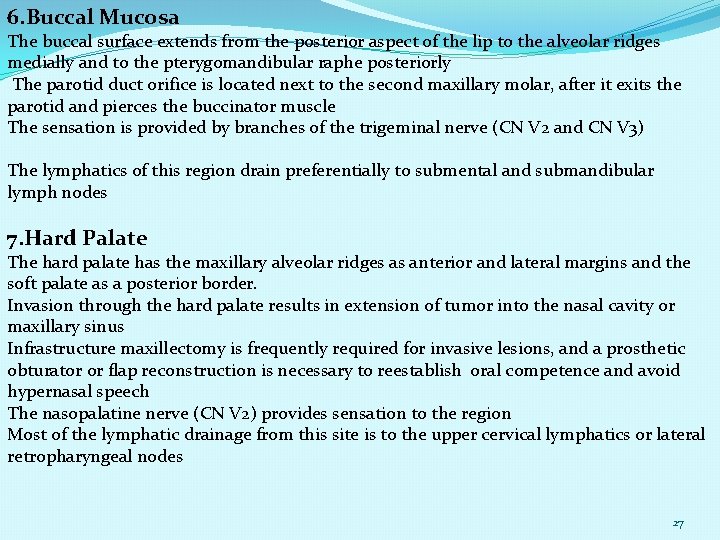
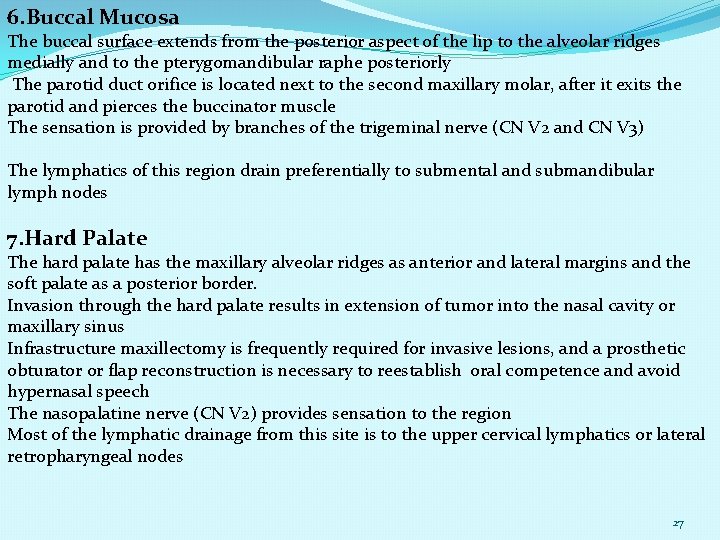
6. Buccal Mucosa The buccal surface extends from the posterior aspect of the lip to the alveolar ridges medially and to the pterygomandibular raphe posteriorly The parotid duct orifice is located next to the second maxillary molar, after it exits the parotid and pierces the buccinator muscle The sensation is provided by branches of the trigeminal nerve (CN V 2 and CN V 3) The lymphatics of this region drain preferentially to submental and submandibular lymph nodes 7. Hard Palate The hard palate has the maxillary alveolar ridges as anterior and lateral margins and the soft palate as a posterior border. Invasion through the hard palate results in extension of tumor into the nasal cavity or maxillary sinus Infrastructure maxillectomy is frequently required for invasive lesions, and a prosthetic obturator or flap reconstruction is necessary to reestablish oral competence and avoid hypernasal speech The nasopalatine nerve (CN V 2) provides sensation to the region Most of the lymphatic drainage from this site is to the upper cervical lymphatics or lateral retropharyngeal nodes 27
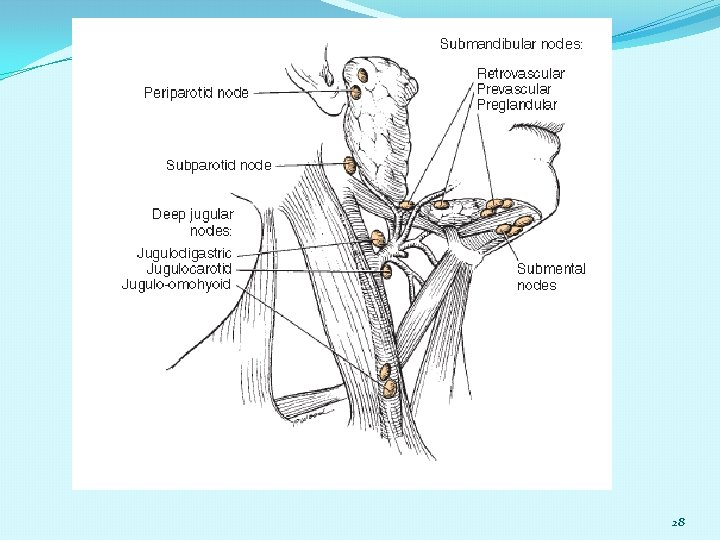
28
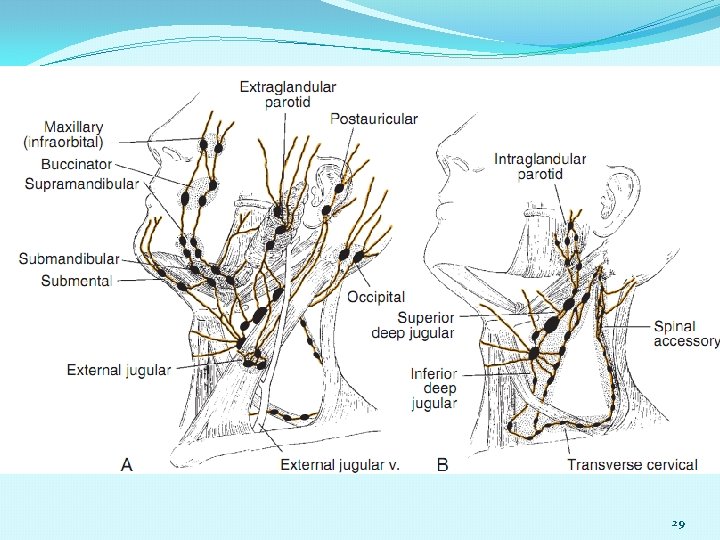
29
30
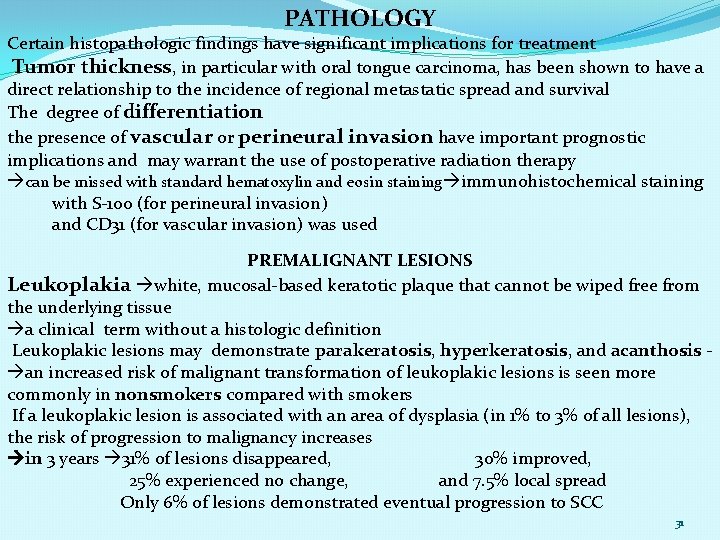
PATHOLOGY Certain histopathologic findings have significant implications for treatment Tumor thickness, in particular with oral tongue carcinoma, has been shown to have a direct relationship to the incidence of regional metastatic spread and survival The degree of differentiation the presence of vascular or perineural invasion have important prognostic implications and may warrant the use of postoperative radiation therapy can be missed with standard hematoxylin and eosin staining immunohistochemical staining with S-100 (for perineural invasion) and CD 31 (for vascular invasion) was used PREMALIGNANT LESIONS Leukoplakia white, mucosal-based keratotic plaque that cannot be wiped free from the underlying tissue a clinical term without a histologic definition Leukoplakic lesions may demonstrate parakeratosis, hyperkeratosis, and acanthosis an increased risk of malignant transformation of leukoplakic lesions is seen more commonly in nonsmokers compared with smokers If a leukoplakic lesion is associated with an area of dysplasia (in 1% to 3% of all lesions), the risk of progression to malignancy increases in 3 years 31% of lesions disappeared, 30% improved, 25% experienced no change, and 7. 5% local spread Only 6% of lesions demonstrated eventual progression to SCC 31
Erythroplakia is a red mucosal plaque that does not arise from any obvious mechanical cause and persists after removal of possible etiologic factors The associated risk for progression to carcinoma is significantly greater than that for leukoplakic lesions 91% had evidence of invasive dysplasia, carcinoma in situ, or severe dysplasia Oral submucosal fibrosis (OSF) betel nut and is associated with poor oral hygiene, advanced periodontitis, and the potential development of oral carcinoma With betel nut use, the buccal mucosa becomes thickened and the entire cheek becomes fibrotic, which results in trismus. Resection of tumors that arise in the buccal mucosa in patients with submucosal fibrosis can be challenging, and reconstruction can be complicated by wound breakdown. 371 patients from India with oral cancer, 112 of whom had a history of prior OSF in association with habitual betel nut use The most common oral cancer subsite was the buccal mucosa in more than 50% of cases, followed by the oral tongue Patients younger men (mean age, 45 years) with better histologic differentiation, lower rates of regional metastasis, and less extranodal spread 32
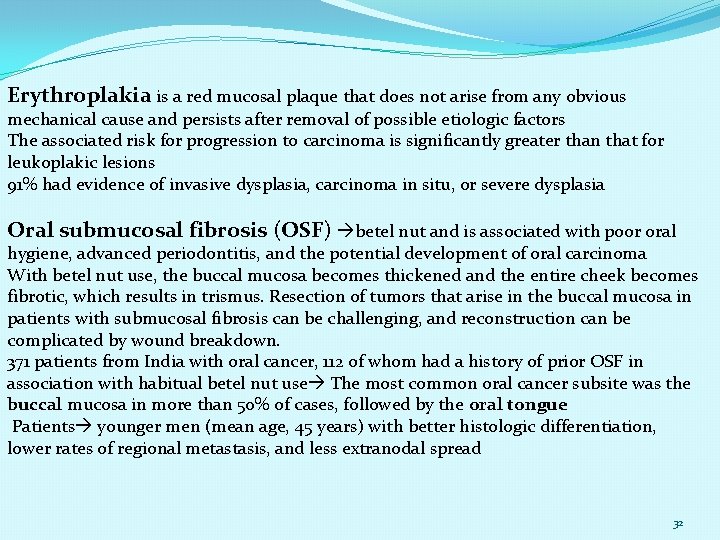
Lichen planus, in particular the erosive subtype, oral carcinoma etiology of lichen planus is unknown T-cell lymphocyte infiltration is not typically associated with immunologic disorders The typical patient a female in the fourth decade of life Lesions demonstrate a lacy pattern of white striae; atrophic lesions are red and smooth, whereas erosive lesions have depressed margins and are covered by a layer of fibrinous exudate Dysplasia is the abnormal maturation and differentiation of mucosal epithelium with features of an increased nuclear/ cytoplasmic ratio, loss of polarity, increased mitoses, and loss of intercellular adherence Dysplasia is graded as mild, moderate, or severe Verrucous hyperplasia is a histologic finding that appears similar to verrucous carcinoma yet differs from the malignant form in that it does not invade the lamina propria Necrotizing sialometaplasia, although it appears clinically ominous, is benign. The typical feature is a butterfly-shaped area of ulceration at the junction of the hard and soft palate in the region of the palatine foramen The etiology of this clinical lesion is necrosis of minor salivary acini usually secondary to a localized pressure injury This may be seen in the scenario of a poorly fitting or overused denture 33
SQUAMOUS CELL CARCINOMA AND SQUAMOUS CELL CARCINOMA VARIANTS --The spindle cell variant of SCC, also known as sarcomatoid SCC, is typically diagnosed in the oral cavity, oropharynx, or larynx heterogeneous appearance with spindle-shaped cells interwoven with squamous cells immunohistochemical staining for keratin markers high risk of locoregional recurrence; however, OS is similar to that of conventional SCC. more responsive to primary surgical management than to chemoradiation --Basaloid carcinoma been considered a high-grade variant with a predilection for regional and distant metastasis; however, when clinical staging is matched, the 5 -year DFS associated for oral basaloid carcinoma is similar to that of poorly differentiated and moderately differentiated oral carcinomas -- verrucous carcinoma, a thick zone of nonproliferation and nonkeratinizing cells distinguishes this entity histologically. The typical presentation is on the buccal mucosa (50%) a low-grade variant of SCC and is exophytic in appearance, has the capacity to invade locally and yet carries a low risk of regional spread considered to be “radioresistant, ” surgical excision treatment of choice 34
OTHER PATHOLOGIES Other differential diagnosis: pyogenic granuloma, pseudoepitheliomatous hyperplasia, lymphoma, minor salivary gland tumors, and sarcomas The most common minor salivary gland malignancies are: adenoid cystic carcinoma, mucoepidermoid carcinoma (low and high grade), polymorphous low-grade adenocarcinoma and adenocarcinoma All of these may present as a painless, slowgrowing, submucosal mass at the junction of the hard and soft palate Adenoid cystic carcinoma perineural invasion the greater palatine nerve pterygopalatine ganglion ascend to the skull base Sarcomas of the oral cavity usually arise in the mandible or hard palate and include: osteosarcoma , chondrosarcoma, malignant fibrous histiocytoma, rhabdomyosarcoma, and liposarcoma 5 -year local control rate for head and neck osteosarcoma of 78% and OS of 70% --- osteosarcoma maxilla =mandible Surgery was performed in all patients, and neoadjuvant chemotherapy was used in 68%. Positive surgical margins were found to be the only significant negative predictor with respect to disease-specific survival 35

Osteosarcoma specimen of the right hemimandible 36
Ewing sarcoma Typically presenting in children, has a 1% to 2% incidence of presentation in the facial skeleton. The most common site of diagnosis in the mandible is at the ramus Treatment typically entails wide surgical excision in combination with chemotherapy. If possible, radiation is avoided to minimize the impact on subsequent facial growth Kaposi sarcoma is the most common HIV-associated malignancy The head and neck is the site for 63% of all presentation a mucosal or cutaneous lesion with a nodular or macular appearance and most commonly occurs on the hard palate Despite being considered an incurable disorder, a variety of treatment options that may offer remission for limited disease are available Local therapies include radiation, intralesional injection of chemotherapy, cryotherapy, alitretinoin gel, laser therapy, and surgical excision Systemic chemotherapy is reserved for advanced disease Desmoplastic neurotrophic melanoma is a nonpigmented lesion of the lower lip that presents as an ulceration and has a high incidence for perineural invasion Mucosal melanoma typically presents as a pigmented lesion of the oral cavity that may be associated with preexisting melanosis Pigmented lesions of the oral cavity should be considered for biopsy to exclude this diagnosis 37
DIAGNOSTIC EVALUATION SCREENING conventional oral examination brush cytology, tissue reflectance systems, and narrow-emission tissue fluorescence --gene microarray data from patient-matched normal controls and oral SCC create a tissue-specific gene-expression signature. They identified 92 genes differentially expressed between normal mucosa and oral carcinoma and created a 25 -gene predictor with the goal of clinical use to aid screening for early oral carcinoma average accuracy rate of greater than 87% was achieved eight genes that had significantly higher levels of DNA methylation in patients with oral SCC. Oral carcinoma was diagnosed with 100% sensitivity and 87. 5% specificity when positive for the combination of E-cadherin, transmembrane protein with epidermal growth factor–like and two follistatin–like 2 domains, retinoic acid receptor β, and O-6 methylguanine DNA methyltransferase. This technique of screening for methylated gene combinations through an oral rinse was considered promising for the purposes of screening for oral cancer. Future screening for oral cancer may be possible with outpatient biomarker laboratory assays St. John and colleagues have described the use of an assay for salivary interleukin-8 and serum interleukin-6 with promising results in patients with oral cavity and oropharyngeal carcinoma 38
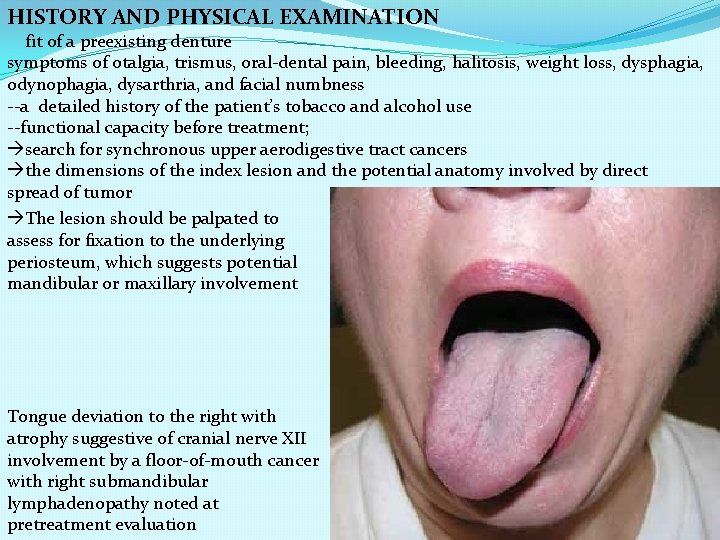
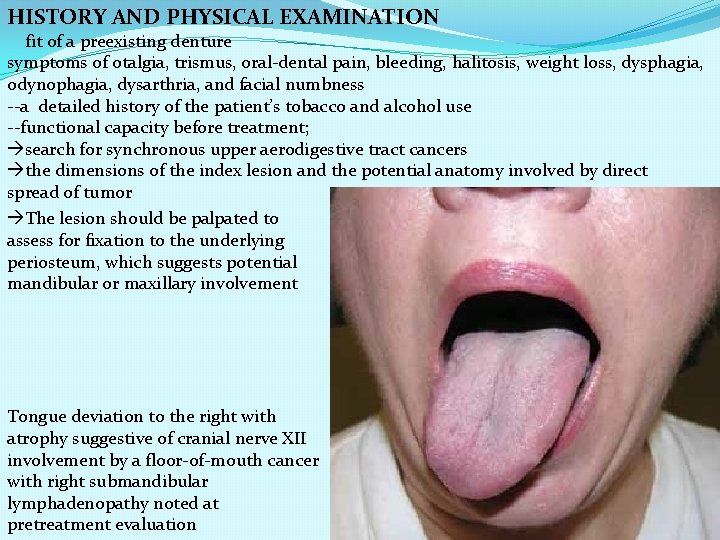
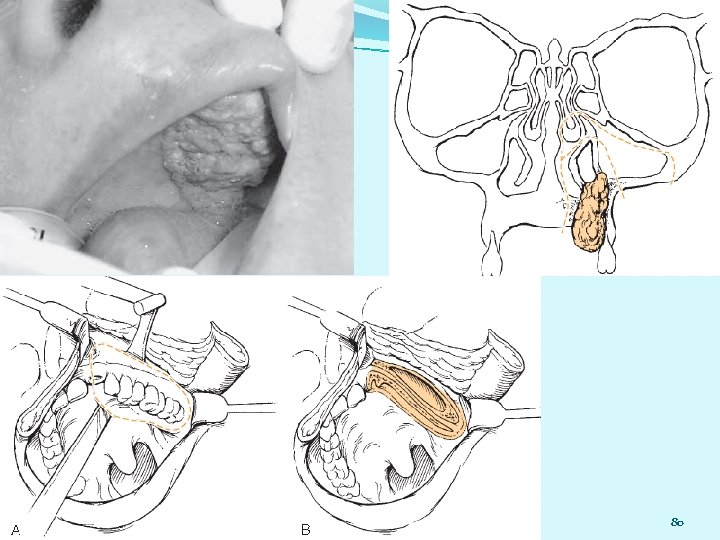
HISTORY AND PHYSICAL EXAMINATION fit of a preexisting denture symptoms of otalgia, trismus, oral-dental pain, bleeding, halitosis, weight loss, dysphagia, odynophagia, dysarthria, and facial numbness --a detailed history of the patient’s tobacco and alcohol use --functional capacity before treatment; search for synchronous upper aerodigestive tract cancers the dimensions of the index lesion and the potential anatomy involved by direct spread of tumor The lesion should be palpated to assess for fixation to the underlying periosteum, which suggests potential mandibular or maxillary involvement Tongue deviation to the right with atrophy suggestive of cranial nerve XII involvement by a floor-of-mouth cancer with right submandibular lymphadenopathy noted at pretreatment evaluation 39
. Determination of midline extension, regional lymphatic spread, and the need for reconstruction should be considered The appropriateness of specific donor sites for free and/or pedicled flap reconstruction should also be assessed. At the initial evaluation, if tissue pathology has not been previously obtained, a punch biopsy of the perimeter of the primary tumor and/or fine-needle aspiration (FNA, potentially ultrasound-guided) of suspected regional metastases should be performed. If the patient underwent biopsy at an outlying site before consultation, the specimen should be obtained and reviewed with the pathologist at the surgeon’s facility to confirm the tissue diagnosis. For patients who have already had imaging performed, films are reviewed for the extent of the primary disease and for regional lymphadenopathy. Imaging quality, timing relative to presentation, and need for supplemental imaging should be assessed. Before initiating treatment, the patient’s case should be presented at a multidisciplinary tumor conference with representation by surgeons, radiation oncologists, medical oncologists, and reconstructive surgeons for a discussion of available treatment options 40
PREOPERATIVE ASSESSMENT Imaging to assess the primary extent of tumor and cervical lymph nodes includes either computed tomography (CT) or magnetic resonance imaging (MRI) CT to demonstrate cortical bone erosion and lymph node metastases, MRI soft tissue invasion by tumor and extension into medullary bone A Panorex suspected mandibular invasion and can assist dental evaluation Denta. Scan imaging using a dental CT-based software program can be helpful in assessing the likelihood of mandibular invasion and has a reported sensitivity of 95% cortical invasion of the mandible best assessed by conventional contrast-enhanced CT, as well as the CT component of positron emission tomography (PET-CT), with a sensitivity of 100% and accuracy of 97% The extent of imaging physician preference and the complexity of the presenting lesion Patients with T 1 lesions, without clinical lymphadenopathy, may not require extensive imaging to aid operative decision making. Perineural invasion is associated with a threefold increase in locoregional recurrence the most commonly affected CNs in order of incidence : the maxillary (V 2), hypoglossal, mandibular (V 3), and facial nerves. 41
Retrospective review could not identify radiographic evidence of perineural invasion in 21% of cases with histologic confirmation of the finding T 1 -weighted MRI Loss of marrow signal, denervation atrophy, and neural enhancement CT CT and loss of fat planes with widening of neural foramina PET, PET-CT, and single photon emission computed tomography scanning Assessment for distant metastases via CT of the chest with contrast Suspicion of distant metastases may require CT-guided biopsy for confirmation distant metastases not candidates for curative treatment may be better served by exploring palliative care options while preserving the maximal quality of life PREOPERATIVE INTERVENTIONS Malnutrition perioperative period wound complications preoperative consultation for gastrostomy tube placement should be considered for those patients in whom the ability to take oral nutrition is compromised before surgery or is anticipated to extend for a prolonged period of time postoperatively For those who require postoperative radiation therapy, mucositis can result in a delay in the normal resumption of oral intake for several weeks to months. dental evaluation is essential for patients with poor dentition and for those who may require radiation as part of their treatment Prosthodontic evaluation is indicated for those who will undergo maxillectomy and will require a surgical obturator. For patients with the potential for significant speech and swallowing impairment postoperatively, consultation and counseling with a speech-language pathologist can aid in long-term rehabilitation. 42
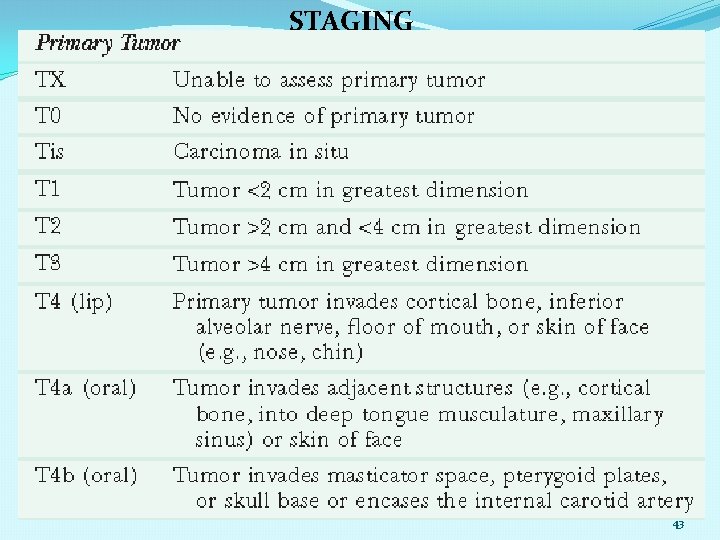
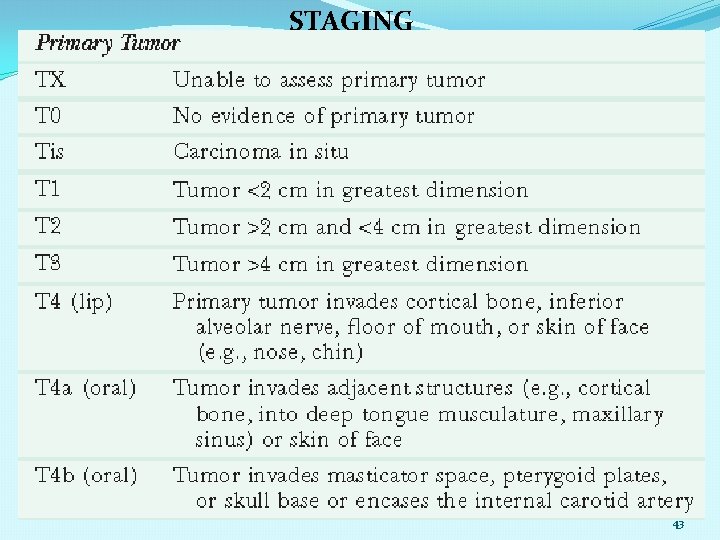
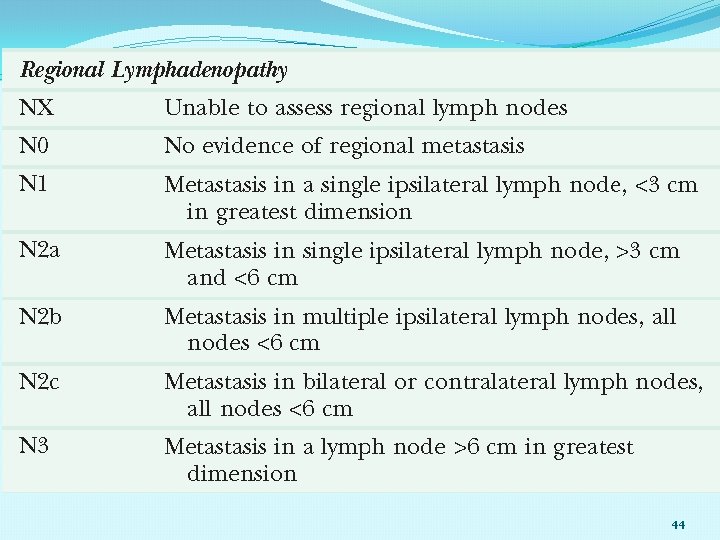
STAGING 43
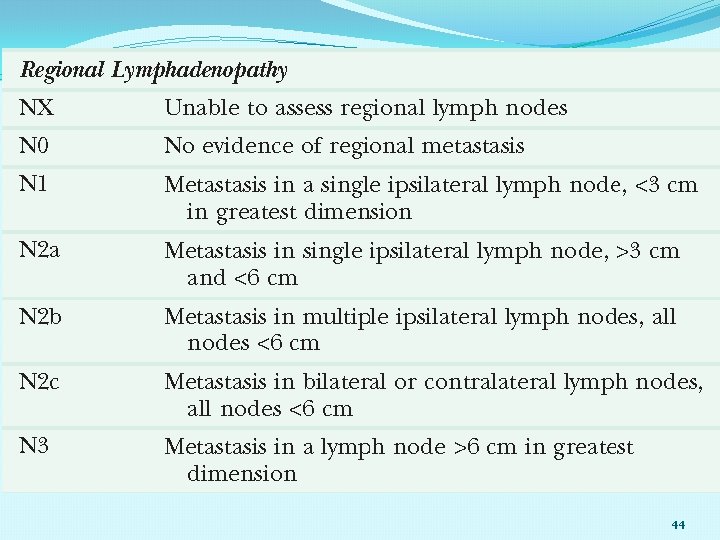
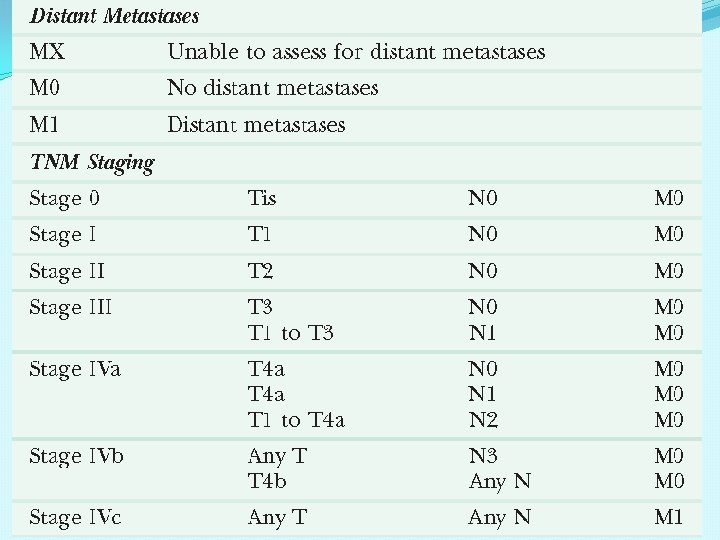
44
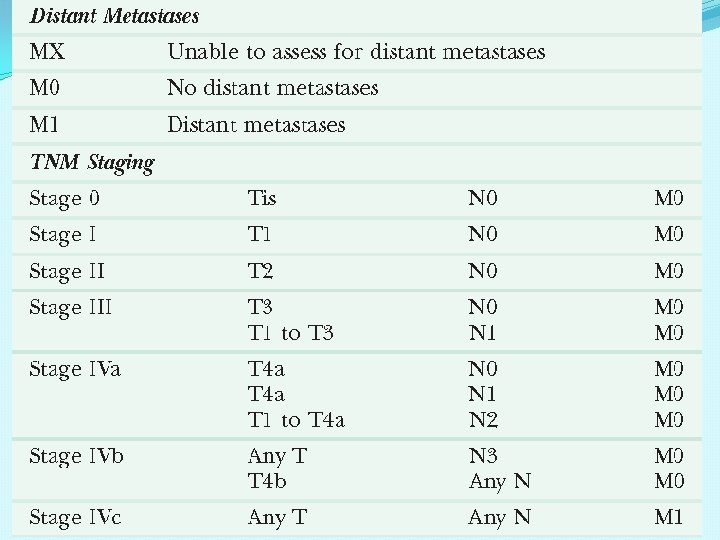
45
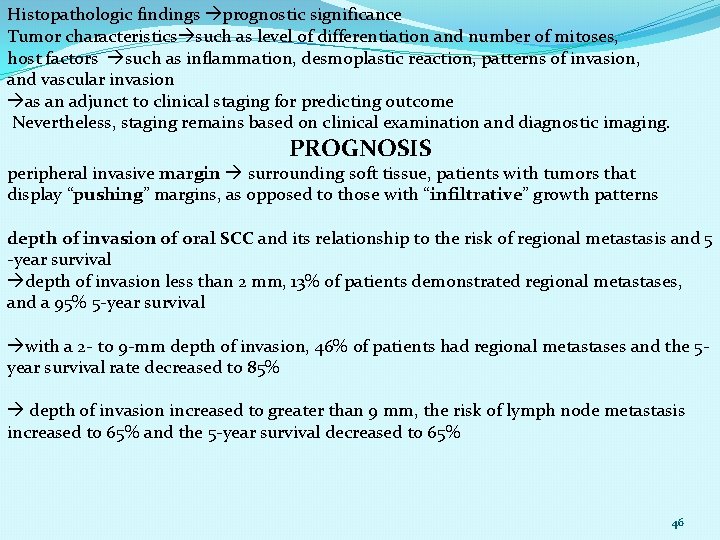
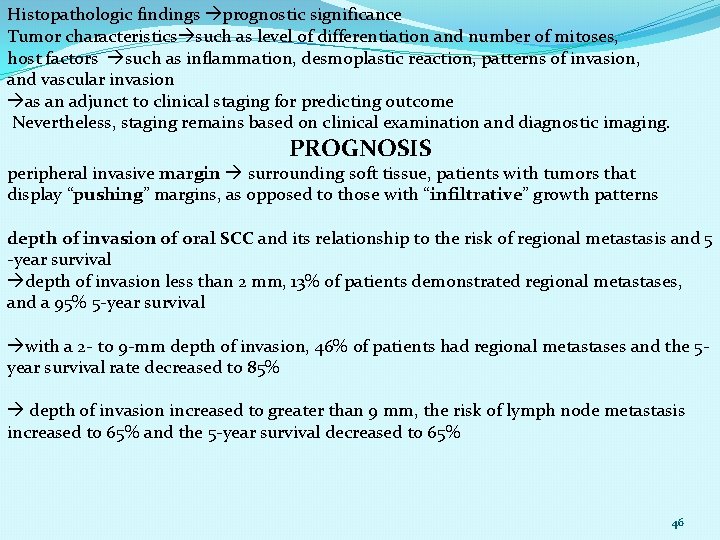
Histopathologic findings prognostic significance Tumor characteristics such as level of differentiation and number of mitoses, host factors such as inflammation, desmoplastic reaction, patterns of invasion, and vascular invasion as an adjunct to clinical staging for predicting outcome Nevertheless, staging remains based on clinical examination and diagnostic imaging. PROGNOSIS peripheral invasive margin surrounding soft tissue, patients with tumors that display “pushing” margins, as opposed to those with “infiltrative” growth patterns depth of invasion of oral SCC and its relationship to the risk of regional metastasis and 5 -year survival depth of invasion less than 2 mm, 13% of patients demonstrated regional metastases, and a 95% 5 -year survival with a 2 - to 9 -mm depth of invasion, 46% of patients had regional metastases and the 5 year survival rate decreased to 85% depth of invasion increased to greater than 9 mm, the risk of lymph node metastasis increased to 65% and the 5 -year survival decreased to 65% 46
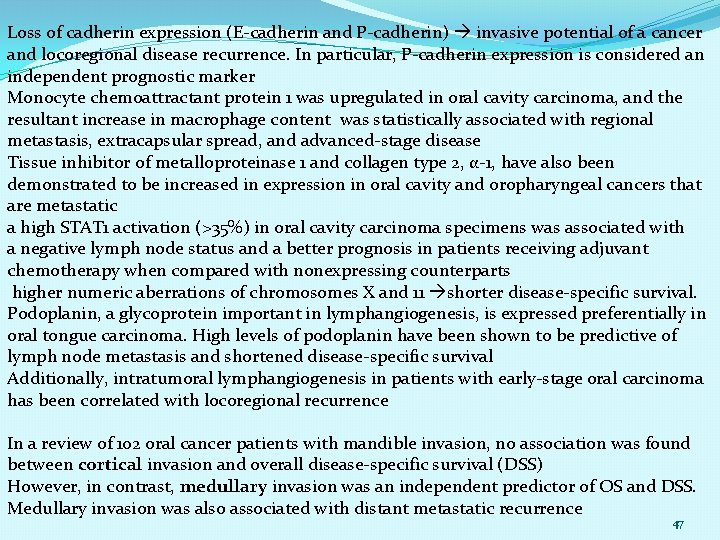
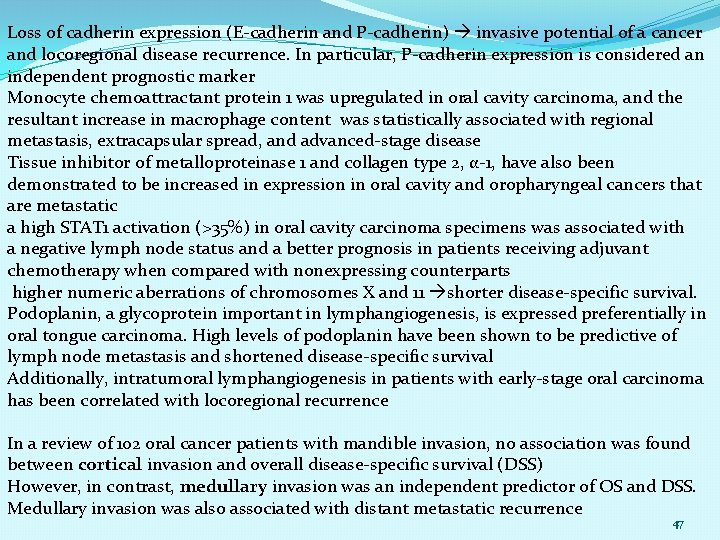
Loss of cadherin expression (E-cadherin and P-cadherin) invasive potential of a cancer and locoregional disease recurrence. In particular, P-cadherin expression is considered an independent prognostic marker Monocyte chemoattractant protein 1 was upregulated in oral cavity carcinoma, and the resultant increase in macrophage content was statistically associated with regional metastasis, extracapsular spread, and advanced-stage disease Tissue inhibitor of metalloproteinase 1 and collagen type 2, α-1, have also been demonstrated to be increased in expression in oral cavity and oropharyngeal cancers that are metastatic a high STAT 1 activation (>35%) in oral cavity carcinoma specimens was associated with a negative lymph node status and a better prognosis in patients receiving adjuvant chemotherapy when compared with nonexpressing counterparts higher numeric aberrations of chromosomes X and 11 shorter disease-specific survival. Podoplanin, a glycoprotein important in lymphangiogenesis, is expressed preferentially in oral tongue carcinoma. High levels of podoplanin have been shown to be predictive of lymph node metastasis and shortened disease-specific survival Additionally, intratumoral lymphangiogenesis in patients with early-stage oral carcinoma has been correlated with locoregional recurrence In a review of 102 oral cancer patients with mandible invasion, no association was found between cortical invasion and overall disease-specific survival (DSS) However, in contrast, medullary invasion was an independent predictor of OS and DSS. Medullary invasion was also associated with distant metastatic recurrence 47
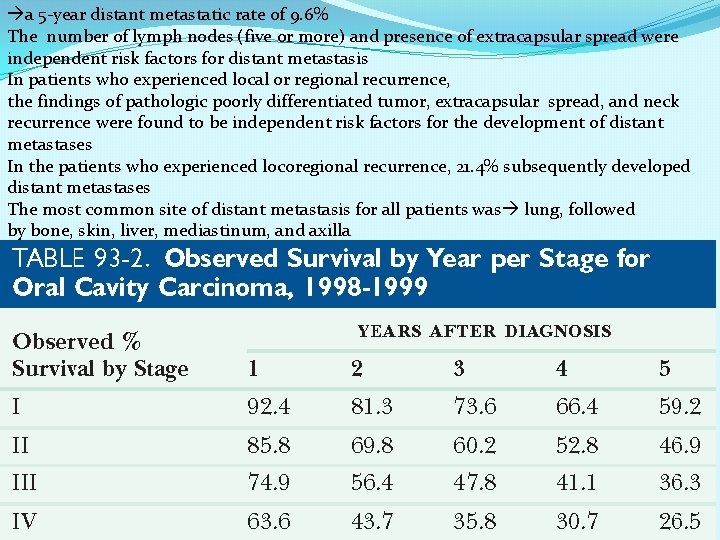
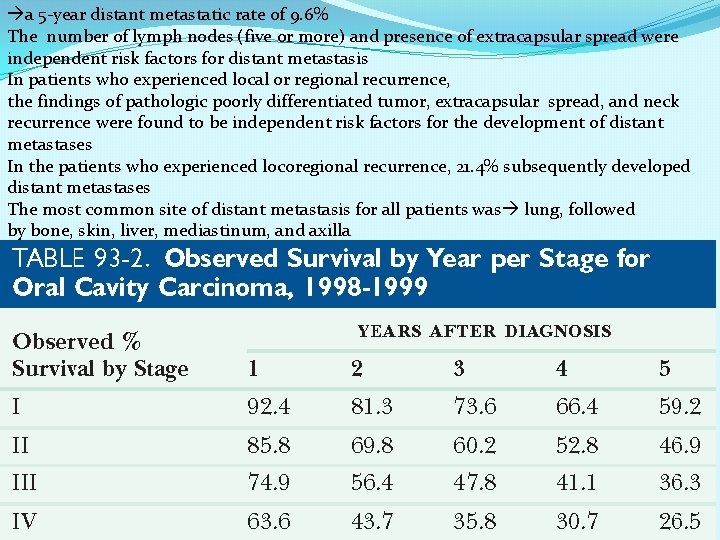
a 5 -year distant metastatic rate of 9. 6% The number of lymph nodes (five or more) and presence of extracapsular spread were independent risk factors for distant metastasis In patients who experienced local or regional recurrence, the findings of pathologic poorly differentiated tumor, extracapsular spread, and neck recurrence were found to be independent risk factors for the development of distant metastases In the patients who experienced locoregional recurrence, 21. 4% subsequently developed distant metastases The most common site of distant metastasis for all patients was lung, followed by bone, skin, liver, mediastinum, and axilla 48
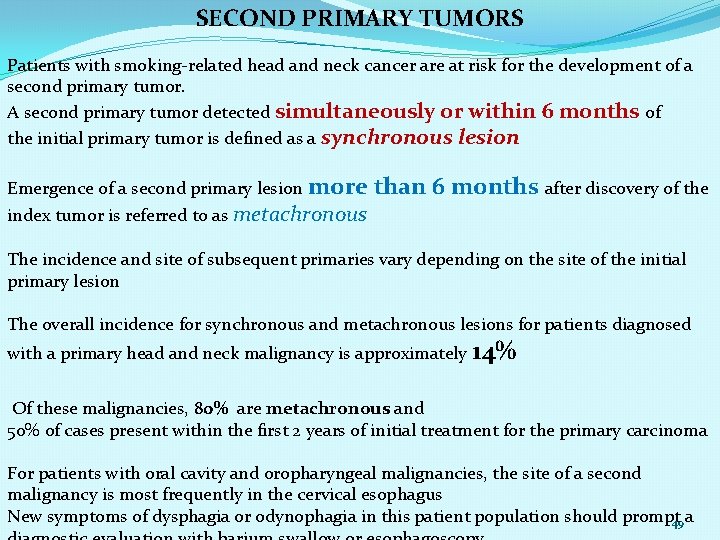
SECOND PRIMARY TUMORS Patients with smoking-related head and neck cancer are at risk for the development of a second primary tumor. A second primary tumor detected simultaneously or within 6 months of the initial primary tumor is defined as a synchronous lesion Emergence of a second primary lesion more index tumor is referred to as metachronous than 6 months after discovery of the The incidence and site of subsequent primaries vary depending on the site of the initial primary lesion The overall incidence for synchronous and metachronous lesions for patients diagnosed with a primary head and neck malignancy is approximately 14% Of these malignancies, 80% are metachronous and 50% of cases present within the first 2 years of initial treatment for the primary carcinoma For patients with oral cavity and oropharyngeal malignancies, the site of a second malignancy is most frequently in the cervical esophagus New symptoms of dysphagia or odynophagia in this patient population should prompt 49 a
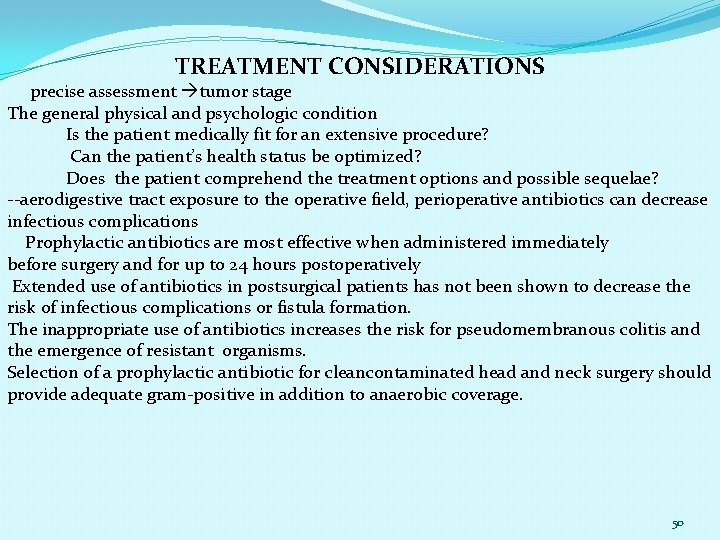
TREATMENT CONSIDERATIONS precise assessment tumor stage The general physical and psychologic condition Is the patient medically fit for an extensive procedure? Can the patient’s health status be optimized? Does the patient comprehend the treatment options and possible sequelae? --aerodigestive tract exposure to the operative field, perioperative antibiotics can decrease infectious complications Prophylactic antibiotics are most effective when administered immediately before surgery and for up to 24 hours postoperatively Extended use of antibiotics in postsurgical patients has not been shown to decrease the risk of infectious complications or fistula formation. The inappropriate use of antibiotics increases the risk for pseudomembranous colitis and the emergence of resistant organisms. Selection of a prophylactic antibiotic for cleancontaminated head and neck surgery should provide adequate gram-positive in addition to anaerobic coverage. 50
For early-stage lesions of the oral cavity (T 1/T 2), transoral resection tends to be possible with complete tumor removal and adequate margin control. Primary closure, healing by secondary intention, or placement of a split-thickness skin graft may be used for reconstruction of small defects. Larger and more posteriorly located lesions may require a pullthrough or mandibulotomybased technique to aid exposure for resection and reconstruction. When the tumor closely approximates the mandible, a marginal versus segmental mandibulectomy needs to be considered. High levels of local control have been reported for transorally resected early and advanced T-stage oral cavity carcinoma, using the principles of transoral laser microsurgery. This technique incorporates transtumoral laser incisions to assess deep margins 95 patients with oral cavity carcinoma (75% T 1/T 2, 25% T 3/T 4) treated with transoral laser microsurgery, a margin negativity of 95% and 3 -year local control of 80% Reconstructive options for advanced T-stage lesions include microvascular free tissue or pedicled flap reconstruction. Traditionally, T 4 b lesions have been considered inoperable. equivalent results with T 4 a and selected T 4 b lesions, without carotid encasement and skull base extension, when aggressive surgical management of the primary site and regional lymphatics with postoperative radiation or chemoradiation therapy was performed. Free tissue reconstruction was necessary in 95% of patients. Local control and disease free and OS numbers were similar. 51
When considering options for repairing larger soft tissue defects, the surgeon must consider the impact on speech and swallowing and on the airway. Patients may require temporary tracheostomy and feeding tube placement in the perioperative period, until adequate healing has occurred. The cosmetic implications of composite resection in advanced lesions also need to be weighed with the individual patient’s expectations; however, the goal of treatment should remain an oncologic approach to achieve the best opportunity for long-term survival while maintaining quality of life. quality-of-life scores have been demonstrated to be lower with patients diagnosed with advanced-stage tumor, those who experienced gastrostomy tube dependence, and patients who had a surgical complication and/or posttreatment recurrence SURGICAL TREATMENT OF THE PRIMARY LESION Primary surgical management of oral cavity carcinomas is the standard of care in most circumstances and can be associated with excellent oncologic control of early-stage tumors with acceptable functional results. Advanced-stage oral cavity malignancies require combined modality therapy, and patients typically undergo surgical resection up front followed by adjuvant radiation with or without chemotherapy Size and location of the tumor and the anatomic region involved relative to the tumor’s presentation. Resection of limited primary lesions (T 1 and small T 2 s) can typically be performed transorally. In advanced-stage oral tongue lesions, in particular those with posterior extension, a lingual release may rarely require a mandibulotomy-based approach to provide adequate access for the resection of the posterior margin of the tumor and to allow for reconstruction. One issue to consider when performing a mandibulotomy is that most patients with advanced tumors will require postoperative radiation, and irradiation to the mandibulotomy site may predispose the patient to radiation necrosis 52 or
1. LIP The majority on the lower lip (88% to 95%) SCC upper lip (2% to 7%) BCC commissure (1%) : keratoacanthoma, minor salivary gland tumors, malignant melanoma, and tumors of mesenchymal origin such as malignant fibrous histiocytoma, leiomyosarcoma, fibrosarcoma, angiosarcoma, and rhabdomyosarcoma. The typical patient with SCC of the lip is a man 50 to 70 years of age. Risk factors include prolonged exposure to sunlight, fair complexion, immunosuppression, and tobacco use. Clinical findings in lip cancer usually include an ulcerated lesion on the vermilion or cutaneous surface or, less commonly, on the mucosal surface. The majority of patients come to medical attention with early-stage lesions and without evidence of neck metastases. A nodular or sclerotic lesion may infiltrate the deeper tissues, and careful palpation is important for determining the actual size of the lesion. Minor salivary gland tumors present as a submucosal nodule on the inner surface of the lower lip. The presence of paresthesias or dysesthesias in the area adjacent to the lesion indicates possible mental nerve involvement. Neck metastases are an infrequent finding with lower-lip SCCs and occur in only 10% of cases. Lower-lip lesions may metastasize bilaterally because of the communicating pattern of the lymphatics. An increased risk of regional metastasis is associated with commissure and upper-lip lesions. Adverse prognostic features of lip primaries include perineural invasion, bony involvement, cancer that arises on the upper lip or the commissure, regional lymphatic metastasis, and age younger than 40 years at onset. 80 Obtaining an adequate cosmetic result and functional outcome without microstomia can be challenging 53
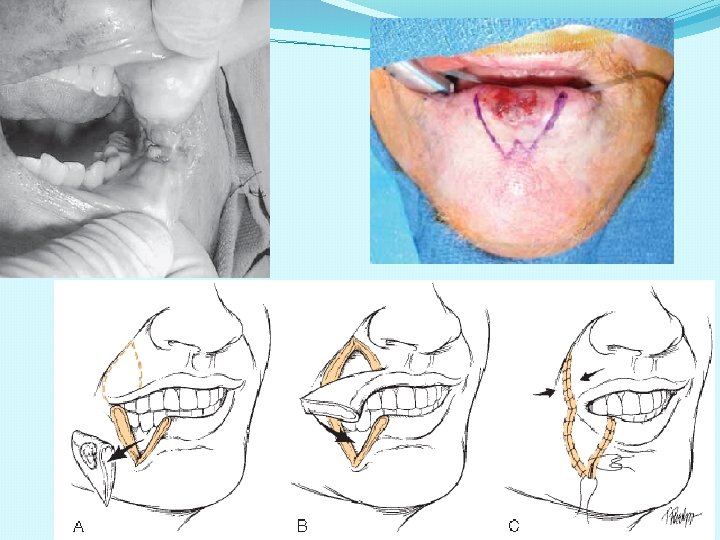
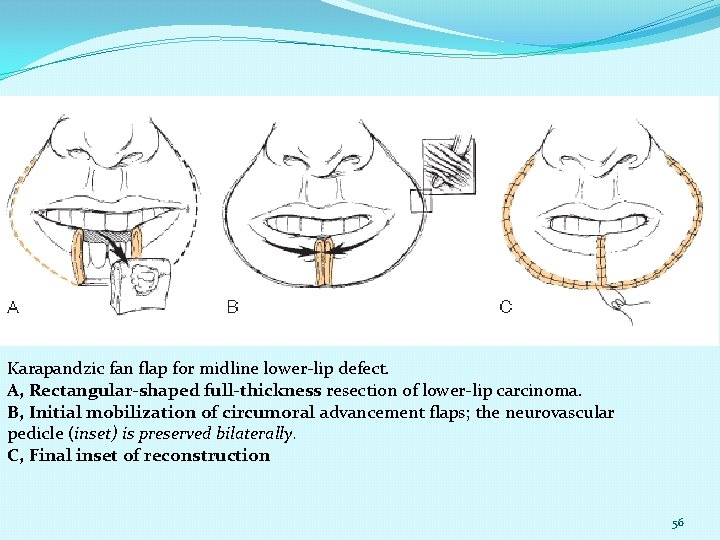
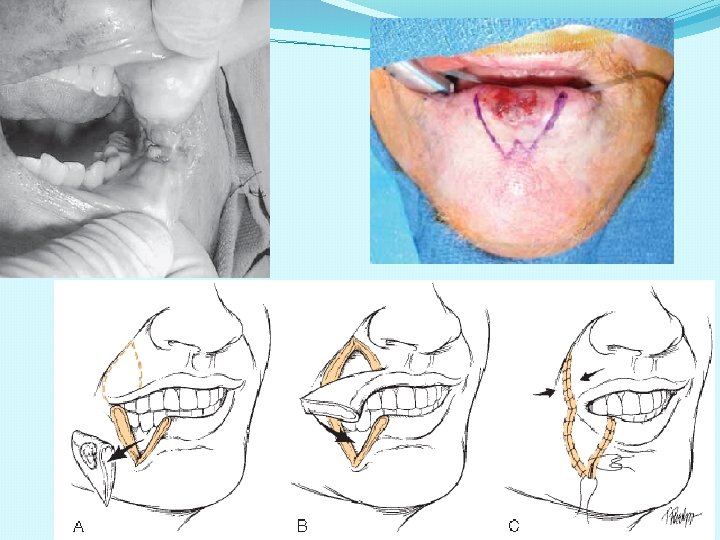
The typical lip length is 6 to 8 cm, and reconstructive algorithms are based on the proportion of the lip resected. Realignment of the vermilion border during the reconstruction and preservation of the oral commissure when possible are important principles in attempting to attain an acceptable cosmetic and functional result. Small primary lesions may be treated with surgery or radiation with equal success and acceptable cosmetic results. However, surgical excision with histologic confirmation of tumor-free margins is the preferred modality. The reconstruction of lip defects after tumor excision requires innovative techniques to provide oral competence, maintenance of dynamic function, and acceptable cosmesis. With small lesions—that is, defects of up to one third of the lip’s length—simple excision with primary closure is possible. When lesions require resection of up to one third to two thirds of a lip’s length, reconstructive options include a lip switch (Abbe-Estlander procedure). . For tumors that require resection of more than two thirds of the lip, the reconstructive options are the Gilles fan flap, bilateral advancement flaps, Karapandzic flap, or free radial forearm flap with the palmaris longus tendon. The Karapandzic flap is a sensate neuromuscular flap that includes the remaining orbicularis oris muscle. The blood supply for this flap is provided by the corresponding branches of the labial artery. Microstomia is a potential complication with these methods of lip reconstruction. 81 For large defects, Websteror Bernard procedures using lateral nasolabial flaps with buccal advancement have been described. In addition, for aggressive and advanced-stage lesions, an evaluation for perineural spread should be performed at the time of resection. With extensive perineural invasion, a drillout of the mental nerve or a hemimandibulectomy may be required 54
55
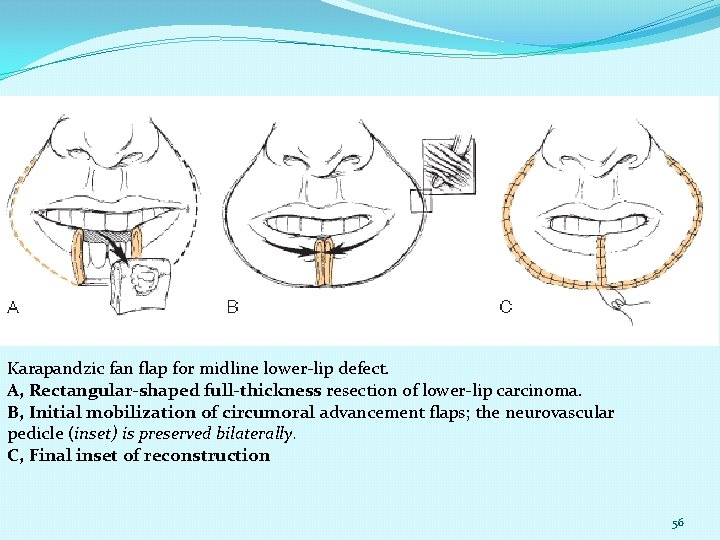
Karapandzic fan flap for midline lower-lip defect. A, Rectangular-shaped full-thickness resection of lower-lip carcinoma. B, Initial mobilization of circumoral advancement flaps; the neurovascular pedicle (inset) is preserved bilaterally. C, Final inset of reconstruction 56
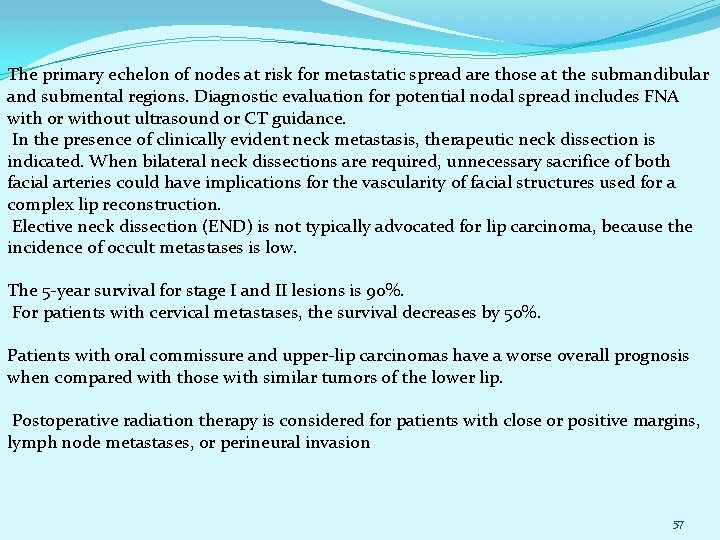
The primary echelon of nodes at risk for metastatic spread are those at the submandibular and submental regions. Diagnostic evaluation for potential nodal spread includes FNA with or without ultrasound or CT guidance. In the presence of clinically evident neck metastasis, therapeutic neck dissection is indicated. When bilateral neck dissections are required, unnecessary sacrifice of both facial arteries could have implications for the vascularity of facial structures used for a complex lip reconstruction. Elective neck dissection (END) is not typically advocated for lip carcinoma, because the incidence of occult metastases is low. The 5 -year survival for stage I and II lesions is 90%. For patients with cervical metastases, the survival decreases by 50%. Patients with oral commissure and upper-lip carcinomas have a worse overall prognosis when compared with those with similar tumors of the lower lip. Postoperative radiation therapy is considered for patients with close or positive margins, lymph node metastases, or perineural invasion 57
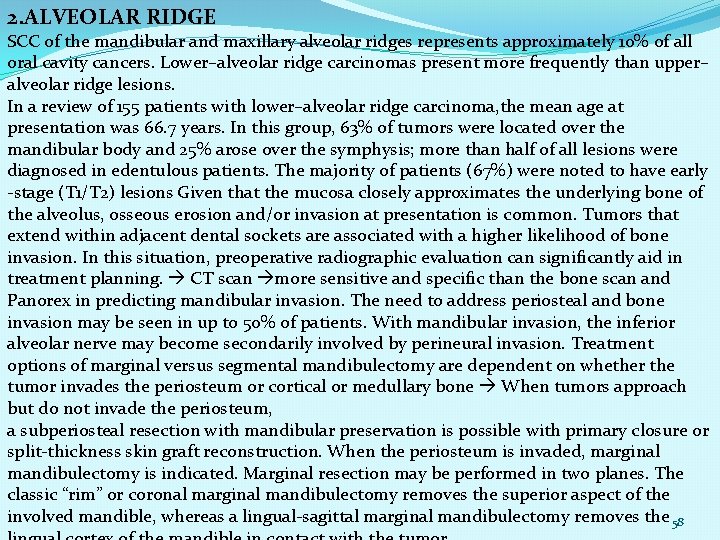
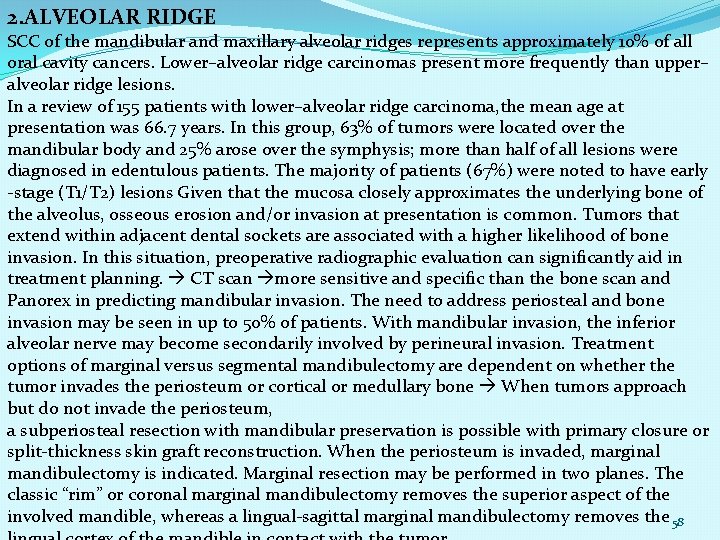
2. ALVEOLAR RIDGE SCC of the mandibular and maxillary alveolar ridges represents approximately 10% of all oral cavity cancers. Lower–alveolar ridge carcinomas present more frequently than upper– alveolar ridge lesions. In a review of 155 patients with lower–alveolar ridge carcinoma, the mean age at presentation was 66. 7 years. In this group, 63% of tumors were located over the mandibular body and 25% arose over the symphysis; more than half of all lesions were diagnosed in edentulous patients. The majority of patients (67%) were noted to have early -stage (T 1/T 2) lesions Given that the mucosa closely approximates the underlying bone of the alveolus, osseous erosion and/or invasion at presentation is common. Tumors that extend within adjacent dental sockets are associated with a higher likelihood of bone invasion. In this situation, preoperative radiographic evaluation can significantly aid in treatment planning. CT scan more sensitive and specific than the bone scan and Panorex in predicting mandibular invasion. The need to address periosteal and bone invasion may be seen in up to 50% of patients. With mandibular invasion, the inferior alveolar nerve may become secondarily involved by perineural invasion. Treatment options of marginal versus segmental mandibulectomy are dependent on whether the tumor invades the periosteum or cortical or medullary bone When tumors approach but do not invade the periosteum, a subperiosteal resection with mandibular preservation is possible with primary closure or split-thickness skin graft reconstruction. When the periosteum is invaded, marginal mandibulectomy is indicated. Marginal resection may be performed in two planes. The classic “rim” or coronal marginal mandibulectomy removes the superior aspect of the involved mandible, whereas a lingual-sagittal marginal mandibulectomy removes the 58
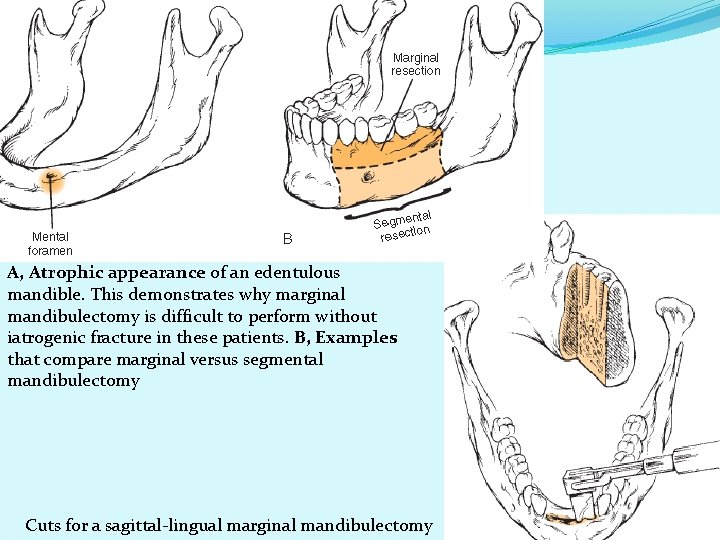
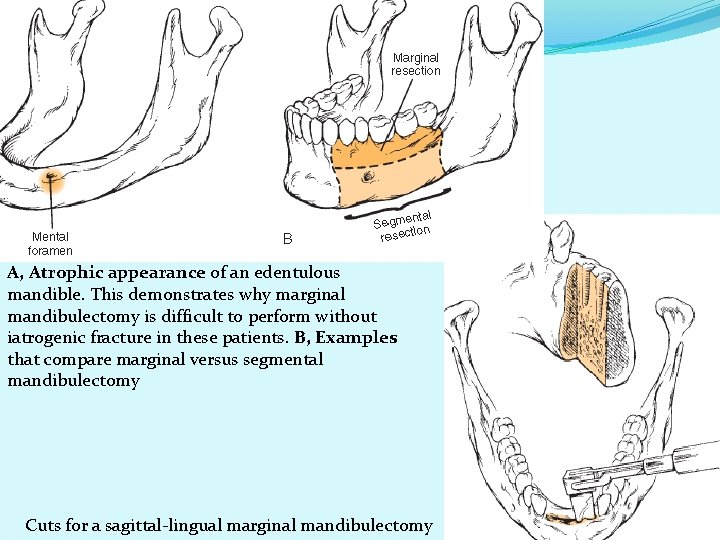
A, Atrophic appearance of an edentulous mandible. This demonstrates why marginal mandibulectomy is difficult to perform without iatrogenic fracture in these patients. B, Examples that compare marginal versus segmental mandibulectomy Cuts for a sagittal-lingual marginal mandibulectomy 59
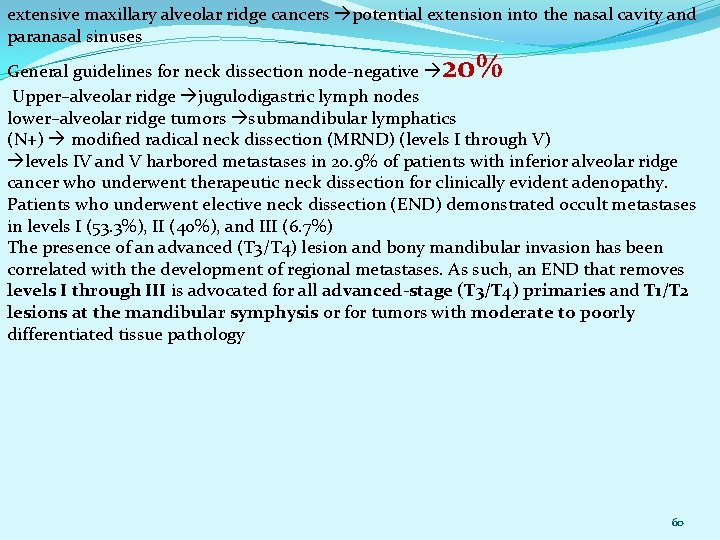
extensive maxillary alveolar ridge cancers potential extension into the nasal cavity and paranasal sinuses 20% General guidelines for neck dissection node-negative Upper–alveolar ridge jugulodigastric lymph nodes lower–alveolar ridge tumors submandibular lymphatics (N+) modified radical neck dissection (MRND) (levels I through V) levels IV and V harbored metastases in 20. 9% of patients with inferior alveolar ridge cancer who underwent therapeutic neck dissection for clinically evident adenopathy. Patients who underwent elective neck dissection (END) demonstrated occult metastases in levels I (53. 3%), II (40%), and III (6. 7%) The presence of an advanced (T 3/T 4) lesion and bony mandibular invasion has been correlated with the development of regional metastases. As such, an END that removes levels I through III is advocated for all advanced-stage (T 3/T 4) primaries and T 1/T 2 lesions at the mandibular symphysis or for tumors with moderate to poorly differentiated tissue pathology 60
The overall risk of metastases with alveolar ridge carcinoma 25% clinically N 0 neck, occult metastases 15% of operative The 2 - and 5 -year survival for patients with occult metastases who underwent END is better than for patients who underwent therapeutic neck dissection after the eventual development of metastatic adenopathy The 5 -year survival ranges from 85% (T 1/T 2) to 65% (T 3/T 4) for patients who do not have metastatic spread Decreased local control rates are seen with lesions greater than 3 cm and with positive surgical margins Significant prognostic factors include advanced T stage (T 3/T 4) margin status mandibular invasion the presence of regional metastases Neither local control nor survival are affected by: the extent of mandibular resection, dental intervention near the site of the primary, perineural invasion, or histologic grade of the tumor Postoperative radiation therapy is advocated for patients with T 4 tumors, positive margins, perineural invasion, and regional metastasis 61
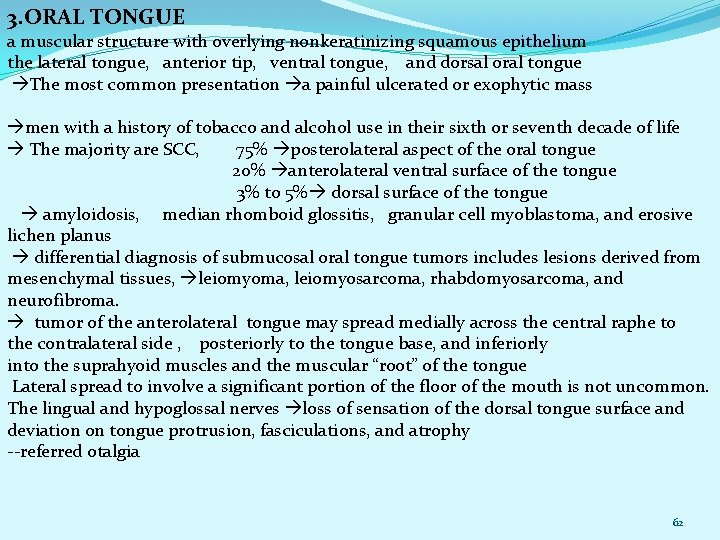
3. ORAL TONGUE a muscular structure with overlying nonkeratinizing squamous epithelium the lateral tongue, anterior tip, ventral tongue, and dorsal oral tongue The most common presentation a painful ulcerated or exophytic mass men with a history of tobacco and alcohol use in their sixth or seventh decade of life The majority are SCC, 75% posterolateral aspect of the oral tongue 20% anterolateral ventral surface of the tongue 3% to 5% dorsal surface of the tongue amyloidosis, median rhomboid glossitis, granular cell myoblastoma, and erosive lichen planus differential diagnosis of submucosal oral tongue tumors includes lesions derived from mesenchymal tissues, leiomyoma, leiomyosarcoma, rhabdomyosarcoma, and neurofibroma. tumor of the anterolateral tongue may spread medially across the central raphe to the contralateral side , posteriorly to the tongue base, and inferiorly into the suprahyoid muscles and the muscular “root” of the tongue Lateral spread to involve a significant portion of the floor of the mouth is not uncommon. The lingual and hypoglossal nerves loss of sensation of the dorsal tongue surface and deviation on tongue protrusion, fasciculations, and atrophy --referred otalgia 62
. The extreme of lateral tumor extension beyond the floor of the mouth includes direct invasion of the mandible, which requires composite resection At the time of diagnosis, the majority of oral tongue carcinomas (75%) are staged T 2 or smaller (T 1/T 2) primary tumors transoral wide local excision frozen-section confirmation of the margin status is frequently used before pursuing reconstruction Advanced mandible or invade the deep musculature are best accessed via a pullthrough or mandibulotomy technique When a segmental resection is warranted, entry into the oral cavity through the mandibulotomy cuts provides wide access to the primary tumor deep margins. A partial glossectomy, which may remove a significant portion of the lateral oral tongue, can still permit reasonably effective postoperative function larger tumors that invade deeply within the tongue can result in a significant functional impairment With resection of approximately one quarter to one third of the oral tongue, healing by secondary intention is an acceptable option If a limited portion of the floor of mouth is resected, reconstruction with a split thickness skin or dermal graft should be considered to prevent tongue tethering Resection of approximately one half of the tongue results in loss of tongue bulk and scar contracture, if primary closure or healing by secondary intention is pursued 63
Lingual contact with the palate, lip, and teeth is decreased and can result in impaired articulation; posterior propulsion of foods and liquids may also be affected The use of soft, pliable fasciocutaneous free flaps, such as a radial forearm or anterolateral thigh free flap, can provide intraoral bulk and preservation of existing tongue mobility A palatal augmentation prosthesis allows for contact between the remaining tongue tissue and the palate and may improve speech and swallowing function For patients who undergo a partial glossectomy with a significant resection of the floor of the mouth, free flap reconstruction to maintain tongue mobility is indicated. Negative factors positive surgical margin and depth of invasion greater than 2 mm occult regional metastases (28%) had a fivefold increased risk of dying of disease compared with pathologic N 0 patients (5 -year DSS, 48. 5% vs. 85. 5%) Of the patients with occult metastases, 100% had a depth of invasion of 2 mm or more, and 92% had tumors with a depth of invasion of 4 mm or more Also of note, 93% of patients with occult metastases had either moderately or poorly differentiated tumors Occult metastases were not identified in any patients with superficial (<2 mm) welldifferentiated tumors Patients who received postoperative radiation therapy for a node-positive neck (based on neck dissection findings) did not have improvement of their DSS to levels comparable with N 0 patients, although radiation did decrease the rate of subsequent neck recurrence The rate of extracapsular spread for node-positive patients was 42%. 64
positive surgical margins after resection main tumor–involved margin or tumor satellite–involved margin. Tumor satellites, separate islands of tumor with intervening nontumor normal tissue, did not increase the risk of local recurrence greater than that seen with main tumor–involved margins However, the risk of regional nodal recurrence of tumor was significantly greater in patients with tumor satellite–involved margins At initial presentation, 40% evidence of cervical metastases T 1 and T 2 tumors with clinical N 0 , 20% to 30% of END pathologically 15. 8% of lateral tongue carcinoma “skip” metastases to lymph nodes, bypassing levels I and II and presenting with level III or IV metastatic disease elective supraomohyoid neck dissection (SOHND) inadequate for the control of regional lymphatics of oral tongue carcinoma patients levels I through IV in this situation When lesions approach the midline, the likelihood for bilateral regional metastasis is high; thus it requires bilateral lymphadenectomy In young patients with head and neck cancer, the oral tongue is the most common primary site, and approximately 1 in 1000 cases of head and neck SCC present in a patient 20 years of age or younger In a small series that reviewed the outcomes of pediatric-age patients diagnosed with oral tongue cancer, younger patients were found to have 5 -year OS rates similar to those of stage-matched adults. Additionally, the 5 -year DSS and recurrence-free survival were equivalent in the two groups 65 The 5 -year survival for stage I or II tumors is 75%, and it is less than 40% for stage III or IV
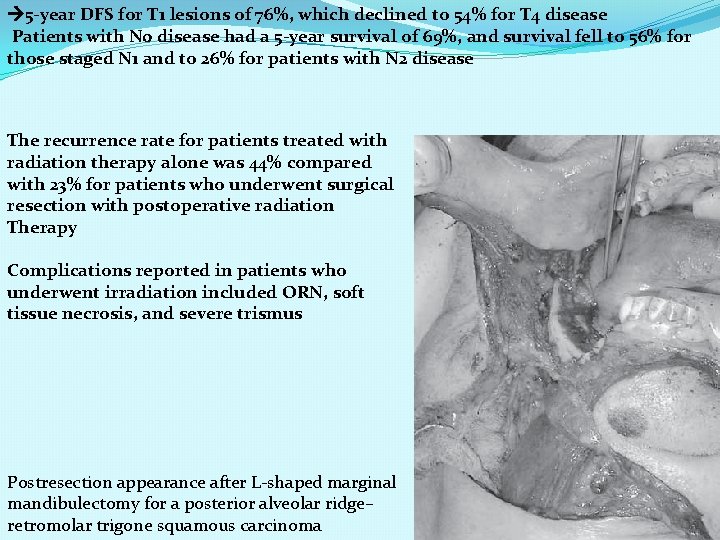
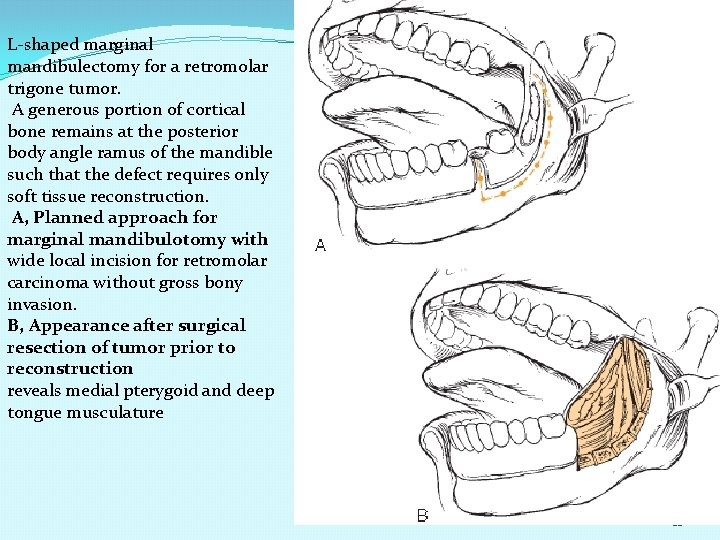
4. RETROMOLAR TRIGONE The majority advanced disease At the time of presentation, up to 50% of patients have regional metastatic disease. Mandible involvement is common given the thin layer of soft tissue that separates these tumors from the ascending ramus. Trismus suggests involvement of the medial pterygoid muscle. As tumors progress in this location, extension to the faucial arch, tonsillar fossa, and base of the tongue is common In addition to SCC minor salivary gland neoplasms, osteosarcoma, and soft tissue sarcomas. Given the proximity of the mucosa to the underlying ramus of the mandible, surgical resection of early-stage retromolar trigone lesions may require a resection of a portion of the mandible an L-shaped coronal marginal mandibulectomy, segmental mandibulectomy, and hemimandibulectomy. With the L-shaped marginal mandibulectomy, the superior aspect of the body— extending toward the angle and ascending the ramus—is resected Segmental mandibulectomy is performed for more extensive lesions with gross bone destruction. 66
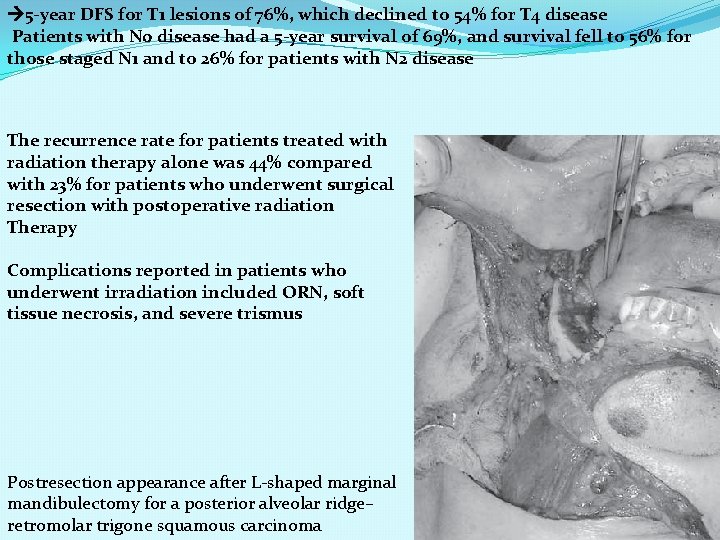
5 -year DFS for T 1 lesions of 76%, which declined to 54% for T 4 disease Patients with N 0 disease had a 5 -year survival of 69%, and survival fell to 56% for those staged N 1 and to 26% for patients with N 2 disease The recurrence rate for patients treated with radiation therapy alone was 44% compared with 23% for patients who underwent surgical resection with postoperative radiation Therapy Complications reported in patients who underwent irradiation included ORN, soft tissue necrosis, and severe trismus Postresection appearance after L-shaped marginal mandibulectomy for a posterior alveolar ridge– retromolar trigone squamous carcinoma 67
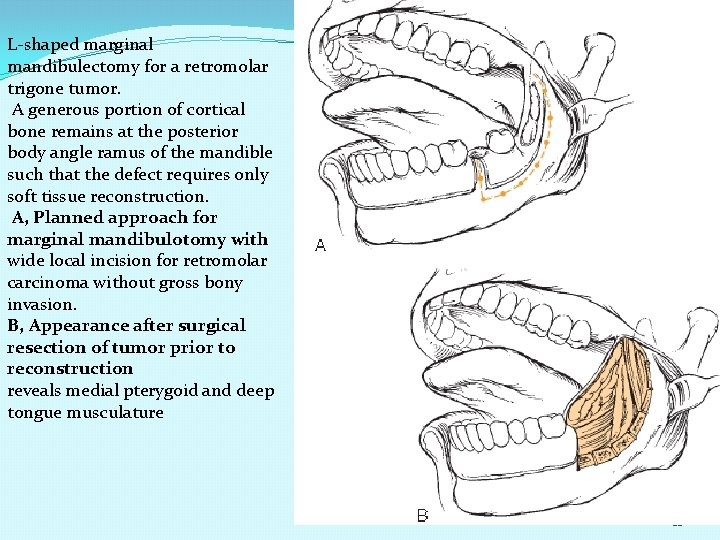
L-shaped marginal mandibulectomy for a retromolar trigone tumor. A generous portion of cortical bone remains at the posterior body angle ramus of the mandible such that the defect requires only soft tissue reconstruction. A, Planned approach for marginal mandibulotomy with wide local incision for retromolar carcinoma without gross bony invasion. B, Appearance after surgical resection of tumor prior to reconstruction reveals medial pterygoid and deep tongue musculature 68
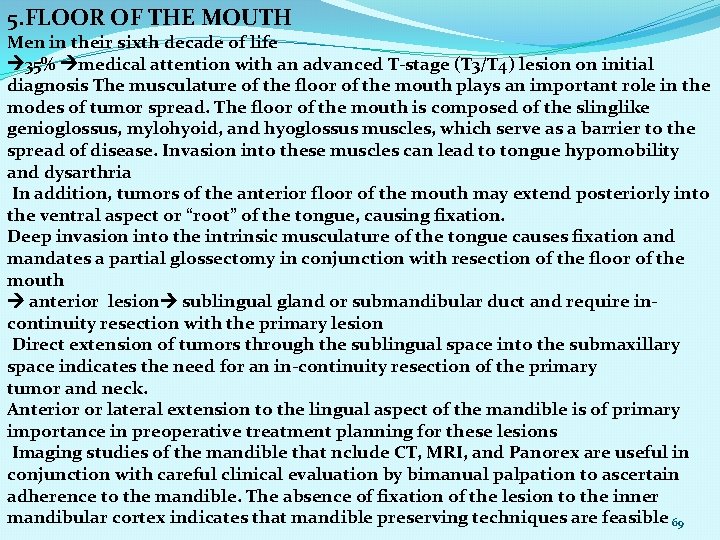
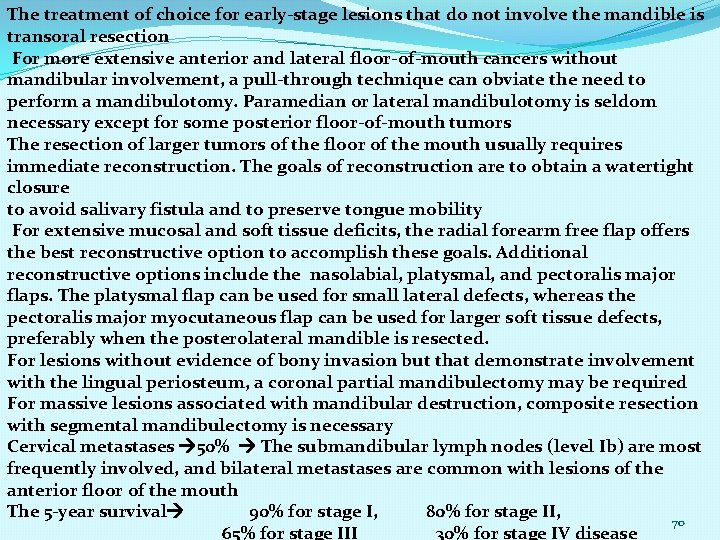
5. FLOOR OF THE MOUTH Men in their sixth decade of life 35% medical attention with an advanced T-stage (T 3/T 4) lesion on initial diagnosis The musculature of the floor of the mouth plays an important role in the modes of tumor spread. The floor of the mouth is composed of the slinglike genioglossus, mylohyoid, and hyoglossus muscles, which serve as a barrier to the spread of disease. Invasion into these muscles can lead to tongue hypomobility and dysarthria In addition, tumors of the anterior floor of the mouth may extend posteriorly into the ventral aspect or “root” of the tongue, causing fixation. Deep invasion into the intrinsic musculature of the tongue causes fixation and mandates a partial glossectomy in conjunction with resection of the floor of the mouth anterior lesion sublingual gland or submandibular duct and require incontinuity resection with the primary lesion Direct extension of tumors through the sublingual space into the submaxillary space indicates the need for an in-continuity resection of the primary tumor and neck. Anterior or lateral extension to the lingual aspect of the mandible is of primary importance in preoperative treatment planning for these lesions Imaging studies of the mandible that nclude CT, MRI, and Panorex are useful in conjunction with careful clinical evaluation by bimanual palpation to ascertain adherence to the mandible. The absence of fixation of the lesion to the inner mandibular cortex indicates that mandible preserving techniques are feasible 69
The treatment of choice for early-stage lesions that do not involve the mandible is transoral resection For more extensive anterior and lateral floor-of-mouth cancers without mandibular involvement, a pull-through technique can obviate the need to perform a mandibulotomy. Paramedian or lateral mandibulotomy is seldom necessary except for some posterior floor-of-mouth tumors The resection of larger tumors of the floor of the mouth usually requires immediate reconstruction. The goals of reconstruction are to obtain a watertight closure to avoid salivary fistula and to preserve tongue mobility For extensive mucosal and soft tissue deficits, the radial forearm free flap offers the best reconstructive option to accomplish these goals. Additional reconstructive options include the nasolabial, platysmal, and pectoralis major flaps. The platysmal flap can be used for small lateral defects, whereas the pectoralis major myocutaneous flap can be used for larger soft tissue defects, preferably when the posterolateral mandible is resected. For lesions without evidence of bony invasion but that demonstrate involvement with the lingual periosteum, a coronal partial mandibulectomy may be required For massive lesions associated with mandibular destruction, composite resection with segmental mandibulectomy is necessary Cervical metastases 50% The submandibular lymph nodes (level Ib) are most frequently involved, and bilateral metastases are common with lesions of the anterior floor of the mouth The 5 -year survival 90% for stage I, 80% for stage II, 70 65% for stage III 30% for stage IV disease
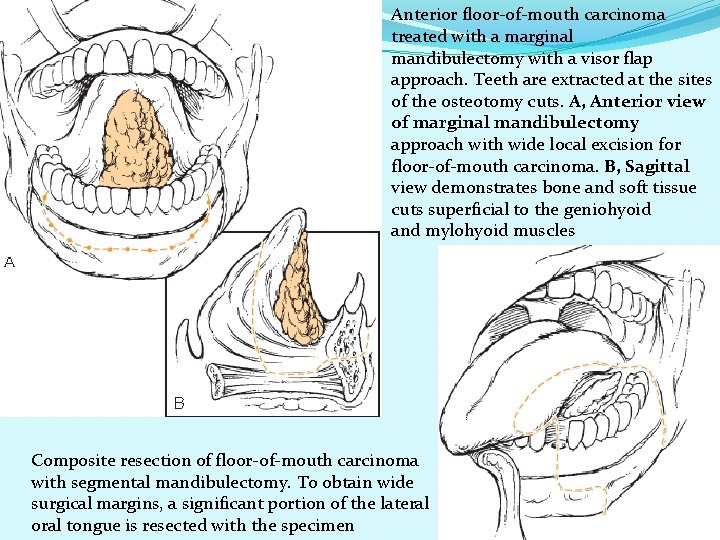
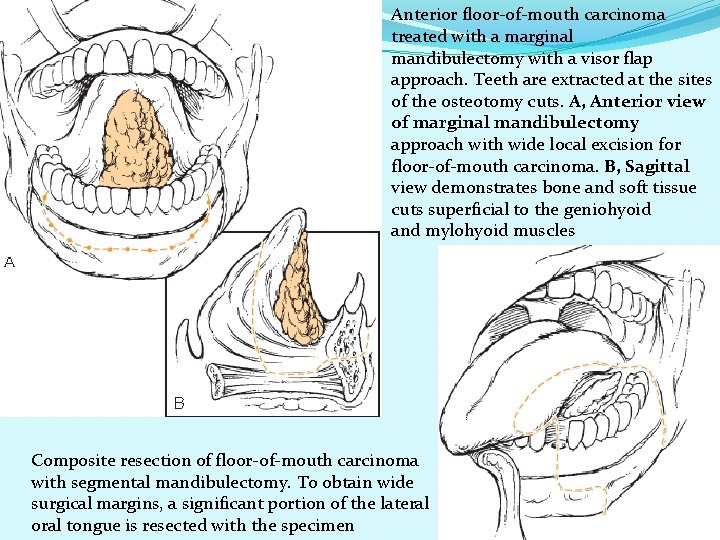
Anterior floor-of-mouth carcinoma treated with a marginal mandibulectomy with a visor flap approach. Teeth are extracted at the sites of the osteotomy cuts. A, Anterior view of marginal mandibulectomy approach with wide local excision for floor-of-mouth carcinoma. B, Sagittal view demonstrates bone and soft tissue cuts superficial to the geniohyoid and mylohyoid muscles Composite resection of floor-of-mouth carcinoma with segmental mandibulectomy. To obtain wide surgical margins, a significant portion of the lateral oral tongue is resected with the specimen 71
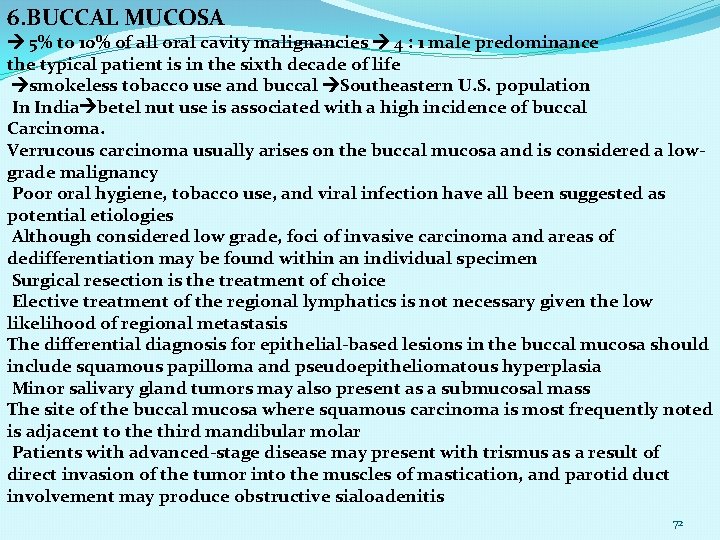
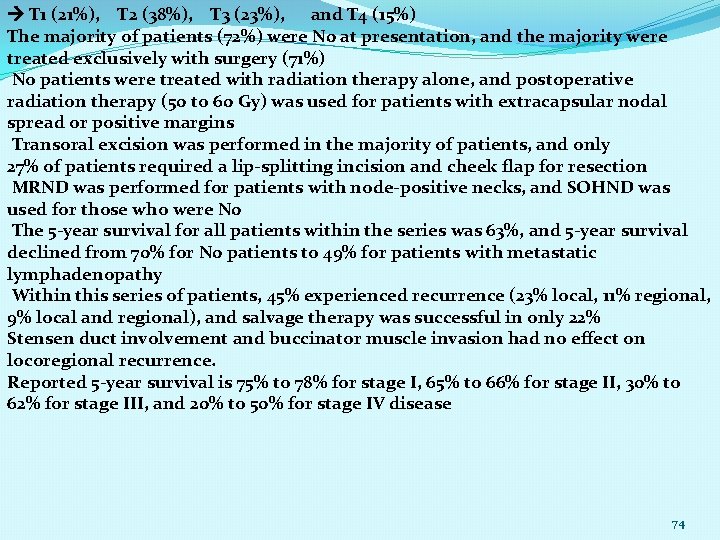
6. BUCCAL MUCOSA 5% to 10% of all oral cavity malignancies 4 : 1 male predominance the typical patient is in the sixth decade of life smokeless tobacco use and buccal Southeastern U. S. population In India betel nut use is associated with a high incidence of buccal Carcinoma. Verrucous carcinoma usually arises on the buccal mucosa and is considered a lowgrade malignancy Poor oral hygiene, tobacco use, and viral infection have all been suggested as potential etiologies Although considered low grade, foci of invasive carcinoma and areas of dedifferentiation may be found within an individual specimen Surgical resection is the treatment of choice Elective treatment of the regional lymphatics is not necessary given the low likelihood of regional metastasis The differential diagnosis for epithelial-based lesions in the buccal mucosa should include squamous papilloma and pseudoepitheliomatous hyperplasia Minor salivary gland tumors may also present as a submucosal mass The site of the buccal mucosa where squamous carcinoma is most frequently noted is adjacent to the third mandibular molar Patients with advanced-stage disease may present with trismus as a result of direct invasion of the tumor into the muscles of mastication, and parotid duct involvement may produce obstructive sialoadenitis 72
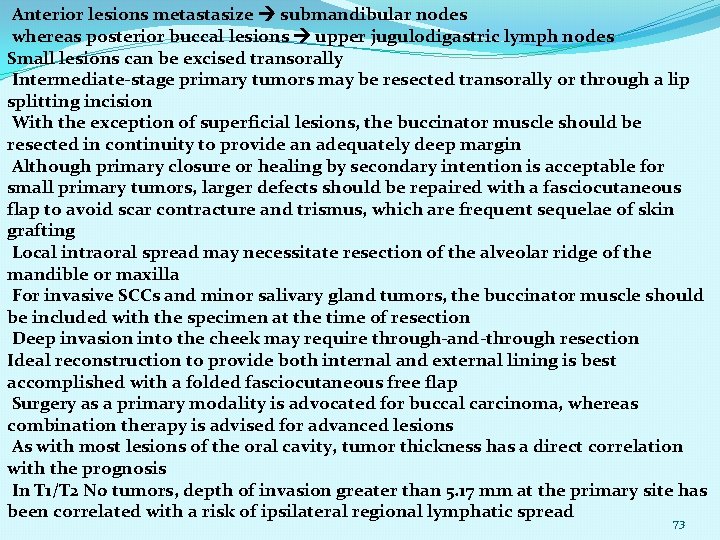
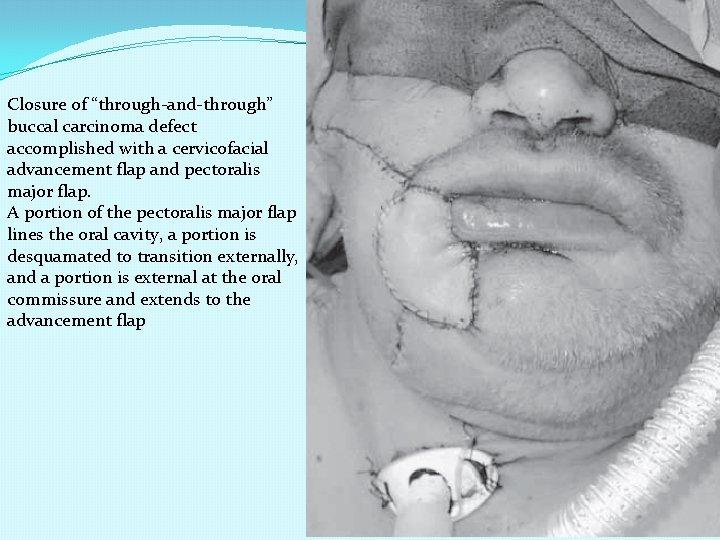
Anterior lesions metastasize submandibular nodes whereas posterior buccal lesions upper jugulodigastric lymph nodes Small lesions can be excised transorally Intermediate-stage primary tumors may be resected transorally or through a lip splitting incision With the exception of superficial lesions, the buccinator muscle should be resected in continuity to provide an adequately deep margin Although primary closure or healing by secondary intention is acceptable for small primary tumors, larger defects should be repaired with a fasciocutaneous flap to avoid scar contracture and trismus, which are frequent sequelae of skin grafting Local intraoral spread may necessitate resection of the alveolar ridge of the mandible or maxilla For invasive SCCs and minor salivary gland tumors, the buccinator muscle should be included with the specimen at the time of resection Deep invasion into the cheek may require through-and-through resection Ideal reconstruction to provide both internal and external lining is best accomplished with a folded fasciocutaneous free flap Surgery as a primary modality is advocated for buccal carcinoma, whereas combination therapy is advised for advanced lesions As with most lesions of the oral cavity, tumor thickness has a direct correlation with the prognosis In T 1/T 2 N 0 tumors, depth of invasion greater than 5. 17 mm at the primary site has been correlated with a risk of ipsilateral regional lymphatic spread 73
T 1 (21%), T 2 (38%), T 3 (23%), and T 4 (15%) The majority of patients (72%) were N 0 at presentation, and the majority were treated exclusively with surgery (71%) No patients were treated with radiation therapy alone, and postoperative radiation therapy (50 to 60 Gy) was used for patients with extracapsular nodal spread or positive margins Transoral excision was performed in the majority of patients, and only 27% of patients required a lip-splitting incision and cheek flap for resection MRND was performed for patients with node-positive necks, and SOHND was used for those who were N 0 The 5 -year survival for all patients within the series was 63%, and 5 -year survival declined from 70% for N 0 patients to 49% for patients with metastatic lymphadenopathy Within this series of patients, 45% experienced recurrence (23% local, 11% regional, 9% local and regional), and salvage therapy was successful in only 22% Stensen duct involvement and buccinator muscle invasion had no effect on locoregional recurrence. Reported 5 -year survival is 75% to 78% for stage I, 65% to 66% for stage II, 30% to 62% for stage III, and 20% to 50% for stage IV disease 74
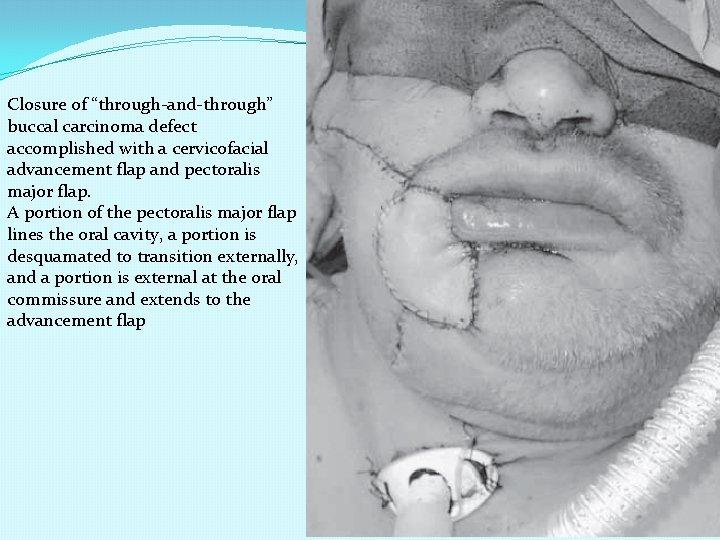
Closure of “through-and-through” buccal carcinoma defect accomplished with a cervicofacial advancement flap and pectoralis major flap. A portion of the pectoralis major flap lines the oral cavity, a portion is desquamated to transition externally, and a portion is external at the oral commissure and extends to the advancement flap 75
7. HARD PALATE SCC is the most common malignancy of the palate Running a close second in frequency are minor salivary gland tumors that include adenoid cystic carcinoma, mucoepidermoid carcinoma, adenocarcinoma, and polymorphous lowgrade adenocarcinoma Mucosal melanoma most commonly arises on the hard palate and the maxillary gingiva and presents as a nonulcerated, pigmented plaque. The typical patient is 40 to 50 years of age, and the prognosis is poor because of the locoregional aggressiveness of the tumor and its propensity for distant metastases The palate is also the most common oral site for Kaposi sarcoma. Chronic irritation from ill-fitting dentures may also play a causal role in the development of dysplasia Inflammatory lesions may mimic malignancy and can be differentiated by biopsy Necrotizing sialometaplasia on the palate as a butterfly-shaped ulcer and resembles a malignancy Treatment is symptomatic, and biopsy confirms its benign nature Torus palatini exostosis or bony outgrowth of the midline palate and maxillary bone that does not require surgical treatment unless patients are symptomatic The typical patient with a carcinoma of the hard palate is an elderly man with a history of tobacco use A high incidence of hard palate carcinoma is seen in countries where reverse smoking is practiced. 76
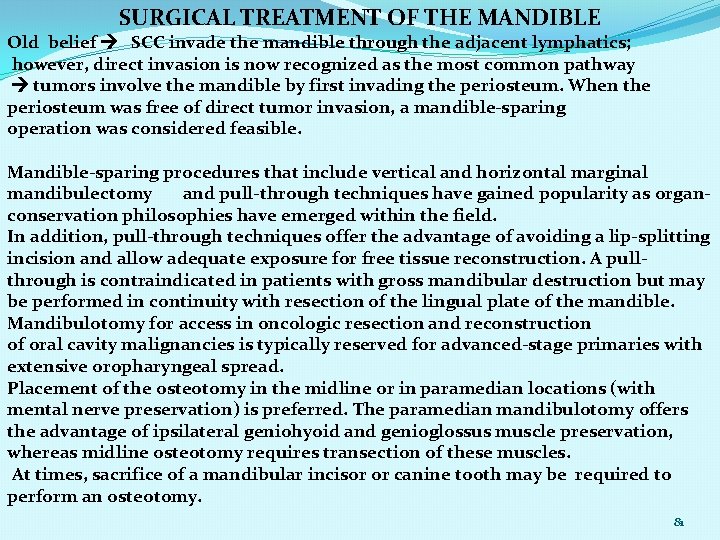
Minor salivary gland tumors submucosal nodule Ulceration is uncommon, and lesions tend to arise at the junction of the hard and soft palate Direct infiltration of bone may lead to extension into the floor of the nose or the maxillary antrum Neurotropic spread along the greater palatine nerve may result in extension to the foramen rotundum or CN V ganglion Squamous carcinoma of the hard palate is treated surgically, and small lesions may be treated with transoral wide local excision. The resection may be performed to the level of the bony portion of the hard palate with anticipated reepithelialization. Because the periosteum of the palatal bone acts as a barrier to spread, excision with bony preservation is adequate for small lesions Involvement of the periosteum requires removal of a portion of the bony palate, and partial or subtotal maxillectomy is required for larger lesions and for those that involve the maxillary antrum For malignancies that extend along the greater palatine nerve, biopsy of this nerve is important for identifying neurotropic spread. Small to medium-sized defects may be reconstructed with the aid of local advancement flaps or a buccal fat pad flap. 77
Oronasal postresection fistulae of the palate require a dental prosthesis for rehabilitation of speech and swallowing. For lesions that result in a palatal defect after resection, prosthetic rehabilitation can offer the patient an excellent functional result. In this circumstance, a maxillofacial prosthodontist may construct a splint preoperatively for use at the time of resection. A split-thickness skin graft is used to cover edges of bone from the osteotomy and to replace sites within the sinuses where mucosa was removed as part of the resection. The cavity is then packed with petroleum gauze, and a lag screw can be used to secure the prosthesis to the maxilla and to provide support to the underlying repair The temporary prosthesis is removed approximately 1 week later, and the packing is evacuated; an interim prosthesis is worn until a more permanent option can be tailored to the resultant defect. Adjuvant radiation is indicated for advanced-stage tumors, perineural invasion, and positive margins. Primary radiotherapy investigated as a therapy for hard palate carcinoma with an 80% 5 -year local control rate reported for T 1 and T 2 tumors; however, this control rate falls to 24% for T 3 and T 4 lesions surgery is the favored primary modality for carcinoma of the hard palate 5 -year survival was 48% for SCC and 63% for minor salivary gland carcinoma the rate of regional nodal metastasis based on stage was 4. 1% for T 1, 14. 9% for T 2, 10. 3% for T 3, and 24. 7% for T 4 tumors. 78
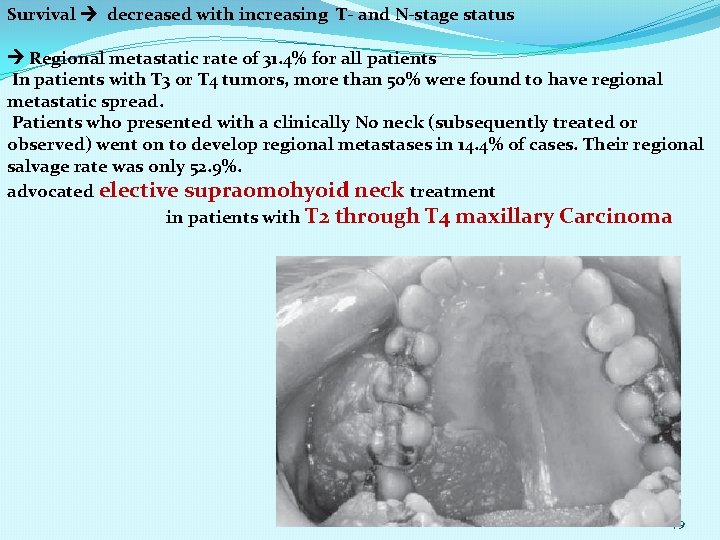
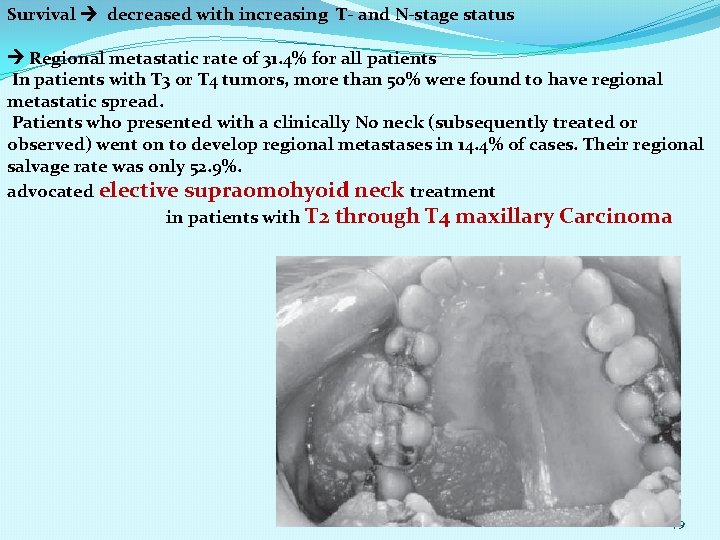
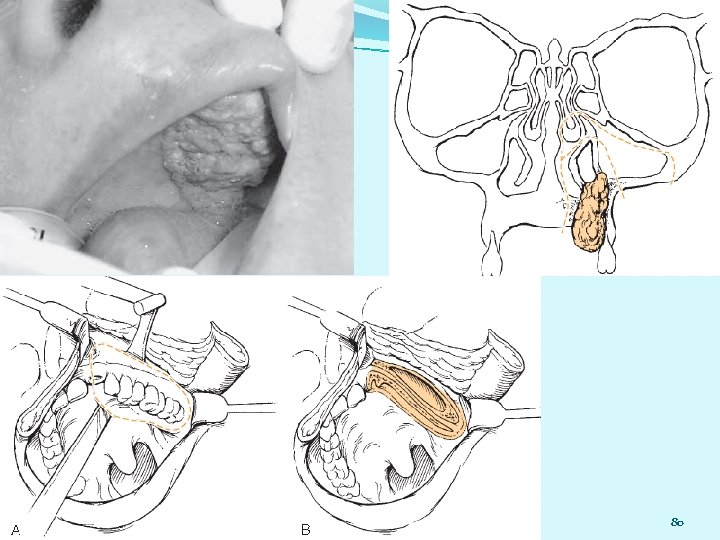
Survival decreased with increasing T- and N-stage status Regional metastatic rate of 31. 4% for all patients In patients with T 3 or T 4 tumors, more than 50% were found to have regional metastatic spread. Patients who presented with a clinically N 0 neck (subsequently treated or observed) went on to develop regional metastases in 14. 4% of cases. Their regional salvage rate was only 52. 9%. advocated elective supraomohyoid neck treatment in patients with T 2 through T 4 maxillary Carcinoma 79
80
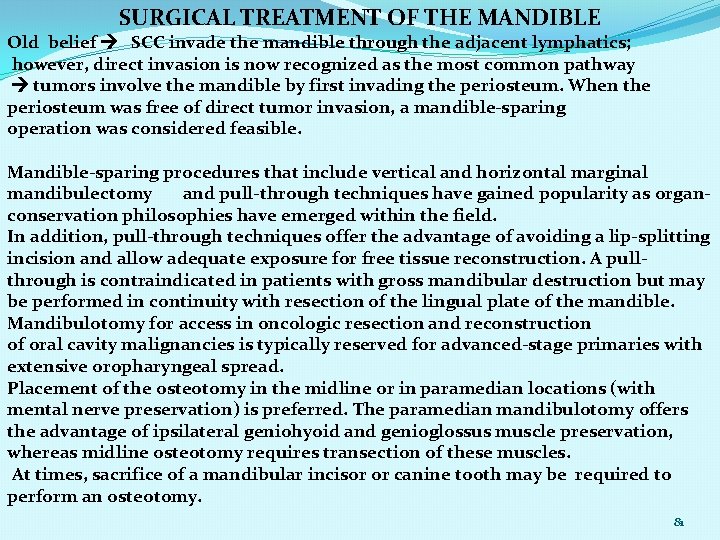
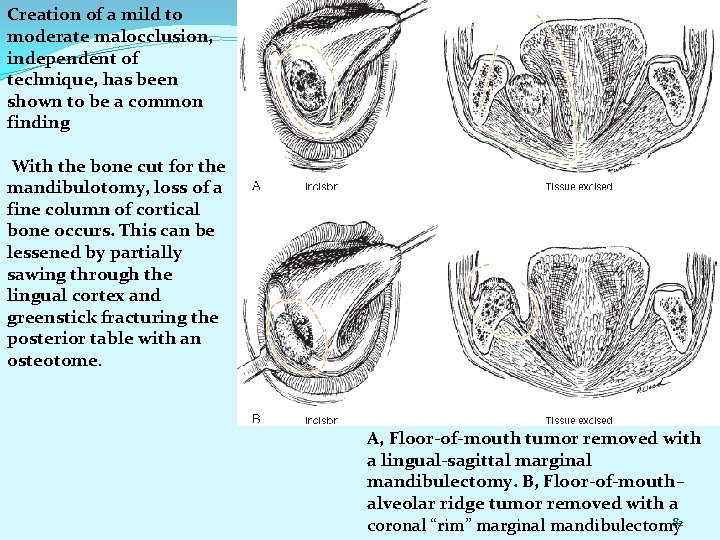
SURGICAL TREATMENT OF THE MANDIBLE Old belief SCC invade the mandible through the adjacent lymphatics; however, direct invasion is now recognized as the most common pathway tumors involve the mandible by first invading the periosteum. When the periosteum was free of direct tumor invasion, a mandible-sparing operation was considered feasible. Mandible-sparing procedures that include vertical and horizontal marginal mandibulectomy and pull-through techniques have gained popularity as organconservation philosophies have emerged within the field. In addition, pull-through techniques offer the advantage of avoiding a lip-splitting incision and allow adequate exposure for free tissue reconstruction. A pullthrough is contraindicated in patients with gross mandibular destruction but may be performed in continuity with resection of the lingual plate of the mandible. Mandibulotomy for access in oncologic resection and reconstruction of oral cavity malignancies is typically reserved for advanced-stage primaries with extensive oropharyngeal spread. Placement of the osteotomy in the midline or in paramedian locations (with mental nerve preservation) is preferred. The paramedian mandibulotomy offers the advantage of ipsilateral geniohyoid and genioglossus muscle preservation, whereas midline osteotomy requires transection of these muscles. At times, sacrifice of a mandibular incisor or canine tooth may be required to perform an osteotomy. 81
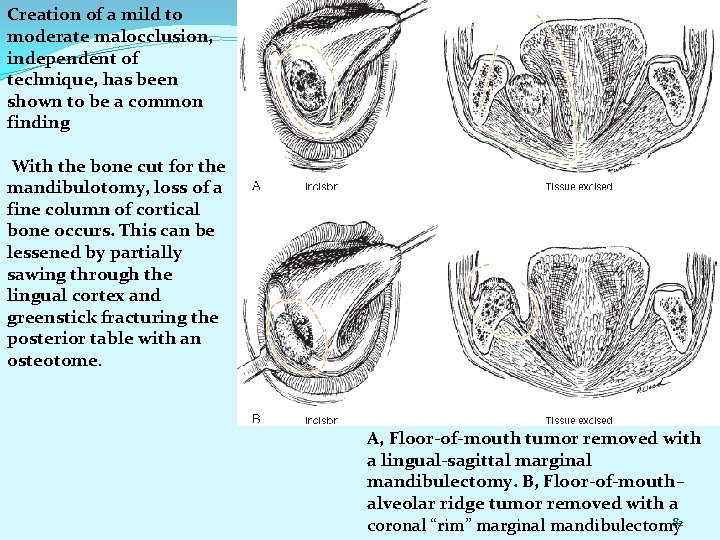
Creation of a mild to moderate malocclusion, independent of technique, has been shown to be a common finding With the bone cut for the mandibulotomy, loss of a fine column of cortical bone occurs. This can be lessened by partially sawing through the lingual cortex and greenstick fracturing the posterior table with an osteotome. A, Floor-of-mouth tumor removed with a lingual-sagittal marginal mandibulectomy. B, Floor-of-mouth– alveolar ridge tumor removed with a 82 coronal “rim” marginal mandibulectomy
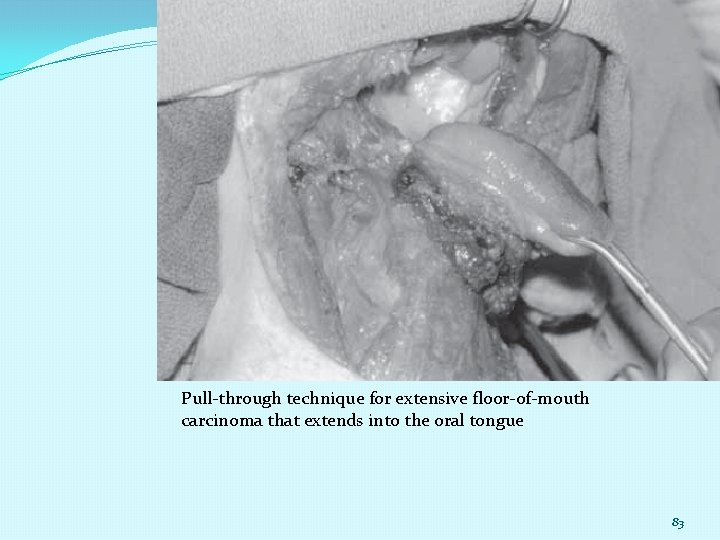
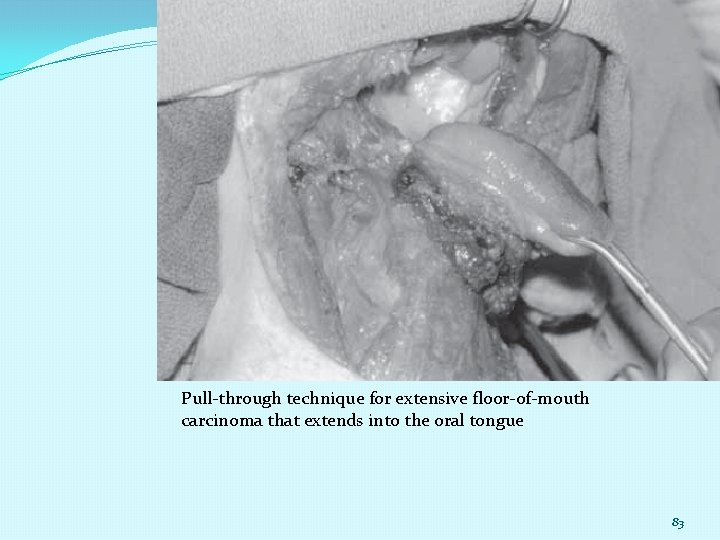
Pull-through technique for extensive floor-of-mouth carcinoma that extends into the oral tongue 83
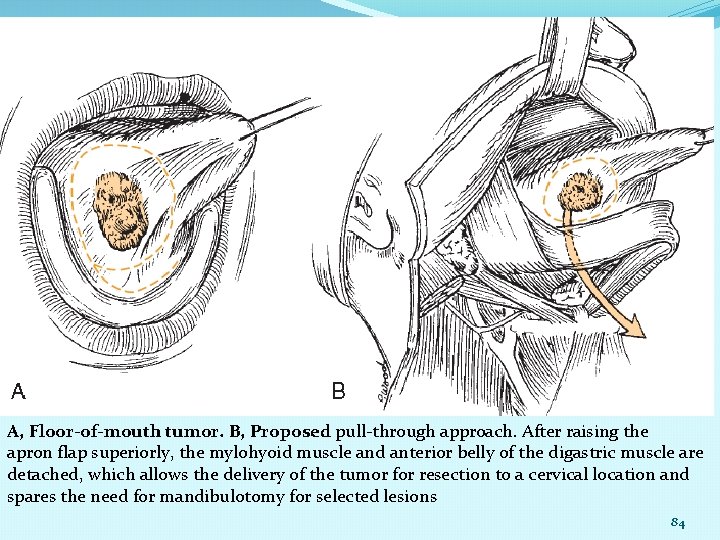
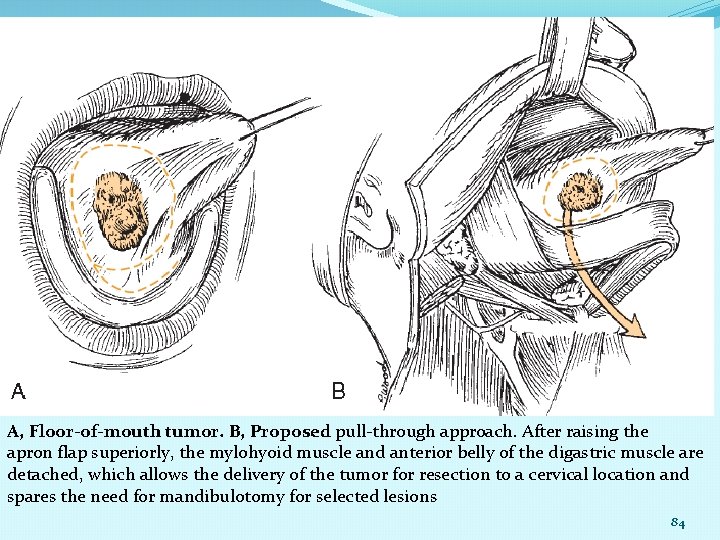
A, Floor-of-mouth tumor. B, Proposed pull-through approach. After raising the apron flap superiorly, the mylohyoid muscle and anterior belly of the digastric muscle are detached, which allows the delivery of the tumor for resection to a cervical location and spares the need for mandibulotomy for selected lesions 84
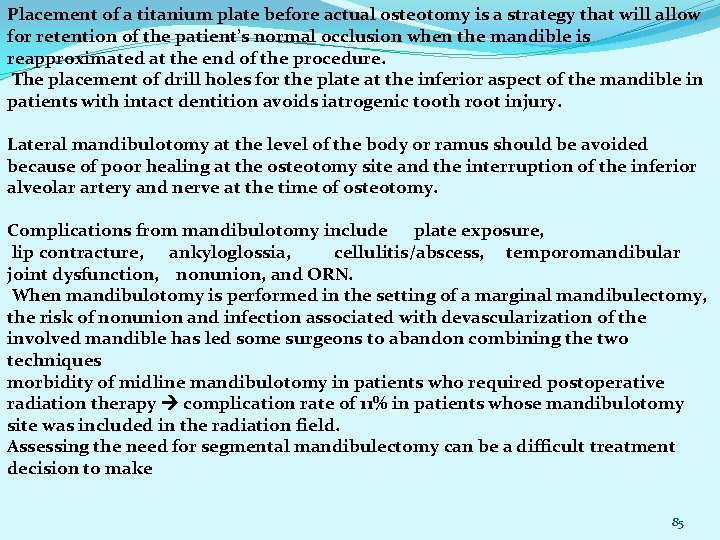
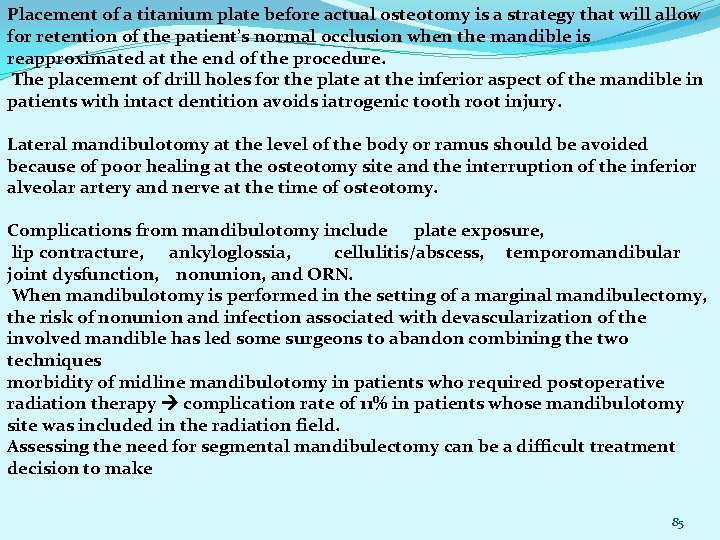
Placement of a titanium plate before actual osteotomy is a strategy that will allow for retention of the patient’s normal occlusion when the mandible is reapproximated at the end of the procedure. The placement of drill holes for the plate at the inferior aspect of the mandible in patients with intact dentition avoids iatrogenic tooth root injury. Lateral mandibulotomy at the level of the body or ramus should be avoided because of poor healing at the osteotomy site and the interruption of the inferior alveolar artery and nerve at the time of osteotomy. Complications from mandibulotomy include plate exposure, lip contracture, ankyloglossia, cellulitis/abscess, temporomandibular joint dysfunction, nonunion, and ORN. When mandibulotomy is performed in the setting of a marginal mandibulectomy, the risk of nonunion and infection associated with devascularization of the involved mandible has led some surgeons to abandon combining the two techniques morbidity of midline mandibulotomy in patients who required postoperative radiation therapy complication rate of 11% in patients whose mandibulotomy site was included in the radiation field. Assessing the need for segmental mandibulectomy can be a difficult treatment decision to make 85
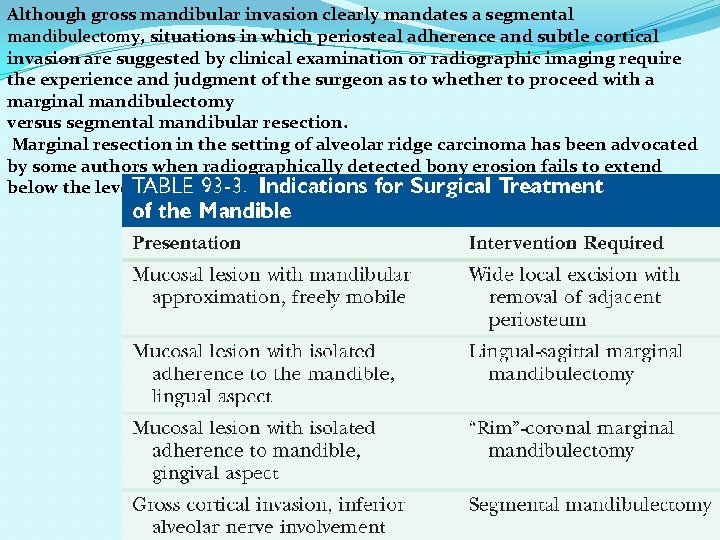
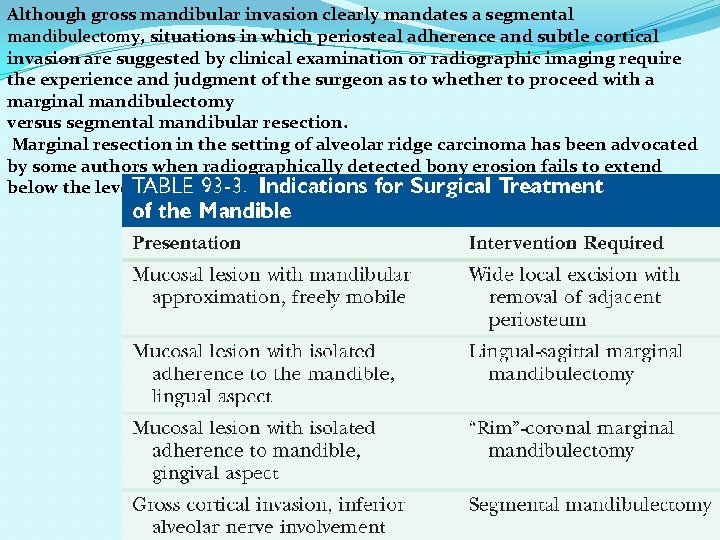
Although gross mandibular invasion clearly mandates a segmental mandibulectomy, situations in which periosteal adherence and subtle cortical invasion are suggested by clinical examination or radiographic imaging require the experience and judgment of the surgeon as to whether to proceed with a marginal mandibulectomy versus segmental mandibular resection. Marginal resection in the setting of alveolar ridge carcinoma has been advocated by some authors when radiographically detected bony erosion fails to extend below the level of the mandibular canal. 86
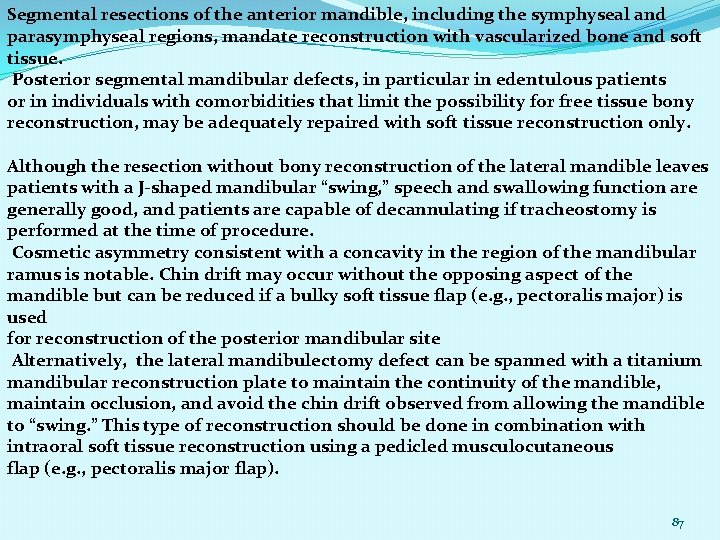
Segmental resections of the anterior mandible, including the symphyseal and parasymphyseal regions, mandate reconstruction with vascularized bone and soft tissue. Posterior segmental mandibular defects, in particular in edentulous patients or in individuals with comorbidities that limit the possibility for free tissue bony reconstruction, may be adequately repaired with soft tissue reconstruction only. Although the resection without bony reconstruction of the lateral mandible leaves patients with a J-shaped mandibular “swing, ” speech and swallowing function are generally good, and patients are capable of decannulating if tracheostomy is performed at the time of procedure. Cosmetic asymmetry consistent with a concavity in the region of the mandibular ramus is notable. Chin drift may occur without the opposing aspect of the mandible but can be reduced if a bulky soft tissue flap (e. g. , pectoralis major) is used for reconstruction of the posterior mandibular site Alternatively, the lateral mandibulectomy defect can be spanned with a titanium mandibular reconstruction plate to maintain the continuity of the mandible, maintain occlusion, and avoid the chin drift observed from allowing the mandible to “swing. ” This type of reconstruction should be done in combination with intraoral soft tissue reconstruction using a pedicled musculocutaneous flap (e. g. , pectoralis major flap). 87
SURGICAL TREATMENT OF THE NECK Patterns of spread from primary tumor sites in the head and neck to cervical lymphatics are well described. The location and incidence of metastasis vary according to the primary site. Primary tumors within the oral cavity and lip typically metastasize to the nodes in levels I, II, and III Compromise of the immune response may be correlated to the risk of regional metastatic spread of oral carcinoma. Positive lymph nodes demonstrate higher densities of immature dendritic cells and lower densities of activated cytotoxic T lymphocytes when compared with uninvolved lymph nodes from the same cyclin D 1 gene numeric aberrations assessed on FNA samples in stage I and II oral cancer patients. Cluster-type amplification of the cyclin D 1 gene correlated with future regional recurrence in patients when the neck was not treated electively. sentinel lymph node biopsy (SLNB) in 108 patients with oral and cutaneous Malignancies negative predictive value of SLNB for oral cancer was 92% upstaging of 16% of cases from N 0 to N 1. the sentinel node location was outside of the expected lymphatic drainage region in 13. 6% of cases. Complications with the use of the technique were minimal 88
Overall sensitivity of 94% and a negative predictive value of 96% with the use of SLNB in the setting of oral cancer. In previously treated oral carcinoma patients, SLNB has also been shown to have a high reported negative predictive value (91%) N 0, 20%, elective treatment to the regional lymphatics should be considered. Options for treatment include elective neck irradiation versus neck dissection. Modifications of neck dissection have evolved from radical neck dissection (RND) through modified radical neck dissection (MRND) to selective neck dissection (SND), which can serve as a staging procedure to determine the need for postoperative adjuvant radiotherapy. For the clinically node-positive neck, the surgical treatment of choice has traditionally been MRND or RND, although some authors advocate SND for the treatment of limited N 1 disease. quality-of-life data for patients undergoing RND, MRND, and SND. Shoulder disability at 6 months was the least for SND patients and was similar for SND and MRND patients at 12 months. Additionally, MRND and SND patients were noted to have fewer problems with pain than RND patients. 89
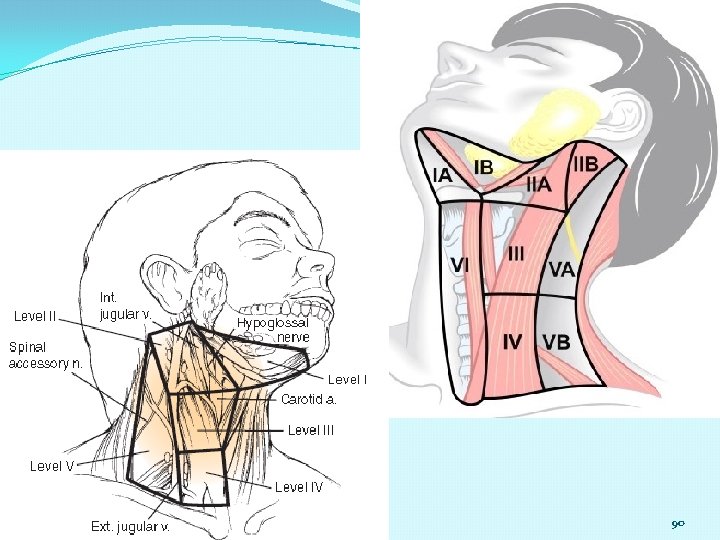
90
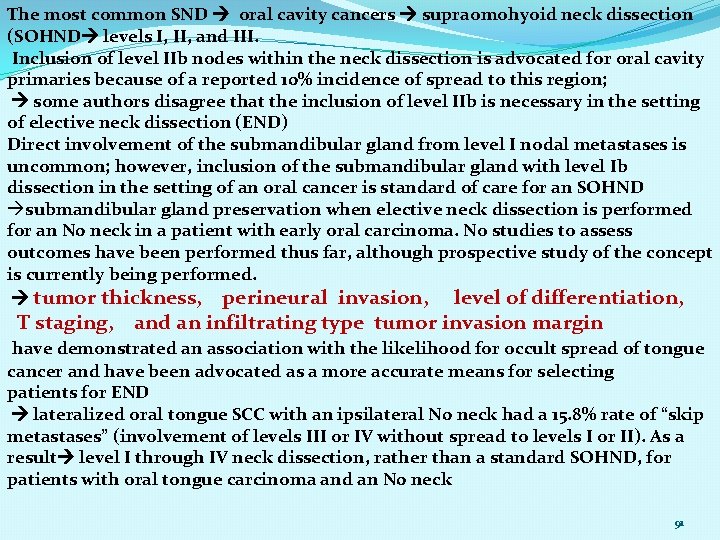
The most common SND oral cavity cancers supraomohyoid neck dissection (SOHND levels I, II, and III. Inclusion of level IIb nodes within the neck dissection is advocated for oral cavity primaries because of a reported 10% incidence of spread to this region; some authors disagree that the inclusion of level IIb is necessary in the setting of elective neck dissection (END) Direct involvement of the submandibular gland from level I nodal metastases is uncommon; however, inclusion of the submandibular gland with level Ib dissection in the setting of an oral cancer is standard of care for an SOHND submandibular gland preservation when elective neck dissection is performed for an N 0 neck in a patient with early oral carcinoma. No studies to assess outcomes have been performed thus far, although prospective study of the concept is currently being performed. tumor thickness, perineural invasion, level of differentiation, T staging, and an infiltrating type tumor invasion margin have demonstrated an association with the likelihood for occult spread of tongue cancer and have been advocated as a more accurate means for selecting patients for END lateralized oral tongue SCC with an ipsilateral N 0 neck had a 15. 8% rate of “skip metastases” (involvement of levels III or IV without spread to levels I or II). As a result level I through IV neck dissection, rather than a standard SOHND, for patients with oral tongue carcinoma and an N 0 neck 91
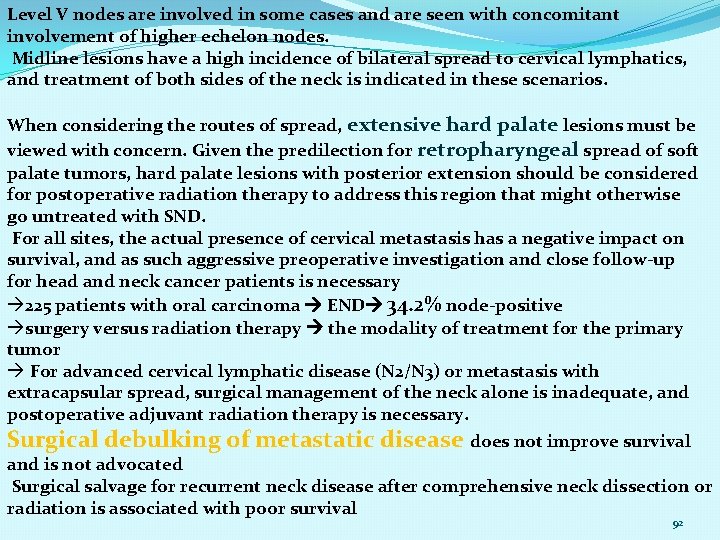
Level V nodes are involved in some cases and are seen with concomitant involvement of higher echelon nodes. Midline lesions have a high incidence of bilateral spread to cervical lymphatics, and treatment of both sides of the neck is indicated in these scenarios. When considering the routes of spread, extensive hard palate lesions must be viewed with concern. Given the predilection for retropharyngeal spread of soft palate tumors, hard palate lesions with posterior extension should be considered for postoperative radiation therapy to address this region that might otherwise go untreated with SND. For all sites, the actual presence of cervical metastasis has a negative impact on survival, and as such aggressive preoperative investigation and close follow-up for head and neck cancer patients is necessary 225 patients with oral carcinoma END 34. 2% node-positive surgery versus radiation therapy the modality of treatment for the primary tumor For advanced cervical lymphatic disease (N 2/N 3) or metastasis with extracapsular spread, surgical management of the neck alone is inadequate, and postoperative adjuvant radiation therapy is necessary. Surgical debulking of metastatic disease does not improve survival and is not advocated Surgical salvage for recurrent neck disease after comprehensive neck dissection or radiation is associated with poor survival 92
93
94
 Body cavity
Body cavity Peripheral giant cell granuloma
Peripheral giant cell granuloma Thoracic cavity and abdominal cavity
Thoracic cavity and abdominal cavity Lesser peritoneal cavity
Lesser peritoneal cavity Peritoneum,
Peritoneum, Spinal cavity
Spinal cavity Digestive system cavity
Digestive system cavity Epithelial component
Epithelial component Normal flora of oral cavity
Normal flora of oral cavity Pharynx to esophagus
Pharynx to esophagus Rugae area
Rugae area Chapter 10 landmarks of the face and oral cavity
Chapter 10 landmarks of the face and oral cavity The monophasic liquid dosage form is solution
The monophasic liquid dosage form is solution White lesions
White lesions Exercise 38 review sheet art-labeling activity 2
Exercise 38 review sheet art-labeling activity 2 Palatine aponeurosis
Palatine aponeurosis Hypertensive emergency
Hypertensive emergency Carcinoma in situ
Carcinoma in situ Neuroleptic malignant syndrome
Neuroleptic malignant syndrome Malignant mesothelioma
Malignant mesothelioma Cataractectomy
Cataractectomy Local invasion
Local invasion Hypokalemia
Hypokalemia Benign or malignant
Benign or malignant Benign and malignant tumor
Benign and malignant tumor Perdida de polaridad celular
Perdida de polaridad celular Malignant and benign tumors
Malignant and benign tumors Hematocrit
Hematocrit Norepinephrine computation
Norepinephrine computation Malignant neuroleptic syndrome
Malignant neuroleptic syndrome Schizophrenia disorganized behavior
Schizophrenia disorganized behavior Prostate adenocarcinoma perineural invasion
Prostate adenocarcinoma perineural invasion Kitwood malignant social psychology
Kitwood malignant social psychology Hypertensive emergency vs urgency
Hypertensive emergency vs urgency Malignant neoplasm of the blood-forming organs
Malignant neoplasm of the blood-forming organs Risk factors for malignant melanoma
Risk factors for malignant melanoma 101012 bằng
101012 bằng Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Lời thề hippocrates
Lời thề hippocrates đại từ thay thế
đại từ thay thế Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Công thức tính thế năng
Công thức tính thế năng Các môn thể thao bắt đầu bằng tiếng chạy
Các môn thể thao bắt đầu bằng tiếng chạy Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Dot
Dot Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 độ dài liên kết
độ dài liên kết Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan điện thế nghỉ
điện thế nghỉ Một số thể thơ truyền thống
Một số thể thơ truyền thống Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Lp html
Lp html Số nguyên là gì
Số nguyên là gì Tia chieu sa te
Tia chieu sa te đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Tư thế worm breton là gì
Tư thế worm breton là gì Sơ đồ cơ thể người
Sơ đồ cơ thể người ưu thế lai là gì
ưu thế lai là gì Tư thế ngồi viết
Tư thế ngồi viết Bàn tay mà dây bẩn
Bàn tay mà dây bẩn Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Bổ thể
Bổ thể Tư thế ngồi viết
Tư thế ngồi viết V cc cc
V cc cc Thẻ vin
Thẻ vin Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Chúa sống lại
Chúa sống lại Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Hổ sinh sản vào mùa nào
Hổ sinh sản vào mùa nào Diễn thế sinh thái là
Diễn thế sinh thái là Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Glenoid cavity articulates
Glenoid cavity articulates Nasal pharynx
Nasal pharynx Nasal cavity
Nasal cavity Stomach physiology
Stomach physiology Body cavities
Body cavities Chorda tympani
Chorda tympani Lateral strabismus cranial nerve
Lateral strabismus cranial nerve Sagittal section of the abdominopelvic cavity
Sagittal section of the abdominopelvic cavity Pseudocoelomate present in
Pseudocoelomate present in Operator position in dentistry
Operator position in dentistry Chapter 5 the skeletal system figure 5-13
Chapter 5 the skeletal system figure 5-13 Narrow cavity in the dermis from which hair cells grow
Narrow cavity in the dermis from which hair cells grow Skirt in cast metal restoration
Skirt in cast metal restoration Felix rettig
Felix rettig Body cell
Body cell Cavity ring down
Cavity ring down Organ found within the mesentery that stores blood frog
Organ found within the mesentery that stores blood frog