Malignant Epithelial Tumors Fig 9 1 Histological features


- Slides: 26
Malignant Epithelial Tumors
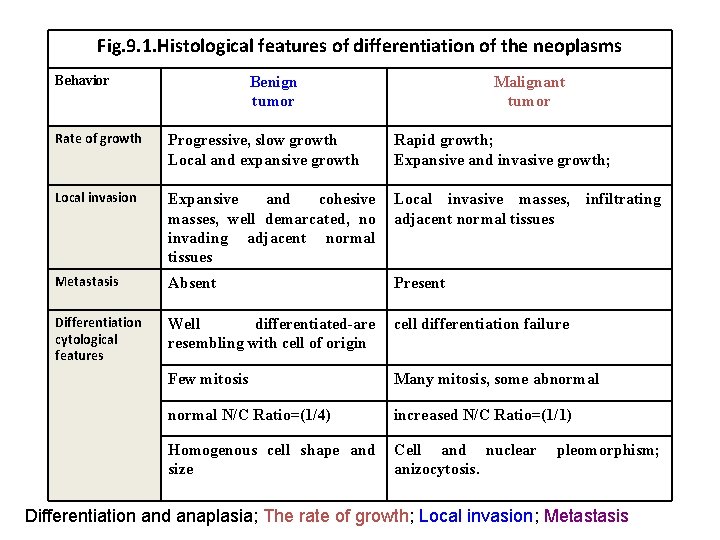
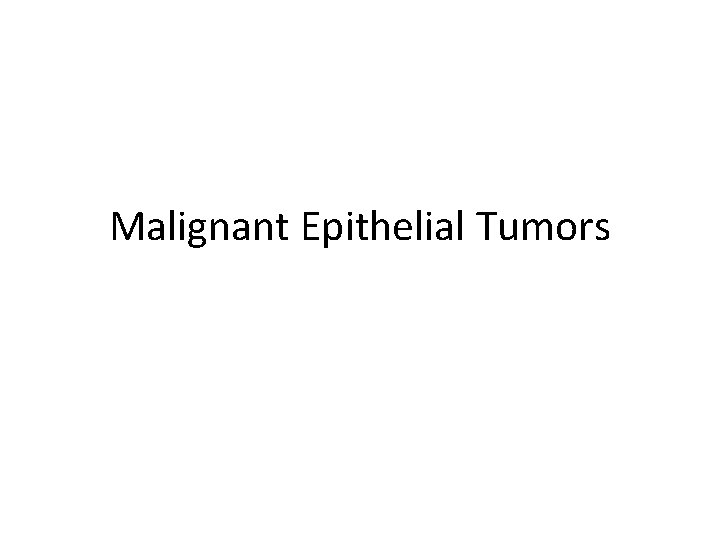
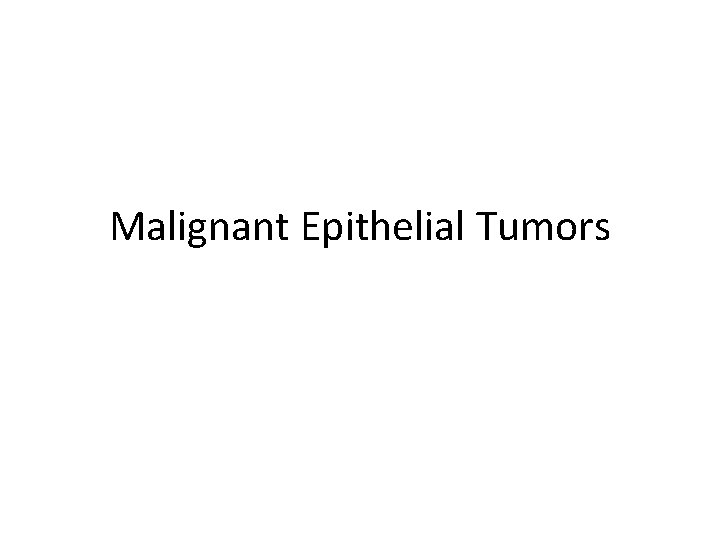
Fig. 9. 1. Histological features of differentiation of the neoplasms Behavior Benign tumor Malignant tumor Rate of growth Progressive, slow growth Local and expansive growth Rapid growth; Expansive and invasive growth; Local invasion Expansive and cohesive masses, well demarcated, no invading adjacent normal tissues Local invasive masses, infiltrating adjacent normal tissues Metastasis Absent Present Differentiation cytological features Well differentiated-are resembling with cell of origin cell differentiation failure Few mitosis Many mitosis, some abnormal N/C Ratio=(1/4) increased N/C Ratio=(1/1) Homogenous cell shape and size Cell and nuclear anizocytosis. pleomorphism; Differentiation and anaplasia; The rate of growth; Local invasion; Metastasis
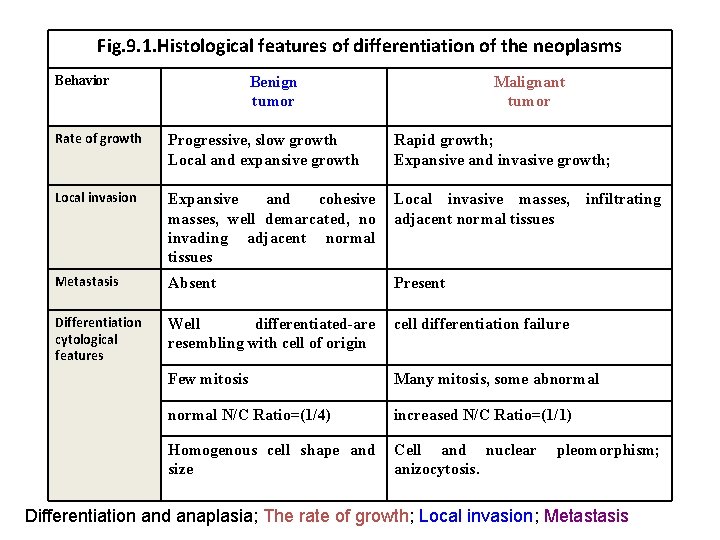
Differentiation=morphological and functional similarity of neoplastic cells with cells of origin From: Stevens A. J Lowe J. Pathology. Mosby 1995 Normal Fig. 9. 2. Differentiation and anaplasia: WD
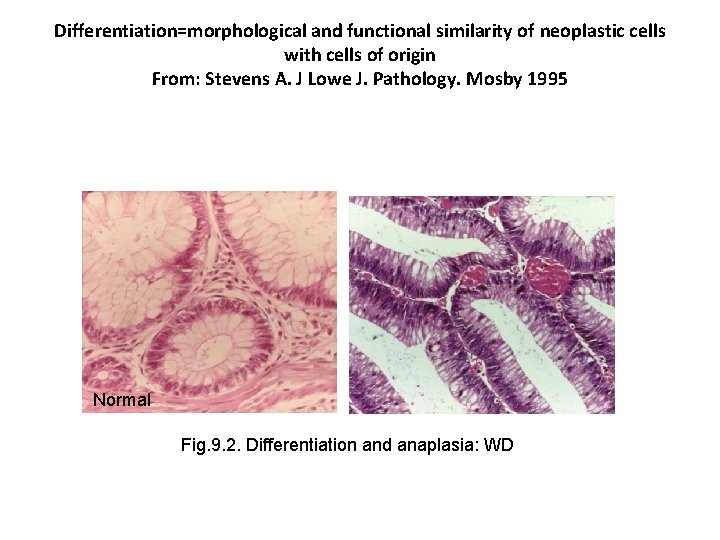
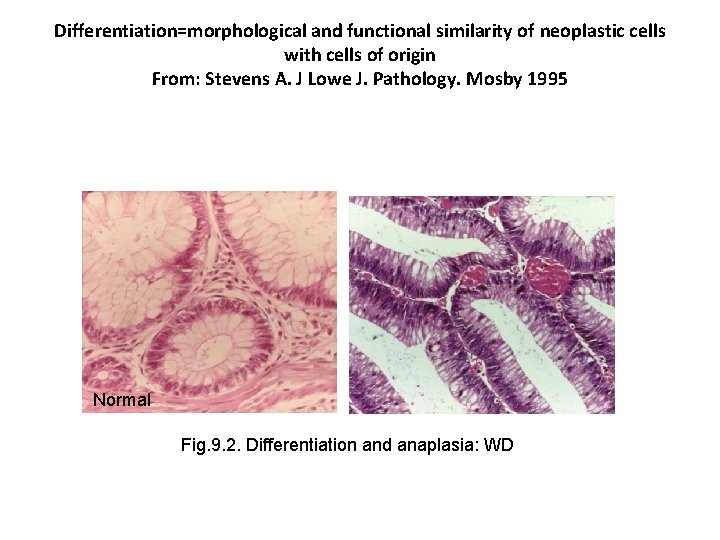
normal WD MD ND Fig. 9. 3. TM are more or less differentiated, showing various degrees of differentiation ranging from well-differentiated forms (BD) to non-differentiated (ND) or anaplastic forms.
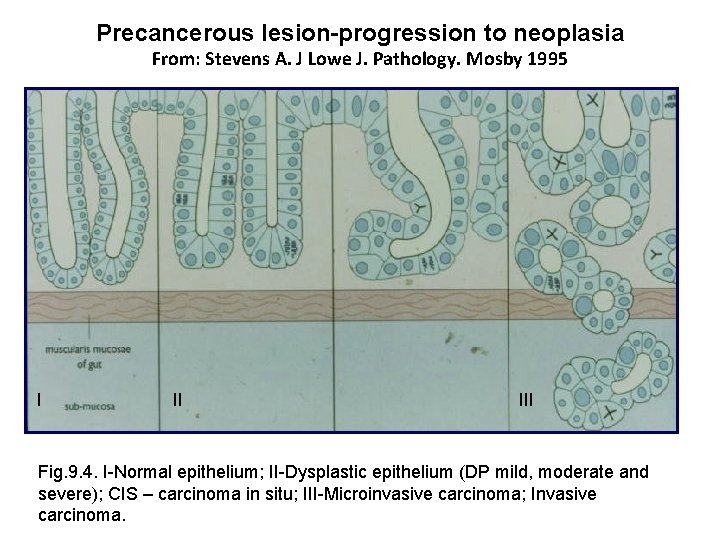
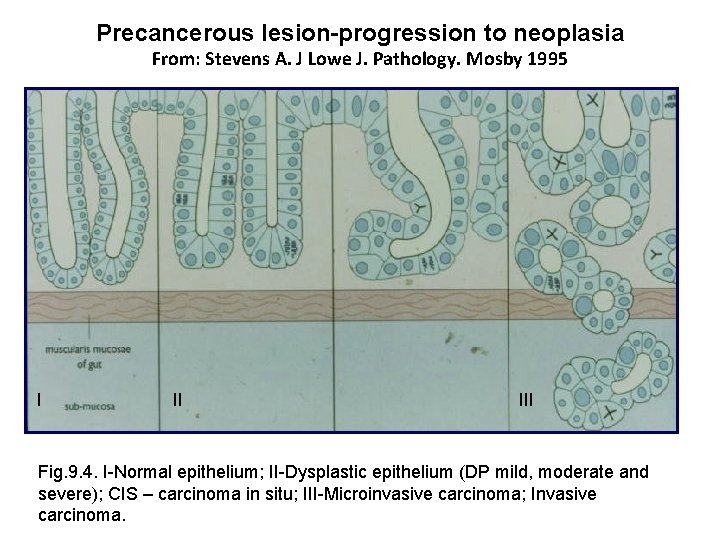
Precancerous lesion-progression to neoplasia From: Stevens A. J Lowe J. Pathology. Mosby 1995 I II III Fig. 9. 4. I-Normal epithelium; II-Dysplastic epithelium (DP mild, moderate and severe); CIS – carcinoma in situ; III-Microinvasive carcinoma; Invasive carcinoma.

CIS – carcinoma in situ-skin Fig. 9. 5. CIS-cell and nuclear pleomorphysm; intact BM.
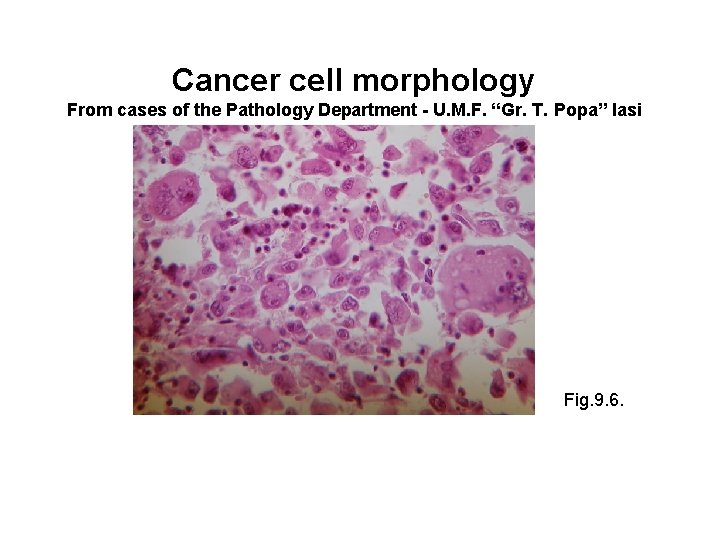
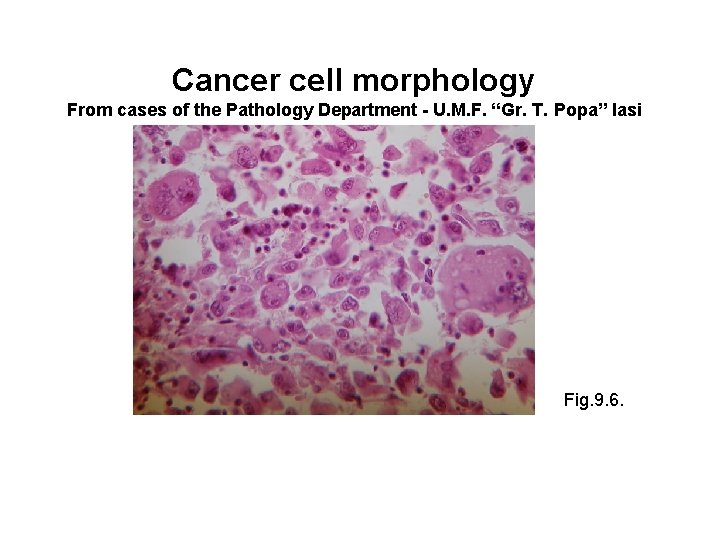
Cancer cell morphology From cases of the Pathology Department - U. M. F. “Gr. T. Popa” Iasi Fig. 9. 6.
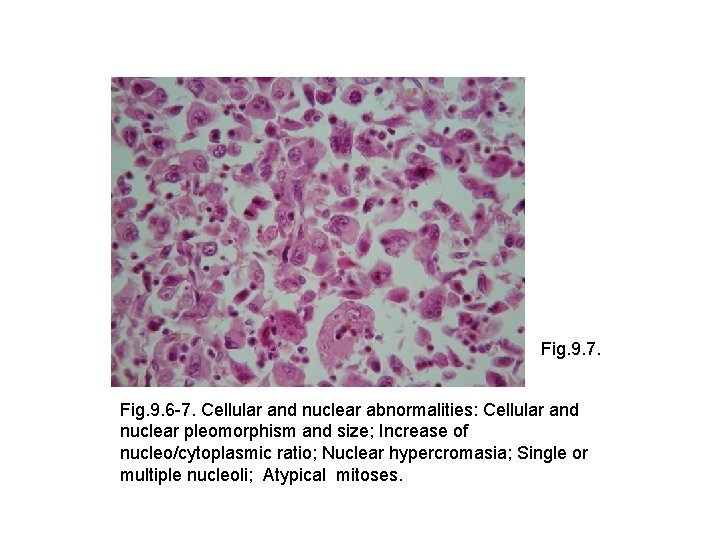
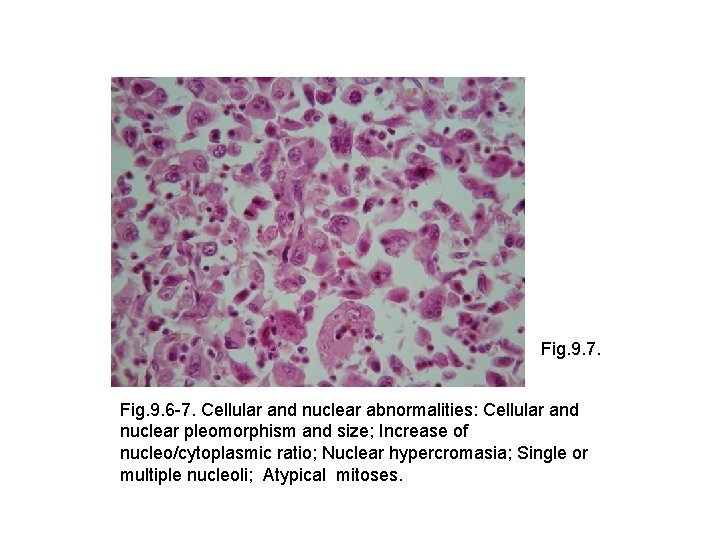
Fig. 9. 7. Fig. 9. 6 -7. Cellular and nuclear abnormalities: Cellular and nuclear pleomorphism and size; Increase of nucleo/cytoplasmic ratio; Nuclear hypercromasia; Single or multiple nucleoli; Atypical mitoses.
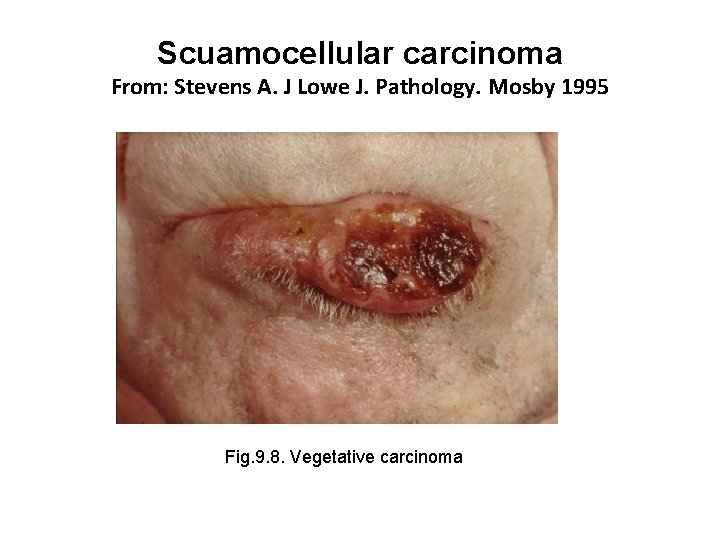
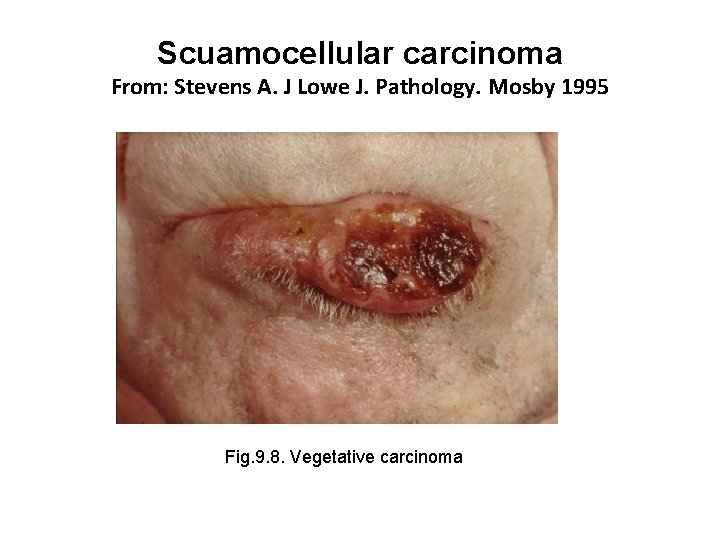
Scuamocellular carcinoma From: Stevens A. J Lowe J. Pathology. Mosby 1995 Fig. 9. 8. Vegetative carcinoma

Fig. 9. 9. Ulcerative carcinoma
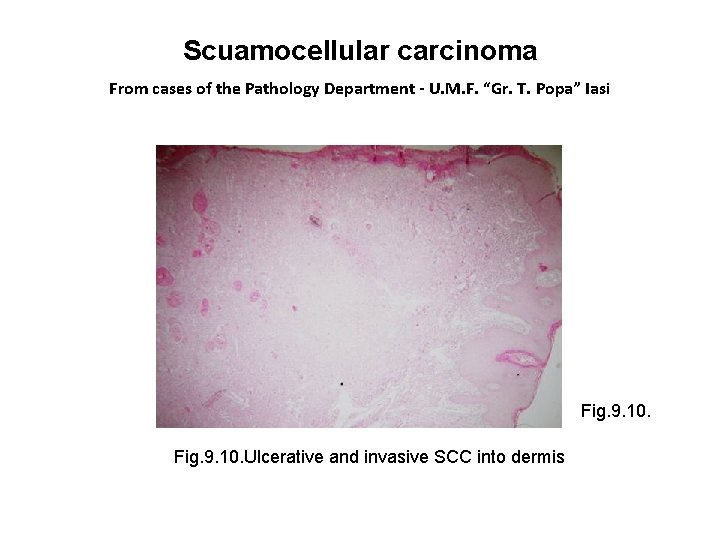
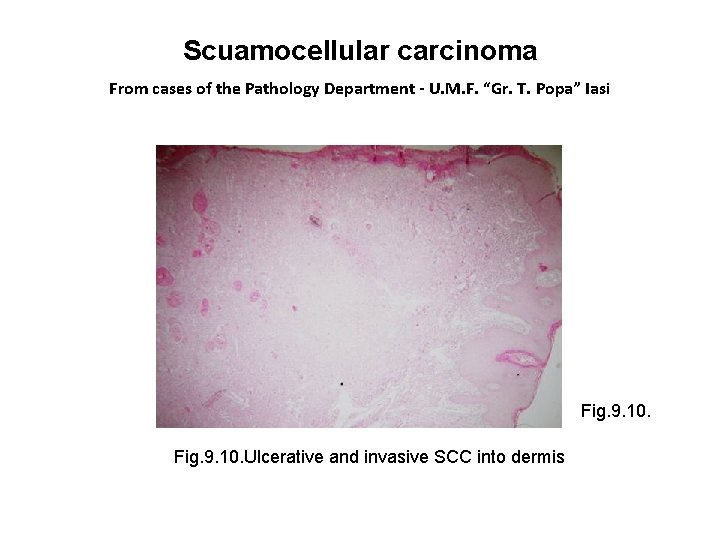
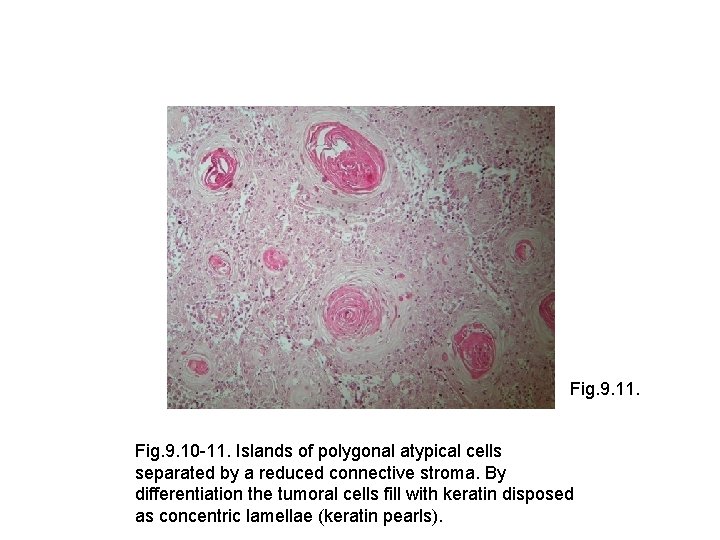
Scuamocellular carcinoma From cases of the Pathology Department - U. M. F. “Gr. T. Popa” Iasi Fig. 9. 10. Ulcerative and invasive SCC into dermis
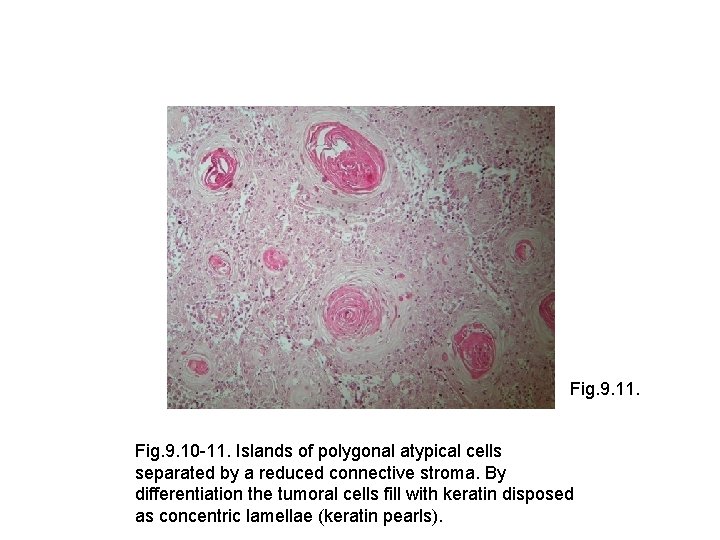
Fig. 9. 11. Fig. 9. 10 -11. Islands of polygonal atypical cells separated by a reduced connective stroma. By differentiation the tumoral cells fill with keratin disposed as concentric lamellae (keratin pearls).
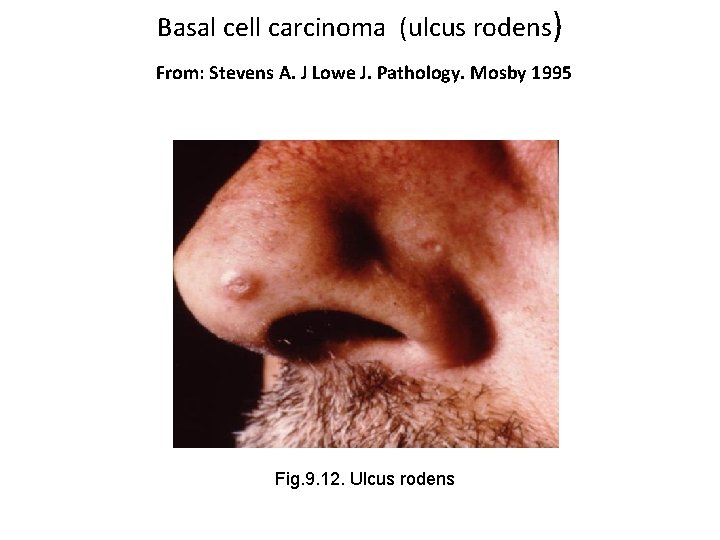
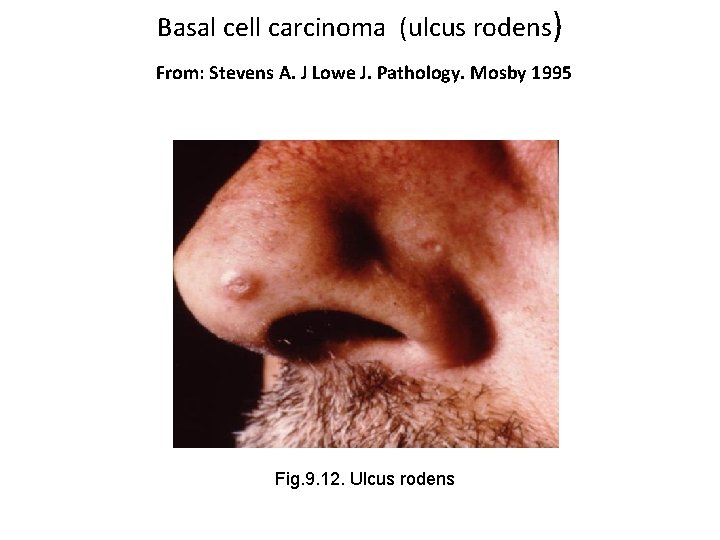
Basal cell carcinoma (ulcus rodens) From: Stevens A. J Lowe J. Pathology. Mosby 1995 Fig. 9. 12. Ulcus rodens
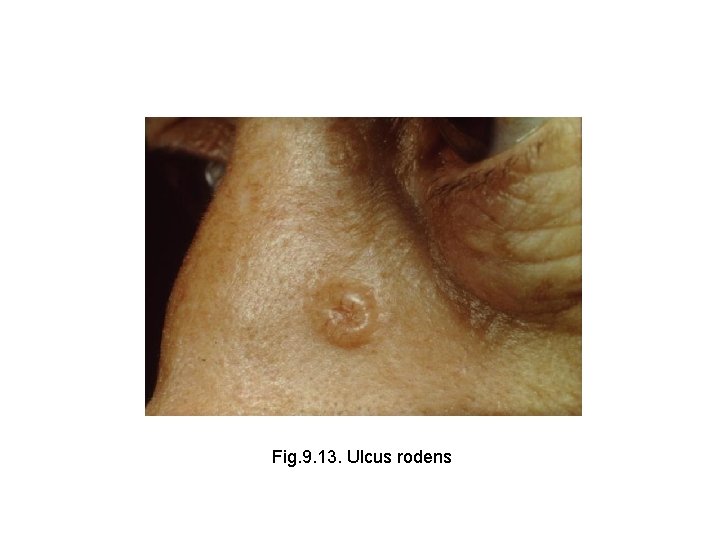
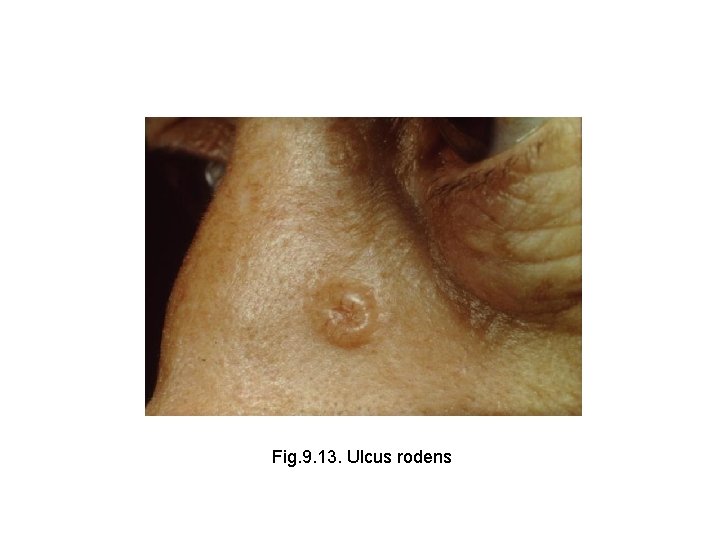
Fig. 9. 13. Ulcus rodens
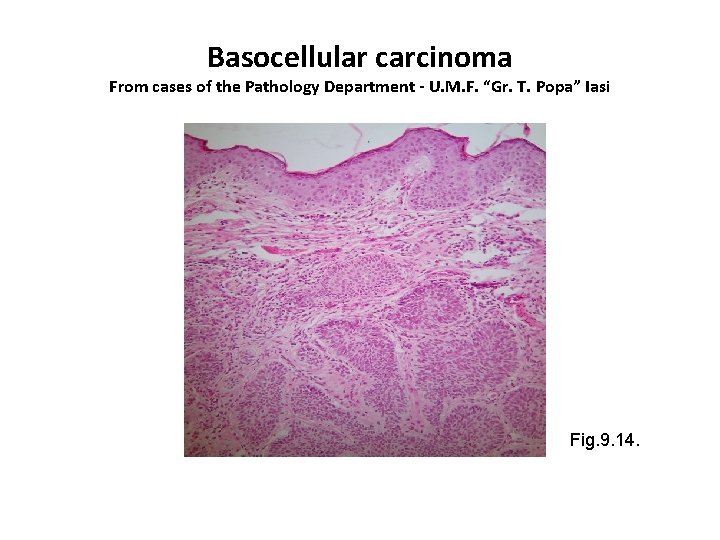
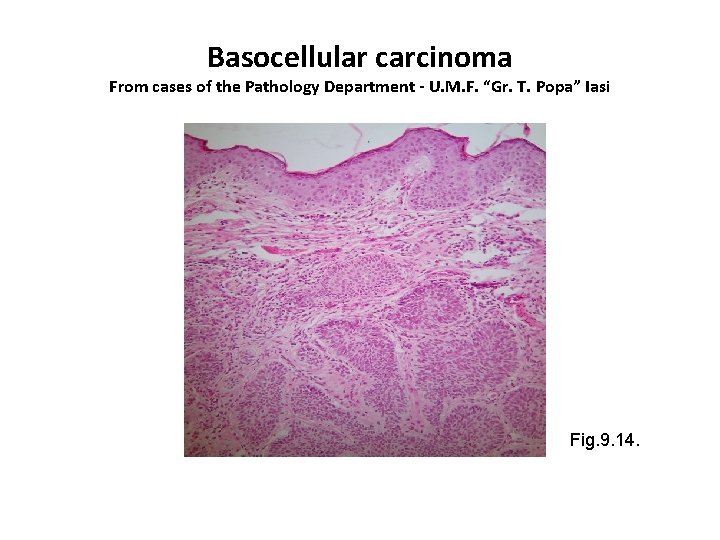
Basocellular carcinoma From cases of the Pathology Department - U. M. F. “Gr. T. Popa” Iasi Fig. 9. 14.
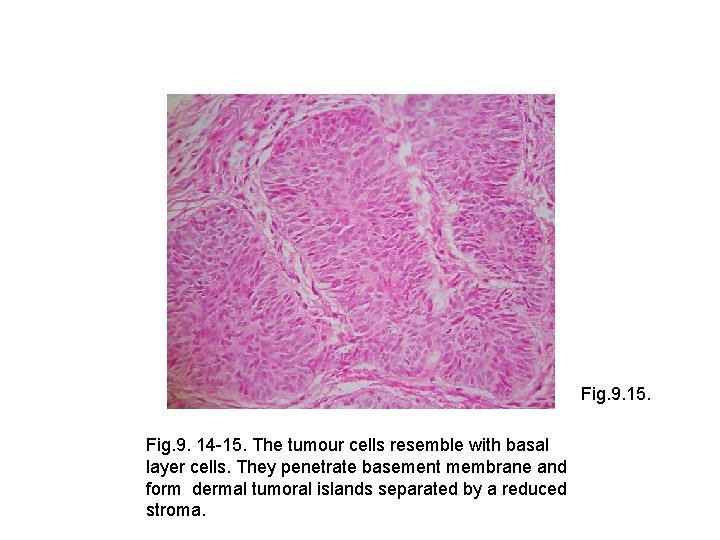
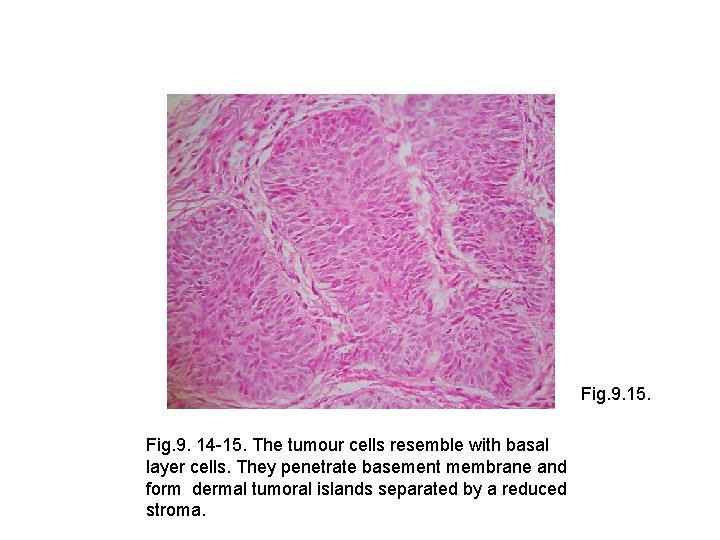
Fig. 9. 15. Fig. 9. 14 -15. The tumour cells resemble with basal layer cells. They penetrate basement membrane and form dermal tumoral islands separated by a reduced stroma.
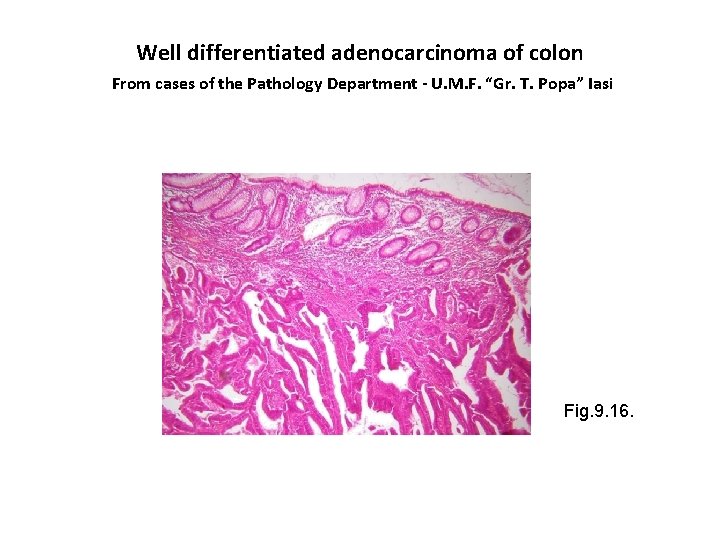
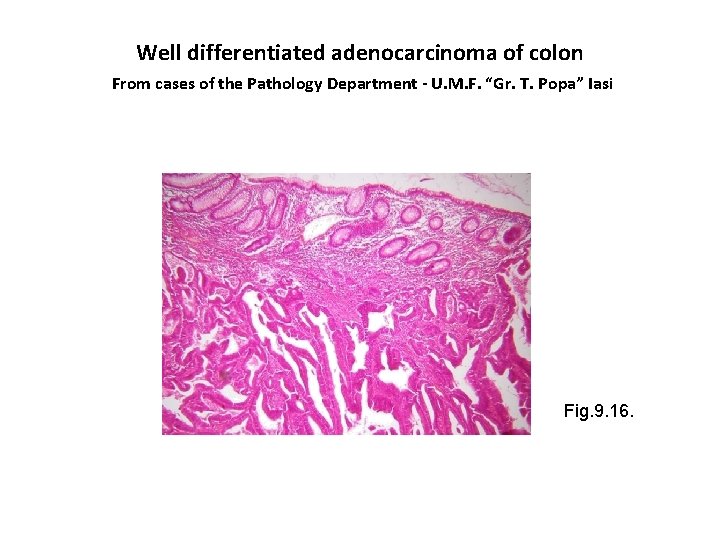
Well differentiated adenocarcinoma of colon From cases of the Pathology Department - U. M. F. “Gr. T. Popa” Iasi Fig. 9. 16.
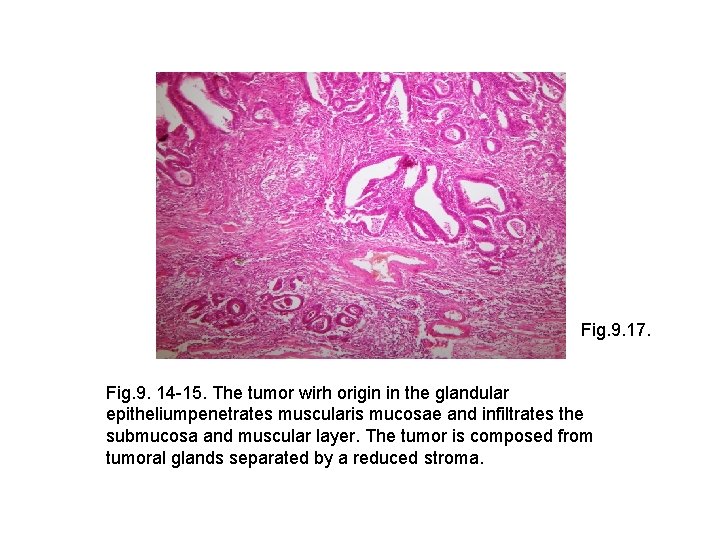
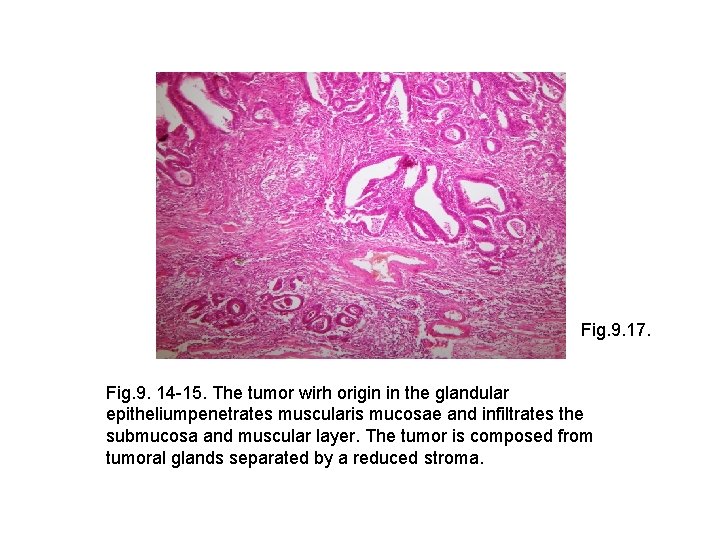
Fig. 9. 17. Fig. 9. 14 -15. The tumor wirh origin in the glandular epitheliumpenetrates muscularis mucosae and infiltrates the submucosa and muscular layer. The tumor is composed from tumoral glands separated by a reduced stroma.
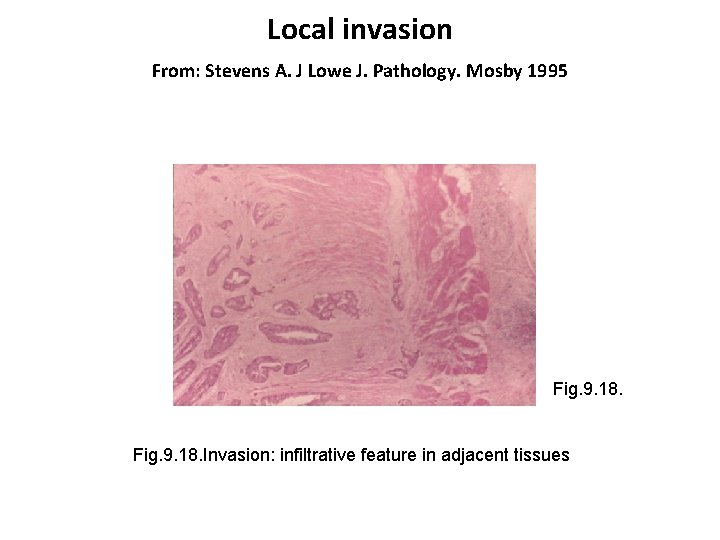
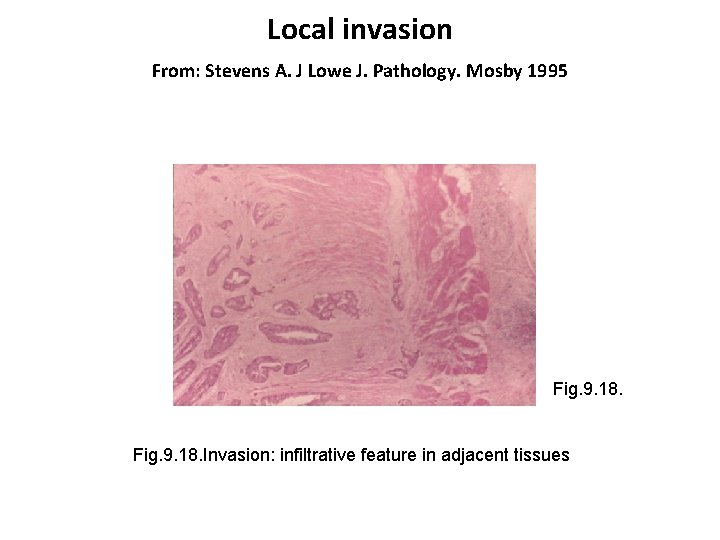
Local invasion From: Stevens A. J Lowe J. Pathology. Mosby 1995 Fig. 9. 18. Invasion: infiltrative feature in adjacent tissues
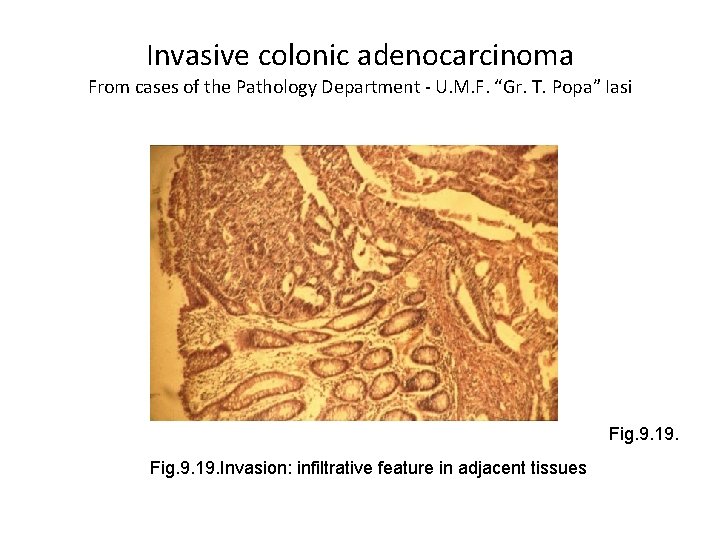
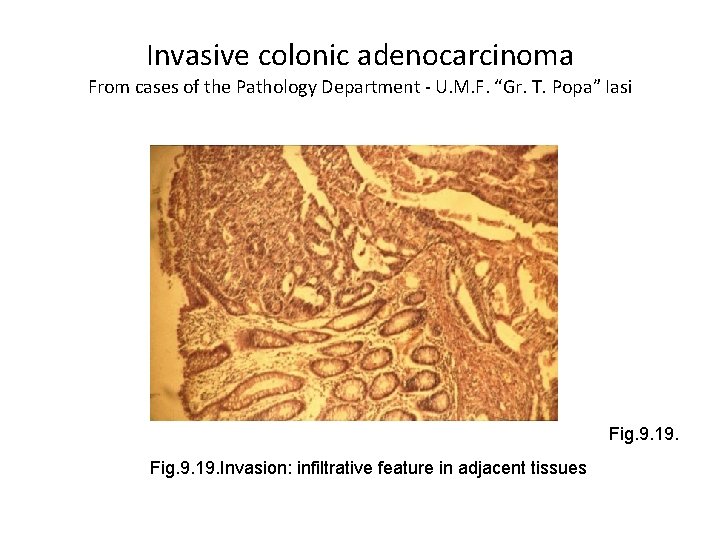
Invasive colonic adenocarcinoma From cases of the Pathology Department - U. M. F. “Gr. T. Popa” Iasi Fig. 9. 19. Invasion: infiltrative feature in adjacent tissues
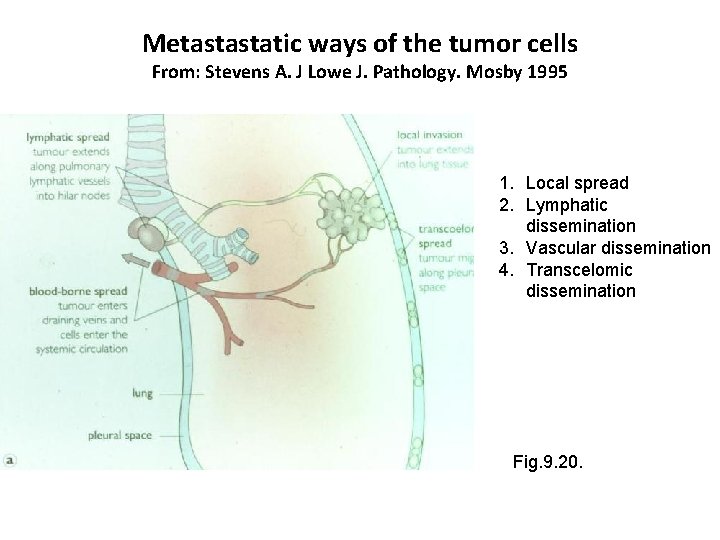
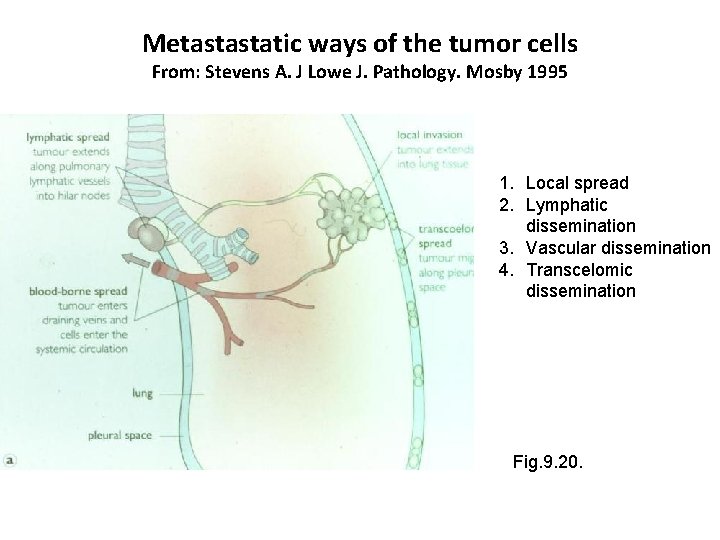
Metastastatic ways of the tumor cells From: Stevens A. J Lowe J. Pathology. Mosby 1995 1. Local spread 2. Lymphatic dissemination 3. Vascular dissemination 4. Transcelomic dissemination Fig. 9. 20.
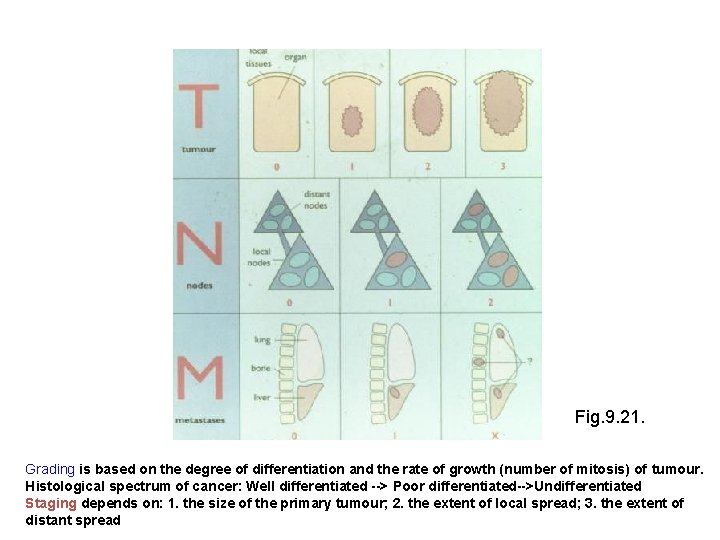
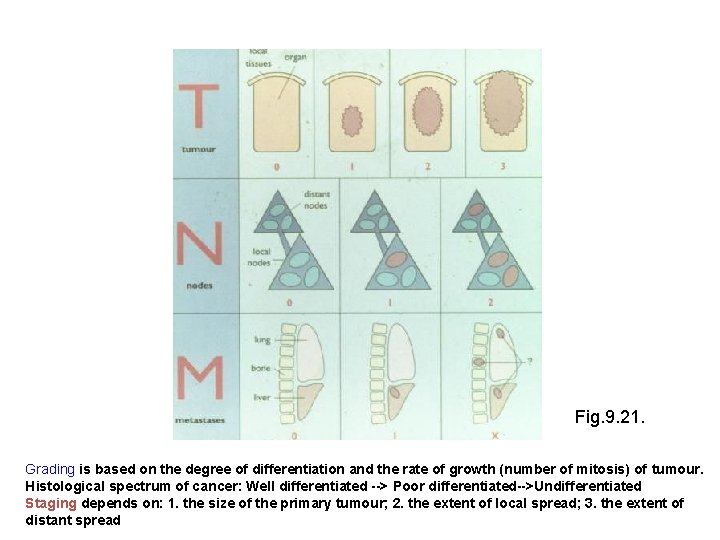
Fig. 9. 21. Grading is based on the degree of differentiation and the rate of growth (number of mitosis) of tumour. Histological spectrum of cancer: Well differentiated --> Poor differentiated-->Undifferentiated Staging depends on: 1. the size of the primary tumour; 2. the extent of local spread; 3. the extent of distant spread
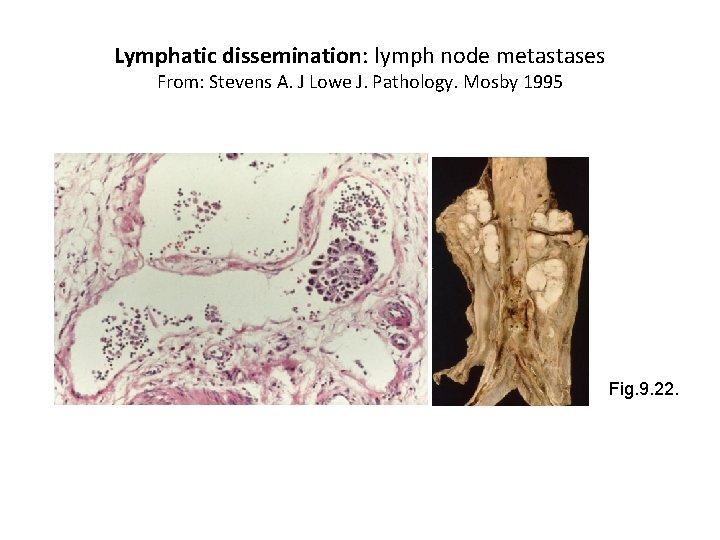
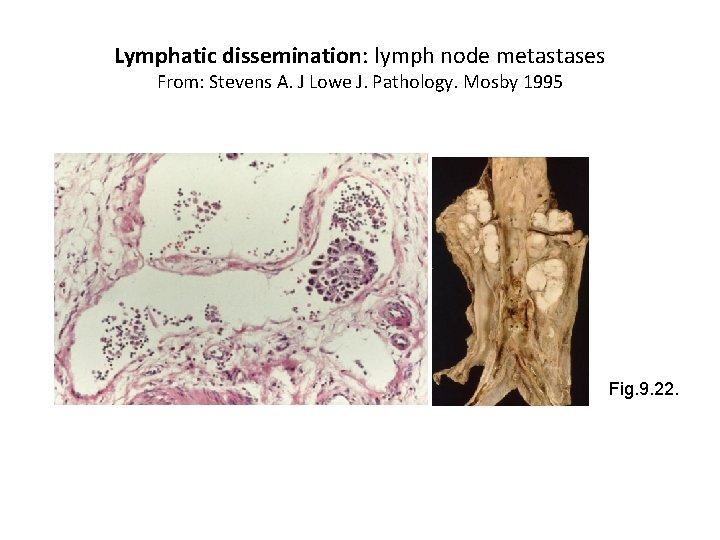
Lymphatic dissemination: lymph node metastases From: Stevens A. J Lowe J. Pathology. Mosby 1995 Fig. 9. 22.
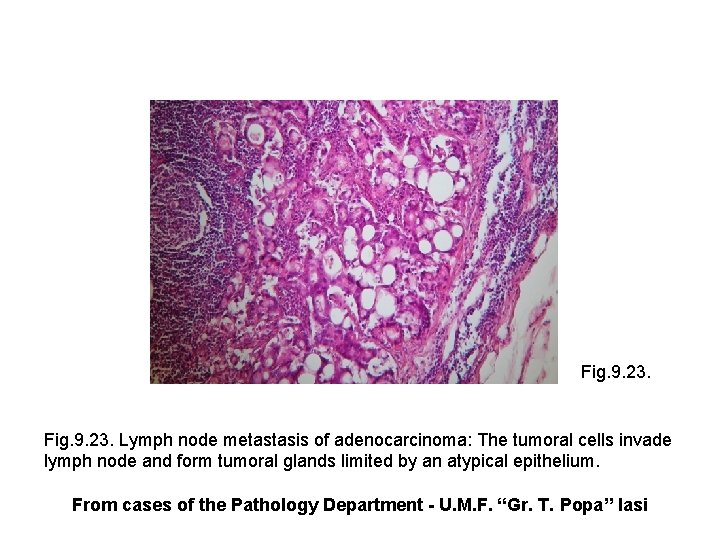
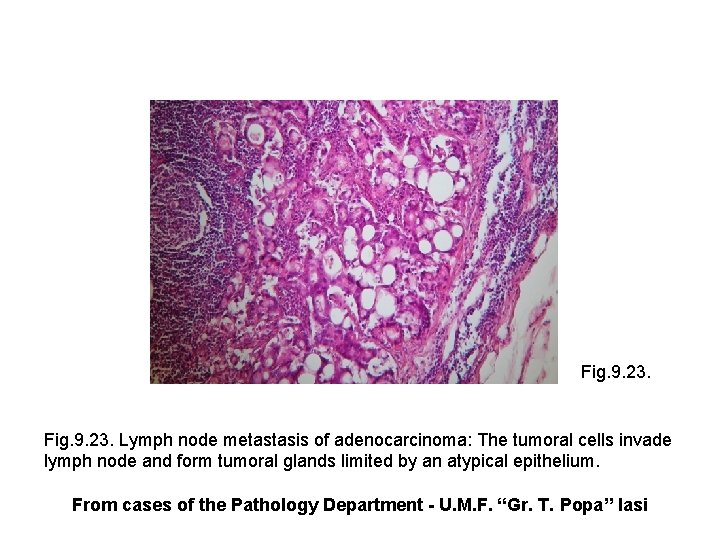
Fig. 9. 23. Lymph node metastasis of adenocarcinoma: The tumoral cells invade lymph node and form tumoral glands limited by an atypical epithelium. From cases of the Pathology Department - U. M. F. “Gr. T. Popa” Iasi
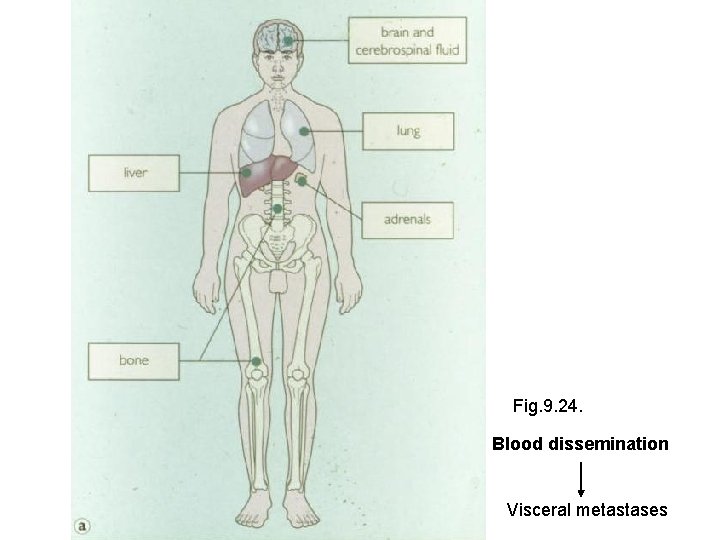
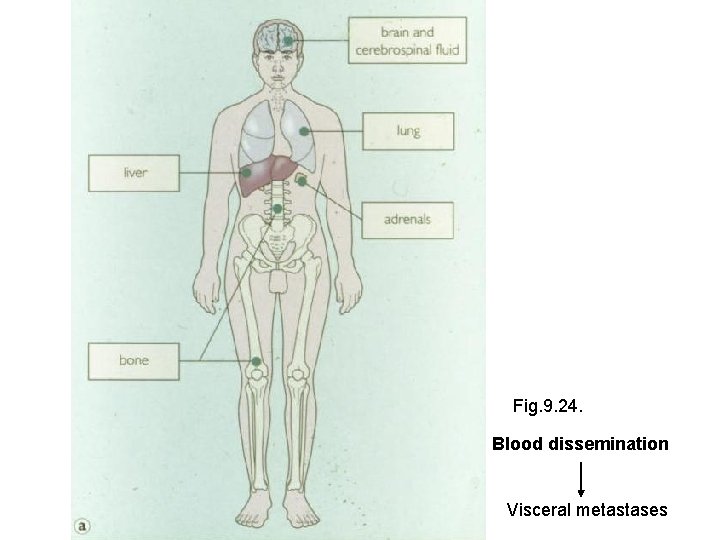
Fig. 9. 24. Blood dissemination Visceral metastases
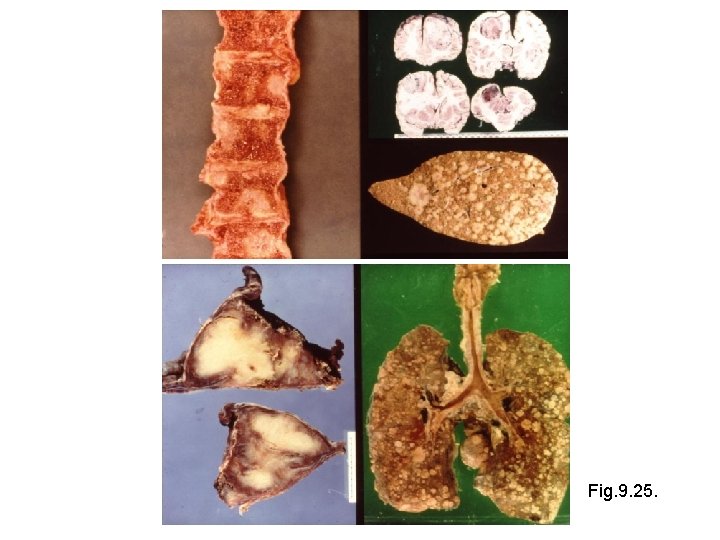
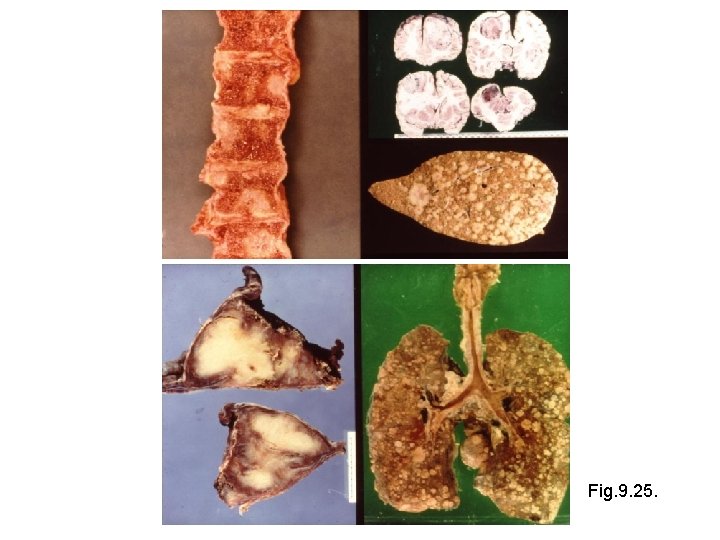
Fig. 9. 25.