Human Anatomy and Physiology Unit 5 Part 2











- Slides: 94
Human Anatomy and Physiology Unit 5, Part 2: The Digestive System
Organization 1. Gastrointestinal tract (alimentary canal) Tube for transit of food during processing. Functional segments include: 2. Mouth, esophagus, stomach, S. I, L. I Accessory structures Contribute to the food processing. Teeth, tongue, salivary glands, liver, gallbladder, and pancreas.

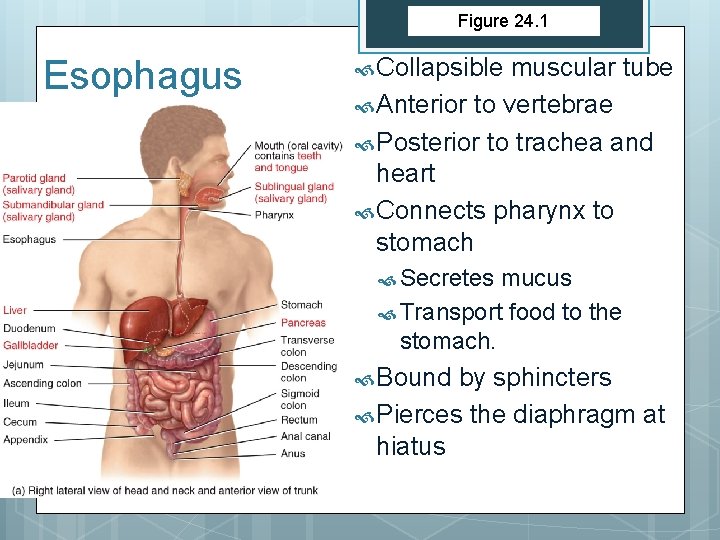
Figure 24. 1 Organs of the Digestive System Important Diagram
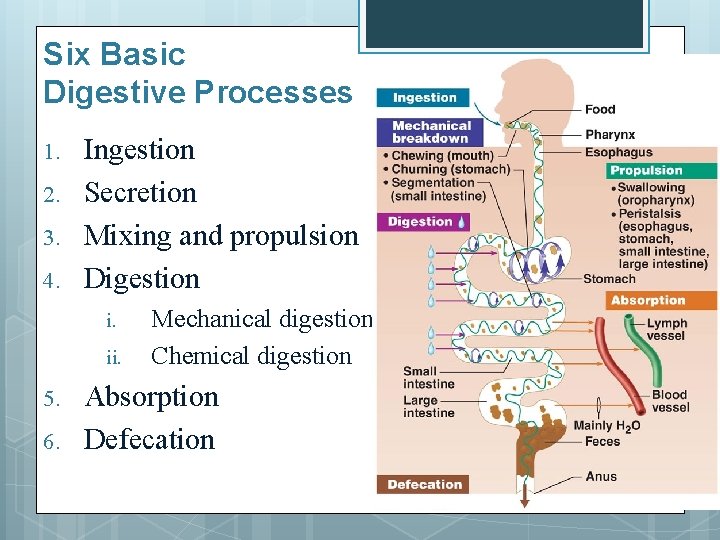
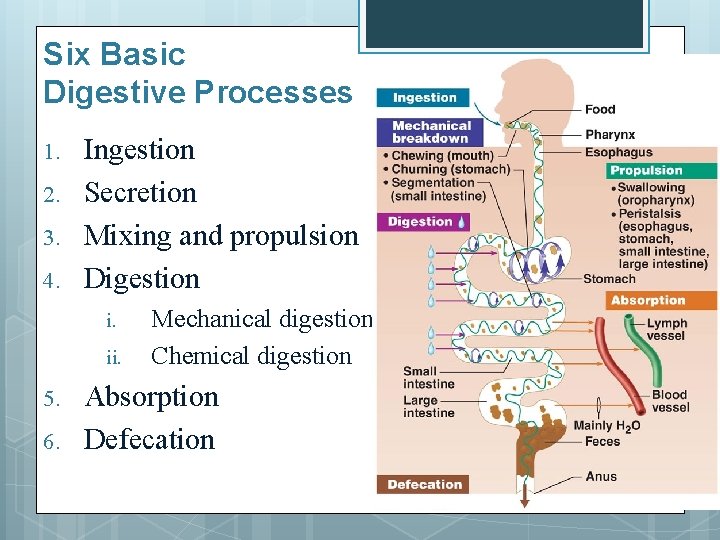
Six Basic Digestive Processes 1. 2. 3. 4. Ingestion Secretion Mixing and propulsion Digestion i. ii. 5. 6. Mechanical digestion Chemical digestion Absorption Defecation
LAYERS OF THE GI TRACT
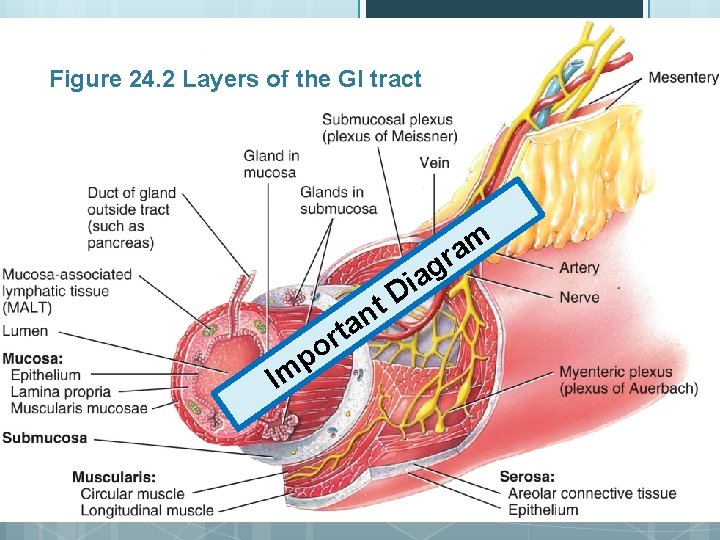
Four Layers of the GI tract 1. Mucosa - innermost 2. Submucosa 3. Muscularis 4. Serosa - outermost
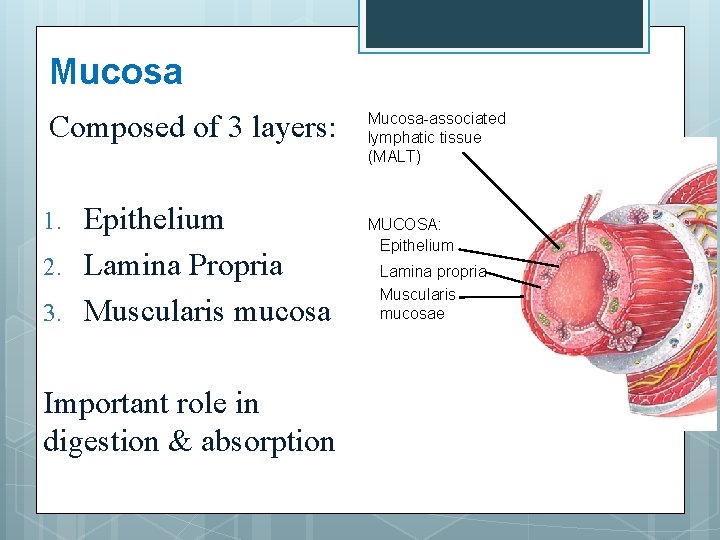
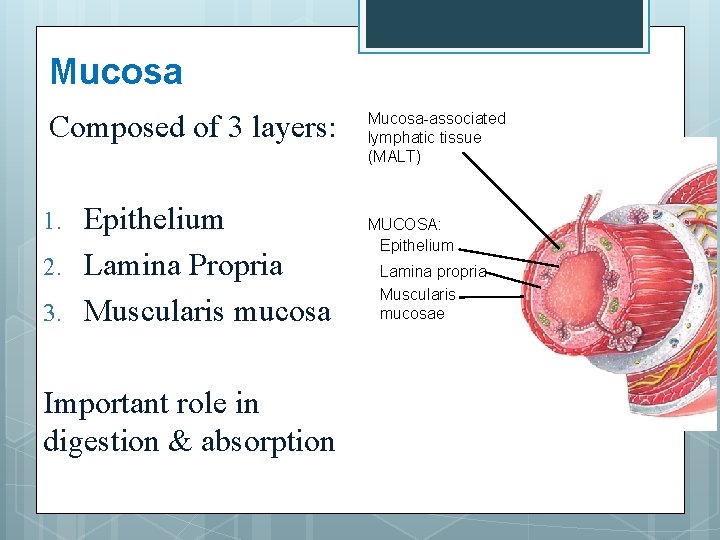
Mucosa Composed of 3 layers: 1. 2. 3. Epithelium Lamina Propria Muscularis mucosa Important role in digestion & absorption Mucosa-associated lymphatic tissue (MALT) MUCOSA: Epithelium Lamina propria Muscularis mucosae
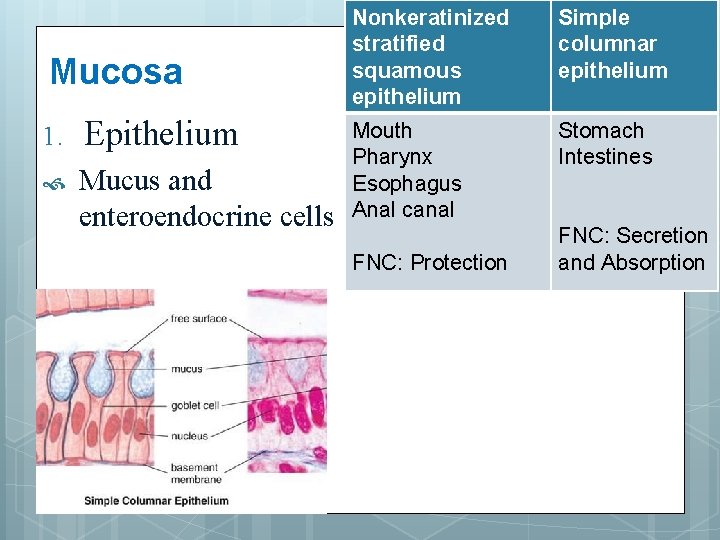
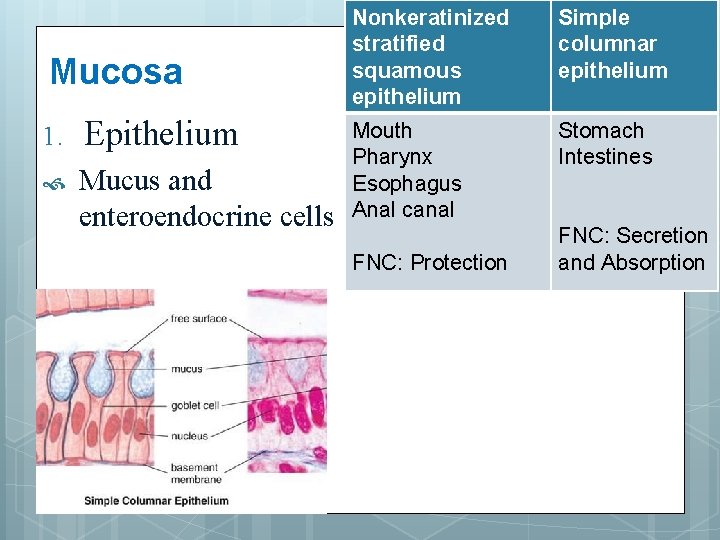
Mucosa 1. Epithelium Mucus and enteroendocrine cells Nonkeratinized stratified squamous epithelium Simple columnar epithelium Mouth Pharynx Esophagus Anal canal Stomach Intestines FNC: Protection FNC: Secretion and Absorption
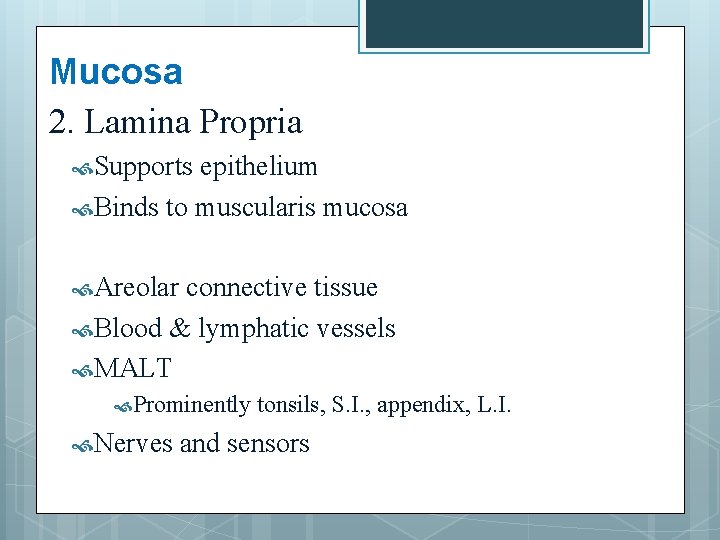
Mucosa 2. Lamina Propria Supports epithelium Binds to muscularis mucosa Areolar connective tissue Blood & lymphatic vessels MALT Prominently Nerves tonsils, S. I. , appendix, L. I. and sensors

Mucosa 3. Muscularis mucosa Smooth muscle Creates folds in stomach and S. I Increases surface area
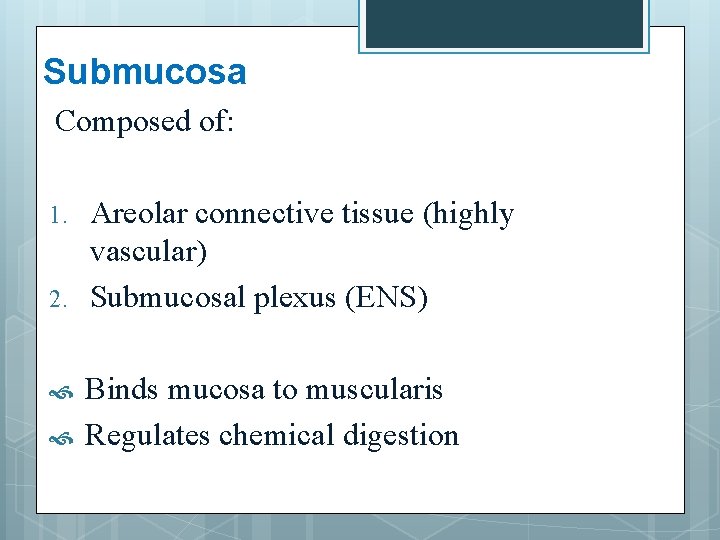
Submucosa Composed of: 1. 2. Areolar connective tissue (highly vascular) Submucosal plexus (ENS) Binds mucosa to muscularis Regulates chemical digestion
Muscularis Skeletal muscle in mouth, pharynx, superior esophagus, and external anal sphincter Rest of GI tract is composed of smooth muscle: 1. Inner circular muscle 2. Outer longitudinal muscle Contains myenteric plexus between (ENS) Important role in mixing and propulsion
Serosa Serous membrane Areolar connective tissue Simple squamous epithelium Esophagus lacks serosa – replaced with adventitia (single layer of loose areolar CT) Inf to diaphragm = Visceral peritoneum Secretes serous fluid
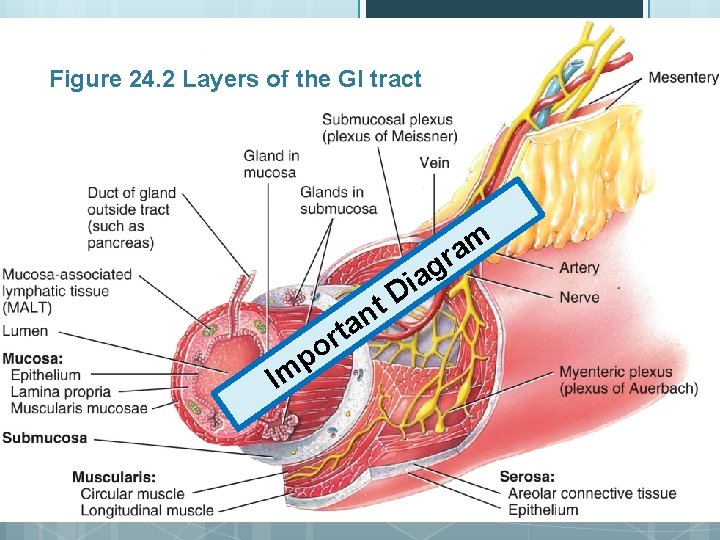
Figure 24. 2 Layers of the GI tract m a gr t n a Im p t r o a i D
NEURAL INNERVATION OF THE GI TRACT
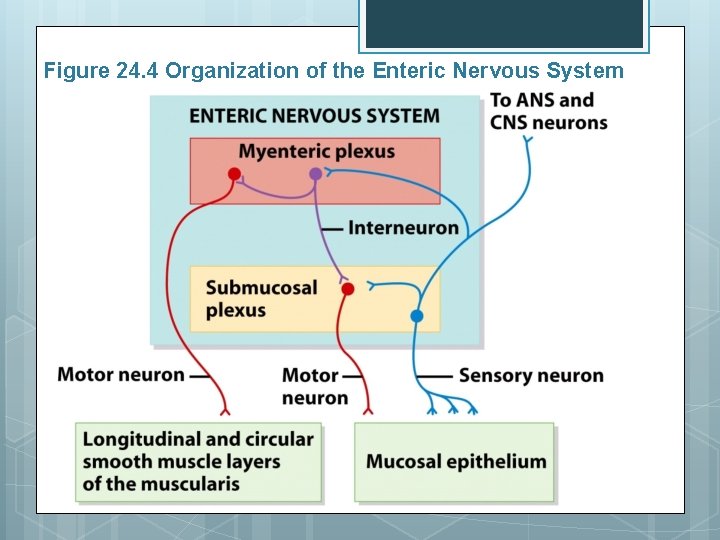
Enteric Nervous System o o Second brain “Brain of the gut. ” Consists of 100 million motor neurons, interneurons, and sensory neurons that extend from the esophagus to the anus. o o Located in sheaths of tissue lining the esophagus, stomach, S. I and colon Neurons arranged into the myenteric plexus and the submucosal plexus.
Enteric Nervous System Submucosal neurons control the secretory cells. Myenteric neurons control gastric motility. Can function independently of the CNS.
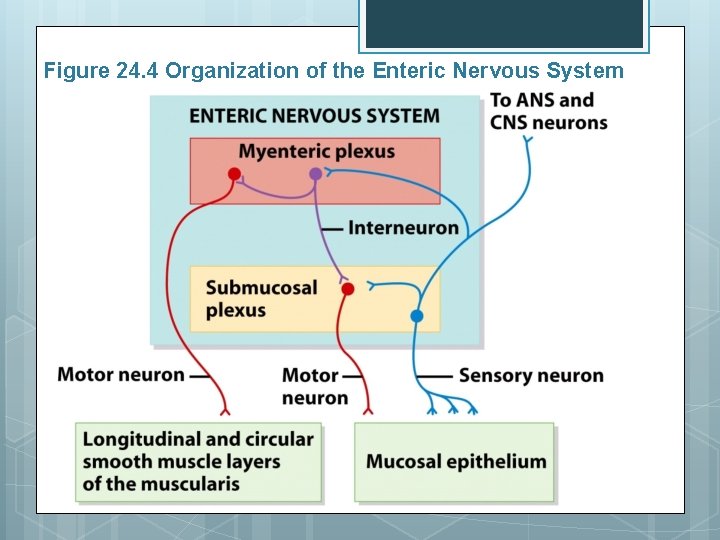
Figure 24. 4 Organization of the Enteric Nervous System
Autonomic Nervous System Vagus nerve (X) parasympathetic fibers stimulate ENS neurons. Stimulate GI secretion and motility Sympathetic nerves (thoracic & upper lumbar regions of SC) inhibit synapse of ENS neurons. Anger, fear and anxiety slow digestion
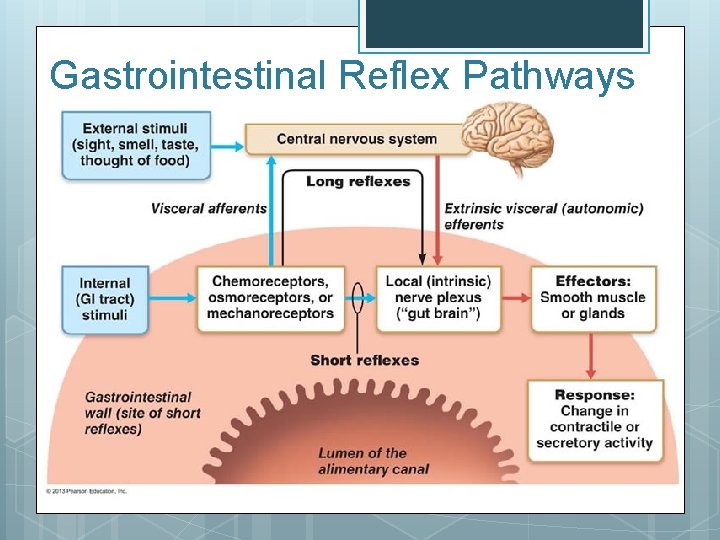
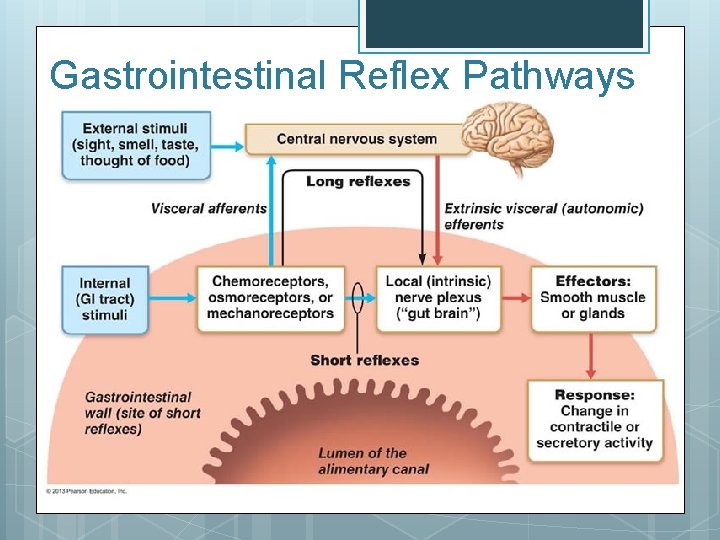
Gastrointestinal Reflex Pathways Regulate secretions and motility in response to stimuli present in the lumen. Reflexes begin with receptors associated with sensory neurons of the ENS, CNS, and ANS can modulate reflexes.
Sensory Receptors in G. I Tract Chemoreceptors Mechanoreceptors Controls of the digestive activity are both extrinsic and intrinsic (nervous and hormonal)
Gastrointestinal Reflex Pathways
PERITONEUM
Key Terms Serous Membrane - Smooth, transparent, two-layered membrane that lines internal cavities of the body, lubricated by a fluid derived from serum. Mesothelium. Peritoneum – body’s largest serous membrane Parietal peritoneum – lines abdominal wall Visceral peritoneum - covers most abdominal organs (serosa); some organs (kidneys, pancreas) are retroperitoneal Peritoneal cavity - potential space between parietal and visceral peritoneum; contains serous fluid.
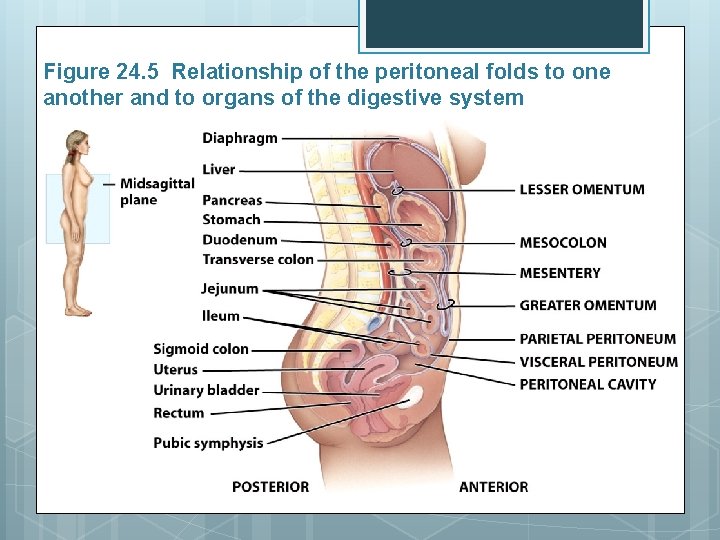
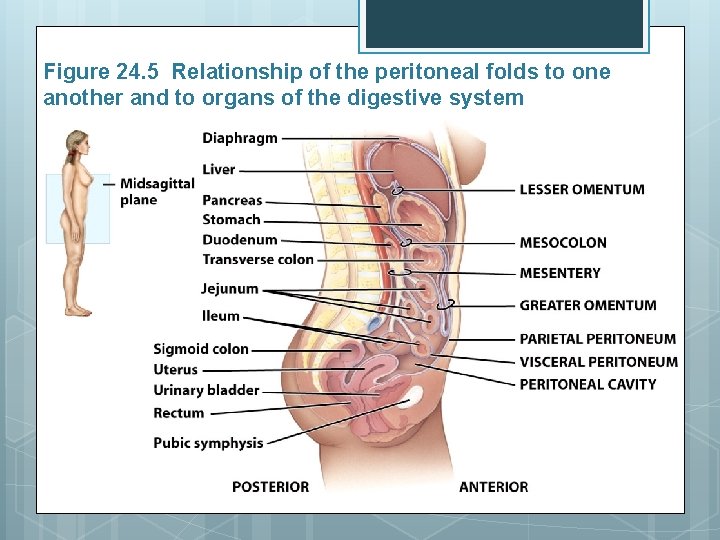
Figure 24. 5 Relationship of the peritoneal folds to one another and to organs of the digestive system

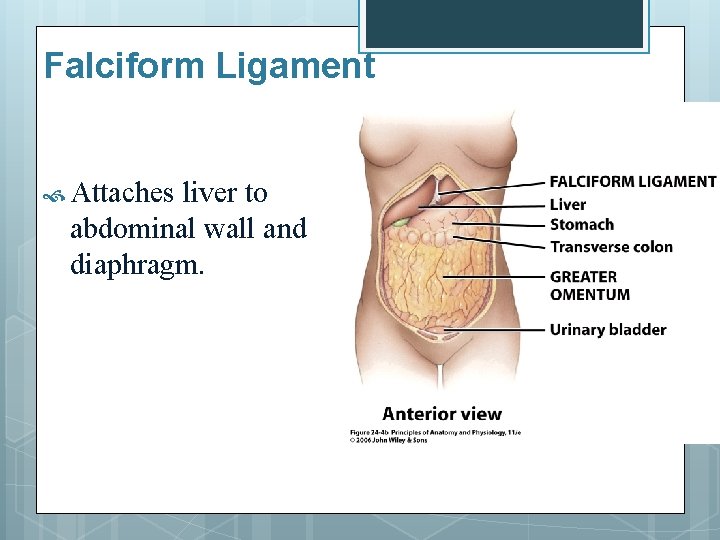
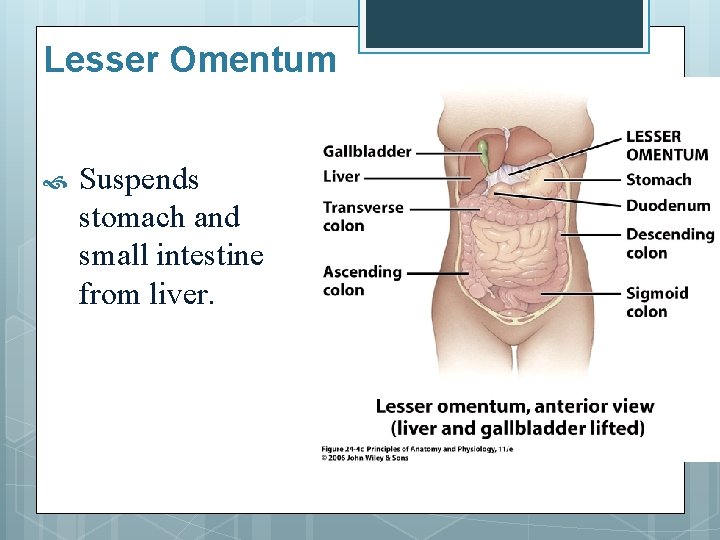
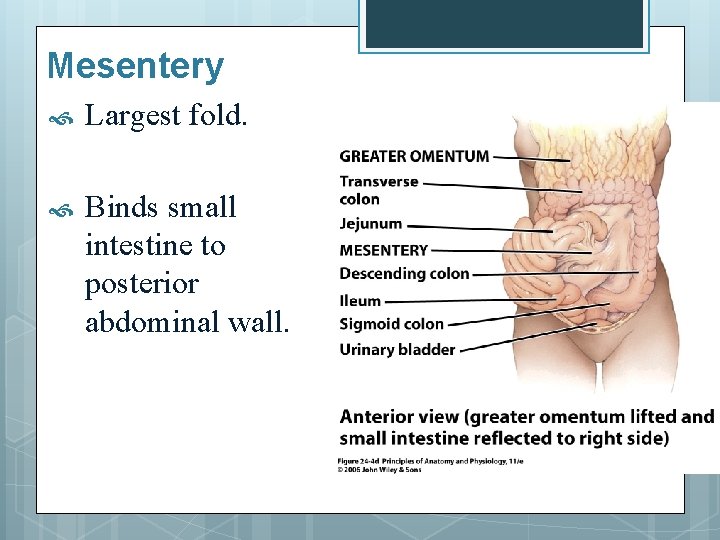
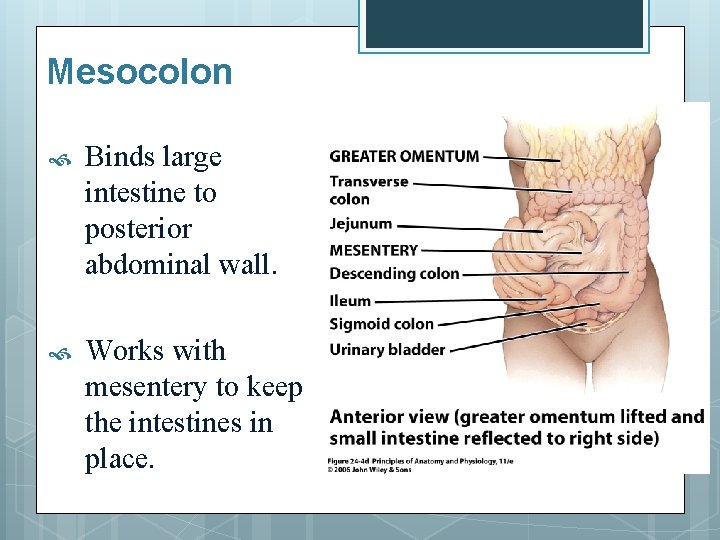
Main extensions of the peritoneum 1. 2. 3. 4. 5. Greater omentum Falciform ligament Lesser omentum Mesentery Mesocolon
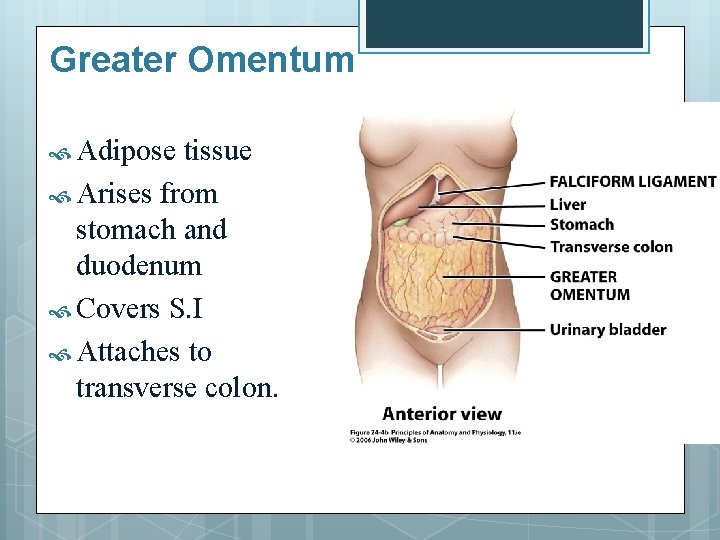
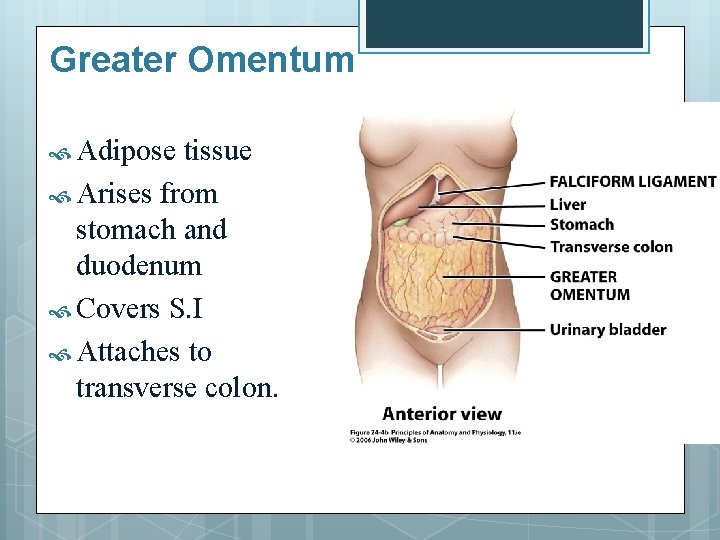
Greater Omentum Adipose tissue Arises from stomach and duodenum Covers S. I Attaches to transverse colon.
Falciform Ligament Attaches liver to abdominal wall and diaphragm.
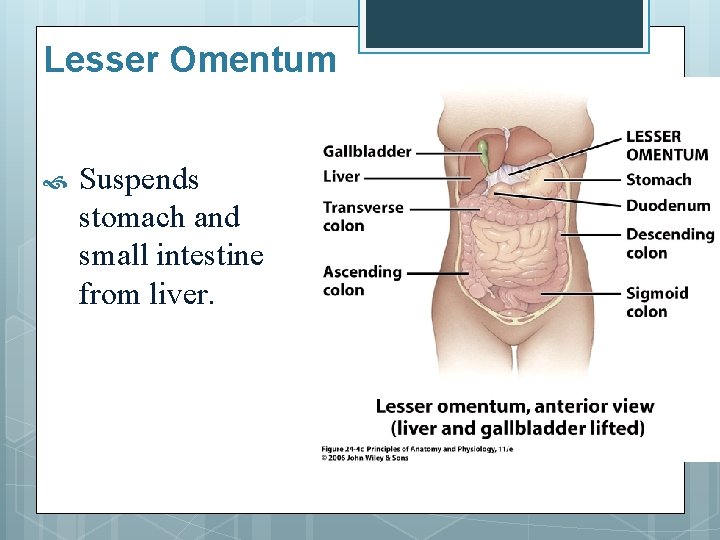
Lesser Omentum Suspends stomach and small intestine from liver.
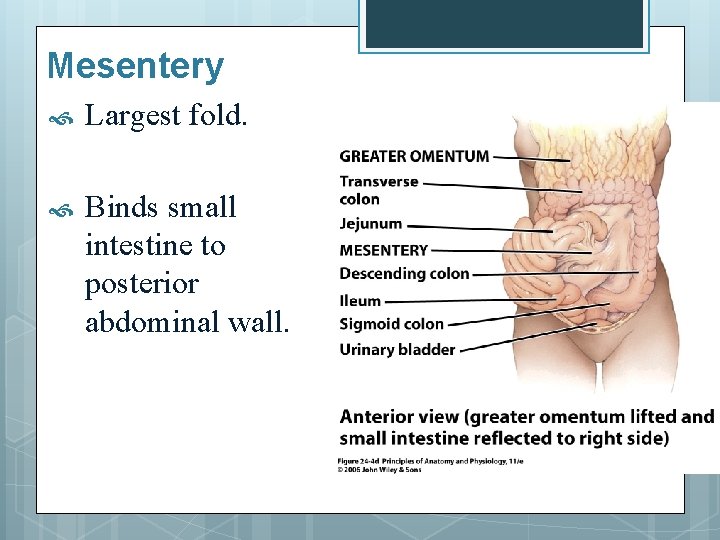
Mesentery Largest fold. Binds small intestine to posterior abdominal wall.
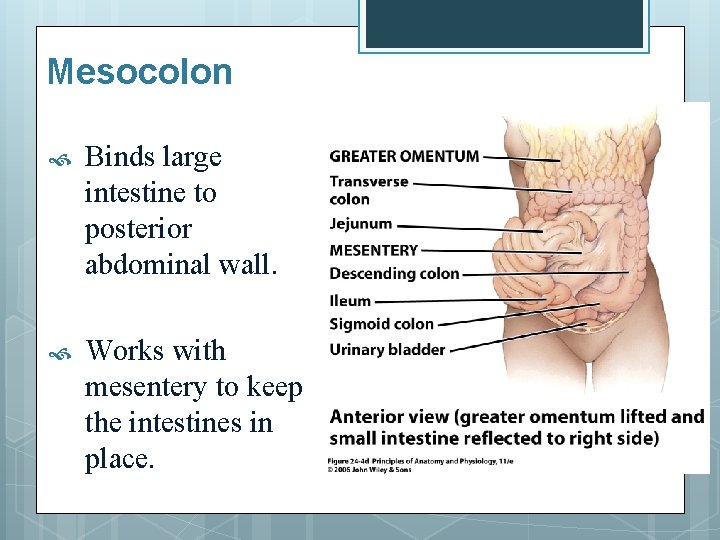
Mesocolon Binds large intestine to posterior abdominal wall. Works with mesentery to keep the intestines in place.
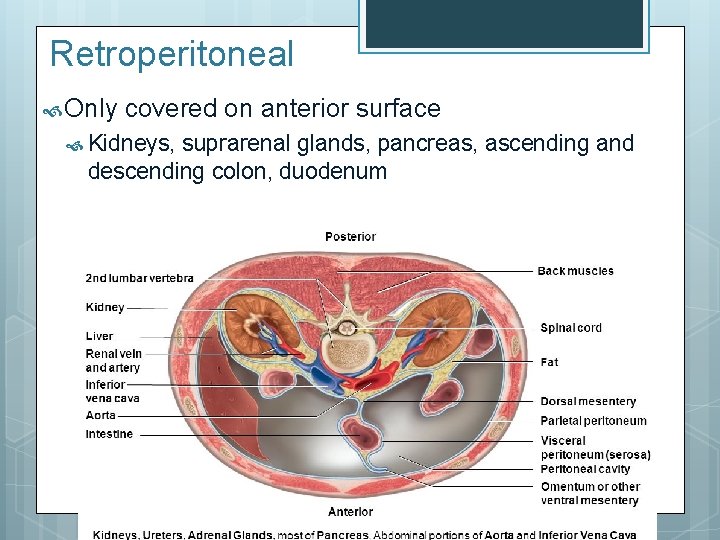
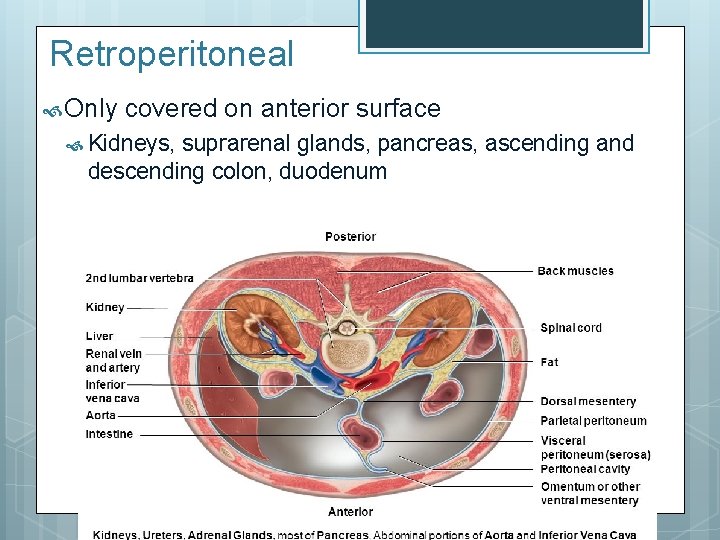
Retroperitoneal Only covered on anterior surface Kidneys, suprarenal glands, pancreas, ascending and descending colon, duodenum
MOUTH
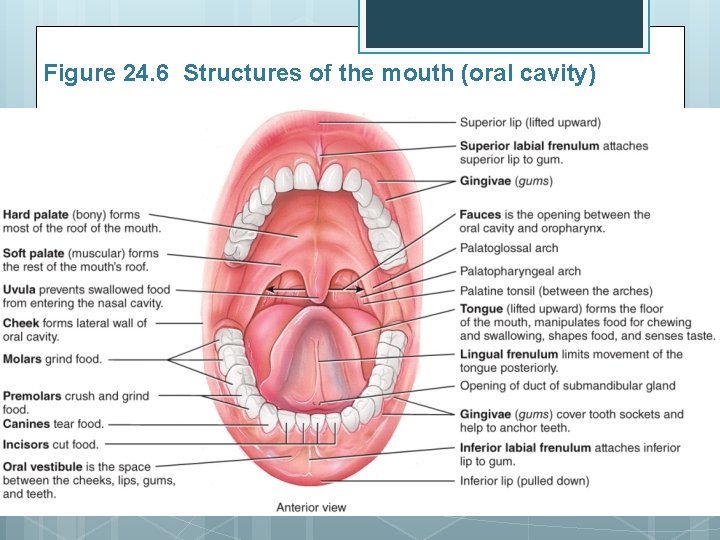
Mouth (oral or buccal cavity) Cheeks, hard & soft palate, lips, tongue. Covered externally by skin. Covered internally by mucous membrane.
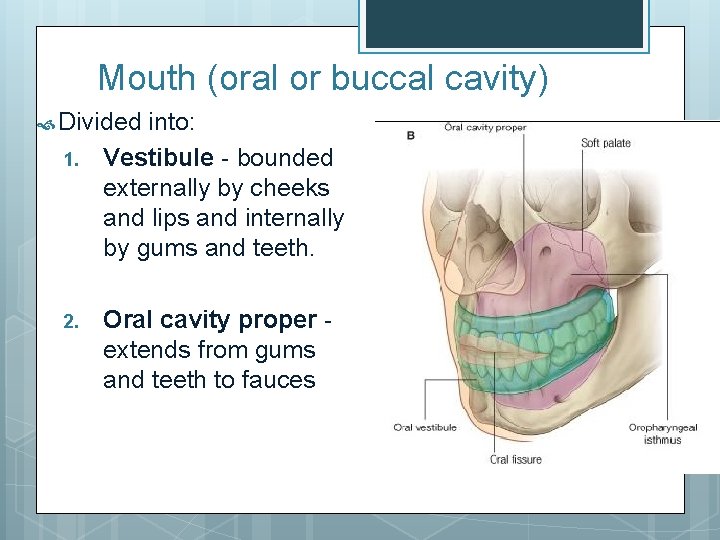
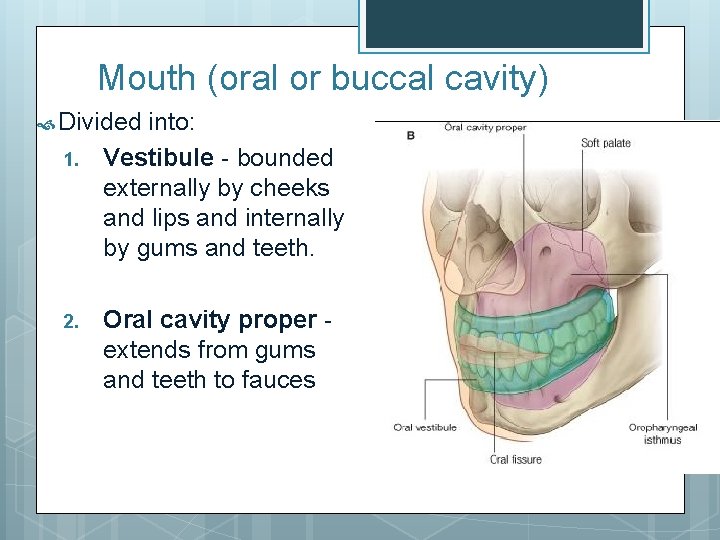
Mouth (oral or buccal cavity) Divided 1. 2. into: Vestibule - bounded externally by cheeks and lips and internally by gums and teeth. Oral cavity proper extends from gums and teeth to fauces
Cheeks – contain buccinator muscles Lips (labia) – contain orbicularis oris muscles; attached to gum by labial frenulum Lips and cheeks keep food between teeth and assist in speech. Uvula – muscular structure hanging at the back of the throat; blocks nasopharyngeal opening during swallowing
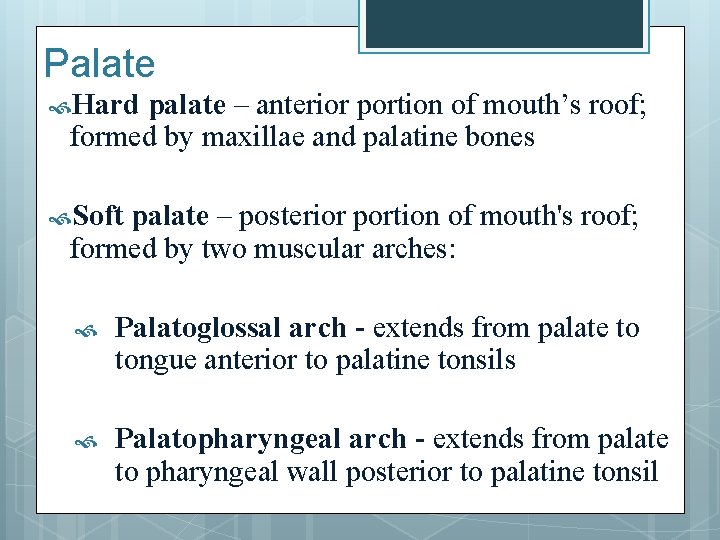
Palate Hard palate – anterior portion of mouth’s roof; formed by maxillae and palatine bones Soft palate – posterior portion of mouth's roof; formed by two muscular arches: Palatoglossal arch - extends from palate to tongue anterior to palatine tonsils Palatopharyngeal arch - extends from palate to pharyngeal wall posterior to palatine tonsil

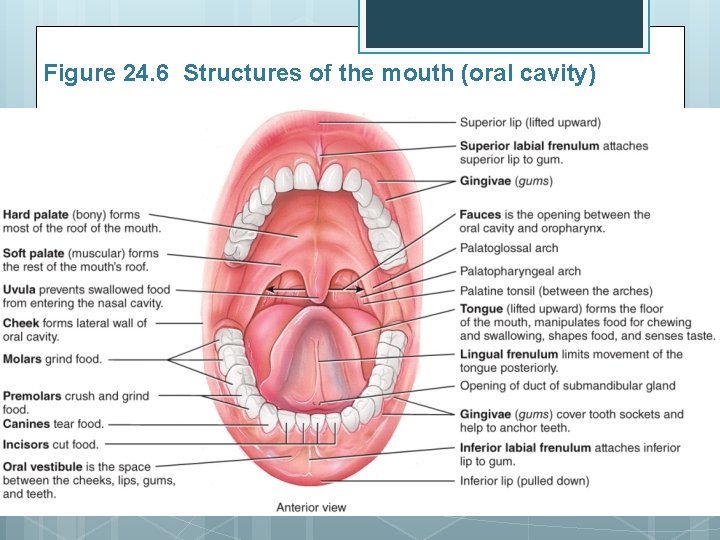
Figure 24. 6 Structures of the mouth (oral cavity)
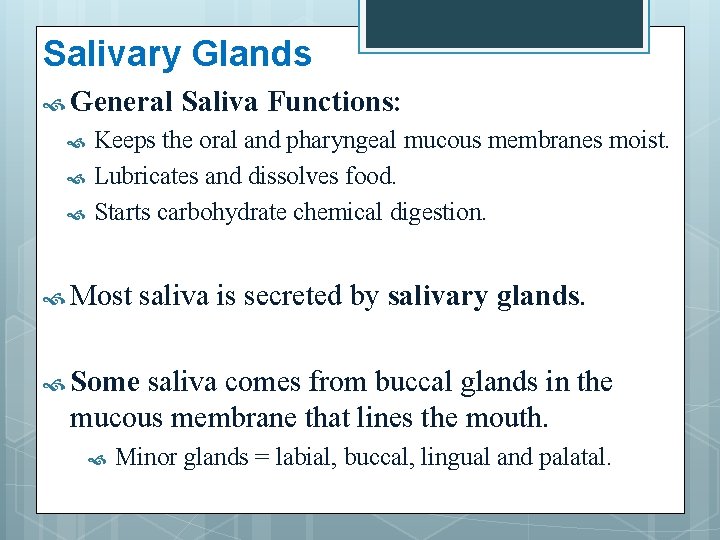
Salivary Glands General Saliva Functions: Keeps the oral and pharyngeal mucous membranes moist. Lubricates and dissolves food. Starts carbohydrate chemical digestion. Most saliva is secreted by salivary glands. Some saliva comes from buccal glands in the mucous membrane that lines the mouth. Minor glands = labial, buccal, lingual and palatal.
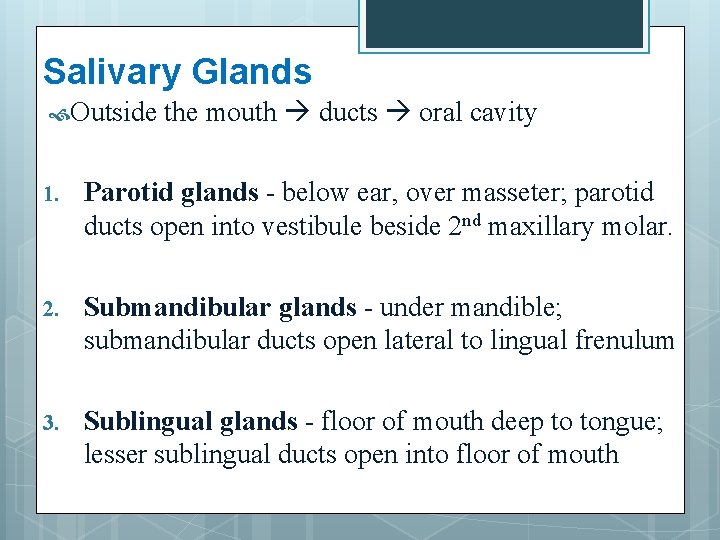
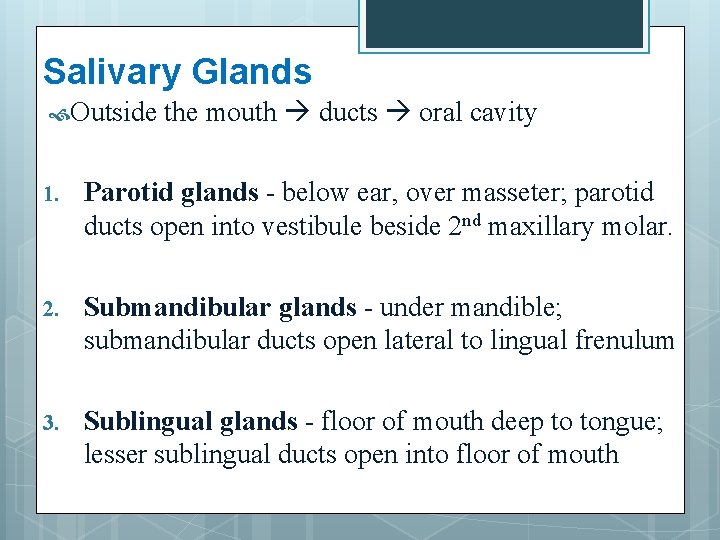
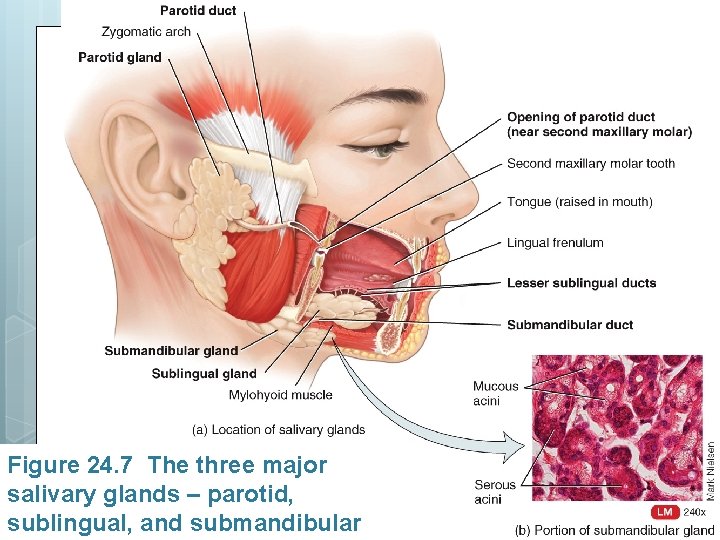
Salivary Glands Outside the mouth ducts oral cavity 1. Parotid glands - below ear, over masseter; parotid ducts open into vestibule beside 2 nd maxillary molar. 2. Submandibular glands - under mandible; submandibular ducts open lateral to lingual frenulum 3. Sublingual glands - floor of mouth deep to tongue; lesser sublingual ducts open into floor of mouth
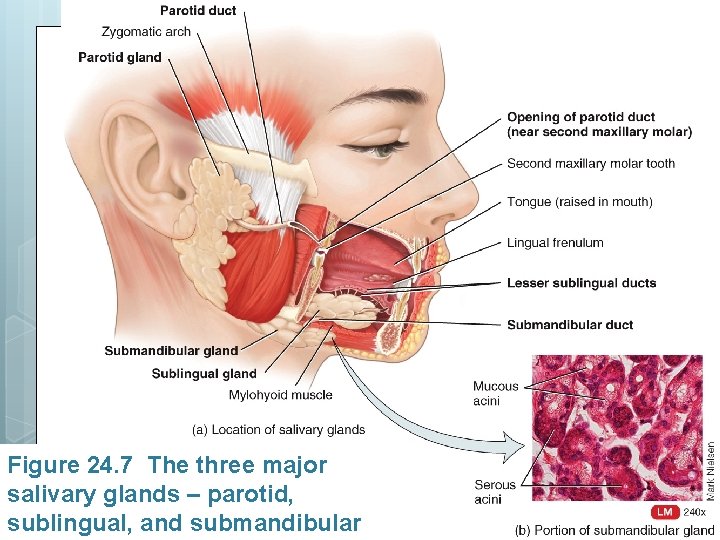
Figure 24. 7 The three major salivary glands – parotid, sublingual, and submandibular
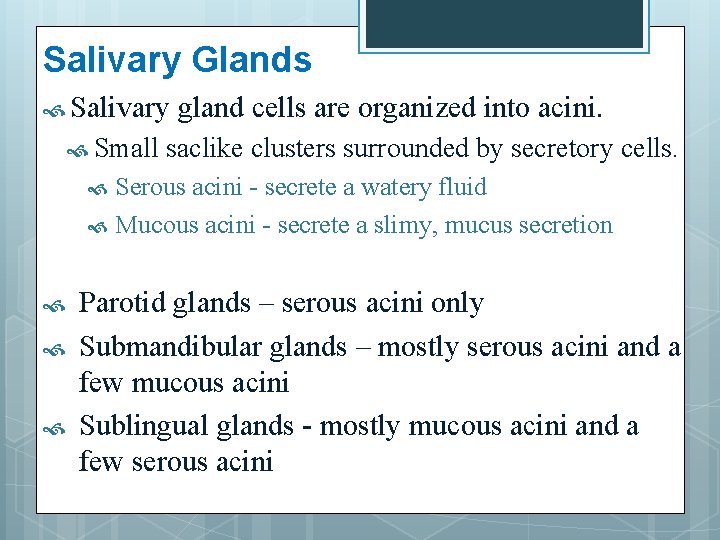
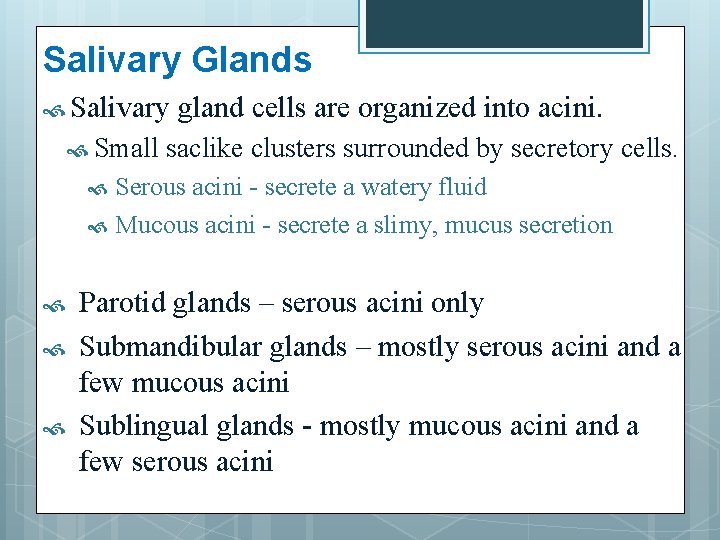
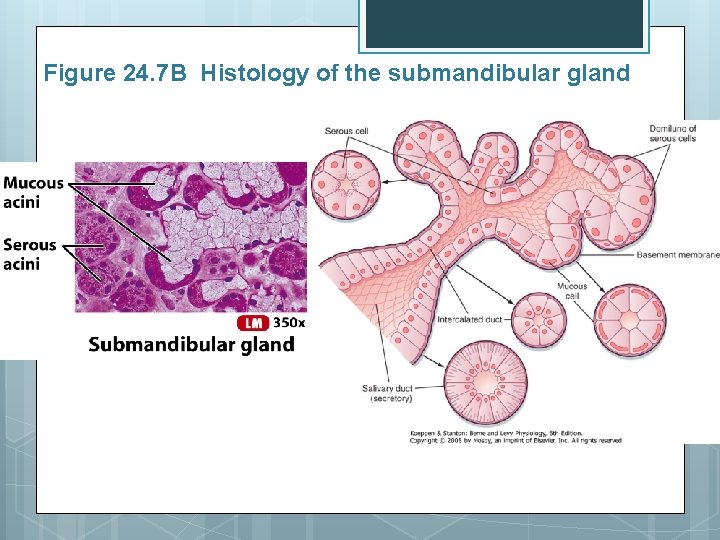
Salivary Glands Salivary Small gland cells are organized into acini. saclike clusters surrounded by secretory cells. Serous acini - secrete a watery fluid Mucous acini - secrete a slimy, mucus secretion Parotid glands – serous acini only Submandibular glands – mostly serous acini and a few mucous acini Sublingual glands - mostly mucous acini and a few serous acini
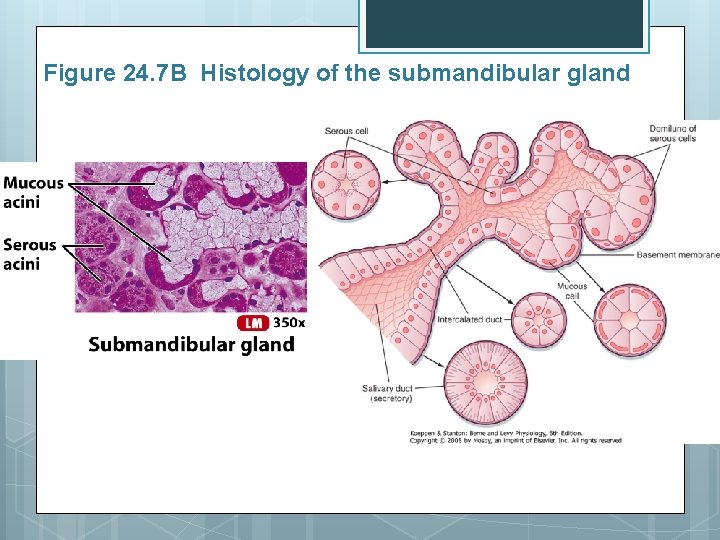
Figure 24. 7 B Histology of the submandibular gland
Composition and Functions of Saliva Composition: 1. 2. 99. 5% water 0. 5% solutes (salts, gases, mucous, ions, enzymes, lysozyme, Ig. A) Functions: 1. 2. 3. 4. 5. 6. 7. 8. Lubricate food Dissolve food for tasting Moistens mucous membranes Bicarbonate ions buffer acidic foods Waste removal – urea + uric acid Salivary amylase begins chemical digestion of starch (maltose) Lysozyme antibacterial Ig. A 1 st line of defense
Salivation Secretion Moisten mucous membranes Speech Reabsorption Dehydration ANS control
Salivation 1. Increase salivation Sight, smell, sounds, thoughts/memory. Tongue stimulation Salivatory nuclei increase salivation Parasympathetic Facial 2. fibers in CN VII & CN IX nerve impulses stimulate saliva (VII) and glossopharyngeal (IX) nerves. Stop salivation Sympathetic nerves inhibit salivation
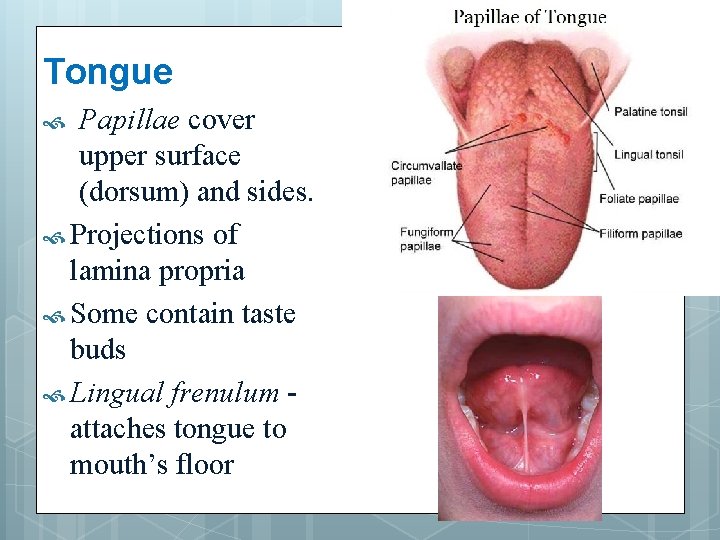
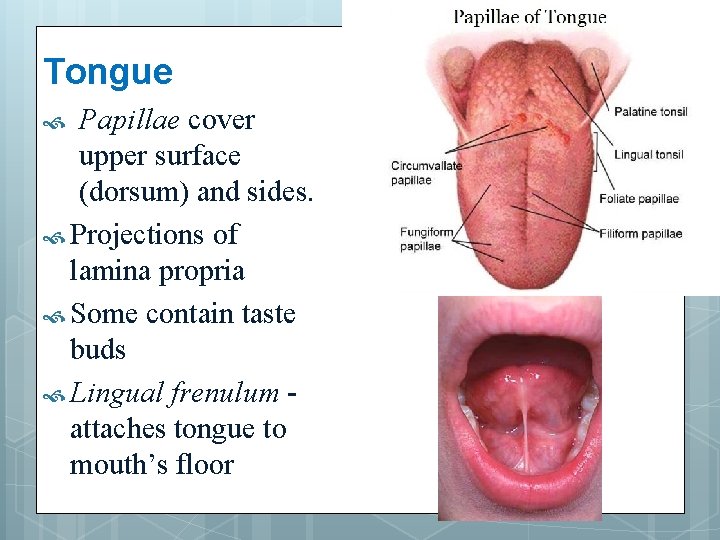
Tongue Papillae cover upper surface (dorsum) and sides. Projections of lamina propria Some contain taste buds Lingual frenulum attaches tongue to mouth’s floor
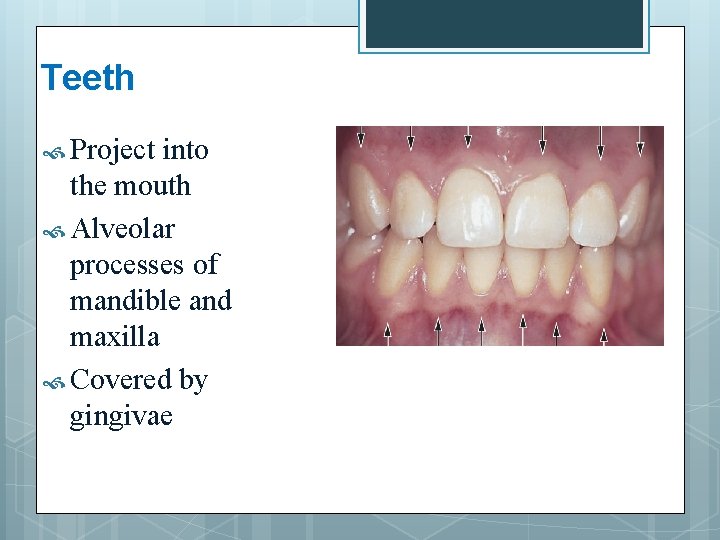
Teeth Project into the mouth Alveolar processes of mandible and maxilla Covered by gingivae
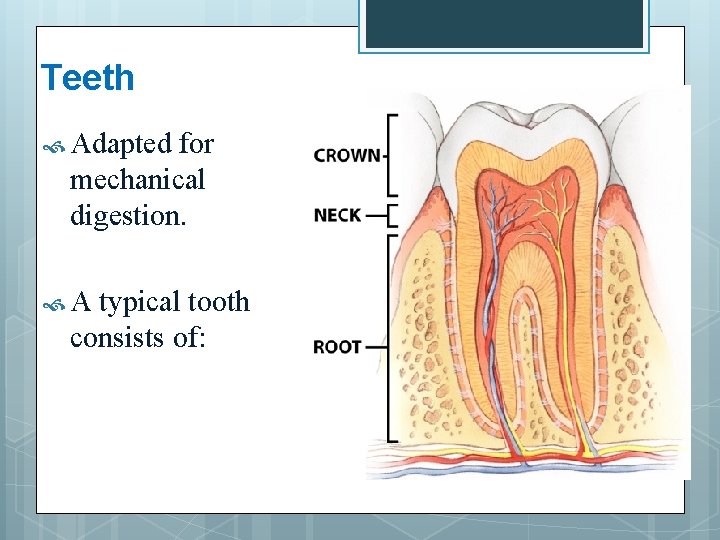
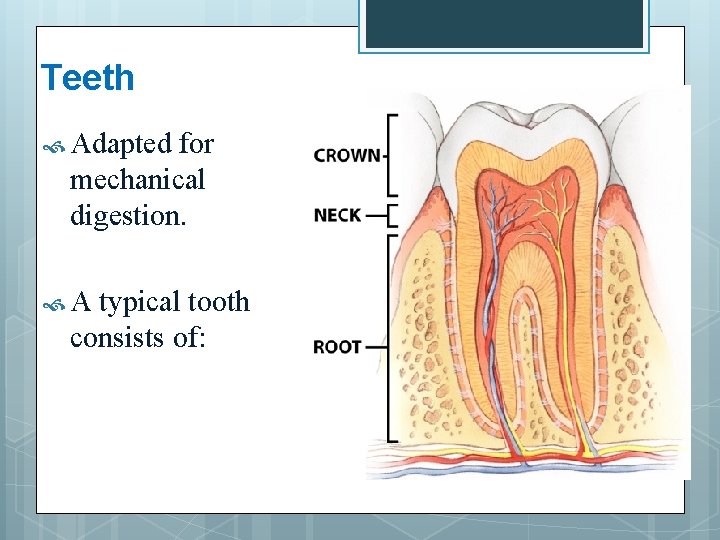
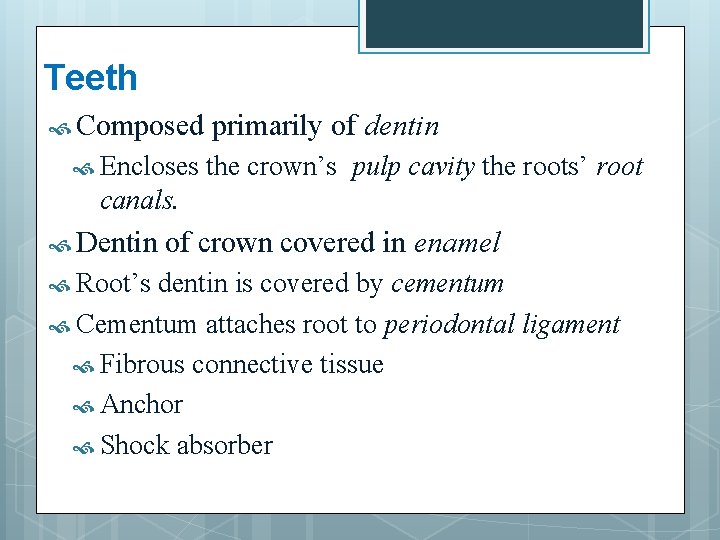
Teeth Adapted for mechanical digestion. A typical tooth consists of:
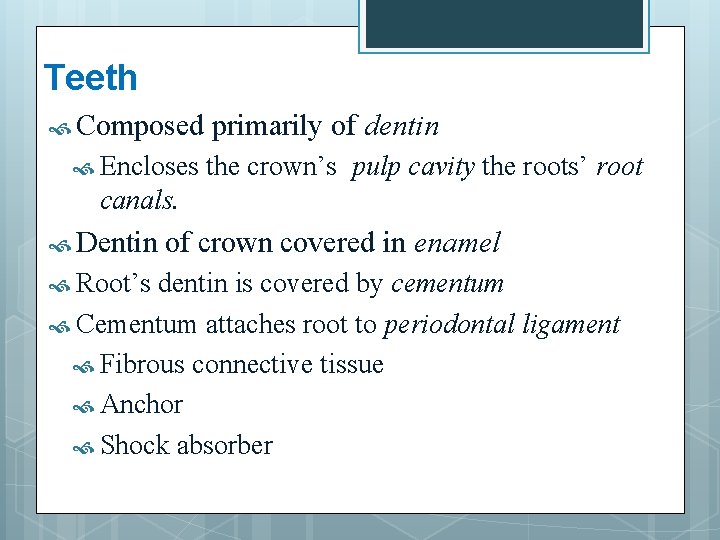
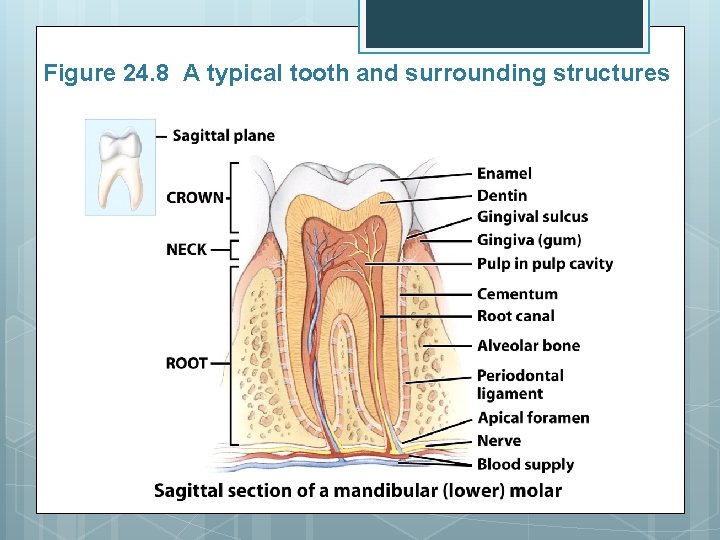
Teeth Composed Encloses primarily of dentin the crown’s pulp cavity the roots’ root canals. Dentin Root’s of crown covered in enamel dentin is covered by cementum Cementum attaches root to periodontal ligament Fibrous connective tissue Anchor Shock absorber
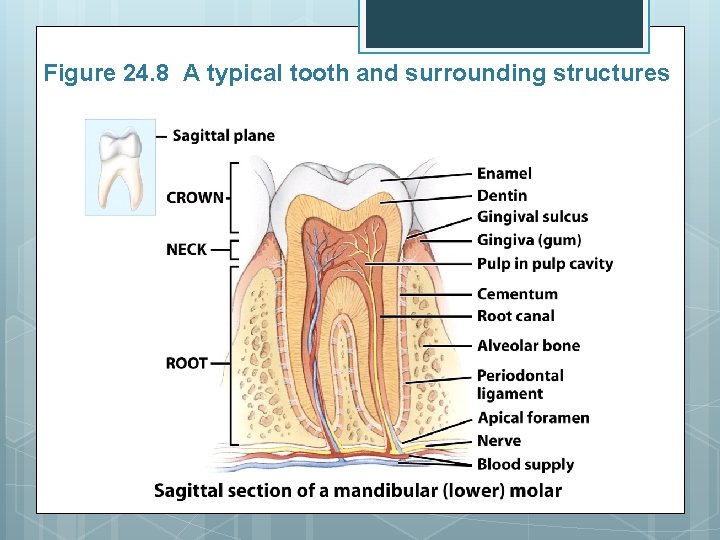
Figure 24. 8 A typical tooth and surrounding structures
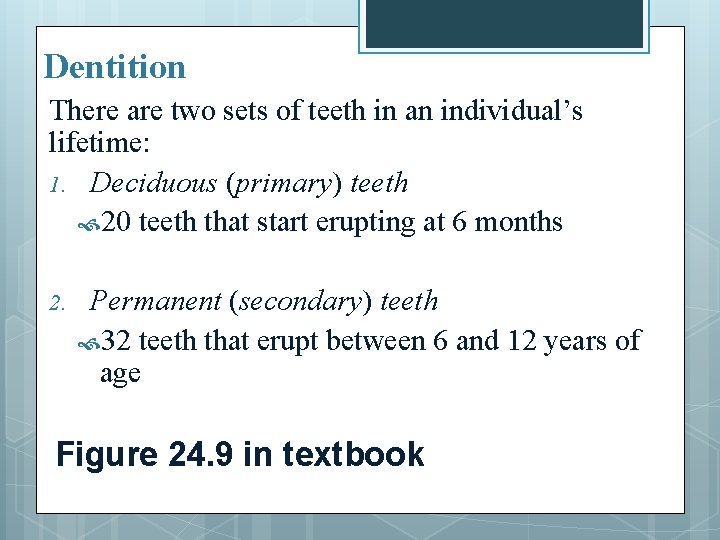
Dentition There are two sets of teeth in an individual’s lifetime: 1. Deciduous (primary) teeth 20 teeth that start erupting at 6 months 2. Permanent (secondary) teeth 32 teeth that erupt between 6 and 12 years of age Figure 24. 9 in textbook
Tooth Types 1. Incisors – chisel shaped; cutting 2. Cuspids (canines) – pointed; tearing 3. Premolars – bicuspid; crushing and grinding 4. Molars – four cusps; crushing and grinding
Digestion in the Mouth Mechanical digestion (mastication or chewing) Mixes with saliva bolus Chemical digestion Amylase Begins starch digestion at p. H of 6. 5 or 7. 0 When bolus & enzymes hit the p. H of 2. 5 (gastric juices), hydrolysis ceases Lingual lipase Secreted by glands in tongue Begins breakdown of triglycerides once it reaches the acidic p. H in the stomach
Look at Table 24. 1

PHARYNX
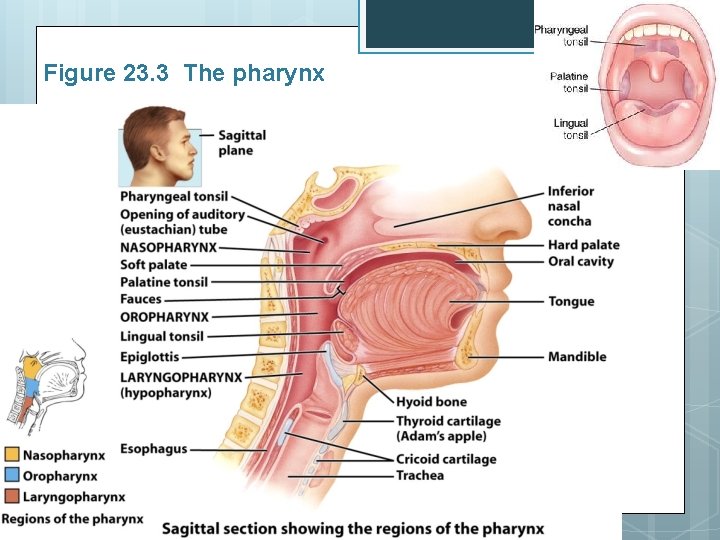
Pharynx Figures 23. 3 / 24. 11 Funnel-shaped tube Internal nares esophagus and larynx Skeletal muscle + mucous membrane 3 parts: Nasopharynx – respiratory Oropharynx – digestive & respiratory Laryngopharynx – digestive & respiratory
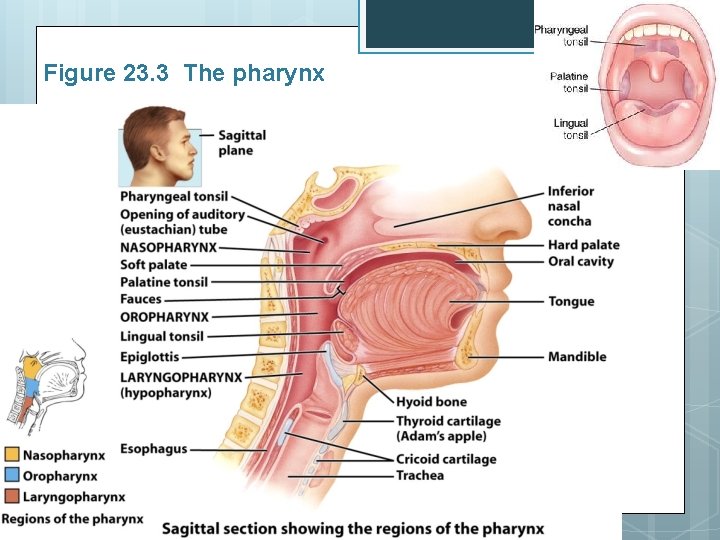
Figure 23. 3 The pharynx
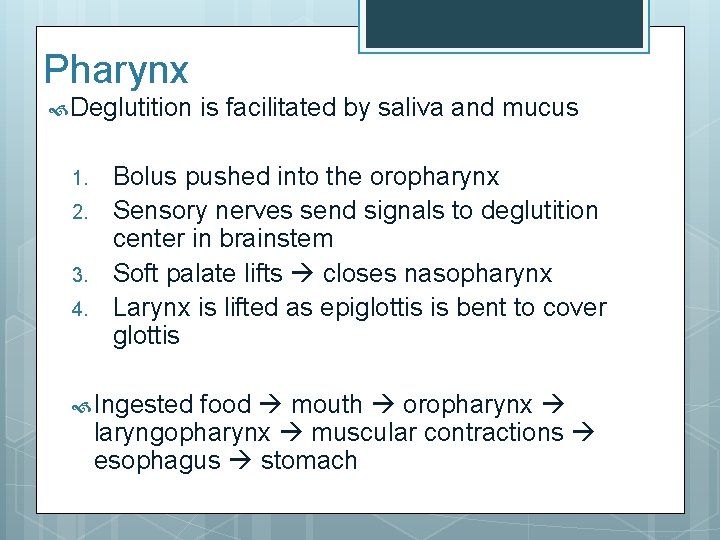
Pharynx Deglutition 1. 2. 3. 4. is facilitated by saliva and mucus Bolus pushed into the oropharynx Sensory nerves send signals to deglutition center in brainstem Soft palate lifts closes nasopharynx Larynx is lifted as epiglottis is bent to cover glottis Ingested food mouth oropharynx laryngopharynx muscular contractions esophagus stomach
ESOPHAGUS
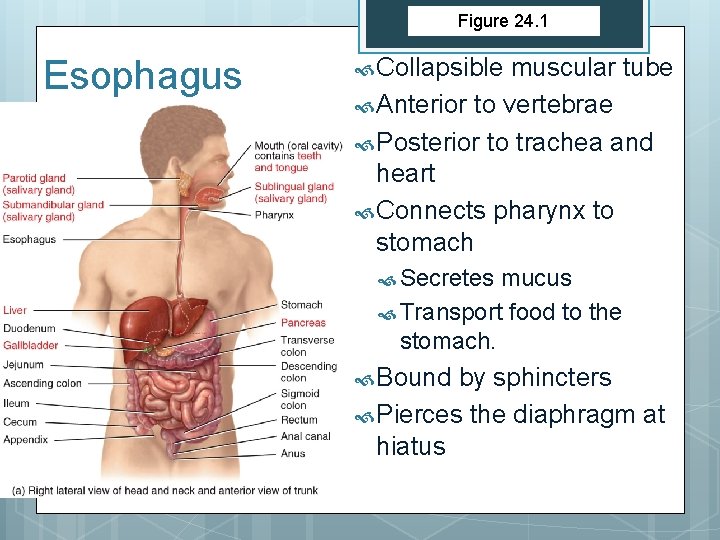
Figure 24. 1 Esophagus Collapsible muscular tube Anterior to vertebrae Posterior to trachea and heart Connects pharynx to stomach Secretes mucus Transport food to the stomach. Bound by sphincters Pierces the diaphragm at hiatus

Histology of the Esophagus Wall has 3 layers: Mucosa Protection Normal 3 layers (NKSSE, LP, MM) Mucous glands Submucosa ACT, BV and large mucous glands Muscularis Upper 1/3 is skeletal Middle is mixed Lower 1/3 is smooth Upper & lower esophageal sphincters are prominent circular muscle Figure 24. 10 Skeletal and smooth
Histology of the Esophagus Adventitia Outermost layer of CT Blends with surrounding connective tissue No peritoneum Differences from serosa Serosa lubrication secretions Adventitia binds structures no secretions

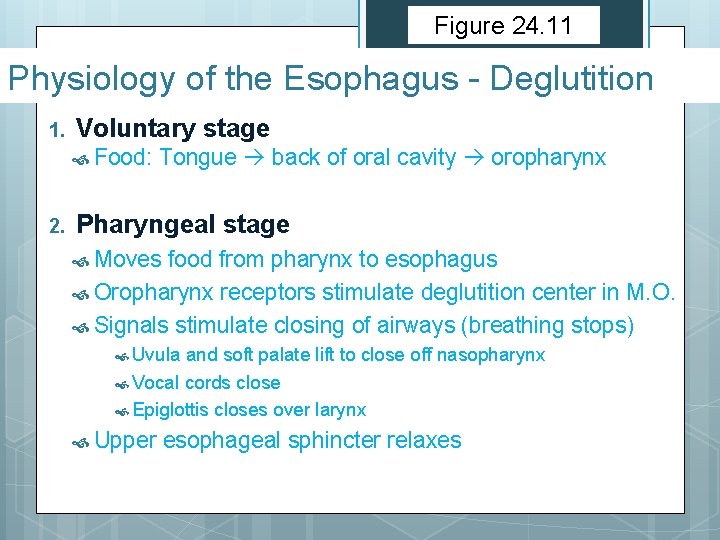
Figure 24. 11 Physiology of the Esophagus - Deglutition Moves bolus from the mouth to the stomach. Mouth, Saliva 3 tongue, pharynx, esophagus and mucus. stages: 1. Voluntary stage 2. Pharyngeal stage 3. Esophageal stage
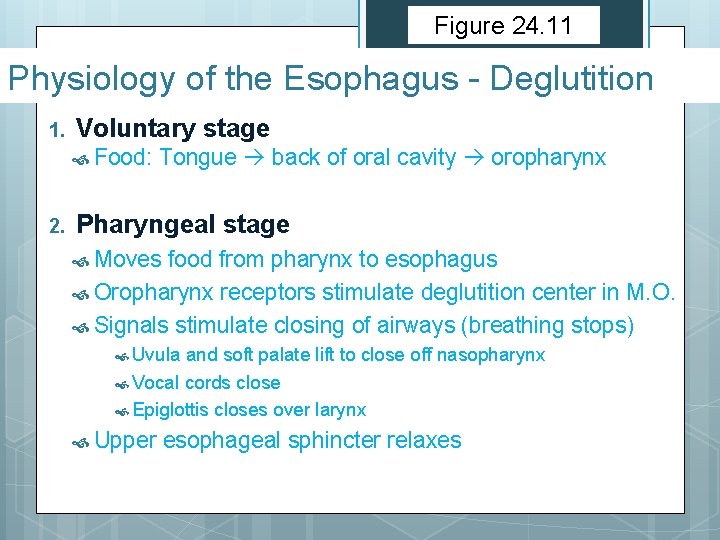
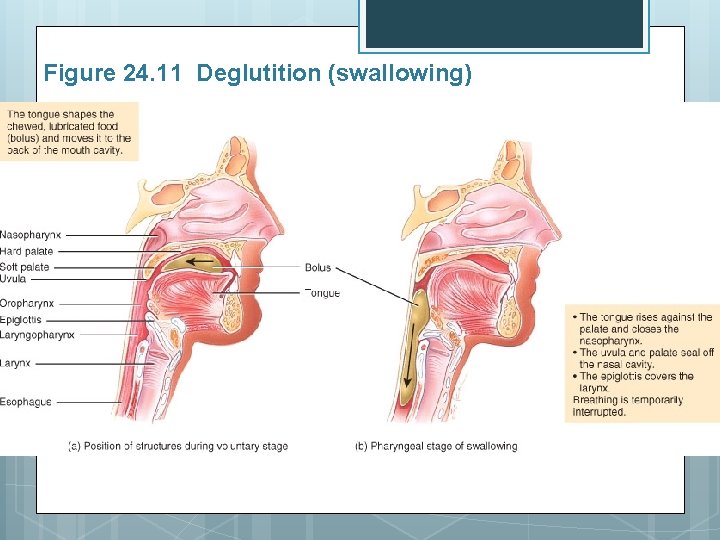
Figure 24. 11 Physiology of the Esophagus - Deglutition 1. Voluntary stage Food: 2. Tongue back of oral cavity oropharynx Pharyngeal stage Moves food from pharynx to esophagus Oropharynx receptors stimulate deglutition center in M. O. Signals stimulate closing of airways (breathing stops) Uvula and soft palate lift to close off nasopharynx Vocal cords close Epiglottis closes over larynx Upper esophageal sphincter relaxes
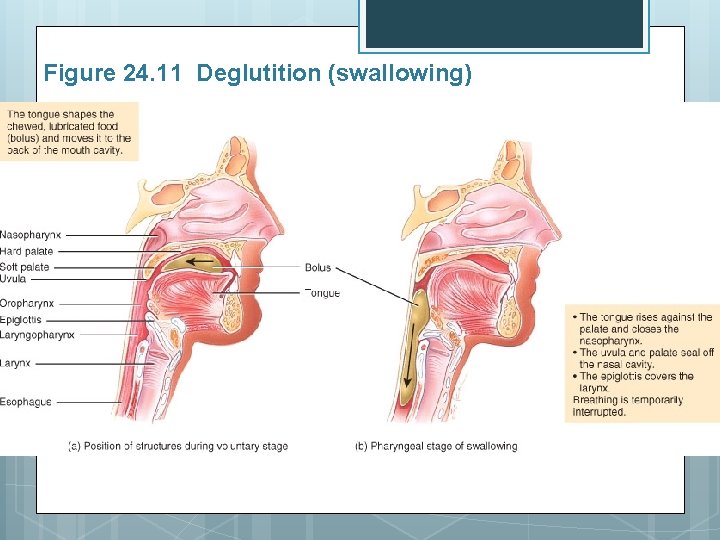
Figure 24. 11 Deglutition (swallowing)
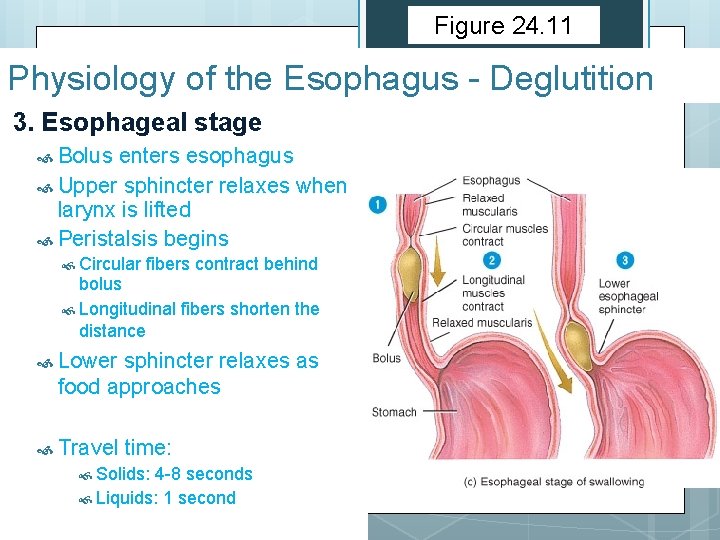
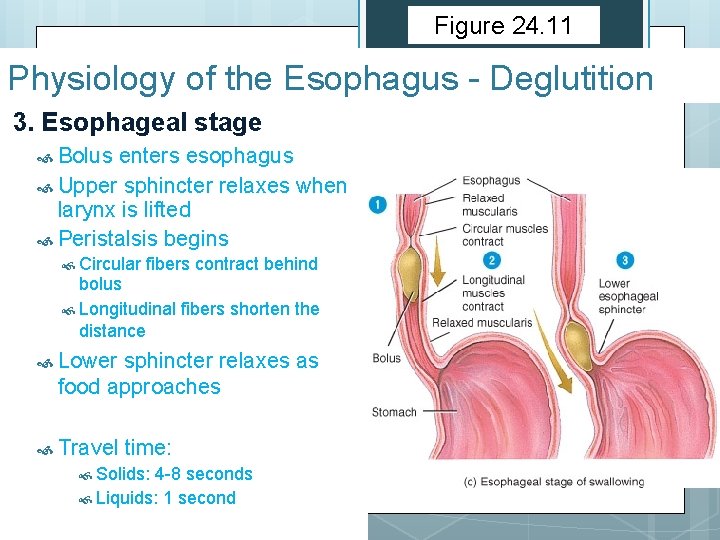
Figure 24. 11 Physiology of the Esophagus - Deglutition 3. Esophageal stage Bolus enters esophagus Upper sphincter relaxes when larynx is lifted Peristalsis begins Circular fibers contract behind bolus Longitudinal fibers shorten the distance Lower sphincter relaxes as food approaches Travel time: Solids: 4 -8 seconds Liquids: 1 second
Deglutition Summary Swallowed food Mouth Oropharynx Laryngopharynx Upper esophageal sphincter Esophagus (peristalsis) Lower esophageal sphincter Stomach

STOMACH
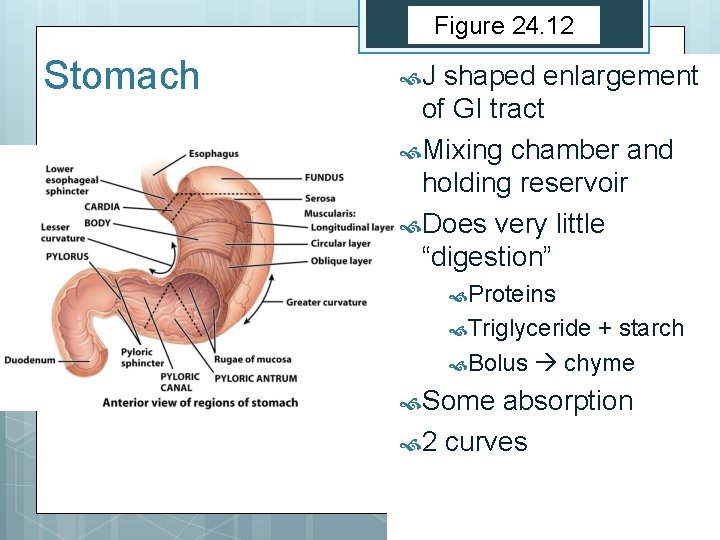
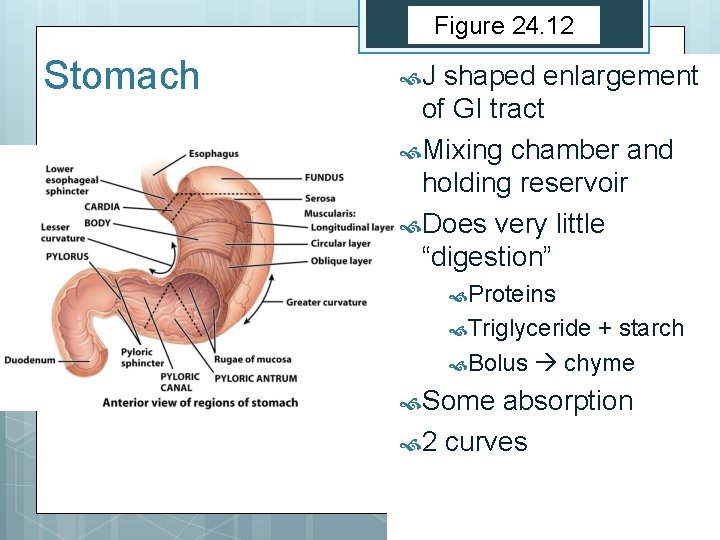
Figure 24. 12 Stomach J shaped enlargement of GI tract Mixing chamber and holding reservoir Does very little “digestion” Proteins Triglyceride + starch Bolus chyme Some absorption 2 curves
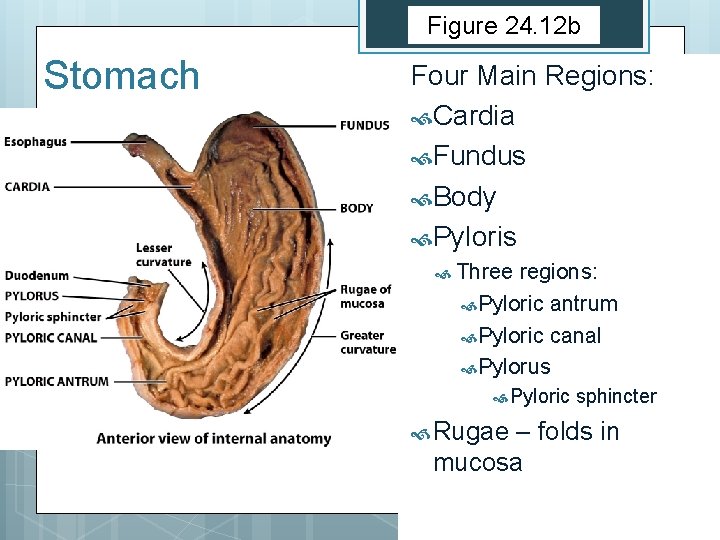
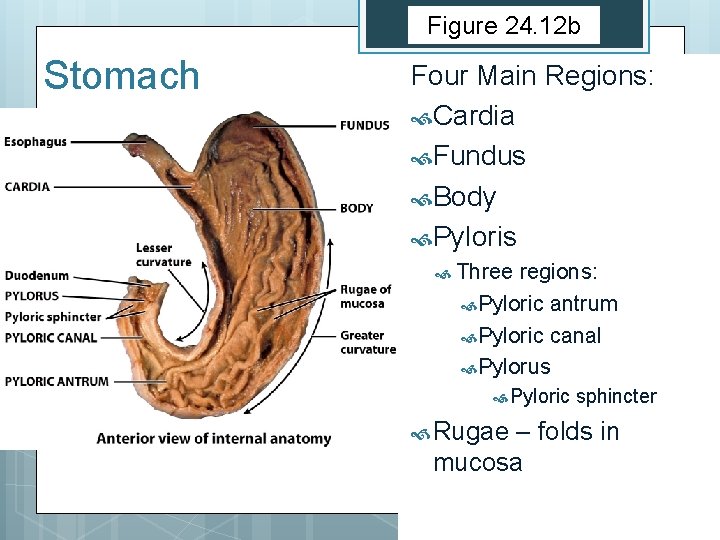
Figure 24. 12 b Stomach Four Main Regions: Cardia Fundus Body Pyloris Three regions: Pyloric antrum Pyloric canal Pylorus Pyloric Rugae sphincter – folds in mucosa
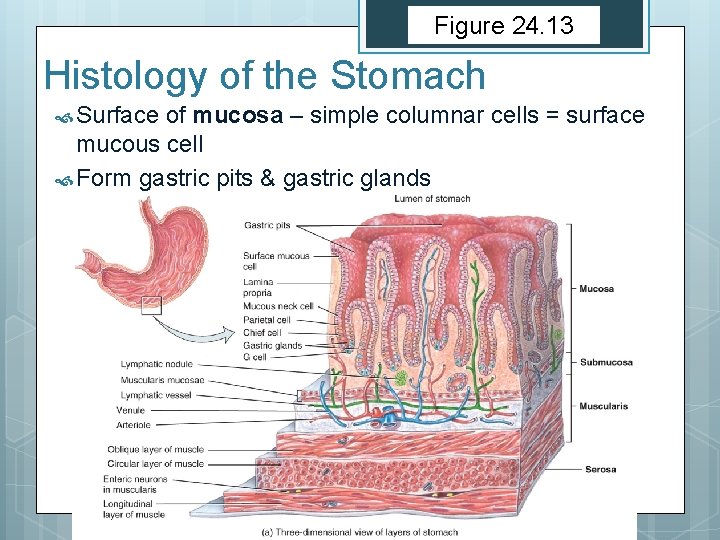
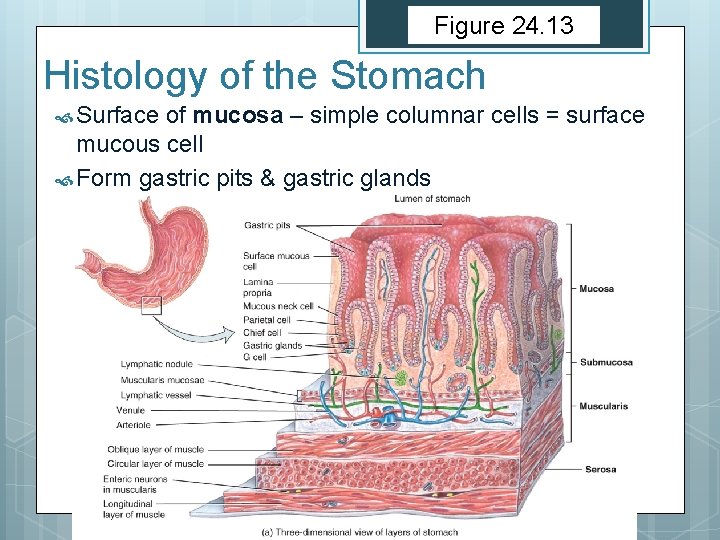
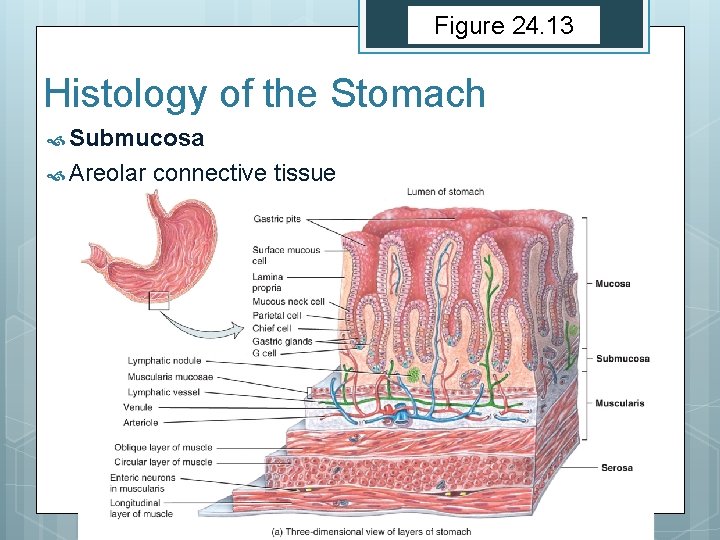
Figure 24. 13 Histology of the Stomach Surface of mucosa – simple columnar cells = surface mucous cell Form gastric pits & gastric glands
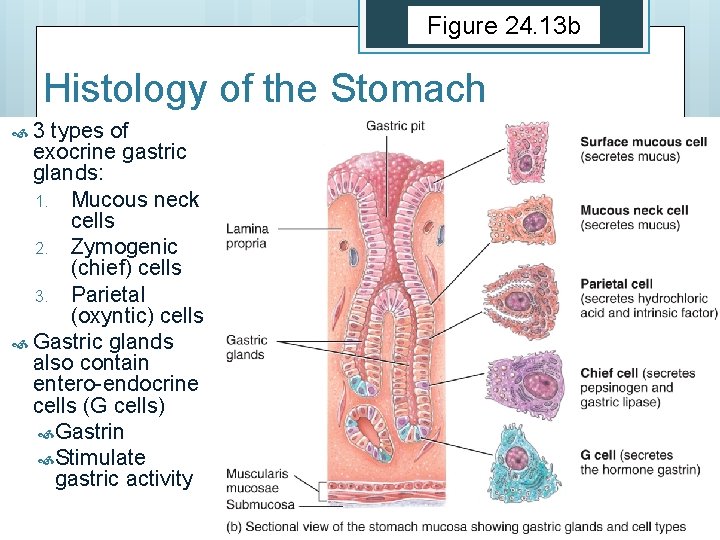
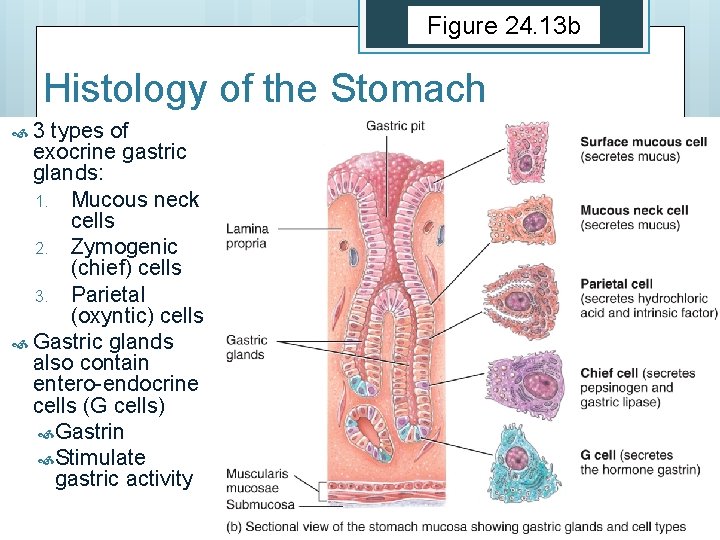
Figure 24. 13 b Histology of the Stomach 3 types of exocrine gastric glands: 1. Mucous neck cells 2. Zymogenic (chief) cells 3. Parietal (oxyntic) cells Gastric glands also contain entero-endocrine cells (G cells) Gastrin Stimulate gastric activity
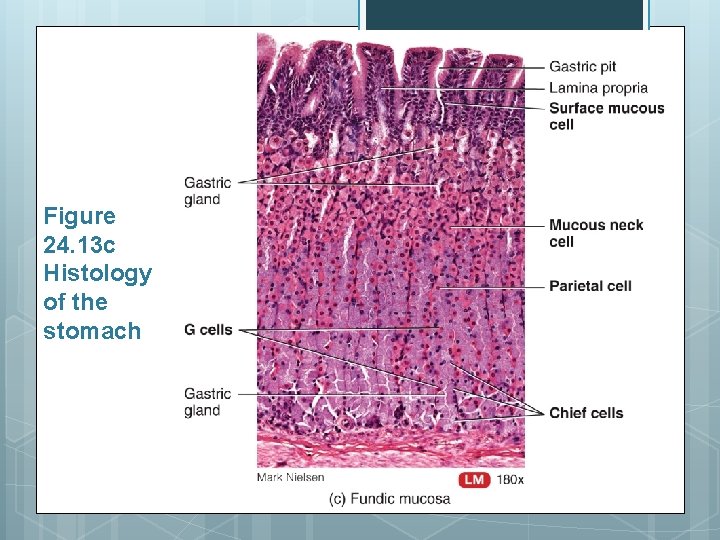
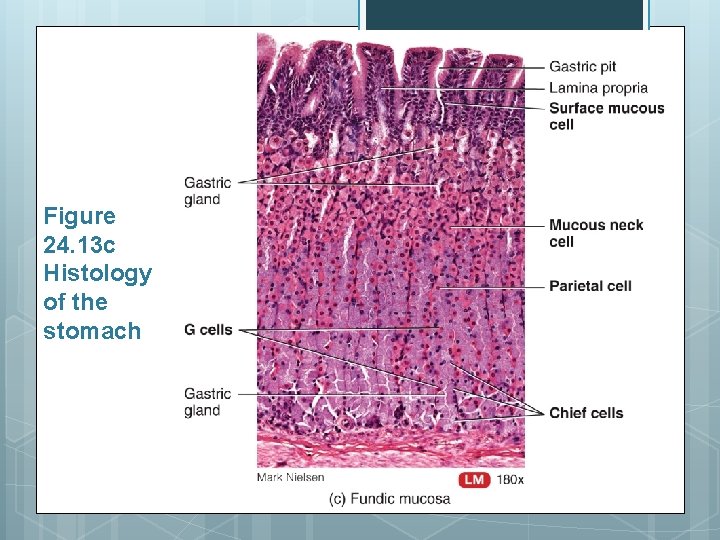
Figure 24. 13 c Histology of the stomach
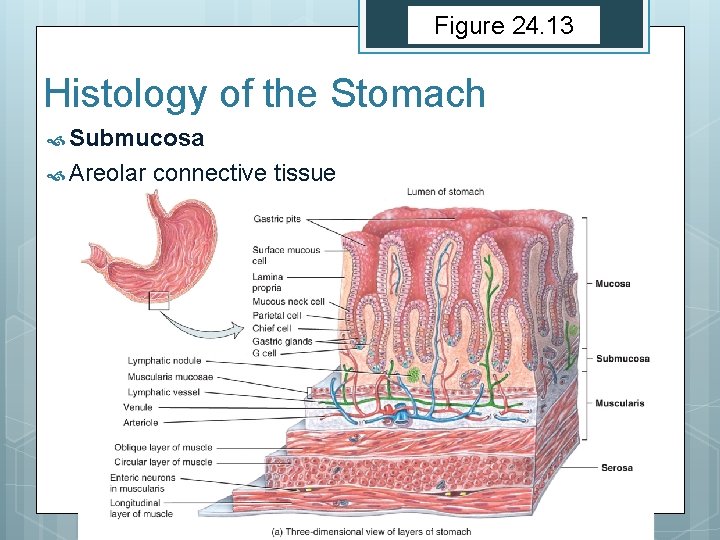
Figure 24. 13 Histology of the Stomach Submucosa Areolar connective tissue
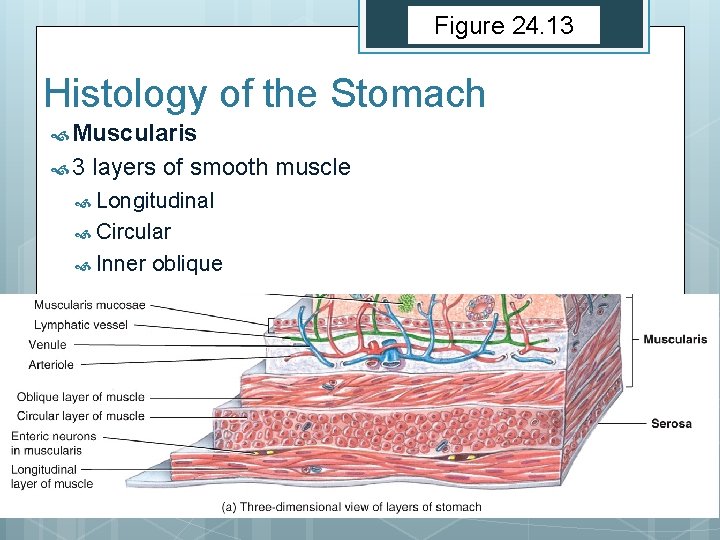
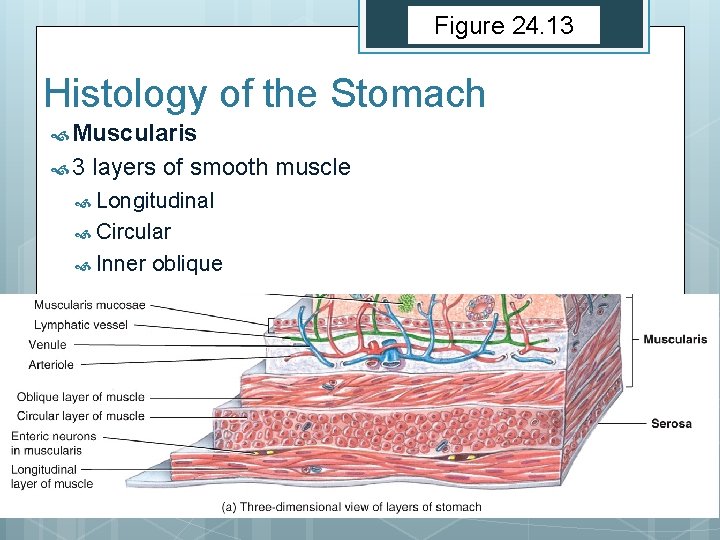
Figure 24. 13 Histology of the Stomach Muscularis 3 layers of smooth muscle Longitudinal Circular Inner oblique
Figure 24. 12 Histology of the Stomach Serosa Lesser curvature, visceral peritoneum = lesser omentum Greater curvature, visceral peritoneum = greater omentum
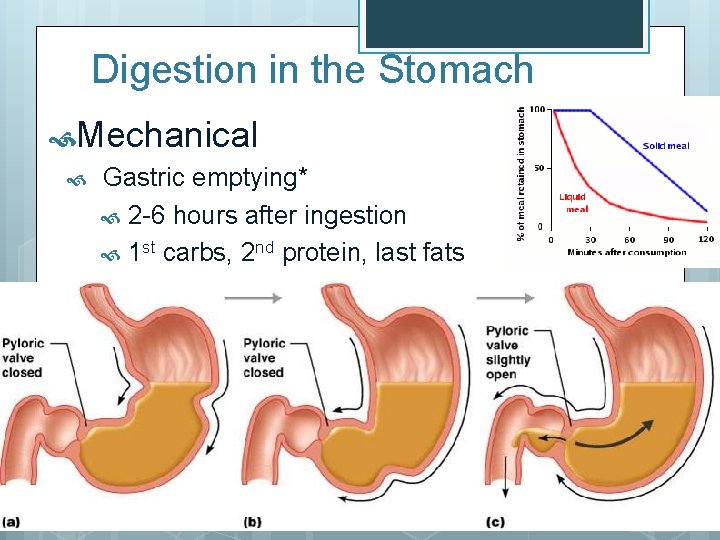
Figure 24. 12 Digestion in the Stomach Mechanical Peristalsis Propulsion Retropulsion https: //www. youtube. com/watch? v=hp. S 5 k. Mn_B 0 I https: //www. youtube. com/watch? v=KAfn. IPYN 0 X 0 Gastric emptying*
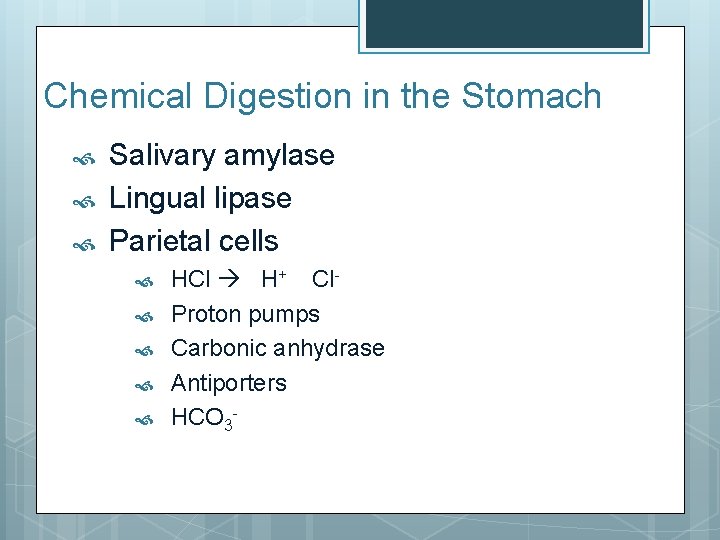
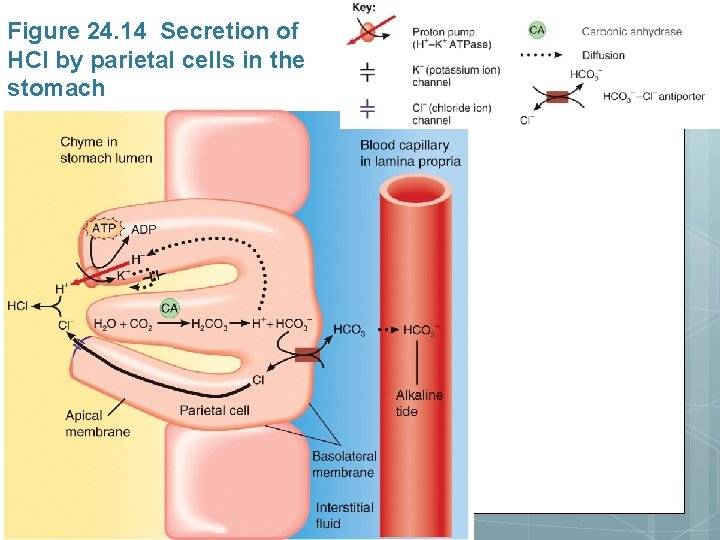
Chemical Digestion in the Stomach Salivary amylase Lingual lipase Parietal cells HCl H+ Cl. Proton pumps Carbonic anhydrase Antiporters HCO 3 -
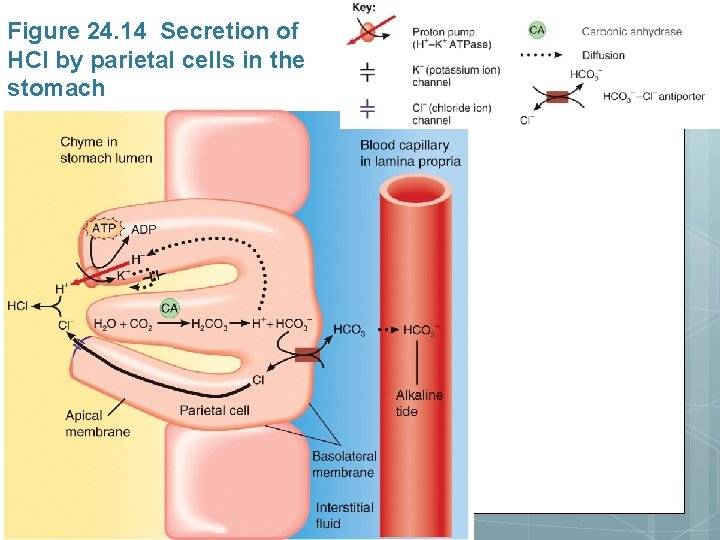
Figure 24. 14 Secretion of HCl by parietal cells in the stomach
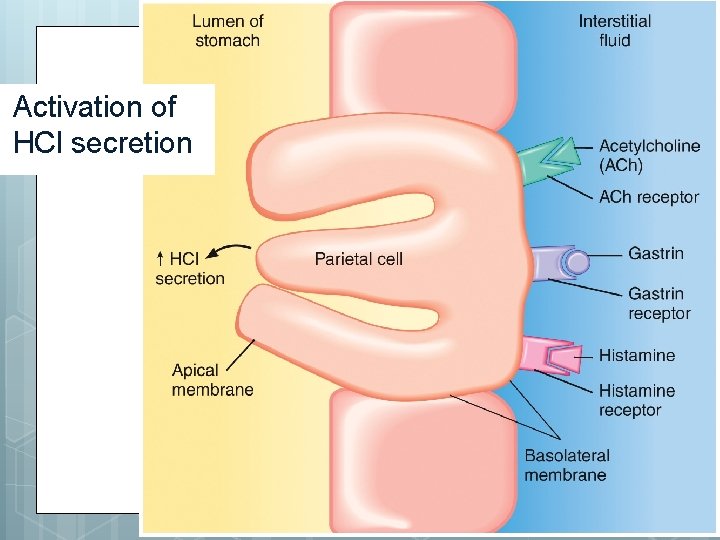
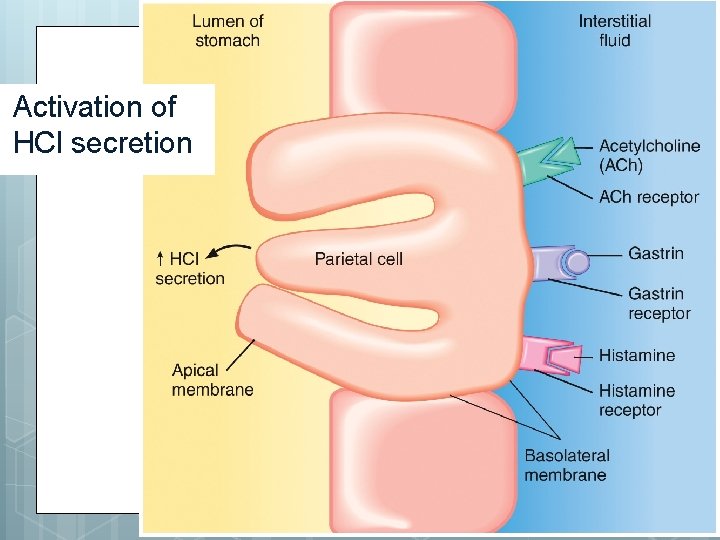
Activation of HCl secretion

Chemical Digestion in the Stomach Pepsinogen pepsin Chief (zymogenic cells) p. H of 2 activates Proteins peptides Gastric lipase Triglycerides (milk) fatty acids + monoglycerides Limited in adult stomach p. H 5 -6
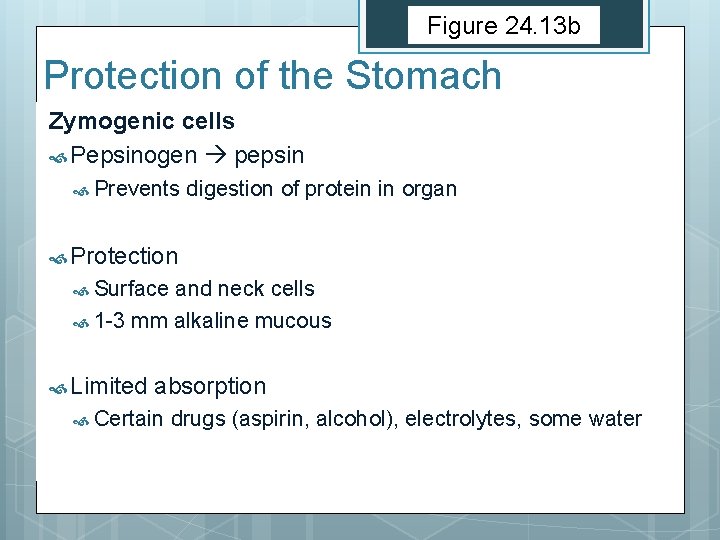
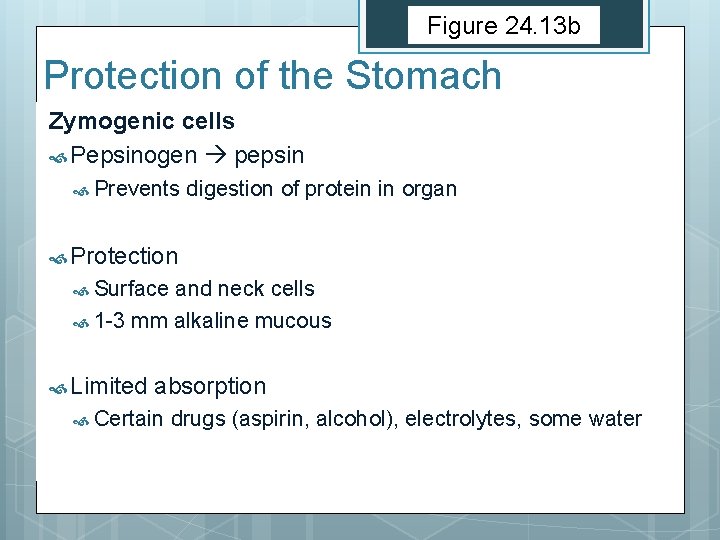
Figure 24. 13 b Protection of the Stomach Zymogenic cells Pepsinogen pepsin Prevents digestion of protein in organ Protection Surface and neck cells 1 -3 mm alkaline mucous Limited absorption Certain drugs (aspirin, alcohol), electrolytes, some water
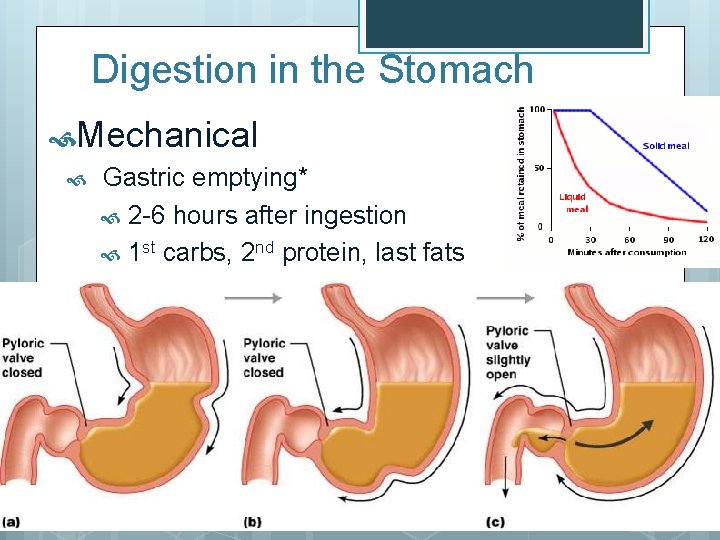
Digestion in the Stomach Mechanical Gastric emptying* 2 -6 hours after ingestion 1 st carbs, 2 nd protein, last fats
Look at Table 24. 3
PANCREAS
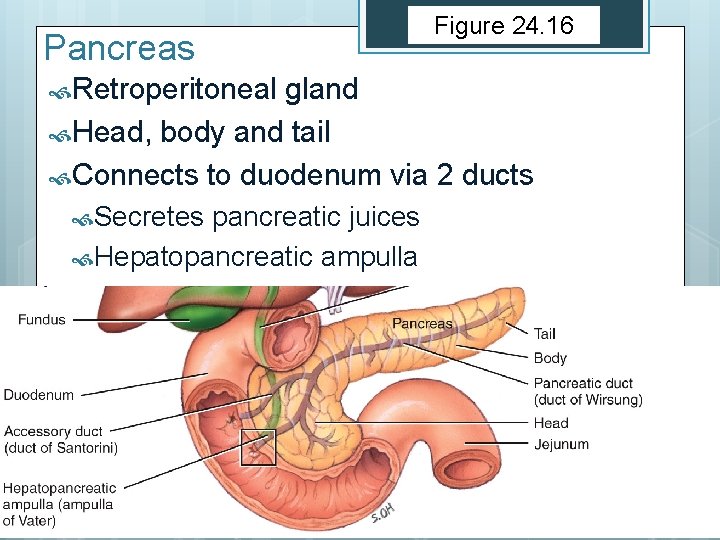
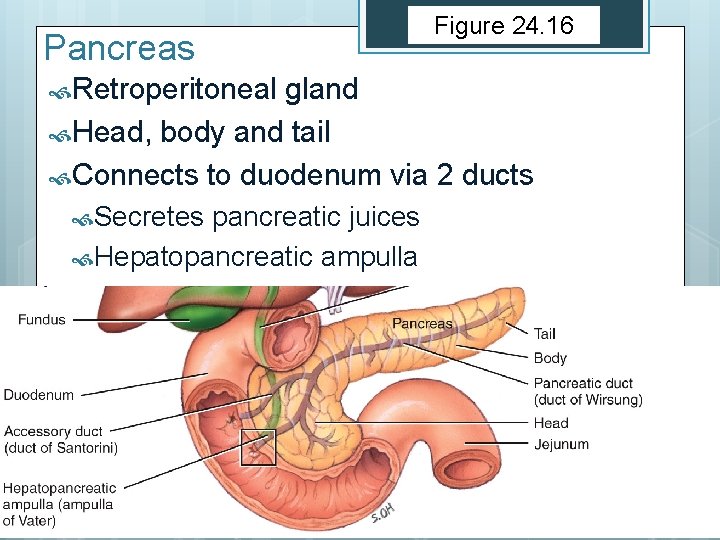
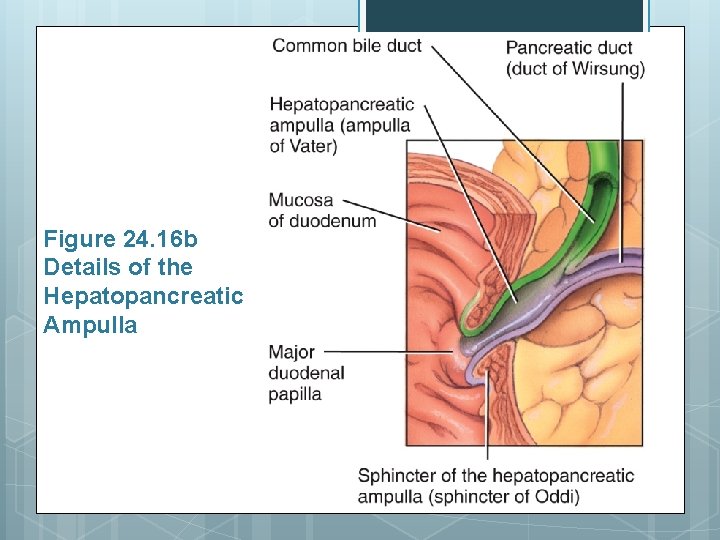
Pancreas Retroperitoneal Figure 24. 16 gland Head, body and tail Connects to duodenum via 2 ducts Secretes pancreatic juices Hepatopancreatic ampulla
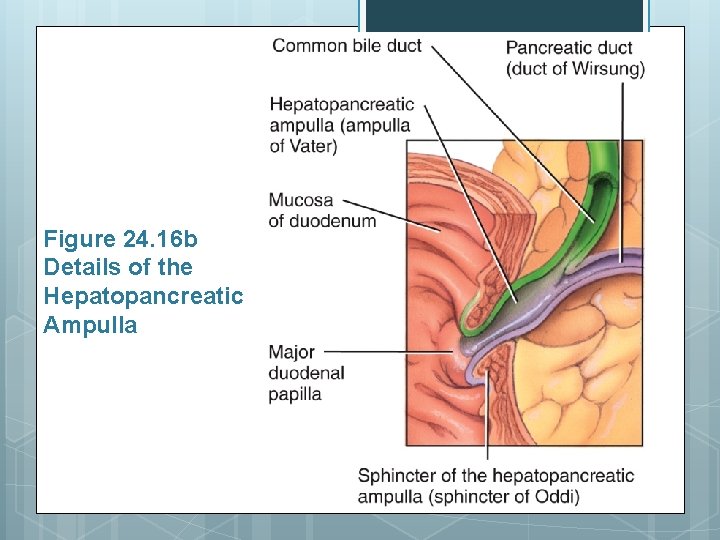
Figure 24. 16 b Details of the Hepatopancreatic Ampulla

Figure 24. 16 c
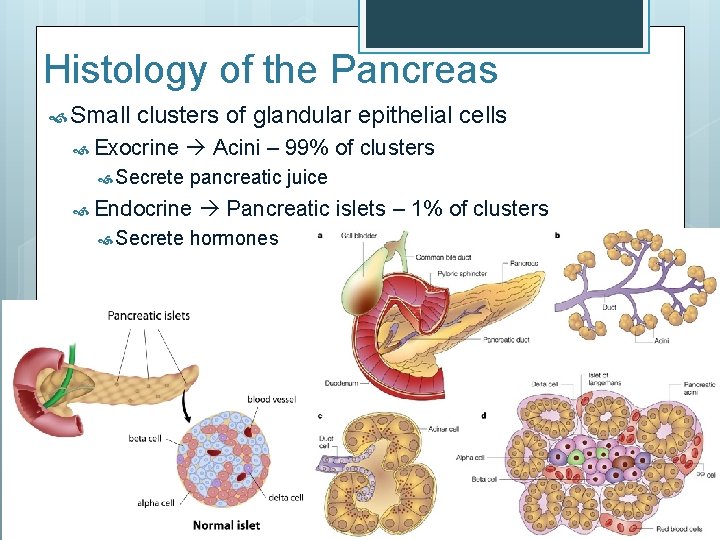
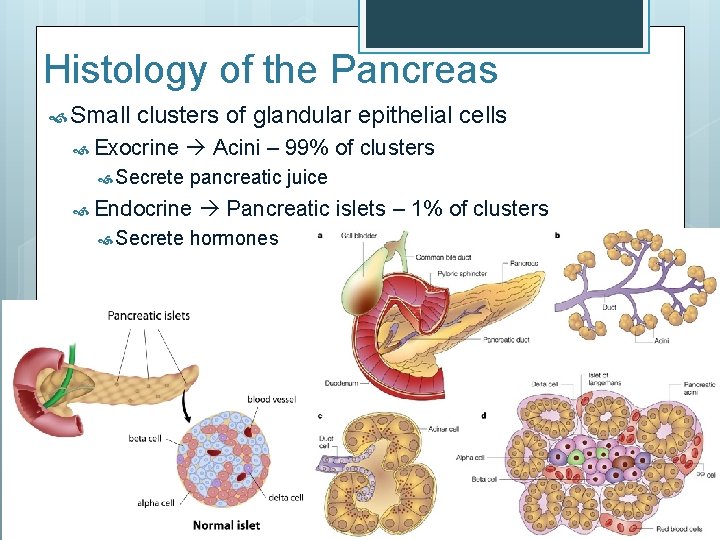
Histology of the Pancreas Small clusters of glandular epithelial cells Exocrine Secrete Acini – 99% of clusters pancreatic juice Endocrine Secrete Pancreatic islets – 1% of clusters hormones

Pancreatic Juice 1200 -1500 Clear m. L liquid: Water, salt, Na. HCO 3, enzymes Starch – pancreatic amylase Proteins – trypsin, chymotrypsin, carboxypeptidase Fats – pancreatic lipase Nucleic acids – ribonuclease, deoxyribonuclease Sodium bicarbonate – brings p. H to 7. 1 -8. 2 Inactivates pepsin Stimulates pancreatic enzymes
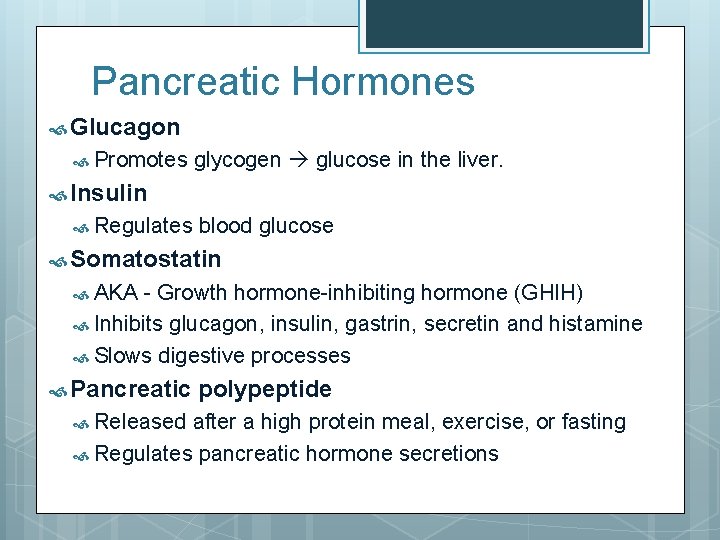
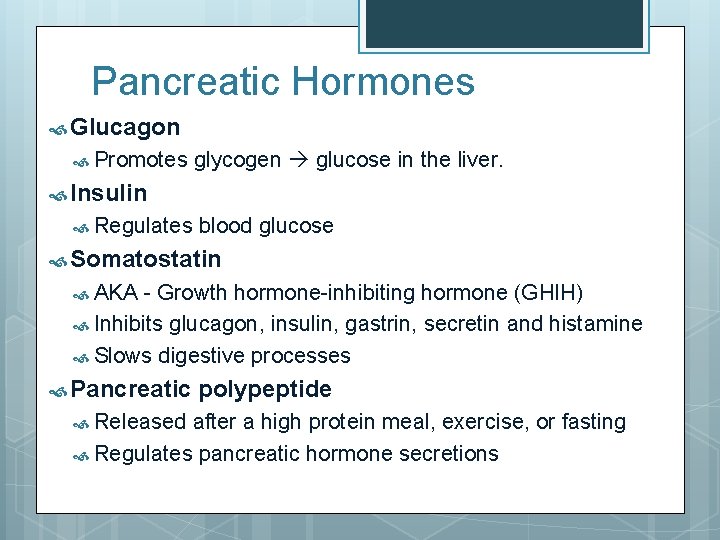
Pancreatic Hormones Glucagon Promotes glycogen glucose in the liver. Insulin Regulates blood glucose Somatostatin AKA - Growth hormone-inhibiting hormone (GHIH) Inhibits glucagon, insulin, gastrin, secretin and histamine Slows digestive processes Pancreatic Released polypeptide after a high protein meal, exercise, or fasting Regulates pancreatic hormone secretions