Malignant Hyperthermia What is Malignant Hyperthermia Malignant hyperthermia



- Slides: 29

Malignant Hyperthermia
What is Malignant Hyperthermia? § Malignant hyperthermia (MH) is an inherited hypermetabolic syndrome, that when triggered, causes sustained skeletal muscle contractions. § Can lead to severe hyperthermia, left ventricular failure, brain damage, organ failure, disseminated intravascular coagulation (DIC), cardiac arrest, and death. § Usually triggered during or after administration of commonly used general anesthetics
History of MH § 19 th century – monitoring of patients minimal, deaths with surgery not uncommon and often unexplained. § Early 20 th century – first reports of fever and tachycardia during or after anesthesia that ended in death, cause unknown. § 1960’s- first documented case of MH § Past mortality was 70%-80%, now with treatment ~5% within treatment hospital, 20% surgery centers or transferring hospitals.
Incidences Of MH § One in every 100, 000 hospital discharges complicated by MH § 500 -600 cases in US each year § Most common between ages 2 – 42 § 2/3 cases are men § More common in adults than children § 1 st degree relative of someone who has had MH or MH susceptible is at greater risk § Higher risk in someone with a muscle disorder
Goal of Treatment § Prevention – Perioperative nurse includes risk assessment during routine pre-op interview § prior complications from previous surgery § Personal history of muscle disorder § Family history of complications with surgery § Caffeine intolerance § If MH occurs – quickest response possible to prevent complications and death
Triggers § Known triggers: – Volatile anesthetics - sevoflurane, isoflurane, and desflurane – Inhaled anesthetics (except nitrous oxide) – Muscle relaxant – succinylcholine § Do Not Trigger: – All local anesthetics, barbiturates, Benzodiazepines, etomidate, Ketamine, nitrous oxide, Nondepolarizing muscle relaxants, propofol
Malignant Hyperthermia Screening § Only definitive diagnostic test for MH is caffeine halothane contracture test (CHCT). – Done with thigh muscle biopsy – Only 4 centers in the US perform test, 2 in Canada – Patient must travel to testing centers, biopsy must be fresh – Cost $6, 000 (not including travel), Cost usually not covered by insurance § Can use DNA analysis but only 30% effective, cost $200.
What’s Going ON § A MH-susceptible person has an abnormal structure and function of a calcium channel within their skeletal muscle § When exposed to trigger drugs an abnormal release of calcium inside the muscle cell occurs causing sustained muscle contraction, abnormal increase in energy utilization and heat production. § The muscle cell eventually runs out of energy and dies releasing large amounts of K and myoglobin into the bloodstream leading to arrhythmias and kidney failure.
Signs & Symptoms § § § Unexplained tachyarrhythmia (96% of cases) Unexplained tachypnea (85% of cases) Increased end-tidal CO 2, hypoxemia Acidosis (80%) General muscle rigidity – one of earliest signs, especially in masseter muscle of the jaw (80%) § Cyanotic or mottled skin – generally starts with a generalized flush (70%) § Rapid, sustained increase in body temperature – late sign only 30% of cases. Temperature can be as high as 110° § Cola-colored urine due to rhabdomyolysis (later sign)
LABORATORY FINDINGS OF ACUTE MH § ABG decreased p. H decreased PO 2 increased PCO 2 § Electrolytes increased K increased Ca increased Mg decreased Na
LABORATORY FINDINGS OF ACUTE MH (cont. ) § Serum increased Lactate increased Pyruvate increased CPK increased LDH increased Aldolase increased Myoglobin increased Glucose increased Creatinine decreased PTT decreased Platelets
www. nursetoons. com
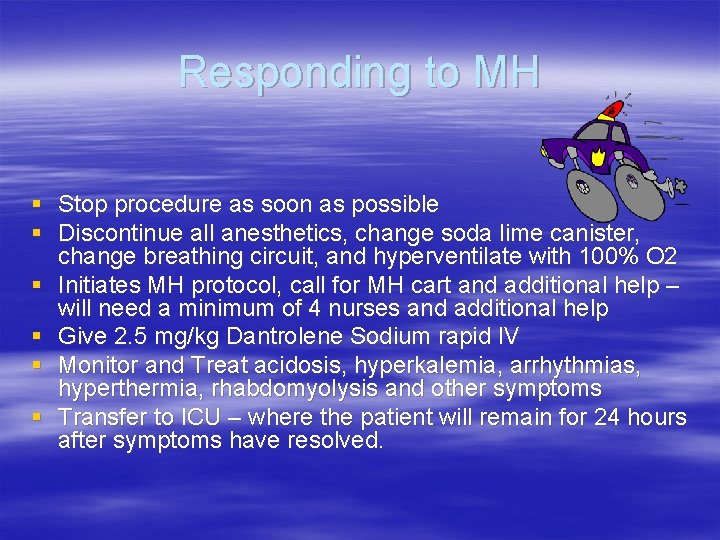
Responding to MH § Stop procedure as soon as possible § Discontinue all anesthetics, change soda lime canister, change breathing circuit, and hyperventilate with 100% O 2 § Initiates MH protocol, call for MH cart and additional help – will need a minimum of 4 nurses and additional help § Give 2. 5 mg/kg Dantrolene Sodium rapid IV § Monitor and Treat acidosis, hyperkalemia, arrhythmias, hyperthermia, rhabdomyolysis and other symptoms § Transfer to ICU – where the patient will remain for 24 hours after symptoms have resolved.
Circulating Nurse (1) § Calls immediately for additional help and MH cart § Assist anesthesia with anesthesia machine and as needed § Place additional IV lines § Draws blood/ ABG’s § Monitors patient including urine output
Dantrolene Nurse (2) § Bring MH cart § Start mixing Dantrolene ( will need up to 36 vials and 2 liters sterile water) § Administer Dantrolene as soon as possible
Dantrolene § The key to controlling a MH crisis is the quick administration of Dantrolene. § It is the first-line defense against reducing MH mortality. § Dantrolene is a muscle relaxant that restores a healthy level of calcium in the muscle and reduces high body temperature.
Dantrolene § Mix: – Mix each vial with 60 cc sterile H 20 (without bacteriostatic agents) use IV spike transfer pins to reconstitute – Shake vigorously to reconstitute, mix until clear- this may take several minutes – Give rapid continuous IV push. Administer 2. 5 mg/kg. Repeat up to 10 mg/kg or until symptoms subside – When mixed keep from light and use within 6 hours § Avoid use of calcium channel blockers with dantrolene - may cause life-threatening hyperkalemia and myocardial depression.
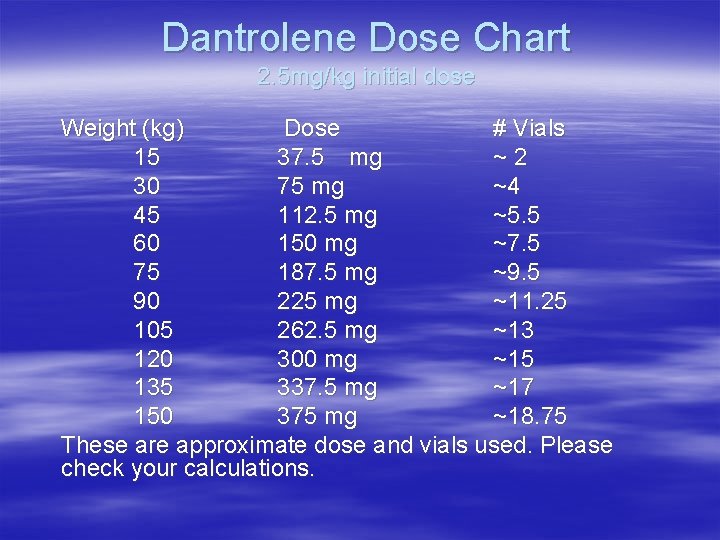
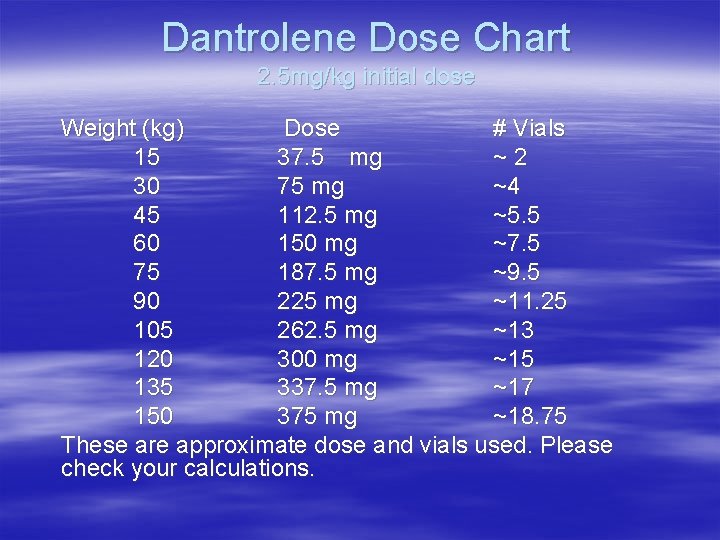
Dantrolene Dose Chart 2. 5 mg/kg initial dose Weight (kg) Dose # Vials 15 37. 5 mg ~2 30 75 mg ~4 45 112. 5 mg ~5. 5 60 150 mg ~7. 5 75 187. 5 mg ~9. 5 90 225 mg ~11. 25 105 262. 5 mg ~13 120 300 mg ~15 135 337. 5 mg ~17 150 375 mg ~18. 75 These are approximate dose and vials used. Please check your calculations.
New research § Recent research revealed that – intravenous administration of life-saving Dantrolene can occur significantly faster by warming the diluent used in mixing – Thirty seconds or more can be shaved off the process which normally take at least two minutes EVERY SECOND COUNTS WHEN TREATING A PATIENT WITH MALIGNANT HYPERTHERMIA This research indicates that it is possible to administer Dantrolene faster, therefore increasing the chances of a successful patient outcome. §Journal of the American Association of Nurse Anesthetist April 2007
Medication Nurse (3) § Brings crash cart into room § Mix and administer drugs as needed: – Sodium bicarbonate to correct metabolic acidosis – IV glucose, insulin and calcium chloride to treat hyperkalemia – Antiarrhythmic agents to treat arrhythmias (Do not use calcium channel blockers) – Diuretics to prevent rhabdomyolysis § Lasix, mannitol and IV NS to maintain urine output of 1 -2 ml/kg/hr
Cooling Nurse (4) § § § Obtains cooled IV solutions and ice Monitor patient’s temperature Cools the patient by : – – – – Use of hypothermia blanket Cooling room Placing ice packs around patient IV refrigerated solutions Cold lavage through NG Insert 3 -way foley and irrigate with cool saline If patient has open abdominal or thoracic cavity give scrub sterile refrigerated saline for surgeon to use in cavity STOP COOLING WHEN PATIENT’S TEMP IS 38° C (100° F) TO PREVENT HYPOTHERMIA
Additional Help § Help cooling nurse get ice from cafeteria and cooled saline from anesthesia fridge § Help make ice packs § Bring other supplies as needed § Run labs § Limit excessive traffic in room
www. nursetoons. com
Post - Op § MH is most likely to occur in the OR, however, it can also occur in PACU within the first hour and up to 24 hours post-op. § MH may recur within hours of the initial episode and temperature fluctuations may continue for several days. § Dantrolene should be continued at 1 mg/kg every 4 -6 hours for 48 hours in the ICU to prevent reappearance of symptoms.

Documentation should include: § All medications and times given § Labs drawn and times § Cooling methods used on patients § Vitals including temp. § All personal involved § All procedures completed (foley, NG, IV’s)
Legalities § Perioperative nurses should be aware of the legal considerations of MH. Lawsuits have been decided for the plaintiff when: – Risk factors were not identified preoperatively – Body temperature not monitored continuously – Failure to recognize signs and symptoms of MH – Failure to institute prompt and appropriate treatment
In Conclusion: EVERY SECOND COUNTS WHEN TREATING A PATIENT WITH MALIGNANT HYPERTHERMIA A malignant hyperthermia event is life-altering and can be deadly. But, with proper preparation, training, and teamwork a MH crisis can be managed without loss of life or serious adverse consequences. The MH Association of the US (MHAUS), maintains a 24 -hour hot line that is staffed by anesthesiologists who are available to help those dealing with a MH event. There is a 1 -800 number posted on all phones in the OR rooms, PACU and stage II.
References § Malignant hyperthermia-the perioperative nurse’s role. Ruth Hommertzheim, RN & Elaine Steinke, RN. AORN January 2006 pg 151 § Standards, Recommended Practices, and Guidelines. AORN, Inc. 2007 Ed. Pg 219 -227. § Journal of the American Association of Nurse Anesthetist April 2007 Pg. 101 -106 § Additional information also available on Malignant Hyperthermia carts and the Malignant Hyperthermia Association web site : www. mhaus. org
