Uterus A pear shaped thick walled muscular organ
- Slides: 61
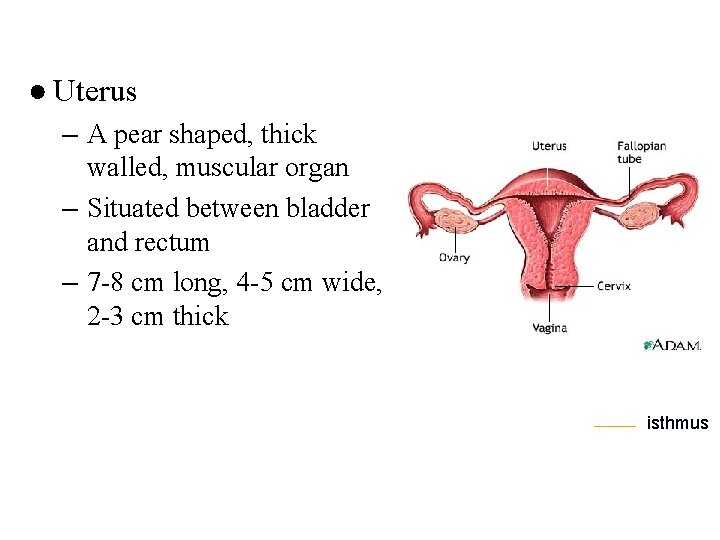
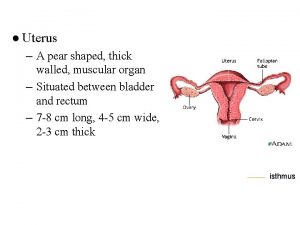
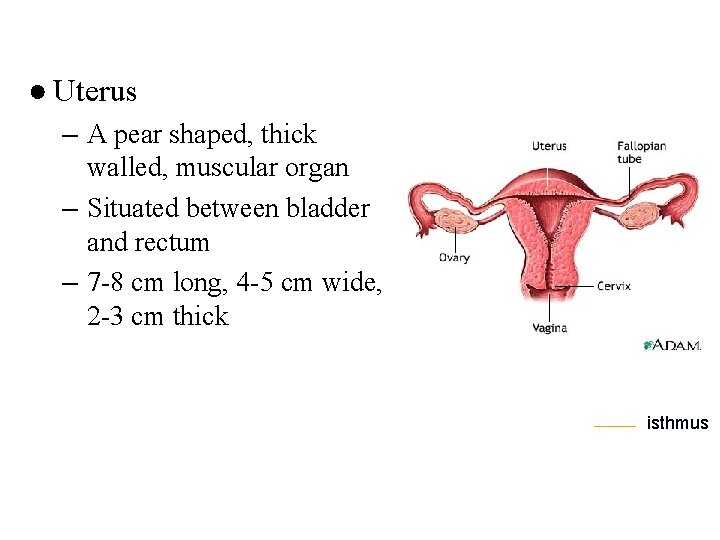
● Uterus – A pear shaped, thick walled, muscular organ – Situated between bladder and rectum – 7 -8 cm long, 4 -5 cm wide, 2 -3 cm thick isthmus
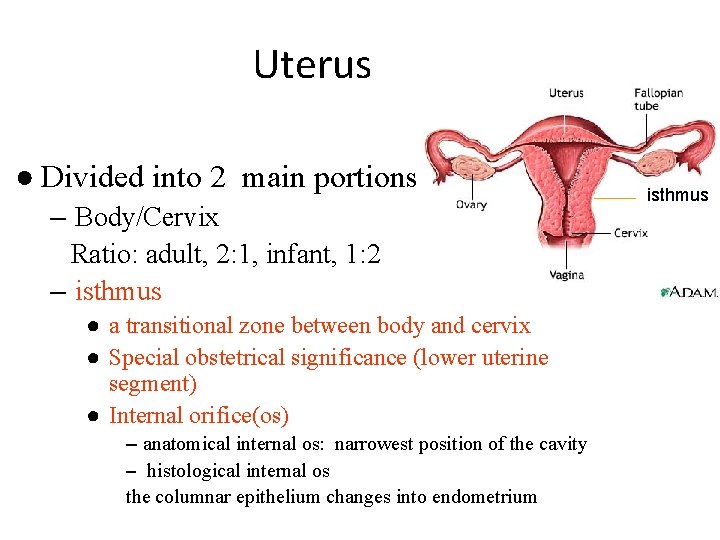
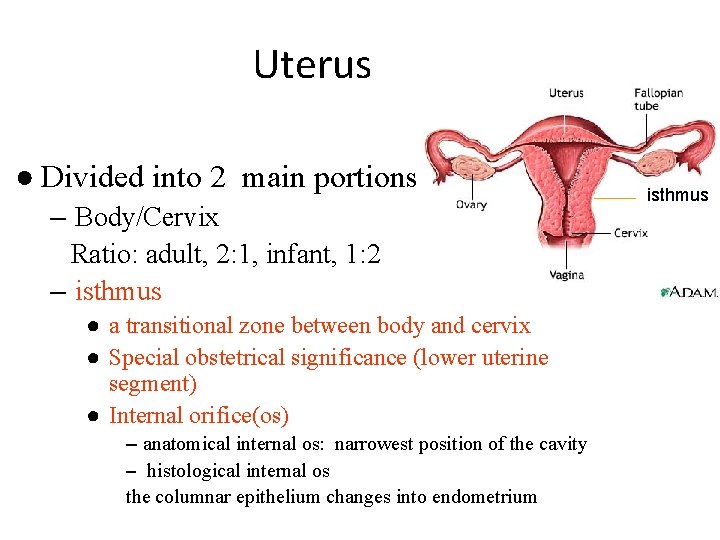
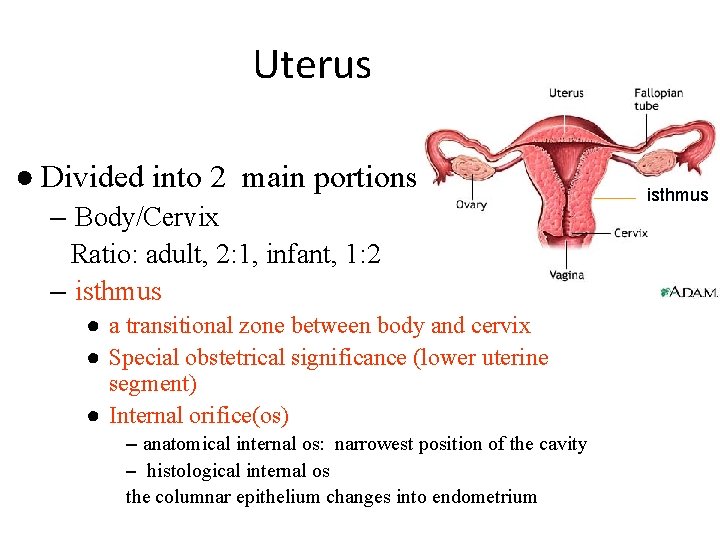
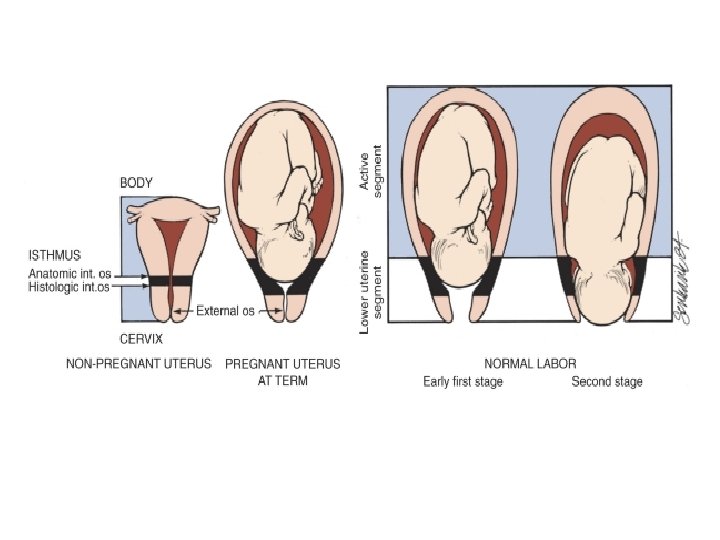
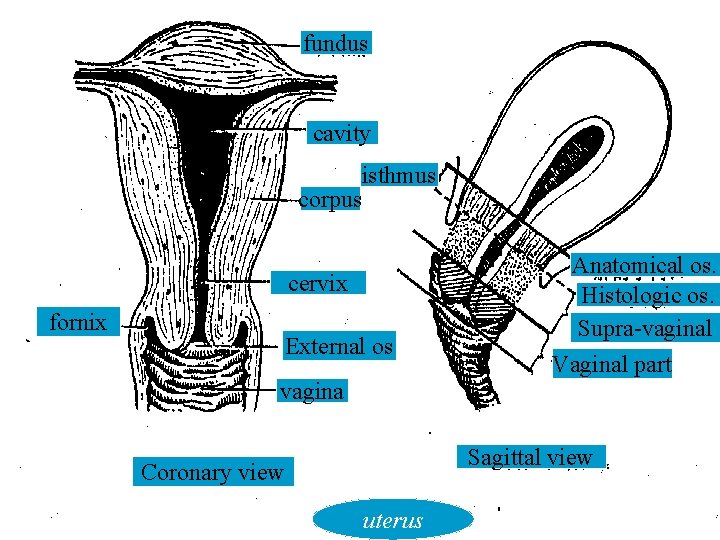
Uterus ● Divided into 2 main portions – Body/Cervix Ratio: adult, 2: 1, infant, 1: 2 – isthmus ● a transitional zone between body and cervix ● Special obstetrical significance (lower uterine segment) ● Internal orifice(os) – anatomical internal os: narrowest position of the cavity – histological internal os the columnar epithelium changes into endometrium isthmus
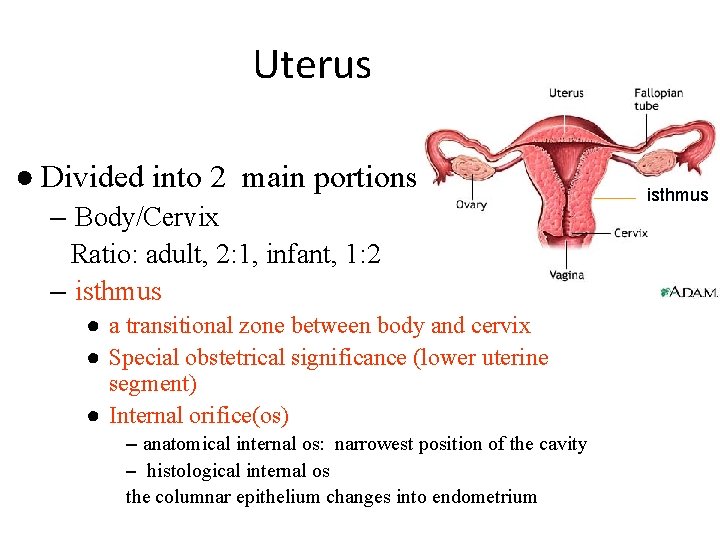
Uterus ● Divided into 2 main portions – Body/Cervix Ratio: adult, 2: 1, infant, 1: 2 – isthmus ● a transitional zone between body and cervix ● Special obstetrical significance (lower uterine segment) ● Internal orifice(os) – anatomical internal os: narrowest position of the cavity – histological internal os the columnar epithelium changes into endometrium isthmus
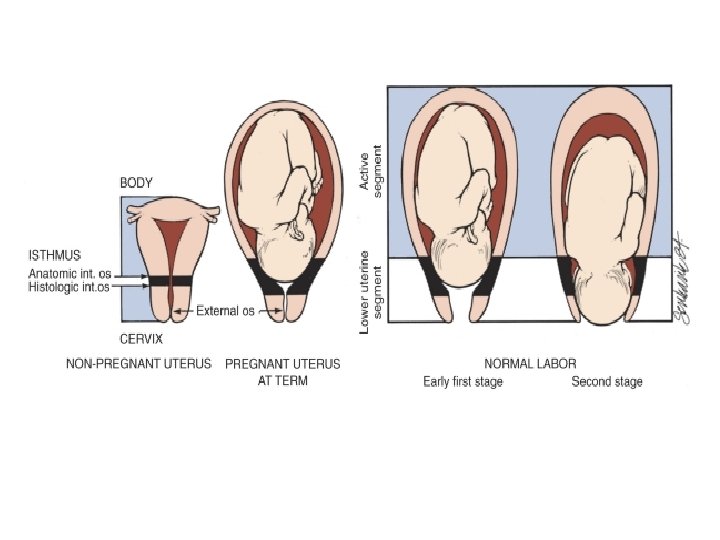
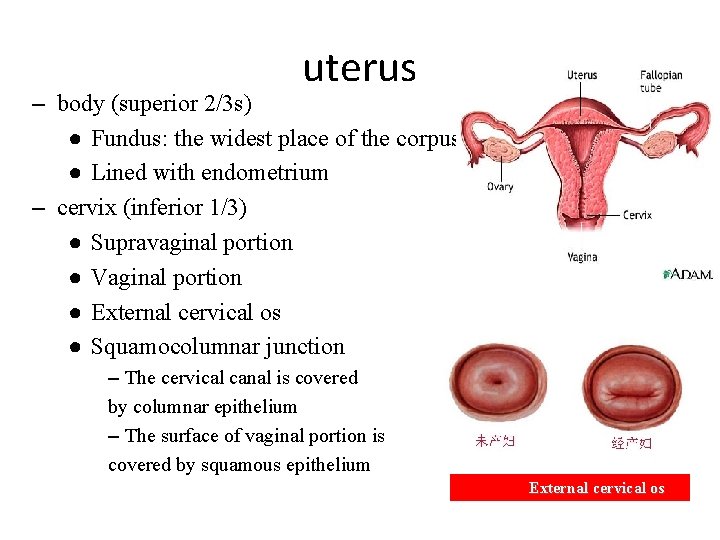
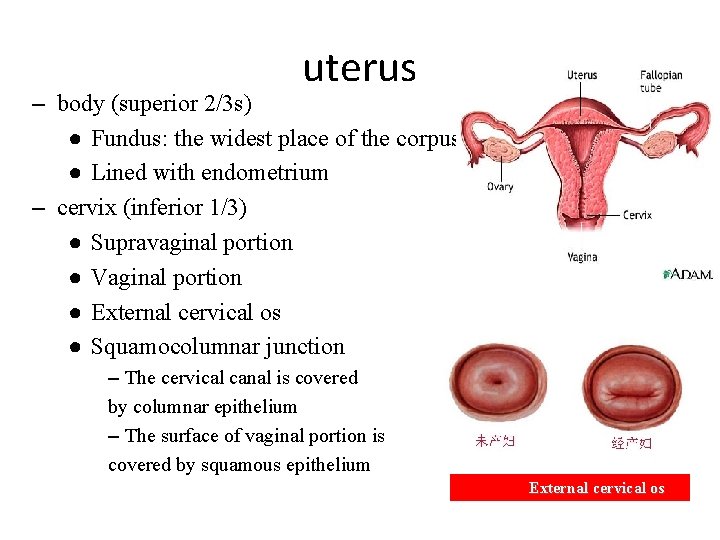
uterus – body (superior 2/3 s) ● Fundus: the widest place of the corpus ● Lined with endometrium – cervix (inferior 1/3) ● Supravaginal portion ● Vaginal portion ● External cervical os ● Squamocolumnar junction – The cervical canal is covered by columnar epithelium – The surface of vaginal portion is covered by squamous epithelium External cervical os
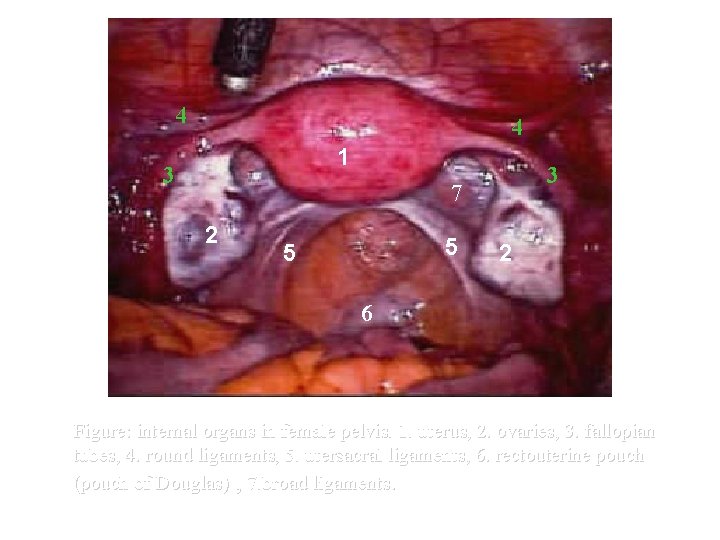
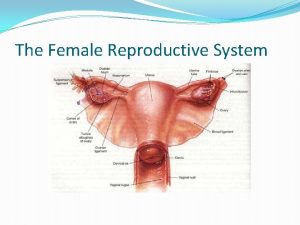
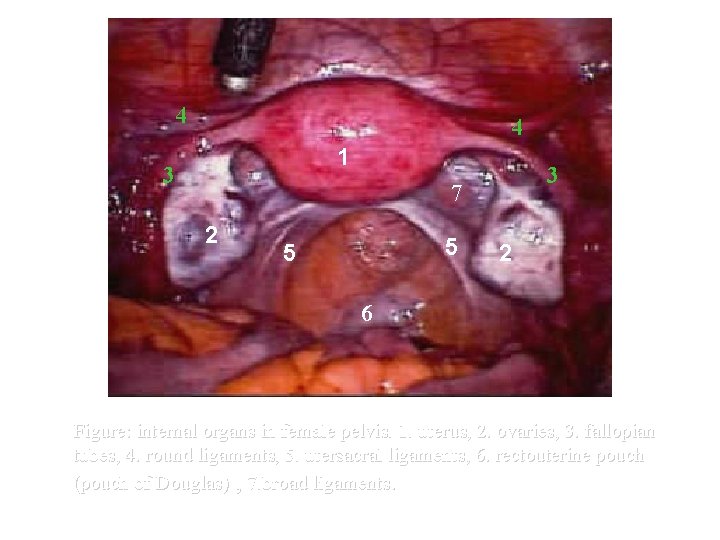
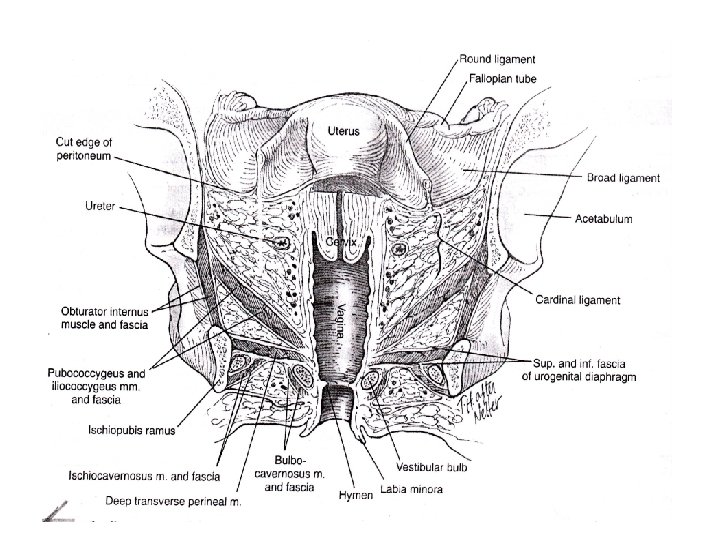
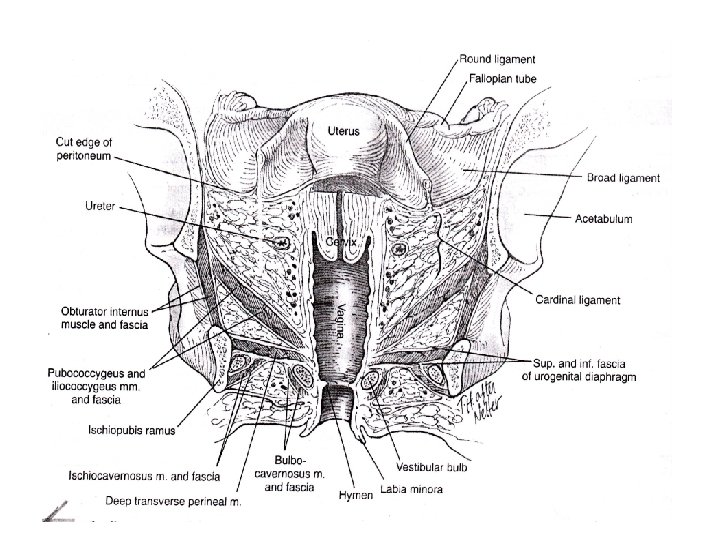
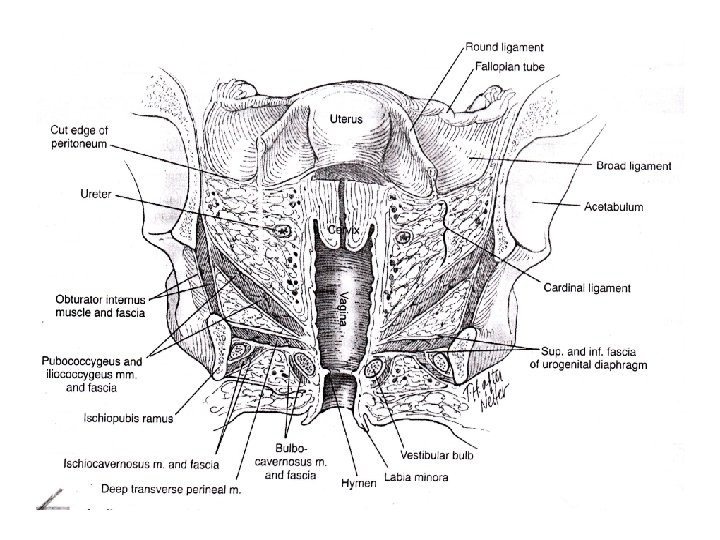
4 4 1 3 3 7 2 5 5 2 6 Figure: internal organs in female pelvis. 1. uterus, 2. ovaries, 3. fallopian tubes, 4. round ligaments, 5. utersacral ligaments, 6. rectouterine pouch (pouch of Douglas) , 7. broad ligaments.
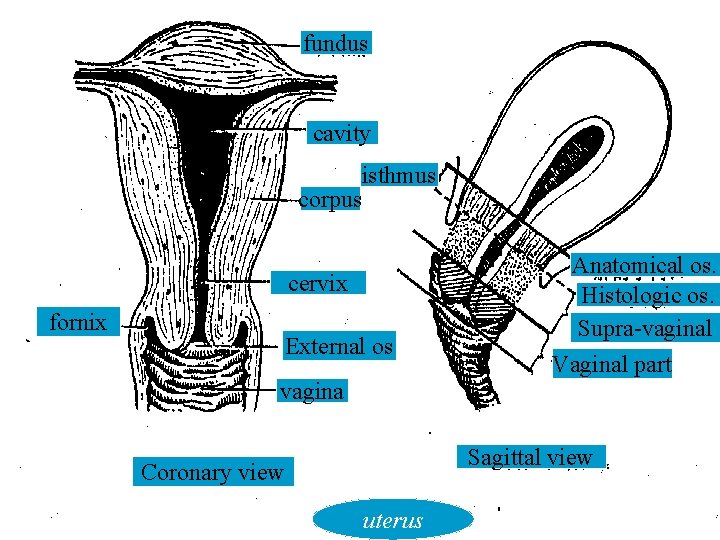
fundus cavity isthmus corpus cervix fornix External os Anatomical os. Histologic os. Supra-vaginal Vaginal part vagina Sagittal view Coronary view uterus
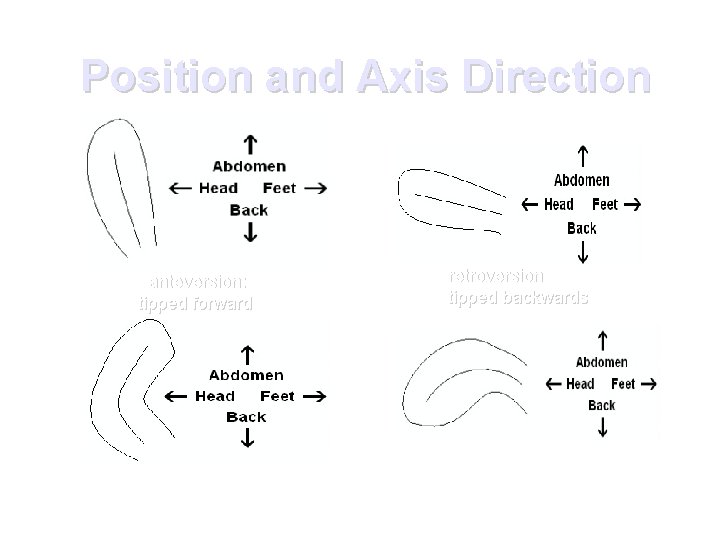
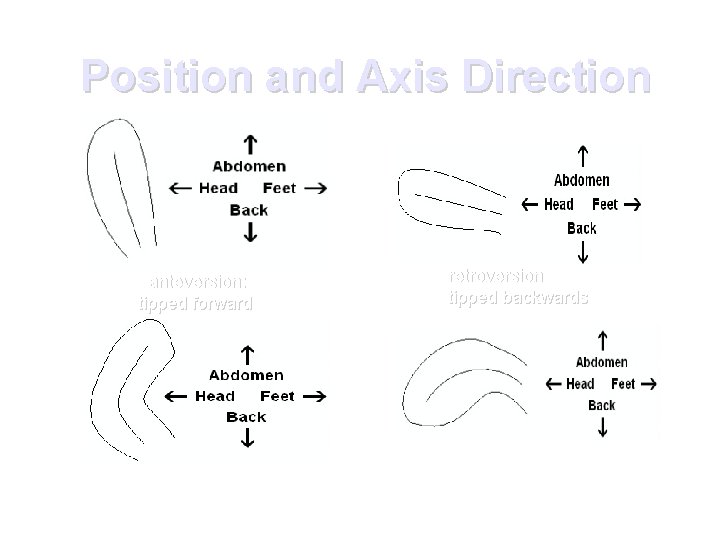
Position and Axis Direction anteversion: tipped forward anteflexion: the fundus is pointing forwards. The isthmus is bend. retroversion tipped backwards retroflexion: the fundus is pointing backwards. Anterior of uterus is convex.
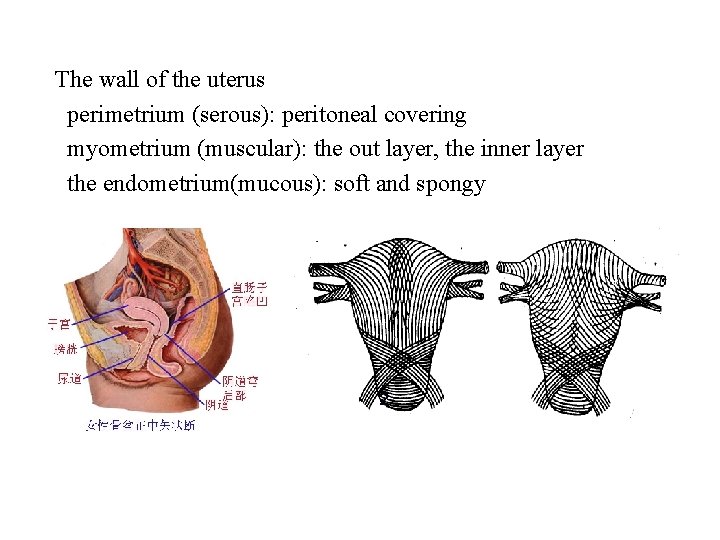
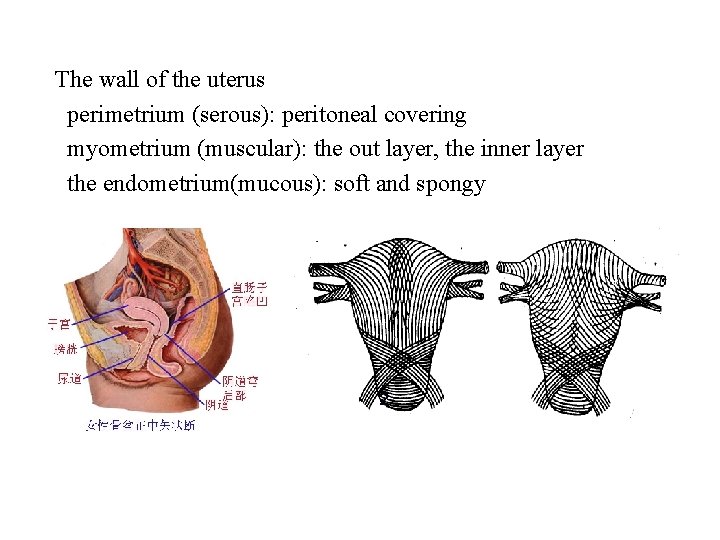
The wall of the uterus perimetrium (serous): peritoneal covering myometrium (muscular): the out layer, the inner layer the endometrium(mucous): soft and spongy 1 2 The myometrium of the uterus: 1. the out layer, 2. the inner layer
SUPPORTS OF UTERUS
INTRODUCTION ● The normal position & support of uterus, vagina, bladder & rectum rely on interdependent system of bony, muscular & connective tissue. ● Subtle alterations in one, lead to failure of normal anatomy. ● Understanding of normal applied pelvic anatomy is esential in repair of pelvic organ prolapse.
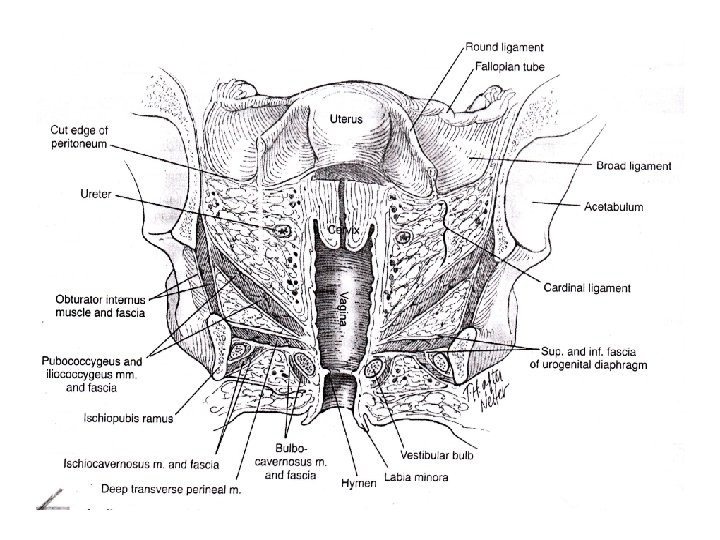
Classification of Supports of Uterus ● Primary supports 1} muscular or active a) pelvic diaphragm b) urogenital diaphragm c) perineal body 2} fibromuscular or mechanical a} uterine axis b} round ligament of uterus c} endopelvic fascia
● Secondary supports a} broad ligaments b} UV fold of peritoneum c} rectovaginal fold of peritoneum
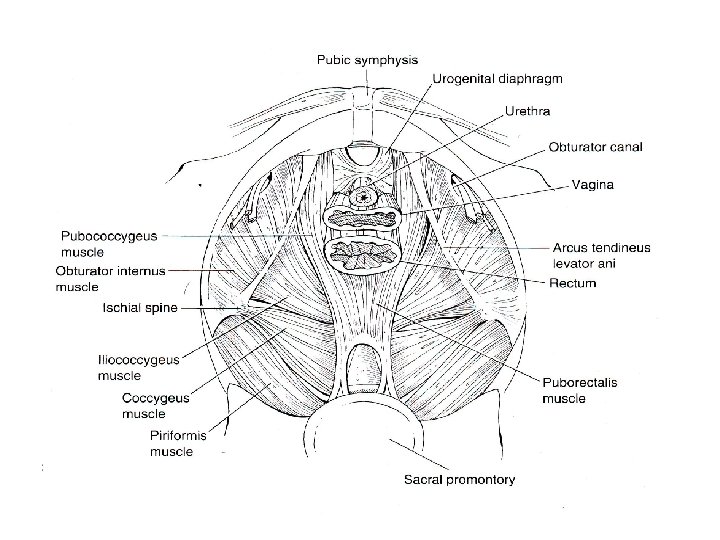
Pelvic diaphragm ● Consists of 2 levator ani muscles ● Each levator ani consists of 3 divisions pubococcygeus iliococcygeus ischiococcygeus / coccygeus ● Covered superiorly & inferiorly by pelvic fascia which separates it from parametrium above & ischiorectal fossa below. ● Levator ani fix the perineal body & make it as an anchor for levator ani.
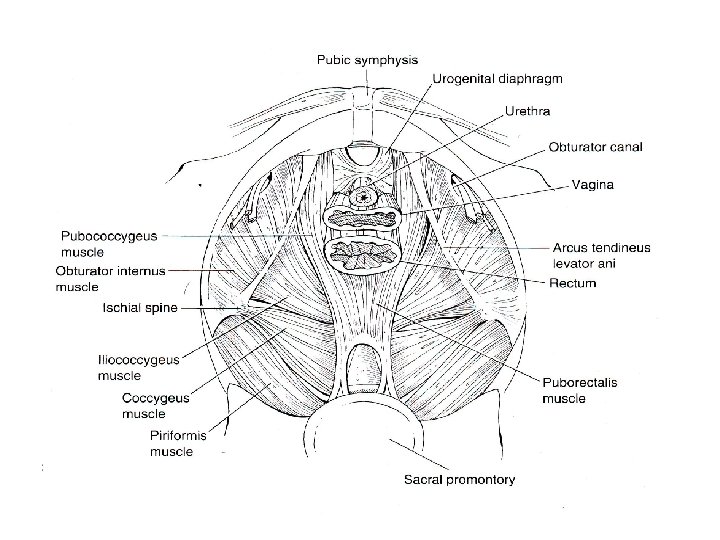
Pubococcygeus ● Origin- posterior surface of body of pubis. ● Insertion- into the anococcygeal raphe & coccyx by passing backwards, lateral to vagina & rectum. ● Some of the inner fibres form puborectalis, pubovaginalis, perineal body. ● Nerve supply- inferior rectal nerve s 3 -4 ● Fibres near perineal body divide the space anterior- hiatus urogenitalis- urethra & vagina posterior- hiatus rectalis- rectum
Iliococcygeus ● Fan shaped muscle ● Origin- broad margin along the white line of pelvic fascia known as arcus tendineus levator ani. ● Insertion- into the coccyx by passing backwards & inwards from the origin. ● Nerve supply- inferior rectal nerve s 3 -4.
Ischiococcygeus / coccygeus ● Origin- narrow origin from ischial spine. ● Insertion- in front of coccyx by spreading out posteriorly from the origin. ● Nerve supply- supplied by s 4 -5.
Applied anatomy ● Perineal tears during parturition ● Postmenopausal state ● Perineal nerve injury ● Asthenic states ● Levator ani constitutes pelvic diaphragm, support pelvic viscera, ● Assist ant abdominal wall muscles in containing abdominal & pelvic contents
● Supports post wall of vagina ● Facilitates defecation ● Aids in fecal continence ● During parturition supports fetal head and helps in internal rotation of head.
How levator ani helps in containing pelvic viscera? ● Contraction of levator ani pulls the rectum and vagina towards pubis ● Thereby kinking the rectum and narrowing vagina anteroposteriorly preventing its descent.
How levator ani helps In internal rotation? ● With contraction of levator ani posterior attachments are pulled towards pubis which help in internal rotation of presenting part. (? ) ● Uterine contraction pushes presenting part down & cause muscle to contract. ● Lowest part of fetus is carried forwards during contraction & ant fibres are directed inwards & forwards.
Examination of levator muscle tone? ● Levator ani tone is examined by placing two fingers in vagina & is flexed laterally, the thumb being applied externally over labium majus. ● Patient is asked to contract her pelvic floor muscles and thus levator muscles can be palpated to determine its tone & assess size of hiatus urogenitalis.
Kegel ‘ exercises ● Quick pumps- 15 reps of quick pumps, pause for 30 sec and repeat. Start at 15 and work upto 100 two times a day. ● Hold & release- contract the muscle slowly & hold for 5 sec, release slowly. Work your way to atleast 25 reps two times a day. ● Elevator- slowly contract 1/3 of way, pause, then 2/3 rd of way, pause then all the way. Do 10 reps two times a
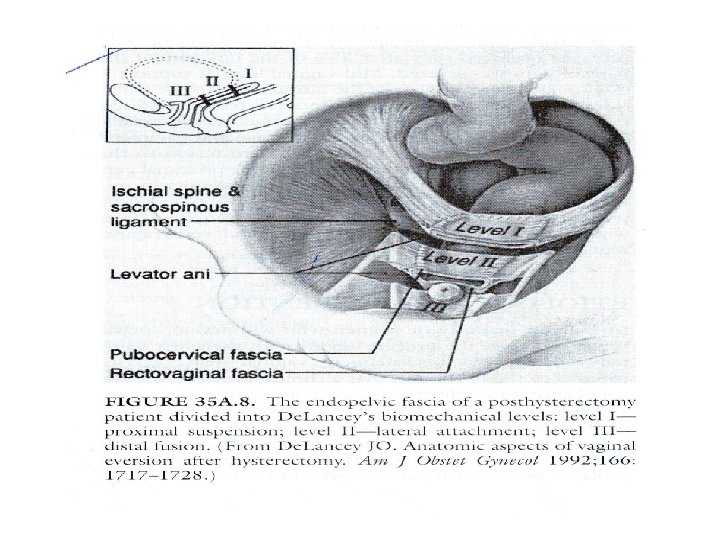
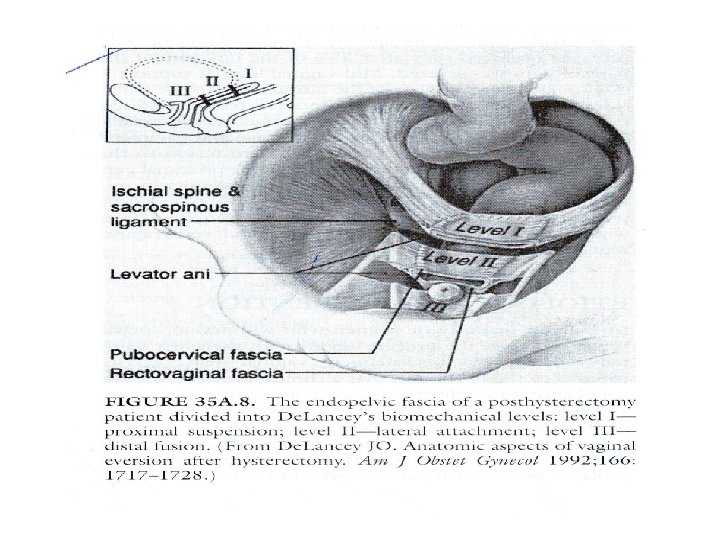
De Lancey s levels of vaginal support ● Level 1 - suspension by ligaments of paracolpium. damage to it results in uterovaginal prolapse, post hysterectomy vaginal prolapse, enterocele. the cause is at or above the level of ischial spines. primary loading bearing elements are uterosacral & lesser extent cardinal lig
● Level 2 - due to lateral attachment of fascial septa to pelvic sidewalls. the septa attach to arcus tendineus fascia pelvis & arcus tendineus fascia rectovaginalis. damage to it results in paravaginal & pararectal defects.
● Level 3 - attributed to fusion to the urogenital diaphragm anteriorly & proximal perineum posteriorly. damage to it result in urinary incontinence anteriorly & perineal body defects posteriorly. cystocele & rectocele are central defects.
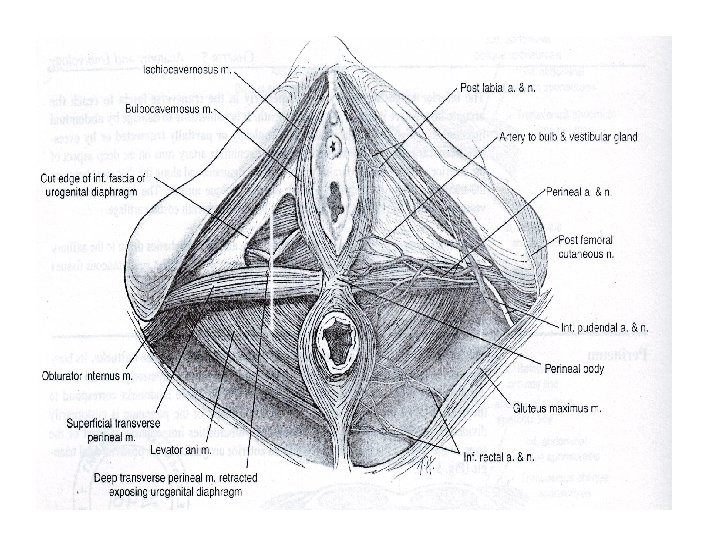
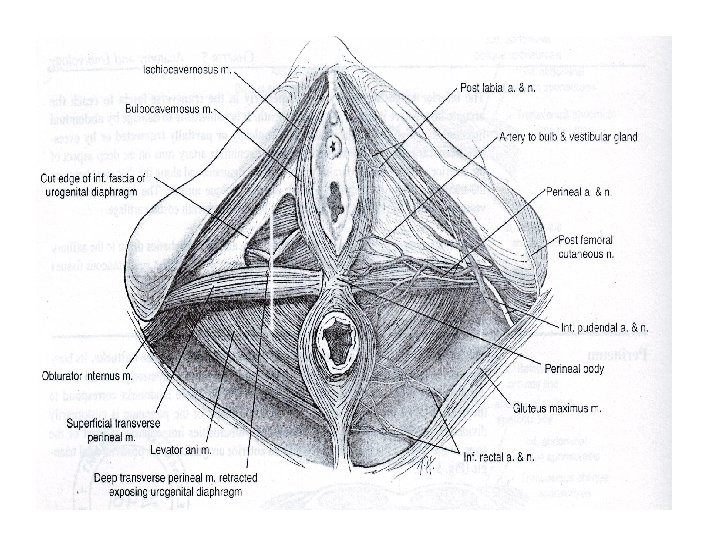
Urogenital diaphragm ● Also known as triangular ligament. ● Not so well developed in females as in males. ● Enclosed superiorly & inferiorly by fascia through which urethra & vagina pass. ● Inferior fascia of the diaphragm is known as perineal membrane. ● It is triangular sheet of dense fibromuscular tissue that spans ant half of pelvic outlet. ● Muscles include deep transverse perinei sphincter urethrae ● Reinforce with pelvic diaphragm anteriorly.
Deep transverse perinei ● Origin- medial aspect of ischiopubic rami ● Insertion- lower part of the vaginal wall, ant fibres blend with those of sphincter urethrae. ● Action- steadies the central perineal tendon ● Nerve supply- perineal nerve s 2 -4.
Sphincter urethrae ● Origin- medial aspect of ischiopubic rami ● Insertion- urethra & vagina ● Action- compresses the urethra ● Nerve supply- perineal nerve s 2 -4
Applied anatomy ● Lower tier support for uterus along with pelvic diaphragm & perineal body. ● Perineal nerve injury cause atonicity of muscles- contributory factor for prolapse. ● Provides support to posterior vaginal wall by attaching perineal body & vagina and in turn perineal body to ischiopubic rami limiting downward
Perineal body ● Also known as central point of tendon. ● Triangle shaped structure ● Fibromuscular node situated in median plane about 1. 25 cms in front of anus. ● Formed by tendinous attachments of bulbocavernosus external anal sphincter superficial transverse perinei ● Central connection to both pelvic & urogenital diaphragm and posteriorly to anococcygeal raphe.
Applied anatomy ● Important in females for support of pelvic organs. ● May be damaged during childbirth resulting in prolapse of pelvic organs. ● In posterior colpoperineorrhaphy, the perineal body is artificially constructed.
Perineal tear ● First degree- involves remnants of hymen, fourchette, lower part of vagina & perineal skin. Perineal body is intact ● Second degree- involves posterior vaginal
● Third degree- involves post vaginal wall, perineal body, anal sphincter complex. excluding anal canal or rectum ● Fourth degree- involving anal sphincter complex with anal & rectal mucosa involvement.
Episiotomy ● Inflicted second degree perineal injury ● Structures cut are post vaginal wall sup & deep transverse perinei bulbospongiosus part of levator ani fascia covering these muscles transverse perineal branches of pudendal vessels & nerves subcutaneous tissue & skin
Uterine axis ● Anteverted position of uterus itself prevents the organ from sagging down through vagina. ● Increase in intra abd pressure tends to push uterus against bladder & pubis which further accentuates anteversion. ● Angle maintained by uterosacral & round ligament of uterus. ● Anteversion 90 degree and anteflexion 120 degree
● Roughly long axis of uterus corresponds to the axis of pelvic inlet ● And axis of vagina correspnds to axis of pelvic cavity & outlet. • Applied anatomy uterine prolapse usually starts with retroversion of uterus and hence its importance.
Round ligament of uterus ● Two fibromuscular flat bands 10 -12 cms long. ● Lies between 2 layers of broad lig anteroinferior to uterine tube. ● Begins at the lateral angle of uterus , runs forwards & laterally, passes through deep inguinal ring, traverses inguinal canal and merges with areolar tissues of labium majus after breaking up into thin filaments.
Applied anatomy ● It keeps the fundus of uterus pulled forwards & maintain the angle of anteversion against the backward pull of the uterosacral ligaments. ● Lymphatics from fundus of uterus pass along it to the superficial inguinal nodes. ● Round ligament is plicated to facilitate anteversion in conservative
Endopelvic fascia ● Connective tissue of the pelvis ● Consists of loose areolar tissue containing varying aounts of smooth muscle. ● Bounded above- peritoneum below- sup fascia covering levator ani lateral- pelvic wall fascia medial- supports & invests midline organs such as uterus & upper part of vagina. ● At various locations act as loose areolar tissue capable of distension, neurovascular sheaths, septa & ligaments that support & separate the pelvic organs.
● Between different layers are bloodless spaces which are important to identify in vaginal plastic operations & oncosurgery. ● Endopelvic fascia divided into 3 parts parietal fascia- obturator, levator ani, coccygeus & piriformis visceral fascia deep endopelvic connective tissueuterosacral lig cardinal lig pubocervical & rectovaginal septum / fascia pericervical ring
Parietal pelvic fascia ● Obturator fascia- well defined in area superior to the arcus tendineus levator ani & below linea terminalis. it represents a vestigial portion of levator ani whose origin has been lowered through evolution to the level of muscular arch. ● Levator ani fascia- this fascia is continous across the pelvic floor blending laterally with obturator fascia at arcus tendineus levator ani and centrally with levator plate & visceral fascia at the urogenital hiatus.
● Coccygeus fascia (sacrospinous ligament)this important pelvic support structure extends from ischial spine lateraly to the sacrum medially. important alternative source of proximal support when uterosacral ligament is unavailable or insufficient. it is also important in repair of vault prolapse by transvaginal sacrospinous colpopexy. ● Piriformis fascia- this is the thinnest fascia and most posterior of the fascia of pelvis.
Visceral pelvic fascia ● These are loose highly elastic ill defined encasements of central pelvic organs which allow for high degree of physiologic distension necessitated by the function of pelvic organs. ● They blend intimately with organs that they encase. ● Structures invested by it are uterus, vagina, bladder & rectum. ● Structures not invested by it are fallopian tube, ovaries
Deep endopelvic connective tissue ● Central importance in the applied anatomy of pelvis & significant for pelvic reconstructive surgery. ● The six pericervical ligaments form the paracolpium. ● Net effect is suspension of the cervix in the posterior pelvis, placement of upper 2/3 rd of vagina directly over the levator plate and away from direct exposure to urogenital hiatus. ● In normal anatomic position, pressure from above tends to close the vaginal vault & results in no tendency towards prolapse.
● The two fascia/ septa & their supports when intact, the vaginal & rectal axis have a posterior angle of 30 degree at anterior point of their suspension over levator plate. ● Proximal 2/3 of vagina is nearly horizontal & suspended over levator plate. ● Distal 1/3 of vagina below puborectalis muscle, the vagina is nearly vertical as it passes through urogenital hiatus. ● The normal vaginal axis is oriented posteriorly toward a point just above the centre of 4 th sacral vertebrae which is at the level of origin uterosacral ligaments.
● The six pericervical ligaments are uterosacral lig cardinal lig pubocervical septum rectovaginal septum pericervical ring
Uterosacral ligaments ● Origin- periosteum of sacral vertebrae 2, 3 & 4 ● Insertion- on the posterior & lateral supravaginal cervix at 5 & 7 o ‘clock position. It is continous with & form part of pericervical ring. ● Neurologic content- uterosacral plexus of autonomic nerves ● Vascular content- minimal ● Muscular content- rectouterine muscle
● Function- these are primary proximal suspensory elements of uterovaginal complex. they hold the cervix in posterior pelvis at the level of ischial spines with the uterus in anteflexion and the vagina suspended over levator plate. the uterosacral lig blend as continous structure superiorly & laterally with cardinal ligaments and
Cardinal ligaments ● Origin- lateral pelvic walls ● Insertion- inserted on the lateral supravaginal cervix at 3 & 9 o’ clock positions. It is also continous with & form part of pericervical ring. ● Neurologic content- portions of uterosacral plexus ● Vascular content- cervical branch of uterine artery & veins. ● Muscular content- minimal smooth muscle content.
● Urinary- distal ureter passes under uterine artery within the superior portion of cardinal ligament. ● Function- these are the primary vascular conduits ot the uterus & vagina, provide lateral stabilization to the cervix at the level of ischial spines.
Applied anatomy of endopelvic fascia ● The ureter passes through the parametrium via ureteric tunnel in an anteroposterior direction about 1 cm lateral to cervix to reach the bladder. and passes below the level of uterine vessels which cross the ureter as they run transversely through the pelvis to reach uterus. ● Sympathetic nerve ganglia & nerve fibres are plentiful in parametrium. ● Lymphatics from upper 2/3 rd of vagina & uterus fallopian tube pass through pelvic cellular tissue.
● In CA Cervix > stage 2 b cancer cells infiltrate the parametrium and spread laterally along cardinal ligament and posteriorly along uterosacral ligaments. ● Factors which prevent prolapse of pelvic organs are seen in cases such as endometriosis cancerous spread to endopelvic fascia after radiotherapy pelvic tumor preventing the descent.
● ● Blood supply The uterus is supplied by arterial blood both from the uterine artery and the ovarian artery. Another anastomotic branch may also supply the uterus from anastomosis of these two arteries. Nerve supply Afferent nerves supplying uterus are T 11 and T 12. Sympathetic supply is from hypogastric plexus[disambiguation needed] and ovarian plexus. Parasympathetic supply is from second, third and fourth sacral nerves.
References ● Te Lindes operative gynecology ● Novak s gynecology ● Shaw s Text book of gynecology ● Gray s anatomy ● Chaurasia s human anatomy ● Dutta obstetrics & gynecology Textbook
THANK YOU
 Pear-shaped organ
Pear-shaped organ A sac shaped like an upside down pear with a thick lining
A sac shaped like an upside down pear with a thick lining Gall sac
Gall sac Cam and follower mechanism examples
Cam and follower mechanism examples Pear shaped pad mandible
Pear shaped pad mandible Sublingual artery
Sublingual artery Lingual bar vs lingual plate
Lingual bar vs lingual plate Anterior palatal strap
Anterior palatal strap Maxillary tuberosity
Maxillary tuberosity Major and minor retainer
Major and minor retainer Importance of retromylohyoid fossa
Importance of retromylohyoid fossa Difference between strength and endurance
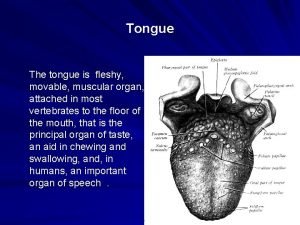
Difference between strength and endurance The fleshy muscular organ that helps in speaking
The fleshy muscular organ that helps in speaking J shaped muscular bag
J shaped muscular bag J shaped muscular sac
J shaped muscular sac J shaped muscular bag
J shaped muscular bag Tissues group together to form
Tissues group together to form Penyusun sistem saraf pusat adalah
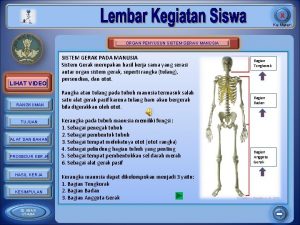
Penyusun sistem saraf pusat adalah Organ penyusun sistem gerak adalah ….
Organ penyusun sistem gerak adalah …. Organ and organ system
Organ and organ system Cell tissue organ organ system organism
Cell tissue organ organ system organism Tractus respiratorius
Tractus respiratorius Splenactomy
Splenactomy City and guilds walled garden
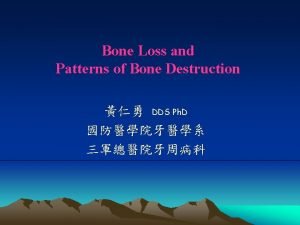
City and guilds walled garden Bone loss and patterns of bone destruction
Bone loss and patterns of bone destruction Lymphatic capillaries are thin-walled closed-ended tubes
Lymphatic capillaries are thin-walled closed-ended tubes Hapa hatchery
Hapa hatchery Thin walled rectangular pressure vessel
Thin walled rectangular pressure vessel Walled world map
Walled world map Hotspot server profile mikrotik
Hotspot server profile mikrotik City & guilds walled garden
City & guilds walled garden Walled city
Walled city Thin walled hollow cylinder moment of inertia
Thin walled hollow cylinder moment of inertia Atlanta kriterleri
Atlanta kriterleri Thin walled hollow cylinder moment of inertia
Thin walled hollow cylinder moment of inertia Eduqas electronics a level
Eduqas electronics a level Epa
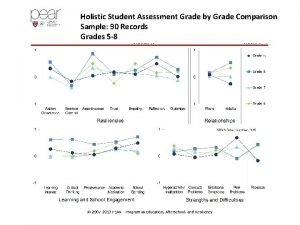
Epa Pear holistic student assessment
Pear holistic student assessment Pear paragraphs
Pear paragraphs Pear process effectiveness assessment report
Pear process effectiveness assessment report As9101e
As9101e Ways to refuse peer pressure
Ways to refuse peer pressure Pear deck powerpoint
Pear deck powerpoint Pear deck with powerpoint
Pear deck with powerpoint How to write a pear paragraph
How to write a pear paragraph Do you like pears
Do you like pears Partridge in a pear tree
Partridge in a pear tree Pear deck join.com
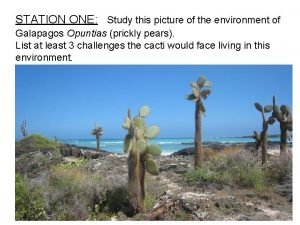
Pear deck join.com Prickly pear reproduction
Prickly pear reproduction Nonsense rhymes examples
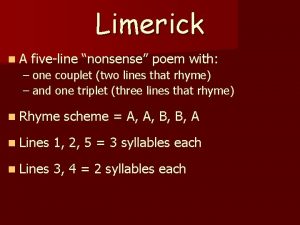
Nonsense rhymes examples Powerpoint pear deck
Powerpoint pear deck Pear placentation
Pear placentation Pear deck examples
Pear deck examples Pear deck add in powerpoint
Pear deck add in powerpoint Creative wonders
Creative wonders Cakes countable or uncountable
Cakes countable or uncountable Pear paragraph structure
Pear paragraph structure Pear theraputics
Pear theraputics Pear model faa
Pear model faa Pomegranate seed dispersal
Pomegranate seed dispersal Pear deck
Pear deck Pear deck for powerpoint
Pear deck for powerpoint