Muscular Dystrophies What is Muscular Dystrophy MD Muscular
- Slides: 35
Muscular Dystrophies
What is Muscular Dystrophy? (MD) • Muscular Dystrophy is a group of genetic disorders that cause progressive muscle weakness. • MD is caused by a genetic mutation. The protein in the muscle is deformed which causes the patients muscle to deteriorate. • MD is characterized by degeneration and regeneration of muscle fibers (in contrast with static or structural myopathies) progressive skeletal muscle weakness, defects in muscle proteins, and the death of muscle cells and tissue
Symptoms • Lack of coordination • Muscle weakness • Loss of mobility
General Diagnostic Testing • Creatine kinase : – greatly elevated (50 times normal) – Increased in DMD, BMD, polymyositis, and rhabdomyolysis – Nonspecific if mildly elevated 2 -3 x normal – Lower late in MD course due to severely reduced muscle mass – Not helpful for carrier detection
General Diagnostic Testing • Electromyography – Useful if diagnosis not clear (biopsy has mixed features) – Differentiates neuropathic vs. myopathic – Characteristic myotonic discharges in adults with myotonia – “dive bomber” sound – Perform after the CK
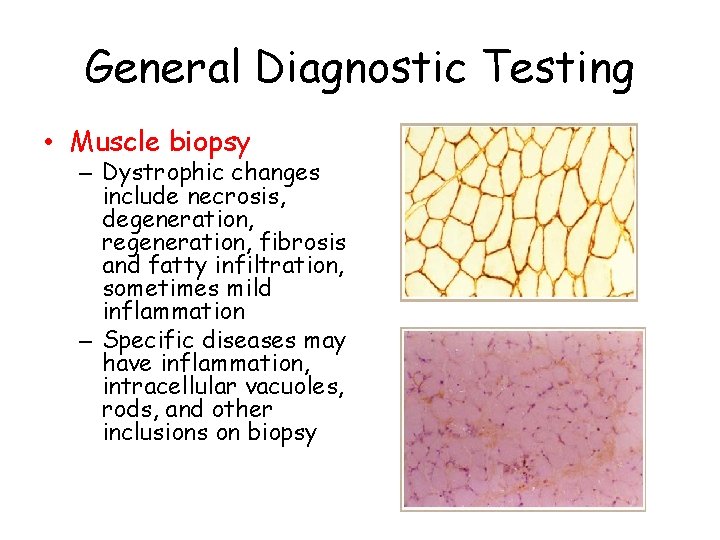
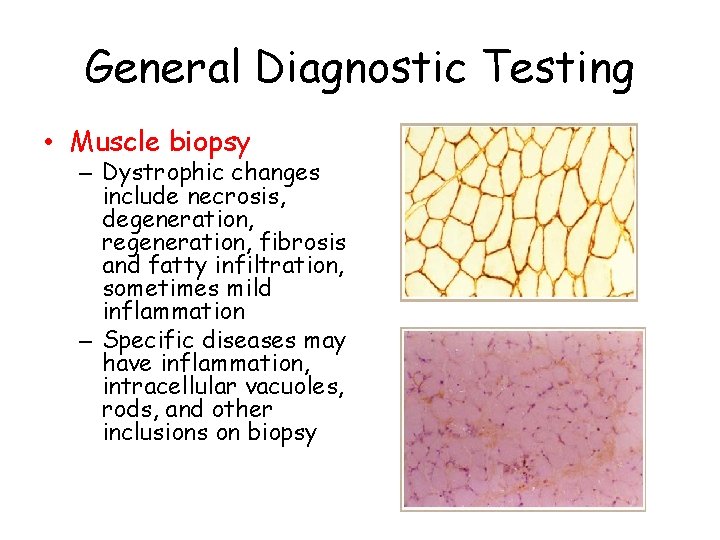
General Diagnostic Testing • Muscle biopsy – Dystrophic changes include necrosis, degeneration, regeneration, fibrosis and fatty infiltration, sometimes mild inflammation – Specific diseases may have inflammation, intracellular vacuoles, rods, and other inclusions on biopsy
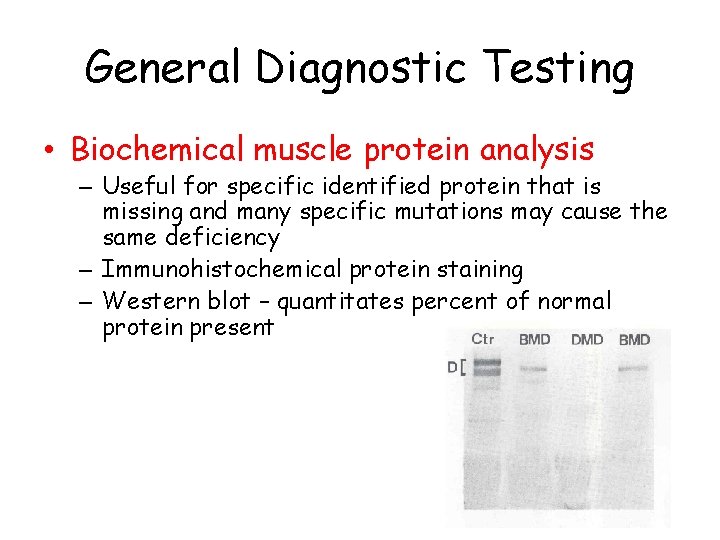
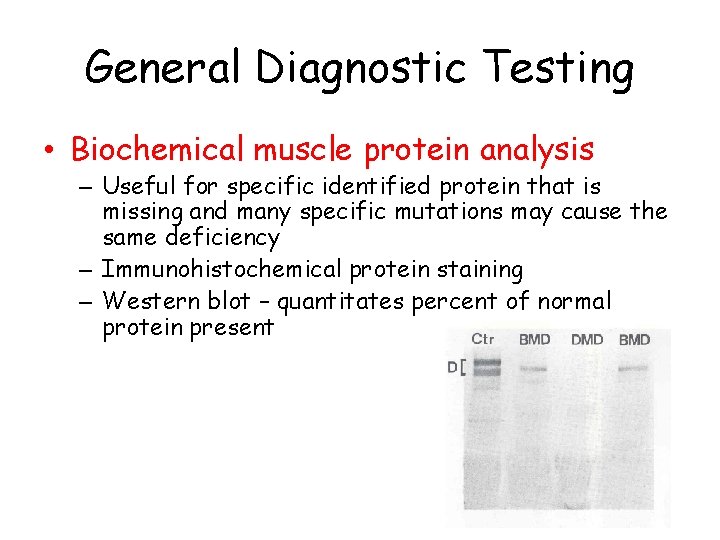
General Diagnostic Testing • Biochemical muscle protein analysis – Useful for specific identified protein that is missing and many specific mutations may cause the same deficiency – Immunohistochemical protein staining – Western blot – quantitates percent of normal protein present
General Diagnostic Testing • Genetic analysis – PCR for specific known defects – Southern blot for nucleotide repeats
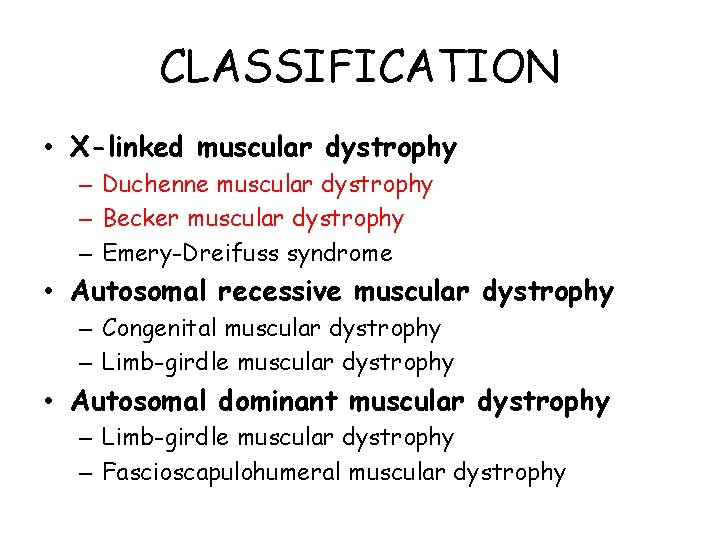
CLASSIFICATION • X-linked muscular dystrophy – Duchenne muscular dystrophy – Becker muscular dystrophy – Emery-Dreifuss syndrome • Autosomal recessive muscular dystrophy – Congenital muscular dystrophy – Limb-girdle muscular dystrophy • Autosomal dominant muscular dystrophy – Limb-girdle muscular dystrophy – Fascioscapulohumeral muscular dystrophy
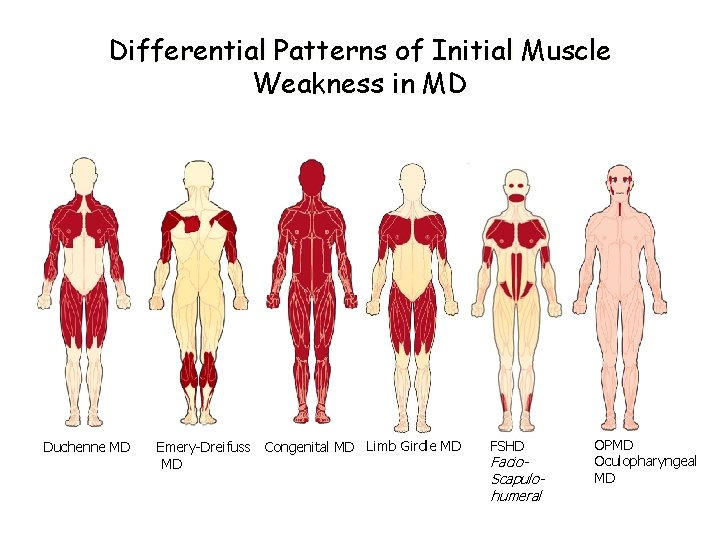
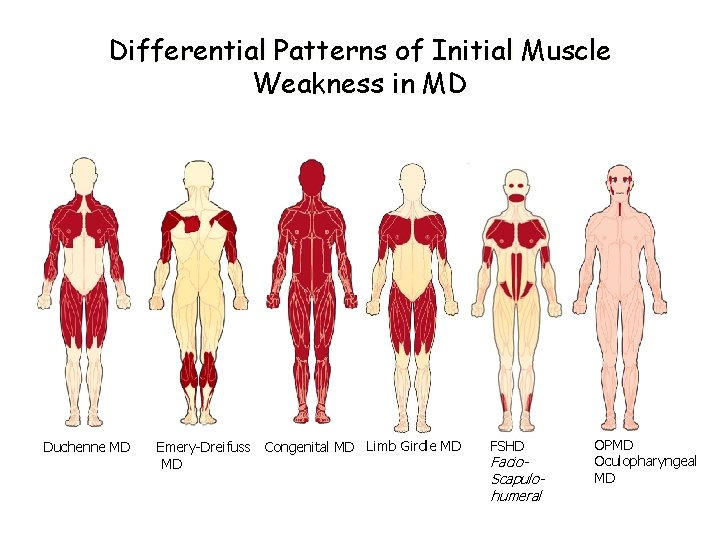
Differential Patterns of Initial Muscle Weakness in MD Duchenne MD Emery-Dreifuss Congenital MD Limb Girdle MD MD FSHD Facio. Scapulohumeral OPMD Oculopharyngeal MD
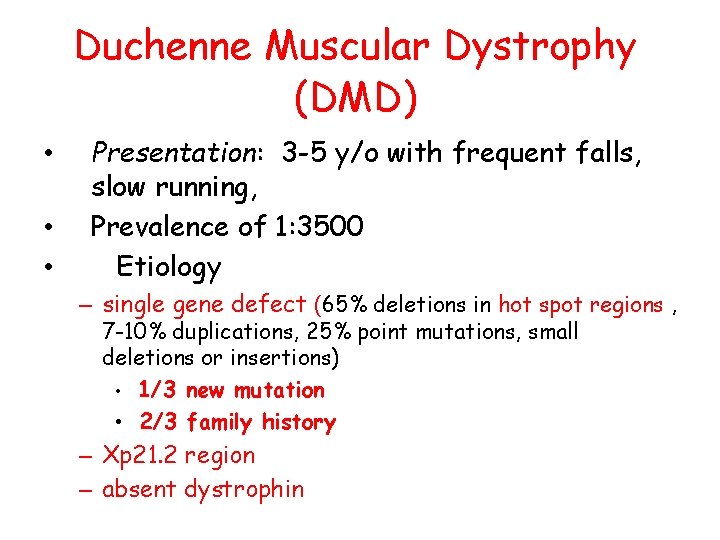
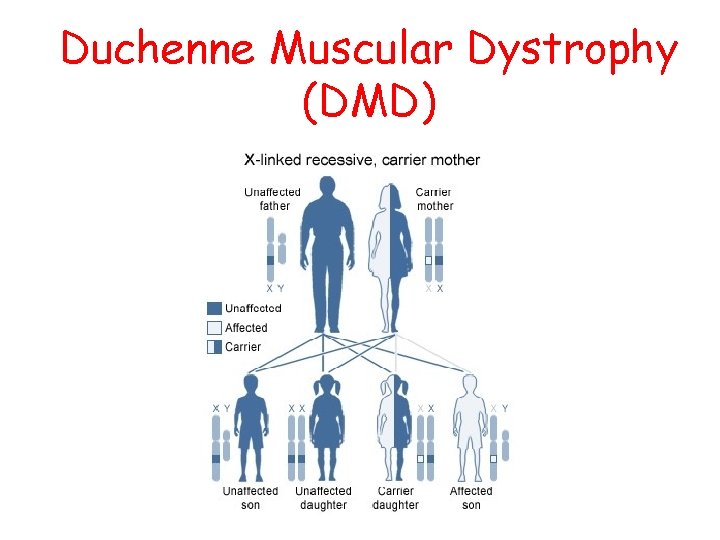
Duchenne Muscular Dystrophy (DMD) • • • Presentation: 3 -5 y/o with frequent falls, slow running, Prevalence of 1: 3500 Etiology – single gene defect (65% deletions in hot spot regions , 7 -10% duplications, 25% point mutations, small deletions or insertions) • 1/3 new mutation • 2/3 family history – Xp 21. 2 region – absent dystrophin
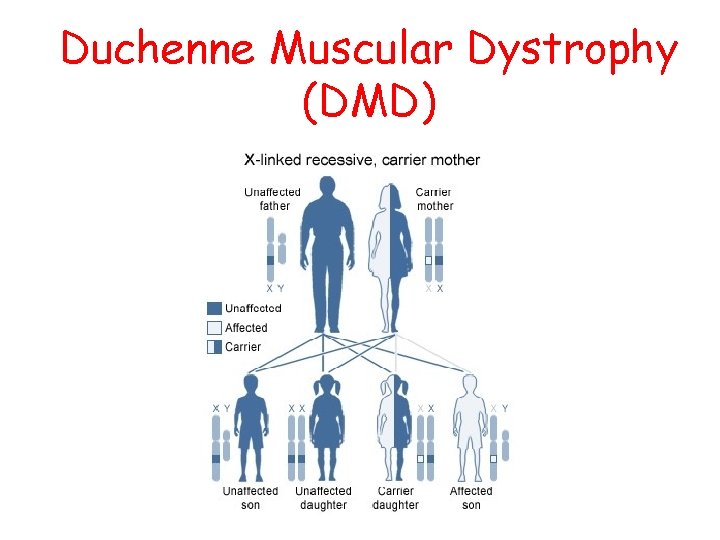
Duchenne Muscular Dystrophy (DMD)
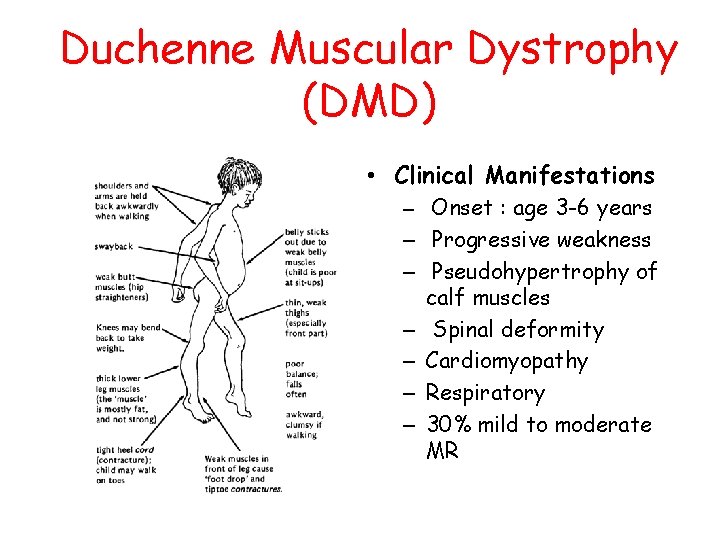
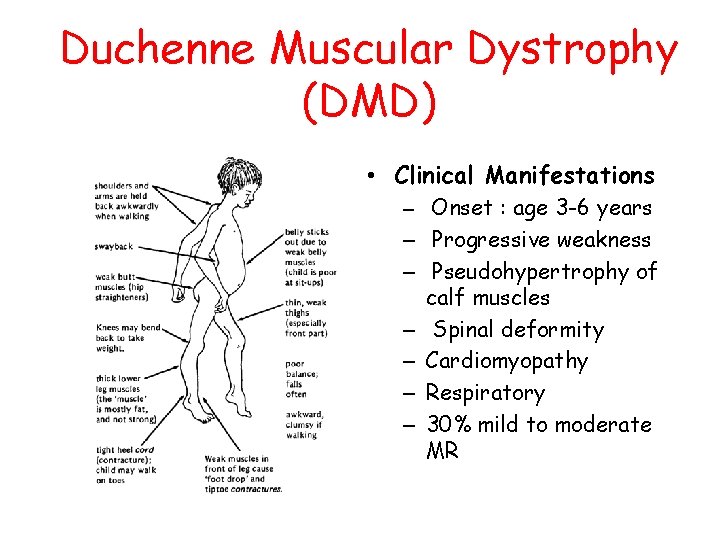
Duchenne Muscular Dystrophy (DMD) • Clinical Manifestations – Onset : age 3 -6 years – Progressive weakness – Pseudohypertrophy of calf muscles – Spinal deformity – Cardiomyopathy – Respiratory – 30% mild to moderate MR
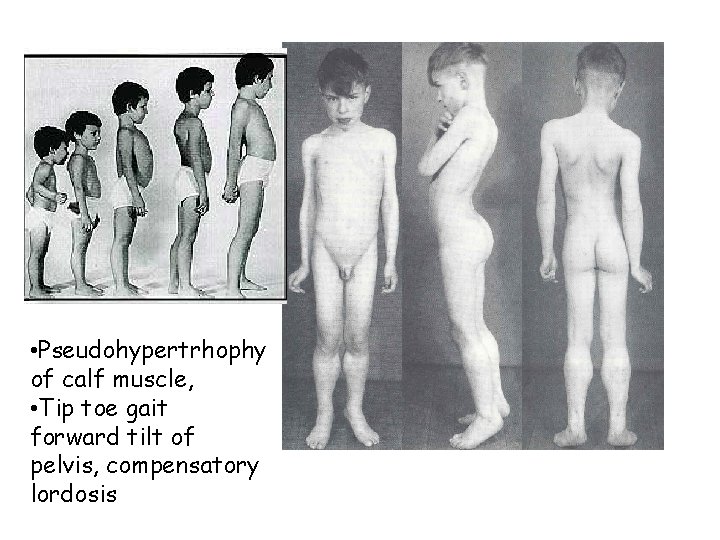
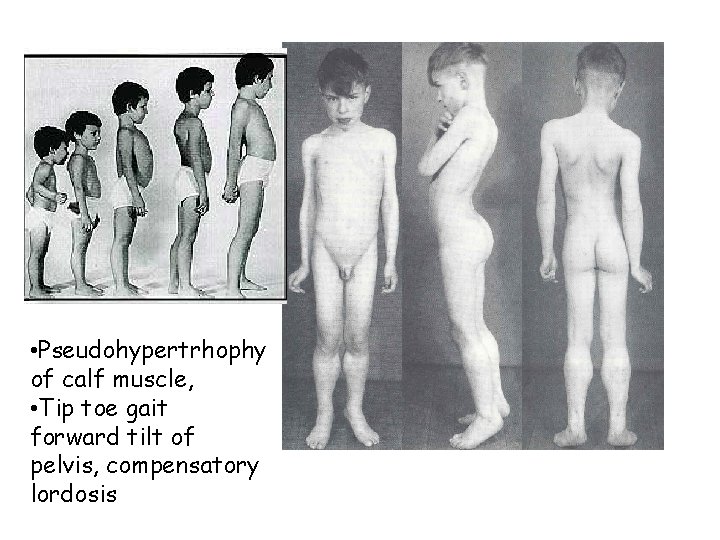
• Pseudohypertrhophy of calf muscle, • Tip toe gait forward tilt of pelvis, compensatory lordosis
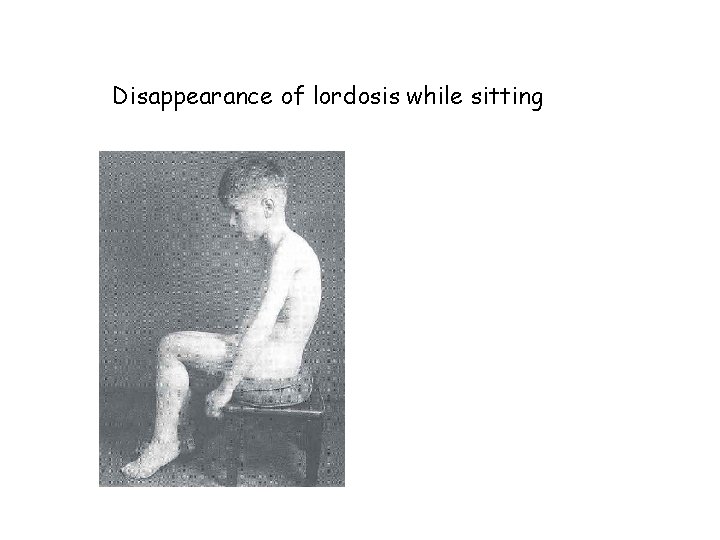
Disappearance of lordosis while sitting
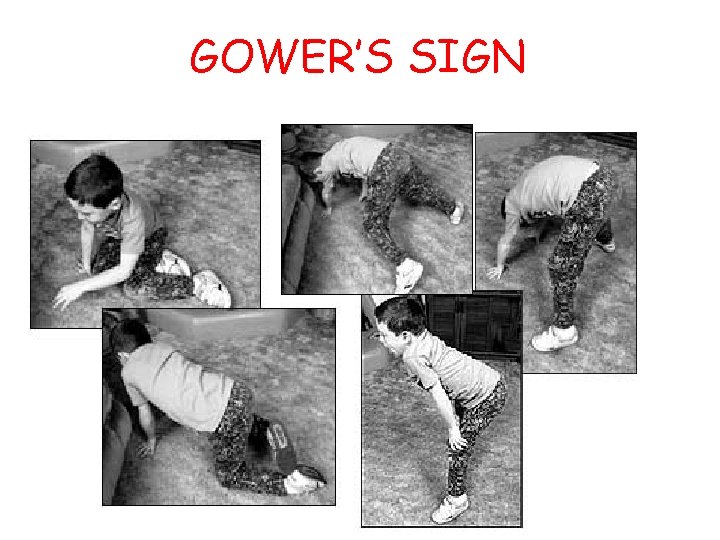
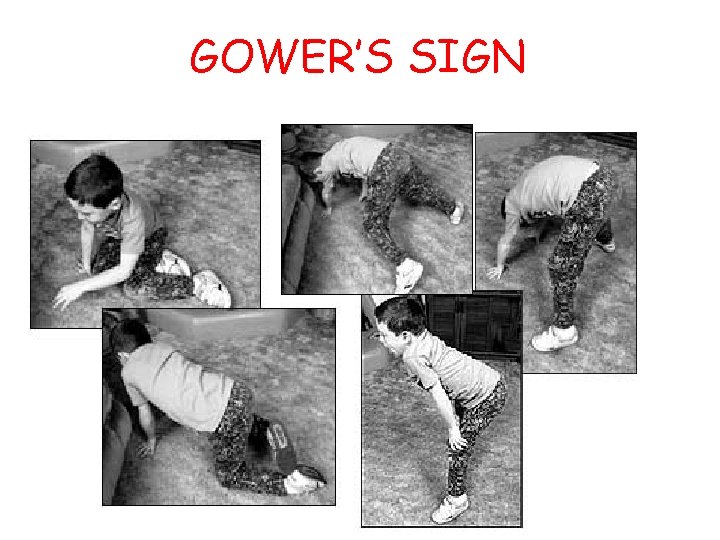
GOWER’S SIGN
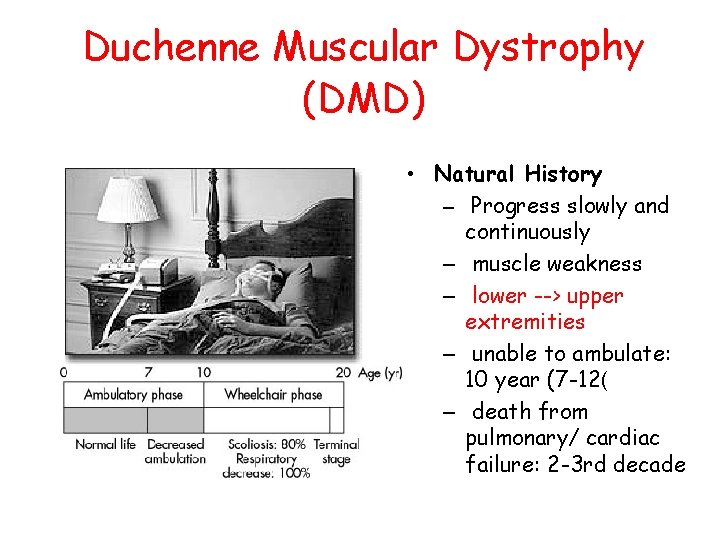
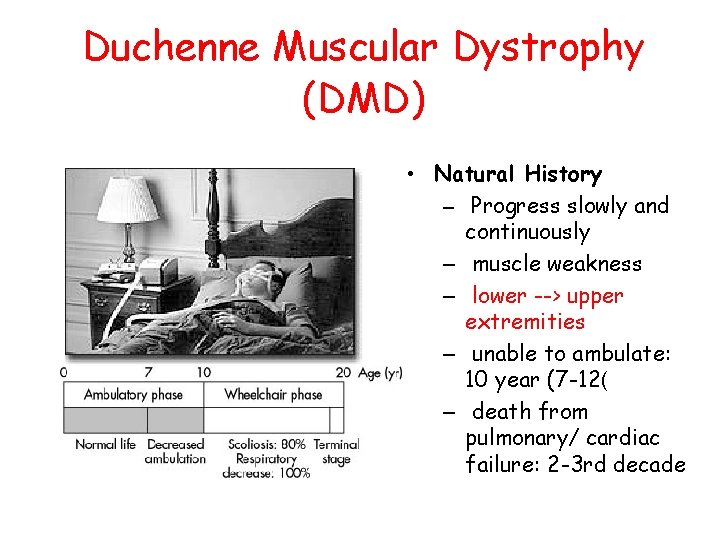
Duchenne Muscular Dystrophy (DMD) • Natural History – Progress slowly and continuously – muscle weakness – lower --> upper extremities – unable to ambulate: 10 year (7 -12( – death from pulmonary/ cardiac failure: 2 -3 rd decade
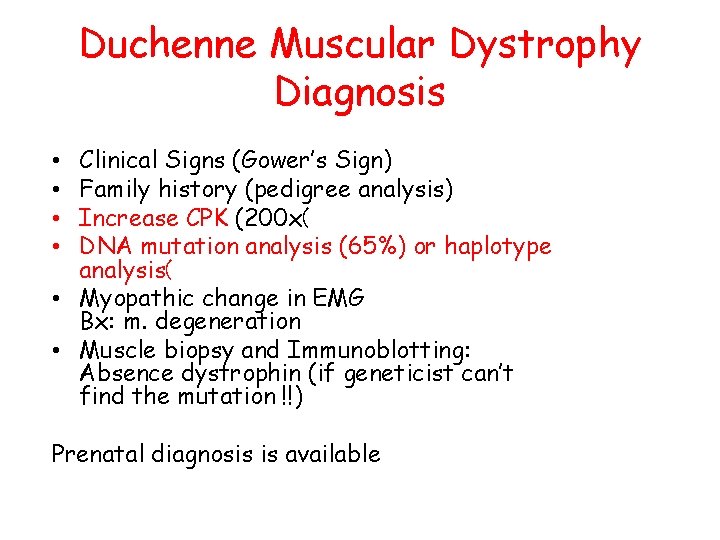
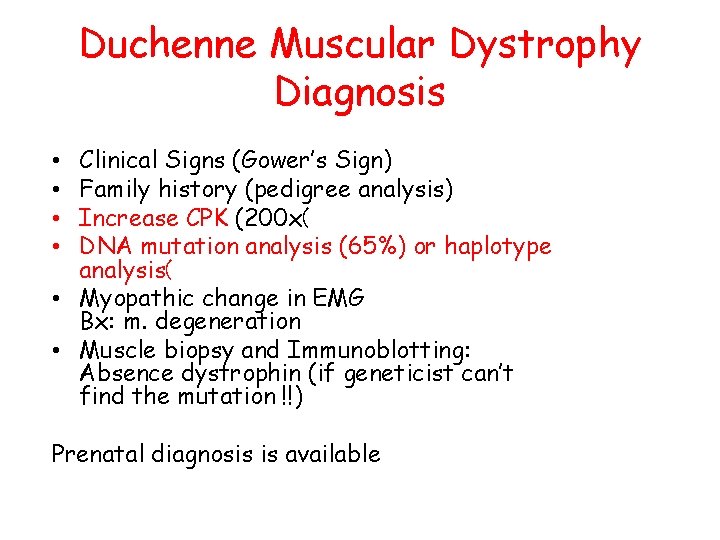
Duchenne Muscular Dystrophy Diagnosis Clinical Signs (Gower’s Sign) Family history (pedigree analysis) Increase CPK (200 x( DNA mutation analysis (65%) or haplotype analysis( • Myopathic change in EMG Bx: m. degeneration • Muscle biopsy and Immunoblotting: Absence dystrophin (if geneticist can’t find the mutation !!) • • Prenatal diagnosis is available
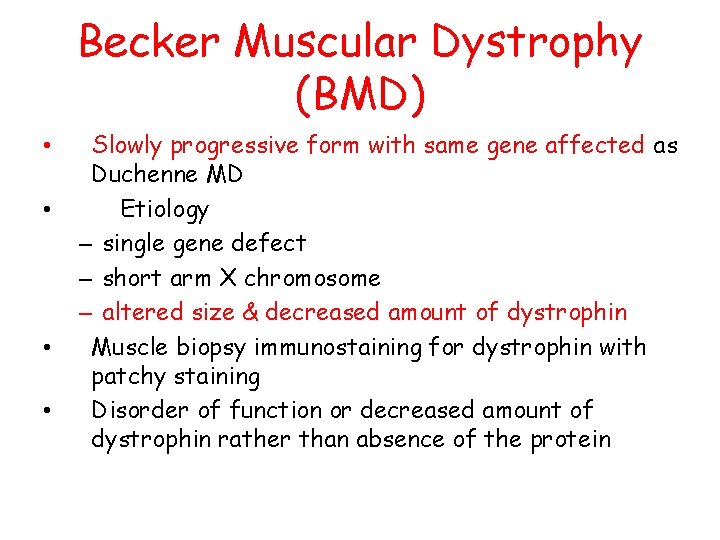
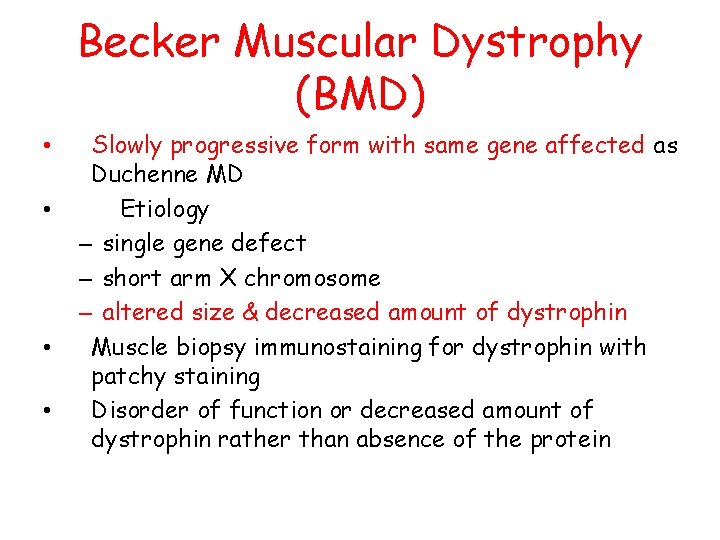
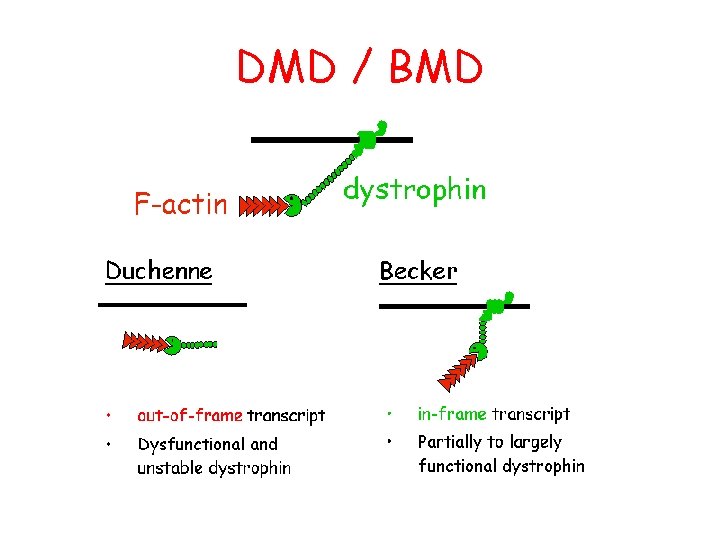
Becker Muscular Dystrophy (BMD) • • Slowly progressive form with same gene affected as Duchenne MD Etiology – single gene defect – short arm X chromosome – altered size & decreased amount of dystrophin Muscle biopsy immunostaining for dystrophin with patchy staining Disorder of function or decreased amount of dystrophin rather than absence of the protein
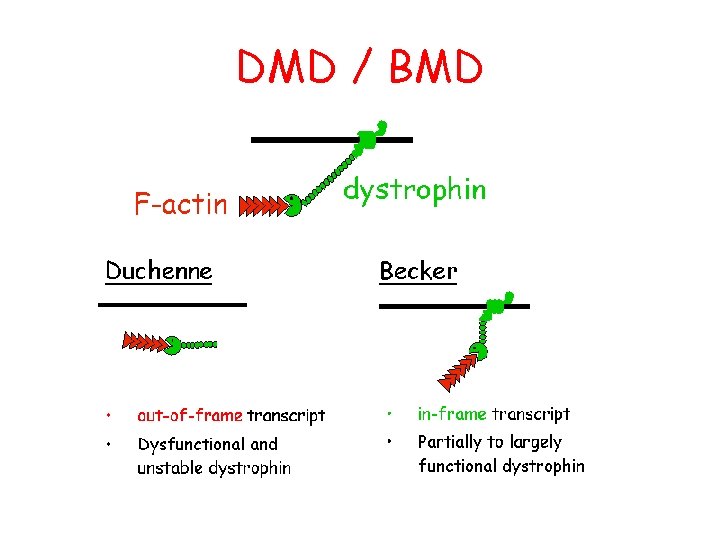
DMD / BMD
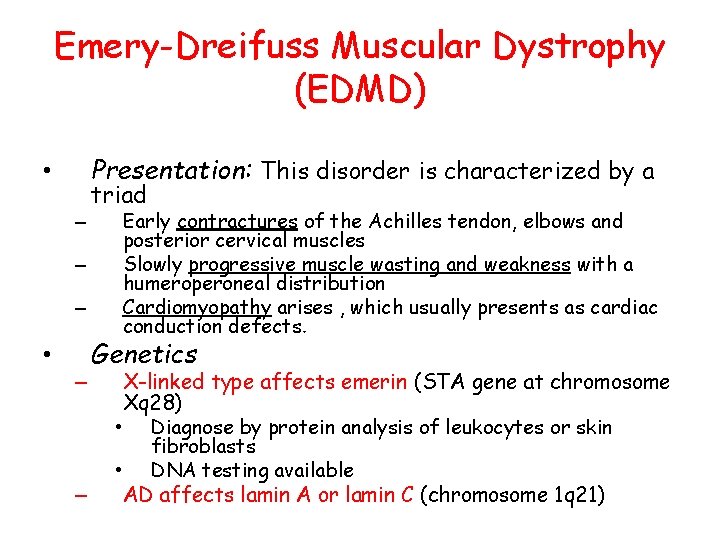
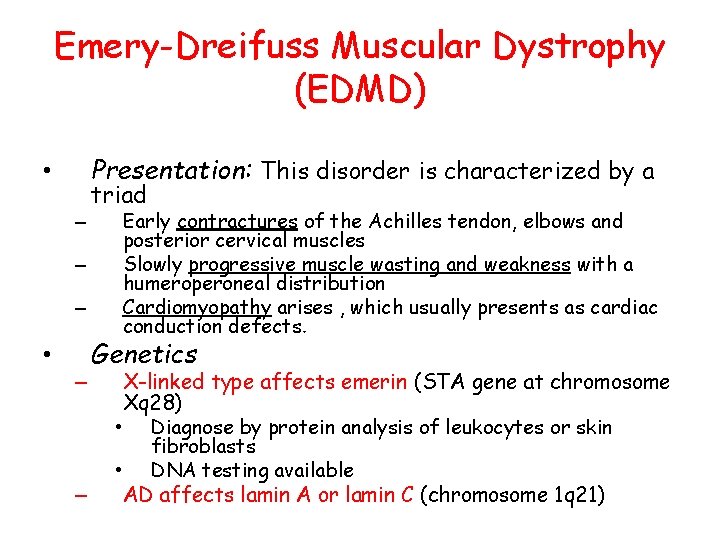
Emery-Dreifuss Muscular Dystrophy (EDMD) Presentation: This disorder is characterized by a • – – – • – – triad Early contractures of the Achilles tendon, elbows and posterior cervical muscles Slowly progressive muscle wasting and weakness with a humeroperoneal distribution Cardiomyopathy arises , which usually presents as cardiac conduction defects. Genetics X-linked type affects emerin (STA gene at chromosome Xq 28) • Diagnose by protein analysis of leukocytes or skin fibroblasts • DNA testing available AD affects lamin A or lamin C (chromosome 1 q 21)
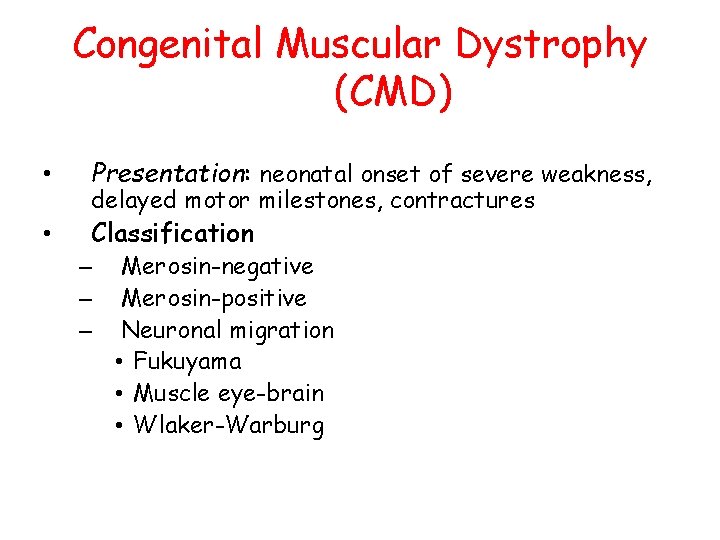
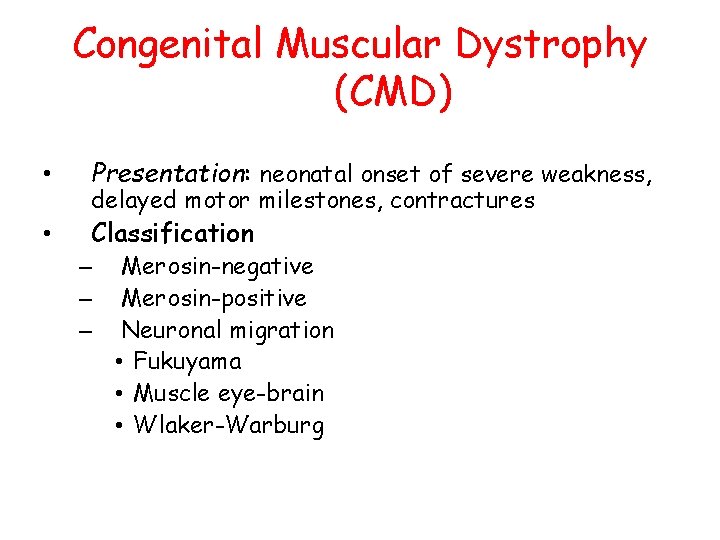
Congenital Muscular Dystrophy (CMD) • Presentation: neonatal onset of severe weakness, • Classification delayed motor milestones, contractures – – – Merosin-negative Merosin-positive Neuronal migration • Fukuyama • Muscle eye-brain • Wlaker-Warburg
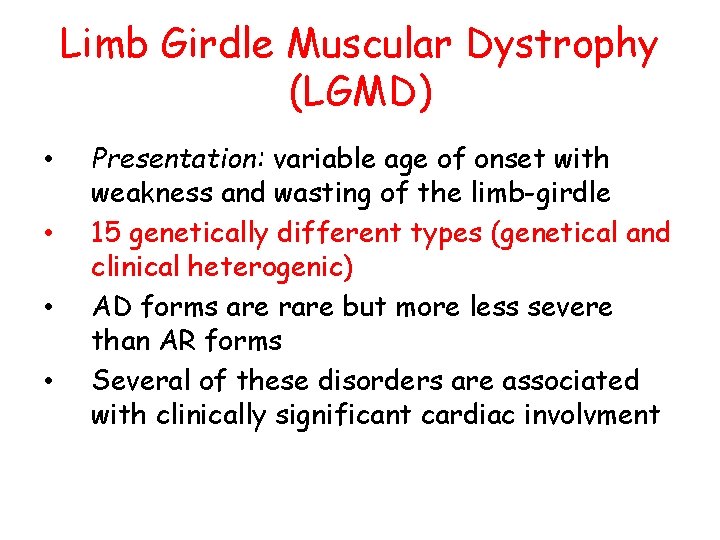
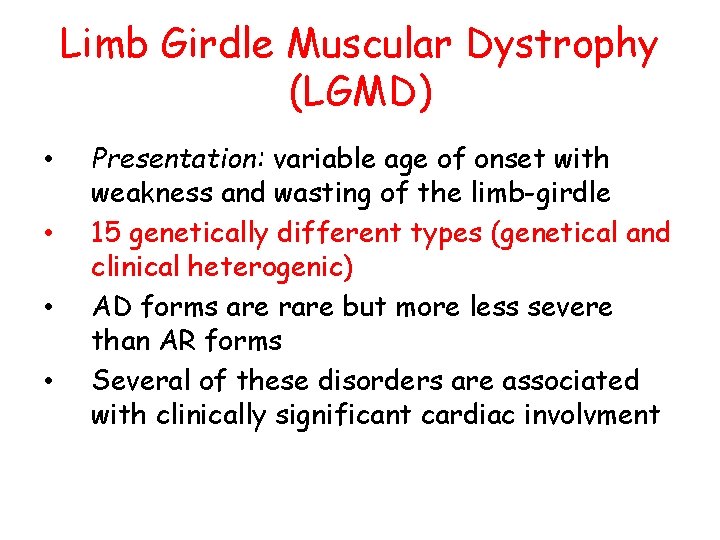
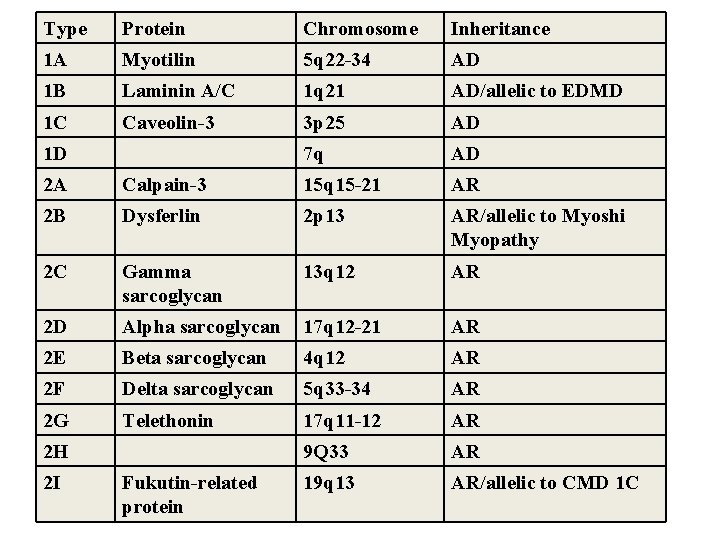
Limb Girdle Muscular Dystrophy (LGMD) • • Presentation: variable age of onset with weakness and wasting of the limb-girdle 15 genetically different types (genetical and clinical heterogenic) AD forms are rare but more less severe than AR forms Several of these disorders are associated with clinically significant cardiac involvment
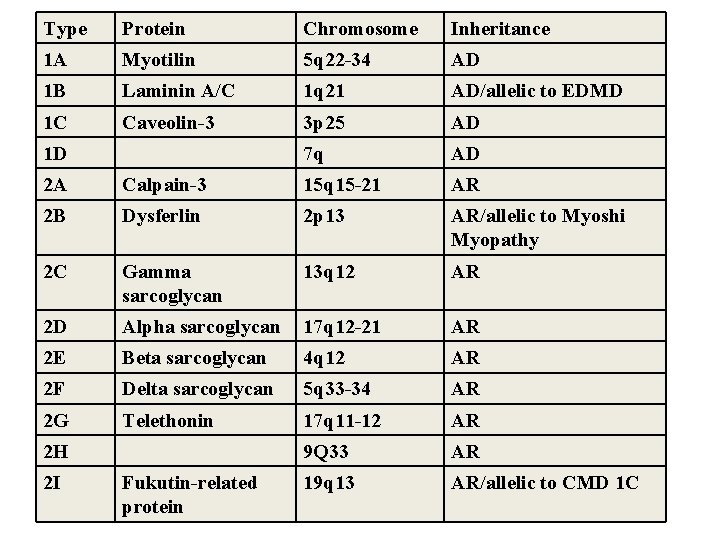
Type Protein Chromosome Inheritance 1 A Myotilin 5 q 22 -34 AD 1 B Laminin A/C 1 q 21 AD/allelic to EDMD 1 C Caveolin-3 3 p 25 AD 7 q AD 1 D 2 A Calpain-3 15 q 15 -21 AR 2 B Dysferlin 2 p 13 AR/allelic to Myoshi Myopathy 2 C Gamma sarcoglycan 13 q 12 AR 2 D Alpha sarcoglycan 17 q 12 -21 AR 2 E Beta sarcoglycan 4 q 12 AR 2 F Delta sarcoglycan 5 q 33 -34 AR 2 G Telethonin 17 q 11 -12 AR 9 Q 33 AR 19 q 13 AR/allelic to CMD 1 C 2 H 2 I Fukutin-related protein
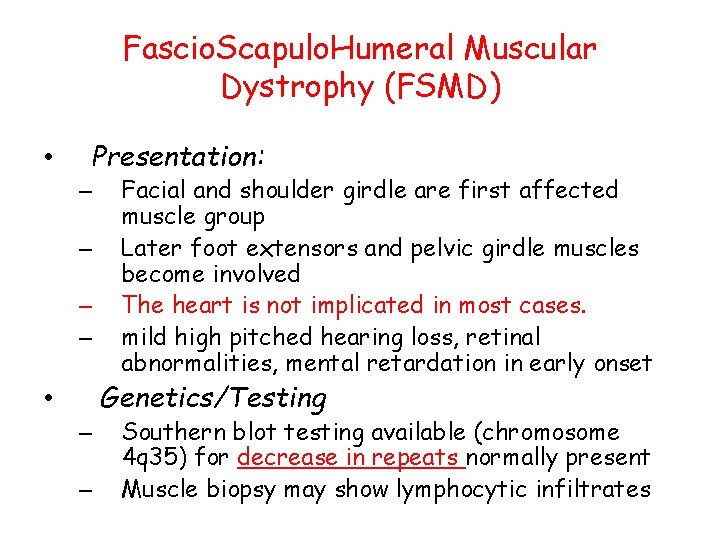
Fascio. Scapulo. Humeral Muscular Dystrophy (FSMD) • Presentation: – – Facial and shoulder girdle are first affected muscle group Later foot extensors and pelvic girdle muscles become involved The heart is not implicated in most cases. mild high pitched hearing loss, retinal abnormalities, mental retardation in early onset Genetics/Testing • – – Southern blot testing available (chromosome 4 q 35) for decrease in repeats normally present Muscle biopsy may show lymphocytic infiltrates
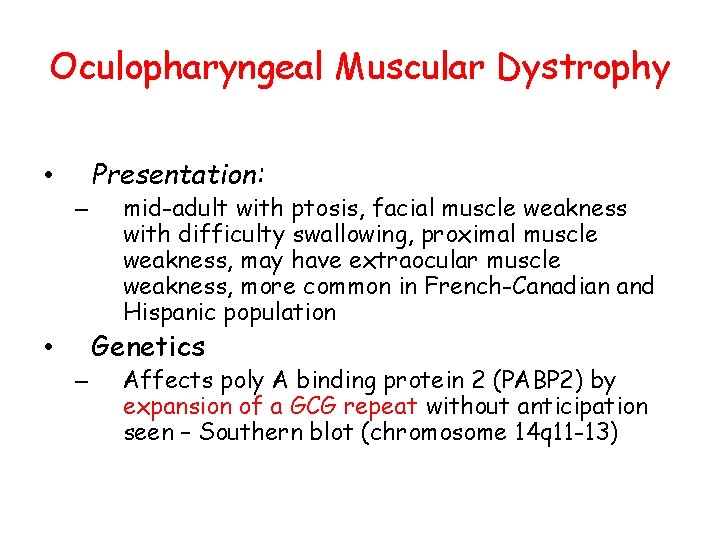
Oculopharyngeal Muscular Dystrophy Presentation: • – mid-adult with ptosis, facial muscle weakness with difficulty swallowing, proximal muscle weakness, may have extraocular muscle weakness, more common in French-Canadian and Hispanic population Genetics • – Affects poly A binding protein 2 (PABP 2) by expansion of a GCG repeat without anticipation seen – Southern blot (chromosome 14 q 11 -13)
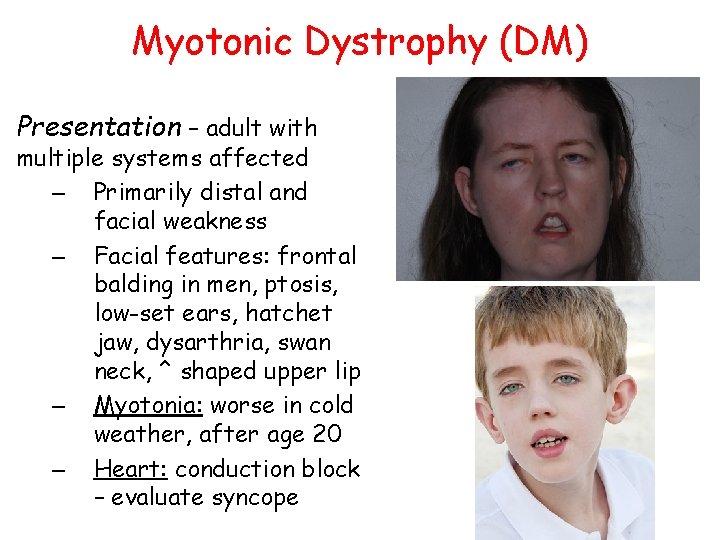
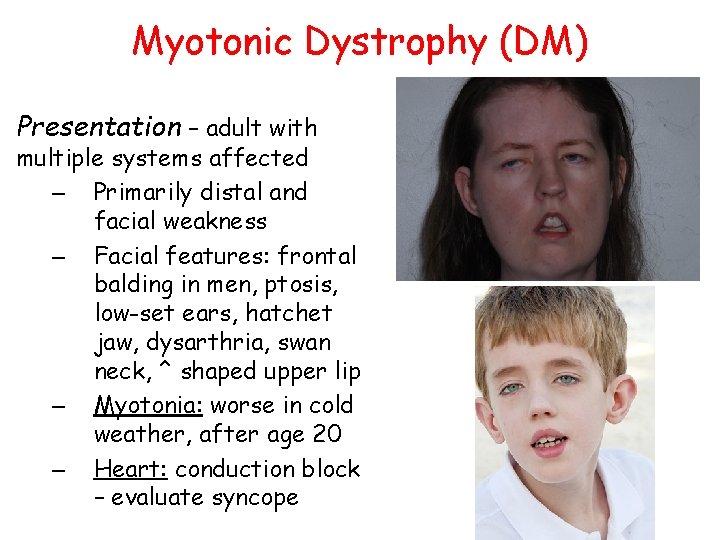
Myotonic Dystrophy (DM) Presentation – adult with multiple systems affected – Primarily distal and facial weakness – Facial features: frontal balding in men, ptosis, low-set ears, hatchet jaw, dysarthria, swan neck, ^ shaped upper lip – Myotonia: worse in cold weather, after age 20 – Heart: conduction block – evaluate syncope
– – Smooth muscle: constipation, care with swallowing, gallstones, problems with childbirth, BP lability Brain: learning disabilities, increased sleep requirement Ophthalmology: cataracts Endocrine: insulin resistance, hypothyroidism, testicular atrophy
Myotonic Dystrophy • Genetics • Myotonic dystrophy is caused by a triple nucleotide (triplet) expansion (CTG) in the noncoding region of the myotonin gene at chromosome 19 q 13. 3. • The condition is characterized by extreme variability, anticipation and differential expansion in the maternal and paternal germline. – 4 -37 repeats Normal – >50 repeats Affected
Myotonic Dystrophy (DM) • Congenital: severe form – initial respiratory distress after birth with ventilatory requirement or apnea, – feeding difficulty, – mental retardation, – club feet, scoliosis, – strabismus
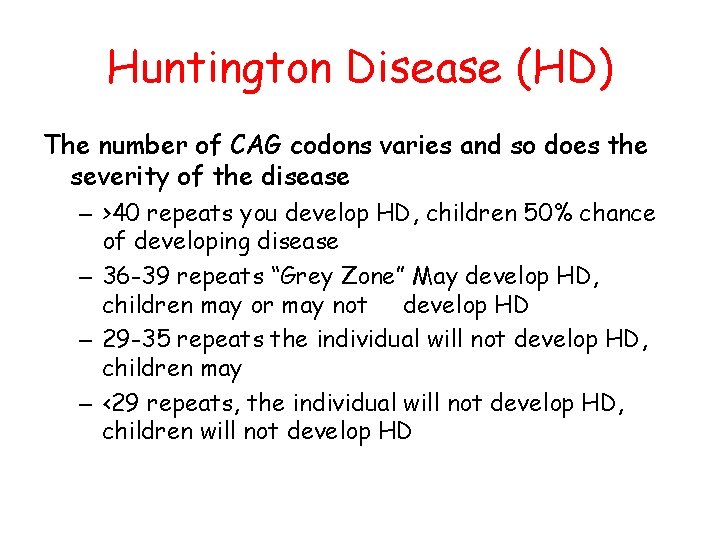
Huntington Disease (HD) • • • – – – Presentation Mood Swings Impaired cognitive functions Chorea Huntington’s Disease is an Autosomal Dominant “Trinucleotide Repeat” Disorder caused by a mutation of a gene on the 4 th chromosome which is responsible for producing the protein Huntingtin, that creates excess copies of the CAG codon which genetically program the degeneration of the neurons of the brain. Age of onset is found generally in adults around the age of 40 but varies based on the number of repeats. The earliest onset of Huntington’s ever documented was a two year old boy who was found to have nearly 100 CAG repeats. The symptoms of HD can also develop at 55 or later, in which case it is harder to recognize.
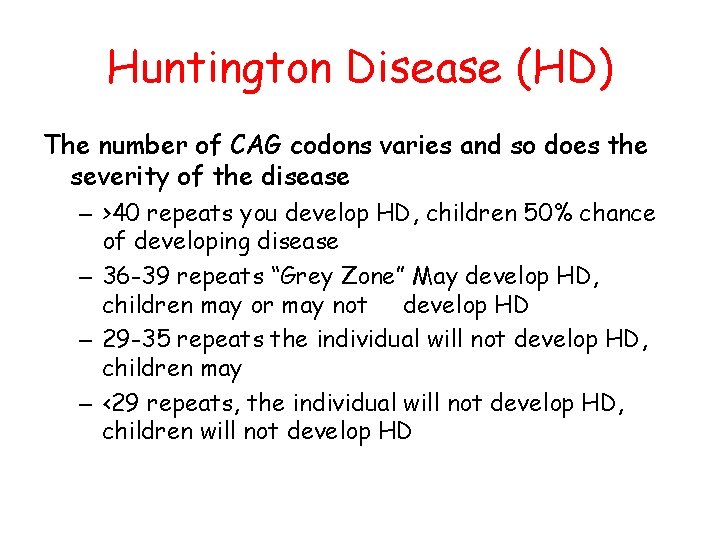
Huntington Disease (HD) The number of CAG codons varies and so does the severity of the disease – >40 repeats you develop HD, children 50% chance of developing disease – 36 -39 repeats “Grey Zone” May develop HD, children may or may not develop HD – 29 -35 repeats the individual will not develop HD, children may – <29 repeats, the individual will not develop HD, children will not develop HD
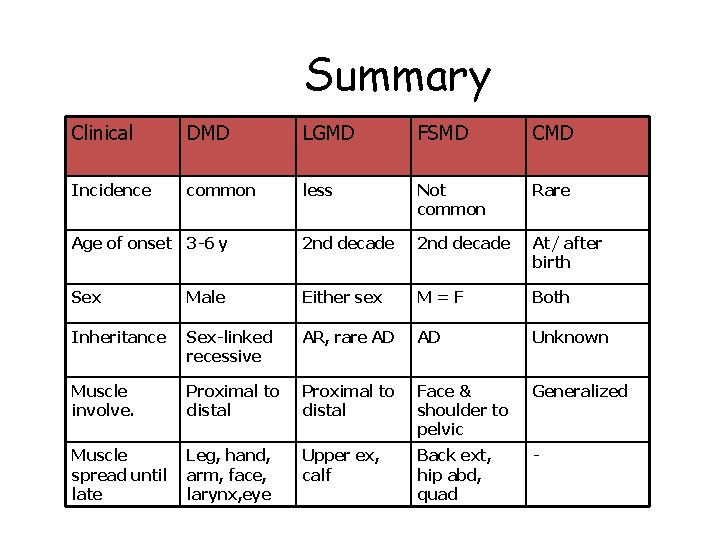
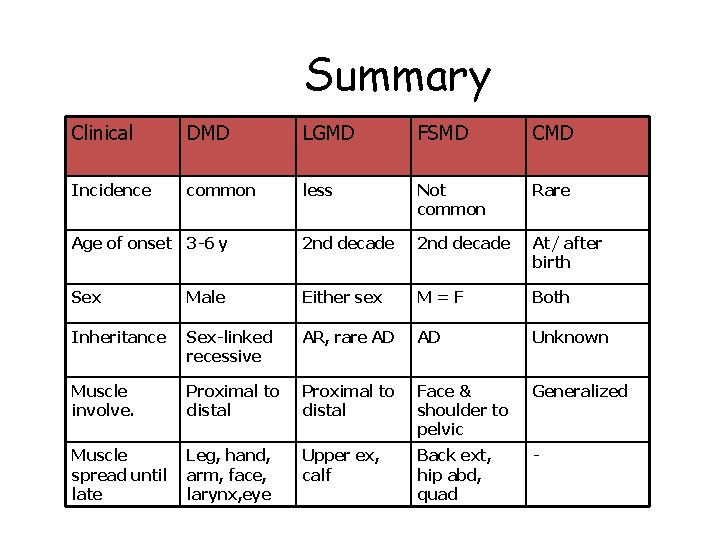
Summary Clinical DMD LGMD FSMD CMD Incidence common less Not common Rare Age of onset 3 -6 y 2 nd decade At/ after birth Sex Male Either sex M=F Both Inheritance Sex-linked recessive AR, rare AD AD Unknown Muscle involve. Proximal to distal Face & shoulder to pelvic Generalized Muscle spread until late Leg, hand, arm, face, larynx, eye Upper ex, calf Back ext, hip abd, quad -
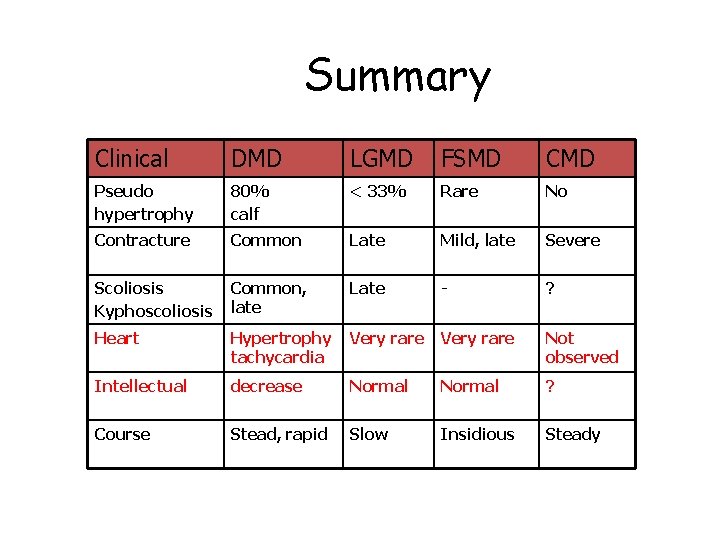
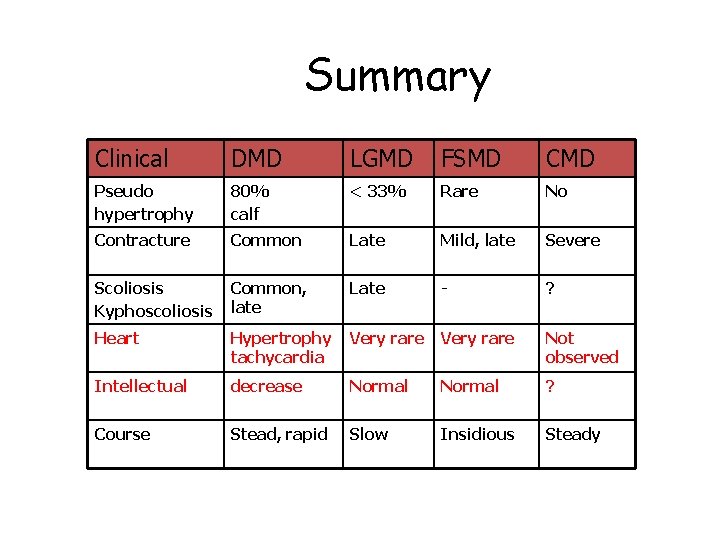
Summary Clinical DMD LGMD FSMD CMD Pseudo hypertrophy 80% calf < 33% Rare No Contracture Common Late Mild, late Severe Scoliosis Kyphoscoliosis Common, late Late - ? Heart Hypertrophy tachycardia Very rare Not observed Intellectual decrease Normal ? Course Stead, rapid Slow Insidious Steady
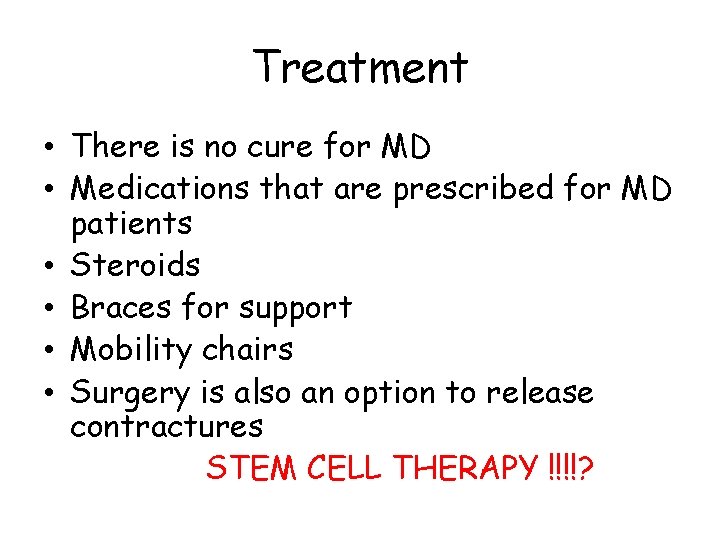
Treatment • There is no cure for MD • Medications that are prescribed for MD patients • Steroids • Braces for support • Mobility chairs • Surgery is also an option to release contractures STEM CELL THERAPY !!!!?
 Genetics
Genetics Duchenne muscular dystrophy
Duchenne muscular dystrophy Signs of duchenne muscular dystrophy
Signs of duchenne muscular dystrophy The pedigree below tracks the presence of dimples
The pedigree below tracks the presence of dimples Gowers sign
Gowers sign Duchenne
Duchenne Becker muscular dystrophy
Becker muscular dystrophy Jon durrani
Jon durrani Duchenne muscular dystrophy
Duchenne muscular dystrophy Limb girdle muscular dystrophy
Limb girdle muscular dystrophy Dr katie green
Dr katie green Duchenne muscular dystrophy
Duchenne muscular dystrophy Muscular dystrophy definition
Muscular dystrophy definition Mooren ulcer
Mooren ulcer Myotonic dystrophy type 2 vs type 1
Myotonic dystrophy type 2 vs type 1 Vulvar dystrophy thyroid
Vulvar dystrophy thyroid Keratoglobus vs keratoconus
Keratoglobus vs keratoconus Oil droplet reflex
Oil droplet reflex Corneal dystrophy mnemonic
Corneal dystrophy mnemonic Differentiate muscular strength from muscular endurance
Differentiate muscular strength from muscular endurance Entrenamiento fisico
Entrenamiento fisico Chapter 7:5 muscular system
Chapter 7:5 muscular system Tono muscular
Tono muscular Suprasternal notch
Suprasternal notch Muscles
Muscles 2 functions of muscles
2 functions of muscles Organo tendinoso de golgi y huso muscular
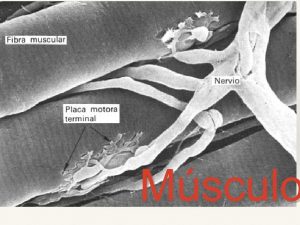
Organo tendinoso de golgi y huso muscular Muscular pectinati
Muscular pectinati Tubulos sarcoplasmicos longitudinales
Tubulos sarcoplasmicos longitudinales Whats the job of the muscular system
Whats the job of the muscular system Microscopic anatomy of skeletal muscle figure 6-2
Microscopic anatomy of skeletal muscle figure 6-2 Muscular contraction
Muscular contraction Contracción muscular pasos
Contracción muscular pasos Tenar e hipotenar
Tenar e hipotenar Chapter 9 muscular system
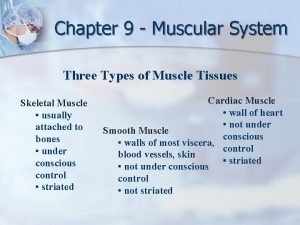
Chapter 9 muscular system Diadas musculo cardiaco
Diadas musculo cardiaco