Muscle Dystrophy Jon Durrani DO Attending Neurologist Dayton
- Slides: 33
Muscle Dystrophy Jon Durrani, DO Attending Neurologist Dayton Center for Neurologic Disorders
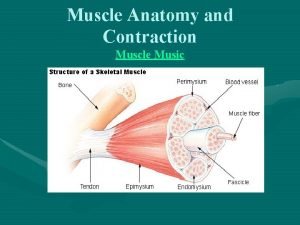
What is Muscle Dystrophy? • Essentially a group of muscle wasting disorders that cause a breakdown and subsequent of skeletal muscle over time. • There is great variability among the various dystrophies, including the muscle groups effected, the degree of weakness, the rate of decline, and the when the symptoms first appear. • Despite all the technology of today, there is no known cure yet discovered.
Types of Muscle Dystrophy • There are nine main categories of muscle dystrophy, within those categories there are more than thirty types of specific muscle dystrophies that can be diagnosed. • This discussion today will focus on the three main ones likely to be seen in practice: Duchenne Muscle Dystrophy (DMD), Becker Muscle Dystrophy, and Myotonic Dystrophy.
General Symptoms of Muscle Dystrophy • Poor Balance • Scoliosis • Progressive inability to walk
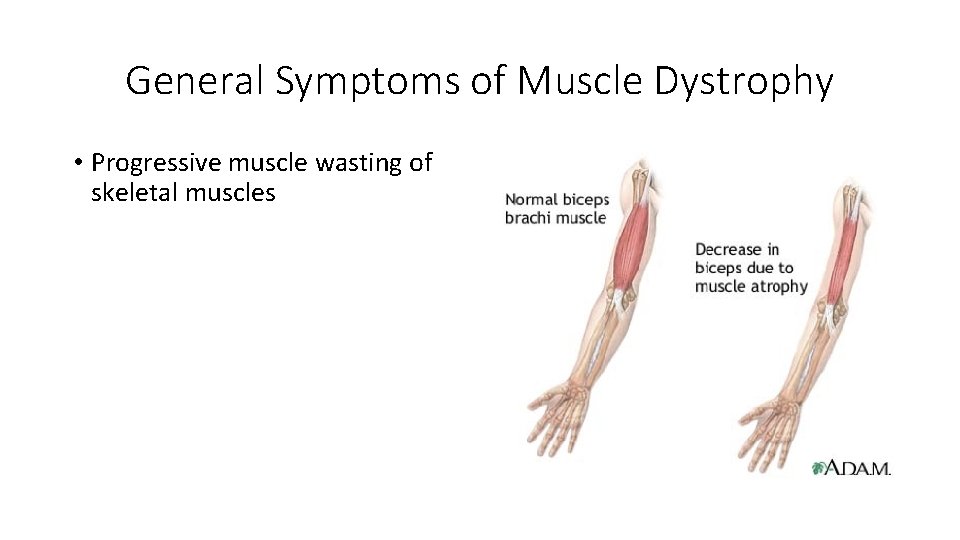
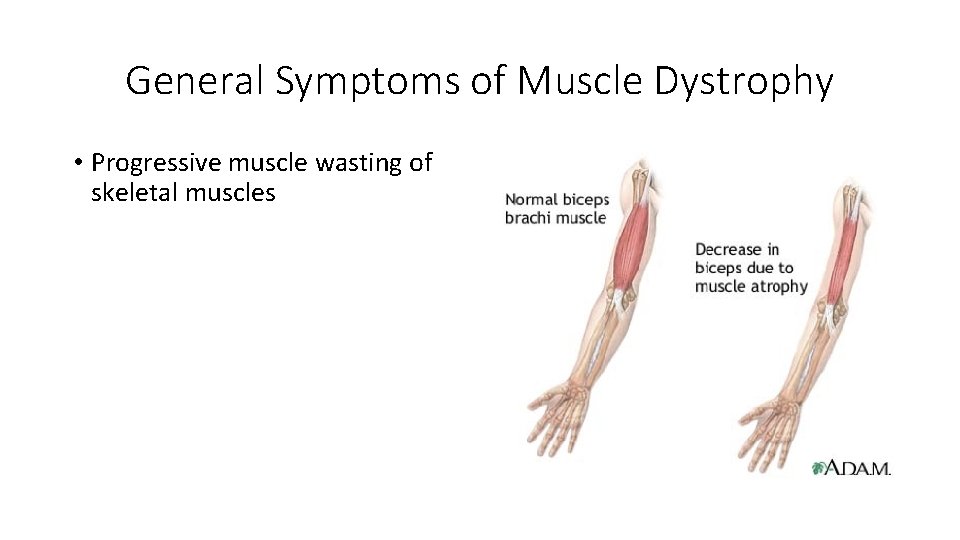
General Symptoms of Muscle Dystrophy • Progressive muscle wasting of skeletal muscles
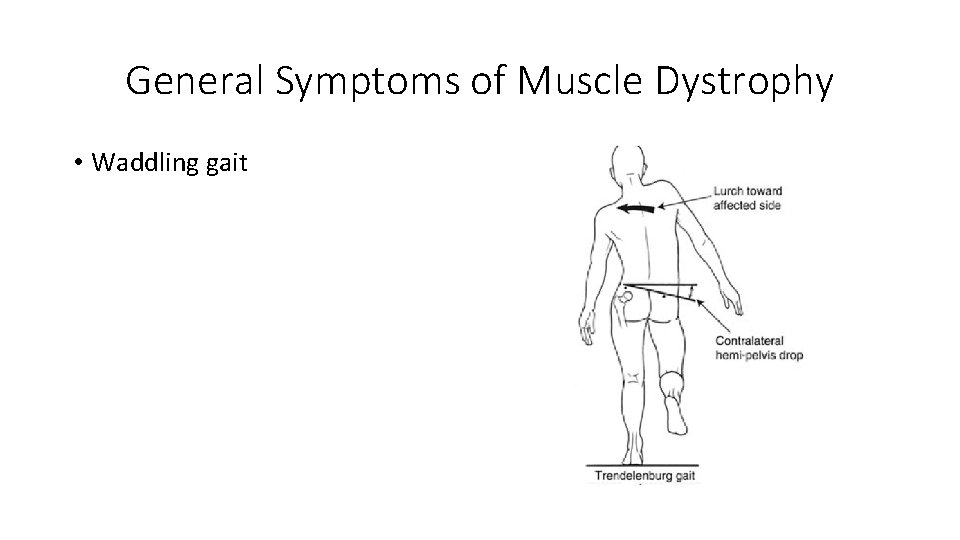
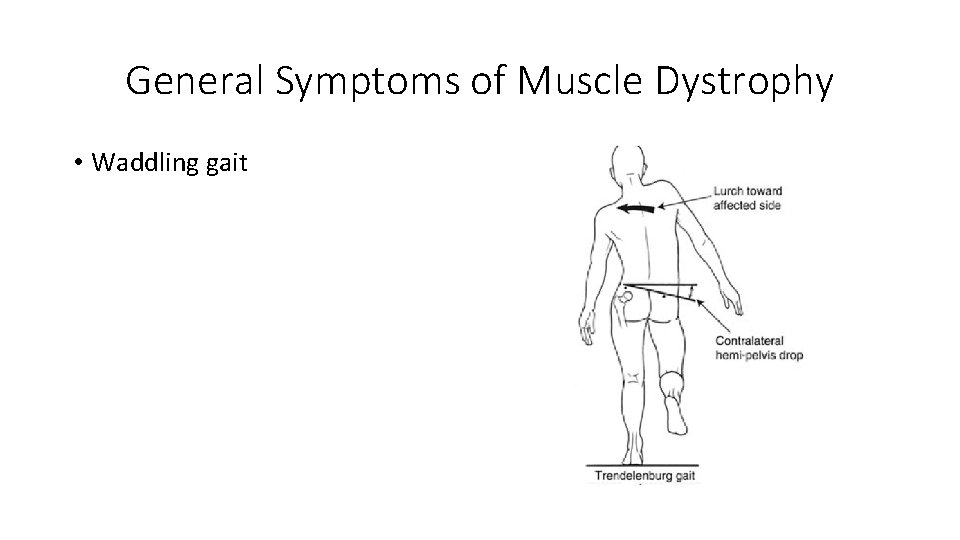
General Symptoms of Muscle Dystrophy • Waddling gait
General Symptoms of Muscle Dystrophy • Calf deformation • Limited range of movement • Respiratory difficulty • Cardiomyopathy • Muscle Spasms
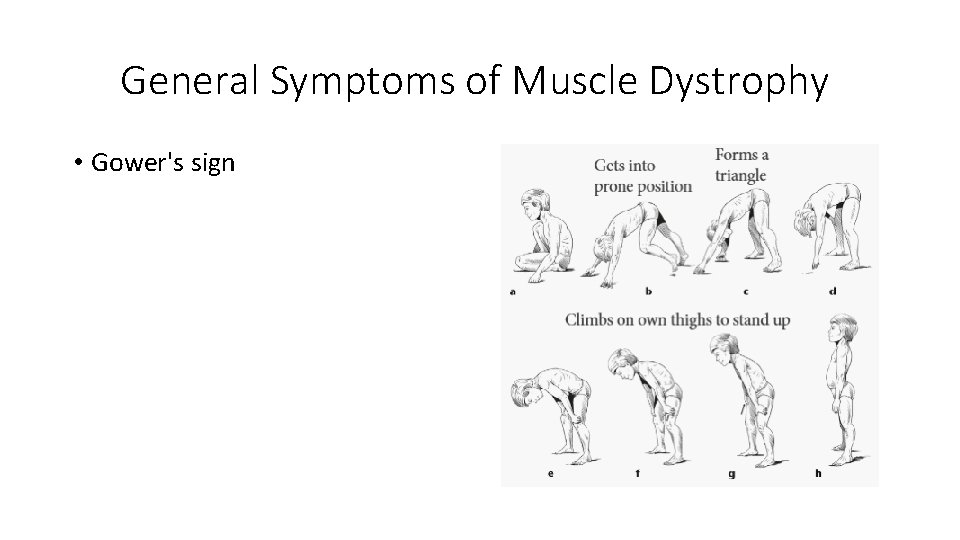
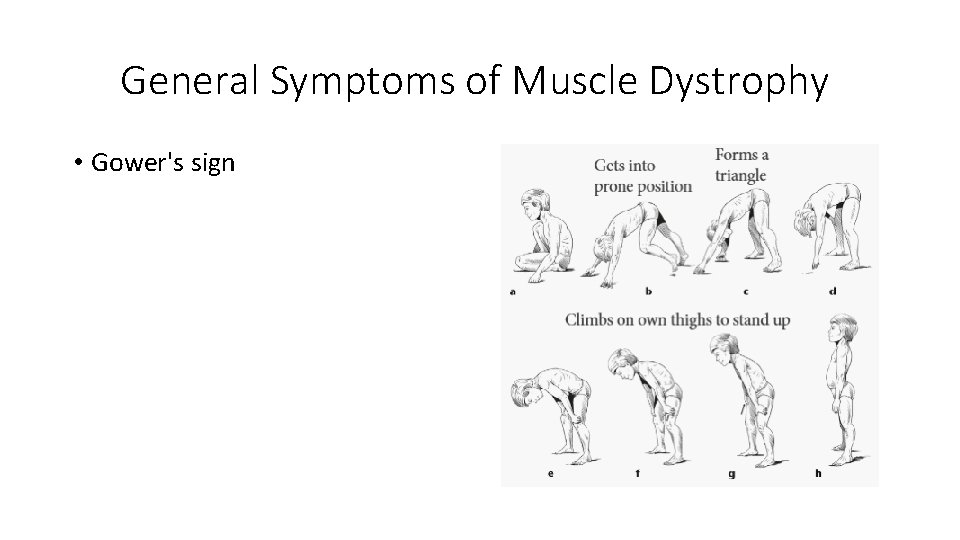
General Symptoms of Muscle Dystrophy • Gower's sign
Causes of Muscle Dystrophy • Generally speaking, these are inherited genetic disorders. • There are many patterns of inheritance and very from each subtype of muscle dystrophy, and can be X-linked, recessive, or dominant. • There are rare instances where there is de novo mutations within the individual with on family history of muscle dystrophy.
Diagnosis of Muscle Dystrophy • History of the patient and family members that may have been affected. • Initial testing of muscle testing includes a physical examination, look for the aforementioned signs and symptoms. • Additionally, further investigation includes muscle biopsy, CK testing, EMG, and genetic testing.
Diagnosis of Muscle Dystrophy • Additionally, Chest X-rays, Echocardiogram can be performed as well.
Treatment of Muscle Dystrophy • Even in 2018, unfortunately we do not have a cure for muscle dystrophy. • The main stays of treatment today are: • • • Physical therapy Occupational Therapy Orthortic Intervention (AFO, etc. ) Speech Therapy Respiratory Therapy Steroids (Prednisone)
Duchenne Muscular Dystrophy
Duchenne Muscular Dystrophy • X-linked recessive, 1: 3300 males • Xp 21, dystrophin gene mutation (2/3 familial, 1/3 new mutations) • Females with a single copy of the gene may show mild symtpoms • Typically presents at 5 years old • difficulty running • abnormal gait (waddling) • historic motor delay
Duchenne Muscular Dystrophy • Physical Exam: • Musculoskeletal • Lumbar lordosis • Pseudohypertrophy (enlarging) of tongue and calf muscles. The muscle tissue is eventually replaced by fat and connective tissue, hence the term pseudohypertrophy.
Duchenne Muscular Dystrophy • Neurologic Exam: • Neck flexor weakness • Symmetric and proximal UE and LE weakness, LE > UE • Diffuse hypotonia, DTRs 1+ diffusely
Duchenne Muscular Dystrophy • Other system involvement • Dystrophin is found in skeletal muscle, smooth muscle, cardiac muscle and brain • May have cognitive impairment • All develop cardiomyopathy • Cardiac involvement may require a pacemaker • May develop intestinal pseudo-obstruction • Higher risk of neurobehavioral disorders (e. g. , ADHD), learning disorders (dyslexia), and non-progressive weaknesses in specific cognitive skills (in particular short-term verbal memory), which are believed to be the result of absent or dysfunctional dystrophin in the brain.
Duchenne Muscular Dystrophy • Diagnosis • • CK elevated (10 x upper limit normal) Muscle biopsy (absent dystrophin) Genetic/DNA testing +/- EMG/NCV
Duchenne Muscular Dystrophy • Prognosis • • Supportive care +/- steroids Wheelchair bound by 13 years old Death in 20 s from respiratory or cardiac failure
Becker Muscle Dystrophy
Becker Muscle Dystrophy • Same pathogenesis as DMD • Except for inframe mutations for BMD, out of frame for DMD
Becker Muscle Dystrophy • Slower course • Present between 5 -15 years old • Wheelchair bound after 16 years old • Live through their 30 s-40 s
Becker Muscle Dystrophy • Less severe course, less likely to have • • • Cognitive impairment Cardiac disease Contractures Scoliosis GI issues
Becker Muscle Dystrophy • CK elevated (5 x upper limit of normal) • Muscle biopsy with decreased dystrophin
Congenital Myotonic Dystrophy
Congenital Myotonic Dystrophy • Autosomal Dominant • > 1000 CTG repeats in the DMPK gene, 19 q 13. 3 (anticipation) • Mom is typically the affected parent (check her grip!)
Congenital Myotonic Dystrophy • Poor fetal movement, polyhydramnios • Feeding and respiratory difficulties, cognitive • impairment, developmental delay
Congenital Myotonic Dystrophy • There are two kinds of Myotonic Dystrophy • DM 1 and DM 2 • DM 1 has an error in the DMPK gene. • DM 2 has an error in CNBP gene.
Congenital Myotonic Dystrophy • Neurologic Exam: • • Facial diplegia Hypotonia Decreased DTRs Intellectual disability
Congenital Myotonic Dystrophy • Other Physical Exam findings: • Joint deformities, from clubfoot to arthrogryposis • Cataracts • Heart Conduction problems
Congenital Myotonic Dystrophy • No clinical or EMG myotonia until 2 years of age • Genetic testing
Congenital Myotonic Dystrophy • Treatment • There is no treatment for myotonic dystrophy • Pain can be treated with tricyclic antidepressants (Amitryptiline, Nortyptiline) or NSAIDs • Associated Sleep Apnea – OSA, CSA treated with appropriate devices. • Orthotics • Physical Therapy
Muscle Dystrophy • The future: • Research Currently in the United States and the UK with gene research and neuromuscular regeneration.
 Duchenne muscular dystrophy
Duchenne muscular dystrophy Santosh thomas
Santosh thomas Thank you for attending open house
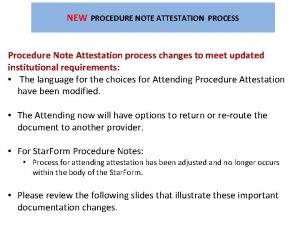
Thank you for attending open house Attestation note
Attestation note Attending vs resident
Attending vs resident Why is attending school important
Why is attending school important Attending responding personalizing initiating
Attending responding personalizing initiating Requirements for erf teacher 3
Requirements for erf teacher 3 Neurology consultants northern ireland
Neurology consultants northern ireland Richard perry neurologist
Richard perry neurologist Dr richard perry neurologist
Dr richard perry neurologist What is a neurologist?
What is a neurologist? Dr michelle lee jones neurologist
Dr michelle lee jones neurologist Kelly clarkson neurologist
Kelly clarkson neurologist Dr anthony fok
Dr anthony fok Dr madhavan neurologist
Dr madhavan neurologist Dr nin bajaj
Dr nin bajaj Dr bennetto neurologist
Dr bennetto neurologist Dr aminian neurologist
Dr aminian neurologist Ernie butler neurologist
Ernie butler neurologist Dr pearson neurologist
Dr pearson neurologist Adrian pace neurologist
Adrian pace neurologist Alina webber
Alina webber Dr paul cooper neurologist
Dr paul cooper neurologist Epilepsy
Epilepsy University of dayton premed
University of dayton premed Watsons dayton ohio
Watsons dayton ohio Presidents club of dayton
Presidents club of dayton Dayton juniors volleyball club
Dayton juniors volleyball club Clasroomü
Clasroomü Loa dayton
Loa dayton Dps infonet
Dps infonet Dayton mn police
Dayton mn police Flyer pitch competition
Flyer pitch competition