Investigating dementia Dr Richard Perry Consultant Neurologist Imperial

- Slides: 35
Investigating dementia Dr Richard Perry Consultant Neurologist Imperial College Healthcare NHS Trust

Overview • Structural imaging – CT and MRI – MRI and vascular disease – MRI and focal atrophy – MRI and microhaemorrhages • CSF – Biomarkers -Tau and abeta • EEG • Functional imaging - 18 F FDG PET • Illustrative cases • Amyloid imaging
Structural brain imaging in cognitive impairment • MRI modality of choice • 1. 5 T or 3 T • CT useful for acute presentations: – Hydrocephalus – acute – Haemorrhage – Mass lesions • If MRI unavailable, CT can give information on – Atrophy – Vascular load
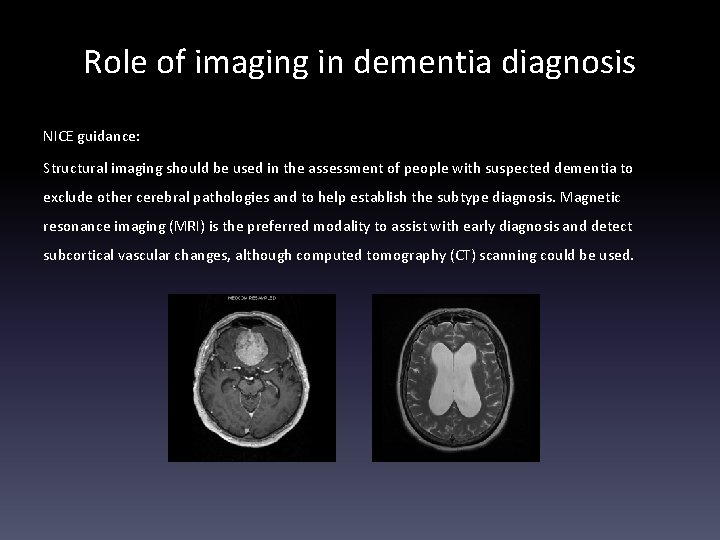
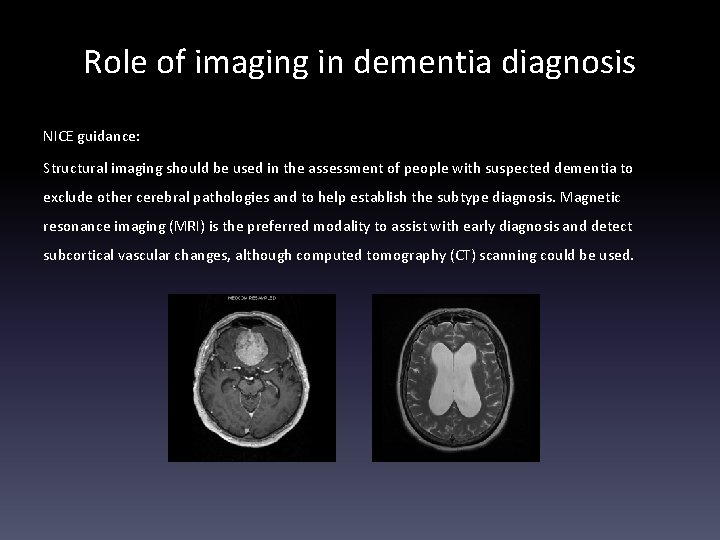
Role of imaging in dementia diagnosis NICE guidance: Structural imaging should be used in the assessment of people with suspected dementia to exclude other cerebral pathologies and to help establish the subtype diagnosis. Magnetic resonance imaging (MRI) is the preferred modality to assist with early diagnosis and detect subcortical vascular changes, although computed tomography (CT) scanning could be used.
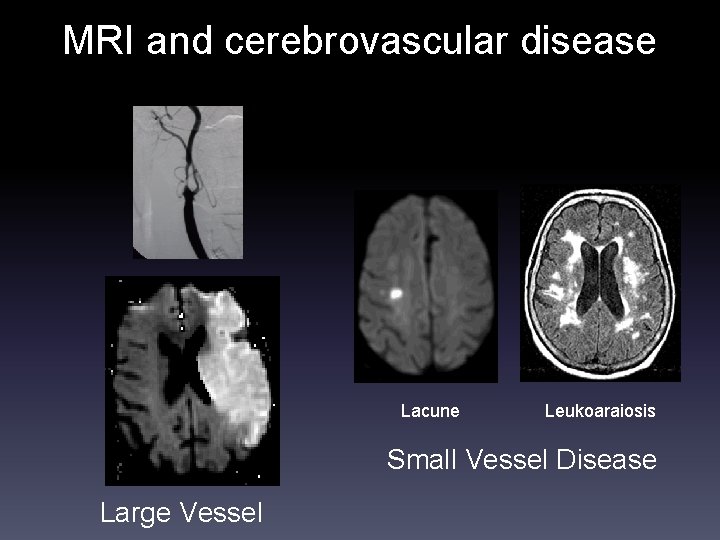
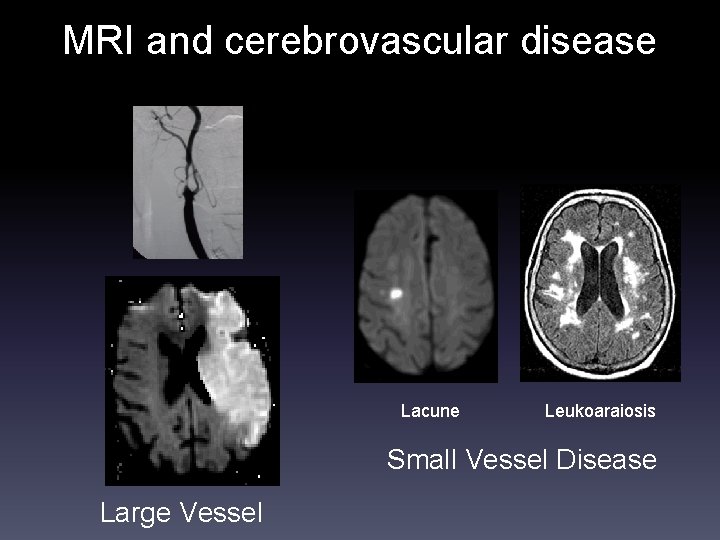
MRI and cerebrovascular disease Lacune Leukoaraiosis Small Vessel Disease Large Vessel
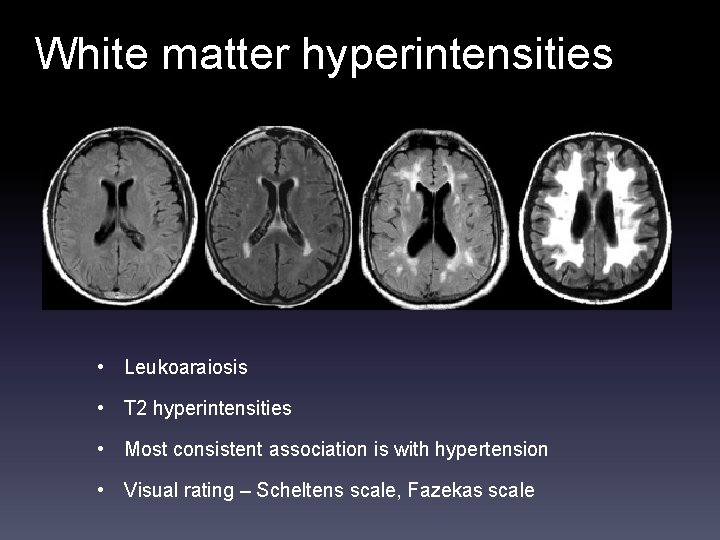
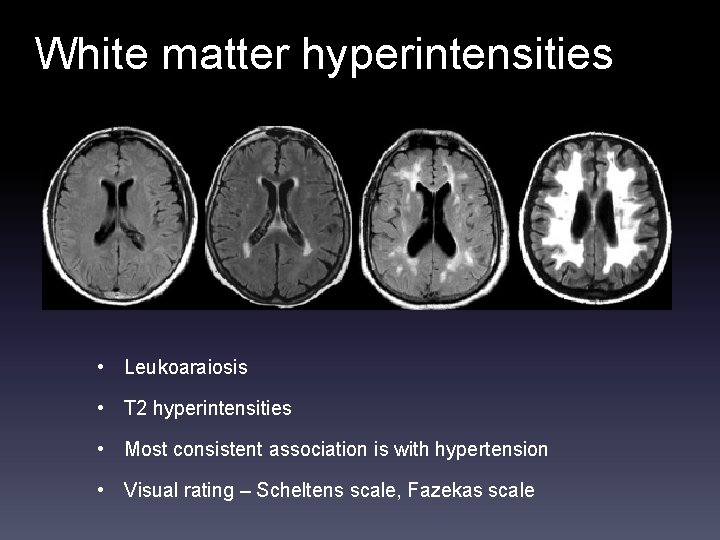
White matter hyperintensities • Leukoaraiosis • T 2 hyperintensities • Most consistent association is with hypertension • Visual rating – Scheltens scale, Fazekas scale
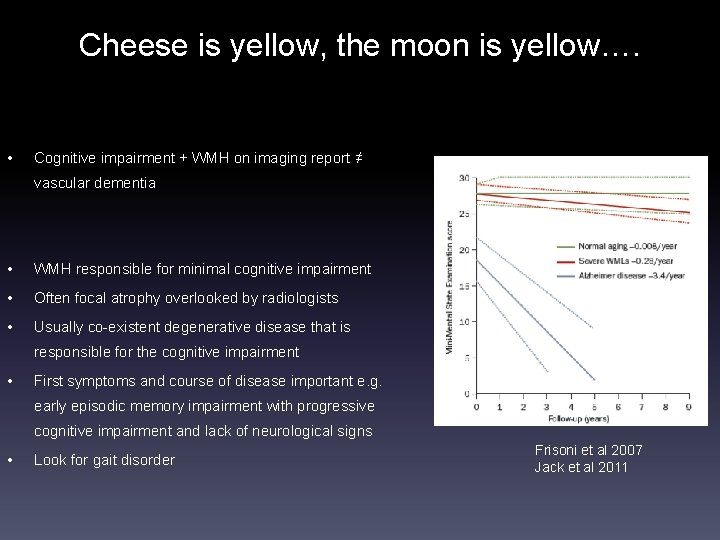
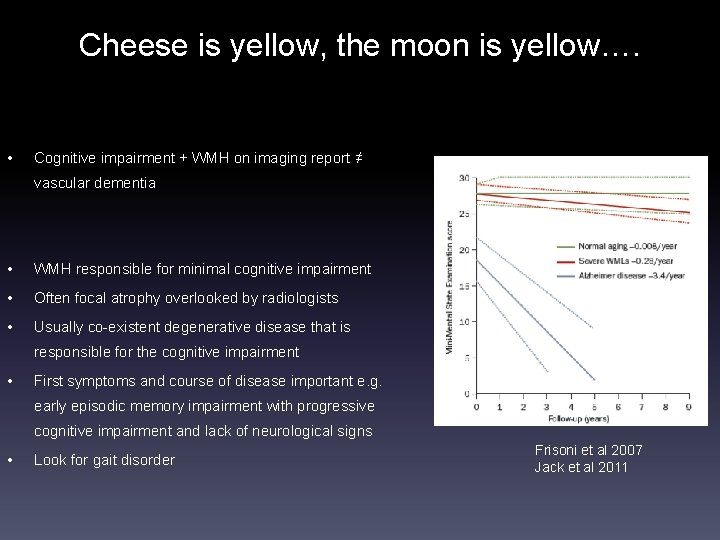
Cheese is yellow, the moon is yellow…. • Cognitive impairment + WMH on imaging report ≠ vascular dementia • WMH responsible for minimal cognitive impairment • Often focal atrophy overlooked by radiologists • Usually co-existent degenerative disease that is responsible for the cognitive impairment • First symptoms and course of disease important e. g. early episodic memory impairment with progressive cognitive impairment and lack of neurological signs • Look for gait disorder Frisoni et al 2007 Jack et al 2011
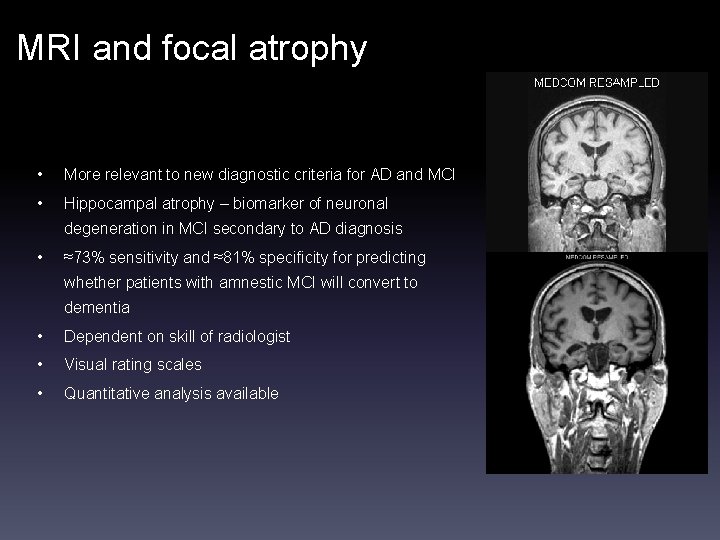
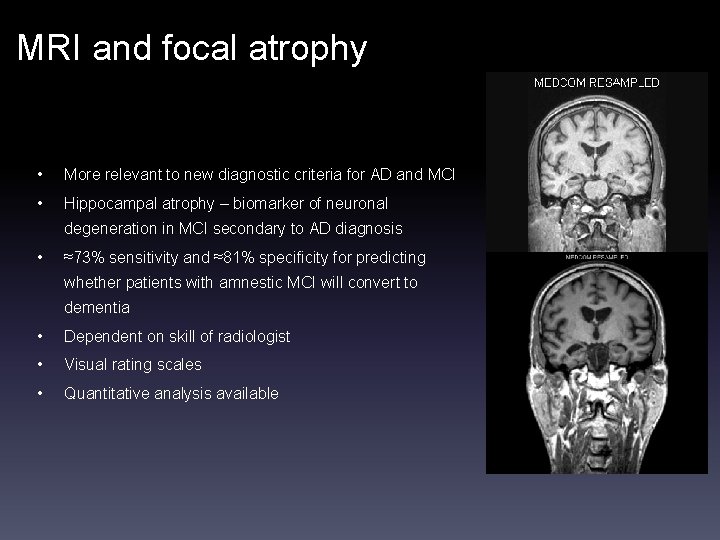
MRI and focal atrophy • More relevant to new diagnostic criteria for AD and MCI • Hippocampal atrophy – biomarker of neuronal degeneration in MCI secondary to AD diagnosis • ≈73% sensitivity and ≈81% specificity for predicting whether patients with amnestic MCI will convert to dementia • Dependent on skill of radiologist • Visual rating scales • Quantitative analysis available
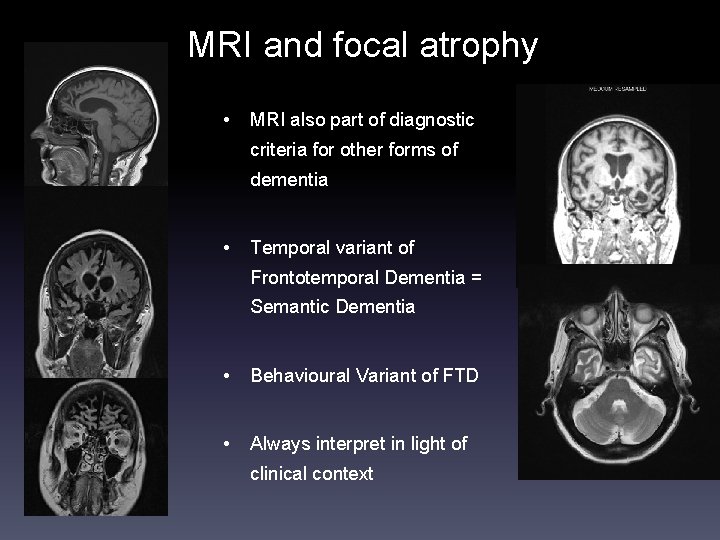
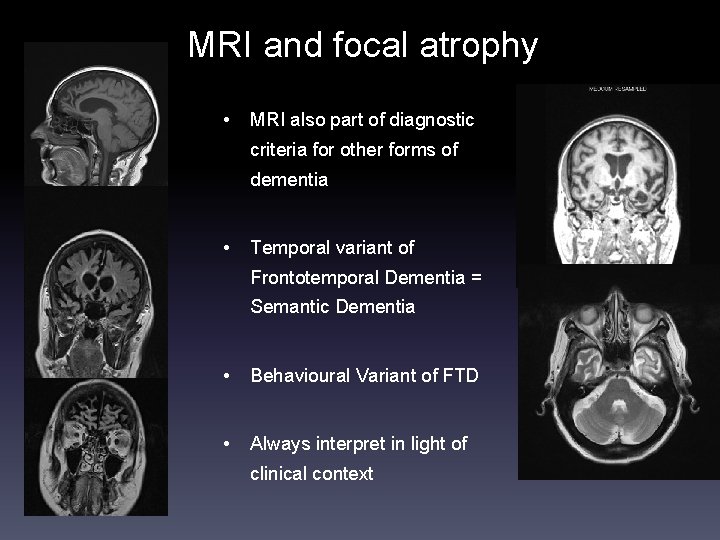
MRI and focal atrophy • MRI also part of diagnostic criteria for other forms of dementia • Temporal variant of Frontotemporal Dementia = Semantic Dementia • Behavioural Variant of FTD • Always interpret in light of clinical context
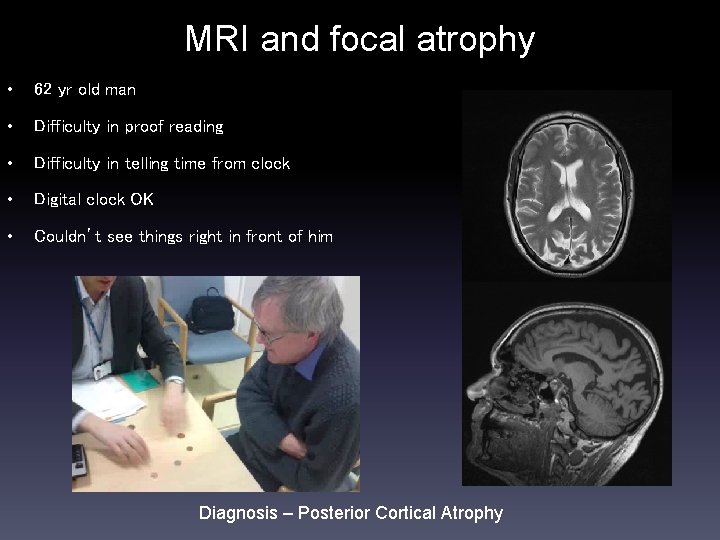
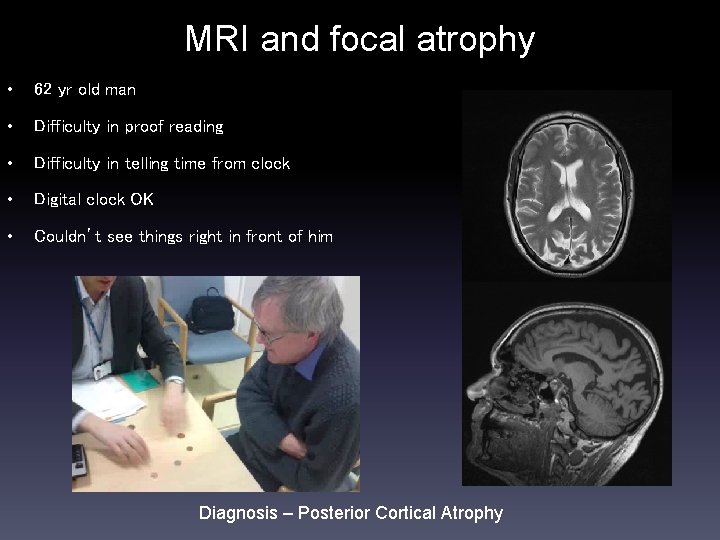
MRI and focal atrophy • 62 yr old man • Difficulty in proof reading • Difficulty in telling time from clock • Digital clock OK • Couldn’t see things right in front of him Diagnosis – Posterior Cortical Atrophy
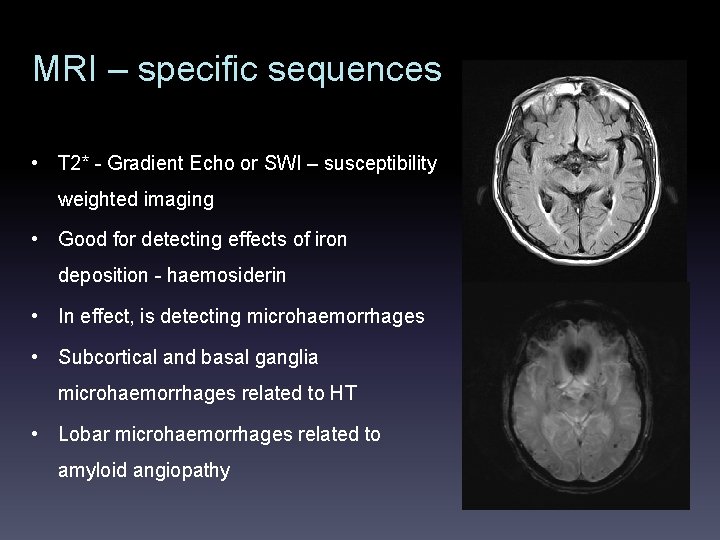
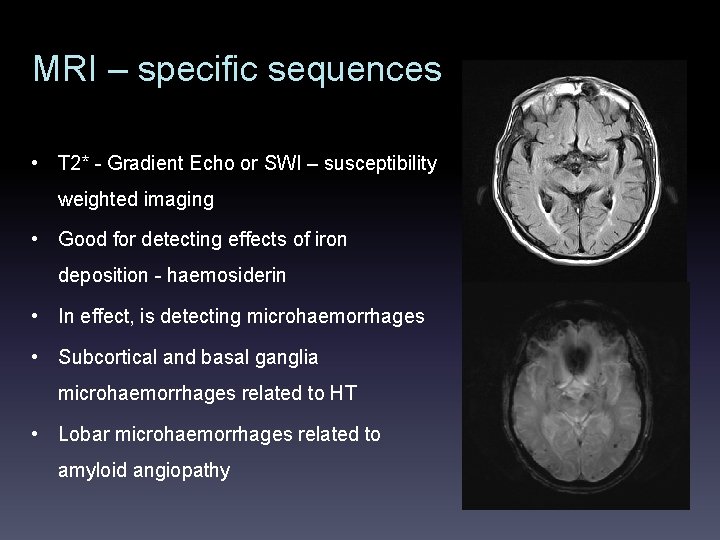
MRI – specific sequences • T 2* - Gradient Echo or SWI – susceptibility weighted imaging • Good for detecting effects of iron deposition - haemosiderin • In effect, is detecting microhaemorrhages • Subcortical and basal ganglia microhaemorrhages related to HT • Lobar microhaemorrhages related to amyloid angiopathy
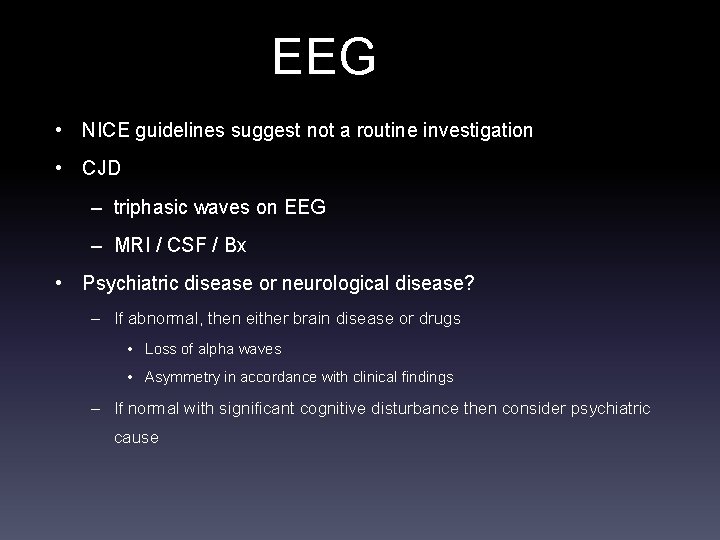
EEG • NICE guidelines suggest not a routine investigation • CJD – triphasic waves on EEG – MRI / CSF / Bx • Psychiatric disease or neurological disease? – If abnormal, then either brain disease or drugs • Loss of alpha waves • Asymmetry in accordance with clinical findings – If normal with significant cognitive disturbance then consider psychiatric cause
CSF • LP quick and minimally invasive (? ) • Requires bed and operator • Exclude infection and inflammation • Now biomarkers for neurodegenerative disease available – A beta 1 -42 – Total tau – Phospho tau • Low abeta levels indicate amyloidopathy • Raised tau levels indicate ongoing neuronal damage • Sensitive and specific tests - require counselling prior to test • Processing of samples important as reliability of assay sub-optimal
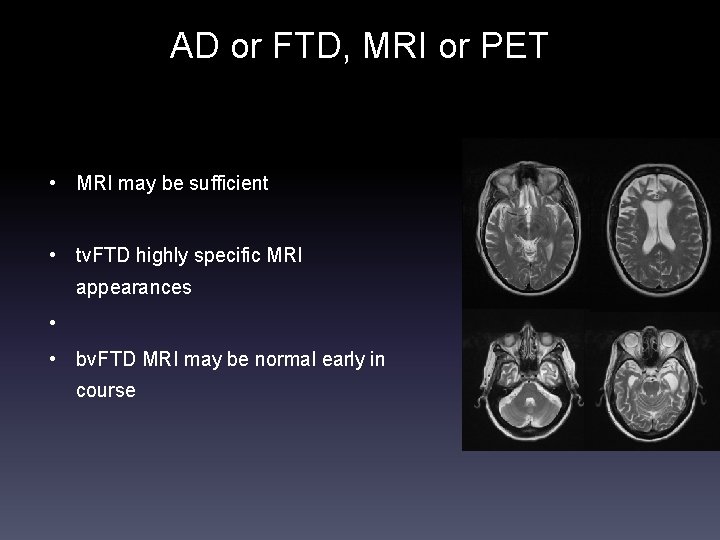
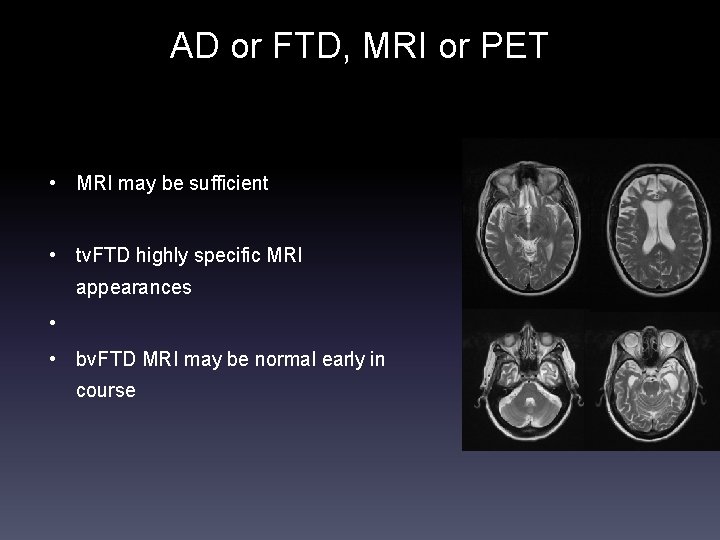
AD or FTD, MRI or PET • MRI may be sufficient • tv. FTD highly specific MRI appearances • • bv. FTD MRI may be normal early in course
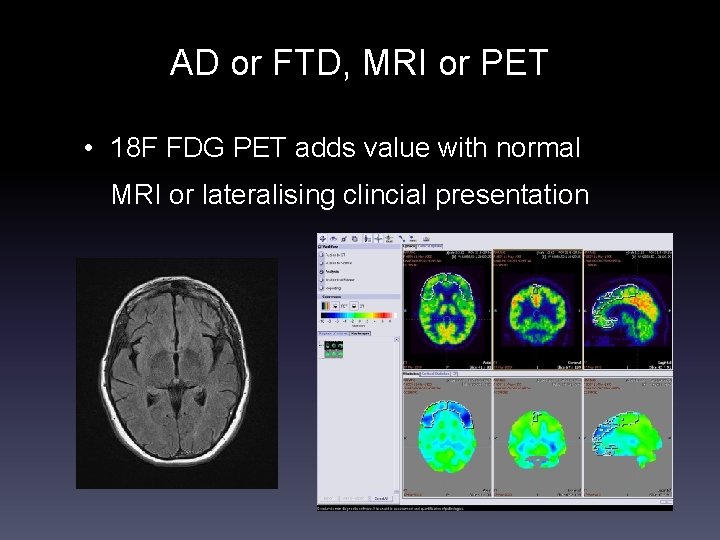
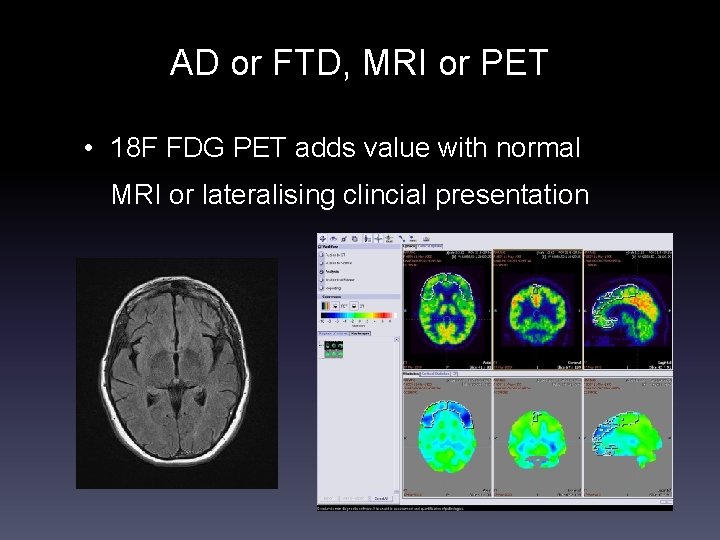
AD or FTD, MRI or PET • 18 F FDG PET adds value with normal MRI or lateralising clincial presentation
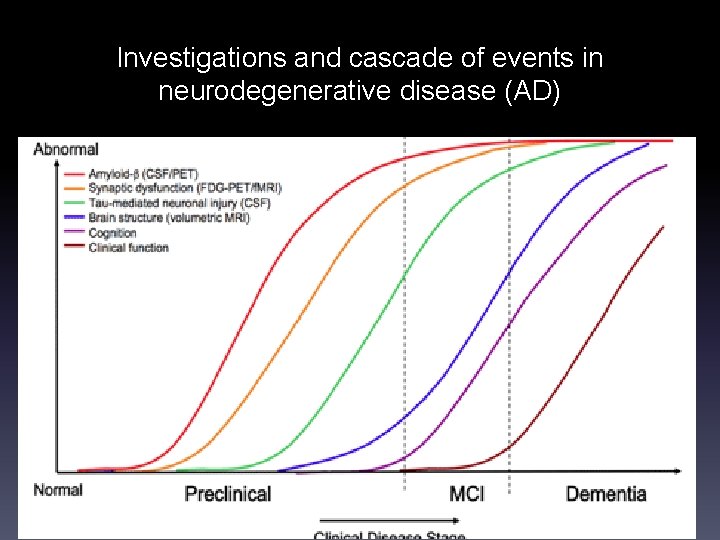
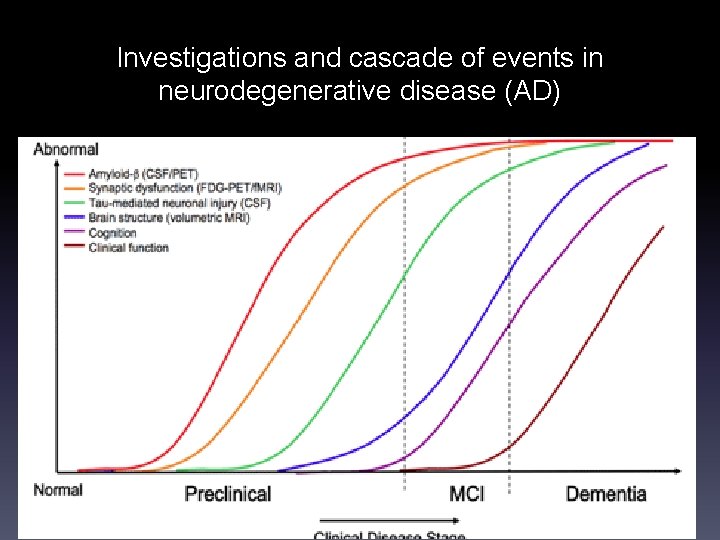
Investigations and cascade of events in neurodegenerative disease (AD)
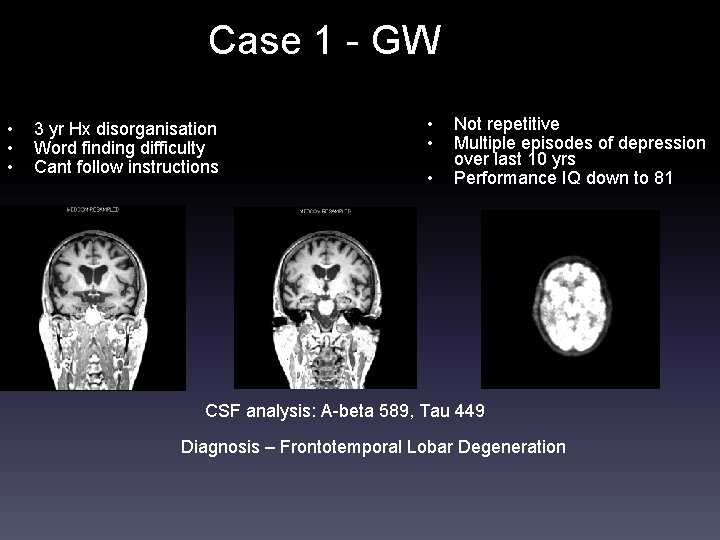
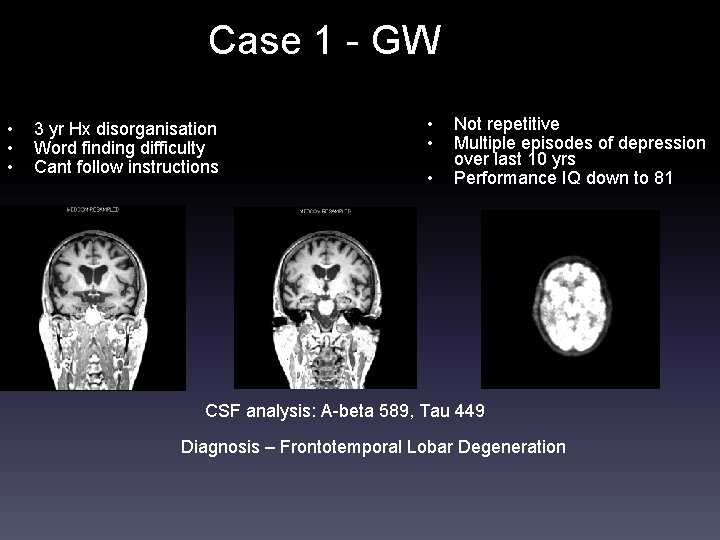
Case 1 - GW • • • 3 yr Hx disorganisation Word finding difficulty Cant follow instructions • • • Not repetitive Multiple episodes of depression over last 10 yrs Performance IQ down to 81 CSF analysis: A-beta 589, Tau 449 Diagnosis – Frontotemporal Lobar Degeneration
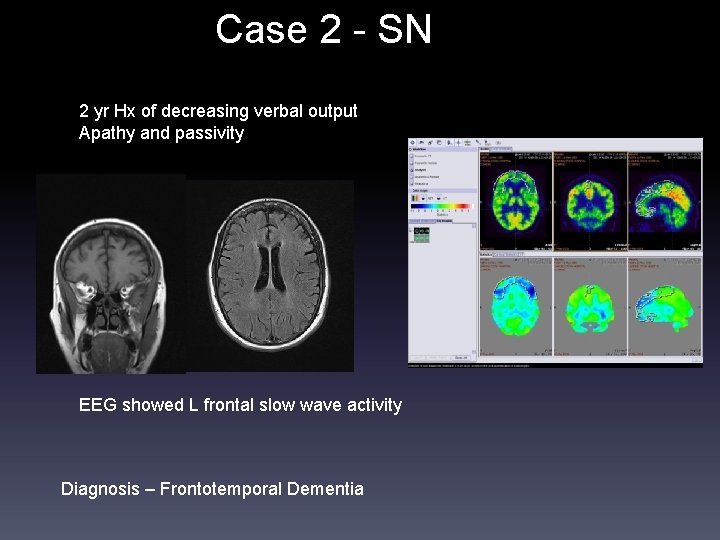
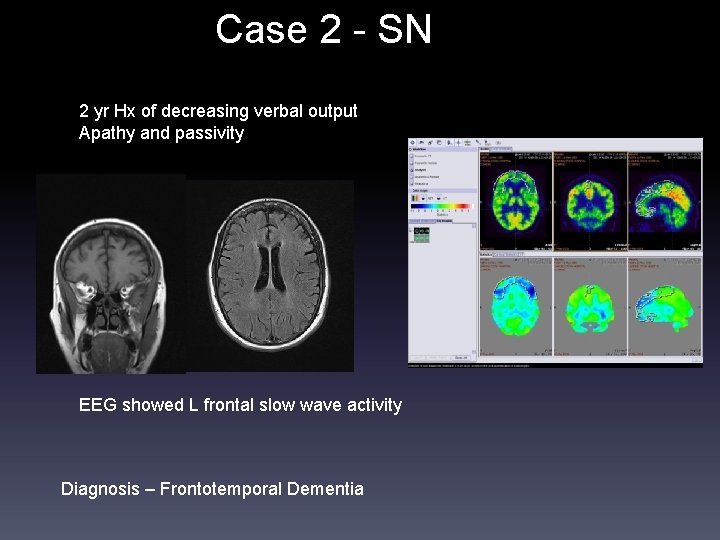
Case 2 - SN 2 yr Hx of decreasing verbal output Apathy and passivity EEG showed L frontal slow wave activity Diagnosis – Frontotemporal Dementia
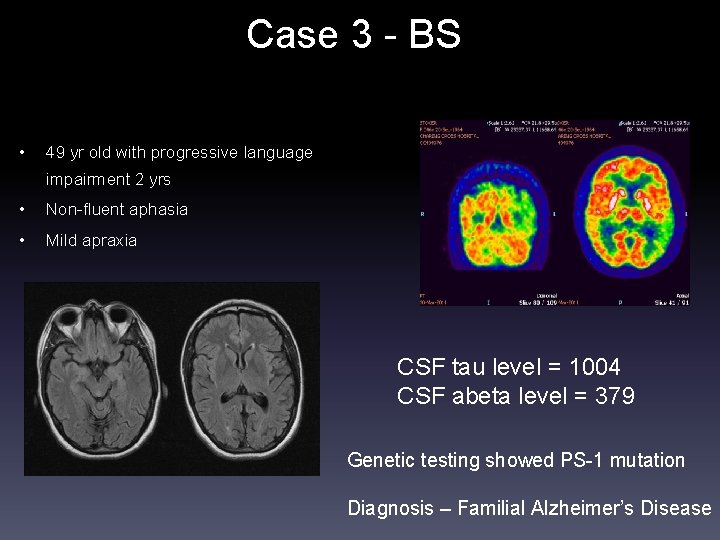
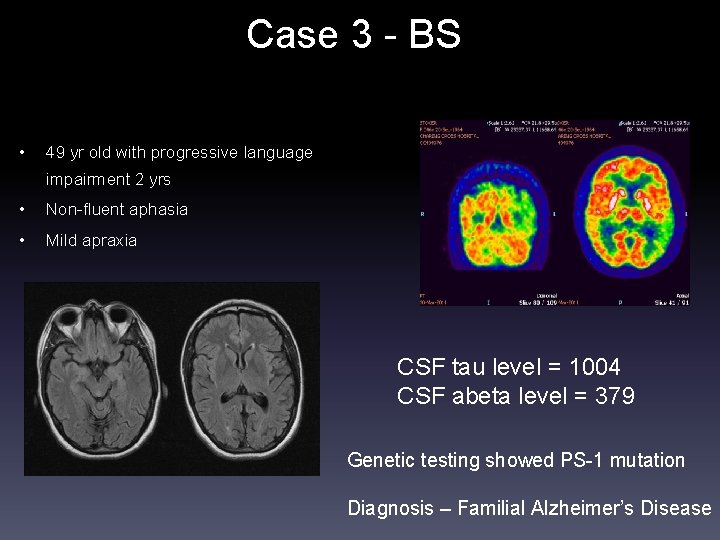
Case 3 - BS • 49 yr old with progressive language impairment 2 yrs • Non-fluent aphasia • Mild apraxia CSF tau level = 1004 CSF abeta level = 379 Genetic testing showed PS-1 mutation Diagnosis – Familial Alzheimer’s Disease
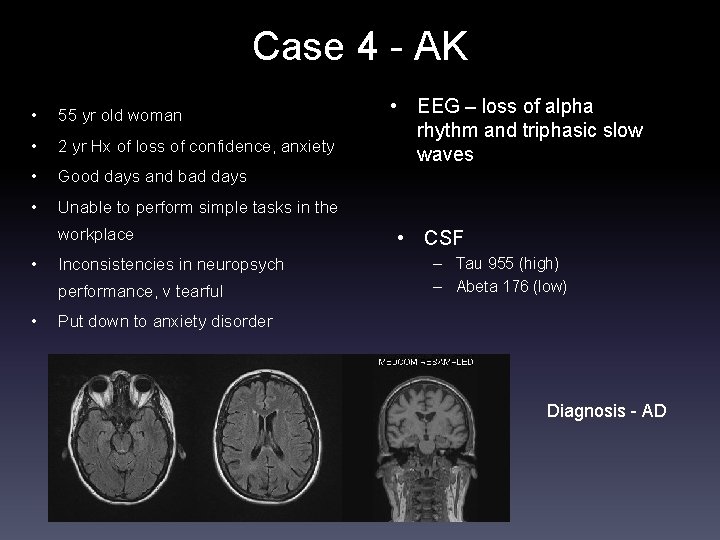
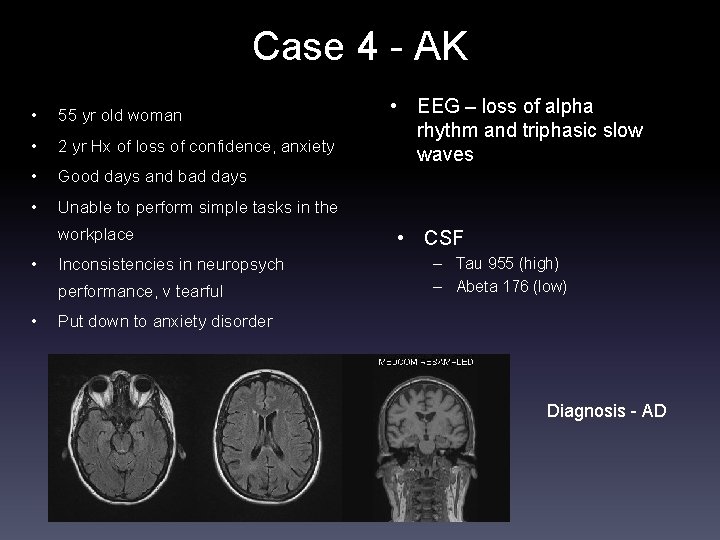
Case 4 - AK • 55 yr old woman • 2 yr Hx of loss of confidence, anxiety • Good days and bad days • Unable to perform simple tasks in the workplace • Inconsistencies in neuropsych performance, v tearful • • EEG – loss of alpha rhythm and triphasic slow waves • CSF – Tau 955 (high) – Abeta 176 (low) Put down to anxiety disorder Diagnosis - AD
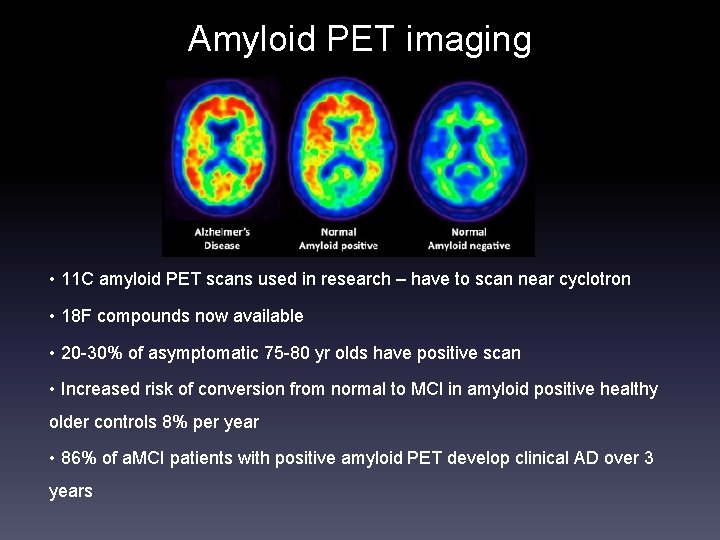
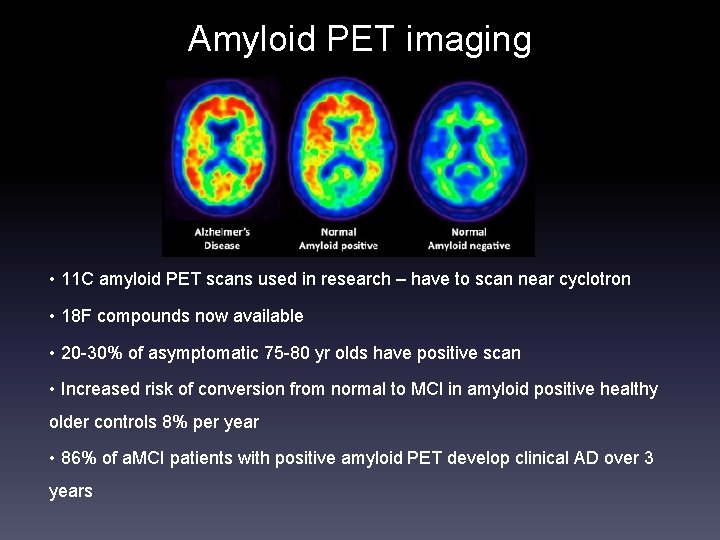
Amyloid PET imaging • 11 C amyloid PET scans used in research – have to scan near cyclotron • 18 F compounds now available • 20 -30% of asymptomatic 75 -80 yr olds have positive scan • Increased risk of conversion from normal to MCI in amyloid positive healthy older controls 8% per year • 86% of a. MCI patients with positive amyloid PET develop clinical AD over 3 years
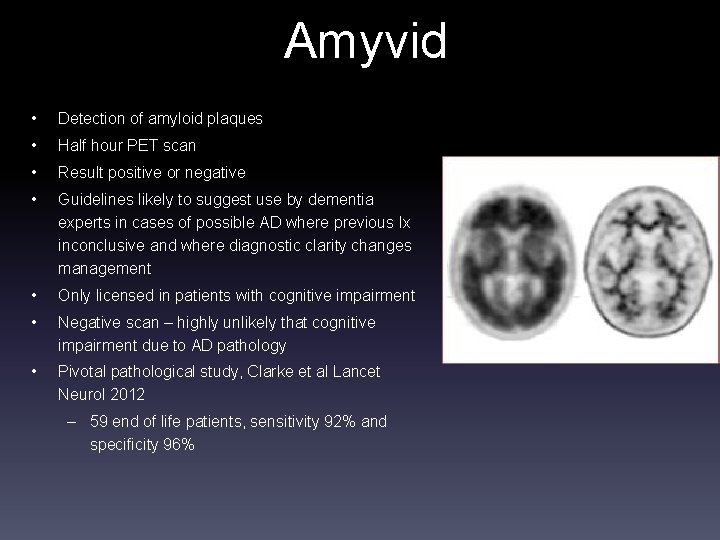
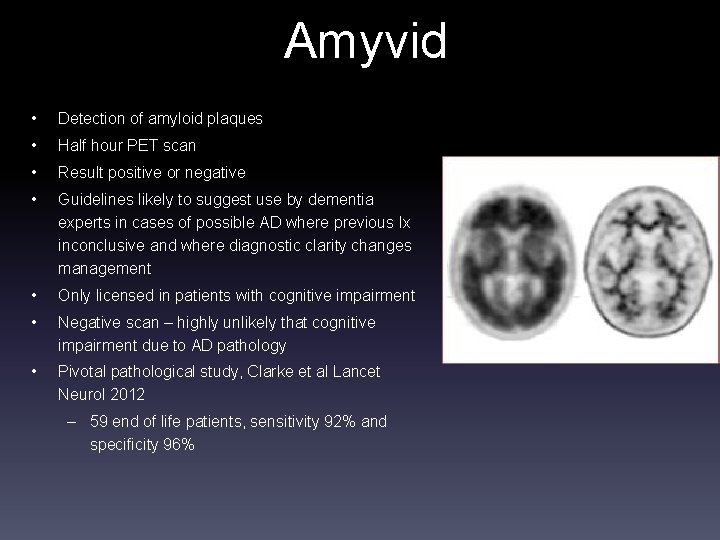
Amyvid • Detection of amyloid plaques • Half hour PET scan • Result positive or negative • Guidelines likely to suggest use by dementia experts in cases of possible AD where previous Ix inconclusive and where diagnostic clarity changes management • Only licensed in patients with cognitive impairment • Negative scan – highly unlikely that cognitive impairment due to AD pathology • Pivotal pathological study, Clarke et al Lancet Neurol 2012 – 59 end of life patients, sensitivity 92% and specificity 96%
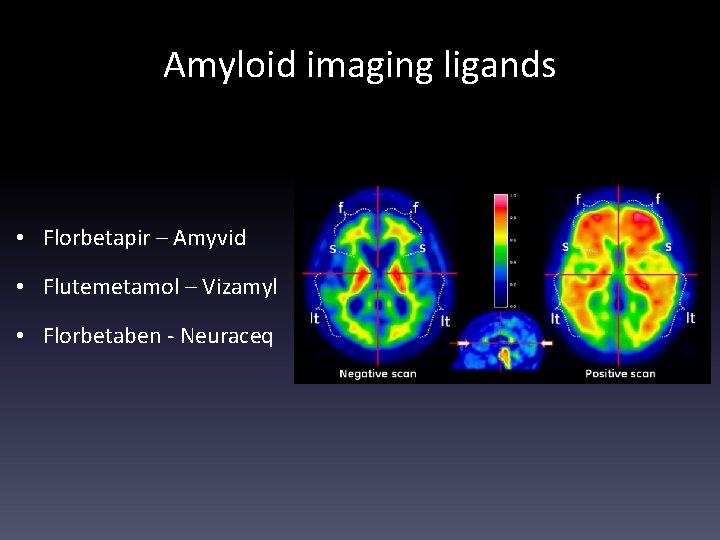
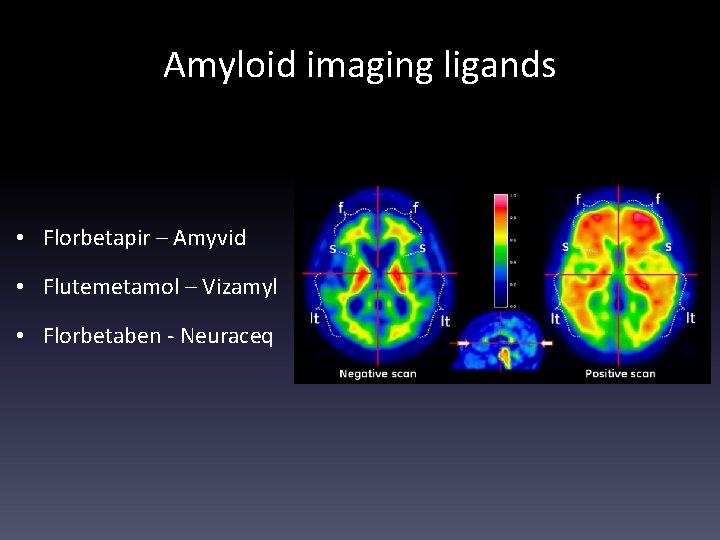
Amyloid imaging ligands • Florbetapir – Amyvid • Flutemetamol – Vizamyl • Florbetaben - Neuraceq
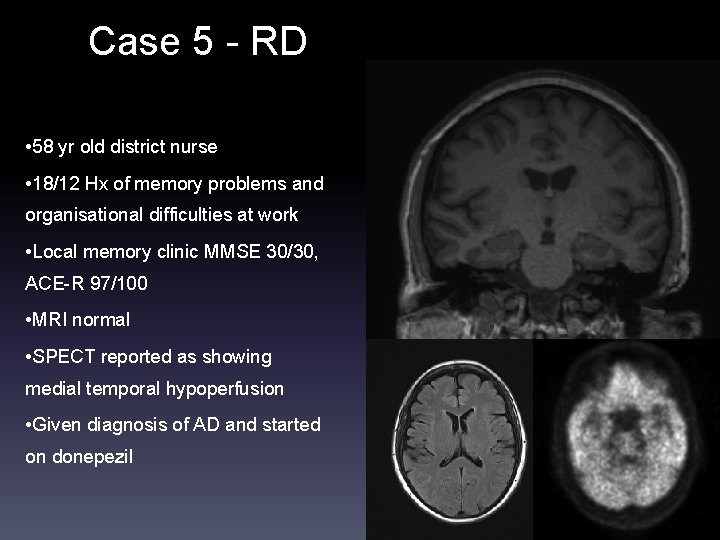
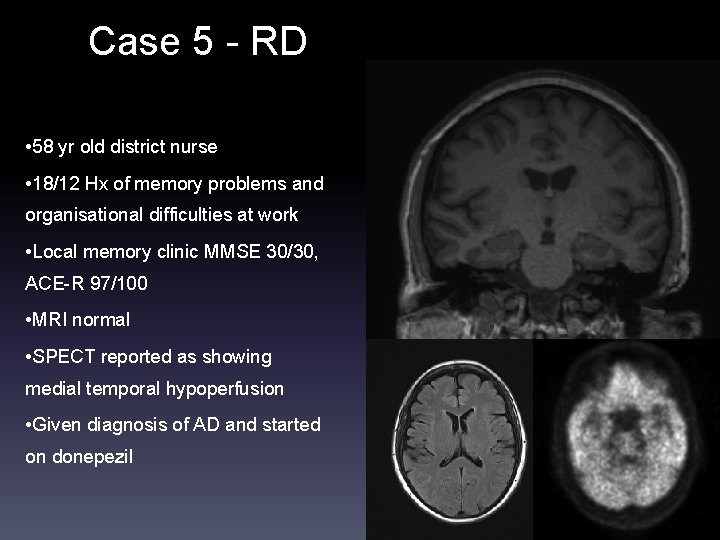
Case 5 - RD • 58 yr old district nurse • 18/12 Hx of memory problems and organisational difficulties at work • Local memory clinic MMSE 30/30, ACE-R 97/100 • MRI normal • SPECT reported as showing medial temporal hypoperfusion • Given diagnosis of AD and started on donepezil
Case 5 - RD • Referred for second opinion • Husband felt that memory OK • Daughter reported her as repetitive and more noticeable symptoms over last year • FDG – PET again reported as medial temporal hypometabolism • CSF analysis – tau 108 and abeta 874 • ACE -96, MMSE 28 – one point on orientation and one on memory
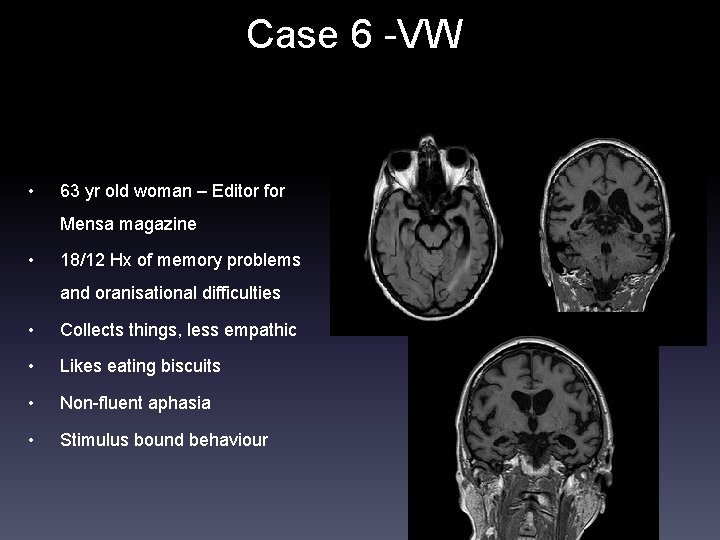
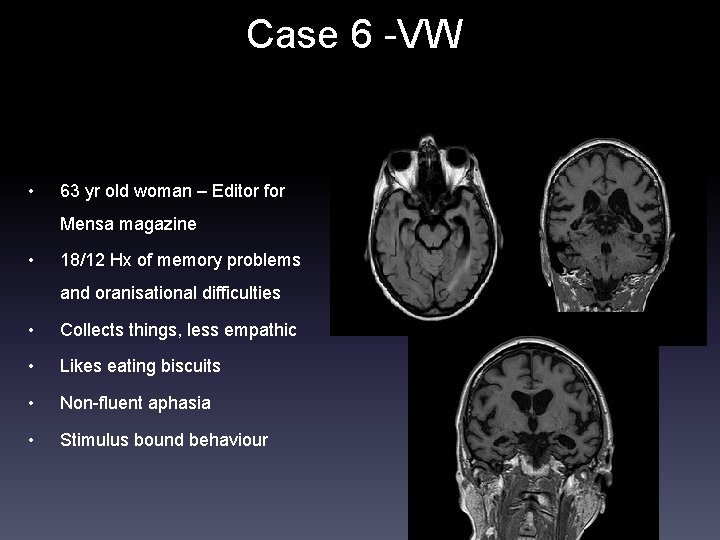
Case 6 -VW • 63 yr old woman – Editor for Mensa magazine • 18/12 Hx of memory problems and oranisational difficulties • Collects things, less empathic • Likes eating biscuits • Non-fluent aphasia • Stimulus bound behaviour
Case 6 - VW
Case 7 - LC • Progressive memory deficits corroborated by husband • Previous Hx of ME, anxiety, and depression • MMSE 26/30 • Neuropsych showed memory deficits and attentional dysfunction consistent with MCI • MRI unremarkable
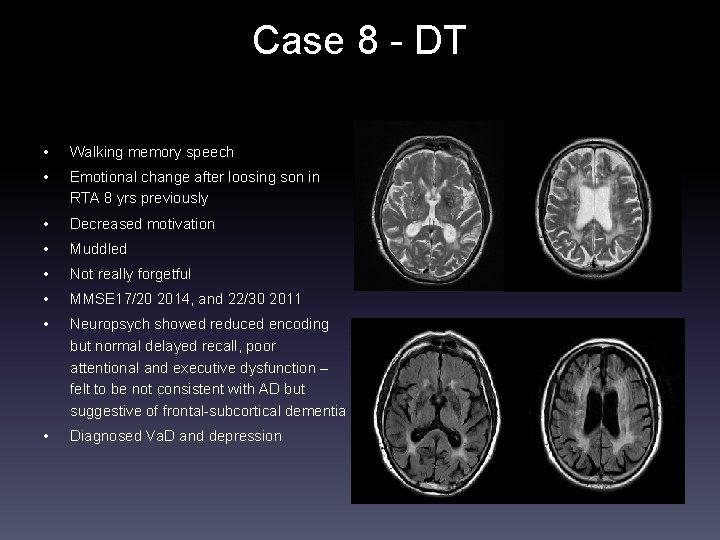
Case 8 - DT • Walking memory speech • Emotional change after loosing son in RTA 8 yrs previously • Decreased motivation • Muddled • Not really forgetful • MMSE 17/20 2014, and 22/30 2011 • Neuropsych showed reduced encoding but normal delayed recall, poor attentional and executive dysfunction – felt to be not consistent with AD but suggestive of frontal-subcortical dementia • Diagnosed Va. D and depression
Case 8 DT
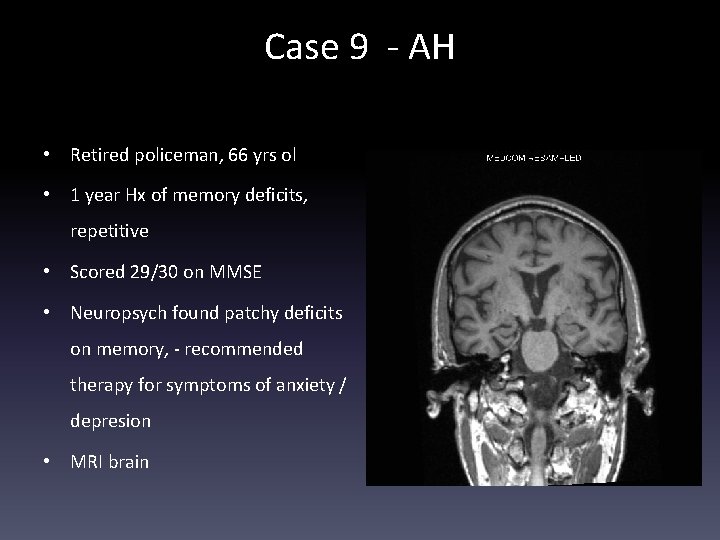
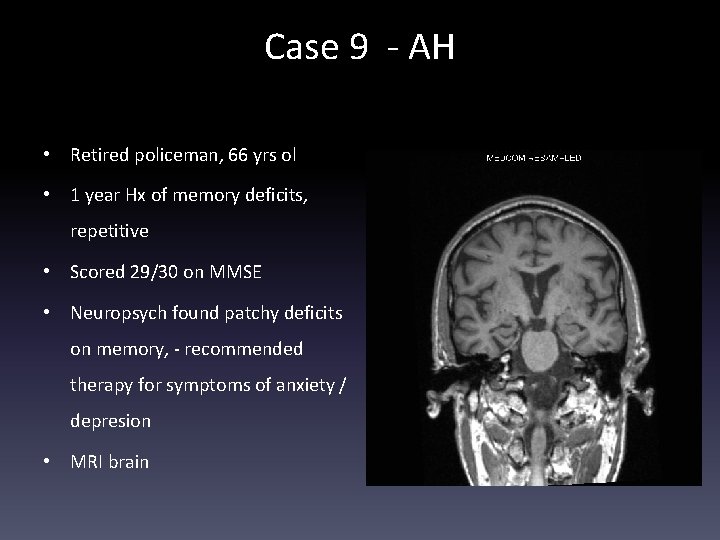
Case 9 - AH • Retired policeman, 66 yrs ol • 1 year Hx of memory deficits, repetitive • Scored 29/30 on MMSE • Neuropsych found patchy deficits on memory, - recommended therapy for symptoms of anxiety / depresion • MRI brain
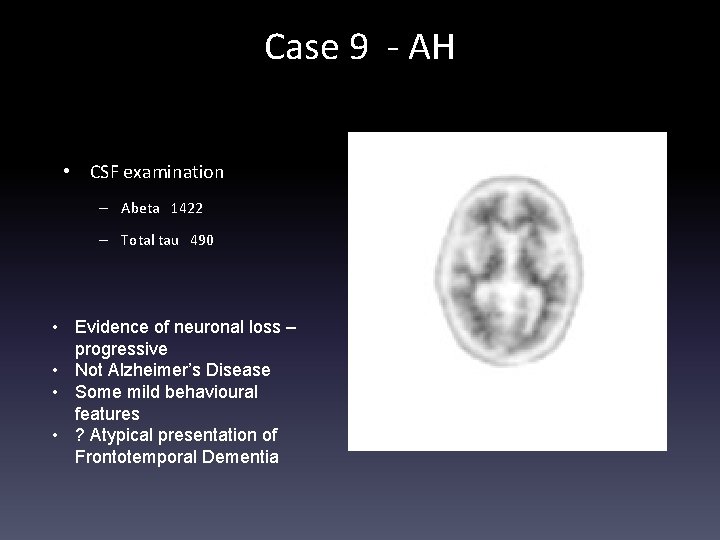
Case 9 - AH • CSF examination – Abeta 1422 – Total tau 490 • Evidence of neuronal loss – progressive • Not Alzheimer’s Disease • Some mild behavioural features • ? Atypical presentation of Frontotemporal Dementia
Which patients are suitable for amyloid imaging? • It’s a new area, so we are still calibrating • Currently, we are focusing on: – Younger patients – less probability of ‘false positive’ – Atypical AD presentations – e. g. PCA, Progressive Aphasia – AD / FTD differentiation – MCI if clarification helpful – Multiple possible causes of cognitive impairment e. g depression / vascular
Conclusions • Investigations support clinical diagnosis • Investigations can be thought of as biomarkers that are: – Supportive of neurodegeneration and / or – Pathology or disease specific • Familiarity with Ix important and important to review actual pictures • Amyloid imaging e. g. Amyvid now available for use within guidelines