MichelleLee Jones Neurology PGY3 July 15 th 2009








- Slides: 35
Michelle-Lee Jones Neurology PGY-3 July 15 th, 2009
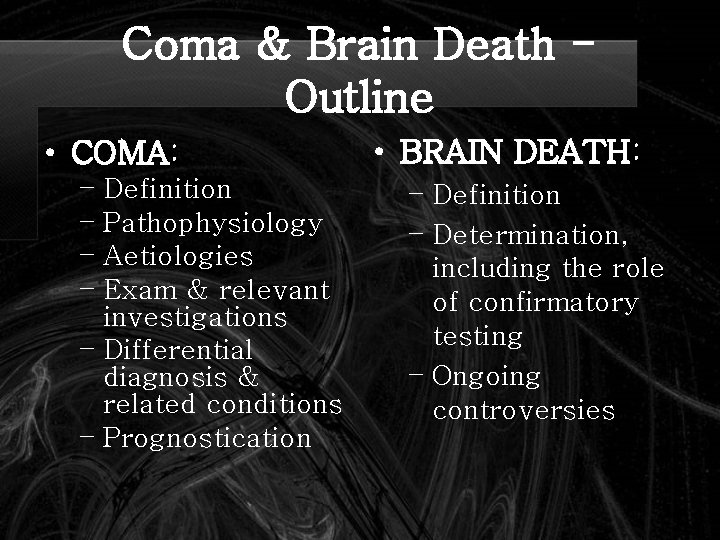
Coma & Brain Death Outline • COMA: – Definition – Pathophysiology – Aetiologies – Exam & relevant investigations – Differential diagnosis & related conditions – Prognostication • BRAIN DEATH: – Definition – Determination, including the role of confirmatory testing – Ongoing controversies
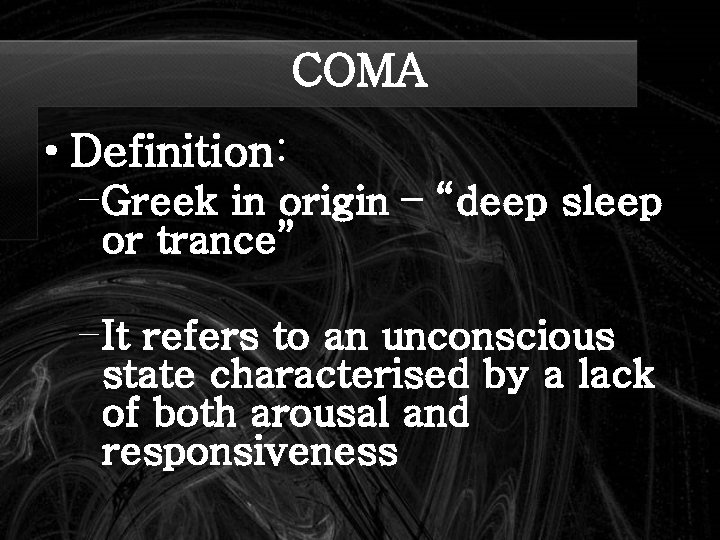
COMA • Definition: – Greek in origin – “deep sleep or trance” – It refers to an unconscious state characterised by a lack of both arousal and responsiveness

COMA • Related disorders of consciousness: – Stupor (Latin “ to be stunned”): aroused by and responsive to only the most vigorous stimuli – Minimally conscious state: Markedly impaired consciousness with evidence of self or environmental awareness (intermittent rudimentary vocal or motor responses)
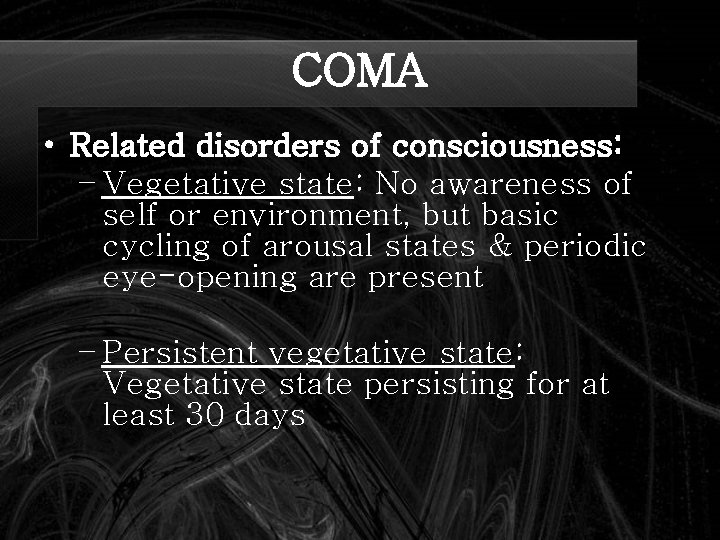
COMA • Related disorders of consciousness: – Vegetative state: No awareness of self or environment, but basic cycling of arousal states & periodic eye-opening are present – Persistent vegetative state: Vegetative state persisting for at least 30 days
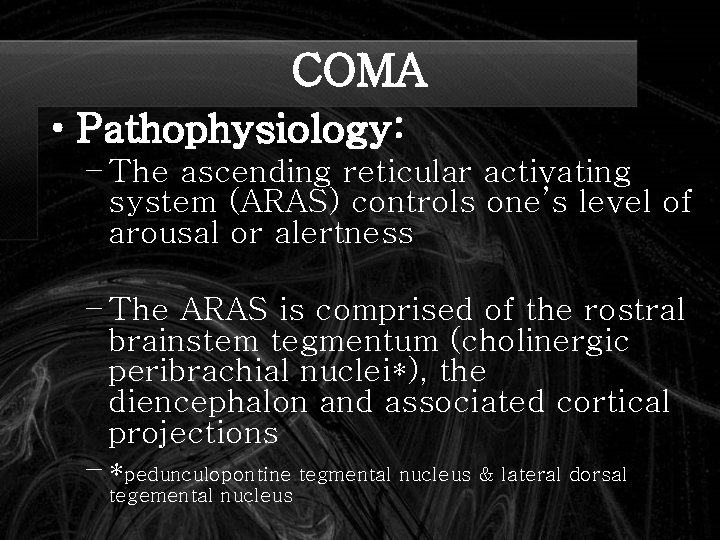
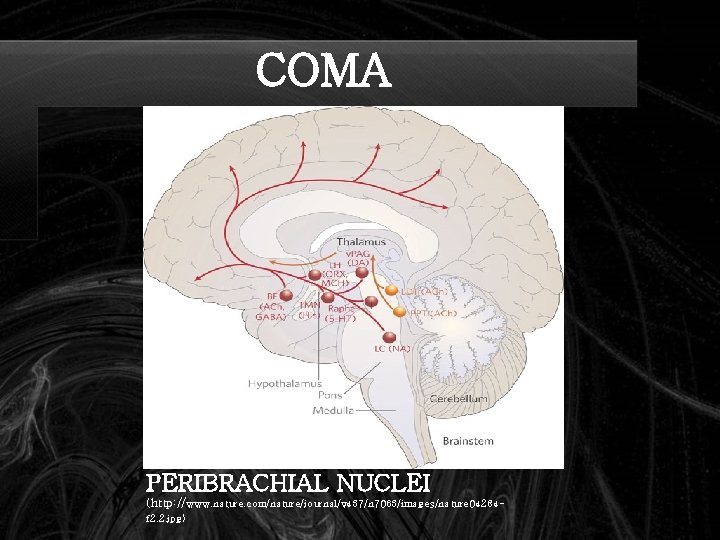
COMA • Pathophysiology: – The ascending reticular activating system (ARAS) controls one’s level of arousal or alertness – The ARAS is comprised of the rostral brainstem tegmentum (cholinergic peribrachial nuclei*), the diencephalon and associated cortical projections – *pedunculopontine tegmental nucleus & lateral dorsal tegemental nucleus

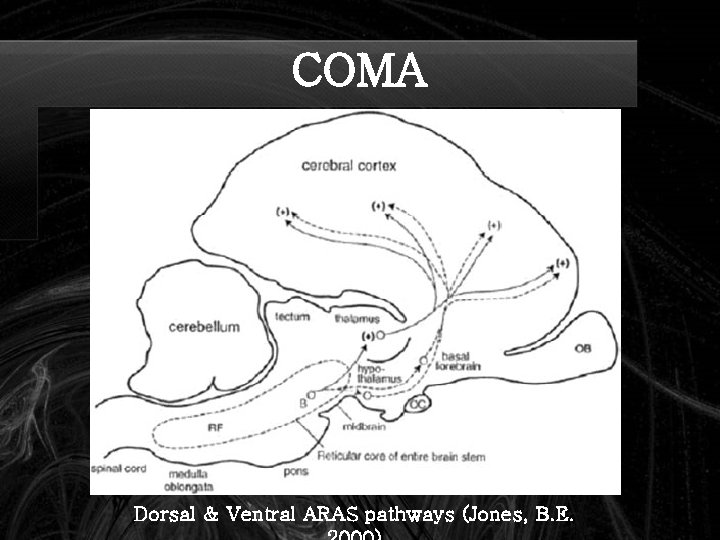
COMA • Pathophysiology: – The peribrachial nuclei project via 2 major pathways – dorsal & ventral pathways – Dorsal: glutaminergic projections from thalamic nuclei to various cortical areas – Ventral: histaminergic projections from the posterior hypothalamus (hypocretin, orexin also) & cholinergic projections from the basal forebrain to many cortical areas (Mc. Gill connection Herbert Jasper 1961 & Barbara Jones 2000)

COMA • Pathophysiology: – Sleep centre: Preoptic area of hypothalamus (GABAergic) – Notably, the ARAS pathways exhibit redundancy that may facilitate recovery of the arousal system (within 2 -3 weeks if lesions are more rostral)
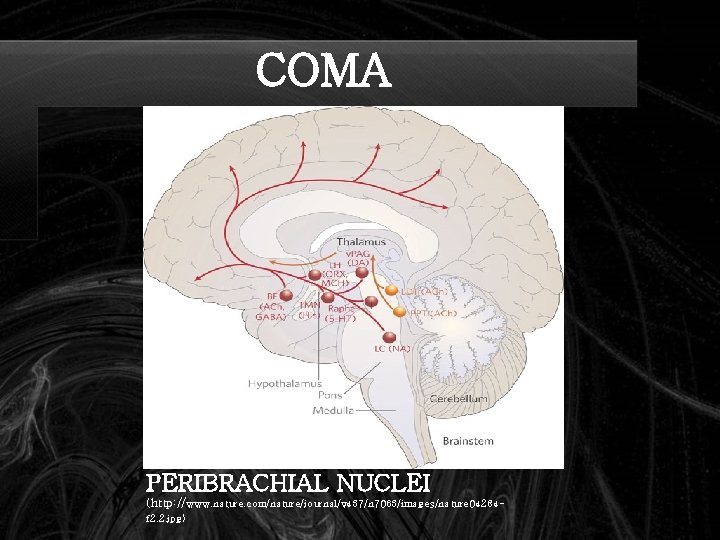
COMA PERIBRACHIAL NUCLEI (http: //www. nature. com/nature/journal/v 437/n 7063/images/nature 04284 f 2. 2. jpg)
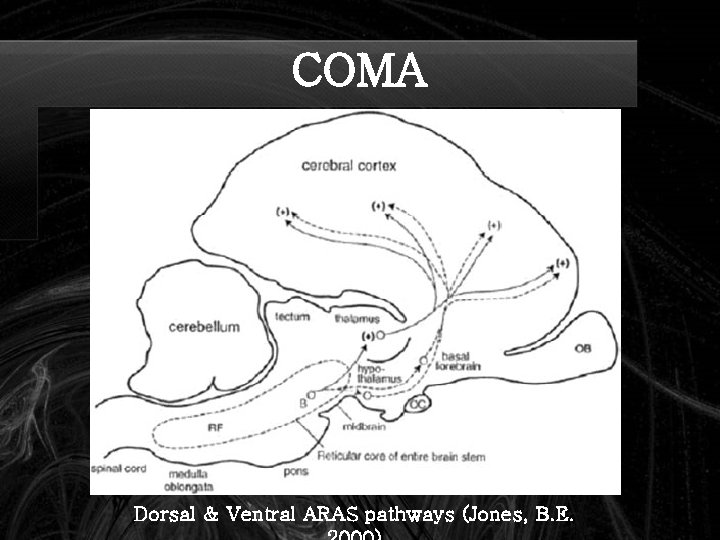
COMA Dorsal & Ventral ARAS pathways (Jones, B. E.
COMA • CAVEAT: Damage to the ARAS and associated structures or both hemispheres is usually necessary to cause a comatose state. Occasionally, left hemispheric dysfunction can per se lead to coma. . .
COMA • Aetiologies – Structural lesions: • Destructive & compressive • Ischemic stroke, haemorrhage, tumours & inflammation/infection • Long list including SDH, EDH, SAH, cerebral contusion, pontine hemorrhage, cerebellar hemorrhage/infarction, brain abscess, vasculitis, venous sinus thrombosis, etc.
COMA • Aetiologies – Herniation Syndromes: • Munro-Kellie doctrine to consider • Lateral displacement of the diencephalon (e. g. basal ganglia bleed) – monitor via displacement of the calcified pineal gland; need 9 to 13 mm shift to produce coma; related to initial impairment of consciousness
COMA • Aetiologies – Herniation Syndromes: • Falcine herniation – – expanding mass causes the cingulate gurus & pericallosal/callosomarginal arteries to be compressed & displaced under the falx – Medial wall of hemisphere - infarction & edema – Diencephalic distortion via downward herniation or midline shift
COMA • Aetiologies – Herniation Syndromes: • Uncal hernation – – expanding mass causes medial and downward herniation of the medial temporal lobe into the tentorial notch – ipsilateral fixed & dilated pupil – ocular dysmotility – contralateral (uncus presses on nearby cerebral peduncle) or ipsilateral hemiparesis (Kernohan’s sign) – PCA infarction
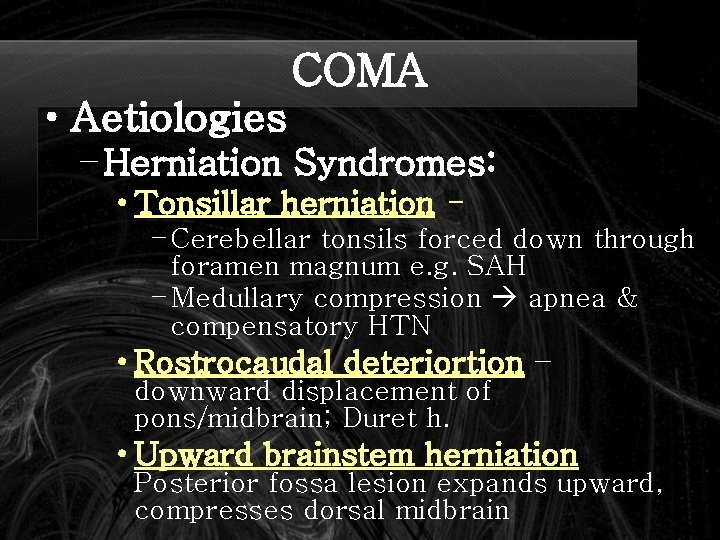
COMA • Aetiologies – Herniation Syndromes: • Central transtentorial herniation – expanding mass causes downward herniation of the diencephalon and pressure on the midbrain – Ischemia & infarction as feeder vessels are stretched and compressed – Diabetes insipidus with pituitary stalk avulsion
COMA • Aetiologies – Herniation Syndromes: • Tonsillar herniation – Cerebellar tonsils forced down through foramen magnum e. g. SAH – Medullary compression apnea & compensatory HTN • Rostrocaudal deteriortion – downward displacement of pons/midbrain; Duret h. • Upward brainstem herniation Posterior fossa lesion expands upward, compresses dorsal midbrain

COMA Herniation Syndromes http: //www. lfhk. cuni. cz/patfyz/I ntranet/Figures/88/5. 26. jpg
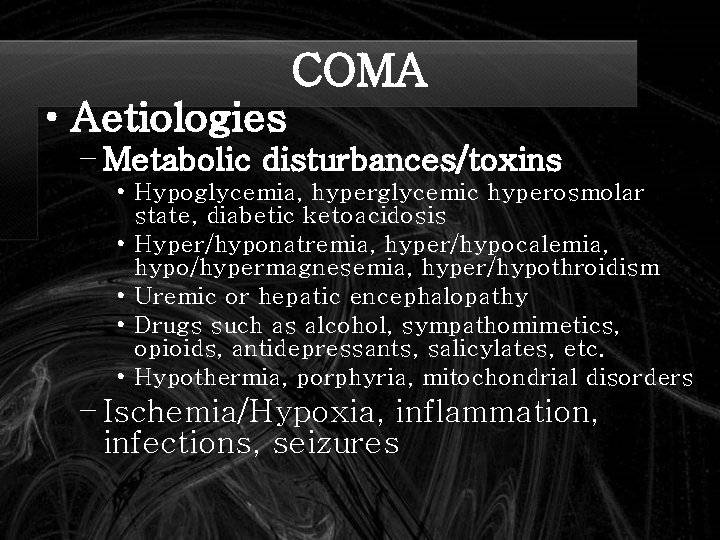
COMA • Aetiologies – Metabolic disturbances/toxins • Hypoglycemia, hyperglycemic hyperosmolar state, diabetic ketoacidosis • Hyper/hyponatremia, hyper/hypocalemia, hypo/hypermagnesemia, hyper/hypothroidism • Uremic or hepatic encephalopathy • Drugs such as alcohol, sympathomimetics, opioids, antidepressants, salicylates, etc. • Hypothermia, porphyria, mitochondrial disorders – Ischemia/Hypoxia, inflammation, infections, seizures
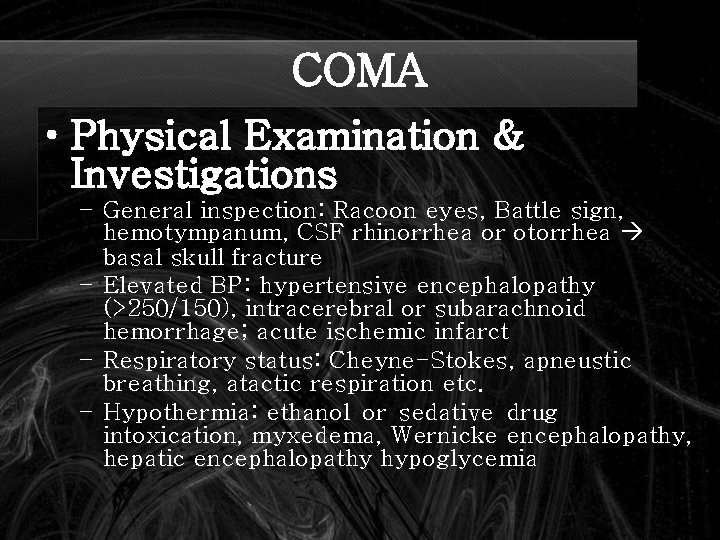
COMA • Physical Examination & Investigations – General inspection: Racoon eyes, Battle sign, hemotympanum, CSF rhinorrhea or otorrhea basal skull fracture – Elevated BP: hypertensive encephalopathy (>250/150), intracerebral or subarachnoid hemorrhage; acute ischemic infarct – Respiratory status: Cheyne-Stokes, apneustic breathing, atactic respiration etc. – Hypothermia: ethanol or sedative drug intoxication, myxedema, Wernicke encephalopathy, hepatic encephalopathy hypoglycemia
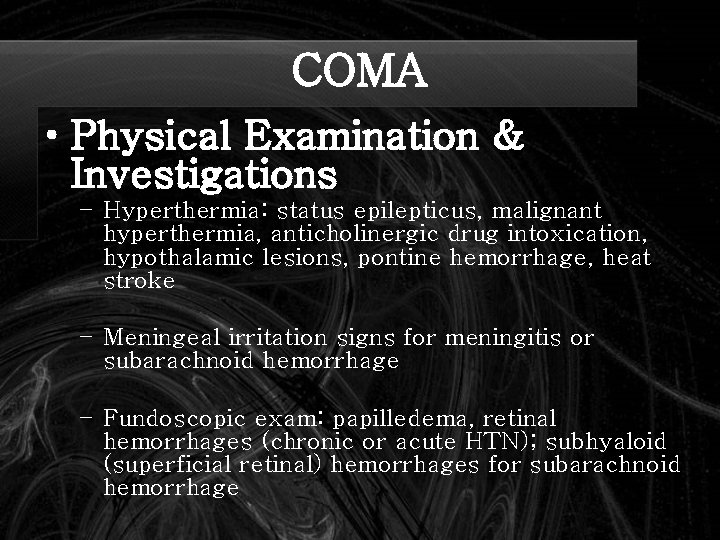
COMA • Physical Examination & Investigations – Hyperthermia: status epilepticus, malignant hyperthermia, anticholinergic drug intoxication, hypothalamic lesions, pontine hemorrhage, heat stroke – Meningeal irritation signs for meningitis or subarachnoid hemorrhage – Fundoscopic exam: papilledema, retinal hemorrhages (chronic or acute HTN); subhyaloid (superficial retinal) hemorrhages for subarachnoid hemorrhage
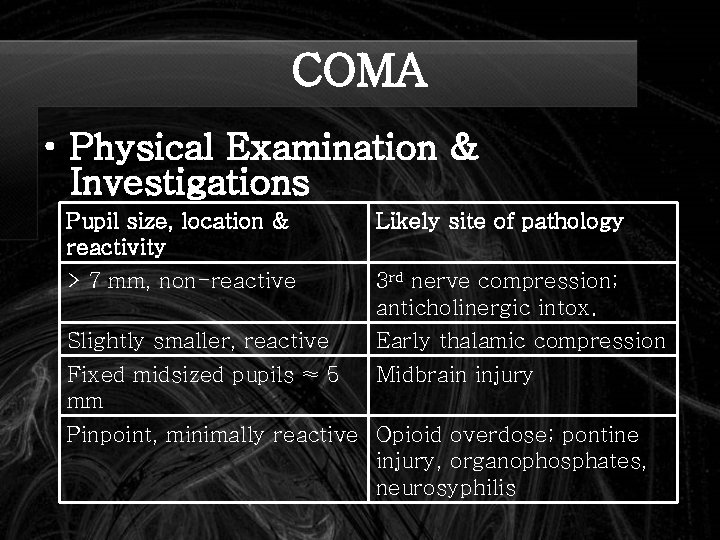
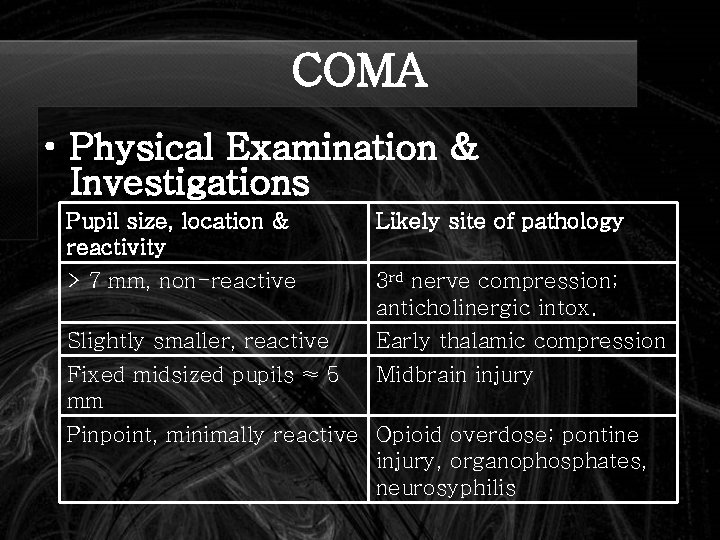
COMA • Physical Examination & Investigations Pupil size, location & reactivity Likely site of pathology > 7 mm, non-reactive 3 rd nerve compression; anticholinergic intox. Slightly smaller, reactive Early thalamic compression Fixed midsized pupils ≈ 5 mm Midbrain injury Pinpoint, minimally reactive Opioid overdose; pontine injury, organophosphates, neurosyphilis
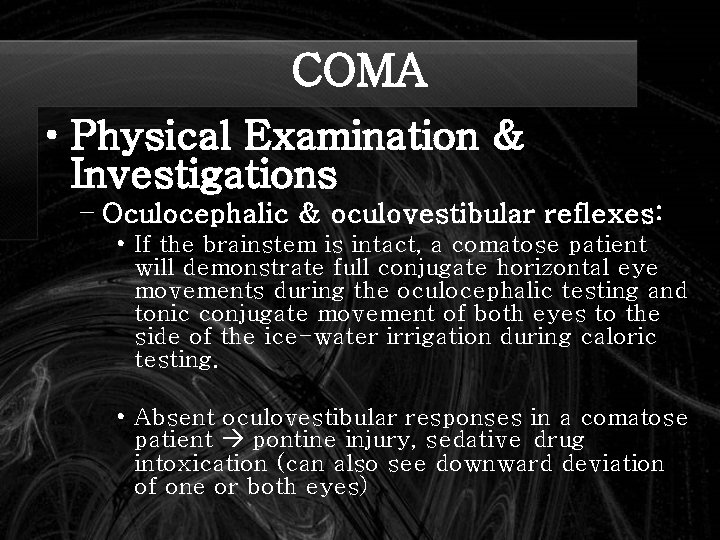
COMA • Physical Examination & Investigations – Oculocephalic & oculovestibular reflexes: • If the brainstem is intact, a comatose patient will demonstrate full conjugate horizontal eye movements during the oculocephalic testing and tonic conjugate movement of both eyes to the side of the ice-water irrigation during caloric testing. • Absent oculovestibular responses in a comatose patient pontine injury, sedative drug intoxication (can also see downward deviation of one or both eyes)
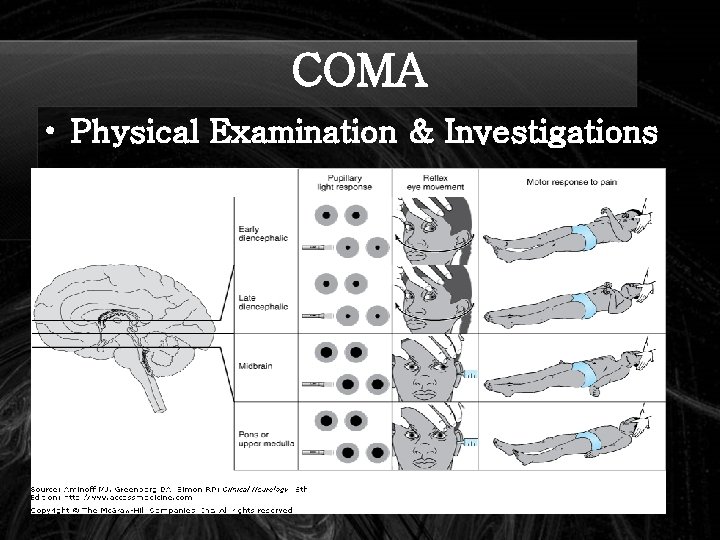
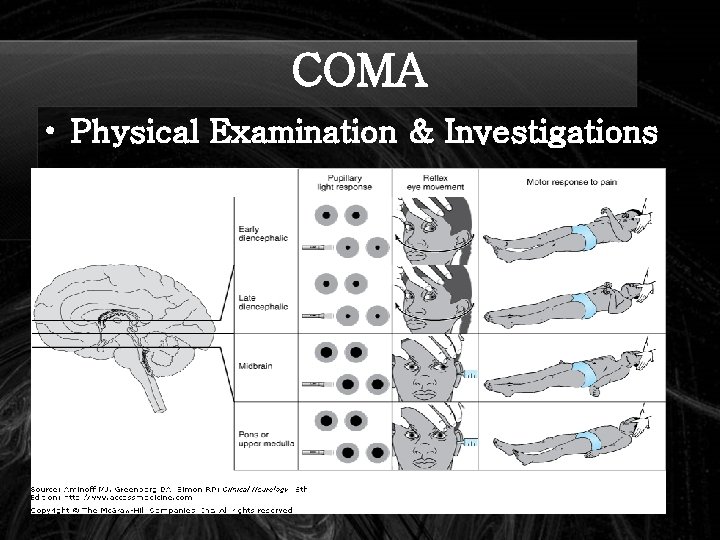
COMA • Physical Examination & Investigations
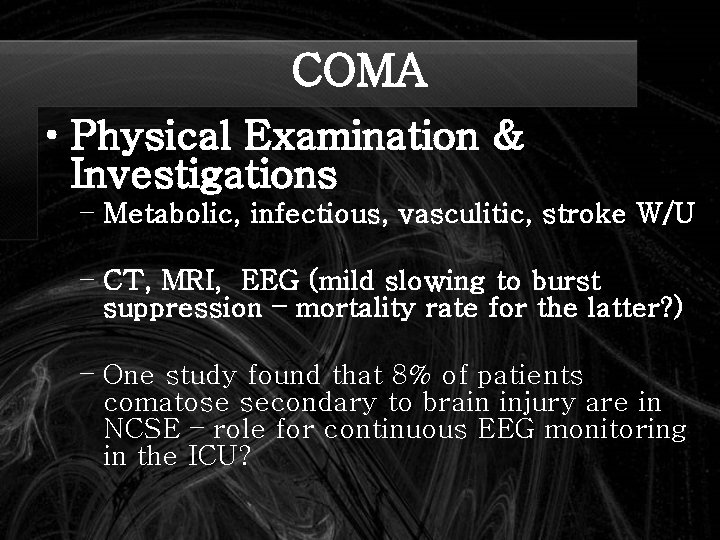
COMA • Physical Examination & Investigations – Metabolic, infectious, vasculitic, stroke W/U – CT, MRI, EEG (mild slowing to burst suppression – mortality rate for the latter? ) – One study found that 8% of patients comatose secondary to brain injury are in NCSE – role for continuous EEG monitoring in the ICU?
COMA • Differential Diagnosis – the pseudocomas: – Locked-in syndrome – Akinetic mutism – Catatonia – Psychogenic unresponsiveness (which tests can help us differentiate it from a true coma) – Minimally conscious – Vegetative states
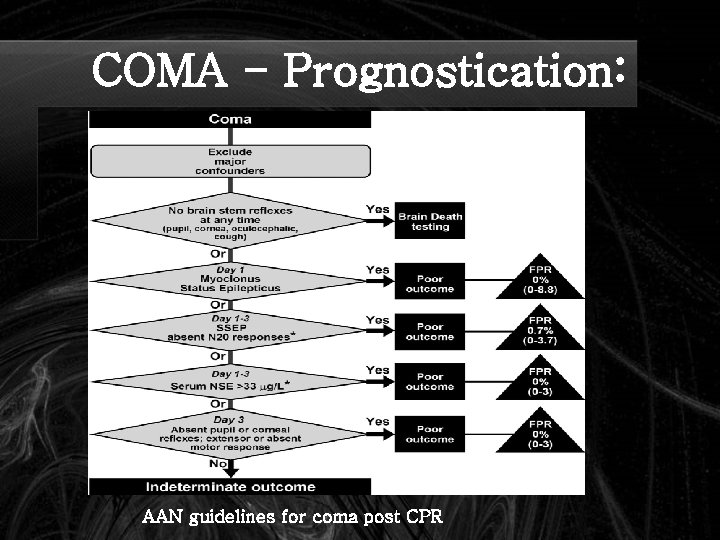
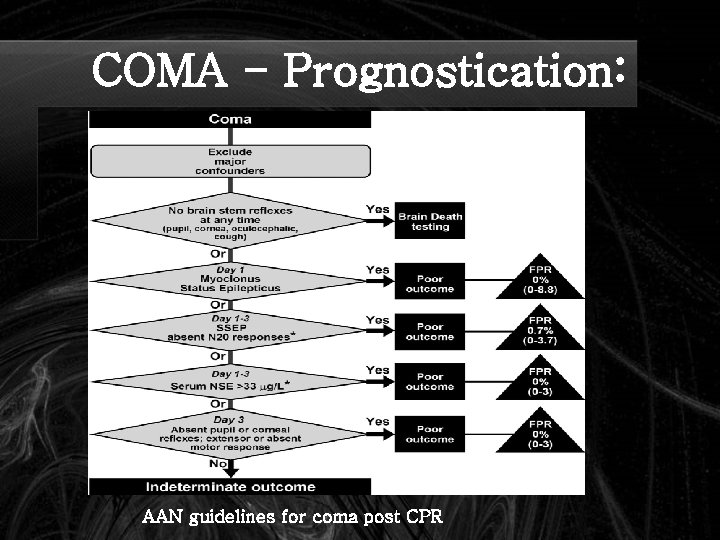
COMA - Prognostication: AAN guidelines for coma post CPR

COMA - Prognostication Probability of Recovering Independent Function (%) Time Since onset of Coma (Days) Sign 0 1 3 7 Data from Levy et al 2 No verbal response 13 8 5 6 No eye opening 11 6 4 0 Unreactive pupils 0 0 No spontaneous eye movements 6 5 2 0 No caloric responses 5 6 6 0 Extensor posturing 18 0 0 0 Flexor posturing 14 3 0 0 Absent motor responses 4 3 0 0 Data from Edgren et al 3 No eye opening to pain 31 8 0 0 Unreactive pupils 17 7 0 0 Prognostic Signs in Coma from Global Cerebral Ischemia. Comparison of the Findings in Two Studies (Clinical Neurology, Aminoff)
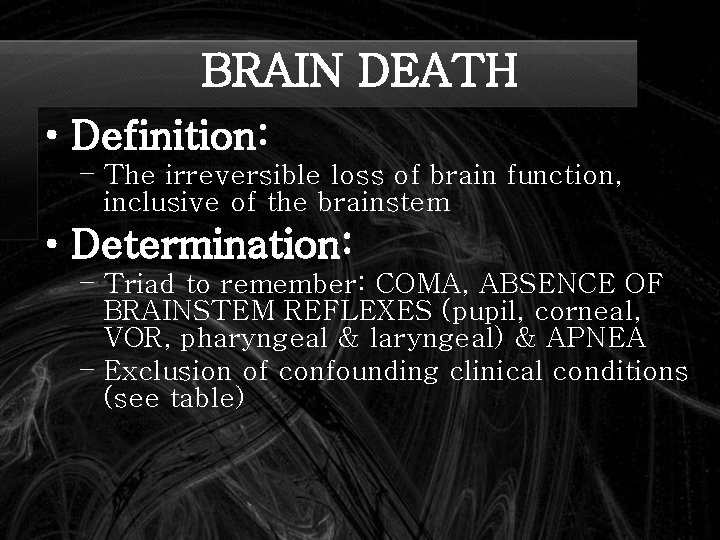
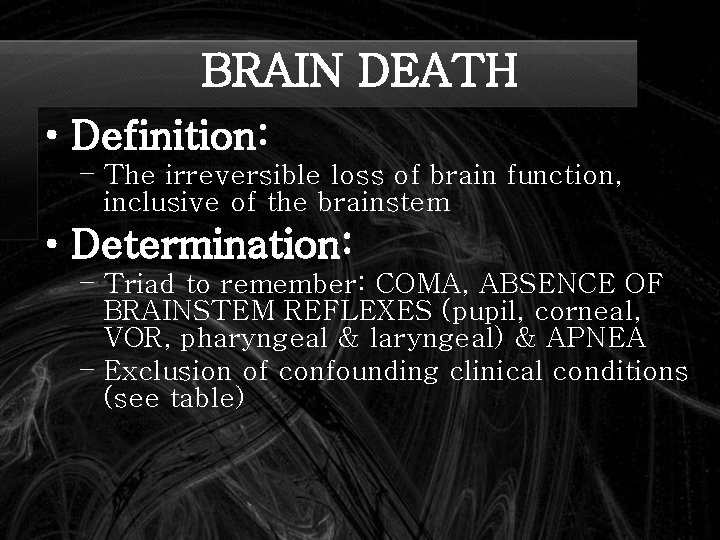
BRAIN DEATH • Definition: – The irreversible loss of brain function, inclusive of the brainstem • Determination: – Triad to remember: COMA, ABSENCE OF BRAINSTEM REFLEXES (pupil, corneal, VOR, pharyngeal & laryngeal) & APNEA – Exclusion of confounding clinical conditions (see table)
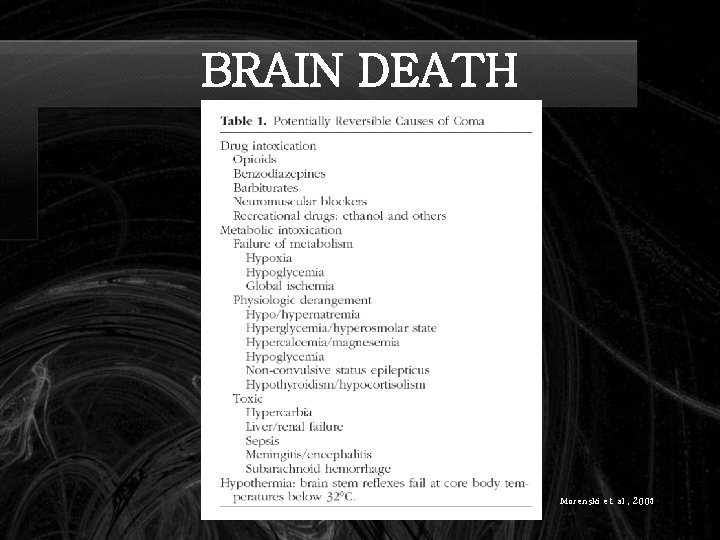
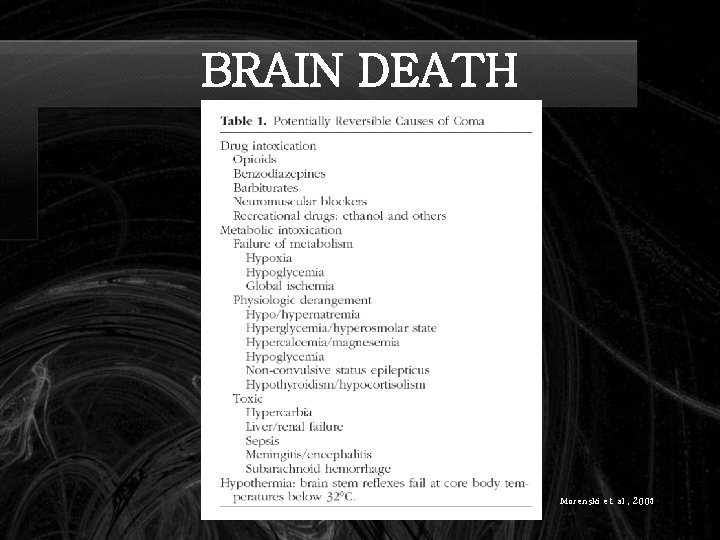
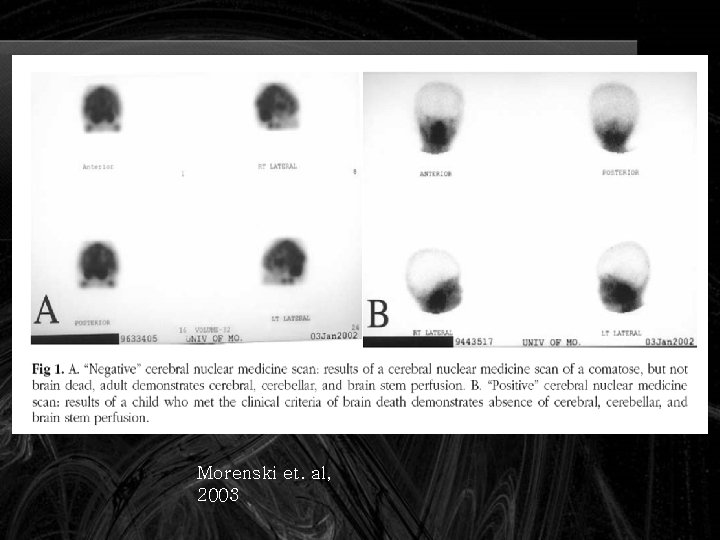
BRAIN DEATH Morenski et. al , 2003

BRAIN DEATH • Determination continued:

BRAIN DEATH • Spontaneous and reflex movements that may be seen in brain death:

BRAIN DEATH • Ancillary tests: – Transcranial doppler US – Conventional angiography – EEG – Technetium-99 m brain scan – SSEPs: N 20 -P 22 absence bilaterally with median nerve stimulation
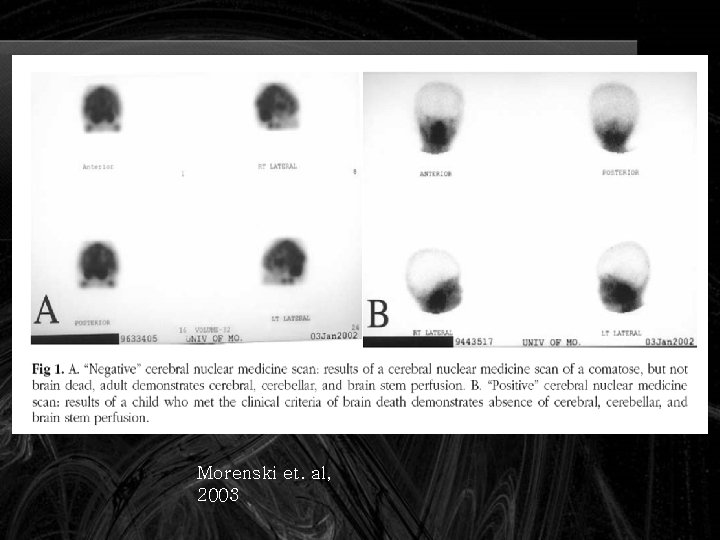
Morenski et. al, 2003
A few good references • AAN Determining Brain Death in Adults Current guidelines • Prediction of Outcome in Comatose Survivors after Cardiopulmonary Resuscitation Current guidelines July 2006 • Plum and Posner's Diagnosis of Stupor and Coma, 4 th edition (☆☆☆☆☆) – great book!
 July 30 2009 nasa
July 30 2009 nasa Nbme surgery shelf percentiles 2021
Nbme surgery shelf percentiles 2021 The walton centre for neurology and neurosurgery
The walton centre for neurology and neurosurgery Neurology near loomis
Neurology near loomis Mppd unhas
Mppd unhas Joseph berger md neurology
Joseph berger md neurology Mary bridge neurology clinic
Mary bridge neurology clinic Midwest neurology
Midwest neurology Midwest neurology
Midwest neurology Nlff neurology
Nlff neurology Neurology strength scale
Neurology strength scale Tufts neurology residency
Tufts neurology residency Ulster hospital neurology consultants
Ulster hospital neurology consultants Jung
Jung Transcranial ultrasound
Transcranial ultrasound Monomyth amplification
Monomyth amplification Neurology
Neurology Nlff neuro
Nlff neuro Vanderbilt neurology residents
Vanderbilt neurology residents Crude touch
Crude touch Nlff neuro
Nlff neuro Dr nin bajaj
Dr nin bajaj West coast neurology
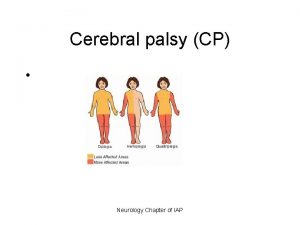
West coast neurology Cerebral palsy iap
Cerebral palsy iap Miqtu
Miqtu Nex exam neurology
Nex exam neurology Pmg neurology
Pmg neurology Uf neurology residents
Uf neurology residents Umass surgery residents
Umass surgery residents July 2 1937 amelia earhart
July 2 1937 amelia earhart Miss cuba receives an invitation
Miss cuba receives an invitation Tender definition
Tender definition Harris burdick oscar and alphonse
Harris burdick oscar and alphonse Catawba indian nation bingo
Catawba indian nation bingo On july 18 2001 a train carrying hazardous chemicals
On july 18 2001 a train carrying hazardous chemicals July 1969
July 1969