Pathophysiology Urinary System Diseases Kidney Anatomy Histology Located
- Slides: 34
Pathophysiology Urinary System Diseases
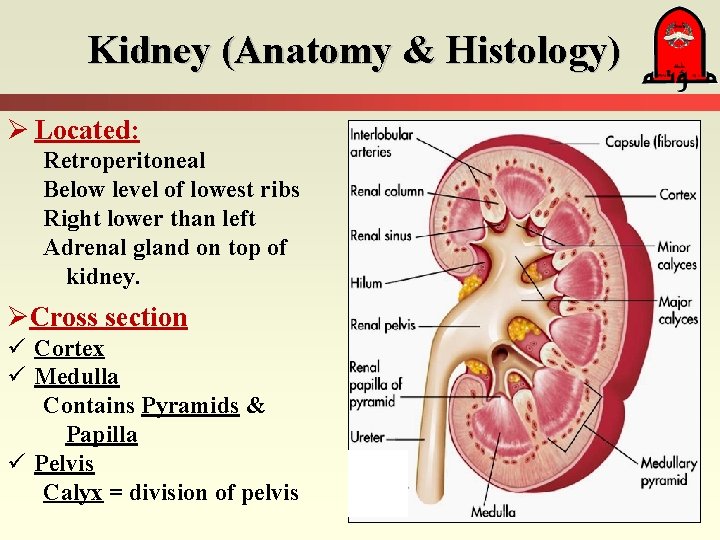
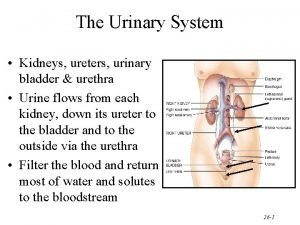
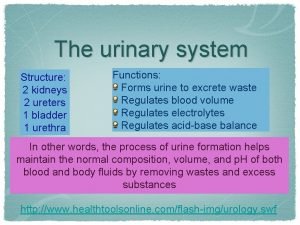
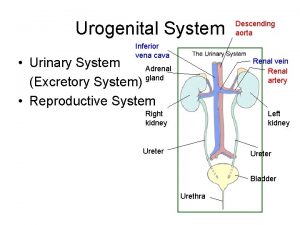
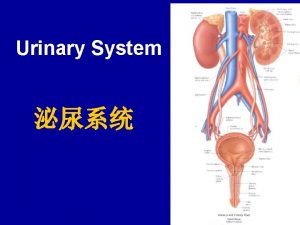
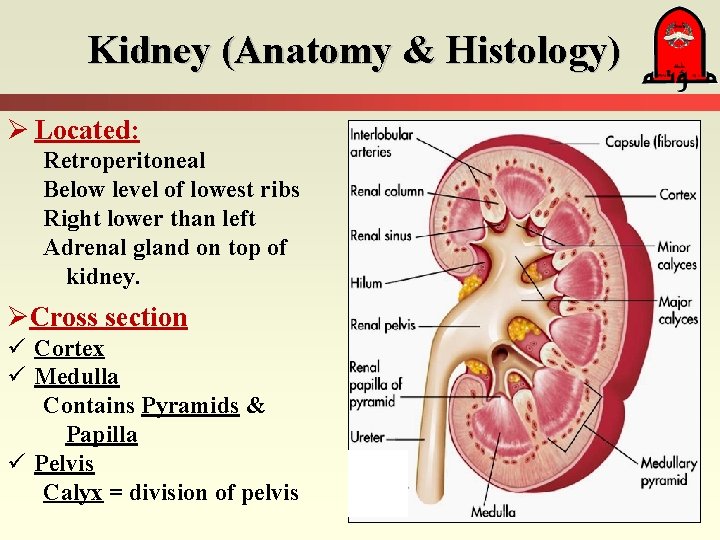
Kidney (Anatomy & Histology) Ø Located: Retroperitoneal Below level of lowest ribs Right lower than left Adrenal gland on top of kidney. ØCross section ü Cortex ü Medulla Contains Pyramids & Papilla ü Pelvis Calyx = division of pelvis
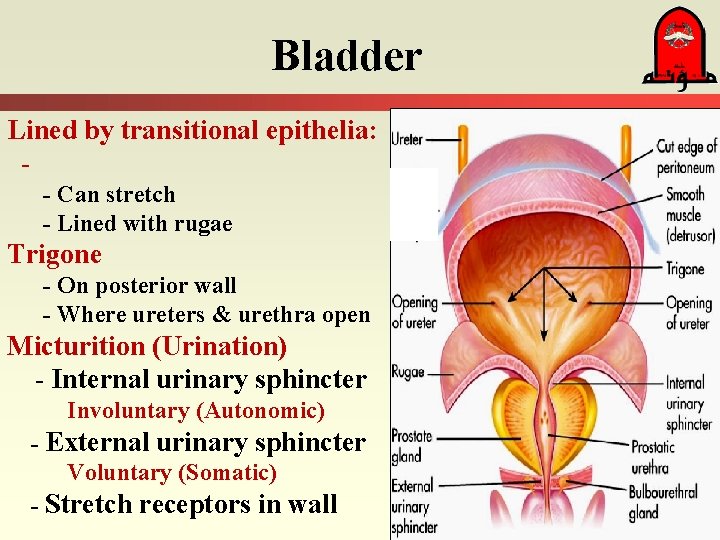
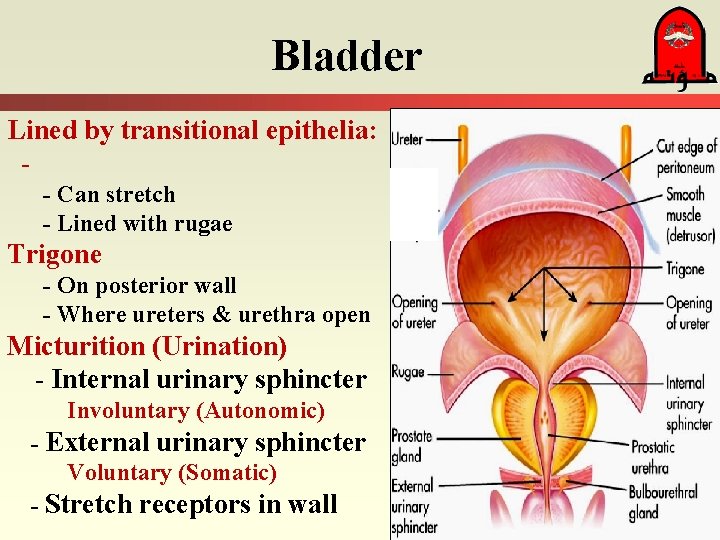
Bladder Lined by transitional epithelia: - Can stretch - Lined with rugae Trigone - On posterior wall - Where ureters & urethra open Micturition (Urination) - Internal urinary sphincter Involuntary (Autonomic) - External urinary sphincter Voluntary (Somatic) - Stretch receptors in wall
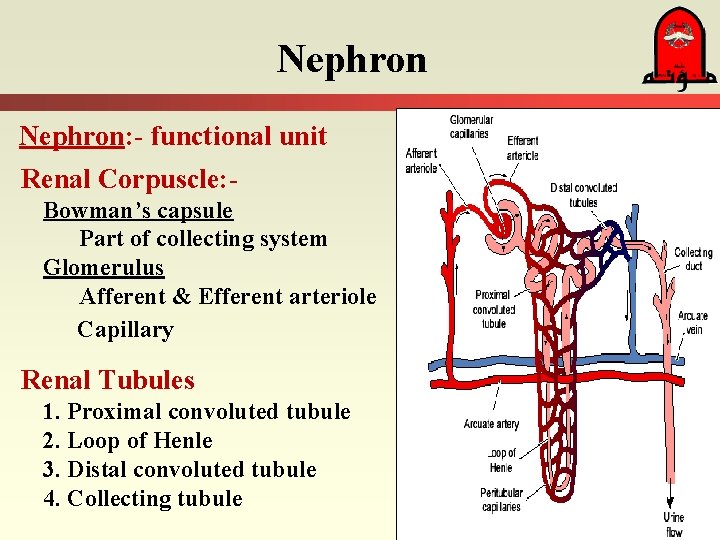
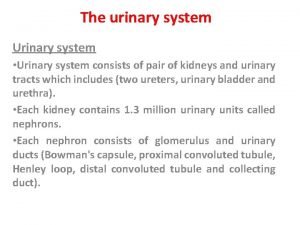
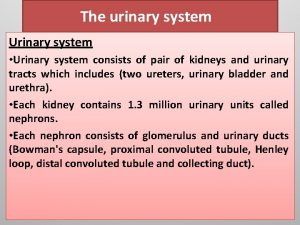
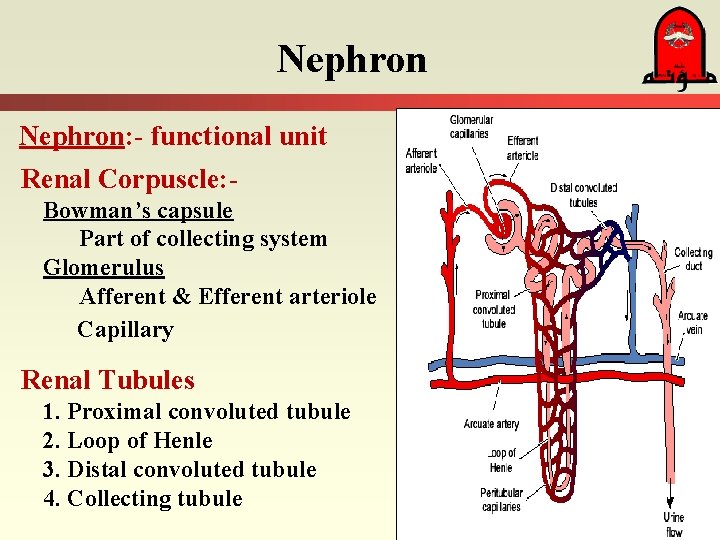
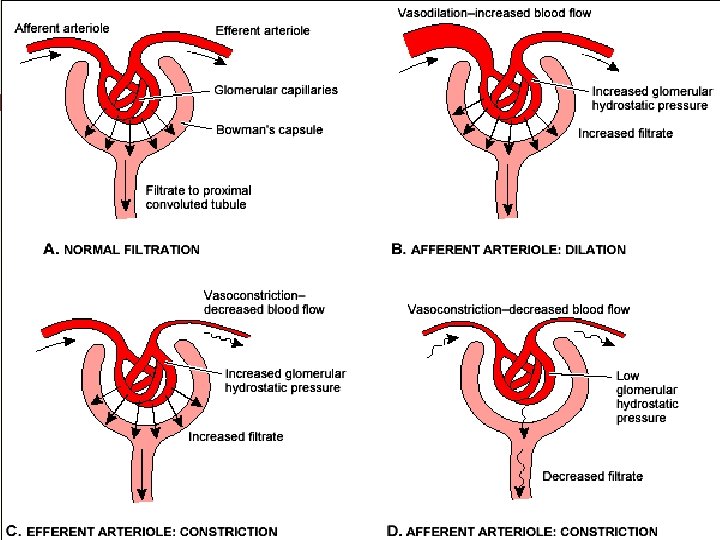
Nephron: - functional unit Renal Corpuscle: Bowman’s capsule Part of collecting system Glomerulus Afferent & Efferent arteriole Capillary Renal Tubules 1. Proximal convoluted tubule 2. Loop of Henle 3. Distal convoluted tubule 4. Collecting tubule
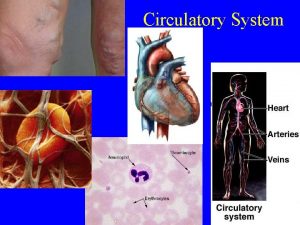
Functions of the kidney 1. Excretion - Removes nitrogenous wastes: Urea, Uric acid, Creatinine, Ammonia - Removes toxic subs. 2. Maintains homeostasis: Balance of - Fluid - Electrolyte - Acid-base 3. Regulation of Blood volume & Pressure - Renin-Angiotensin - Aldosterone - ADH - Erythropoietin
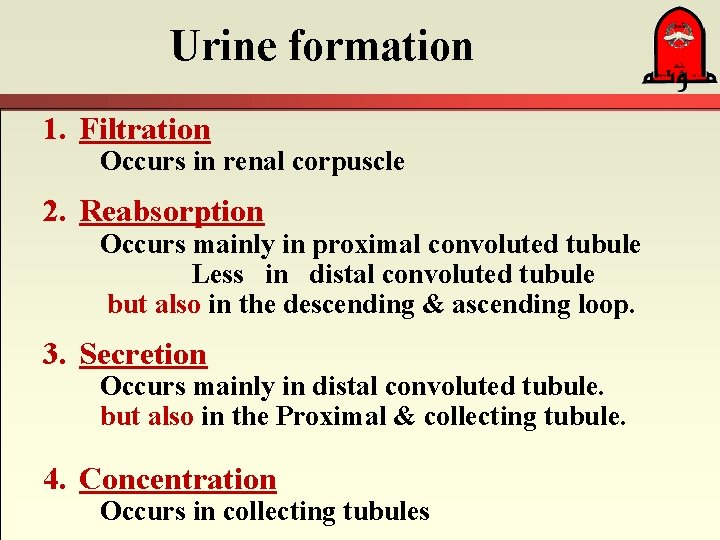
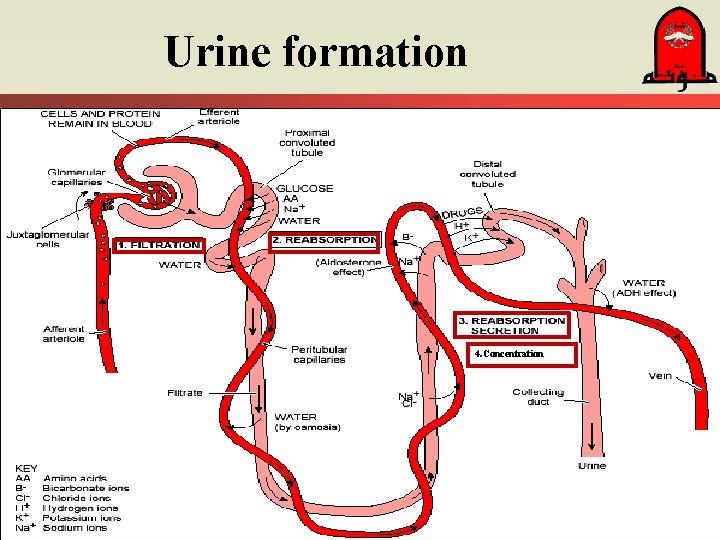
Urine formation 1. Filtration Occurs in renal corpuscle 2. Reabsorption Occurs mainly in proximal convoluted tubule Less in distal convoluted tubule but also in the descending & ascending loop. 3. Secretion Occurs mainly in distal convoluted tubule. but also in the Proximal & collecting tubule. 4. Concentration Occurs in collecting tubules
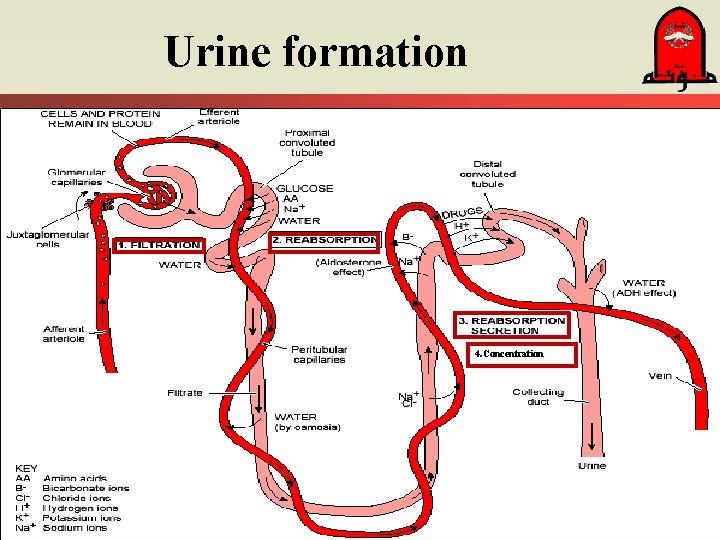
Urine formation 4. Concentration
Factors affect urine Vol. production: 1. Glomerular filtration rate (GFR) Determined by unique arrangement of B. flow. 2. Hormonal secretion Determined by fluid & electrolyte balance
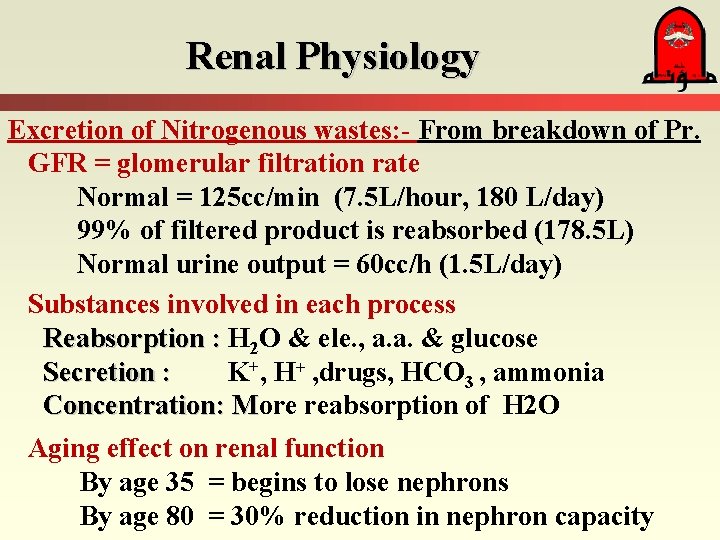
Renal Physiology Excretion of Nitrogenous wastes: - From breakdown of Pr. GFR = glomerular filtration rate Normal = 125 cc/min (7. 5 L/hour, 180 L/day) 99% of filtered product is reabsorbed (178. 5 L) Normal urine output = 60 cc/h (1. 5 L/day) Substances involved in each process Reabsorption : H 2 O & ele. , a. a. & glucose Secretion : K+, H+ , drugs, HCO 3 , ammonia Concentration: More reabsorption of H 2 O M Aging effect on renal function By age 35 = begins to lose nephrons By age 80 = 30% reduction in nephron capacity
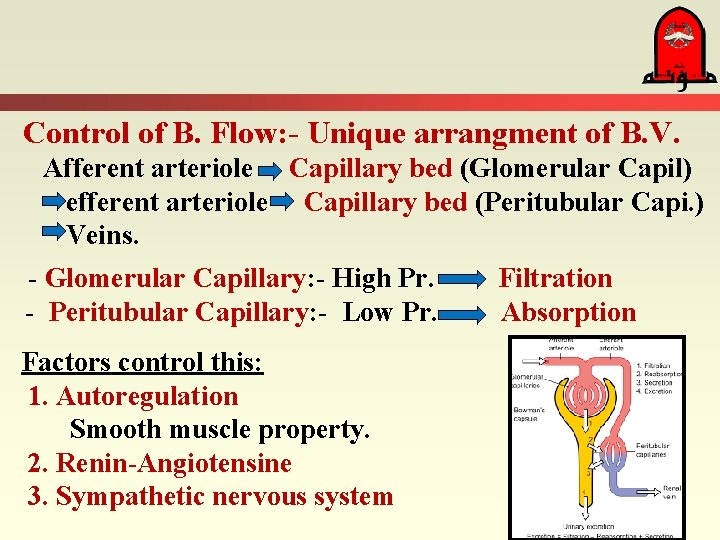
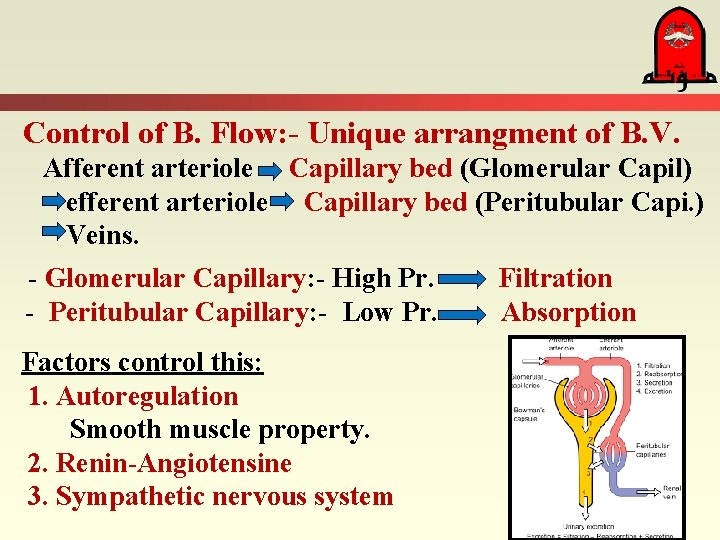
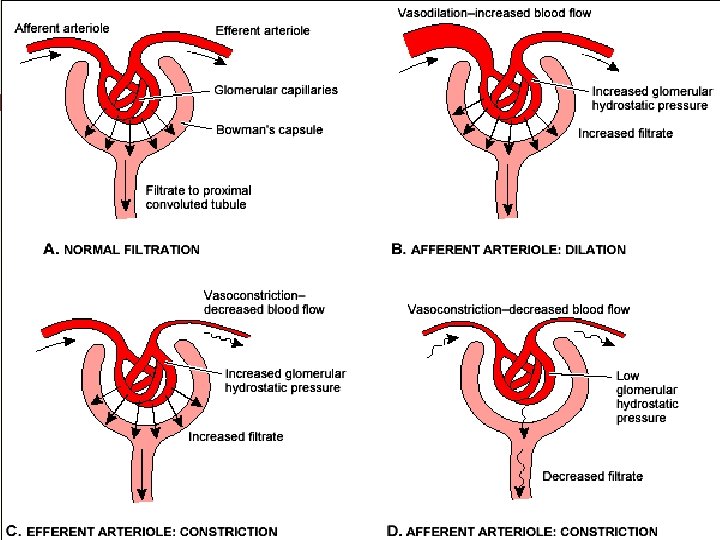
Control of B. Flow: - Unique arrangment of B. V. Afferent arteriole Capillary bed (Glomerular Capil) efferent arteriole Capillary bed (Peritubular Capi. ) Veins. - Glomerular Capillary: - High Pr. - Peritubular Capillary: - Low Pr. Factors control this: 1. Autoregulation Smooth muscle property. 2. Renin-Angiotensine 3. Sympathetic nervous system Filtration Absorption
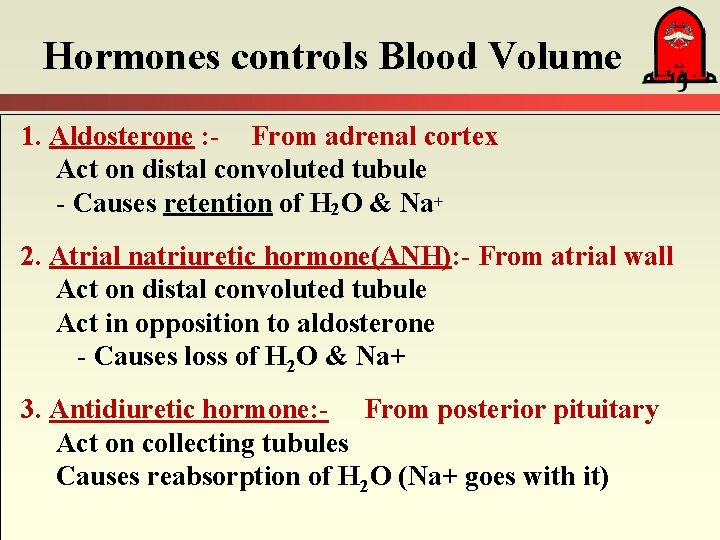
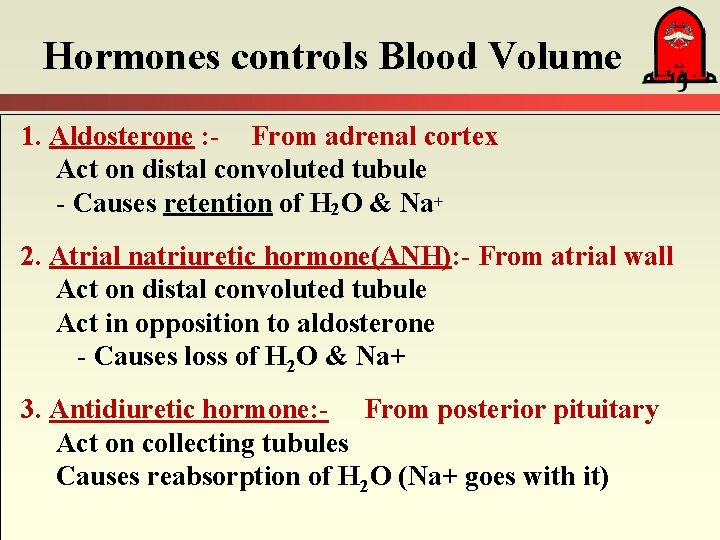
Hormones controls Blood Volume 1. Aldosterone : - From adrenal cortex Act on distal convoluted tubule - Causes retention of H 2 O & Na+ 2. Atrial natriuretic hormone(ANH): - From atrial wall Act on distal convoluted tubule Act in opposition to aldosterone - Causes loss of H 2 O & Na+ 3. Antidiuretic hormone: - From posterior pituitary Act on collecting tubules Causes reabsorption of H 2 O (Na+ goes with it)
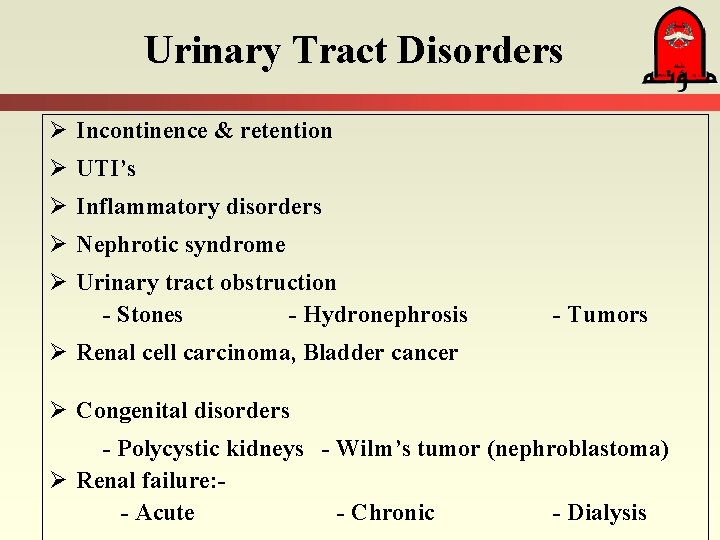
Urinary Tract Disorders Ø Incontinence & retention Ø UTI’s Ø Inflammatory disorders Ø Nephrotic syndrome Ø Urinary tract obstruction - Stones - Hydronephrosis - Tumors Ø Renal cell carcinoma, Bladder cancer Ø Congenital disorders - Polycystic kidneys - Wilm’s tumor (nephroblastoma) Ø Renal failure: - Acute - Chronic - Dialysis
Incontinence, retention & catheters Urinary Incontinence: - (Enuresis) Loss of voluntary control of bladder Frequently called “neurogenic bladder” Enuresis = involuntary urination after age 4 -5 y Types of incontinence: - Stress: with laughing, coughing - Urge: - Overflow Urinary retention Called “residual urine” Causes : - Anatomical defects: - Prostate - Neurogenic defects: - Spinal cord ingury Treated with “catheterization” (Foley catheter).
Urinary Tract Infections Urethritis; Cystitis; Pyelonephritis Etiology: – Ascending infection ----- women > men – Blood borne pathogens – Incomplete emptying of bladder with urinary stasis * Prostatic hypertrophy with urinary retention * Pregnancy associated with stasis, stone Diagnosis: • Dysuria, urgency, & nocturia • Systemically get fever & malaise • Tenderness in pyelonephritis § Note glomerulonephritis is vastly different with regards etiology & pathophysiology
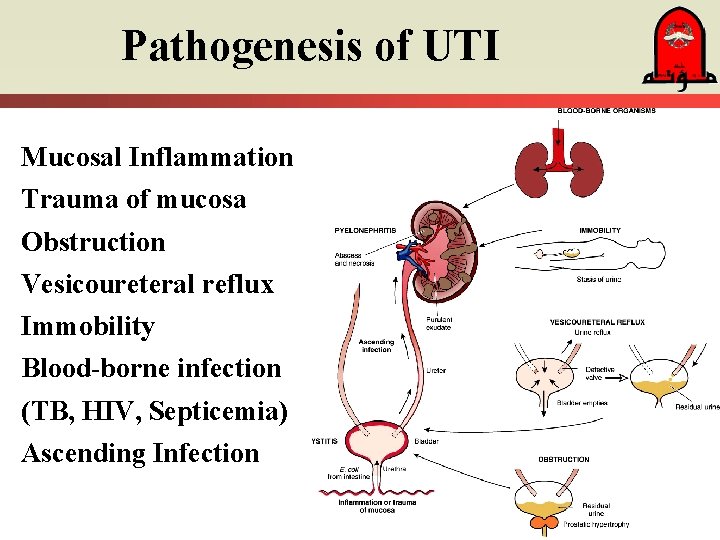
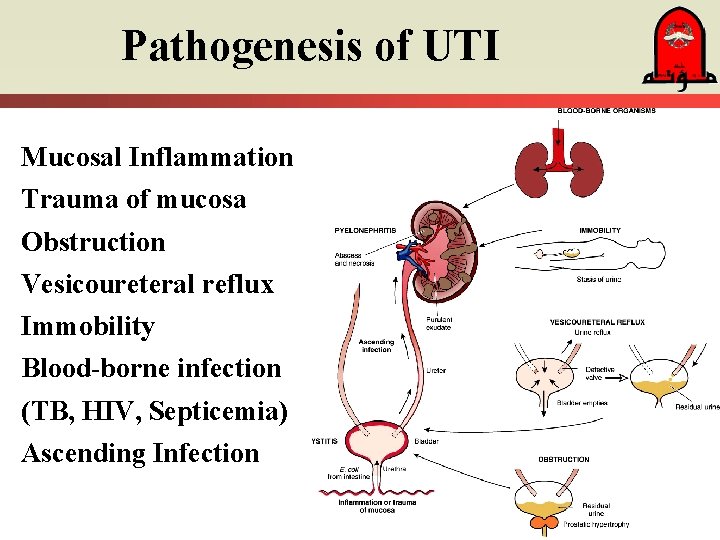
Pathogenesis of UTI Mucosal Inflammation Trauma of mucosa Obstruction Vesicoureteral reflux Immobility Blood-borne infection (TB, HIV, Septicemia) Ascending Infection
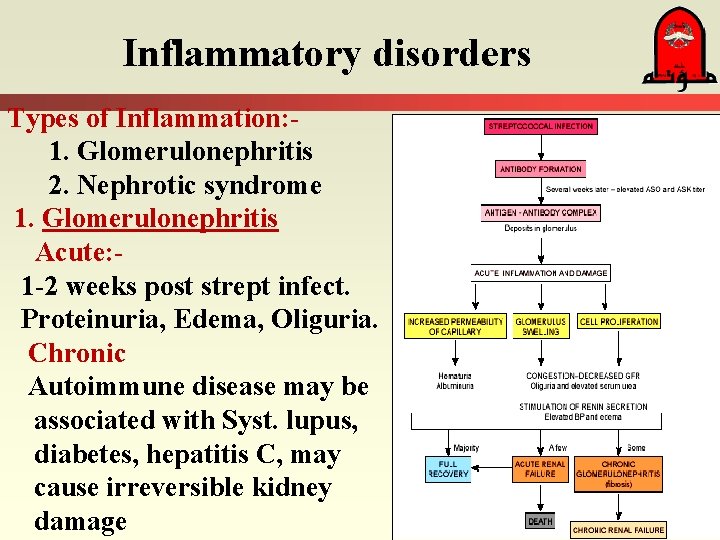
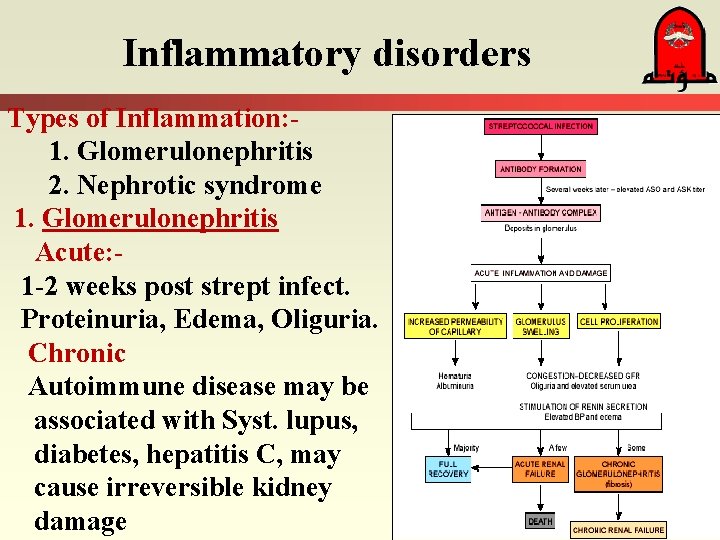
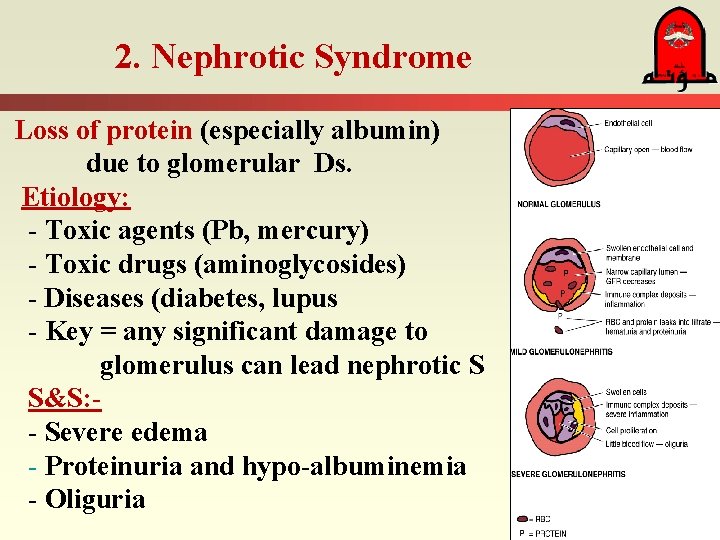
Inflammatory disorders Types of Inflammation: 1. Glomerulonephritis 2. Nephrotic syndrome 1. Glomerulonephritis Acute: 1 -2 weeks post strept infect. Proteinuria, Edema, Oliguria. Chronic Autoimmune disease may be associated with Syst. lupus, diabetes, hepatitis C, may cause irreversible kidney damage
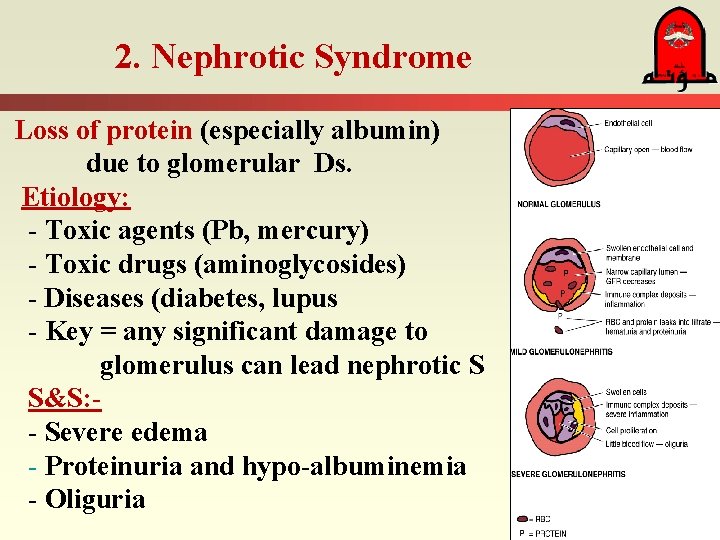
2. Nephrotic Syndrome Loss of protein (especially albumin) due to glomerular Ds. Etiology: - Toxic agents (Pb, mercury) - Toxic drugs (aminoglycosides) - Diseases (diabetes, lupus - Key = any significant damage to glomerulus can lead nephrotic S S&S: - Severe edema - Proteinuria and hypo-albuminemia - Oliguria
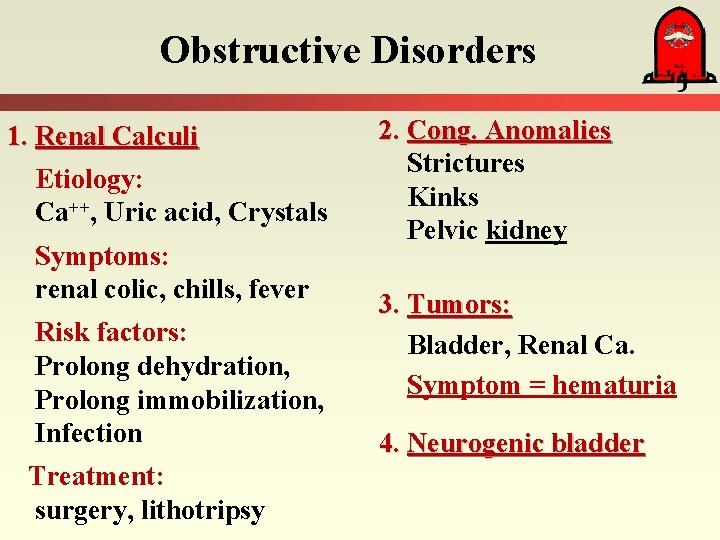
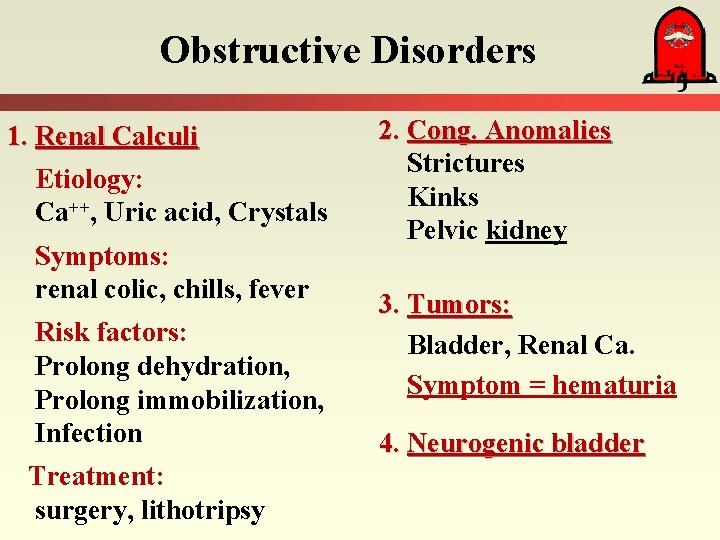
Obstructive Disorders 1. Renal Calculi Etiology: Ca++, Uric acid, Crystals Symptoms: renal colic, chills, fever Risk factors: Prolong dehydration, Prolong immobilization, Infection Treatment: surgery, lithotripsy 2. Cong. Anomalies Strictures Kinks Pelvic kidney 3. Tumors: Bladder, Renal Ca. Symptom = hematuria 4. Neurogenic bladder
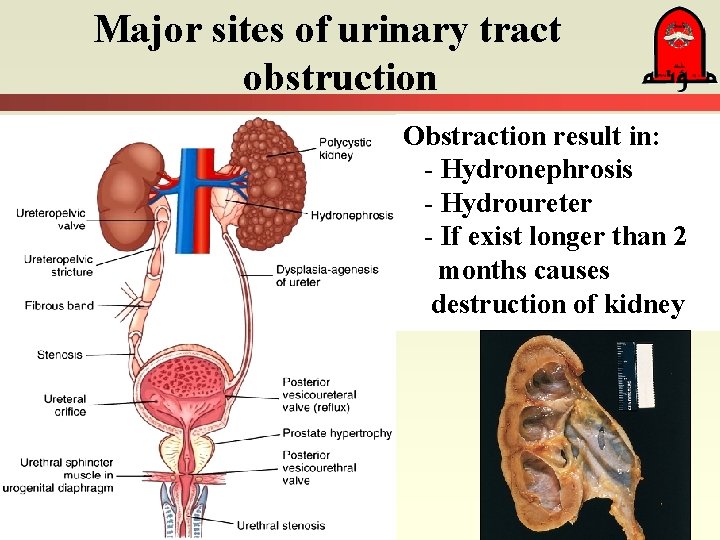
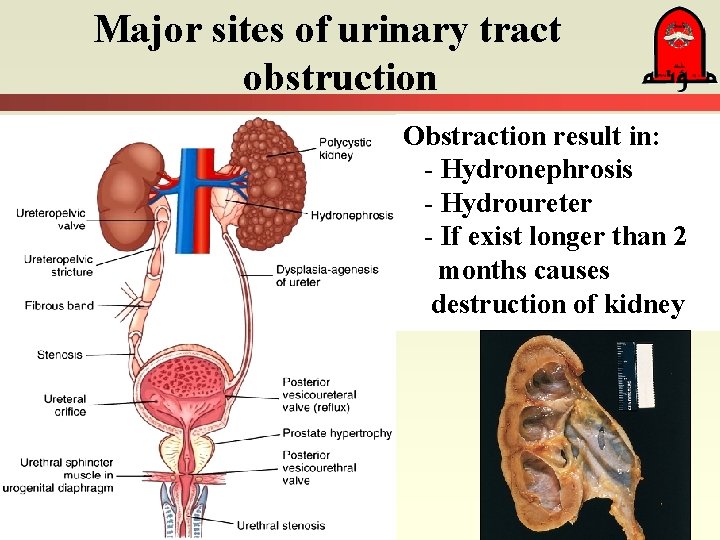
Major sites of urinary tract obstruction Obstraction result in: - Hydronephrosis - Hydroureter - If exist longer than 2 months causes destruction of kidney
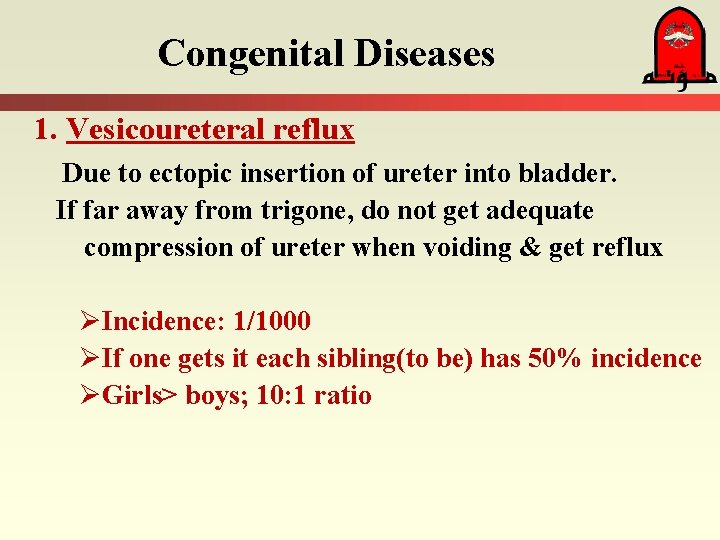
Congenital Diseases 1. Vesicoureteral reflux Due to ectopic insertion of ureter into bladder. If far away from trigone, do not get adequate compression of ureter when voiding & get reflux ØIncidence: 1/1000 ØIf one gets it each sibling(to be) has 50% incidence ØGirls> boys; 10: 1 ratio
Congenital Diseases 2. Ectopic kidney • May get kinking of ureter • Usually in pelvis • Asymptomatic 3. Renal agenesis Usually unilateral, left kidney > right 2 types: (1) occurs randomly (2) genetic - Asymptomatic: Remaining kidney becomes large due to compensatory hypertrophy
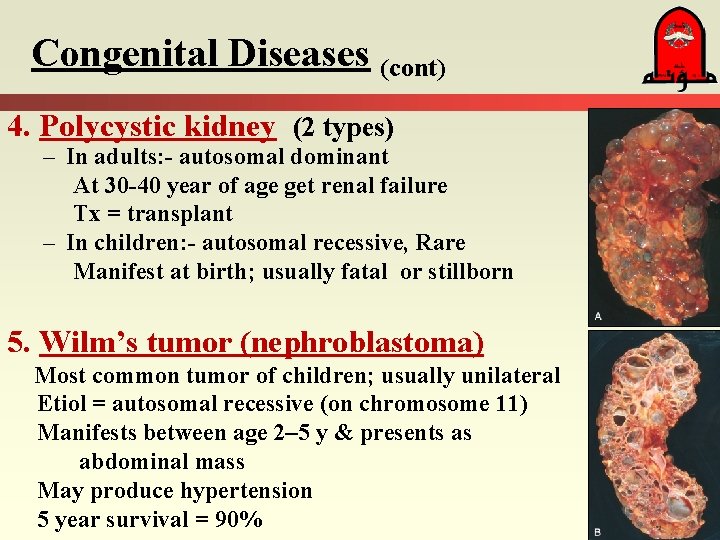
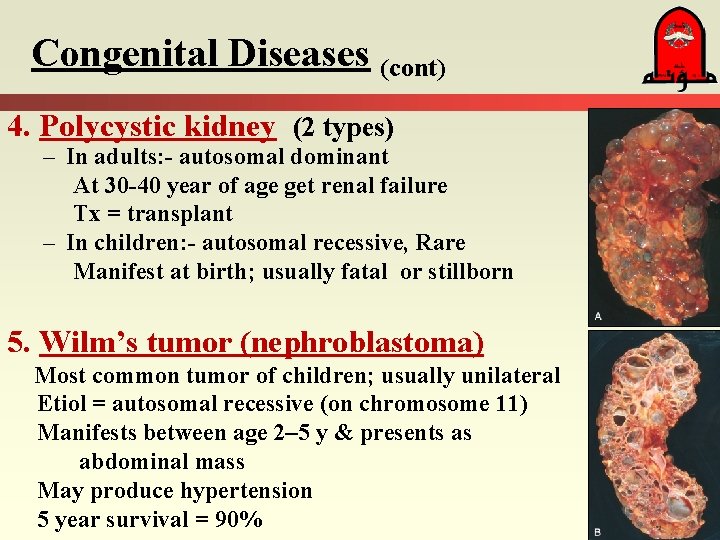
Congenital Diseases (cont) 4. Polycystic kidney (2 types) – In adults: - autosomal dominant At 30 -40 year of age get renal failure Tx = transplant – In children: - autosomal recessive, Rare Manifest at birth; usually fatal or stillborn 5. Wilm’s tumor (nephroblastoma) Most common tumor of children; usually unilateral Etiol = autosomal recessive (on chromosome 11) Manifests between age 2– 5 y & presents as abdominal mass May produce hypertension 5 year survival = 90%
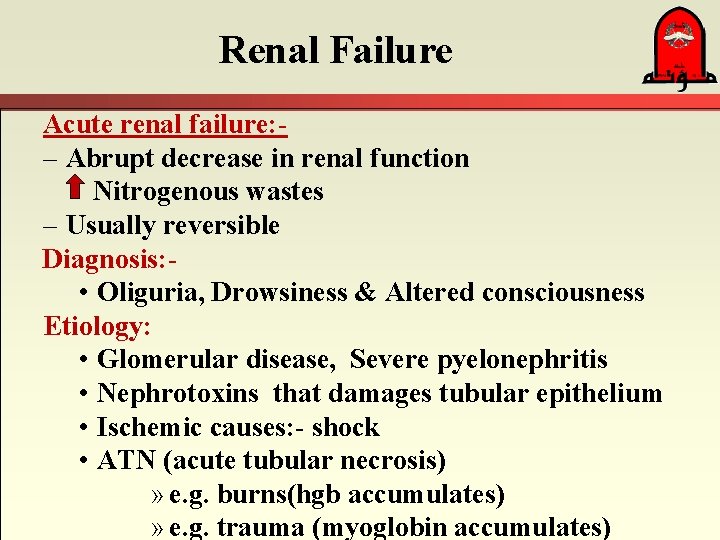
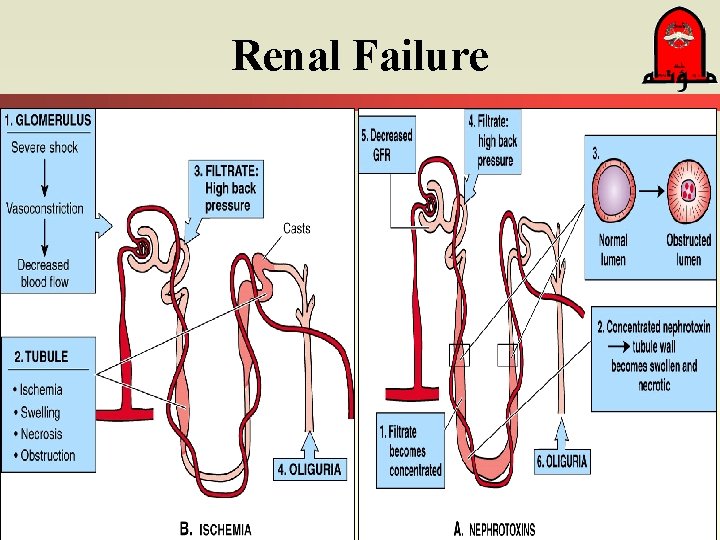
Renal Failure Acute renal failure: – Abrupt decrease in renal function Nitrogenous wastes – Usually reversible Diagnosis: • Oliguria, Drowsiness & Altered consciousness Etiology: • Glomerular disease, Severe pyelonephritis • Nephrotoxins that damages tubular epithelium • Ischemic causes: - shock • ATN (acute tubular necrosis) » e. g. burns(hgb accumulates) » e. g. trauma (myoglobin accumulates)
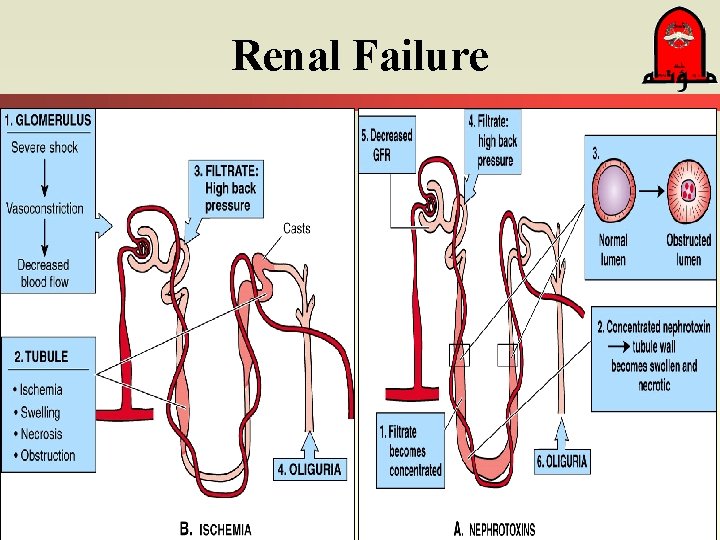
Renal Failure
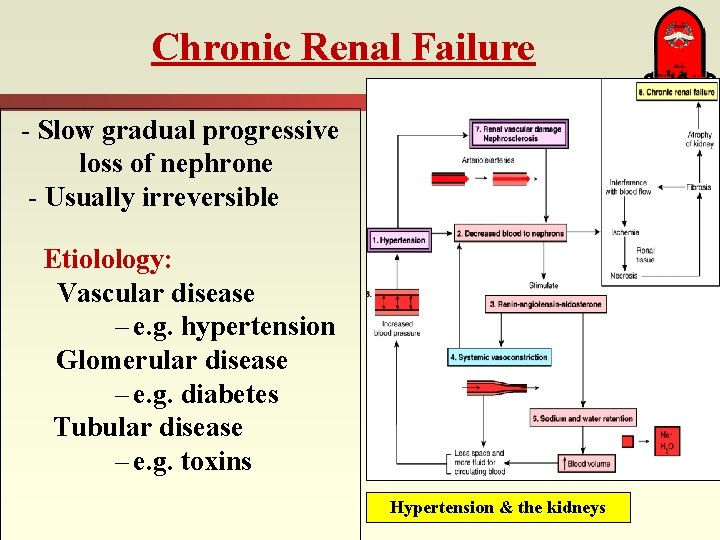
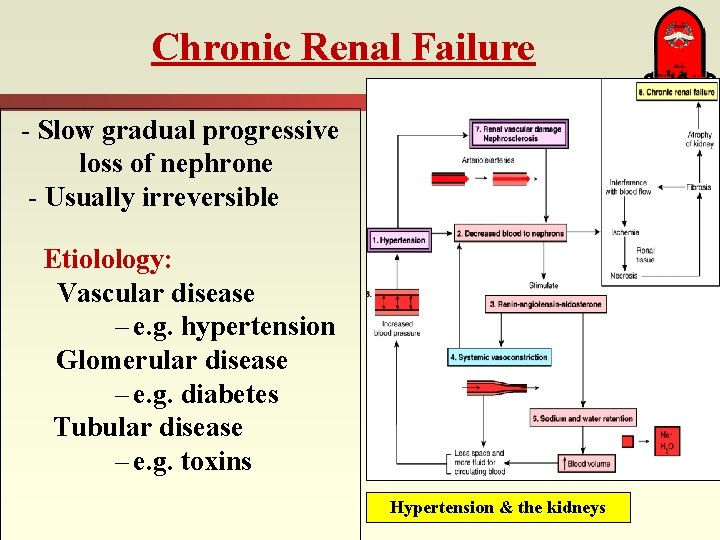
Chronic Renal Failure - Slow gradual progressive loss of nephrone - Usually irreversible Etiolology: Vascular disease – e. g. hypertension Glomerular disease – e. g. diabetes Tubular disease – e. g. toxins Hypertension & the kidneys
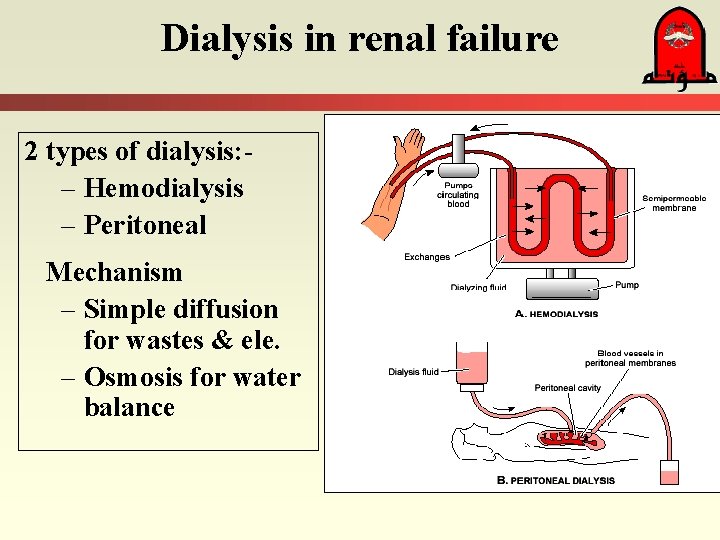
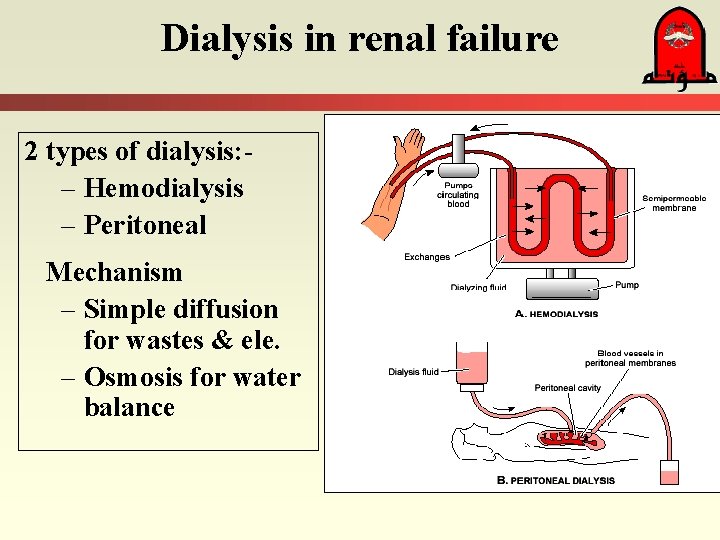
Dialysis in renal failure 2 types of dialysis: – Hemodialysis – Peritoneal Mechanism – Simple diffusion for wastes & ele. – Osmosis for water balance
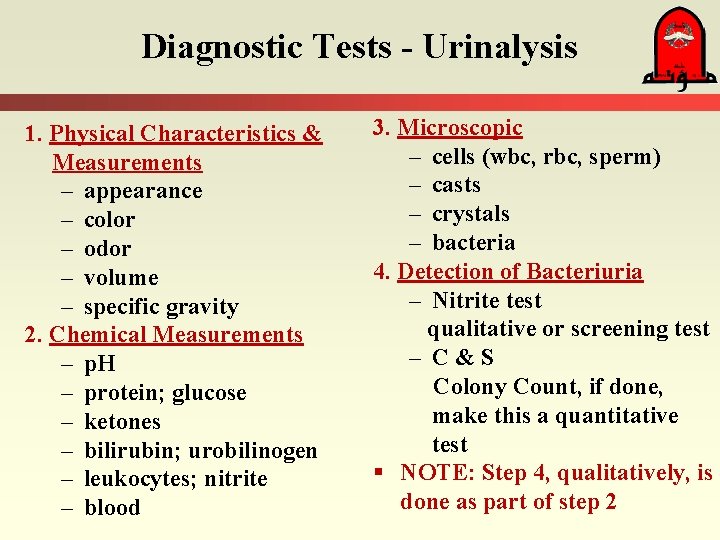
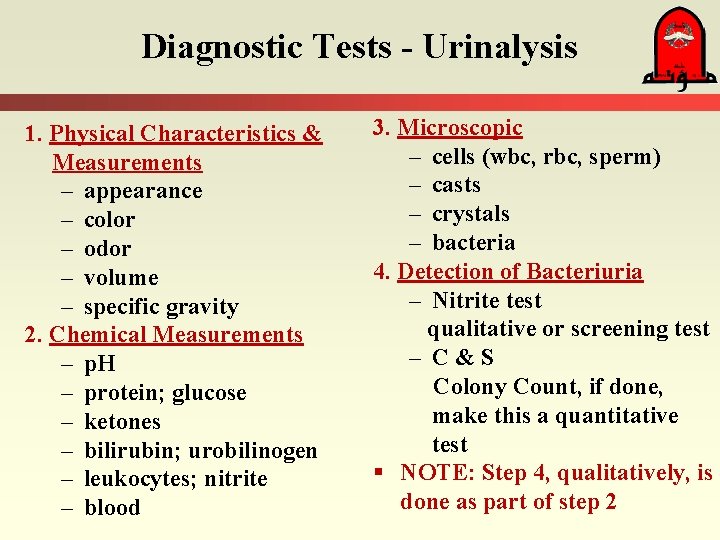
Diagnostic Tests - Urinalysis 1. Physical Characteristics & Measurements – appearance – color – odor – volume – specific gravity 2. Chemical Measurements – p. H – protein; glucose – ketones – bilirubin; urobilinogen – leukocytes; nitrite – blood 3. Microscopic – cells (wbc, rbc, sperm) – casts – crystals – bacteria 4. Detection of Bacteriuria – Nitrite test qualitative or screening test – C&S Colony Count, if done, make this a quantitative test § NOTE: Step 4, qualitatively, is done as part of step 2
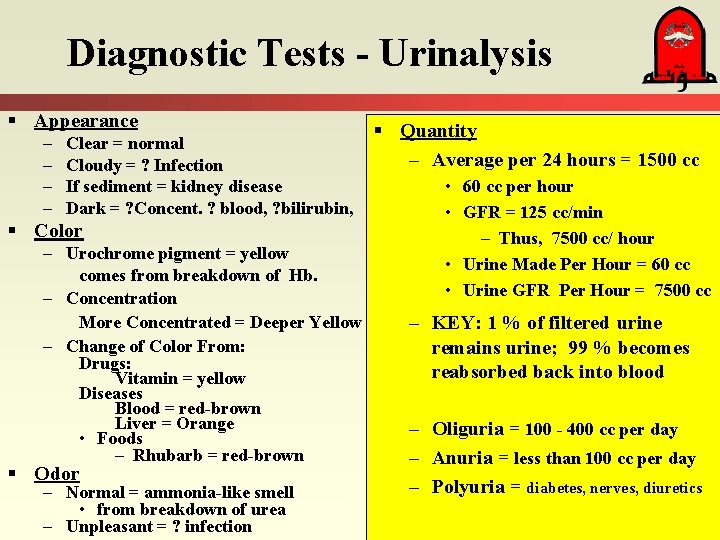
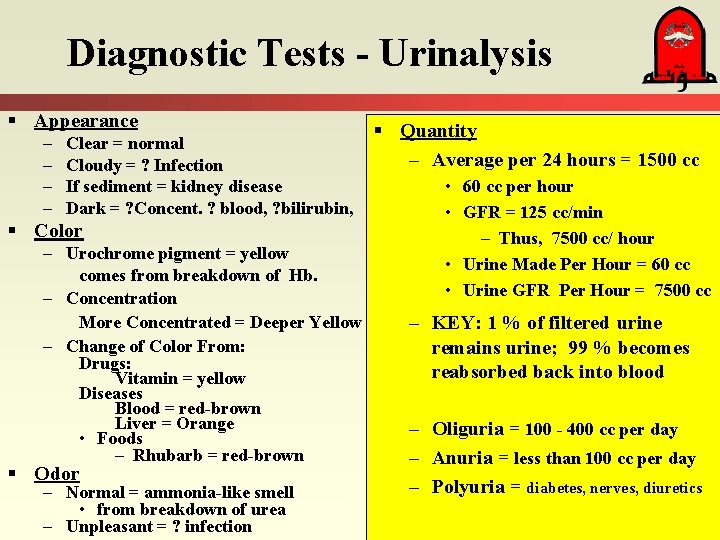
Diagnostic Tests - Urinalysis § Appearance – – Clear = normal Cloudy = ? Infection If sediment = kidney disease Dark = ? Concent. ? blood, ? bilirubin, § Color – Urochrome pigment = yellow comes from breakdown of Hb. – Concentration More Concentrated = Deeper Yellow – Change of Color From: Drugs: Vitamin = yellow Diseases Blood = red-brown Liver = Orange • Foods – Rhubarb = red-brown § Odor – Normal = ammonia-like smell • from breakdown of urea – Unpleasant = ? infection § Quantity – Average per 24 hours = 1500 cc • 60 cc per hour • GFR = 125 cc/min – Thus, 7500 cc/ hour • Urine Made Per Hour = 60 cc • Urine GFR Per Hour = 7500 cc – KEY: 1 % of filtered urine remains urine; 99 % becomes reabsorbed back into blood – Oliguria = 100 - 400 cc per day – Anuria = less than 100 cc per day – Polyuria = diabetes, nerves, diuretics
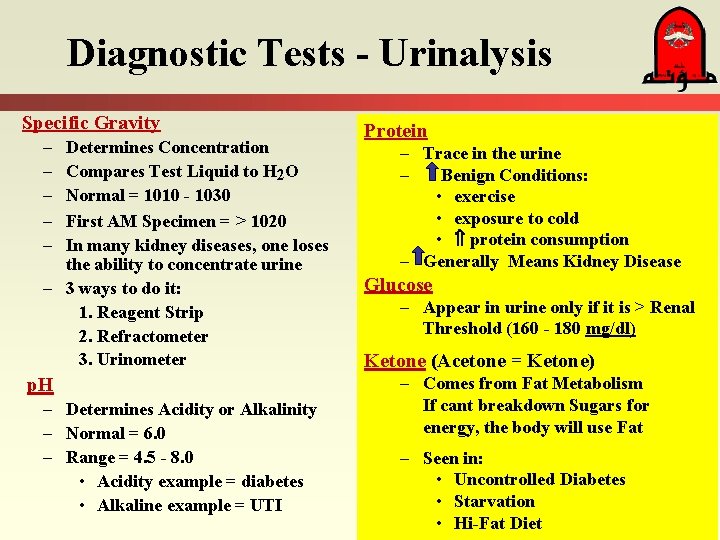
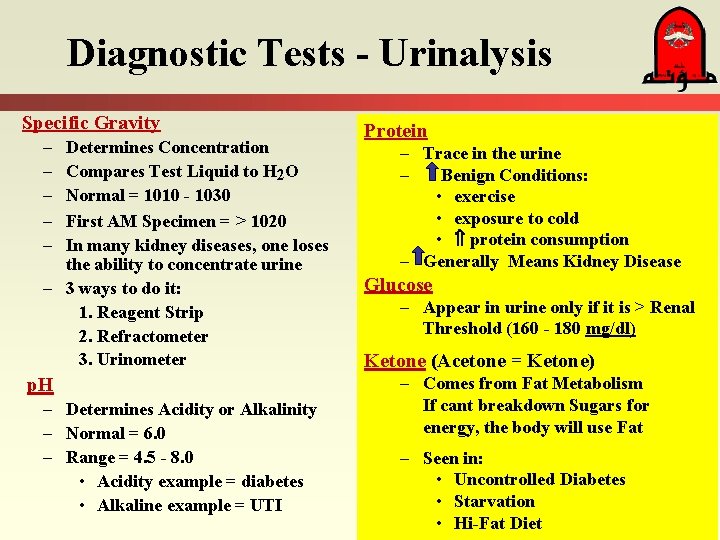
Diagnostic Tests - Urinalysis Specific Gravity – – – Determines Concentration Compares Test Liquid to H 2 O Normal = 1010 - 1030 First AM Specimen = > 1020 In many kidney diseases, one loses the ability to concentrate urine – 3 ways to do it: 1. Reagent Strip 2. Refractometer 3. Urinometer p. H – Determines Acidity or Alkalinity – Normal = 6. 0 – Range = 4. 5 - 8. 0 • Acidity example = diabetes • Alkaline example = UTI Protein – Trace in the urine – Benign Conditions: • exercise • exposure to cold • protein consumption – Generally Means Kidney Disease Glucose – Appear in urine only if it is > Renal Threshold (160 - 180 mg/dl) Ketone (Acetone = Ketone) – Comes from Fat Metabolism If cant breakdown Sugars for energy, the body will use Fat – Seen in: • Uncontrolled Diabetes • Starvation • Hi-Fat Diet
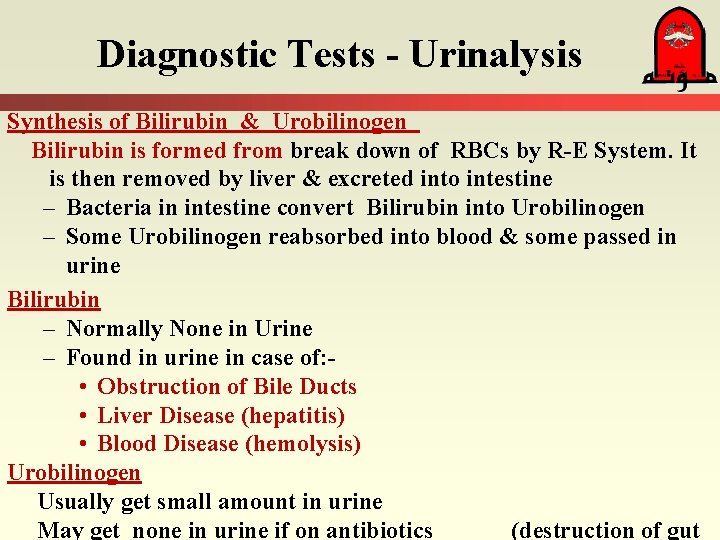
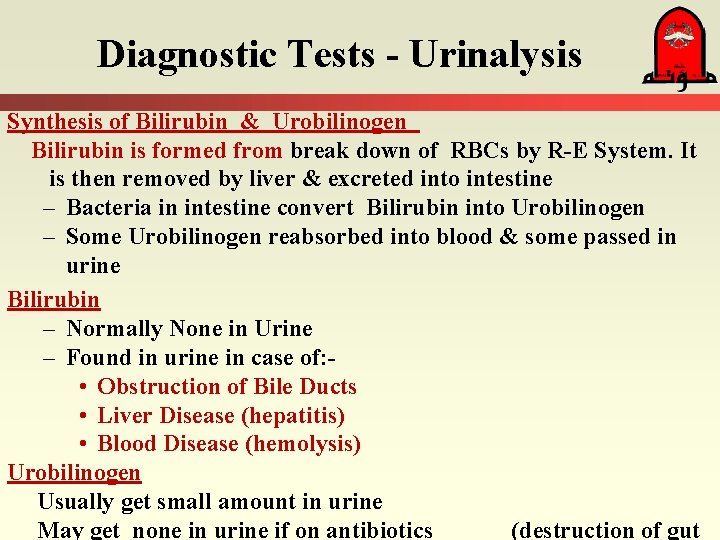
Diagnostic Tests - Urinalysis Synthesis of Bilirubin & Urobilinogen Bilirubin is formed from break down of RBCs by R-E System. It is then removed by liver & excreted into intestine – Bacteria in intestine convert Bilirubin into Urobilinogen – Some Urobilinogen reabsorbed into blood & some passed in urine Bilirubin – Normally None in Urine – Found in urine in case of: • Obstruction of Bile Ducts • Liver Disease (hepatitis) • Blood Disease (hemolysis) Urobilinogen Usually get small amount in urine May get none in urine if on antibiotics (destruction of gut
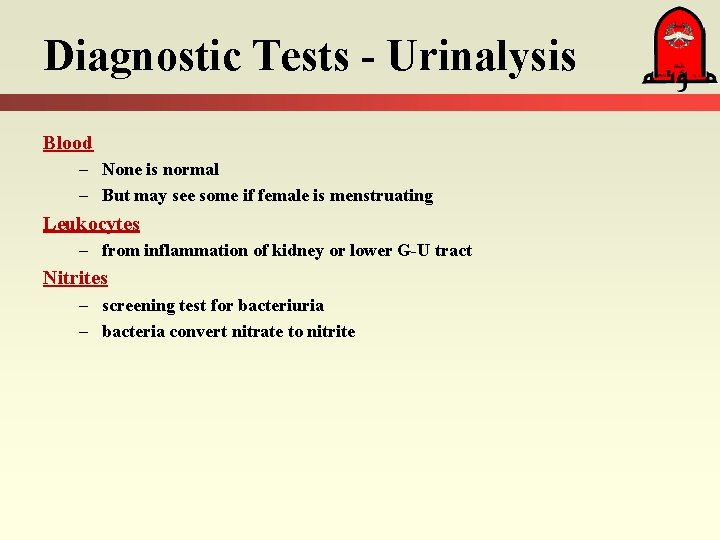
Diagnostic Tests - Urinalysis Blood – None is normal – But may see some if female is menstruating Leukocytes – from inflammation of kidney or lower G-U tract Nitrites – screening test for bacteriuria – bacteria convert nitrate to nitrite
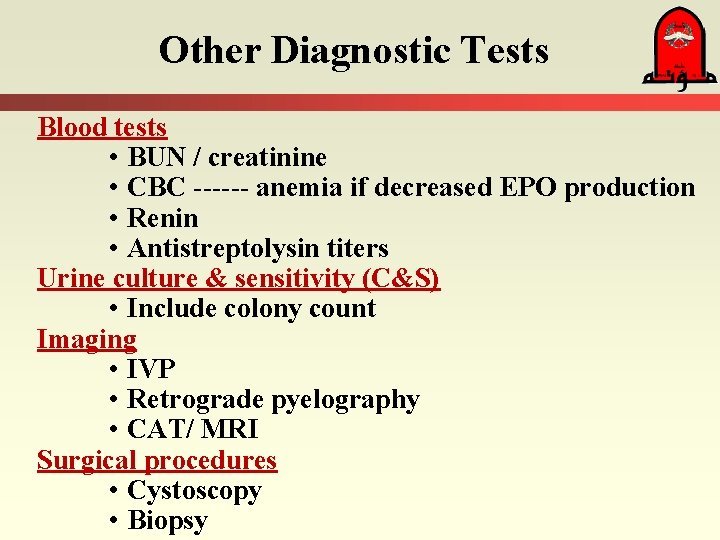
Other Diagnostic Tests Blood tests • BUN / creatinine • CBC ------ anemia if decreased EPO production • Renin • Antistreptolysin titers Urine culture & sensitivity (C&S) • Include colony count Imaging • IVP • Retrograde pyelography • CAT/ MRI Surgical procedures • Cystoscopy • Biopsy
 Urinary bladder
Urinary bladder Uti symptoms
Uti symptoms Pathophysiology of kidney stones
Pathophysiology of kidney stones What is this called
What is this called Urinary system
Urinary system Urinary bladder
Urinary bladder Red and white blood cells difference
Red and white blood cells difference Renal angle surface anatomy
Renal angle surface anatomy Figure 15-2 is a longitudinal section of a kidney
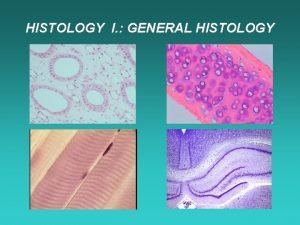
Figure 15-2 is a longitudinal section of a kidney What are the 4 types of tissues
What are the 4 types of tissues Anatomy histology slides
Anatomy histology slides Inferior view of sheep brain labeled
Inferior view of sheep brain labeled Pancreas histology slide
Pancreas histology slide Liver histology
Liver histology Introduction of urinary system
Introduction of urinary system Figure 15-3 the urinary system
Figure 15-3 the urinary system Pyel medical terminology
Pyel medical terminology Interesting facts about urinary system
Interesting facts about urinary system Fetal pig masseter muscle
Fetal pig masseter muscle Chapter 30 the urinary system workbook answers
Chapter 30 the urinary system workbook answers Chapter 15 the urinary system figure 15-3
Chapter 15 the urinary system figure 15-3 Chapter 20 urinary/excretory system
Chapter 20 urinary/excretory system Urinary system model
Urinary system model Urinary system model
Urinary system model Optic lobes
Optic lobes Urinary system powerpoint
Urinary system powerpoint The urinary system is also known as
The urinary system is also known as Adh hormone function
Adh hormone function Figure 15-4 is a diagram of a nephron
Figure 15-4 is a diagram of a nephron Urinary system x ray labeled
Urinary system x ray labeled Defination of urinary system
Defination of urinary system Urinary system label
Urinary system label Rat appendix
Rat appendix Rat urinary system
Rat urinary system Vena cava excretory system
Vena cava excretory system