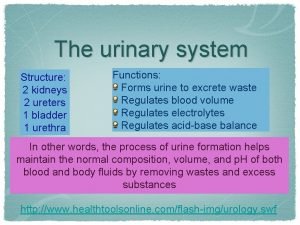
Urinary System Diseases Review of Urinary Anatomy Physiology






- Slides: 31
Urinary System Diseases

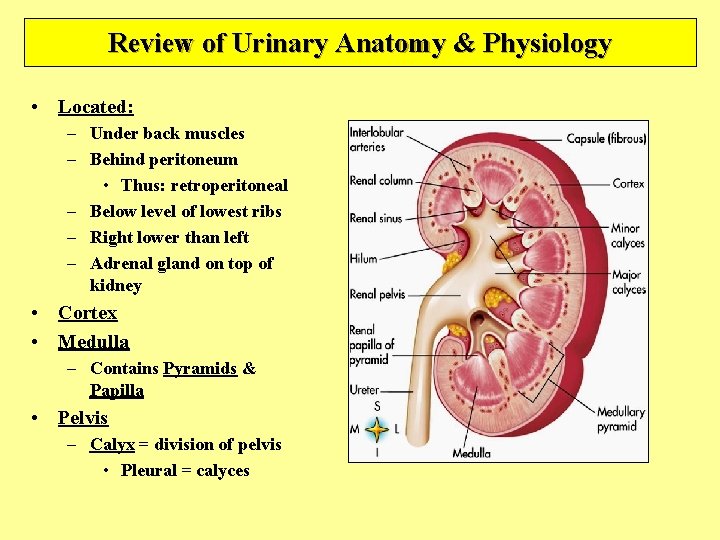
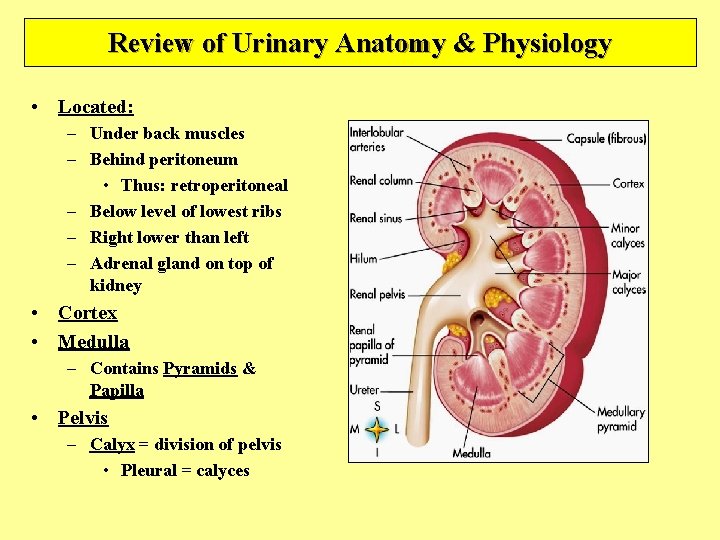
Review of Urinary Anatomy & Physiology • Located: – Under back muscles – Behind peritoneum • Thus: retroperitoneal – Below level of lowest ribs – Right lower than left – Adrenal gland on top of kidney • Cortex • Medulla – Contains Pyramids & Papilla • Pelvis – Calyx = division of pelvis • Pleural = calyces
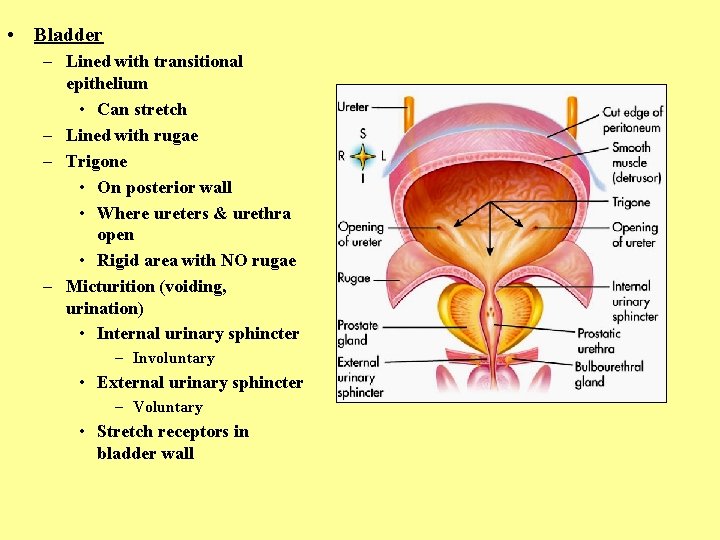
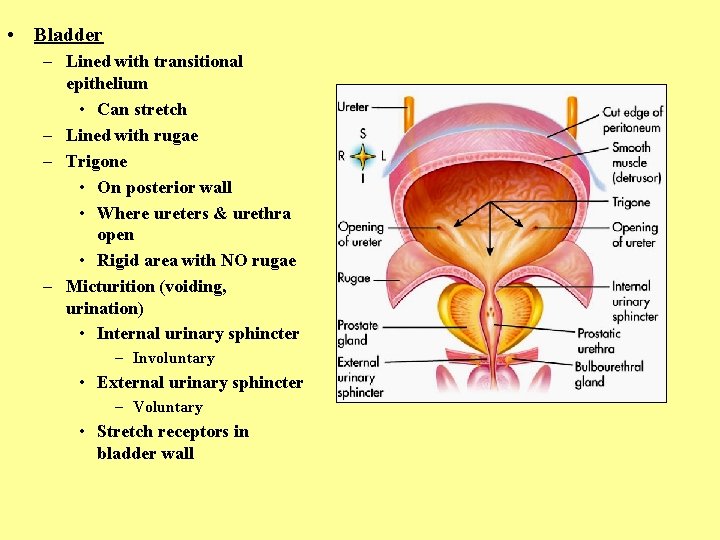
• Bladder – Lined with transitional epithelium • Can stretch – Lined with rugae – Trigone • On posterior wall • Where ureters & urethra open • Rigid area with NO rugae – Micturition (voiding, urination) • Internal urinary sphincter – Involuntary • External urinary sphincter – Voluntary • Stretch receptors in bladder wall
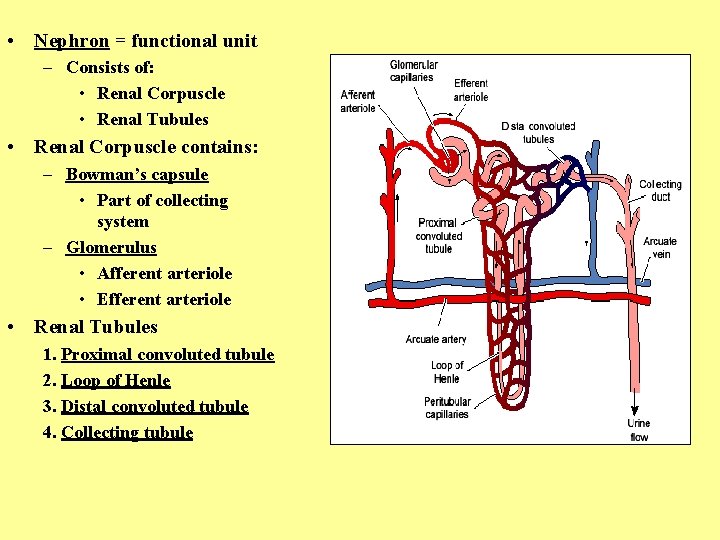
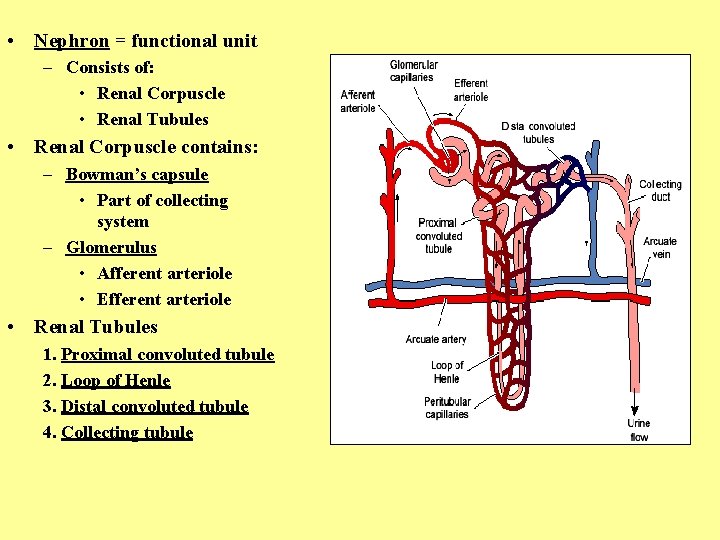
• Nephron = functional unit – Consists of: • Renal Corpuscle • Renal Tubules • Renal Corpuscle contains: – Bowman’s capsule • Part of collecting system – Glomerulus • Afferent arteriole • Efferent arteriole • Renal Tubules 1. Proximal convoluted tubule 2. Loop of Henle 3. Distal convoluted tubule 4. Collecting tubule
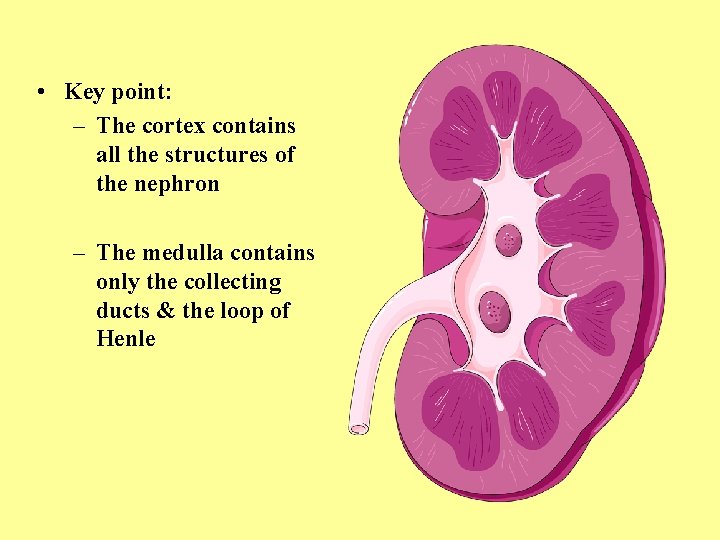
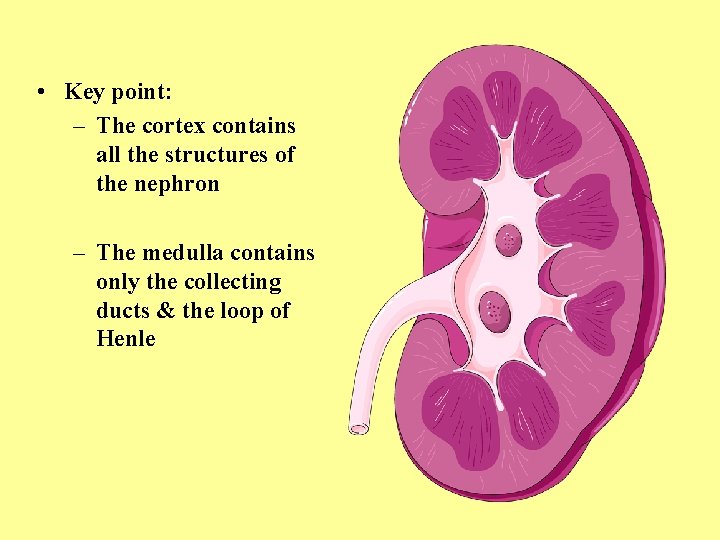
• Key point: – The cortex contains all the structures of the nephron – The medulla contains only the collecting ducts & the loop of Henle
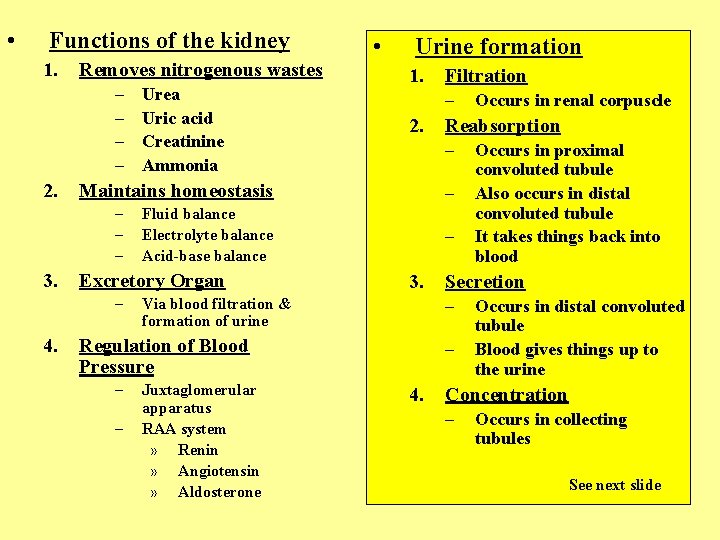
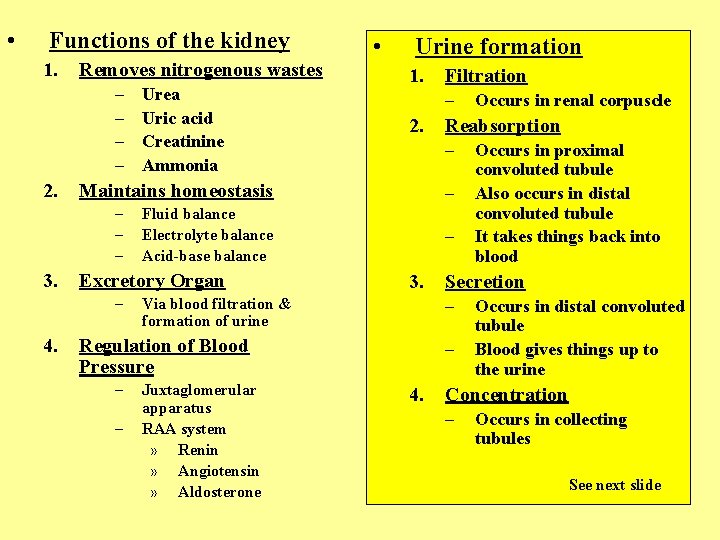
• Functions of the kidney 1. Removes nitrogenous wastes – – 2. 1. 2. – – 3. Via blood filtration & formation of urine – Juxtaglomerular apparatus RAA system » Renin » Angiotensin » Aldosterone Occurs in proximal convoluted tubule Also occurs in distal convoluted tubule It takes things back into blood Secretion – – 4. Occurs in renal corpuscle Reabsorption – Regulation of Blood Pressure – Filtration – Fluid balance Electrolyte balance Acid-base balance Excretory Organ – 4. Urine formation Maintains homeostasis – – – 3. Urea Uric acid Creatinine Ammonia • Occurs in distal convoluted tubule Blood gives things up to the urine Concentration – Occurs in collecting tubules See next slide

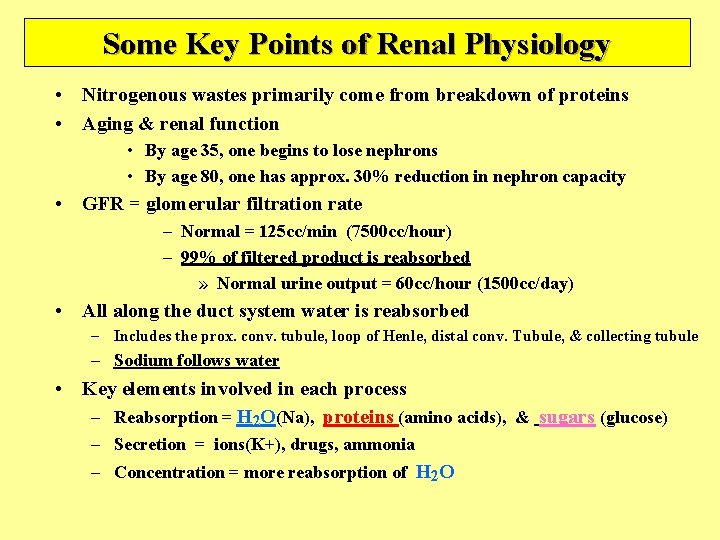
Some Key Points of Renal Physiology • Nitrogenous wastes primarily come from breakdown of proteins • Aging & renal function • By age 35, one begins to lose nephrons • By age 80, one has approx. 30% reduction in nephron capacity • GFR = glomerular filtration rate – Normal = 125 cc/min (7500 cc/hour) – 99% of filtered product is reabsorbed » Normal urine output = 60 cc/hour (1500 cc/day) • All along the duct system water is reabsorbed – Includes the prox. conv. tubule, loop of Henle, distal conv. Tubule, & collecting tubule – Sodium follows water • Key elements involved in each process – Reabsorption = H 2 O(Na), proteins (amino acids), & sugars (glucose) – Secretion = ions(K+), drugs, ammonia – Concentration = more reabsorption of H 2 O

• 2 key factors determine volume of urine produces 1. Glomerular filtration rate (GFR) – Determined by the unique arrangment of blood vessels 2. Hormonal secretion – Determined by fluid & electrolyte balance

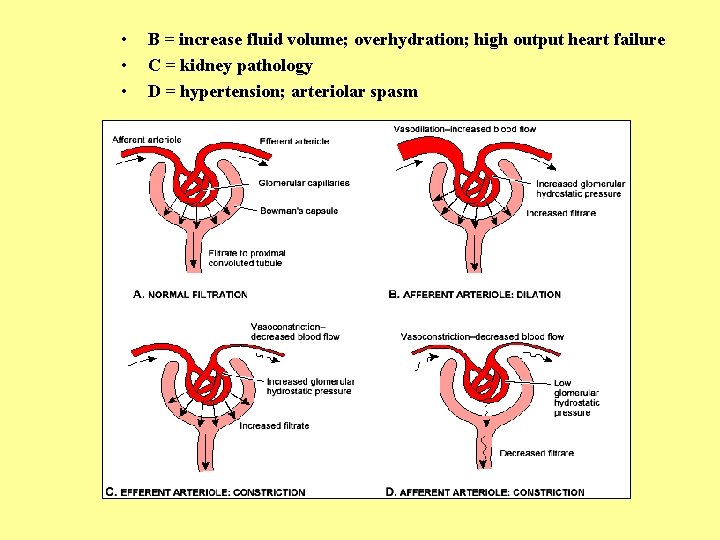
Volume of urine also controlled by glomerular filtration rate • • • Unique arrangment of blood vessels – Afferent arteriole -----to----capillary bed-----to----efferent arteriole -----to----capillary bed ----to---- veins • First capillary bed = glomerular capillaries • Second capillary bed = peritubular capillaries Purpose of this = to control the pressure in the glomerular capillaries & consequently the glomerular filtration pressure 3 factors control this: • (1) autoregulation • Local feedback from muscle tension in afferent arteriole • Local feedback from DCT at JGA • Mediated via endothelial secretions of glomerular capillaries • (2) sympathetic nervous system • (3) renin
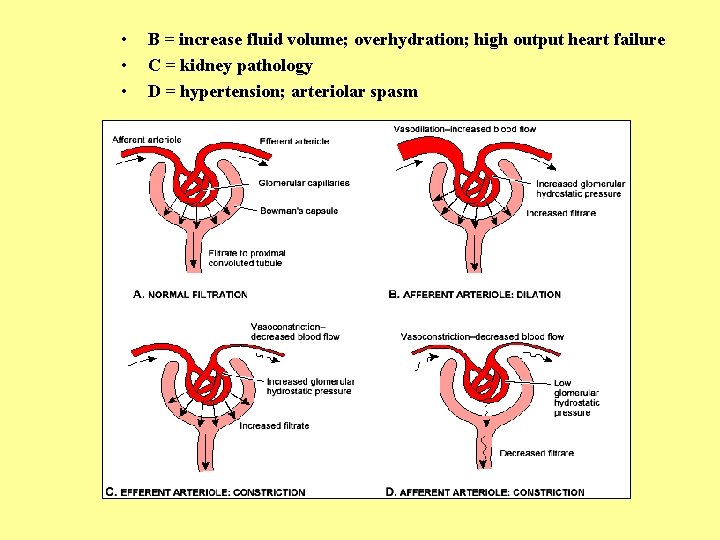
• • • B = increase fluid volume; overhydration; high output heart failure C = kidney pathology D = hypertension; arteriolar spasm
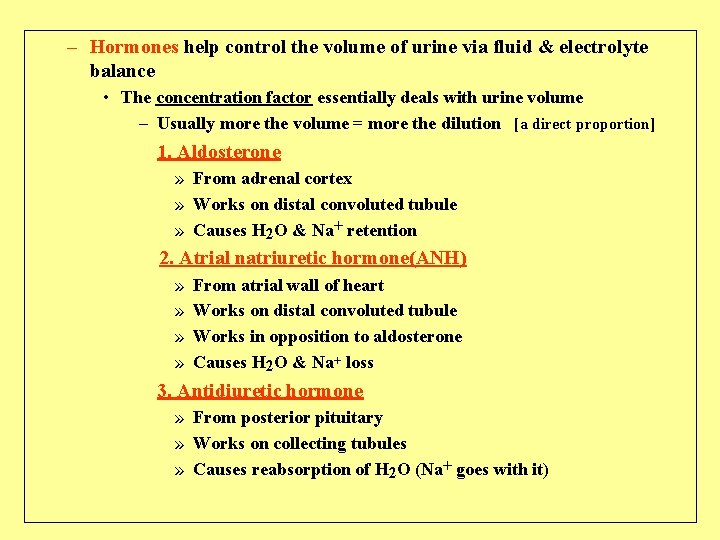
– Hormones help control the volume of urine via fluid & electrolyte balance • The concentration factor essentially deals with urine volume – Usually more the volume = more the dilution [a direct proportion] 1. Aldosterone » From adrenal cortex » Works on distal convoluted tubule » Causes H 2 O & Na+ retention 2. Atrial natriuretic hormone(ANH) » » From atrial wall of heart Works on distal convoluted tubule Works in opposition to aldosterone Causes H 2 O & Na+ loss 3. Antidiuretic hormone » From posterior pituitary » Works on collecting tubules » Causes reabsorption of H 2 O (Na+ goes with it)
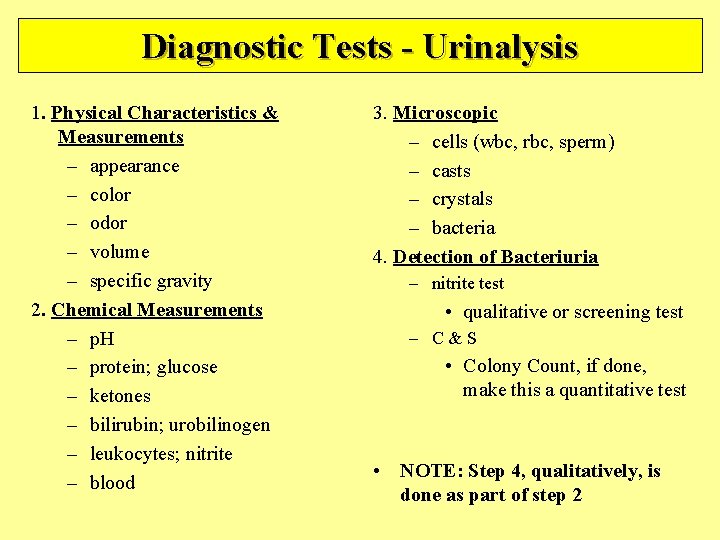
Diagnostic Tests - Urinalysis 1. Physical Characteristics & Measurements – appearance – color – odor – volume – specific gravity 2. Chemical Measurements – p. H – protein; glucose – ketones – bilirubin; urobilinogen – leukocytes; nitrite – blood 3. Microscopic – cells (wbc, rbc, sperm) – casts – crystals – bacteria 4. Detection of Bacteriuria – nitrite test • qualitative or screening test – C&S • Colony Count, if done, make this a quantitative test • NOTE: Step 4, qualitatively, is done as part of step 2
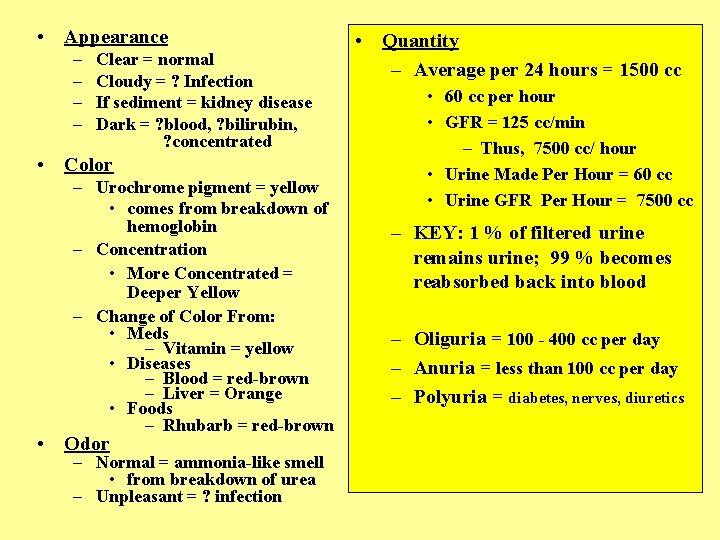
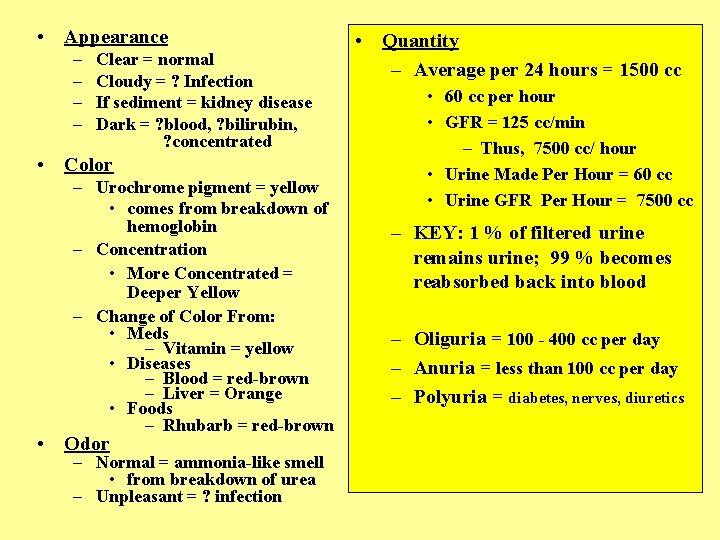
• Appearance – – Clear = normal Cloudy = ? Infection If sediment = kidney disease Dark = ? blood, ? bilirubin, ? concentrated • Color – Urochrome pigment = yellow • comes from breakdown of hemoglobin – Concentration • More Concentrated = Deeper Yellow – Change of Color From: • Meds – Vitamin = yellow • Diseases – Blood = red-brown – Liver = Orange • Foods – Rhubarb = red-brown • Odor – Normal = ammonia-like smell • from breakdown of urea – Unpleasant = ? infection • Quantity – Average per 24 hours = 1500 cc • 60 cc per hour • GFR = 125 cc/min – Thus, 7500 cc/ hour • Urine Made Per Hour = 60 cc • Urine GFR Per Hour = 7500 cc – KEY: 1 % of filtered urine remains urine; 99 % becomes reabsorbed back into blood – Oliguria = 100 - 400 cc per day – Anuria = less than 100 cc per day – Polyuria = diabetes, nerves, diuretics
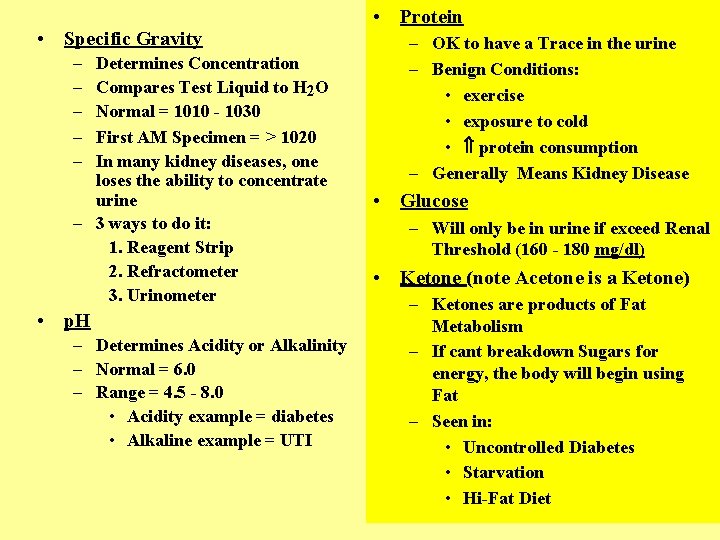
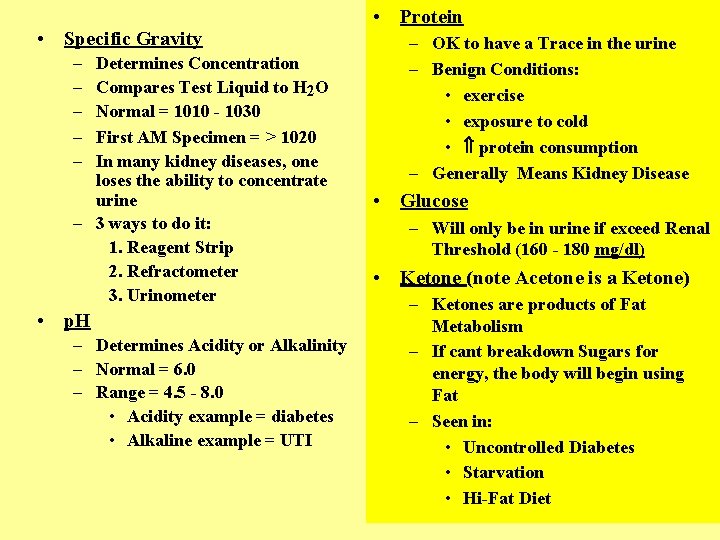
• Specific Gravity – – – Determines Concentration Compares Test Liquid to H 2 O Normal = 1010 - 1030 First AM Specimen = > 1020 In many kidney diseases, one loses the ability to concentrate urine – 3 ways to do it: 1. Reagent Strip 2. Refractometer 3. Urinometer • p. H – Determines Acidity or Alkalinity – Normal = 6. 0 – Range = 4. 5 - 8. 0 • Acidity example = diabetes • Alkaline example = UTI • Protein – OK to have a Trace in the urine – Benign Conditions: • exercise • exposure to cold • protein consumption – Generally Means Kidney Disease • Glucose – Will only be in urine if exceed Renal Threshold (160 - 180 mg/dl) • Ketone (note Acetone is a Ketone) – Ketones are products of Fat Metabolism – If cant breakdown Sugars for energy, the body will begin using Fat – Seen in: • Uncontrolled Diabetes • Starvation • Hi-Fat Diet
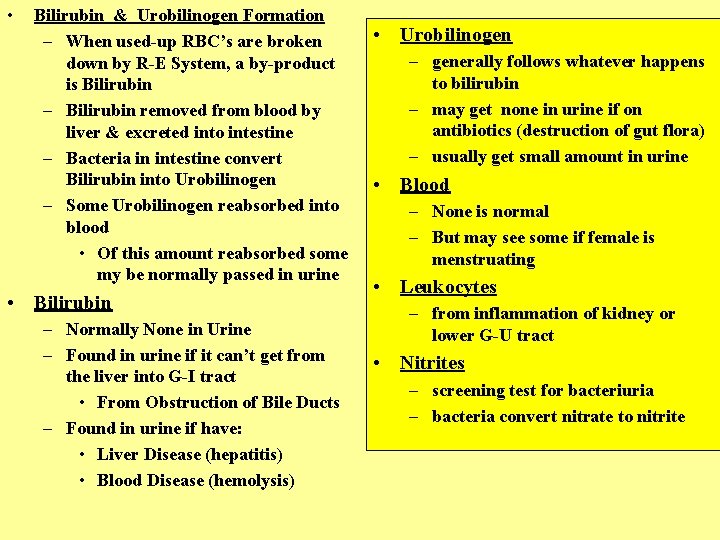
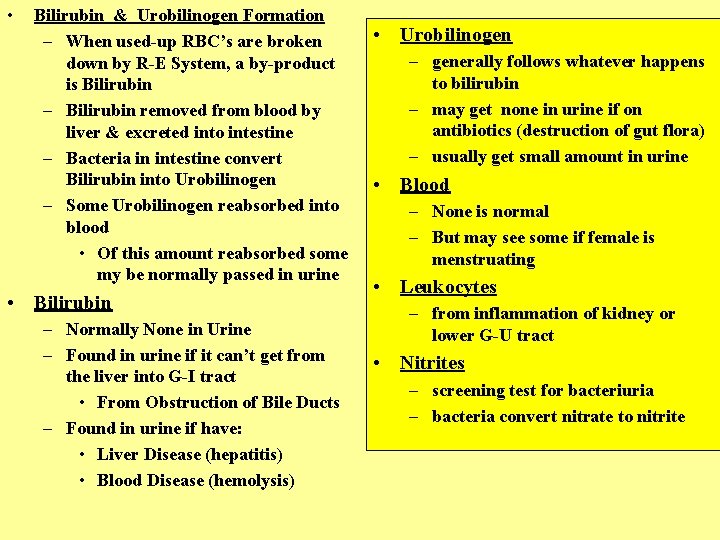
• Bilirubin & Urobilinogen Formation – When used-up RBC’s are broken down by R-E System, a by-product is Bilirubin – Bilirubin removed from blood by liver & excreted into intestine – Bacteria in intestine convert Bilirubin into Urobilinogen – Some Urobilinogen reabsorbed into blood • Of this amount reabsorbed some my be normally passed in urine • Bilirubin – Normally None in Urine – Found in urine if it can’t get from the liver into G-I tract • From Obstruction of Bile Ducts – Found in urine if have: • Liver Disease (hepatitis) • Blood Disease (hemolysis) • Urobilinogen – generally follows whatever happens to bilirubin – may get none in urine if on antibiotics (destruction of gut flora) – usually get small amount in urine • Blood – None is normal – But may see some if female is menstruating • Leukocytes – from inflammation of kidney or lower G-U tract • Nitrites – screening test for bacteriuria – bacteria convert nitrate to nitrite
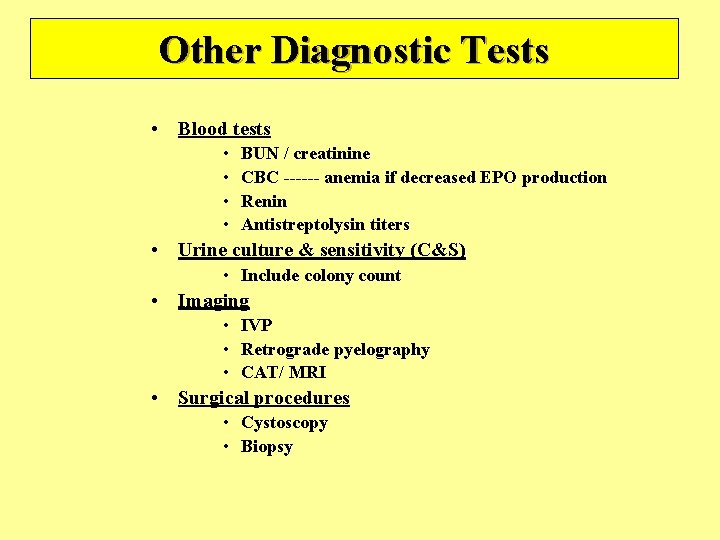
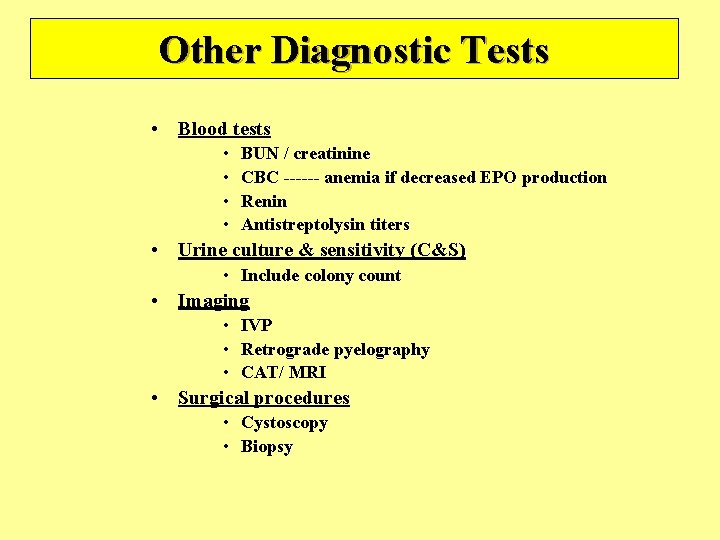
Other Diagnostic Tests • Blood tests • • BUN / creatinine CBC ------ anemia if decreased EPO production Renin Antistreptolysin titers • Urine culture & sensitivity (C&S) • Include colony count • Imaging • IVP • Retrograde pyelography • CAT/ MRI • Surgical procedures • Cystoscopy • Biopsy
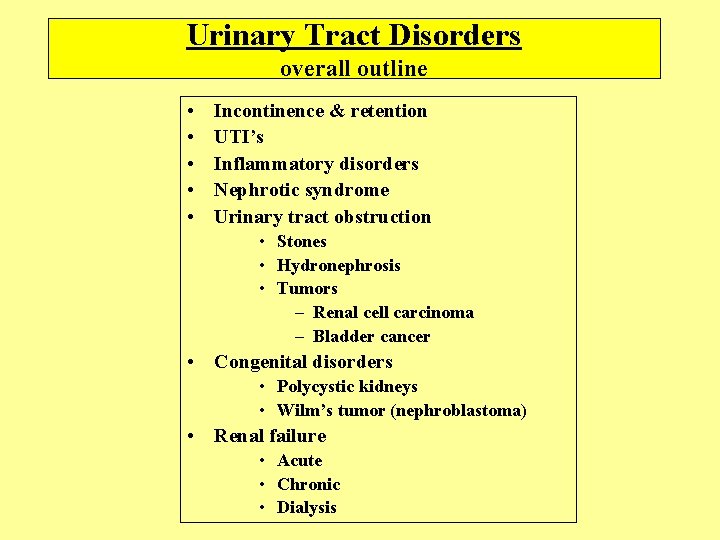
Urinary Tract Disorders overall outline • • • Incontinence & retention UTI’s Inflammatory disorders Nephrotic syndrome Urinary tract obstruction • Stones • Hydronephrosis • Tumors – Renal cell carcinoma – Bladder cancer • Congenital disorders • Polycystic kidneys • Wilm’s tumor (nephroblastoma) • Renal failure • Acute • Chronic • Dialysis
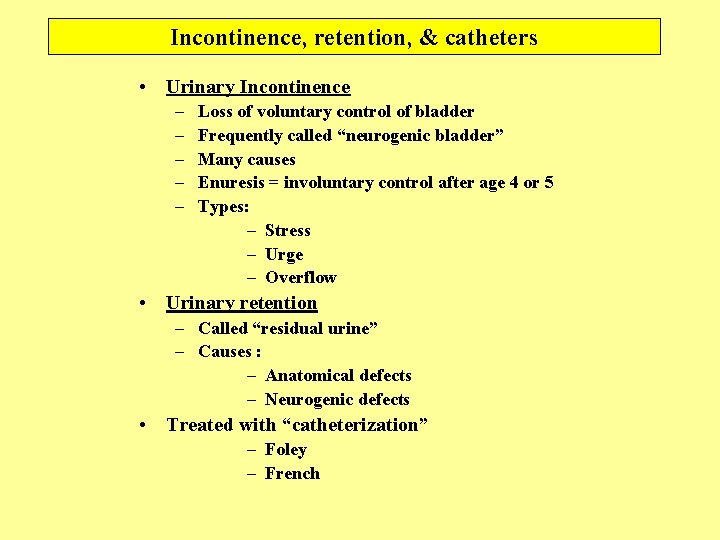
Incontinence, retention, & catheters • Urinary Incontinence – – – Loss of voluntary control of bladder Frequently called “neurogenic bladder” Many causes Enuresis = involuntary control after age 4 or 5 Types: – Stress – Urge – Overflow • Urinary retention – Called “residual urine” – Causes : – Anatomical defects – Neurogenic defects • Treated with “catheterization” – Foley – French
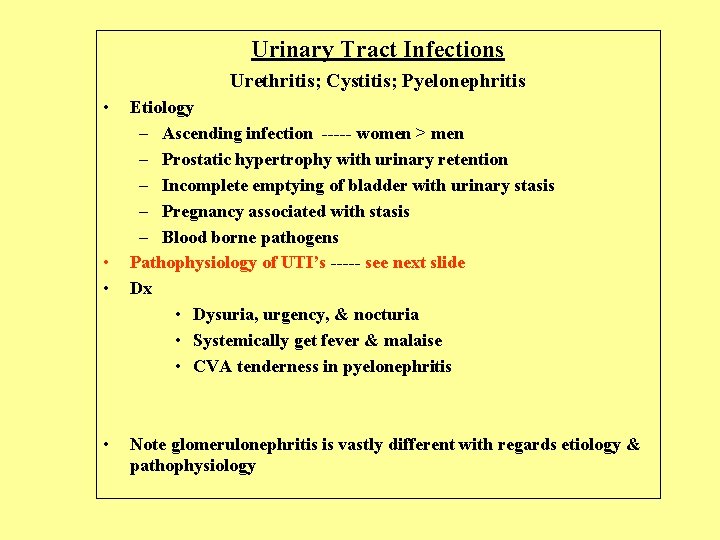
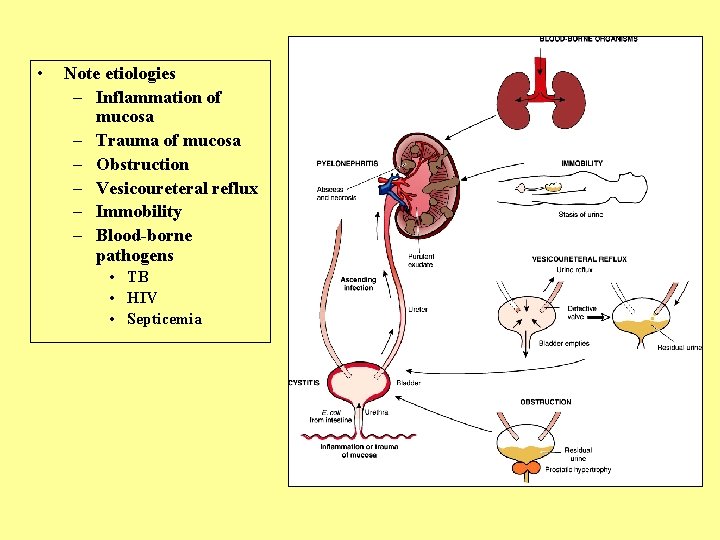
Urinary Tract Infections Urethritis; Cystitis; Pyelonephritis • • Etiology – Ascending infection ----- women > men – Prostatic hypertrophy with urinary retention – Incomplete emptying of bladder with urinary stasis – Pregnancy associated with stasis – Blood borne pathogens Pathophysiology of UTI’s ----- see next slide Dx • Dysuria, urgency, & nocturia • Systemically get fever & malaise • CVA tenderness in pyelonephritis Note glomerulonephritis is vastly different with regards etiology & pathophysiology
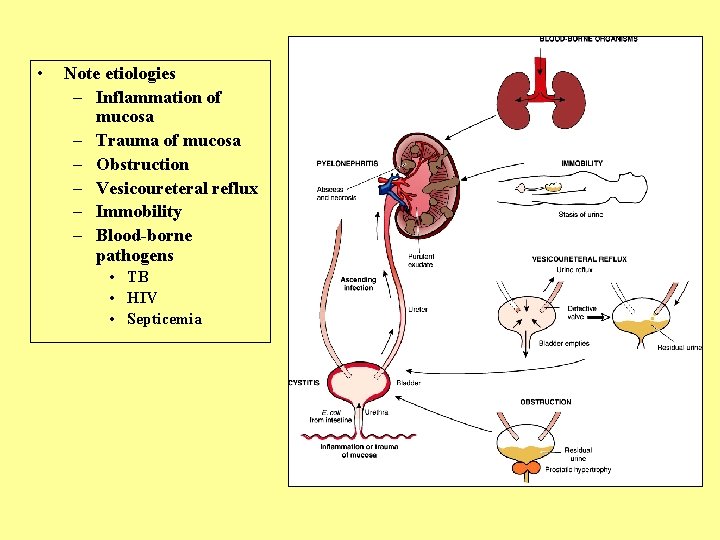
• Note etiologies – Inflammation of mucosa – Trauma of mucosa – Obstruction – Vesicoureteral reflux – Immobility – Blood-borne pathogens • TB • HIV • Septicemia
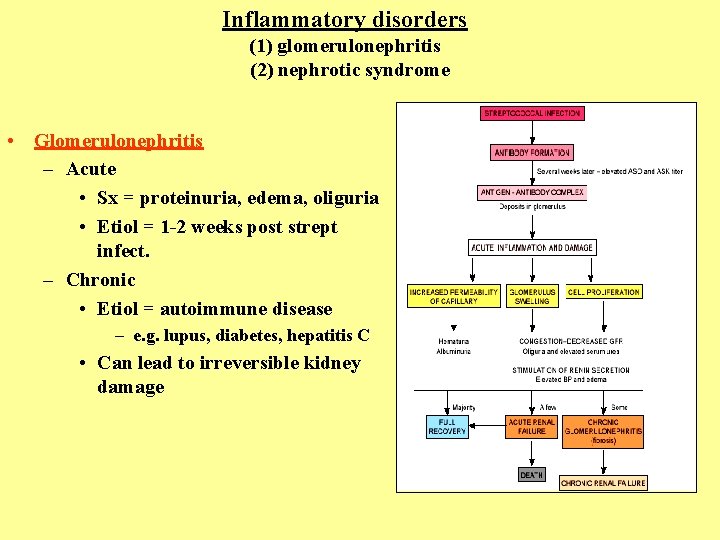
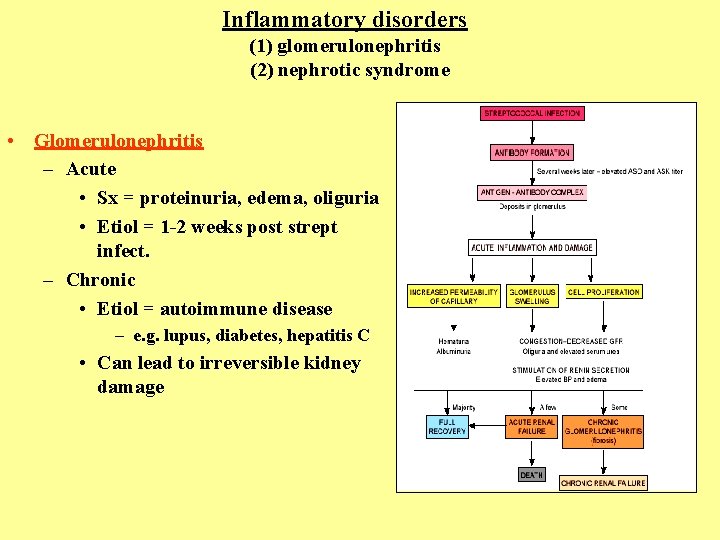
Inflammatory disorders (1) glomerulonephritis (2) nephrotic syndrome • Glomerulonephritis – Acute • Sx = proteinuria, edema, oliguria • Etiol = 1 -2 weeks post strept infect. – Chronic • Etiol = autoimmune disease – e. g. lupus, diabetes, hepatitis C • Can lead to irreversible kidney damage
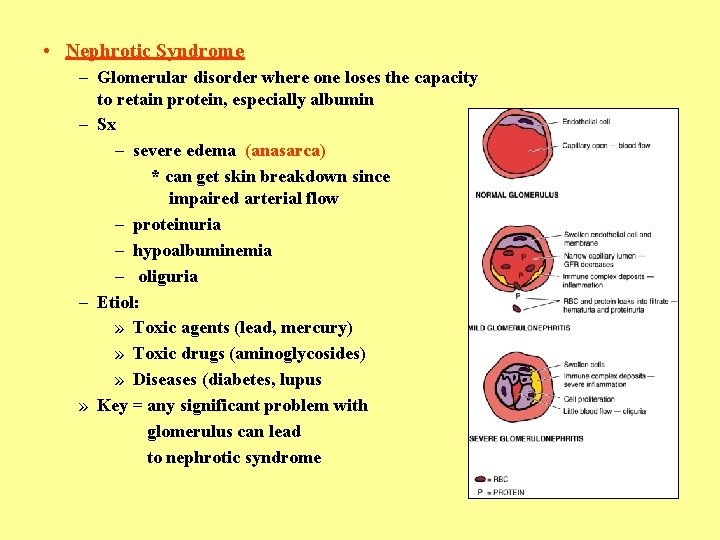
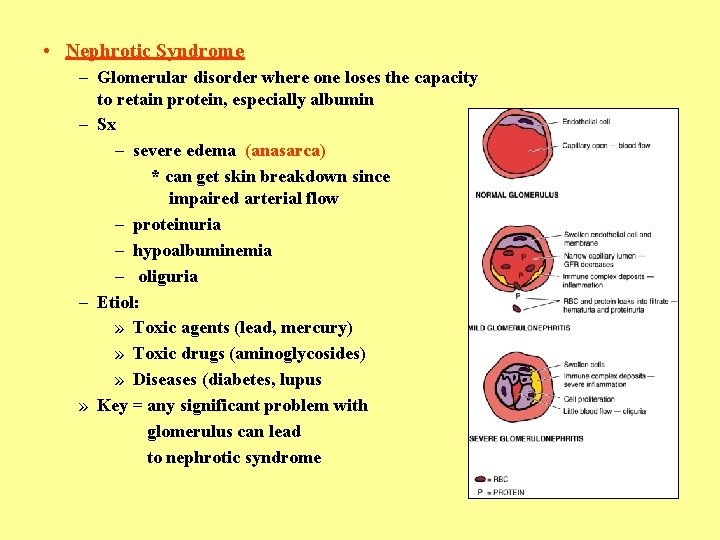
• Nephrotic Syndrome – Glomerular disorder where one loses the capacity to retain protein, especially albumin – Sx – severe edema (anasarca) * can get skin breakdown since impaired arterial flow – proteinuria – hypoalbuminemia – oliguria – Etiol: » Toxic agents (lead, mercury) » Toxic drugs (aminoglycosides) » Diseases (diabetes, lupus » Key = any significant problem with glomerulus can lead to nephrotic syndrome
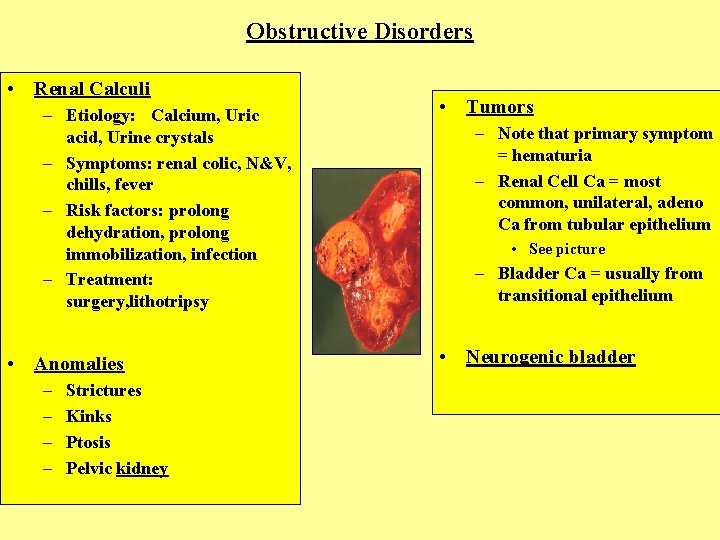
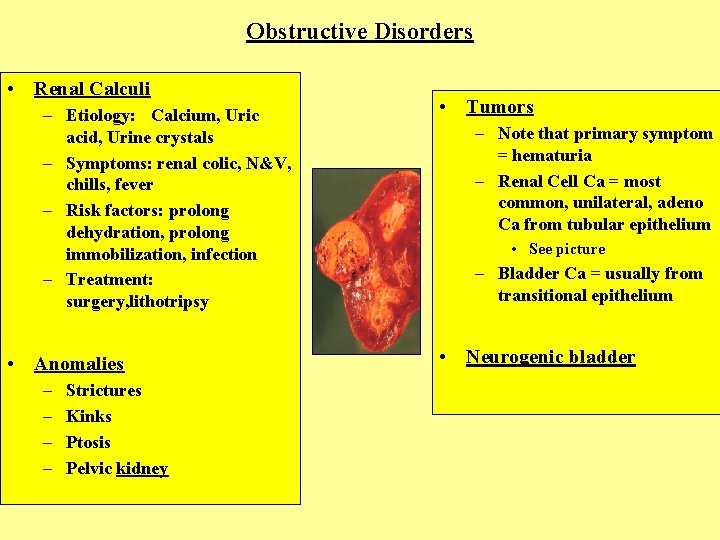
Obstructive Disorders • Renal Calculi – Etiology: Calcium, Uric acid, Urine crystals – Symptoms: renal colic, N&V, chills, fever – Risk factors: prolong dehydration, prolong immobilization, infection – Treatment: surgery, lithotripsy • Anomalies – – Strictures Kinks Ptosis Pelvic kidney • Tumors – Note that primary symptom = hematuria – Renal Cell Ca = most common, unilateral, adeno Ca from tubular epithelium • See picture – Bladder Ca = usually from transitional epithelium • Neurogenic bladder
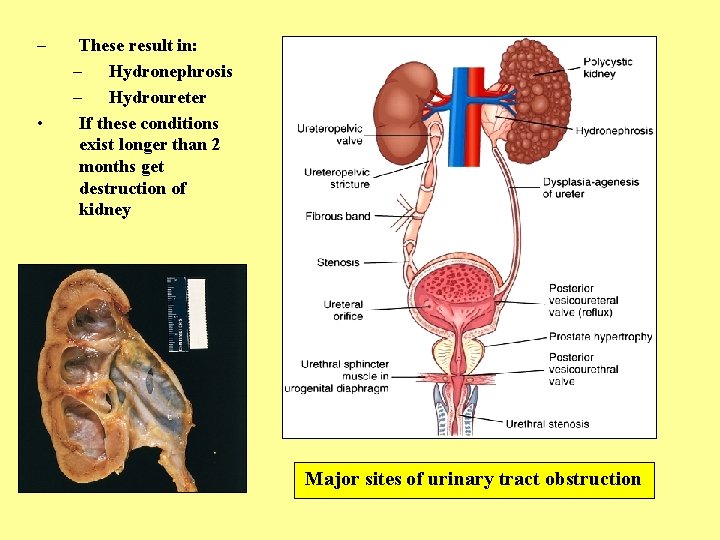
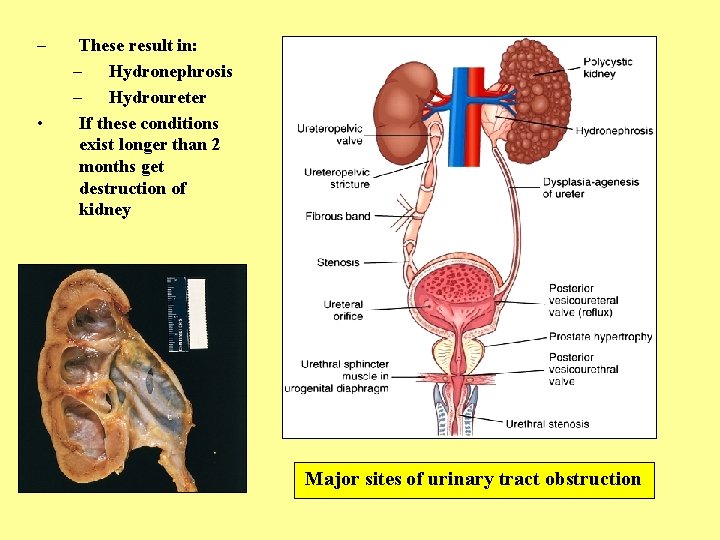
– • These result in: – Hydronephrosis – Hydroureter If these conditions exist longer than 2 months get destruction of kidney Major sites of urinary tract obstruction
Congenital Diseases • Vesicoureteral reflux • Due to ectopic insertion of ureter into bladder. If far away from trigone, do not get adequate compression of ureter when voiding & get reflux • Incidence: 1/1000 • If one gets it each sibling(to be) has 50% incidence • Girls> boys; 10: 1 ratio • Ectopic kidney • May get kinking of ureter • Usually in pelvis • Asymptomatic • Renal agenesis • • Usually unilateral & left kidney 2 types: (1) occurs randomly (2) genetic Asymptomatic Remaining kidney becomes large since compensatory hypertrophy
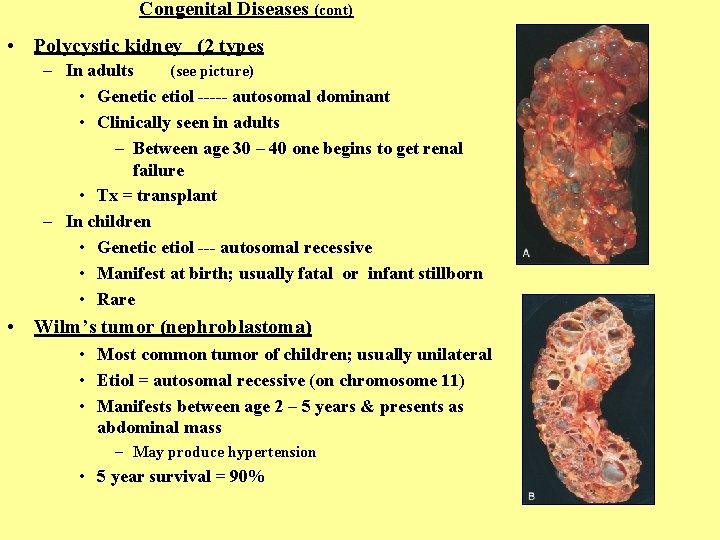
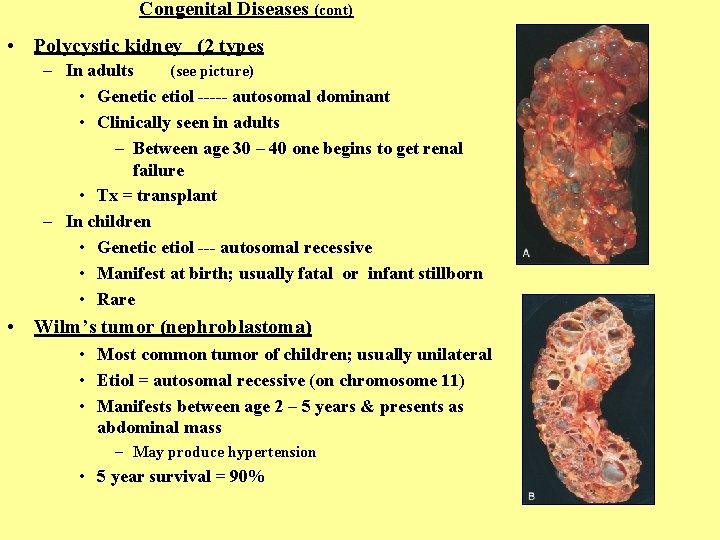
Congenital Diseases (cont) • Polycystic kidney (2 types – In adults (see picture) • Genetic etiol ----- autosomal dominant • Clinically seen in adults – Between age 30 – 40 one begins to get renal failure • Tx = transplant – In children • Genetic etiol --- autosomal recessive • Manifest at birth; usually fatal or infant stillborn • Rare • Wilm’s tumor (nephroblastoma) • Most common tumor of children; usually unilateral • Etiol = autosomal recessive (on chromosome 11) • Manifests between age 2 – 5 years & presents as abdominal mass – May produce hypertension • 5 year survival = 90%

Renal Failure • Acute renal failure – Abrupt decrease in renal function • Nitrogenous wastes accumulate – Usually reversible – Sx: • Oliguria • Drowsiness • Altered levels of consciousness – Etiol: • Glomerular disease • Severe pyelonephritis • Nephrotoxins that damages tubular epithelium • Ischemic causes – shock • ATN (acute tubular necrosis) » e. g. burns(hgb accumulates) » e. g. trauma (myoglobin accumulates)

• Chronic Renal Failure – Get slow progressive loss of neurons – Usually irreversible – Course = gradual – Etiol: • Vascular disease – e. g. hypertension – Disease called nephrosclerosis • Glomerular disease – e. g. diabetes • Tubular disease – e. g. toxins Hypertension & the kidneys
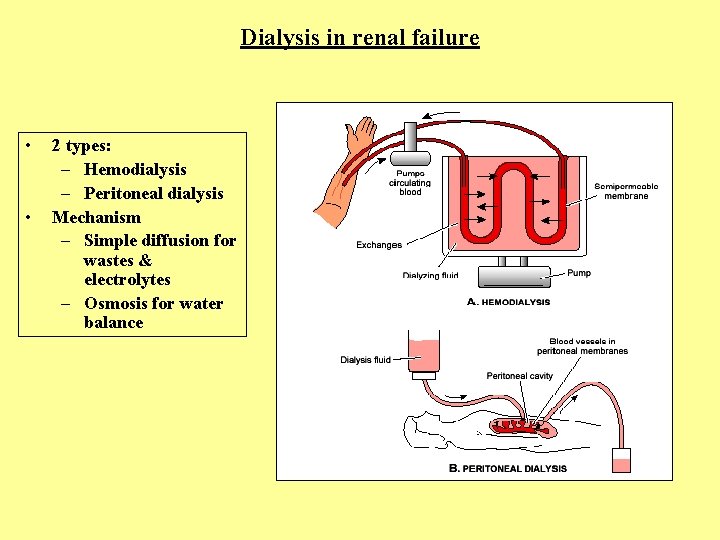
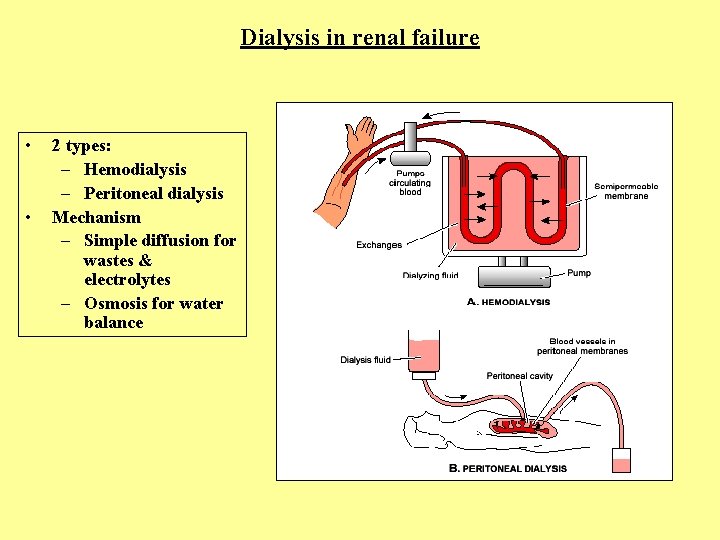
Dialysis in renal failure • • 2 types: – Hemodialysis – Peritoneal dialysis Mechanism – Simple diffusion for wastes & electrolytes – Osmosis for water balance
 What is the name
What is the name Urinary system
Urinary system Anatomy and physiology unit 7 cardiovascular system
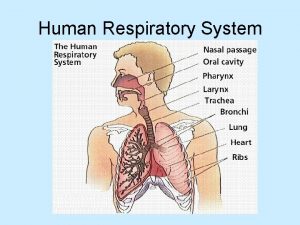
Anatomy and physiology unit 7 cardiovascular system Respiratory system
Respiratory system Male vs female skeleton pelvis
Male vs female skeleton pelvis Bronchial tree
Bronchial tree Chapter 8 skin disorders and diseases
Chapter 8 skin disorders and diseases 10 nail diseases and disorders
10 nail diseases and disorders Urethra
Urethra Red and white blood cells difference
Red and white blood cells difference Upper respiratory tract
Upper respiratory tract Tattoo anatomy and physiology
Tattoo anatomy and physiology International anatomy olympiad
International anatomy olympiad Crown plants examples
Crown plants examples Bone metabolism
Bone metabolism Anatomy of peptic ulcer
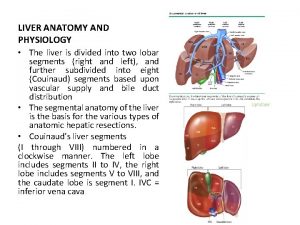
Anatomy of peptic ulcer Sheep liver lobes
Sheep liver lobes Podbřišek
Podbřišek Hypogastric region
Hypogastric region Straw colored fluid
Straw colored fluid The central sulcus divides which two lobes? (figure 14-13)
The central sulcus divides which two lobes? (figure 14-13) Human anatomy and physiology seventh edition marieb
Human anatomy and physiology seventh edition marieb Http://anatomy and physiology
Http://anatomy and physiology Chapter 1 introduction to human anatomy and physiology
Chapter 1 introduction to human anatomy and physiology Anatomy and physiology of appendicitis
Anatomy and physiology of appendicitis Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 2
Aohs foundations of anatomy and physiology 2 Anatomical planes
Anatomical planes Anatomy and physiology chapter 8 special senses
Anatomy and physiology chapter 8 special senses Chapter 13 anatomy and physiology of pregnancy
Chapter 13 anatomy and physiology of pregnancy Agriscience unit 26 self evaluation answers
Agriscience unit 26 self evaluation answers Science olympiad forensics cheat sheet
Science olympiad forensics cheat sheet