Anatomy Physiology Urinary Reproductive System Unit X Urinary
- Slides: 40
Anatomy & Physiology Urinary & Reproductive System Unit X
Urinary Terms • Renal – kidney • Nephrology – study of kidney function • Urology – study of urinary system
Kidneys (located on posterior wall) Structures: -Renal cortex – outer region • Projects to inner region as renal columns that separate the renal pyramids - Renal medulla – inner region • Forms renal pyramids Calyces – cuplike units -Renal pelvis • Collects urine made • Upper end of the ureters
Kidney Functions • Excrete waste • Regulate blood volume • Regulate electrolytes • Regulate acid- base balance • Regulate BP • Regulate RBC production
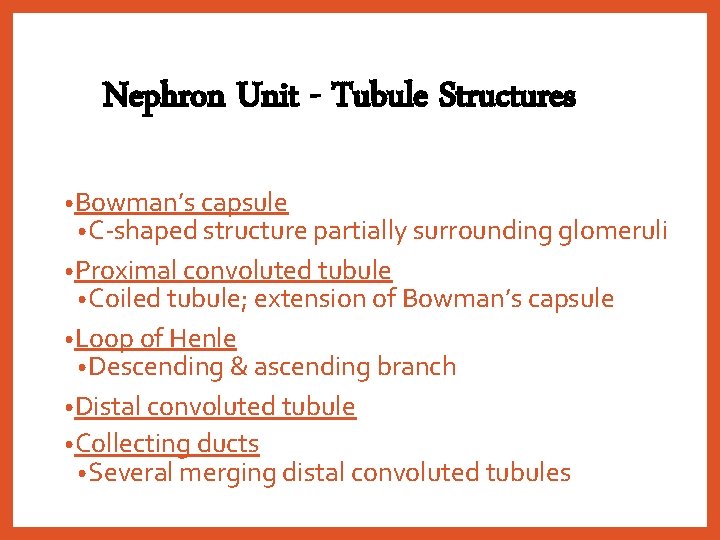
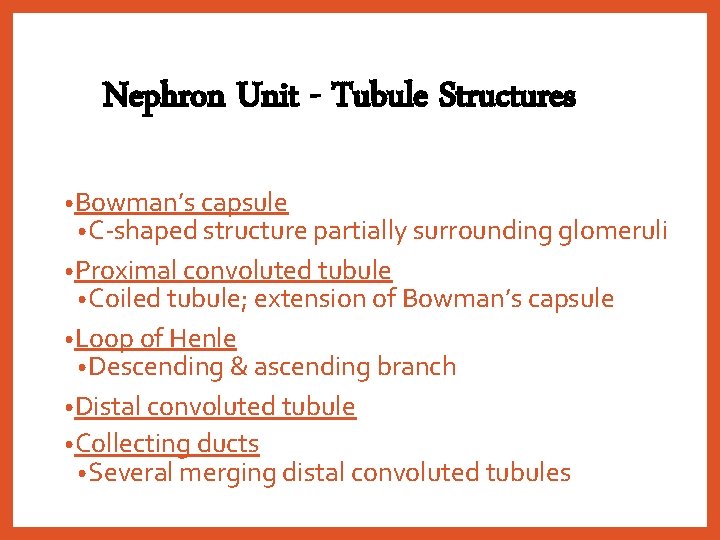
Nephron Unit - Tubule Structures • Bowman’s capsule • C-shaped structure partially surrounding glomeruli • Proximal convoluted tubule • Coiled tubule; extension of Bowman’s capsule • Loop of Henle • Descending & ascending branch • Distal convoluted tubule • Collecting ducts • Several merging distal convoluted tubules
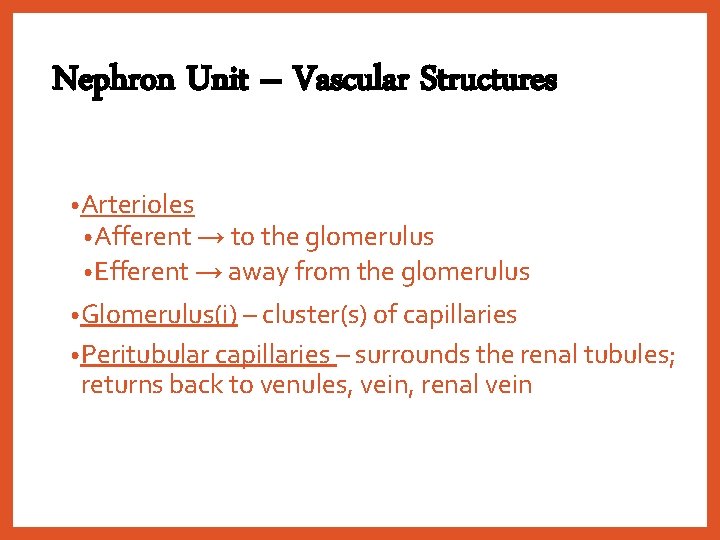
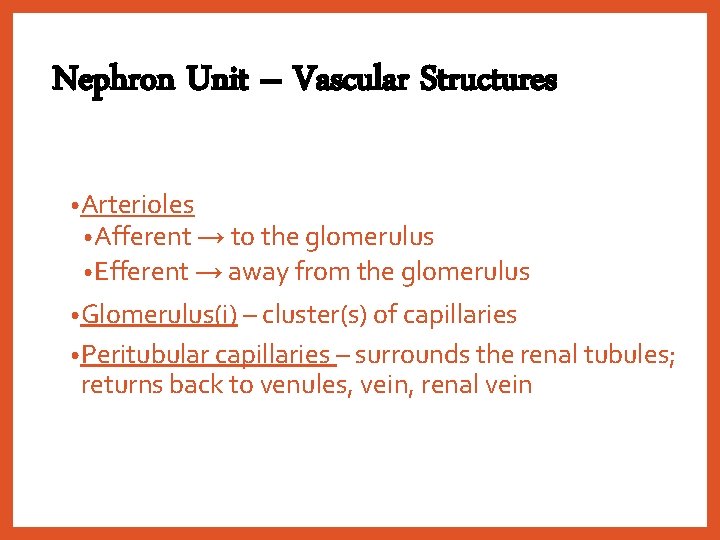
Nephron Unit – Vascular Structures • Arterioles • Afferent → to the glomerulus • Efferent → away from the glomerulus • Glomerulus(i) – cluster(s) of capillaries • Peritubular capillaries – surrounds the renal tubules; returns back to venules, vein, renal vein
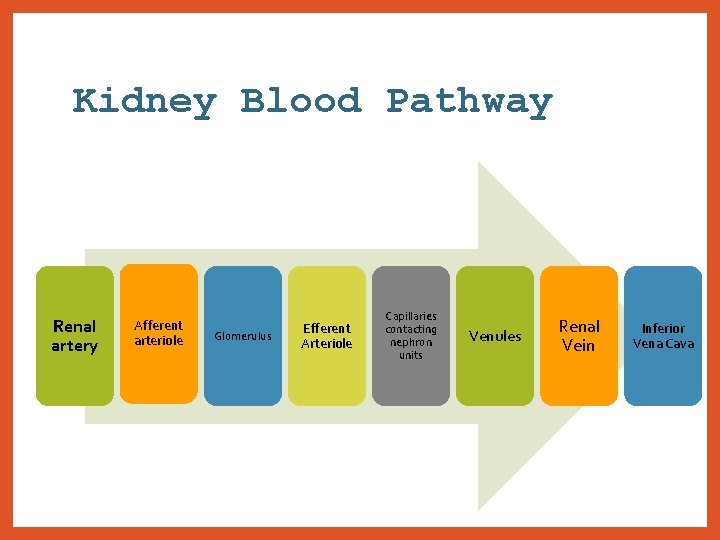
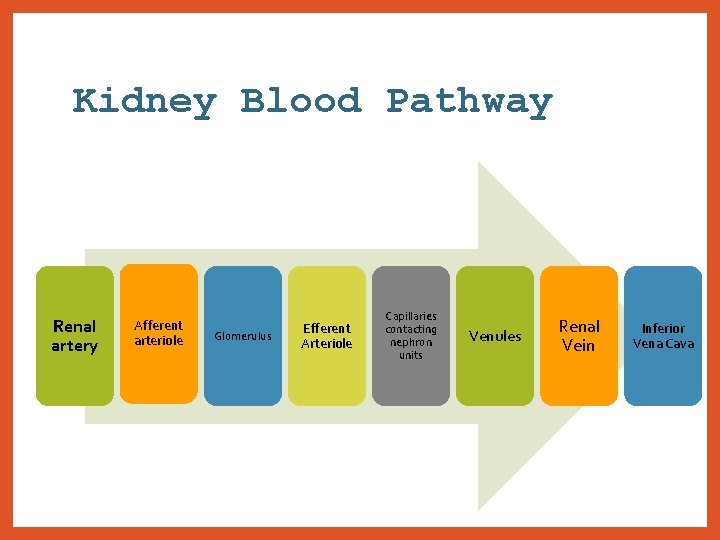
Kidney Blood Pathway Renal artery Afferent arteriole Glomerulus Efferent Arteriole Capillaries contacting nephron units Venules Renal Vein Inferior Vena Cava
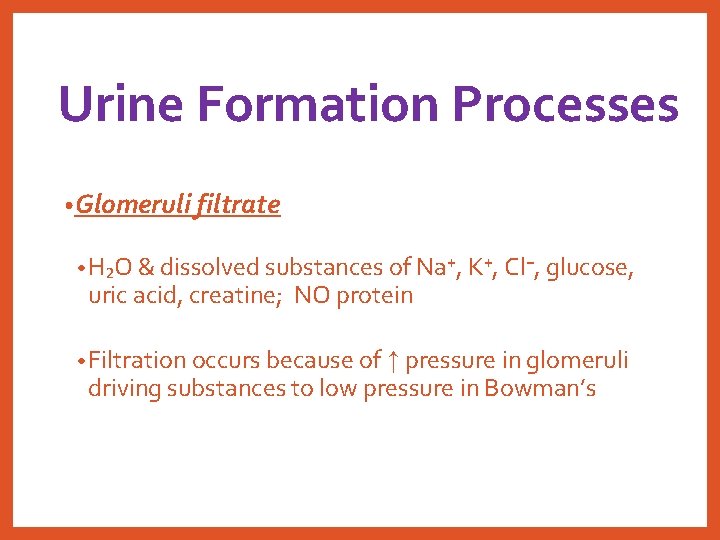
Urine Formation Processes • Glomeruli filtrate • H₂O & dissolved substances of Na⁺, K⁺, Cl⁻, glucose, uric acid, creatine; NO protein • Filtration occurs because of ↑ pressure in glomeruli driving substances to low pressure in Bowman’s
Urine Formation Processes • Tubular reabsorption • From tubules back into peritubular capillaries; mostly @ proximal convoluted tubules • Kidneys decide type & amt. • Achieved through active transport (pumping Na⁺ from the tubules) OR passive transport (where Na⁺ goes, H₂O follows); also hormones • Tubular secretions • Small amt. of substances move from capillaries into the tubules
Antidiuretic Hormone (ADH) • Released from posterior pituitary gland • Stimulates collecting ducts to allow H₂O reabsorption to peritubular capillaries • Stimulus comes from low blood volume
Aldosterone • Mineralcorticoid • Secreted by the adrenal cortex after stimulation by ACTH • Stimulates distal tubule to reabsorb Na⁺ & H₂O = expanding blood volume & eliminates K⁺ in the urine • Released in response to the enzyme renin
Renin-Angiotensin-Aldosterone System • Juxtaglomerular apparatus (JGA): arterioles specialized cells in the afferent • Renin: enzyme released from the JGA when blood volume or BP ↓ • Angiotensinogen • Inactive form located in liver • Is activated by renin to convert to angiotensin I • Converting enzyme • In blood • Converts angiotensin I to angiotensin II
Renin-Angiotensin-Aldosterone • Angiotensin II • Stimulates release of aldosterone • Also is a vasopressor
Urine Composition • Mostly H₂O, waste, electrolytes • 1500 m. L/day • p. H: 5. 0 – 8. 0 (usually acidic) • Characteristic odor • Specific gravity: 1. 001 – 1. 030
Urinary Structures – Ureters • Carries urine from renal pelvis to bladder
Urinary Structures – Bladder • Temporary urine storage (rugae) • Mucosa, submucosa, muscle, serosa • Internal sphincter - at exit of bladder • Smooth muscle; involuntary • External sphincter – below internal • Skeletal muscle; voluntary • Urination, micturition, void • Micturition reflex: full bladder; sensory nerves to spinal cord; motor response back to bladder; bladder wall contracts & internal sphincter relaxes
Urethra • Carries urine from bladder to outside (meatus) • Lined with mucous membrane • Length varies
Male Reproductive System Functions • Produces, nourishes, transports sperm • Deposits sperm within female reproductive tract • Secretes hormones that determine secondary sex characteristics
Internal Male Structures & Functions - Testes • Male gonad • Produce sperm & secrete testosterone • Begins developing within abdominopelvic cavity & descends into scrotum to live at lower than body temperature environment • Made of lobules • Seminiferous tubules • Sperm production • Interstitial cells • Secrete the androgens • Spermatogenesis • Sperm formation • Primary spermatocyte undergoes meiosis
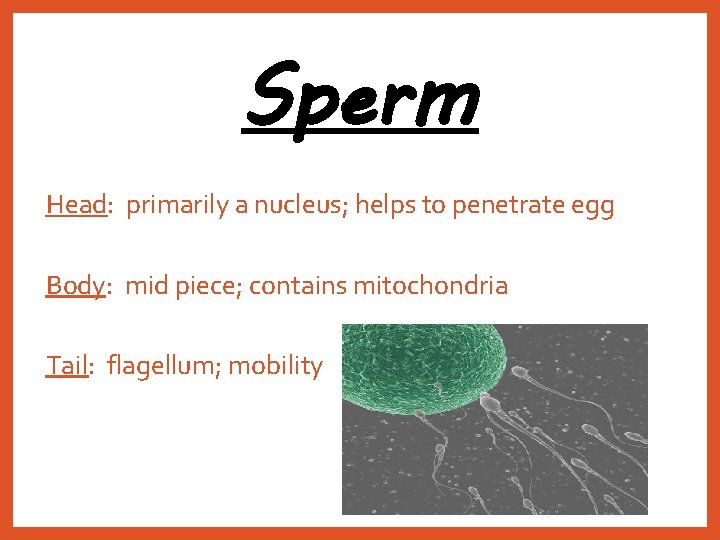
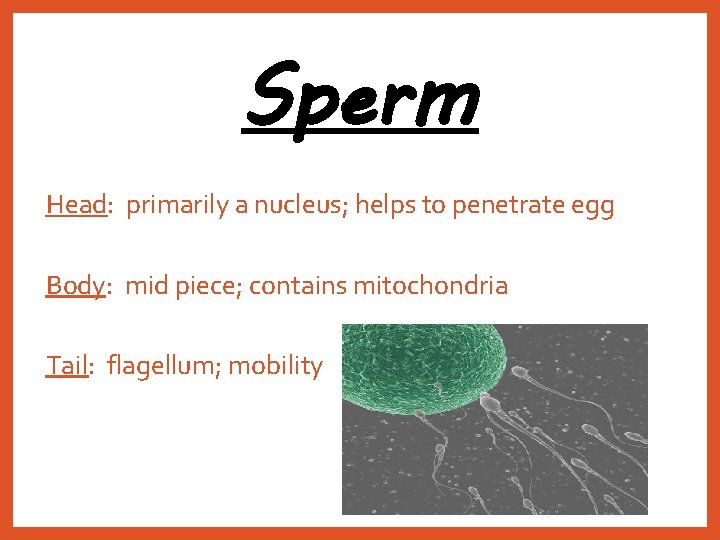
Sperm Head: primarily a nucleus; helps to penetrate egg Body: mid piece; contains mitochondria Tail: flagellum; mobility
Genital Ducts • Epididymis • Tightly coiled structure sitting on top of testes; • Sperm matures here • Vas deferens • Ascend with spermatic cord into pelvic cavity, curves over bladder
Genital Ducts • Ejaculatory ducts • The joining of the vas deferens with the seminal vesicles • R. & L. duct merge to join urethra • Urethra • Extends from bladder to tip of penis • Surrounded by prostate gland • Transports urine & semen
Accessory Glands • Seminal vesicles • Base of bladder • Adds a nutritious secretion to semen • Prostate gland • Encircles urethra just below the bladder • Produces alkaline secretion to neutralize vaginal acid & ↑ sperm mobility • Contracts during ejaculation to move semen • Bulbourethral glands • Cowper’s glands • Secrete lubricating mucus into distal urethra
Semen Functions • Nourishes • Transports • Lubricates sperm lower structures of reproductive tract
Male External Genitals Penis • Shaft • 3 columns of erectile tissue • Accumulation of blood causes erection • Glans penis: distal end • Urinary meatus: penetrates the glans • Prepuce • Foreskin; covers the glans • Function • Expels urine & is intercourse organ
Male External Genitals Scrotum • Sac that holds the testes
Testosterone • Primary sex characteristics • Testes & penis size • Secondary sex characteristics • Hair growth & distribution • ↓ voice • Musculoskeletal growth • ↑ activity of skin glands
Male Hormone System • Hypothalamus – releasing hormones → anterior pituitary gland = gonadotropins • FSH • Stimulates spermatogenic cells = sensitivity ↑ to testosterone • LH • Stimulates interstitial cells to secrete testosterone • Negative feedback effect • As plasma levels of testosterone ↑, ant. pituitary ↓ LH output
Female Reproductive Functions • Produces ova • Secretes hormones • Nurtures & protects a developing fetus during 9 months of pregnancy
Internal Structures & Functions Ovaries – female gonad • Egg development – the ovarian follicle (a tiny saclike structure; MANY) • Each follicle contains an immature oocyte (egg) & surrounding follicular cells • Oocyte → meiosis • Follicular cells → estrogen • Mature ovarian follicle = graafian follicle
OVULATION eject 1 egg/month from surface • Egg swept up by the fimbriae of the fallopian tubes • Follicular cells remain in the ovary; become corpus luteum (gland structure) → progesterone • Corpus luteum = YELLOW BODY • Corpus albicans = WHITE BODY
Internal Structures Fallopian Tubes • Oviduct, uterine tubes • Site of fertilization • Transports egg to uterus • Infundibulum – distal tube
Internal Structures Uterus • Fundus • Upper dome shape part • Body • Center • Cervix • Long narrow region • Layers • Epimetrium (outer) • Myometrium (muscle) • Endometrium (inner)
Internal Structure Vagina • Part of birth canal • Receives penis during intercourse
External Female Genitalia Vulva • Labia majora & minora • Prevents drying of the mucous membrane • Clitoris • Erectile tissue • Vestibule • Between labia minora • Contains urethral & vaginal openings • Bartholin’s glands • Vestibular glands near the vaginal opening; secrete mucus • Perineum • Between vaginal & anus
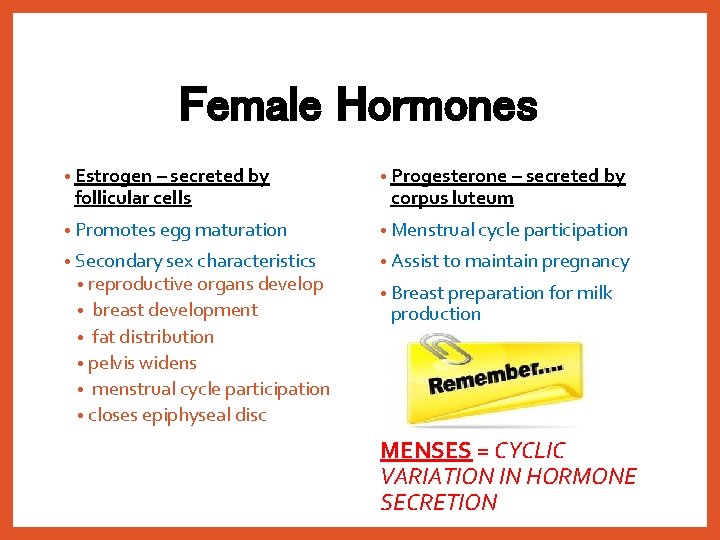
Female Hormones • Estrogen – secreted by • Progesterone – secreted by • Promotes egg maturation • Menstrual cycle participation • Secondary sex characteristics • reproductive organs develop • Assist to maintain pregnancy follicular cells breast development • fat distribution • pelvis widens • menstrual cycle participation • closes epiphyseal disc • corpus luteum • Breast preparation for milk production MENSES = CYCLIC VARIATION IN HORMONE SECRETION
Ovarian Cycle Follicular phase • Hypothalamus → releasing hormones → ant. pituitary gland → gonadotropins • FSH → development of ovarian follicle which the follicular cells secrete estrogen (which dominates this phase) • LH → ovulation @ about 14 days & starts luteal phase
Ovarian Cycle Luteal phase • Dominated by the progesterone secreted by the corpus luteum • ↑ levels of estrogen & progesterone • Prevent release of gonadotropins • Build up endometrial lining (progesterone) in preparation for pregnancy
Uterine Cycle • Menstrual phase • Shedding of endometrial lining due to ↓ in ovarian hormones when corpus luteum dies • Proliferative phase • Buildup of endometrial lining after menstruation due to estrogen secretion • Secretory phase • Endometrial thickening from progesterone secretion
Pregnant State Human chorionic gonadotropin (h. CG) • Will be secreted by the trophoblastic cells of the embryo to maintain corpeus luteum to continue secreting hormones to maintain endometrial tissue