Peptic Ulcer Disease Anatomy and Physiology of GI



- Slides: 54
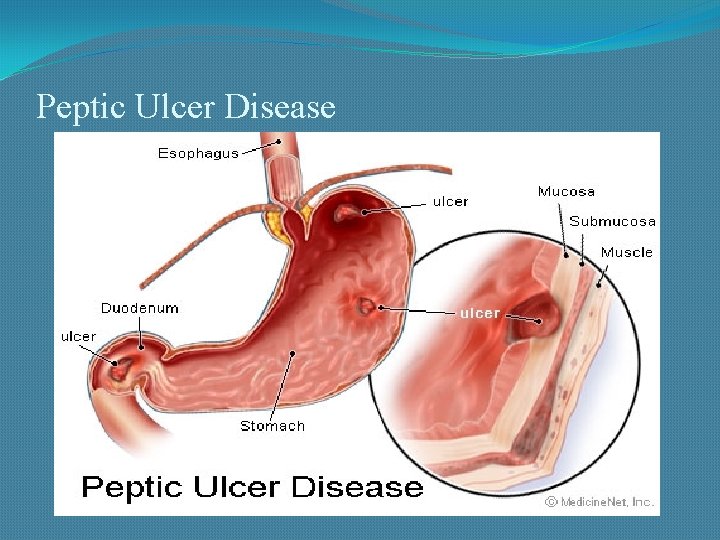
Peptic Ulcer Disease
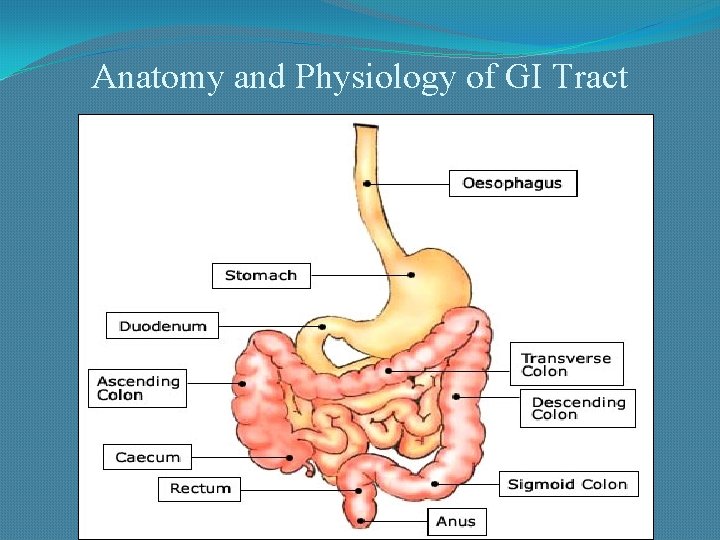
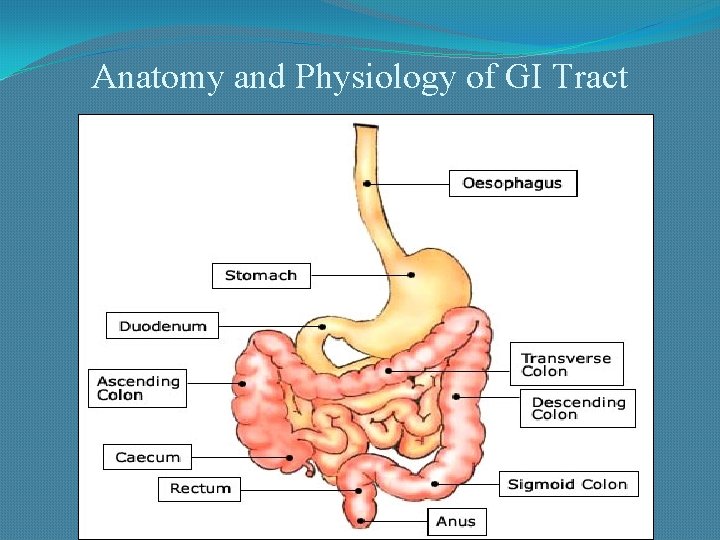
Anatomy and Physiology of GI Tract
Definition: � Peptic ulcer disease (PUD) = Mucosal break/defect in the gastrointestinal tract (gastric or duodenal) exposed to acid and pepsin secretion �Gastritis is the precursor to PUD and it is clinically difficult to differentiate the two
Sites of Peptic Ulcer �Duodenum: First portion ( few cms from the pyloric ring). Anterior wall is more often affected. �Stomach: Usually antrum. Lesser curvature (common). Anterior and posterior wall and greater curvature (less common). �Lower esophagus �In the margins of a gastroenterostomy (stomal ulcer) �In the duodenum, stomach or jejunum of patients with Zollinger. Ellison syndrome.
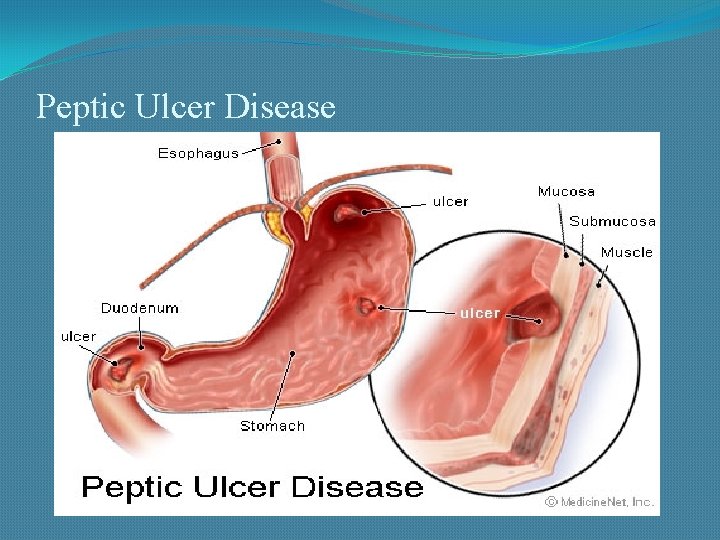
Peptic Ulcer Disease
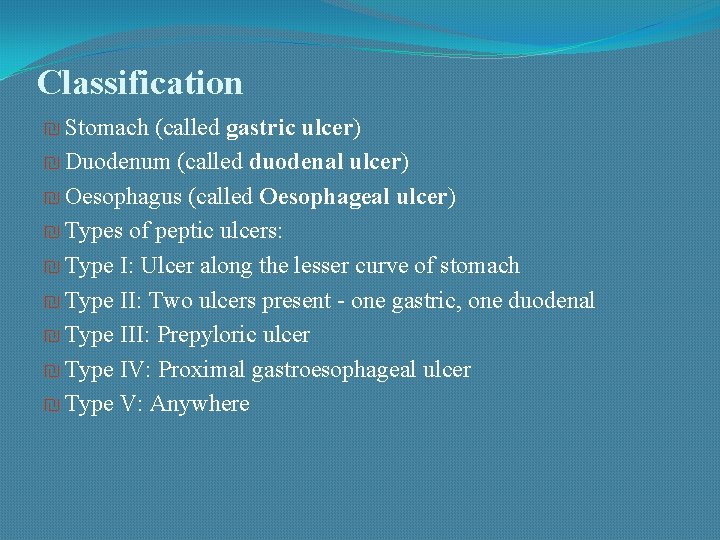
Classification ₪ Stomach (called gastric ulcer) ₪ Duodenum (called duodenal ulcer) ₪ Oesophagus (called Oesophageal ulcer) ₪ Types of peptic ulcers: ₪ Type I: Ulcer along the lesser curve of stomach ₪ Type II: Two ulcers present - one gastric, one duodenal ₪ Type III: Prepyloric ulcer ₪ Type IV: Proximal gastroesophageal ulcer ₪ Type V: Anywhere
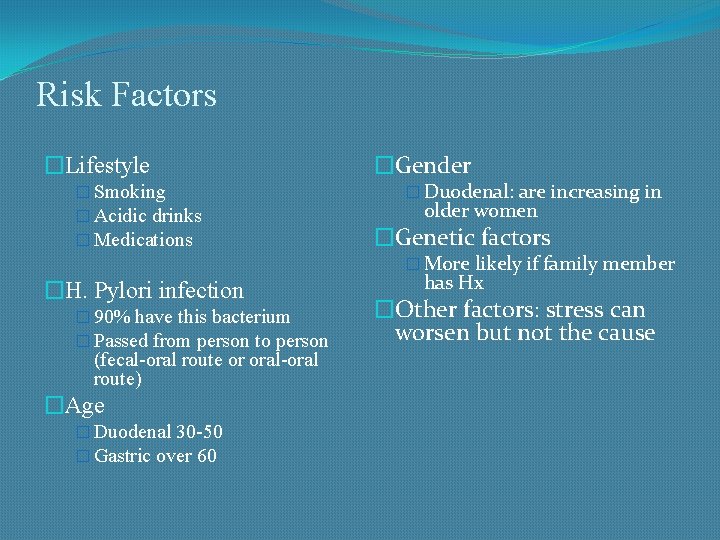
Risk Factors �Lifestyle � Smoking � Acidic drinks � Medications �Gender � Duodenal: are increasing in older women �Genetic factors � More likely if family member �H. Pylori infection � 90% have this bacterium � Passed from person to person (fecal-oral route or oral-oral route) �Age � Duodenal 30 -50 � Gastric over 60 has Hx �Other factors: stress can worsen but not the cause
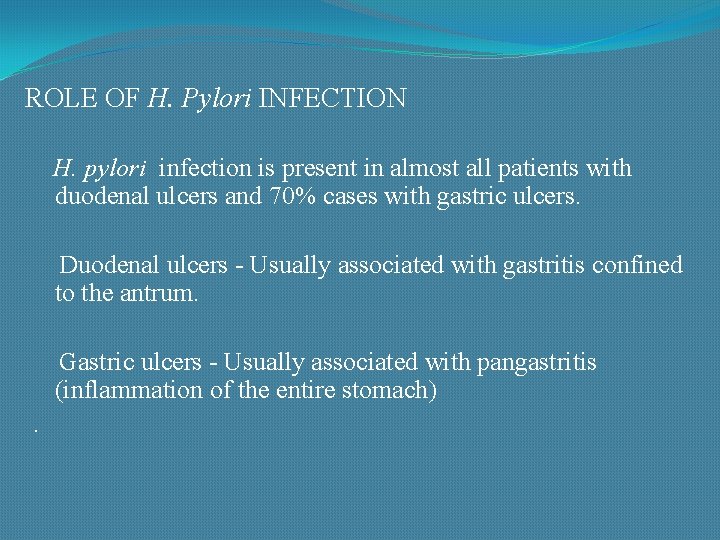
ROLE OF H. Pylori INFECTION H. pylori infection is present in almost all patients with duodenal ulcers and 70% cases with gastric ulcers. Duodenal ulcers - Usually associated with gastritis confined to the antrum. Gastric ulcers - Usually associated with pangastritis (inflammation of the entire stomach).
Mechanism of H pylori �H pylori secretes urease (generates ammonia), protease (breaks down glycoprotein in gastric mucus) �- breakdown of mucosal defense �Damage of the protective mucosal layer. The epithelial cells are exposed to the damaging effect of acid-peptic digestion. �Inflammation of the gastric mucosa. �Chronically inflamed mucosa more susceptible to acid- peptic injury and prone to peptic ulceration. � Ulcers occur at sites of chronic inflammation Eg - Antrum
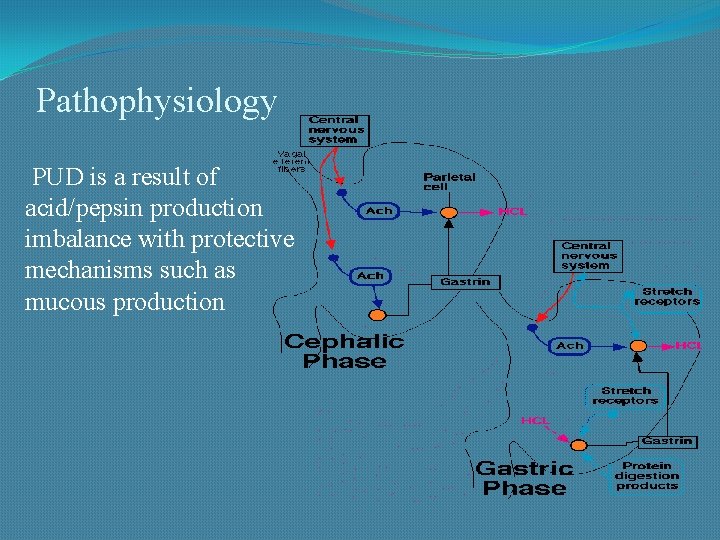
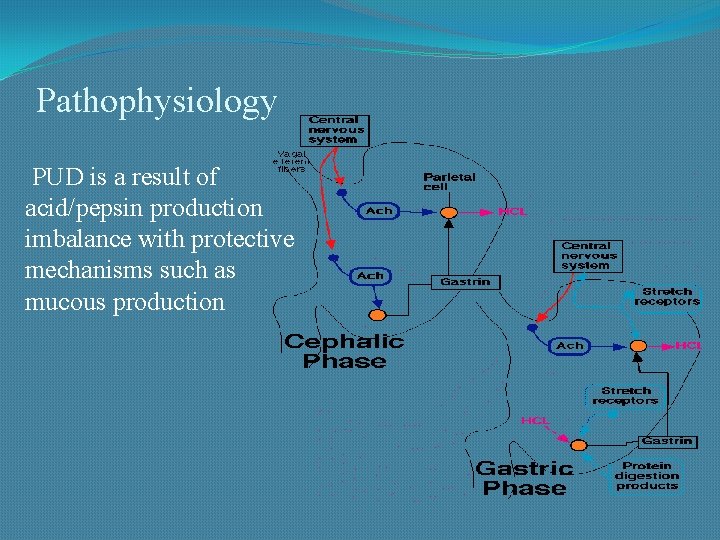
Pathophysiology PUD is a result of acid/pepsin production imbalance with protective mechanisms such as mucous production
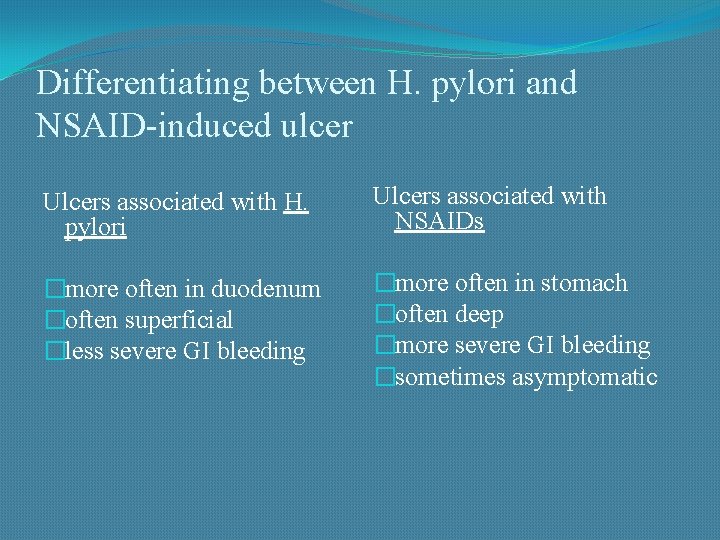
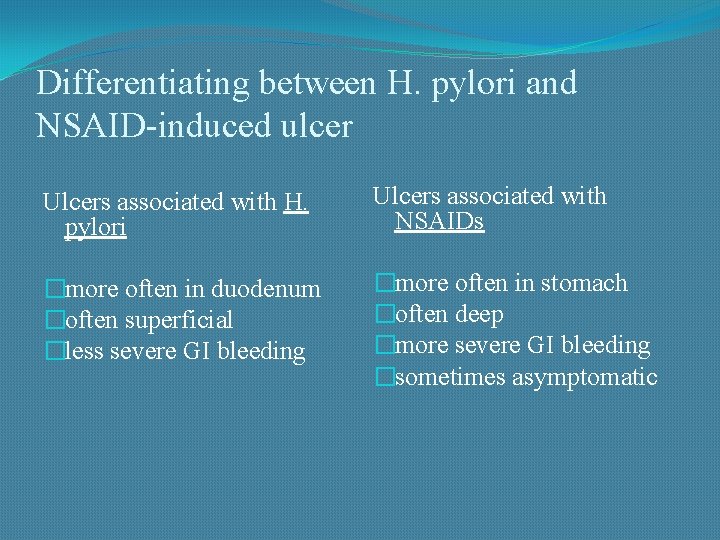
Differentiating between H. pylori and NSAID-induced ulcer Ulcers associated with H. pylori Ulcers associated with NSAIDs �more often in duodenum �often superficial �less severe GI bleeding �more often in stomach �often deep �more severe GI bleeding �sometimes asymptomatic
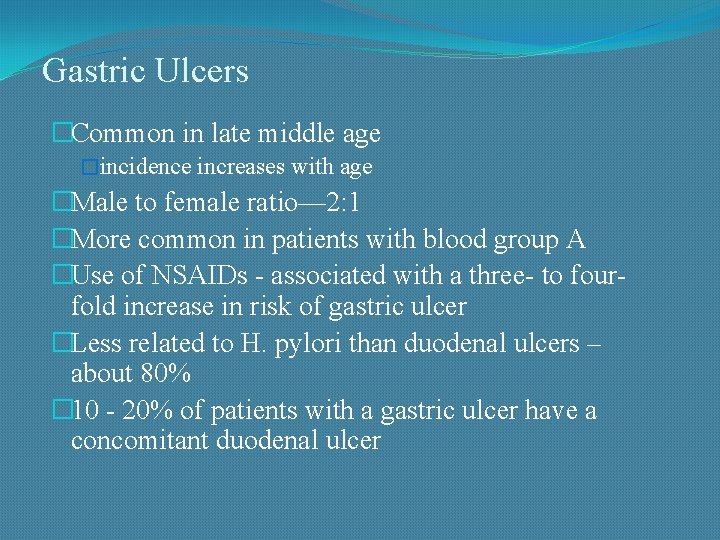
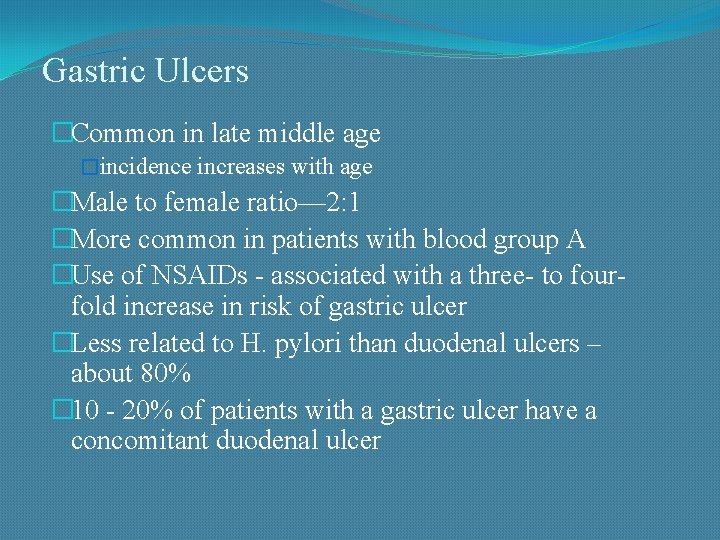
Gastric Ulcers �Common in late middle age �incidence increases with age �Male to female ratio— 2: 1 �More common in patients with blood group A �Use of NSAIDs - associated with a three- to fourfold increase in risk of gastric ulcer �Less related to H. pylori than duodenal ulcers – about 80% � 10 - 20% of patients with a gastric ulcer have a concomitant duodenal ulcer
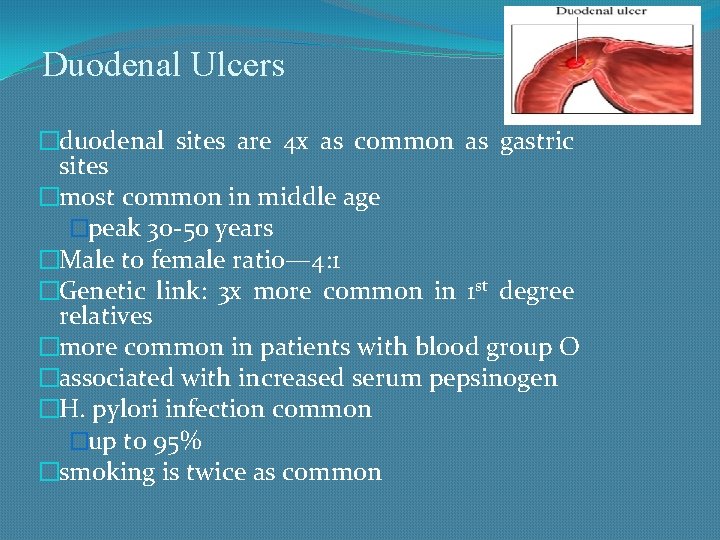
Duodenal Ulcers �duodenal sites are 4 x as common as gastric sites �most common in middle age �peak 30 -50 years �Male to female ratio— 4: 1 �Genetic link: 3 x more common in 1 st degree relatives �more common in patients with blood group O �associated with increased serum pepsinogen �H. pylori infection common �up to 95% �smoking is twice as common
Lab Studies to Evaluate PUD �CBC - evaluate acute/chronic blood loss �H. Pylori - Serologic antibody test for HP – does not active HP infection - Fecal antigen tests for active HP - Urea breath tests for active HP determine if
Diagnosis of H pyloric �Breath Tests & Stool antigen tests - Urea Breath Test ( 95 -100% specificity) -In office test (breath) �Urea Blood test – Less Specific �Endoscopy – culture of organism to determine antibiotic therapy �Serologic test – not reliable (persisting antibiodies)
PUD Diagnosis Initial Differential Diagnosis More Common: �Gastroesophageal reflux disease �Nonulcer dyspepsia/ Gastritis �Ulcer disease �Gastroenteritis �Biliary colic or cholecystitis �Pancreatitis �Irritable bowel disease
Signs and Symptoms of PUD �Epigastric pain is most common symptom �Pain described as gnawing/ burning / annoying �May radiate to the back (consider penetration) �Pain occurs when stomach is empty �Relieved by food, antacids (duodenal), Dyspepsia including belching/ bloating �Hematemesis or melena with GI bleeding �NSAID-induced gastritis or ulcers are frequently “silent”
Complications �Perforation & Penetration—into pancreas, liver and retroperitoneal space �Peritonitis �Bowel obstruction, Gastric outflow obstruction, & Pyloric stenosis �Bleeding--occurs in 25% to 33% of cases and accounts for 25% of ulcer deaths. �Gastric CA
Prevention �Consider prophylactic therapy for the following patients: �Pts with NSAID-induced ulcers who require daily NSAID therapy �Pts older than 60 years �Pts with a history of PUD or a complication such as GI bleeding �Pts taking steroids or anticoagulants or patients with significant comorbid medical illnesses
�Prophylactic regimens that have been shown to dramatically reduce the risk of NSAID-induced gastric and duodenal ulcers include the use of a prostaglandin analogue or a proton pump inhibitor. �Misoprostol --- 100 -200 mcg PO 4 times per day �Omeprazole ---- 20 -40 mg PO every day �Lansoprazole ------- 15 -30 mg PO every day
Treatment Goals �Relieve symptoms �Healing of ulcer �Eliminating cause of ulcer • lowering the amount of acid that stomach makes, • neutralizing the acid • protecting the injured area so it can heal • It's also very important to stop smoking and drinking alcohol • Prevent complications (bleeding, perforation, penetration, obstruction) • Minimize recurrences • Reduce financial costs
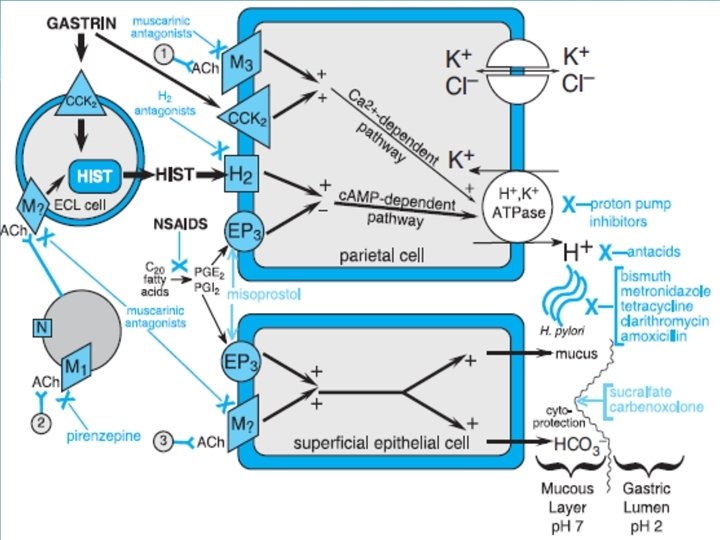
Classification 1. Acid Neutralizing agents: (ANTACIDS) • Systemic: Sodium Bicarbonate and Sod. Citrate • Nonsystemic: Magnesium hydroxide, Mag. Treisilicate, Aluminium hydroxide gel, Magaldrate and calcium carbonate
2. Reduction in Gastric acid secretion: � H 2 antihistamines: Cimetidine, Ranitidine, Famotidine, Nizatidine and Roxatidine � Proton pump inhibitors: Omeprazole, Lansoprazole Pantoprazole, Rabeprazole and Esomeprazole � Anticholinergics: Pirenzepine, Propantheline and Oxyphenonium � Prostaglandin analogue: Misoprostol
3. 4. Ulcer protectives: Sucralfate, Colloidal Bismuth sudcitrate Anti-H. pylori Drugs: Amoxicillin, Clarithromycin, metronidazole, tinidazole and tetracycline
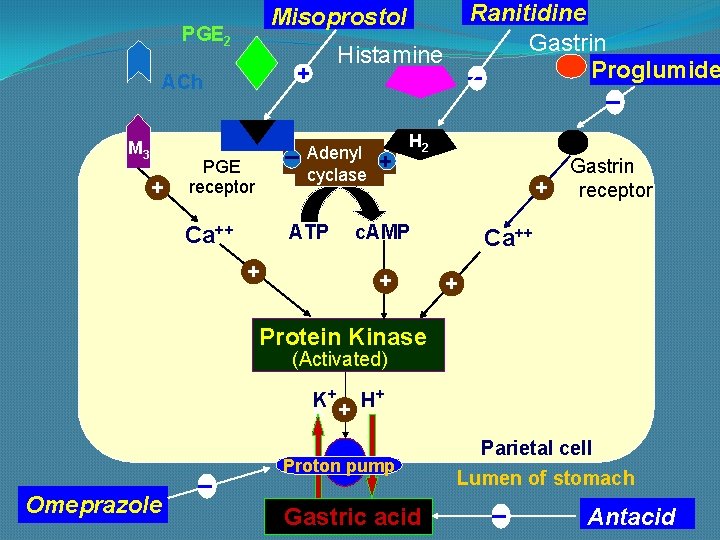
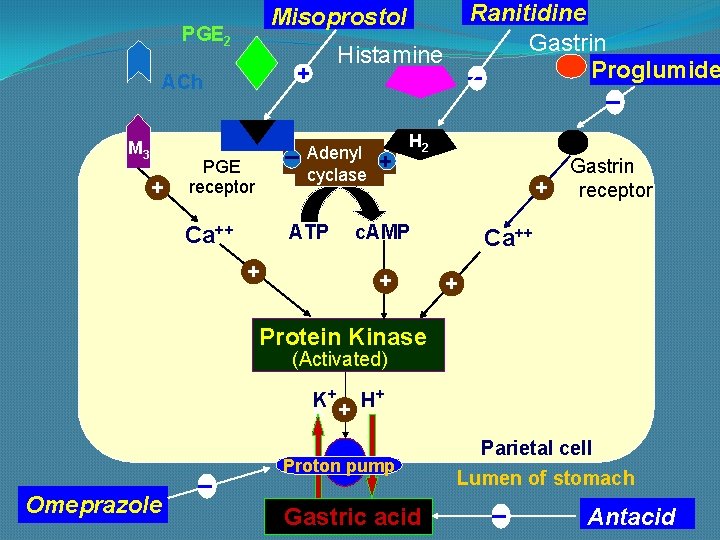
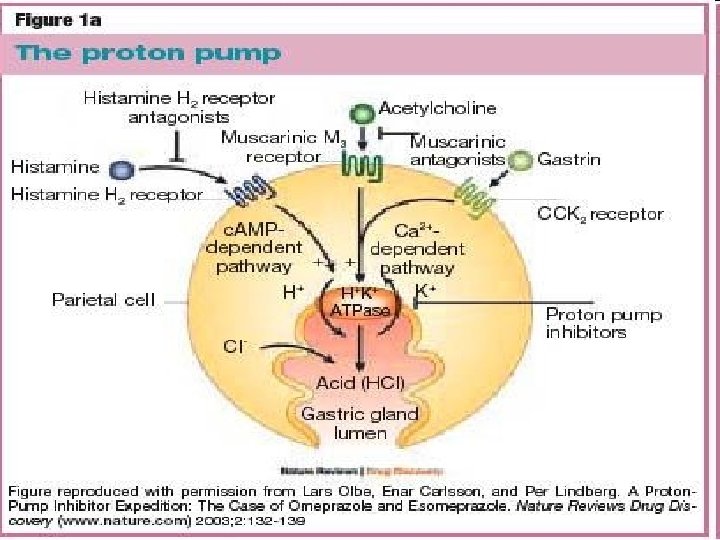
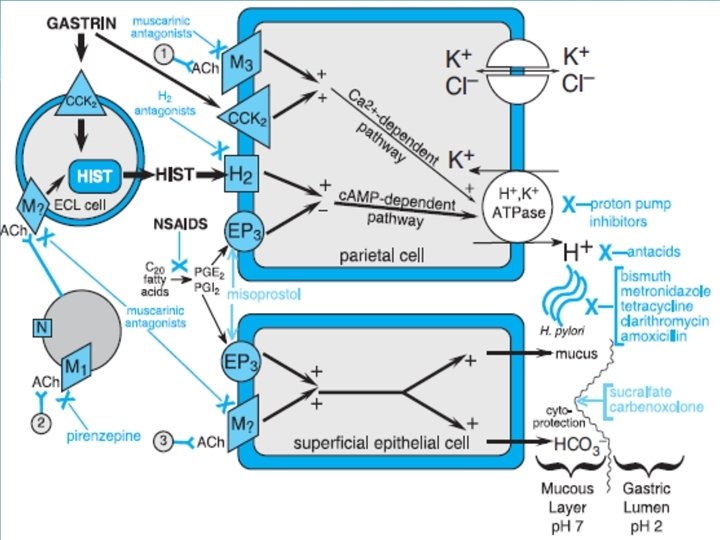
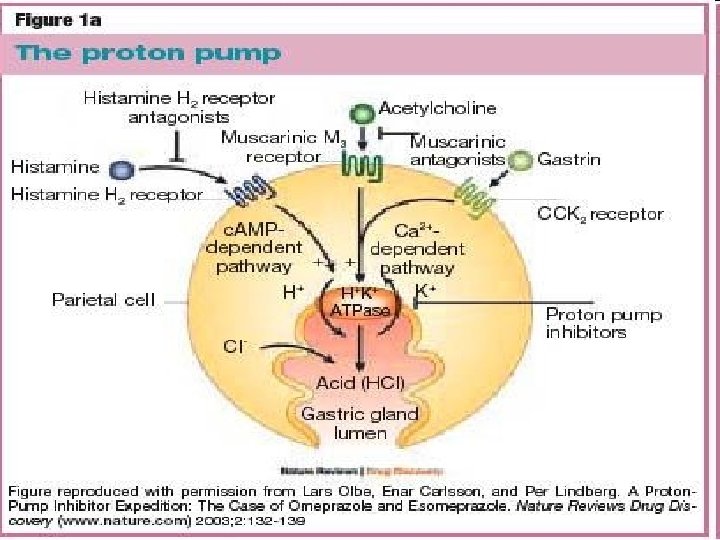
PGE 2 + Histamine + ACh M 3 Ranitidine Gastrin _ Proglumide _ Misoprostol _ PGE receptor Adenyl cyclase ATP Ca++ + + H 2 + c. AMP + Gastrin receptor Ca++ + Protein Kinase (Activated) K+ + H+ K _ Omeprazole Proton pump Gastric acid Parietal cell Lumen of stomach _ Antacid
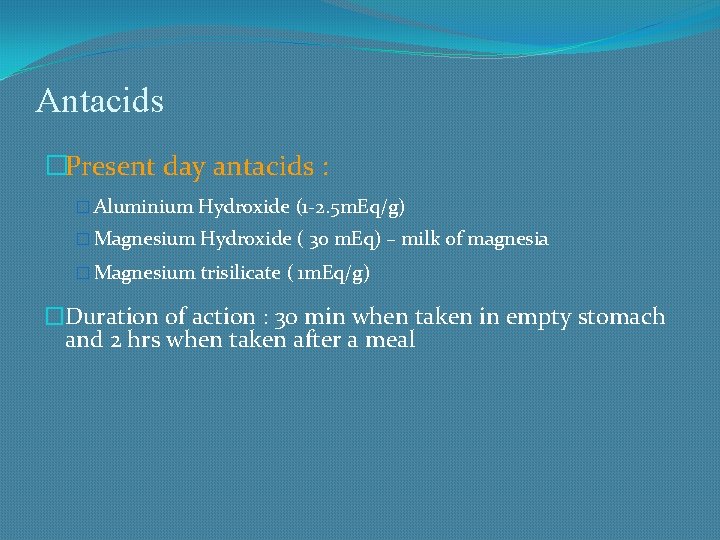
Antacids �Present day antacids : � Aluminium Hydroxide (1 -2. 5 m. Eq/g) � Magnesium Hydroxide ( 30 m. Eq) – milk of magnesia � Magnesium trisilicate ( 1 m. Eq/g) �Duration of action : 30 min when taken in empty stomach and 2 hrs when taken after a meal
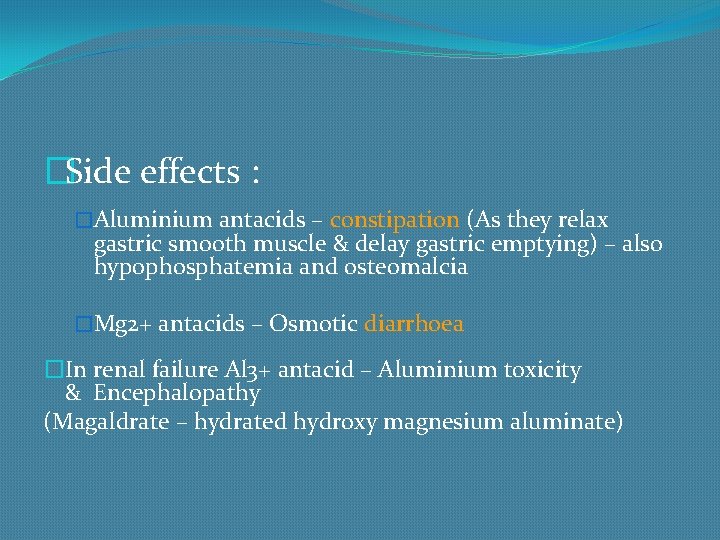
�Side effects : �Aluminium antacids – constipation (As they relax gastric smooth muscle & delay gastric emptying) – also hypophosphatemia and osteomalcia �Mg 2+ antacids – Osmotic diarrhoea �In renal failure Al 3+ antacid – Aluminium toxicity & Encephalopathy (Magaldrate – hydrated hydroxy magnesium aluminate)
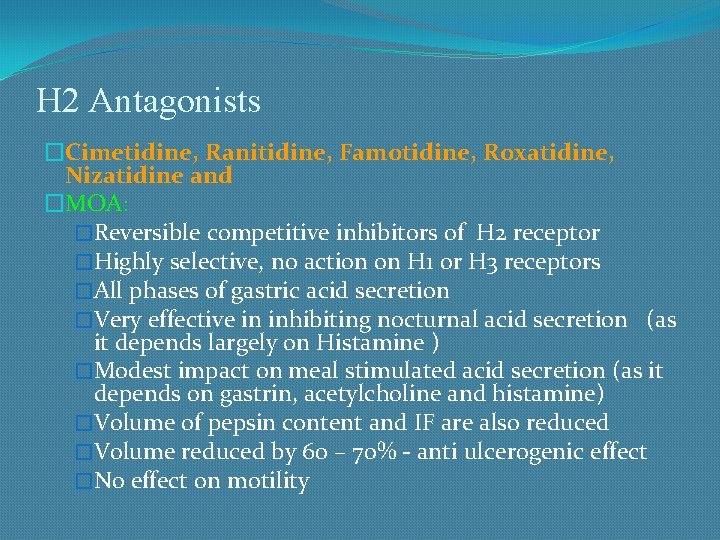
H 2 Antagonists �Cimetidine, Ranitidine, Famotidine, Roxatidine, Nizatidine and �MOA: �Reversible competitive inhibitors of H 2 receptor �Highly selective, no action on H 1 or H 3 receptors �All phases of gastric acid secretion �Very effective in inhibiting nocturnal acid secretion (as it depends largely on Histamine ) �Modest impact on meal stimulated acid secretion (as it depends on gastrin, acetylcholine and histamine) �Volume of pepsin content and IF are also reduced �Volume reduced by 60 – 70% - anti ulcerogenic effect �No effect on motility
�Kinetics: �All drugs are absorbed orally adequately �Bioavailability upto 80 % �Absorption is not interfered by presence of food �Can cross placental barrier and reaches milk �Poor CNS penetration � 2/3 rd of the drugs are excreted unchanged in bile and urine �Preparations: available as tablets, injections
ADRs �Extremely safe drugs and well tolerated �Main ADRs are related to Cimetidine: �Antiandrogenic effects �Increases prolactin secretion and inhibits degradation of estradiol by liver �Cytochrome P 450 inhibition – theophylline, metronidazole, phenytoin, imipramine etc. �Antacids
�Others: �Headache, dizziness, bowel upset, dry mouth �Bolus IV – release histamine – bradycardia, arrhythmia, cardiac arrest �Elderly - precaution
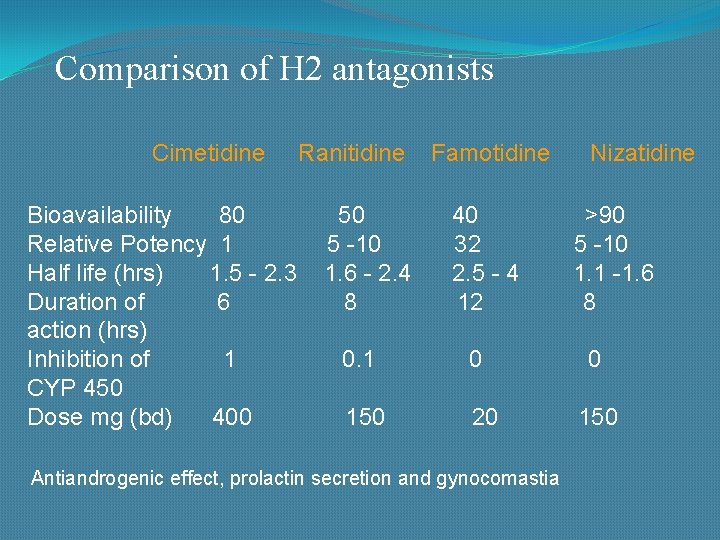
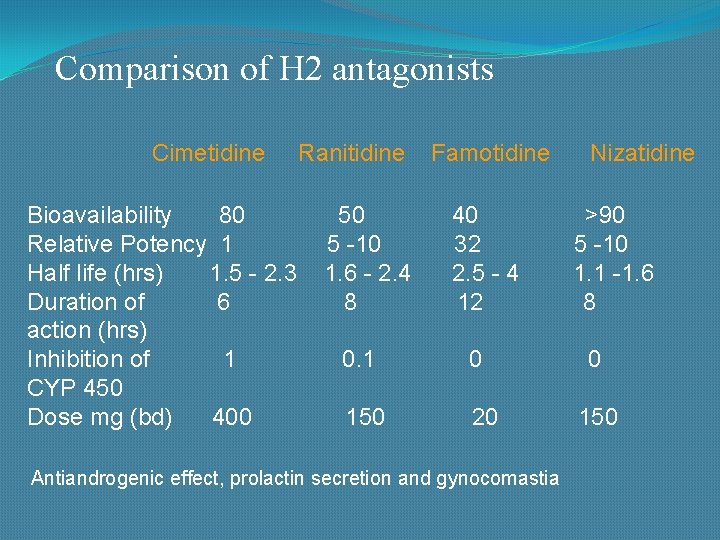
Comparison of H 2 antagonists Cimetidine Ranitidine Famotidine Nizatidine Bioavailability 80 50 40 >90 Relative Potency 1 5 -10 32 5 -10 Half life (hrs) 1. 5 - 2. 3 1. 6 - 2. 4 2. 5 - 4 1. 1 -1. 6 Duration of 6 8 12 8 action (hrs) Inhibition of 1 0. 1 0 CYP 450 Dose mg (bd) 400 150 20 150 Antiandrogenic effect, prolactin secretion and gynocomastia
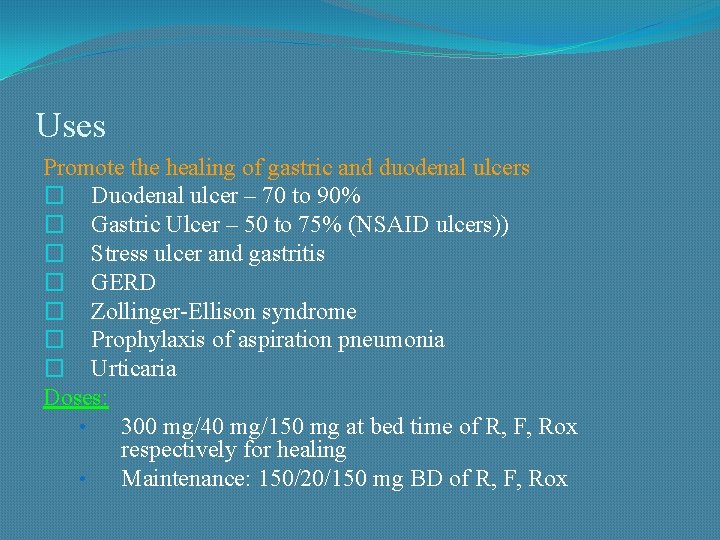
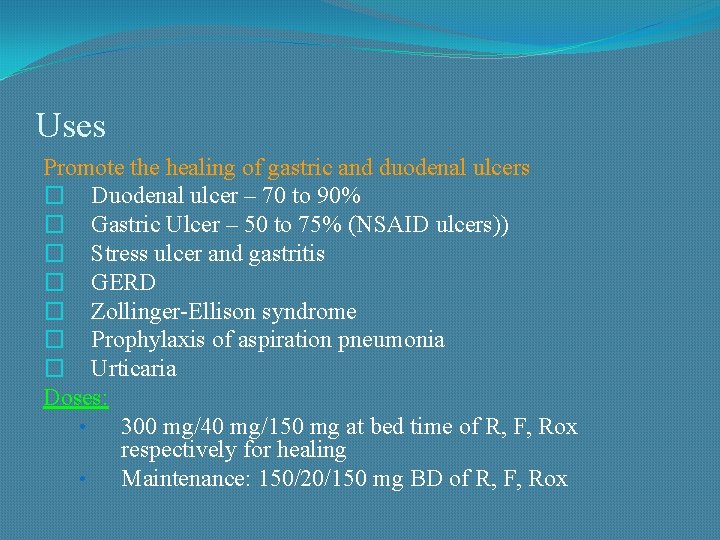
Uses Promote the healing of gastric and duodenal ulcers � Duodenal ulcer – 70 to 90% � Gastric Ulcer – 50 to 75% (NSAID ulcers)) � Stress ulcer and gastritis � GERD � Zollinger-Ellison syndrome � Prophylaxis of aspiration pneumonia � Urticaria Doses: • 300 mg/40 mg/150 mg at bed time of R, F, Rox respectively for healing • Maintenance: 150/20/150 mg BD of R, F, Rox
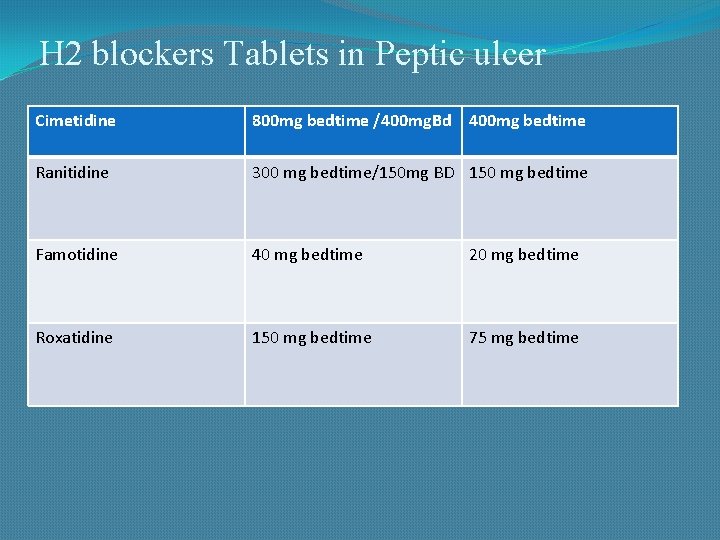
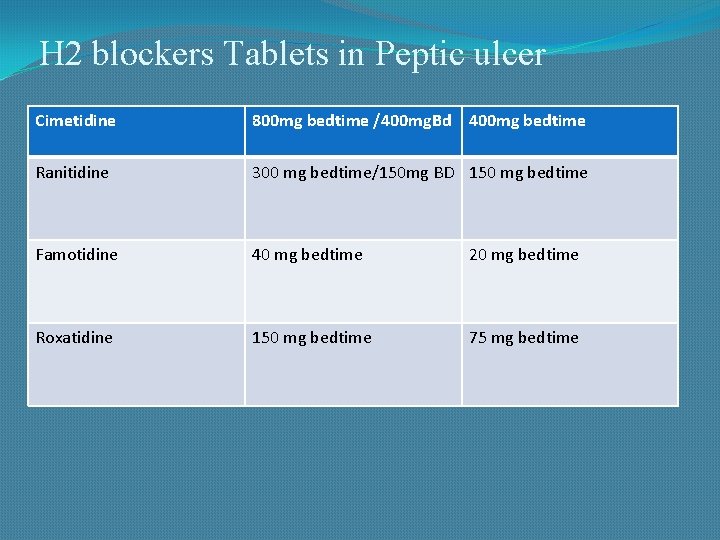
H 2 blockers Tablets in Peptic ulcer Cimetidine 800 mg bedtime /400 mg. Bd 400 mg bedtime Ranitidine 300 mg bedtime/150 mg BD 150 mg bedtime Famotidine 40 mg bedtime 20 mg bedtime Roxatidine 150 mg bedtime 75 mg bedtime
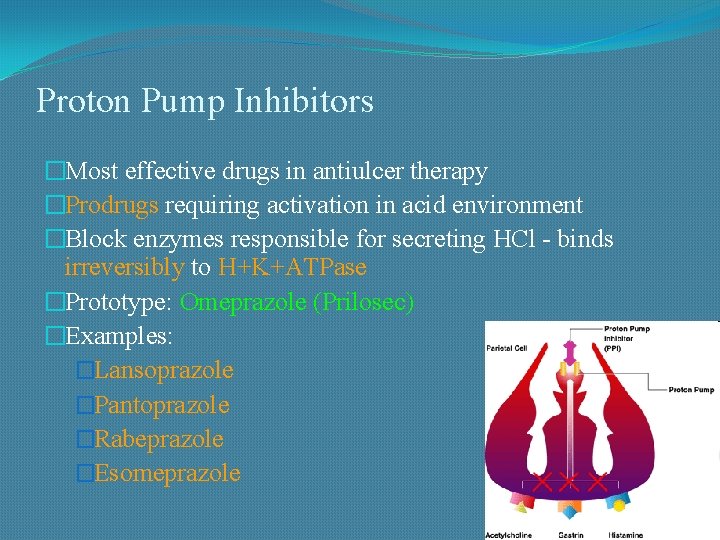
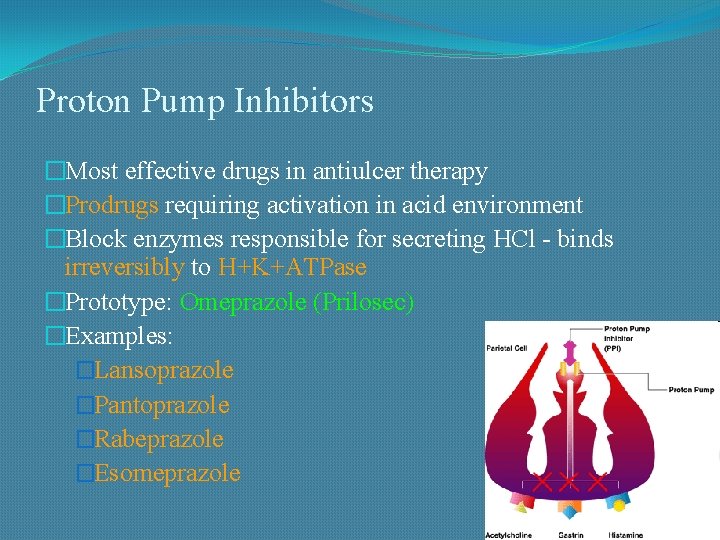
Proton Pump Inhibitors �Most effective drugs in antiulcer therapy �Prodrugs requiring activation in acid environment �Block enzymes responsible for secreting HCl - binds irreversibly to H+K+ATPase �Prototype: Omeprazole (Prilosec) �Examples: �Lansoprazole �Pantoprazole �Rabeprazole �Esomeprazole
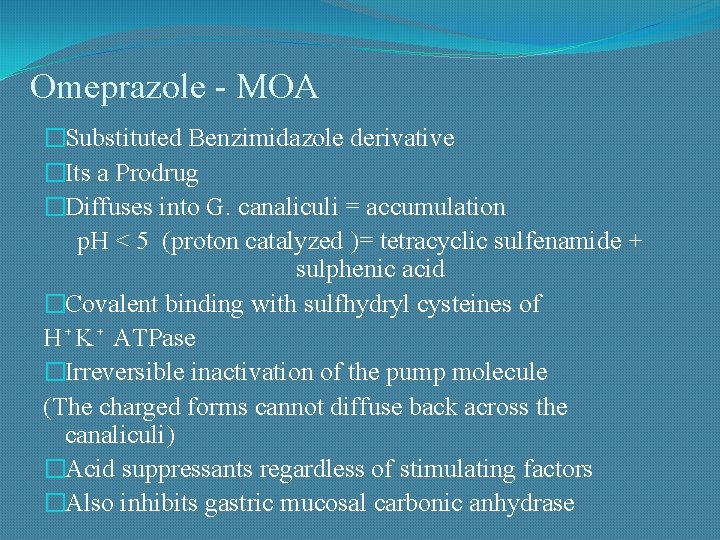
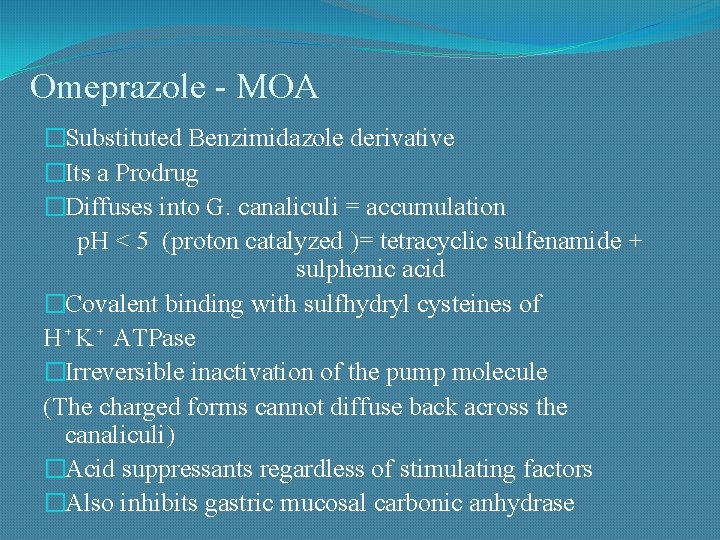
Omeprazole - MOA �Substituted Benzimidazole derivative �Its a Prodrug �Diffuses into G. canaliculi = accumulation p. H < 5 (proton catalyzed )= tetracyclic sulfenamide + sulphenic acid �Covalent binding with sulfhydryl cysteines of H⁺K⁺ ATPase �Irreversible inactivation of the pump molecule (The charged forms cannot diffuse back across the canaliculi) �Acid suppressants regardless of stimulating factors �Also inhibits gastric mucosal carbonic anhydrase
Pharmacokinetics - PPI • Oral forms are prepared as acid resistant formulations that release the drug in the intestine (because they are degraded in acid media) • After absorption, they are distributed by blood to parietal cell canaliculi • They irreversibly inactivate the proton pump molecule – but half life is very short and only 1 -2 Hrs • Still action persists for 24 Hrs to 48 hrs after a single dose – irreversible inhibition of PPI and new PP synthesis takes time (24 to 48 hour suppression of acid secretion, despite the much shorter plasma half-lives of the parent compounds) • Platue state is attained after 4 -5 days of dosing • Action lasts for 4 -5 days even after stoppage of the drug
• Given on an empty stomach because food affects absorption • They should be given 30 minutes to 1 hour before food intake because an acidic p. H in the parietal cell acid canaliculi is required for drug activation, and food stimulates acid production • Concomitant use of other antisecretory drugs - H 2 receptor antagonists – reduces action • Highly protein bound and rapidly Metabolized by the liver by CYP 2 C 19 and CYP 3 A 4 – dose reduction necessary in severe hepatic failure • Excreted in Kidneys minimally (no dose reduction needed in renal failure and elderly)
Adverse Effects • The most common are GIT troubles in the form of nausea, abdominal pain, constipation, flatulence, and diarrhea • Subacute myopathy, arthralgias, headaches, and skin rashes • Prolonged use: • Gynaecomastia, erectile dysfunction • Leucopenia and hepatic dysfunction • Vitamin B 12 deficiency • Hypergastrinemia which may predispose to rebound hypersecretion of gastric acid upon discontinuation of therapy and may promote the growth of gastrointestinal tumors (carcinoid tumors )
Drug Interaction: Inhibits metabolism of Warfarin, Diazepam Therapeutic uses: � � � � Gastroesophageal reflux disease (GERD) Peptic Ulcer - Gastric and duodenal ulcers Bleeding peptic Ulcer Zollinger ellison Syndrome Prevention of recurrence of nonsteroidal antiinflammatory drug (NSAID) - associated gastric ulcers in patients who continue NSAID use. Reducing the risk of duodenal ulcer recurrence associated with H. pylori infections Aspiration Pneumonia
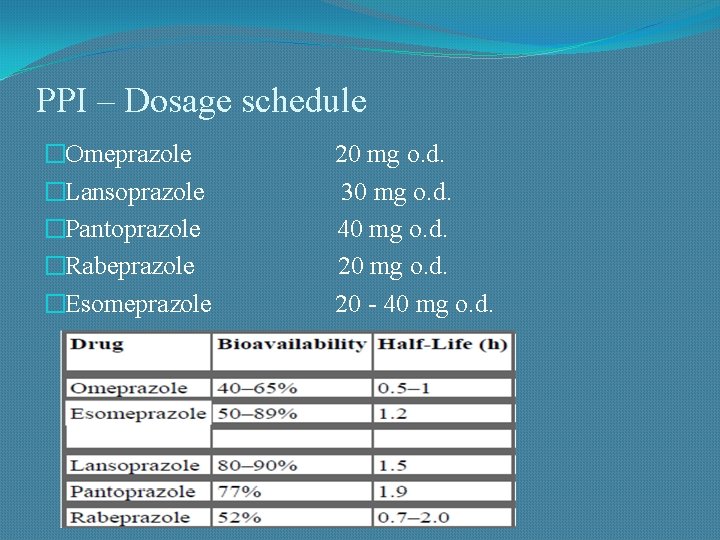
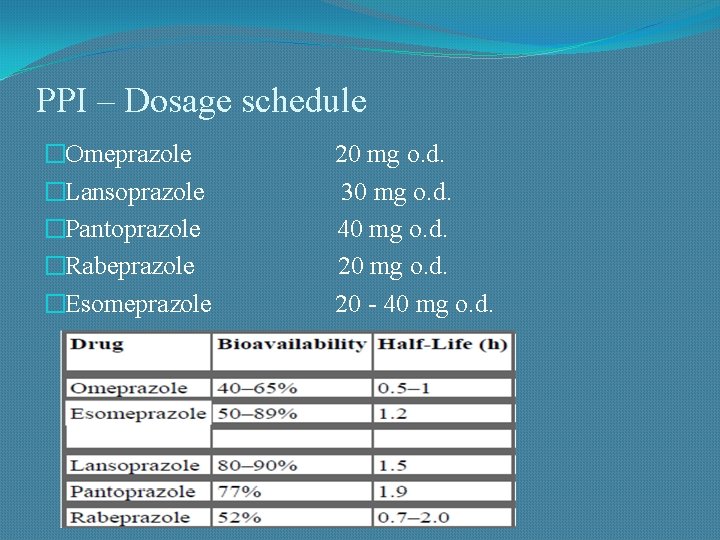
PPI – Dosage schedule �Omeprazole �Lansoprazole �Pantoprazole �Rabeprazole �Esomeprazole 20 mg o. d. 30 mg o. d. 40 mg o. d. 20 - 40 mg o. d.
Muscarinic antagonists Atropine: � Block the M 1 class receptors � Reduce acid production � Abolish gastrointestinal spasm Pirenzepine and Telenzepine Mechanism of action: • Reduce meal stimulated HCl secretion by reversible blockade of muscarinic (M 1) receptors on the cell bodies of the intramural cholinergic ganglia (receptors on parietal cells are M 3). � Unpopular as a first choice because of high incidence of anticholinergic side effects (dry mouth and blurred vision)
Prostaglandin analogues �Inhibit gastric acid secretion �Exhibit ‘cytoprotective’ activity �Enhance local production of mucus or bicarbonate �Promote local cell regeneration �Help to maintain mucosal blood
Prostaglandin analogues - Misoprostol Actions: Inhibit histamine-stimulated gastric acid secretion Stimulation of mucin and bicarbonate secretion Increase mucosal blood flow (Reinforcing of mucous layer buffered by HCO 3 secretion from epithelial cells) Therapeutic uses: Prevent ion of NSAID-induced mucosal injury (rarely used because it needs frequent administration – 4 times daily)
Misoprostol � Doses: 200 mcg 4 times a day (Misoprost) � ADRs: � Diarrhoea and abdominal cramps � Uterine bleeding � Abortion � Exacerbations of inflammatory bowel disease and should be avoided in patients with this disorder Contraindications: 1. Inflammatory bowel disease 2. Pregnancy (may cause abortion)
Omeprazole Amoxicillin Clarithromycin Metronidazole Eradication of H. pylori

Triple Therapy The BEST among all the Triple therapy regimen is: Omeprazole / Lansoprazole - 20 / 30 mg bd Clarithromycin - 500 mg bd Amoxycillin / Metronidazole - 1 gm / 500 mg bd Given for 14 days followed by P. P. I for 4 – 6 weeks Short regimens for 7 – 10 days not very effective
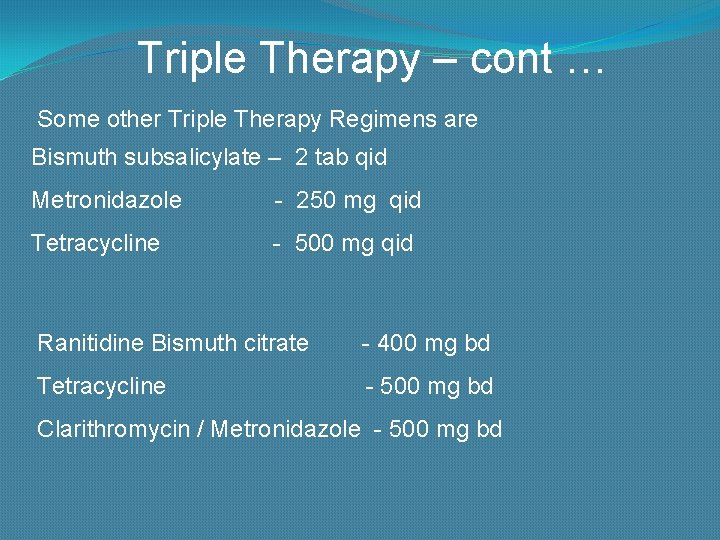
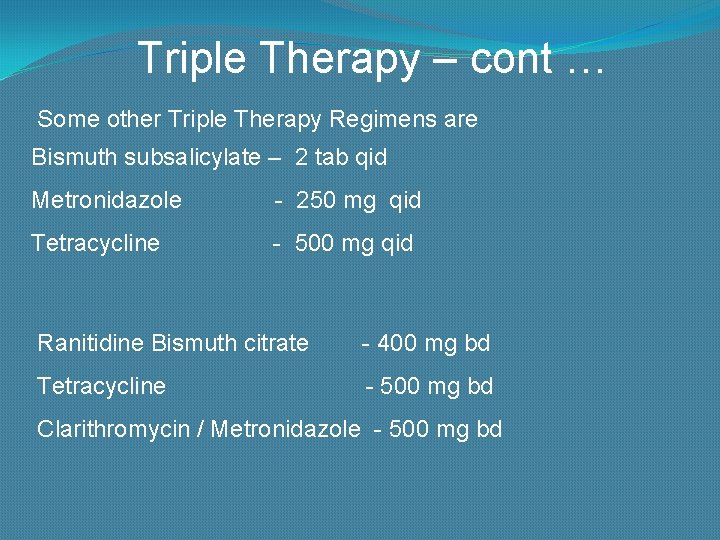
Triple Therapy – cont … Some other Triple Therapy Regimens are Bismuth subsalicylate – 2 tab qid Metronidazole - 250 mg qid Tetracycline - 500 mg qid Ranitidine Bismuth citrate - 400 mg bd Tetracycline - 500 mg bd Clarithromycin / Metronidazole - 500 mg bd
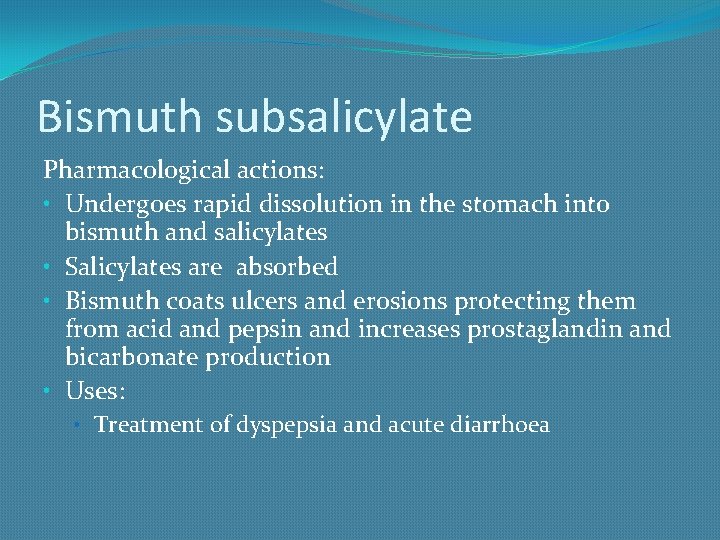
Bismuth subsalicylate Pharmacological actions: • Undergoes rapid dissolution in the stomach into bismuth and salicylates • Salicylates are absorbed • Bismuth coats ulcers and erosions protecting them from acid and pepsin and increases prostaglandin and bicarbonate production • Uses: • Treatment of dyspepsia and acute diarrhoea
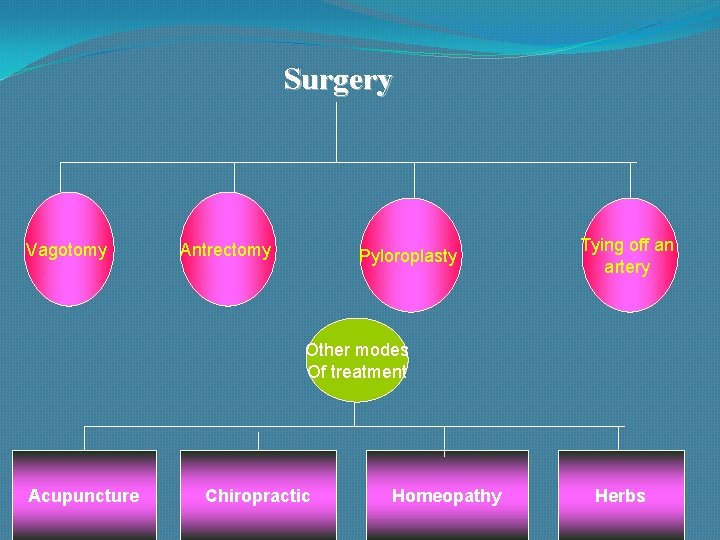
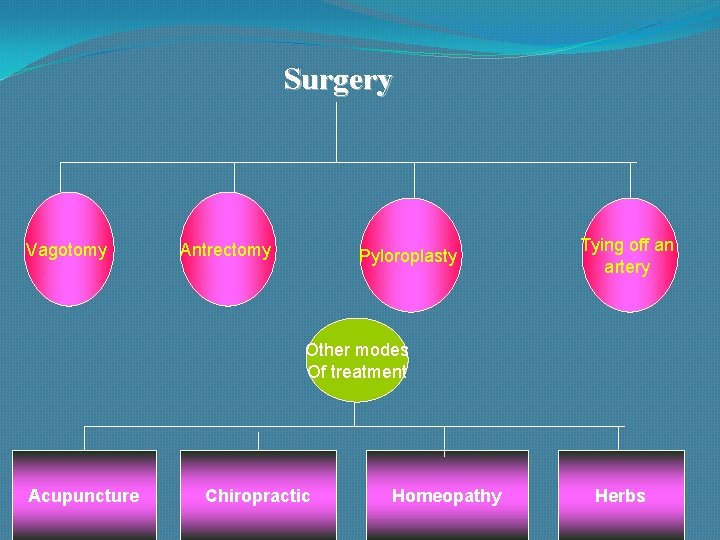
Surgery Vagotomy Antrectomy Pyloroplasty Tying off an artery Other modes Of treatment Acupuncture Chiropractic Homeopathy Herbs

Use of Olive Oil Don't smoke Limit or avoid alcohol Avoid nonsteroidal anti-inflammatory drugs (NSAIDs) Less Coffee and Carbonated Beverages Exercise Fruits and Vegetables Stress Relief

H 2 Receptor Antagonists THANK YOU - in stomach at all stages decreases formation of HCl by selective blocking of H 2 receptors - therapeutic effect after 4 weeks - 60 -80% efficiency, after 8 weeks even 90%, 10 -15% resistance Ranitidine, Famotidine /more effective/, Nizatidine: /12 x daily/ - good pharmacokinetic /p. o. absorbtion, metabolism in liver/ and safety profile, good tollerance - long-term maintenance therapy after uncomplicated peptic ulcer healing and treatment of some forms of gastric dyspepsias