Urinary System Sanjaya Adikari Department of Anatomy Urinary


- Slides: 54
Urinary System Sanjaya Adikari Department of Anatomy
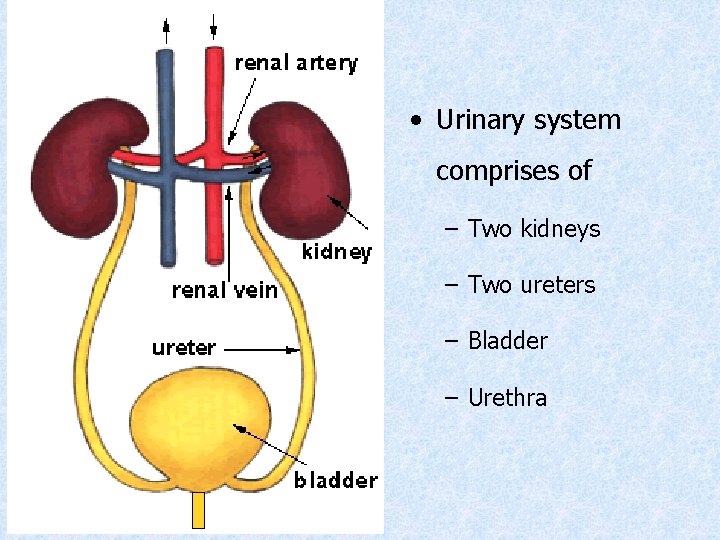
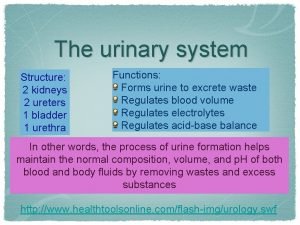
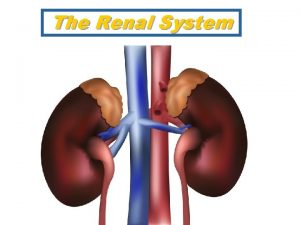
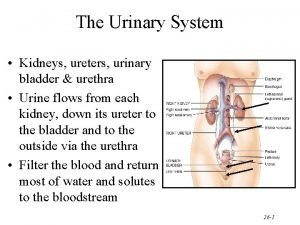
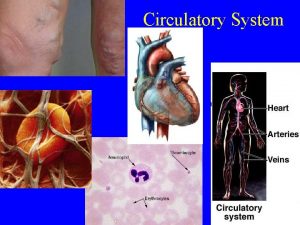
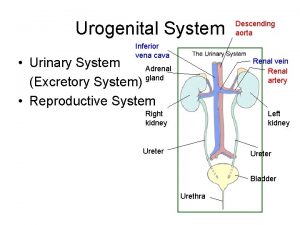
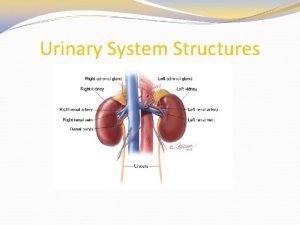
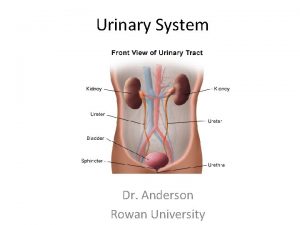
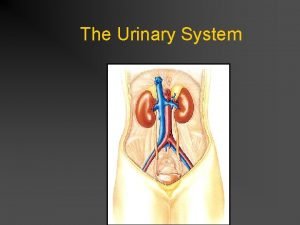
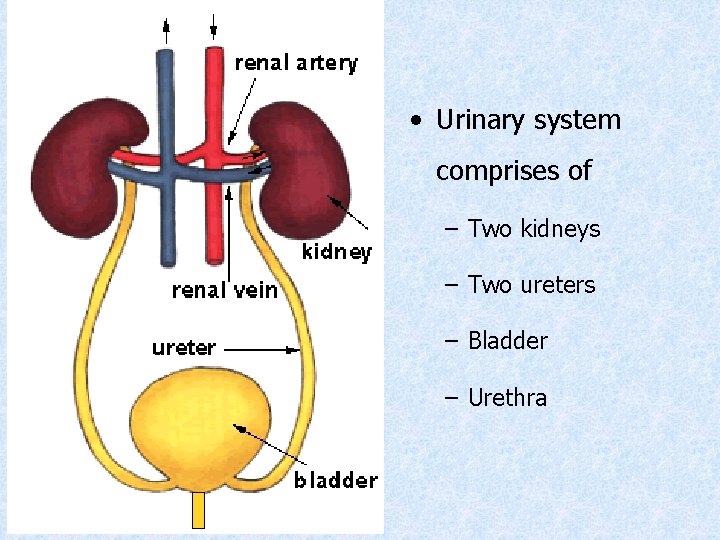
• Urinary system comprises of – Two kidneys – Two ureters – Bladder – Urethra
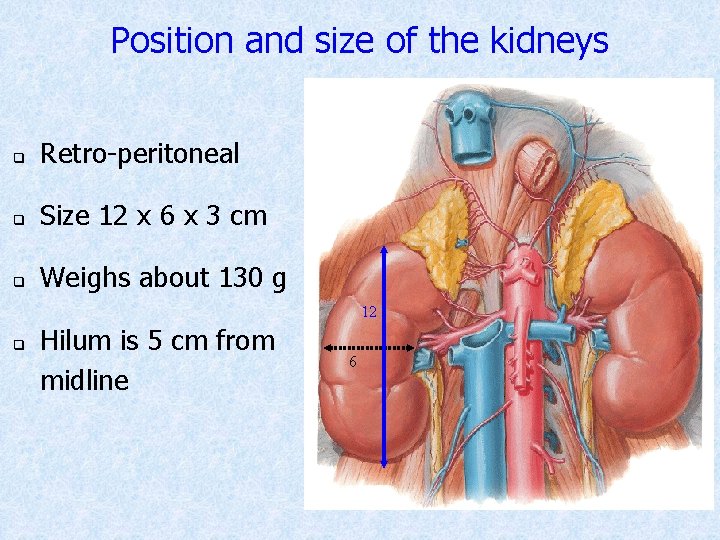
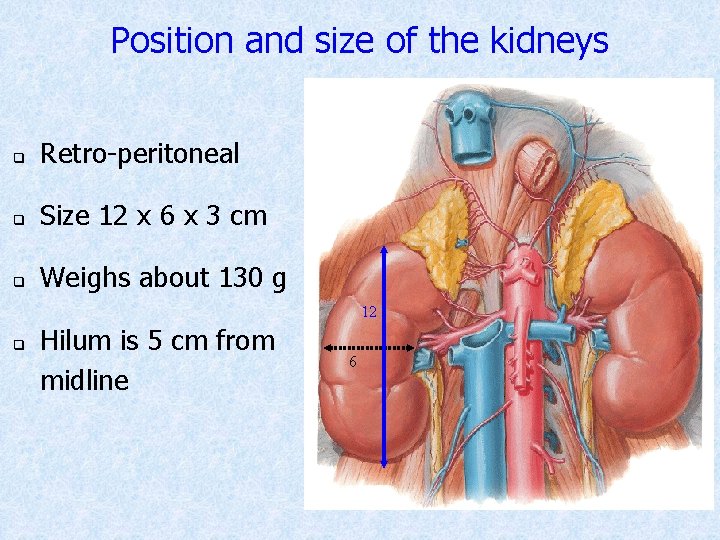
Position and size of the kidneys q Retro-peritoneal q Size 12 x 6 x 3 cm q Weighs about 130 g 12 q Hilum is 5 cm from midline 6
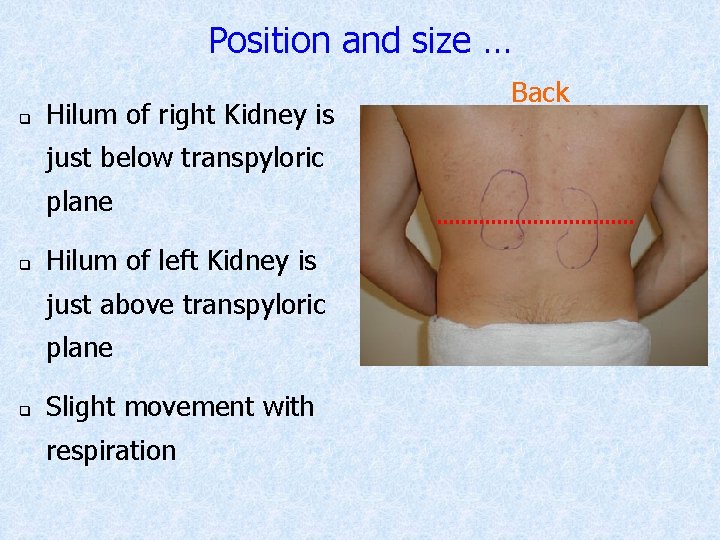
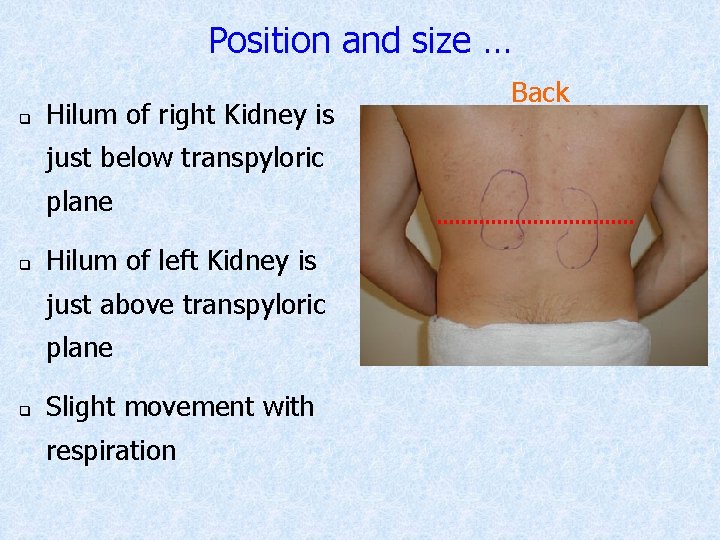
Position and size … q Hilum of right Kidney is just below transpyloric plane q Hilum of left Kidney is just above transpyloric plane q Slight movement with respiration Back
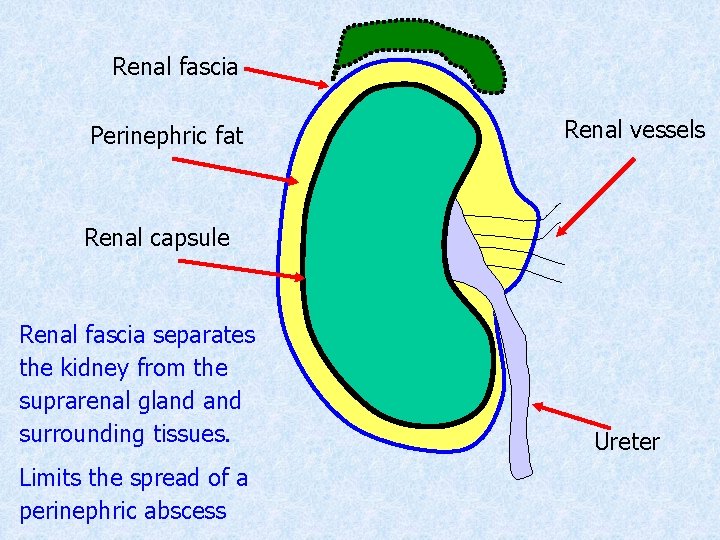
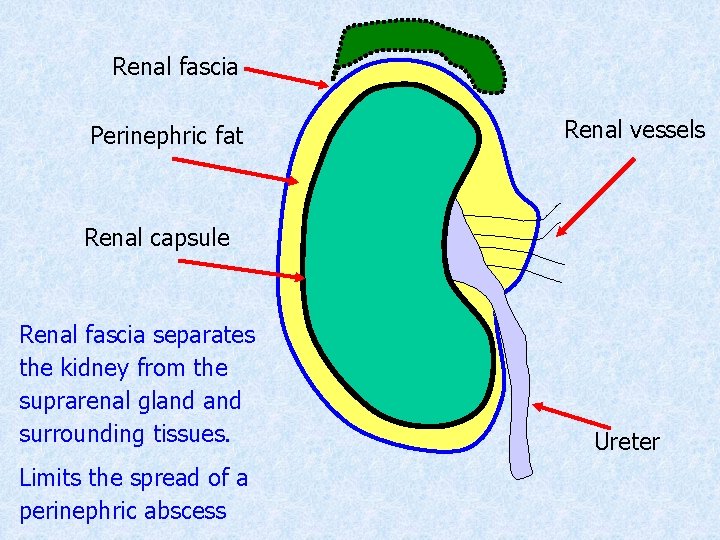
Renal fascia Perinephric fat Renal vessels Renal capsule Renal fascia separates the kidney from the suprarenal gland surrounding tissues. Limits the spread of a perinephric abscess Ureter
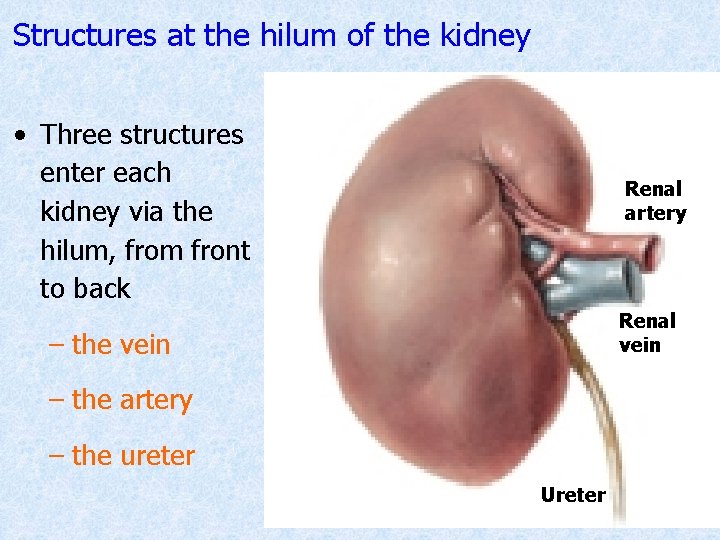
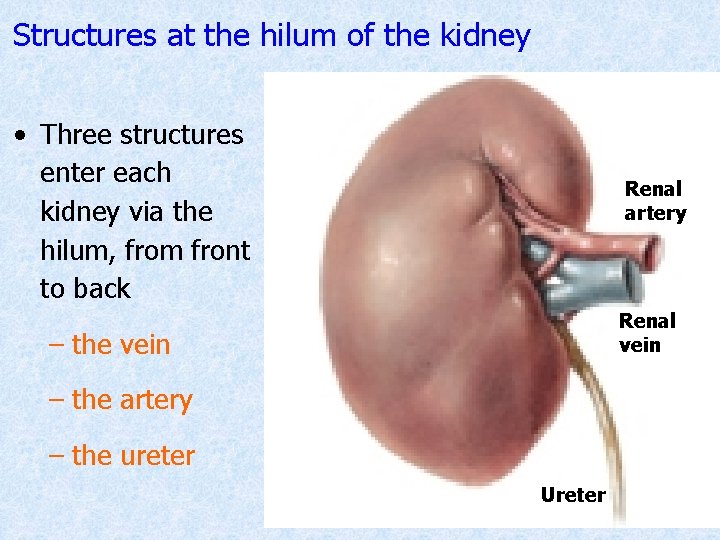
Structures at the hilum of the kidney • Three structures enter each kidney via the hilum, from front to back Renal artery Renal vein – the artery – the ureter Ureter
Functions of the kidney • Filtration • Selective reabsorption • Secretion • Control of renin-angiotensin-aldosterone mechanism • Secretion of erythropoietin • Production of 1, 25 -dihydroxycholecalciferol
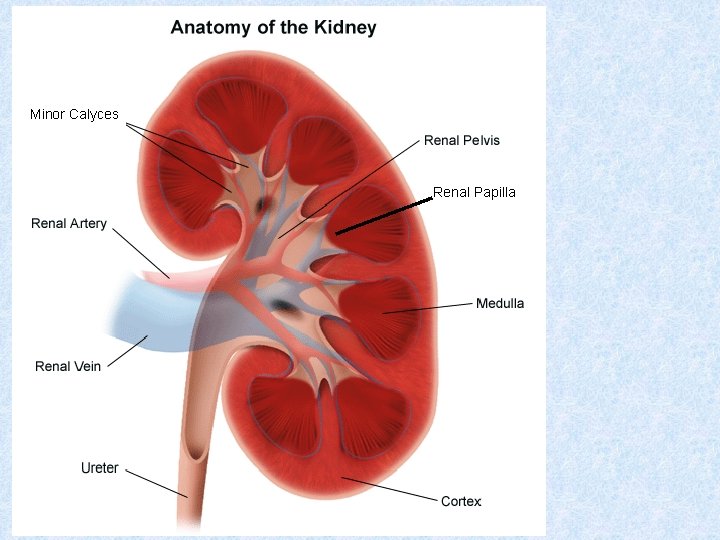
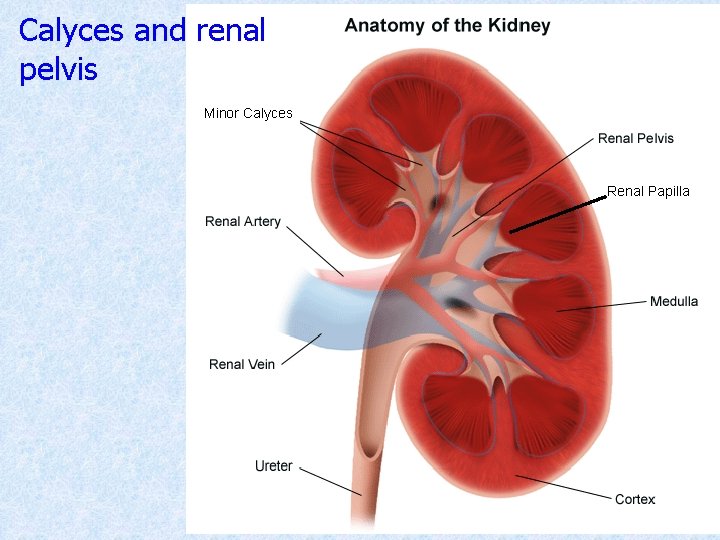
Structure of the kidney • Capsulated • Outer cortex and inner medulla • Medulla is arranged into medullary pyramids • Apices of pyramids are called renal papillae • Papillae project into calyces • Calyces converge to form the renal pelvis
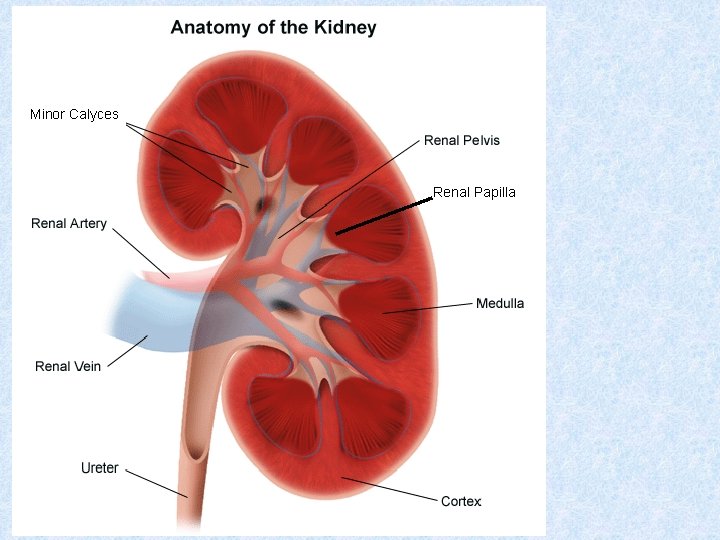
Minor Calyces Renal Papilla
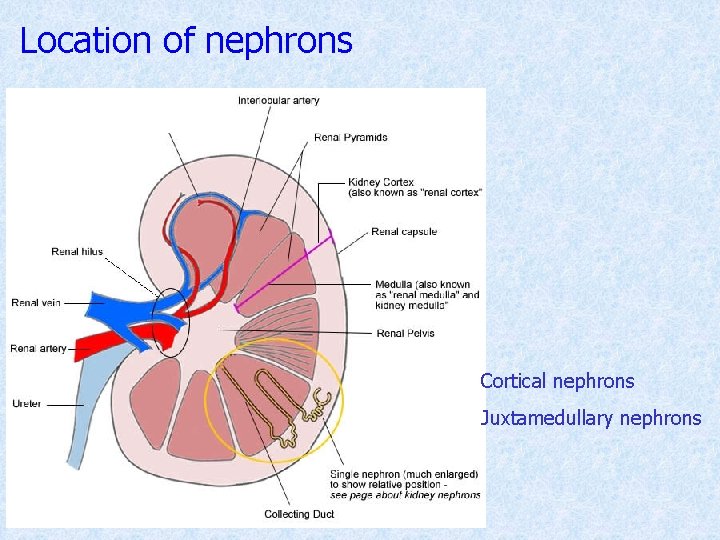
Structure of the kidney… • Functional unit is the nephron • Approximately 1. 3 million nephrons in each kidney • Part of a nephron is in cortex and part in medulla
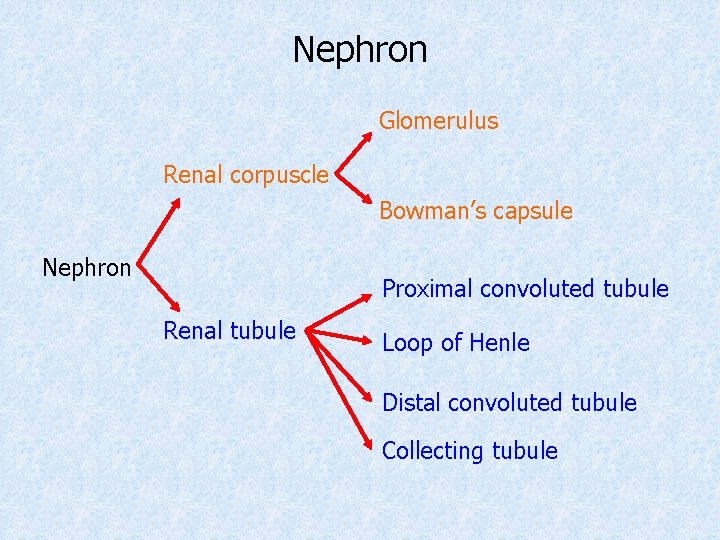
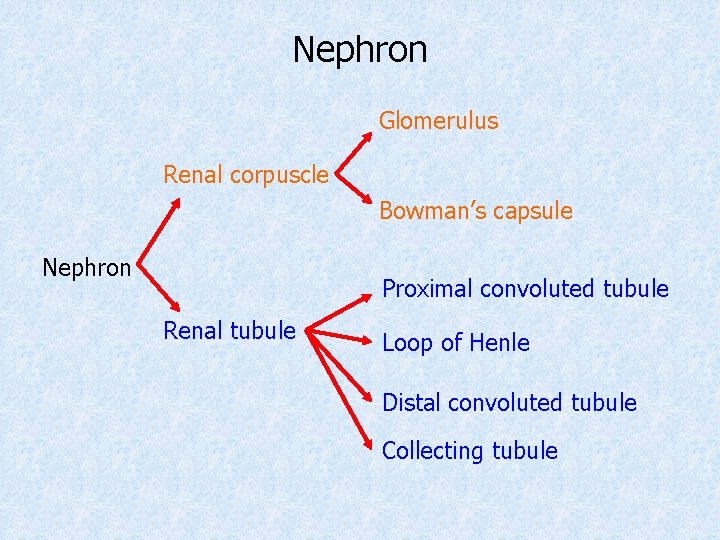
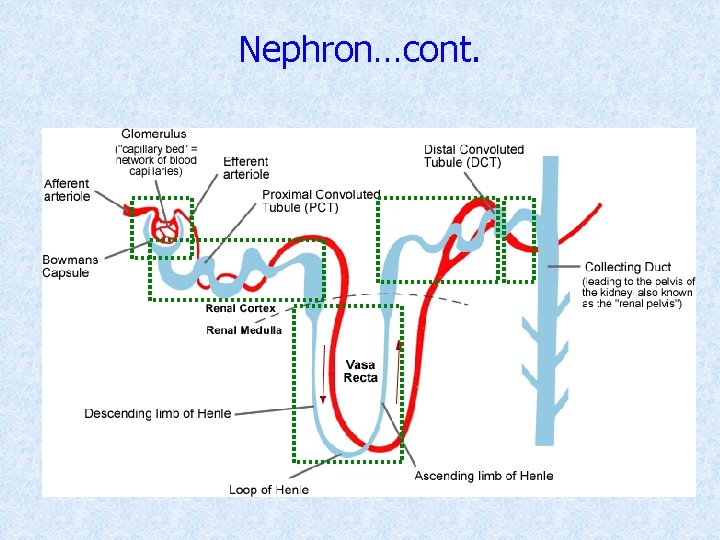
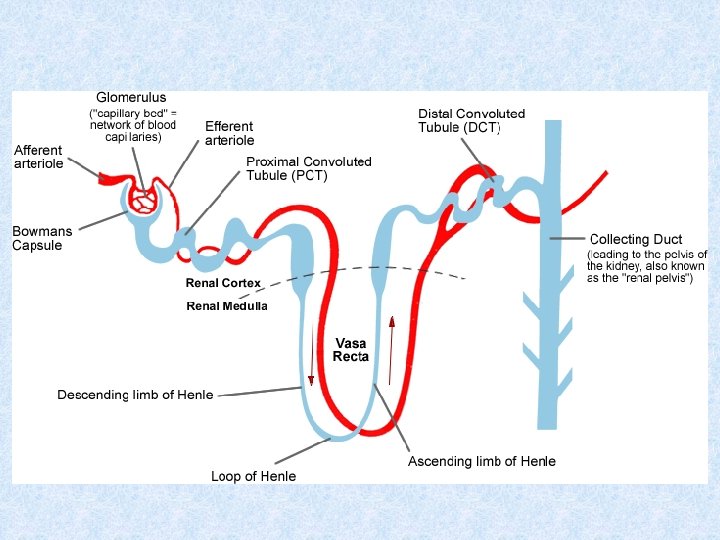
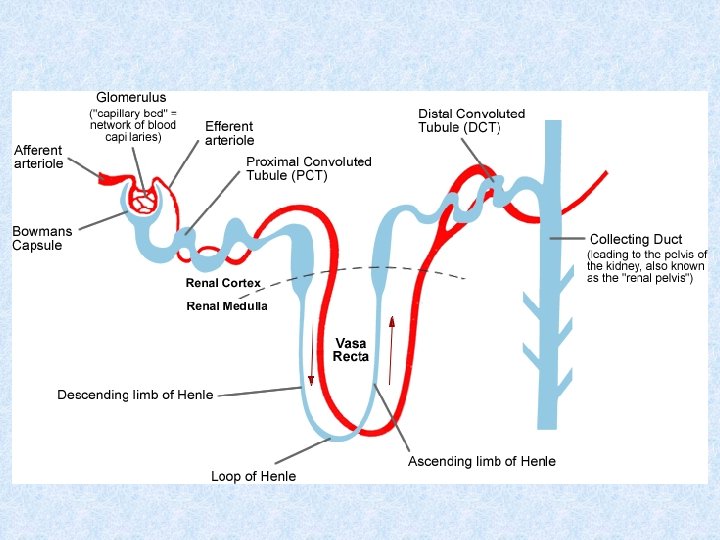
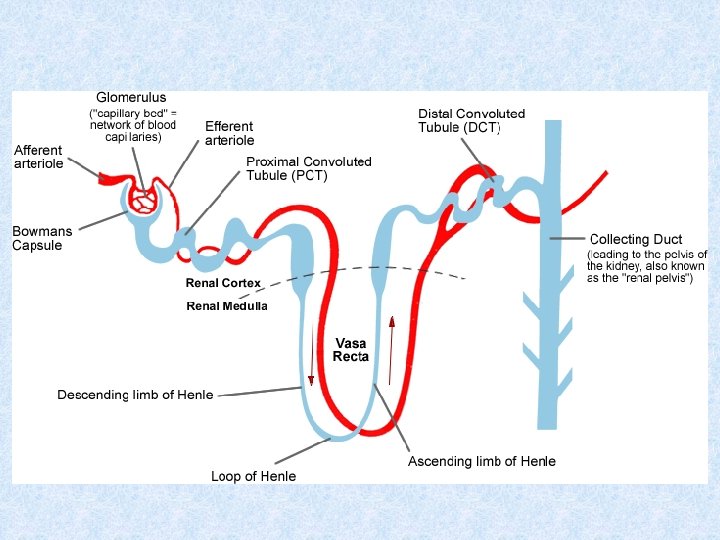
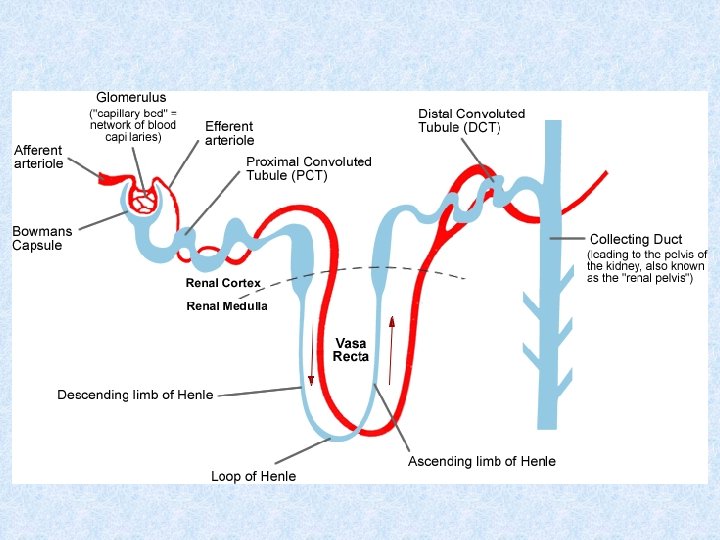
Nephron Glomerulus Renal corpuscle Bowman’s capsule Nephron Proximal convoluted tubule Renal tubule Loop of Henle Distal convoluted tubule Collecting tubule
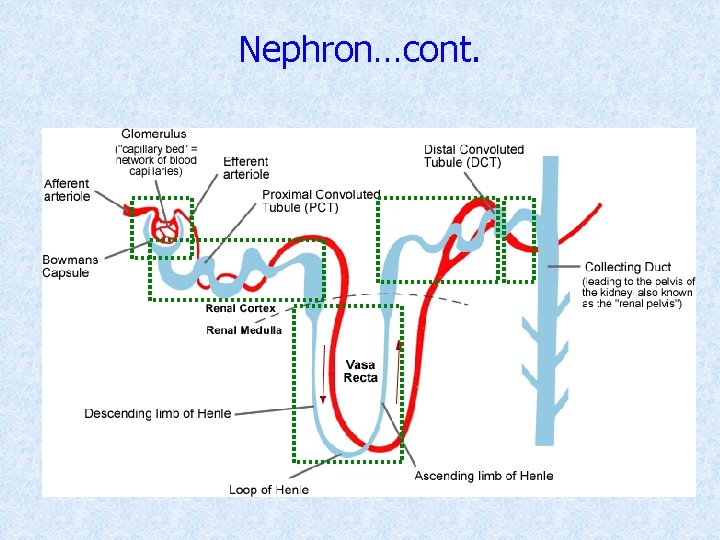
Nephron…cont.
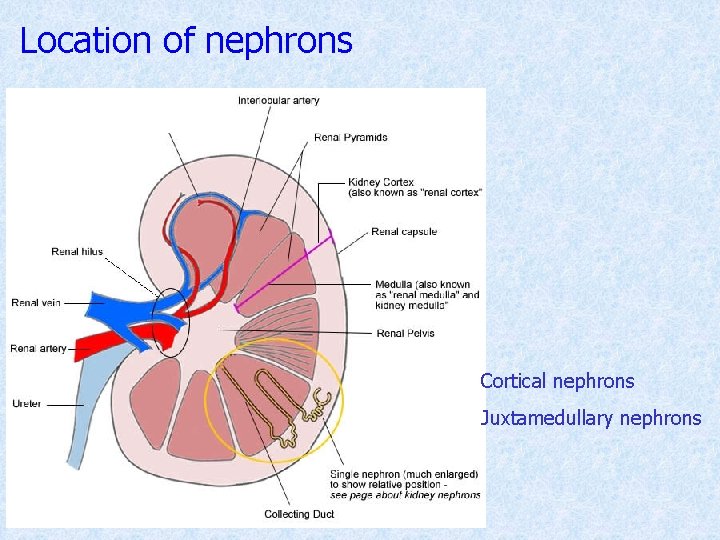
Location of nephrons Cortical nephrons Juxtamedullary nephrons
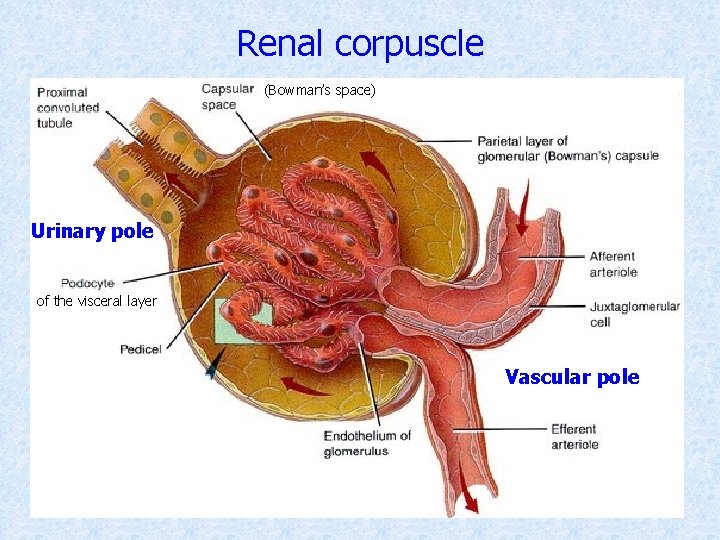
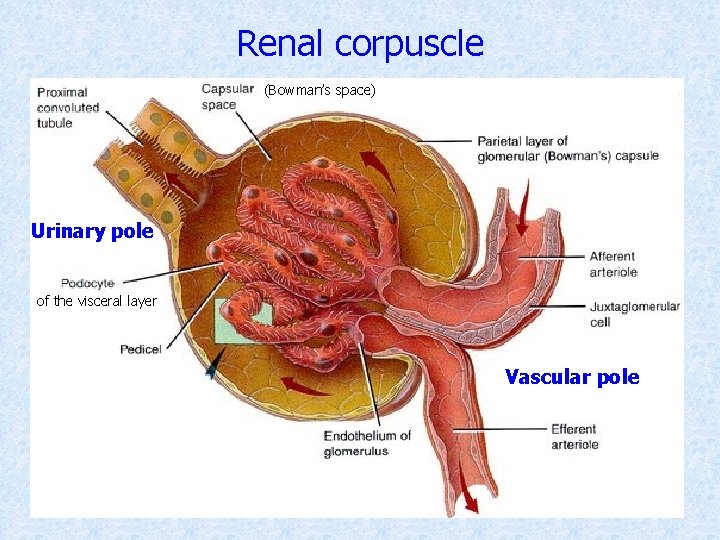
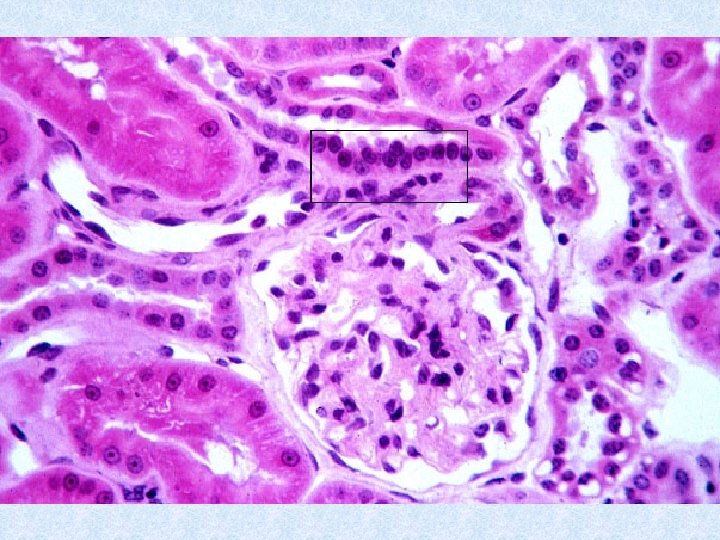
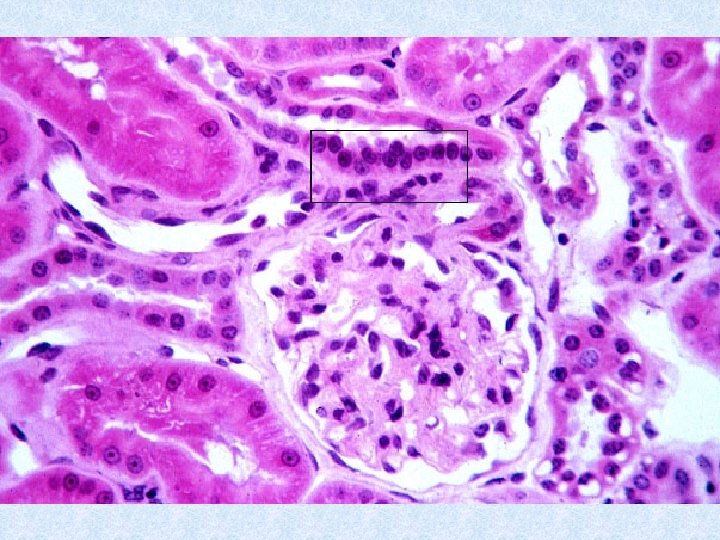
Renal corpuscle (Bowman’s space) Urinary pole of the visceral layer Vascular pole
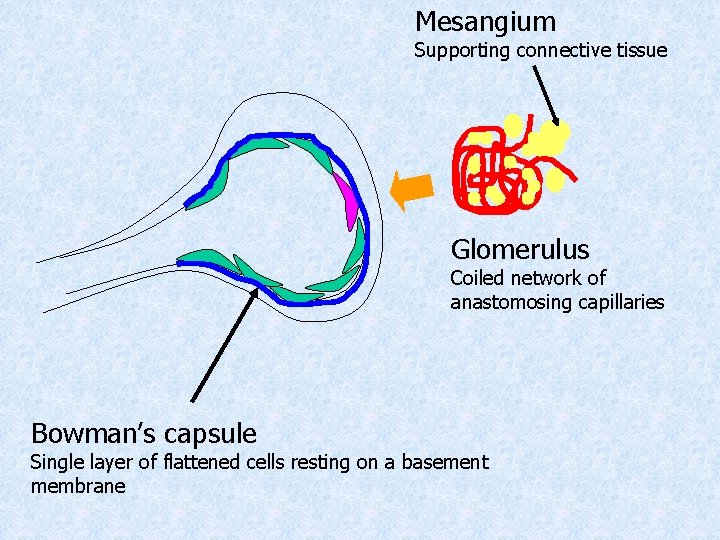
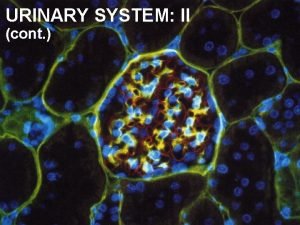
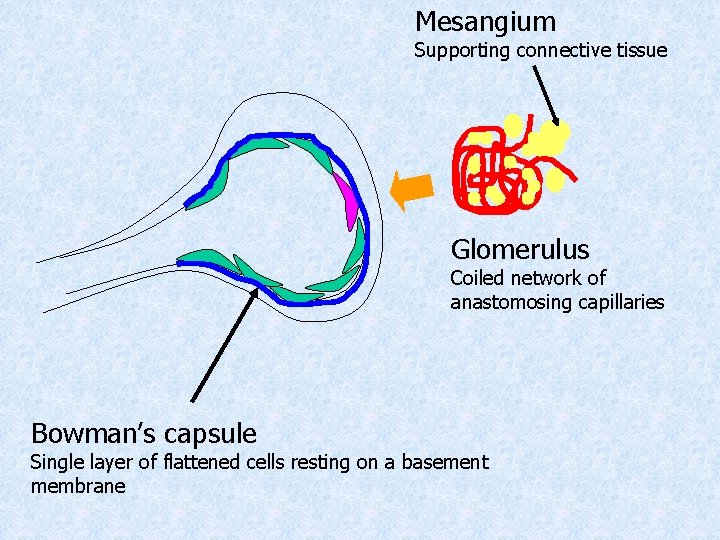
Mesangium Supporting connective tissue Glomerulus Coiled network of anastomosing capillaries Bowman’s capsule Single layer of flattened cells resting on a basement membrane
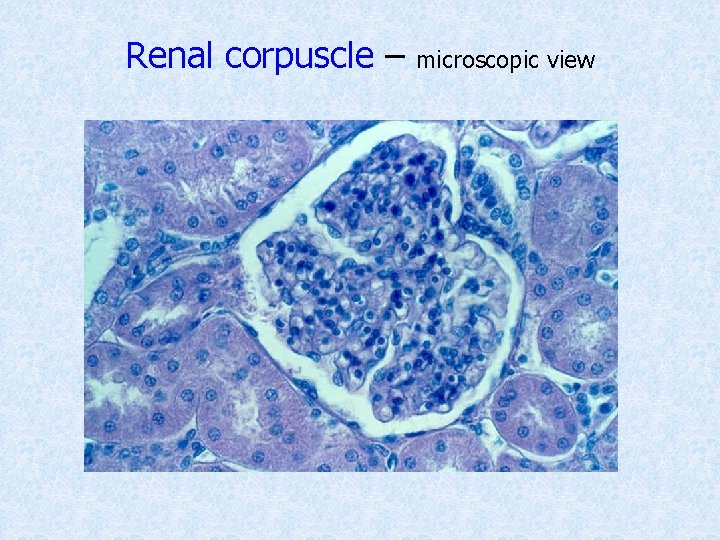
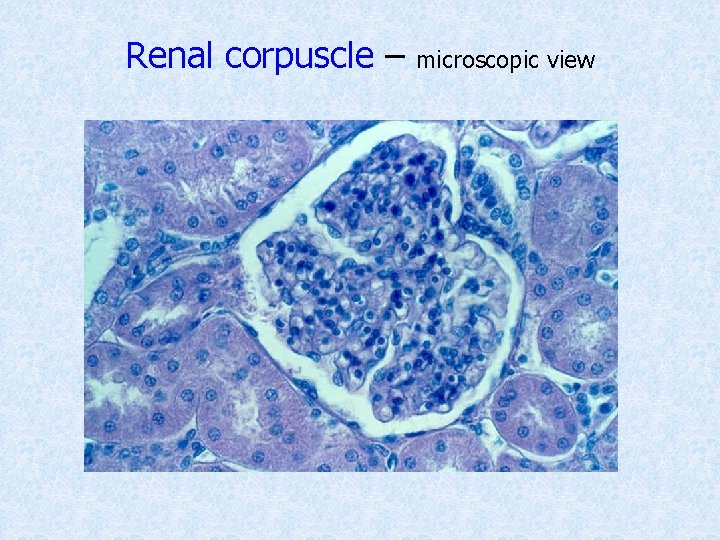
Renal corpuscle – microscopic view
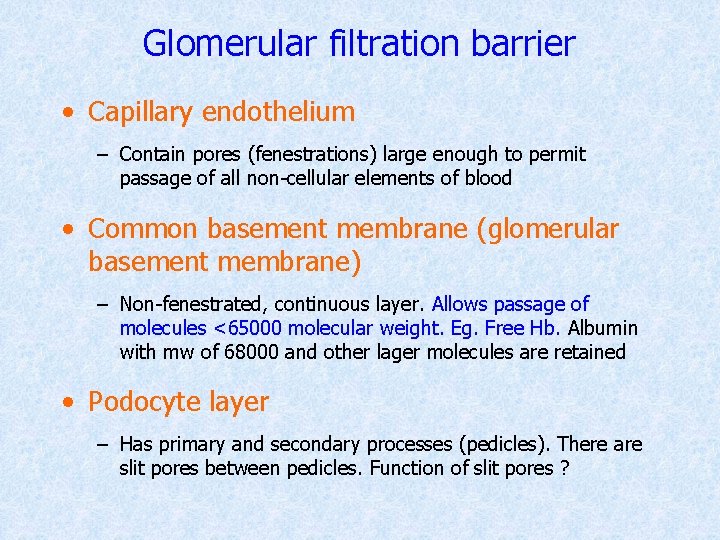
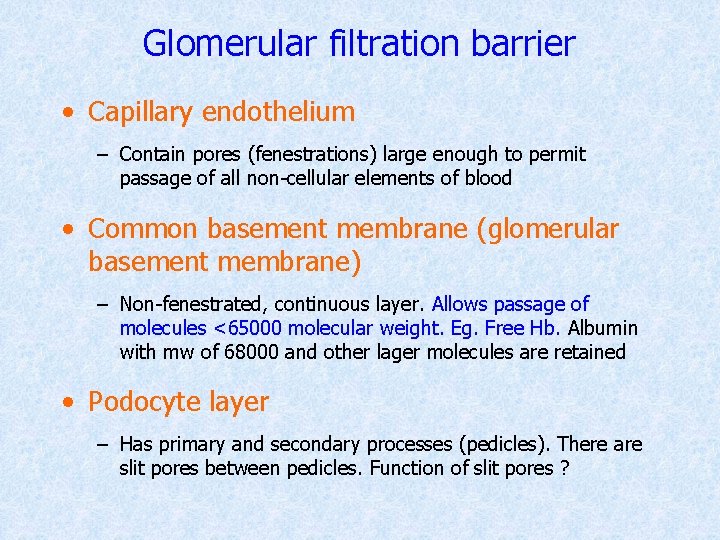
Glomerular filtration barrier • Capillary endothelium – Contain pores (fenestrations) large enough to permit passage of all non-cellular elements of blood • Common basement membrane (glomerular basement membrane) – Non-fenestrated, continuous layer. Allows passage of molecules <65000 molecular weight. Eg. Free Hb. Albumin with mw of 68000 and other lager molecules are retained • Podocyte layer – Has primary and secondary processes (pedicles). There are slit pores between pedicles. Function of slit pores ?
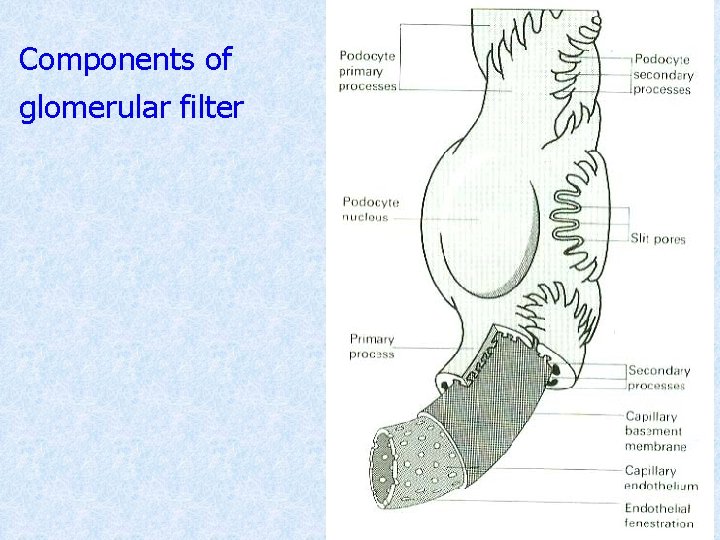
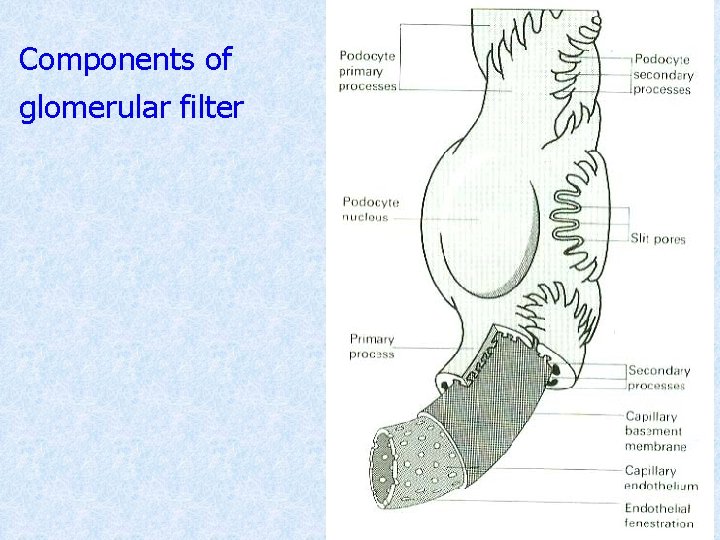
Components of glomerular filter
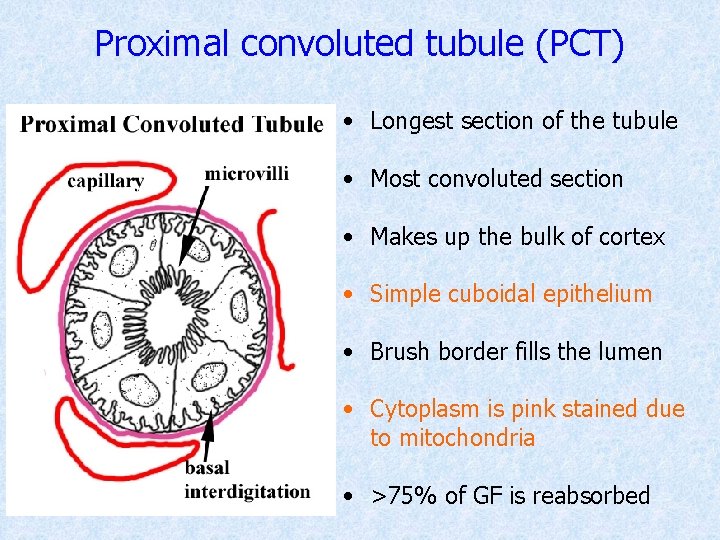
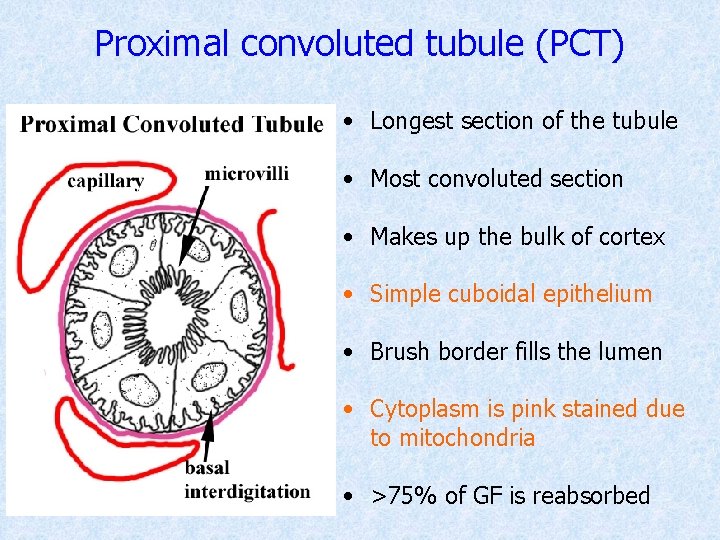
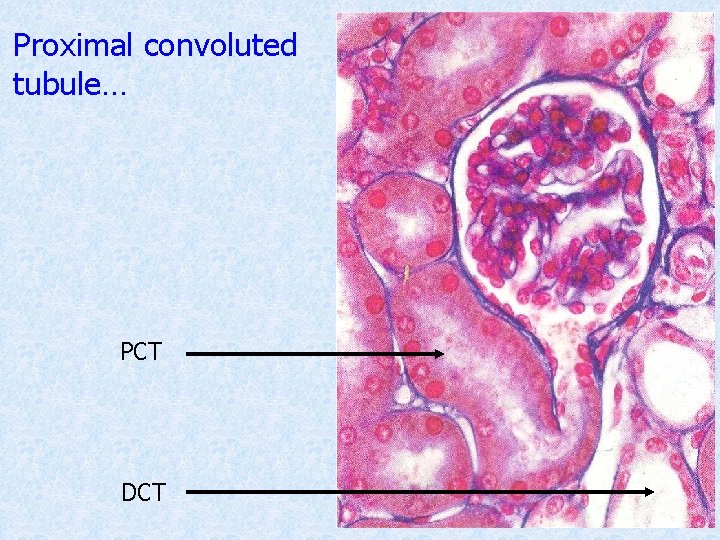
Proximal convoluted tubule (PCT) • Longest section of the tubule • Most convoluted section • Makes up the bulk of cortex • Simple cuboidal epithelium • Brush border fills the lumen • Cytoplasm is pink stained due to mitochondria • >75% of GF is reabsorbed
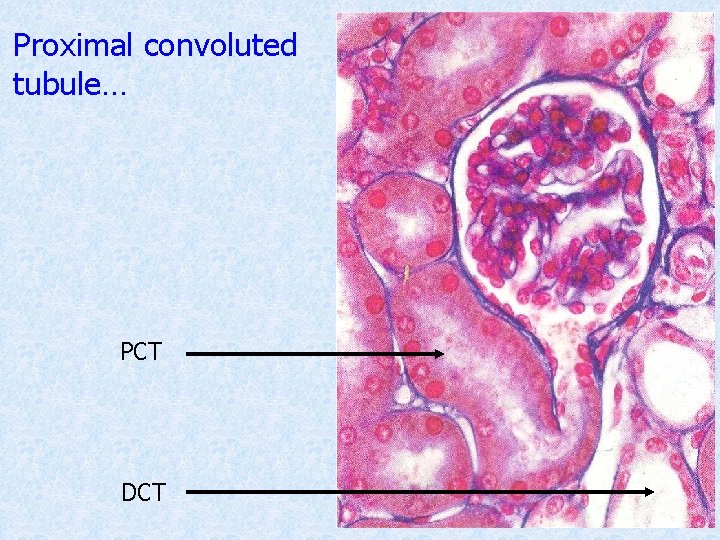
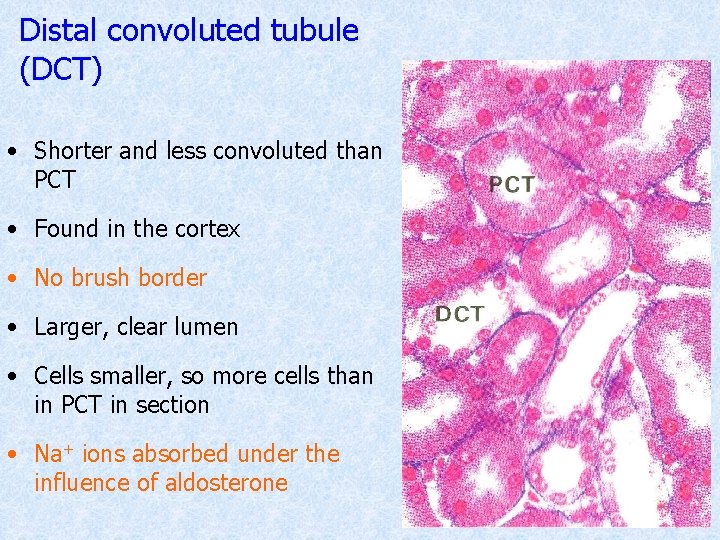
Proximal convoluted tubule… PCT DCT
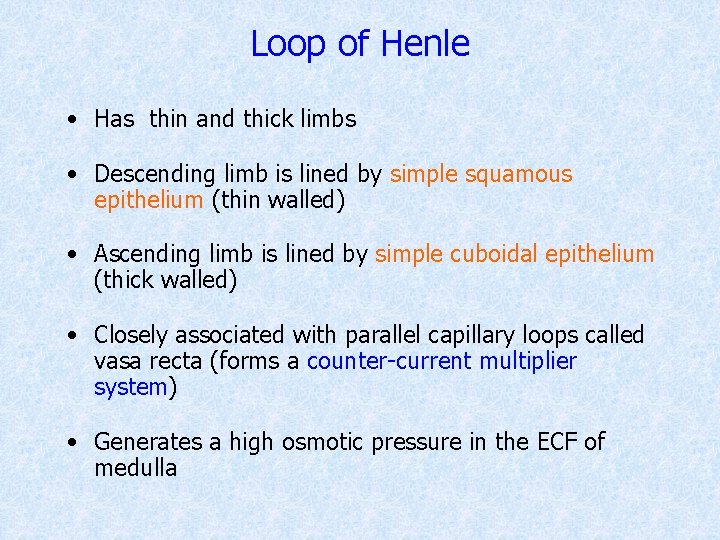
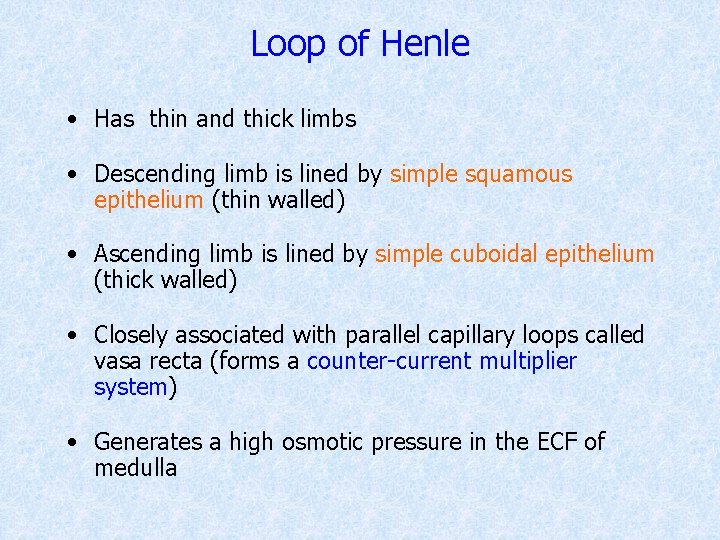
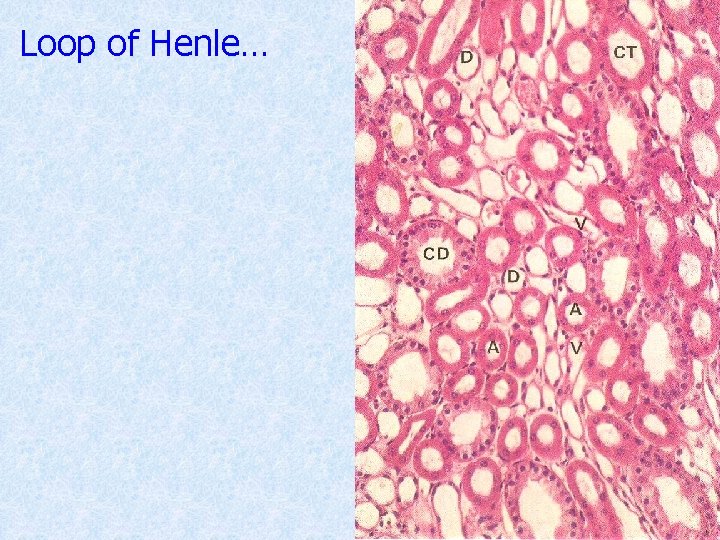
Loop of Henle • Has thin and thick limbs • Descending limb is lined by simple squamous epithelium (thin walled) • Ascending limb is lined by simple cuboidal epithelium (thick walled) • Closely associated with parallel capillary loops called vasa recta (forms a counter-current multiplier system) • Generates a high osmotic pressure in the ECF of medulla
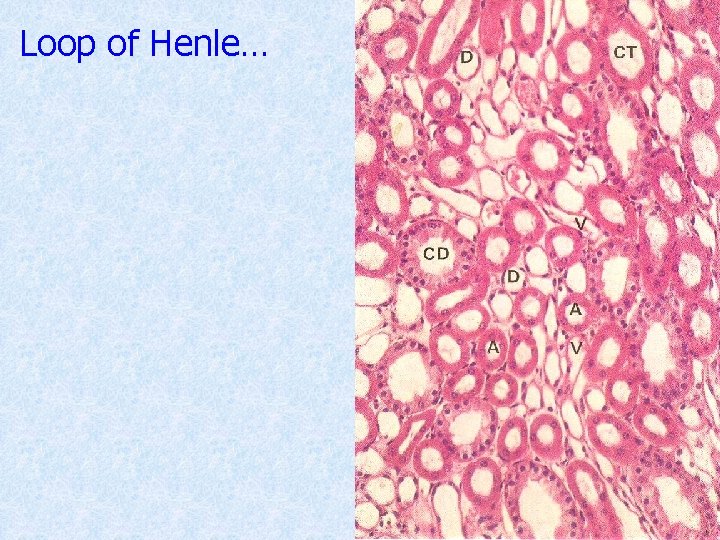
Loop of Henle…
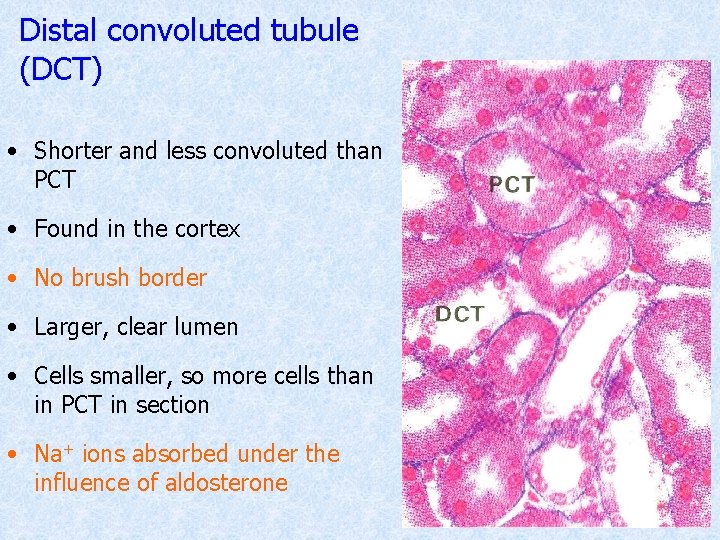
Distal convoluted tubule (DCT) • Shorter and less convoluted than PCT • Found in the cortex • No brush border • Larger, clear lumen • Cells smaller, so more cells than in PCT in section • Na+ ions absorbed under the influence of aldosterone
Collecting tubule • This is the terminal part of the DCT • Opens into collecting ducts • Together with collecting ducts form ‘medullary rays’ • Collecting tubules and ducts are not normally permeable to water • Becomes permeable to water in the presence of ADH • Site of reabsorption of water
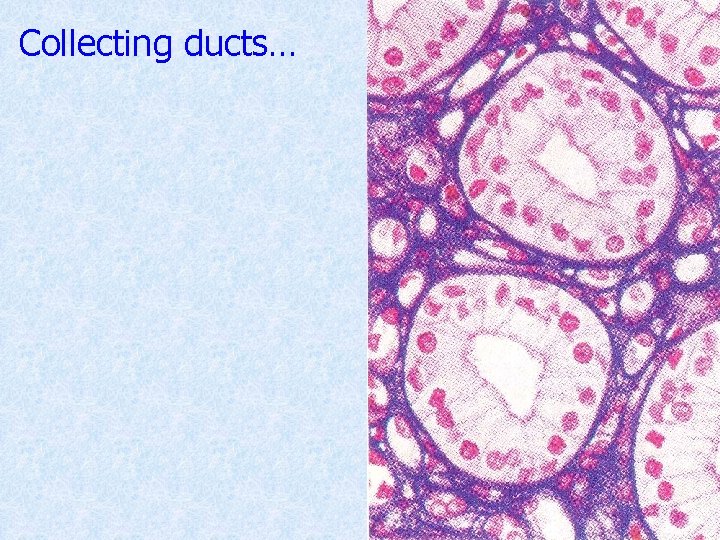
Collecting ducts • Formed by fusion of collecting tubules • They fuse with adjacent ducts and form larger ducts called ducts of Bellini • Ducts of Bellini convey urine into the calyceal space through renal papillae • Lined by tall, pale stained columnar cells • No brush border • Water reabsorption under ADH control
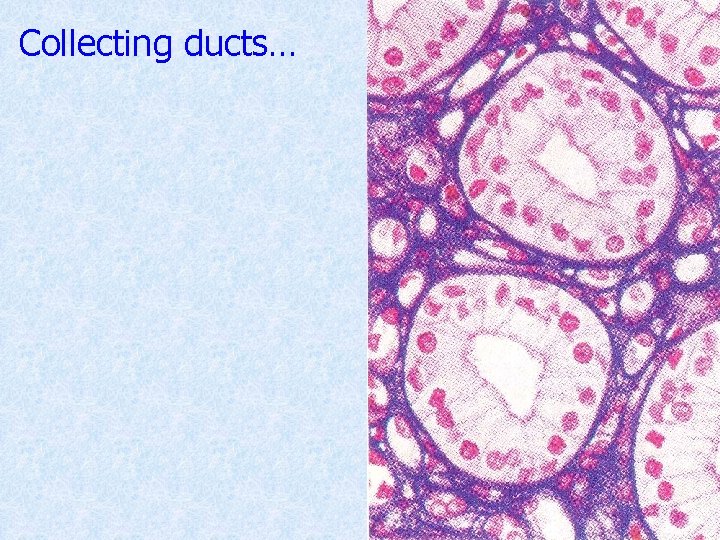
Collecting ducts…
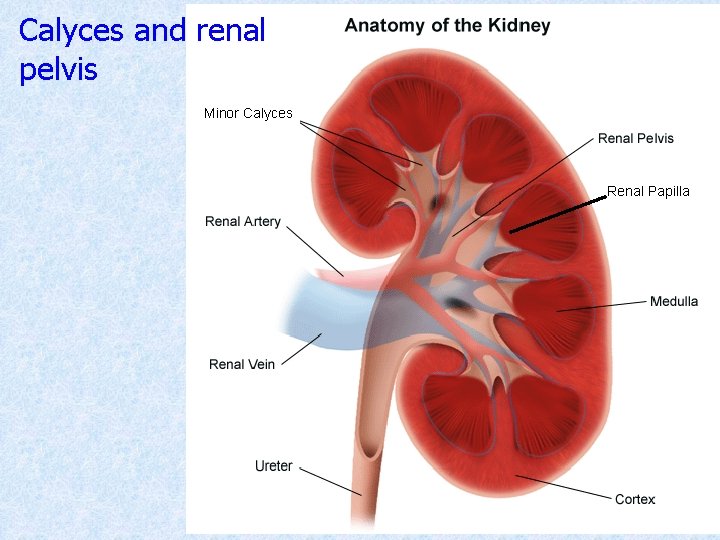
Calyces and renal pelvis Minor Calyces Renal Papilla
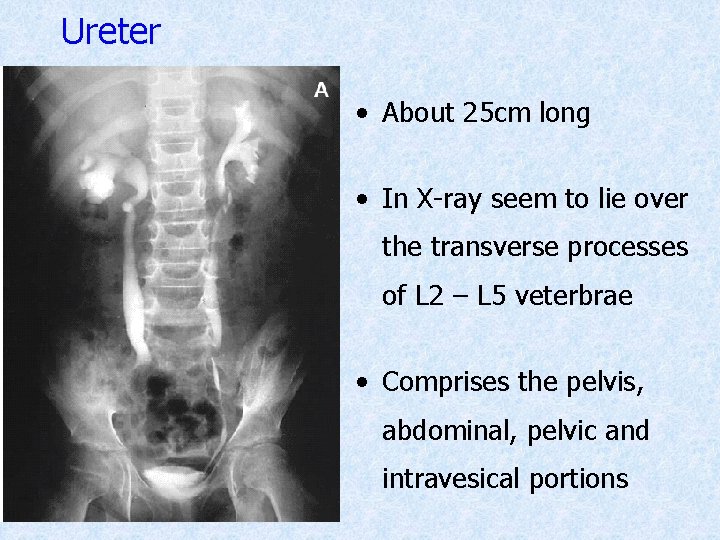
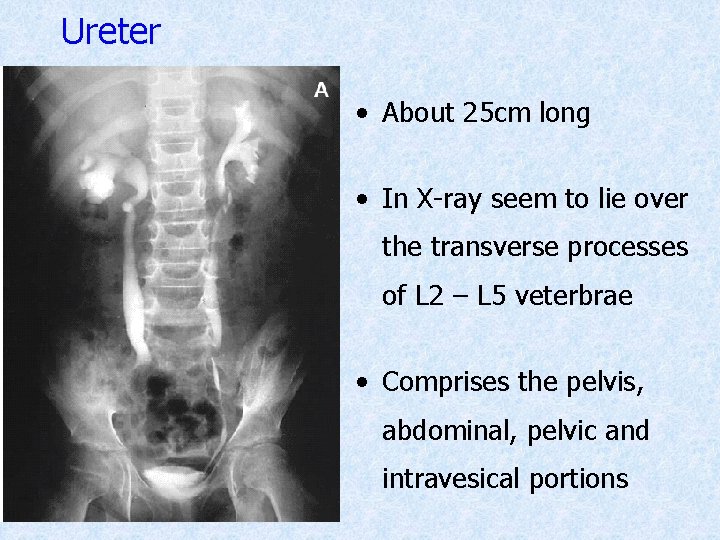
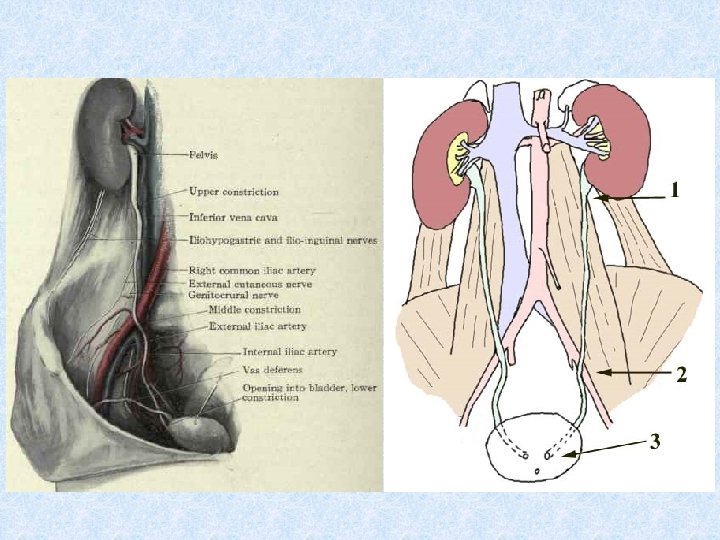
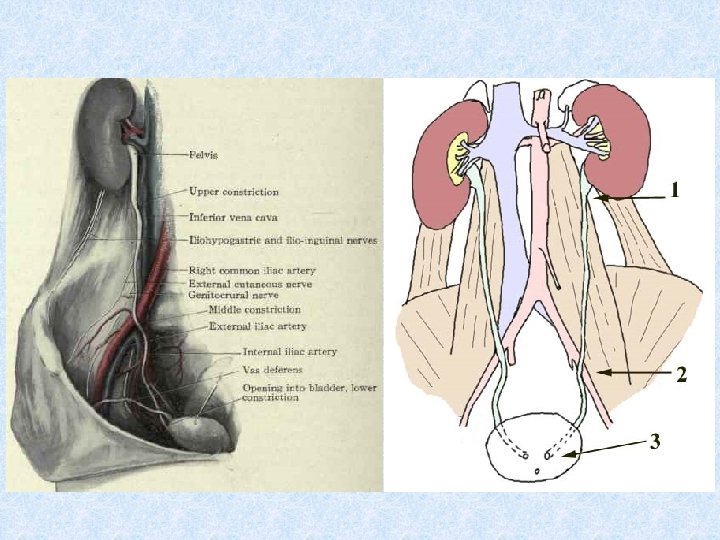
Ureter • About 25 cm long • In X-ray seem to lie over the transverse processes of L 2 – L 5 veterbrae • Comprises the pelvis, abdominal, pelvic and intravesical portions
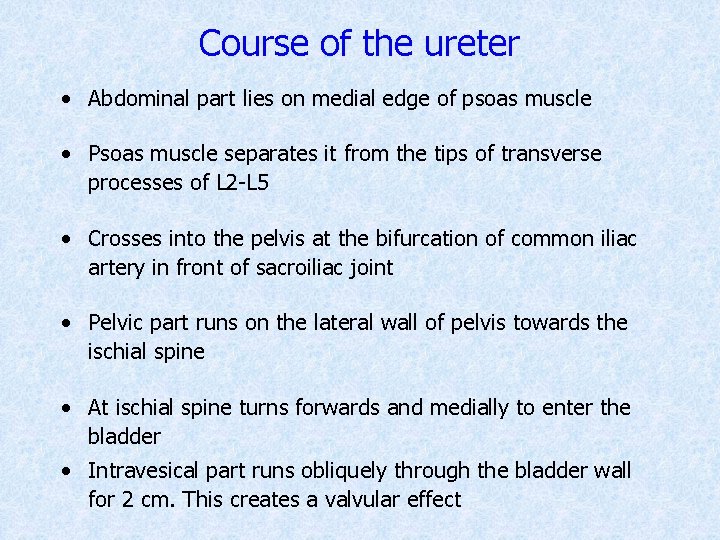
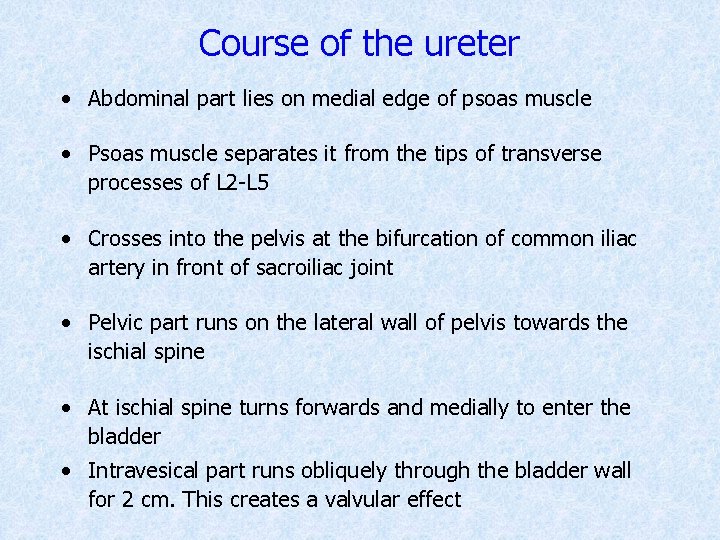
Course of the ureter • Abdominal part lies on medial edge of psoas muscle • Psoas muscle separates it from the tips of transverse processes of L 2 -L 5 • Crosses into the pelvis at the bifurcation of common iliac artery in front of sacroiliac joint • Pelvic part runs on the lateral wall of pelvis towards the ischial spine • At ischial spine turns forwards and medially to enter the bladder • Intravesical part runs obliquely through the bladder wall for 2 cm. This creates a valvular effect
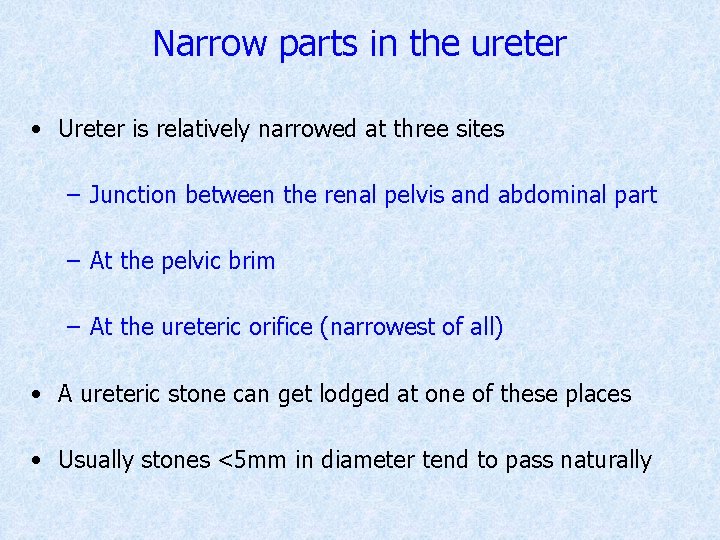
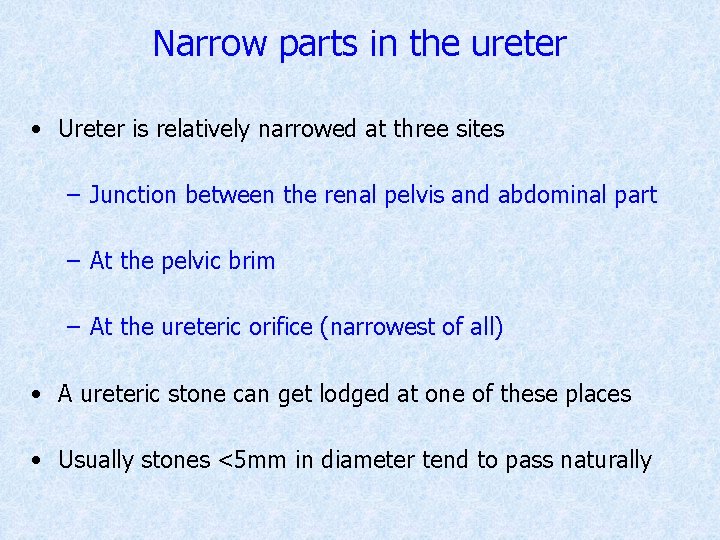
Narrow parts in the ureter • Ureter is relatively narrowed at three sites – Junction between the renal pelvis and abdominal part – At the pelvic brim – At the ureteric orifice (narrowest of all) • A ureteric stone can get lodged at one of these places • Usually stones <5 mm in diameter tend to pass naturally
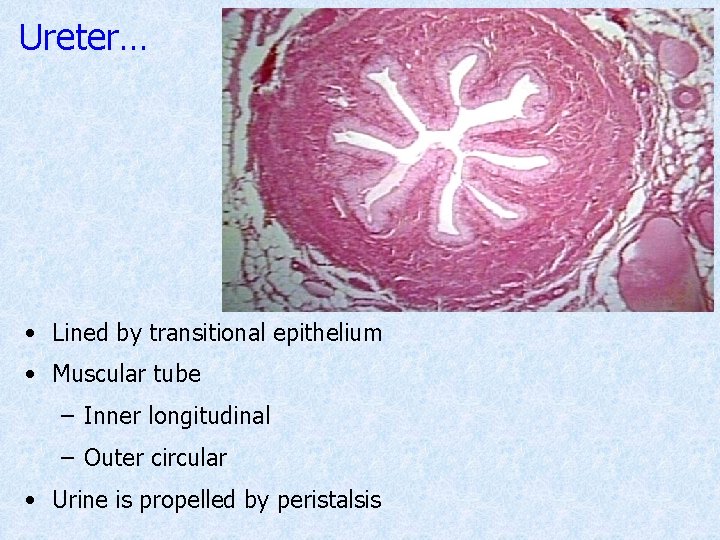
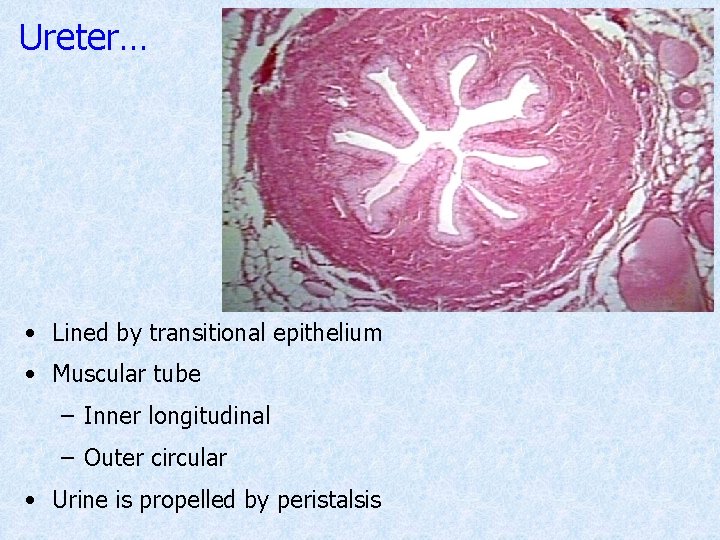
Ureter… • Lined by transitional epithelium • Muscular tube – Inner longitudinal – Outer circular • Urine is propelled by peristalsis
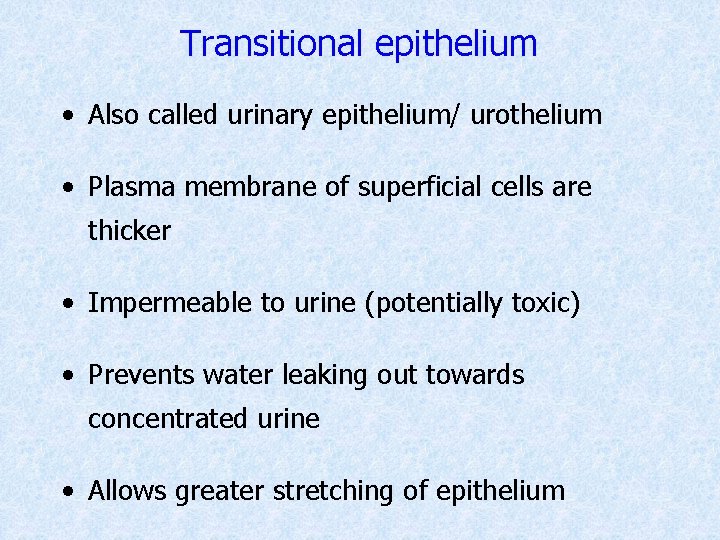
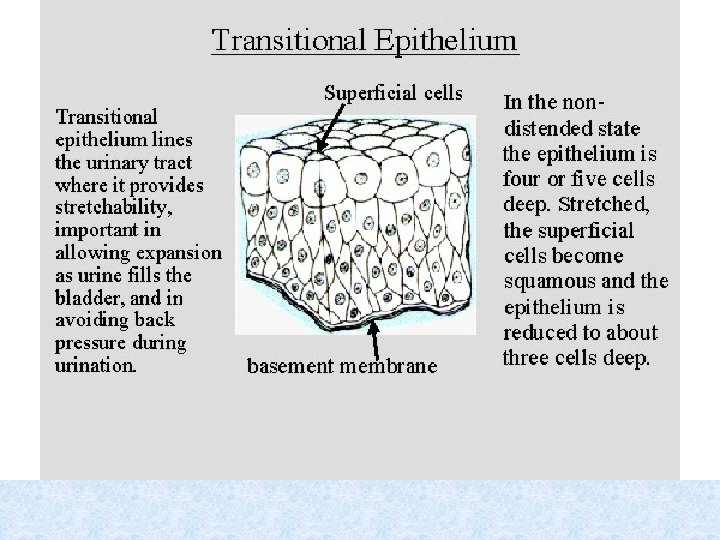
Transitional epithelium • Also called urinary epithelium/ urothelium • Plasma membrane of superficial cells are thicker • Impermeable to urine (potentially toxic) • Prevents water leaking out towards concentrated urine • Allows greater stretching of epithelium

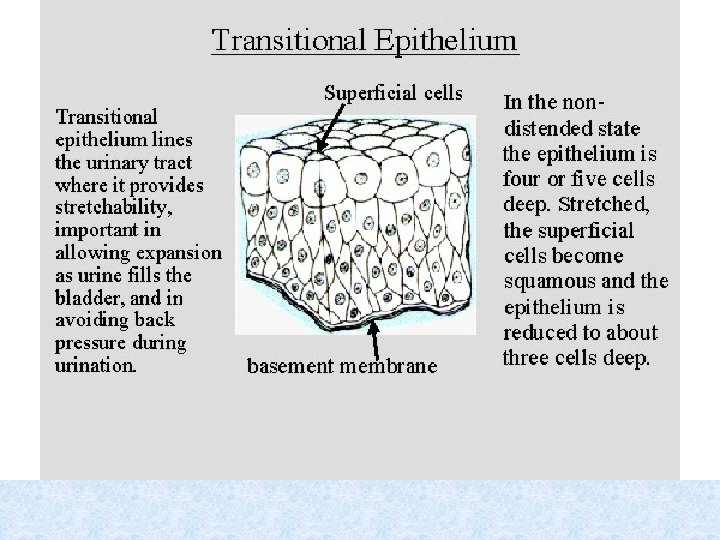
Transitional epithelium…

Bladder • Lined by transitional epithelium • Wall has three smooth muscle layers (Detrusor muscle)
Urethra • In males, has three parts – Prostatic urethra – Membranous urethra – Spongy urethra (penile urethra) • Prostatic urethra is lined by urinary epithelium • Urethral meatus is lined by stratified squamous epithelium • Other parts are lined by stratified or pseudostratified columnar epithelium • External orifice is the narrowest part
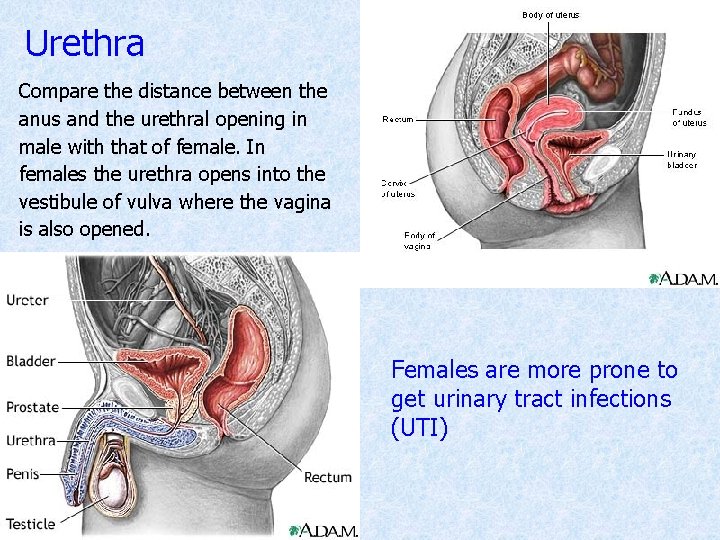
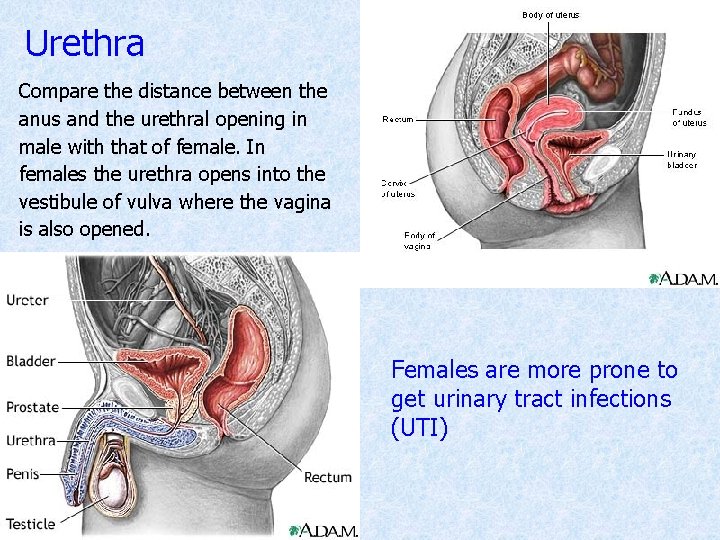
Urethra Compare the distance between the anus and the urethral opening in male with that of female. In females the urethra opens into the vestibule of vulva where the vagina is also opened. Females are more prone to get urinary tract infections (UTI)
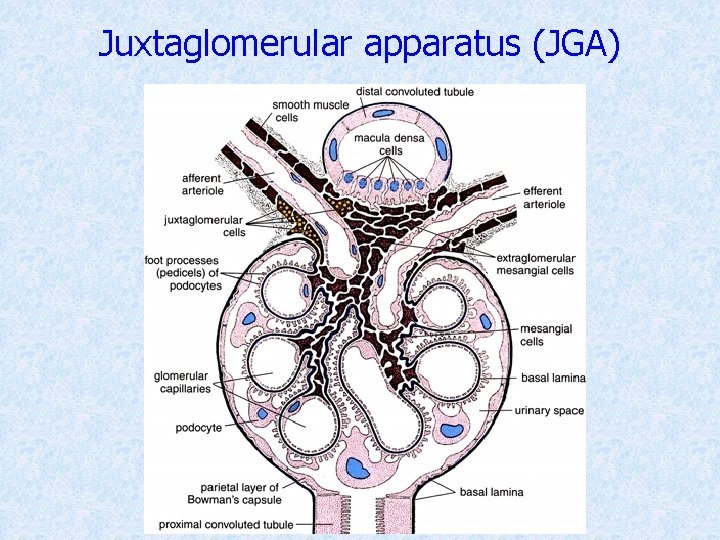
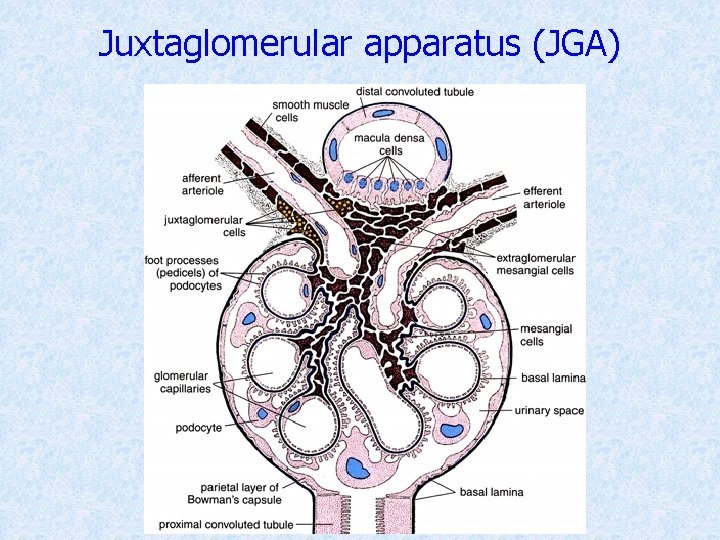
Juxtaglomerular apparatus (JGA)
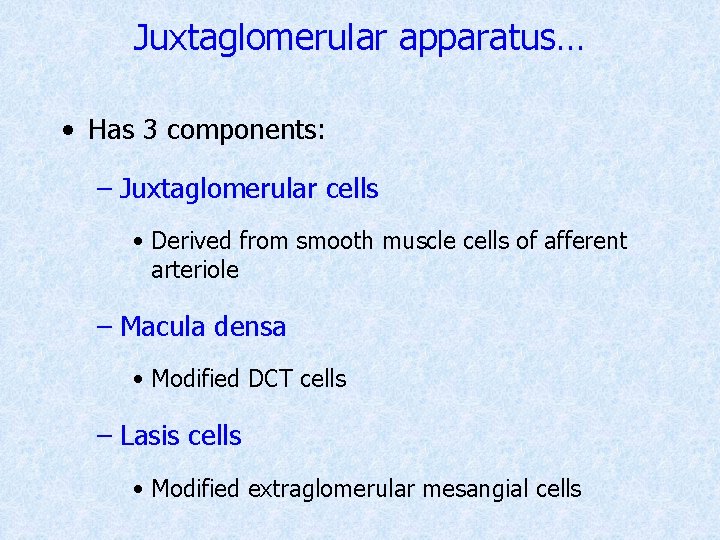
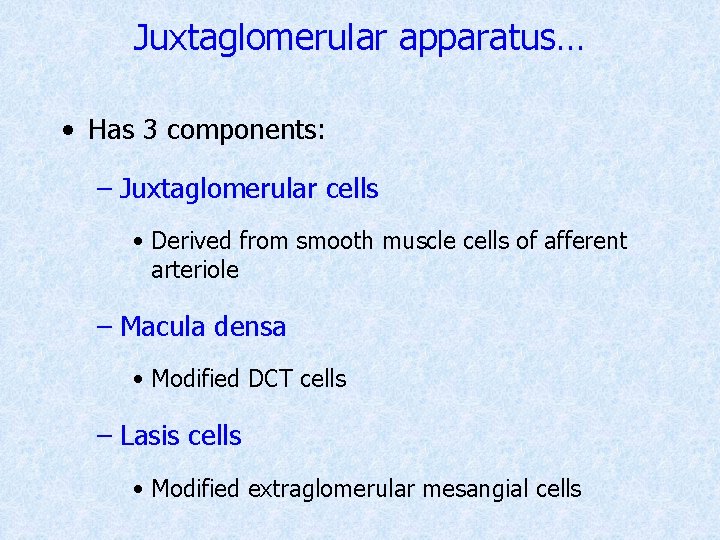
Juxtaglomerular apparatus… • Has 3 components: – Juxtaglomerular cells • Derived from smooth muscle cells of afferent arteriole – Macula densa • Modified DCT cells – Lasis cells • Modified extraglomerular mesangial cells
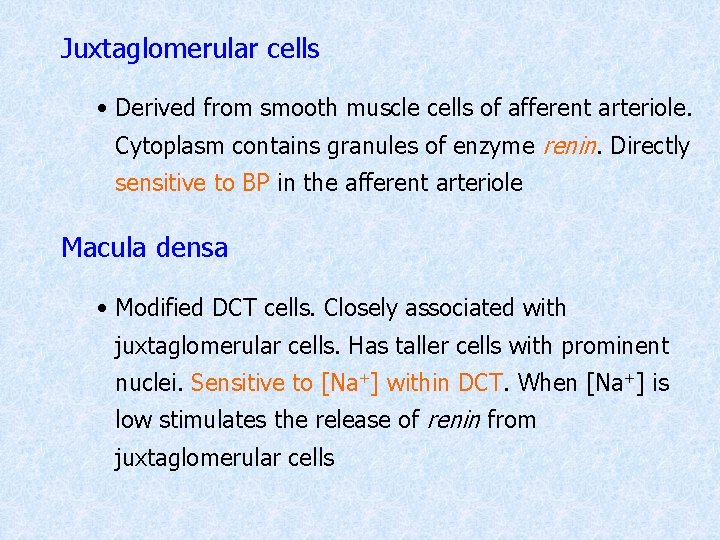
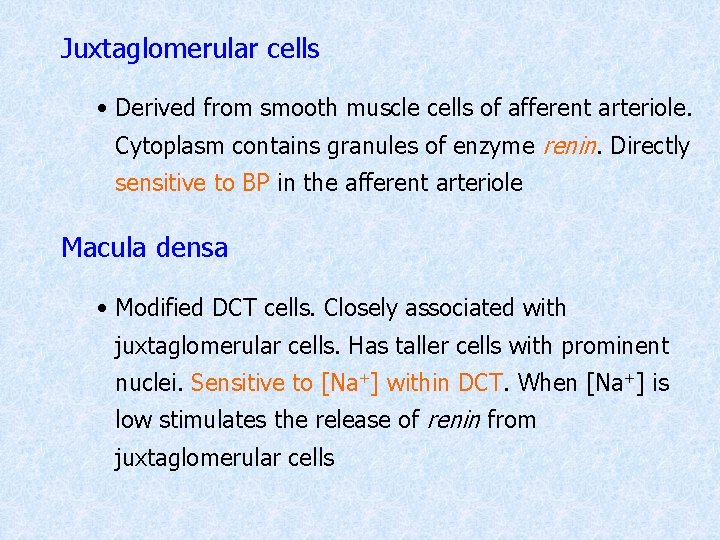
Juxtaglomerular cells • Derived from smooth muscle cells of afferent arteriole. Cytoplasm contains granules of enzyme renin. Directly sensitive to BP in the afferent arteriole Macula densa • Modified DCT cells. Closely associated with juxtaglomerular cells. Has taller cells with prominent nuclei. Sensitive to [Na+] within DCT. When [Na+] is low stimulates the release of renin from juxtaglomerular cells
Lasis cells • Modified extraglomerular mesangial cells. Lie between macula densa and Bowman’s capsule. Produce the hormone erythropoietin
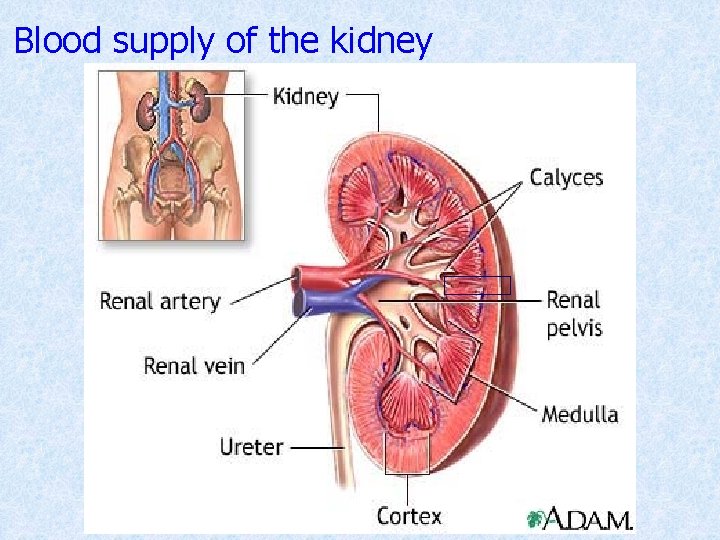
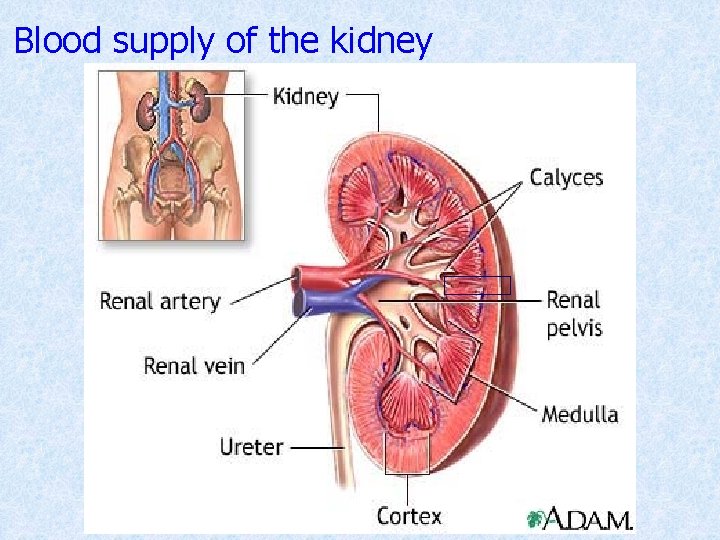
Blood supply of the kidney
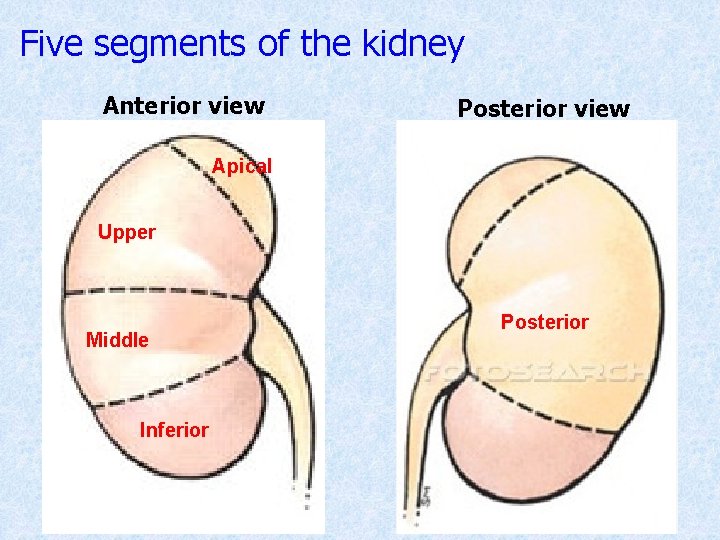
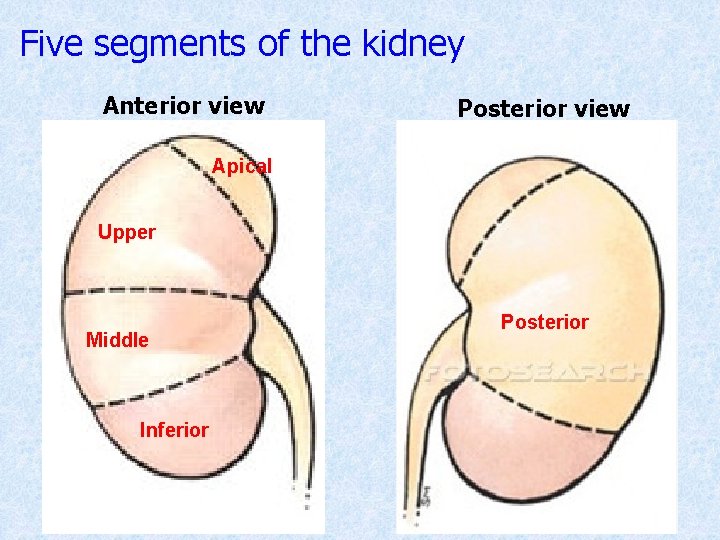
Five segments of the kidney Anterior view Posterior view Apical Upper Middle Inferior Posterior
q q They are supplied by five segmental branches of the renal artery. In the region of the hilum, the artery divides into anterior and posterior branches The posterior branch supplies the posterior segment of the kidney. The anterior branch further divides into four branches and supply the remaining 4 segments
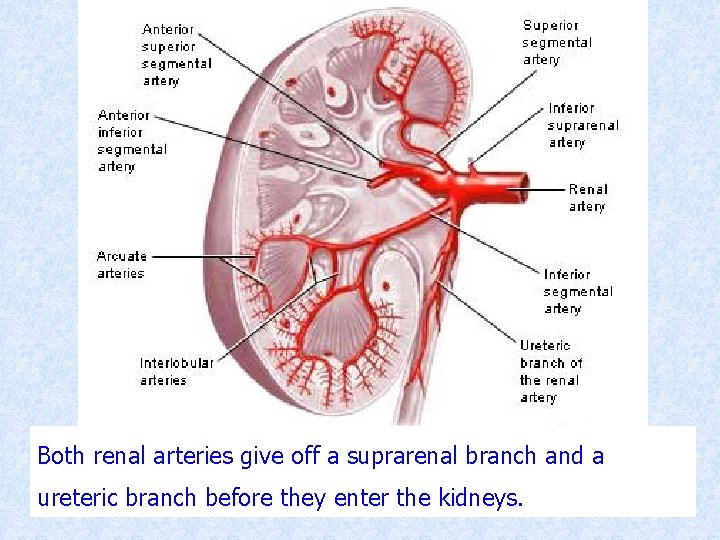
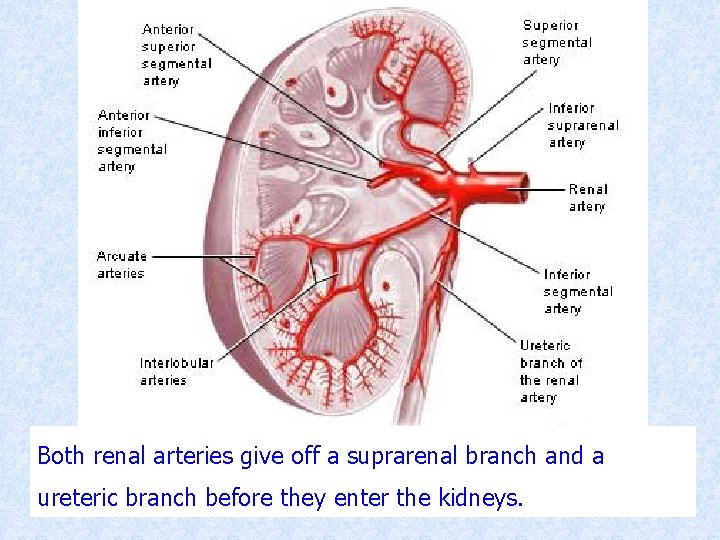
Both renal arteries give off a suprarenal branch and a ureteric branch before they enter the kidneys.
q The pattern of branching of vessels may vary, but always five segmental arteries are present. q Branches of renal arteries do not have collateral circulations between them.
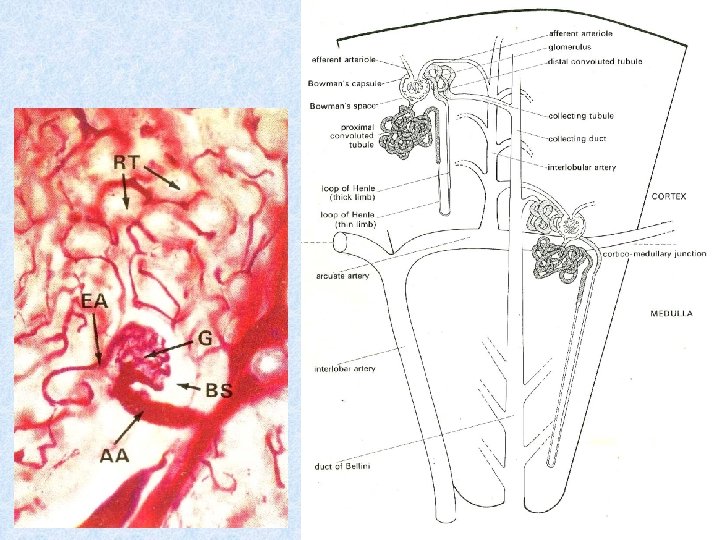
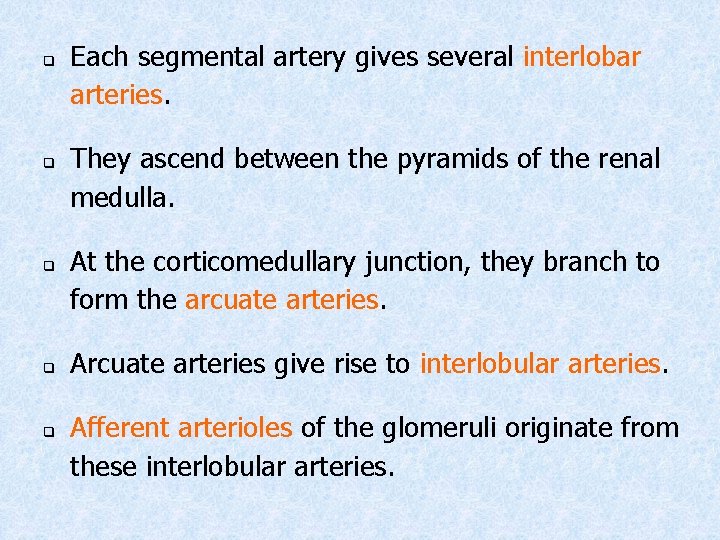
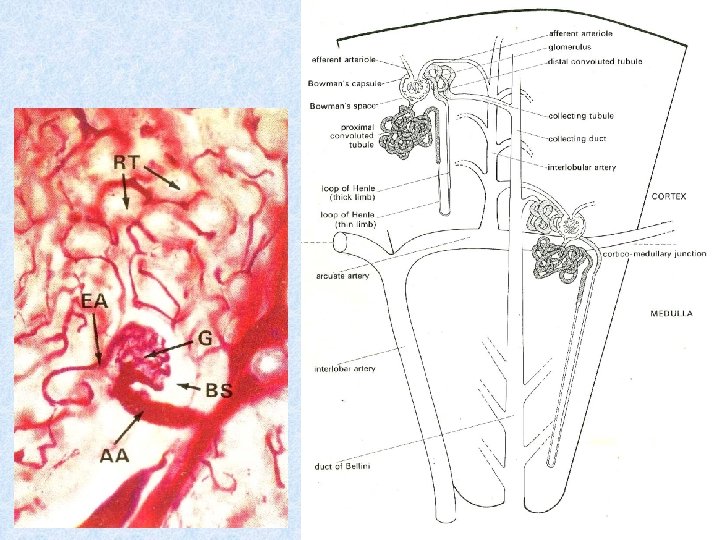
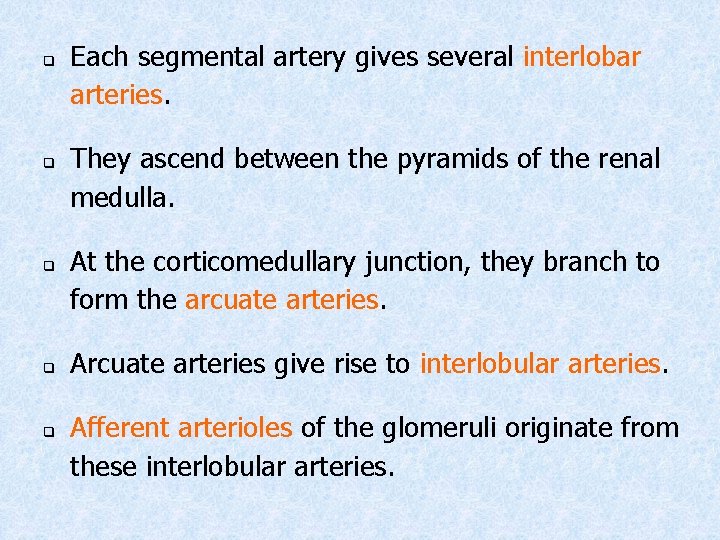
q q q Each segmental artery gives several interlobar arteries. They ascend between the pyramids of the renal medulla. At the corticomedullary junction, they branch to form the arcuate arteries. Arcuate arteries give rise to interlobular arteries. Afferent arterioles of the glomeruli originate from these interlobular arteries.
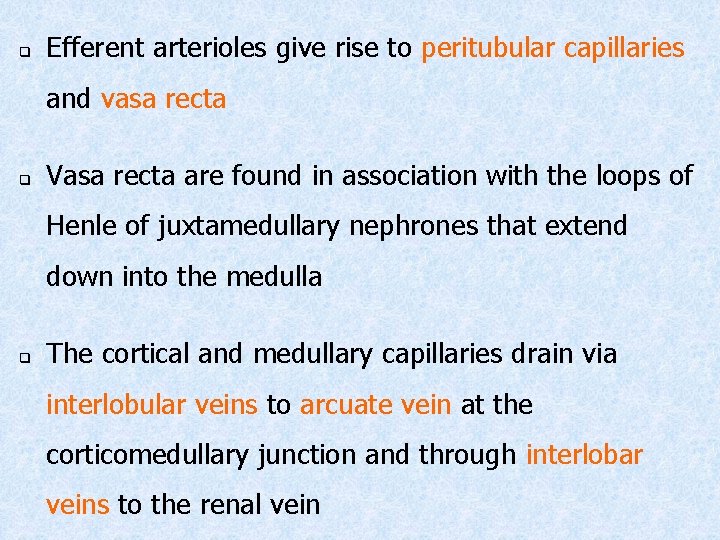
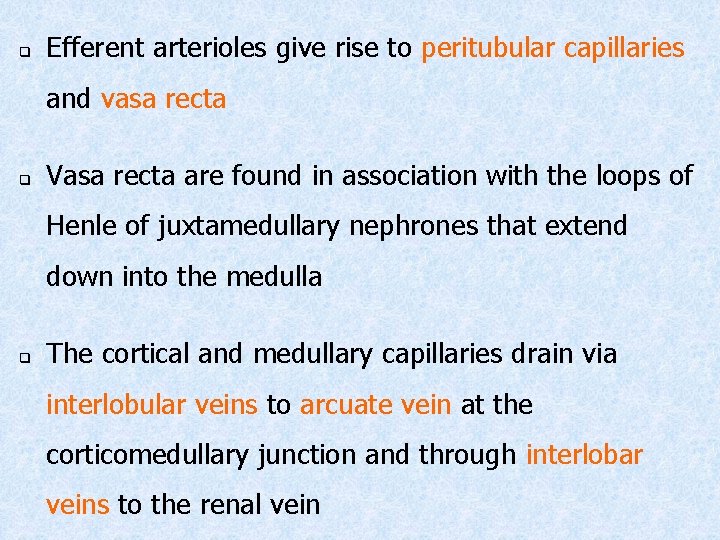
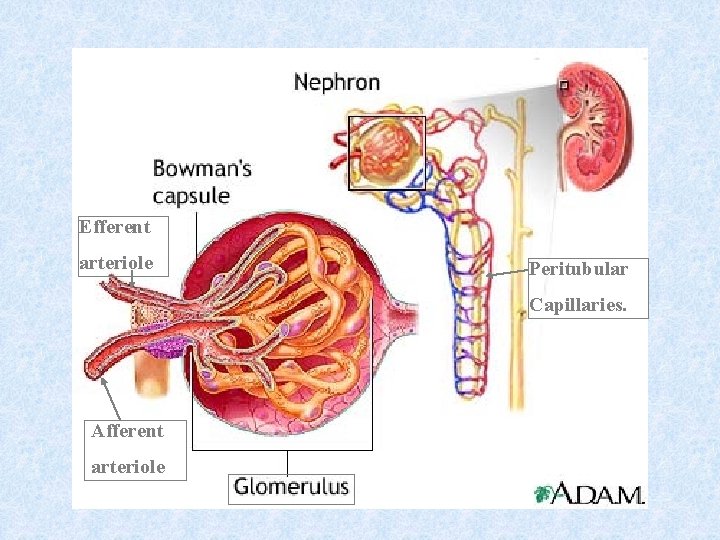
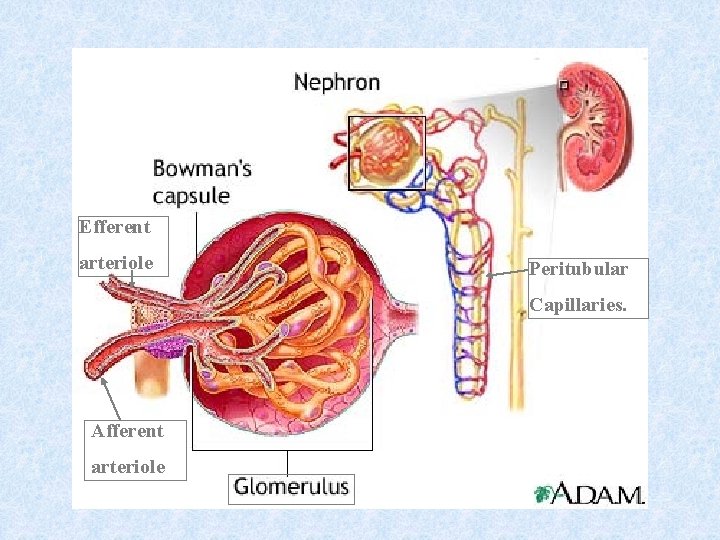
q Efferent arterioles give rise to peritubular capillaries and vasa recta q Vasa recta are found in association with the loops of Henle of juxtamedullary nephrones that extend down into the medulla q The cortical and medullary capillaries drain via interlobular veins to arcuate vein at the corticomedullary junction and through interlobar veins to the renal vein
Efferent arteriole Peritubular Capillaries. Afferent arteriole
 Perforators of lower limb
Perforators of lower limb Sanjaya adikari
Sanjaya adikari What is the name
What is the name Urinary system
Urinary system Urinary bladder
Urinary bladder Dokter ayling sanjaya
Dokter ayling sanjaya Ayling sanjaya
Ayling sanjaya Dr ayling sanjaya
Dr ayling sanjaya Dr ayling sanjaya
Dr ayling sanjaya Jenis spina bifida
Jenis spina bifida Dr. ayling
Dr. ayling Interpretasi cdc growth chart
Interpretasi cdc growth chart Ayling sanjaya
Ayling sanjaya Lymphatic system and urinary system
Lymphatic system and urinary system Physiology of urine formation
Physiology of urine formation Glomerular filtration
Glomerular filtration Pyel medical terminology
Pyel medical terminology Whats gametes
Whats gametes Fetal pig diagram labeled answers
Fetal pig diagram labeled answers Chapter 30 the urinary system
Chapter 30 the urinary system Chapter 15 the urinary system figure 15-3
Chapter 15 the urinary system figure 15-3 Chapter 20 urinary/excretory system
Chapter 20 urinary/excretory system Urinary system model
Urinary system model Urinary system fun fact
Urinary system fun fact Osteichthyes
Osteichthyes Urinary system powerpoint
Urinary system powerpoint Urinary system also known as
Urinary system also known as Adh hormone function
Adh hormone function Urinary bladder
Urinary bladder Figure 15-4 is a diagram of a nephron
Figure 15-4 is a diagram of a nephron Aescending
Aescending Defination of urine
Defination of urine Urinary system label
Urinary system label Endocrine system of rat
Endocrine system of rat Rat urinary system
Rat urinary system Vena cava urinary system
Vena cava urinary system Figure 15-3 the urinary system
Figure 15-3 the urinary system Dct
Dct Bowmans capsule
Bowmans capsule Urinary system
Urinary system Normal constituents of urine
Normal constituents of urine Normal and abnormal constituents of urine
Normal and abnormal constituents of urine Efferent
Efferent Lith-oh-trip-see
Lith-oh-trip-see Urinary infection symptoms
Urinary infection symptoms Arneriole
Arneriole Youtube urinary system
Youtube urinary system The urinary system chapter 15
The urinary system chapter 15 Anatomical structure of urinary system
Anatomical structure of urinary system Chapter 9 the urinary system learning exercises answer key
Chapter 9 the urinary system learning exercises answer key Chapter 25 the urinary system
Chapter 25 the urinary system Urinary
Urinary Length of male urethra
Length of male urethra Ureter blood supply
Ureter blood supply Infrolateral
Infrolateral