Urinary System Dr Anderson Rowan University Urinary System









- Slides: 52
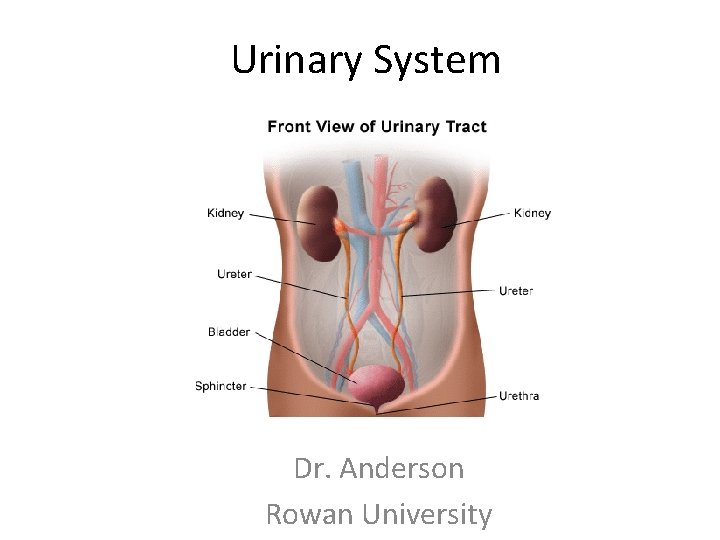
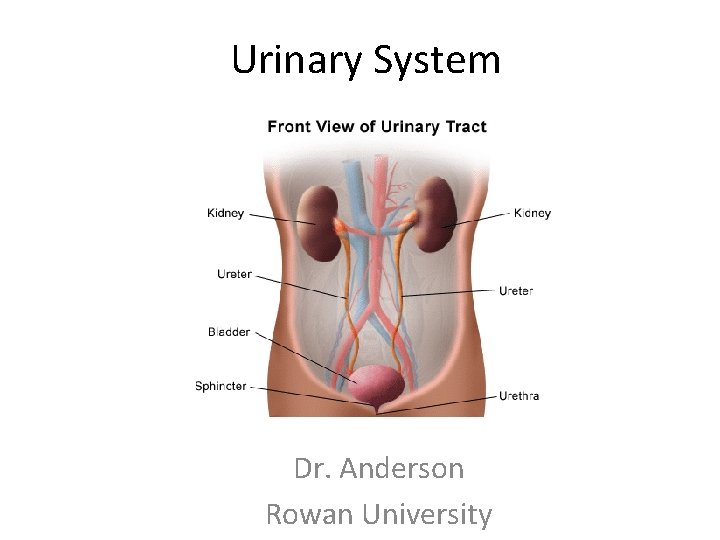
Urinary System Dr. Anderson Rowan University
Urinary System • Function – To remove liquid wastes from the blood and regulate blood volume (and pressure) • Wastes – Excess electrolytes (ions) – Nitrogenous and other metabolic wastes (urea)
Renal Activity • Kidneys consume roughly 2025% of oxygen used by the body at rest • Kidneys filter your entire blood volume roughly 60 times each day • Highly dependent on blood pressure! https: //www. youtube. com/watch? v=Oky. FPMXa 28 c
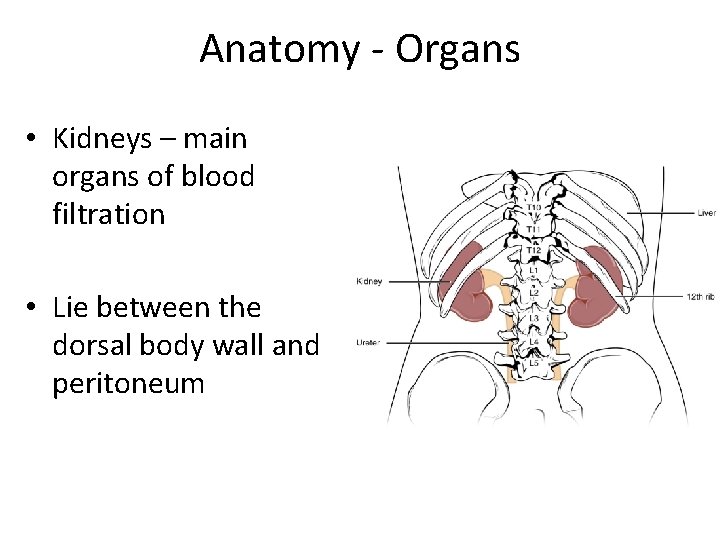
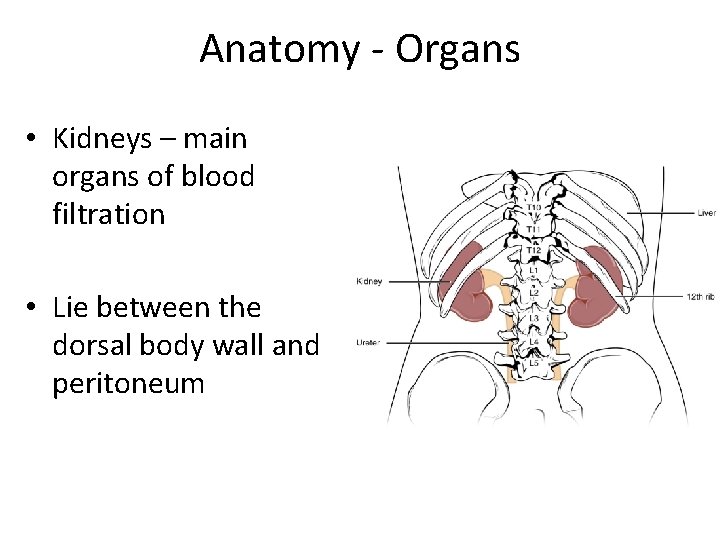
Anatomy - Organs • Kidneys – main organs of blood filtration • Lie between the dorsal body wall and peritoneum
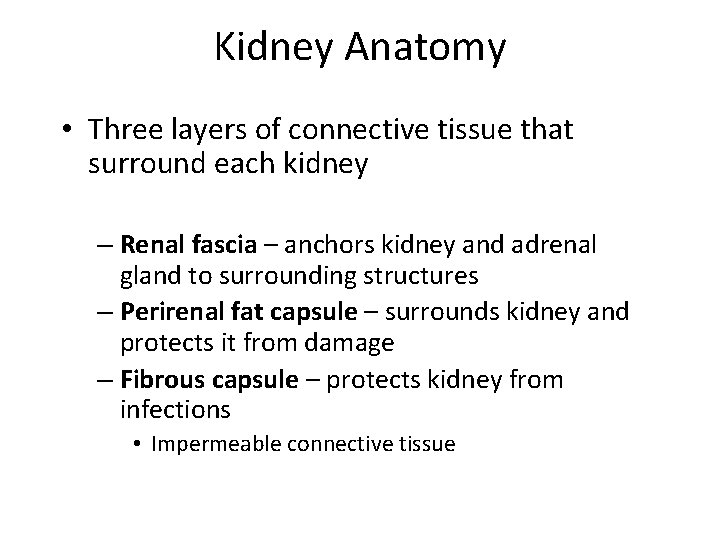
Kidney Anatomy • Three layers of connective tissue that surround each kidney – Renal fascia – anchors kidney and adrenal gland to surrounding structures – Perirenal fat capsule – surrounds kidney and protects it from damage – Fibrous capsule – protects kidney from infections • Impermeable connective tissue
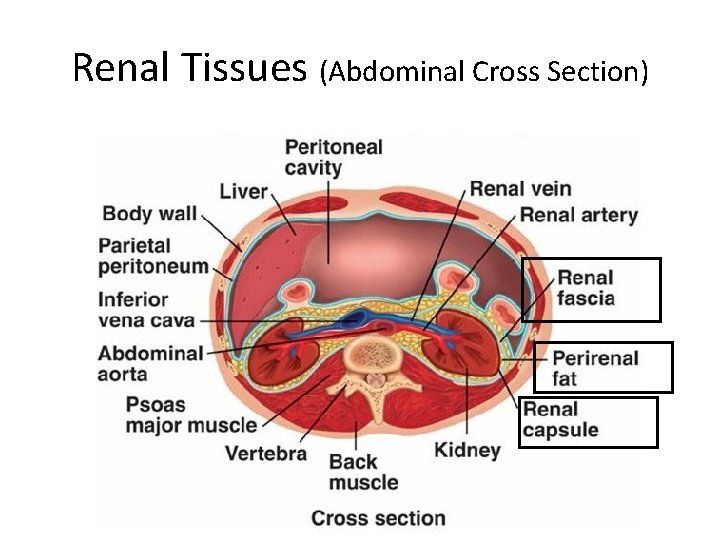
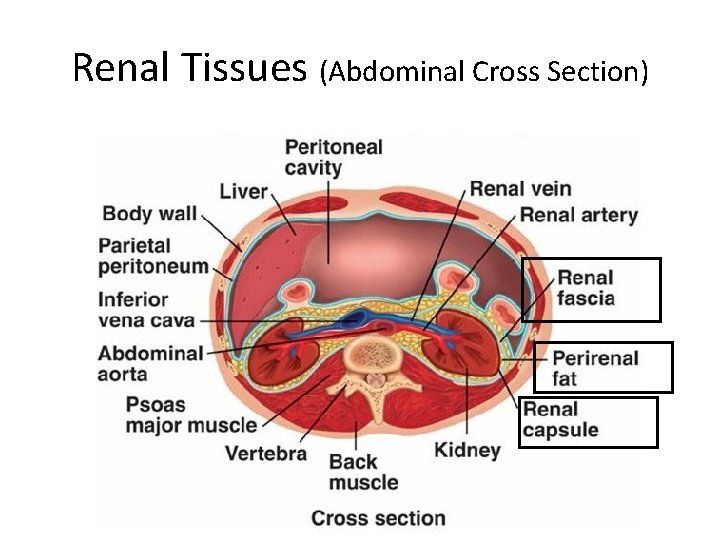
Renal Tissues (Abdominal Cross Section)

Gross Anatomy – External Kidney • Renal Artery – Supplies blood to be filtered • Renal Vein – Filtered blood returns to circulation • Hilum – Concave surface (medial surface)
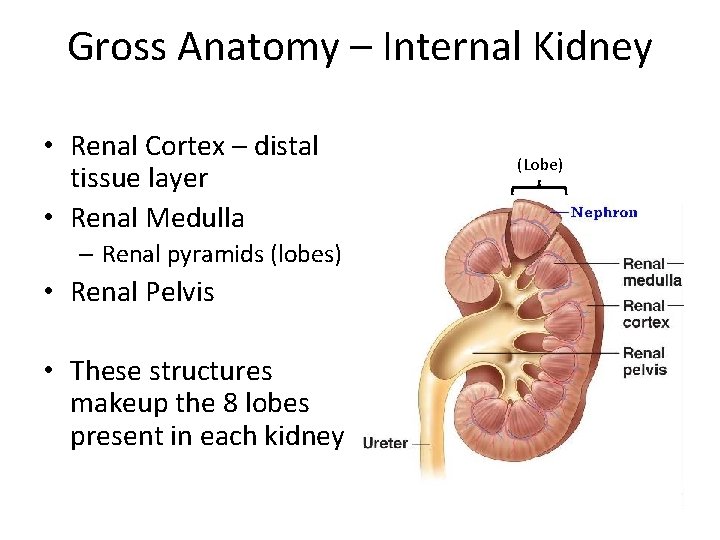
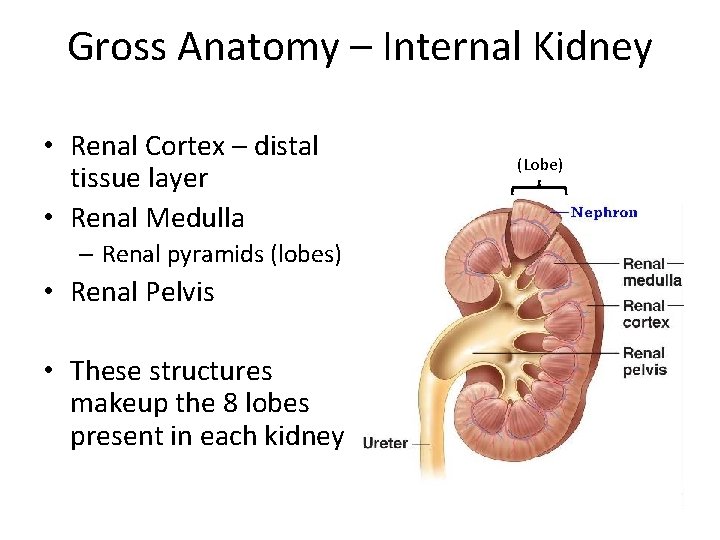
Gross Anatomy – Internal Kidney • Renal Cortex – distal tissue layer • Renal Medulla – Renal pyramids (lobes) • Renal Pelvis • These structures makeup the 8 lobes present in each kidney (Lobe)
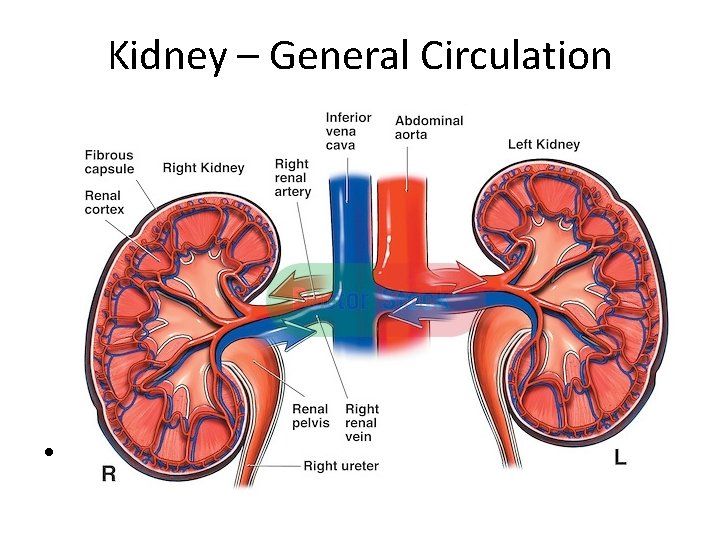
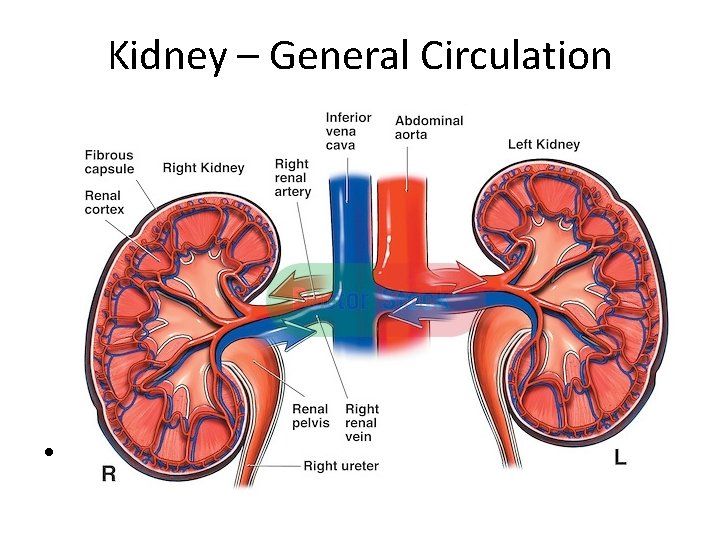
Kidney – General Circulation •
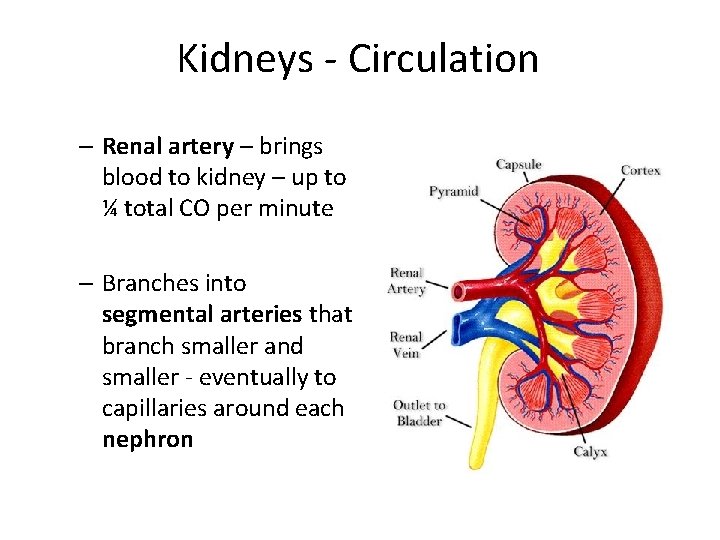
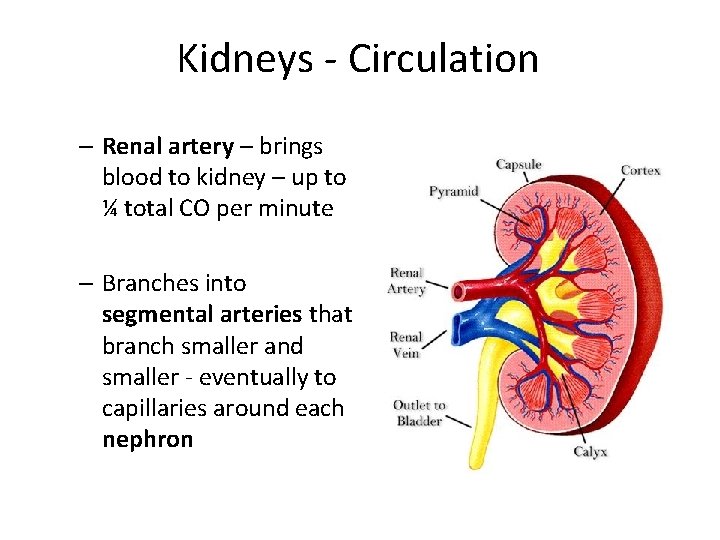
Kidneys - Circulation – Renal artery – brings blood to kidney – up to ¼ total CO per minute – Branches into segmental arteries that branch smaller and smaller - eventually to capillaries around each nephron

Circulation is Extensive What is this showing? Why so extensive?
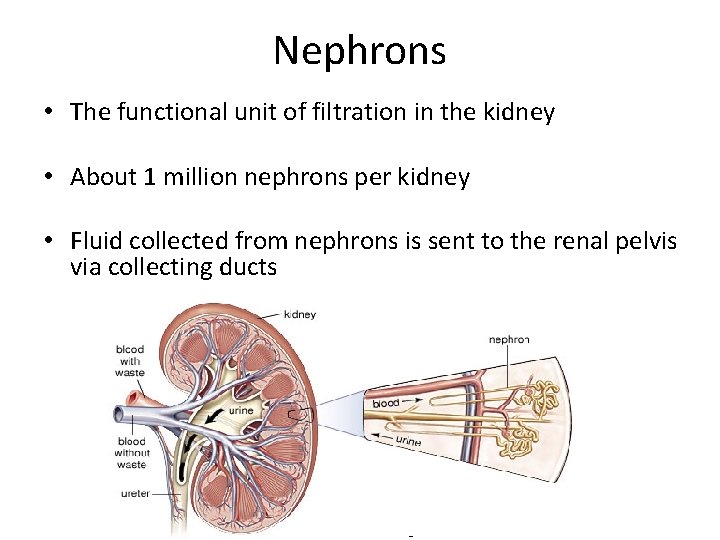
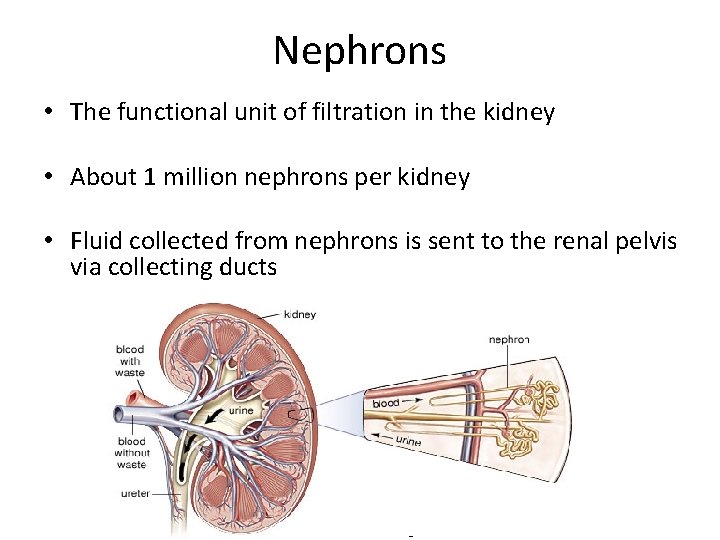
Nephrons • The functional unit of filtration in the kidney • About 1 million nephrons per kidney • Fluid collected from nephrons is sent to the renal pelvis via collecting ducts
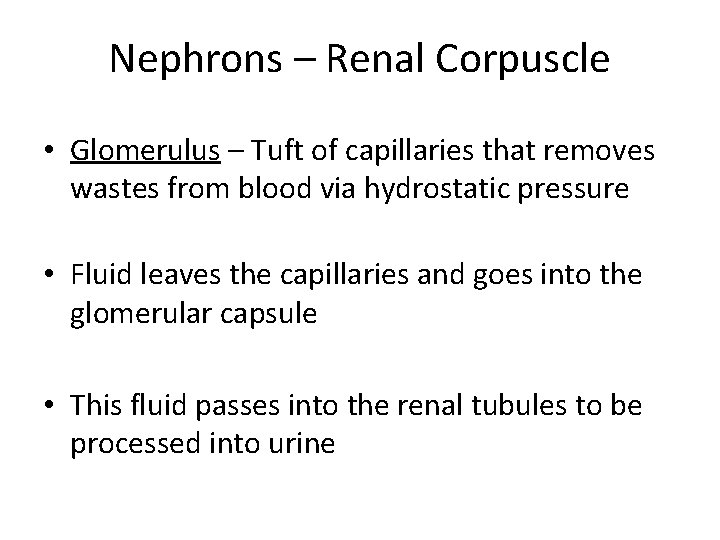
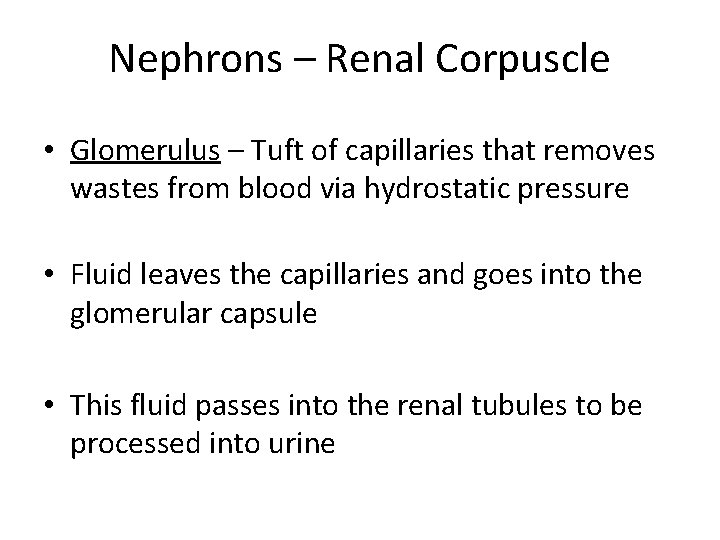
Nephrons – Renal Corpuscle • Glomerulus – Tuft of capillaries that removes wastes from blood via hydrostatic pressure • Fluid leaves the capillaries and goes into the glomerular capsule • This fluid passes into the renal tubules to be processed into urine
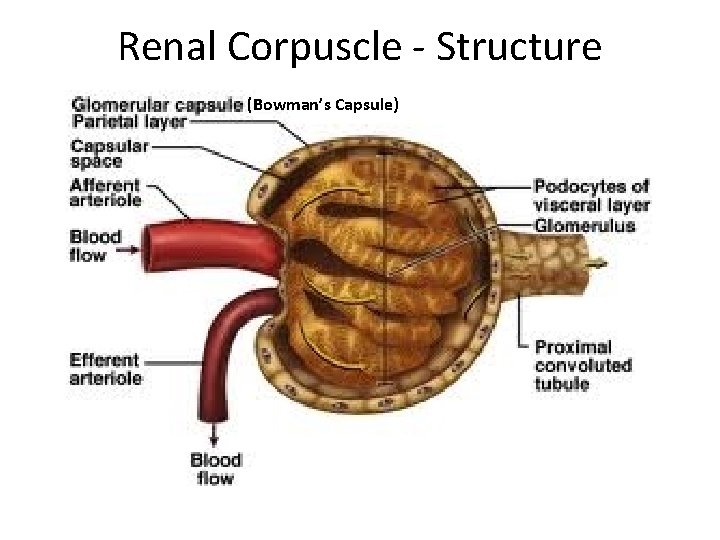
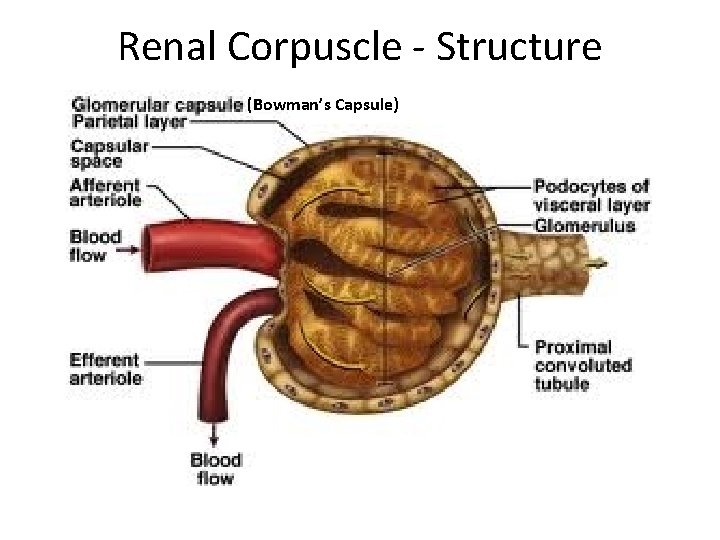
Renal Corpuscle - Structure (Bowman’s Capsule)

Capillaries • Glomerulus – A tuft of fenestrated capillaries inside the Bowman’s capsule • Fenestrated capillaries are very porous, allowing liquids to move out under pressure • Fenestrae (holes) are restrictive – only very small solute molecules can pass through (H 20, sugars, salts, etc – NOT proteins!)
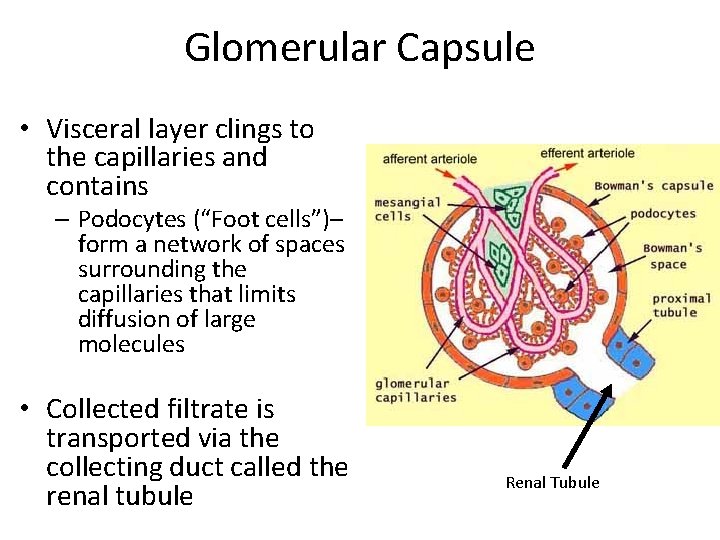
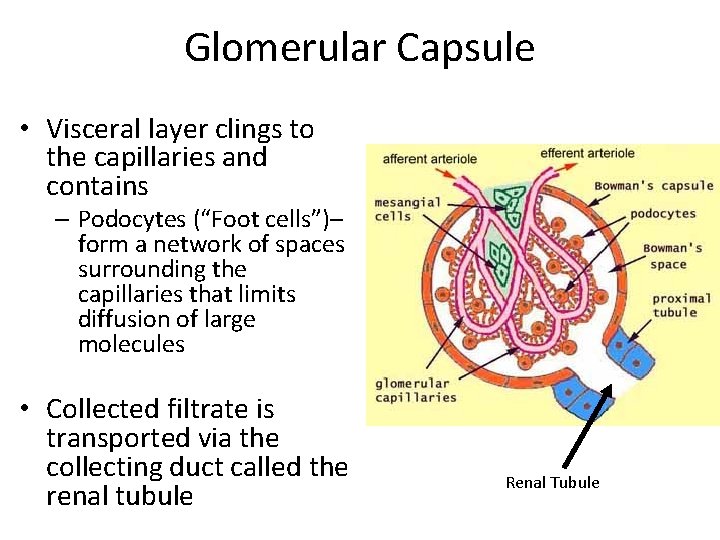
Glomerular Capsule • Visceral layer clings to the capillaries and contains – Podocytes (“Foot cells”)– form a network of spaces surrounding the capillaries that limits diffusion of large molecules • Collected filtrate is transported via the collecting duct called the renal tubule Renal Tubule
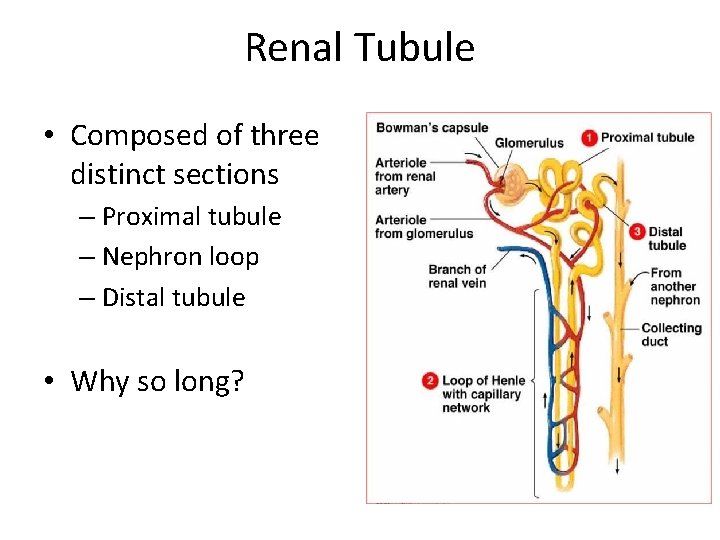
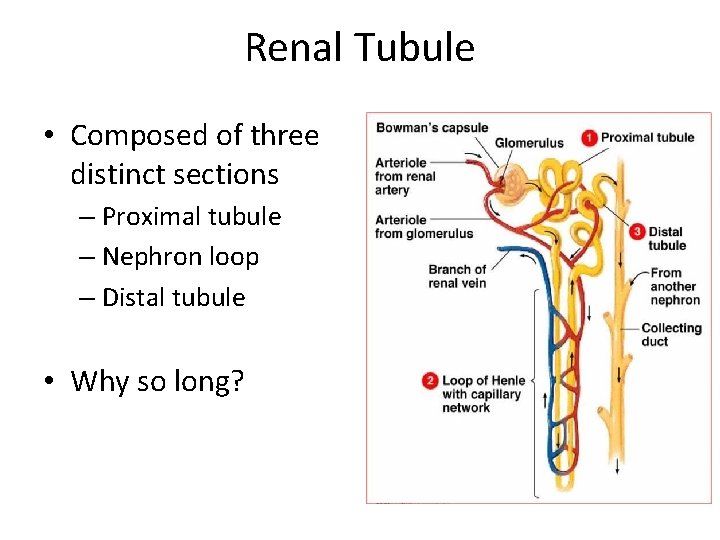
Renal Tubule • Composed of three distinct sections – Proximal tubule – Nephron loop – Distal tubule • Why so long?
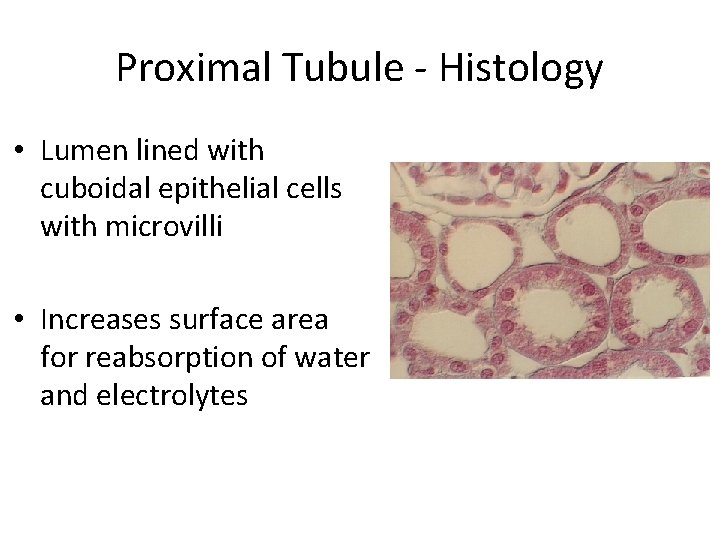
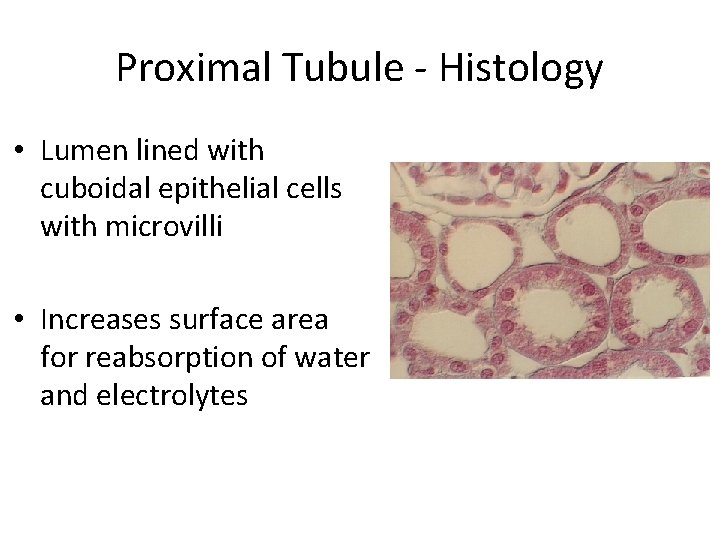
Proximal Tubule - Histology • Lumen lined with cuboidal epithelial cells with microvilli • Increases surface area for reabsorption of water and electrolytes
Nephron Loop and Distal Tubule • Serve to further remove water and useful substances (e. g. electrolytes) from the filtrate collected from the renal capsule • Squamous epithelia • Cuboidal epithelia (no microvilli)

Nephron Capillary Beds • Glomerulus – under high (arterial) pressure – forces fluid out of the blood and into the renal capsule • Peritubular Capillaries – Cling to and readily absorb water and solutes from the filtrate in the renal tubules
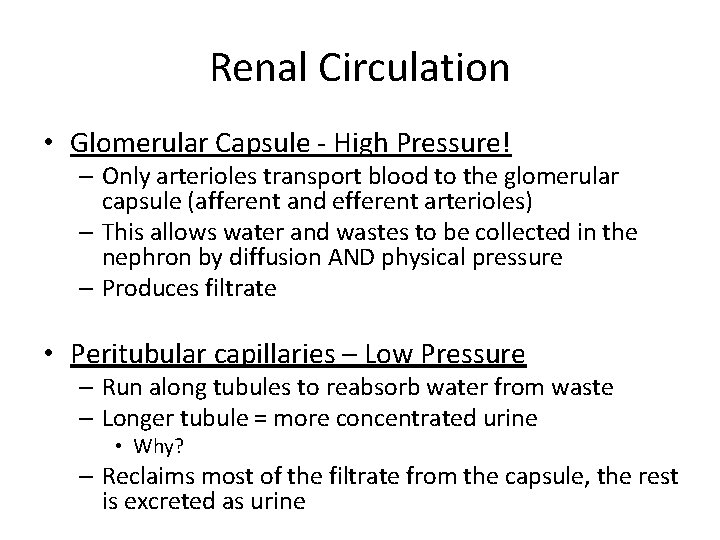
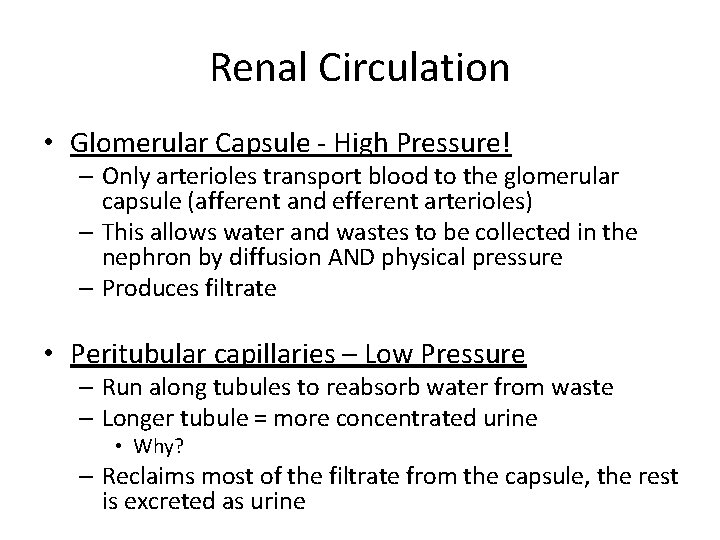
Renal Circulation • Glomerular Capsule - High Pressure! – Only arterioles transport blood to the glomerular capsule (afferent and efferent arterioles) – This allows water and wastes to be collected in the nephron by diffusion AND physical pressure – Produces filtrate • Peritubular capillaries – Low Pressure – Run along tubules to reabsorb water from waste – Longer tubule = more concentrated urine • Why? – Reclaims most of the filtrate from the capsule, the rest is excreted as urine
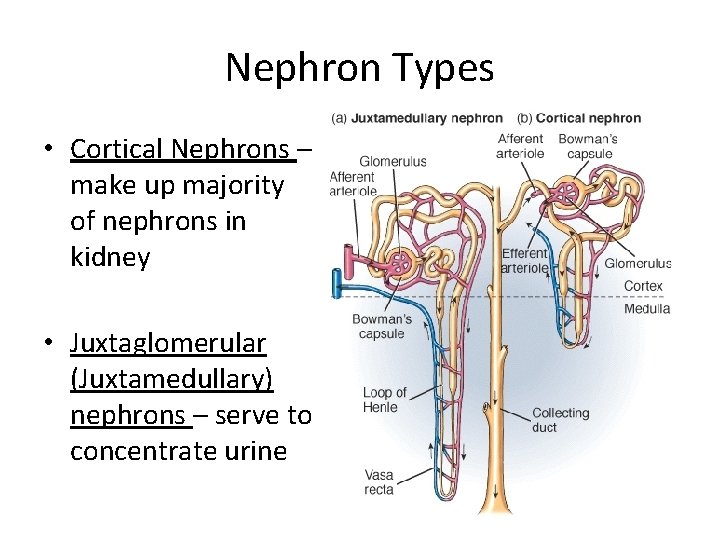
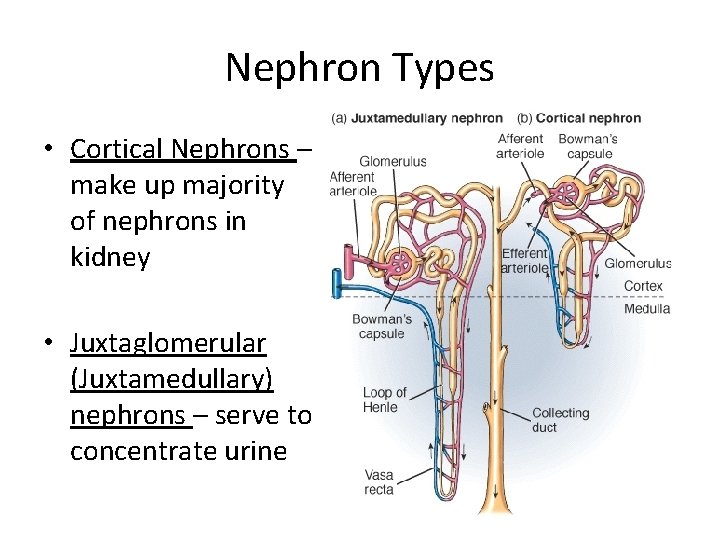
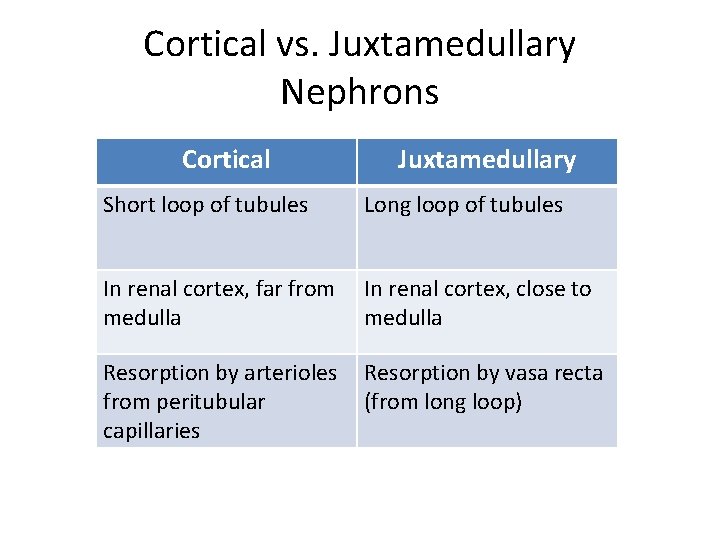
Nephron Types • Cortical Nephrons – make up majority of nephrons in kidney • Juxtaglomerular (Juxtamedullary) nephrons – serve to concentrate urine
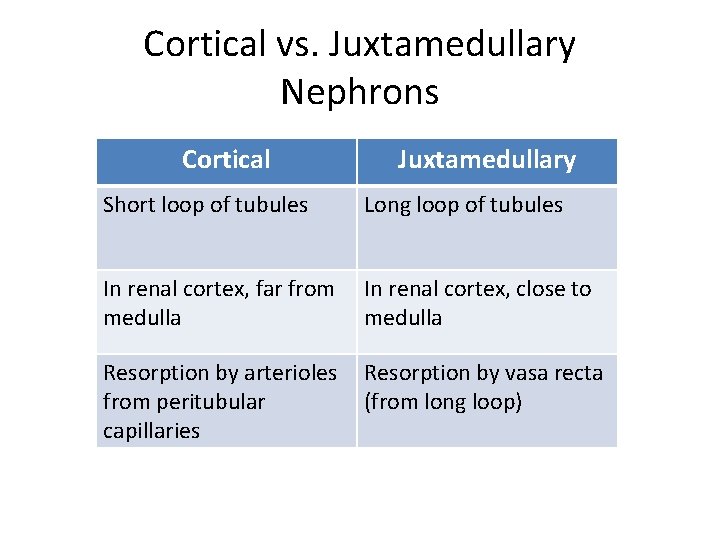
Cortical vs. Juxtamedullary Nephrons Cortical Juxtamedullary Short loop of tubules Long loop of tubules In renal cortex, far from medulla In renal cortex, close to medulla Resorption by arterioles from peritubular capillaries Resorption by vasa recta (from long loop)
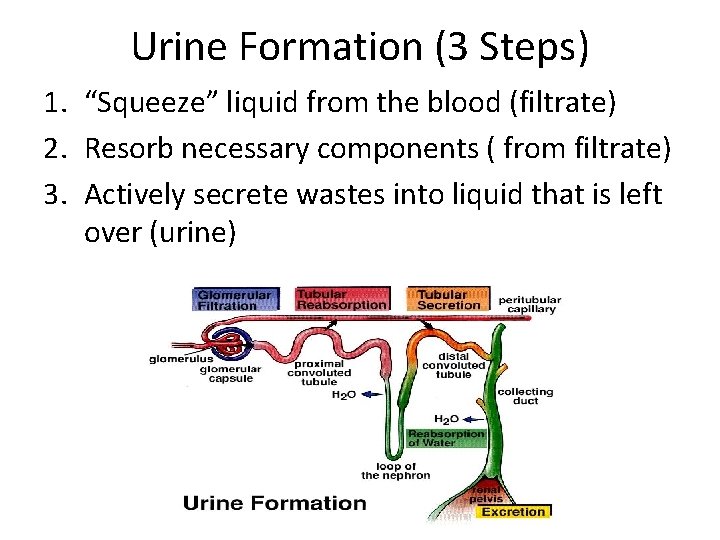
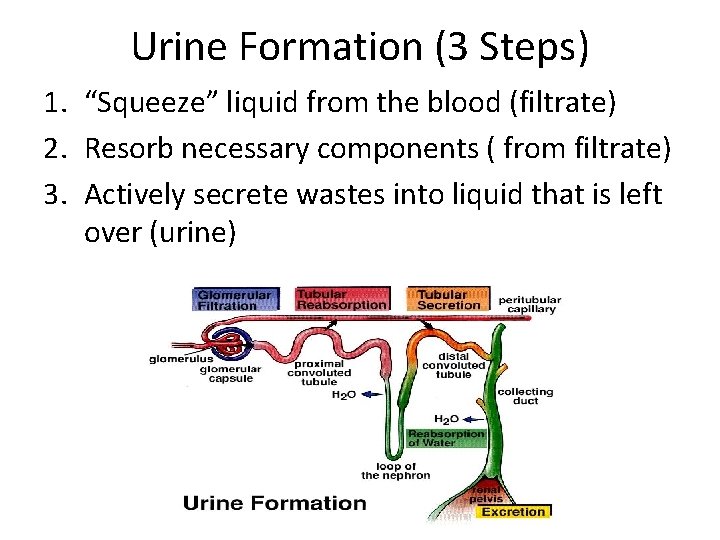
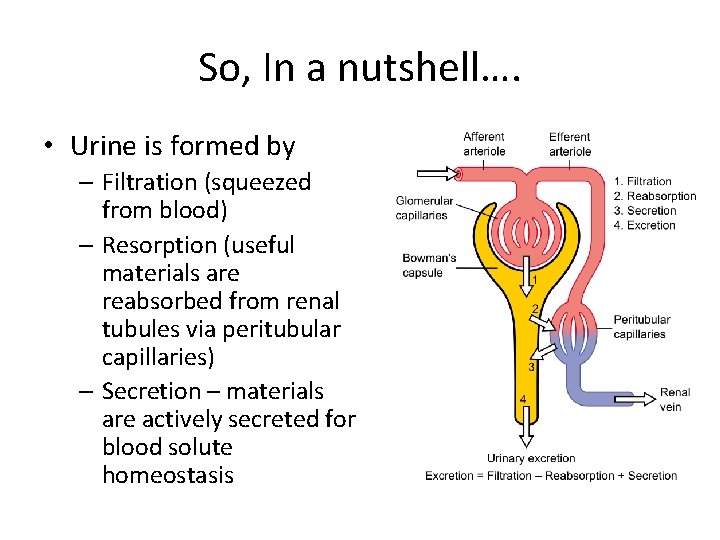
Urine Formation (3 Steps) 1. “Squeeze” liquid from the blood (filtrate) 2. Resorb necessary components ( from filtrate) 3. Actively secrete wastes into liquid that is left over (urine)
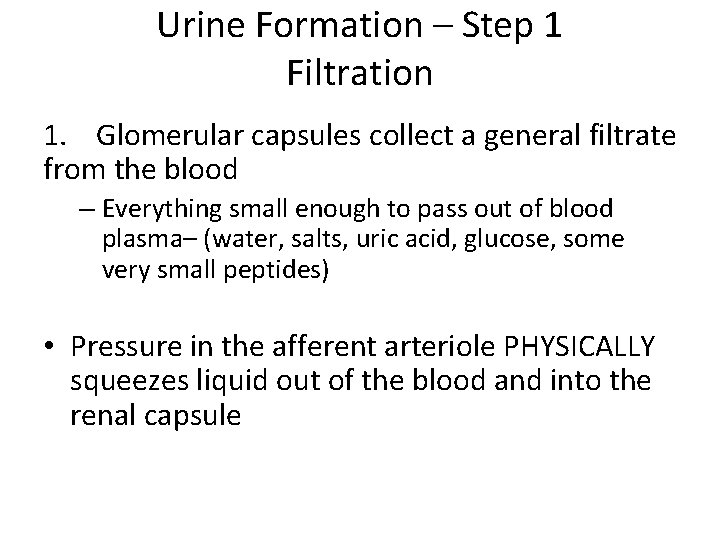
Urine Formation – Step 1 Filtration 1. Glomerular capsules collect a general filtrate from the blood – Everything small enough to pass out of blood plasma– (water, salts, uric acid, glucose, some very small peptides) • Pressure in the afferent arteriole PHYSICALLY squeezes liquid out of the blood and into the renal capsule
Factors Affecting Filtrate Formation Outward pressure • Blood (hydrostatic) pressure – glomerular capillaries have high pressure to squeeze liquid out of blood – Enhances filtrate formation Inward Pressure • Capsule pressure and osmotic pressure in blood – Hinders filtrate formation
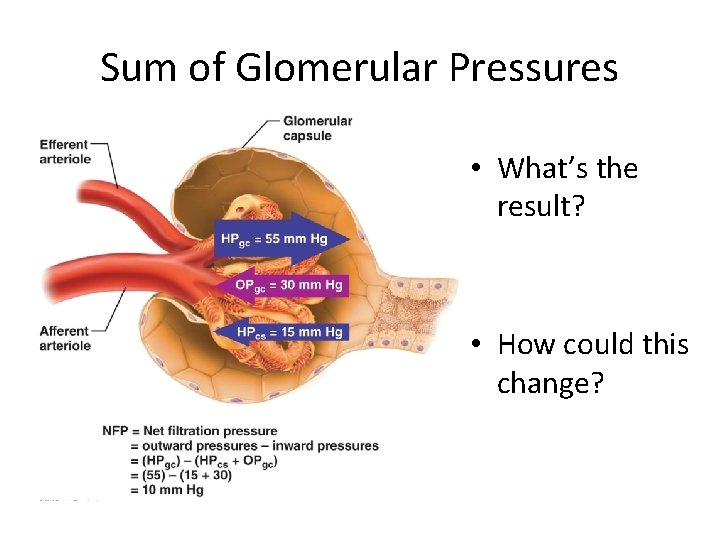
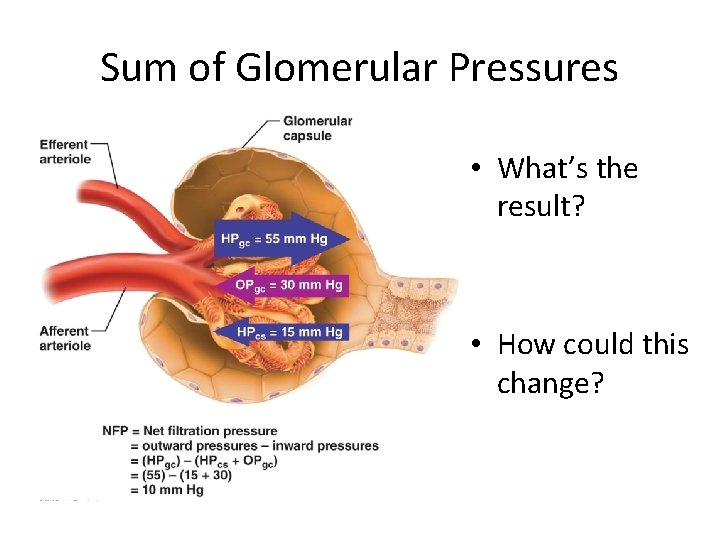
Sum of Glomerular Pressures • What’s the result? • How could this change?

Filtration Rate Factors • Pressure (discussed previously) • Total surface area for filtration! • Filtration membrane permeability • These factors lead to glomerular filtration rate (GFR) – volume of filtrate produced each minute by both kidneys

How can GFR vary? • What happens if blood pressure drops? Increases? • Intrinsic and extrinsic controls maintain a relatively constant GFR under most conditions
Urine Formation – Step 2 Reabsorption Tubules resorb everything the body needs – water, and other important dissolved solutes. Anything not resorbed becomes urine (glucose, vitamins, electrolytes, etc. ) This is accomplished by both active diffusion (requiring ATP) and passive diffusion https: //www. youtube. com/watch? v=s 0 O 9 ute 2 N 1 o
Active Transport • ATP-powered pumps move Na+ from the filtrate and back into the artery (into the blood) • This creates a diffusion gradient as well as an electrochemical gradient
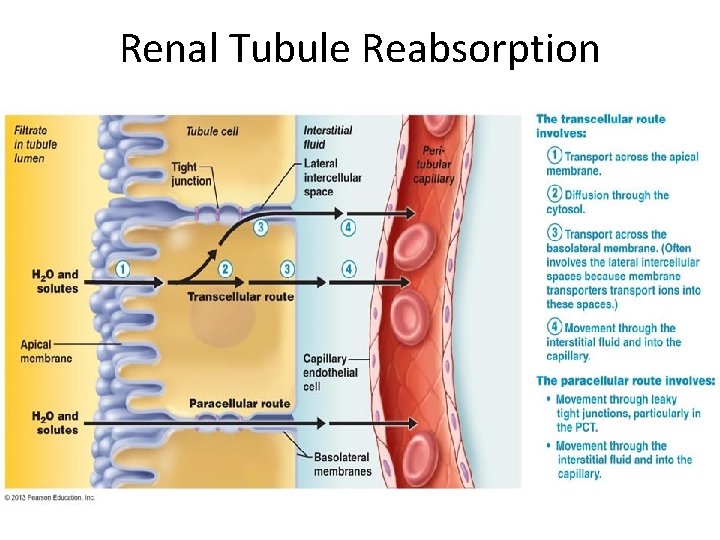
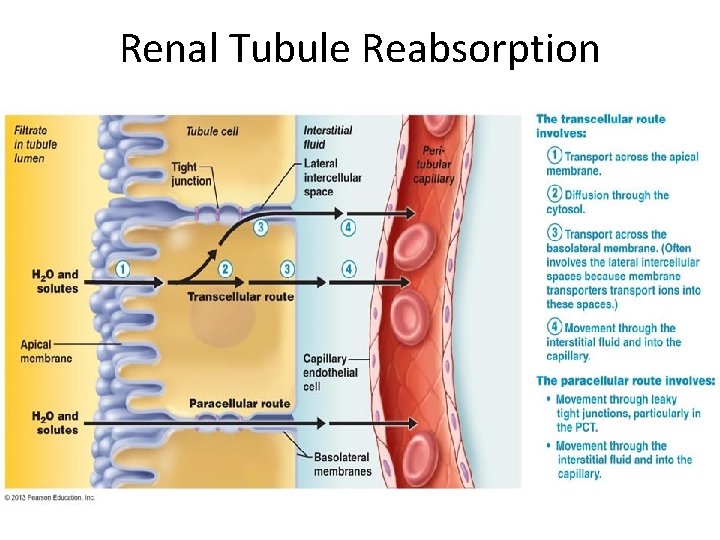
Renal Tubule Reabsorption
Reabsorption Regulation • Limited by the number of primary transport proteins for each substance – E. g. - sodium, potassium • Secondary Active Transport – solutes (glucose, amino acids, other ions) are co-transported back into the blood with sodium • Water then follows solutes into the blood via passive diffusion, helping to maintain blood pressure
Hormonal Regulation • Anti-diuretic Hormone (ADH) – increases permeability of the collecting ducts to water, putting water back into the blood – Stimulated: increased blood solutes or decreased blood pressure – Inhibited: adequate hydration, alcohol consumption • Aldosterone – Reduces Na+ secretion (stimulates resorption) – Stimulated: increased K+, low blood pressure (via renin-angiotensin mechanism) – Inhibited: decreased K+, high blood pressure
Step 3 - Secretion Tubules also add substances to urine by SECRETING them in order to: 1. 2. 3. 4. Eliminate drugs and toxic metabolites Eliminate undesirable resorbed substances Regulate K+ Controls blood p. H levels

Regulation of Urine Concentration
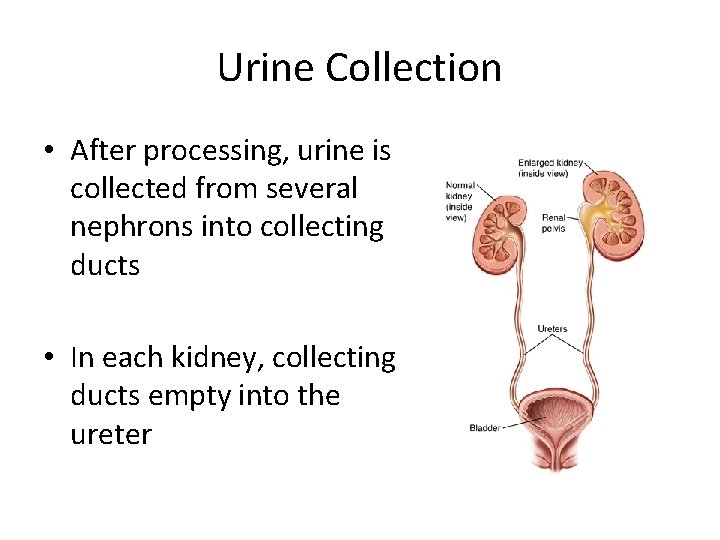
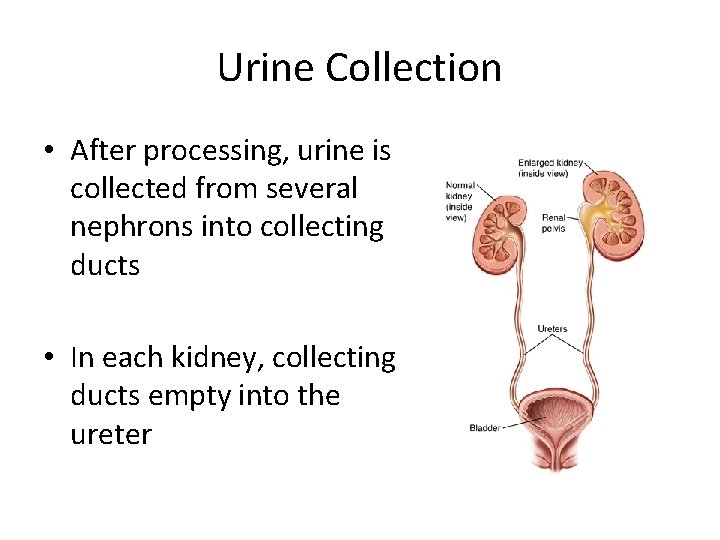
Urine Collection • After processing, urine is collected from several nephrons into collecting ducts • In each kidney, collecting ducts empty into the ureter

Renal Failure Kidney Damage (physical or chemical) – Reduces urine output resulting in a reduction or stop to urine production • Dialysis needed – sometimes for life

Kidney Stones Precipitated Minerals can cause kidney stones
Diuretics • Enhance water excretion by: – Inhibiting ADH secretion – Inhibiting Na+ resorption into the blood (and the water that goes with it) • Why would these be prescribed?
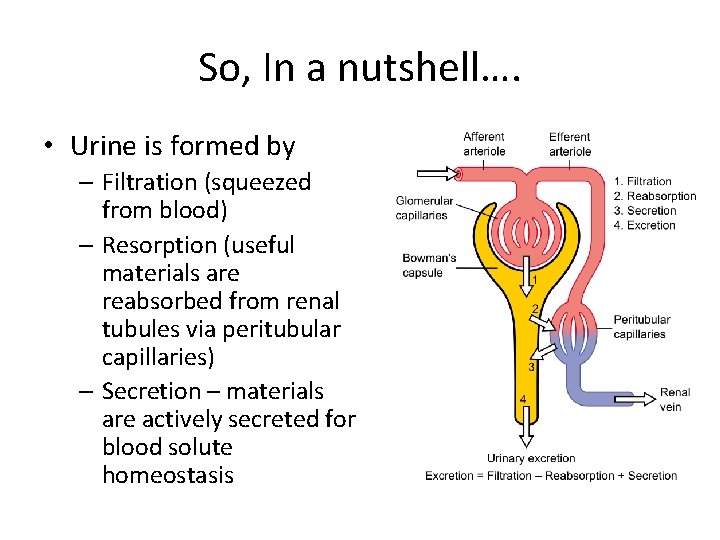
So, In a nutshell…. • Urine is formed by – Filtration (squeezed from blood) – Resorption (useful materials are reabsorbed from renal tubules via peritubular capillaries) – Secretion – materials are actively secreted for blood solute homeostasis
Sum up of Nephron Function • https: //www. youtube. com/watch? v=o. Xc. EAH_ yes. Y
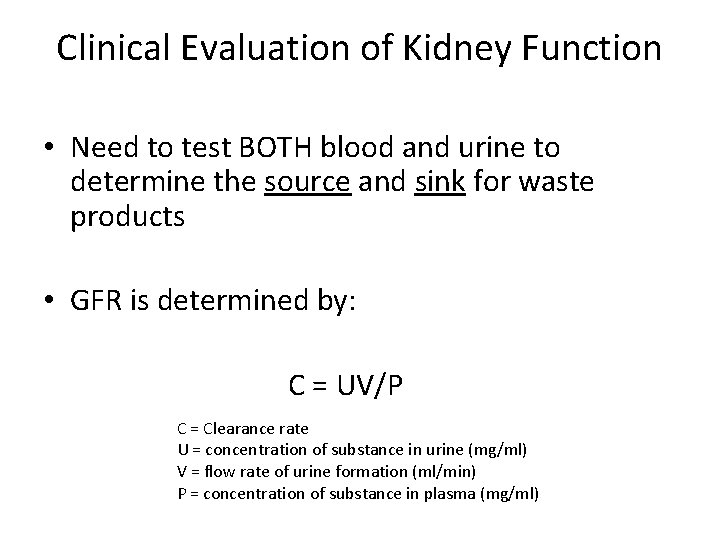
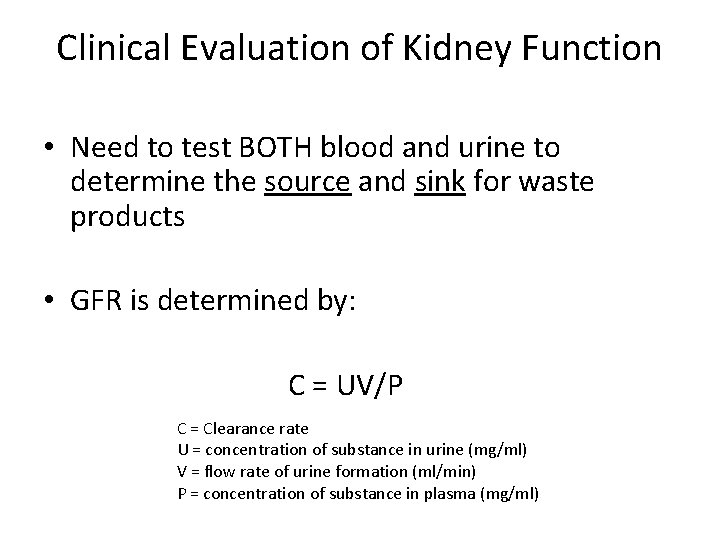
Clinical Evaluation of Kidney Function • Need to test BOTH blood and urine to determine the source and sink for waste products • GFR is determined by: C = UV/P C = Clearance rate U = concentration of substance in urine (mg/ml) V = flow rate of urine formation (ml/min) P = concentration of substance in plasma (mg/ml)
Urine Characteristics • Sterile - What if it isn’t? • Pale yellow – What if it isn’t? • Specific gravity (density) – greater than that of water, varies according to solute concentration
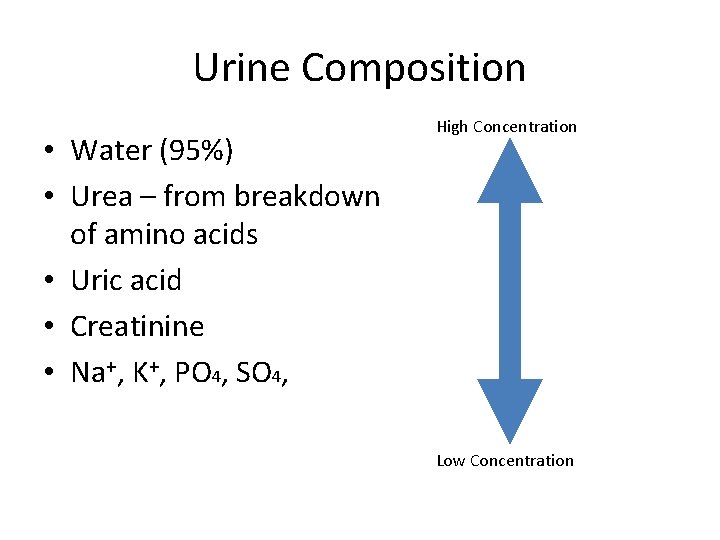
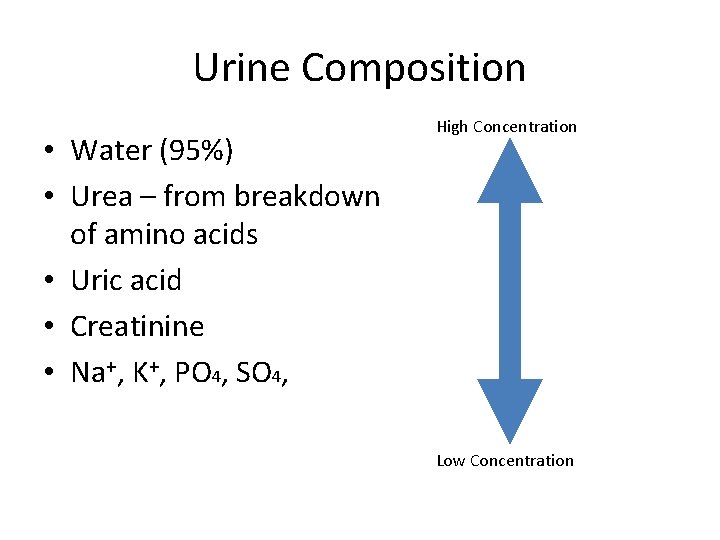
Urine Composition • Water (95%) • Urea – from breakdown of amino acids • Uric acid • Creatinine • Na+, K+, PO 4, SO 4, High Concentration Low Concentration
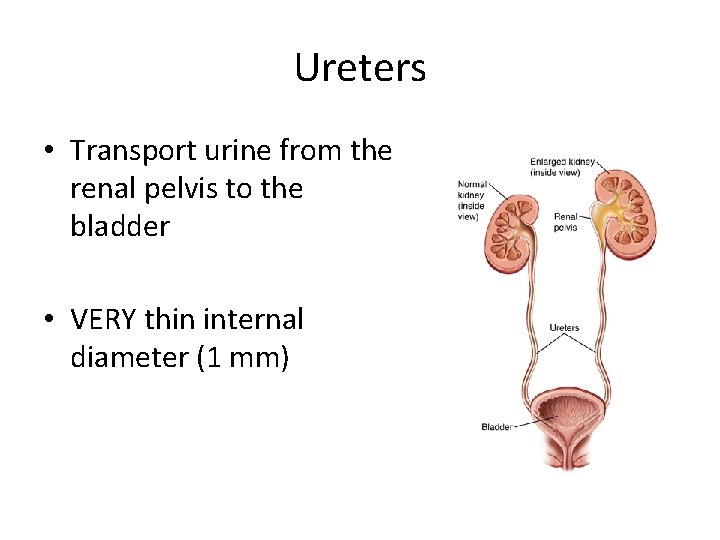
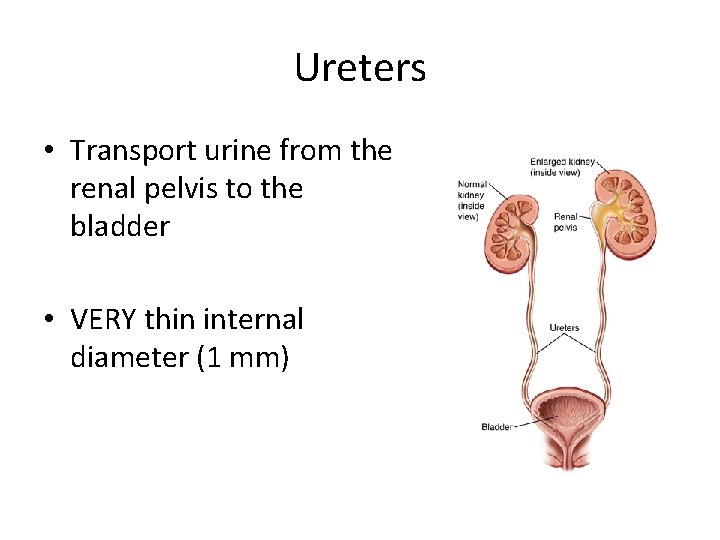
Ureters • Transport urine from the renal pelvis to the bladder • VERY thin internal diameter (1 mm)
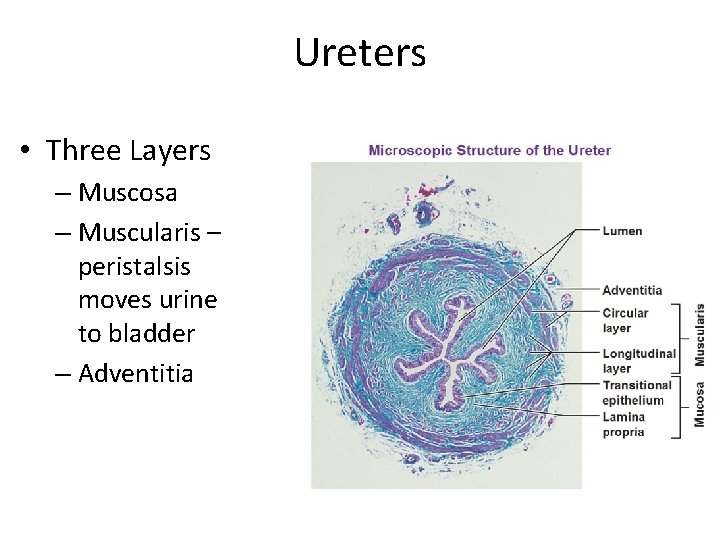
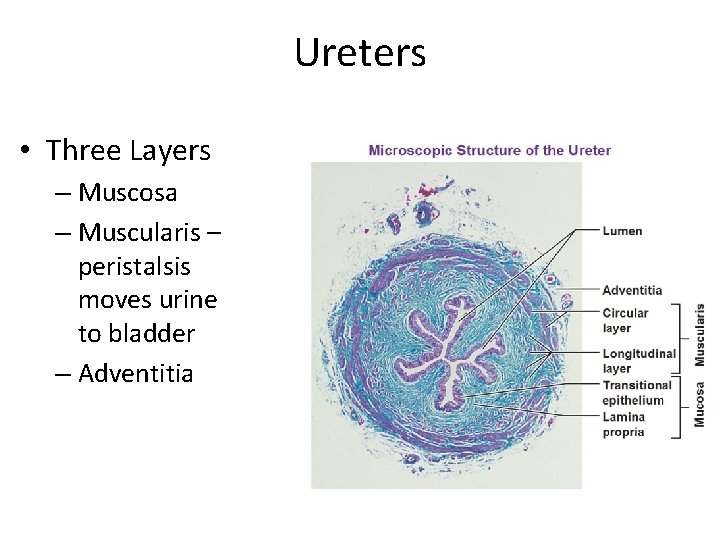
Ureters • Three Layers – Muscosa – Muscularis – peristalsis moves urine to bladder – Adventitia
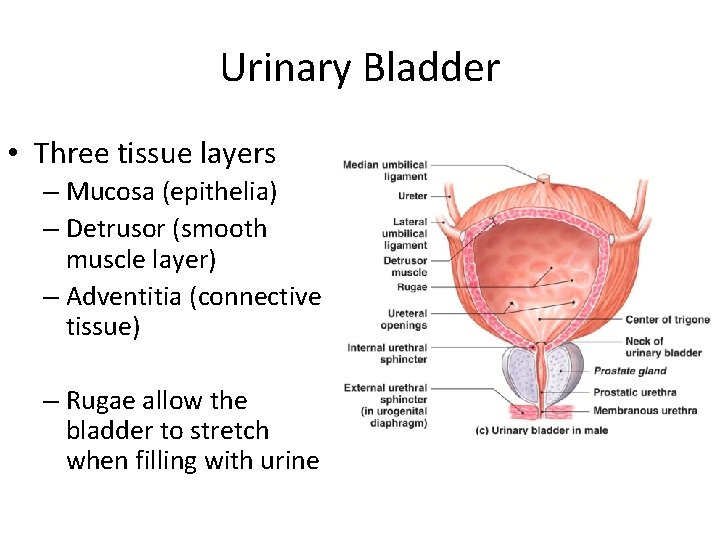
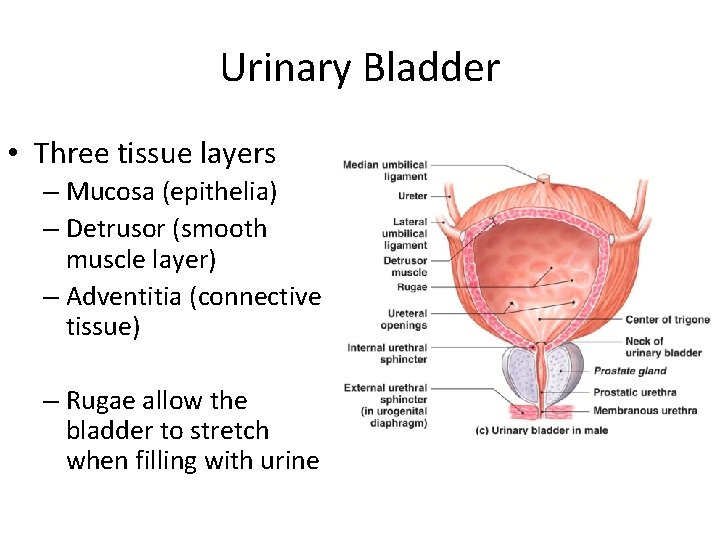
Urinary Bladder • Three tissue layers – Mucosa (epithelia) – Detrusor (smooth muscle layer) – Adventitia (connective tissue) – Rugae allow the bladder to stretch when filling with urine
Bladder Capacities • Empty bladder (after urination) should have 5 ml or less of urine • Full bladder can hold 500 ml of urine • Distended bladder can hold ~1000 ml of urine – Bladder can herniate or rupture
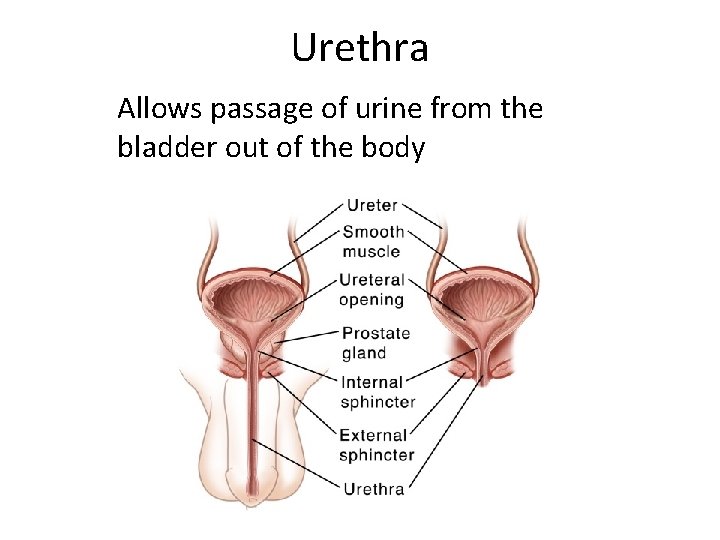
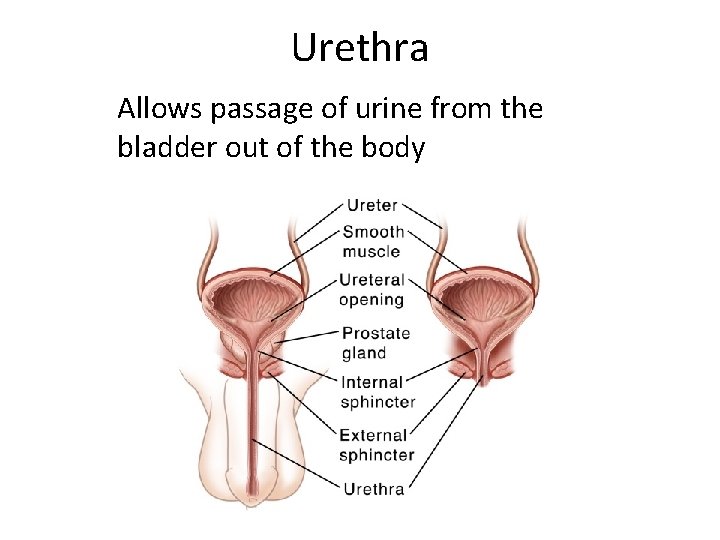
Urethra Allows passage of urine from the bladder out of the body
Urination • Controlled by a cascade of events 1. Bladder muscle (detrusor) must contract 2. Internal urethral sphincter relaxes (involuntary) 3. External urethral sphincter relaxes (voluntary) Largely controlled by autonomic nervous system
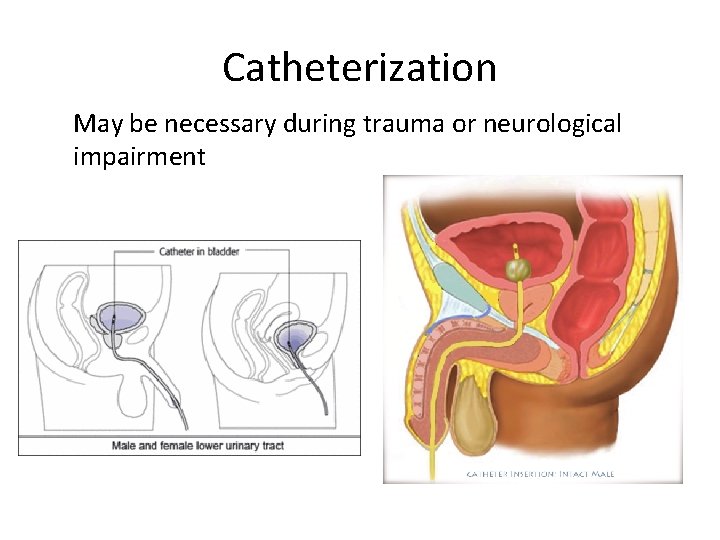
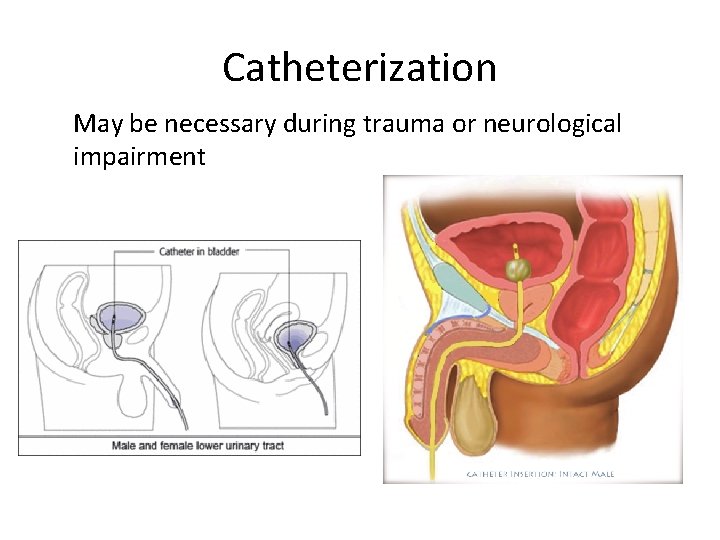
Catheterization May be necessary during trauma or neurological impairment