Fig 46 1 Fig 46 2 Fig 46


- Slides: 42

Fig. 46 -1
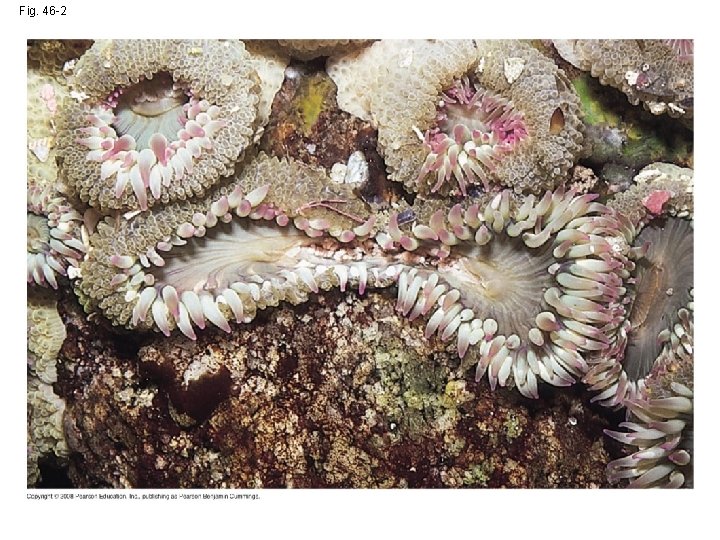
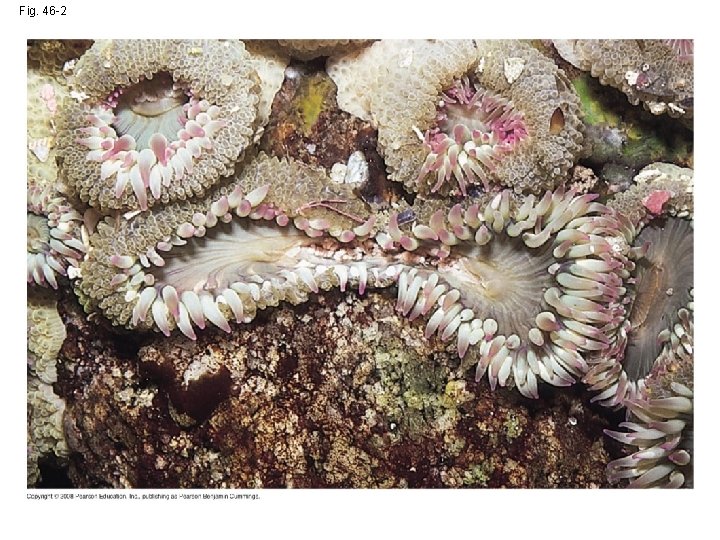
Fig. 46 -2
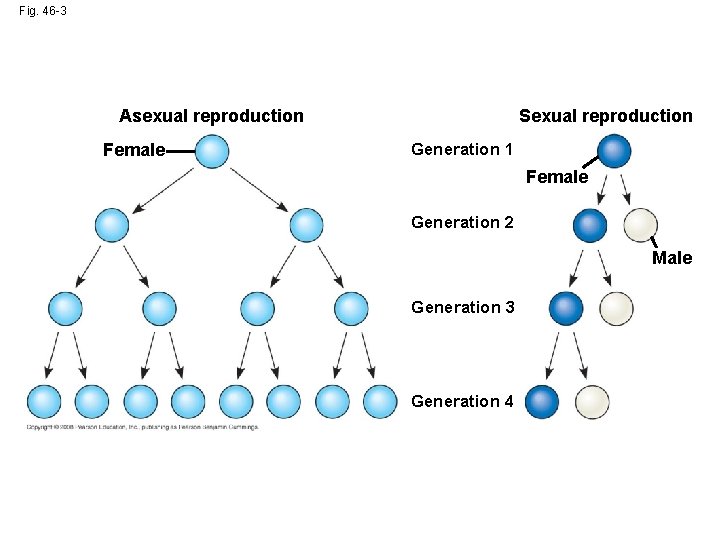
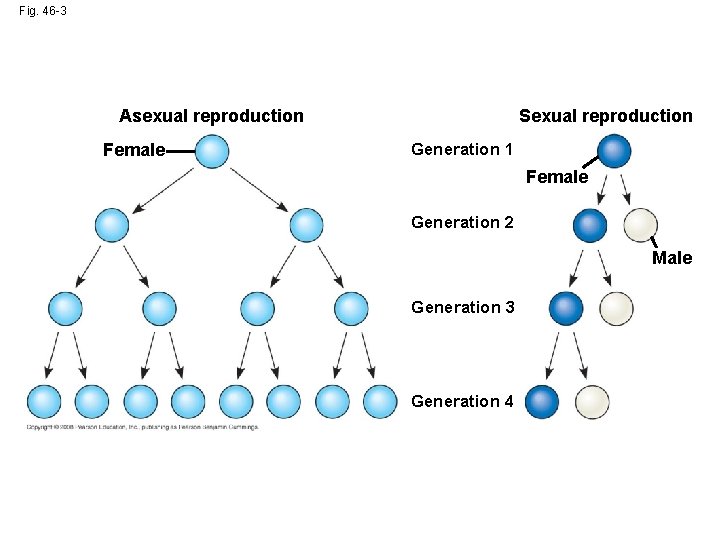
Fig. 46 -3 Sexual reproduction Asexual reproduction Female Generation 1 Female Generation 2 Male Generation 3 Generation 4
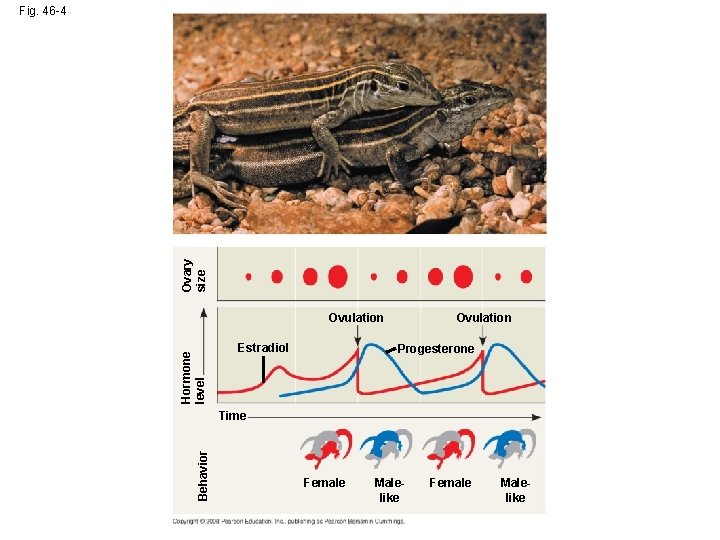
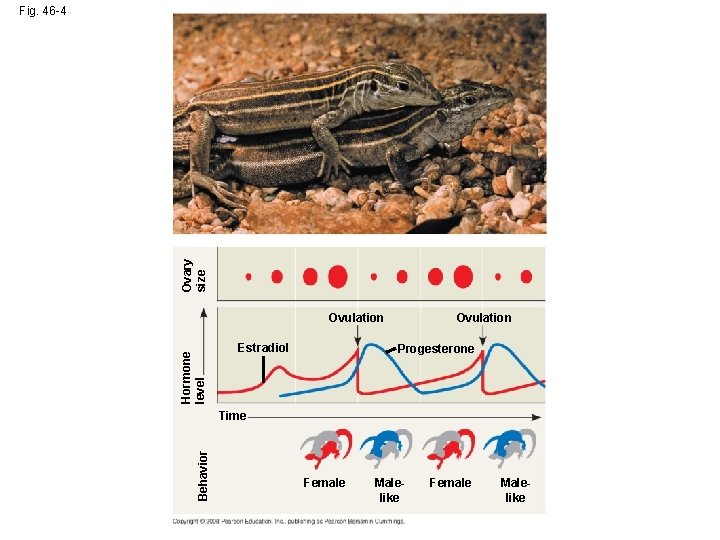
Ovary size Fig. 46 -4 Hormone level Ovulation Estradiol Ovulation Progesterone Behavior Time Female Malelike

Fig. 46 -4 a
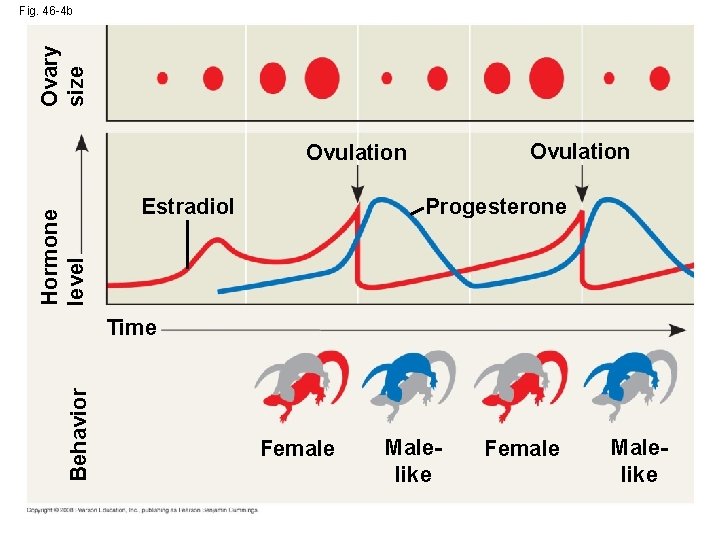
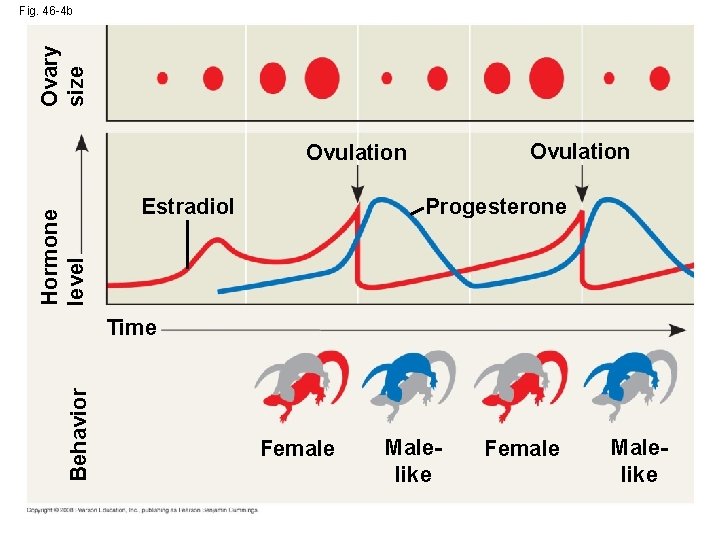
Ovary size Fig. 46 -4 b Ovulation Hormone level Ovulation Progesterone Estradiol Behavior Time Female Malelike
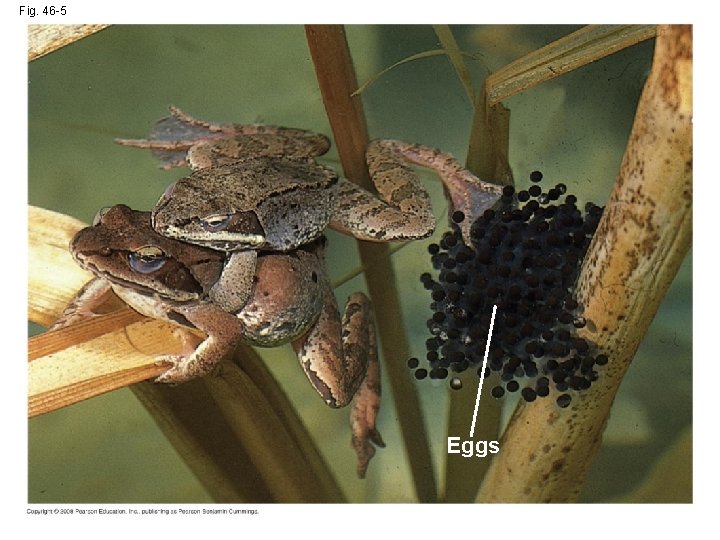
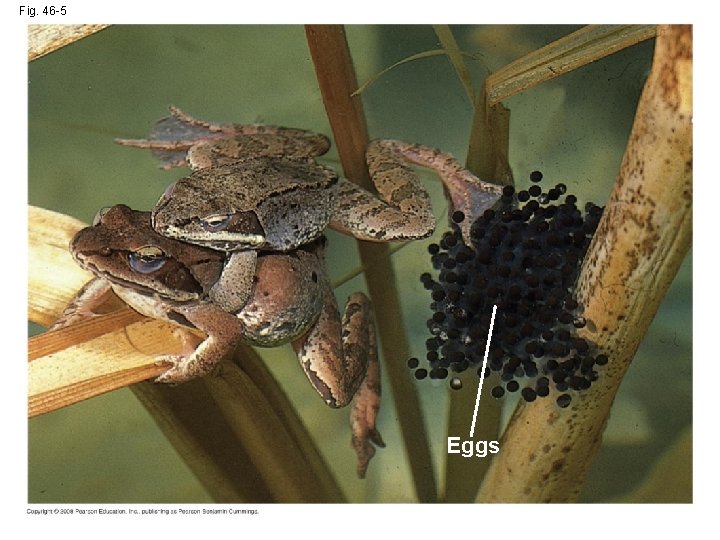
Fig. 46 -5 Eggs
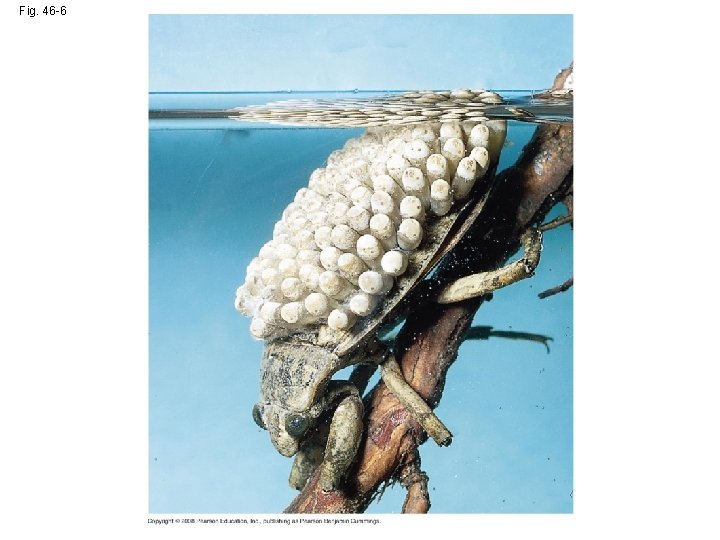
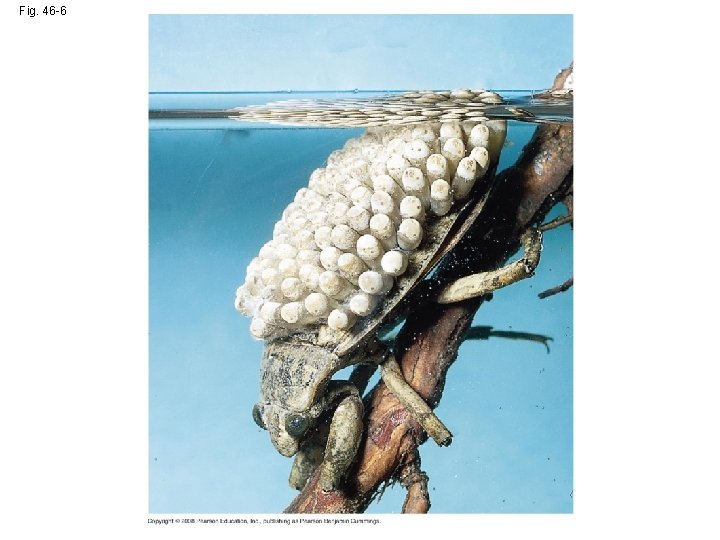
Fig. 46 -6
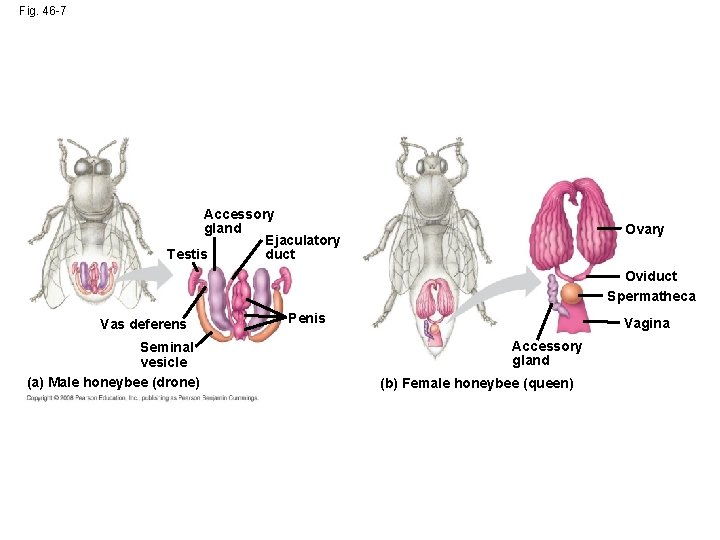
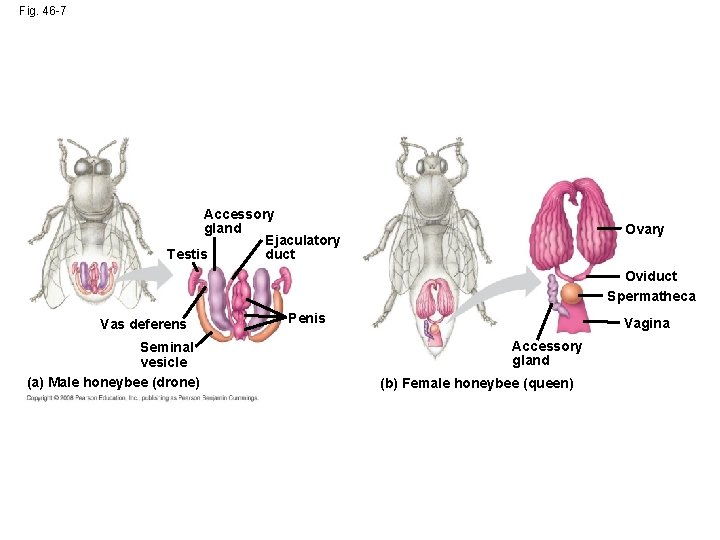
Fig. 46 -7 Accessory gland Ejaculatory duct Testis Ovary Oviduct Spermatheca Vas deferens Seminal vesicle (a) Male honeybee (drone) Penis Vagina Accessory gland (b) Female honeybee (queen)
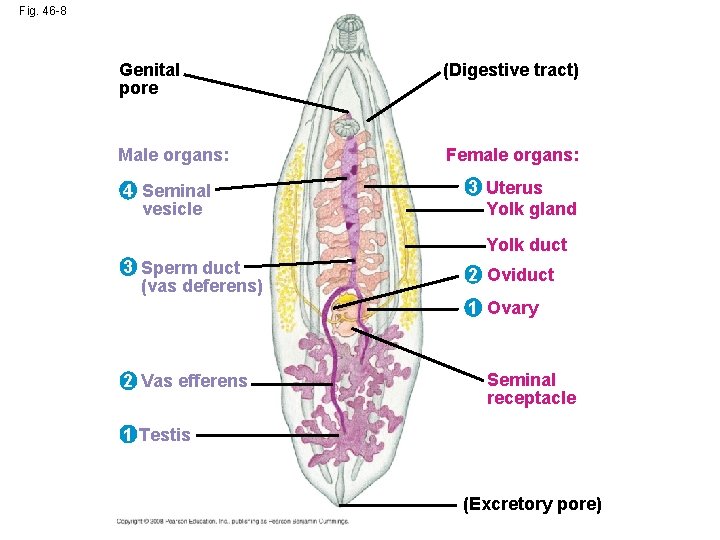
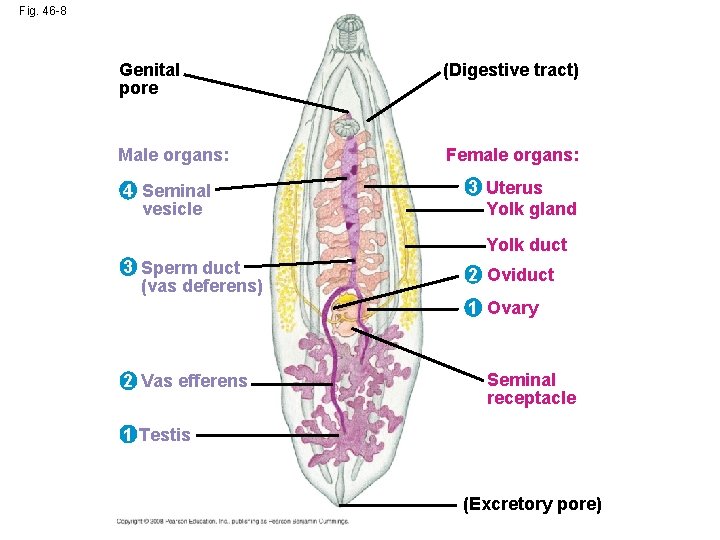
Fig. 46 -8 Genital pore (Digestive tract) Male organs: Female organs: 4 Seminal vesicle 3 Uterus Yolk gland Yolk duct 3 Sperm duct (vas deferens) 2 Oviduct 1 Ovary 2 Vas efferens Seminal receptacle 1 Testis (Excretory pore)
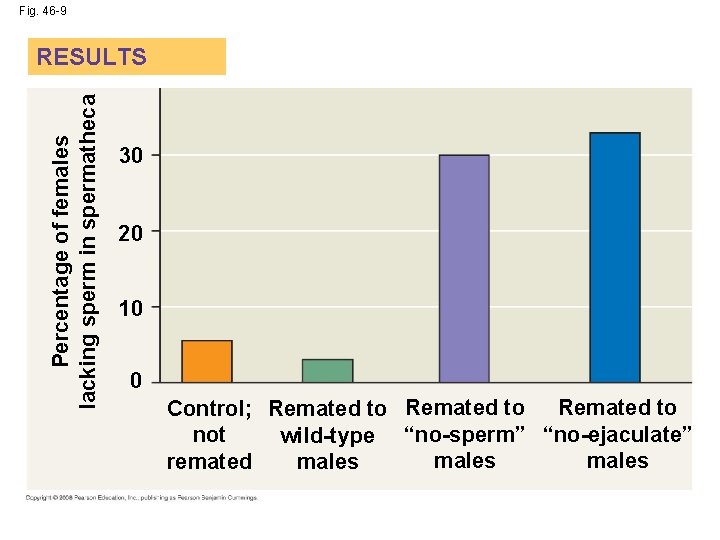
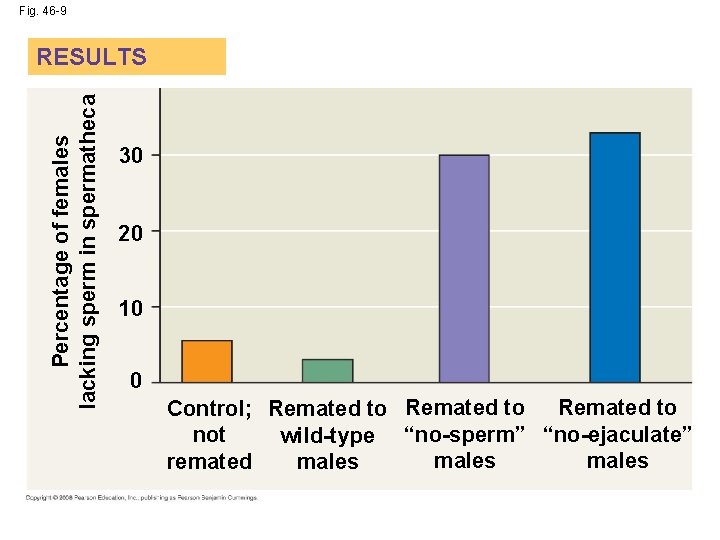
Fig. 46 -9 Percentage of females lacking sperm in spermatheca RESULTS 30 20 10 0 Control; Remated to not wild-type “no-sperm” “no-ejaculate” males remated males
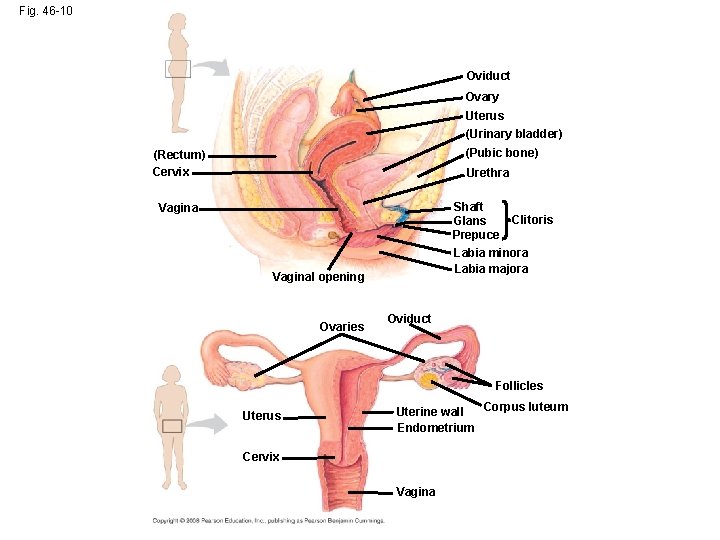
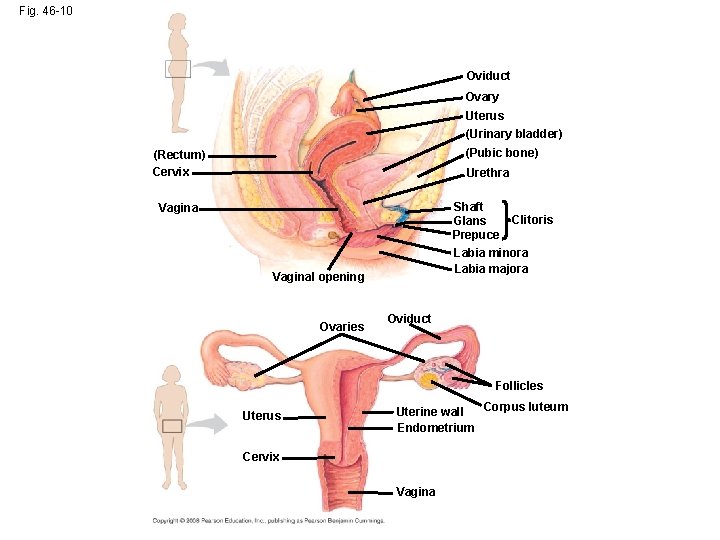
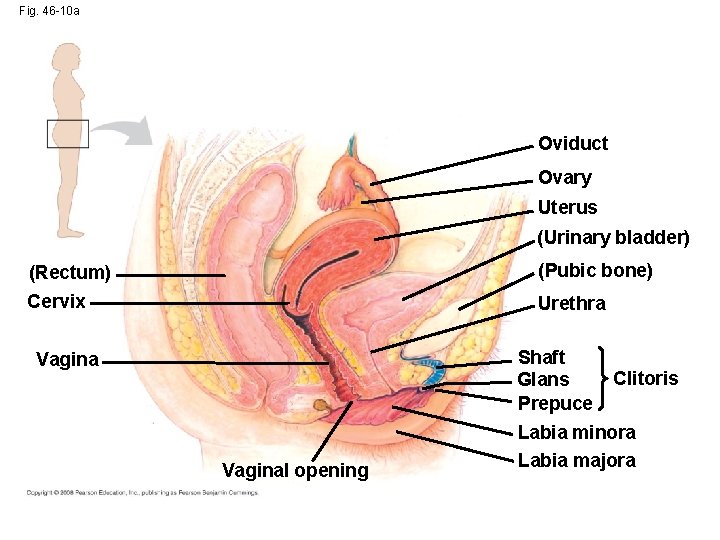
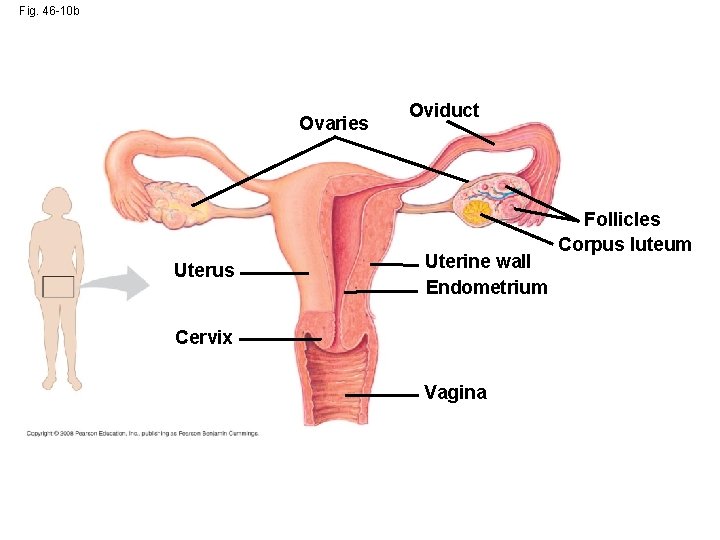
Fig. 46 -10 Oviduct Ovary Uterus (Urinary bladder) (Pubic bone) (Rectum) Cervix Urethra Shaft Glans Prepuce Vagina Labia minora Labia majora Vaginal opening Ovaries Clitoris Oviduct Follicles Uterus Corpus luteum Uterine wall Endometrium Cervix Vagina
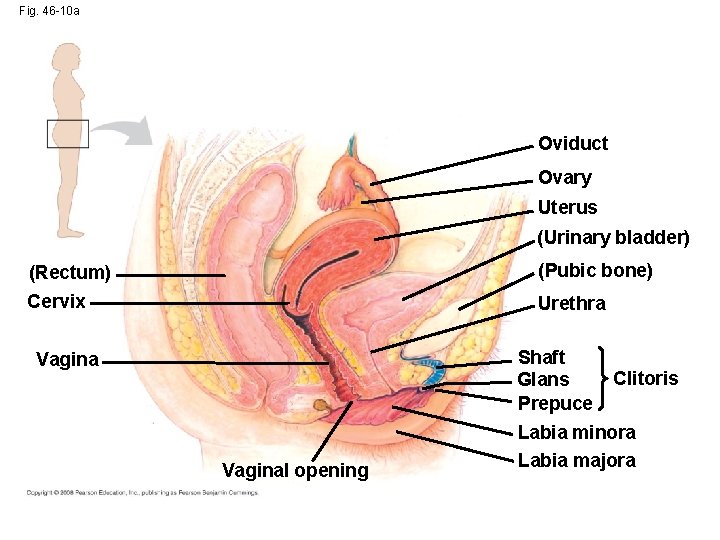
Fig. 46 -10 a Oviduct Ovary Uterus (Urinary bladder) (Rectum) (Pubic bone) Cervix Urethra Shaft Glans Prepuce Vaginal opening Clitoris Labia minora Labia majora
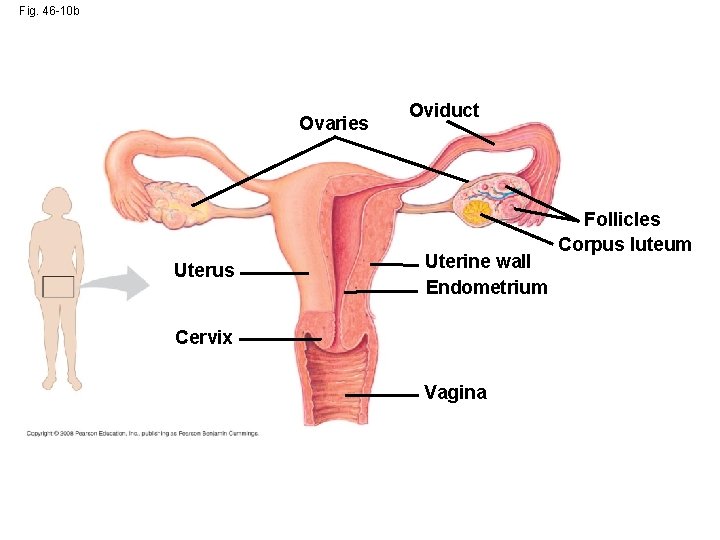
Fig. 46 -10 b Ovaries Uterus Oviduct Uterine wall Endometrium Cervix Vagina Follicles Corpus luteum
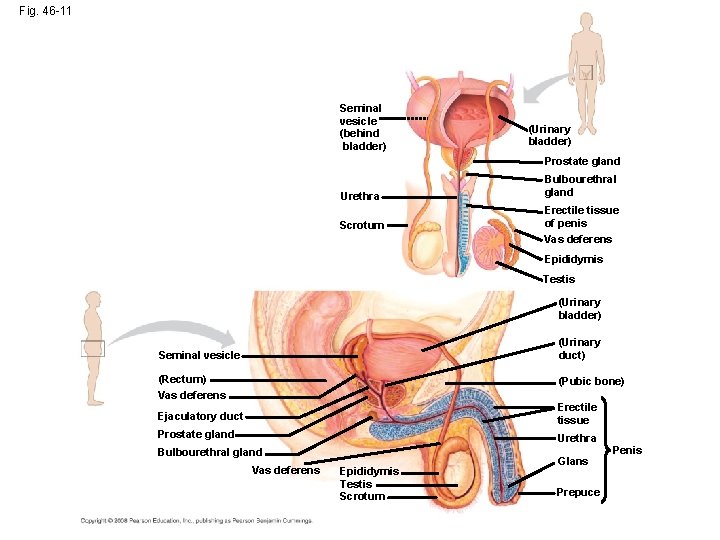
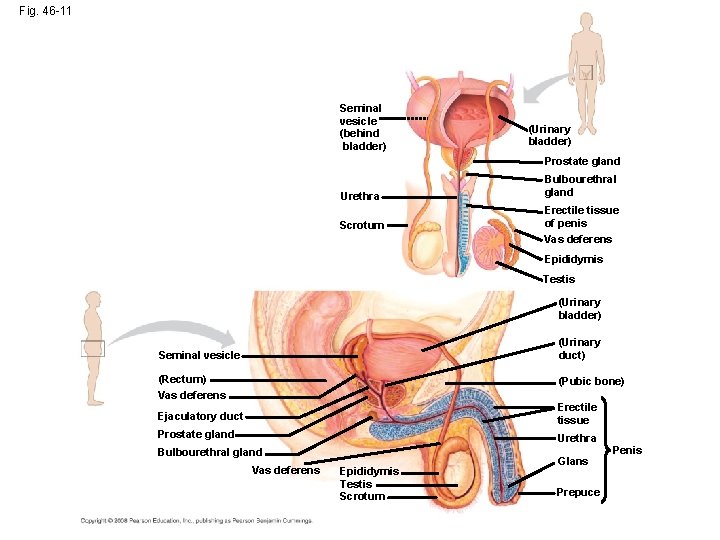
Fig. 46 -11 Seminal vesicle (behind bladder) (Urinary bladder) Prostate gland Urethra Scrotum Bulbourethral gland Erectile tissue of penis Vas deferens Epididymis Testis (Urinary bladder) (Urinary duct) Seminal vesicle (Rectum) Vas deferens (Pubic bone) Ejaculatory duct Erectile tissue Prostate gland Urethra Bulbourethral gland Vas deferens Epididymis Testis Scrotum Glans Prepuce Penis
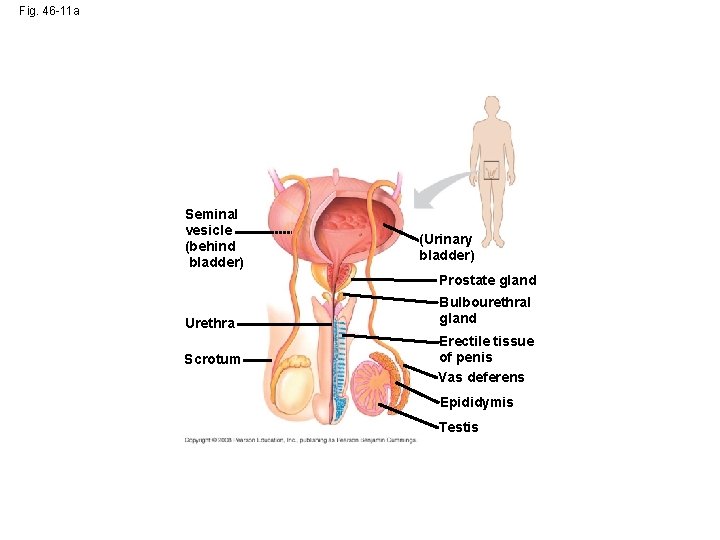
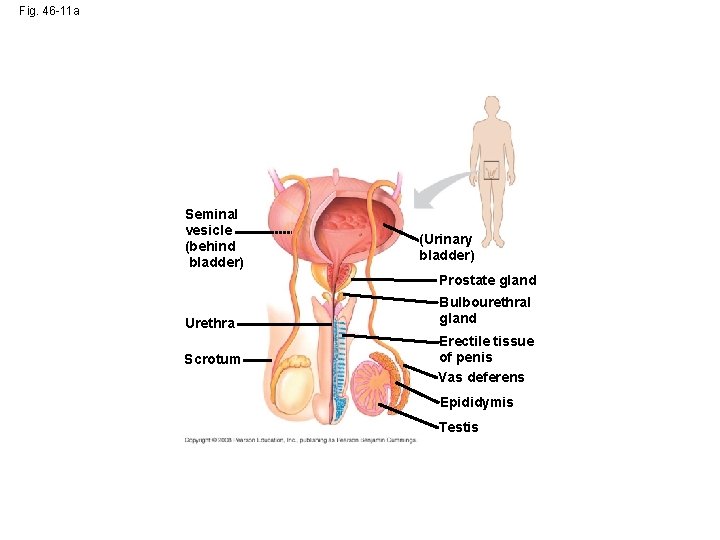
Fig. 46 -11 a Seminal vesicle (behind bladder) (Urinary bladder) Prostate gland Urethra Scrotum Bulbourethral gland Erectile tissue of penis Vas deferens Epididymis Testis
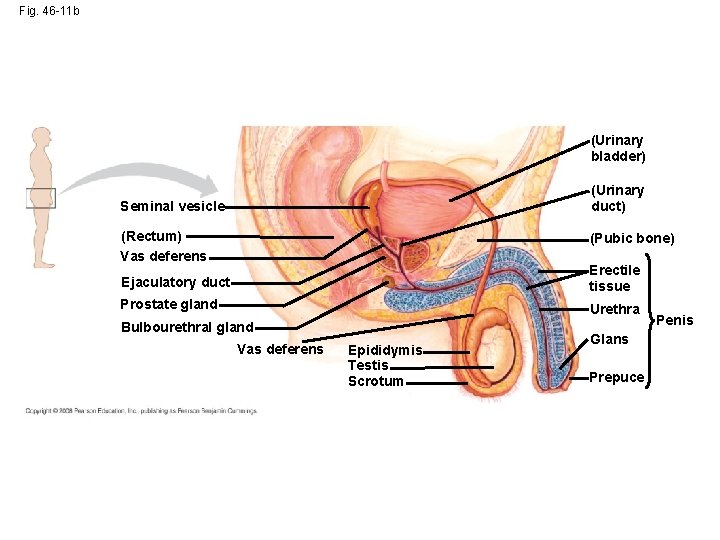
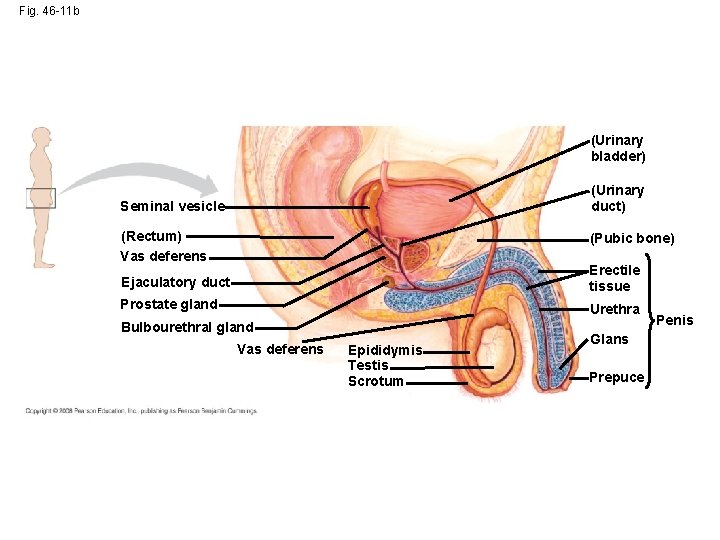
Fig. 46 -11 b (Urinary bladder) (Urinary duct) Seminal vesicle (Rectum) Vas deferens (Pubic bone) Ejaculatory duct Erectile tissue Prostate gland Urethra Bulbourethral gland Vas deferens Epididymis Testis Scrotum Glans Prepuce Penis
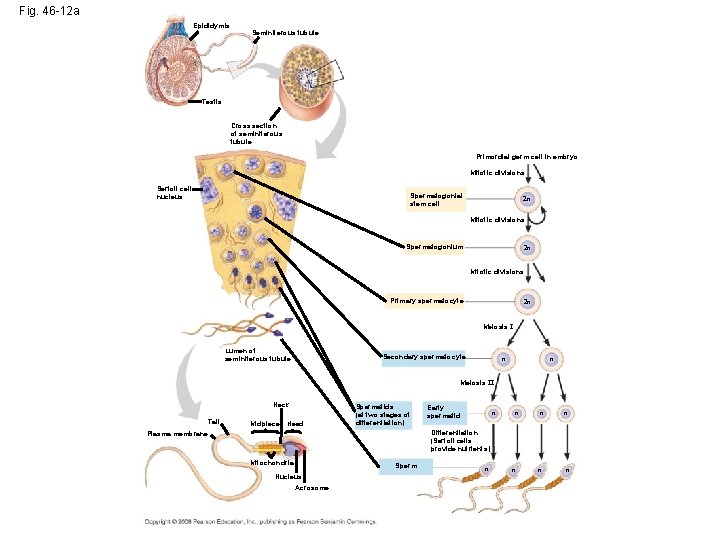
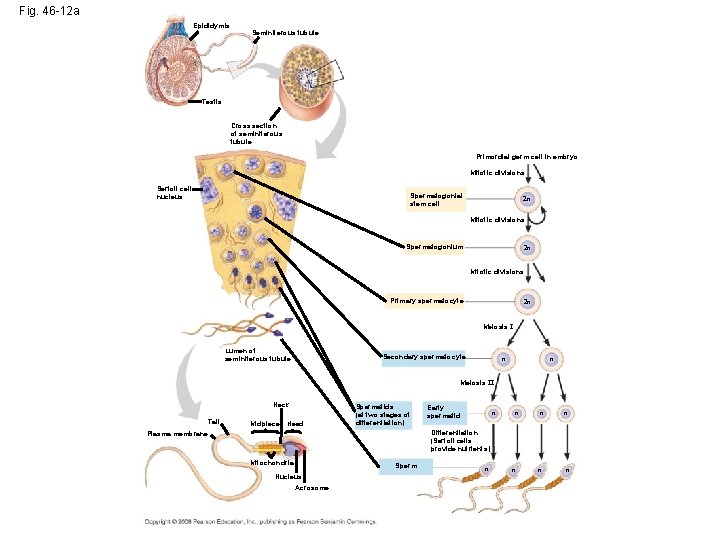
Fig. 46 -12 a Epididymis Seminiferous tubule Testis Cross section of seminiferous tubule Primordial germ cell in embryo Mitotic divisions Sertoli cell nucleus Spermatogonial stem cell 2 n Mitotic divisions Spermatogonium 2 n Mitotic divisions Primary spermatocyte 2 n Meiosis I Lumen of seminiferous tubule Secondary spermatocyte n n Meiosis II Neck Tail Midpiece Head Spermatids (at two stages of differentiation) Early spermatid n n n Differentiation (Sertoli cells provide nutrients) Plasma membrane Mitochondria Sperm Nucleus Acrosome n n
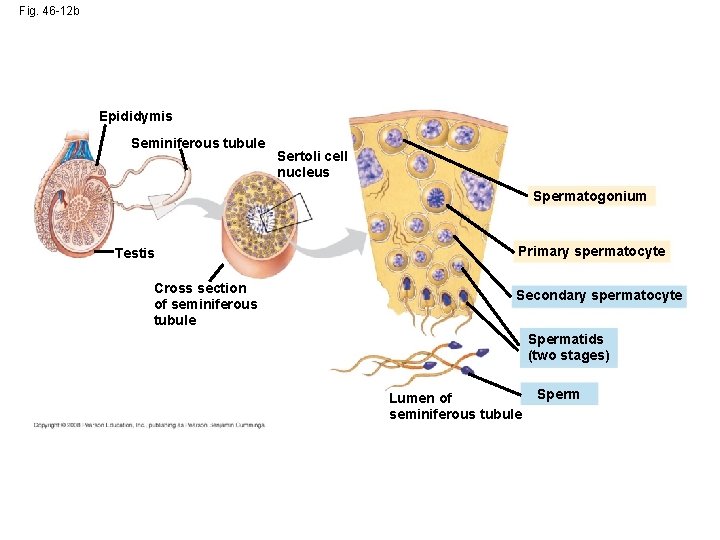
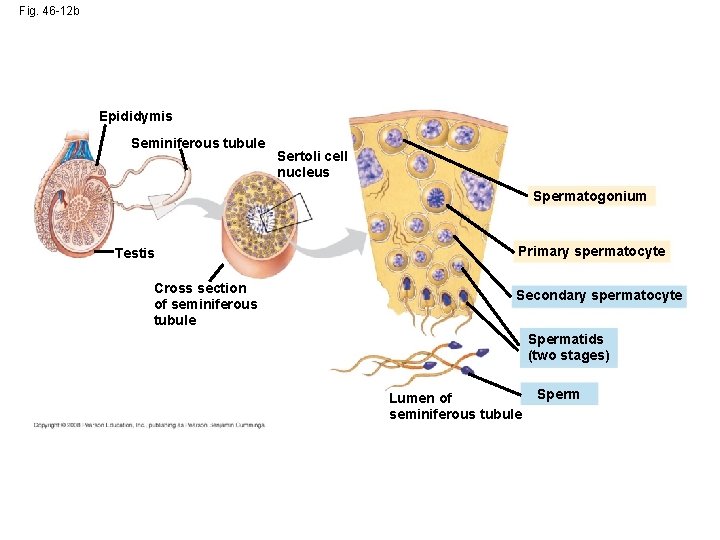
Fig. 46 -12 b Epididymis Seminiferous tubule Sertoli cell nucleus Spermatogonium Testis Cross section of seminiferous tubule Primary spermatocyte Secondary spermatocyte Spermatids (two stages) Lumen of seminiferous tubule Sperm
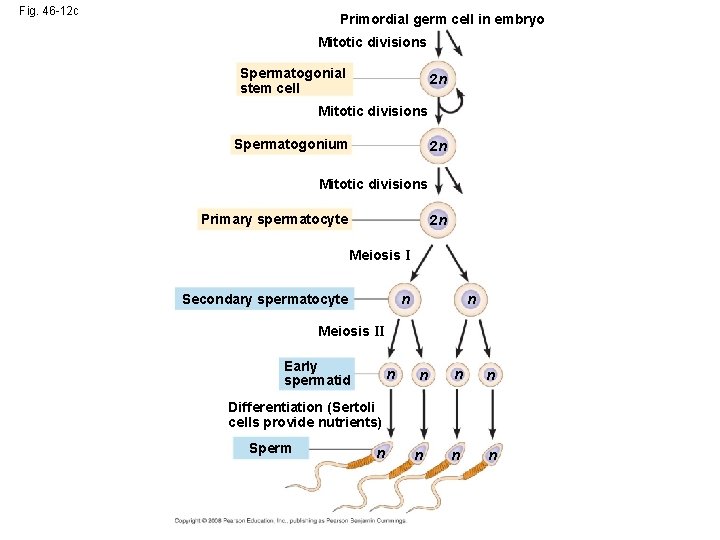
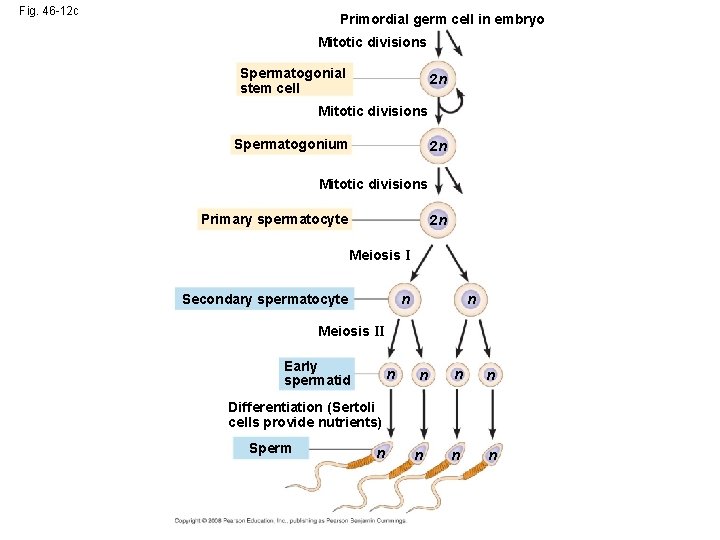
Fig. 46 -12 c Primordial germ cell in embryo Mitotic divisions Spermatogonial stem cell 2 n Mitotic divisions Spermatogonium 2 n Mitotic divisions Primary spermatocyte 2 n Meiosis I Secondary spermatocyte n n Meiosis II Early spermatid n n n Differentiation (Sertoli cells provide nutrients) Sperm n n
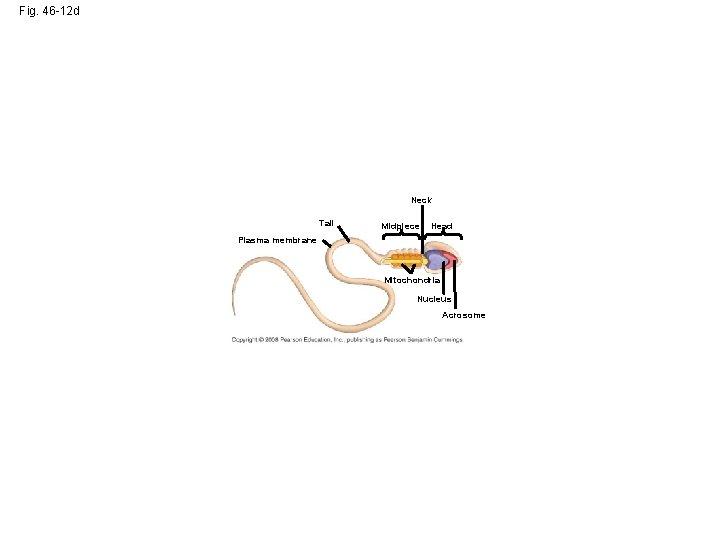
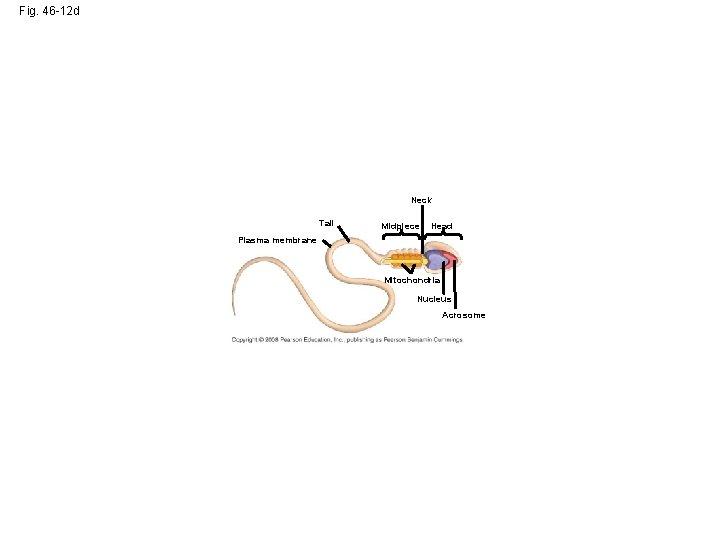
Fig. 46 -12 d Neck Tail Midpiece Head Plasma membrane Mitochondria Nucleus Acrosome
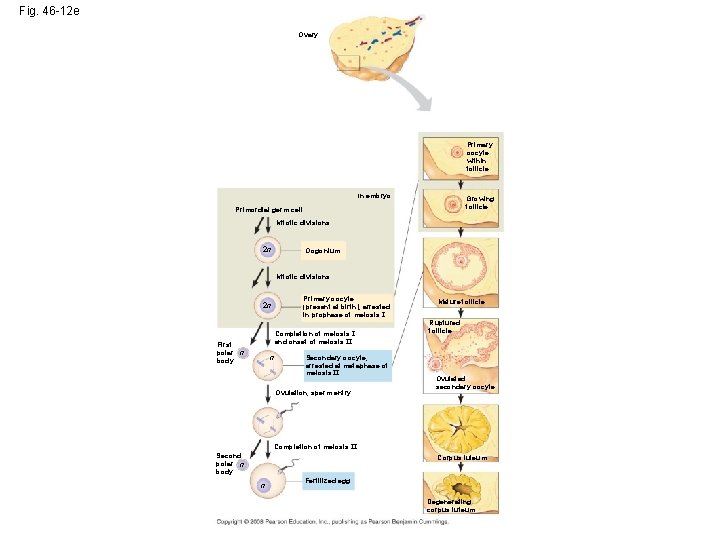
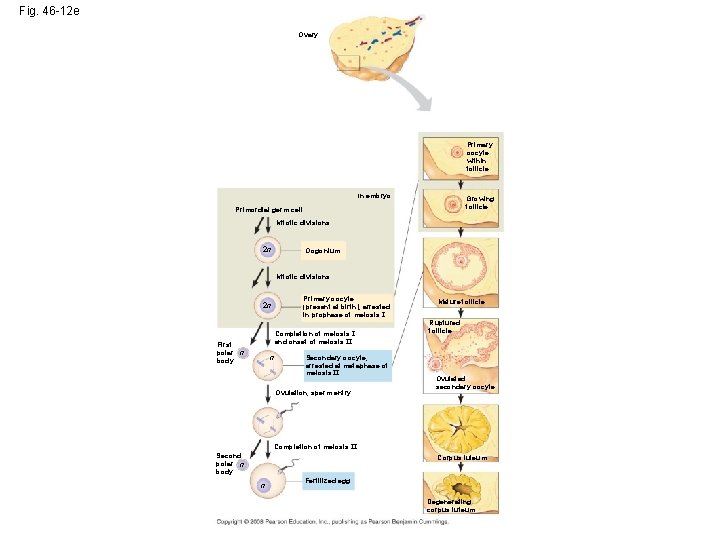
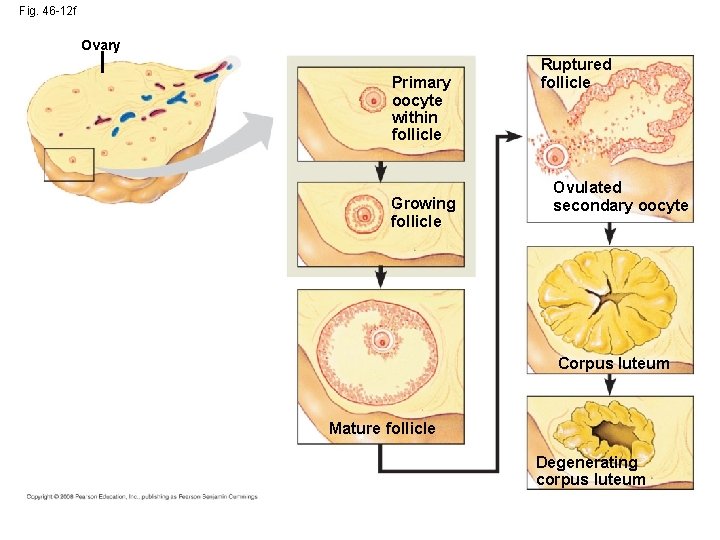
Fig. 46 -12 e Ovary Primary oocyte within follicle In embryo Growing follicle Primordial germ cell Mitotic divisions 2 n Oogonium Mitotic divisions Primary oocyte (present at birth), arrested in prophase of meiosis I 2 n Completion of meiosis I and onset of meiosis II First polar n body n Secondary oocyte, arrested at metaphase of meiosis II Ovulation, sperm entry Mature follicle Ruptured follicle Ovulated secondary oocyte Completion of meiosis II Second polar n body Corpus luteum n Fertilized egg Degenerating corpus luteum
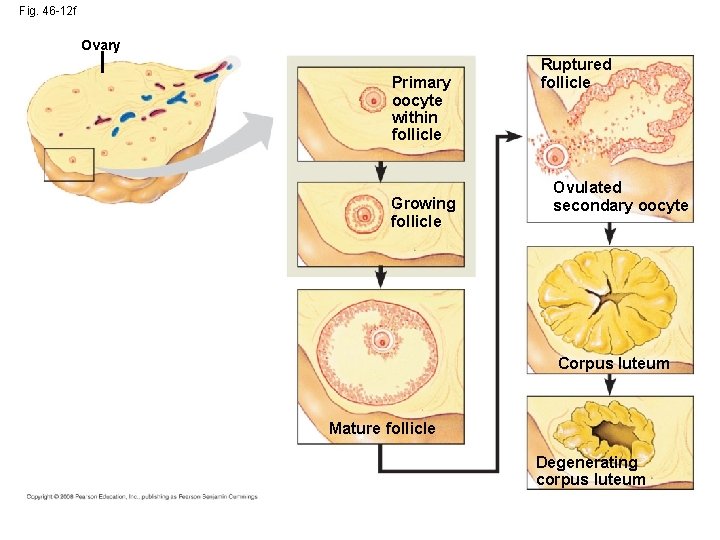
Fig. 46 -12 f Ovary Primary oocyte within follicle Growing follicle Ruptured follicle Ovulated secondary oocyte Corpus luteum Mature follicle Degenerating corpus luteum
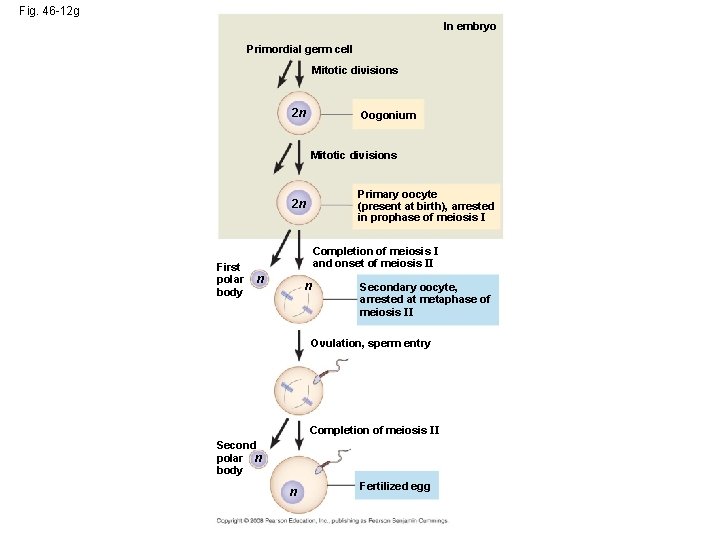
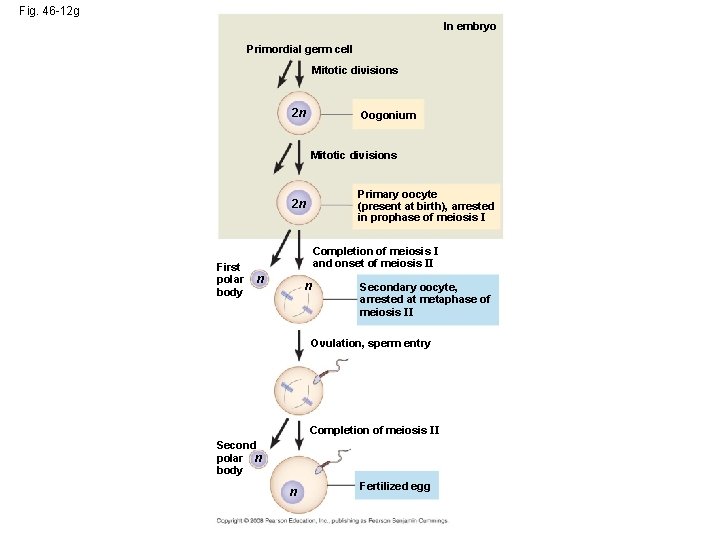
Fig. 46 -12 g In embryo Primordial germ cell Mitotic divisions 2 n Oogonium Mitotic divisions Primary oocyte (present at birth), arrested in prophase of meiosis I 2 n First polar body Completion of meiosis I and onset of meiosis II n n Secondary oocyte, arrested at metaphase of meiosis II Ovulation, sperm entry Completion of meiosis II Second polar n body n Fertilized egg
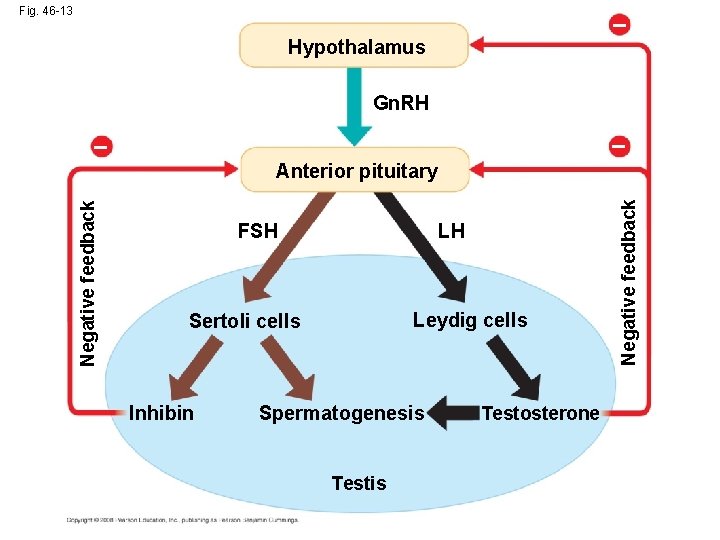
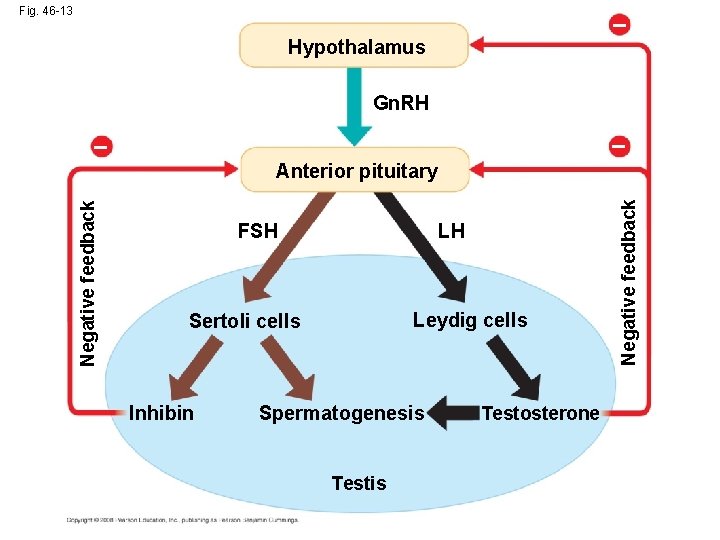
Fig. 46 -13 – Hypothalamus Gn. RH – – FSH LH Leydig cells Sertoli cells Inhibin Spermatogenesis Testosterone Negative feedback Anterior pituitary
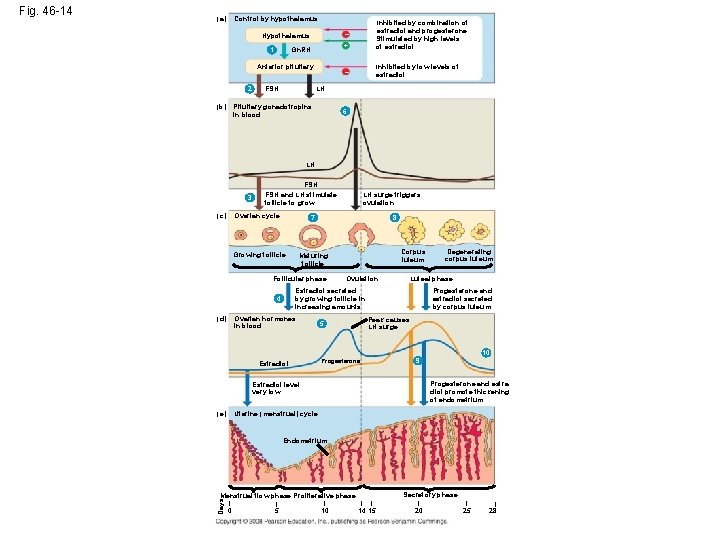
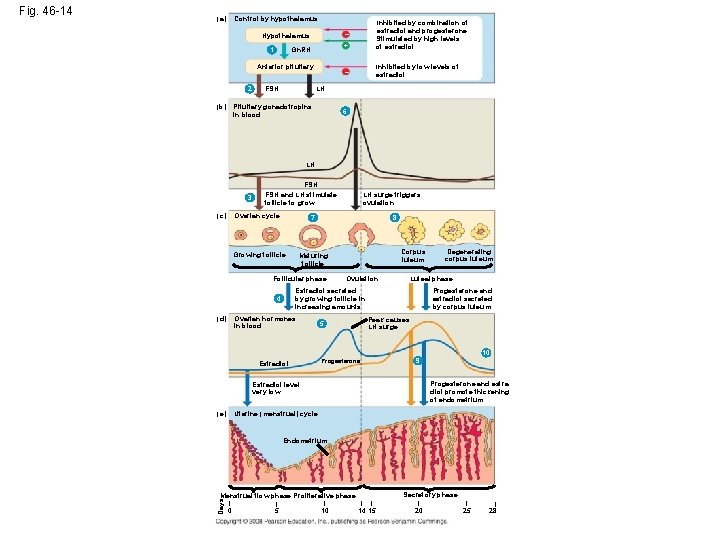
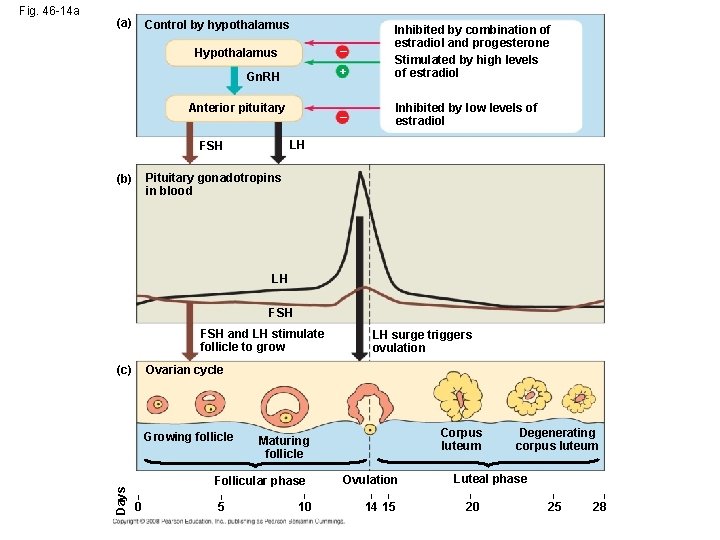
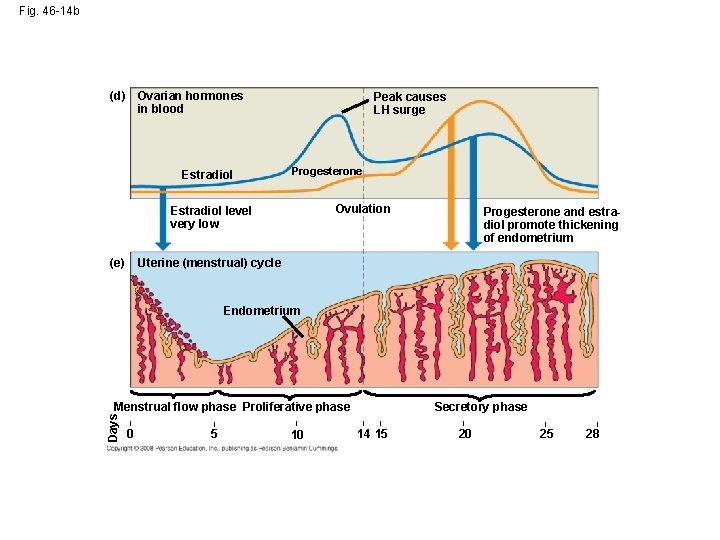
Control by hypothalamus (a) Hypothalamus – Gn. RH + Inhibited by combination of estradiol and progesterone Stimulated by high levels of estradiol – Inhibited by low levels of estradiol 1 Anterior pituitary 2 (b) FSH LH Pituitary gonadotropins in blood 6 LH FSH 3 (c) FSH and LH stimulate follicle to grow Ovarian cycle 8 Corpus luteum Maturing follicle Follicular phase Ovulation Ovarian hormones in blood Degenerating corpus luteum Luteal phase Estradiol secreted by growing follicle in increasing amounts 4 (d) LH surge triggers ovulation 7 Growing follicle Progesterone and estradiol secreted by corpus luteum Peak causes LH surge 5 10 Estradiol 9 Progesterone and estradiol promote thickening of endometrium Estradiol level very low Uterine (menstrual) cycle (e) Endometrium Secretory phase Menstrual flow phase Proliferative phase Days Fig. 46 -14 | 0 | 5 | 10 | | 14 15 | 20 | 25 | 28
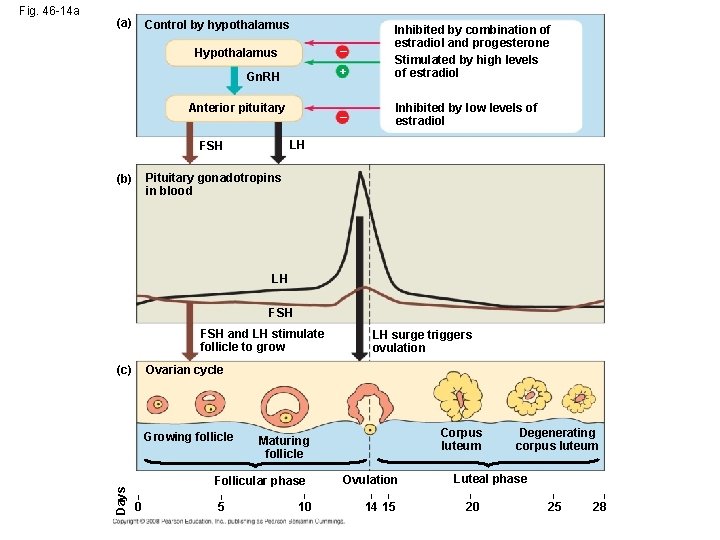
(a) Control by hypothalamus Hypothalamus – Gn. RH + Inhibited by combination of estradiol and progesterone Stimulated by high levels of estradiol – Inhibited by low levels of estradiol Anterior pituitary LH FSH Pituitary gonadotropins in blood (b) LH FSH and LH stimulate follicle to grow LH surge triggers ovulation Ovarian cycle (c) Growing follicle Days Fig. 46 -14 a Corpus luteum Maturing follicle Follicular phase | | | 0 5 10 Ovulation | | 14 15 Degenerating corpus luteum Luteal phase | 20 | 25 | 28
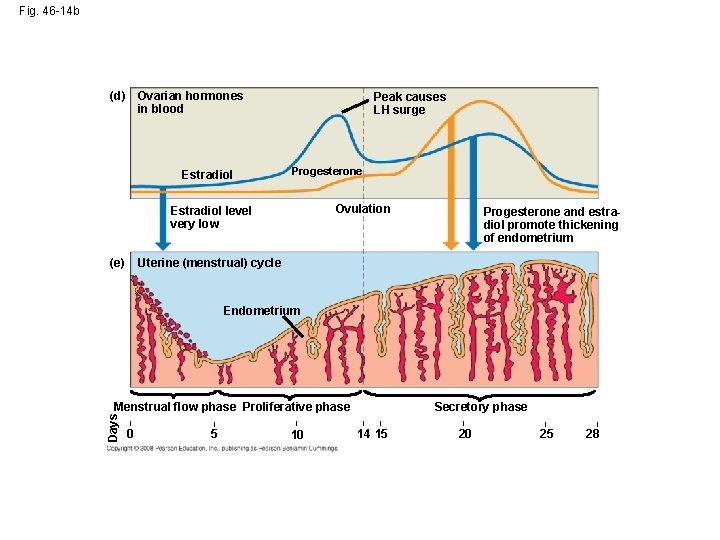
Fig. 46 -14 b (d) Ovarian hormones in blood Estradiol Peak causes LH surge Progesterone Ovulation Estradiol level very low (e) Progesterone and estradiol promote thickening of endometrium Uterine (menstrual) cycle Endometrium Days Menstrual flow phase Proliferative phase | 0 | | 5 10 Secretory phase | | 14 15 | 20 | 25 | 28
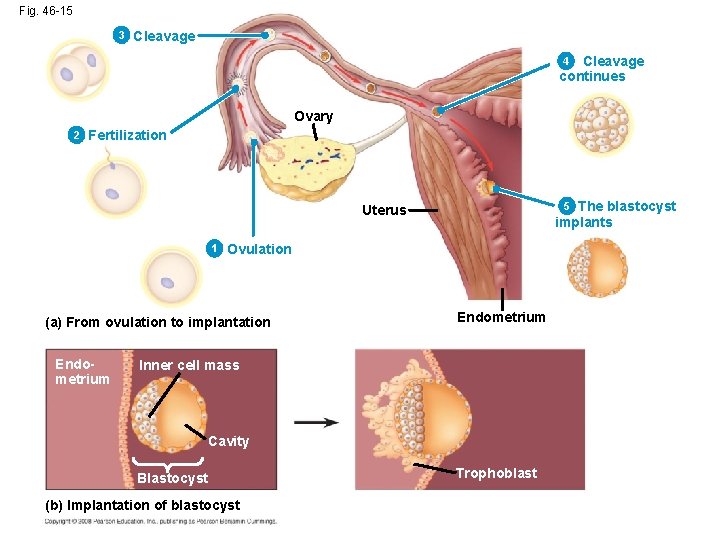
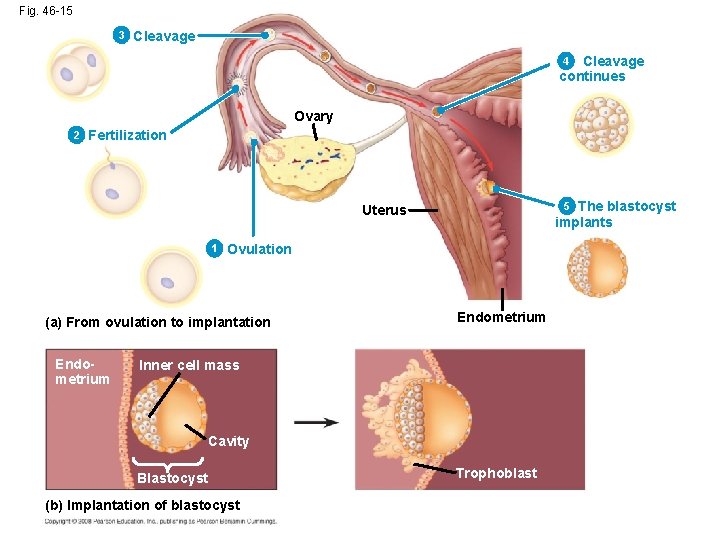
Fig. 46 -15 3 Cleavage continues 4 Ovary 2 Fertilization The blastocyst implants 5 Uterus 1 Ovulation (a) From ovulation to implantation Endometrium Inner cell mass Cavity Blastocyst (b) Implantation of blastocyst Trophoblast
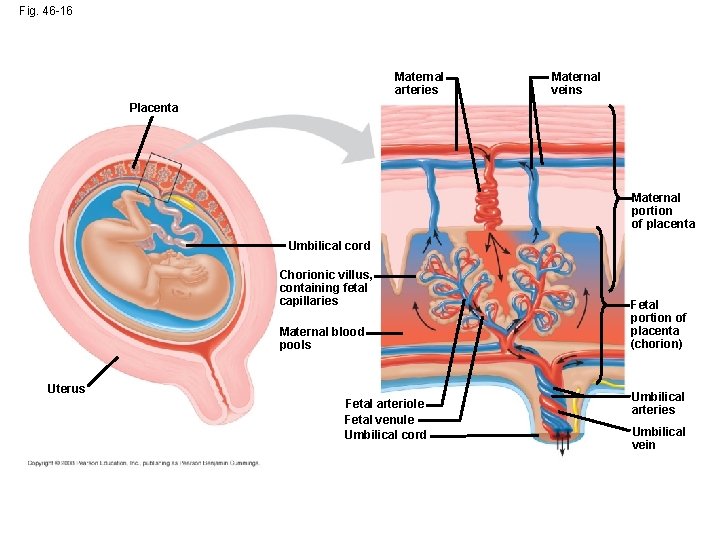
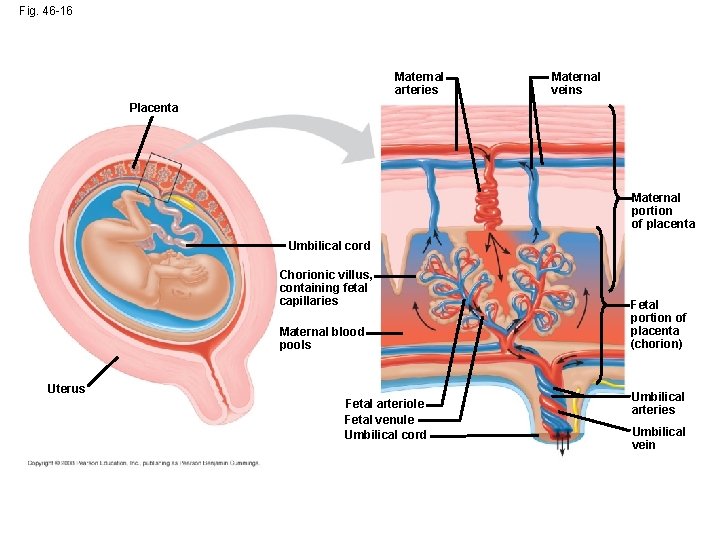
Fig. 46 -16 Maternal arteries Maternal veins Placenta Maternal portion of placenta Umbilical cord Chorionic villus, containing fetal capillaries Maternal blood pools Uterus Fetal arteriole Fetal venule Umbilical cord Fetal portion of placenta (chorion) Umbilical arteries Umbilical vein
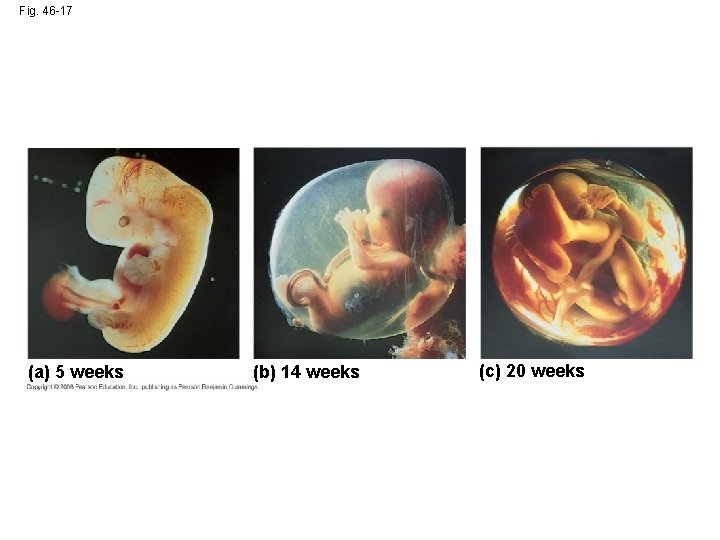
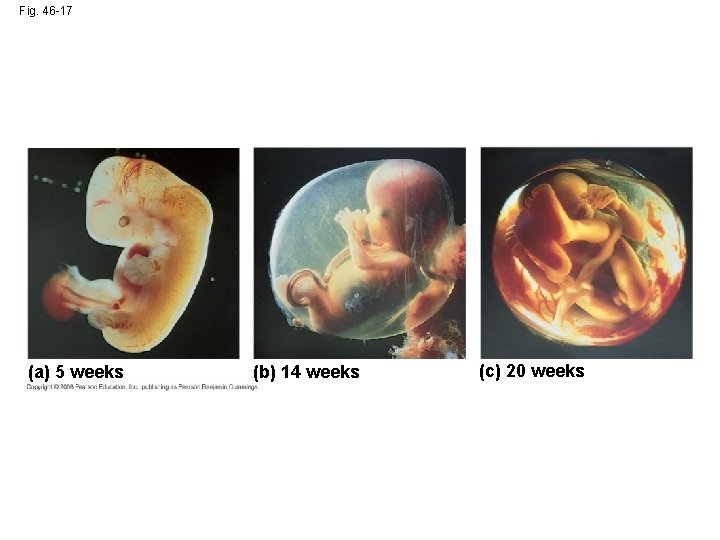
Fig. 46 -17 (a) 5 weeks (b) 14 weeks (c) 20 weeks
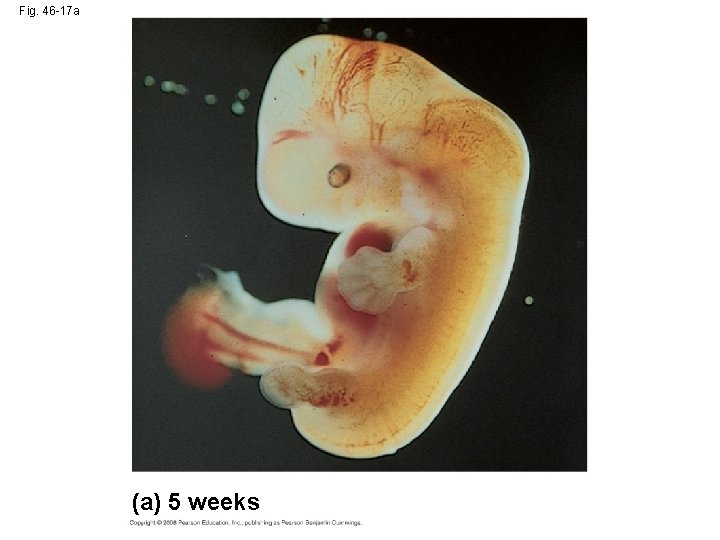
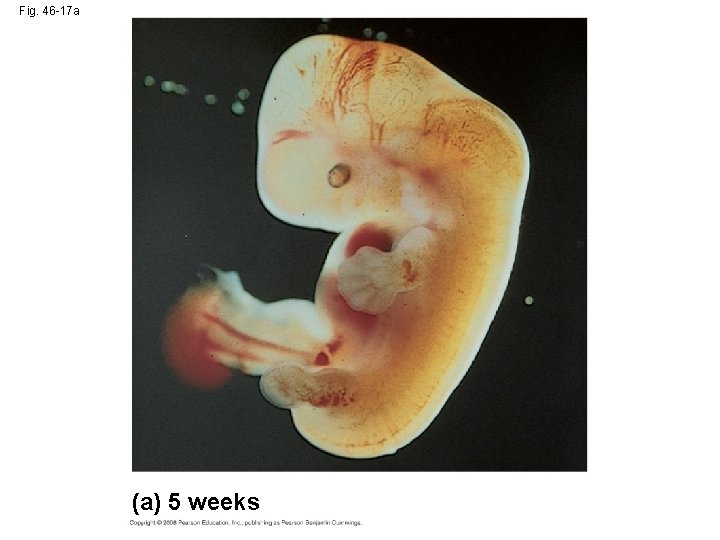
Fig. 46 -17 a (a) 5 weeks
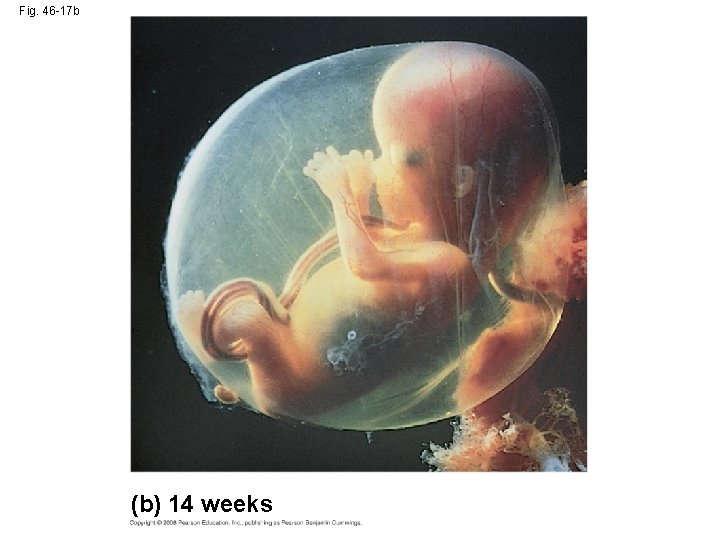
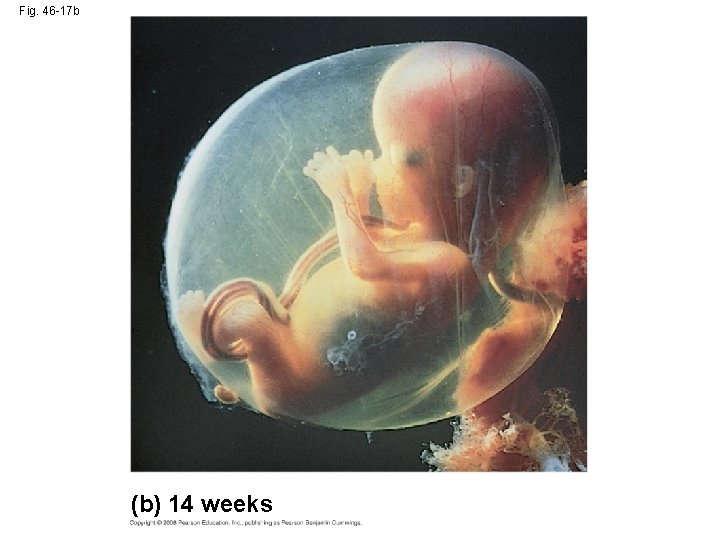
Fig. 46 -17 b (b) 14 weeks
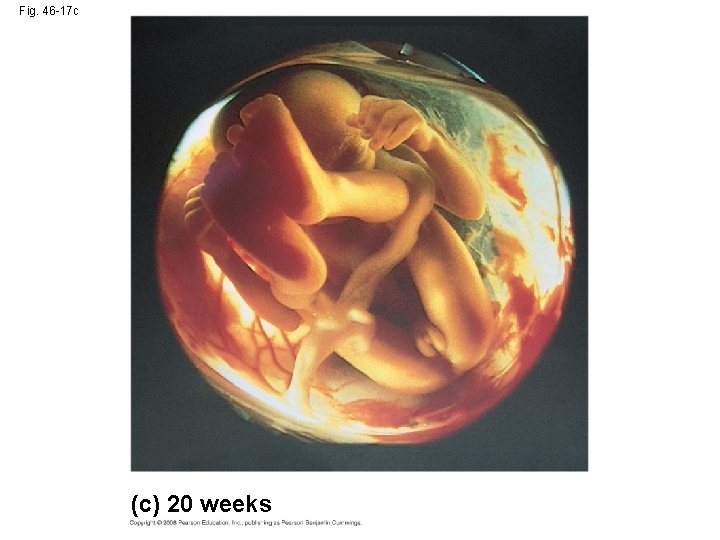
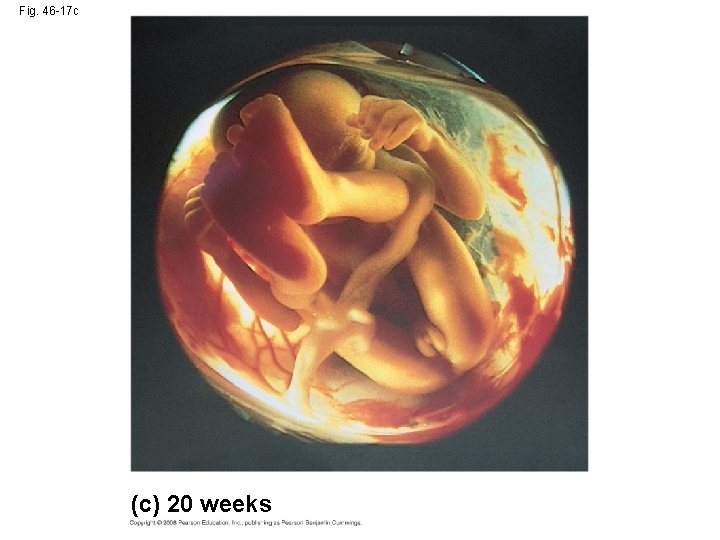
Fig. 46 -17 c (c) 20 weeks
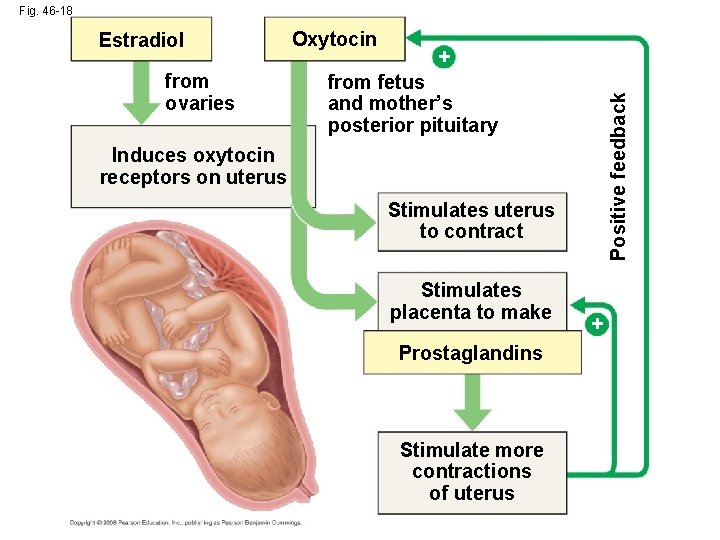
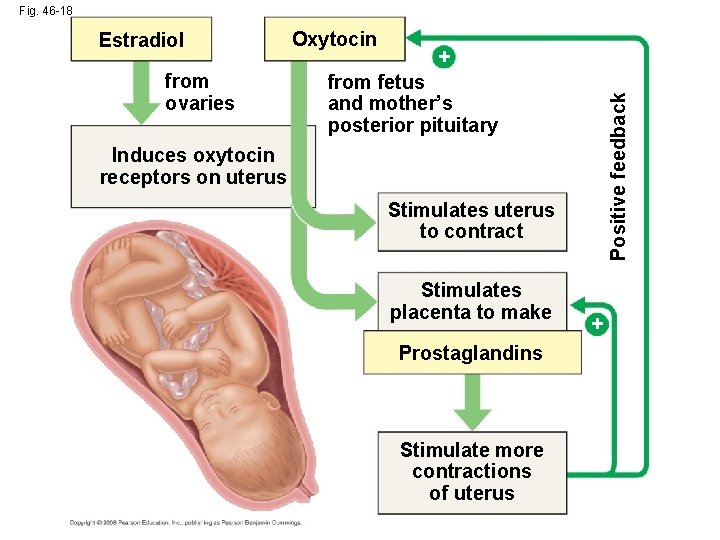
Fig. 46 -18 from ovaries Oxytocin + from fetus and mother’s posterior pituitary Positive feedback Estradiol Induces oxytocin receptors on uterus Stimulates uterus to contract Stimulates placenta to make Prostaglandins Stimulate more contractions of uterus +
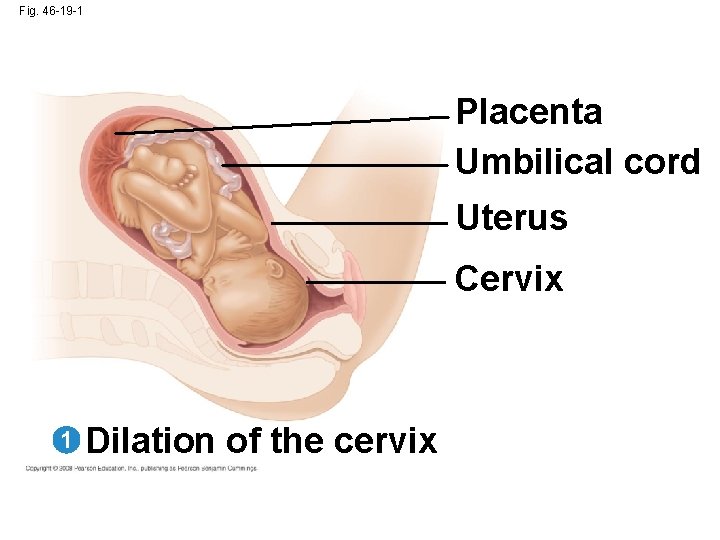
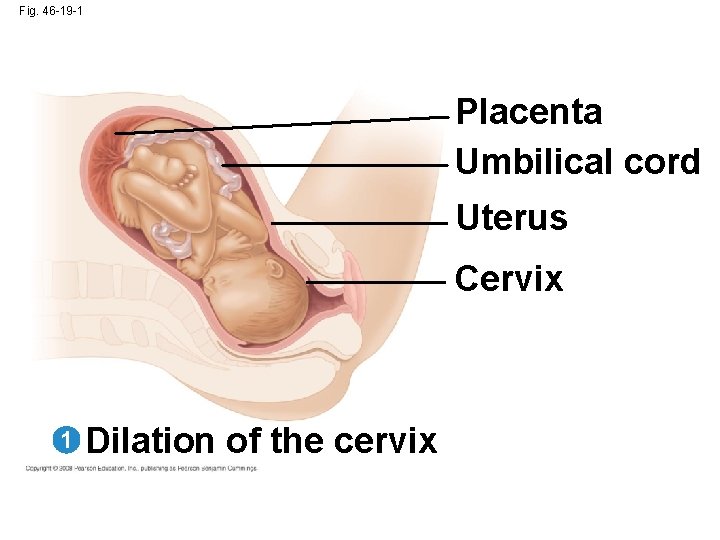
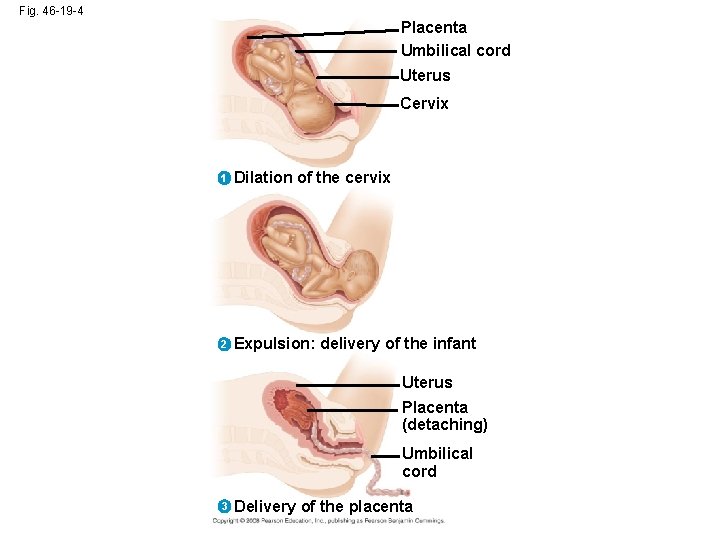
Fig. 46 -19 -1 Placenta Umbilical cord Uterus Cervix 1 Dilation of the cervix
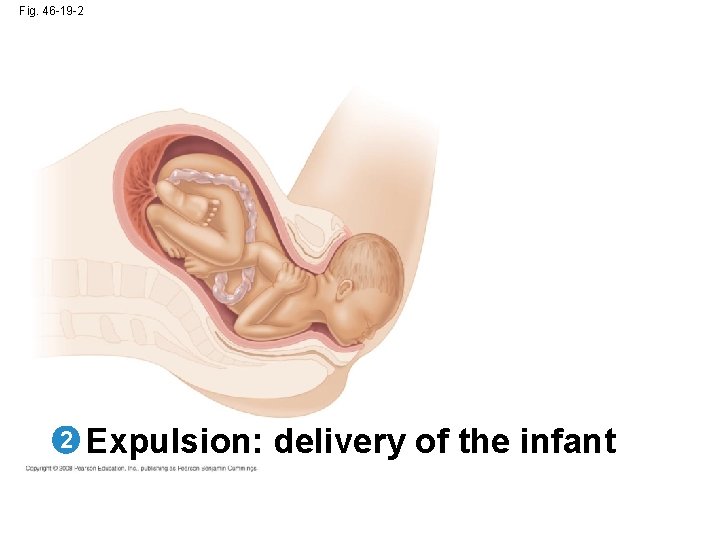
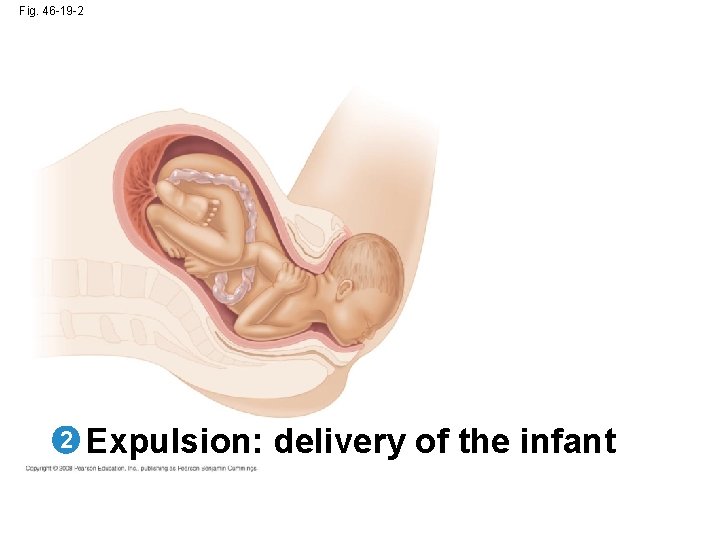
Fig. 46 -19 -2 2 Expulsion: delivery of the infant
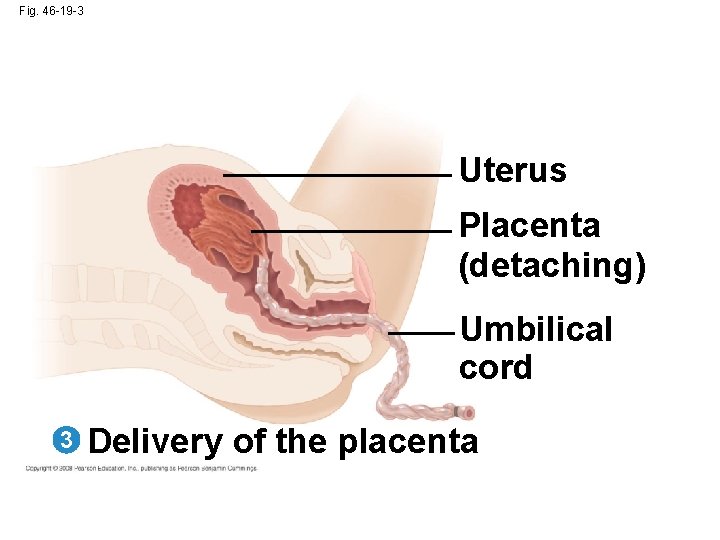
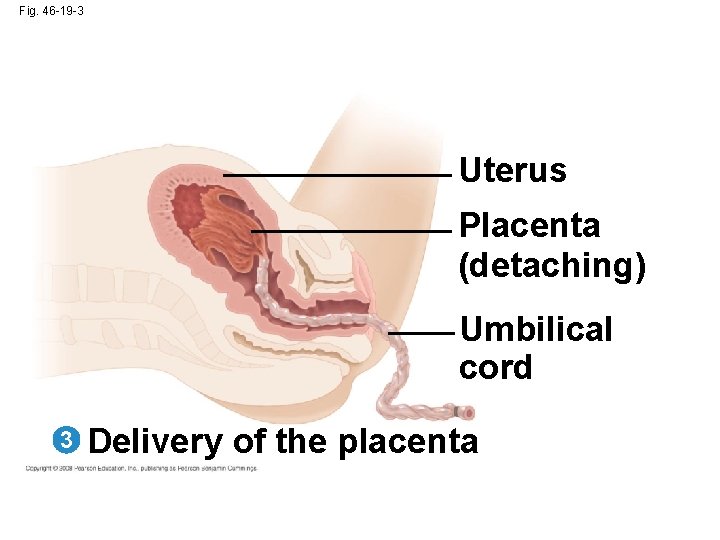
Fig. 46 -19 -3 Uterus Placenta (detaching) Umbilical cord 3 Delivery of the placenta
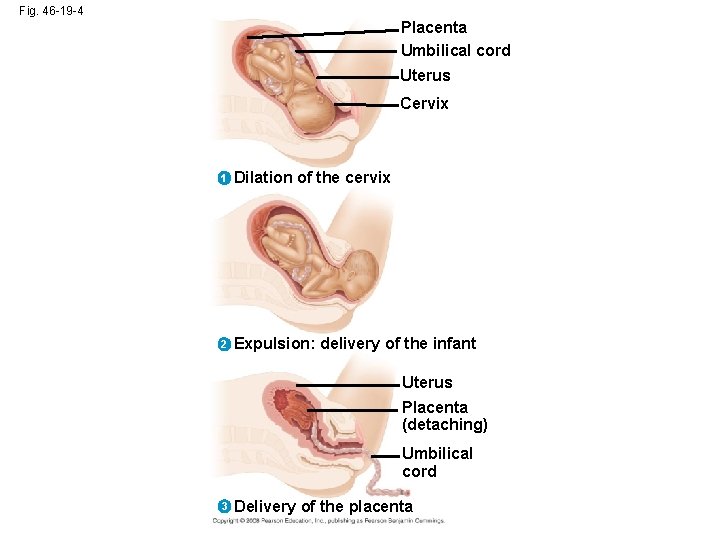
Fig. 46 -19 -4 Placenta Umbilical cord Uterus Cervix 1 Dilation of the cervix 2 Expulsion: delivery of the infant Uterus Placenta (detaching) Umbilical cord 3 Delivery of the placenta
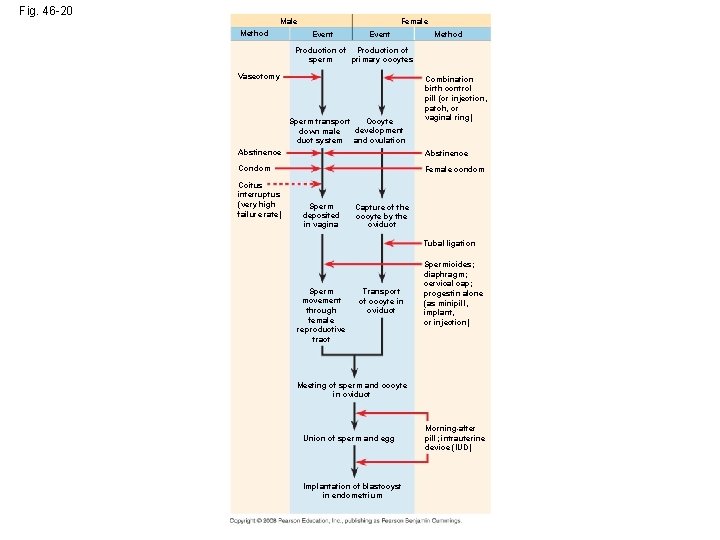
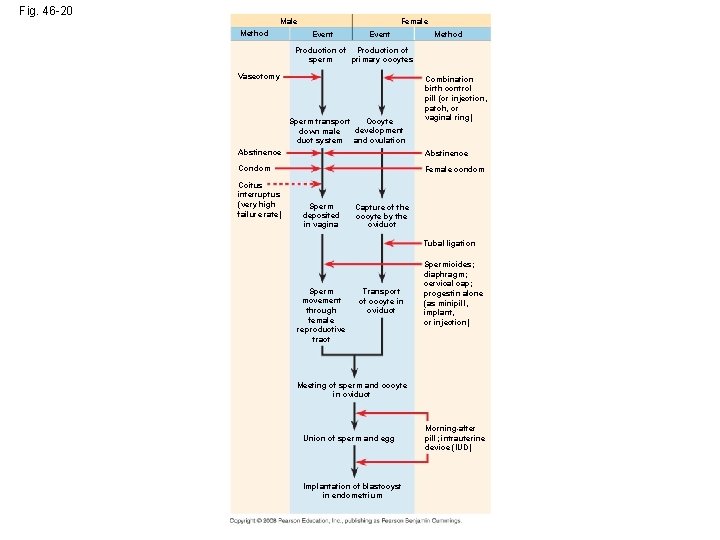
Fig. 46 -20 Male Method Female Event Method Production of sperm primary oocytes Vasectomy Oocyte Sperm transport development down male duct system and ovulation Combination birth control pill (or injection, patch, or vaginal ring) Abstinence Condom Female condom Coitus interruptus (very high failure rate) Sperm deposited in vagina Capture of the oocyte by the oviduct Tubal ligation Sperm movement through female reproductive tract Transport of oocyte in oviduct Spermicides; diaphragm; cervical cap; progestin alone (as minipill, implant, or injection) Meeting of sperm and oocyte in oviduct Union of sperm and egg Implantation of blastocyst in endometrium Morning-after pill; intrauterine device (IUD)
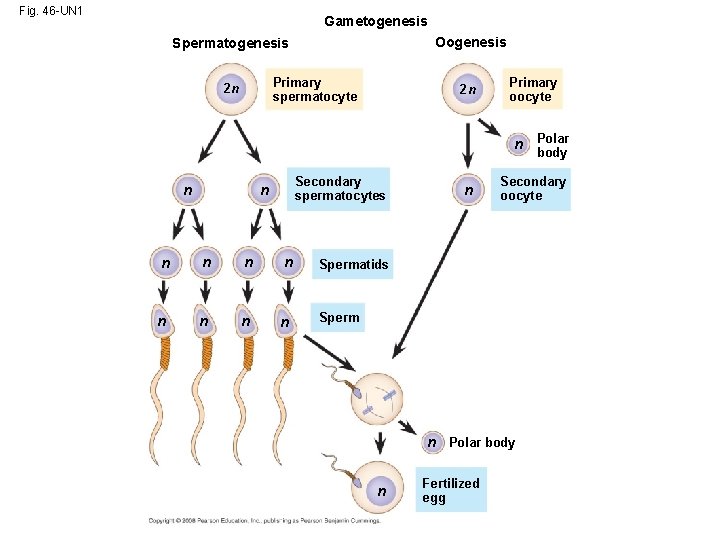
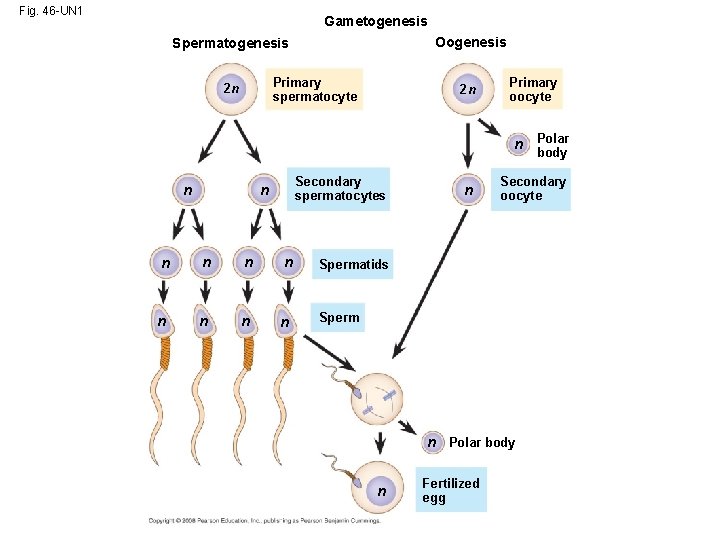
Fig. 46 -UN 1 Gametogenesis Oogenesis Spermatogenesis Primary spermatocyte 2 n 2 n Primary oocyte n Polar body n Secondary spermatocytes n n n n n Secondary oocyte Spermatids Sperm n Polar body n Fertilized egg
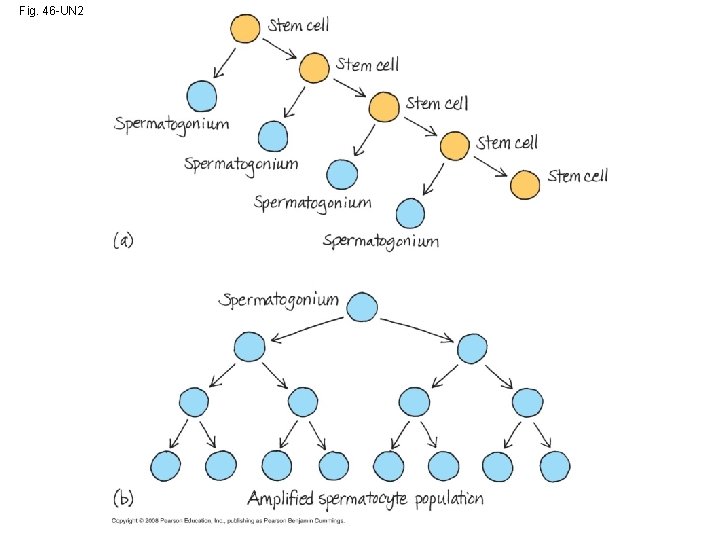
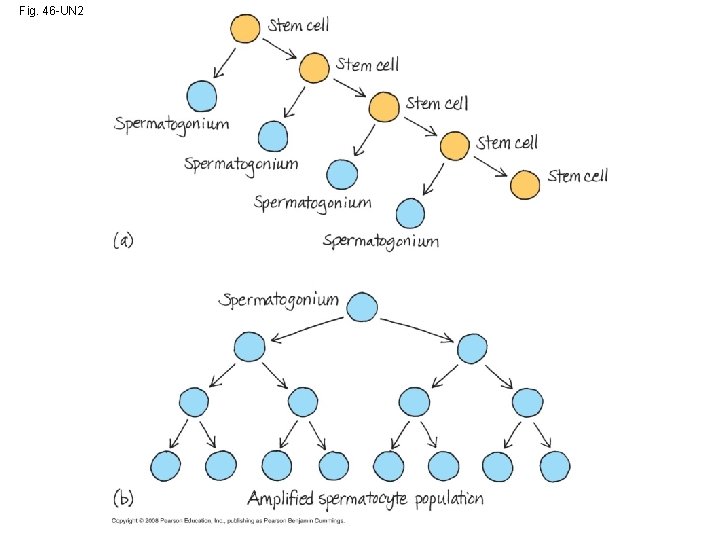
Fig. 46 -UN 2