Chapter 19 Special Senses Vision Fig 19 9


- Slides: 35
Chapter 19 Special Senses: Vision
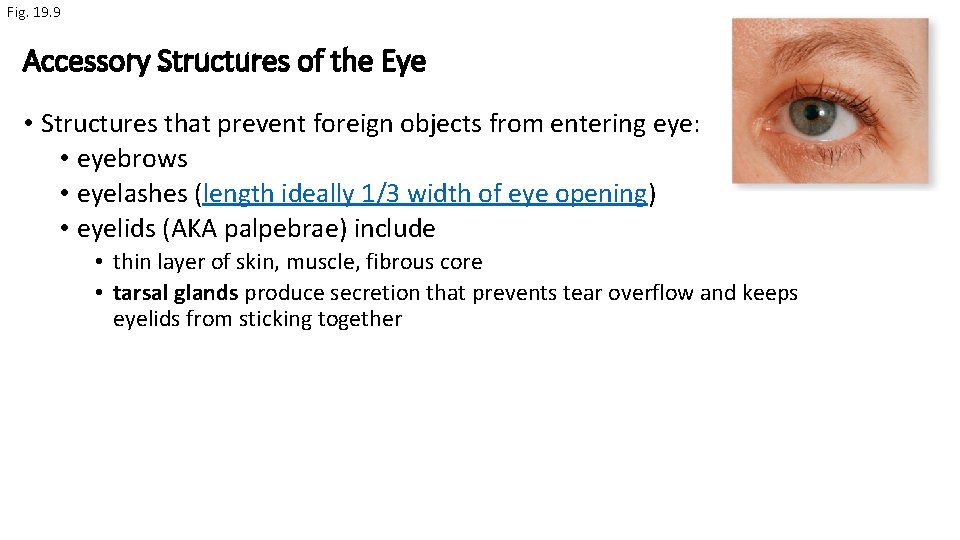
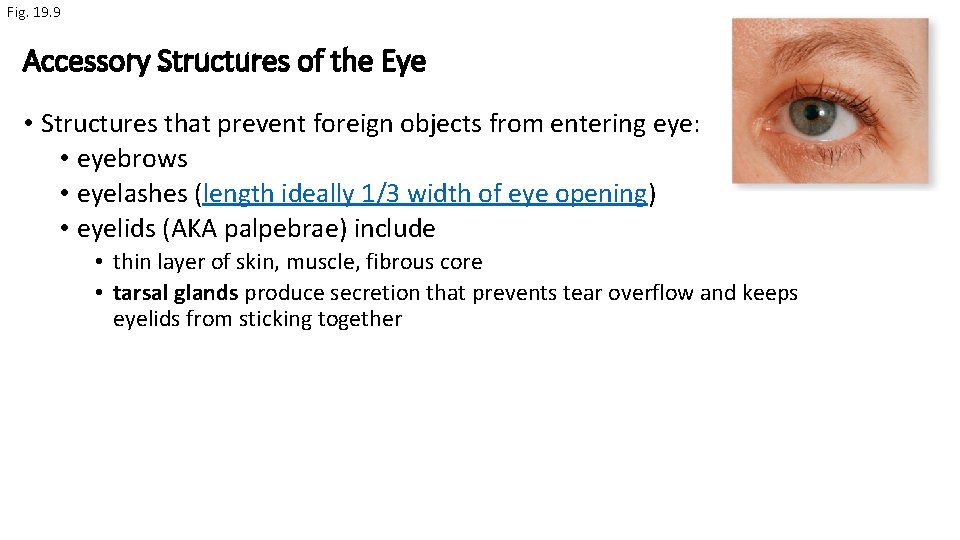
Fig. 19. 9 Accessory Structures of the Eye • Structures that prevent foreign objects from entering eye: • eyebrows • eyelashes (length ideally 1/3 width of eye opening) • eyelids (AKA palpebrae) include • thin layer of skin, muscle, fibrous core • tarsal glands produce secretion that prevents tear overflow and keeps eyelids from sticking together
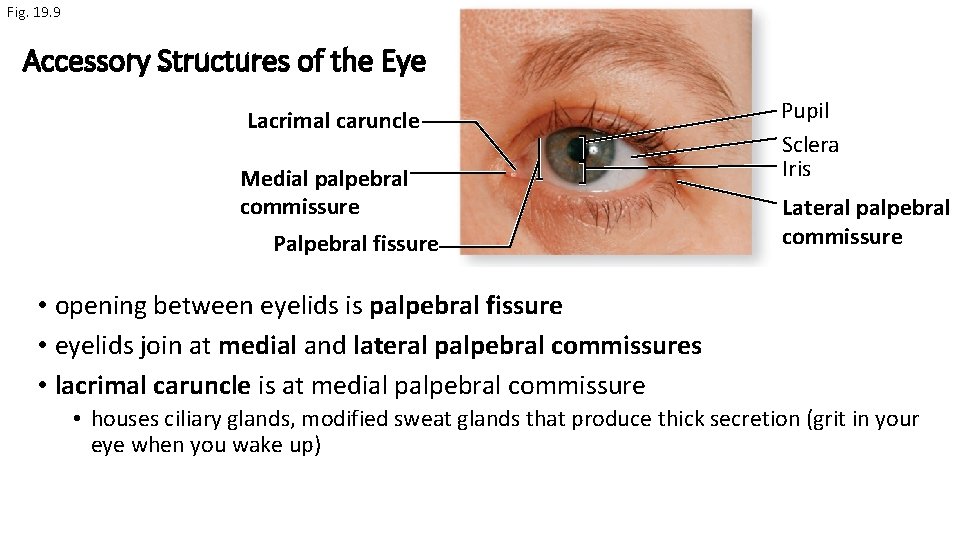
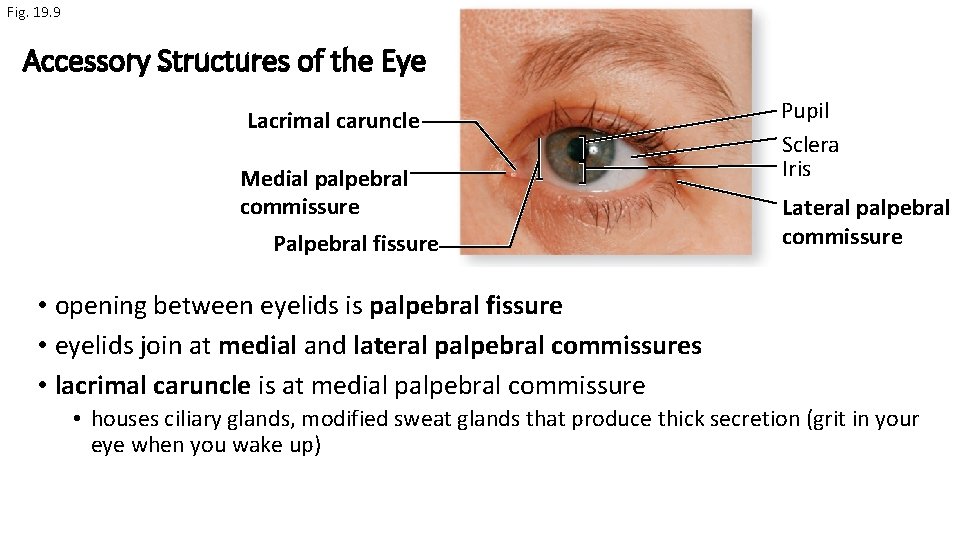
Fig. 19. 9 Accessory Structures of the Eye Lacrimal caruncle Medial palpebral commissure Palpebral fissure Pupil Sclera Iris Lateral palpebral commissure • opening between eyelids is palpebral fissure • eyelids join at medial and lateral palpebral commissures • lacrimal caruncle is at medial palpebral commissure • houses ciliary glands, modified sweat glands that produce thick secretion (grit in your eye when you wake up)
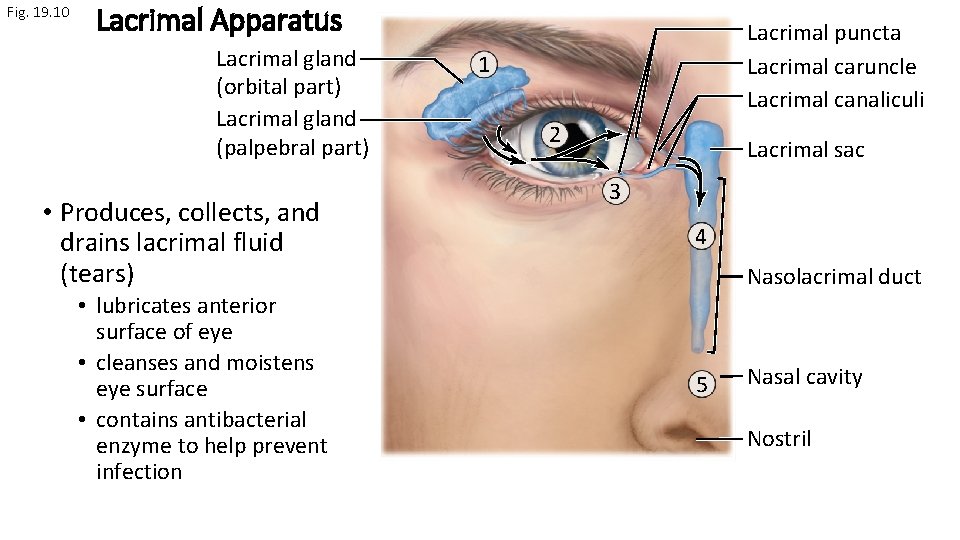
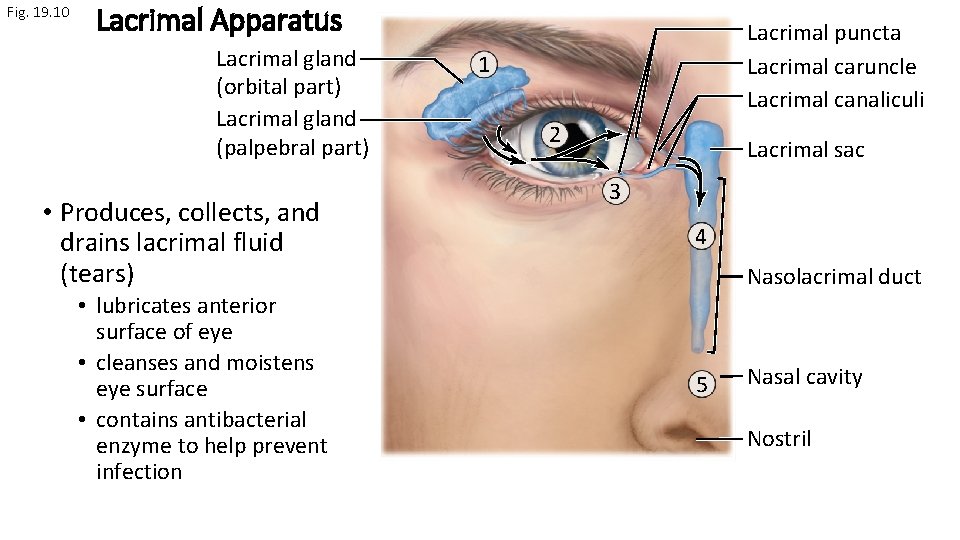
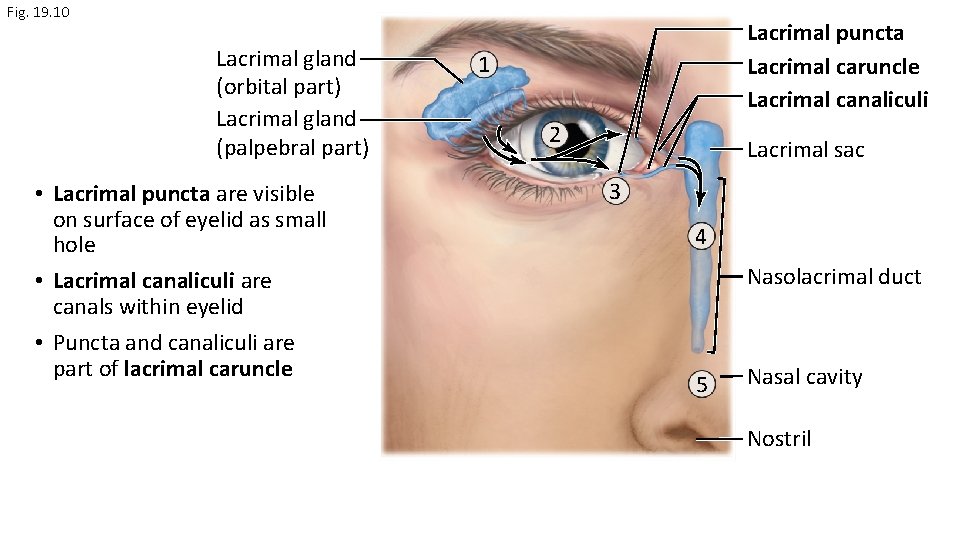
Fig. 19. 10 Lacrimal Apparatus Lacrimal gland (orbital part) Lacrimal gland (palpebral part) • Produces, collects, and drains lacrimal fluid (tears) • lubricates anterior surface of eye • cleanses and moistens eye surface • contains antibacterial enzyme to help prevent infection Lacrimal puncta Lacrimal caruncle Lacrimal canaliculi 1 2 Lacrimal sac 3 4 Nasolacrimal duct 5 Nasal cavity Nostril
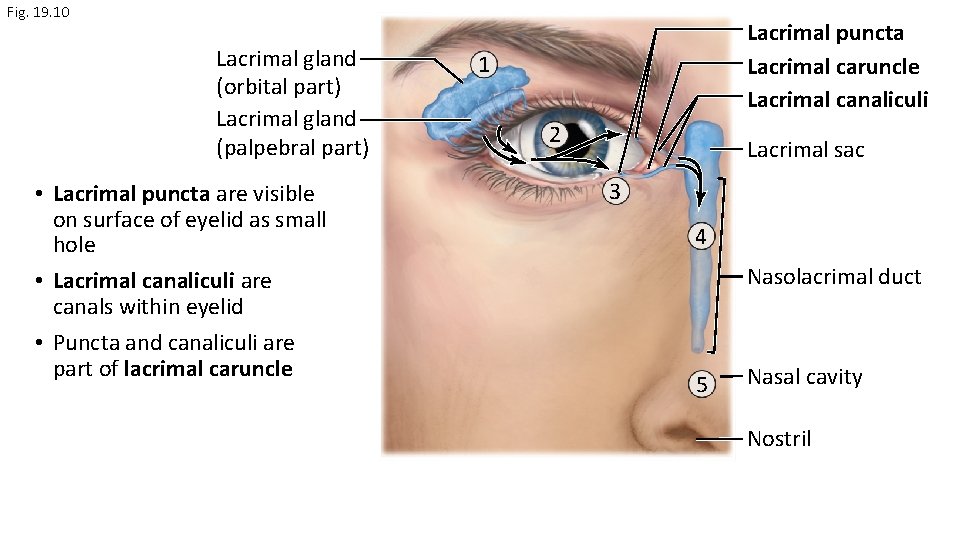
Fig. 19. 10 Lacrimal gland (orbital part) Lacrimal gland (palpebral part) • Lacrimal puncta are visible on surface of eyelid as small hole • Lacrimal canaliculi are canals within eyelid • Puncta and canaliculi are part of lacrimal caruncle Lacrimal puncta Lacrimal caruncle Lacrimal canaliculi 1 2 Lacrimal sac 3 4 Nasolacrimal duct 5 Nasal cavity Nostril
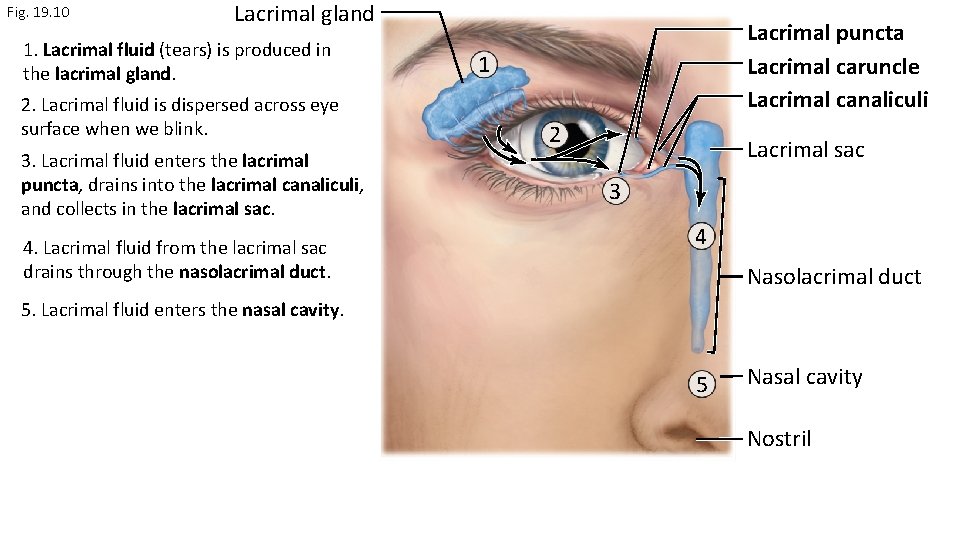
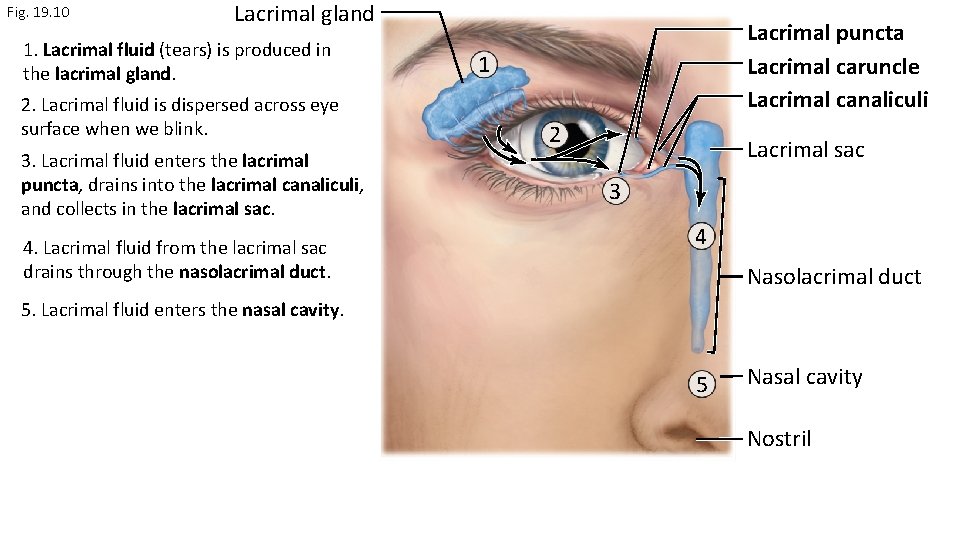
Fig. 19. 10 Lacrimal gland 1. Lacrimal fluid (tears) is produced in the lacrimal gland. 2. Lacrimal fluid is dispersed across eye surface when we blink. 3. Lacrimal fluid enters the lacrimal puncta, drains into the lacrimal canaliculi, and collects in the lacrimal sac. 4. Lacrimal fluid from the lacrimal sac drains through the nasolacrimal duct. Lacrimal puncta Lacrimal caruncle Lacrimal canaliculi 1 2 Lacrimal sac 3 4 Nasolacrimal duct 5. Lacrimal fluid enters the nasal cavity. 5 Nasal cavity Nostril
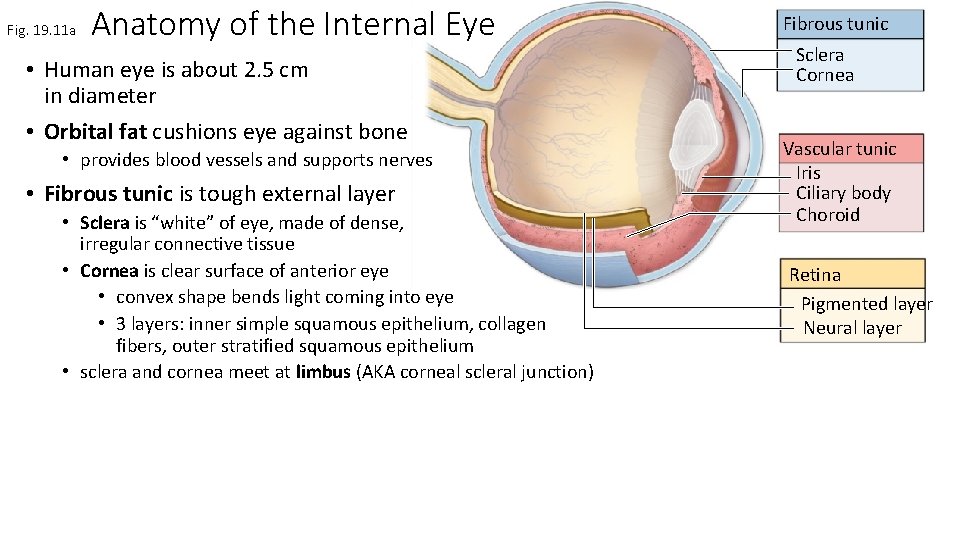
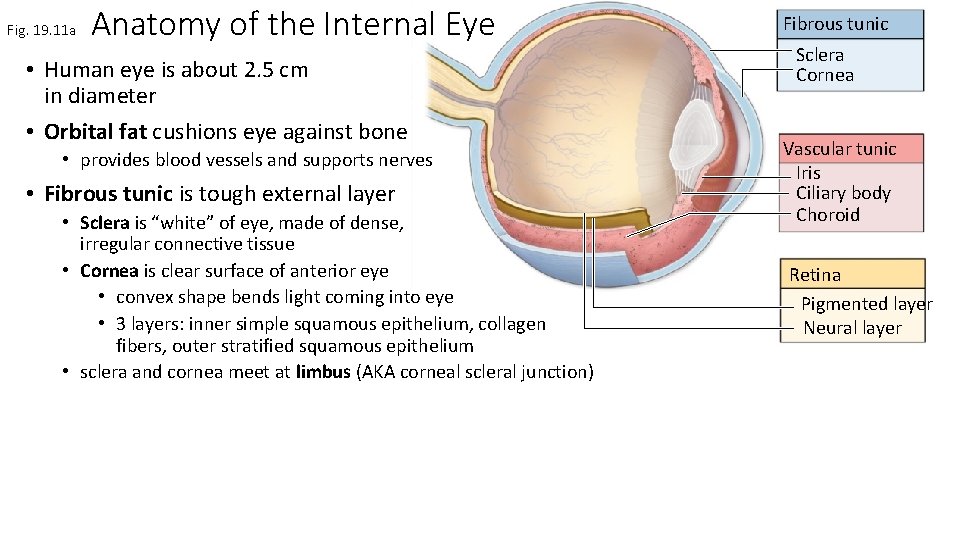
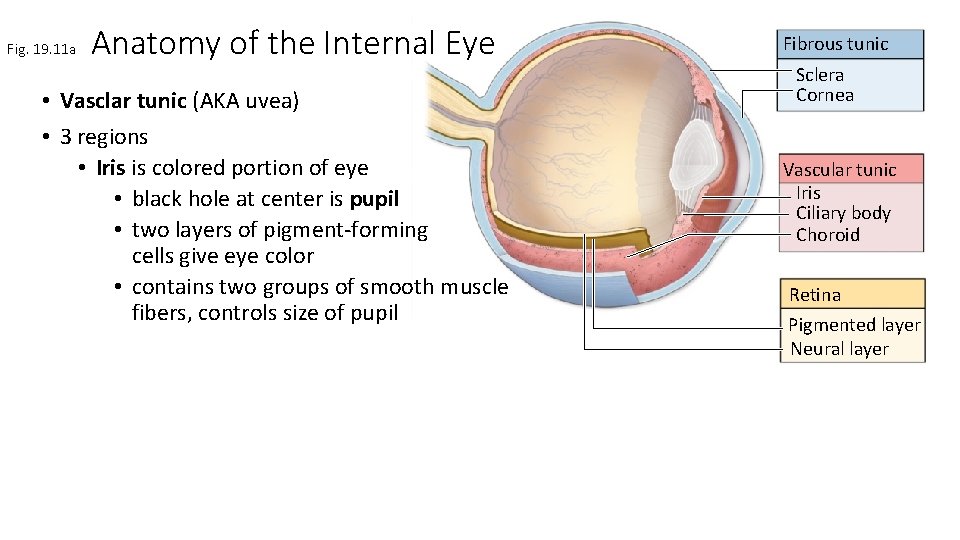
Fig. 19. 11 a Anatomy of the Internal Eye • Human eye is about 2. 5 cm in diameter • Orbital fat cushions eye against bone • provides blood vessels and supports nerves • Fibrous tunic is tough external layer • Sclera is “white” of eye, made of dense, irregular connective tissue • Cornea is clear surface of anterior eye • convex shape bends light coming into eye • 3 layers: inner simple squamous epithelium, collagen fibers, outer stratified squamous epithelium • sclera and cornea meet at limbus (AKA corneal scleral junction) Fibrous tunic Sclera Cornea Vascular tunic Iris Ciliary body Choroid Retina Pigmented layer Neural layer
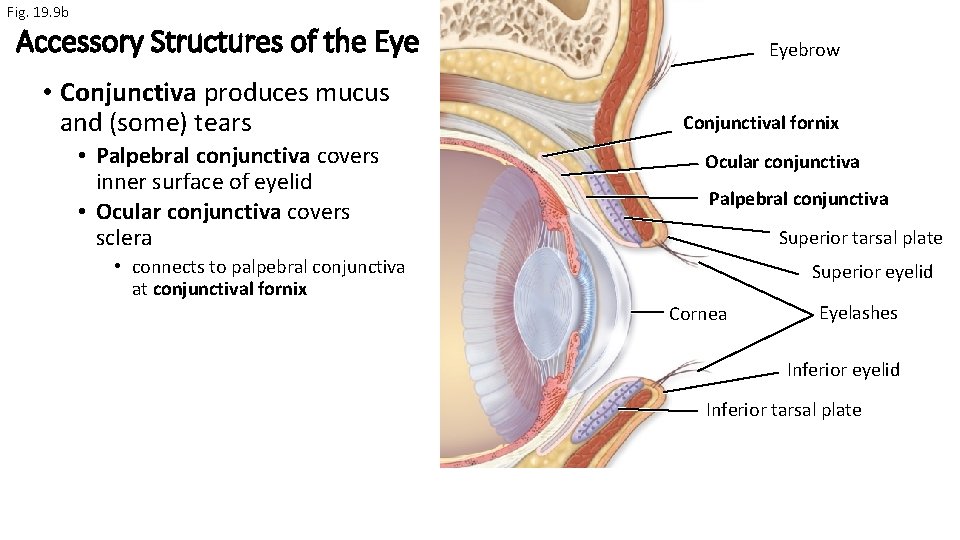
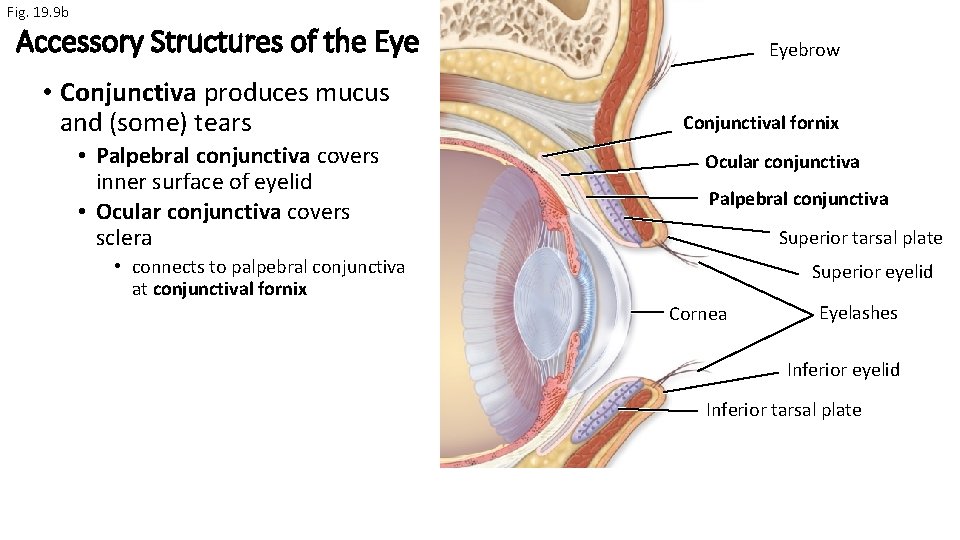
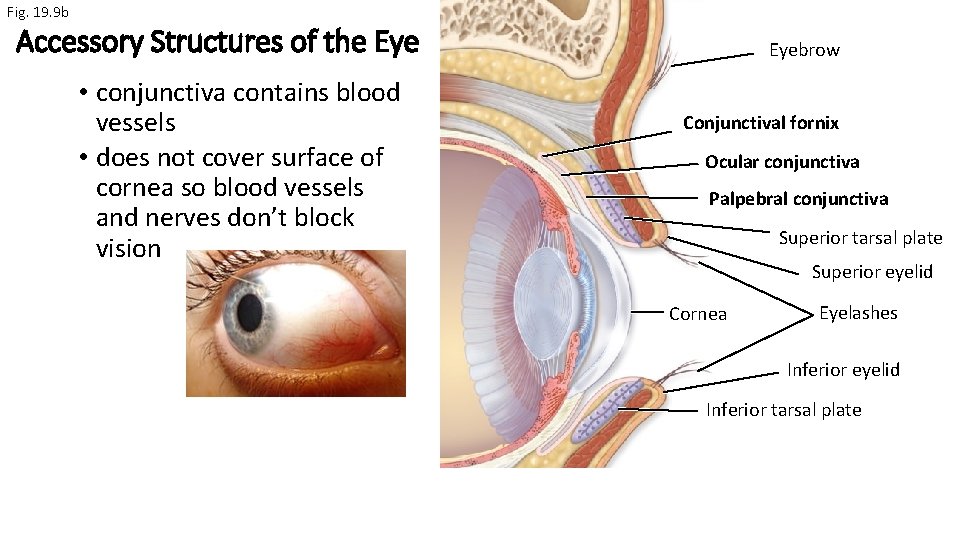
Fig. 19. 9 b Accessory Structures of the Eye • Conjunctiva produces mucus and (some) tears • Palpebral conjunctiva covers inner surface of eyelid • Ocular conjunctiva covers sclera Eyebrow Conjunctival fornix Ocular conjunctiva Palpebral conjunctiva Superior tarsal plate • connects to palpebral conjunctiva at conjunctival fornix Superior eyelid Cornea Eyelashes Inferior eyelid Inferior tarsal plate
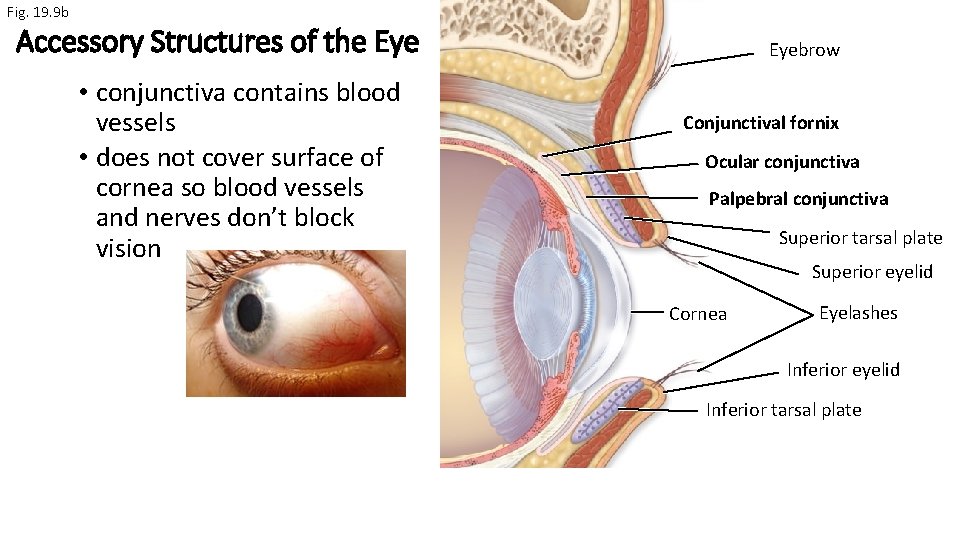
Fig. 19. 9 b Accessory Structures of the Eye • conjunctiva contains blood vessels • does not cover surface of cornea so blood vessels and nerves don’t block vision Eyebrow Conjunctival fornix Ocular conjunctiva Palpebral conjunctiva Superior tarsal plate Superior eyelid Cornea Eyelashes Inferior eyelid Inferior tarsal plate
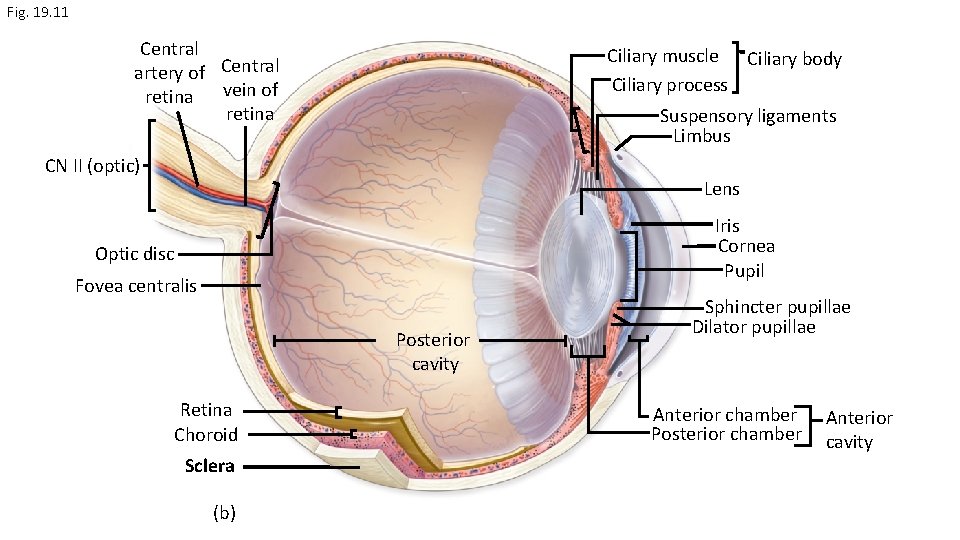
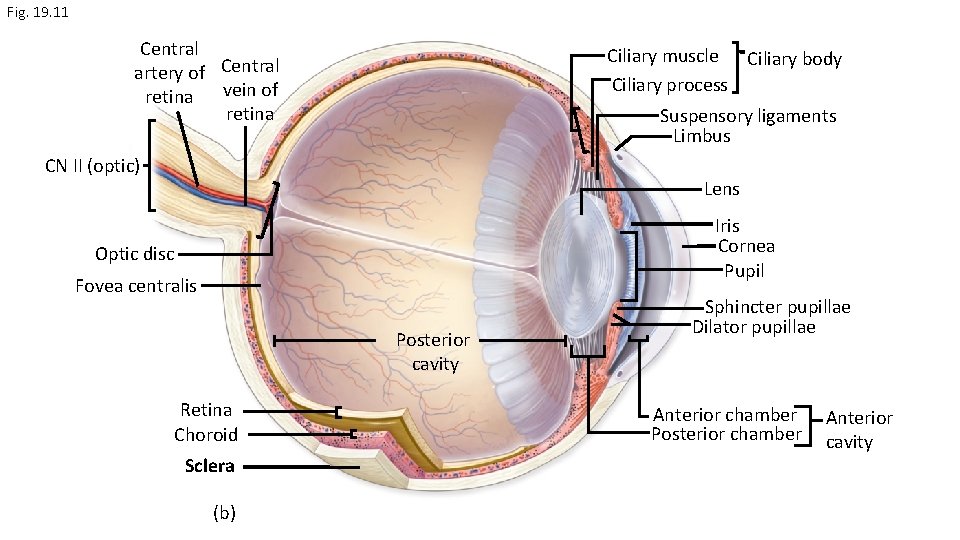
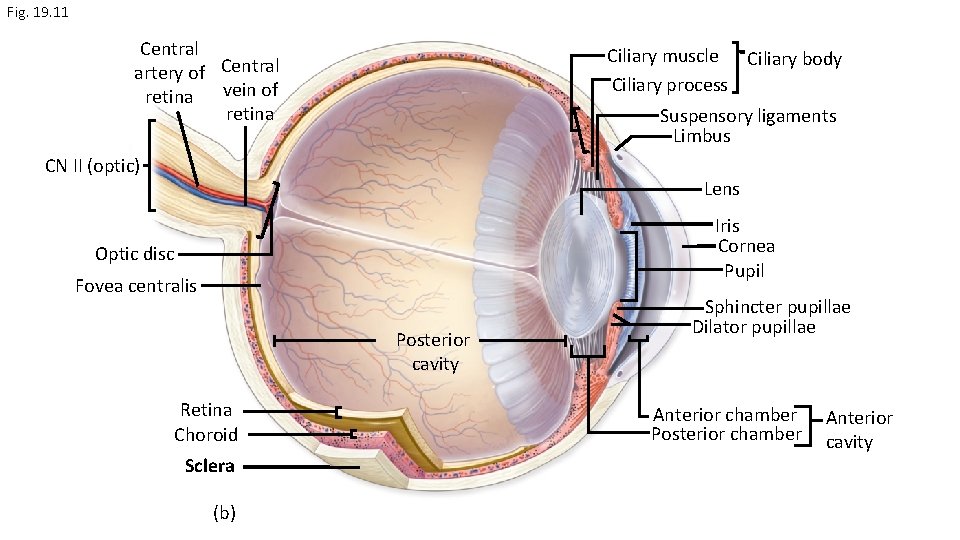
Fig. 19. 11 Central artery of Central retina vein of retina Ciliary muscle Ciliary body Ciliary process Suspensory ligaments Limbus CN II (optic) Lens Iris Cornea Pupil Optic disc Fovea centralis Posterior cavity Retina Choroid Sclera (b) Sphincter pupillae Dilator pupillae Anterior chamber Posterior chamber Anterior cavity
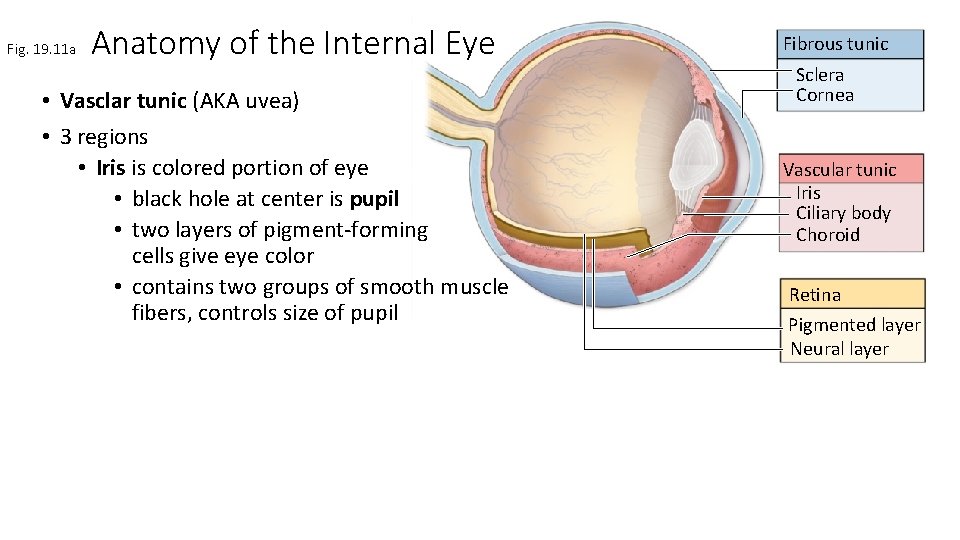
Fig. 19. 11 a Anatomy of the Internal Eye • Vasclar tunic (AKA uvea) • 3 regions • Iris is colored portion of eye • black hole at center is pupil • two layers of pigment-forming cells give eye color • contains two groups of smooth muscle fibers, controls size of pupil Fibrous tunic Sclera Cornea Vascular tunic Iris Ciliary body Choroid Retina Pigmented layer Neural layer
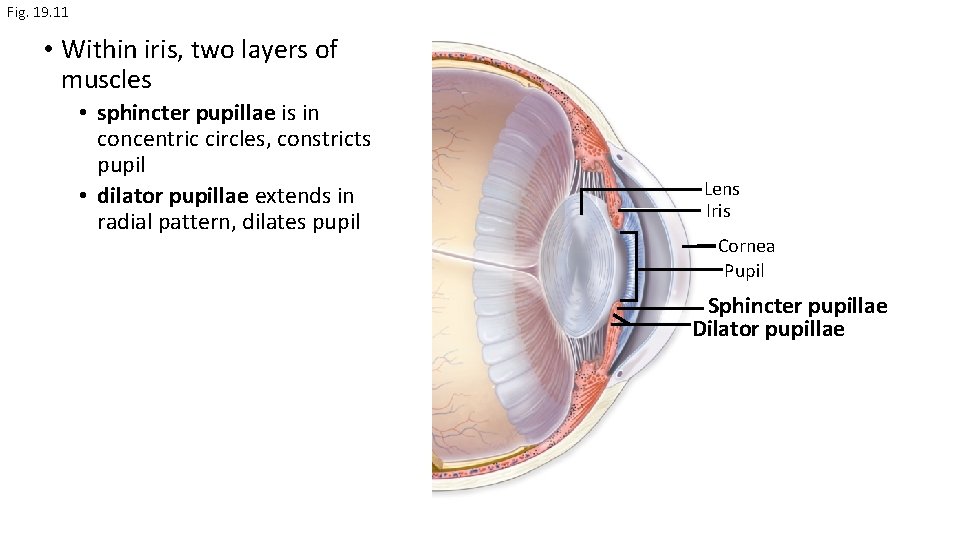
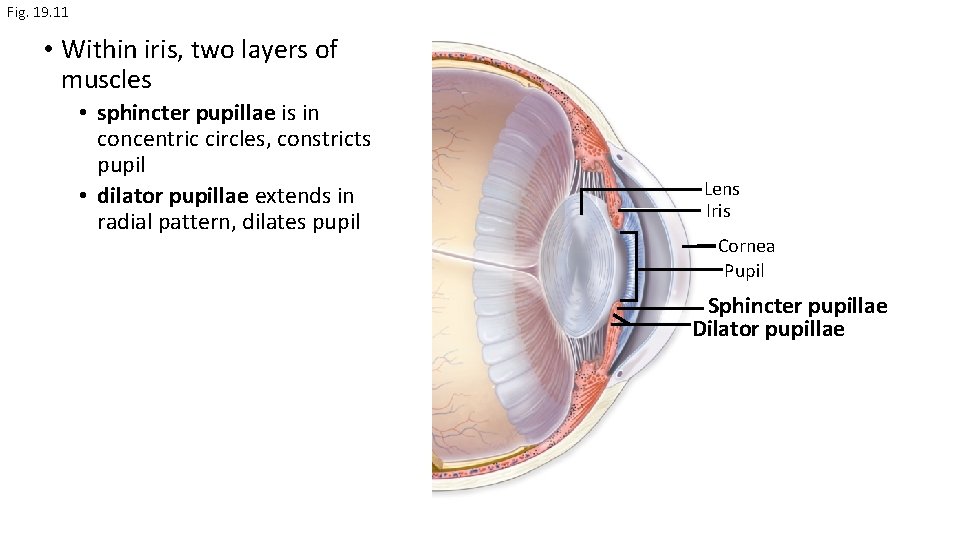
Fig. 19. 11 • Within iris, two layers of muscles • sphincter pupillae is in concentric circles, constricts pupil • dilator pupillae extends in radial pattern, dilates pupil Lens Iris Cornea Pupil Sphincter pupillae Dilator pupillae

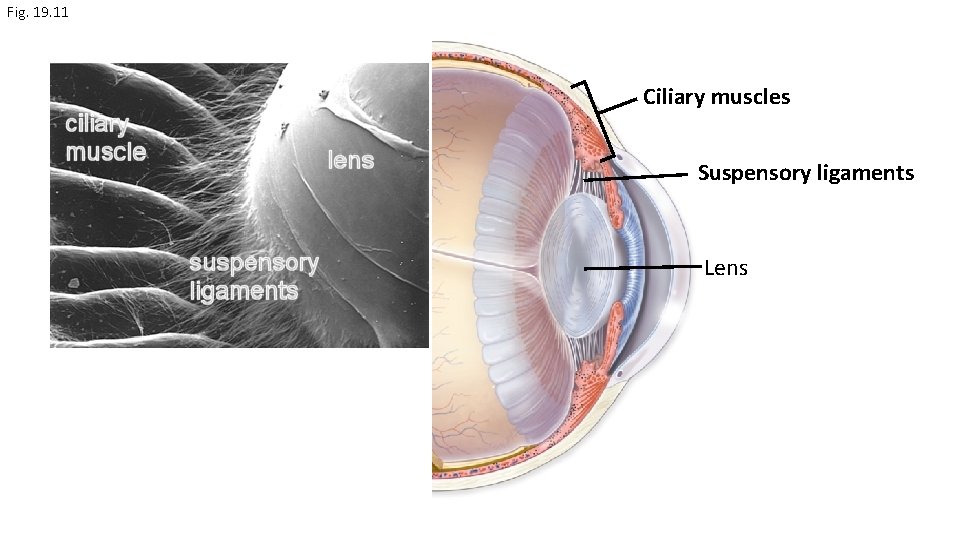
Fig. 19. 11 a Anatomy of the Internal Eye • Vascular tunic (AKA uvea) • 3 regions • Ciliary body is continuous with iris • composed of ciliary muscles and ciliary processes that cover muscles • suspensory ligaments extend to lens, focus eye by contracting or relaxing Fibrous tunic Sclera Cornea Vascular tunic Iris Ciliary body Choroid Retina Pigmented layer Neural layer
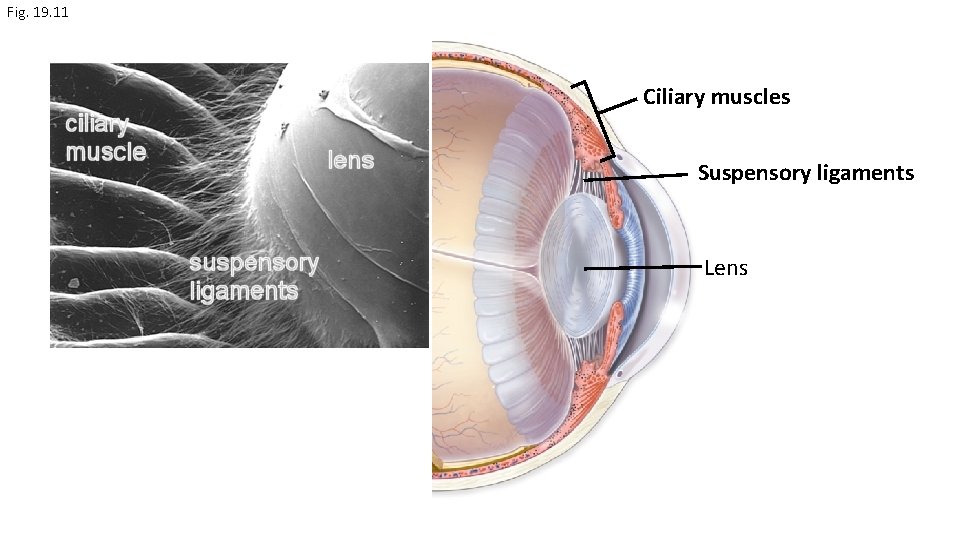
Fig. 19. 11 Ciliary muscles Suspensory ligaments Lens
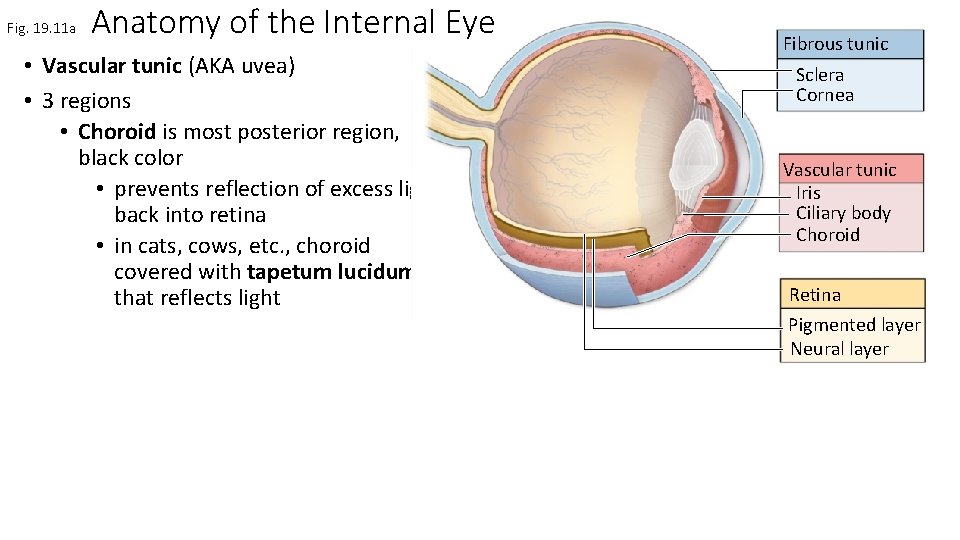
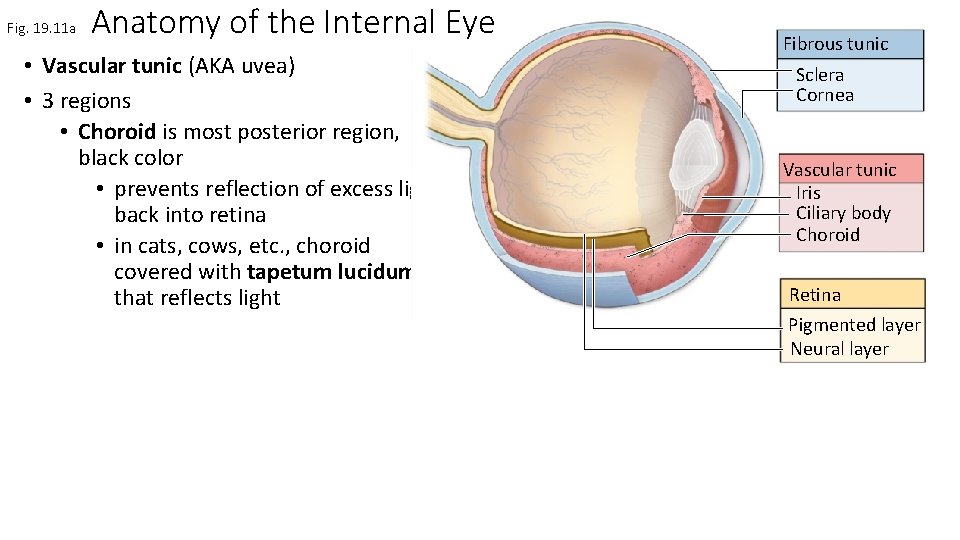
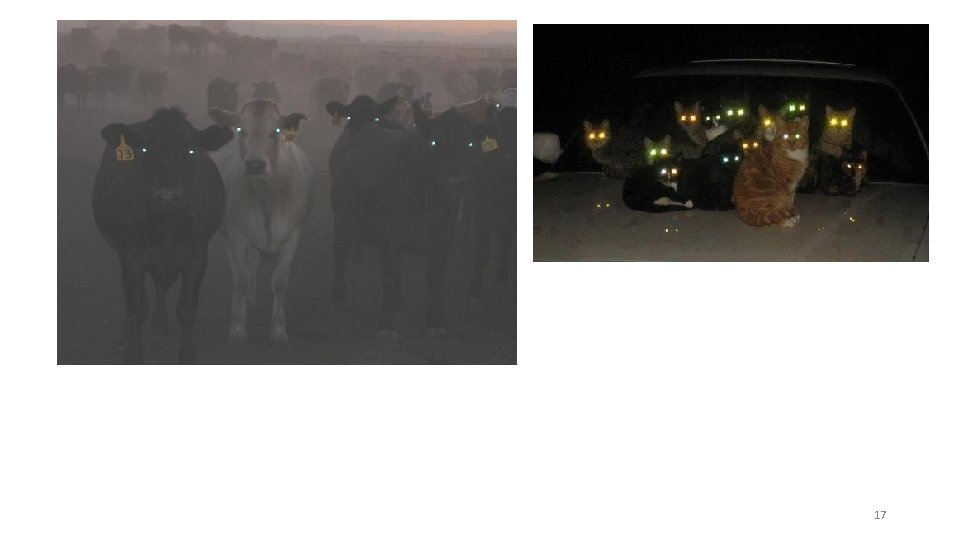
Fig. 19. 11 a Anatomy of the Internal Eye • Vascular tunic (AKA uvea) • 3 regions • Choroid is most posterior region, black color • prevents reflection of excess light back into retina • in cats, cows, etc. , choroid covered with tapetum lucidum that reflects light Fibrous tunic Sclera Cornea Vascular tunic Iris Ciliary body Choroid Retina Pigmented layer Neural layer
17
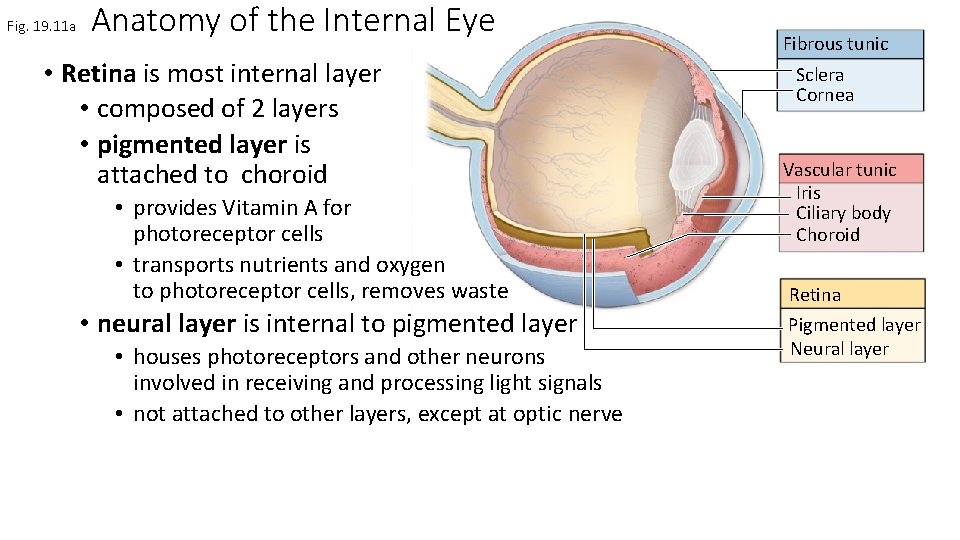
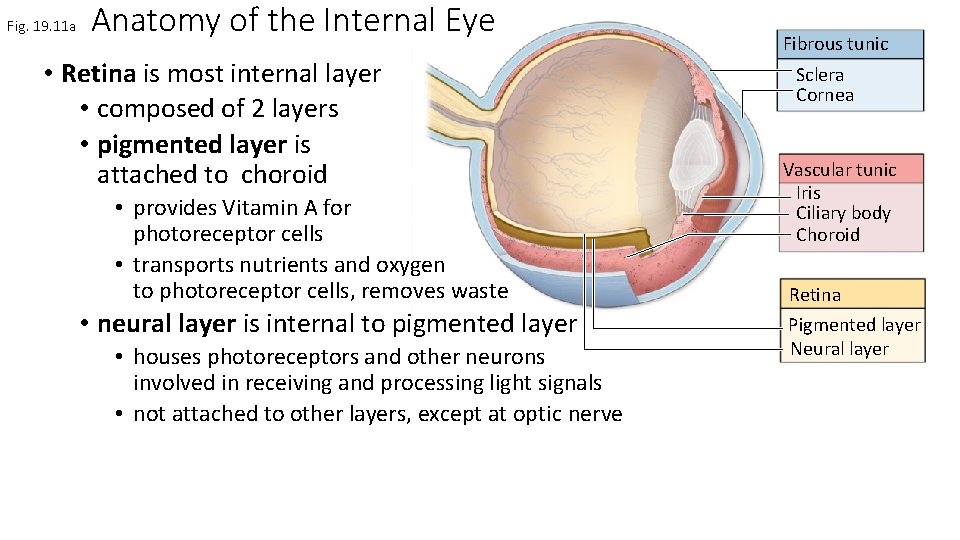
Fig. 19. 11 a Anatomy of the Internal Eye • Retina is most internal layer • composed of 2 layers • pigmented layer is attached to choroid • provides Vitamin A for photoreceptor cells • transports nutrients and oxygen to photoreceptor cells, removes waste • neural layer is internal to pigmented layer • houses photoreceptors and other neurons involved in receiving and processing light signals • not attached to other layers, except at optic nerve Fibrous tunic Sclera Cornea Vascular tunic Iris Ciliary body Choroid Retina Pigmented layer Neural layer
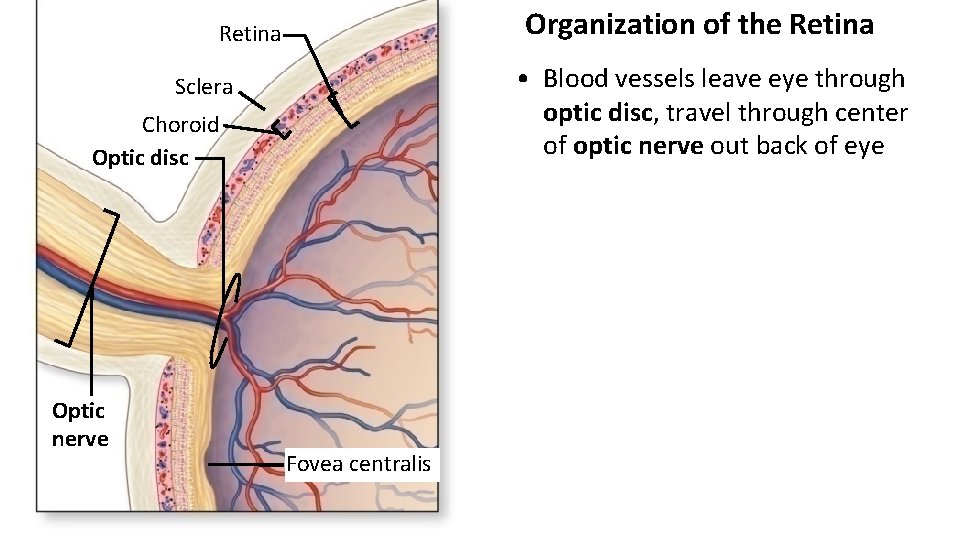
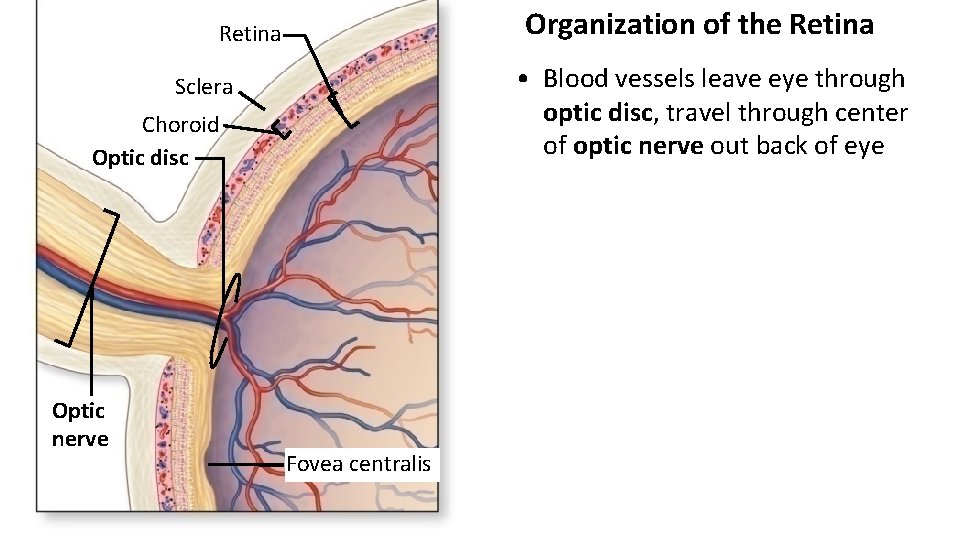
Organization of the Retina • Blood vessels leave eye through optic disc, travel through center of optic nerve out back of eye Sclera Choroid Optic disc Optic nerve Fovea centralis
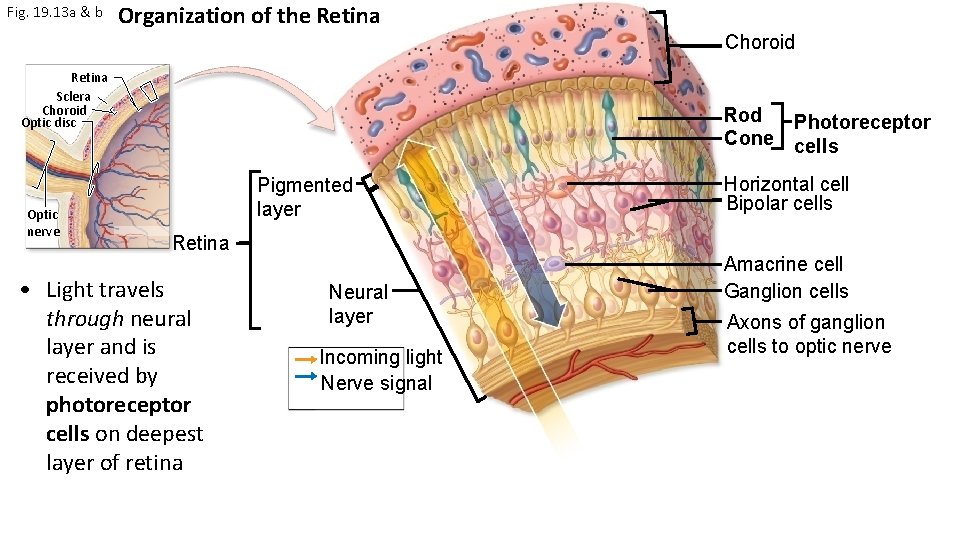
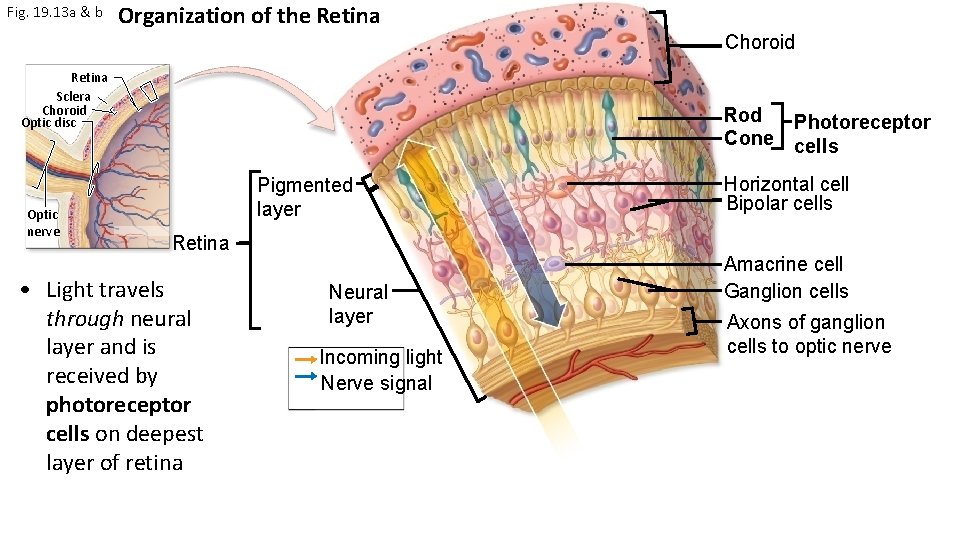
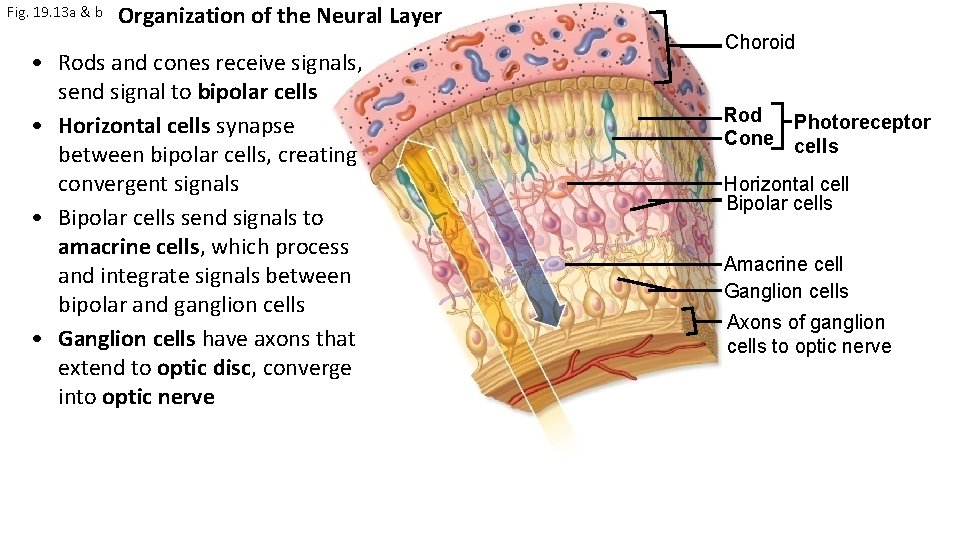
Fig. 19. 13 a & b Organization of the Retina Choroid Retina Sclera Choroid Optic disc Optic nerve Rod Photoreceptor Cone cells Pigmented layer Retina • Light travels through neural layer and is received by photoreceptor cells on deepest layer of retina Neural layer Incoming light Nerve signal Horizontal cell Bipolar cells Amacrine cell Ganglion cells Axons of ganglion cells to optic nerve
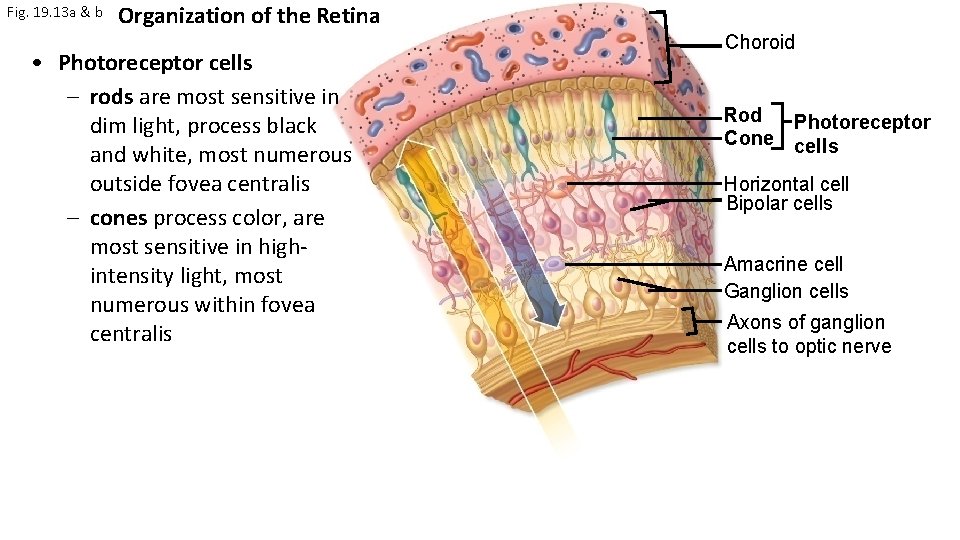
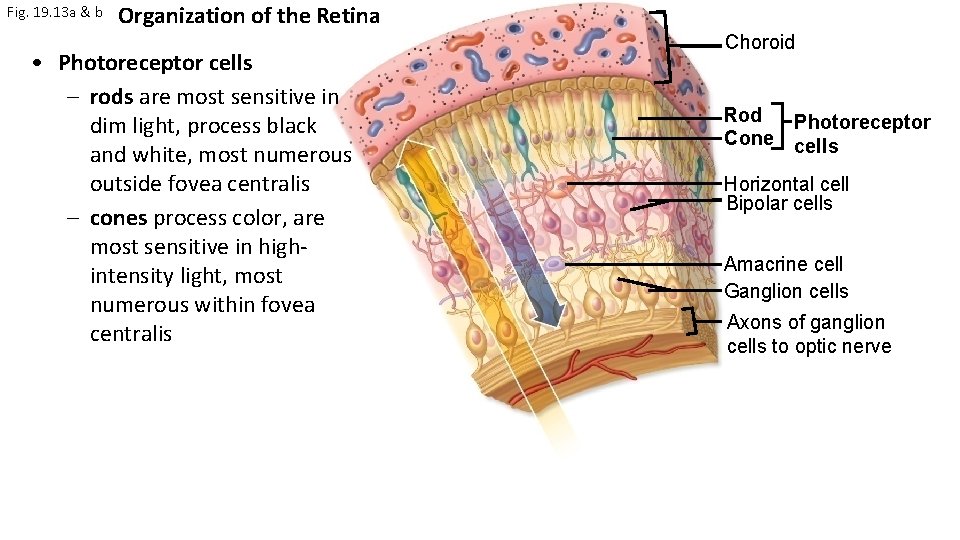
Fig. 19. 13 a & b Organization of the Retina • Photoreceptor cells – rods are most sensitive in dim light, process black and white, most numerous outside fovea centralis – cones process color, are most sensitive in highintensity light, most numerous within fovea centralis Choroid Rod Photoreceptor Cone cells Horizontal cell Bipolar cells Amacrine cell Ganglion cells Axons of ganglion cells to optic nerve
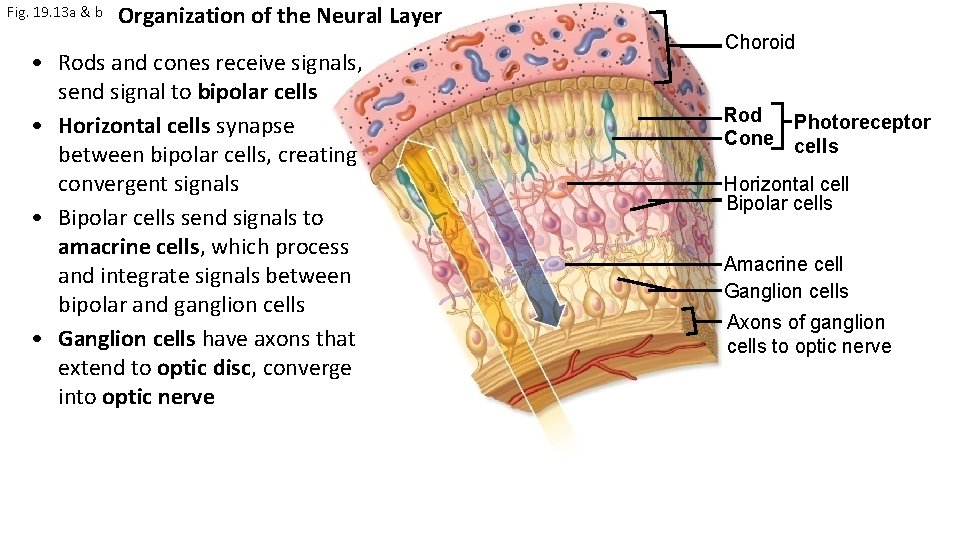
Fig. 19. 13 a & b Organization of the Neural Layer • Rods and cones receive signals, send signal to bipolar cells • Horizontal cells synapse between bipolar cells, creating convergent signals • Bipolar cells send signals to amacrine cells, which process and integrate signals between bipolar and ganglion cells • Ganglion cells have axons that extend to optic disc, converge into optic nerve Choroid Rod Photoreceptor Cone cells Horizontal cell Bipolar cells Amacrine cell Ganglion cells Axons of ganglion cells to optic nerve
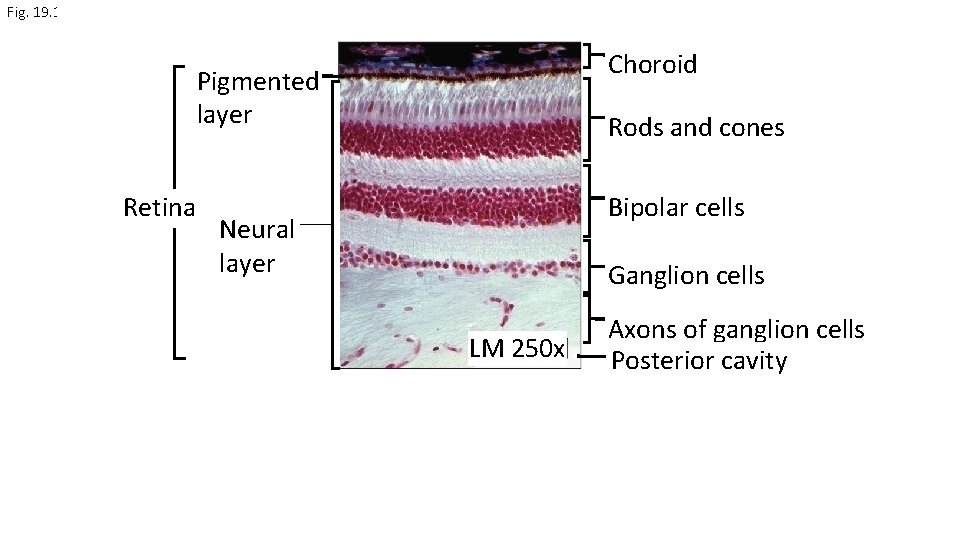
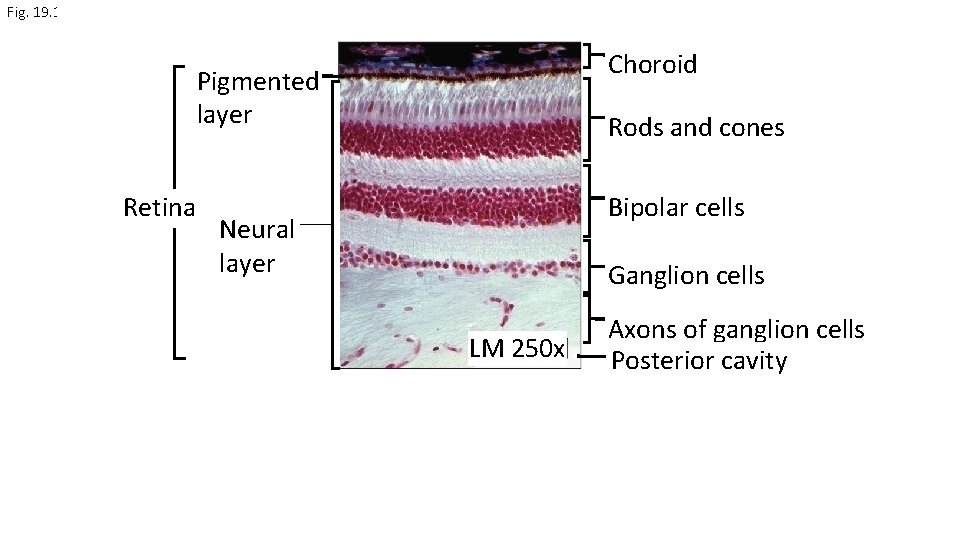
Fig. 19. 11 Choroid Pigmented layer Retina Rods and cones Bipolar cells Neural layer Ganglion cells LM 250 x Axons of ganglion cells Posterior cavity
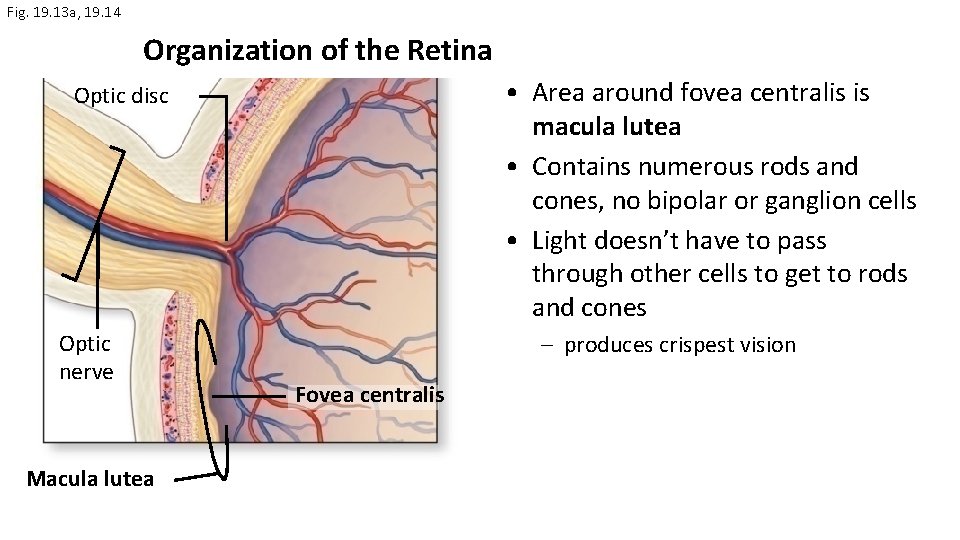
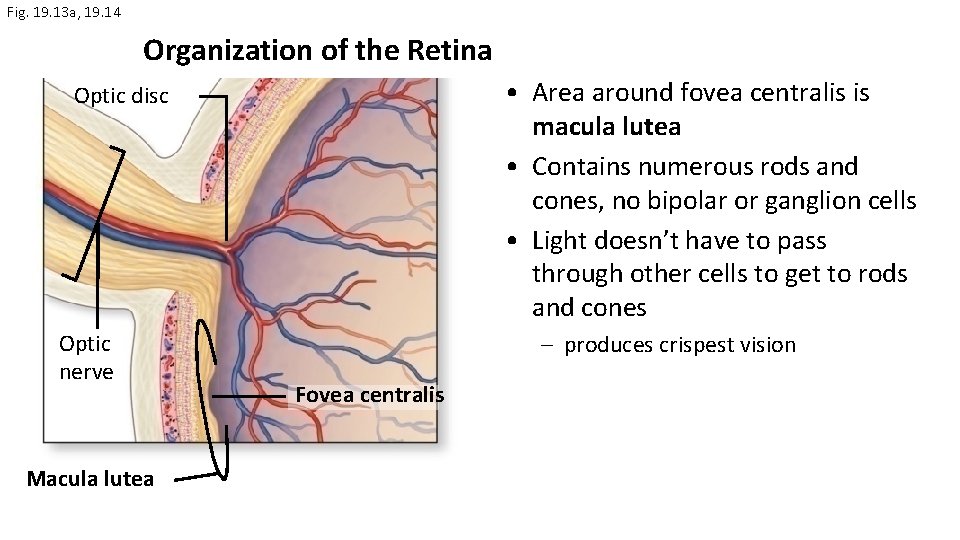
Fig. 19. 13 a, 19. 14 Organization of the Retina • Area around fovea centralis is macula lutea • Contains numerous rods and cones, no bipolar or ganglion cells • Light doesn’t have to pass through other cells to get to rods and cones Optic disc Optic nerve Macula lutea – produces crispest vision Fovea centralis
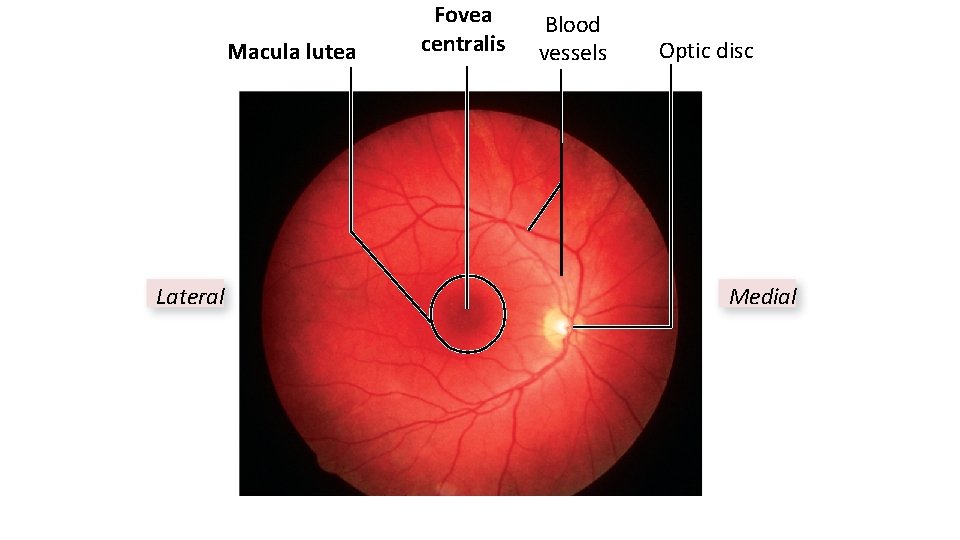
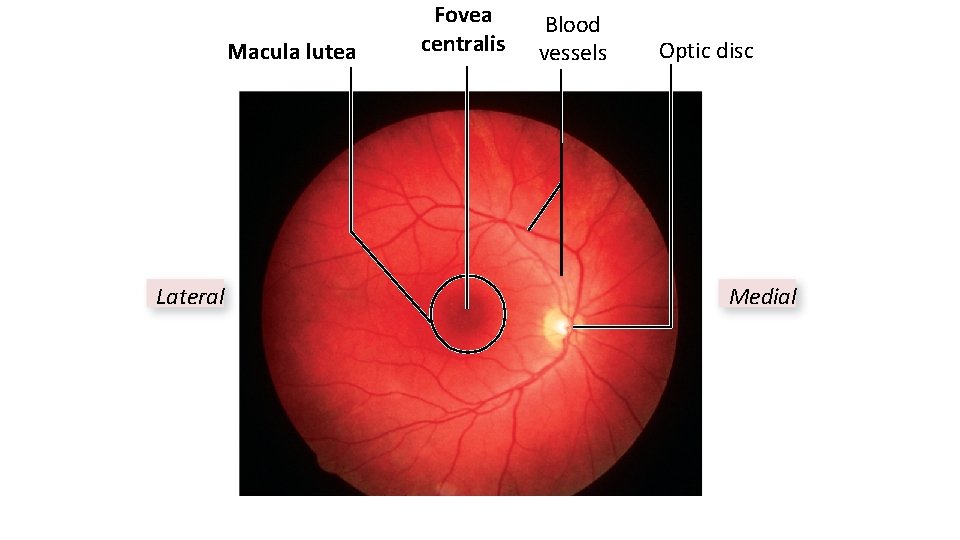
Macula lutea Lateral Fovea centralis Blood vessels Optic disc Medial
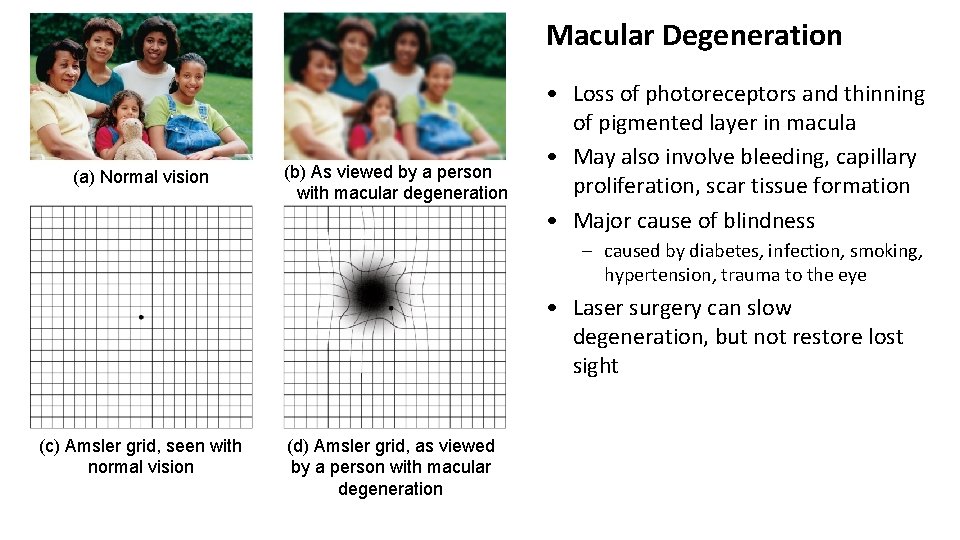
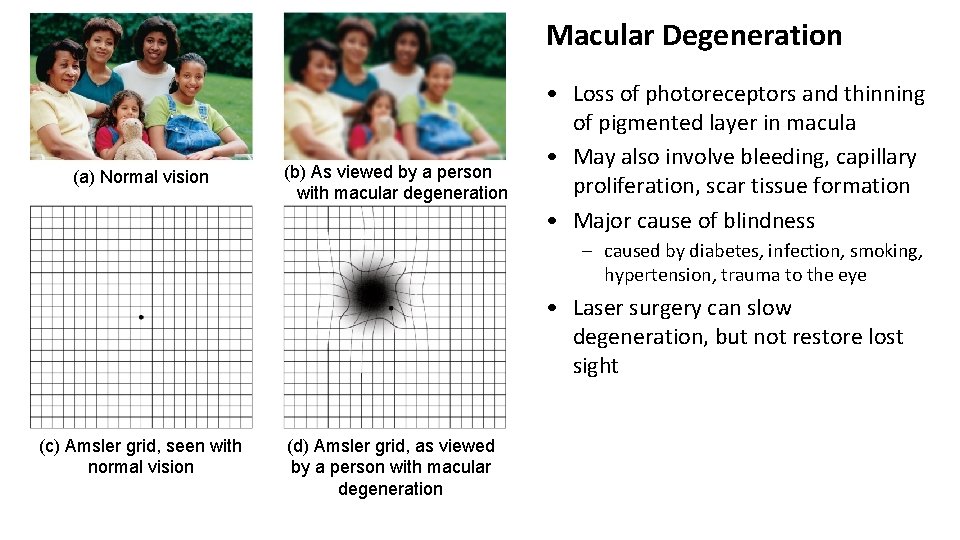
Macular Degeneration (a) Normal vision (b) As viewed by a person with macular degeneration • Loss of photoreceptors and thinning of pigmented layer in macula • May also involve bleeding, capillary proliferation, scar tissue formation • Major cause of blindness – caused by diabetes, infection, smoking, hypertension, trauma to the eye • Laser surgery can slow degeneration, but not restore lost sight (c) Amsler grid, seen with normal vision (d) Amsler grid, as viewed by a person with macular degeneration

• Space between lens and cornea is anterior cavity • divided into anterior chamber between iris and cornea, and posterior chamber between iris and lens • filled with aqueous humor (clear liquid) 27
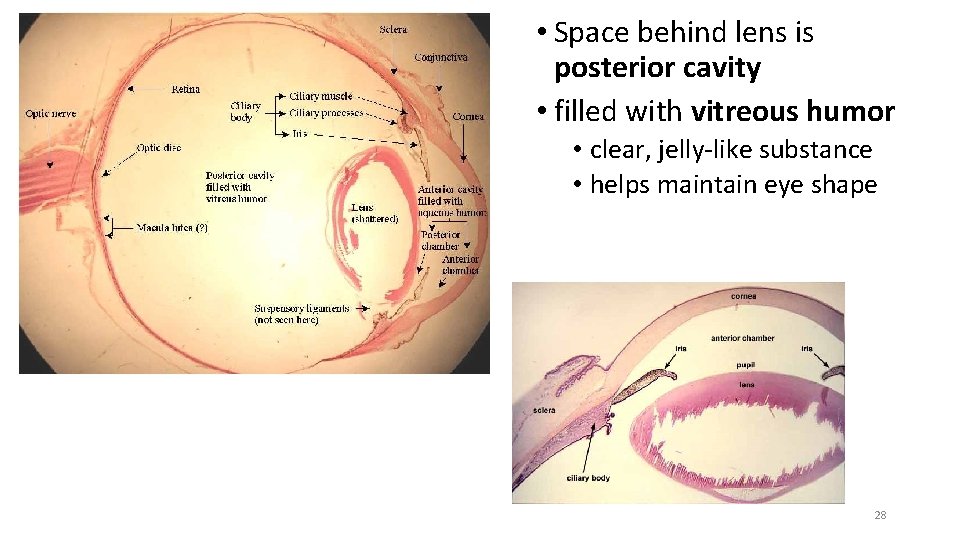
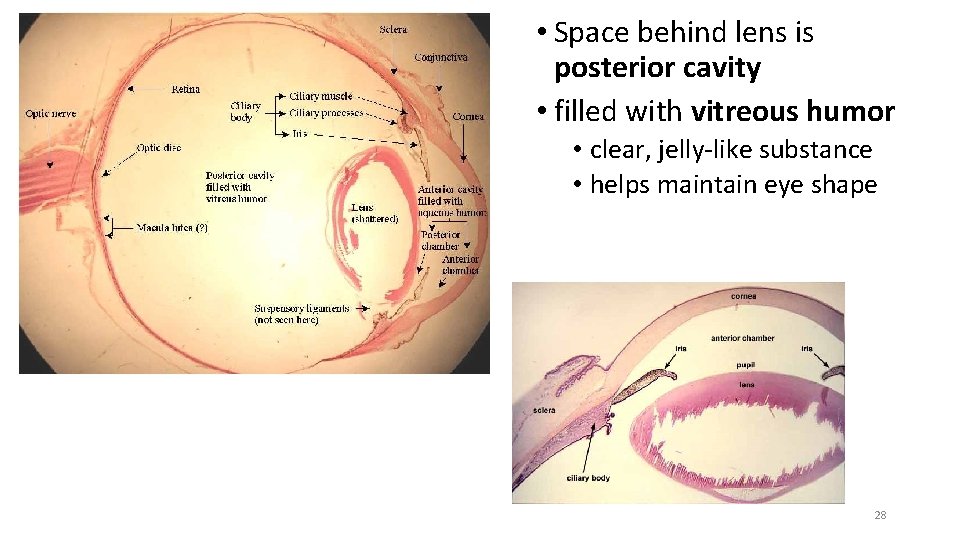
• Space behind lens is posterior cavity • filled with vitreous humor • clear, jelly-like substance • helps maintain eye shape 28
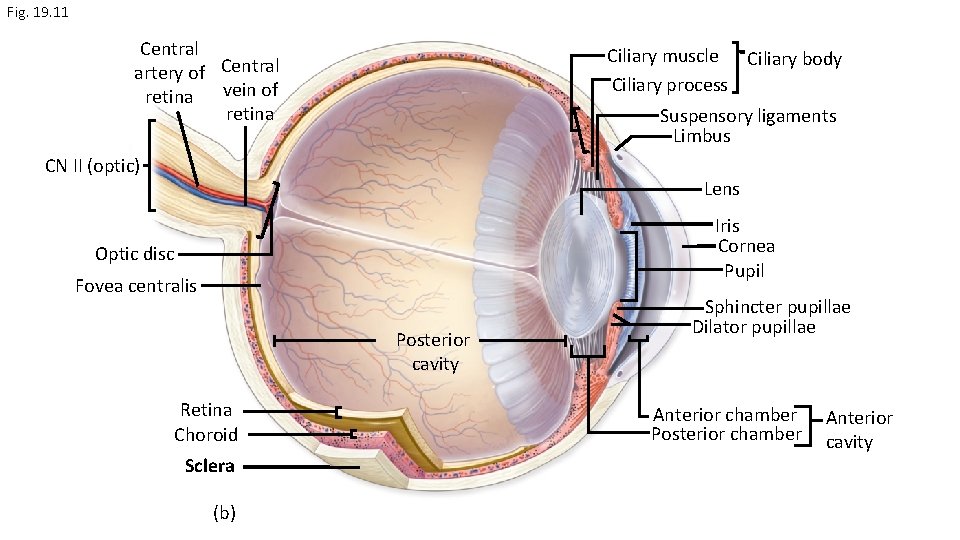
Fig. 19. 11 Central artery of Central retina vein of retina Ciliary muscle Ciliary body Ciliary process Suspensory ligaments Limbus CN II (optic) Lens Iris Cornea Pupil Optic disc Fovea centralis Posterior cavity Retina Choroid Sclera (b) Sphincter pupillae Dilator pupillae Anterior chamber Posterior chamber Anterior cavity
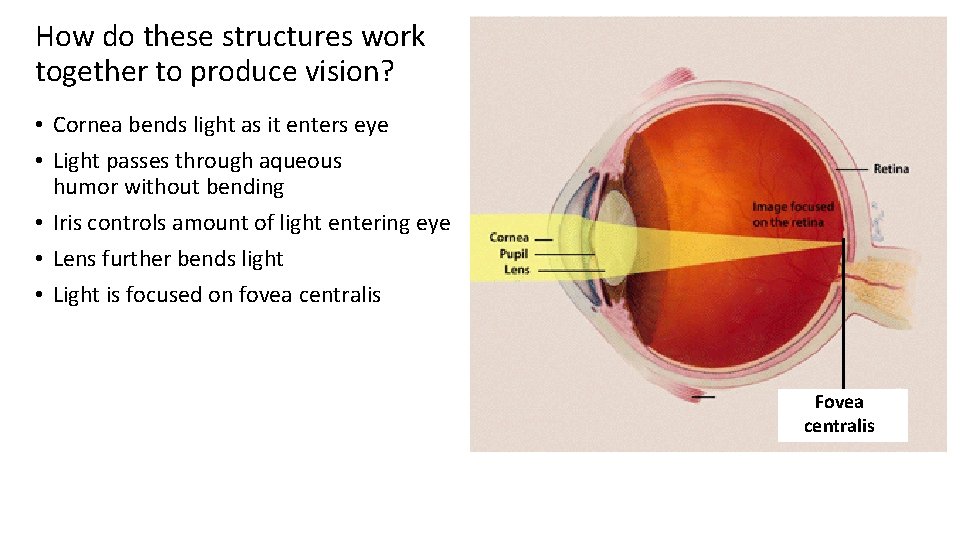
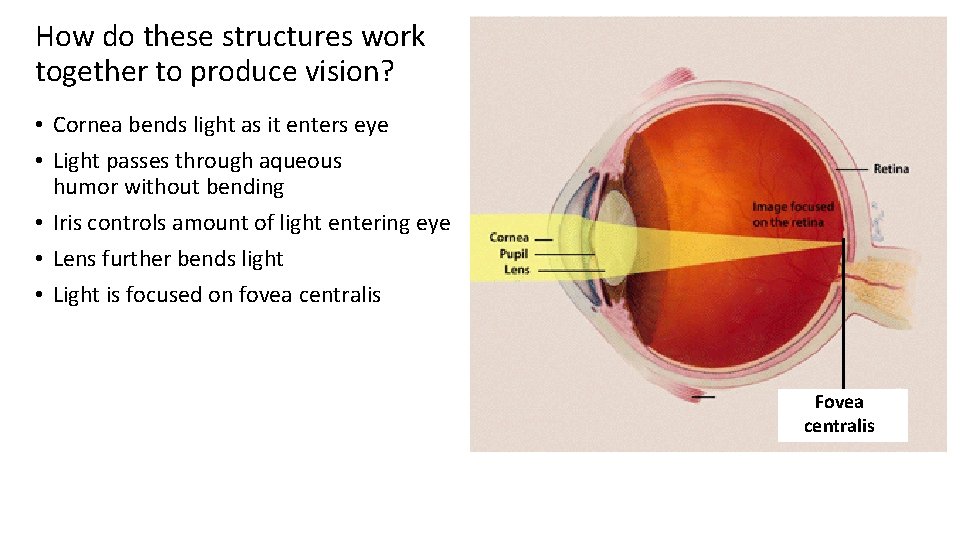
How do these structures work together to produce vision? • Cornea bends light as it enters eye • Light passes through aqueous humor without bending • Iris controls amount of light entering eye • Lens further bends light • Light is focused on fovea centralis Fovea centralis
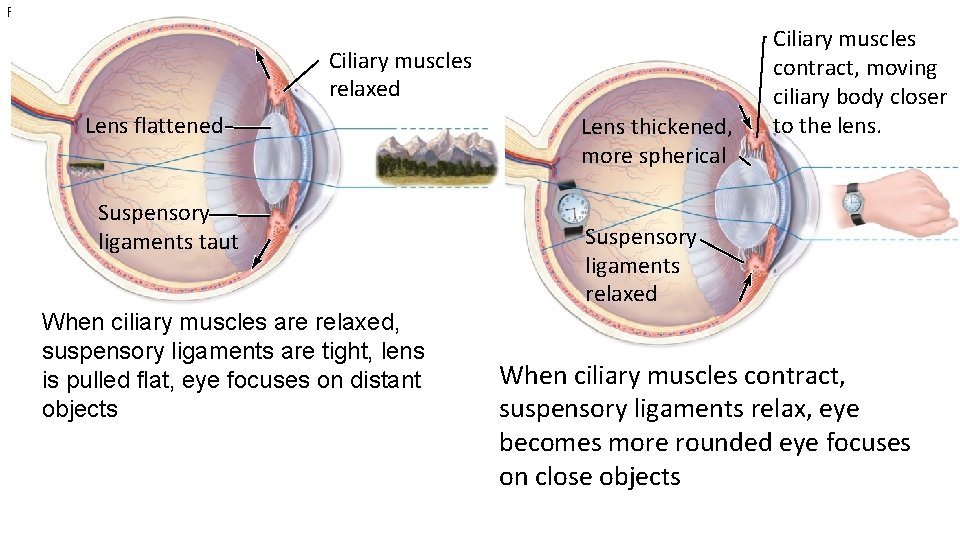
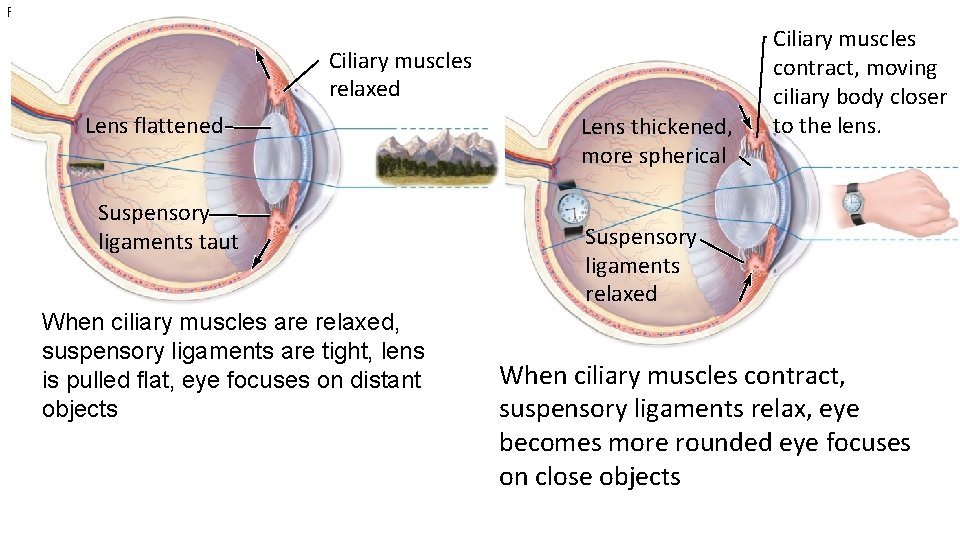
Fig. 19. 15 Ciliary muscles relaxed Lens flattened Suspensory ligaments taut When ciliary muscles are relaxed, suspensory ligaments are tight, lens is pulled flat, eye focuses on distant objects Lens thickened, more spherical Ciliary muscles contract, moving ciliary body closer to the lens. Suspensory ligaments relaxed When ciliary muscles contract, suspensory ligaments relax, eye becomes more rounded eye focuses on close objects
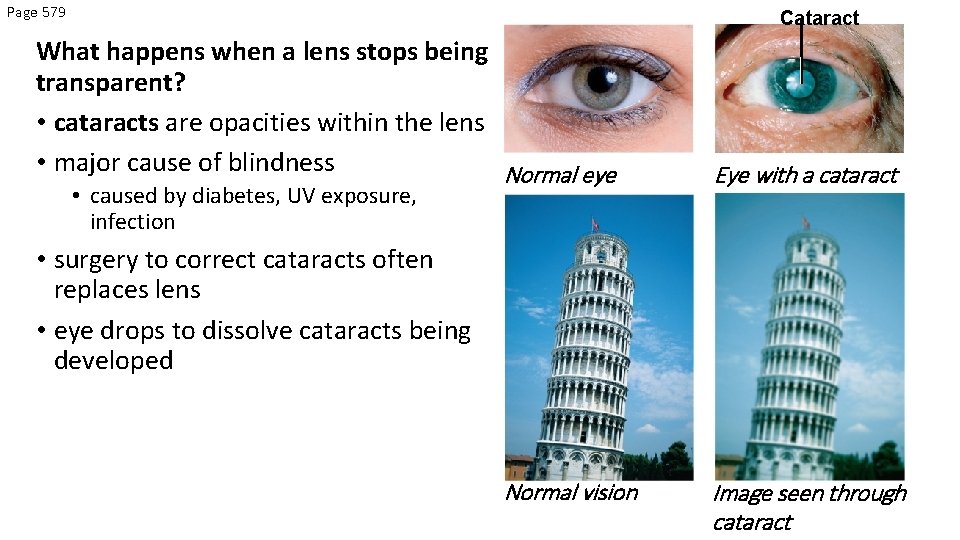
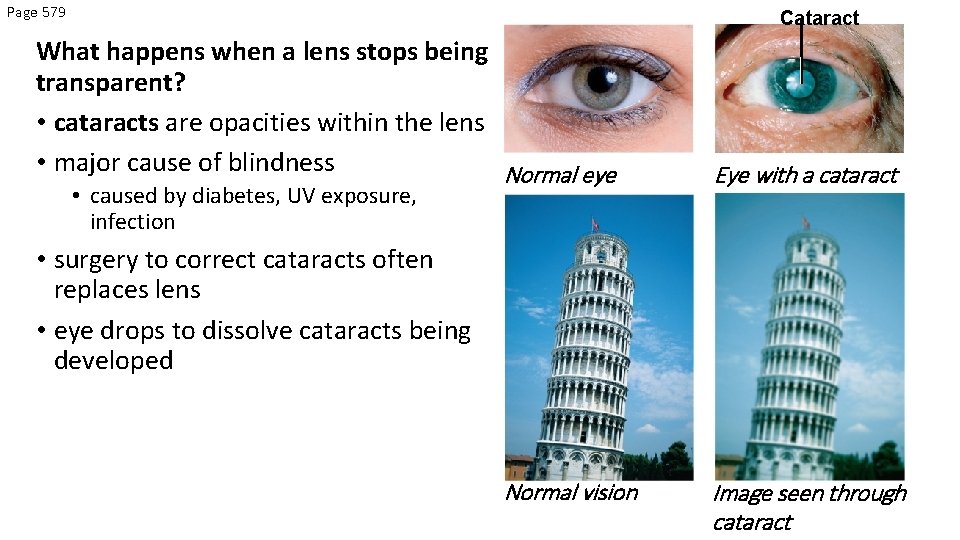
Page 579 Cataract What happens when a lens stops being transparent? • cataracts are opacities within the lens • major cause of blindness Normal eye • caused by diabetes, UV exposure, infection Eye with a cataract • surgery to correct cataracts often replaces lens • eye drops to dissolve cataracts being developed Normal vision Image seen through cataract
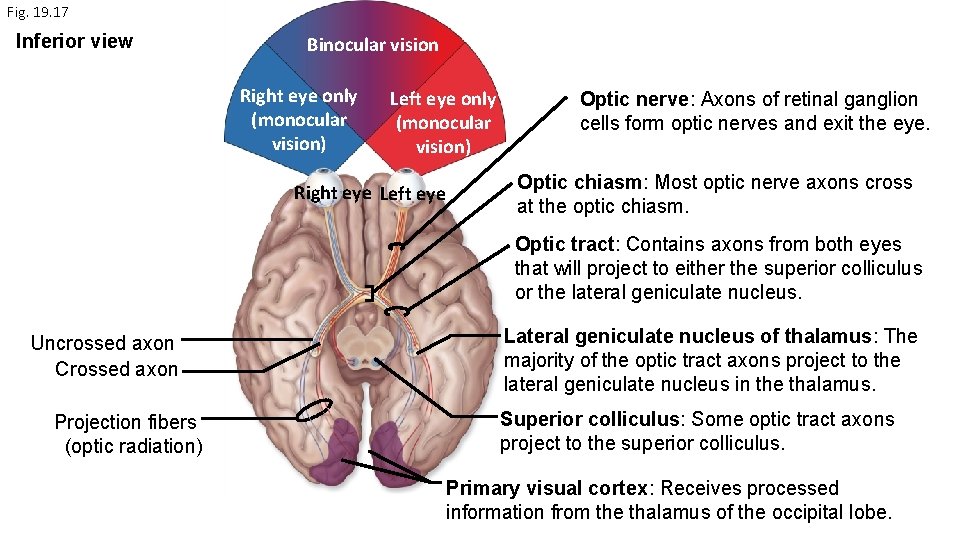
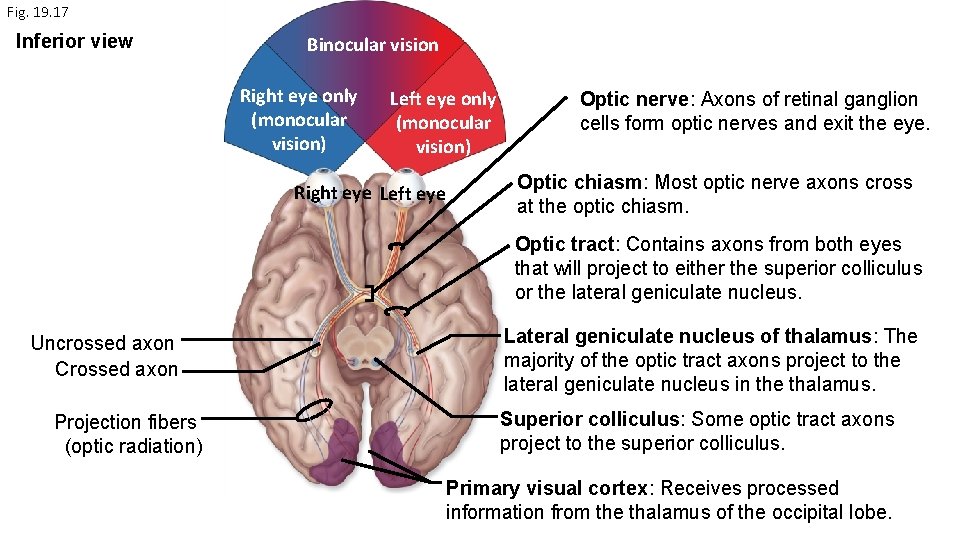
Fig. 19. 17 Inferior view Binocular vision Right eye only (monocular vision) Left eye only (monocular vision) Right eye Left eye Optic nerve: Axons of retinal ganglion cells form optic nerves and exit the eye. Optic chiasm: Most optic nerve axons cross at the optic chiasm. Optic tract: Contains axons from both eyes that will project to either the superior colliculus or the lateral geniculate nucleus. Uncrossed axon Crossed axon Projection fibers (optic radiation) Lateral geniculate nucleus of thalamus: The majority of the optic tract axons project to the lateral geniculate nucleus in the thalamus. Superior colliculus: Some optic tract axons project to the superior colliculus. Primary visual cortex: Receives processed information from the thalamus of the occipital lobe.
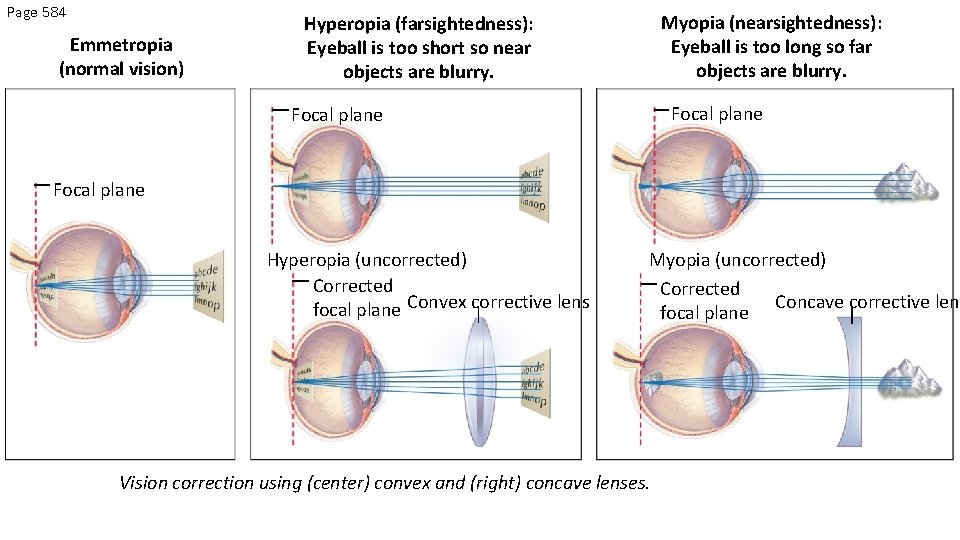
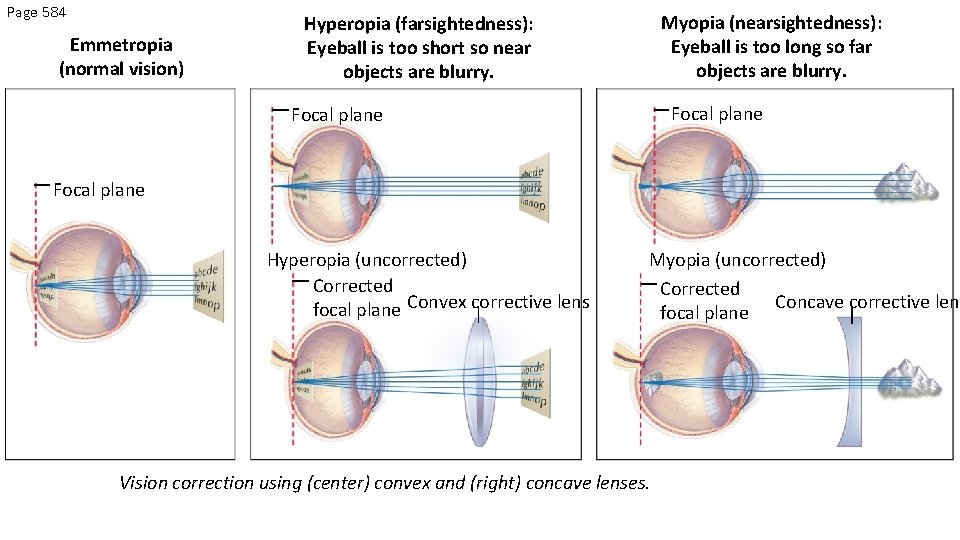
Page 584 Emmetropia (normal vision) Myopia (nearsightedness): Eyeball is too long so far objects are blurry. Hyperopia (farsightedness): Eyeball is too short so near objects are blurry. Focal plane Hyperopia (uncorrected) Corrected focal plane Convex corrective lens Myopia (uncorrected) Corrected Concave corrective lens focal plane Vision correction using (center) convex and (right) concave lenses.
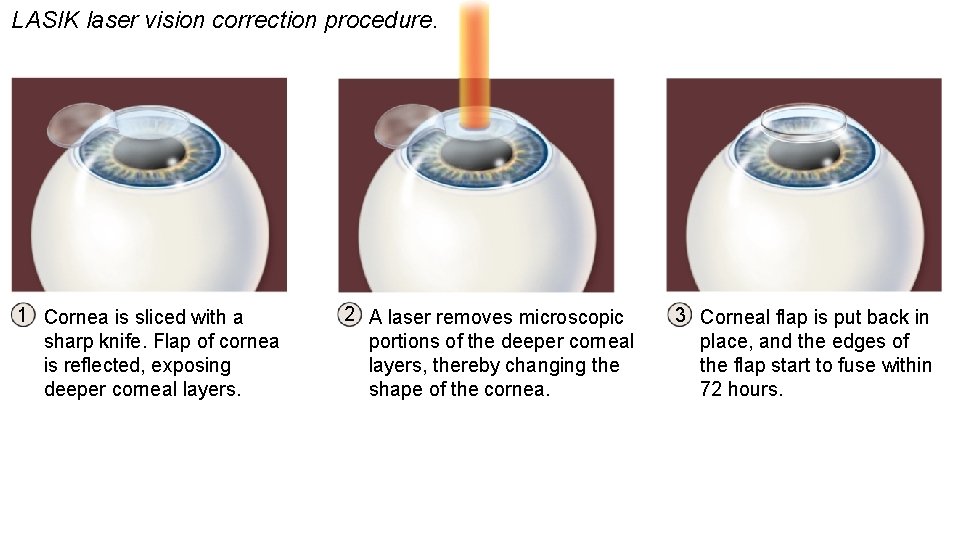
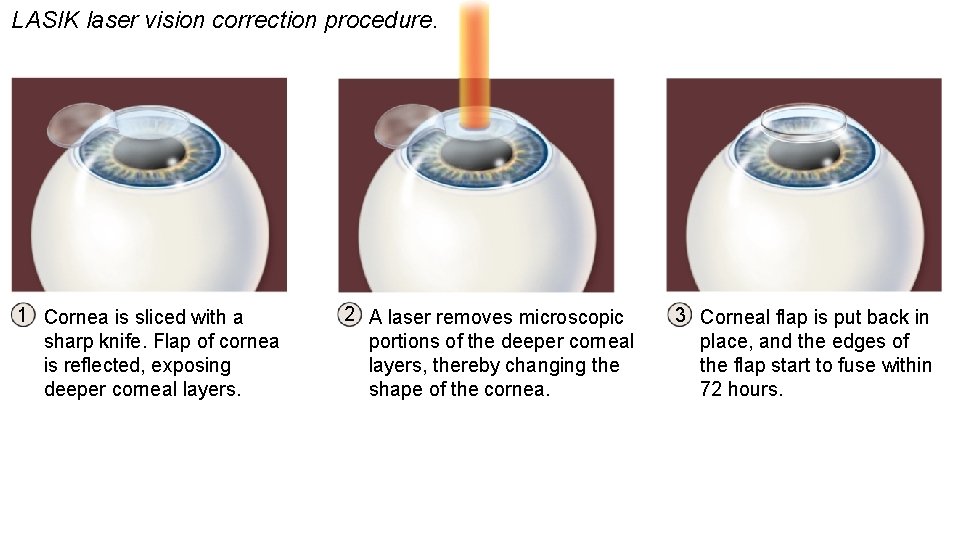
LASIK laser vision correction procedure. 1 Cornea is sliced with a sharp knife. Flap of cornea is reflected, exposing deeper corneal layers. 2 A laser removes microscopic portions of the deeper corneal layers, thereby changing the shape of the cornea. 3 Corneal flap is put back in place, and the edges of the flap start to fuse within 72 hours.