Approach to Hypertension Dr Duaa Hiasat l l
- Slides: 67
Approach to Hypertension Dr. Duaa Hiasat
l l l l DEFINITION: Diagnosis PREVALENCE Screening How blood pressure measured Ambulatory blood pressure monitoring CLASSIFICATION OF BLOOD PRESSURE Risk factors for development of HTN Essential hypertension: SECONDARY HYPERTENSION Diagnosis workup of hypertension complications Treatment malignant hypertension Hypertensive urgencies Hypertensive emergencies
DEFINITION: l systolic blood pressure ≥ 140 mmhg or diastolic blood pressure ≥ 90 mmhg. l On diabetic HTN is defined as ( ≥ 130 mmhg systolic and/or ≥ 80 mmhg diastolic).
Diagnosis l l l Dx of HTN should be based on high blood pressure measurements ( ≥ 140 mmhg systolic and/or ≥ 90 mmhg diastolic) on at least 3 occasions over at least 6 week. or 180 mmhg systolic and/or 110 mmhg diastolic on one occasion. or if measurements ( ≥ 140 mmhg systolic and/or ≥ 90 mmhg diastolic) and target organ damage.
Isolated systolic HTN : l Systolic Bp more than 140 mm. Hg and DBP less than 90 mm. Hg. l Is common in the elderly.
PREVALENCE: l l l Increases with ages. More common in black &African than in white. systolic BP is more pronounce in men. Isolated systolic HTN is associated with a two-to three fold increase in cardiac mortality. The mortality rates for stroke , coronary heart disease are the major complications of hypertension. All adult should have BP measured routinely at least every 3 years until the age of 80.
Screening l l l The first step in treating hypertension is finding it. Every family physician should have a strategy for detecting hypertension in his or her patient population. the US Preventive Services Task Force strongly recommends that clinicians screen adults 18 years and older for hypertension, but makes no recommendation regarding the interval at which screening should take place (Strength of Recommendation A).
Screening l l l Most screening for hypertension occurs opportunistically, in that patients presenting to a clinic for any reason will have their BP measured. This approach works well for those patients who come to the physician several times per year. Some groups, however, such as younger to middleaged men and underserved populations do not regularly seek medical care and may require special contact via mailings, health fairs, or work-site screening.
How blood pressure measured l l l BP should be measured with a well- calibrated sphygmomanometer. The patient should be seated with the arm bare and supported The bladder width within the cuff should encircle at 80% of the arm circumference. A wider cuff should be used on obese or thick arms A small cuff or the presence of clothing under the cuff will falsely elevate the reading by 10 -15 mm. Hg.
l l l With the auscultatory method the ipsilateral radial pulse should be palpated during inflation to be certain that systolic pressure has been exceeded. The pulse should disappear when the cuff is adequately presurized. Reading should be taken after the patient has been resting for at least 5 minutes &at least 30 minutes after smoking or coffee ingestion. A distended bladder or the recent use of tobacco or caffeine may give high reading
l On initial measurement Bp should be checked in both arms. l BP should always be examined in the supine and standing positions to detect postural changes. l Standing BP should be measured in diabetic &elderly subjects to exclude orthostatic hypotension. l When assessing the cardiovascular risk, the average BP at separate visits is more accurate than measurements taken at a single visit.
Ambulatory blood pressure monitoring l Indirect automatic blood pressure measurements can be made over a 24 - hour period using a measuring device worn by the patient. l they are used to confirmed the diagnosis in those patient with (white –coat hypertension ) i. e. in those subjects whose blood pressure is completely normal at all stages except during a clinical consultation. these patients do not have any evidence of target-organ damage , &unnecessary treatment can be avoided. l
l l These devices may also be used to monitor the response of patients to drug treatment & in particular , can be used to determine the adequacy of 24 -hour control with once-daily medication. It is better predictors of cardiovascular risk than clinical measurements. Analysis of the diurnal variation in blood pressure suggests that those hypertensives with loss of the usual nocturnal fall in blood pressure have a worse prognosis than those who retain this pattern. Normal out of office Bp is about 10 mm. Hg lower than normal office Bp.
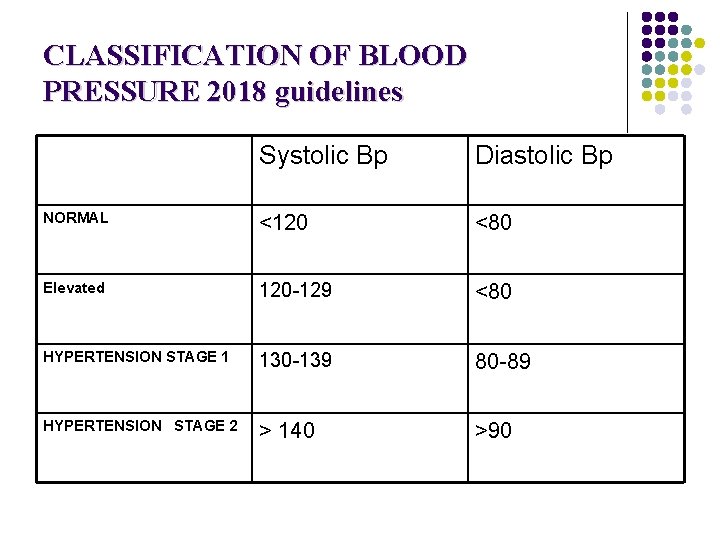
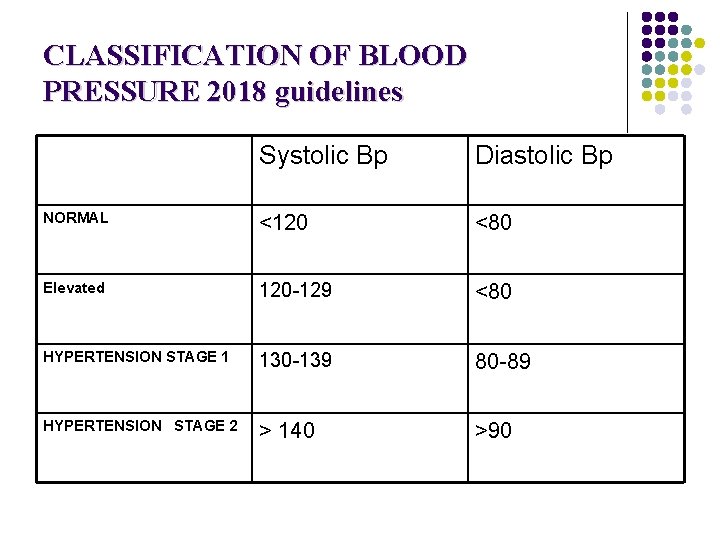
CLASSIFICATION OF BLOOD PRESSURE 2018 guidelines Systolic Bp Diastolic Bp NORMAL <120 <80 Elevated 120 -129 <80 HYPERTENSION STAGE 1 130 -139 80 -89 HYPERTENSION STAGE 2 > 140 >90
Risk factors for development of HTN l l l l l Increasing age (>55 for men, >65 for women). Smoking Male sex Race Obesity Family Hx of HTN High sodium intake Ethanol intake stress
Essential hypertension: >95% of cases. l The onset between ages 25&55 years l has multifactorial aetiology. Genetic factors: l BP tends to run in families. l Children of hypertensive parents tend to have higher BP than age-matched children of people with normal BP. l
Fetal factors: Low birth weight is associated with subsequent high BP due to the fetal adaptation to intrauterine undernutrition with long- term changes in the blood vessel structure or in the function of the crucial hormonal therapy Environmental factors: Obesity, Alcohol intake, sodium intake, stress Humoral mechanisms:
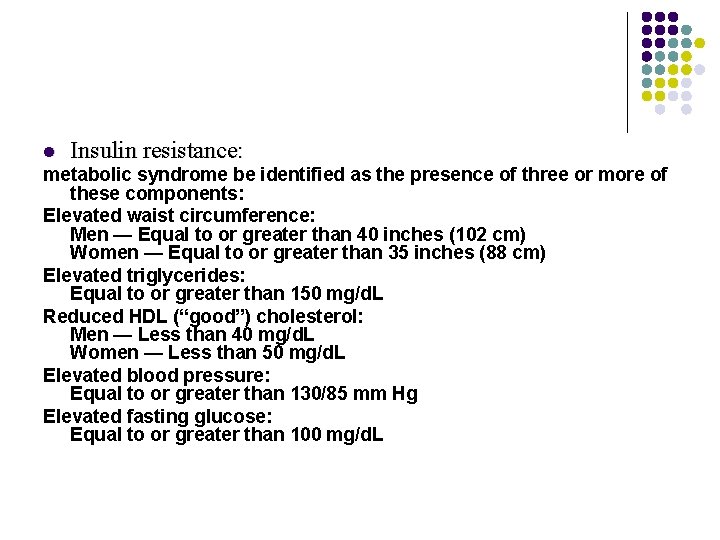
l Insulin resistance: metabolic syndrome be identified as the presence of three or more of these components: Elevated waist circumference: Men — Equal to or greater than 40 inches (102 cm) Women — Equal to or greater than 35 inches (88 cm) Elevated triglycerides: Equal to or greater than 150 mg/d. L Reduced HDL (“good”) cholesterol: Men — Less than 40 mg/d. L Women — Less than 50 mg/d. L Elevated blood pressure: Equal to or greater than 130/85 mm Hg Elevated fasting glucose: Equal to or greater than 100 mg/d. L
SECONDARY HYPERTENSION l Secondary hypertension is where blood pressure elevation is the result of a specific &potentially treatable cause.
RENAL DISEASES : DISEASES 80% of the case of secondary hypertension. l The common causes are: l diabetic nephropathy l chronic glomerulonephritis l adult poly cystic disease l chronic tubulointerstitial nephritis l renal vascular disease. Hypertension can itself cause or worsen renal disease. The mechanism of this blood pressure elevation is primarily due to sodium &water retention, although there can be inappropriate elevation of plasma rennin levels.
ENDOCRINE CAUSES l 1. conn’s syndrome ( aldesterone-producing adrenal adenoma). l 2. congenital adrenal hyperplasia. l 3. phaeochromocytoma (paroxysmal or sustained HTN). l 4. cushing’s syndrom (70%). l 5. acromegaly. l 6. primary hyperaldosteronism (0, 5%) ser. K is low. l 7. carcinoid tumer. l 8. thyroid ¶throid diseases. CONGENITAL CARDIOVASULAR (coarctaion of the aorta. ) (
DRUGS: 1. NSAIDs. 2. oral contraceptive. 3. steroids. 4. carbenoxolone. 5. liquorice. 6. sympathmimetics. 7. vasopressin. Patients taking monoamine oxidase inhibitors , who consume tyramine-contaning food , may develop paroxysms of sever hypertension. PREGNANCY
Diagnosis workup of hypertension: l history &physical examination l Asses risk factor &co-morbidities l secondary causes of hypertension should be excluded. l Target organ damage from BP should be evaluated. l any concomitant conditions (e. g. dyslipidemia or diabetes) should be identified. . l Obtain laboratory tests l Obtain electrocardiogram.
HISTORY l l patient with mild hypertension is usually asymptomatic. higher level of BP may be associated with headaches , epistaxis or nocturia l Onest l Duration l levels at time of onest l Family history of( HTN, CAD, stroke, Dyslipedemia, DM, premature cardiovascular death, renal disease) l Cardiovascular risk factor ( Dyslipedemia, DM, smoking obesity)
l symptoms suggesting end organ disease (chest pain orthopnea, paroxysmal noctural dyspnea, lower extremity edema, claudication , transient visual loss) l Specific question to rule out secondery HTN : (hairsutism, easy bruising, sweating , headaches & palpitations , muscle cramps leg claudication) l Past medical HX (renal disease, pre eclampsia)
l l l l Drug HX Smoking alcohol caffeine Diet Wt. gain Exercise Work and family environment education
examination l l l l Elevated blood pressure is usually the only abnormal sign. pulse BMI Hand: sweating , tremor, yellowish finger staining Skin : pigmentation, chronic renal failure Xanthelasmata Stigmata of cushing Neck: carotid bruits , distended vessels , thyroid enlargement Lung: basal crepitation Cardiac : size, rhythm, S 3, S 4, JVD, edema, radiofemoral delay in coarctation of the aorta. abdomen: renal artery bruits , masses, enlarged kidneys, aortic pulsation, signs of liver disease Neurologic: focal weakness , abnormal gait Extremities: pulse, edema Fundocopy
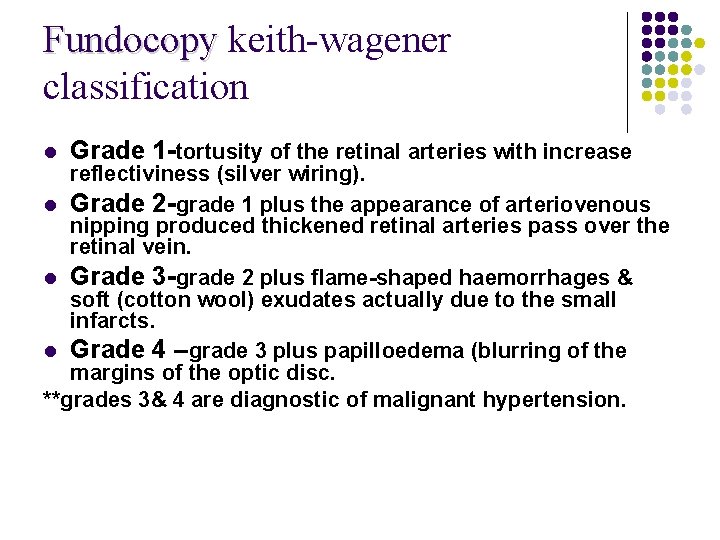
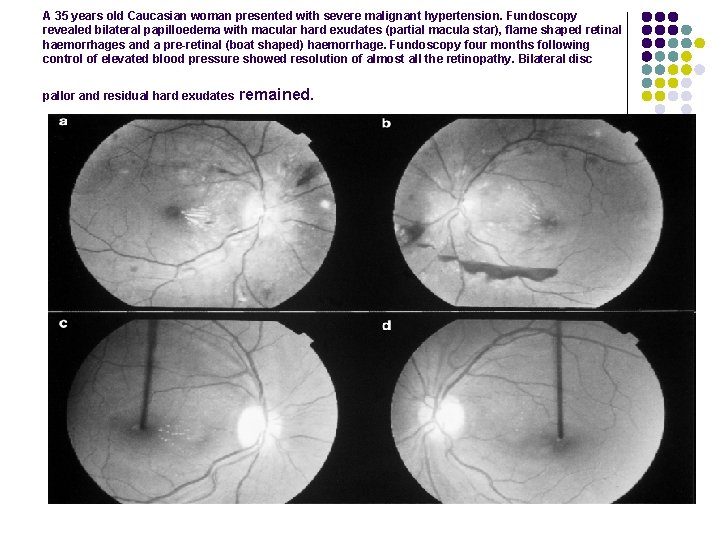
Fundocopy keith-wagener classification l Grade 1 -tortusity of the retinal arteries with increase reflectiviness (silver wiring). l Grade 2 -grade 1 plus the appearance of arteriovenous nipping produced thickened retinal arteries pass over the retinal vein. l Grade 3 -grade 2 plus flame-shaped haemorrhages & soft (cotton wool) exudates actually due to the small infarcts. l Grade 4 –grade 3 plus papilloedema (blurring of the margins of the optic disc. **grades 3& 4 are diagnostic of malignant hypertension.
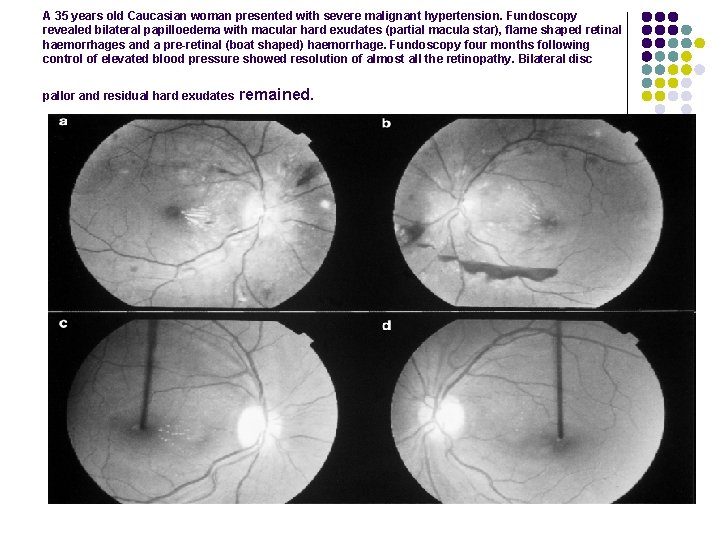
A 35 years old Caucasian woman presented with severe malignant hypertension. Fundoscopy revealed bilateral papilloedema with macular hard exudates (partial macula star), flame shaped retinal haemorrhages and a pre-retinal (boat shaped) haemorrhage. Fundoscopy four months following control of elevated blood pressure showed resolution of almost all the retinopathy. Bilateral disc pallor and residual hard exudates remained.
Investigation l l l CBC Urine sticks test for protein &blood. if neg. for protein Urinary microalbumin to screen for early nephropathy. Fasting blood for lipid (total &high density lipoprotein cholesterol) &glucose. Serum urea , creatinine. Uric acid electrolytes. A low serum potassium may indicate an (either primary hyperaldosteronism or glucocorticoid excess) &aldosterone, cortisol &renin measurements must then be made
l l l If urea & creatinine is elevated , more specific renal investigations are indicated creatinine clearance. . GFR renal U/S (in case of polycystic kidney disease , or parenchymal renal artery disease ) &renal isotope scan or renal angiography if renovascular disease (either atheromatous or fibromuscular dysplasiais suspected. Clinical suspecion of phaeochromocytoma should be investigated with measurement of urinary metanephrines &plasma or urinary catecholamines.
l l ECG If ECG shows evidence of coronary artery disease the coronary vascular status should be assessed. If left ventricular hypertrophy is suspected echocardiography or MRI should be undertaken. A chest X-ray is indicated if cardiac involvement or aortic coarctation is likely.
complications l Cerebrovascular disease &coronary artery disease are the most common causes of death. l Hypertensives have a sixfold increase in stroke(both haemorrhagic & atherothrombotic). l There is threefold increase in cardiac death (due either to coronary events or to cardiac failure ). l Peripheral arterial disease is twice as common. l hypertensive patients are also prone to renal failure. l Aortic aneurysm l retinopathy
Treatment l The Aim of treatment is to prevent complication. S. l Unless the patient has severe or malignant hypertension, there should be a period of assessment with repeated blood pressure measurements, combined with advice and nonpharmacological measures prior to the initiation of drug therapy.
l non-pharmacological measures: (3 -6 months) l weight reduction - BMI should be < 25 kg/m 2 low-fat and saturated fat diet low-sodium diet - < 6 g sodium chloride per day limited alcohol consumption - ≤ 21 units/week for men and ≤ 14 units/week for women dynamic exercise - at least 30 minutes' brisk walk per day increased fruit and vegetable consumption reduce cardiovascular risk by stopping smoking and increasing oily fish consumption l l l
l l Pharmacological therapy should be based on the following: The initiation of antihypertensive therapy in subjects with sustained systolic blood pressure (BP) ≥ 160 mm. Hg, or sustained diastolic BP ≥ 100 mm. Hg. Decide on treatment in subjects with sustained systolic blood pressure between 140 and 159 mm. Hg, or sustained diastolic BP between 90 and 99 mm. Hg, according to the presence or absence of target organ damage or a cardiovascular disease risk In patients with diabetes mellitus, the initiation of antihypertensive drug therapy if systolic BP is sustained ≥ 130 mm. Hg, or diastolic BP is sustained ≥ 80 mm. Hg.
l The main determinant of outcome following treatment is the level of blood pressure reduction that is achieved rather than the specific drug used to lower blood pressure. l Most hypertensive patients will require a combination of antihypertensive drugs to achieve the recommended targets. l In most hypertensive patients therapy with statins and aspirin to reduce the overall cardiovascular risk. l Glycaemic control should be optimized in diabetics (Hb. A 1 c < 7%).
Diuretics l Thiazide diuretics- : bendroflumethiazide (2. 5 -5 mg daily) and cyclopenthiazide (0. 250. 5 mg daily), Hydrochlorothiazide(12. 5 or 25 mg daily) l reduce the risk of stroke in patients with hypertension. l Slow the demineralization process in bone. l The lower doses seems to be equally effective as higher doses in the reduction of blood pressure and most have a duration of up to 24 hours. l The major concern with these agents is their adverse metabolic effects, particularly increased serum cholesterol, impaired glucose tolerance, hyperuricaemia (which may precipitate gout) and hypokalaemia. These tend to occur with higher doses of thiazide diuretics.
l l Loop diuretics : furosemide (40 mg daily) do have a hypotensive effect, but are not routinely used in the treatment of essential hypertension. Potassium-sparing : amiloride (5 -10 mg daily) or spironolactone (50 -200 mg daily) are not effective agents when used alone, with the exception of spironolactone in the treatment of hypertension and hypokalaemia associated with primary hyperaldosteronism.
beta-blocker l The beta-blockers: reduce cardiac output and decrease renin angiotensin mediated sodium and water reabsorption l Cardioselective: atenolol and bisoprolol. Intrinsic sympathomimetic activity. : cause less bradycardia. oxprenolol and pindolol. l l Lipid soluble: The agents that are less lipid-soluble are less likely to cause central nervous system side-effects. l These agents are especially useful in the treatment of patients with both hypertension and angina, previous MI, stable congestive heart failure , migraine headeches
l side-effects : Bradycardia bronchospasm cold extremities fatigue bad dreams hallucinations. Raynaud phenomen Depression Impotence Increase plasma TG Depress HDL
l contraindicated : in patients with unstable congestive heart failure. l B Blockers are used cautiously in patients with type 1 diabetes, since they can mask the symptoms of hypoglycemia l they may increase blood glucose levels in type 2 diabetics l These drugs should also be used with caution in patients with advanced peripheral vascular disease associated with rest pain or nonhealing ulcers, but they are generally well tolerated in patients with mild claudication. .
Angiotensin-converting enzyme (ACE) inhibitors l l l l These drugs block the conversion of angiotensin I to angiotensin II, which is a potent vasoconstrictor. They also block the degradation of bradykinin, a potent vasodilator. captopril (50 -150 mg daily in divided doses) ramipril (2. 5 -10 mg daily), enalapril or lisinopril (10 -20 mg daily), and trandolapril (1 -4 mg daily). There is evidence that black African patients respond less well to ACE inhibitors unless combined with diuretics. They are particularly useful in diabetics with nephropathy, where they have been shown to slow disease progression, and in those patients with symptomatic or asymptomatic left ventricular dysfunction, where they have been shown to improve survival
side-effects : l hypotension following the first dose, which is usually seen in sodium-depleted patients or in those on treatment with large doses of diuretics. l deterioration of renal function in those with severe bilateral renovascular disease (in whom the production of angiotensin II is playing a major role in maintaining renal perfusion by causing efferent arteriolar constriction at the glomerulus). l They also cause mild dry cough due to their effect on bradykinin.
l l Hyperkalemia may develop in patients with intrinsic kidney disease and type IV renal tubular acidosis (commonly seen in diabetics) and in the elderly. Skin rashes Angioedema Exposure of the fetus to ACE inhibitors during the second and third trimesters of pregnancy has been associated with a variety of defects due to hypotension and reduced renal blood flow
Angiotensin II receptor antagonists l This group of agents selectively block the receptors for angiotensin II . l They share many of the actions of ACE inhibitors but, since they do not have any effect on bradykinin, do not cause a cough . They are currently used for patients who cannot tolerate ACE inhibitors because of persistent cough. l Angioneurotic oedema and renal dysfunction are encountered less with these drugs than with ACE inhibitors. l The agents include losartan (50 -100 mg daily), candesartan (16 mg daily) valsartan (80 -160 mg daily), irbesartan (75 -300 mg daily) and telmisartan (20 -80 mg/daily). l
Calcium-channel blockers These agents effectively reduce blood pressure by causing arteriolar dilatation, and some also reduce the force of cardiac contraction. l l nifedipine (10 -20 mg three times daily) amlodipine (5 -10 mg daily) felodipine (5 -20 mg daily) long-acting nifedipine (20 -90 mg daily). they are especially useful in patients with concomitant IHD. The major side-effects are particularly seen with the short-acting agents and include l headache, l sweating, l swelling of the ankles, l palpitations l and flushing. Many of these side-effects can be lessened by the co-administration of a beta-blocker.
Alpha-blockers l Prazosin, terazosin, and doxazosin : block postsynaptic -receptors, relax smooth muscle, and reduce blood pressure by lowering peripheral vascular resistance. These agents are effective as single-drug therapy in some individuals l tachyphylaxis may appear during long-term therapy. l hypotension and syncope after the first dose which, therefore, should be small and given at bedtime. l Post-dosing palpitations, headache, and nervousness may continue to occur during long-term therapy; these symptoms may be less frequent or severe with doxazosin because of its more gradual onset of action. l Cataractectomy in patients exposed to alfa -blockers can be complicated by the floppy iris syndrome, even after discontinuation of the drug, so the ophthalmologist should be alerted that the patient has been taking the drug prior to surgery l
l l l they increase HDL cholesterol while reducing total cholesterol. should generally not be used as initial agents to treat hypertension—except in men with symptomatic prostatism Labetalol is an agent that has combined alphaand beta-blocking properties, but is not commonly used, except in pregnancy-induced hypertension.
Drugs with Central Sympatholytic Action l l l l Methyldopa, clonidine, guanabenz, and guanfacine : lower blood pressure by stimulating -adrenergic receptors in the central nervous system, thus reducing efferent peripheral sympathetic outflow. These agents are effective as single therapy in some patients, they are usually used as second- or third-line agents because of the high frequency of drug intolerance including sedation, fatigue, dry mouth, postural hypotension, and impotence. An important concern is rebound hypertension following withdrawal. Methyldopa also causes hepatitis and hemolytic anemia and is avoided except in individuals who have already tolerated long-term therapy. There is considerable experience with methyldopa in pregnant women, and it is still used for this population. Clonidine is available in patches and may have particular value in patients in whom compliance is a troublesome issue
Arteriolar Dilators l Hydralazine and minoxidil : relax vascular smooth muscle and produce peripheral vasodilation. l When given alone, they stimulate reflex tachycardia, increase myocardial contractility, and cause headache, palpitations, and fluid retention. l They are usually given in combination with diuretics and Bblockers in resistant patients. l Hydralazine produces frequent gastrointestinal disturbances and may induce a lupus-like syndrome. l Minoxidil causes hirsutism and marked fluid retention
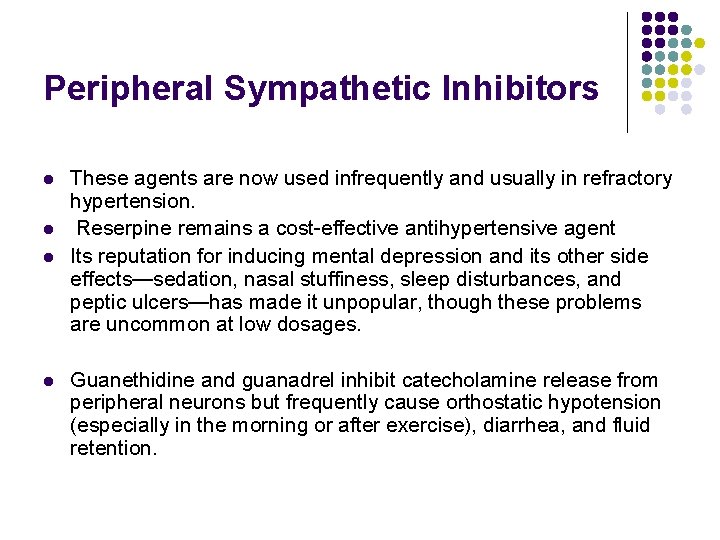
Peripheral Sympathetic Inhibitors l l These agents are now used infrequently and usually in refractory hypertension. Reserpine remains a cost-effective antihypertensive agent Its reputation for inducing mental depression and its other side effects—sedation, nasal stuffiness, sleep disturbances, and peptic ulcers—has made it unpopular, though these problems are uncommon at low dosages. Guanethidine and guanadrel inhibit catecholamine release from peripheral neurons but frequently cause orthostatic hypotension (especially in the morning or after exercise), diarrhea, and fluid retention.
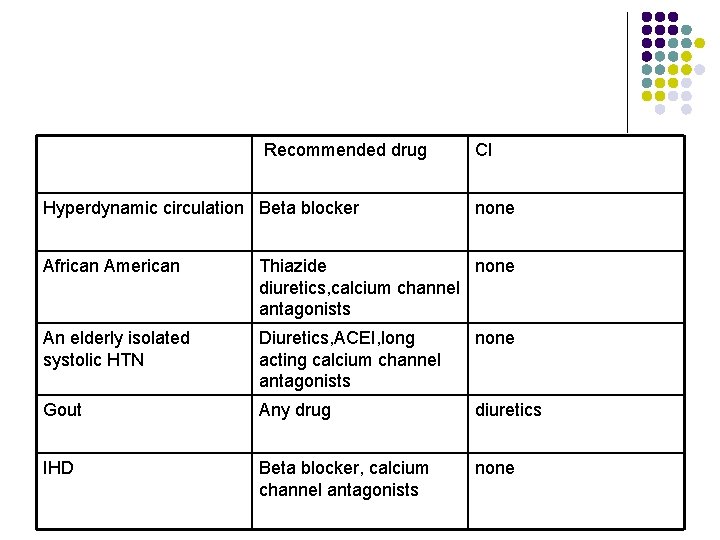
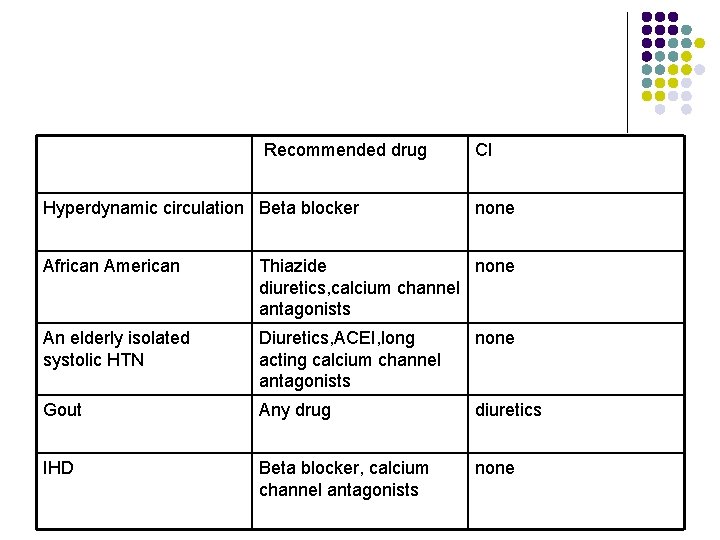
Recommended drug Hyperdynamic circulation Beta blocker CI none African American Thiazide none diuretics, calcium channel antagonists An elderly isolated systolic HTN Diuretics, ACEI, long acting calcium channel antagonists none Gout Any drug diuretics IHD Beta blocker, calcium channel antagonists none
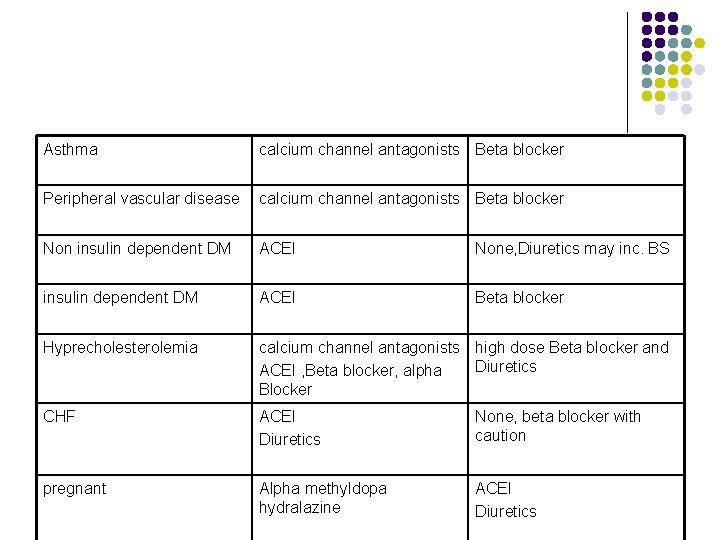
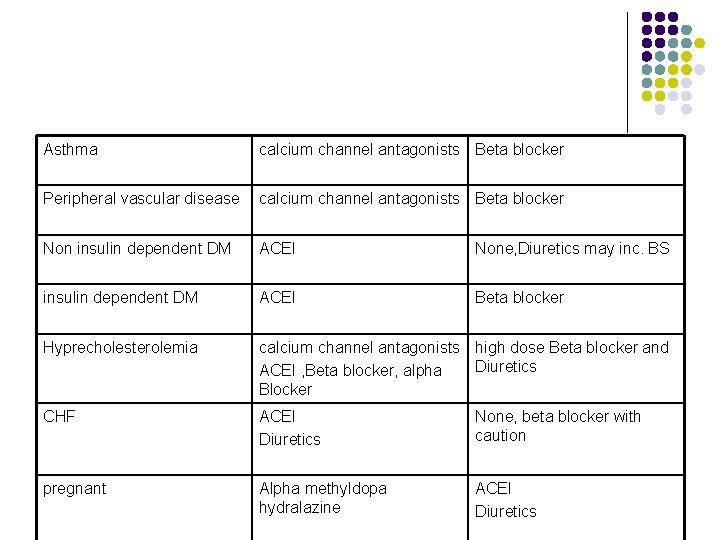
Asthma calcium channel antagonists Beta blocker Peripheral vascular disease calcium channel antagonists Beta blocker Non insulin dependent DM ACEI None, Diuretics may inc. BS insulin dependent DM ACEI Beta blocker Hyprecholesterolemia calcium channel antagonists high dose Beta blocker and Diuretics ACEI , Beta blocker, alpha Blocker CHF ACEI Diuretics None, beta blocker with caution pregnant Alpha methyldopa hydralazine ACEI Diuretics
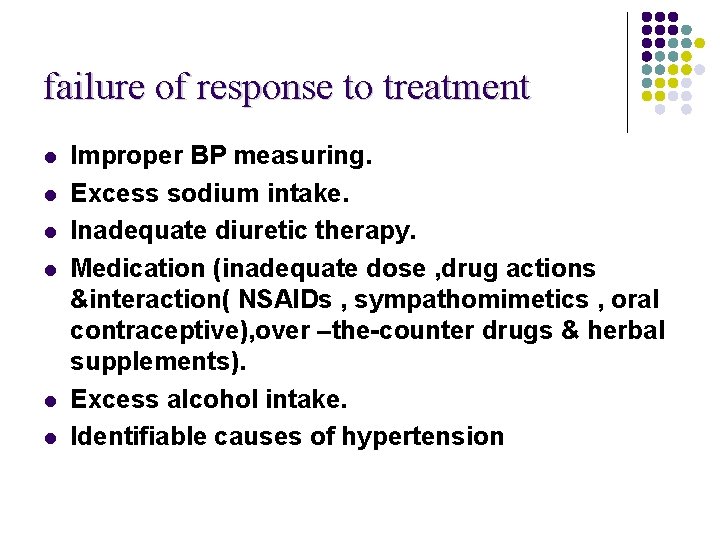
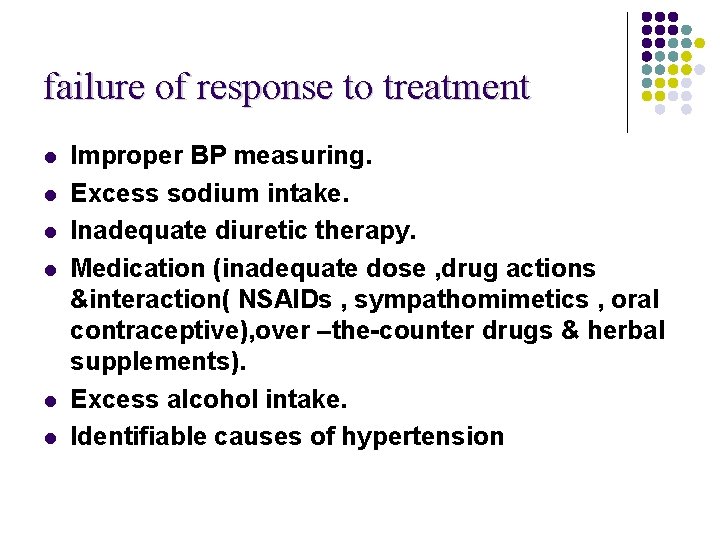
failure of response to treatment l l l Improper BP measuring. Excess sodium intake. Inadequate diuretic therapy. Medication (inadequate dose , drug actions &interaction( NSAIDs , sympathomimetics , oral contraceptive), over –the-counter drugs & herbal supplements). Excess alcohol intake. Identifiable causes of hypertension
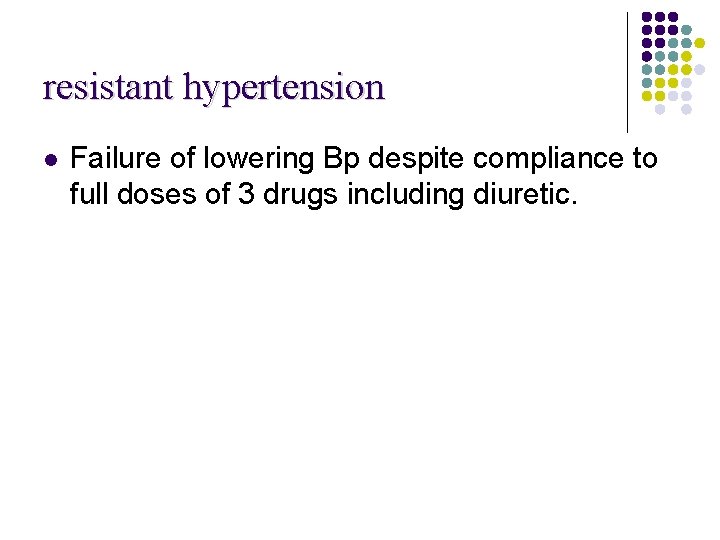
resistant hypertension l Failure of lowering Bp despite compliance to full doses of 3 drugs including diuretic.
malignant hypertension l l l Malignant or accelerated hypertension occurs when BP rises rapidly & is considered with hypertension (diastolic blood pressure › 120 mm. Hg). The characteristic histological change is fibrinoid necrosis of the vessel wall &unless treated , it may lead to death from progressive renal failure, heart failure , aortic dissection or stroke. The changes in rapidly progressive renal failure , proteinuria & haematuria. There is also a high risk of cerebral oedema & haemorrhage with resultant encephalopathy. In retina there may be flame shaped haemorrhages , cotton wool spots , hard exudates & papilloedema , without effective treatment there is a 1 –year survival of less than 20%.
Management of severe or malignant hypertension l Patients with severe hypertension (diastolic pressure > 140 mm. Hg), malignant hypertension (grades 3 or 4 retinopathy), hypertensive encephalopathy or with severe hypertensive complications, such as cardiac failure, should be admitted to hospital for immediate initiation of treatment. l However, it is unwise to reduce the blood pressure too rapidly since this may lead to cerebral, renal, retinal or myocardial infarction l the aim is to reduce the diastolic blood pressure to 100 -110 mm. Hg over 24 -48 hours. l This is usually achieved with oral medication, e. g. atenolol or amlodipine. l The blood pressure can then be normalized over the next 2 -3 days.
l l l When rapid control of blood pressure is required (e. g. in an aortic dissection), the agent of choice is intravenous sodium nitroprusside. Alternatively, an infusion of labetalol can be used. The infusion dosage must be titrated against the blood pressure response. Fenoldopam, a selective peripheral dopamine receptor agonist, is as effective as nitroprusside
Hypertensive urgencies l l l l are situations in which blood pressure must be reduced within a few hours. These include patients with asymptomatic severe hypertension (systolic blood pressure > 220 mm Hg or diastolic pressure > 125 mm Hg that persists after a period of observation) and those with optic disk edema progressive target organ complications, and severe perioperative hypertension. Elevated blood pressure levels alone—in the absence of symptoms or new or progressive target organ damage—rarely require emergency therapy. Parenteral drug therapy is not usually required, and partial reduction of blood pressure with relief of symptoms is the goal.
Hypertensive emergencies require substantial reduction of blood pressure within 1 hour to avoid the risk of serious morbidity or death. Although blood pressure is usually strikingly elevated (diastolic pressure > 130 mm Hg), the correlation between pressure and end-organ damage is often poor. . Emergencies include l hypertensive encephalopathy (headache, irritability, confusion, and altered mental status due to cerebrovascular spasm), l hypertensive nephropathy (hematuria, proteinuria, and progressive kidney dysfunction due to arteriolar necrosis and intimal hyperplasia of the interlobular arteries), l intracranial hemorrhage, l aortic dissection, l preeclampsia-eclampsia, l pulmonary edema, l unstable angina, l or myocardial infarction.
l l Parenteral therapy is indicated in most hypertensive emergencies, especially if encephalopathy is present. The initial goal in hypertensive emergencies is to reduce the pressure by no more than 25% (within minutes to 1 or 2 hours) and then toward a level of 160/100 mm Hg within 2– 6 hours. Excessive reductions in pressure may precipitate coronary, cerebral, or renal ischemia. To avoid such declines, the use of agents that have a predictable, dose-dependent, transient, and not precipitous antihypertensive effect is preferable. the use of sublingual or oral fast-acting nifedipine preparations is best avoided
l l l Acute ischemic stroke is often associated with marked elevation of blood pressure, which will usually fall spontaneously. In such cases, antihypertensives should only be used if the blood pressure exceeds 220/120 mm Hg, and blood pressure should be reduced cautiously by 10– 15%. If thrombolytics are to be given, blood pressure should be maintained at < 185/110 mm Hg during treatment and for 24 hours following treatment.
l l l In hemorrhagic stroke, the aim is to minimize bleeding with a target mean arterial pressure of < 130 mm Hg. In acute subarachnoid hemorrhage, as long as the bleeding source remains uncorrected, a compromise must be struck between preventing further bleeding and maintaining cerebral perfusion in the face of cerebral vasospasm. In this situation, blood pressure goals depend on the patient's usual blood pressure. In normotensive patients, the target should be a systolic blood pressure of 110– 120 mm Hg; in hypertensive patients, blood pressure should be treated to 20% below baseline pressure.
l l l In the treatment of hypertensive emergencies complicated by (or precipitated by) central nervous system injury, labetalol or nicardipine are good choices, since they are nonsedating and do not appear to cause significant increases in cerebral blood flow or intracranial pressure in this setting. In hypertensive emergencies arising from catecholaminergic mechanisms, such as pheochromocytoma or cocaine use, Bblockers can worsen the hypertension because of unopposed peripheral vasoconstriction; phentolamine is a better choice. Labetalol is useful in these patients if the heart rate must be controlled.
THANK YOU l l l Clinical Medicine Kumar Clark Current medical diagnosis and treatment Essential of family medicine Swansons family practice Review Lecture notes on family medicine Blueprints medicine
 Dua allahumma rabba shahr ramadan
Dua allahumma rabba shahr ramadan Friday duaa
Friday duaa Ux research portfolio
Ux research portfolio Hujjat meaning in urdu
Hujjat meaning in urdu Pachyméninges
Pachyméninges Veretigo
Veretigo Calcium channel blockers examples
Calcium channel blockers examples Ocular hypertension dvla
Ocular hypertension dvla Masked hypertension
Masked hypertension Isolated systolic hypertension
Isolated systolic hypertension Presinusoidal portal hypertension
Presinusoidal portal hypertension Health coaches for hypertension control
Health coaches for hypertension control Hypertensive crisis
Hypertensive crisis Pulmonary hypertension
Pulmonary hypertension Pathophysiology of pulmonary hypertension
Pathophysiology of pulmonary hypertension Non pharmacological management of hypertension
Non pharmacological management of hypertension Pulmonary hypertension definition
Pulmonary hypertension definition Essential hypertension
Essential hypertension Hypertension vs hypotension
Hypertension vs hypotension 6 vital signs first aid
6 vital signs first aid Modifiable risk factors for hypertension
Modifiable risk factors for hypertension Sachin gupta md
Sachin gupta md Nursing management of portal hypertension
Nursing management of portal hypertension Pico question examples hypertension
Pico question examples hypertension Hypertension urgency vs emergency
Hypertension urgency vs emergency Med
Med Conclusion of hypertension
Conclusion of hypertension Antihypertensive drugs
Antihypertensive drugs Paedp echo
Paedp echo Traitement hypertension
Traitement hypertension Jnc 8 classification of hypertension ppt
Jnc 8 classification of hypertension ppt Rules of halves in hypertension
Rules of halves in hypertension Presenting complaints of hypertension
Presenting complaints of hypertension Case scenario for hypertension
Case scenario for hypertension Pulmonary hypertension causes
Pulmonary hypertension causes Diagnosis hypertension
Diagnosis hypertension Portal hypertension mayo clinic
Portal hypertension mayo clinic Endorine
Endorine Hypertension
Hypertension Jnc 8 classification of hypertension pdf
Jnc 8 classification of hypertension pdf Nt pro brain natriuretic peptide
Nt pro brain natriuretic peptide Systemic vascular resistance
Systemic vascular resistance Hypertension
Hypertension Signs of increased intracranial pressure
Signs of increased intracranial pressure Conclusion of hypertension
Conclusion of hypertension Cataractectomy
Cataractectomy Hypertension
Hypertension What is office blood pressure
What is office blood pressure Hypertension investigation chart
Hypertension investigation chart Causes of secondary hypertension
Causes of secondary hypertension Classification of hypertension
Classification of hypertension Gastropathie en mosaïque
Gastropathie en mosaïque Hypertensive urgency vs emergency
Hypertensive urgency vs emergency Conclusion of hypertension
Conclusion of hypertension Pratt's test for varicose veins
Pratt's test for varicose veins Demadex
Demadex Mitral stenosis pulmonary hypertension
Mitral stenosis pulmonary hypertension Conclusion of hypertension
Conclusion of hypertension Amas faa medication
Amas faa medication Jnc 7 hypertension
Jnc 7 hypertension Antihypertensive drugs classification
Antihypertensive drugs classification Portal hypertension symptoms and signs
Portal hypertension symptoms and signs Pneumotrieste
Pneumotrieste Stages of pulmonary hypertension
Stages of pulmonary hypertension Definition of hypertension
Definition of hypertension Portal hypertension
Portal hypertension Sohil rangwala
Sohil rangwala Neonatal liver failure
Neonatal liver failure