Liver Cirrhosis 1 Prof Mohamed Elhasafi Hepatology Unit











































- Slides: 85
Liver Cirrhosis (1) Prof. Mohamed Elhasafi, Hepatology Unit, Alexandria Faculty of Medicine.
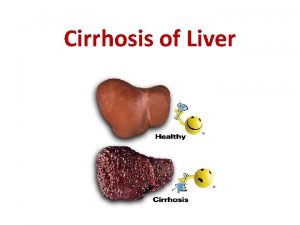
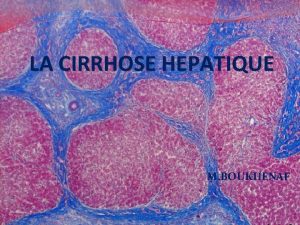
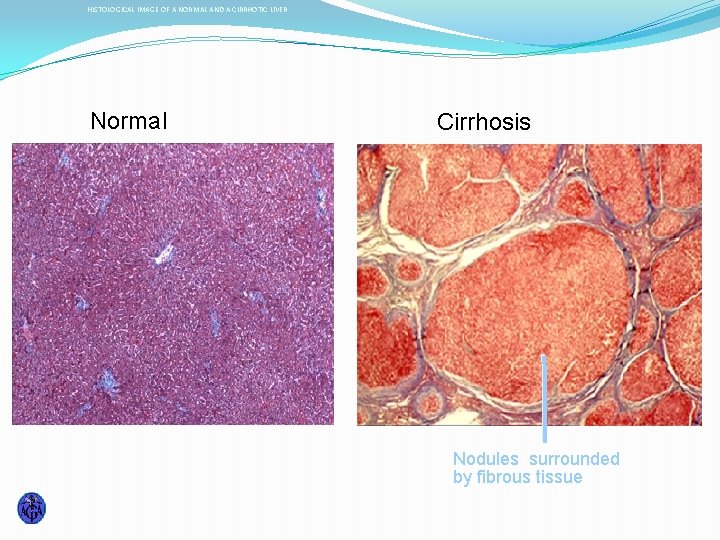
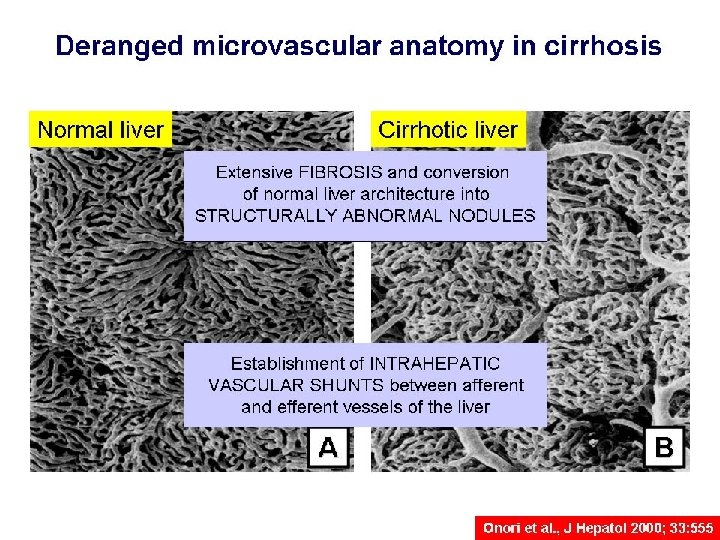
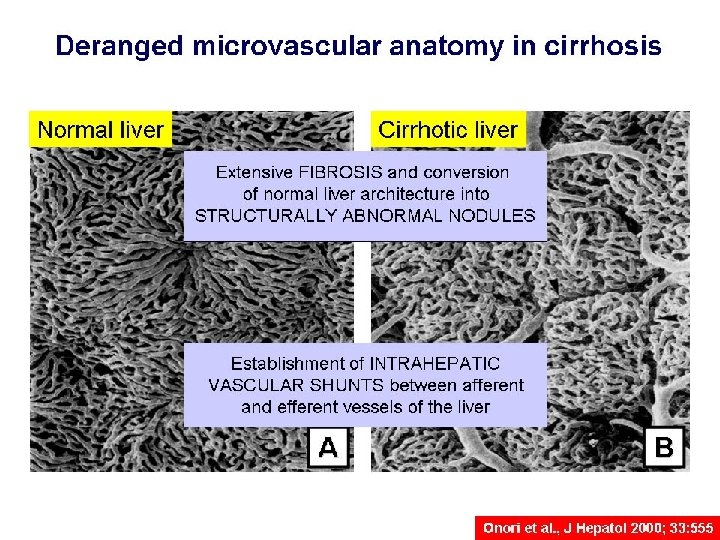
Cirrhosis is defined histologically as a diffuse hepatic process characterized by fibrosis and the conversion of normal liver architecture into structurally abnormal nodules.
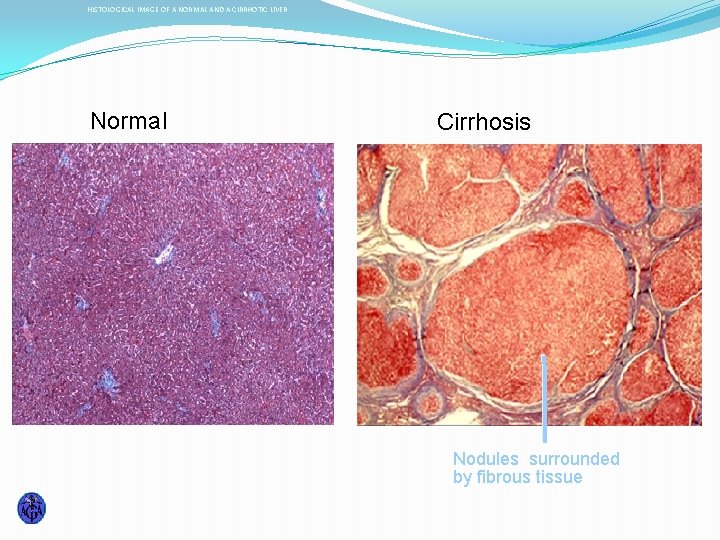
HISTOLOGICAL IMAGE OF A NORMAL AND A CIRRHOTIC LIVER Normal Cirrhosis Nodules surrounded by fibrous tissue
Cirrhosis represents the final common histologic pathway for a wide variety of chronic liver diseases. The progression of liver injury to cirrhosis may occur over weeks to years. Indeed, patients with hepatitis C may have chronic hepatitis for as long as 40 years before progressing to cirrhosis.
Classification of cirrhosis : Morphological classification �Micronodular cirrhosis. �Characterized by thick , regular septa, by regenerating small nodules varying little in size, and by involvement of every nodule. �Macronodular cirrhosis. �Characterized by septa and nodules of variable sizes and by normal lobules in larger nodules. �Mixed cirrhosis.


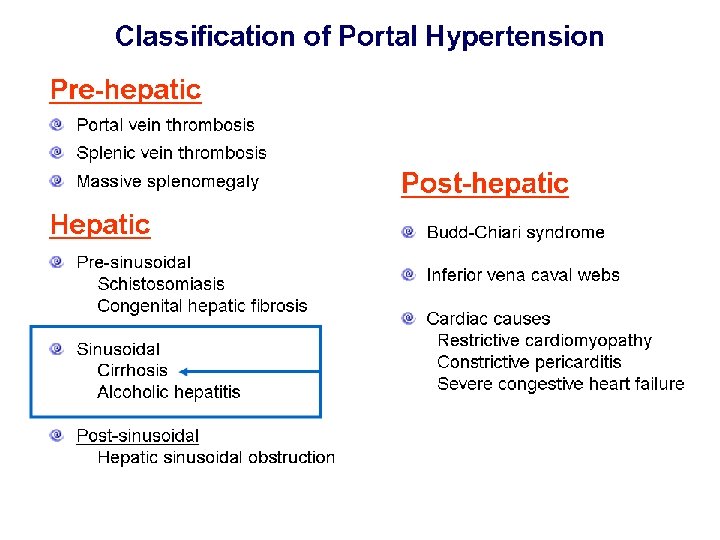
Etiology of cirrhosis : �Viral hepatitis ( B, C, D ). �Autoimmune chronic hepatitis. �Alcohol. �Metabolic ( Non-alcoholic steatohepatitis, hemochromatosis, Wilson's disease, alpha 1 -antitrypsin deficiency, type IV glycogenosis ). �Cholestatic ( Primary biliary cirrhosis, Primary sclerosing cholangitis). �Hepatic venous outflow obstruction ( veno-occlusive disease, Budd-Chiari syndrome ). �Drug-induced ( methotrexate, amiodarone ) �Cryptogenic.






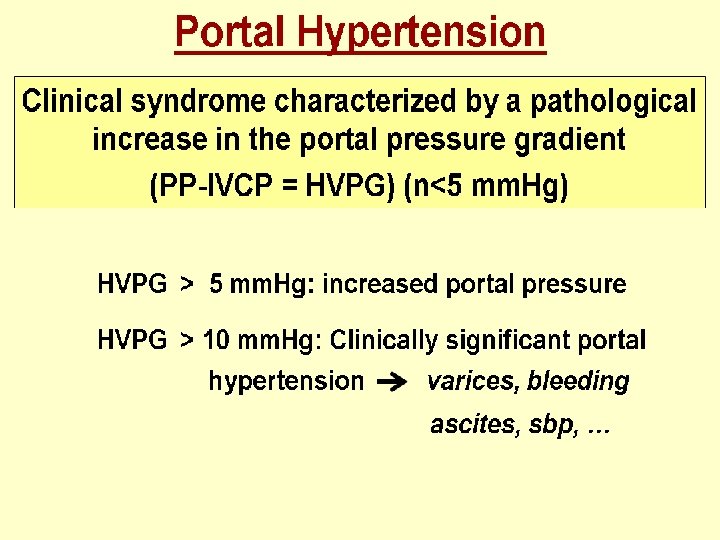
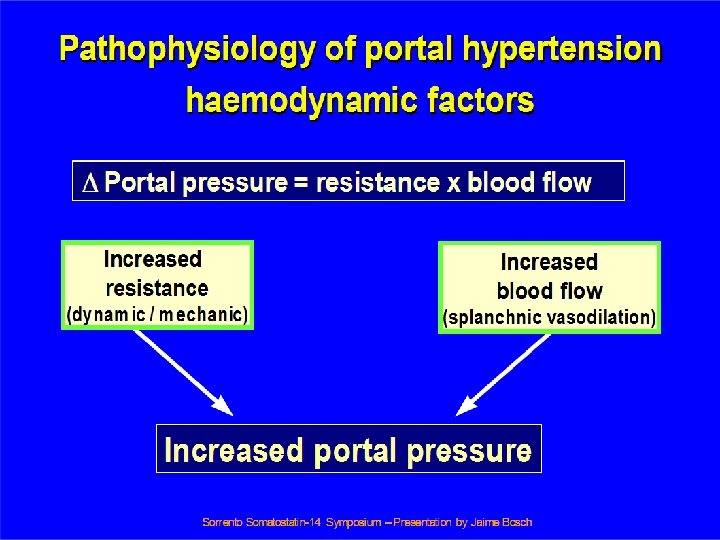


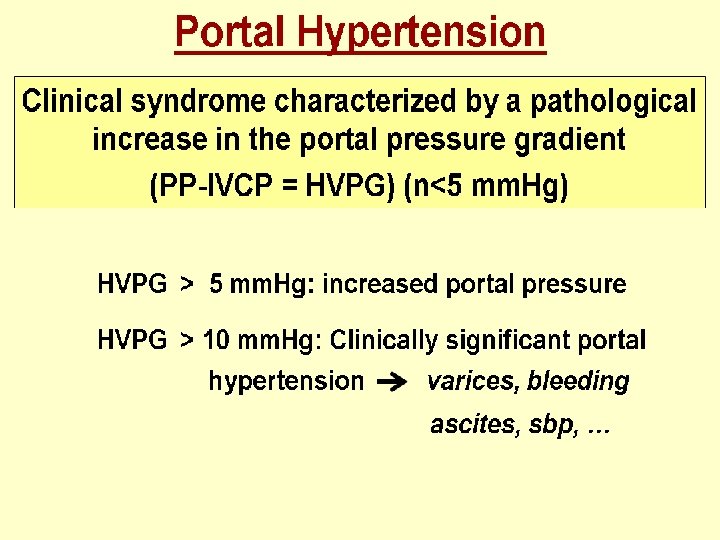
Clinical features : Cirrhosis results in two major clinical events : Manifestations of hepato-cellular failure. & Manifestations of portal hypertention.
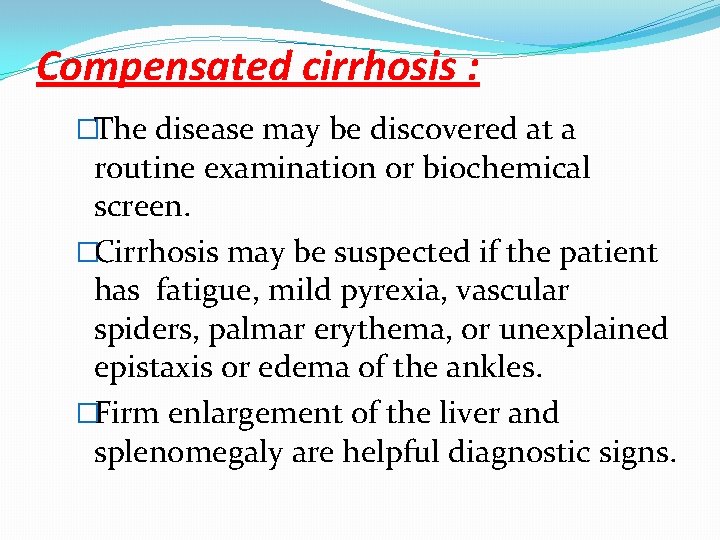
Compensated cirrhosis : �The disease may be discovered at a routine examination or biochemical screen. �Cirrhosis may be suspected if the patient has fatigue, mild pyrexia, vascular spiders, palmar erythema, or unexplained epistaxis or edema of the ankles. �Firm enlargement of the liver and splenomegaly are helpful diagnostic signs.
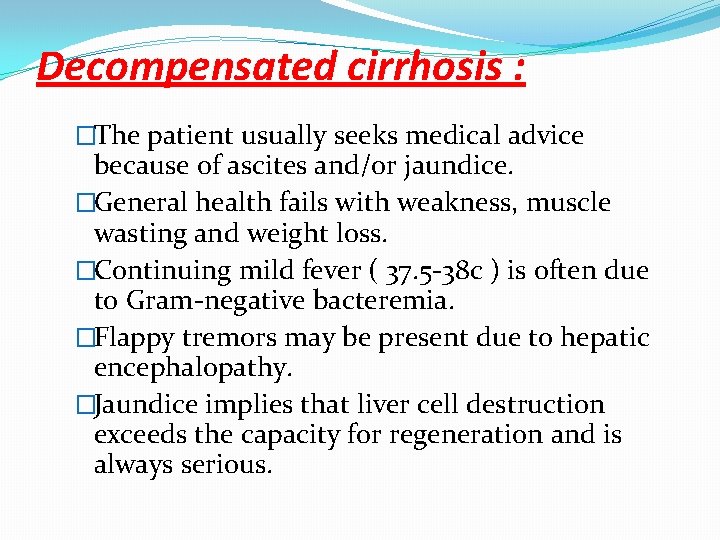
Decompensated cirrhosis : �The patient usually seeks medical advice because of ascites and/or jaundice. �General health fails with weakness, muscle wasting and weight loss. �Continuing mild fever ( 37. 5 -38 c ) is often due to Gram-negative bacteremia. �Flappy tremors may be present due to hepatic encephalopathy. �Jaundice implies that liver cell destruction exceeds the capacity for regeneration and is always serious.

�The skin may be pigmented. �Purpura over the arms, shoulders, and lower limbs may be associated with a low platelets count. �Spontaneous bruising and epistaxis reflect a prothrombin deficiency. �The circulation is overactive. The blood pressure is low. �Sparse body hair, vascular spiders, palmar erythema, white nails and gonadal atrophy and gynecomastia are common.


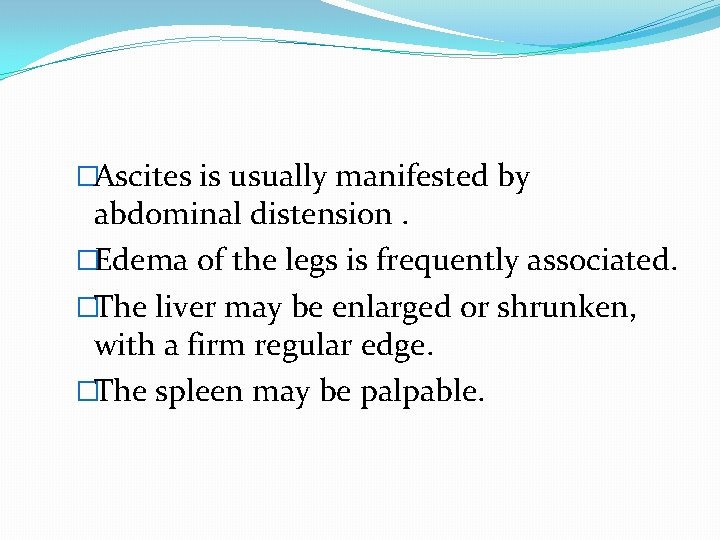
�Ascites is usually manifested by abdominal distension. �Edema of the legs is frequently associated. �The liver may be enlarged or shrunken, with a firm regular edge. �The spleen may be palpable.

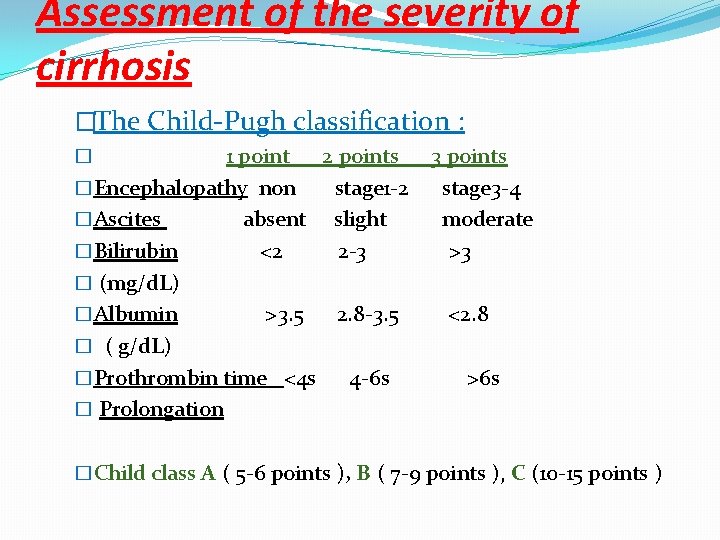
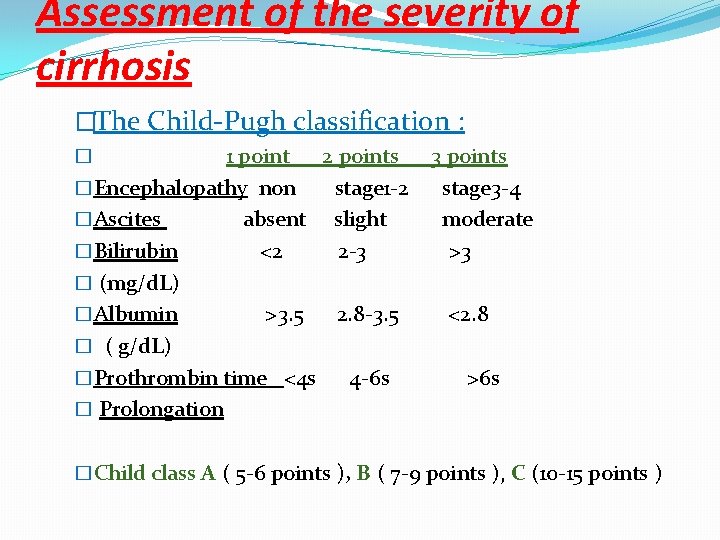
Assessment of the severity of cirrhosis �The Child-Pugh classification : 1 point 2 points �Encephalopathy non stage 1 -2 �Ascites absent slight �Bilirubin <2 2 -3 � (mg/d. L) �Albumin >3. 5 2. 8 -3. 5 � ( g/d. L) �Prothrombin time <4 s 4 -6 s � Prolongation � 3 points stage 3 -4 moderate >3 <2. 8 >6 s �Child class A ( 5 -6 points ), B ( 7 -9 points ), C (10 -15 points )

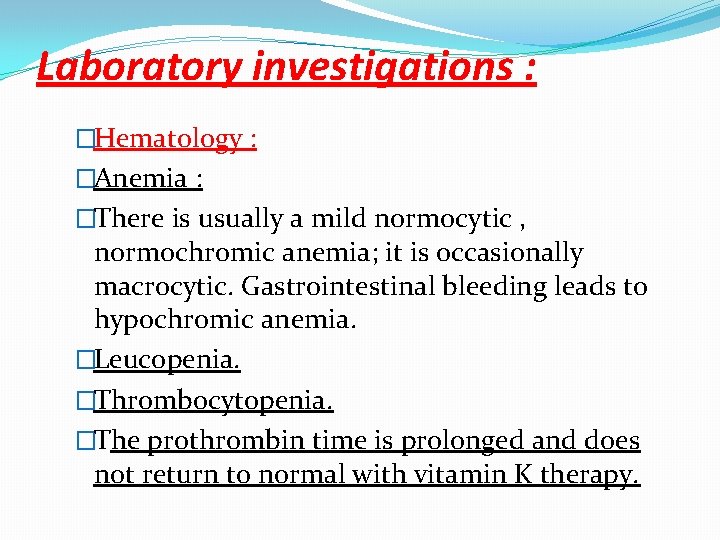
Laboratory investigations : �Hematology : �Anemia : �There is usually a mild normocytic , normochromic anemia; it is occasionally macrocytic. Gastrointestinal bleeding leads to hypochromic anemia. �Leucopenia. �Thrombocytopenia. �The prothrombin time is prolonged and does not return to normal with vitamin K therapy.
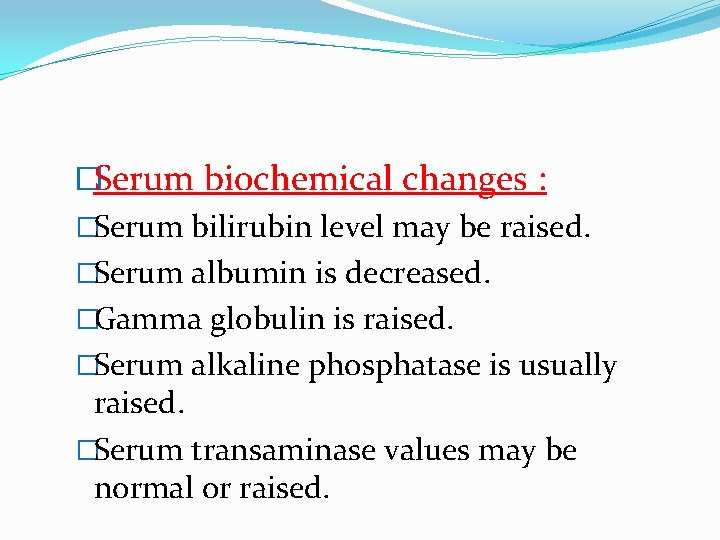
�Serum biochemical changes : �Serum bilirubin level may be raised. �Serum albumin is decreased. �Gamma globulin is raised. �Serum alkaline phosphatase is usually raised. �Serum transaminase values may be normal or raised.
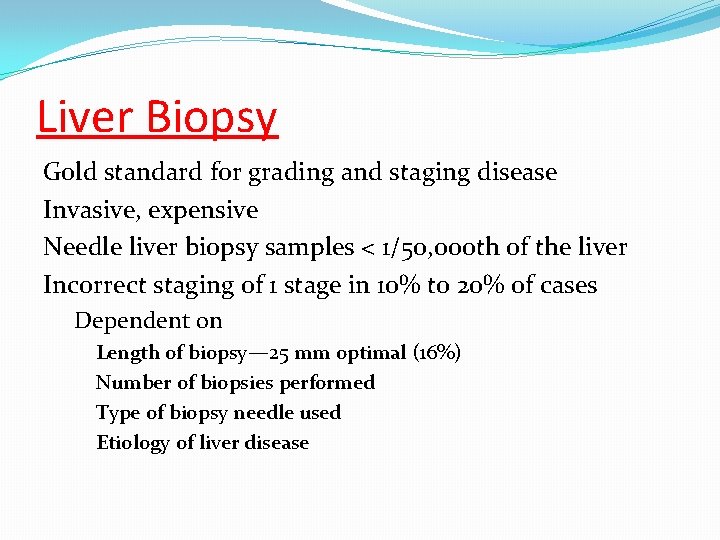
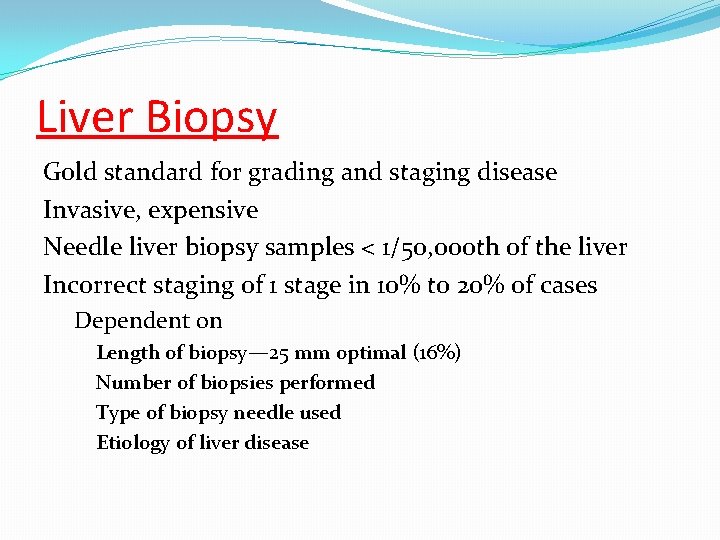
Liver Biopsy Gold standard for grading and staging disease Invasive, expensive Needle liver biopsy samples < 1/50, 000 th of the liver Incorrect staging of 1 stage in 10% to 20% of cases Dependent on Length of biopsy— 25 mm optimal (16%) Number of biopsies performed Type of biopsy needle used Etiology of liver disease
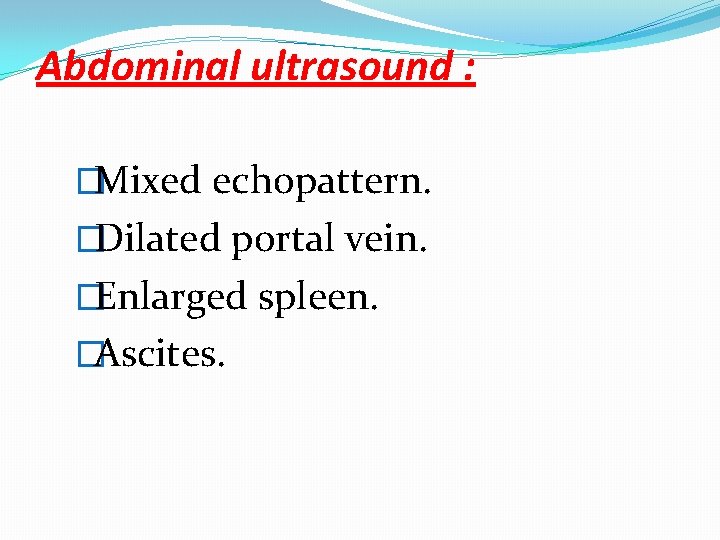
Abdominal ultrasound : �Mixed echopattern. �Dilated portal vein. �Enlarged spleen. �Ascites.

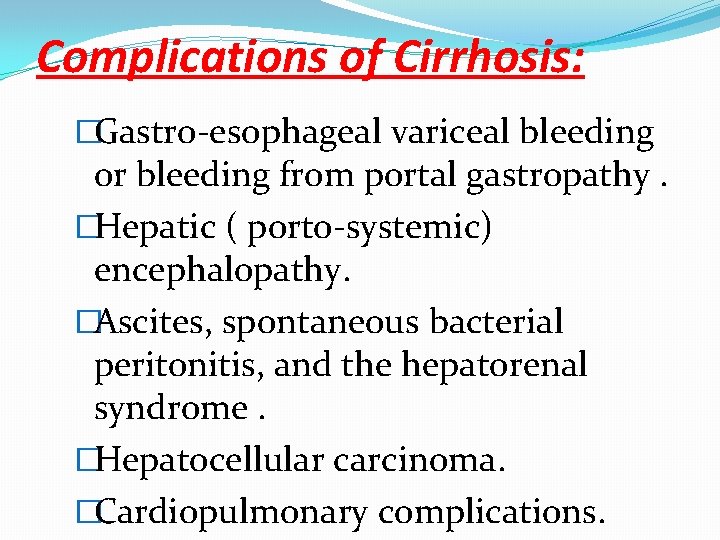
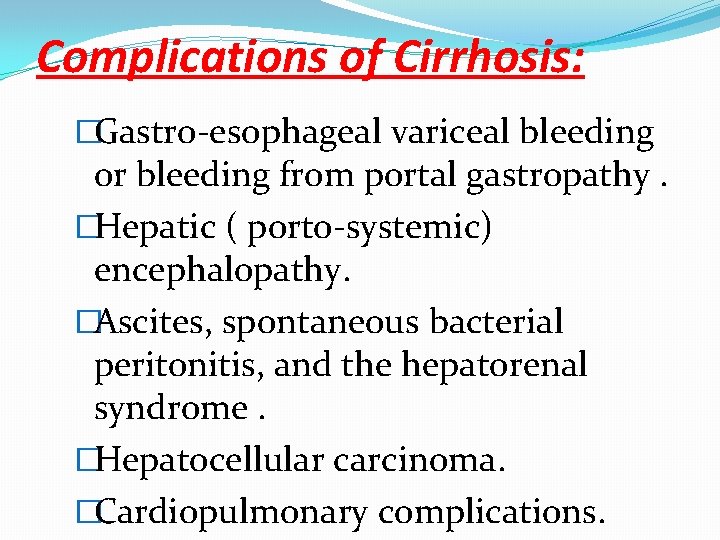
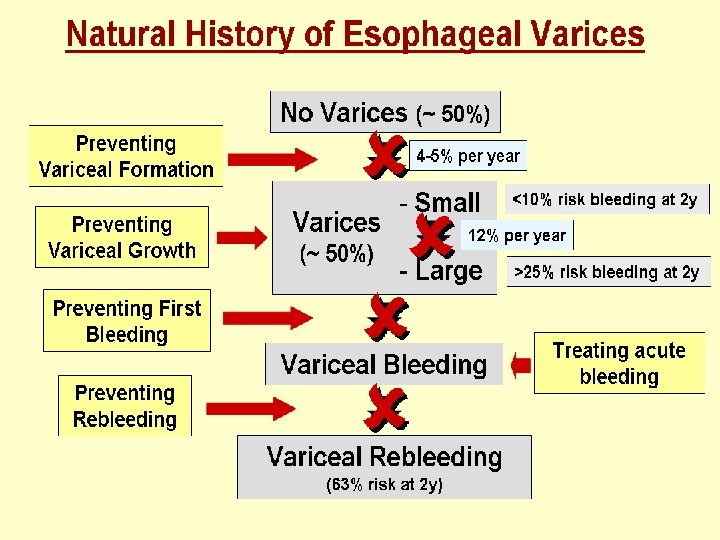
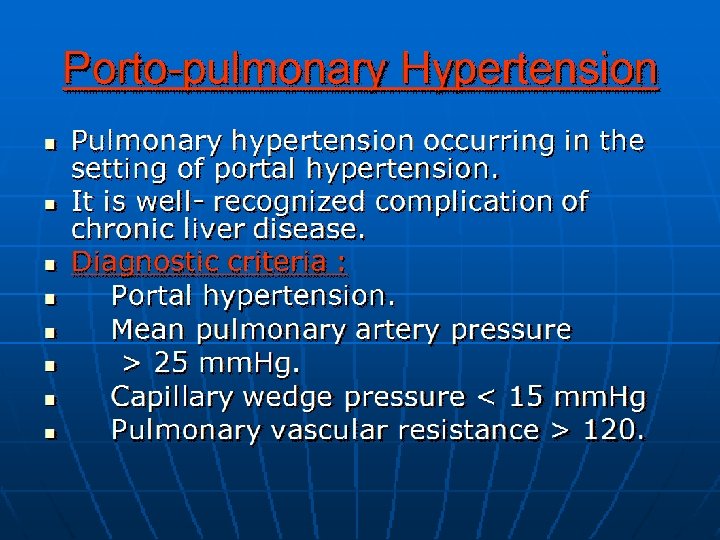
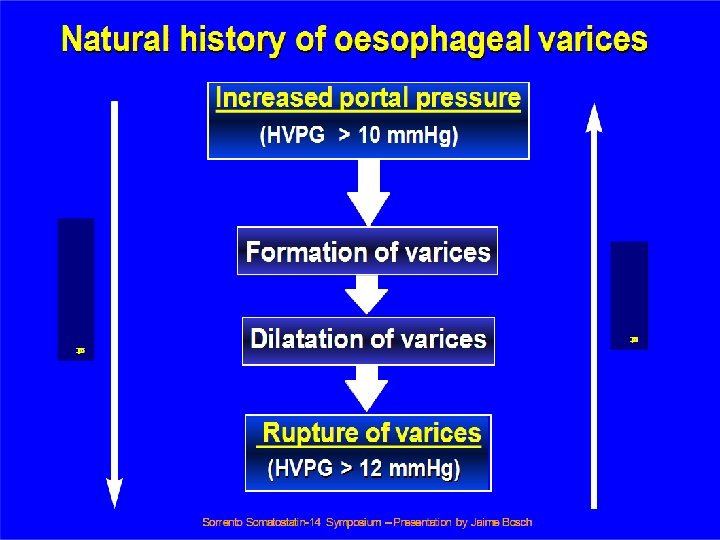
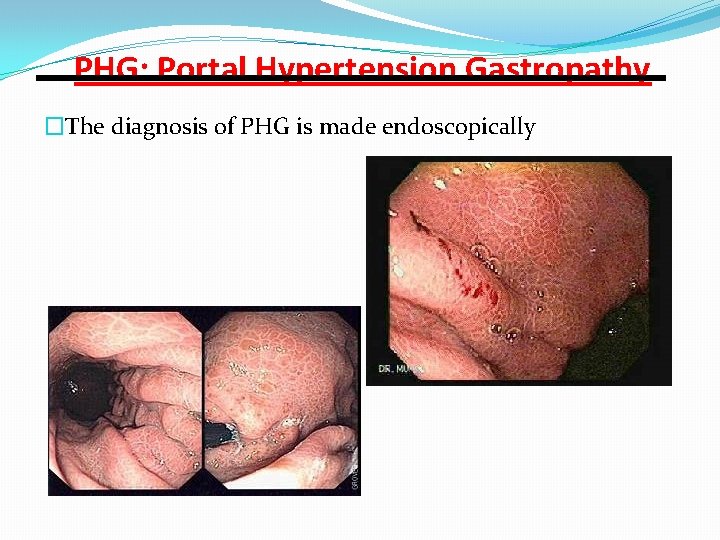
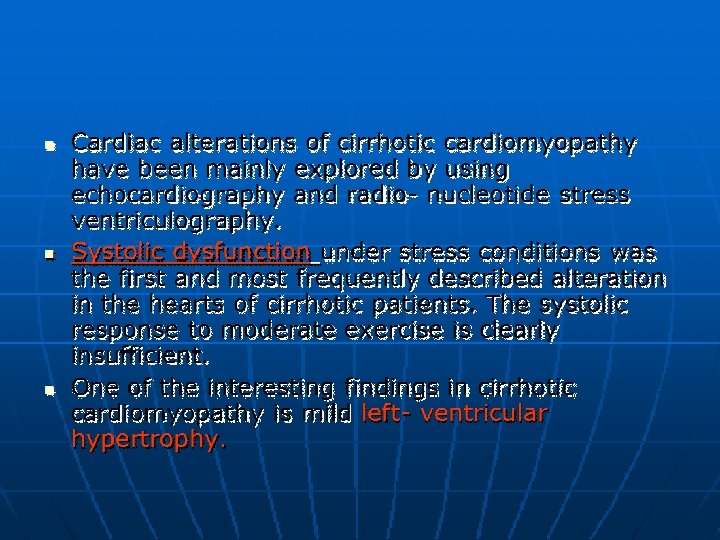
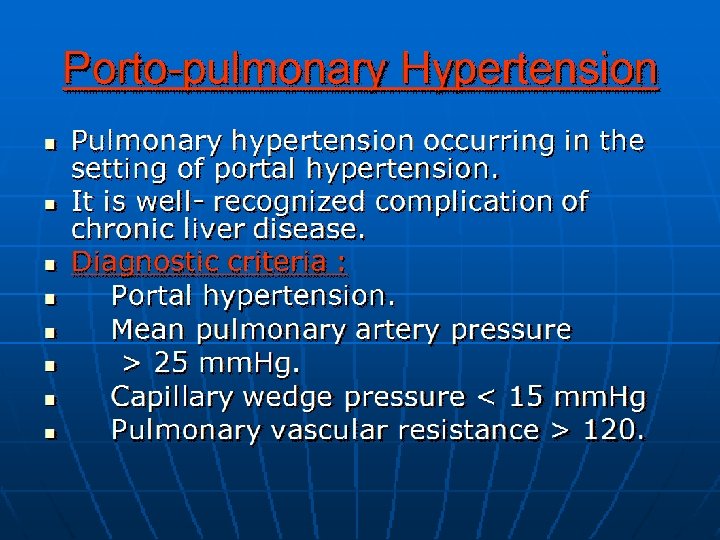
Complications of Cirrhosis: �Gastro-esophageal variceal bleeding or bleeding from portal gastropathy. �Hepatic ( porto-systemic) encephalopathy. �Ascites, spontaneous bacterial peritonitis, and the hepatorenal syndrome. �Hepatocellular carcinoma. �Cardiopulmonary complications.
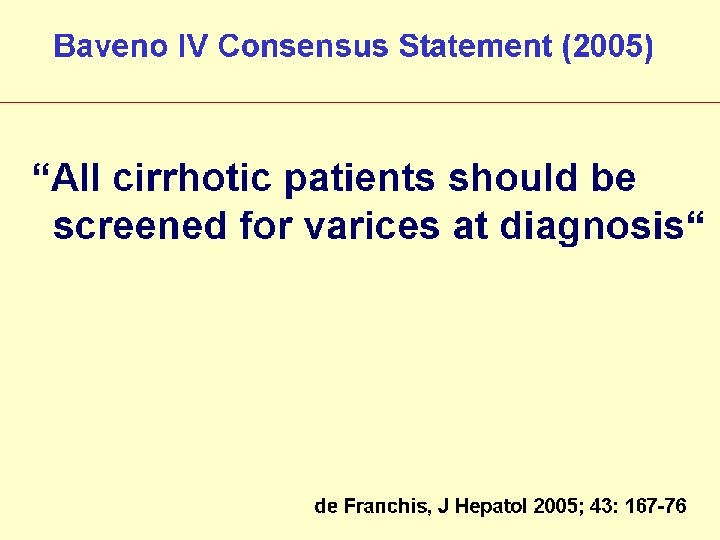

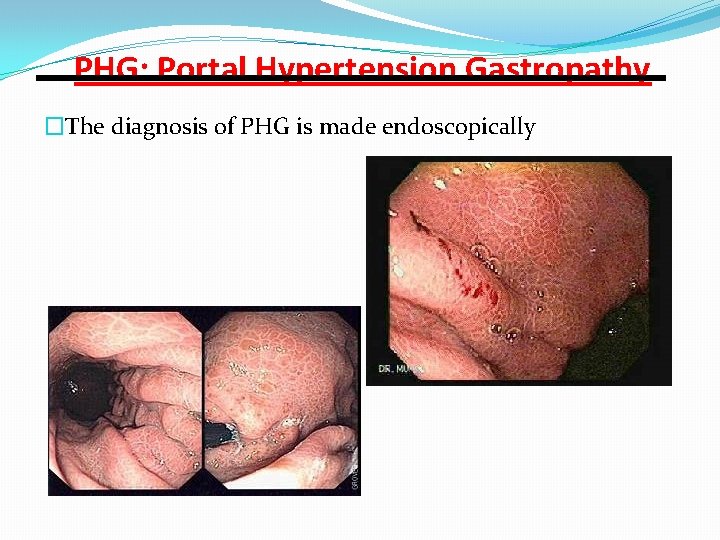
PHG: Portal Hypertension Gastropathy �The diagnosis of PHG is made endoscopically


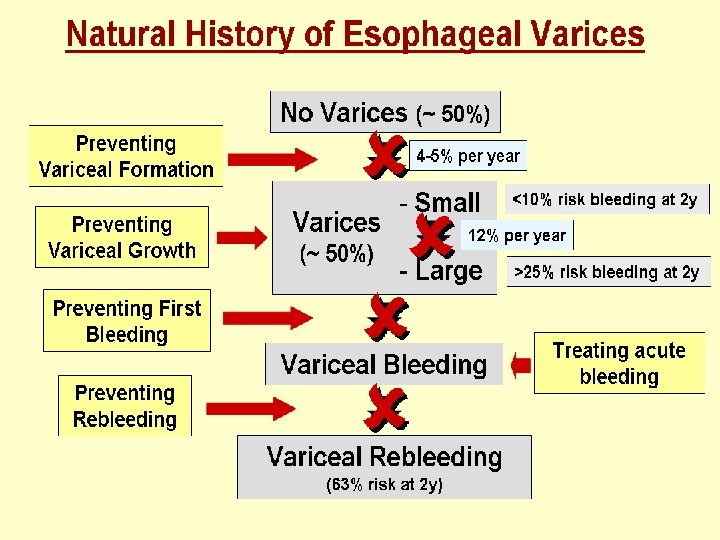


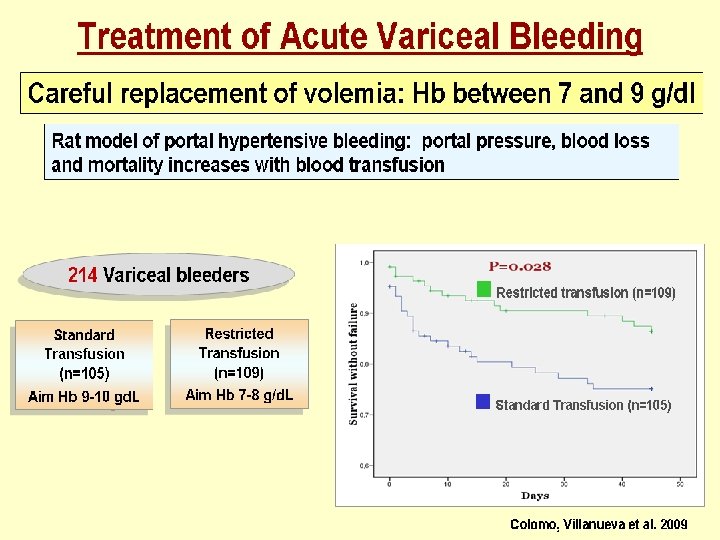
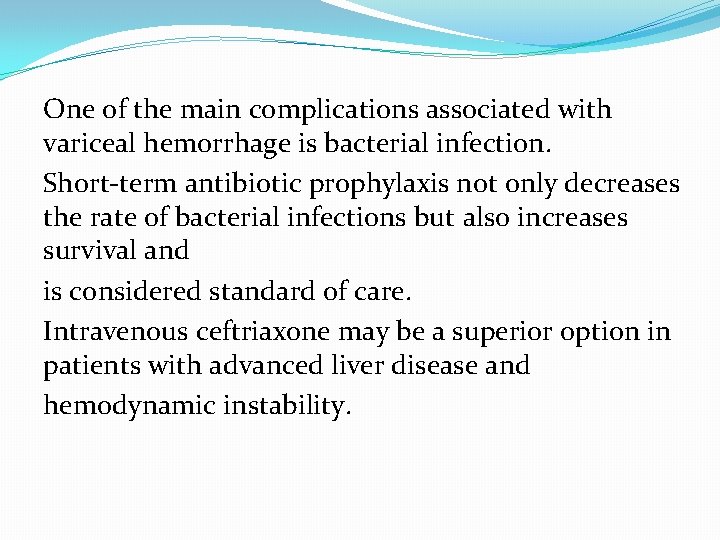
One of the main complications associated with variceal hemorrhage is bacterial infection. Short-term antibiotic prophylaxis not only decreases the rate of bacterial infections but also increases survival and is considered standard of care. Intravenous ceftriaxone may be a superior option in patients with advanced liver disease and hemodynamic instability.
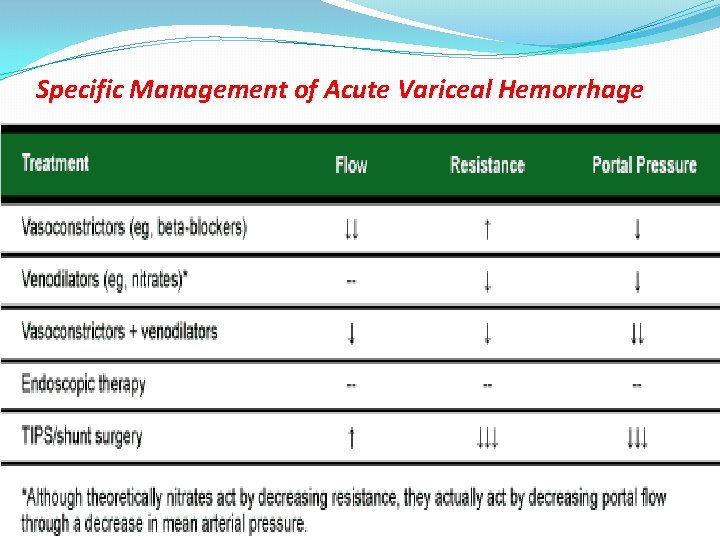
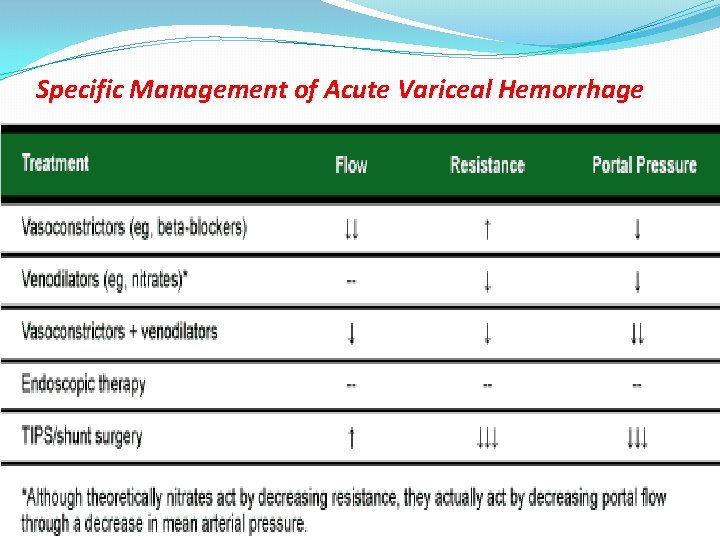
Specific Management of Acute Variceal Hemorrhage

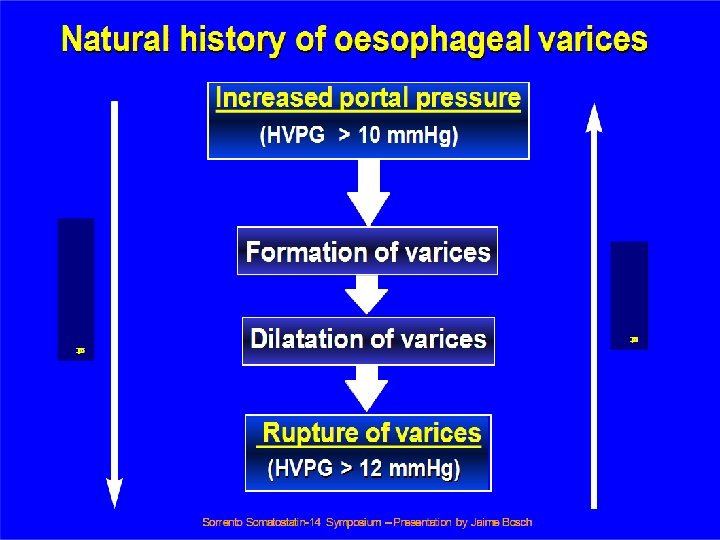
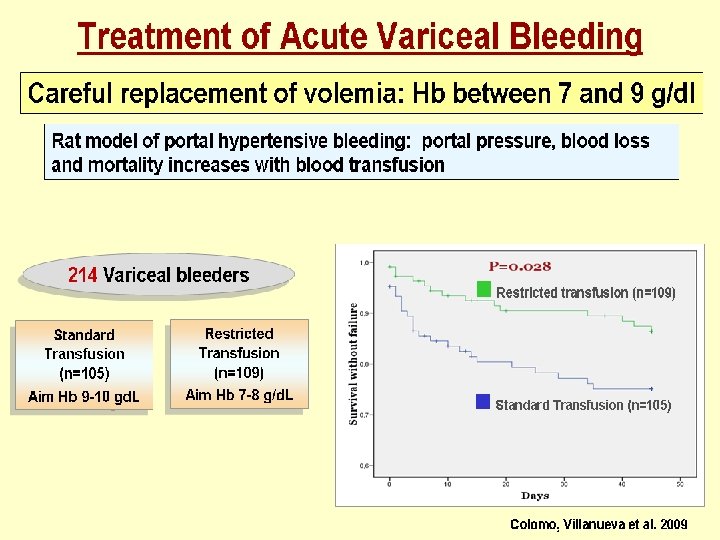
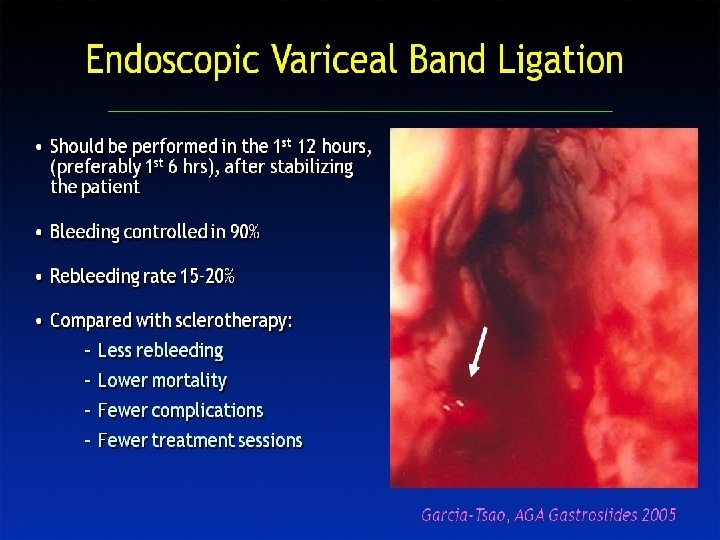
Safe vasoconstrictors available for the treatment of acute variceal hemorrhage (somatostatin, terlipressin, octreotide ). The favorable safety profile of this agent allows initiation of treatment before diagnostic endoscopy —that is, at the time the diagnosis is suspected in the treatment before diagnostic endoscopy—that is, at the time the diagnosis is suspected in the emergency department. Treatment can be continued for the next 2 -5 days when the risk of rebleeding is highest.
In acute variceal hemorrhage, pharmacologic therapy—specifically splanchnic vasoconstrictors—in combination with endoscopic therapy have been found to be more effective controlling bleeding than either treatment alone. However, the addition of pharmacologic therapy to endoscopy did not appear to significantly reduce mortality.
In acute variceal hemorrhage, pharmacologic therapy—specifically splanchnic vasoconstrictors—in combination with endoscopic therapy have been found to be more effective controlling bleeding than either treatment alone. However, the addition of pharmacologic therapy to endoscopy did not appear to significantly reduce mortality.
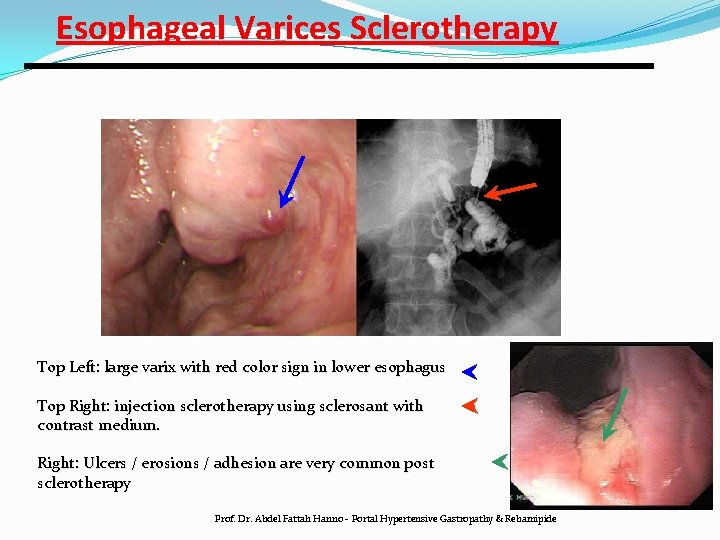
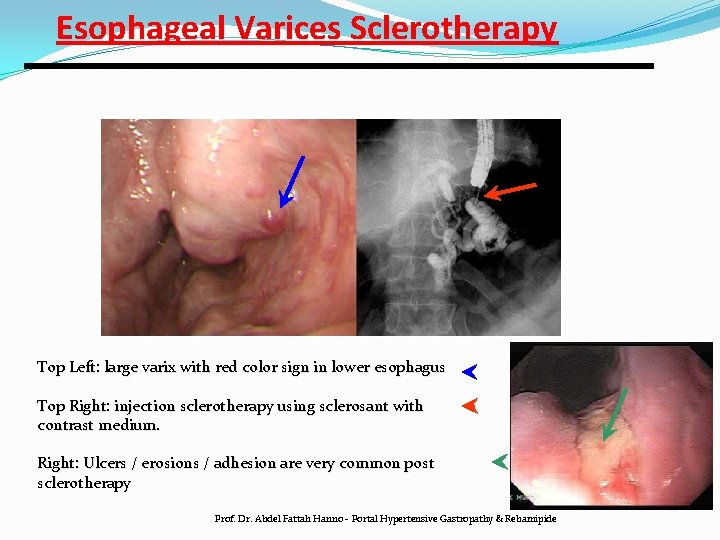
Esophageal Varices Sclerotherapy Top Left: large varix with red color sign in lower esophagus Top Right: injection sclerotherapy using sclerosant with contrast medium. Right: Ulcers / erosions / adhesion are very common post sclerotherapy Prof. Dr. Abdel Fattah Hanno - Portal Hypertensive Gastropathy & Rebamipide
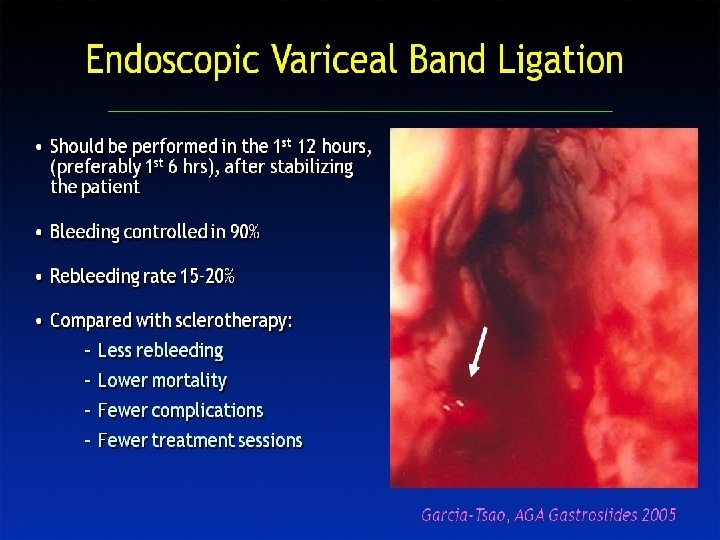

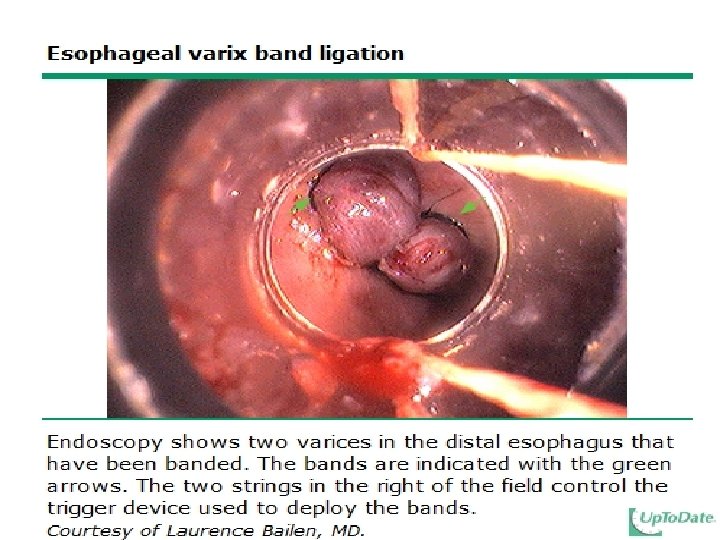
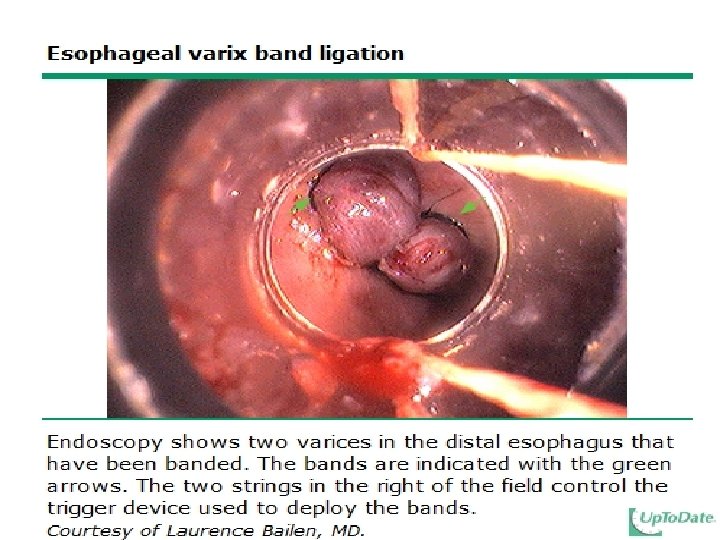
Esophageal Varices Band Ligation Gastroscopy image of esophageal varices with prominent red wale spots Esophageal varices seven days post banding, showing ulceration at the site of banding. Prof. Dr. Abdel Fattah Hanno - Portal Hypertensive Gastropathy & Rebamipide

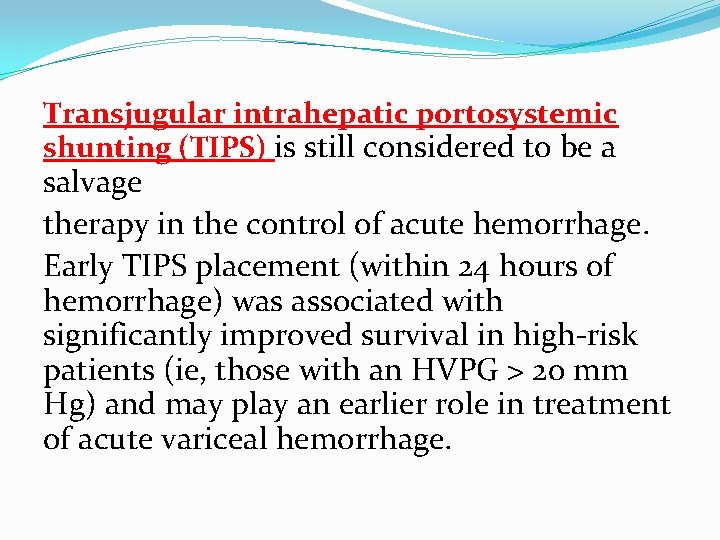
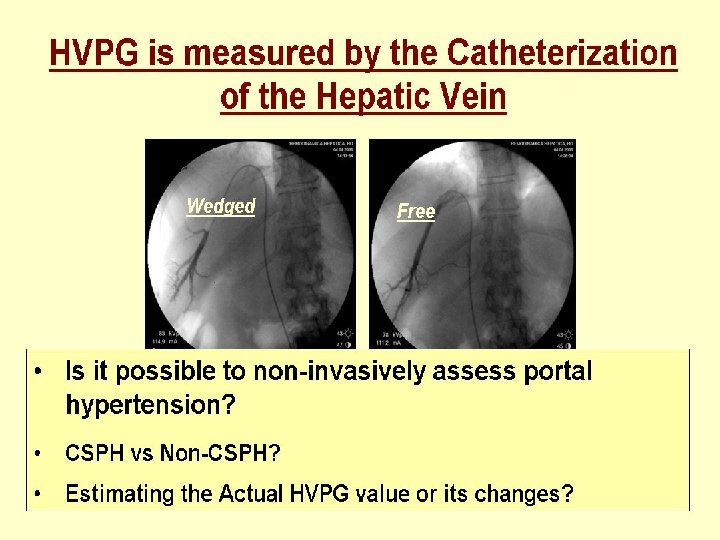
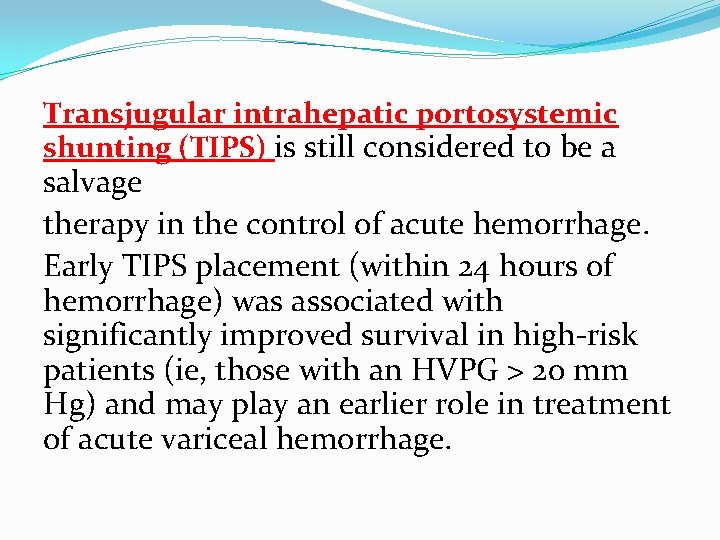
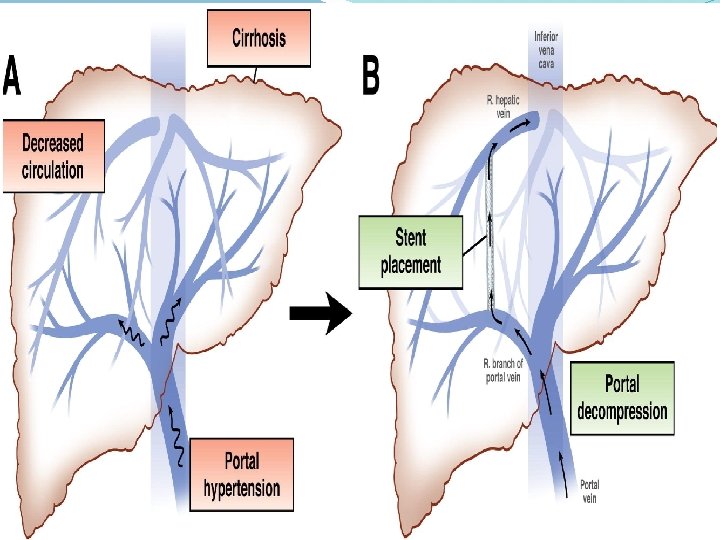
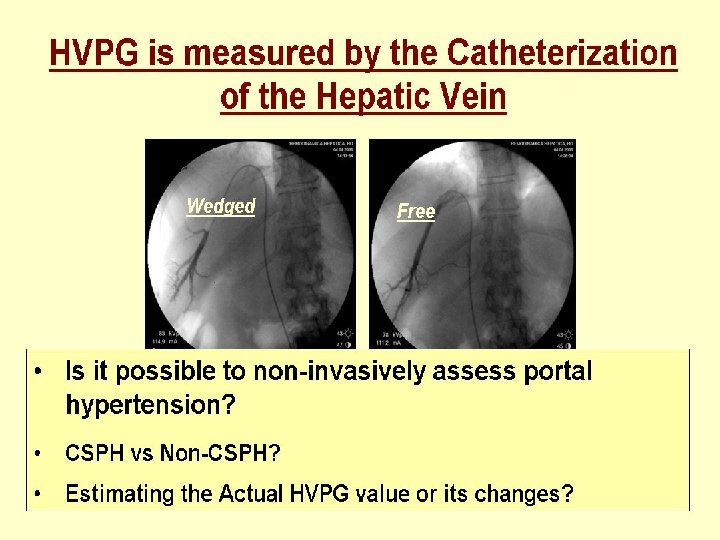
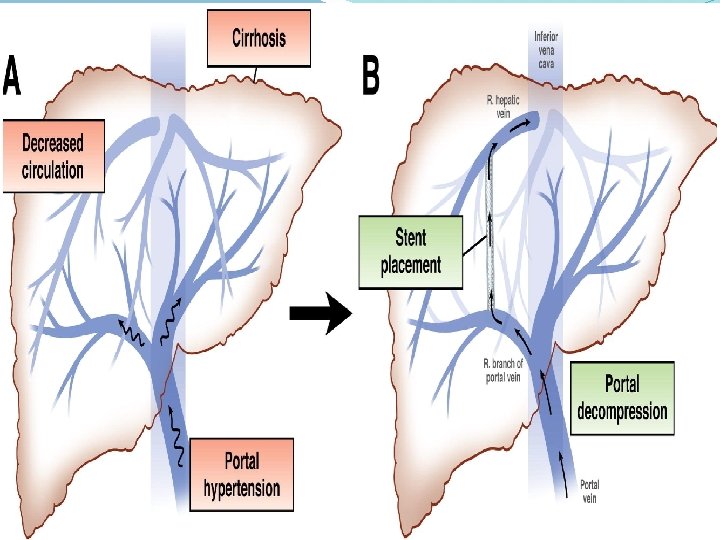
Transjugular intrahepatic portosystemic shunting (TIPS) is still considered to be a salvage therapy in the control of acute hemorrhage. Early TIPS placement (within 24 hours of hemorrhage) was associated with significantly improved survival in high-risk patients (ie, those with an HVPG > 20 mm Hg) and may play an earlier role in treatment of acute variceal hemorrhage.
(DOI: 10. 1016/j. cgh. 2011. 06. 013 ) Copyright © 2011 AGA Institute


















Treatment of cirrhosis The major goals of treating patients with cirrhosis include: Slowing or reversing the progression of liver disease • Preventing superimposed insults to the liver • Preventing and treating the complications • Determining the appropriateness and optimal timing for liver transplantation

 Nursing management of liver cirrhosis
Nursing management of liver cirrhosis Complication of liver cirrhosis
Complication of liver cirrhosis Why does liver disease cause splenomegaly
Why does liver disease cause splenomegaly Complication of liver cirrhosis
Complication of liver cirrhosis S.terre hepatic
S.terre hepatic Primary biliary cholangitis skin
Primary biliary cholangitis skin Hepatocirrosis
Hepatocirrosis Councilman bodies
Councilman bodies Pes statement for liver cirrhosis
Pes statement for liver cirrhosis Pes statement for liver cirrhosis
Pes statement for liver cirrhosis Pathophysiology of cirrhosis of liver
Pathophysiology of cirrhosis of liver Hepatology
Hepatology Hepatobiliary system
Hepatobiliary system Addenbrookes hepatology
Addenbrookes hepatology Diet for hepatitis c
Diet for hepatitis c Stage 1 cirrhosis
Stage 1 cirrhosis What is cirrhosis
What is cirrhosis Micronodular cirrhosis vs macronodular
Micronodular cirrhosis vs macronodular Hyperestrinism cirrhosis
Hyperestrinism cirrhosis Gastrointestinalis
Gastrointestinalis Cirrhosis care near woodland
Cirrhosis care near woodland Nor ursodeoxycholic acid
Nor ursodeoxycholic acid Can ct scan miss cirrhosis
Can ct scan miss cirrhosis Cirrhosis
Cirrhosis Sindrome hepatorrenal
Sindrome hepatorrenal Easl guidelines 2018
Easl guidelines 2018 Riham mohamed aly
Riham mohamed aly Mohamed dahoui
Mohamed dahoui Lodacain
Lodacain Mohamed kossentini
Mohamed kossentini Mohamed homayed death
Mohamed homayed death Mohamed computer technology
Mohamed computer technology Mohamed el merouani
Mohamed el merouani Hopital mohamed seghir nekkache
Hopital mohamed seghir nekkache Dr mohamed bashar shala
Dr mohamed bashar shala Yahye mohamed omar
Yahye mohamed omar Dr nasser mohamed
Dr nasser mohamed Dr mohamed eldeib
Dr mohamed eldeib Mohamed
Mohamed Bouhicha mohamed
Bouhicha mohamed Abdelrahman mohamed
Abdelrahman mohamed Dr mohamed bashar shala
Dr mohamed bashar shala Dr alboushi
Dr alboushi Mohamed salah
Mohamed salah Zofinopril
Zofinopril Mohamed akel
Mohamed akel Mohamed akel
Mohamed akel Zahran nyu
Zahran nyu Mohamed taamouti
Mohamed taamouti Mohamed zahran nyu
Mohamed zahran nyu Mohamed merchant
Mohamed merchant Mohamed akel
Mohamed akel Hassan fareed physics
Hassan fareed physics Mohamed younis umbc
Mohamed younis umbc Mr mohamed chafik el idrissi
Mr mohamed chafik el idrissi Mohamed hmiden
Mohamed hmiden Prophet pbuh family tree
Prophet pbuh family tree I szulejmán oszmán szultán gyermekek
I szulejmán oszmán szultán gyermekek Mohamed samir design
Mohamed samir design Dr mohamed nasr
Dr mohamed nasr Mohamed al-fayed
Mohamed al-fayed Mohamed samir design
Mohamed samir design Soumia ecrit en arabe
Soumia ecrit en arabe The clitoris
The clitoris Mohamed fayad sjsu
Mohamed fayad sjsu Abukar mohamed
Abukar mohamed Mohamed younis umbc
Mohamed younis umbc Mohamed younis umbc
Mohamed younis umbc Mohamed younis umbc
Mohamed younis umbc Mohamed younis umbc
Mohamed younis umbc Unit 6 review questions
Unit 6 review questions Decompensated liver disease
Decompensated liver disease Heterogeneous hypoechoic lesion in liver
Heterogeneous hypoechoic lesion in liver Location of pancreas
Location of pancreas Microscopic anatomy of liver
Microscopic anatomy of liver Enzyme that conjugates bilirubin
Enzyme that conjugates bilirubin What prospect does gatsby offer nick
What prospect does gatsby offer nick Normal size of liver
Normal size of liver Microscopic anatomy of liver
Microscopic anatomy of liver Shifting dullness
Shifting dullness Bile canaliculi
Bile canaliculi Drinkers liver
Drinkers liver Percussion sounds of abdomen
Percussion sounds of abdomen Blood supply of liver
Blood supply of liver Liver injury grading
Liver injury grading Liver injury grading
Liver injury grading