Hepatobiliary Disorders Dr Mohamed Hesham Sayed Professor of
Hepatobiliary Disorders Dr. Mohamed Hesham Sayed Professor of Pediatrics Rabigh Faculty of Medicine, KAU
Objectives Define and classify causes of cholestasis. Describe the consequence of cholestasis Correlate the abnormalities in LFT with cholestasis. Recognize feature of biliary atresia. Discuss viral hepatitis Recognize feature and causes of chronic liver disease. • Describe end stage of liver disease • • •

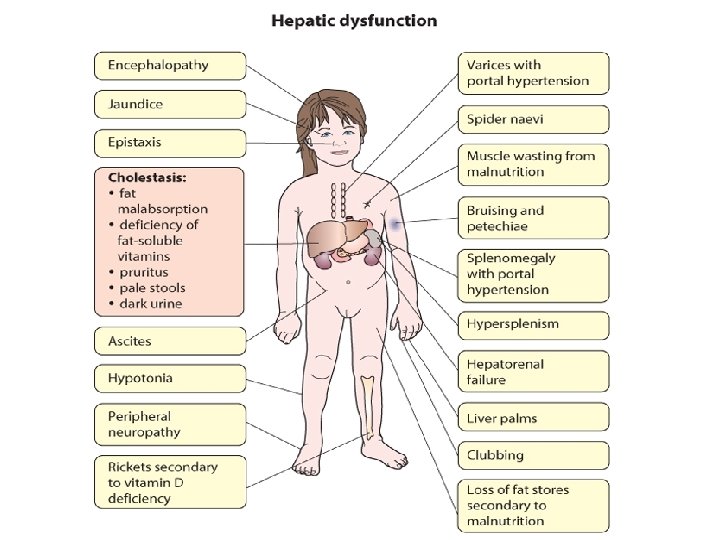
Clinical presentations of liver diseases 1) Hepatomegaly • Infections: viral hepatitis, abscess, Bilharziasis • Congestive: CHF, veno-occlusive disease • Metabolic : Glycogen storage, Wilson disease • Malignant : liver tumors, neuroblastoma 2) Jaundice • Hemolytic anemias • Acute and chronic liver diseases 3) Portal hypertension • Collateral circulation(abd veins &varices) • Splenomegaly • Ascites

4) Acute liver cell failure • Progressive jaundice • Bleeding • Rapidly developing coma 5) Chronic liver cell failure • General: anorexia, wt loss • Jaundice • Ascites • Bleeding • Skin : palmar erythema & spider nevi • Encephalopathy

Reasons for a Delay in Referral of Infants Who Have Liver Disease • Lack of follow-up of neonatal jaundice (including failure to fractionate serum bilirubin) • Inadequate investigation of hemorrhagic disease/ coagulopathy • Misdiagnosis of cholestasis (conjugated hyperbilirubinemia) as human milk jaundice (unconjugated hyperbilirubinemia) • False security due to a fall in serum bilirubin concentrations or presence of pigmented stools

Causes of Liver Diseases • The causes of liver disease in pediatric patients vary with age: • Neonates and infants – Biliary atresia and idiopathic neonatal hepatitis • older children/adolescents – Acetaminophen intoxication and Wilson disease

Causes of Liver Disease in Pediatric Patients According to Age Neonates and Infants • Cholestatic disorders —Biliary atresia —Choledochal cyst —Paucity of intrahepatic bile ducts (eg, Alagille syndrome) —Progressive familial intrahepatic cholestasis syndromes (Byler disease and syndrome) • Idiopathic neonatal hepatitis and mimickers —Cystic fibrosis —Alpha 1 -antitrypsin deficiency

• Viral hepatitis or other infectious diseases —Cytomegalovirus —Herpes simplex virus/herpes zoster virus/human herpesvirus 6 • Metabolic disease – Tyrosinemia, galactosemia, fructosemia • Others – Total parenteral nutrition

Causes of Liver Disease in Pediatric Patients According to Age Older • Hepatitis Children and Adolescents —Viral hepatitis (hepatitis B virus, hepatitis C virus) —Autoimmune hepatitis • • Wilson disease Liver disease associated with inflammatory bowel disease Parasitic infections Toxins and pharmacologic remedies Malignancies Portal hypertension Fatty liver of obesity (nonalcoholic steatohepatitis) Hypotension/ischemia/cardiac failure

Neonatal Cholestasis

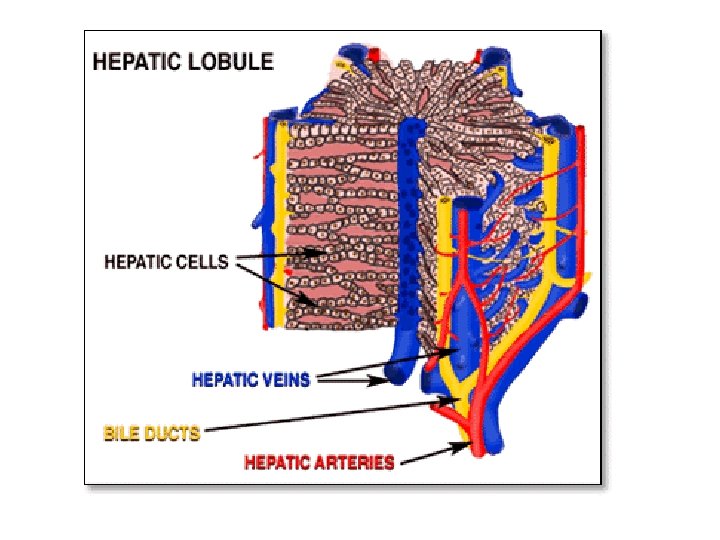
Definition • Failure of bile to reach duodenum due to Liver or biliary disorder Prolonged elevation of serum conjugated bilirubin beyond the first 14 days of life
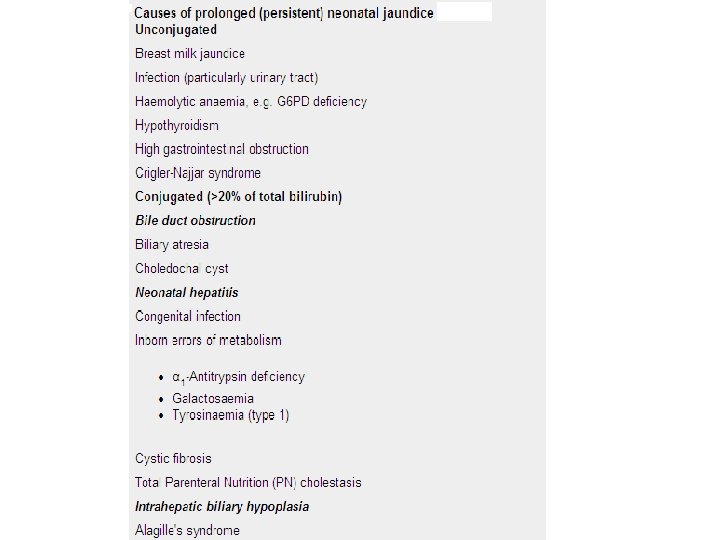

Causes of cholestasis 1) Idiopathic neonatal hepatitis The commonest cause due to unknown etiology 2) Infections : Bacterial, viral or protozoal 3) Metabolic - Carbohydrate (galactosemia), - Amino acids (tyrosinemia), - Others (alpha-1 -antitrypsin deficiency) 4) Bile duct obstruction: Extrahepatic biliary atresia (EHBA), Choledochal cyst 5) Familial syndromes as paucity of intrahepatic bile ducts (Allagile syndrome)

Allagile syndrome

Consequences of cholestasis 1) Decreased bile excretion - Fat malabsorption - Pale or clay colored stool 2) Retention of bile - Jaundice - Pruritis - Progressive liver damage

Clinical features * The diagnosis is considered in case of - Persistent neonatal jaundice > 2 wks - Hepatomegaly, - Pale stools, and - Dark urine * Signs of the cause may include - Low birth weight (TORCH), - Cataract (galactosemia or rubella), or - Abnormal facies in Allagile syndrome

1) α 1 -antitrypsin deficiency
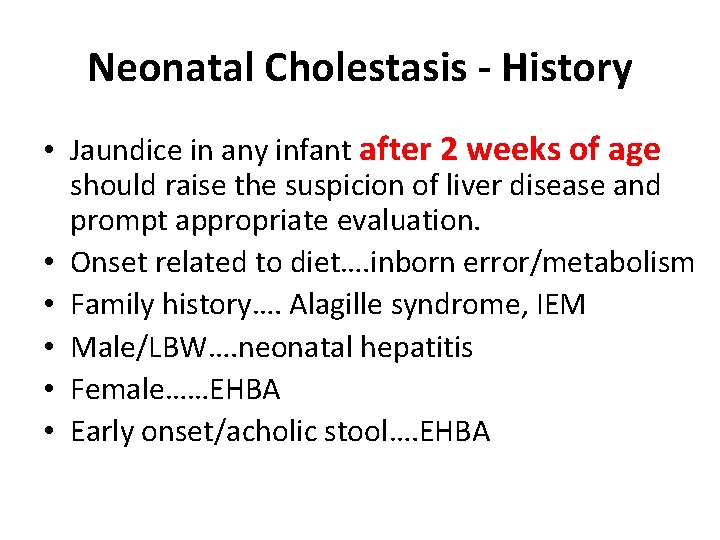
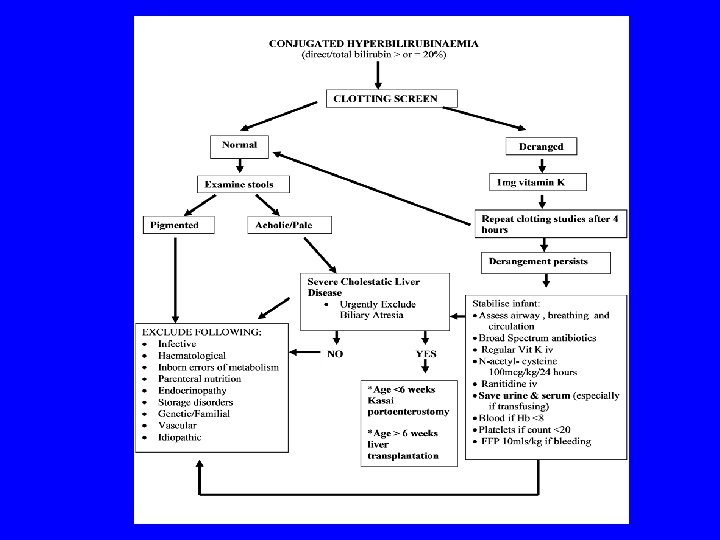
Neonatal Cholestasis - History • Jaundice in any infant after 2 weeks of age should raise the suspicion of liver disease and prompt appropriate evaluation. • Onset related to diet…. inborn error/metabolism • Family history…. Alagille syndrome, IEM • Male/LBW…. neonatal hepatitis • Female……EHBA • Early onset/acholic stool…. EHBA

Goals of timely evaluation • Diagnose and treat known medical and/or lifethreatening conditions. • Identify disorders amenable to surgical therapy within an appropriate time-frame. • Avoid surgical intervention in intrahepatic diseases.

• Surgical correction of biliary atresia ideally should occur within the first 2 months of life. • Rx- Kasai portoenterostomy – Age < 8 wks 90% clear jaundice Age 8 -12 wks 45% Age>12 wks 22%
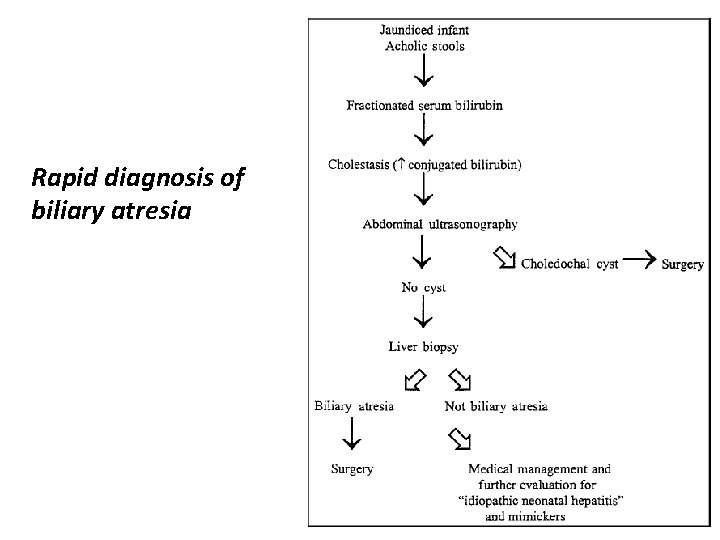
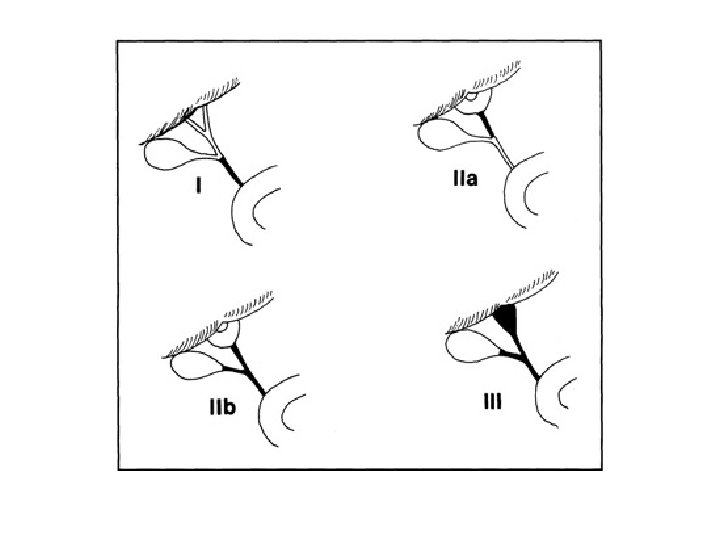
Rapid diagnosis of biliary atresia
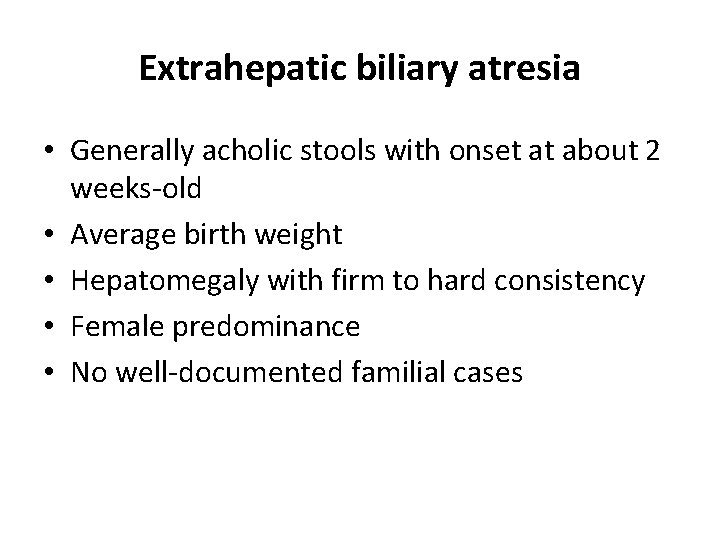
Extrahepatic biliary atresia • Generally acholic stools with onset at about 2 weeks-old • Average birth weight • Hepatomegaly with firm to hard consistency • Female predominance • No well-documented familial cases

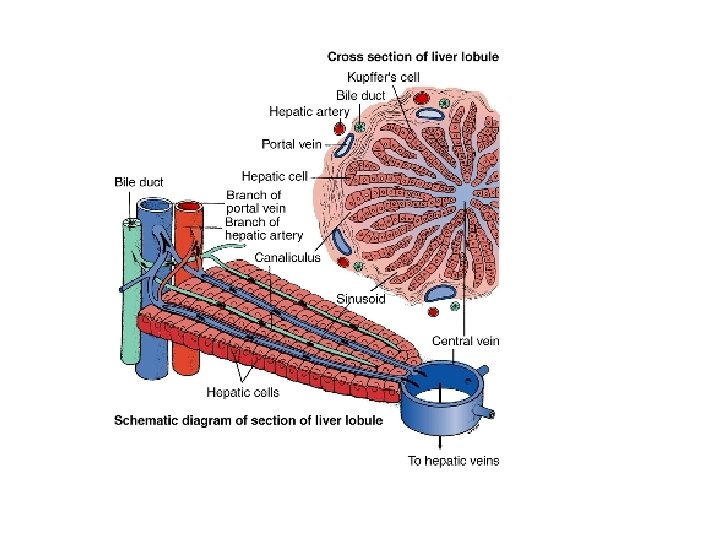
Extrahepatic biliary atresia • Increased incidence of polysplenia syndrome and intra-abdominal vascular anomalies • Normal uptake on radionucleotide scan with absent excretion • Biopsy shows bile duct proliferation, bile plugs, portal or perilobular fibrosis and edema, and intact lobular structure

Idiopathic neonatal hepatitis • Generally normal stools or acholic stools with onset at one month-old • Low birth weight • Normal liver on exam or hepatomegaly with normal to firm consistency • Male predominance • Familial cases (15 -20%)
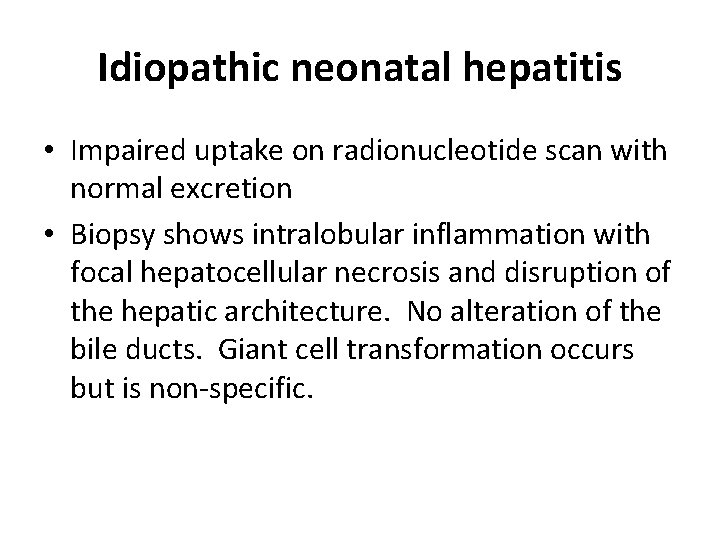
Idiopathic neonatal hepatitis • Impaired uptake on radionucleotide scan with normal excretion • Biopsy shows intralobular inflammation with focal hepatocellular necrosis and disruption of the hepatic architecture. No alteration of the bile ducts. Giant cell transformation occurs but is non-specific.

Infantile Cholestasis - Objectives • Aim 1: Identify a treatable cause • Aim 2: Recognise complications • Aim 3: Early referral to specialist unit when necessary
Etiologies • Basic distinction is between: – Extrahepatic etiologies – Intrahepatic etiologies

Extrahepatic etiologies • • Extrahepatic biliary atresia Choledochal cyst Bile duct stenosis Spontaneous perforation of the bile duct Cholelithiasis Inspissated bile/mucus plug Extrinsic compression of the bile duct

Intrahepatic etiologies • Idiopathic Neonatal Hepatitis • Toxic – TPN-associated cholestasis – Drug-induced cholestasis • • Genetic/Chromosomal Infectious Metabolic Miscellaneous

Presentation • • Jaundice- conjugated bilirubin Pale stools Dark urine Abnormal LFTs - high or low GGT Bleeding Hepatosplenomegaly Abdominal mass Failure to thrive

Investigations of cholestasis A) To document diagnosis of cholestasis - Total and direct serum bilirubin - Liver enzymes: ALT (more liver specific), AST, alkaline phosphatase and gamma glutamyl transpeptidase - Serum proteins (total and albumin) - Prothrombin time and concentration

B) To define the cause of cholestasis 1) Look for treatable conditions - Galactosemia (reducing substance in urine); - Septicemia (sepsis screen) 2) Look for congenital infections - TORCH screenig 3) Look for metabolic conditions - Tyrosinemia and alpha one antitrypsin deficiency 4) Look for choledochal cyst : by abdominal US
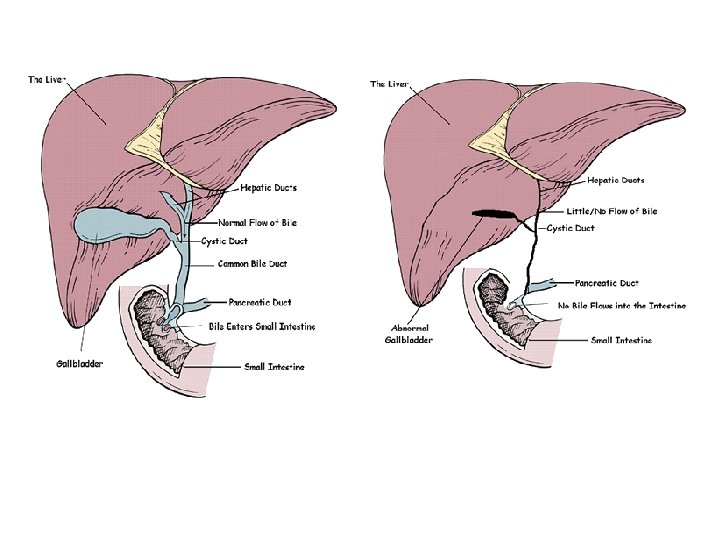
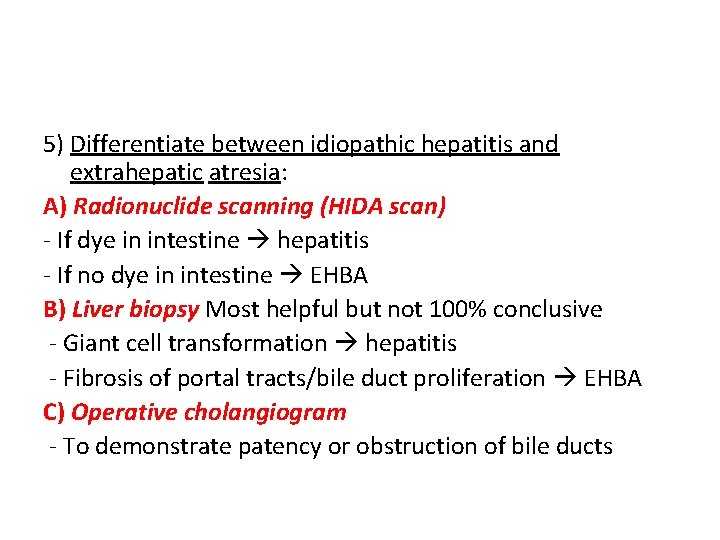
5) Differentiate between idiopathic hepatitis and extrahepatic atresia: A) Radionuclide scanning (HIDA scan) - If dye in intestine hepatitis - If no dye in intestine EHBA B) Liver biopsy Most helpful but not 100% conclusive - Giant cell transformation hepatitis - Fibrosis of portal tracts/bile duct proliferation EHBA C) Operative cholangiogram - To demonstrate patency or obstruction of bile ducts

Biliary Atresia • Radioisotope scan (TBIDA) of liver showing good hepatic uptake of isotope and no excretion into bowel.

Biliary Atresia Liver biopsy of biliary atresia showing bands of fibrous tissue with bile duct proliferation.

Neonatal Hepatitis Liver biopsy in neonatal hepatitis showing inflammatory infiltrate throughout the liver, and giant cell and rosette formation of liver cells.

Biliary cirrhosis
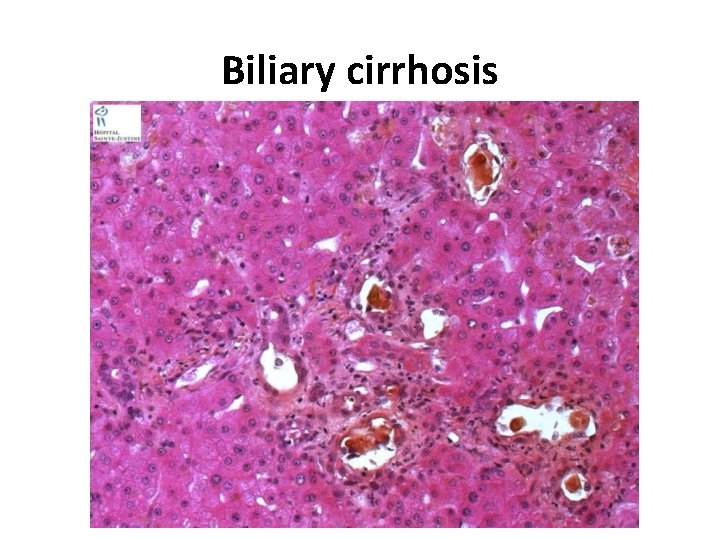
Biliary cirrhosis

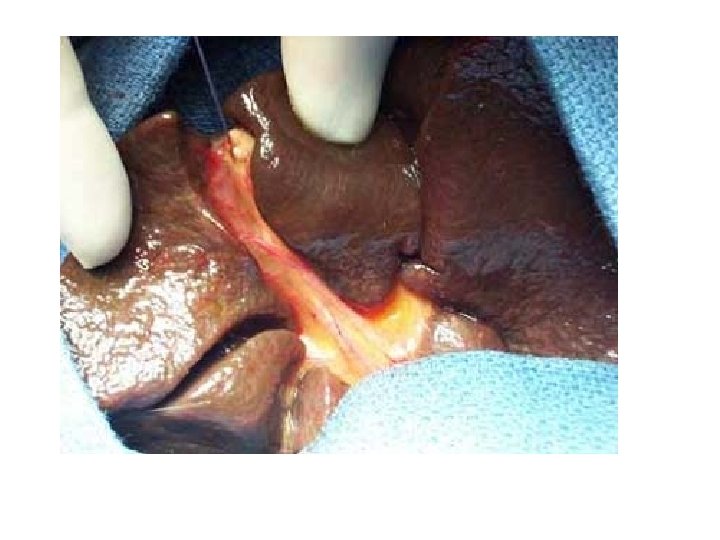
Kasai Portoenterostomy Formation of Roux-en-Y to re establish bile flow by anastomising bowel to ductal remnant

Management of cholestasis 1) Specific treatment - Sepsis antibiotics - Galactosemia Lactose free milk - Choledochal cyst surgical correction - EHBA Kasai operation (hepatic portoenterostomy) Should be done before 60 days to obtain good results as the obliterative process is progressive Delay in operation reduces the chances to find any patent biliary ductules. Procedure: a loop of jejunum is anastomosed to the transected porta hepatis.

2) Nutritional support Medium chain triglycerides and fat soluble vitamins 3) Treatment of complications - Pruritis: ursodeoxycholic acid or bile acid binders as cholestyramine - Varices: sclerotherapy - Hepatic encephalopathy: 10% glucose infusion, bowel wash by enema, oral neomycin, lactulose, …. 4) Liver transplantation - For EHBA who have failed Kasai.

Cholestasis in Older Children • HAV infection (anorexia, fever, vomiting, abdominal pain, darkening of the urine with elevated aminotransferase values in the absence of other known hepatotoxic exposures). • HCV infection (increased exposure to IV blood products (hemodialysis, hemophilia, surgery). • Hepatotoxic medications(isoniazid, nitrofurantoin, sulfonamides, and NSAID , such as acetaminophen and ibuprofen.
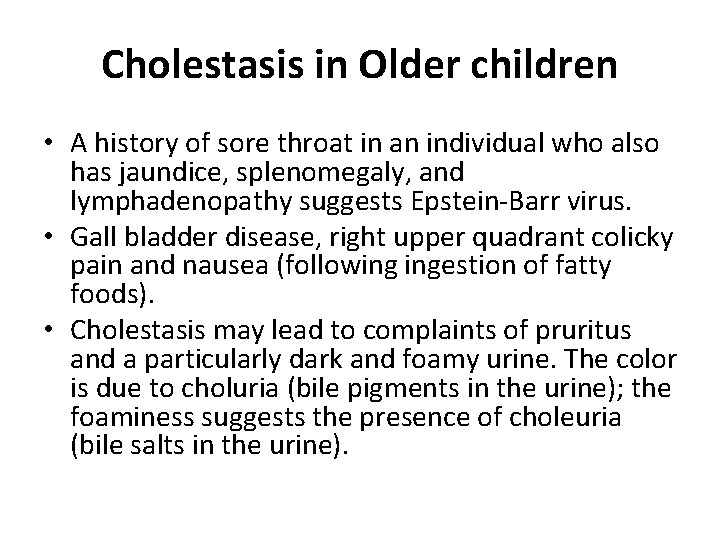
Cholestasis in Older children • A history of sore throat in an individual who also has jaundice, splenomegaly, and lymphadenopathy suggests Epstein-Barr virus. • Gall bladder disease, right upper quadrant colicky pain and nausea (following ingestion of fatty foods). • Cholestasis may lead to complaints of pruritus and a particularly dark and foamy urine. The color is due to choluria (bile pigments in the urine); the foaminess suggests the presence of choleuria (bile salts in the urine).

Viral Hepatitis HAV HBV HCV HDV Type RNA DNA RNA, RNA incomplete Transmission Oral Parenteral Oral Incubation, day 15 -40 50 -150 30 -150 20 - 90 15 -60 Carrier state No yes yes No Diagnosis Anti-HAV HBs. Ag, Anti-HCV, Anti-HDV Ig. M Anti-HBc. Ig. M HCV-RNA Anti-HEV Vaccine Yes No No Treatment Not needed Interferonalpha/ Lamivudine Interferon- Interferonalpha/ alpha Ribavirin Yes HEV No

Diagnosis of viral hepatitis

1) Clinical forms of acute hepatitis (4 forms) a) Icteric hepatitis: the most common Pre - icteric phase : - Mild fever , anorexia , vomiting and abdominal pain - Urine is dark ( bilirubinuria ) Icteric phase : - Jaundice appears - Liver is tender and enlarged - Anorexia is common Convalescent phase : - Gradual decline of symptoms and signs. - This is the rule in hepatitis A.
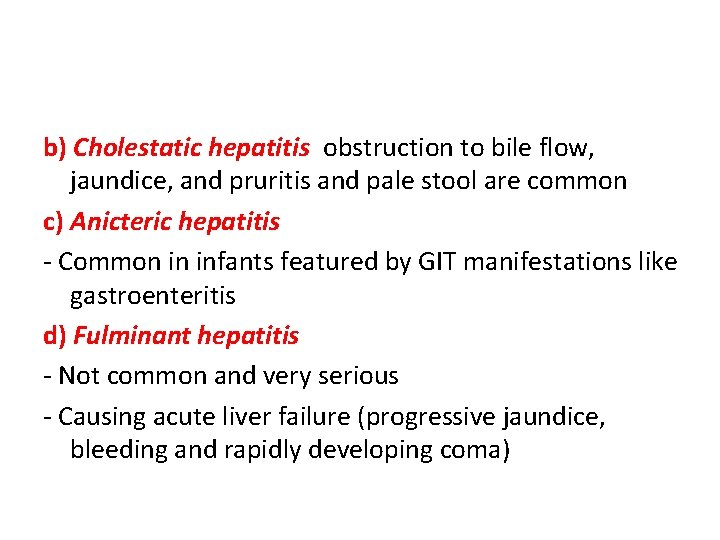
b) Cholestatic hepatitis obstruction to bile flow, jaundice, and pruritis and pale stool are common c) Anicteric hepatitis - Common in infants featured by GIT manifestations like gastroenteritis d) Fulminant hepatitis - Not common and very serious - Causing acute liver failure (progressive jaundice, bleeding and rapidly developing coma)

2) Investigation to confirm acute liver injury - Marked increase of serum bilirubin (direct or mixed) - Marked elevations of transaminases (ALT and AST) to very high levels. - Bilirubin in urine - Evidence of acute hepatic failure 1) Rising serum bilirubin 2) Low serum albumin 3) Prolonged prothrombin time 4) High blood ammonia, and electrolyte imbalance

3) Identification of the virus HAV HBV HCV HDV HEV Onset Acute Insidious More insidious With HBV As HAV Course Short prolonged More prolonged Severe As HAV Chronicity No possible Very possible No Fulminant failure Rare May occur rare With HBV In pregnant females HBs. Ag/ Laboratory Anti-HAV Ig. M (acute), anti. HBc Ig. M diagnosis Anti-HAVIg. G (recovery) (acute), Anti-HBs (recovery), HBs. Ag/ anti. HBc Ig. G (chronicity) Anti-HCV (exposure), Anti-HCV/ HCVRNA (chronic) Anti-HCV and – ve HCVRNA (recovery)
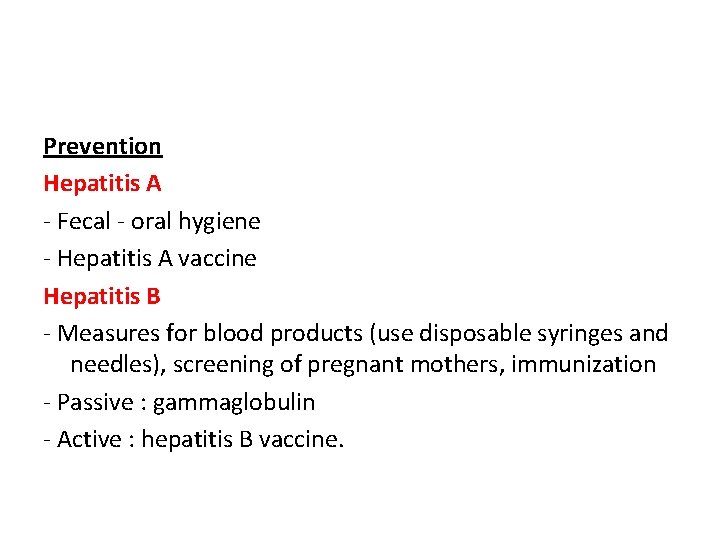
Prevention Hepatitis A - Fecal - oral hygiene - Hepatitis A vaccine Hepatitis B - Measures for blood products (use disposable syringes and needles), screening of pregnant mothers, immunization - Passive : gammaglobulin - Active : hepatitis B vaccine.
Complications : in types B, C, D: (1) Fulminant hepatitis & hepatic failure (2) Chronic hepatitis ( persistent - active ) (3) Cirrhosis (4) Hepatocellular carcinoma (5) Aplastic anemia
Acute liver failure (fulminant hepatitis) § Massive hepatic necrosis with subsequent loss of liver § § function, Uncommon, but has a high mortality. The child may present within hours or weeks with jaundice, encephalopathy, coagulopathy, hypoglycaemia and electrolyte disturbance. Early signs of encephalopathy include alternate periods of irritability and confusion with drowsiness. Older children may be aggressive and unusually difficult. Complications include cerebral oedema, haemorrhage from gastritis or coagulopathy, sepsis and pancreatitis.

Acute liver failure (fulminant hepatitis) Causes 1. Infection…HAV, HBV, HCV, non-A to G 2. Drugs/Poisons…Paracetamol, isoniazide, … 3. Metabolic…Wilsons disease, tyrosinemia… 4. Autoimmune hepatitis 5. Reye’s syndrome

Acute liver failure (fulminant hepatitis) • Management – Maintaining the blood glucose (>4 mmol/L) by IV – – – dextrose. preventing sepsis with broad-spectrum antibiotics preventing haemorrhage IV vitamin K, FFP and H 2 -blockers treating cerebral oedema by fluid restriction and mannitol diuresis.
Acute liver failure (fulminant hepatitis) • Poor prognosis is likely – – when the liver begins to shrink in size, if there is a rising bilirubin with falling transaminases, an increasing coagulopathy or progression to coma. • Without liver transplantation, 70% of children who progress to coma will die.
Reye's syndrome and Reye-like syndrome § Acute non-inflammatory encephalopathy with microvesicular fatty infiltration of the liver. § Aetiology is unknown, there is a close association with aspirin therapy. § Stop give aspirin to children as an antipyretic to avoid it § Reye-like syndrome • Beta oxidation defect, medium chain acyl-Co. A • dehydrogenase deficiency (MCAD). Many of these patients would have presented with acute liver failure and a Reye-like syndrome later in life.
Chronic hepatitis
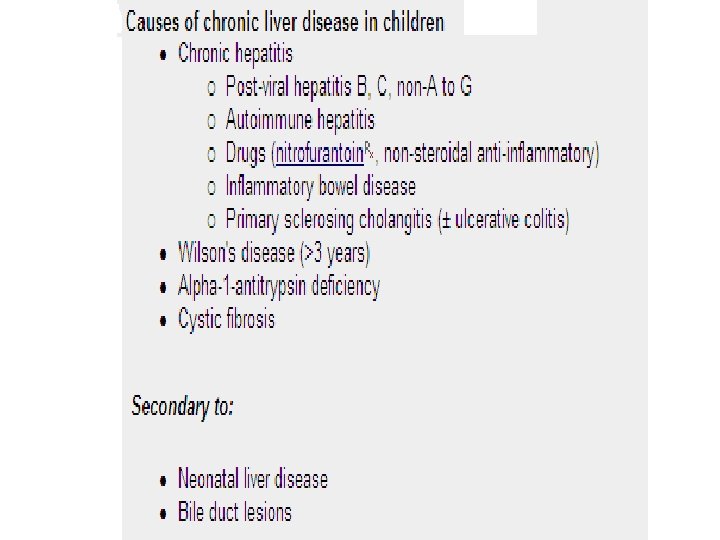
Causes 1) Chronic infection: HBV, HDV, and HCV (not with HAV or HEV) 2) Autoimmune hepatitis 3) Drug-induced: Rifampicin, isoniazid, nitrofurantoin 4) Inborn errors of metabolism As Wilson disease and alpha-one anti-trypsin deficiency

Autoimmune Hepatitis • The mean age is 7 -10 years. More common in girls. • May present as – an acute hepatitis, – as fulminant hepatic failure or – chronic liver disease with autoimmune features such as skin • • rash, lupus erythematosus, arthritis, haemolytic anaemia or nephritis. Diagnosis is based on – hypergammaglobulinaemia (Ig. G >20 g/L); – positive autoantibodies, e. g. smooth muscle antibodies (SMAs), antinuclear antibodies (ANAs) or liver/kidney microsomal antibodies. – a low serum complement (C 4); and typical histology. Most children respond to prednisolone and azathioprine.

Wilson’s Disease Kayser-Fleischer rings from copper in the cornea in a child with Wilson's disease.

Clinical presentations 1) Unresolved hepatitis Acute hepatitis unresolving in 6 months 2) Slowly progressive liver disease Manifestations of chronic liver cell failure

Investigations 1. Liver functions tests: usually abnormal 2. Abdominal ultrasound: to define size of liver and spleen and check for ascites 3. Liver biopsy: is very helpful for diagnosis, it shows chronic inflammatory cell infiltrate 4. Investigations for the cause such as serological markers for hepatitis B and C; autoantibodies for autoimmune hepatitis and low seruloplasmin and high copper in Wilson disease.

Complications 1. Liver cirrhosis and hepatic carcinoma 2. Portal hypertension causing varices and ascites 3. Chronic liver cell failure

Treatment 1) Treatment of cause if possible • Interferon for chronic HBV and HCV • Prednisolone and azathioprine for autoimmune hepatitis • D- penicillamine for Wilson disease 2) Liver transplantation Good option for end stage liver disease with good results

Liver Cirrhosis • Definition : Irreversible condition with widespread liver fibrosis & nodule formation. There is disturbed vascular arrangement leading to portal hypertension • Causes : 1 - Post-hepatitis cirrhosis 2 - Biliary cirrhosis eg. biliary atresia 3 - Metabolic e. g. Wilson's disease. 4 - Cardiovascular: Constrictive pericarditis- Budd chiari synd. • Diffuse fibrosis occur in : - Schistosomiasis - Cong. hepatic fibrosis
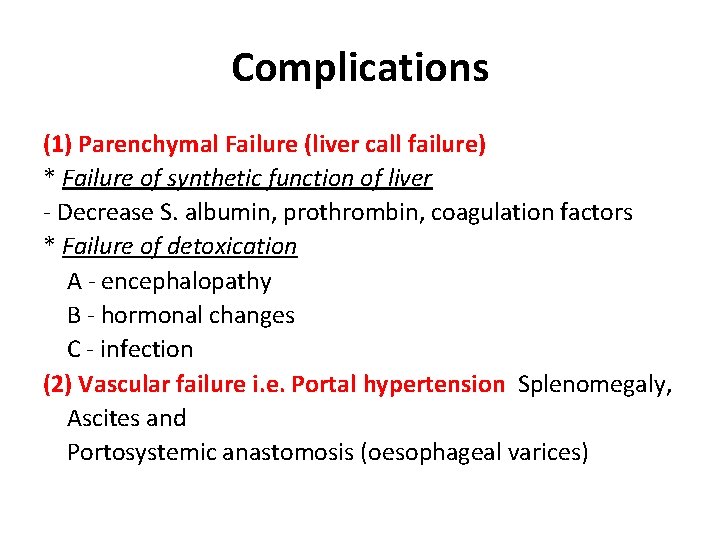
Complications (1) Parenchymal Failure (liver call failure) * Failure of synthetic function of liver - Decrease S. albumin, prothrombin, coagulation factors * Failure of detoxication A - encephalopathy B - hormonal changes C - infection (2) Vascular failure i. e. Portal hypertension Splenomegaly, Ascites and Portosystemic anastomosis (oesophageal varices)
Portal hypertension • Definition: When the portal venous pressure exceeds 12 mm. Hg (normal variation 5 – 10 mm. Hg) • Causes of portal hypertension: 1) Pre hepatic = portal vein obstruction/thrombosis due to - umbilical sepsis or - umbilical vein catheterization * Clinically: 1 - Portal hypertension 2 - Marked splenic enlargement with NORMAL liver

2) Intra hepatic portal hypertension : Hepatic - Chronic hepatitis - Cirrhosis - Bilharzial fibrosis - Wilson disease - Congenital hepatic fibrosis - Veno-occlusive disease Biliary - Extrahepatic biliary atresia - Sclerosing cholangitis * Clinically : - History of hepatic/biliary disease - Portal hypertension - Liver size is variable, usually shrunken with sharp edge.

3) Post hepatic portal hypertension : (postsinusoidal) - Budd-Chiari ( hepatic vein obstruction) - Constrictive pericarditis. * Clinically : - Portal hypertension - Marked liver enlargement - Spleen may be normal or enlarged in late cases

Clinical features 1) Esophageal varices: due to opening of collateral circulation. Also, dilated abdominal veins (caput medusa). Varices lead to hematemesis which may be mild or massive. 2) Splenomegaly: More evident with prehepatic and hepatic causes 3) Ascites: Due to - Hypoproteinemia, - Na retention, - Renal impairment and fluid redistribution. It can be complicated by bacterial peritonitis.
4) Hepatic encephalopathy: induced by GIT hemorrhage, sepsis, electrolyte imbalance and high protein intake. The mechanisms of CNS manifestations include hyperammonemia, false neurotransmitters, high aromatic amino acid levels and GABA accumulation 5) Renal failure: hepatorenal syndrome.

Cirrhosis and Portal Hypertension Cirrhosis and portal hypertension. (i) malnutrition with loss of fat and muscle bulk (ii) distended abdomen from ascites and hepatosplenomegaly (iii) scrotal swelling from ascites (iv) no jaundice despite advanced liver disease.
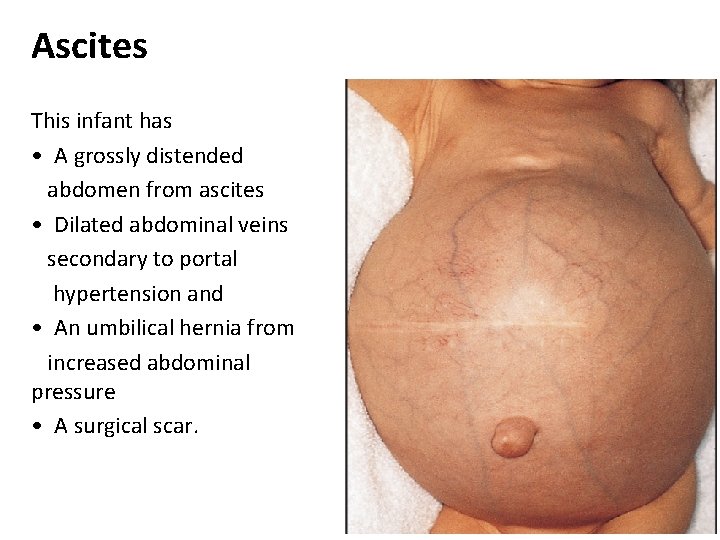
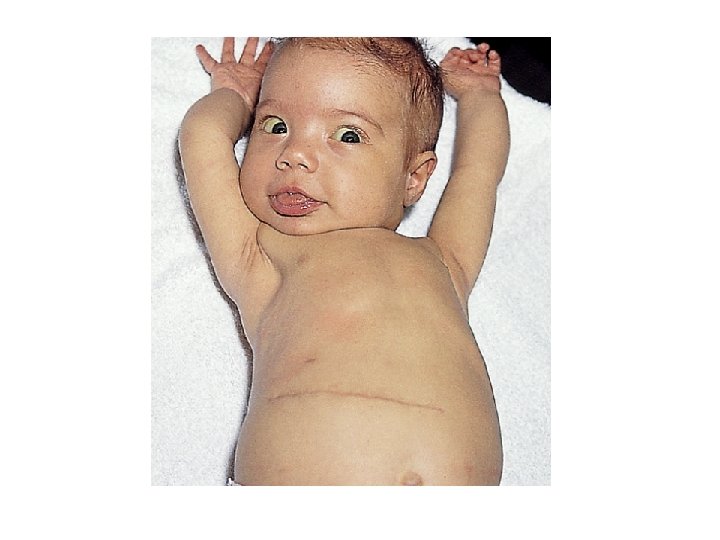
Ascites This infant has • A grossly distended abdomen from ascites • Dilated abdominal veins secondary to portal hypertension and • An umbilical hernia from increased abdominal pressure • A surgical scar.

Cirrhosis and Portal Hypertension
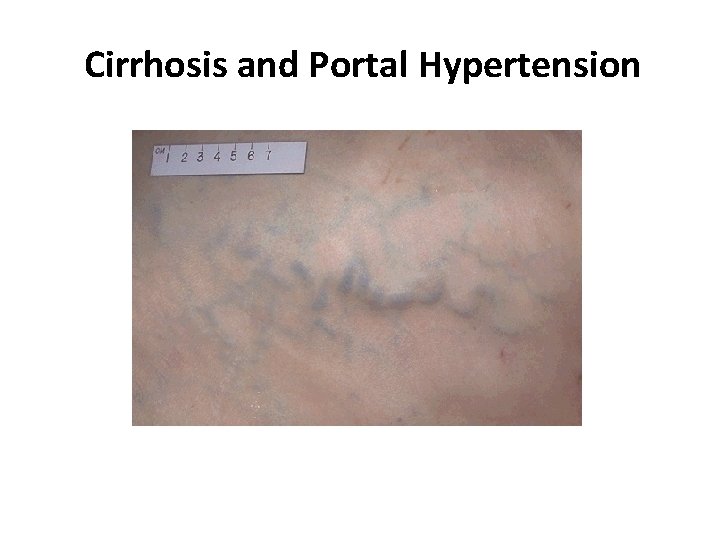
Cirrhosis and Portal Hypertension
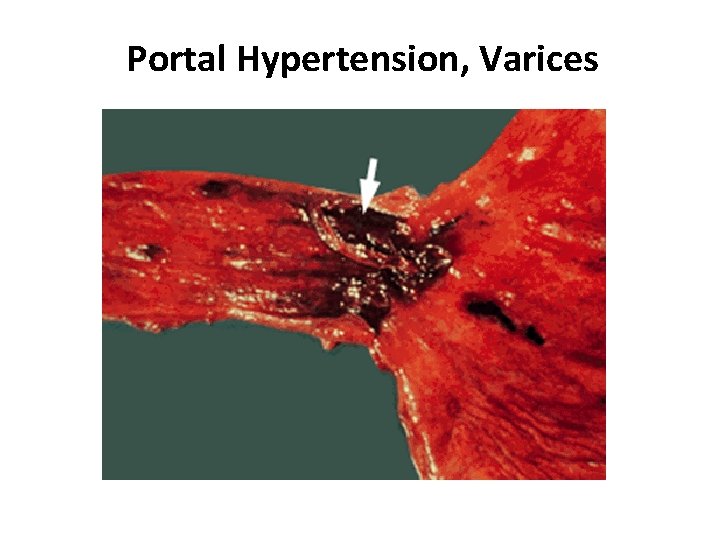
Portal Hypertension, Varices

Portal Hypertension, Varices

Portal Hypertension, Varices

Investigations 1) Upper endoscopy: to detect varices 2) Abdominal ultrasound: may show shrunken liver and splenomegaly 3) Splenoportography to locate site of obstruction 4) Liver function tests 5) Screening for causes of chronic liver disorders
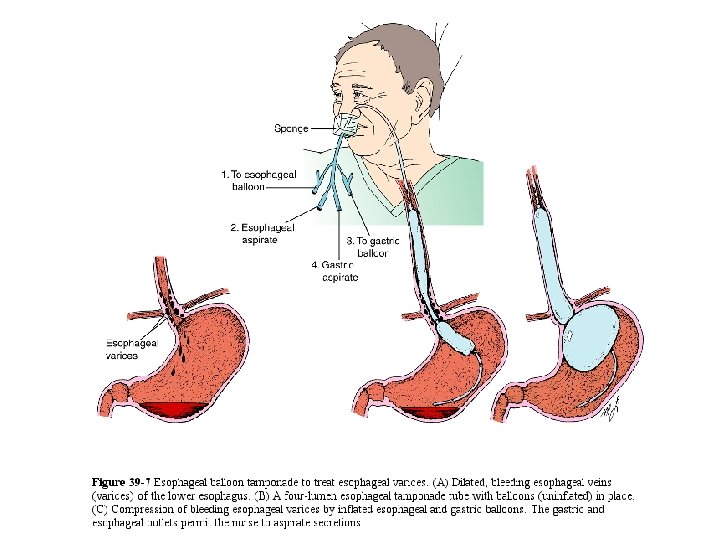
Management • Aim: to prevent or treat bleeding varices A) Emergency treatment of bleeding varices 1. Hospitalization 2. IV fluid resuscitation and blood transfusion 3. H 2 blockers as ranitidine 4. If bleeding persists: vasopressin infusion

B) Endoscopic management by - Sclerotherapy or - Band ligation of the varices C) Surgical treatment by portosystemic shunt (bypass) - Transjugular intrahepatic porto-systemic shunt (TIPSS) - Surgical portosystemic shunts as porticaval shunts
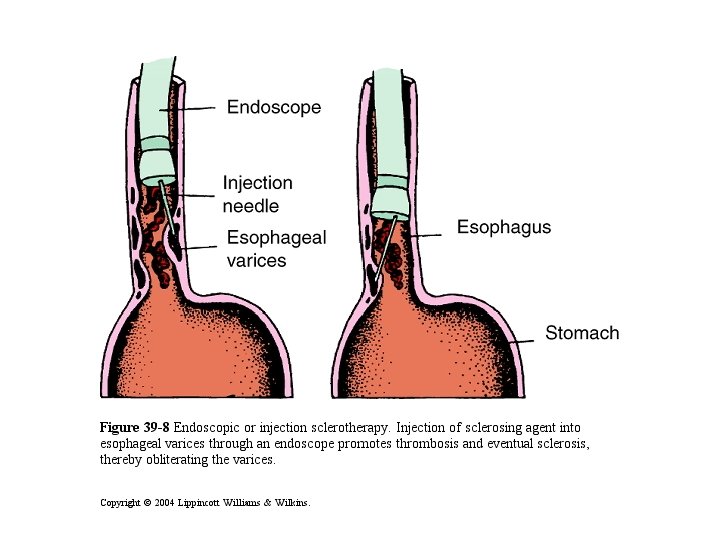
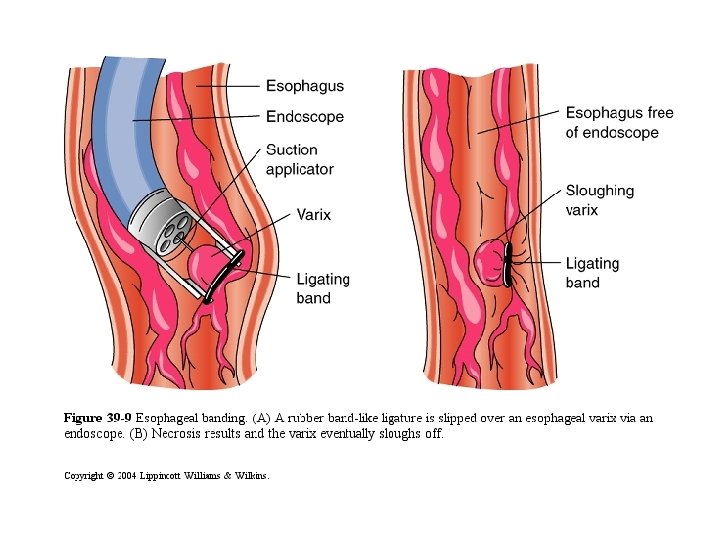
D) Prevention of bleeding - Prevention of first bleeding attack: • Avoid aspirin • Beta blockers as propranolol(reduces portal venous pressure) • prophylactic sclerotherapy or band ligation - Prevention of rebleeding: beta blockers, sclerotherapy, band ligation, surgical portosystemic shunts and liver transplantation

Liver transplantation • Indications include acute or chronic end stage liver failure. • Contraindications include sepsis, untreatable cardiopulmonary disease or cerebrovascular disease. • Most children receive part of an adult’s liver of a living person.
• Complications after transplantation are not uncommon such as hepatic artery thrombosis, biliary leaks, rejection, VOD and sepsis • Outcome: Children who survive the initial postoperative period usually do well. • Short and long term results are much promising for this kind of therapy for previously hopeless cases.
Clinical and laboratory evaluation of liver disease

Physical Examination • The liver span is the distance between the liver edge and the upper margin of dullness obtained by percussion at the right midclavicular line. • The mean span changes from 4. 5 to 5 cm at 1 week of age to 6 to 7 cm in early adolescence.

• If the spleen is enlarged: – Portal hypertension or storage disease • Tender hepatomegaly: – Viral hepatitis or heart failure • Massive hepatomegaly – Congenital hepatic fibrosis • Ascites: – Portal hypertension or liver failure • Massive hepatosplenomegaly: – Storage disorder or malignancy
• Intense pruritus in obstructive liver disease, that primarily is manifested by irritability. • Alagille syndrome – Characteristic facies (beaked nose, high forehead), butterfly vertebrae, a murmur on auscultation due to peripheral pulmonic stenosis, and a posterior embryotoxon on ophthalmologic examination.

Laboratory Evaluation Cholestatic or obstructive Liver cell injury • Elevation of mainly alkaline phosphatase aminotransferases (ALT (AP), gamma glutamyl and AST) transpeptidase (GGT), and conjugated bilirubin.

Liver function tests • The term is NOT accurate… Why? ? • Only two of the parameters commonly obtained are true measures of hepatic function – the prothrombin time (PT) and – serum albumin level, both assess synthetic ability. • All of the other parameters are essentially indirect measures of liver function, and some of these values are altered in settings other than liver disease

Liver function tests • Cholestasis is defined by conjugated hyperbilirubinemia more than 20 % of total serum bilirubin. • Dark urine due to bilirubinuria • The levels of alanine aminotransferase (ALT) and aspartate aminotransferase (AST) are the most sensitive tests of hepatocyte necrosis. • ALT is more specific of liver disease because it is found only in low concentrations in other tissues.
Liver function tests • An elevated serum AP level usually indicates obstructive liver disease especially if the rise in AP is associated with a rise in GGT… Why? ? • A low serum albumin concentration is a late finding in liver disease. When it is present, it suggests chronic disease. • Hyperammonemia and encephalopathy are classic findings of liver failure, and there is a labile correlation between the degree of encephalopathy and serum ammonia levels.
Liver function tests • The PT (prothrombin time) which measures the time required for prothrombin (factor II) to be converted into thrombin, will be elevated in the presence of biliary obstruction. • This is the basis for parenteral administration (not oral) of vitamin K to patients who have elevated PT values.
Liver function tests • No matter what the cause, an elevated PT value in patients who have liver disease is serious. One of the first steps when evaluating a newborn who has cholestasis is to measure PT/PTT and administer vitamin K. • Untreated hypoprothrombinemia may lead to spontaneous bleeding and intracranial hemorrhage.

Imaging and Histopathology of the Liver and Biliary Tract • Abdominal ultrasonography – Liver size and texture – Choledochal cysts and stones (95% accuracy) – Space occupying lesions & dilated bile ducts. – Absence of gallbladder in case of biliary atresia. • Radionuclide imaging (technetium-99) – Detects liver uptake and excretory abilities. – The appearance of the tracer within the intestinal region by 24 hours virtually excludes biliary atresia, but the converse is not true.

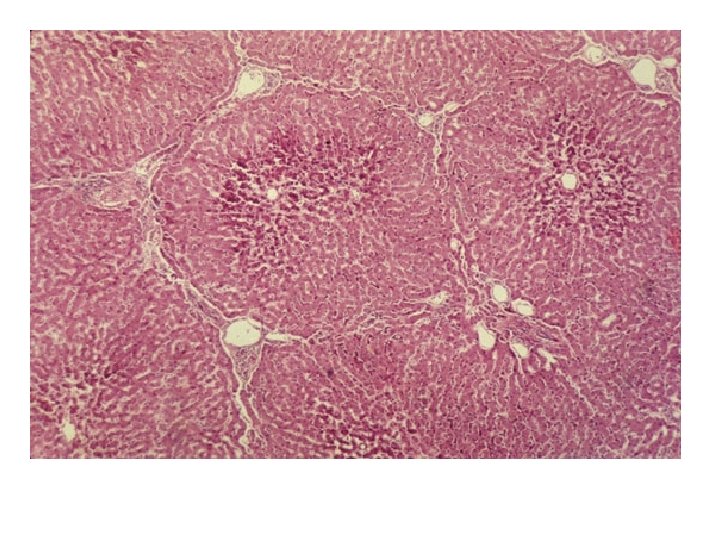
Percutaneous liver biopsy • The cardinal method by which to arrive quickly at a diagnosis of underlying liver disease. • Shows the degree of fibrosis/cirrhosis and permits the diagnosis of biliary atresia, neonatal hepatitis, congenital hepatic fibrosis, and alpha 1 -antitrypsin deficiency. • In neonatal hepatitis there is giant cell transformation with inflammatory infiltrates of the portal zones and an absence of bile ductule proliferation.

Percutaneous liver biopsy • In EHBA there is proliferation of the interlobular bile ducts, periportal fibrosis, and bile plugs in canaliculi and ductules.

Older children • Wilson disease needs to be included in the differential diagnosis of any child who presents with liver disease, neurologic abnormalities, behavioral changes, or Kayser. Fleischer rings.

Management

Liver transplantation • Survival rates approach 80% at 1 year and 70% at 5 years. • Biliary atresia is the most common indication for transplant and may be the initial treatment when detected late or may be used as a salvage procedure for a failed Kasai. • Used early in cases of tyrosinemia

Medical management of liver diseases • Nutritional support • Treatment of pruritus, choleretics and bile acidbinders • Management of portal hypertension and its consequences
Treatment • Nutritional support – Adequate calories and protein – Supplement calories with medium chain triglycerides – Treatment and/or prophylaxis for fat-soluble vitamin deficiencies (vitamins A, D, E, and K)

Treatment • Nutritional support (cont. ) – Supplemental calcium and phosphate when bone disease is present – Prophylaxis for zinc deficiency – Low-copper diet as poorly excreted – Sodium restriction when ascites present

Treatment • Treatment of pruritus – Bile acid-binders: cholestyramine – Ursodeoxycholic acid – Phenobarbital as a choleretic

Treatment • Management of portal hypertension and its consequences – Variceal bleeding • • • Fluid resuscitation Blood products Sclerotherapy Balloon tamponade Portovenous shunting Propanolol

Treatment • Management of portal hypertension and its consequences (cont. ) – Ascites • • Sodium restriction Diuretics: spironolactone, furosemide Albumin Paracentesis

Conclusion • Identifying the presence of serious liver disease in a pediatric patient at the initial presentation is of cardinal importance. • Early recognition of babies who have biliary atresia is critical for optimal medical or surgical intervention.

Case Studies

A 15 -year-old girl who is being evaluated for poor school performance and acting-out behaviors is noted to have a large, firm liver. Kayser- Fleischer rings are apparent on ophthalmologic examination. Determination of which of the following is most likely to confirm the diagnosis in this patient? . A. Hepatic copper concentration. B. Hepatic iron concentration. C. Hepatitis B antibody titers. D. Serum alpha 1 -antitrypsin level. E. Serum chloride level

A 3 -year-old girl who has cholestasis and is malnourished is suspected of having a nutrient deficiency. Which one of the following clinical findings is most likely to be present in this child? . A. Megaloblastic anemia. B. Neuritis. C. Pellagra. D. Photophobia. E. Rachitic rosary

Thank you
- Slides: 126