Approach to Headache Dr Duaa Hiasat Family Medicine




- Slides: 32
Approach to Headache Dr. Dua’a Hiasat. Family Medicine Specialist.
EPIDEMIOLOGY � Headaches � Not are quite common! all seek medical help. � 90% of all headaches fall under a few categories. � 4. 5% of emergency department visits.
TYPES OF HEADACHES PRIMARY � Migraine � Tension-type � Cluster � Other Headache
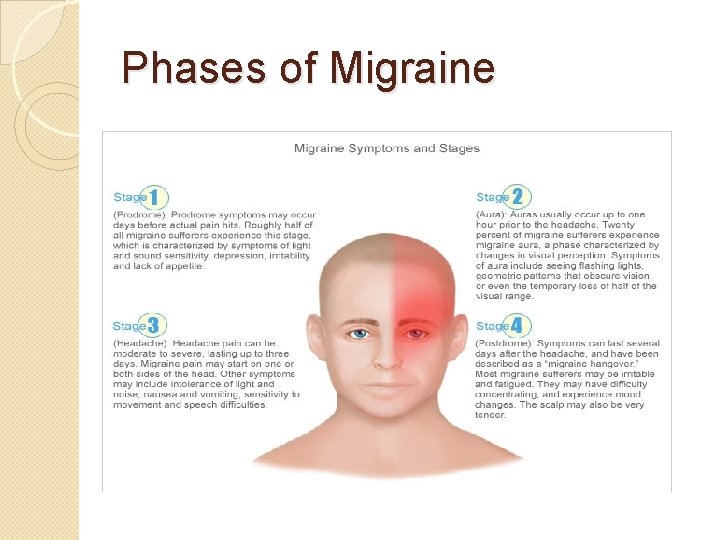
Primary Headaches - Migraine � Epidemiology - Most common headache seen in primary care. � Twice as common in women than men. � Pathophysiology - Vasoconstriction/Vasodialation, Cortical spreading Depression. � Presentation - Variable. � Diagnostic Criteria � Triggers � Four Phases of Migraine
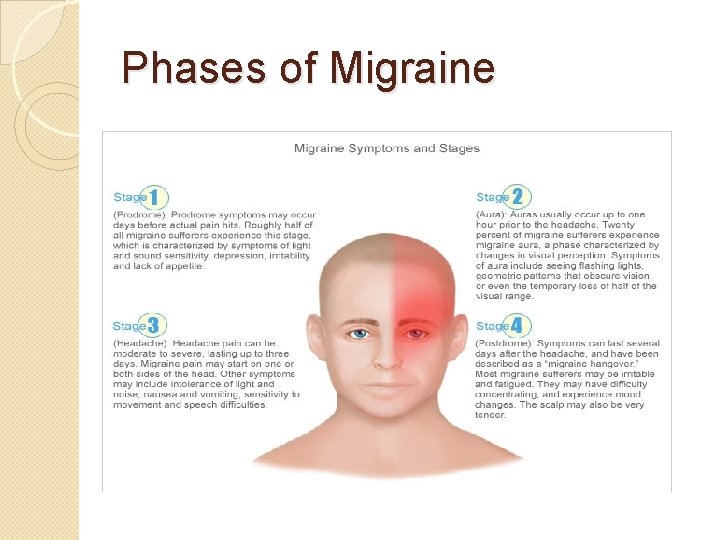
Phases of Migraine
Migraine without aura International Headache Society Diagnostic Criteria � Headache lasts 4 to 72 hours With at least two of the following: v Unilateral location v Moderate or severe. v Pulsating. v Aggravation by or causing avoidance of routine physical activity (e. g. , walking, climbing stairs) � During headache, at least one of the following: v Nausea and/or vomiting v Photophobia and phonophobia � Not attributed to another disorder � History of at least five attacks fulfilling above criteria
Migraine with aura Diagnostic criteria: �Aura consisting of at least one of the following, but no motor weakness: v Fully reversible dysphasic speech disturbance. � Sensory symptoms that are fully reversible, including positive features (pins and needles) and/or negative features (numbness) � Visual symptoms that are fully reversible, including positive features (flickering lights, spots, lines) and/or negative features (loss of vision)
Migraine with aura � At least two of the following: � Homonymous visual symptoms and/or unilateral sensory symptoms � At least one aura symptom develops gradually over five minutes or different aura symptoms occur in succession over five minutes � Each symptom lasts at least five minutes, but no longer than 60 minutes � Headache fulfilling criteria for migraine without aura begins during the aura or follows aura within 60 minutes � Not attributed to another disorder � History of at least two attacks fulfilling above criteria
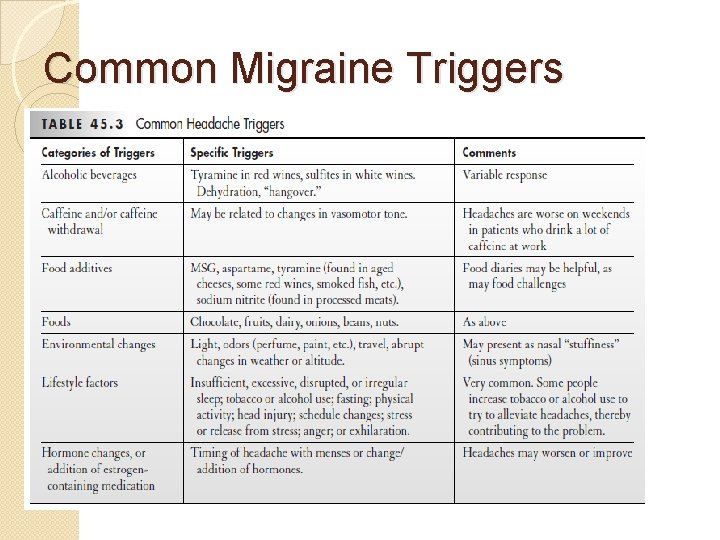
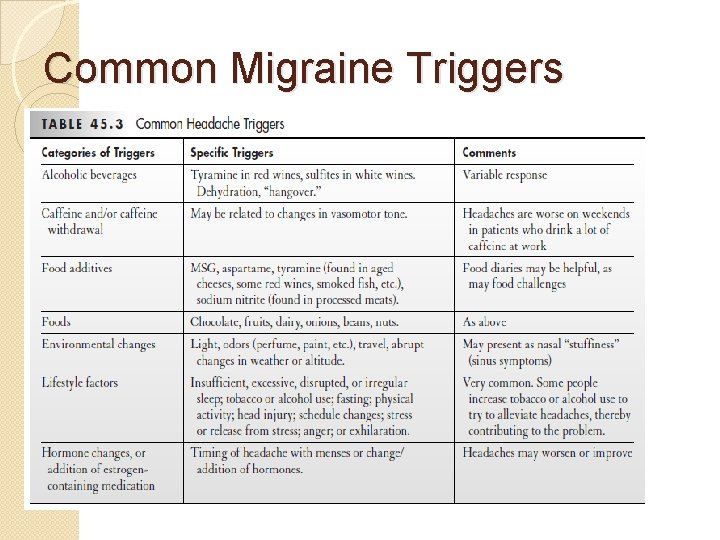
Common Migraine Triggers
Primary Headaches – Tensiontype Headache � Epidemiology - Most common cause of headache overall. � Pathophysiology - Muscle tension around head and neck, malfunctioning pain filter in brainstem. � Characteristics � Causes - Stress, sleep deprivation, bad posture, hunger, eyestrain. Aggravated by TMJ dysfunction.
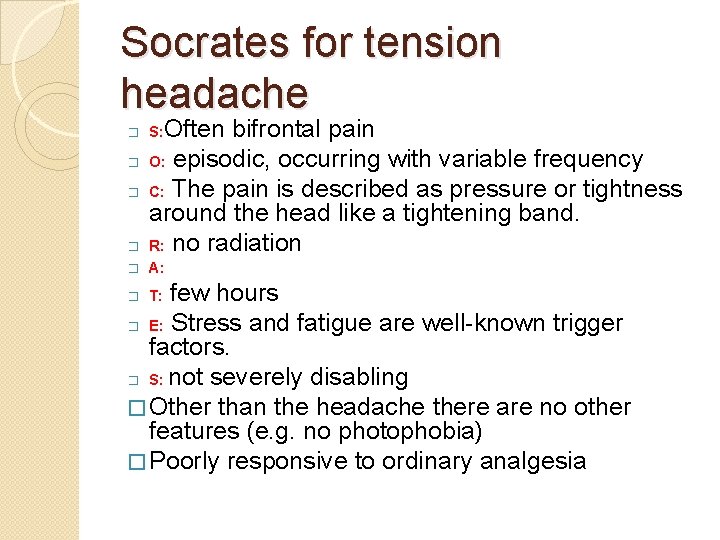
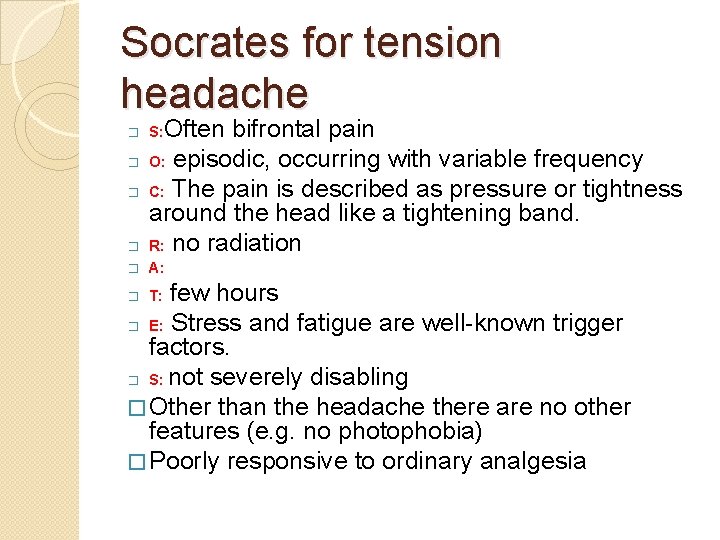
Socrates for tension headache � Often bifrontal pain O: episodic, occurring with variable frequency C: The pain is described as pressure or tightness around the head like a tightening band. R: no radiation � A: � � � S: few hours � E: Stress and fatigue are well-known trigger factors. � S: not severely disabling � Other than the headache there are no other features (e. g. no photophobia) � Poorly responsive to ordinary analgesia � T:
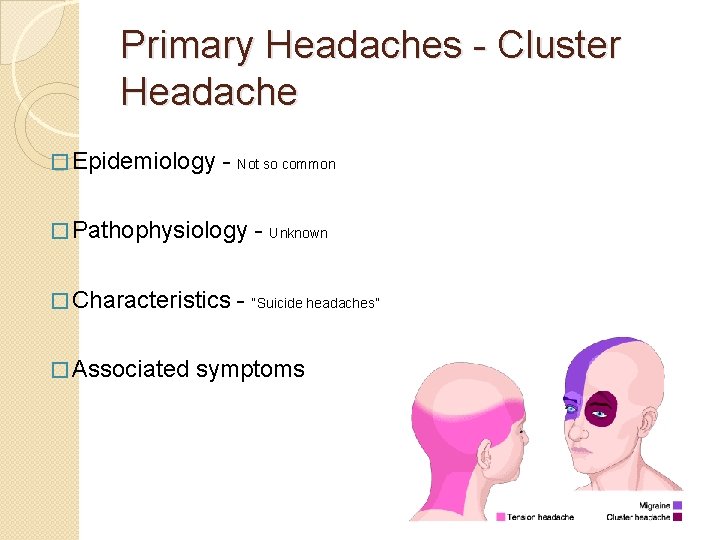
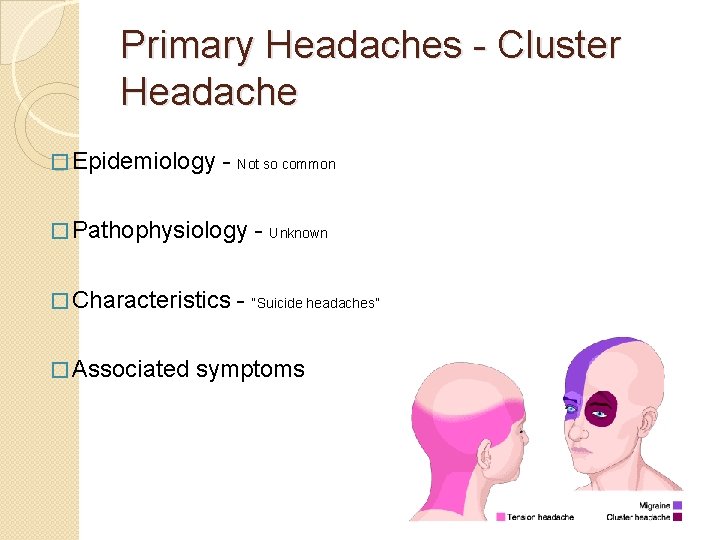
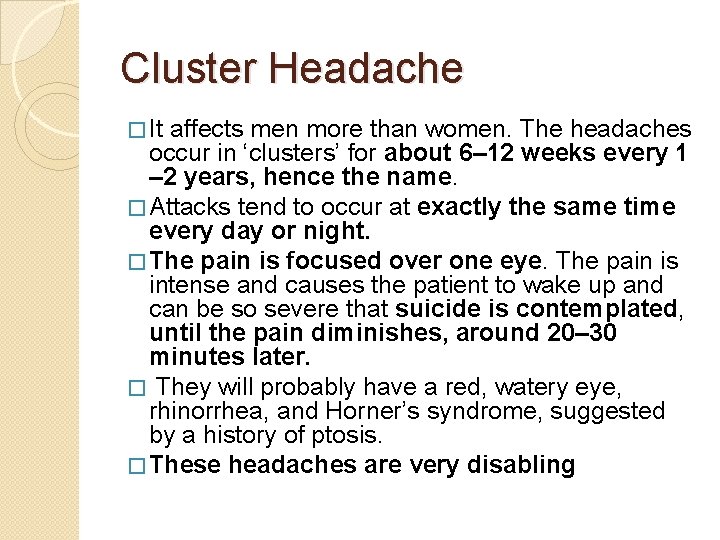
Primary Headaches - Cluster Headache � Epidemiology - Not so common � Pathophysiology � Characteristics � Associated - Unknown - “Suicide headaches” symptoms
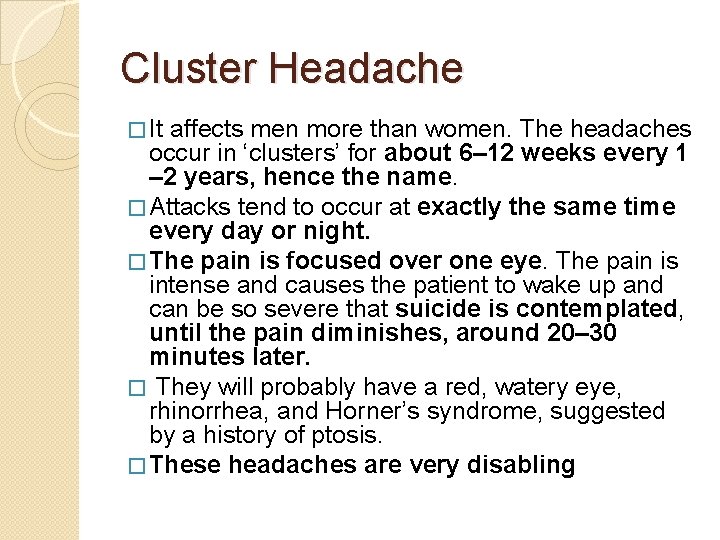
Cluster Headache � It affects men more than women. The headaches occur in ‘clusters’ for about 6– 12 weeks every 1 – 2 years, hence the name. � Attacks tend to occur at exactly the same time every day or night. � The pain is focused over one eye. The pain is intense and causes the patient to wake up and can be so severe that suicide is contemplated, until the pain diminishes, around 20– 30 minutes later. � They will probably have a red, watery eye, rhinorrhea, and Horner’s syndrome, suggested by a history of ptosis. � These headaches are very disabling
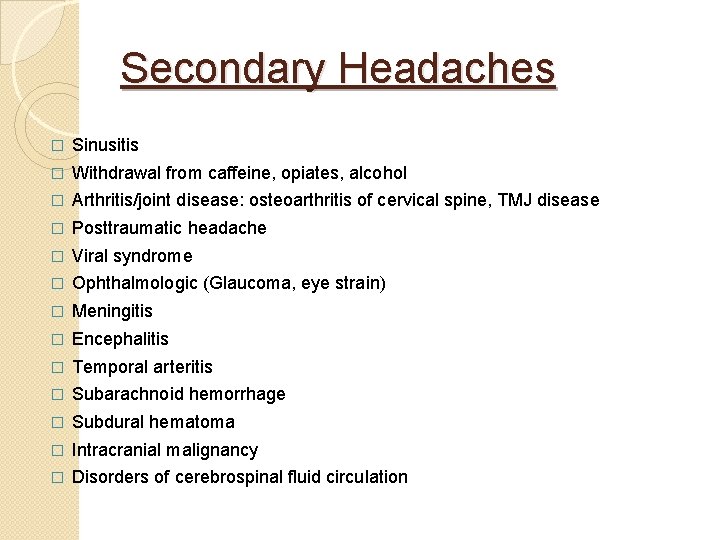
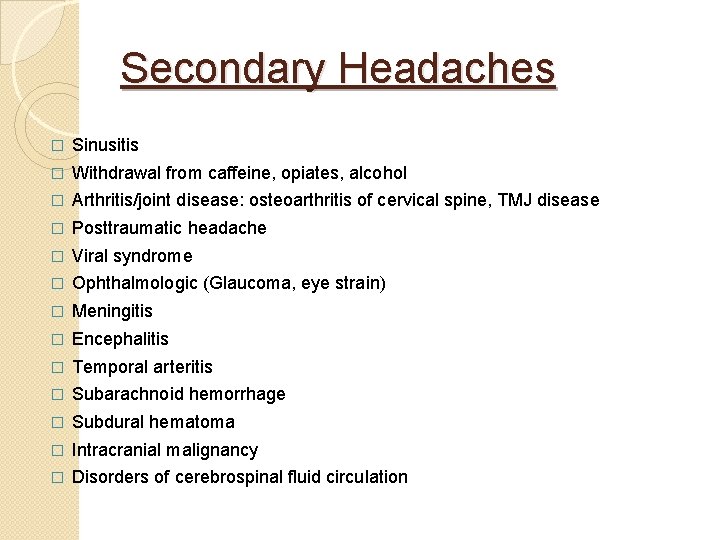
Secondary Headaches � Sinusitis � Withdrawal from caffeine, opiates, alcohol � Arthritis/joint disease: osteoarthritis of cervical spine, TMJ disease � Posttraumatic headache � Viral syndrome � Ophthalmologic (Glaucoma, eye strain) � Meningitis � Encephalitis � Temporal arteritis � Subarachnoid hemorrhage � Subdural hematoma � Intracranial malignancy � Disorders of cerebrospinal fluid circulation
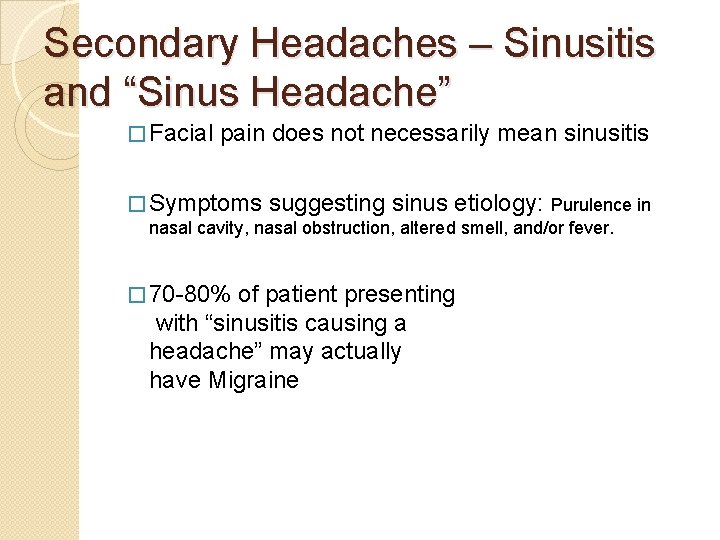
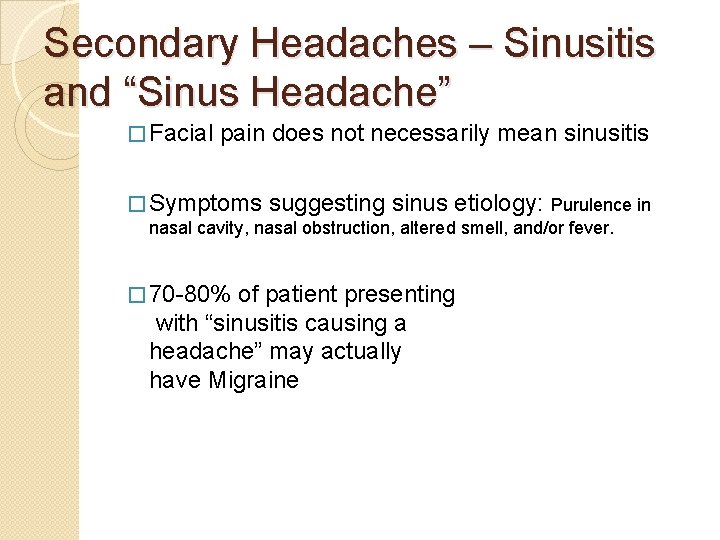
Secondary Headaches – Sinusitis and “Sinus Headache” � Facial pain does not necessarily mean sinusitis � Symptoms suggesting sinus etiology: Purulence in nasal cavity, nasal obstruction, altered smell, and/or fever. � 70 -80% of patient presenting with “sinusitis causing a headache” may actually have Migraine
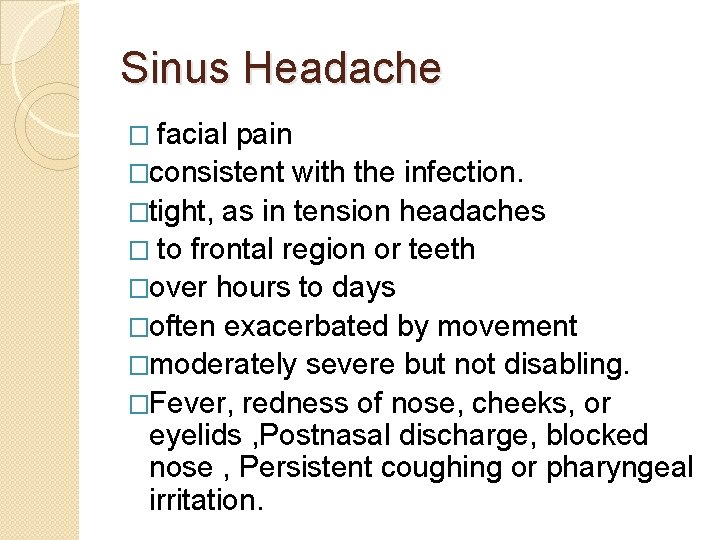
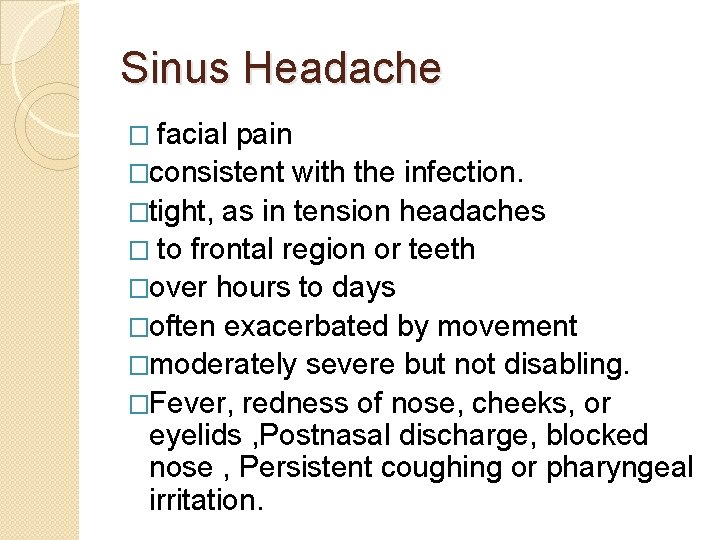
Sinus Headache � facial pain �consistent with the infection. �tight, as in tension headaches � to frontal region or teeth �over hours to days �often exacerbated by movement �moderately severe but not disabling. �Fever, redness of nose, cheeks, or eyelids , Postnasal discharge, blocked nose , Persistent coughing or pharyngeal irritation.

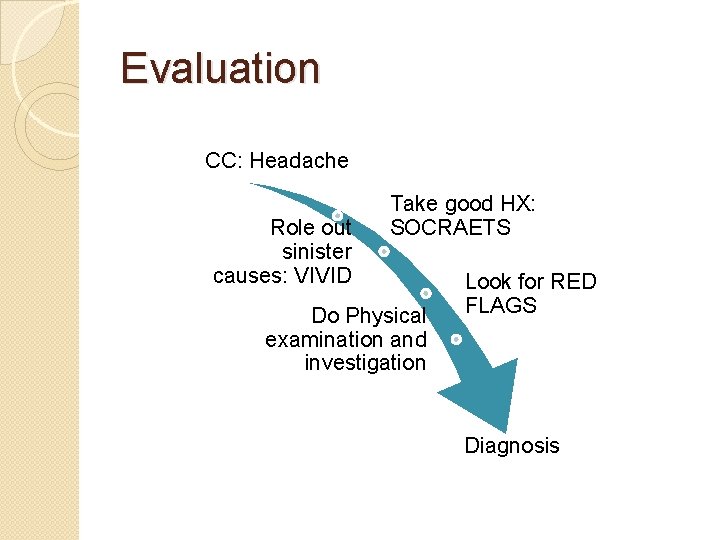
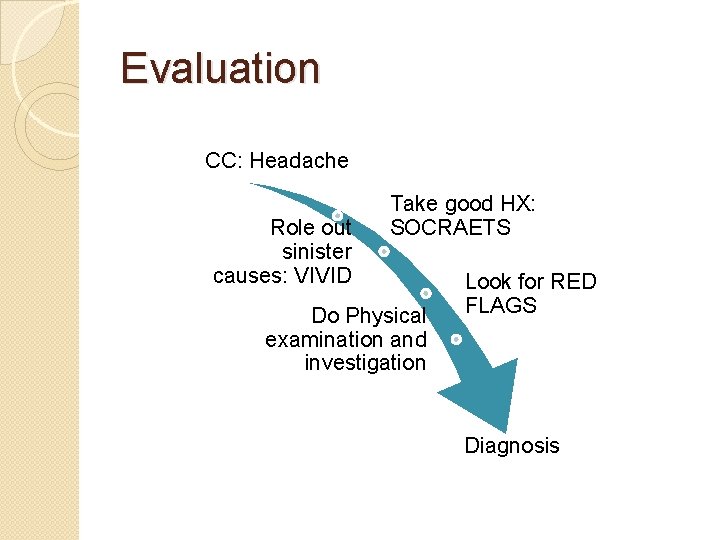
Evaluation CC: Headache Role out sinister causes: VIVID Take good HX: SOCRAETS Do Physical examination and investigation Look for RED FLAGS Diagnosis
Red Flags �Severity of headache (“worst headache of my life”) �Onset of symptoms (abrupt vs. slow) �Accompanying symptoms (Fever, rash, etc…) �History of recent trauma �Presence of neurological deficits
Physical Examination �General appearance and vital signs �Ear, nose and throat exam �Kernig, Brudzinkski and neck stiffness �Neurological Evaluation �Fundoscopy for papilledema �Palpation of temporal artery, TMJ and neighboring muscles

Diagnostic Testing �History and Physical Exam are the best tools �Lumbar Puncture in case of meningitis or SAH �CT scan in certain non-traumatic cases: 1) Recent change in pattern, frequency or severity 2) Progressive worsening despite treatment 3) Focal neurological signs 4) Onset with exertion, cough or sexual activity 5) Orbital Bruit (Aneurysm, carotid artery stenosis/thrombosis) 6) Onset after 50 years of age
Management �Treat underlying cause for secondary headaches �Goals of treatment: 1) Treat the headache and provide symptomatic relief 2) Minimize use of 2 nd line drugs 3) Minimize hospitalization 4) Minimize adverse effects 5) Prevent recurrence
Management: Migraine 1. Migraines: Abortive treatment: • Mild to moderate migraine: Combination analgesics containing aspirin, caffeine, and acetaminophen or NSAID are an effective first-line abortive treatment, Triptans-oral or intranasal- is a second line. • Moderate to severe migraines: Triptans are first-line therapy, then dihydroergotamine • Prophylactic treatment if necessary
Management: Migraine �Medications containing opiates or barbiturates should be avoided for acute migraine �Intravenous metoclopramide is effective for acute migraine treatment
Migraine prophylaxis: �Identify and avoid headache triggers. Prophylaxis treatment is indicated when: 1 - frequency: more than 2 attacks per month 2 - duration more than 24 hrs. 3 - Abortive therapy fails or is overused. 4 - Use of abortive medications more than twice a week. 5 - the attack affect pt’s life style, with significant disability that lasts 3 or more days.

Tension Headaches: Management • Acetaminophen or NSAIDs suffice due to non-debilitating nature • Acupuncture, spinal manipulation and electrotherapy differ in effectiveness • Amitriptyline prophylaxis with 15+ episodes per month
Management Cluster Headaches: • High-flow oxygen or triptans as first line treatment • Verapamil as prophylaxis
Management 4) Chronic Daily Headache: • Amitriptyline is the mainstay of treatment • May improve with acetaminophen or NSAIDs, but overuse could induce chronic headaches �Headache questionnaires are useful in determining the severity of headaches and response to treatment

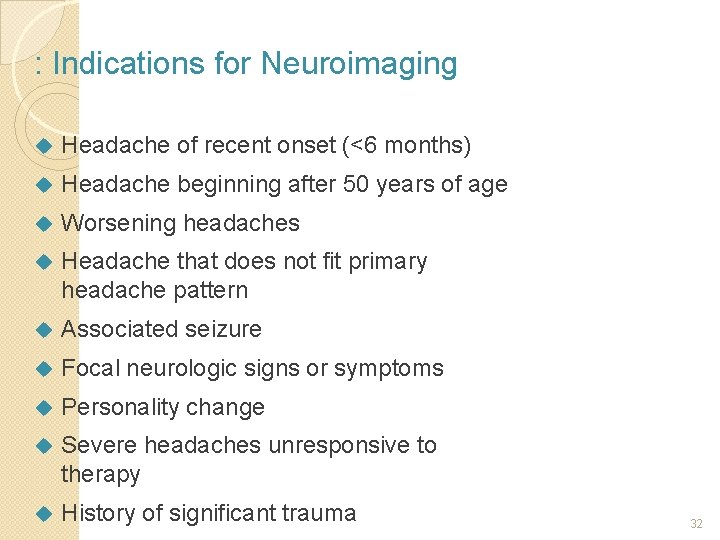
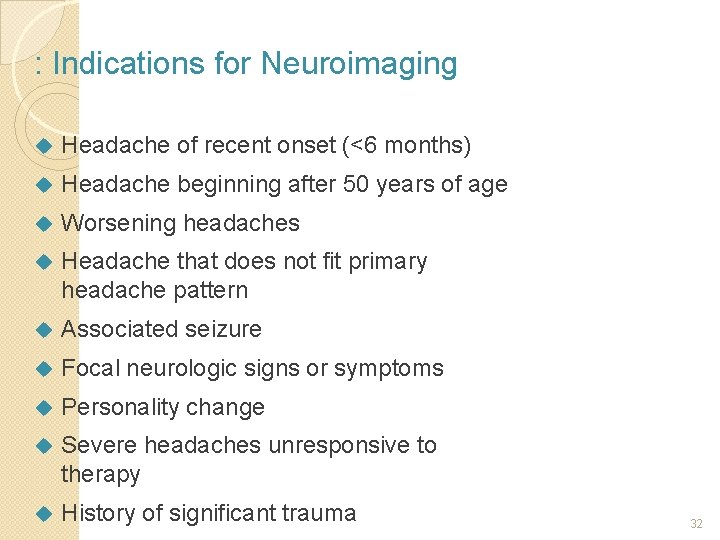
: Indications for Neuroimaging Headache of recent onset (<6 months) Headache beginning after 50 years of age Worsening headaches Headache that does not fit primary headache pattern Associated seizure Focal neurologic signs or symptoms Personality change Severe headaches unresponsive to therapy History of significant trauma 32
 Duaa meaning in english
Duaa meaning in english Dua for first night
Dua for first night Friday duaa
Friday duaa Ux research portfolio
Ux research portfolio Pediatric headache red flags
Pediatric headache red flags Infosys sabbatical leave policy
Infosys sabbatical leave policy Headache pain chart
Headache pain chart Headache red flags
Headache red flags Right side headache
Right side headache Pumcture
Pumcture Snoop headache criteria
Snoop headache criteria Postdrome
Postdrome Ophthalmoplegic migraine
Ophthalmoplegic migraine Headache
Headache Severe anxiety
Severe anxiety Post ictal phase
Post ictal phase Nursing care plan for headache slideshare
Nursing care plan for headache slideshare Meao mudra benefits
Meao mudra benefits Rasmussen's encephalitis
Rasmussen's encephalitis Anish bahra
Anish bahra Epley maneuver
Epley maneuver Snoop headache
Snoop headache Headache
Headache ı have a headache song
ı have a headache song Mauskop
Mauskop Headache
Headache European headache federation
European headache federation Types of family in community medicine
Types of family in community medicine Principles of family medicine
Principles of family medicine Halifax family medicine residency
Halifax family medicine residency Meritus definition
Meritus definition Family medicine fellowship
Family medicine fellowship Milestones family medicine
Milestones family medicine