Headache Painsensitive cranial structures l l l Skin




- Slides: 82


頭痛 Headache
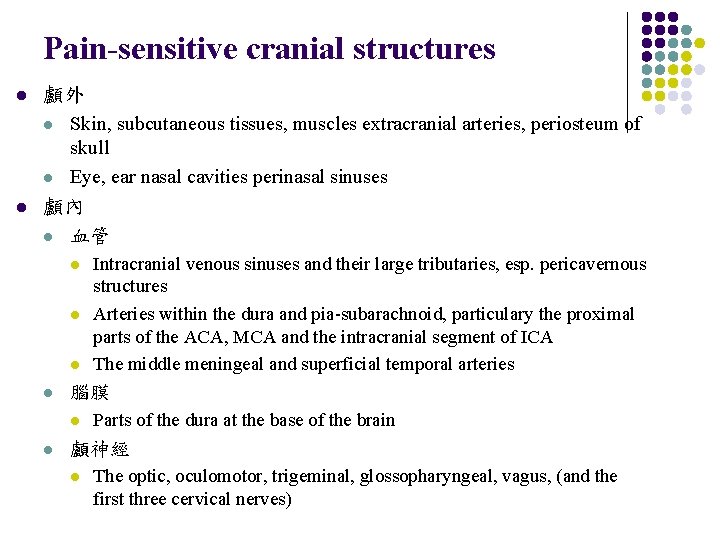
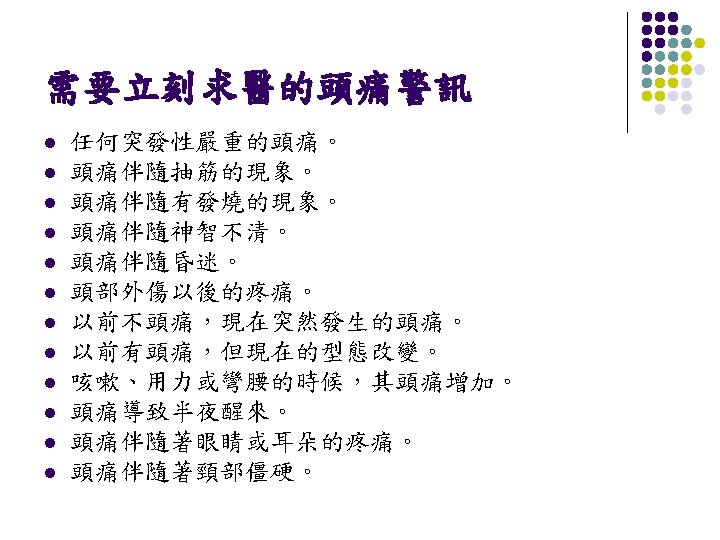
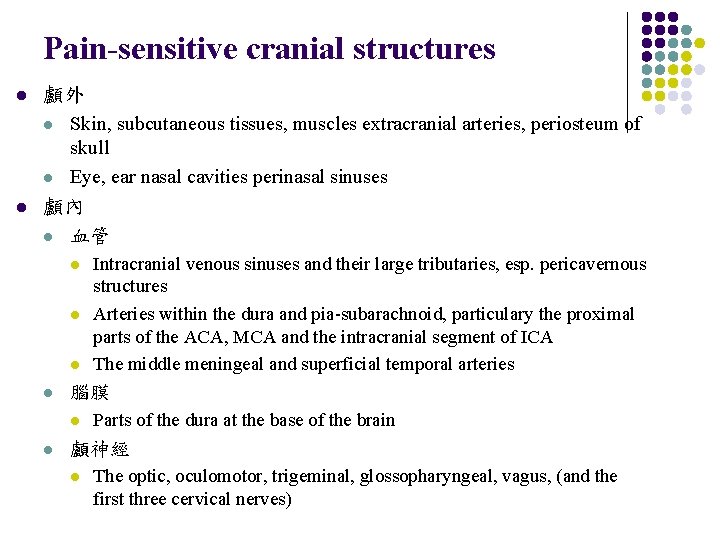
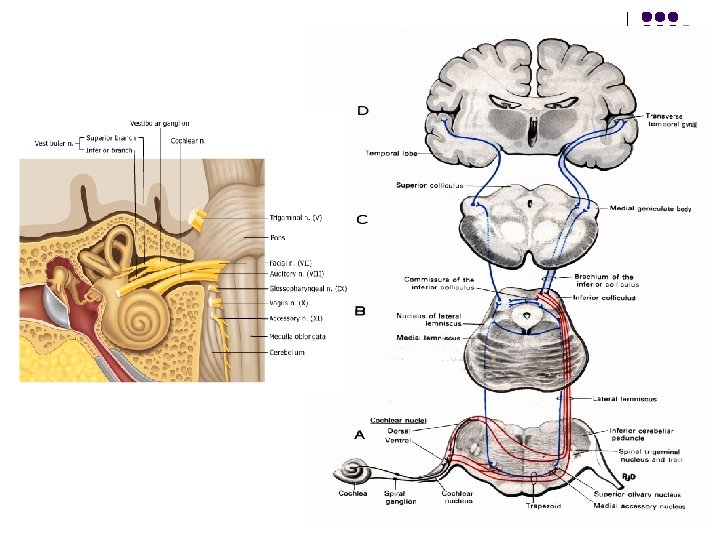
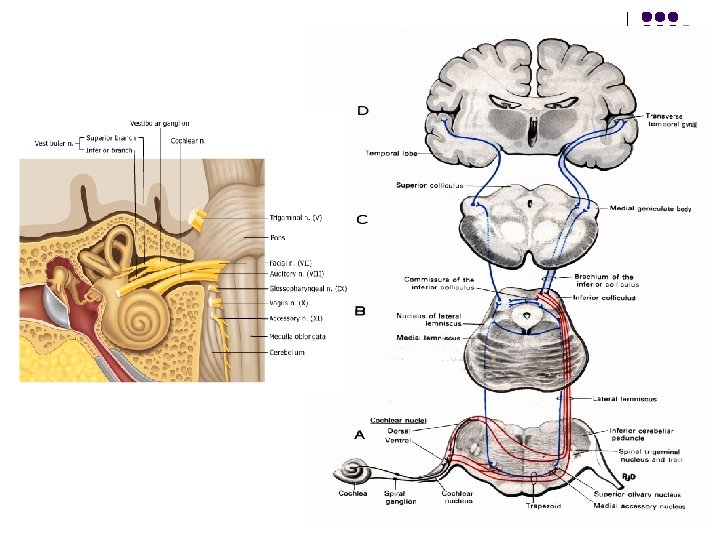
Pain-sensitive cranial structures l l 顱外 l Skin, subcutaneous tissues, muscles extracranial arteries, periosteum of skull l Eye, ear nasal cavities perinasal sinuses 顱內 l 血管 l l 腦膜 l l Intracranial venous sinuses and their large tributaries, esp. pericavernous structures Arteries within the dura and pia-subarachnoid, particulary the proximal parts of the ACA, MCA and the intracranial segment of ICA The middle meningeal and superficial temporal arteries Parts of the dura at the base of the brain 顱神經 l The optic, oculomotor, trigeminal, glossopharyngeal, vagus, (and the first three cervical nerves)
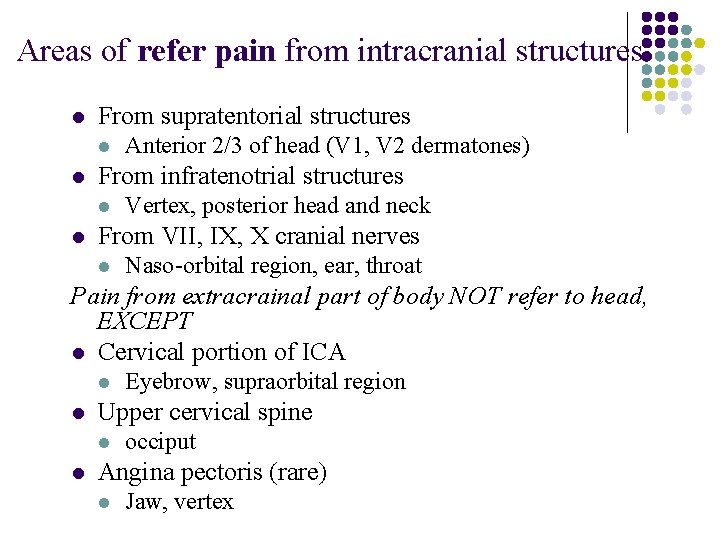
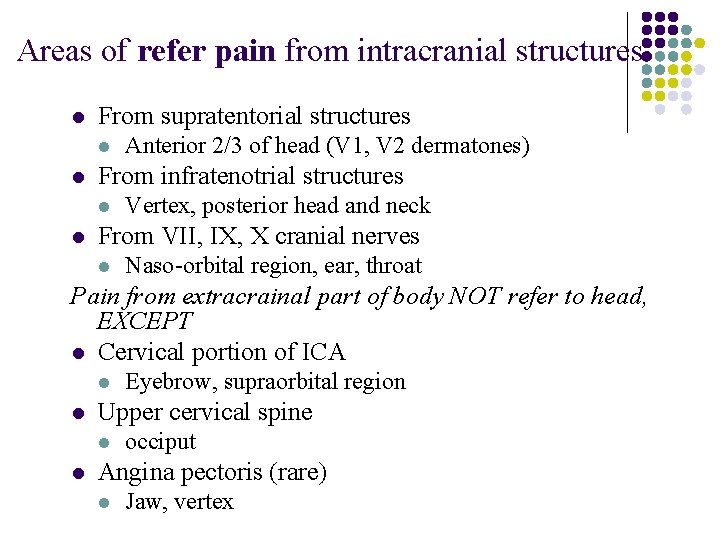
Areas of refer pain from intracranial structures l From supratentorial structures l l From infratenotrial structures l l Anterior 2/3 of head (V 1, V 2 dermatones) Vertex, posterior head and neck From VII, IX, X cranial nerves l Naso-orbital region, ear, throat Pain from extracrainal part of body NOT refer to head, EXCEPT l Cervical portion of ICA l l Upper cervical spine l l Eyebrow, supraorbital region occiput Angina pectoris (rare) l Jaw, vertex
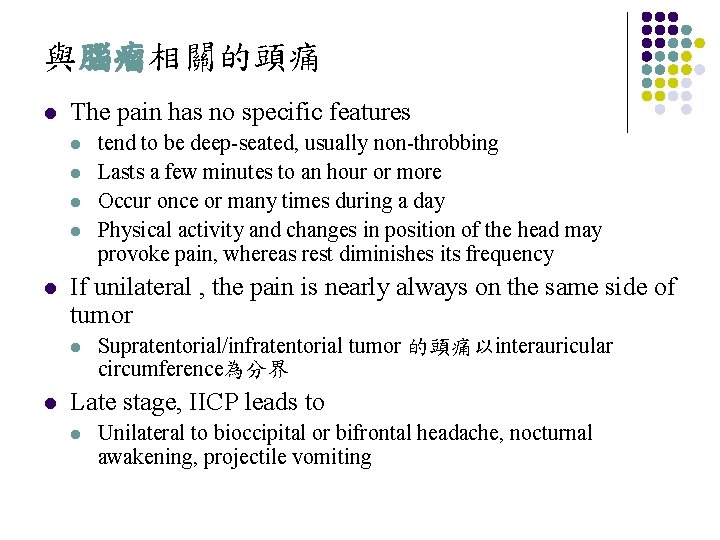
與腦瘤相關的頭痛 l The pain has no specific features l l l If unilateral , the pain is nearly always on the same side of tumor l l tend to be deep-seated, usually non-throbbing Lasts a few minutes to an hour or more Occur once or many times during a day Physical activity and changes in position of the head may provoke pain, whereas rest diminishes its frequency Supratentorial/infratentorial tumor 的頭痛以interauricular circumference為分界 Late stage, IICP leads to l Unilateral to bioccipital or bifrontal headache, nocturnal awakening, projectile vomiting
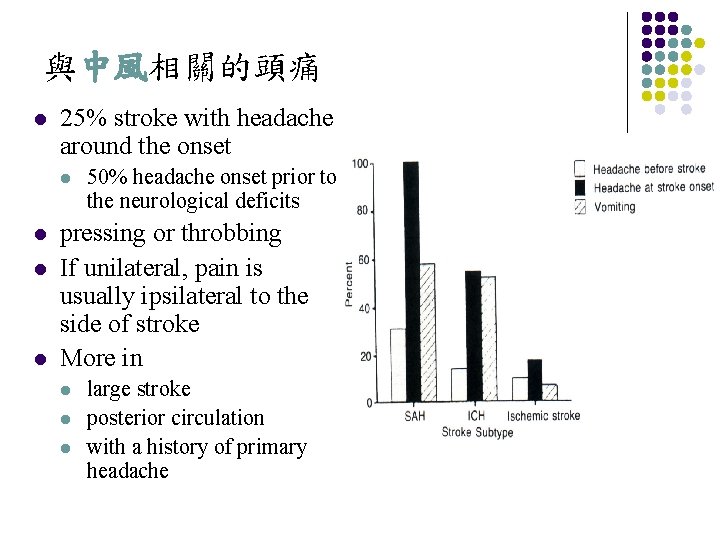
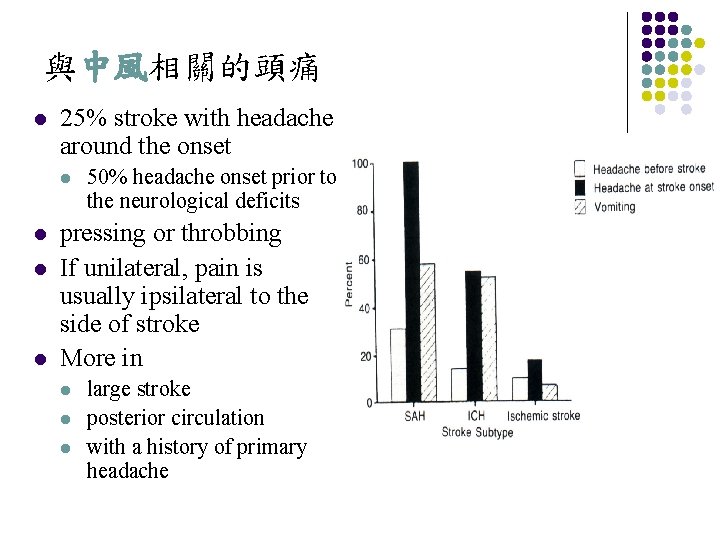
與中風相關的頭痛 l 25% stroke with headache around the onset l l 50% headache onset prior to the neurological deficits pressing or throbbing If unilateral, pain is usually ipsilateral to the side of stroke More in l large stroke posterior circulation with a history of primary headache
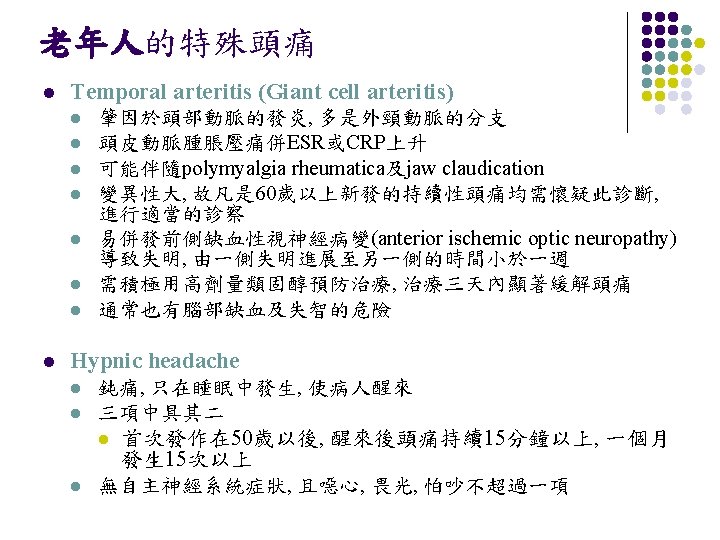
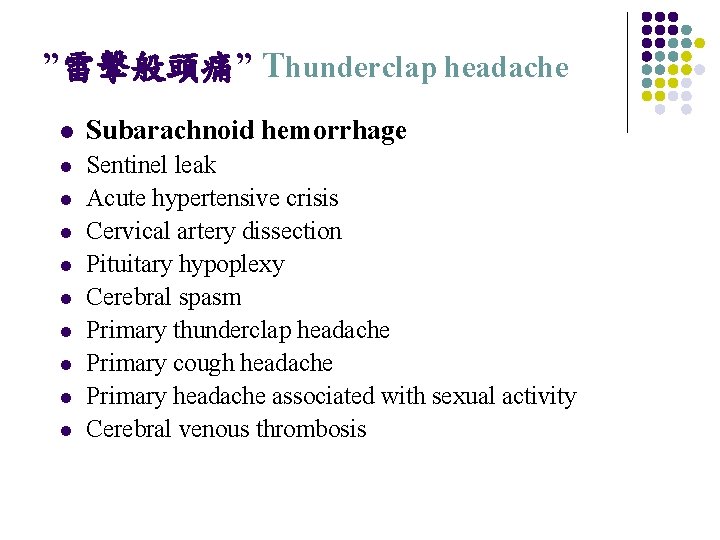
”雷擊般頭痛” Thunderclap headache l Subarachnoid hemorrhage l Sentinel leak Acute hypertensive crisis Cervical artery dissection Pituitary hypoplexy Cerebral spasm Primary thunderclap headache Primary cough headache Primary headache associated with sexual activity Cerebral venous thrombosis l l l l
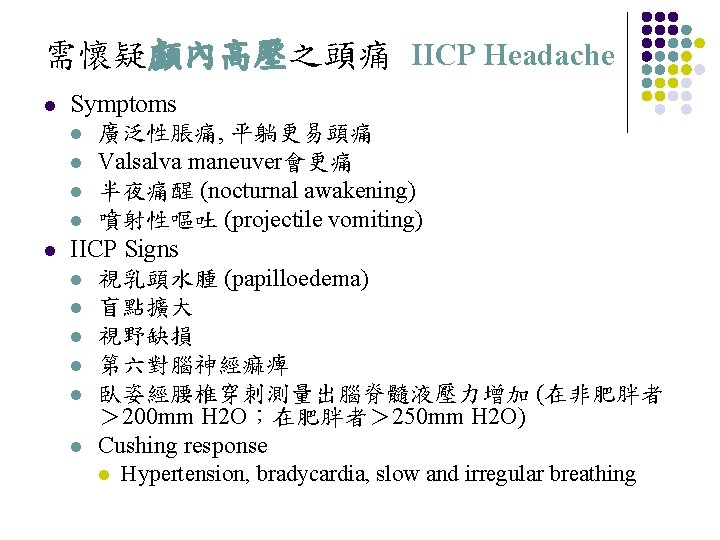
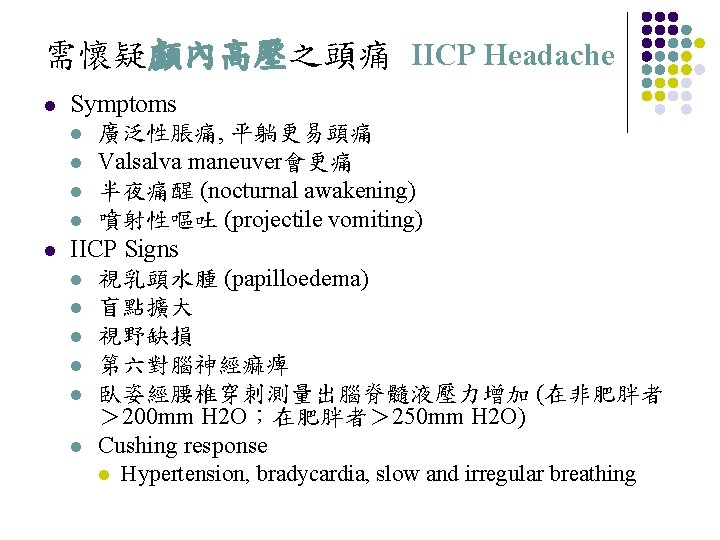
需懷疑顱內高壓之頭痛 IICP Headache l l Symptoms l 廣泛性脹痛, 平躺更易頭痛 l Valsalva maneuver會更痛 l 半夜痛醒 (nocturnal awakening) l 噴射性嘔吐 (projectile vomiting) IICP Signs l 視乳頭水腫 (papilloedema) l 盲點擴大 l 視野缺損 l 第六對腦神經痲痺 l 臥姿經腰椎穿刺測量出腦脊髓液壓力增加 (在非肥胖者 > 200 mm H 2 O;在肥胖者> 250 mm H 2 O) l Cushing response l Hypertension, bradycardia, slow and irregular breathing
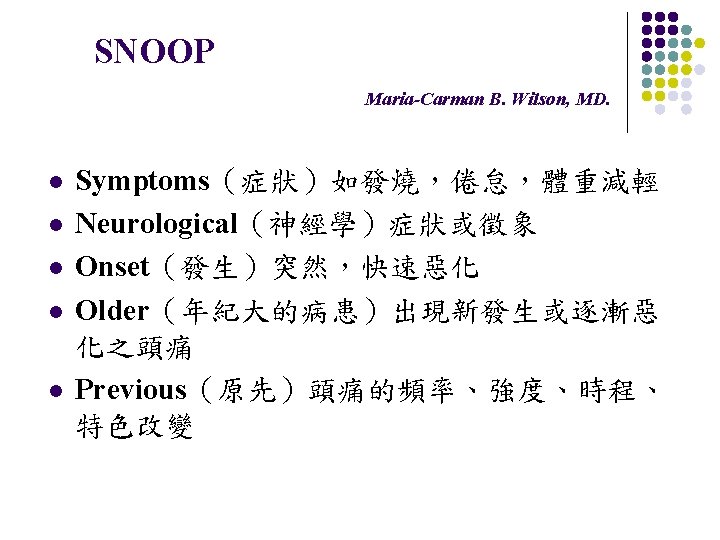
Approach patients with headache
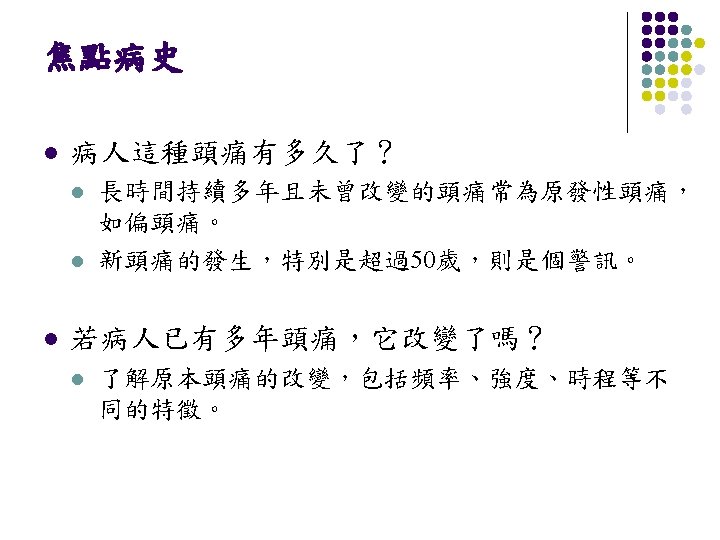
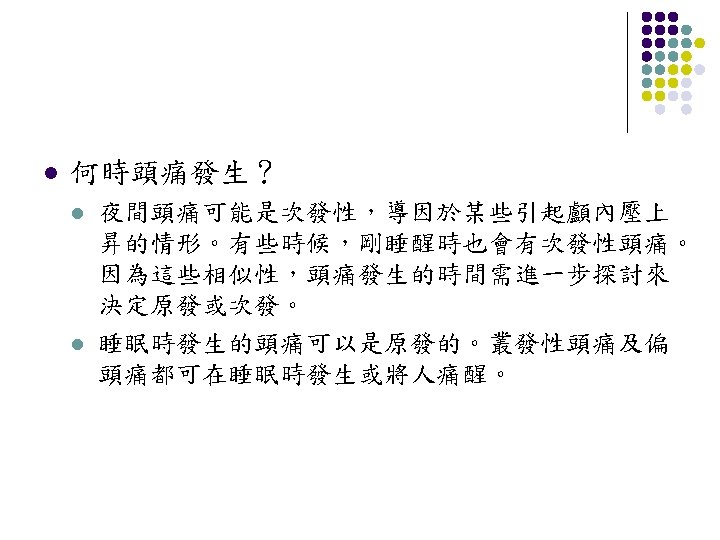
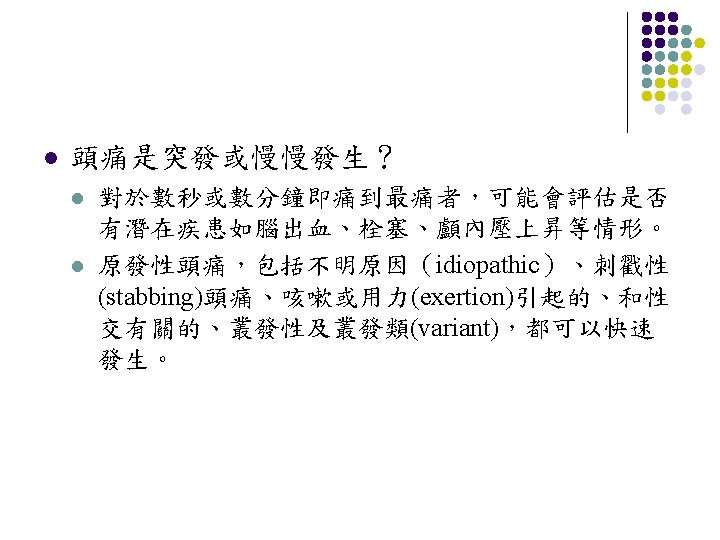
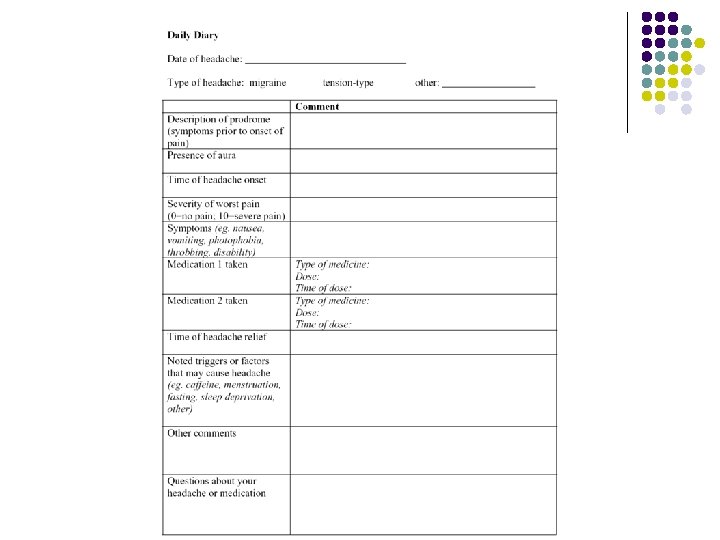
Head Ache … 有關頭痛需要獲得的病史 l l Location Quality l l l Tightness, pressure, throbbing, stabbing… Intensity Mode of onset, time-intensity curve, and duration Precipitating, aggravating and relieving factors Associative symptoms
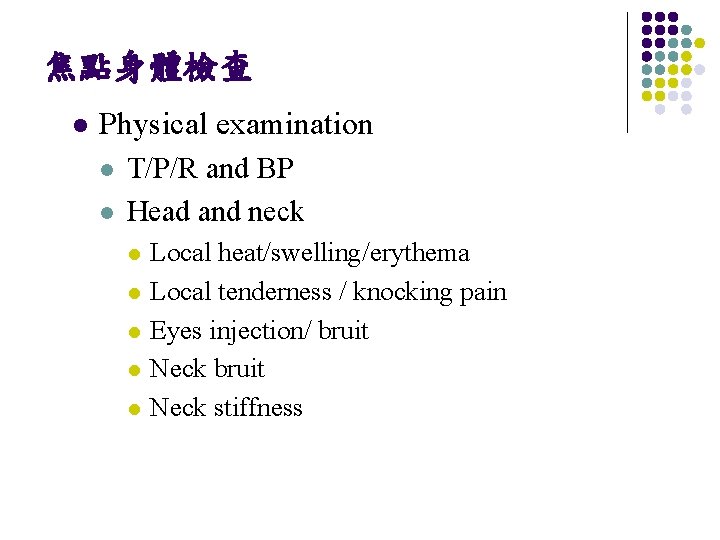
焦點身體檢查 l Physical examination l l T/P/R and BP Head and neck l l l Local heat/swelling/erythema Local tenderness / knocking pain Eyes injection/ bruit Neck stiffness
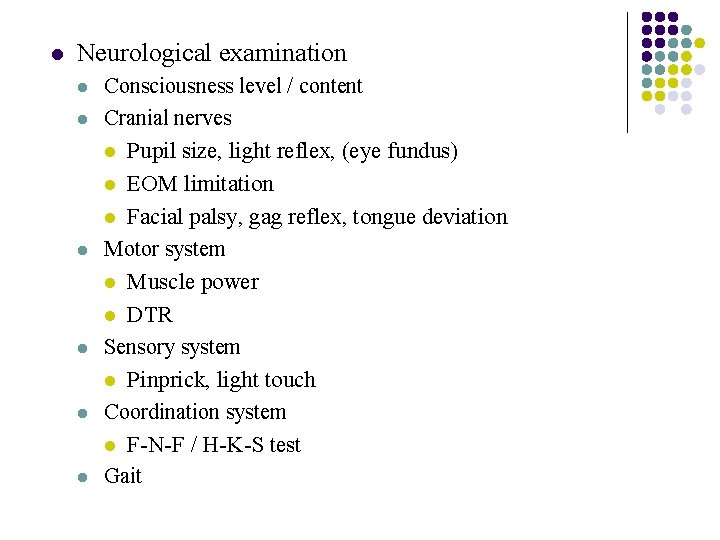
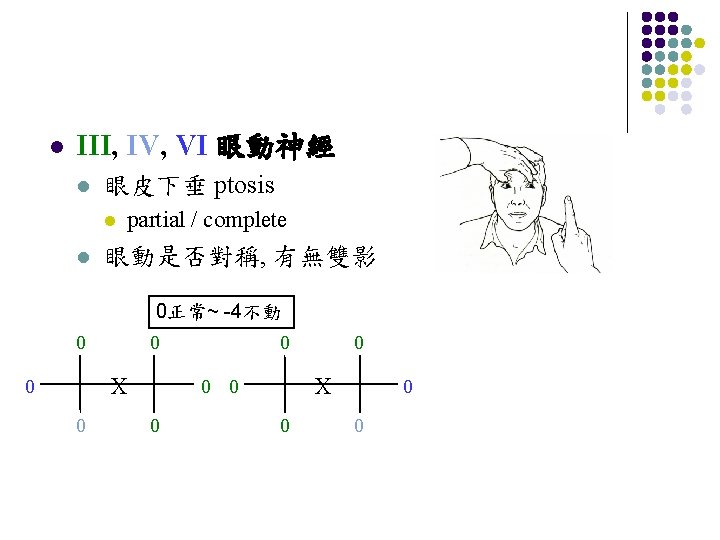
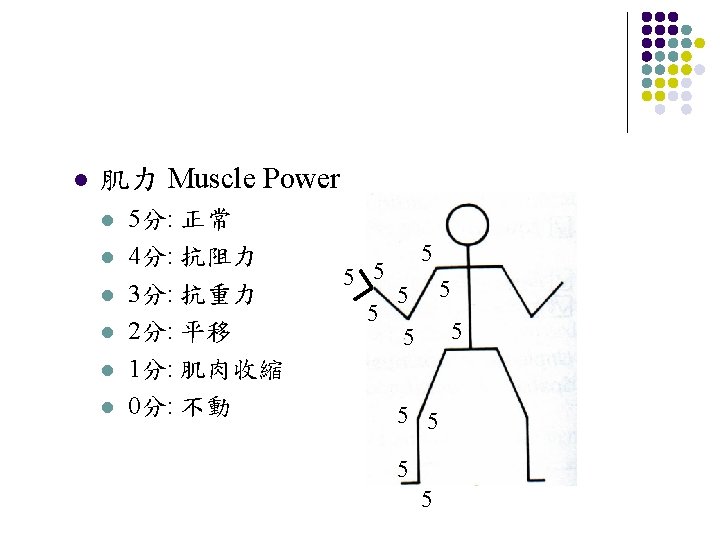
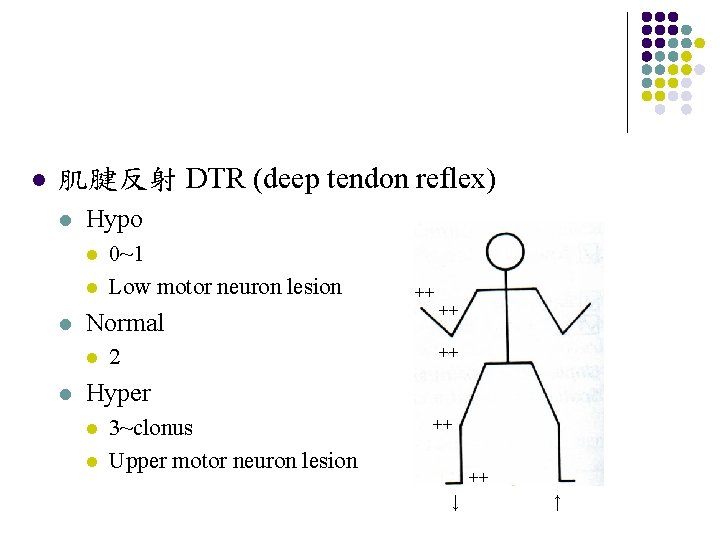
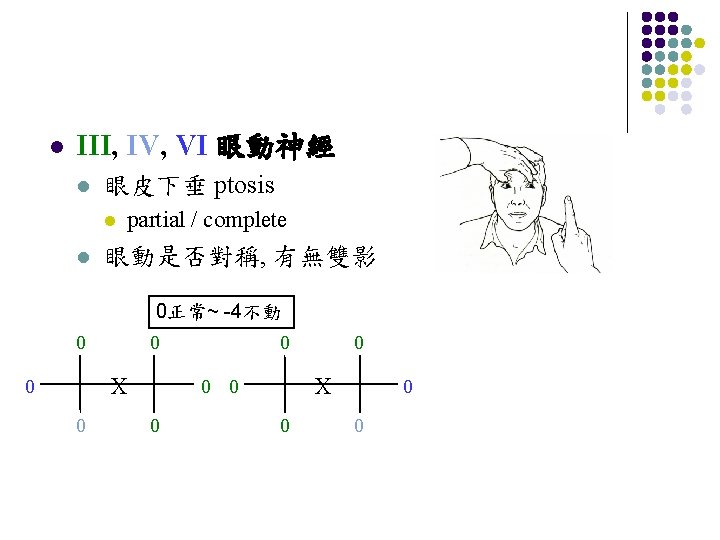
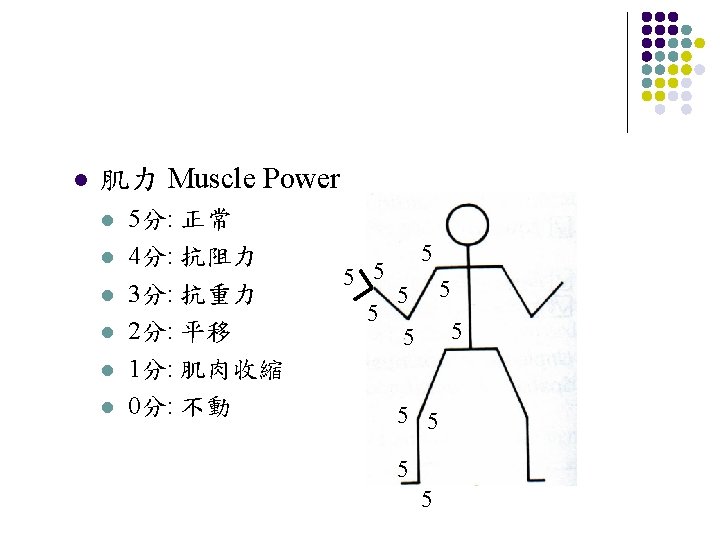
l Neurological examination l l Consciousness level / content Cranial nerves l Pupil size, light reflex, (eye fundus) EOM limitation l Facial palsy, gag reflex, tongue deviation Motor system l Muscle power l DTR Sensory system l Pinprick, light touch Coordination system l F-N-F / H-K-S test Gait l l l
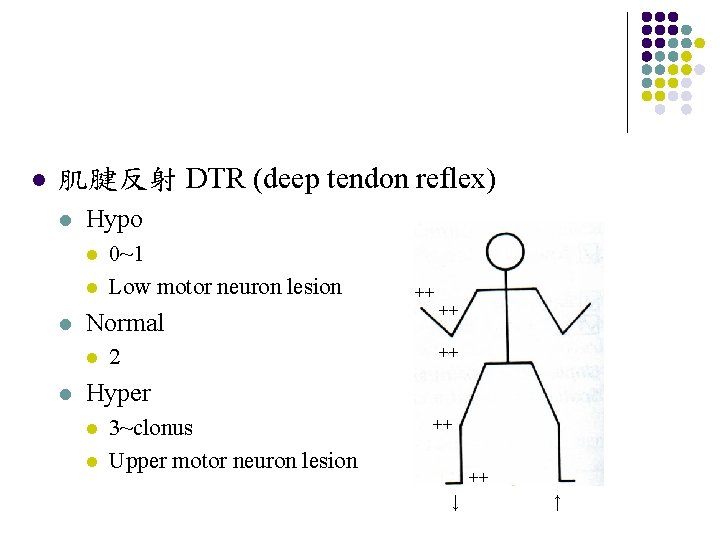
l 肌腱反射 DTR (deep tendon reflex) l Hypo l l l Normal l l 0~1 Low motor neuron lesion 2 ++ ++ ++ Hyper l l 3~clonus Upper motor neuron lesion ++ ++ ↓ ↑
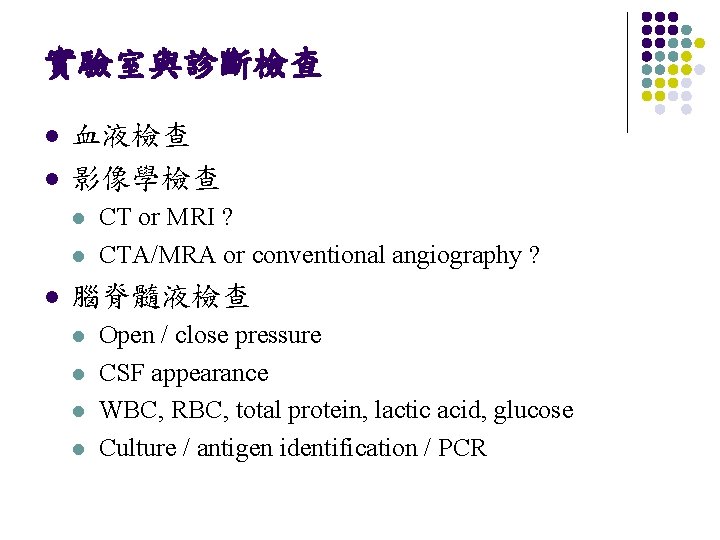
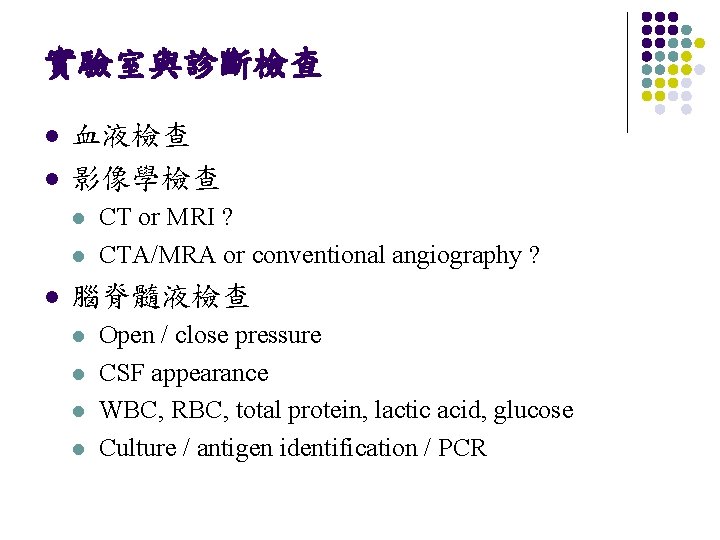
實驗室與診斷檢查 l l 血液檢查 影像學檢查 l l l CT or MRI ? CTA/MRA or conventional angiography ? 腦脊髓液檢查 l l Open / close pressure CSF appearance WBC, RBC, total protein, lactic acid, glucose Culture / antigen identification / PCR
Headache Hygiene Tips (1) l Get Regular Sleep l l Eat Regular Meals l l Go to bed and wake up at regular times each day Do not sleep excessively on the weekends and too little on the weekdays Most adults need approximately 6 -8 hours of sleep per night Low blood sugar can trigger a headache Eat regular meals three times each day including protein, fruits, vegetables and carbohydrates Too much sugar may lead to a rapid increase in blood sugar followed by a rapid decline in blood sugar, which can trigger a headache Get Moderate Amounts of Routine Exercise l l Moderate exercise three to five times each week will help reduce stress and keep you physically fit Too much exercise or inconsistent patterns of exercise may trigger headache
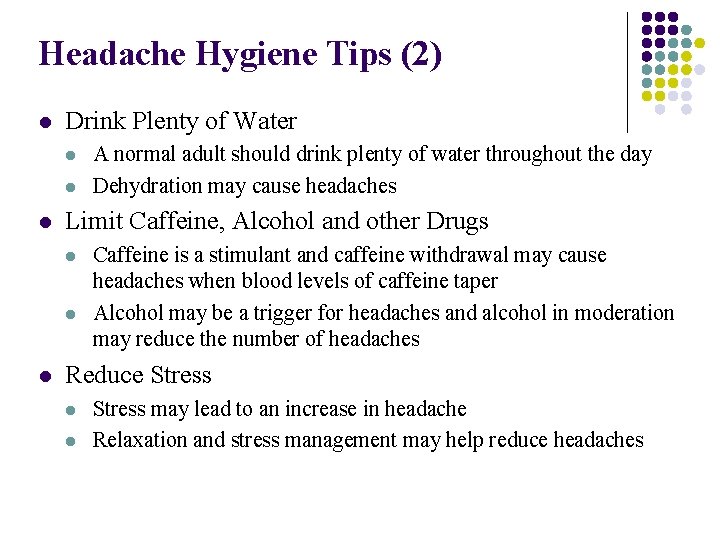
Headache Hygiene Tips (2) l Drink Plenty of Water l l l Limit Caffeine, Alcohol and other Drugs l l l A normal adult should drink plenty of water throughout the day Dehydration may cause headaches Caffeine is a stimulant and caffeine withdrawal may cause headaches when blood levels of caffeine taper Alcohol may be a trigger for headaches and alcohol in moderation may reduce the number of headaches Reduce Stress l l Stress may lead to an increase in headache Relaxation and stress management may help reduce headaches
Headache - Cases discussion

CASE 2 25 year-old female, no underlying disease l Subacute progressive headache for 2 months l l l l Diffuse, swelling sensation Cough and defecation worse the headache Midnight headache, awaking her from sleep nausea/vomiting while headache Blurred vision (+) Body weight loss (+) Fever (-)
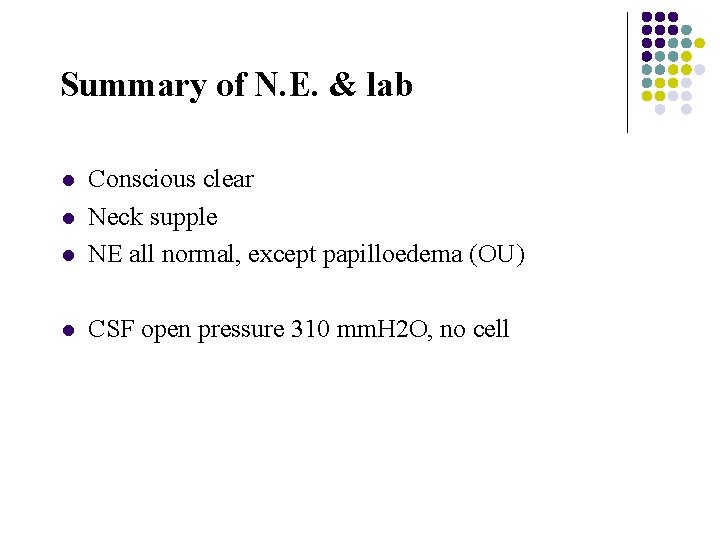
Summary of N. E. & lab l Conscious clear Neck supple NE all normal, except papilloedema (OU) l CSF open pressure 310 mm. H 2 O, no cell l l
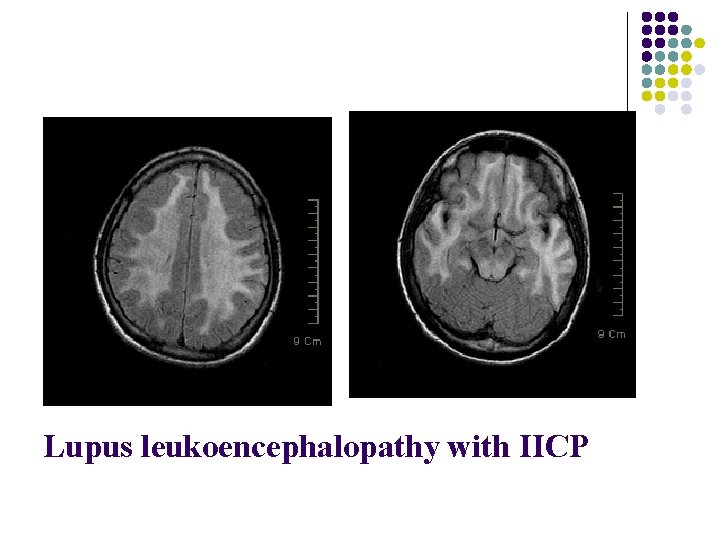
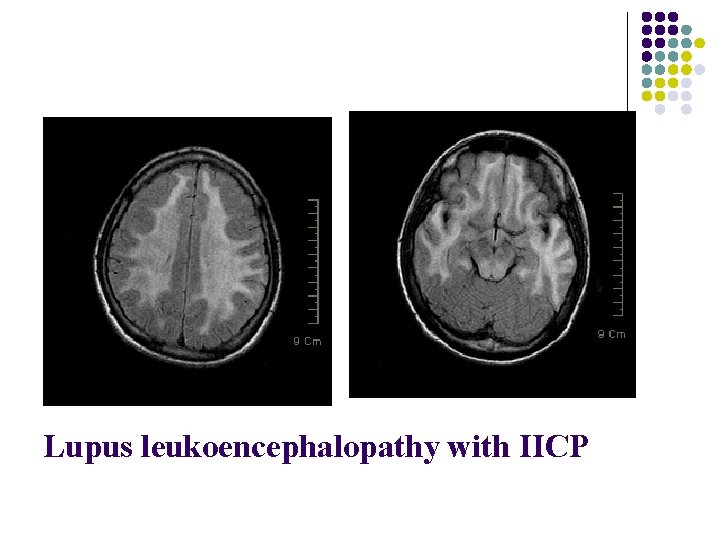
Lupus leukoencephalopathy with IICP

頭暈 Dizziness
病人主訴Dizziness”頭暈”的意思是…. ? l Vertigo 眩暈 l l Nonspecific “dizziness” l l l an illusion of motion “spinning sensation”, ”whirling” , ”tilting” likely to indicate an abnormality of the semicircular canals or the central nervous system structures that process signals from the semicircular canals “giddy” or “lightheaded” Disequilibrium Presyncope
當病人主訴”頭暈”…. l l l 40% have peripheral vestibular dysfunction 25% have other problems, such as presyncope and disequilibrium 15% have a psychiatric disorder 10% have a central brainstem vestibular lesion 10 % remains uncertain in approximately
區分vertigo和dizziness (1) l Time course l l Provoking factors l l Vertigo is never continuous l Even when the vestibular lesion is permanent, the central nervous system adapts to the defect so that vertigo subsides over several weeks Some are precipitated by maneuvers that change head position or middle ear pressure l maneuvers that change head position without lowering blood pressure or decreasing cerebral blood flow is diagnostic Aggravating factors l All vertigo is made worse by moving the head. l If head motion does not worsen the feeling, it is probably another type of dizziness.
區分vertigo和dizziness (2) l Associated signs and symptoms l l Nystagmus l is not always readily visible, although it often can be elicited by provocative maneuvers or with electronystagmography. Postural instability l it is common for patients with vertigo to have difficulty maintaining steady upright posture when walking, standing, and even sitting unsupported, particularly when the symptoms are acute. Hearing loss l very suggestive of a peripheral cause of vertigo, although their absence does not exclude the diagnosis Brainstem signs l The presence of additional neurologic signs strongly suggests the presence of a central vestibular lesion.
Peripheral vertigo
Benign paroxysmal positional vertigo l l The most common form of positional vertigo, accounting for nearly 1/2 of patients with peripheral vestibular dysfunction Most commonly attributed to calcium debris within the posterior semicircular canal, known as canalithiasis l l posterior canal BPPV more often than the anterior (superior) and horizontal semicircular canals Symptoms l l l recurrent episodes of vertigo lasting one minute or less provoked by specific types of head movements typically recur periodically for weeks to months without therapy may be associated with nausea and vomiting have no other neurologic complaints
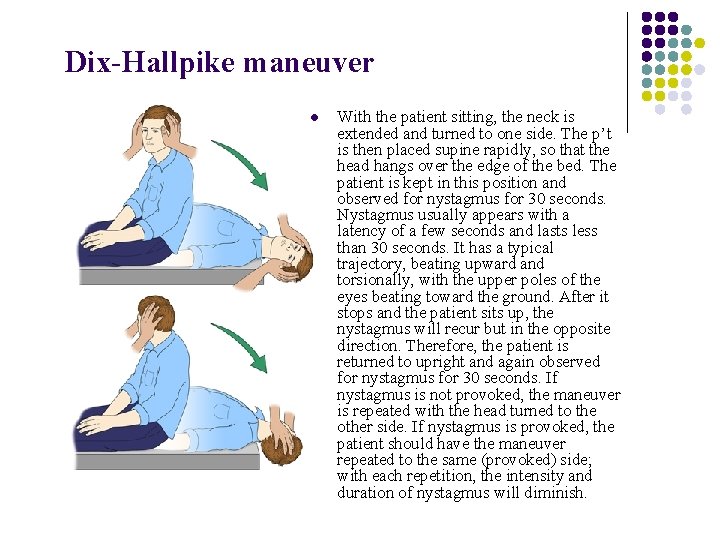
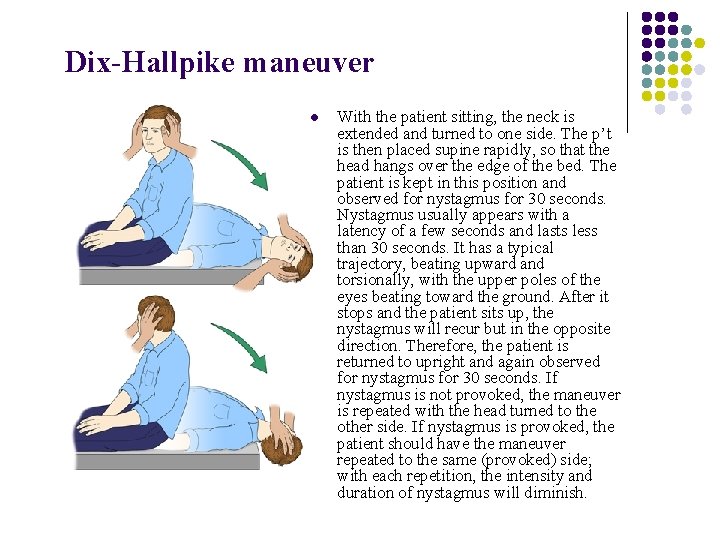
Dix-Hallpike maneuver l With the patient sitting, the neck is extended and turned to one side. The p’t is then placed supine rapidly, so that the head hangs over the edge of the bed. The patient is kept in this position and observed for nystagmus for 30 seconds. Nystagmus usually appears with a latency of a few seconds and lasts less than 30 seconds. It has a typical trajectory, beating upward and torsionally, with the upper poles of the eyes beating toward the ground. After it stops and the patient sits up, the nystagmus will recur but in the opposite direction. Therefore, the patient is returned to upright and again observed for nystagmus for 30 seconds. If nystagmus is not provoked, the maneuver is repeated with the head turned to the other side. If nystagmus is provoked, the patient should have the maneuver repeated to the same (provoked) side; with each repetition, the intensity and duration of nystagmus will diminish.
Vestibular neuritis l l Viral or postviral inflammatory disorder affecting the vestibular portion of the eighth cranial nerve Symptoms l Sapid onset of severe vertigo l nausea, vomiting l gait instability. preserved ability to ambulate. toward the affected side have no other neurologic complaints l l l Signs l Spontaneous vestibular nystagmus l l unilateral, horizontal, or horizontal-torsional suppressed with visual fixation does not change direction with gaze fast phase of nystagmus beats away from the affected side.
Meniere's disease l Arise from abnormal fluid and ion homeostasis in the inner ear l l endolymphatic hydrops with distortion and distention of the membranous, endolymph-containing portions of the labyrinthine system Syndrome l episodic vertigo l l Sensorineural hearing loss l l associated with nausea and vomiting, and persists from 20 minutes to 24 hours duration often initially affects the lower frequencies. progresses over time, and often results in permanent hearing loss at all frequencies in the affected ear over an 8 to 10 year period typically associated with intense aural fullness or pressure in the ear or the side of the head Tinnitus l l characteristically low pitch may be associated with auditory distortion
Central vertigo
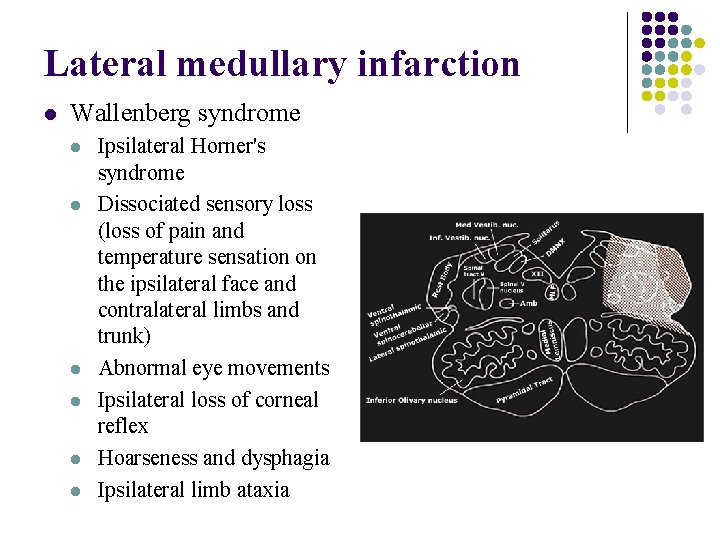
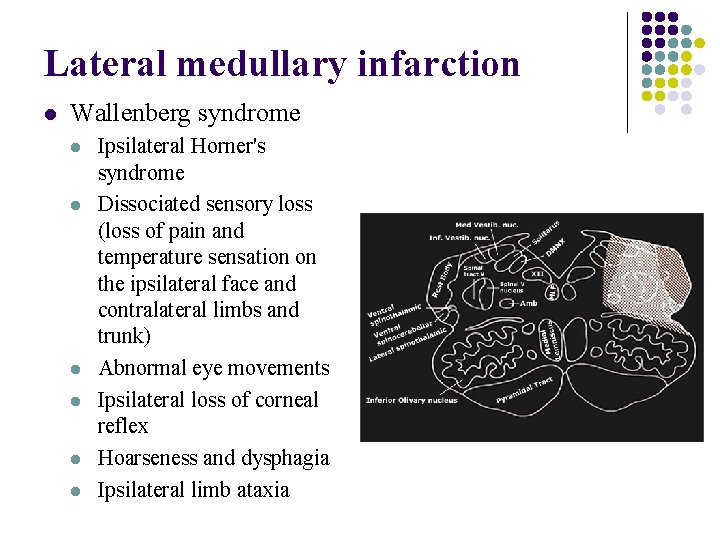
Lateral medullary infarction l Wallenberg syndrome l l l Ipsilateral Horner's syndrome Dissociated sensory loss (loss of pain and temperature sensation on the ipsilateral face and contralateral limbs and trunk) Abnormal eye movements Ipsilateral loss of corneal reflex Hoarseness and dysphagia Ipsilateral limb ataxia
Cerebellar stroke l l l Vertigo, may with nausea/vomiting Limb dysmetria, dysarthria, or headache Usually unable to stand or walk unsupported l The direction of falling is not necessarily opposite to the direction of the nystagmus Nystagmus l other than horizontal or horizontal-torsional, l may change direction with gaze l not suppressed with visual fixation Patients with a vascular event are typically older and/or have atherosclerosis risk factors (hypertension, diabetes, smoking).
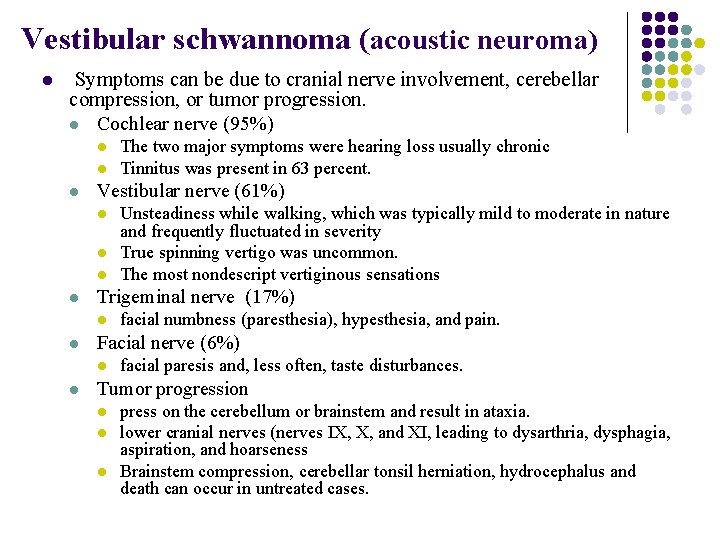
Vestibular schwannoma (acoustic neuroma) l Symptoms can be due to cranial nerve involvement, cerebellar compression, or tumor progression. l Cochlear nerve (95%) l l l Vestibular nerve (61%) l l facial numbness (paresthesia), hypesthesia, and pain. Facial nerve (6%) l l Unsteadiness while walking, which was typically mild to moderate in nature and frequently fluctuated in severity True spinning vertigo was uncommon. The most nondescript vertiginous sensations Trigeminal nerve (17%) l l The two major symptoms were hearing loss usually chronic Tinnitus was present in 63 percent. facial paresis and, less often, taste disturbances. Tumor progression l l l press on the cerebellum or brainstem and result in ataxia. lower cranial nerves (nerves IX, X, and XI, leading to dysarthria, dysphagia, aspiration, and hoarseness Brainstem compression, cerebellar tonsil herniation, hydrocephalus and death can occur in untreated cases.
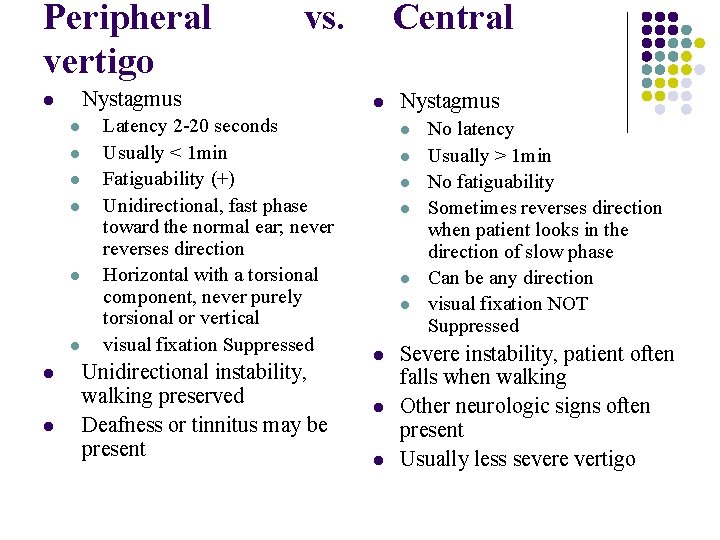
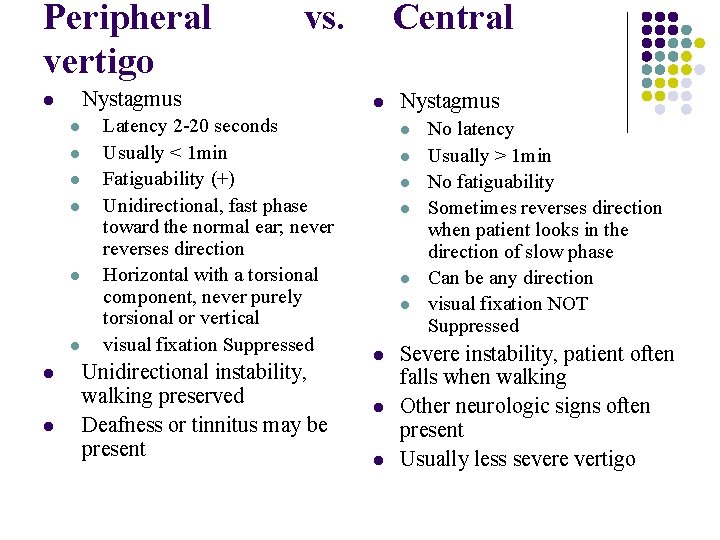
Peripheral vs. Central vertigo Nystagmus l l l l l Latency 2 -20 seconds Usually < 1 min Fatiguability (+) Unidirectional, fast phase toward the normal ear; never reverses direction Horizontal with a torsional component, never purely torsional or vertical visual fixation Suppressed Unidirectional instability, walking preserved Deafness or tinnitus may be present l Nystagmus l l l l l No latency Usually > 1 min No fatiguability Sometimes reverses direction when patient looks in the direction of slow phase Can be any direction visual fixation NOT Suppressed Severe instability, patient often falls when walking Other neurologic signs often present Usually less severe vertigo
Other “dizziness”
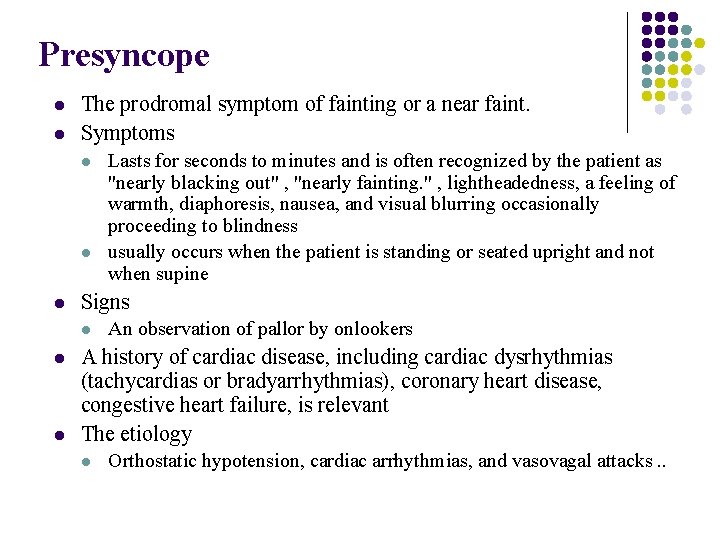
Presyncope l l The prodromal symptom of fainting or a near faint. Symptoms l l l Signs l l l Lasts for seconds to minutes and is often recognized by the patient as "nearly blacking out" , "nearly fainting. " , lightheadedness, a feeling of warmth, diaphoresis, nausea, and visual blurring occasionally proceeding to blindness usually occurs when the patient is standing or seated upright and not when supine An observation of pallor by onlookers A history of cardiac disease, including cardiac dysrhythmias (tachycardias or bradyarrhythmias), coronary heart disease, congestive heart failure, is relevant The etiology l Orthostatic hypotension, cardiac arrhythmias, and vasovagal attacks. .
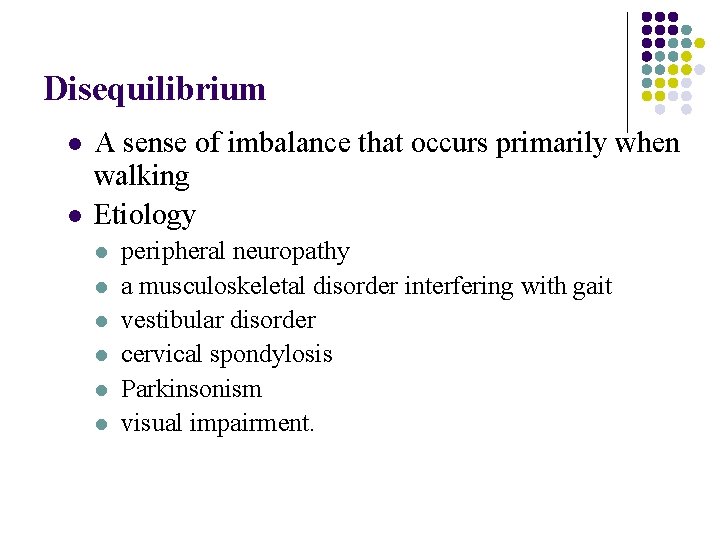
Disequilibrium l l A sense of imbalance that occurs primarily when walking Etiology l l l peripheral neuropathy a musculoskeletal disorder interfering with gait vestibular disorder cervical spondylosis Parkinsonism visual impairment.
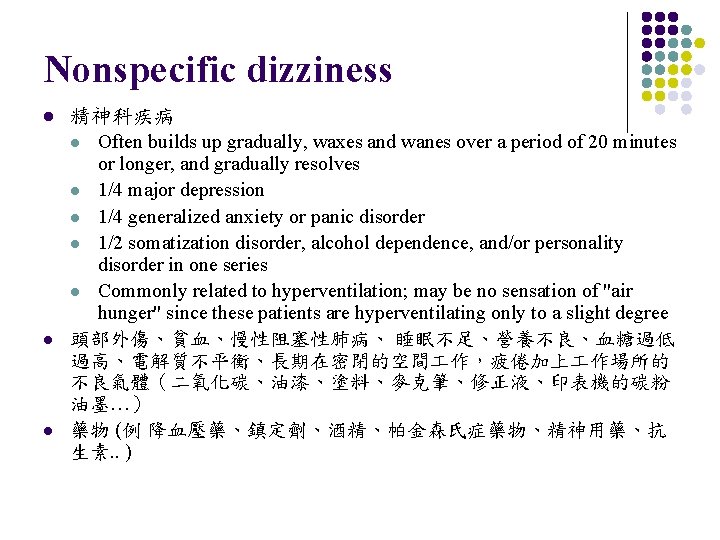
Nonspecific dizziness l l l 精神科疾病 l Often builds up gradually, waxes and wanes over a period of 20 minutes or longer, and gradually resolves l 1/4 major depression l 1/4 generalized anxiety or panic disorder l 1/2 somatization disorder, alcohol dependence, and/or personality disorder in one series l Commonly related to hyperventilation; may be no sensation of "air hunger" since these patients are hyperventilating only to a slight degree 頭部外傷、貧血、慢性阻塞性肺病、 睡眠不足、營養不良、血糖過低 過高、電解質不平衡、長期在密閉的空間 作,疲倦加上 作場所的 不良氣體(二氧化碳、油漆、塗料、麥克筆、修正液、印表機的碳粉 油墨…) 藥物 (例 降血壓藥、鎮定劑、酒精、帕金森氏症藥物、精神用藥、抗 生素. . )
Approach patients with dizziness
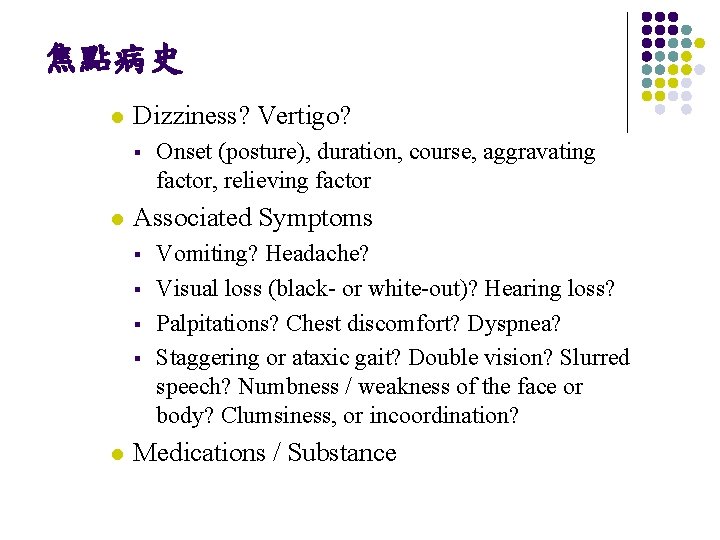
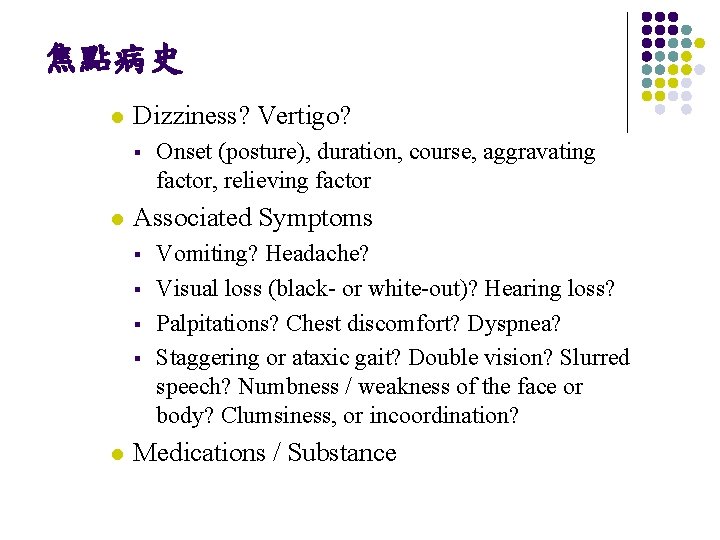
焦點病史 l Dizziness? Vertigo? § l Associated Symptoms § § l Onset (posture), duration, course, aggravating factor, relieving factor Vomiting? Headache? Visual loss (black- or white-out)? Hearing loss? Palpitations? Chest discomfort? Dyspnea? Staggering or ataxic gait? Double vision? Slurred speech? Numbness / weakness of the face or body? Clumsiness, or incoordination? Medications / Substance
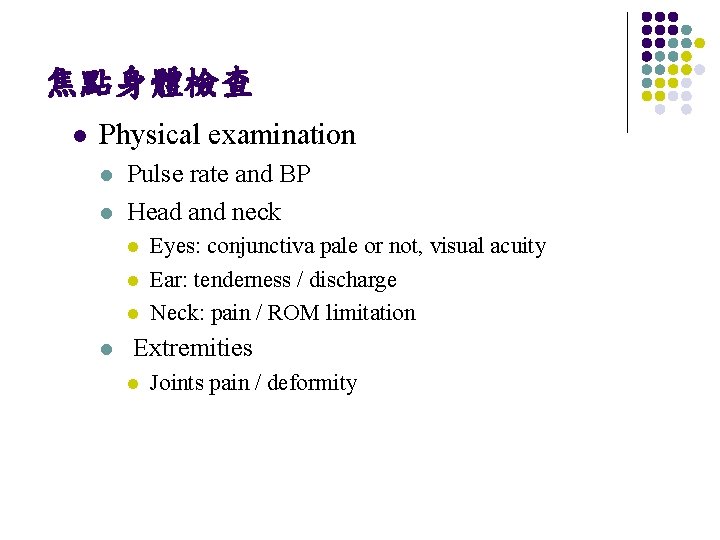
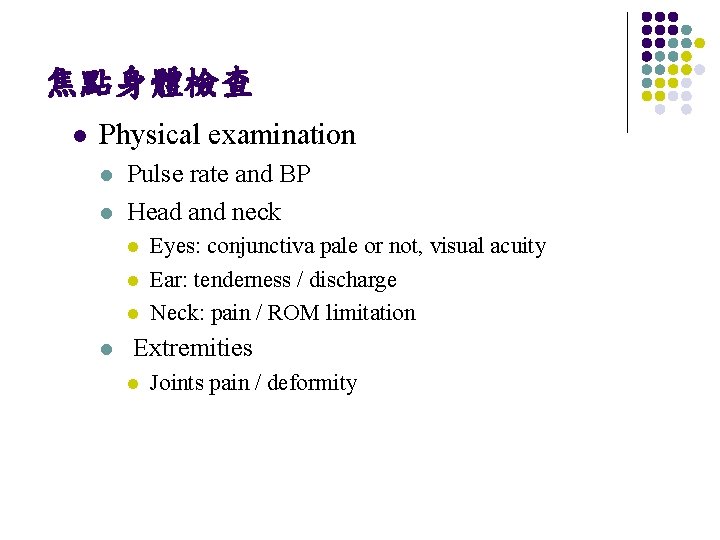
焦點身體檢查 l Physical examination l l Pulse rate and BP Head and neck l l Eyes: conjunctiva pale or not, visual acuity Ear: tenderness / discharge Neck: pain / ROM limitation Extremities l Joints pain / deformity
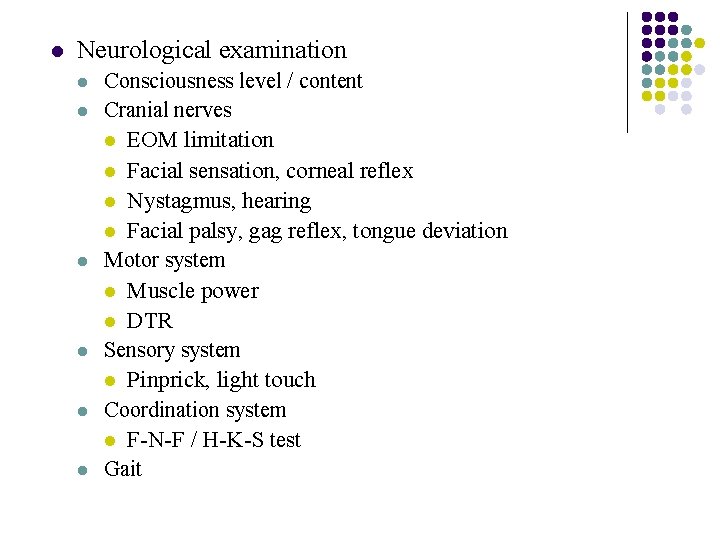
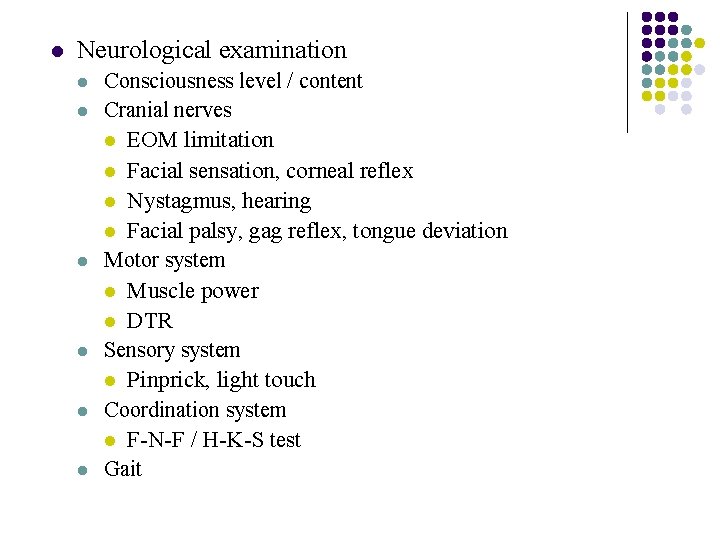
l Neurological examination l l l Consciousness level / content Cranial nerves l EOM limitation l Facial sensation, corneal reflex l Nystagmus, hearing l Facial palsy, gag reflex, tongue deviation Motor system l Muscle power l DTR Sensory system l Pinprick, light touch Coordination system l F-N-F / H-K-S test Gait
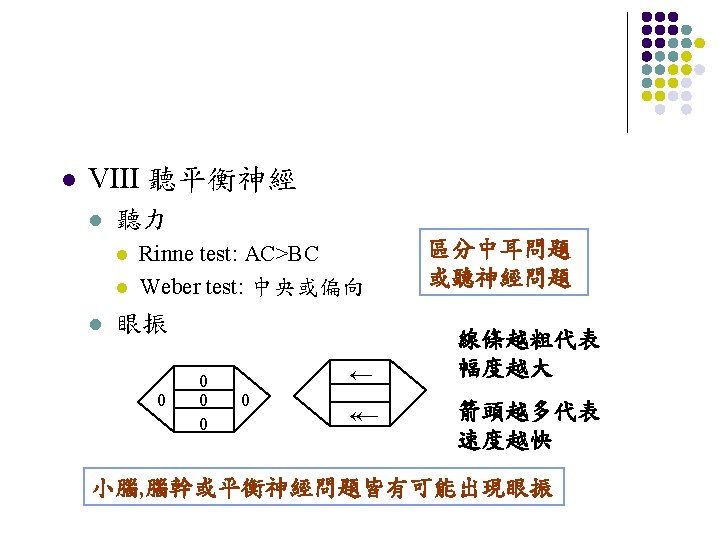
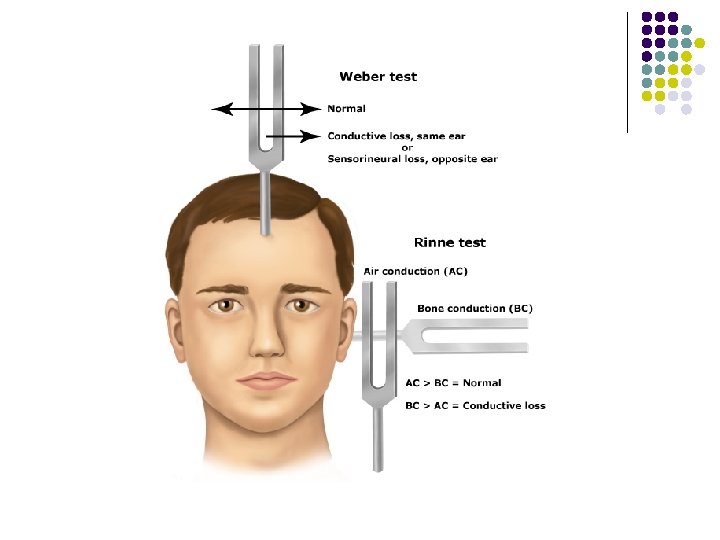
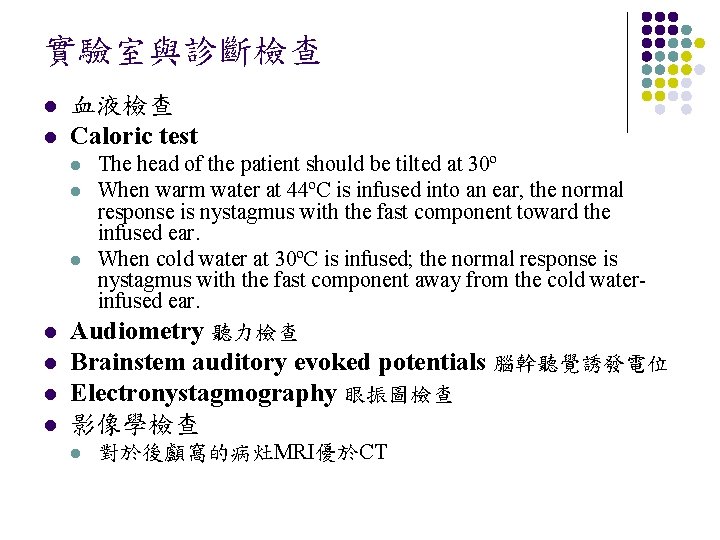
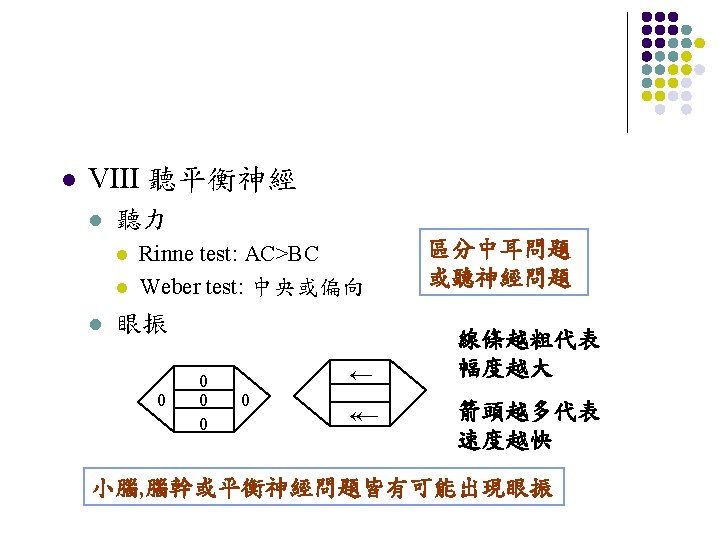
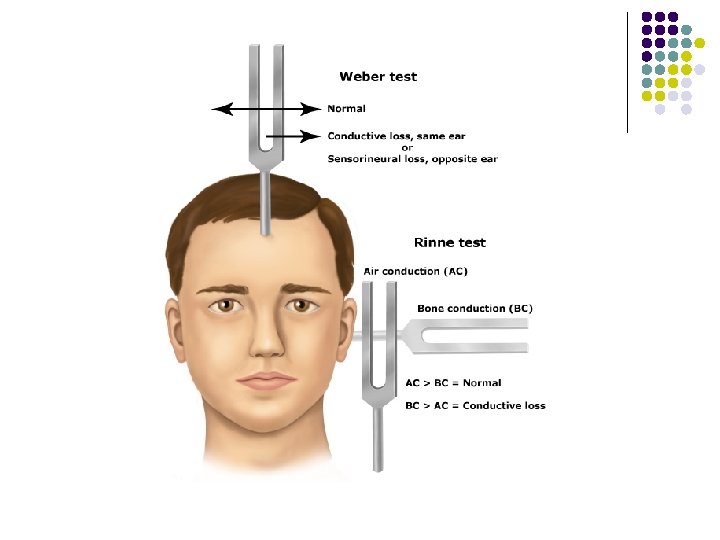
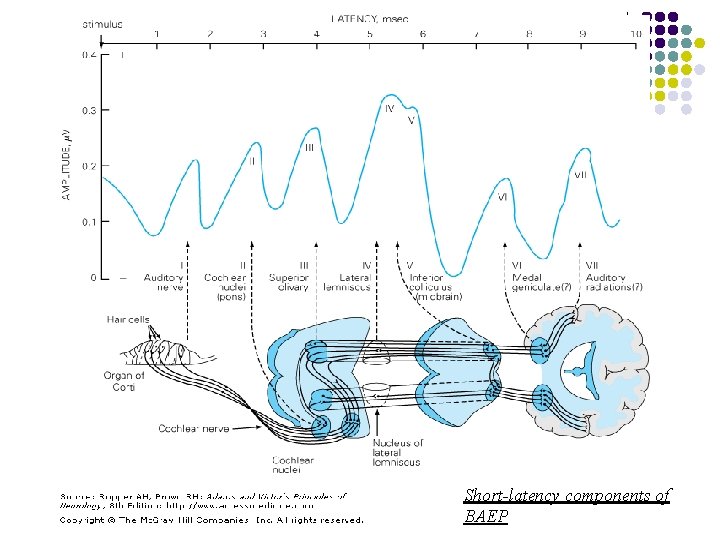
實驗室與診斷檢查 l l 血液檢查 Caloric test The head of the patient should be tilted at 30º l When warm water at 44ºC is infused into an ear, the normal response is nystagmus with the fast component toward the infused ear. l When cold water at 30ºC is infused; the normal response is nystagmus with the fast component away from the cold waterinfused ear. l Audiometry 聽力檢查 l Brainstem auditory evoked potentials 腦幹聽覺誘發電位 l Electronystagmography 眼振圖檢查 l l 影像學檢查 l 對於後顱窩的病灶MRI優於CT
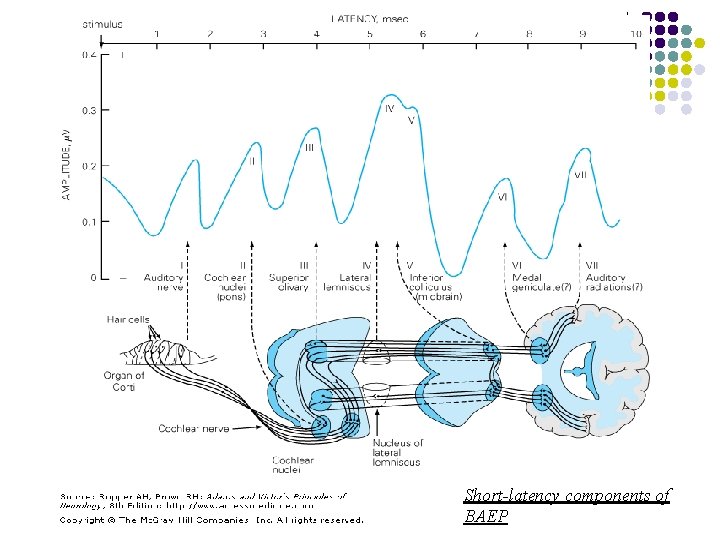
Short-latency components of BAEP
Dizziness- Cases discussion
CASE 1 65 y/o male, DM and H/T poor control l l Acute vertigo and unsteadiness since yesterday morning (noted while getting up) Tend to deviate to right side while walking Can’t use chopstickes well while eating Right occipital dull headache (+), nausea(+) l l l No vomiting, no tinnitus No limbs weakness or numbness, no sphincter problem No ottohrea, ear pain, drug usage or significant infection episode LMD Mx ineffective, thus visit our ER
Summary of N. E. l l l Hearing normal Gaze-evoked nystagmus, fast phase to left side Normal muscle power and sensation Right limbs dysmetria and dysdiadochokinesia Tends deviate to right side while standing and walking
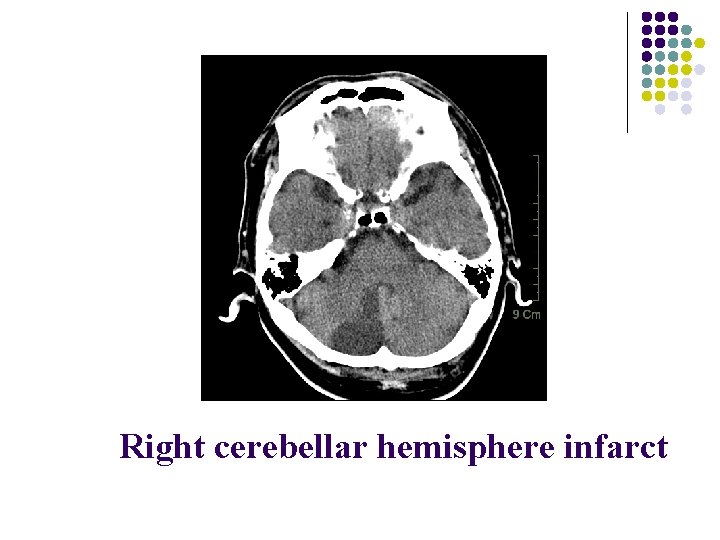
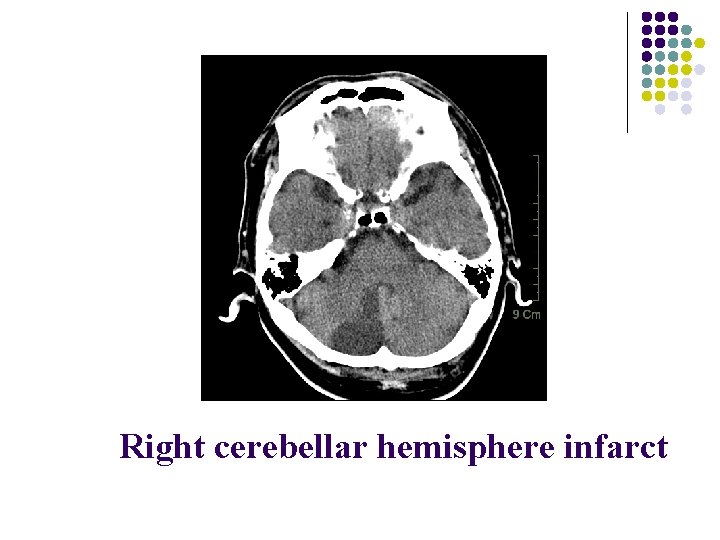
Right cerebellar hemisphere infarct
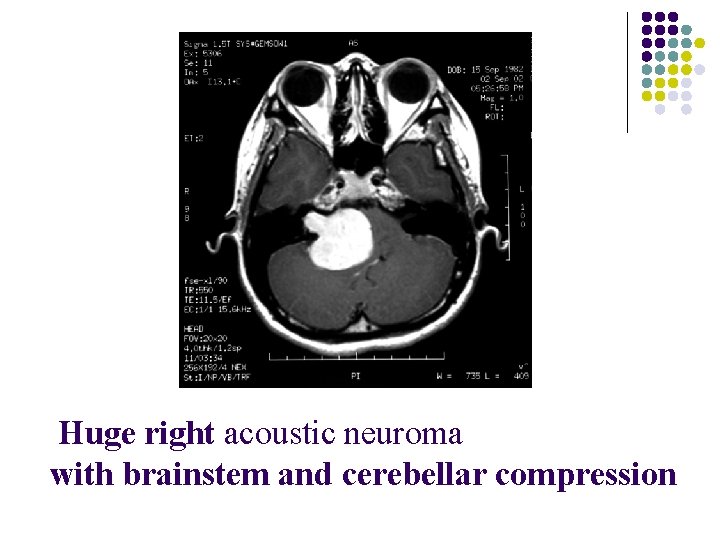
CASE 2 20 y/o female, no significant past history l l l Progressive R’t hearing impairment since about 4 years ago Intermittent vertigo, R’t tinnitus associated with unsteadiness while changing position in recent 1 year, with increasing frequency Mouth angle deviate to L’t, mild slurred speech and occasional choking in recent 1 month l l l Denied facial numbness and double vision No limbs weakness or numbness, no sphincter problem No ottohrea, ear pain, drug usage or significant infection episode
Summary of N. E. l Cranial nerves involvement R’t Facial (VII) nerve palsy R’t Vestibulocochlear (VIII) nerve 0 0 l Suspicious Cr. N IX, X involvement (according to history) l No obvious pyramidal system involvement
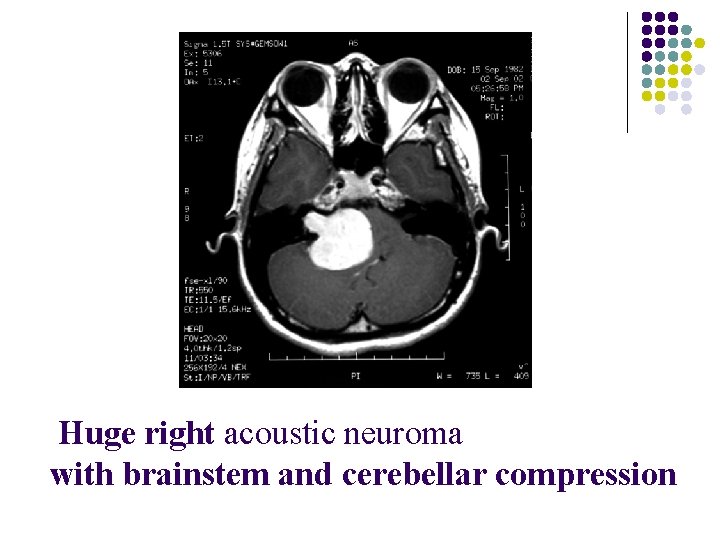
Huge right acoustic neuroma with brainstem and cerebellar compression
Thanks For Your Attention ~