Patient Centered Medical Home Halifax Health Family Medicine






- Slides: 30
Patient Centered Medical Home Halifax Health Family Medicine Residency Faculty Development Workshop
GOALS Ø Explain the rationale for a PCMH Ø Define the characteristics of a PCMH Ø List the ways that we’re currently functioning as a PCMH Ø Identify opportunities for improvement Ø Initiate a process for PCMH certification
History of the PCMH Concept Introduced by American Academy of Pediatrics (AAP) in 1967 Ø Initially referred to a central location for medical records Ø The medical home concept was expanded in 2002 to include: Ø l l l l Accessible Continuous Comprehensive Family-centered Coordinated Compassionate Culturally sensitive care

History of the PCMH Concept Ø In 2007, the AAP, the American Academy of Family Physicians (AAFP), the American Osteopathic Association (AOA), and the American College of Physicians (ACP) adopted a set of joint principles to describe a new level of primary care.
Joint Principles of the Patient Centered Medical Home Ø Ø Ø Ø A personal physician who coordinates all care for patients and leads the team. Physician-directed medical practice – a coordinated team of professionals who work together to care for patients. Whole person orientation – this approach is key to providing comprehensive care. Coordinated care that incorporates all components of the complex health care system. Quality and safety – medical practices voluntarily engage in quality improvement activities to ensure patient safety is always being met. Enhanced access to care – such as through open-access scheduling and communication mechanisms. Payment – a system of reimbursement reflective of the true value of coordinated care and innovation.
Does it Work? Ø Where is the Evidence ?
NCQA Ø The National Committee for Quality Assurance is a private, 501(c)(3) not-forprofit organization dedicated to improving health care quality.
NCQA’s New Medical Home Standards Ø Ø Ø Emphasis on patient-centeredness and patient experience of care Reinforces incentives for meaningful use (HIT) Focuses attention on aspects of primary care that improve quality and reduce cost Based on advances in evidence and changes in practice capability
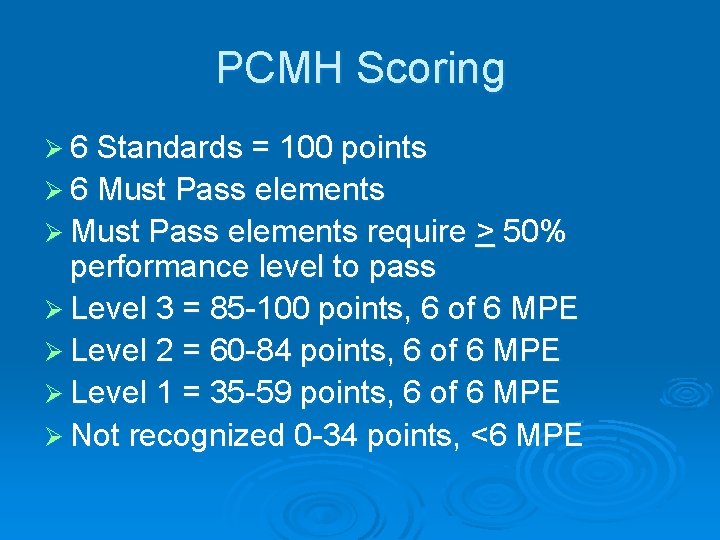
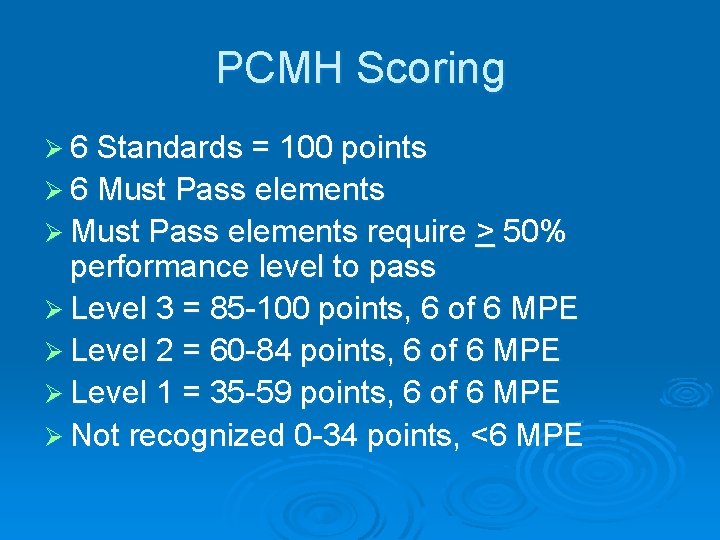
PCMH Scoring Ø 6 Standards = 100 points Ø 6 Must Pass elements Ø Must Pass elements require > 50% performance level to pass Ø Level 3 = 85 -100 points, 6 of 6 MPE Ø Level 2 = 60 -84 points, 6 of 6 MPE Ø Level 1 = 35 -59 points, 6 of 6 MPE Ø Not recognized 0 -34 points, <6 MPE
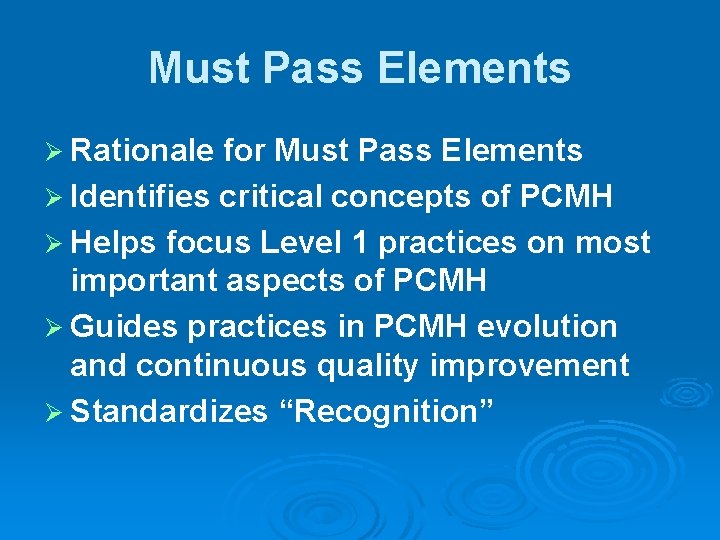
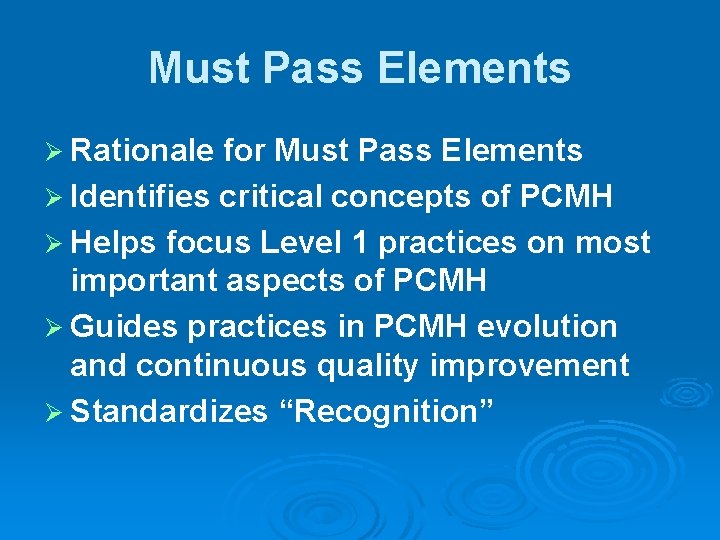
Must Pass Elements Ø Rationale for Must Pass Elements Ø Identifies critical concepts of PCMH Ø Helps focus Level 1 practices on most important aspects of PCMH Ø Guides practices in PCMH evolution and continuous quality improvement Ø Standardizes “Recognition”

Must Pass Elements 1 A: Access During Office Hours 2 D: Use Data for Population Management 3 C: Manage Care 4 A: Self-Care Process 5 B: Referral Tracking and Follow-Up 6 C: Implement Continuous Quality improvement Ø Possible Must Pass Points = 14. 5 points (50% of score) to 29 points (100 %) Ø
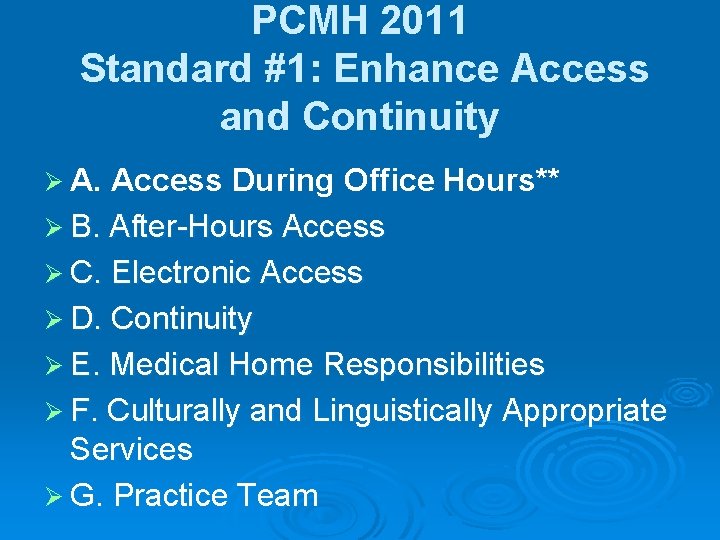
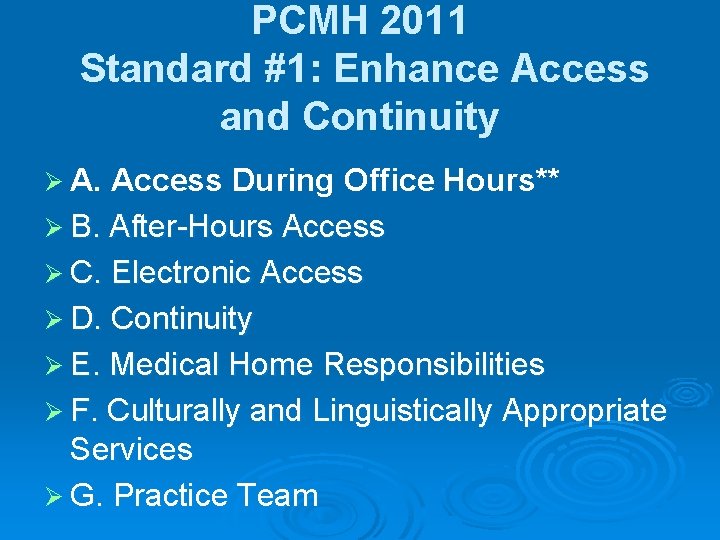
PCMH 2011 Standard #1: Enhance Access and Continuity Ø A. Access During Office Hours** Ø B. After-Hours Access Ø C. Electronic Access Ø D. Continuity Ø E. Medical Home Responsibilities Ø F. Culturally and Linguistically Appropriate Services Ø G. Practice Team
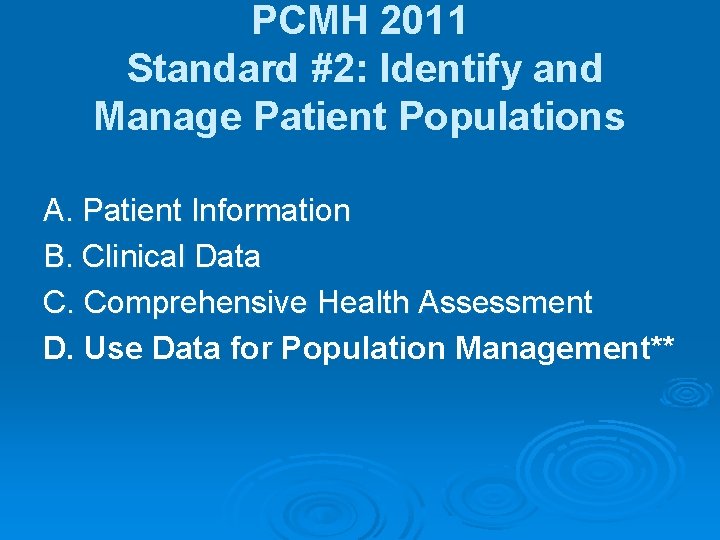
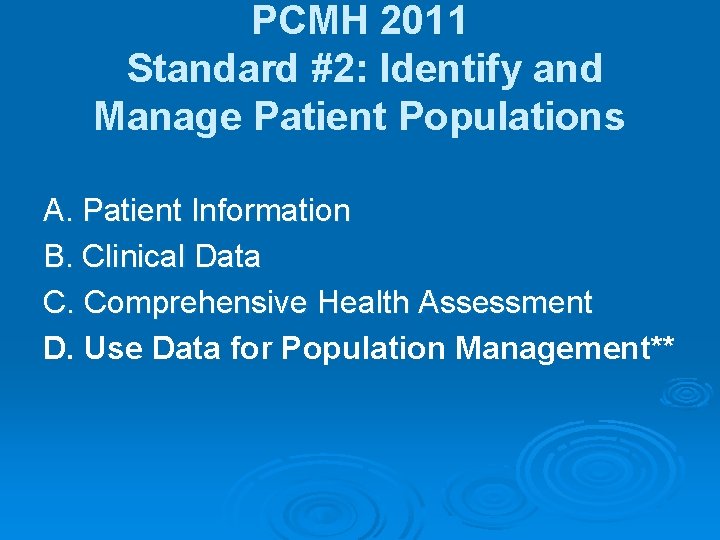
PCMH 2011 Standard #2: Identify and Manage Patient Populations A. Patient Information B. Clinical Data C. Comprehensive Health Assessment D. Use Data for Population Management**
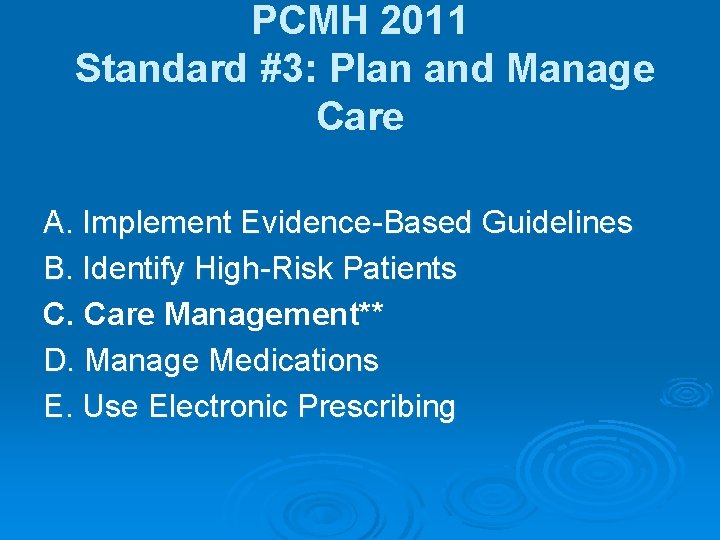
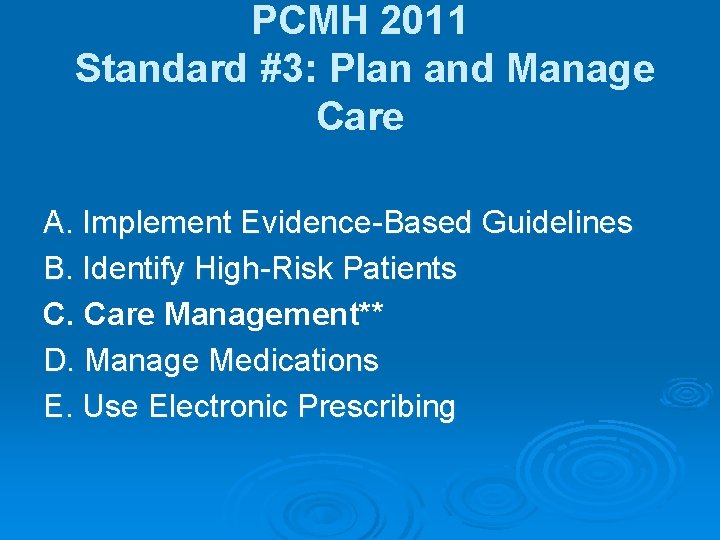
PCMH 2011 Standard #3: Plan and Manage Care A. Implement Evidence-Based Guidelines B. Identify High-Risk Patients C. Care Management** D. Manage Medications E. Use Electronic Prescribing

PCMH 2011 Standard #4: Provide Self-Care Support and Community Resources A. Support Self-Care Process** B. Provide Referrals to Community Resources
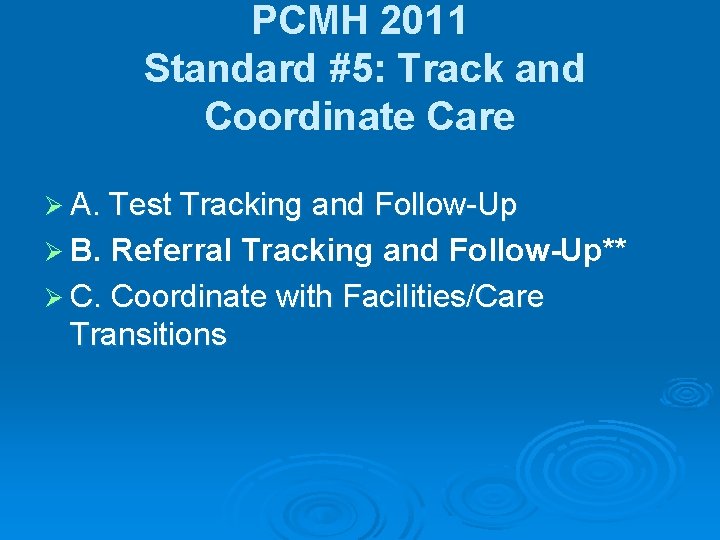
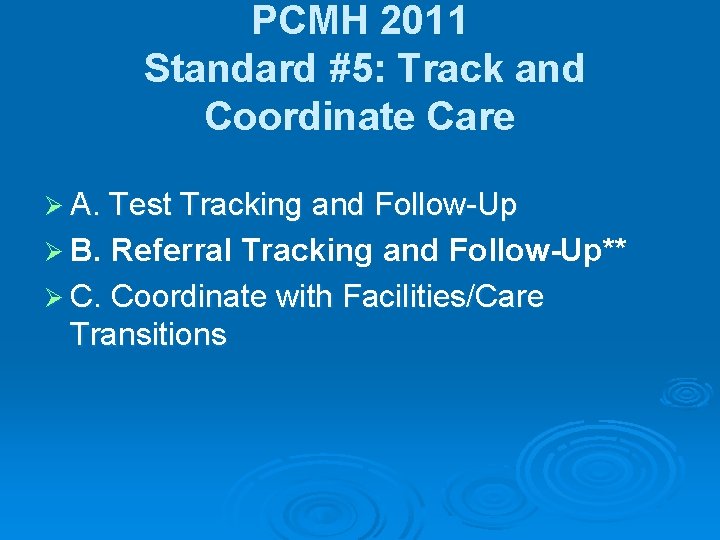
PCMH 2011 Standard #5: Track and Coordinate Care Ø A. Test Tracking and Follow-Up Ø B. Referral Tracking and Follow-Up** Ø C. Coordinate with Facilities/Care Transitions
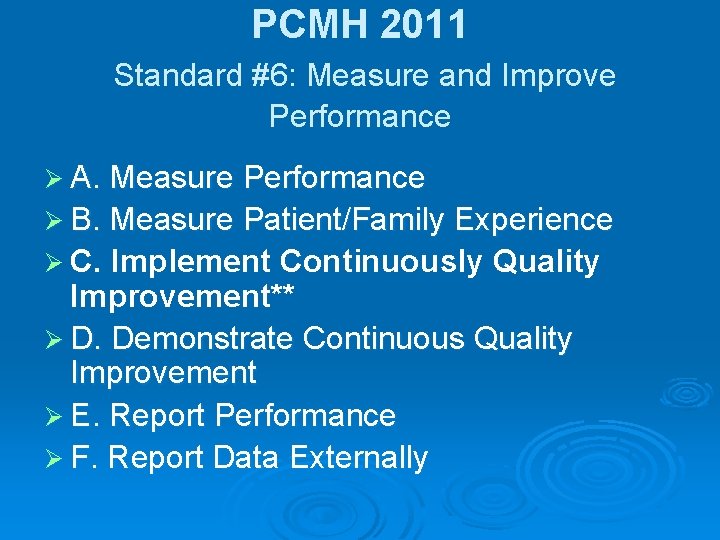
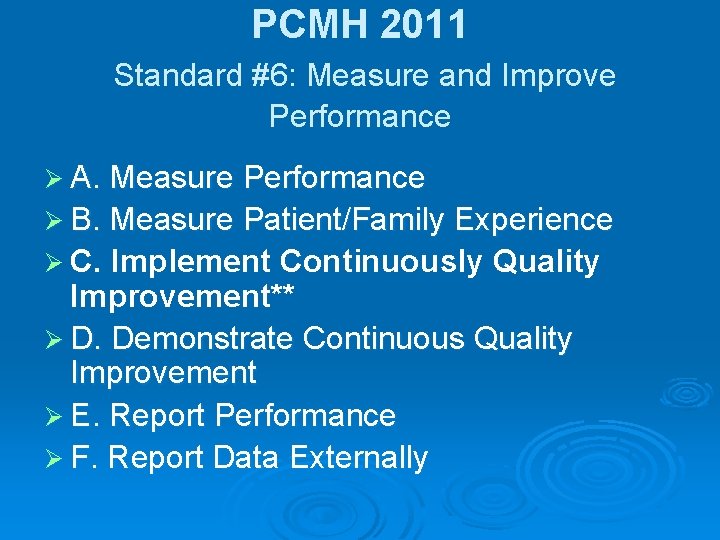
PCMH 2011 Standard #6: Measure and Improve Performance Ø A. Measure Performance Ø B. Measure Patient/Family Experience Ø C. Implement Continuously Quality Improvement** Ø D. Demonstrate Continuous Quality Improvement Ø E. Report Performance Ø F. Report Data Externally
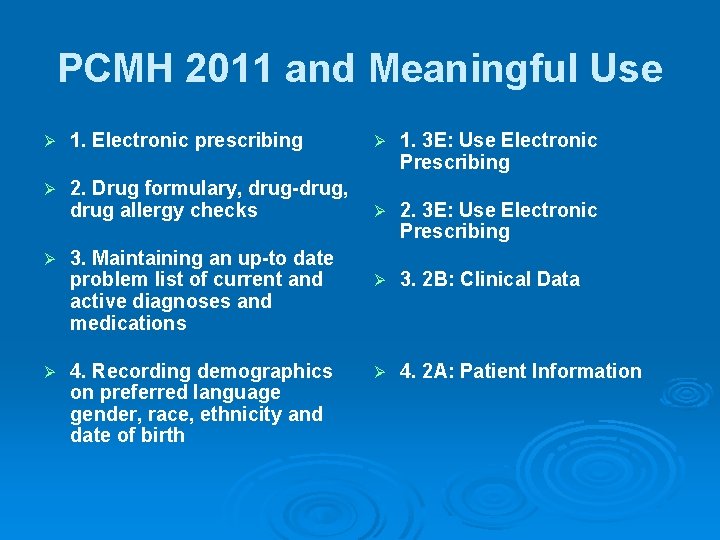
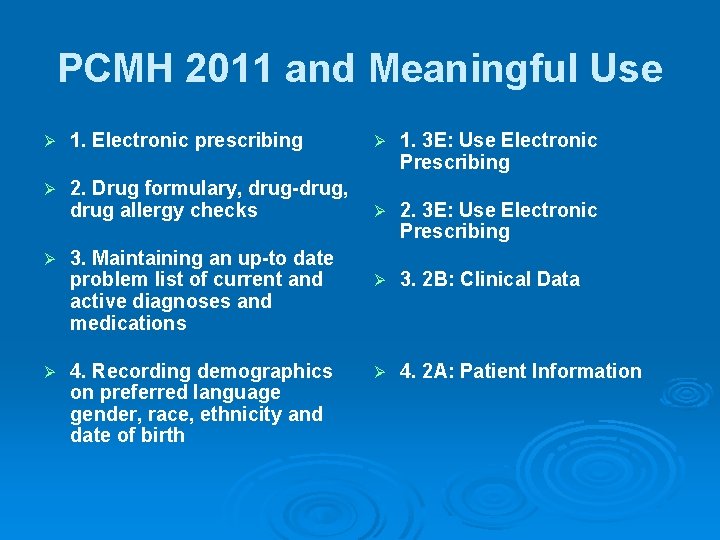
PCMH 2011 and Meaningful Use Ø 1. Electronic prescribing Ø 1. 3 E: Use Electronic Prescribing Ø 2. Drug formulary, drug-drug, drug allergy checks Ø 2. 3 E: Use Electronic Prescribing Ø 3. 2 B: Clinical Data Ø 4. 2 A: Patient Information Ø Ø 3. Maintaining an up-to date problem list of current and active diagnoses and medications 4. Recording demographics on preferred language gender, race, ethnicity and date of birth
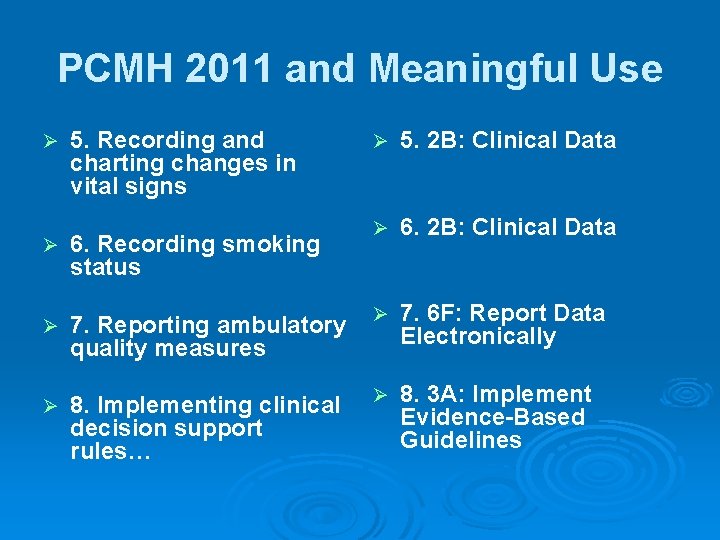
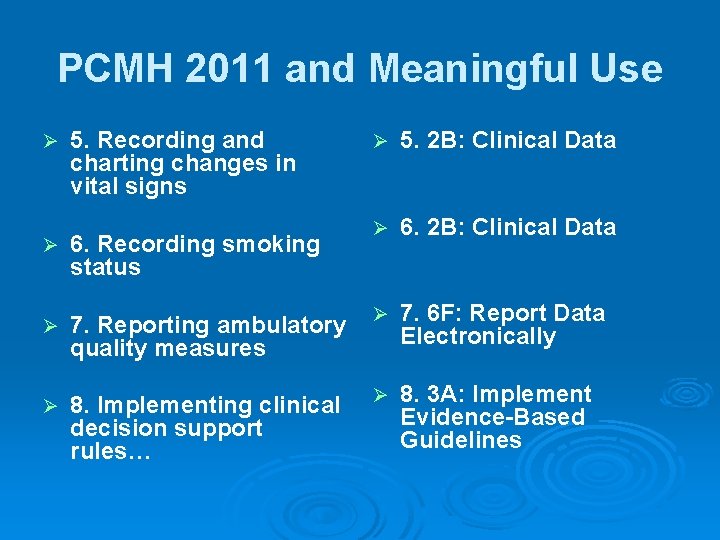
PCMH 2011 and Meaningful Use Ø 5. Recording and charting changes in vital signs Ø 5. 2 B: Clinical Data Ø 6. Recording smoking status Ø 7. Reporting ambulatory quality measures Ø 7. 6 F: Report Data Electronically Ø 8. Implementing clinical decision support rules… Ø 8. 3 A: Implement Evidence-Based Guidelines

NCQA Recognition Ø Where do we start?
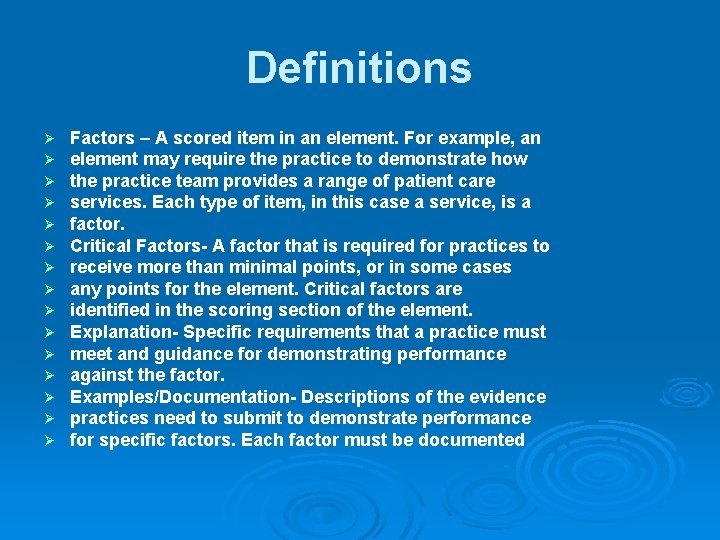
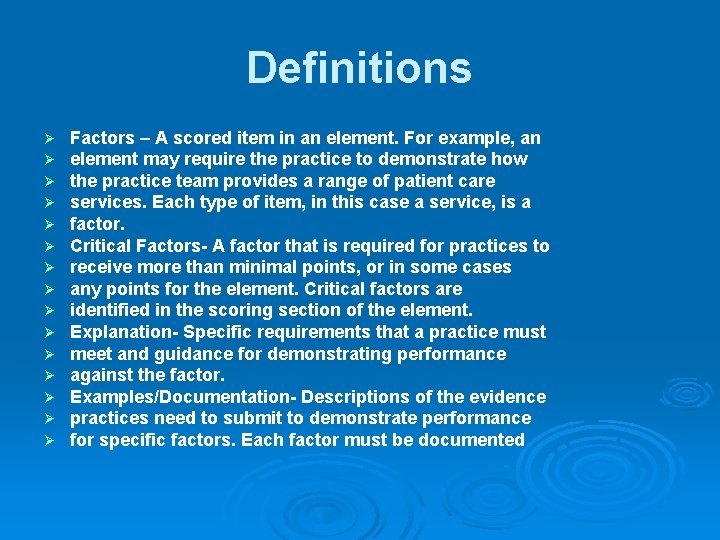
Definitions Ø Ø Ø Ø Factors – A scored item in an element. For example, an element may require the practice to demonstrate how the practice team provides a range of patient care services. Each type of item, in this case a service, is a factor. Critical Factors- A factor that is required for practices to receive more than minimal points, or in some cases any points for the element. Critical factors are identified in the scoring section of the element. Explanation- Specific requirements that a practice must meet and guidance for demonstrating performance against the factor. Examples/Documentation- Descriptions of the evidence practices need to submit to demonstrate performance for specific factors. Each factor must be documented
NCQA Standards Ø Standard 1: Access and Communication A. Has written standards for patient access and patient communication B. Uses data to show it meets its standards for patient access and communication
NCQA Standards Ø Standard 2: Patient Tracking and Registry Functions A. Uses data system for basic patient information B. Has clinical data system with clinical data in searchable data fields C. Uses the clinical data system D. Uses paper or electronic-based charting tools to organize clinical information E. Uses data to identify important diagnoses and conditions in practice F. Generates lists of patients and reminds patients and clinicians of services needed (population management)
NCQA Standards Ø Standard 3: Care Management A. Adopts and implements evidence-based guidelines for three conditions B. Generates reminders about preventive services for clinicians C. Uses non-physician staff to manage patient care addressing progress, addressing barriers D. Conducts care management, including care plans, assessing progress, addressing barriers E. Coordinates care, follow-up for patients who receive care in inpatient and outpatient facilities

NCQA Standards Ø Standard 4: Patient Self-Management Support A. Assesses language preference and other communication barriers B. Actively supports patient selfmanagement
NCQA Standards Ø Standard 5: Electronic Prescribing A. Uses electronic system to write prescriptions B. Has electronic prescription writer with safety checks C. Has electronic prescription writer with cost checks

NCQA Standards Ø Standard 6: Test Tracking A. Tracks tests and identifies abnormal results systematically B. Uses electronic systems to order and retrieve tests and flag duplicate tests
NCQA Standards Ø Standard 7: Referral Tracking A. Tracks referrals using paper-based or electronic system
NCQA Standards Ø Standard 8: Performance Reporting and Improvement A. Measures clinical and/or service performance by physician or across the practice B. Survey of patients’ care experience C. Reports performance for the practice or the physician D. Sets goals and takes action to improve performance E. Produces reports using standardized measures F. Transmits reports with standardized measures electronically to external entities
NCQA Standards Ø Standard 9: Advanced Electronic Communications A. Availability of Interactive Website B. Electronic Patient Identification C. Electronic Care Management Support
 Patient centered medical home conference
Patient centered medical home conference Patient centered medical home
Patient centered medical home Halifax family medicine residency
Halifax family medicine residency Stock image
Stock image Meritus definition
Meritus definition Qsen project examples
Qsen project examples Patient centered primary care collaborative
Patient centered primary care collaborative Patient centered primary care collaborative
Patient centered primary care collaborative Patient centered care
Patient centered care Duke medicine grand rounds
Duke medicine grand rounds Strategies of family centered care
Strategies of family centered care Family centered care definition
Family centered care definition Patient 2 patient
Patient 2 patient The art of medicine consists of amusing the patient meaning
The art of medicine consists of amusing the patient meaning Mobile dispensing unit in pharmacy
Mobile dispensing unit in pharmacy Learn french halifax
Learn french halifax Comfort keepers halifax
Comfort keepers halifax Halifax west course selection
Halifax west course selection French immersion school halifax
French immersion school halifax Gulf of mexico pipeline rupture
Gulf of mexico pipeline rupture Eating disorder clinic halifax
Eating disorder clinic halifax Southeast halifax high school
Southeast halifax high school Halifax ctf
Halifax ctf North halifax grammar school
North halifax grammar school Halifax explosion definition
Halifax explosion definition Cupe 5047 collective agreement
Cupe 5047 collective agreement Halifax resolves definition
Halifax resolves definition Preoperative medical evaluation of the healthy patient
Preoperative medical evaluation of the healthy patient Heaton moor medical centre doctors
Heaton moor medical centre doctors Chafford hundred medical center
Chafford hundred medical center Apa arti home care
Apa arti home care