Putting the Patient in the Patient Centered Medical



- Slides: 43
Putting the Patient in the Patient Centered Medical Home Joseph E. Scherger, MD, MPH November 7, 2009
What Is a Patient-Centered Medical Home? n A Patient-Centered Medical Home (PCMH) is a model for care provided by physician practices that seeks to strengthen the physician-patient relationship by replacing episodic care based on illnesses and patient complaints with coordinated care and a long -term healing relationship (NCQA). Adapted from Joint Principles of the Patient-Centered Medical Home, March 2007. Available at: http: //www. aafp. org/online/etc/medialib/aafp_org/documents/policy/fed/jointprinciplespcmh 0207. Par. 0001. File. dat/0221 07 medicalhome. pdf.

The Holy Grail of Health Care 2009 n Cost Reduction n Quality Improvement n Service Improvement
The Secret Sauce for Success n Care becomes continuous access rather than episodic n Care becomes proactive rather than reactive n Patients become activated for selfmanagement
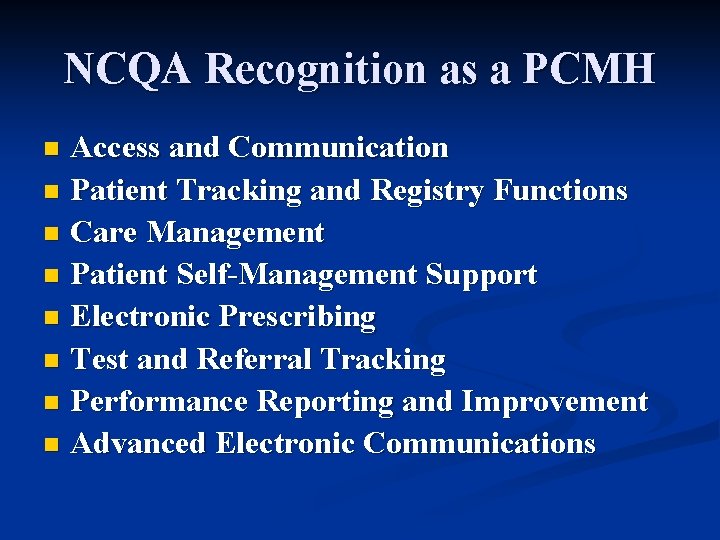
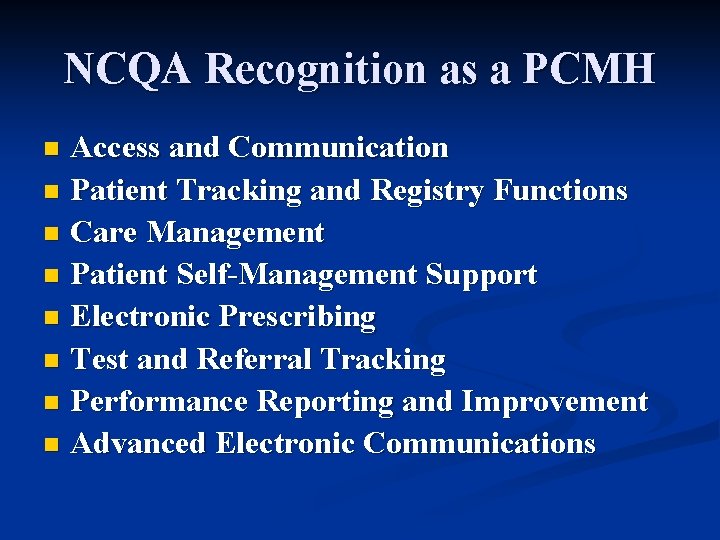
NCQA Recognition as a PCMH Access and Communication n Patient Tracking and Registry Functions n Care Management n Patient Self-Management Support n Electronic Prescribing n Test and Referral Tracking n Performance Reporting and Improvement n Advanced Electronic Communications n
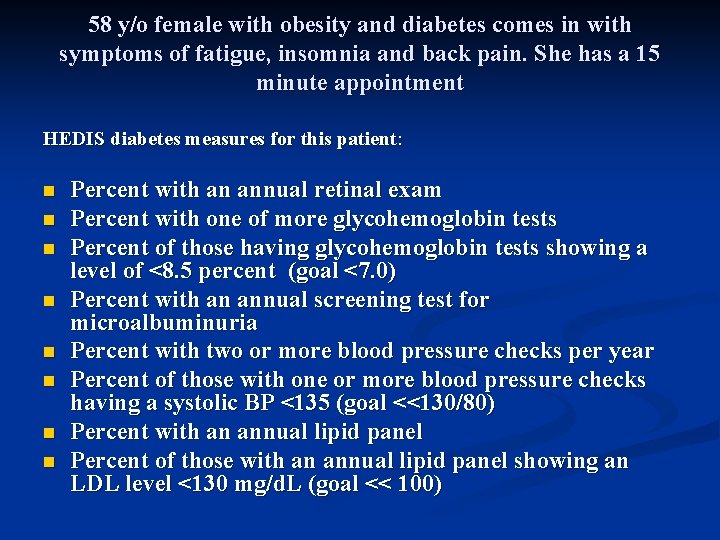
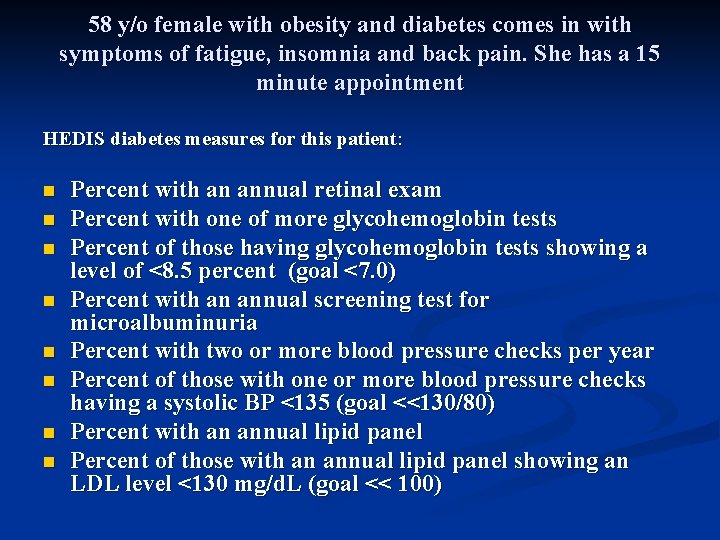
58 y/o female with obesity and diabetes comes in with symptoms of fatigue, insomnia and back pain. She has a 15 minute appointment HEDIS diabetes measures for this patient: n n n n Percent with an annual retinal exam Percent with one of more glycohemoglobin tests Percent of those having glycohemoglobin tests showing a level of <8. 5 percent (goal <7. 0) Percent with an annual screening test for microalbuminuria Percent with two or more blood pressure checks per year Percent of those with one or more blood pressure checks having a systolic BP <135 (goal <<130/80) Percent with an annual lipid panel Percent of those with an annual lipid panel showing an LDL level <130 mg/d. L (goal << 100)
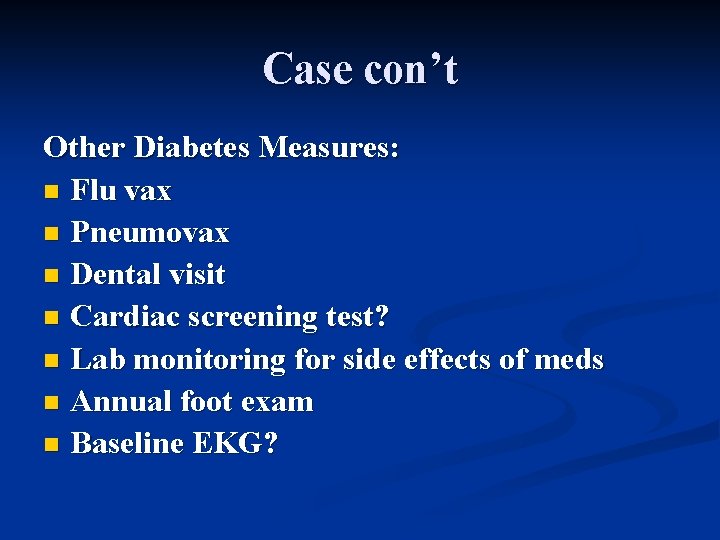
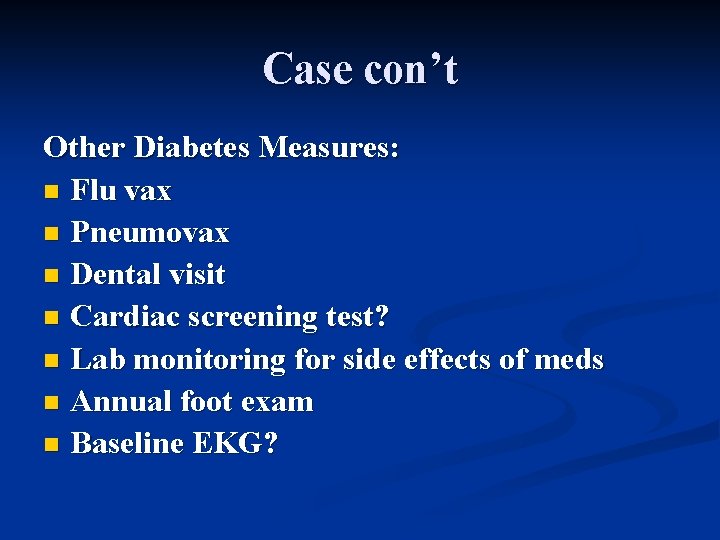
Case con’t Other Diabetes Measures: n Flu vax n Pneumovax n Dental visit n Cardiac screening test? n Lab monitoring for side effects of meds n Annual foot exam n Baseline EKG?
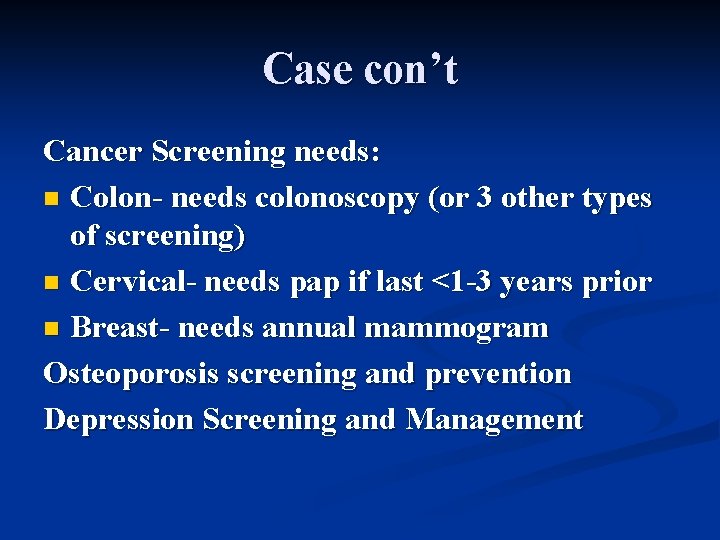
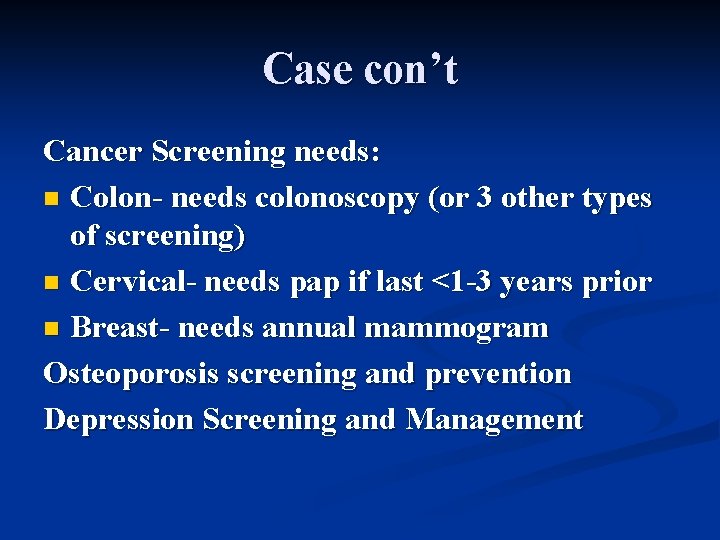
Case con’t Cancer Screening needs: n Colon- needs colonoscopy (or 3 other types of screening) n Cervical- needs pap if last <1 -3 years prior n Breast- needs annual mammogram Osteoporosis screening and prevention Depression Screening and Management
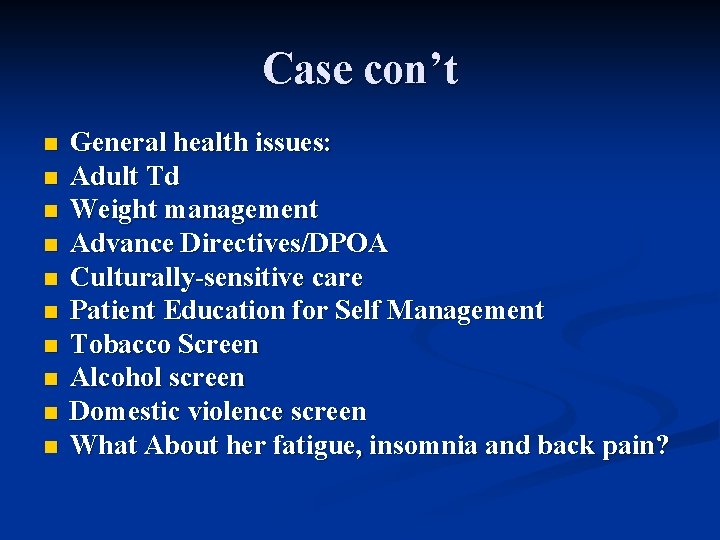
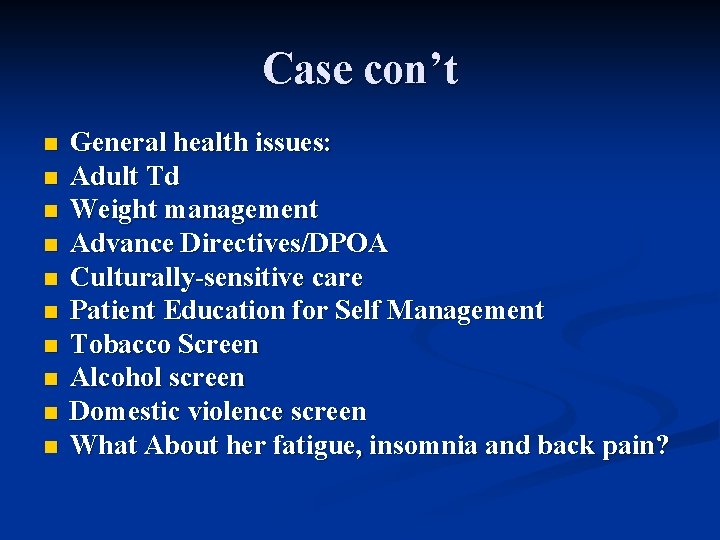
Case con’t n n n n n General health issues: Adult Td Weight management Advance Directives/DPOA Culturally-sensitive care Patient Education for Self Management Tobacco Screen Alcohol screen Domestic violence screen What About her fatigue, insomnia and back pain?
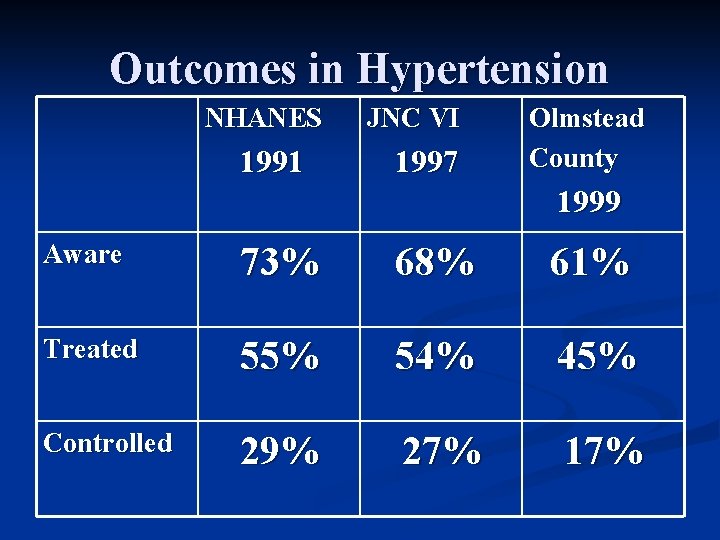
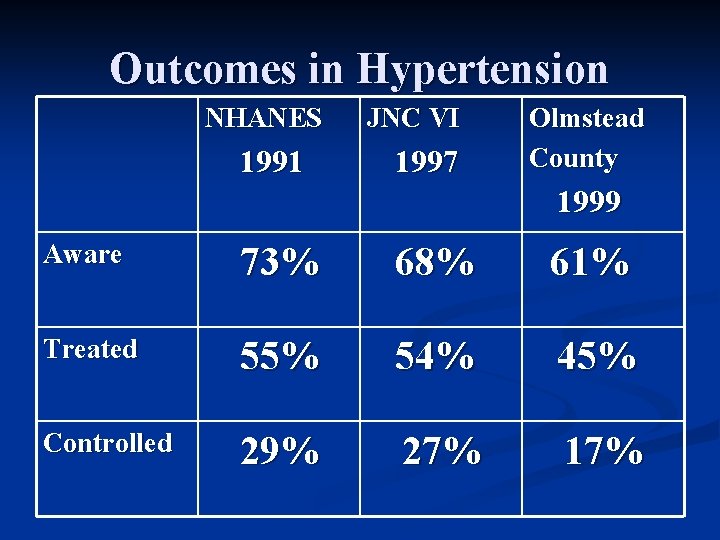
Outcomes in Hypertension NHANES 1991 JNC VI 1997 Olmstead County 1999 Aware 73% 68% 61% Treated 55% 54% 45% Controlled 29% 27% 17%
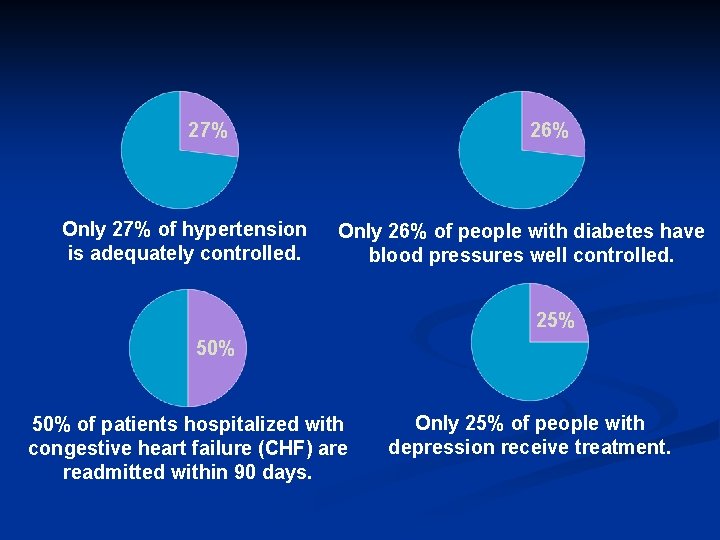
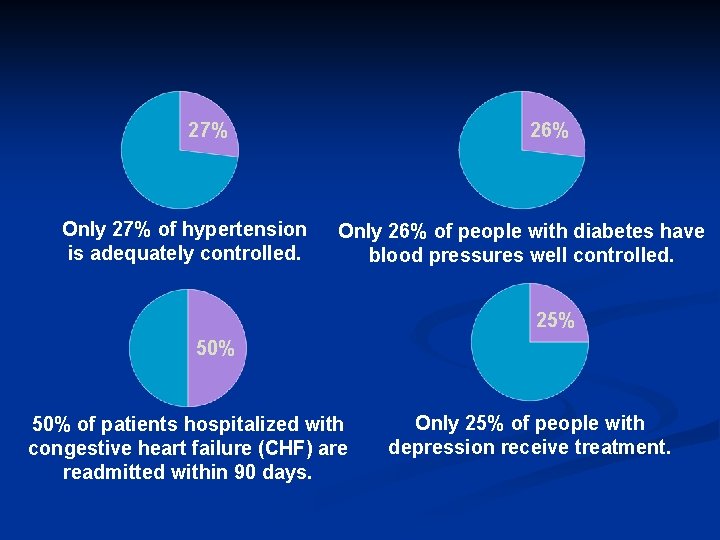
27% Only 27% of hypertension is adequately controlled. 26% Only 26% of people with diabetes have blood pressures well controlled. 25% 50% of patients hospitalized with congestive heart failure (CHF) are readmitted within 90 days. Only 25% of people with depression receive treatment.
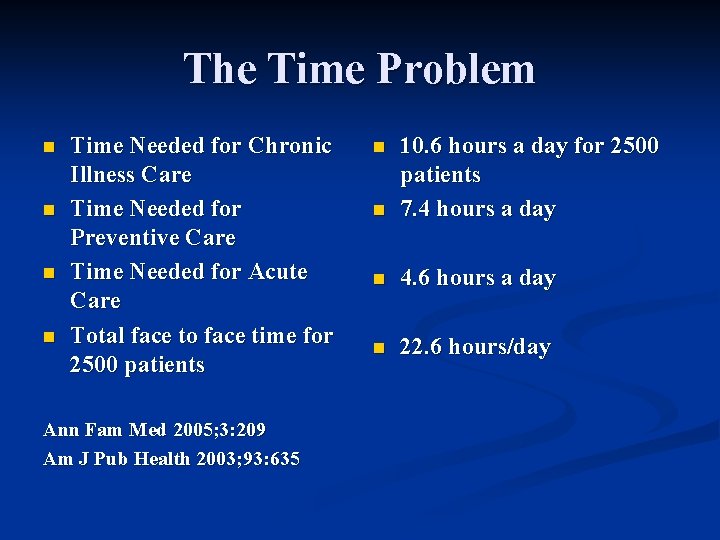
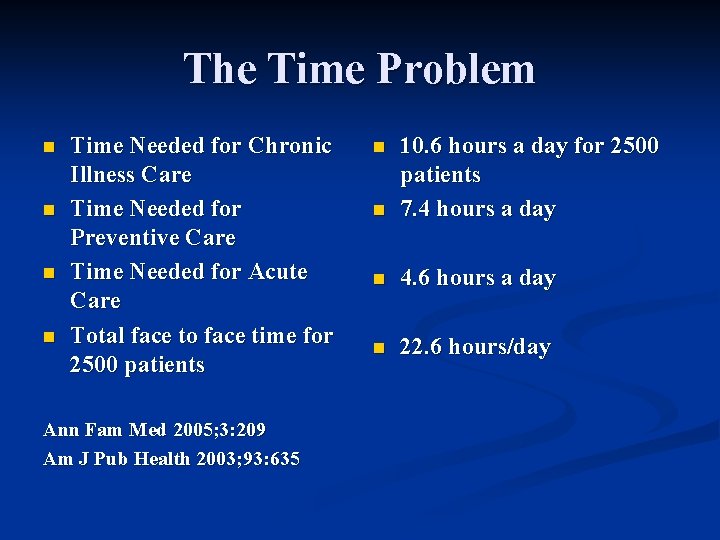
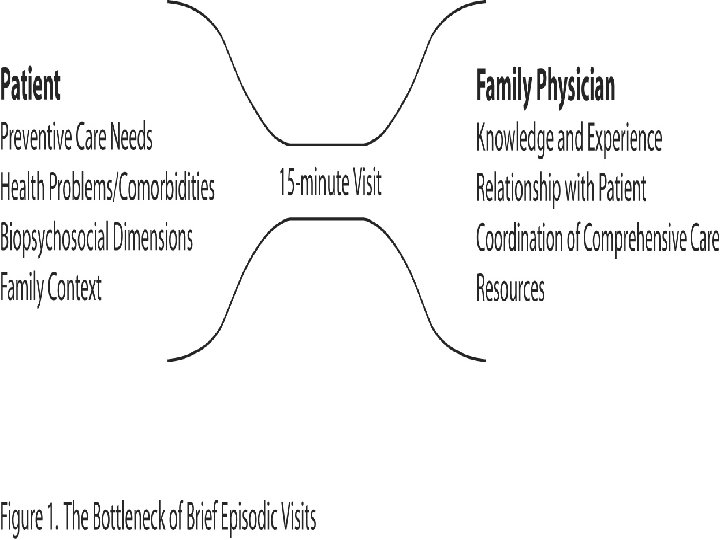
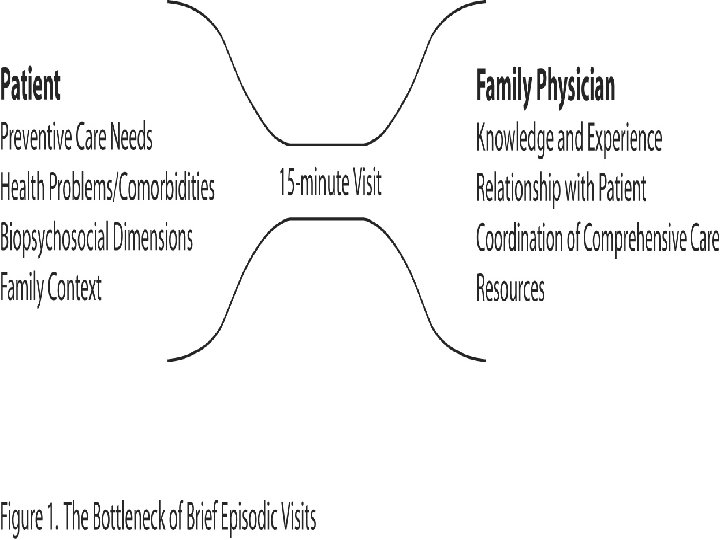
The Time Problem n n Time Needed for Chronic Illness Care Time Needed for Preventive Care Time Needed for Acute Care Total face to face time for 2500 patients Ann Fam Med 2005; 3: 209 Am J Pub Health 2003; 93: 635 n 10. 6 hours a day for 2500 patients 7. 4 hours a day n 4. 6 hours a day n 22. 6 hours/day n
The Ticking Clock in the Doctor’s Office: Patients on routine visits to their primary doctors often have lots of questions but not enough time to get good answers NY Times Feb. 6, 2007
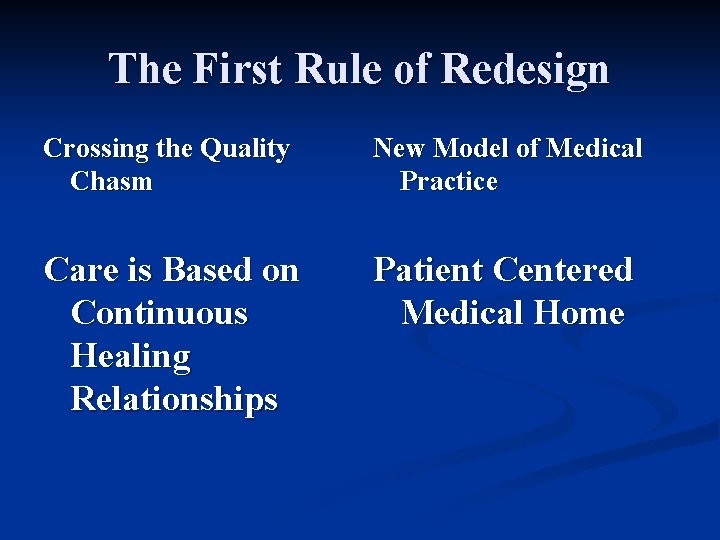
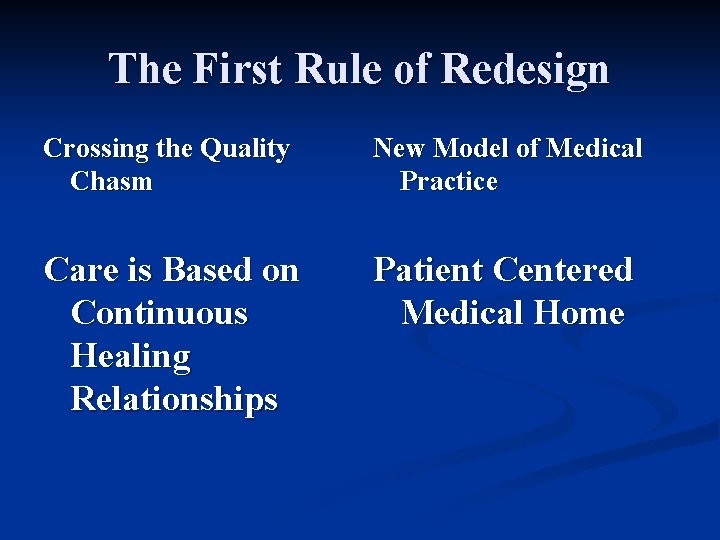
The First Rule of Redesign Crossing the Quality Chasm New Model of Medical Practice Care is Based on Continuous Healing Relationships Patient Centered Medical Home
The Patient’s Life n 6000 hours a year awake n 1350 hours a year making decisions important to diabetes n 2 hours of episodic contact a year with the primary care physician and only urgent access between
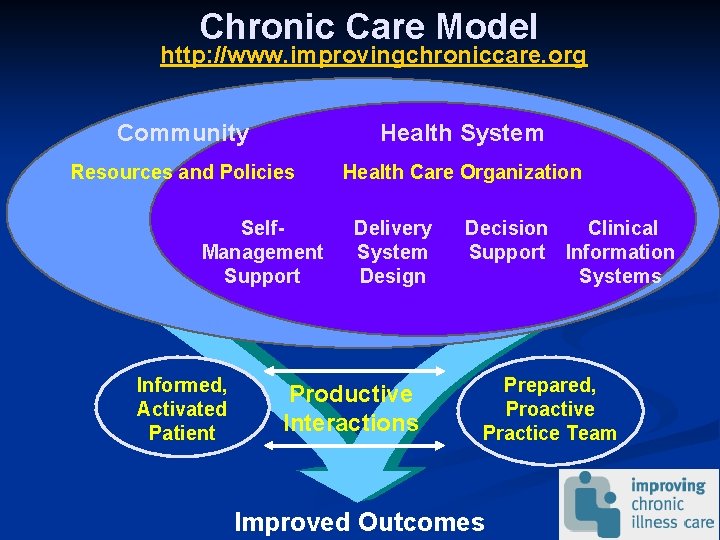
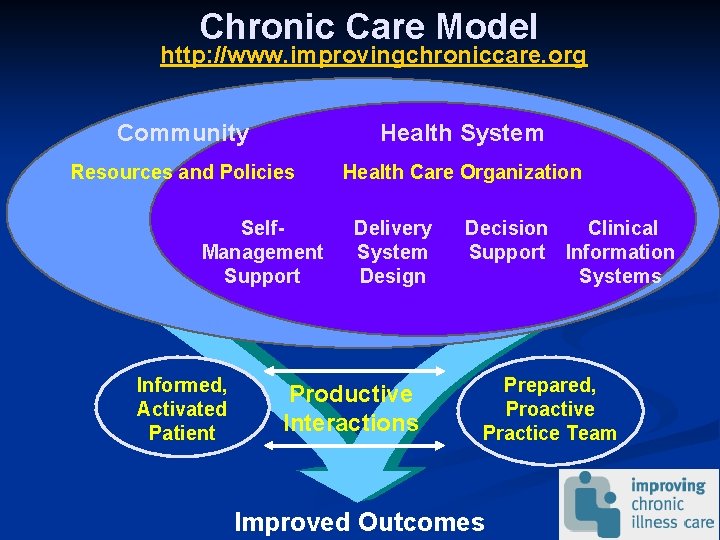
Chronic Care Model http: //www. improvingchroniccare. org Community Health System Resources and Policies Health Care Organization Self. Management Support Informed, Activated Patient Delivery System Design Productive Interactions Decision Clinical Support Information Systems Prepared, Proactive Practice Team Improved Outcomes

Health Care Becomes Continuous n n n Patients Live Their Health and Illnesses Every Day Quality Health Care Offers Continuous Access and Engagement Patients Will Drive the Innovation Patients Will Have Their Medical Records Patients Have Access to All Medical Information – The Return of the Public Library Patients Will Communicate Far and Wide for Care
Stanford Chronic Disease Self. Management Programs n n n Small groups of 10 -16 people People with different diseases in the same group 2 ½ house a week for 6 weeks Peer facilitated Content – symptom management, exercise, nutrition, problem solving, communications, advanced directives Process – self efficacy, action planning, problem solving, sharing
Current Stanford Programs n n n n Chronic Disease Self-Management (English/Spanish with 16 other language translations) Arthritis Self-Management Diabetes Self-Management HIV/AIDS Self-Management Pain Self-Management Cancer Survivor Self-Management All available over the internet
Outcomes of CDSMP n n n Effective across a variety of chronic diseases (randomized trials done) Effective across socioeconomic and education levels – rich international experience Patients can manage progressive and debilitating illness Reduces physician visits, ER visits and hospitalizations Proven consistent results over 3 years Cost of program, $100 -200, Savings $800 -1000 per participant
Physician Engagement is Critical Connection with personal physician the key to success n Physician referral is the most powerful motivator n Integrated physician and self-care critical for the outcomes n
Kaiser Permanente Health. Connect 24 Hour Access to Accurate and Comprehensive Health Care Information and Services
Early Experience Kaiser Northern California n n Build off the self-management research of Kate Lorig and the chronic disease self-management team from Stanford David Sobel – Internist and Medical Director Cohort of patients receive basic education for greater self-management of chronic illness Health Connect platform allows patients to coordinate care with care team
From Patient to Partner: Empowering the Hidden Health Care System David S. Sobel, MD, MPH Medical Director Patient Education and Health Promotion The Permanente Medical Group Northern California
Strategic Questions n n n Where is the excess capacity and underutilized resource within the health care system? Where are the mismatches between patient needs and health care resources that result in ineffective and inefficient care? How can “win-win” solutions be created for consumers, providers, and health care systems?
Strategic Questions What are the active ingredients in effective Self-Management? n If Self-Management is the right thing to do, then why is it often so difficult to initiate, implement and sustain these beneficial interventions … and what can be done? n
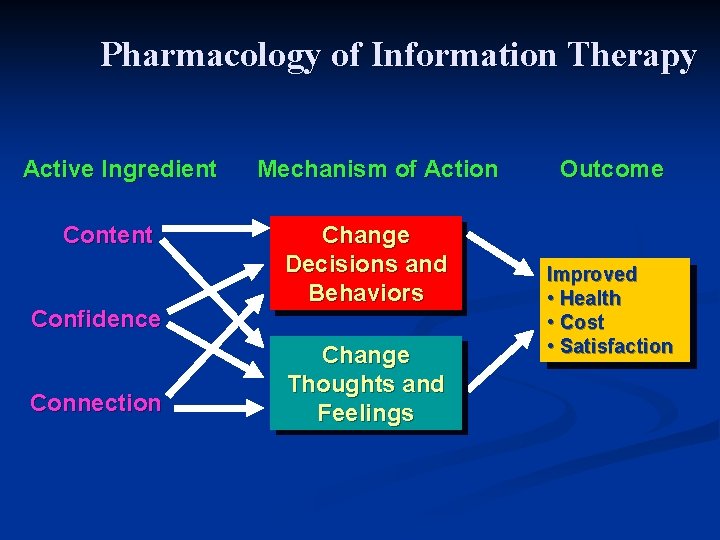
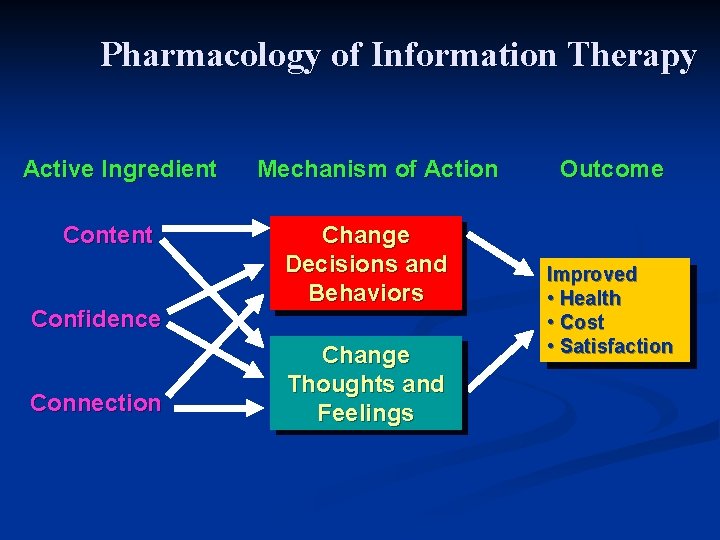
Pharmacology of Information Therapy Active Ingredient Content Confidence Connection Mechanism of Action Change Decisions and Behaviors Change Thoughts and Feelings Outcome Improved • Health • Cost • Satisfaction
The Case for Self-Management Support Patients already self-manage and make decisions (for better or worse) about their chronic conditions 99% of the time n Improved outcome depends on correct diagnosis, correct treatment, and an ongoing series of healthy choices, behaviors and decisions by patients. n
The Case for Self Management Support n To be an informed, activated patient and make healthy decisions, patients need selfmanagement support including: timely, accurate, understandable information n involvement in collaborative decision making n goal setting and problem-solving n help managing psychosocial issues n
Healthier Living: Managing Ongoing Health Conditions Workshop* n n n Small groups 10 -16 people People with different diseases in same group 2 ½ hours a week for 6 weeks Peer taught Content: symptom management, exercise, nutrition, problemsolving, communication, advanced directive Process: Self-efficacy, action planning, sharing Lorig K, Holman H, Sobel D, Laurent D, Gonzalez V, Minor M: Living a Healthy Life with Chronic Conditions, Palo Alto: Bull, 2006 *Chronic Conditions Self-Management Program http: //www. stanford. edu/group/perc/
Healthier Living: What we learned about PROCESS n n n n General coping skills education for heterogeneous conditions complements disease specific information Involve patients in design process Patients are the “experts” in living and coping with chronic illness Modeling more effective than “save and rescue” No significant difference in participants’ outcome with lay vs professional leaders People benefit themselves from helping other people Process is more important than content Lorig, Hurwicz, Sobel, Hobbs, Patient Educ Couns, 2006
Healthier Living: What we learned about OUTCOMES n n n Improves health behaviors, self-efficacy and health status (pain, fatigue, health distress, role function, etc. ) Cost effective (estimated 5: 1 to 10: 1 ROI) from reductions in hospital days, ED and physician visits Outcomes are long-lasting and robust (2+yrs. ) Replicable and dissemination can yield outcomes as good, or better Confidence predicts health outcomes better than behavior change Lorig K et al Medical Care 1999; 37: 5 -14 Lorig K, Sobel DS, Effective Clin Practice 2001; 4: 256 -262 Lorig K, et al Medical Care 2001; 39: 1217 -1223
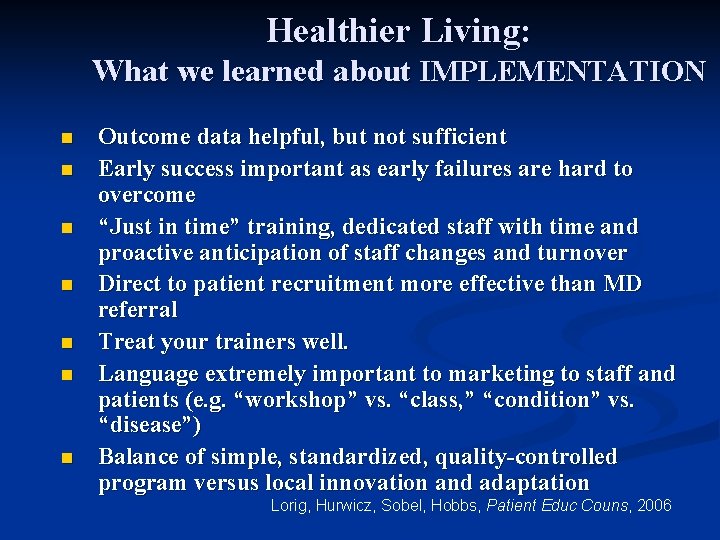
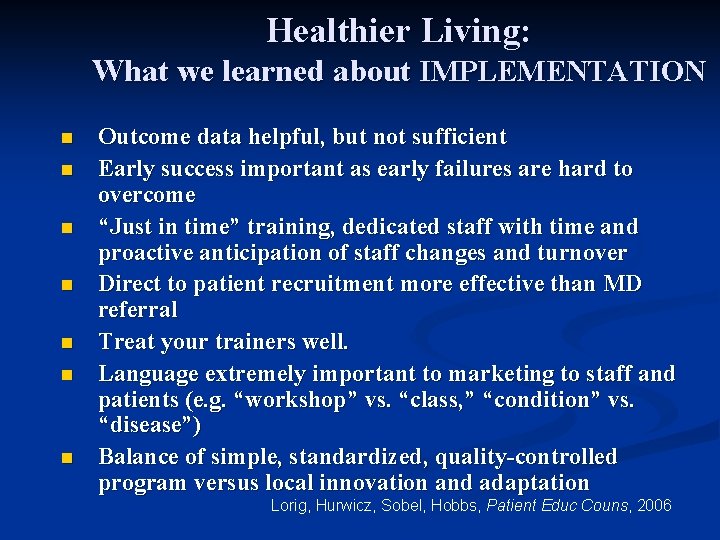
Healthier Living: What we learned about IMPLEMENTATION n n n n Outcome data helpful, but not sufficient Early success important as early failures are hard to overcome “Just in time” training, dedicated staff with time and proactive anticipation of staff changes and turnover Direct to patient recruitment more effective than MD referral Treat your trainers well. Language extremely important to marketing to staff and patients (e. g. “workshop” vs. “class, ” “condition” vs. “disease”) Balance of simple, standardized, quality-controlled program versus local innovation and adaptation Lorig, Hurwicz, Sobel, Hobbs, Patient Educ Couns, 2006
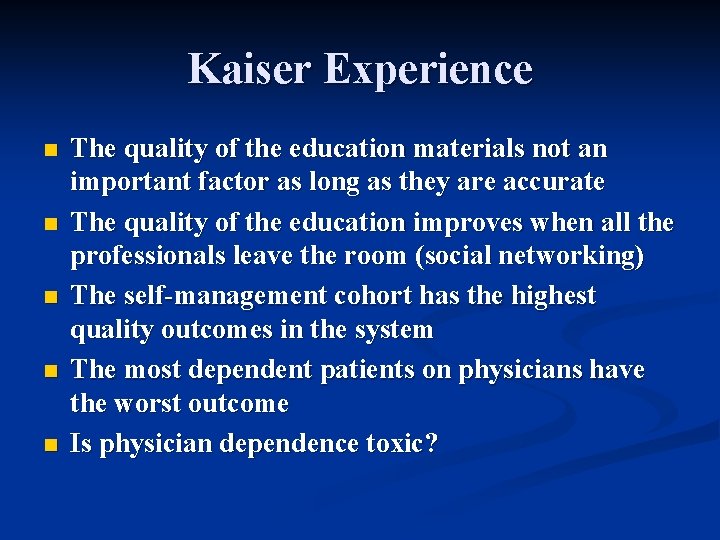
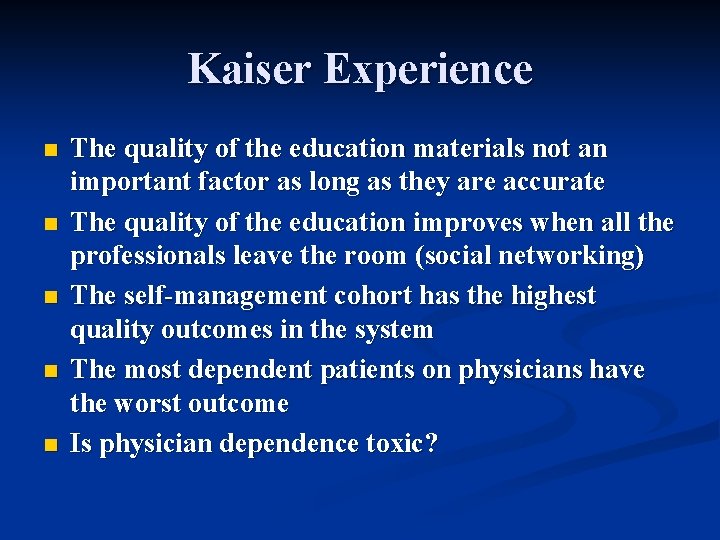
Kaiser Experience n n n The quality of the education materials not an important factor as long as they are accurate The quality of the education improves when all the professionals leave the room (social networking) The self-management cohort has the highest quality outcomes in the system The most dependent patients on physicians have the worst outcome Is physician dependence toxic?
Patient Activation and Self Management are a New Frontier in Medicine Made Possible by the Information Age
The Primary Care Team Goes From Mandatory Caregiver to Advisor, Coach and Personal Resource
Patient, Heal Thyself: How the “New Medicine” Puts the Patient in Charge Robert Veatch Professor of Medical Ethics Georgetown University Oxford University Press, 2008
Resources Stanford CDSMP website: http: //patienteducation. stanford. edu/ n Partners in Care Foundation, June Simmons, CEO www. picf. org n California Health. Care Foundation May 2009 Report, Health Care Without the Doctor: http: //www. chcf. org/documents/policy/Healt h. Care. Without. The. Doctor. pdf n
Whenever you see a successful business, someone once made a courageous decision Peter Drucker
Change Is Disturbing When It Is Done To Us. Change Is Exhilarating When It Is Done By Us Rosabeth Kantor Harvard Business School

Google’s Laws Give people control and we will use it. Don’t and you will lose us. n There is an inverse relationship between control and trust. n Google Health System – Go public with your health record and get help from a network of Patients Like Me n From: What Would Google Do? Jeff Jarvis, 2009
Human Nature Changes Little Caring Remains Primary What Changes Are The Tools And Methods We Use
 Patient centered medical home
Patient centered medical home Patient centered medical home conference
Patient centered medical home conference Stock image
Stock image Patient centered care collaborative
Patient centered care collaborative Patient centered care
Patient centered care Qsen safety competencies examples
Qsen safety competencies examples Patient centered primary care collaborative
Patient centered primary care collaborative Patient 2 patient
Patient 2 patient Putting the enterprise into the enterprise system
Putting the enterprise into the enterprise system Putting-out system
Putting-out system The spatial strategy of organizing your speech
The spatial strategy of organizing your speech Putting-out system
Putting-out system Putting things together is called
Putting things together is called Putting on the new man
Putting on the new man Puts the pieces together if in use maybe
Puts the pieces together if in use maybe A process in sculpture putting additional parts
A process in sculpture putting additional parts Putting it all together motion answer key
Putting it all together motion answer key Putting it all to bed during project closeout includes
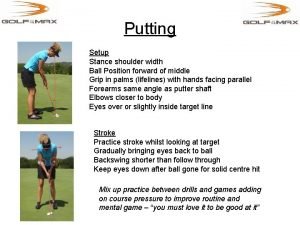
Putting it all to bed during project closeout includes Putting stance ball position
Putting stance ball position What does nasreen say about ice cream with chocolate
What does nasreen say about ice cream with chocolate Practice putting it all together
Practice putting it all together Classify a polynomial
Classify a polynomial The pricing tripod
The pricing tripod Putting two words together
Putting two words together Putting zone
Putting zone Fractions in increasing order
Fractions in increasing order Coherent curriculum
Coherent curriculum Putting a package together
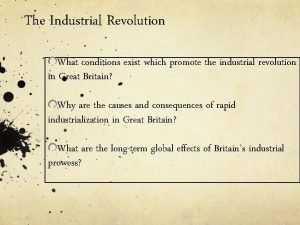
Putting a package together When was the loom invented
When was the loom invented Putting it into practice
Putting it into practice Putting the enterprise into the enterprise system
Putting the enterprise into the enterprise system Putting evidence into practice
Putting evidence into practice Putting objects in perspective
Putting objects in perspective Why we all have
Why we all have Putting to death the old man
Putting to death the old man Putting people first 2007
Putting people first 2007 Putting the pieces together case study answer key
Putting the pieces together case study answer key Proletarianization ap euro
Proletarianization ap euro Putting prevention into practice
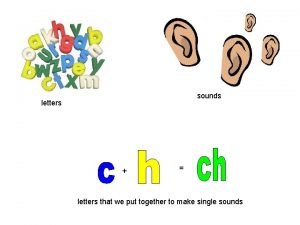
Putting prevention into practice Letters put together
Letters put together The order of putting on ppe
The order of putting on ppe 6x²y³÷xy²= _______.
6x²y³÷xy²= _______. Preoperative medical evaluation of the healthy patient
Preoperative medical evaluation of the healthy patient Heaton moor medical
Heaton moor medical