ANOREXIA NERVOSA THE FAMILY CONNECTION Eating Disorder Specific












- Slides: 43
ANOREXIA NERVOSA: THE FAMILY CONNECTION Eating Disorder Specific Care Clinic Brynn Kelly, Ph. D, Kate Mac. Phee, PDt, Herb Orlik, MD, Jessica Wournell, RN

OUTLINE • Historical background • Brynn Kelly will outline Family Based Therapy • Kate Mac. Phee will describe our special assessment and treatment team • Jessica Wournell will show you statistics of Family Based Therapies carried out so far in our specialty and community clinics.
OBJECTIVES You will be able to: 1. contrast perceptions of the role of the family in anorexia nervosa with recent insights about the family 2. identify principles, procedures and processes in Family Based Treatment (FBT) 3. gain a perspective of FBT according to IWK-based experiences so far
DISCLOSURES • None of the presenters have any connections to industry or financial connections with regard to today’s topic

ACKNOWLEDGEMENTS • Dr. Brynn Kelly has studied with the team of James Lock, one of the main authors of FBT, at Stanford University • The IWK Mental Health and Addictions Program has made it possible for a number of IWK clinicians to be trained, and in some cases, certified by Dr. Blake Woodside, University of Toronto
CONNECTIONS There are many “connections” of interest in anorexia nervosa, for example • the biological connection • the psychosocial connection • the feminist connection • the existential connection • the media connection; and so on Today we want to focus on the family connection
HISTORY • The disorder has been known and has been described in various forms for hundreds of years • A non-clinical assumption was that it was a kind of religious expression, starvation as asceticism, a devotion to a god or to a religion • A common early clinical theme was that it was a form of hysteria (Gull 1874)
HISTORY • Family issues had not been described until mainly psychoanalysts explored early childhood and adolescent experiences retrospectively in adult patients • One prominent psychoanalytic theory was that anorexia nervosa was a sort of fear of oral impregnation or a defense against a wish for (upwardly displaced oral) impregnation (Fraiberg 1972, Sperling 1973) • As with other psychiatric conditions, overprotective, controlling, sometimes punitive mothers and ineffectual, absent fathers were seen to be part of the preceding or perpetuating family dynamic
HISTORY Much attention then began to be focused on family function in the 1970 s and 80’s: • Bruch described the family as functioning as if members could read one another’s minds (Bruch 1973, 1978) • Yager described the family as focused on high achievement, communicating along narrow lines, and failing to recognize the anorexic child’s individuality (Yager, 1981)
HISTORY 1970’s & 1980’s Cont. : • Sours emphasized the need of the family to maintain harmony and disavow distress or upset (Sours, 1980) • Minuchin identified five predominant characteristics of family interaction as excessively present and detrimental to overall family functioning: enmeshment, overprotectiveness, rigidity, lack of conflict resolution and involvement of the sick child in unresolved parental conflict (Minuchin, Baker, Rosman, et al, 1975, 1978)
HISTORY • Other influential authors, Crisp and Selvini-Palazzoli, also described difficulties within the family (Crisp 1980, Selvini-Palazzoli, 1978) • Although all these authors and the analysts before them described family dysfunctions, they were cautious enough not to claim that these were unitary etiologies for anorexia nervosa.
HISTORY • Still, one got the strong impression that families, parents, were to blame. • Therapies therefore were devised to 'correct' these family dysfunctions. • Other interventions were geared to isolate if not separate youngsters with anorexia nervosa from their immediate families, leading to so-called ‘parentectomies’ (Peshkin and Tuft 1956, Harper 1983)

THE ENGLISH CONNECTION • Individual therapies such as psychoanalytically-derived or psychodynamic therapy and CBT were tried extensively but did not show great results. Working on ‘faulty’ family interactions and blaming parents did not go over well with many families and no longer made sense to many clinicians and researchers • At the Maudsley Institute Christopher Dare then developed a new form of family therapy (Dare 1985, Dare, Eisler, Russell, Smuckler, 1990, Dare, Le Grange, 1994, Dare, Eisler, 1997)
THE ENGLISH CONNECTION • The principles are simple and straight forward, though radically different from what had existed so far: • parents are the best treatment resource • parents take over the control of their child’s food intake • therapy initially focuses on weight restoration • parents are not to blame • etiology of the eating disorder is not addressed, is not of concern • the parents’ anxiety is raised to motivate them to intensively engage in therapy
FBT • Subsequently, Dare’s family therapy for anorexia nervosa has become known as “the Maudsley Method”. • Lock and Le. Grange adopted this method, improved, expanded it and manualized their new version. They took it from London to Chicago and then to Stanford University. The first manual was published in 2001 in collaboration with Agras and Dare. A companion book for parents, “Help Your Teenager Beat an Eating Disorder” was brought out in 2005 and the second edition of the “Treatment Manual for Anorexia Nervosa, a Family. Based Approach” came out in 2013. • Numerous trials including RCTs have since shown that FBT is the gold standard and that it has the highest level of evidence of effectiveness compared to other interventions in adolescent anorexia nervosa.

FAMILY BASED TREATMENT (FBT) Brynn Kelly, Ph. D
FAMILY BASED TREATMENT (FBT) • Outpatient, team approach • FBT therapist • Consulting team: physician, nurse, nutritionist or dietician • Focused on behavior, rather than underlying cause • Parents are the agents of change Lock, J. & Le Grange, D. (2013). Treatment Manual for Anorexia Nervosa: A Family-Based Approach. New York: Guilford.

FBT: PHASES Phase I: Weight restoration • 10+ sessions, weekly Phase II: Returning independence to the adolescent • Consider transition to Phase II when: • At least 90% of EBW • Patient compliant with parental meal monitoring • Parents feel empowered to manage AN • Approx. 2 -6 sessions every 2 -3 weeks Lock, J. & Le Grange, D. (2013). Treatment Manual for Anorexia Nervosa: A Family-Based Approach. New York: Guilford.
FBT: PHASES Phase III: Return to healthy adolescent development • Consider transition to Phase III when: • Weight restored and maintained between 95 -100% of EBW with adolescent in control • Family able to discuss non eating-related adolescent issues • Patient is re-aligned with peers • Approx. 1 -4 sessions every 4 -6 weeks Lock, J. & Le Grange, D. (2013). Treatment Manual for Anorexia Nervosa: A Family-Based Approach. New York: Guilford.
PHASE I: WEIGHT RESTORATION/RENOURISHMENT Family role • Parents take charge of meals: • What, where, how much • ↑ portion size, frequency & caloric content (without calorie counting!) • 3 meals, 2 -3 snacks • Re-introducing “trigger” foods • Close supervision • Coaching and support • Parents prevent purging/ exercise • Siblings provide emotional support Lock, J. & Le Grange, D. (2013). Treatment Manual for Anorexia Nervosa: A Family. Based Approach. New York: Guilford.
PHASE I: WEIGHT RESTORATION/RENOURISHMENT Clinician goals • Understand impact of AN on family • Understand impact of family dynamic on fighting AN • Engage family • Empower parents • Mobilize sibling support for patient • Keep family focused on AN Lock, J. & Le Grange, D. (2013). Treatment Manual for Anorexia Nervosa: A Family-Based Approach. New York: Guilford.
PHASE I: WEIGHT RESTORATION/RENOURISHMENT Therapeutic strategies • Weigh patient & plot progress • Create “Intense Scene” • Externalize the illness • Address each family member • “Charge” the parents • In-session family meal • Aligning parents toward “one bite more” and/or normalizing eating • Aligning patient with sibling(s) • Evaluate progress; problem-solve • Redirect focus back to AN • Modify family criticisms of patient Lock, J. & Le Grange, D. (2013). Treatment Manual for Anorexia Nervosa: A Family-Based Approach. New York: Guilford.
PHASE II: TRANSITIONING CONTROL • Support family in reaching the following goals: • Parents monitor & gradually step back, dependent upon progress • Patient eating well • Patient gaining weight • Patient gradually takes control of food & weight • Explore relation between adolescent developmental issues & AN Lock, J. & Le Grange, D. (2013). Treatment Manual for Anorexia Nervosa: A Family-Based Approach. New York: Guilford.

PHASE II: TRANSITIONING CONTROL Therapeutic strategies • Support parents & patient in managing transfer of control • Evaluate progress • Continue to: • Weigh patient & plot progress • Shifting from “gain” to “maintain” • Externalize the illness • Highlight signs of re-emergence of patient & separation from AN • Modify parental & sibling criticism • Normalize difficulties with return of independence • Gradually shift focus to issues of adolescence Lock, J. & Le Grange, D. (2013). Treatment Manual for Anorexia Nervosa: A Family-Based Approach. New York: Guilford.
PHASE III: RETURN TO HEALTHY DEVELOPMENT • Support family in reaching the following goals: • Communicating without AN being the focus • Discussing and problem-solving issues of adolescence • Terminating treatment Lock, J. & Le Grange, D. (2013). Treatment Manual for Anorexia Nervosa: A Family-Based Approach. New York: Guilford.

PHASE III: RETURN TO HEALTHY DEVELOPMENT Therapeutic strategies • “Mini-lecture” on adolescent development, highlighting relevant themes • Involve family in review of adolescent issues as they relate to patient • Check in on how parents are doing as a couple • Planning for future issues • Saying goodbye, reviewing progress, highlighting strengths Lock, J. & Le Grange, D. (2013). Treatment Manual for Anorexia Nervosa: A Family-Based Approach. New York: Guilford.
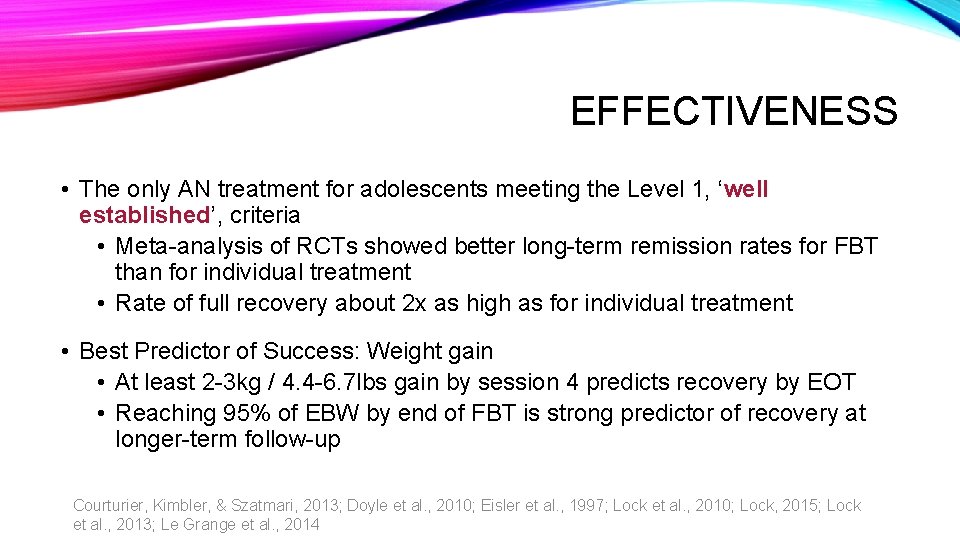
EFFECTIVENESS • The only AN treatment for adolescents meeting the Level 1, ‘well established’, criteria • Meta-analysis of RCTs showed better long-term remission rates for FBT than for individual treatment • Rate of full recovery about 2 x as high as for individual treatment • Best Predictor of Success: Weight gain • At least 2 -3 kg / 4. 4 -6. 7 lbs gain by session 4 predicts recovery by EOT • Reaching 95% of EBW by end of FBT is strong predictor of recovery at longer-term follow-up Courturier, Kimbler, & Szatmari, 2013; Doyle et al. , 2010; Eisler et al. , 1997; Lock et al. , 2010; Lock, 2015; Lock et al. , 2013; Le Grange et al. , 2014
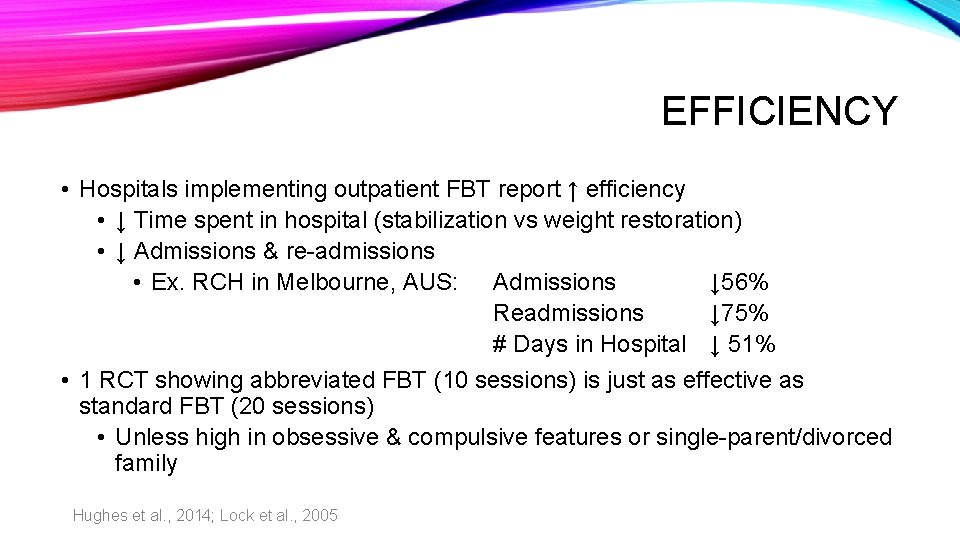
EFFICIENCY • Hospitals implementing outpatient FBT report ↑ efficiency • ↓ Time spent in hospital (stabilization vs weight restoration) • ↓ Admissions & re-admissions • Ex. RCH in Melbourne, AUS: Admissions ↓ 56% Readmissions ↓ 75% # Days in Hospital ↓ 51% • 1 RCT showing abbreviated FBT (10 sessions) is just as effective as standard FBT (20 sessions) • Unless high in obsessive & compulsive features or single-parent/divorced family Hughes et al. , 2014; Lock et al. , 2005

EATING DISORDERS SPECIAL ASSESSMENT AND TREATMENT TEAM Kate Mac. Phee, PDt
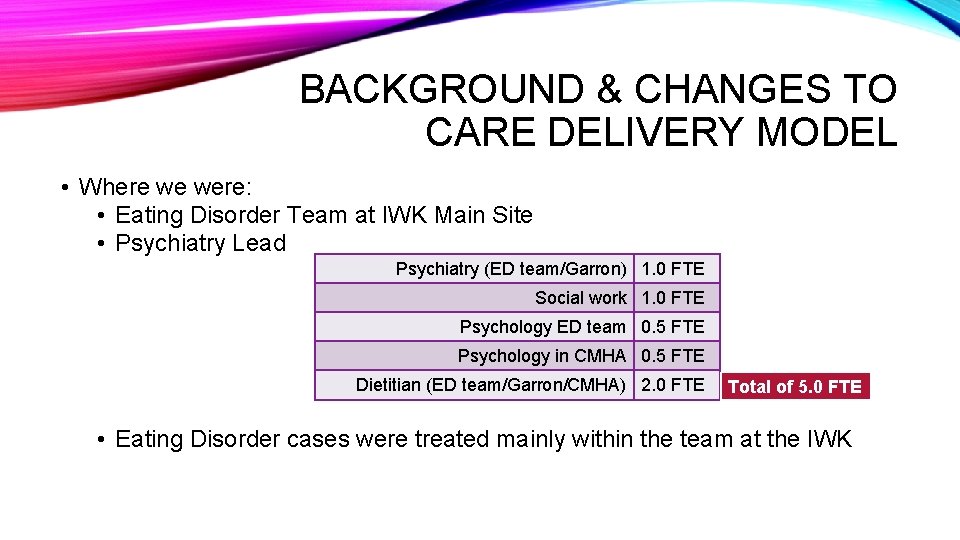
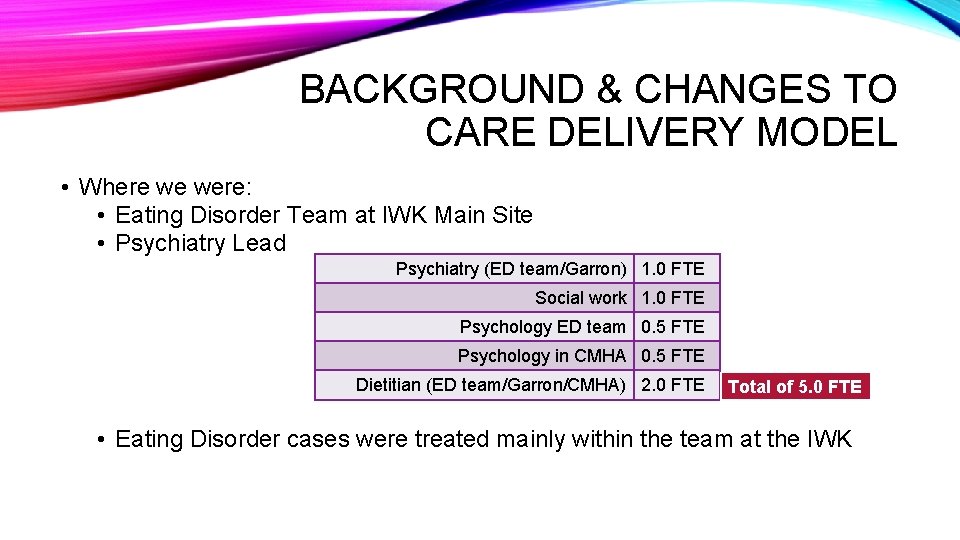
BACKGROUND & CHANGES TO CARE DELIVERY MODEL • Where we were: • Eating Disorder Team at IWK Main Site • Psychiatry Lead Psychiatry (ED team/Garron) 1. 0 FTE Social work 1. 0 FTE Psychology ED team 0. 5 FTE Psychology in CMHA 0. 5 FTE Dietitian (ED team/Garron/CMHA) 2. 0 FTE Total of 5. 0 FTE • Eating Disorder cases were treated mainly within the team at the IWK
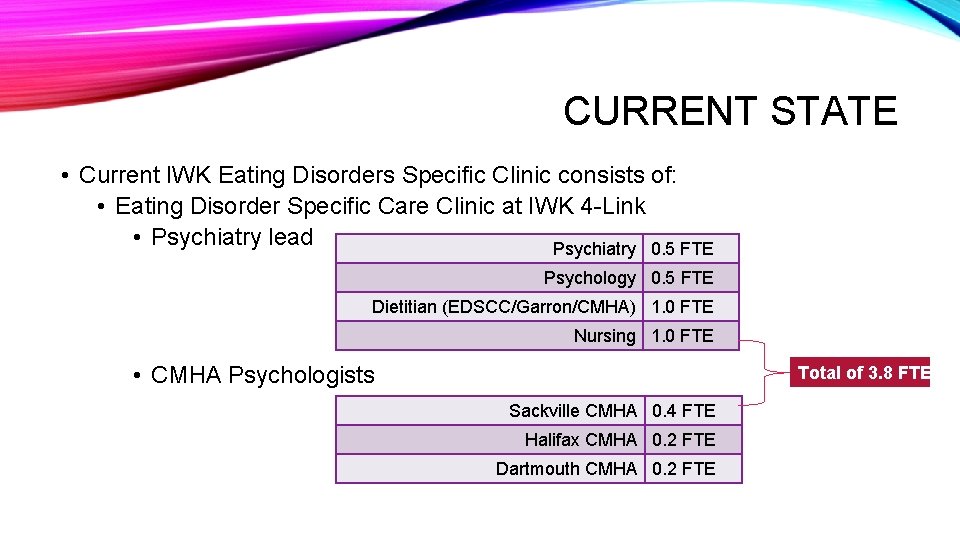
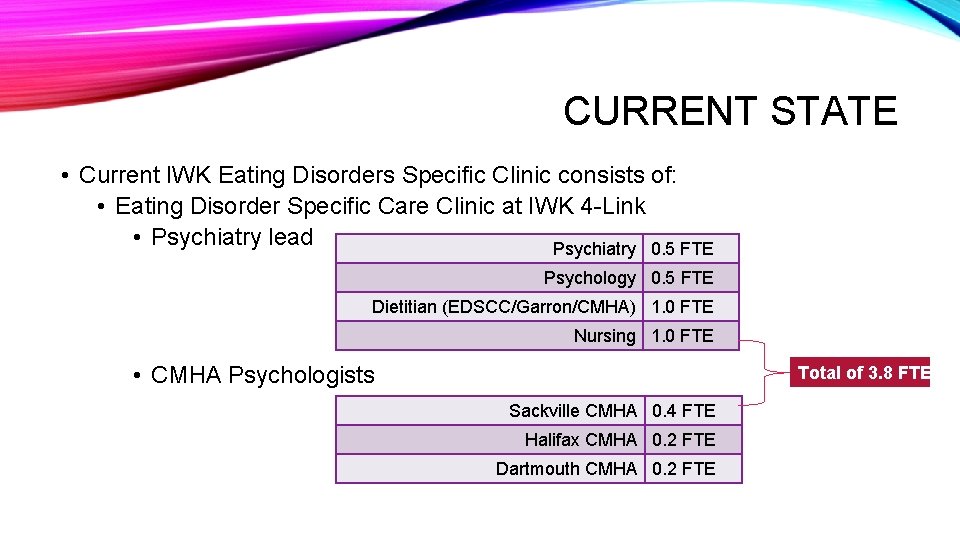
CURRENT STATE • Current IWK Eating Disorders Specific Clinic consists of: • Eating Disorder Specific Care Clinic at IWK 4 -Link • Psychiatry lead Psychiatry 0. 5 FTE Psychology 0. 5 FTE Dietitian (EDSCC/Garron/CMHA) 1. 0 FTE Nursing 1. 0 FTE • CMHA Psychologists Total of 3. 8 FTE Sackville CMHA 0. 4 FTE Halifax CMHA 0. 2 FTE Dartmouth CMHA 0. 2 FTE

ED TRAINING CLINIC OVERVIEW • Certified: • Dr. Amber Johnston (Halifax), Dr. Susan Jerrott (Sackville), Dr. Brynn Kelly (EDSCC) • Advanced Learners: • Dr. Laura Connors (Dartmouth), Dr. Elizabeth Quon (Dartmouth) • Learners: • Dr. Orlik (EDSCC), Jessica Wournell RN (EDSCC), Melissa Kemp RN (EDSCC), Kate Mac. Phee PDt (EDSCC/Garron), Tracy Bourdages RN (Garron)

ED TRAINING CLINIC OVERVIEW • Family Based Treatment (FBT) workshop, leading into weekly peersupervision with Dr. Blake Woodside • Increased capacity in the treatment of eating disorders within CMHA

FBT TRAINING CLINIC DATA September 2015 -Present Jessica Wournell, RN
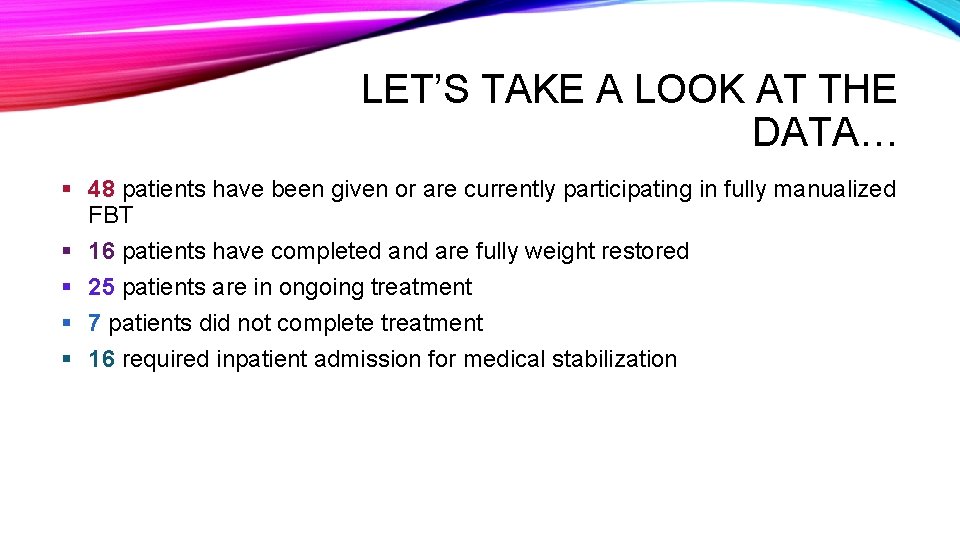
LET’S TAKE A LOOK AT THE DATA… § 48 patients have been given or are currently participating in fully manualized FBT § 16 patients have completed and are fully weight restored § 25 patients are in ongoing treatment § 7 patients did not complete treatment § 16 required inpatient admission for medical stabilization
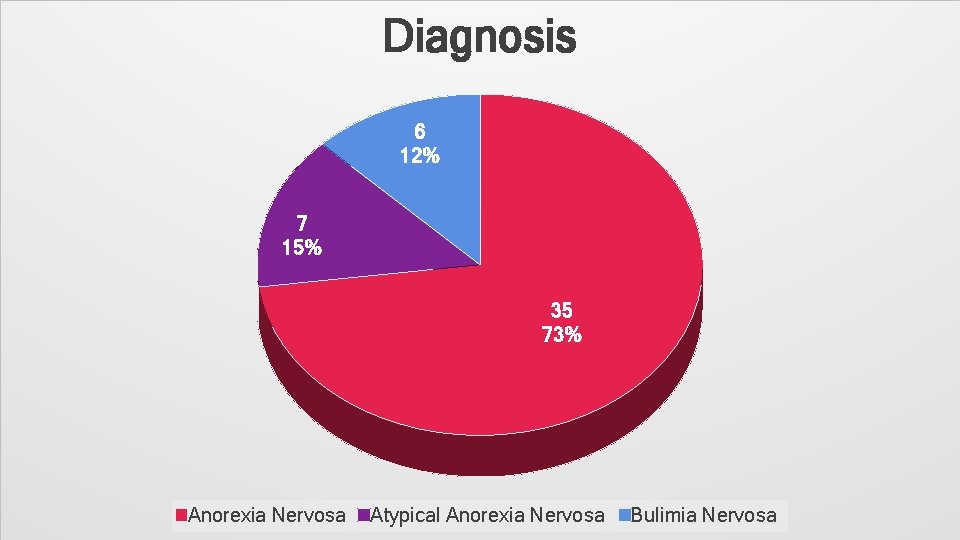
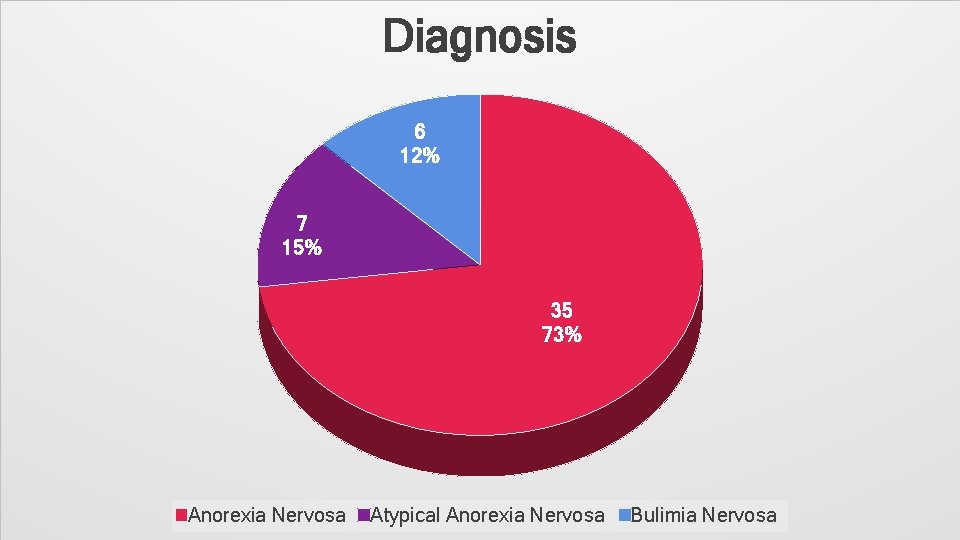
Diagnosis 6 12% 7 15% 35 73% Anorexia Nervosa Atypical Anorexia Nervosa Bulimia Nervosa
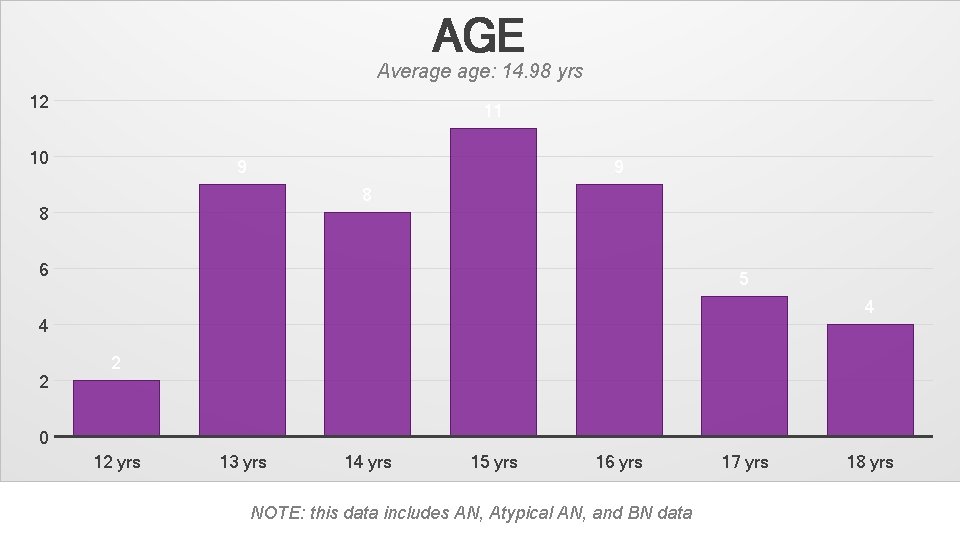
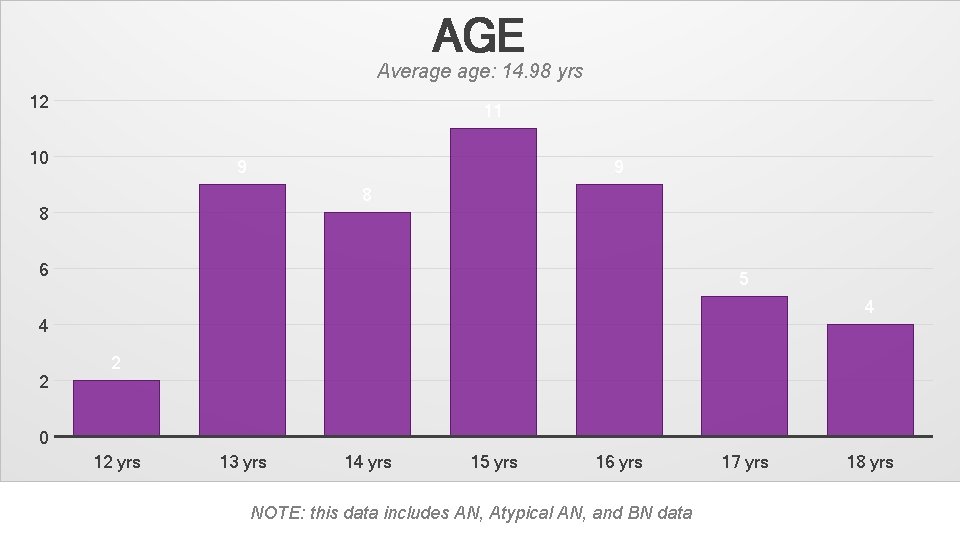
AGE Average age: 14. 98 yrs 12 11 10 9 9 8 8 6 5 4 4 2 2 0 12 yrs 13 yrs 14 yrs 15 yrs 16 yrs NOTE: this data includes AN, Atypical AN, and BN data 17 yrs 18 yrs
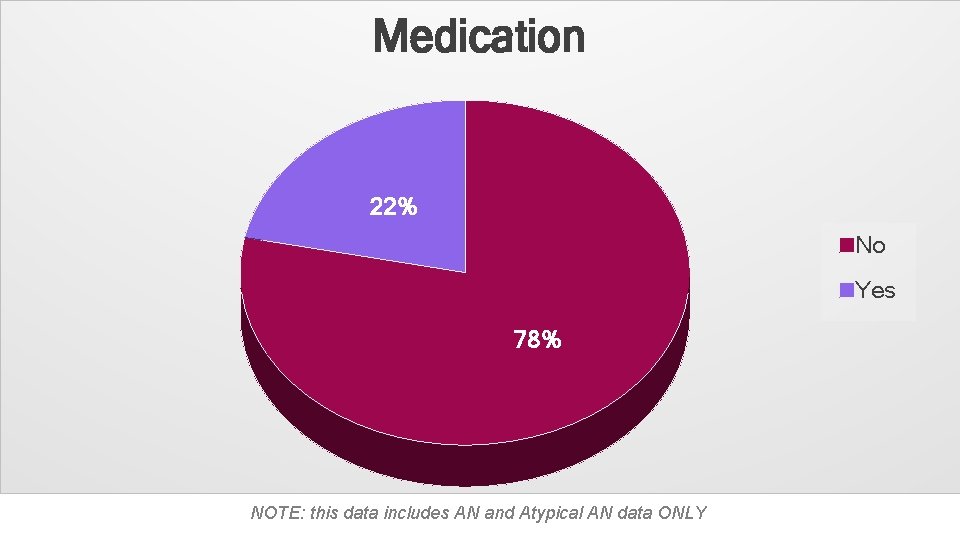
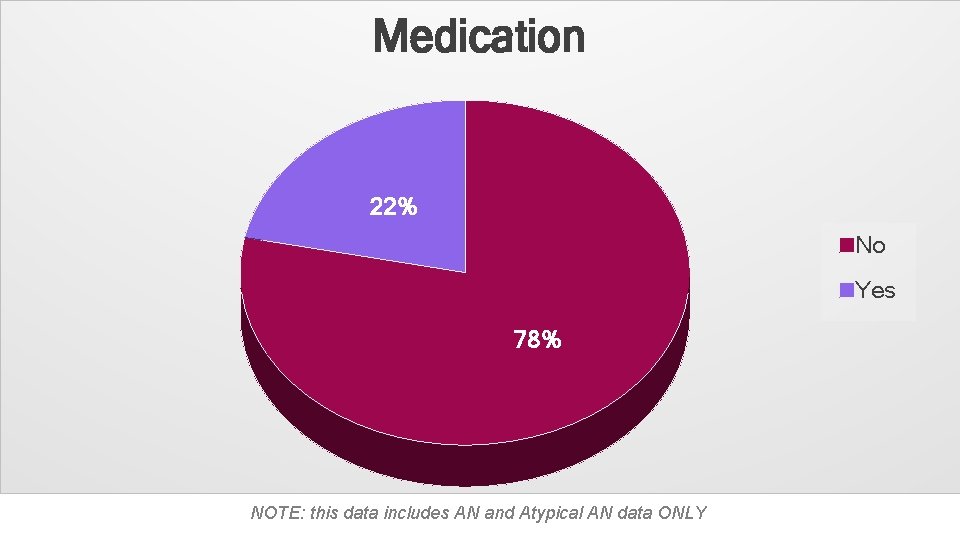
Medication 22% No Yes 78% NOTE: this data includes AN and Atypical AN data ONLY
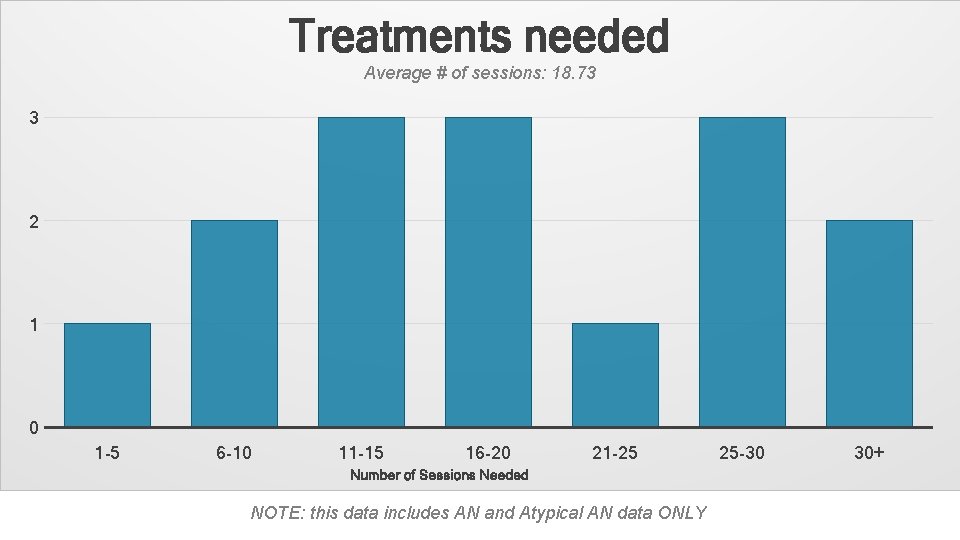
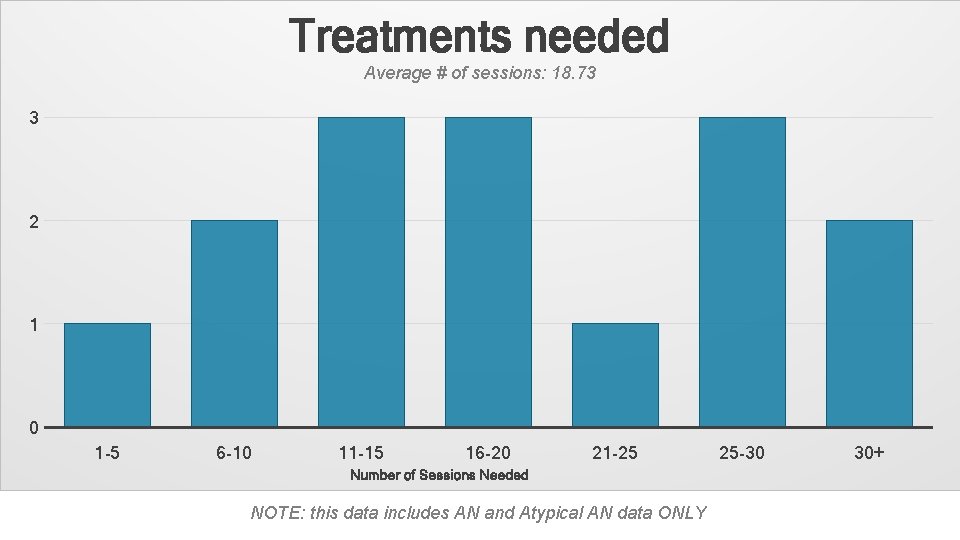
Treatments needed Average # of sessions: 18. 73 3 2 1 0 1 -5 6 -10 11 -15 16 -20 21 -25 Number of Sessions Needed NOTE: this data includes AN and Atypical AN data ONLY 25 -30 30+
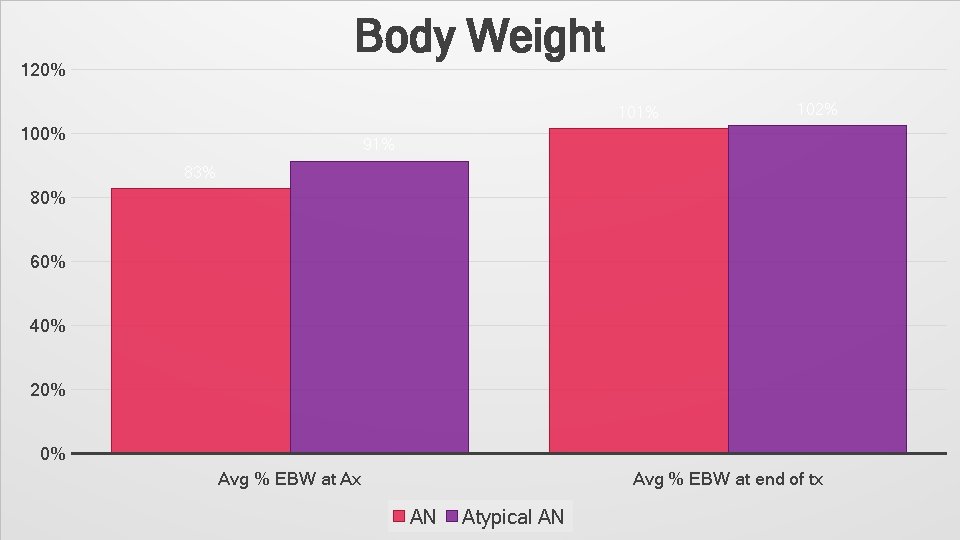
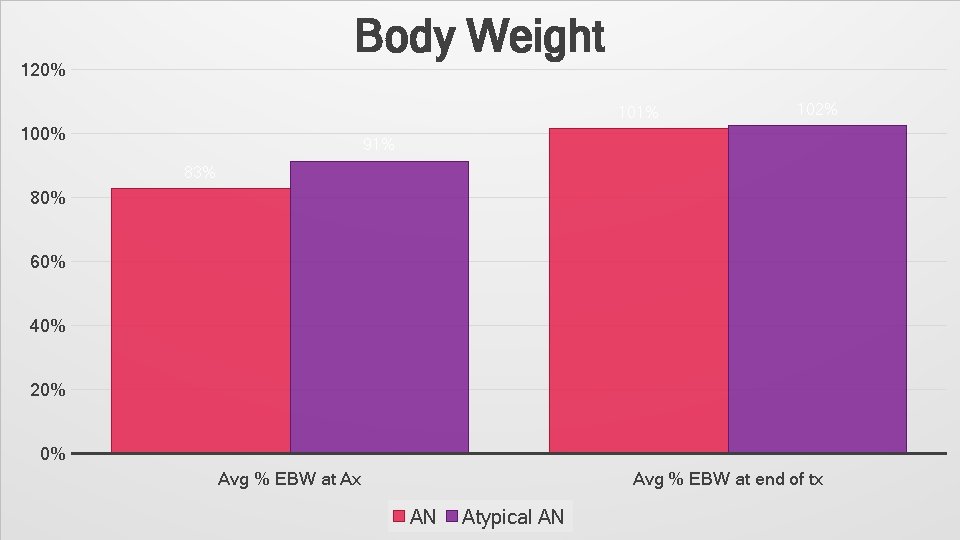
Body Weight 120% 101% 100% 102% 91% 83% 80% 60% 40% 20% 0% Avg % EBW at Ax Avg % EBW at end of tx AN Atypical AN

BODY WEIGHT DATA Disorder Avg. % EBW at Ax Avg. % EBW at end of Avg. increase in body Tx weight Anorexia Nervosa 83% 101% 19% Atypical Anorexia Nervosa 91% 102% 11% Combined AN & Atypical AN 84% 102% 18%
COMPLICATING FACTORS IN TREATMENT • Family not on board • Parental blocks (EFFT*) may be needed) • Scheduling • Complicated family dynamics (i. e. split families, poor relationship with youth) • Stigma *EFFT = Emotion-Focused Family Therapy • Suicidality/ Self harm • Should be assessed on an ongoing basis. • If active SI with plan/ intent that takes priority and treatment may need to go on hold until resolved
QUESTIONS?
 Anorexia nervosa long term effects
Anorexia nervosa long term effects Unit 3 lesson 6 anorexia nervosa and bulimia
Unit 3 lesson 6 anorexia nervosa and bulimia Male
Male Type of anorexia
Type of anorexia Anorexia nervosa
Anorexia nervosa Anorexia nervosa syptoms
Anorexia nervosa syptoms The diagnostic term anorexia nervosa literally means
The diagnostic term anorexia nervosa literally means Anorexia nervosa definition wikipedia
Anorexia nervosa definition wikipedia Myers ap psych unit 8 vocab
Myers ap psych unit 8 vocab Anorexia nervosa is characterized
Anorexia nervosa is characterized Kate moss eating disorder
Kate moss eating disorder Kelly in the kitchen eating disorder
Kelly in the kitchen eating disorder York eating disorders service
York eating disorders service Gisele bundchen anorexia
Gisele bundchen anorexia Private practice eating disorder episode
Private practice eating disorder episode Hypothalamus eating disorders
Hypothalamus eating disorders Eating disorder syptoms
Eating disorder syptoms Eating disorder clinic halifax
Eating disorder clinic halifax Kate bosworth eating disorder
Kate bosworth eating disorder Binge eating disorder
Binge eating disorder Brianna k eating disorder
Brianna k eating disorder Ceds eating disorder
Ceds eating disorder Eating disorder in which people overeat compulsively
Eating disorder in which people overeat compulsively Eating disorder coalition of iowa
Eating disorder coalition of iowa Cedrd certification
Cedrd certification Bolted connection
Bolted connection A325n bolts
A325n bolts Slip critical
Slip critical What are text to text connections
What are text to text connections Conversion disorder
Conversion disorder Specific learning disorder
Specific learning disorder Specific learning disorder
Specific learning disorder Signing naturally 8:10 minidialogue 2
Signing naturally 8:10 minidialogue 2 Family connection naviance
Family connection naviance Specific volume
Specific volume Glass plummet
Glass plummet Winona ryder anorexia
Winona ryder anorexia Freud anorexia
Freud anorexia Iso bmi
Iso bmi Social learning theory anorexia
Social learning theory anorexia Intervention anorexia episodes
Intervention anorexia episodes Dominique anorexia
Dominique anorexia Bullimia nervosa definition
Bullimia nervosa definition Anorexia historia natural de la enfermedad
Anorexia historia natural de la enfermedad