Eating disorder Thaer Ahmad Aljou Eating disorder Eating






- Slides: 43
Eating disorder Thaer Ahmad Aljou
Eating disorder Eating disorders include: 1. Anorexia nervosa 2. Bulimia nervosa 3. Binge-eating disorder Patients with anorexia or bulimia have a disturbed body image and use extensive measures to avoid gaining weight (vomiting, laxatives, diuretics, enemas, fasting, and excessive exercise). Patients with binge-eating disorder typically binge in response to negative emotions.

Anorexia nervosa
The term anorexia nervosa is derived from the Greek term for “loss of appetite” and a Latin word implying nervous origin. Anorexia nervosa Patients with anorexia nervosa are preoccupied with their weight, their body image, and being thin. It is often associated with obsessive-compulsive personality traits
The most common ages of onset is between 14 and 18 years, but up to 5% have the onset in their early 20 s. Epidemiolo gy Is estimated to occur in about 0. 5 to 1 % of adolescent girls. It occurs 10 to 20 times more often in females than in males. It seems to be most frequent in developed countries, and it may be seen with greatest frequency among young women in professions that requires thinness, such as modelling and ballet.
Etiology Biological factors: 1. Neurotransmitters: serotonin, norepinephrine and dopamine dysregulation. 2. PET scan finding: higher metabolism in the caudate nucleus. Social factors: 1. Patients find support for their practices in society’s emphasis on thinness and exercise. 2. Families of children with eating disorders may exhibit high levels of hostility, chaos, and isolation and low levels of nurturance and empathy.
Etiology Psychological and Psychodynamic factors 1. Anorexia nervosa appears to be a reaction to the demand that adolescents behave more independently and increase their social and sexual functioning. 2. Many experience their bodies as somehow under the control of their parents, so that self-starvation may be an effort to gain validation as a unique and special person.
Diagnosis and DSM-5 Criteria Anorexia nervosa is a syndrome characterized by three essential criteria: 1. The first is a self-induced starvation to a significant degree-a behavior. 2. The second is a relentless drive for thinness or a morbid fear of fatness-a psychopathology. 3. The third criterion is the presence of medical signs and symptoms resulting from starvation-a physiological symptomatology. üThe behaviors and psychopathology are present for at least 3 months.
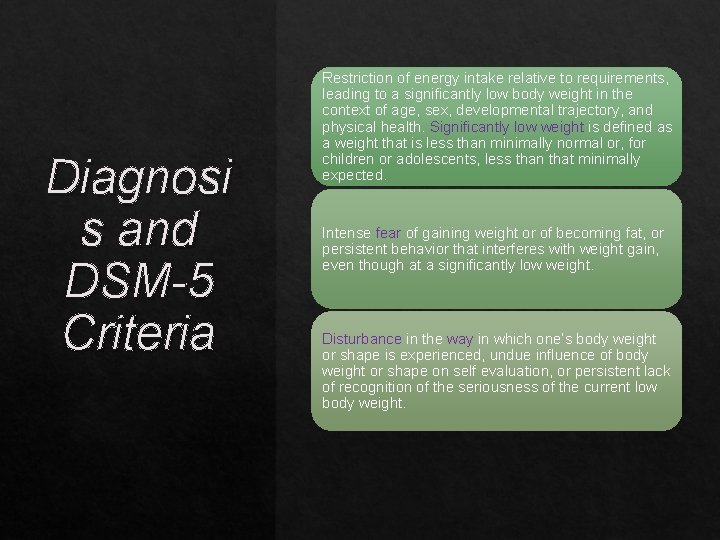
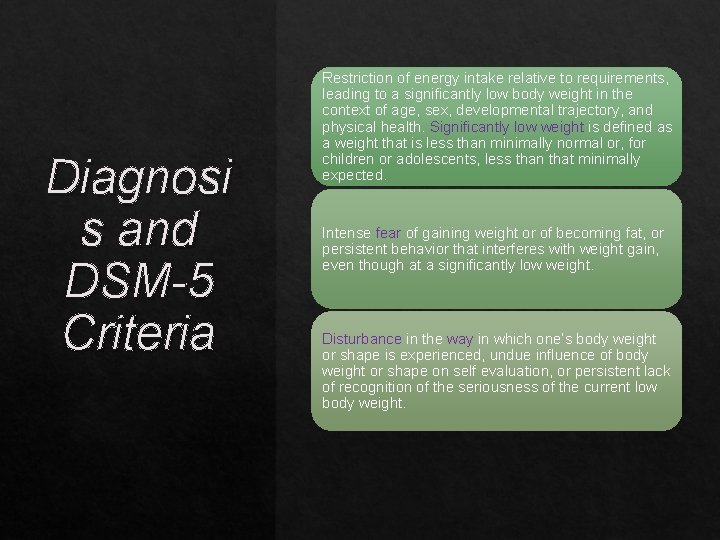
Diagnosi s and DSM-5 Criteria Restriction of energy intake relative to requirements, leading to a significantly low body weight in the context of age, sex, developmental trajectory, and physical health. Significantly low weight is defined as a weight that is less than minimally normal or, for children or adolescents, less than that minimally expected. Intense fear of gaining weight or of becoming fat, or persistent behavior that interferes with weight gain, even though at a significantly low weight. Disturbance in the way in which one’s body weight or shape is experienced, undue influence of body weight or shape on self evaluation, or persistent lack of recognition of the seriousness of the current low body weight.
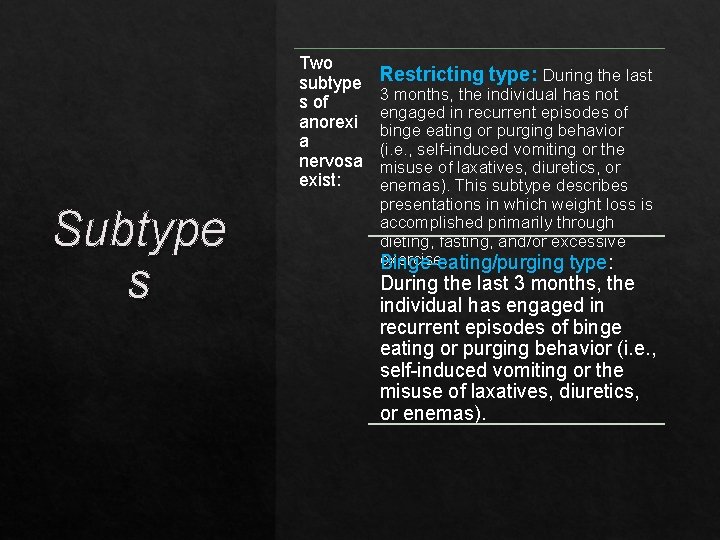
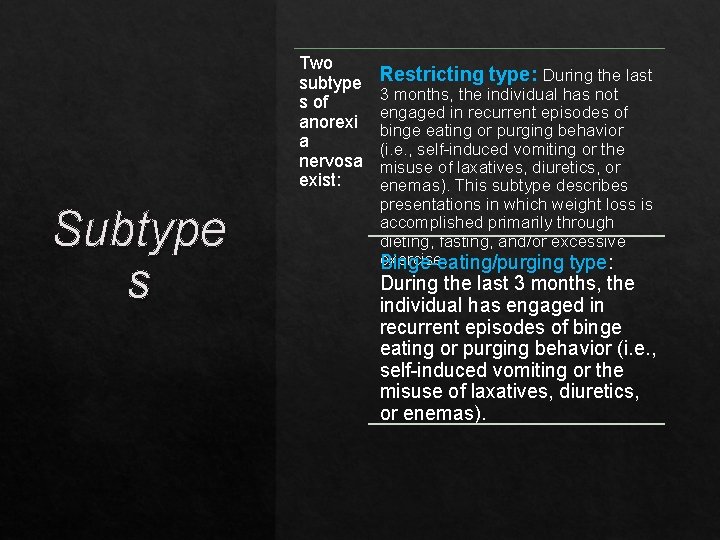
Two subtype s of anorexi a nervosa exist: Subtype s Restricting type: During the last 3 months, the individual has not engaged in recurrent episodes of binge eating or purging behavior (i. e. , self-induced vomiting or the misuse of laxatives, diuretics, or enemas). This subtype describes presentations in which weight loss is accomplished primarily through dieting, fasting, and/or excessive exercise. Binge-eating/purging type: During the last 3 months, the individual has engaged in recurrent episodes of binge eating or purging behavior (i. e. , self-induced vomiting or the misuse of laxatives, diuretics, or enemas).

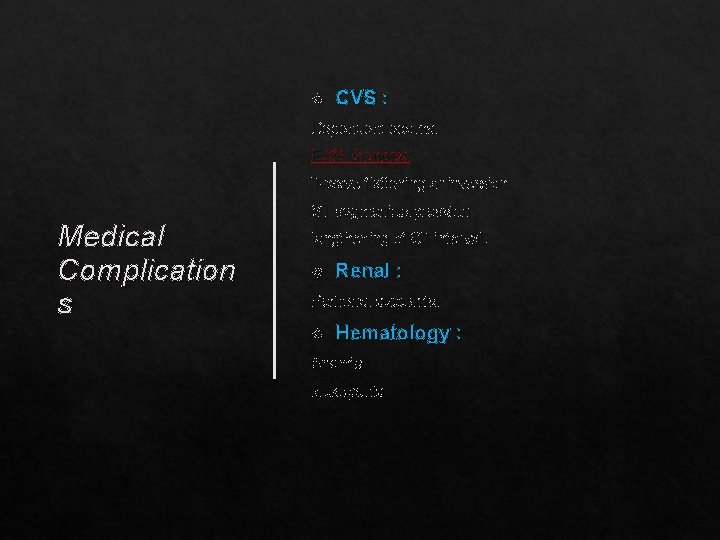
Vital signs: Bradycardia Hypotension (orthostatic) Hypothermia Medical Complication s Poikilothermia General : Muscle atrophy Lanugo hair (appearance of neonatal like hair) Loss of body fat CNS : Generalized brain atrophy with enlarged ventricles Seizure Abnormal cortical mass
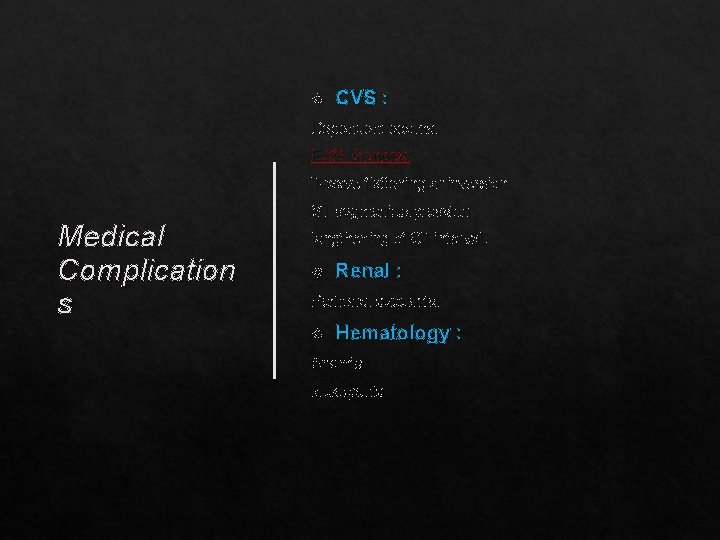
CVS : Dependent edema. ECG changes: T-wave flattening or inversion Medical Complication s ST segment depression lengthening of QT interval. Renal : Perirenal azotemia. Hematology : Anemia leukopenia
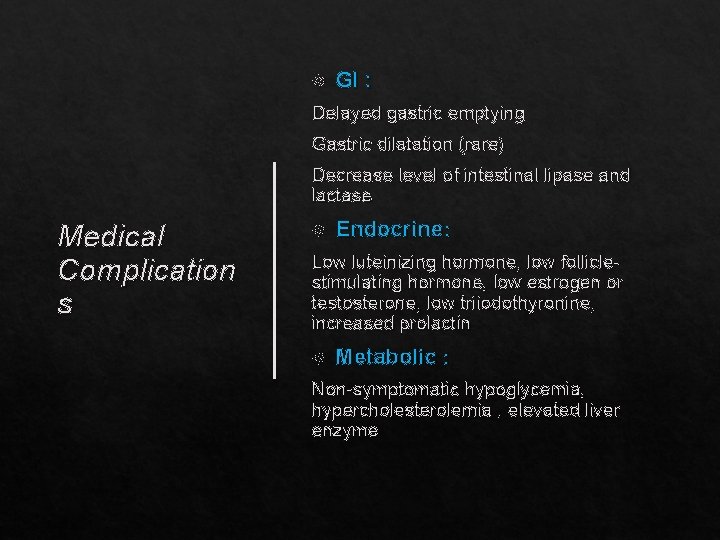
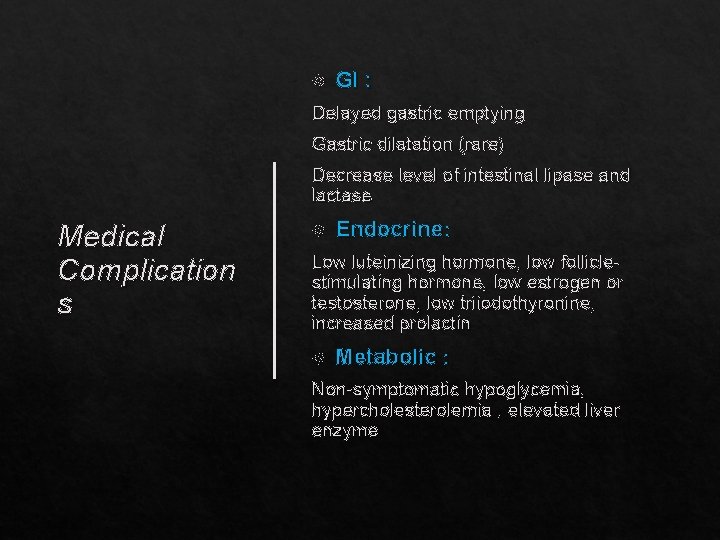
GI : Delayed gastric emptying Gastric dilatation (rare) Decrease level of intestinal lipase and lactase Medical Complication s Endocrine: Low luteinizing hormone, low folliclestimulating hormone, low estrogen or testosterone, low triiodothyronine, increased prolactin Metabolic : Non-symptomatic hypoglycemia, hypercholesterolemia , elevated liver enzyme
Presentation The term anorexia is a misnomer, because loss of appetite is usually rare, until late in the disorder. Patients usually come to medical attention when their weight loss becomes apparent Obsessive-compulsive behavior, depression, and anxiety are other psychiatric symptoms of anorexia nervosa most frequently noted clinically somatic complaints, especially epigastric discomfort, are usual complained Poor sexual adjustment is frequently described in patients with the disorder. 1. Many adolescent patients with anorexia nervosa have delayed psychosocial sexual development 2. In adults, a markedly decreased interest in sex often accompanies onset of the disorder Some female patients with anorexia nervosa come to medical attention because of amenorrhea, which often appears before their weight loss is noticeable
Spontaneous recovery without treatment. Recovery after a variety of treatments. Course and Prognos is A fluctuating course of weight gains followed by relapse. A gradually deteriorating course resulting in death caused by complications of starvation. About half of patients with anorexia nervosa eventually will have the symptoms of bulimia, usually within the first year after the onset of anorexia nervosa. Overall the prognosis is not good. Mortality rates range from 5 -18 % Suicide rate is higher in persons with binge eating-purging type of anorexia nervosa than in those with the restricting type.

Treatment Psychotherapy Cognitive-Behavior Therapy
Pharmacotherapy Treatm ent • Pharmacological studies have not yet identified any medication that yields definitive improvement of the core symptoms of anorexia nervosa. 1. Some reports support the use of cyproheptadine (Periactin), a drug with antihistaminic and anti-serotonergic properties, for patients with the restricting type of anorexia nervosa. 2. In patients with anorexia nervosa and coexisting depressive disorders, the depressive condition should be treated. 3. Trials of fluoxetine (Prozac) have resulted in some reports of weight gain, and serotonergic agents may yield positive responses in some cases. • Once an adequate nutritional status has been attained, the risk of serious adverse effects from the tricyclic drugs may decrease; in some patients, the depression improves with weight gain and normalized nutritional status.

Bulimia Nervosa
The term bulimia nervosa derives from the terms for “ox hunger” in Greek and “nervous involvement” in Latin. Bulimia nervosa is characterized by episodes of binge eating combined with inappropriate ways of stopping weight gain. Physical discomfort-for example, abdominal pain or nausea terminates the binge eating, which is often followed by feelings of guilt, depression, or self-disgust. Unlike patients with anorexia nervosa, those with bulimia nervosa typically maintain a normal body weight. Bulimia Nervosa
Bulimia nervosa is more prevalent than anorexia nervosa. Estimates of bulimia nervosa range from 1 to 4 percent of young women. Epidemiolo gy As with anorexia nervosa, bulimia nervosa is more common in women than in men. Its onset is often later in adolescence than that of anorexia nervosa. The onset may also occur in early adulthood. Although bulimia nervosa is often present in normal-weight young women, they sometimes have a history of obesity.
Etiology Biological Factors: • Neurotransmitters: Because antidepressants often benefit patients with bulimia nervosa and because serotonin has been linked to satiety, serotonin and norepinephrine have been implicated. • MRI suggests that overeating in bulimia nervosa may result from an exaggerated perception hunger signals related to sweet taste mediated by the right anterior insula area of the brain.
Etiology Social Factors: • Patients with bulimia nervosa, as with those with anorexia nervosa, tend to be high achievers and to respond to societal pressures to be slender. • As with anorexia nervosa patients, many patients with bulimia nervosa are depressed and have increased familial depression, but the families of patients with bulimia nervosa are generally less close and more conflictual than the families of those with anorexia nervosa • Patients with bulimia nervosa describe their parents as neglectful and rejecting.
Etiology Psychological factors: • Patients with bulimia nervosa, as with those with anorexia nervosa, have difficulties with adolescent demands, but patients with bulimia nervosa are more outgoing, angry, and impulsive than those with anorexia nervosa. • Alcohol dependence, shoplifting, and emotional lability (including suicide attempts) are associated with bulimia nervosa. • The struggle for separation from a maternal figure is played out in the ambivalence toward food; eating may represent a wish to fuse with the caretaker, and regurgitating may unconsciously express a wish for separation.
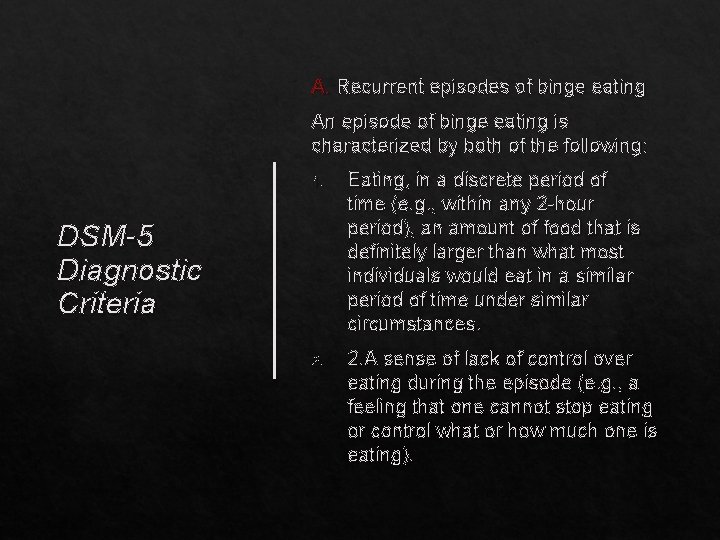
A. Recurrent episodes of binge eating An episode of binge eating is characterized by both of the following: 1. Eating, in a discrete period of time (e. g. , within any 2 -hour period), an amount of food that is definitely larger than what most individuals would eat in a similar period of time under similar circumstances. 2. A sense of lack of control over eating during the episode (e. g. , a feeling that one cannot stop eating or control what or how much one is eating). DSM-5 Diagnostic Criteria
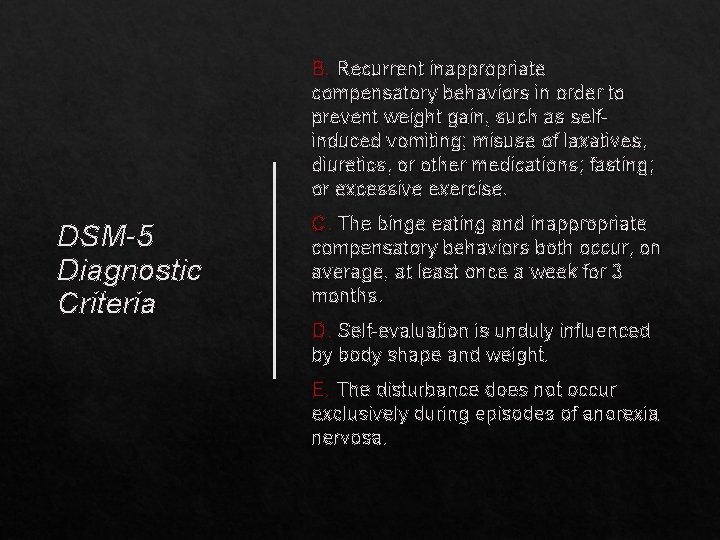
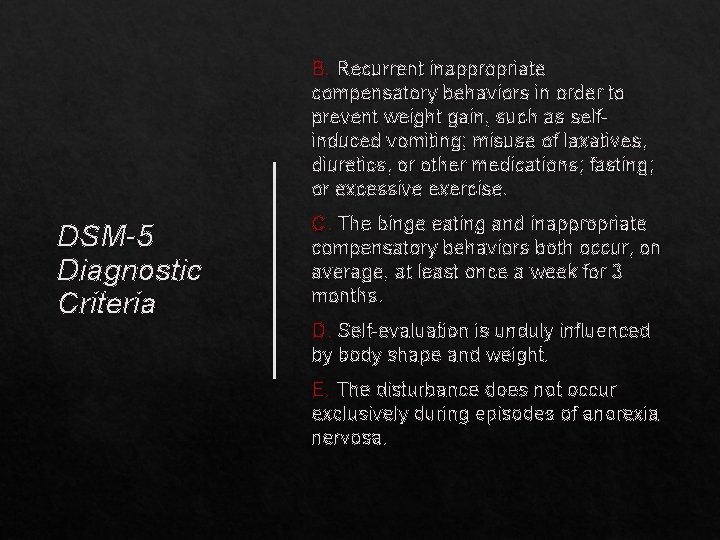
B. Recurrent inappropriate compensatory behaviors in order to prevent weight gain, such as selfinduced vomiting; misuse of laxatives, diuretics, or other medications; fasting; or excessive exercise. DSM-5 Diagnostic Criteria C. The binge eating and inappropriate compensatory behaviors both occur, on average, at least once a week for 3 months. D. Self-evaluation is unduly influenced by body shape and weight. E. The disturbance does not occur exclusively during episodes of anorexia nervosa.
Induced vomiting is common : Vomiting decreases the abdominal pain and the feeling of being bloated and allows patients to continue eating without fear of gaining weight. The acid content of vomitus can damage tooth enamel, a not uncommon finding in patients with the disorder. Presentation Depression, sometimes called post binge anguish, often follows the episode. During binges, patients eat food that is sweet, high in calories, and generally soft or smooth textured, such as cakes and pastry. Some patients prefer bulky foods without regard to taste. The food is eaten secretly and rapidly and is sometimes not even chewed.
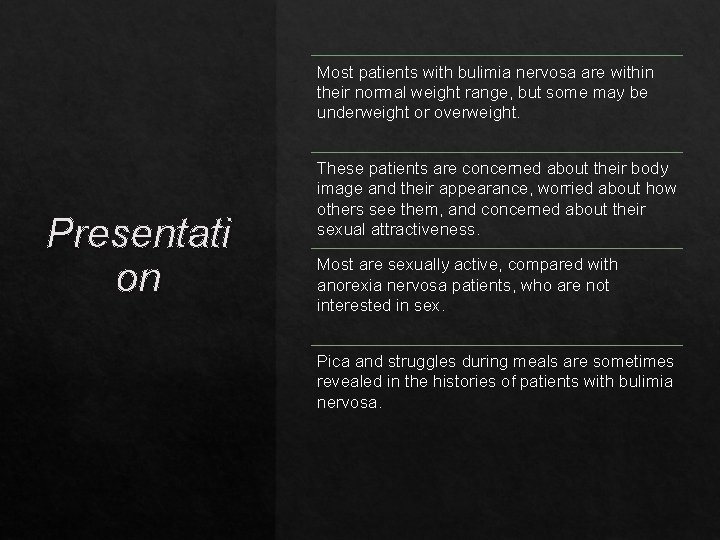
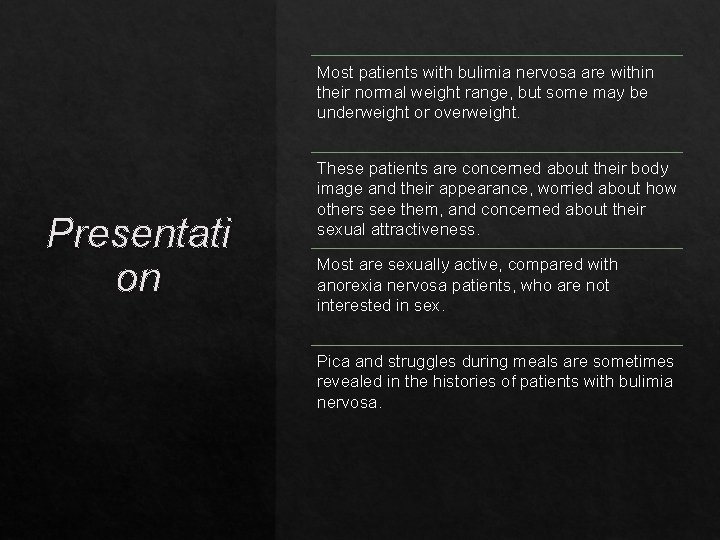
Most patients with bulimia nervosa are within their normal weight range, but some may be underweight or overweight. Presentati on These patients are concerned about their body image and their appearance, worried about how others see them, and concerned about their sexual attractiveness. Most are sexually active, compared with anorexia nervosa patients, who are not interested in sex. Pica and struggles during meals are sometimes revealed in the histories of patients with bulimia nervosa.
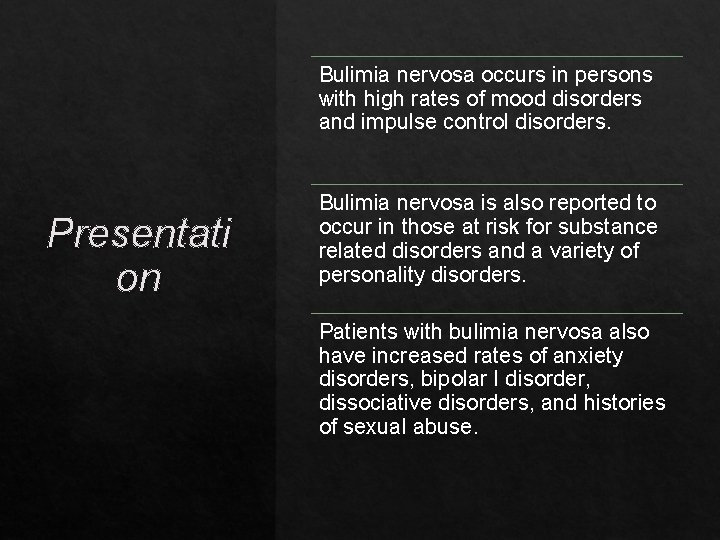
Bulimia nervosa occurs in persons with high rates of mood disorders and impulse control disorders. Presentati on Bulimia nervosa is also reported to occur in those at risk for substance related disorders and a variety of personality disorders. Patients with bulimia nervosa also have increased rates of anxiety disorders, bipolar I disorder, dissociative disorders, and histories of sexual abuse.
Course and Prognosis Bulimia nervosa is characterized by higher rates of partial and full recovery compared with anorexia nervosa. Patients who are untreated tend to remain chronic or may show small, but generally unimpressive, degrees of improvement with time. The mortality rate for bulimia nervosa has been estimated at 2 percent per decade according to DSM-5.

Treatment Psychotherapy Cognitive-Behavior Therapy (CBT)
Treatment Most patients with uncomplicated bulimia nervosa do not require hospitalization. In general, patients with bulimia nervosa are not as secretive about their symptoms as patients with anorexia nervosa. Therefore, outpatient treatment is usually not difficult, but psychotherapy is frequently stormy and may be prolonged. In some cases when eating binges are out of control, outpatient treatment does not work or a patient exhibits such additional psychiatric symptoms as suicidality and substance abuse , hospitalization may become necessary. In addition, electrolyte and metabolic disturbance resulting from severe purging may necessitate hospitalization.
Treatment Pharmacotherapy • Antidepressant medications have been shown to be helpful in treating bulimia; they can reduce binge eating and purging independent of the presence of a mood disorder. This includes the selective serotonin reuptake inhibitors (SSRIs), such as fluoxetine (Prozac). The only FDA approved drug for bulimia nervosa is fluoxetine. Medication is helpful in patients with comorbid depressive disorders and bulimia nervosa.

Binge Eating Disorder
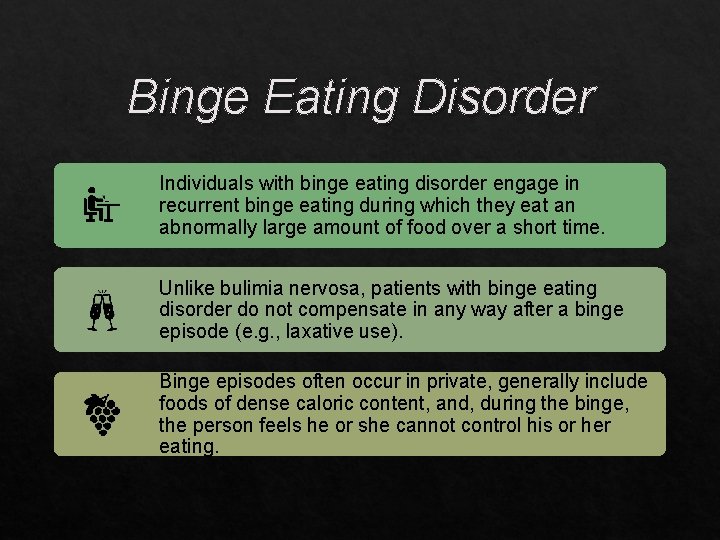
Binge Eating Disorder Individuals with binge eating disorder engage in recurrent binge eating during which they eat an abnormally large amount of food over a short time. Unlike bulimia nervosa, patients with binge eating disorder do not compensate in any way after a binge episode (e. g. , laxative use). Binge episodes often occur in private, generally include foods of dense caloric content, and, during the binge, the person feels he or she cannot control his or her eating.
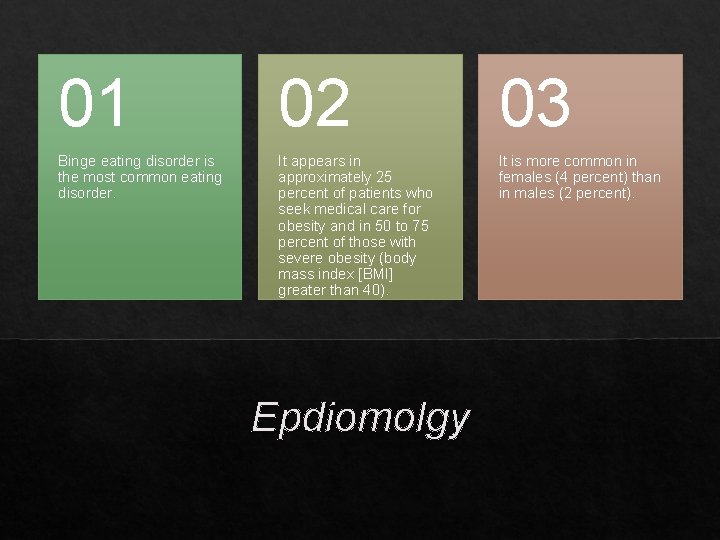
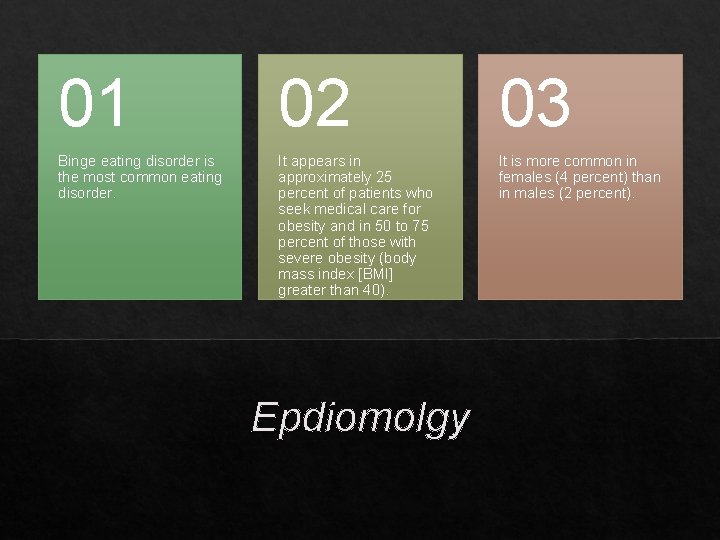
01 02 03 Binge eating disorder is the most common eating disorder. It appears in approximately 25 percent of patients who seek medical care for obesity and in 50 to 75 percent of those with severe obesity (body mass index [BMI] greater than 40). It is more common in females (4 percent) than in males (2 percent). Epdiomolgy
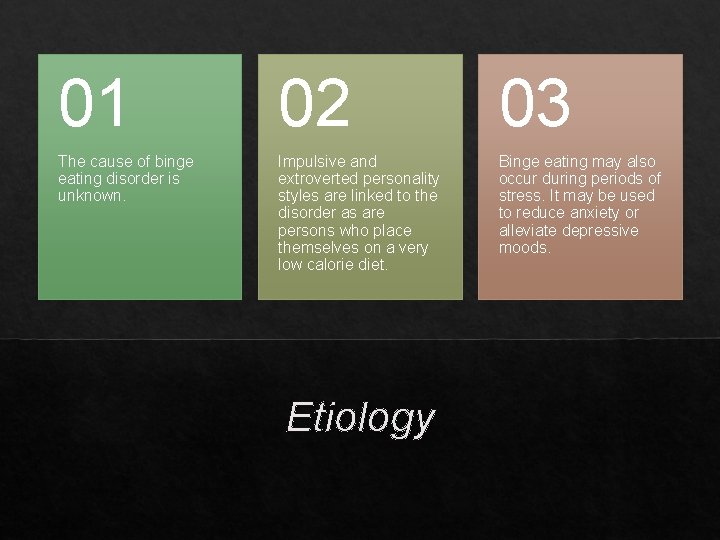
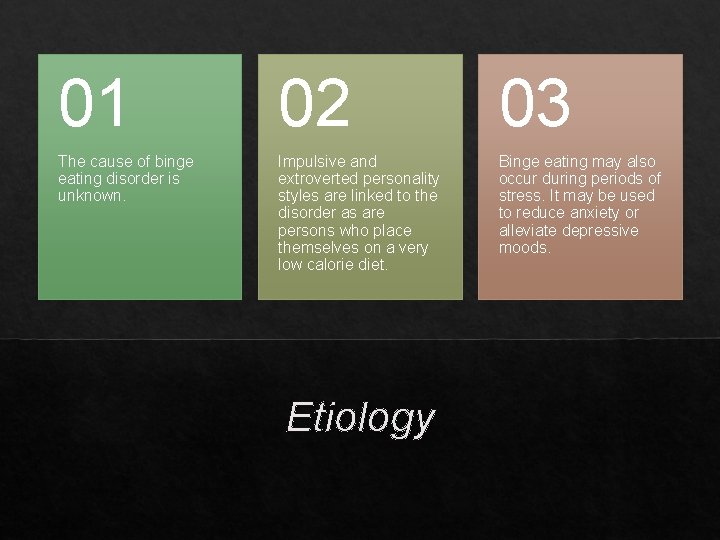
01 02 03 The cause of binge eating disorder is unknown. Impulsive and extroverted personality styles are linked to the disorder as are persons who place themselves on a very low calorie diet. Binge eating may also occur during periods of stress. It may be used to reduce anxiety or alleviate depressive moods. Etiology
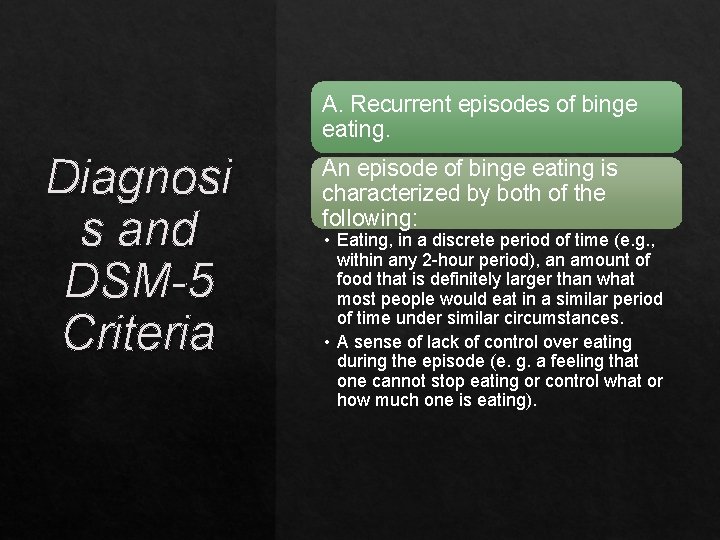
A. Recurrent episodes of binge eating. Diagnosi s and DSM-5 Criteria An episode of binge eating is characterized by both of the following: • Eating, in a discrete period of time (e. g. , within any 2 -hour period), an amount of food that is definitely larger than what most people would eat in a similar period of time under similar circumstances. • A sense of lack of control over eating during the episode (e. g. a feeling that one cannot stop eating or control what or how much one is eating).
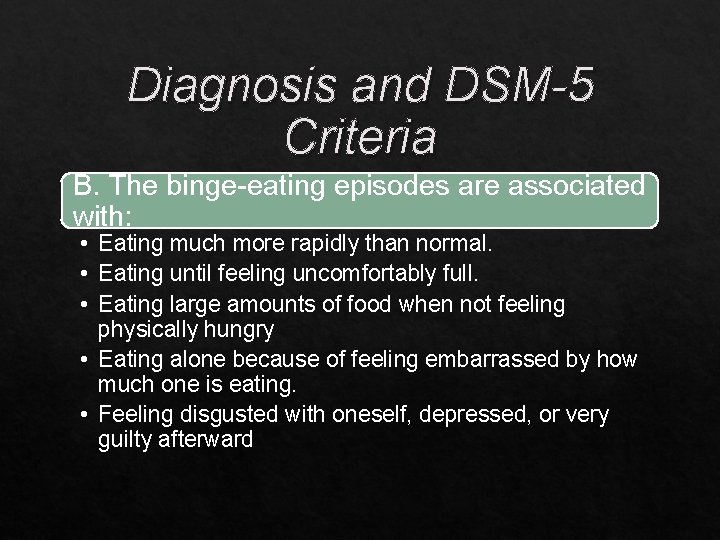
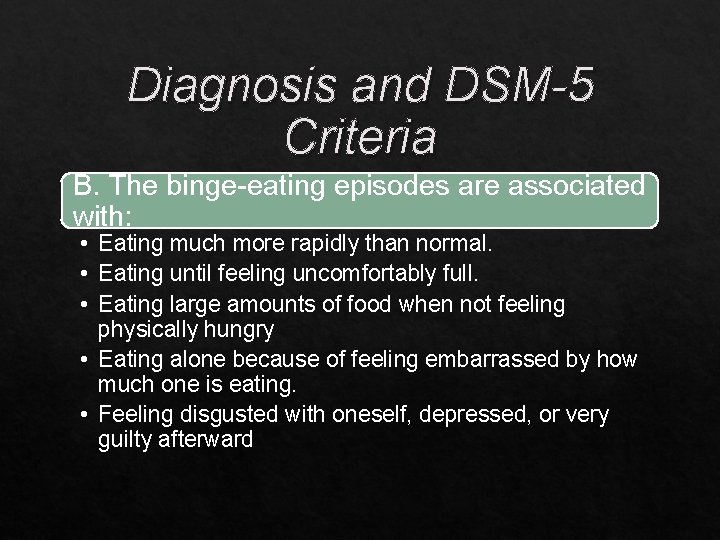
Diagnosis and DSM-5 Criteria B. The binge-eating episodes are associated with: • Eating much more rapidly than normal. • Eating until feeling uncomfortably full. • Eating large amounts of food when not feeling physically hungry • Eating alone because of feeling embarrassed by how much one is eating. • Feeling disgusted with oneself, depressed, or very guilty afterward
C. Marked distress regarding binge eating is present. Diagnosi s and DSM-5 Criteria D. The binge eating occurs, on average, at least once a week for 3 months. E. The binge eating is not associated with the recurrent use of inappropriate compensatory behavior as in bulimia nervosa and does not occur exclusively during the course of bulimia nervosa or anorexia nervosa.
Bulimia nervosa Binge eating disorder and bulimia nervosa share the same can feature of recurrent binge eating. Differential Diagnosis Binge eating disorder is distinct from bulimia nervosa, however, in that binge eating discs der patients do not report recurrent compensatory behavior such as vomiting, laxative abuse, or excessive dieting. Anorexia nervosa Binge eating disorder is distinct from anorexia nervosa in that patients do not exhibit an excessive drive for thinness and are of normal weight or are obese.
Course and Prognosis Little is known about the course of binge eating disorder. Severe obesity is a long-term effect in over 3 percent of patients with the disorder. One prospective study of women in the community with binge eating disorder suggested that by 5 years of follow up fewer than one fifth of the sample still had clinically significant eating disorder symptoms
Psychotherapy Cognitive-Behavior Therapy (CBT) is the most effective psychological treatment. Psychopharmacother apy SSRIs Treatment Most studies show that medication added to CBT is more effective than medication alone.
The End
 Malingering
Malingering Ceds eating disorder
Ceds eating disorder Fear food list
Fear food list Kate bosworth anorexia
Kate bosworth anorexia Walden iop
Walden iop Eating disorder in which people overeat compulsively
Eating disorder in which people overeat compulsively Hypothalamus and eating disorders
Hypothalamus and eating disorders Binge eating disorder
Binge eating disorder Yorkshire centre for eating disorders
Yorkshire centre for eating disorders Cedrd certification
Cedrd certification Eating disorder coalition of iowa
Eating disorder coalition of iowa Eating disorder syptoms
Eating disorder syptoms Anorexic barbie
Anorexic barbie Pamela anderson eating disorder
Pamela anderson eating disorder Eating disorder clinic halifax
Eating disorder clinic halifax Kate moss eating disorder
Kate moss eating disorder Rosli bin ahmad
Rosli bin ahmad Cstr in parallel
Cstr in parallel Advantages of filtration
Advantages of filtration Autocratic leadership
Autocratic leadership Political services of sir syed ahmad khan
Political services of sir syed ahmad khan Logo smk ahmad pekan
Logo smk ahmad pekan Power compensated dsc
Power compensated dsc Ibrahim primary school
Ibrahim primary school Yamin ahmad
Yamin ahmad Kausar ahmad
Kausar ahmad Characteristics of a good research
Characteristics of a good research Nur ahmad husin
Nur ahmad husin Cerpen ibu bapa
Cerpen ibu bapa Nephrotic syndrome causes
Nephrotic syndrome causes Rabiah ahmad
Rabiah ahmad Dr shahzad ahmad
Dr shahzad ahmad Waseem ahmad khan
Waseem ahmad khan Compensated shock
Compensated shock Dr nur ahmad tabri
Dr nur ahmad tabri Fouzia khursheed ahmad
Fouzia khursheed ahmad Phuc dao
Phuc dao Ahmad aulia jusuf
Ahmad aulia jusuf Ahmad rafay alam
Ahmad rafay alam Ahmad albar
Ahmad albar Ahmad boestamam sejarah tingkatan 4
Ahmad boestamam sejarah tingkatan 4 Hadi ahmad md
Hadi ahmad md Ahmad kamal
Ahmad kamal Ain syafinaz mohd razip
Ain syafinaz mohd razip