Somatoform Disorders Somatization Disorder Conversion Disorder Pain Disorder
- Slides: 60
Somatoform Disorders Somatization Disorder Conversion Disorder Pain Disorder Hypochondriasis Factitious Disorder LCSW Psychiatry Annabelle Winne, Introduction to April 16, 2010 annabellewinne@hotmail. com, 332 -2046
Somatoform Disorders: Introduction l l Somatic: (Gk soma body) of, relating to, or affecting the body Assessment tools: medical tests, DSM, defensive structures, attitudes and beliefs, childhood experiences – l Person-as-a-whole/person’s story Spectrum of intensity & duration – Mild intensity, time-limited experiences/symptoms are normal
Theories of Etiology: Stress-Diathesis Model l DIATHESIS/PREDISPOSITION – – l PLUS exposure to STRESS – – l l biological: genetics, IQ, personality environmental: poverty, family dynamics biological: brain damage, biotoxins environmental: injury, trauma, developmental expectation RESULTS IN Dysfunction Multi-deterministic origin of symptoms/disorder – Must have both diathesis and stress to have dysfunction
Theories of Etiology: Psychodynamic Model l External stressor triggers an emotional conflict which is manifested within a physical symptom – Primary gain (intra-psychic) l – Does the symptom in some way resolve the precipitating conflict/stressor? (Avoidance of social role or upcoming change/transition…. ) Secondary gain (inter-psychic) l Reinforcement beyond primary gain, something achieved through taking on sick role (attention, nurturance)
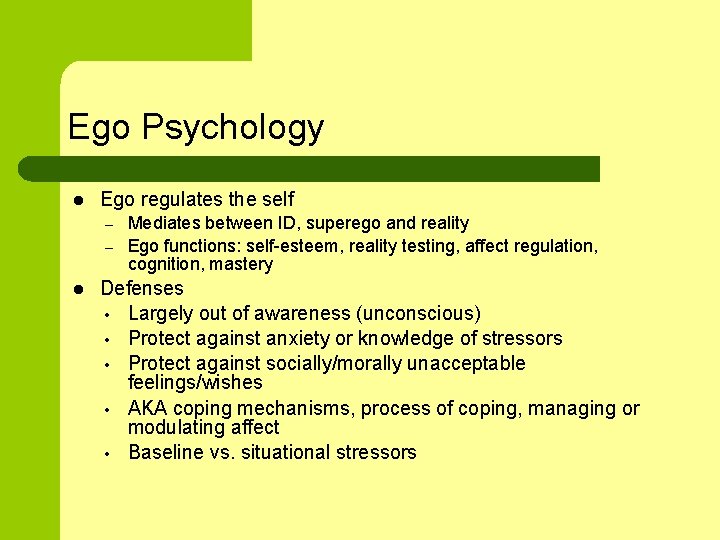
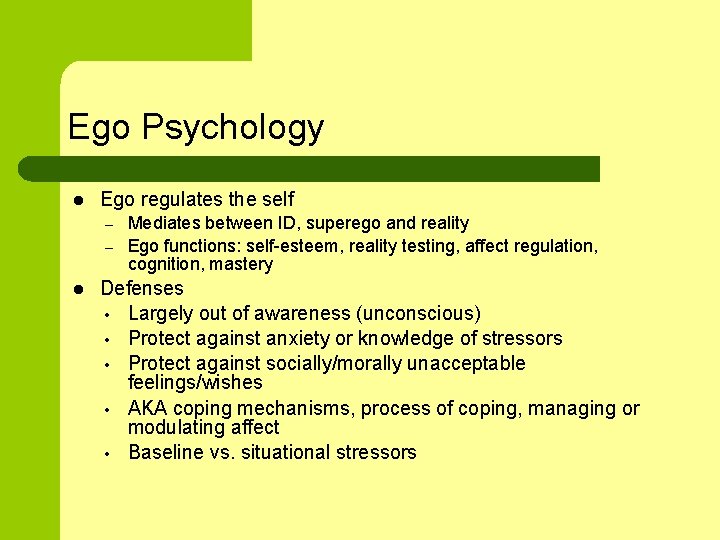
Ego Psychology l Ego regulates the self – – l Mediates between ID, superego and reality Ego functions: self-esteem, reality testing, affect regulation, cognition, mastery Defenses • Largely out of awareness (unconscious) • Protect against anxiety or knowledge of stressors • Protect against socially/morally unacceptable feelings/wishes • AKA coping mechanisms, process of coping, managing or modulating affect • Baseline vs. situational stressors
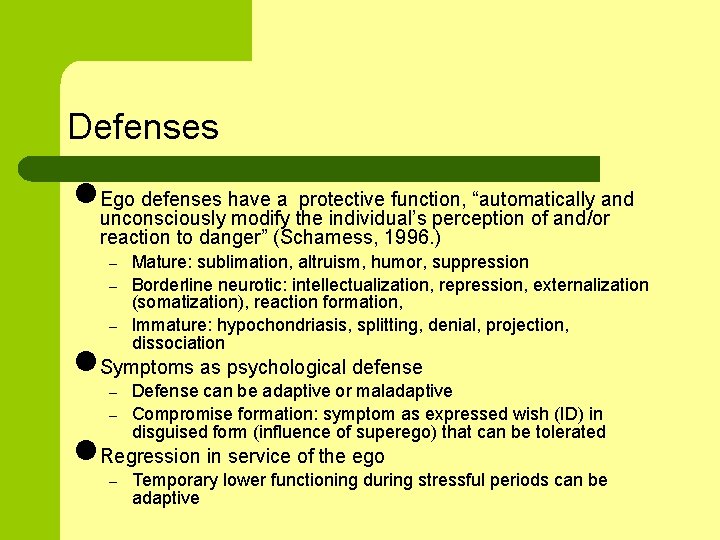
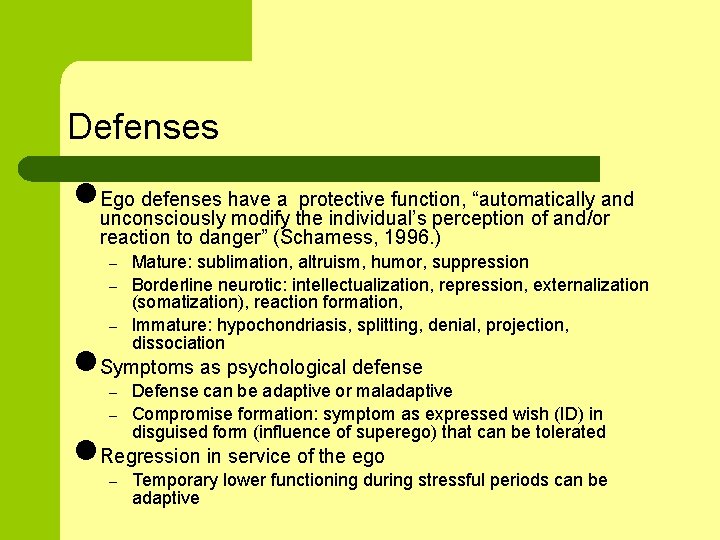
Defenses l. Ego defenses have a protective function, “automatically and unconsciously modify the individual’s perception of and/or reaction to danger” (Schamess, 1996. ) – – – Mature: sublimation, altruism, humor, suppression Borderline neurotic: intellectualization, repression, externalization (somatization), reaction formation, Immature: hypochondriasis, splitting, denial, projection, dissociation l. Symptoms as psychological defense – – Defense can be adaptive or maladaptive Compromise formation: symptom as expressed wish (ID) in disguised form (influence of superego) that can be tolerated l. Regression in service of the ego – Temporary lower functioning during stressful periods can be adaptive
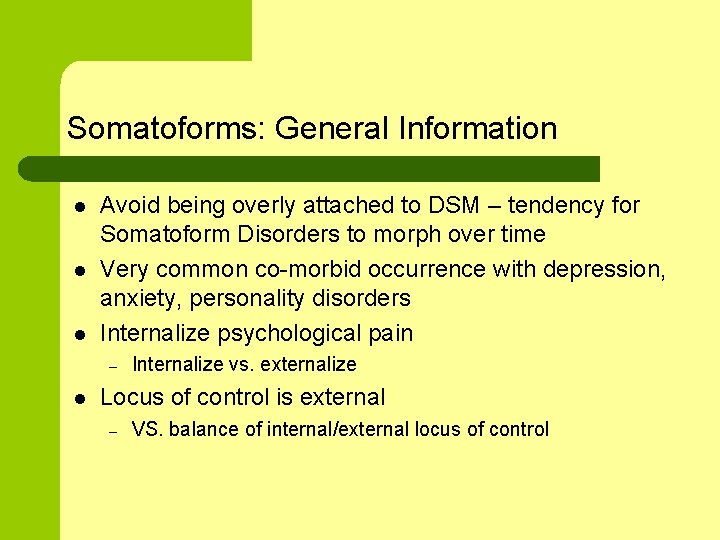
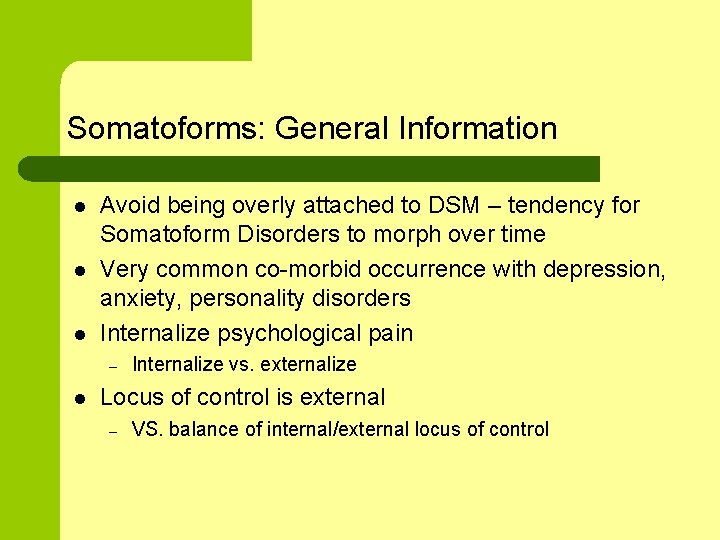
Somatoforms: General Information l l l Avoid being overly attached to DSM – tendency for Somatoform Disorders to morph over time Very common co-morbid occurrence with depression, anxiety, personality disorders Internalize psychological pain – l Internalize vs. externalize Locus of control is external – VS. balance of internal/external locus of control
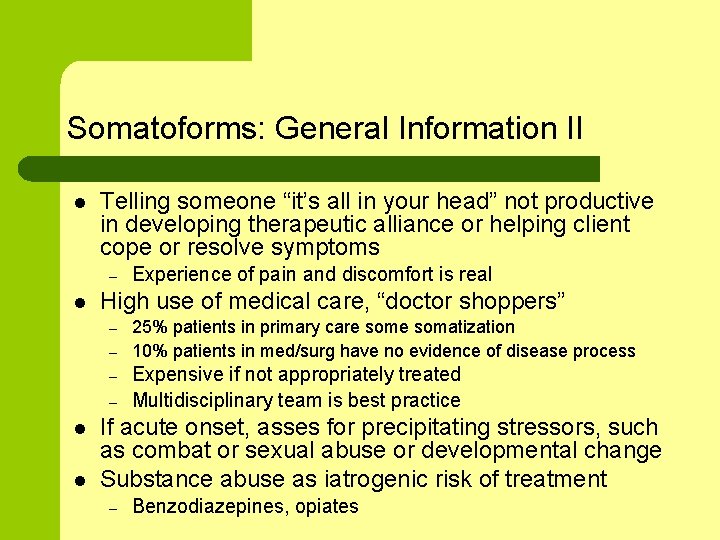
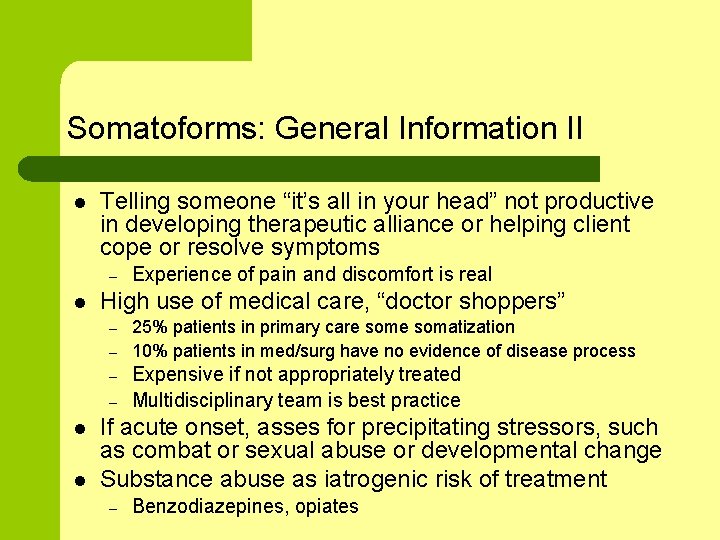
Somatoforms: General Information II l Telling someone “it’s all in your head” not productive in developing therapeutic alliance or helping client cope or resolve symptoms – l High use of medical care, “doctor shoppers” – – l l Experience of pain and discomfort is real 25% patients in primary care somatization 10% patients in med/surg have no evidence of disease process Expensive if not appropriately treated Multidisciplinary team is best practice If acute onset, asses for precipitating stressors, such as combat or sexual abuse or developmental change Substance abuse as iatrogenic risk of treatment – Benzodiazepines, opiates
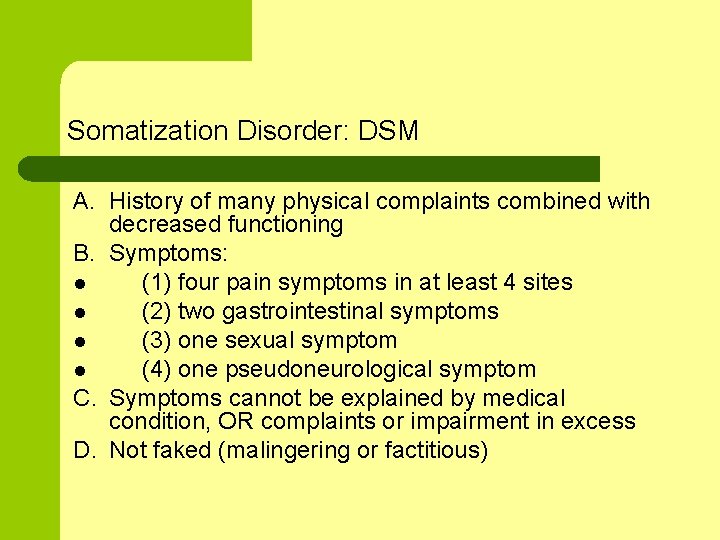
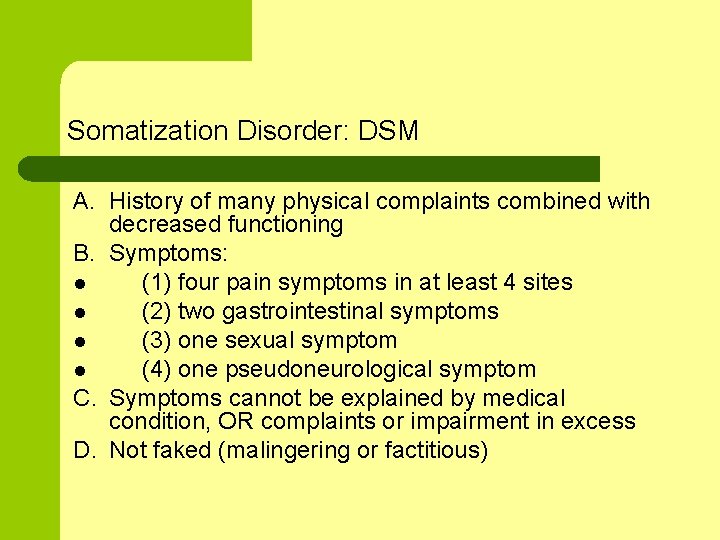
Somatization Disorder: DSM A. History of many physical complaints combined with decreased functioning B. Symptoms: l (1) four pain symptoms in at least 4 sites l (2) two gastrointestinal symptoms l (3) one sexual symptom l (4) one pseudoneurological symptom C. Symptoms cannot be explained by medical condition, OR complaints or impairment in excess D. Not faked (malingering or factitious)
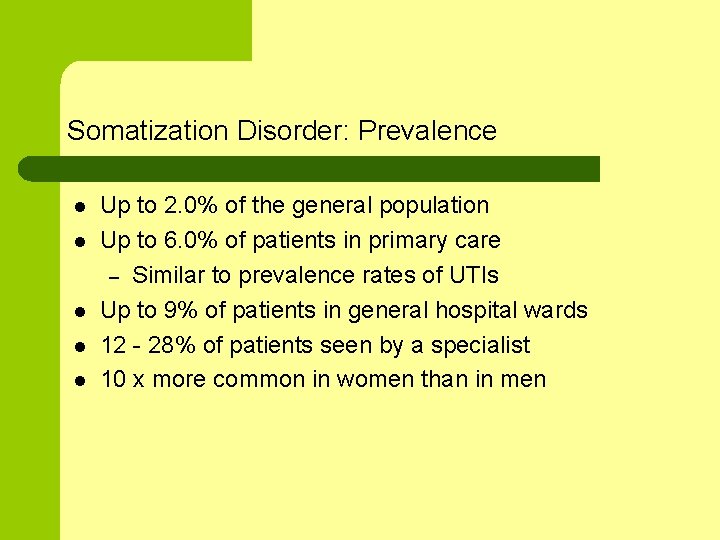
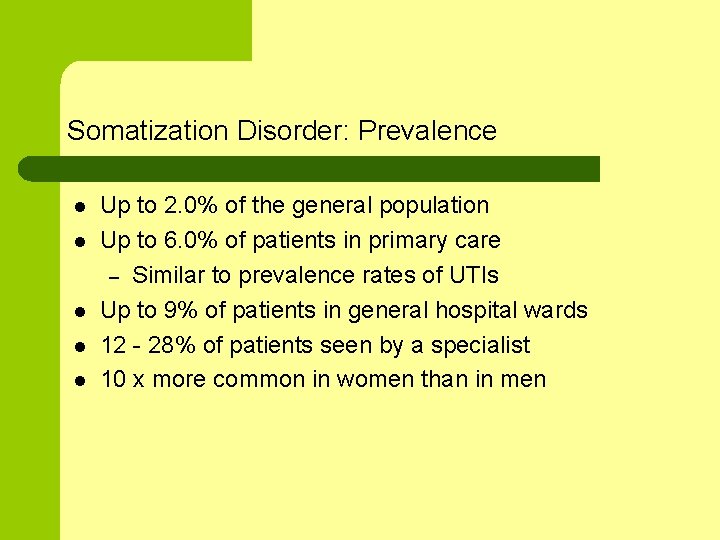
Somatization Disorder: Prevalence l l l Up to 2. 0% of the general population Up to 6. 0% of patients in primary care – Similar to prevalence rates of UTIs Up to 9% of patients in general hospital wards 12 - 28% of patients seen by a specialist 10 x more common in women than in men
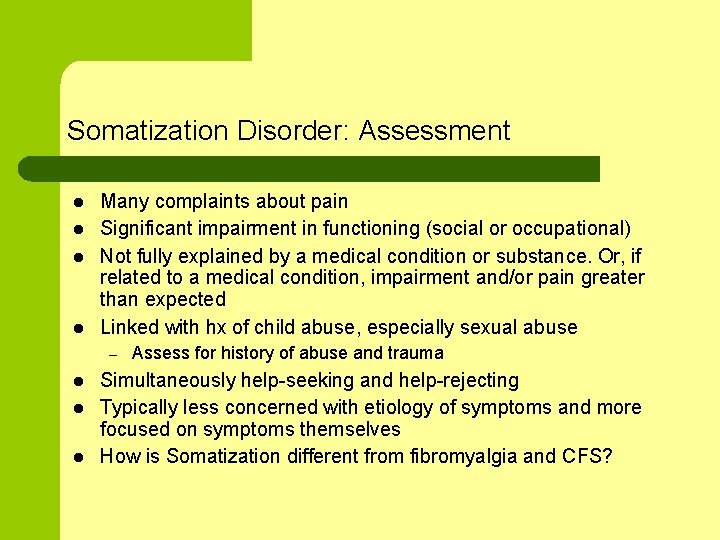
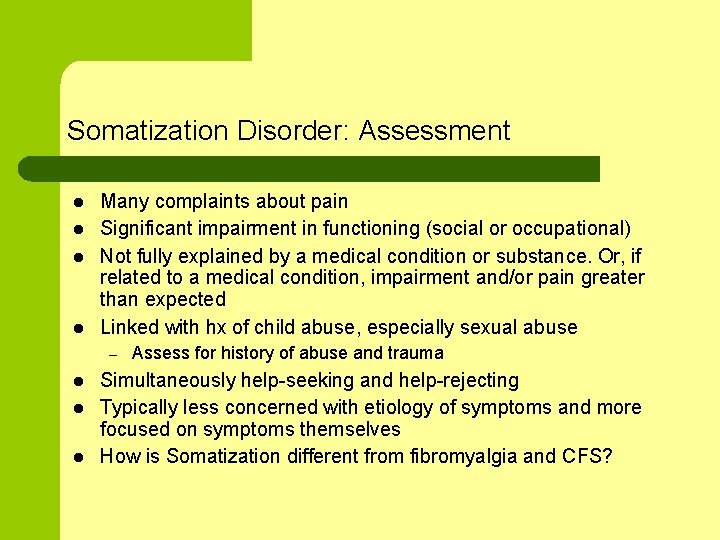
Somatization Disorder: Assessment l l Many complaints about pain Significant impairment in functioning (social or occupational) Not fully explained by a medical condition or substance. Or, if related to a medical condition, impairment and/or pain greater than expected Linked with hx of child abuse, especially sexual abuse – l l l Assess for history of abuse and trauma Simultaneously help-seeking and help-rejecting Typically less concerned with etiology of symptoms and more focused on symptoms themselves How is Somatization different from fibromyalgia and CFS?
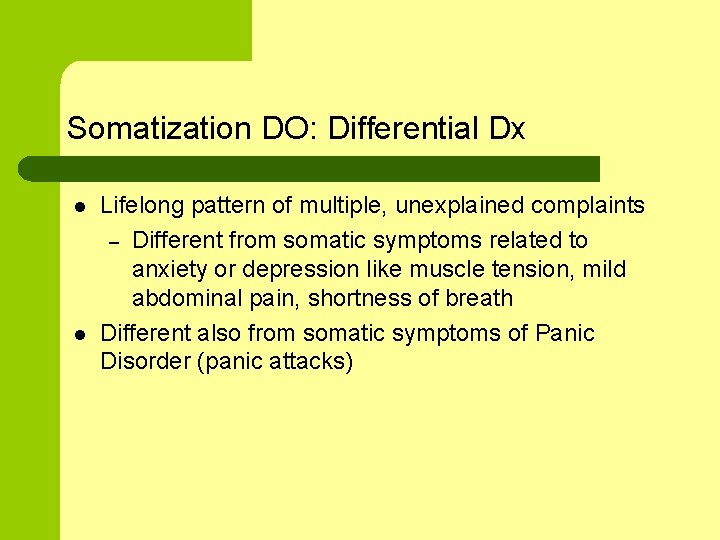
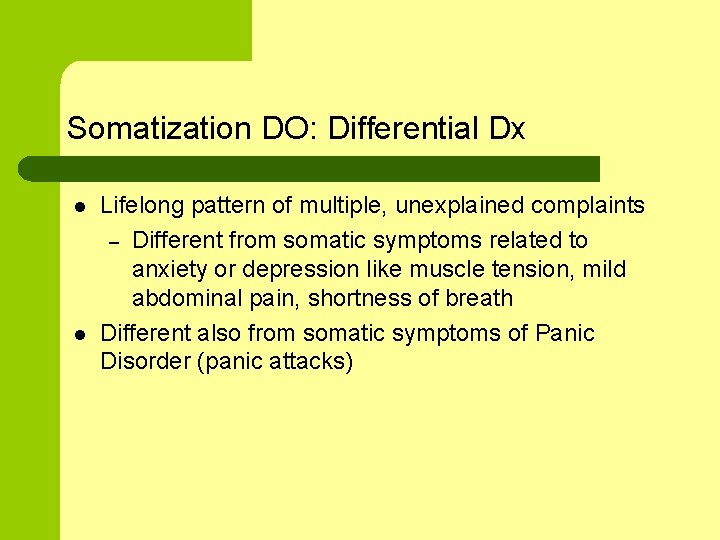
Somatization DO: Differential Dx l l Lifelong pattern of multiple, unexplained complaints – Different from somatic symptoms related to anxiety or depression like muscle tension, mild abdominal pain, shortness of breath Different also from somatic symptoms of Panic Disorder (panic attacks)
Somatization DO: Course of Illness l Chronic with changes in acuity over time – l l l Typical episode 6 -9 months, remission for 9 -12 months Full remission is rare One study showed 95% of patients with somatization disorder had been to health care provider in past 6 months vs. 56% of other community residents Typically episodes of illness are secondary to period of stress – – New symptoms Or seeking health care more frequently l. Accurate diagnosis is key – Otherwise pt is referred to multiple doctors and specialists with many unnecessary, expensive diagnostic procedures and without appropriate treatment
Somatization DO: Common Characteristics l “Sicker than the sick” – l l Pattern of many, many unexplained physical somatic complaints Current DSM – l Poor physical, social and mental health when compared to people with chronic health problems Appear in adolescence and meet full criteria by 30 y. o. , can also develop in late 30’s “Chaotic” social lives – – Many losses Unstable work hx
Somatization Disorder: Treatment l Lead provider for primary care, collaborate with necessary specialists – l R/O underlying physical etiology (cardiac, gastro, neurological etc. ) – – l Very important specialist know about Somatization DO diagnosis Do repeatedly over time as physical disease can develop in future Not either/or (mental or physical) Order additional procedures/tests based on objective data (signs), not subjective data (symptoms) – “conservative management” of comorbid medical conditions – – – Very important to refrain from unnecessary testing – counter indicated with this population because it avoids the recommended treatment Also, pts tend to be very sensitive to invasive procedures Risk of iatrogenic injury
Somatization Disorder: Treatment II l l Brief, regular appointments every 4 -6 weeks – Conduct “partial exam of organ system” that pt is complaining about – More frequent during initial stage of treatment and flare ups Engage, develop trust, refer pt to mental health and continue to treat – Not a dump, pts will sense this and seek out a “better” health care provider – Important how you frame referral – someone who can see pt more frequently to help with stress of symptoms, to help with cooccurring depression or anxiety, to help cope with the discomfort and difficulty of the symptoms Help pt validate and contain their feelings - anxiety, pain, disappointment, wish for relief – Rx for reassurance, validation and empathy Psychoeducation about how stress effects chronic pain
Somatization Disorder: Treatment III l Consult with psychiatric provider ASAP to lessen your anxiety/frustration and result in better tx for pt – – l Team-based is preferable, may be necessary for pt to f/u with medications for co-morbid disorders – l Avoid waiting until your frustration mounts, pt has (yet another) negative relationship with a provider Benefit of in-house psychiatric providers, can bring provider into your office at appointment time Phone calls from team members prompting meds Referral to therapy – individual and/or group – – – Biofeedback Mindfulness-Based Stress Reduction CBT groups
Somatization Disorder: Treatment IV l l Treat comorbid psychiatric disorders – 83 -100% of pts had comorbid conditions – 55% major depression – 34% anxiety disorder – 26% panic disorder – 61% with 1+ personality disorder – avoidant, paranoid and obsessive compulsive Predict difficulties with medications – Pt may somaticize normative side effects – “I stopped using it on the second day because I got a headache” – May have poor follow through – May change dosage without consulting you
Somatization Disorder: Treatment V l Motivational interviewing with goal of referral to mental health provider – – – Be open to very small steps forward; these can be easy to miss, openings for “change talk, ” if provider is mired in attitude of hopelessness Metaphor of tennis ‣ If you can’t see progress, look for smaller, more detailed footwork. What might “change talk” look like for people who somatize?
Somatization Disorder: Case Studies l ER patient transferred from Brighton for SI statement when wanting assessment for exacerbation in chronic pain – l Family with somatic tendencies – – – l Insisted on invasive procedure Mom, dad, daughter Meds for daughter Mom hx of cancer, also pain. Initially no PCP. Suboxone. Adolescent girl with hx of sexual abuse dx with connective tissue disease, pain in other systems (pelvic, gastro, neuro) who had addiction to Percoset – – Stress (abuse, parental response to it) + predisposition (family coping styles, genetic load) Question of primary and secondary gain
Conversion Disorder: Introduction l l l Also known as “hysteria” Term “conversion” was coined by Freud who developed hypothesis that anxiety was unconsciously “converted” into physical symptom Psychoanalytic approach – the symptom simultaneously represents the conflict and provides a solution to it – a “symbolic condensation of the unconscious conflict” (Ford, 2001) – A man anxious about his rage has a paralyzed arm. Thus, he can’t hit anyone.
Conversion Disorder: DSM A. Loss of function of a voluntary motor system or sense organ – – B. C. D. E. Not accounted for by medical or neurological condition Causes significant functional impairment Excludes culturally sanctioned behavior Examples: paralysis, pregnancy in non-pregnant woman, vocal cord dysfunction, pseudoseizures Symptom preceded by stressor Not faked (malingering or factitious) Symptom not limited to pain or sexual dysfunction Symptom/deficit: motor, sensory, seizures
Conversion Disorder: Prevalence l l l All ages – children, adolescents, adults, geriatric In children, occurs equally between boys and girls In adults diagnosed much more in women – l l l Except in predominately male settings (military) 5 -10% of hospital patients referred for psychiatric consultation Up to 14% of Med/Surgical Inpts Up to 3% of neurology patients
Conversion Disorder: Assessment l l Loss of function of a voluntary motor system or sense organ Rule out underlying physical illness – l Very important to consider underlying neurological disorder at present time of conversion disorder and also in future – l Does pt have conscious control of symptom? (Malingering, Factitous DO) Is start of symptom associated with stressor or psychological conflict? Sometimes recent contact with someone who modeled symptom Often associated with depression – l Apparent tie between Conversion DO and Neurological Dysfunction Requires a subjective decision on the part of the provider – l Reflexes in paralyzed limb, EEG is normal, nerve conduction speed WNL Occasionally occurs in people diagnosed with schizophrenia May or may not have personality disorder – If yes, common in dependent and histrionic PDO
Conversion Disorder: Treatment l “Three P’s” to aid with formulation and treatment plan – – – l Predisposition l Tendency to somatize and rigid personality structure l Impaired ability or cultural norm against explicit verbal communication l Underlying psychiatric or neurological disorders Precipitating stressor l Psychological conflicts l Traumatic events (combat, sexual abuse) Perpetuating factors l Primary gain (intra-psychic) - does the symptom in some way resolve the precipitating conflict/stressor? l Secondary gain (inter-psychic) - reinforcement for taking on sick role Treatment consists of symptom relief and also consideration of factors/stressors/conflict which was a precipitant – Some consider Conversion Disorder a symptom of another disorder
Acute Conversion Disorder: Treatment II l l Good prognosis in people with good health prior to disorder, clear precipitating stressor and no cooccurring psychiatric disorder – symptom can stop quickly Reassurance that symptom is not a sign of serious medical disease/problem
Acute Conversion Disorder: Treatment III l Suggestion/Psychoeducation – Gentle and supportive suggestion/interpretation/confrontation l l Symptom as response to stressor – Message from brain to body part is not working properly – Give words to repressed affect/conflict/cognition – Regain use of organ/limb through physical therapy – Validate discomfort of precipitating stressor Lorazepam l l l Repressed affect may emerge Gain historical information May have reduction in symptom Medical risks (compromised cardiac status) Contraindicated in patients who are opposed to procedure and with people who have psychosis
Chronic Conversion Disorder: Treatment IV l Chronic – Worse prognosis related to symptom lasting longer than 6 months, older age and significant secondary gain – Behavior modification – Family therapy – Physical therapy, occupational therapy, speech therapy l Disuse atrophy
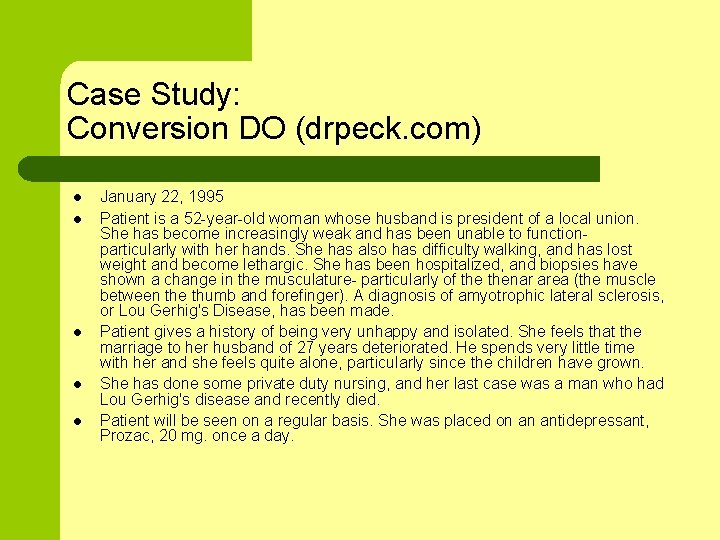
Case Study: Conversion DO (drpeck. com) l l l January 22, 1995 Patient is a 52 -year-old woman whose husband is president of a local union. She has become increasingly weak and has been unable to functionparticularly with her hands. She has also has difficulty walking, and has lost weight and become lethargic. She has been hospitalized, and biopsies have shown a change in the musculature- particularly of thenar area (the muscle between the thumb and forefinger). A diagnosis of amyotrophic lateral sclerosis, or Lou Gerhig's Disease, has been made. Patient gives a history of being very unhappy and isolated. She feels that the marriage to her husband of 27 years deteriorated. He spends very little time with her and she feels quite alone, particularly since the children have grown. She has done some private duty nursing, and her last case was a man who had Lou Gerhig's disease and recently died. Patient will be seen on a regular basis. She was placed on an antidepressant, Prozac, 20 mg. once a day.
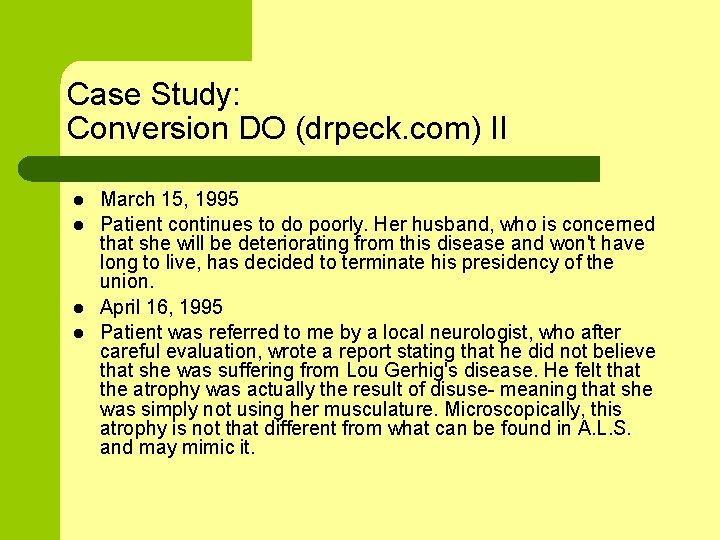
Case Study: Conversion DO (drpeck. com) II l l March 15, 1995 Patient continues to do poorly. Her husband, who is concerned that she will be deteriorating from this disease and won't have long to live, has decided to terminate his presidency of the union. April 16, 1995 Patient was referred to me by a local neurologist, who after careful evaluation, wrote a report stating that he did not believe that she was suffering from Lou Gerhig's disease. He felt that the atrophy was actually the result of disuse- meaning that she was simply not using her musculature. Microscopically, this atrophy is not that different from what can be found in A. L. S. and may mimic it.
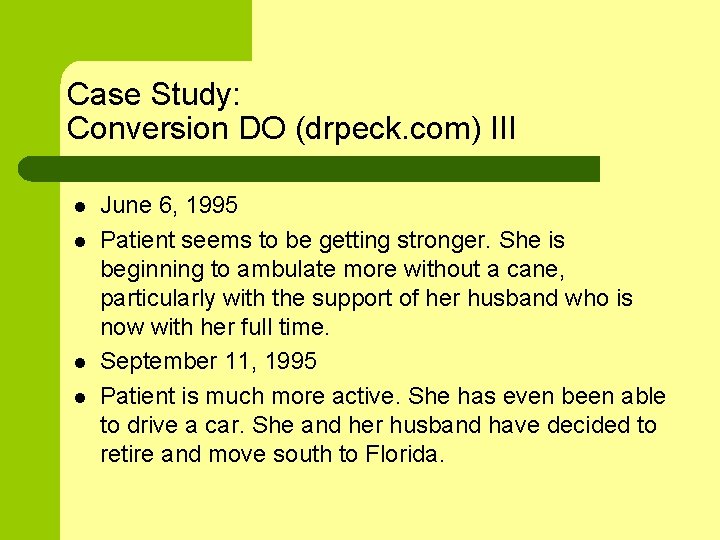
Case Study: Conversion DO (drpeck. com) III l l June 6, 1995 Patient seems to be getting stronger. She is beginning to ambulate more without a cane, particularly with the support of her husband who is now with her full time. September 11, 1995 Patient is much more active. She has even been able to drive a car. She and her husband have decided to retire and move south to Florida.
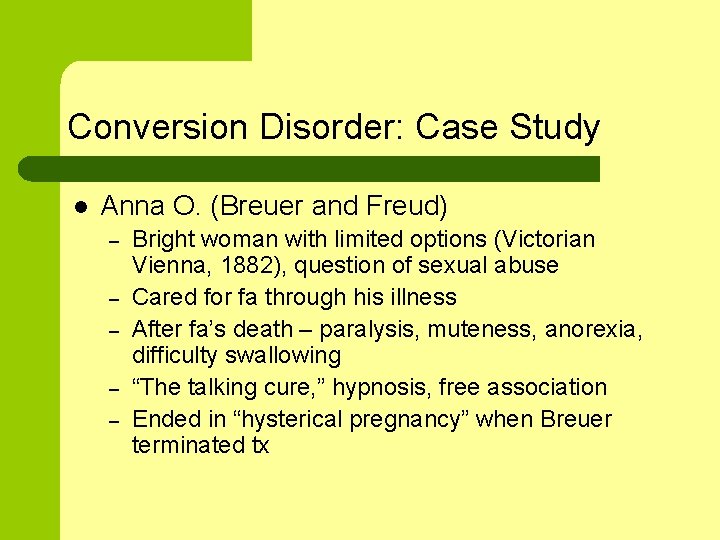
Conversion Disorder: Case Study l Anna O. (Breuer and Freud) – – – Bright woman with limited options (Victorian Vienna, 1882), question of sexual abuse Cared for fa through his illness After fa’s death – paralysis, muteness, anorexia, difficulty swallowing “The talking cure, ” hypnosis, free association Ended in “hysterical pregnancy” when Breuer terminated tx
Conversion Disorder: Case Study l Pt transferred to ED due to paralysis – – Medical work-up negative Worked on ladders, chin strap stuck on ladder and pt was immobilized for approx. 3 minutes
Conversion Disorder: Case Study l Adolescent girl with hx of sexual abuse by relative – – “Pseudoseizures” started after initial psychiatric hospitalization Self-harm became severe and multi-faceted Episodes became ritualized daily event at arranged time Question of Conversion DO vs. Dissociative DO
Pain Disorder: DSM A. Pain is severe and prominent B. It results in functional impairment C. Psychological factors have significant role in pain D. Not faked (malingering or factitious)
Pain Disorder : DSM II l Associated with Psychological Factors – l Associated with both Psychological Factors and General Medical Condition – l Psych. factors have major role in onset, severity, exacerbation or maintenance of pain (not dx if criteria for Somatization DO are met) Both psych. factors and med. condition have important roles Associated with a General Medical Condition – Med. condition has major role (low back, sciatic, headache)
Pain Disorder: Prevalence l l Pain Disorder with Psychological Factors is rare Pain Disorder with Medical Factors and Med/Psych Factors more common, especially in Pain Clinics – US, 10 – 15% of adults/year have some type of back-related work injuries – Most people with acute back injuries recover
Pain Disorder: Course of Illness l Acute pain stems from tissue damage (ED, PCP) – l Chronic pain continues after tissue damage is repaired – – l Most people recover Neurological system dysfunctions Occurs in very small portion of people with acute pain Depression strongly associated with chronic pain (not clear which came first) – over than 50% in most studies (Sullivan, 2001)
Pain Disorder: Treatment l Pain is real – – l l l Common for there to be a discrepancy between subjective report of pain and physical findings Important to attend medically to physical c/o pain Provide psychoeducation when/if patient focuses on “cure” – l l Some people are drug-seeking, but not common Complicated if person has chronic pain and also has an opioid addiction More a question of resuming functioning in light of pain “Doctor shopping” is common. The relationship with health care provider is key. Pain Clinics are best practice – Multidisciplinary team of medical, mental health, vocational services, OP, PT, Neuro
Pain Disorder: Medical Treatments (Sullivan, 2001) l l Avoid unnecessary invasive procedures, risk of iatrogenic injury Medications – Antidepressants l l – Anticonvulsants/Mood stabilizers l – SSRIs when co-morbid depression Tricyclics when no concurrent depression More chance of side effects (vs. SSRIs) Opiates l l Last resort Fixed-schedule – Not as-needed as this draws attention to pain as oppose to focus being on increasing function – Better analgesic effect
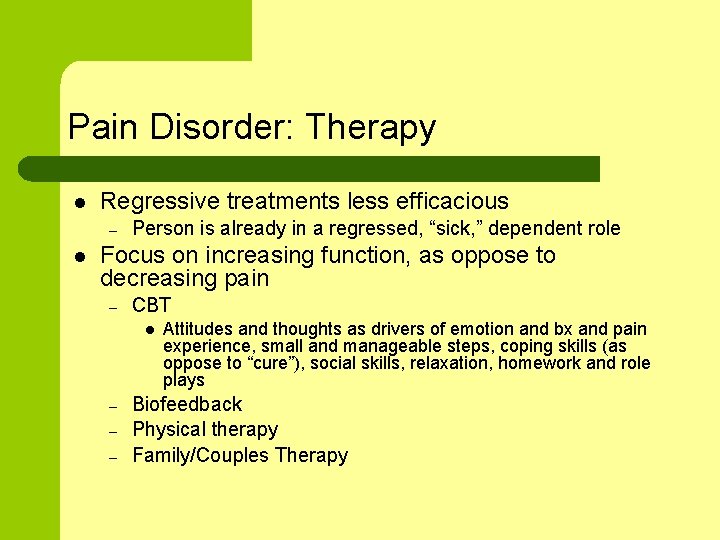
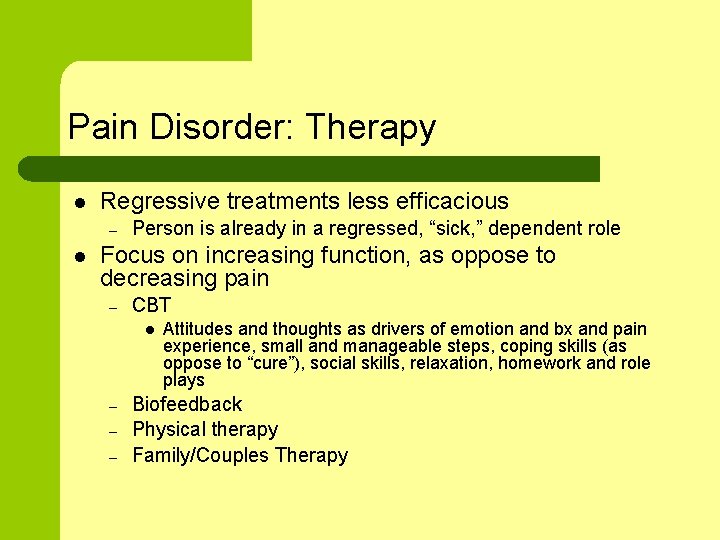
Pain Disorder: Therapy l Regressive treatments less efficacious – l Person is already in a regressed, “sick, ” dependent role Focus on increasing function, as oppose to decreasing pain – CBT l – – – Attitudes and thoughts as drivers of emotion and bx and pain experience, small and manageable steps, coping skills (as oppose to “cure”), social skills, relaxation, homework and role plays Biofeedback Physical therapy Family/Couples Therapy
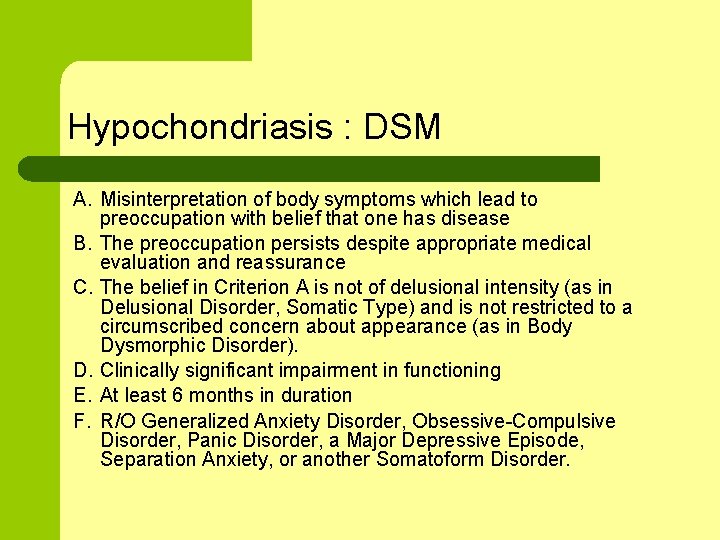
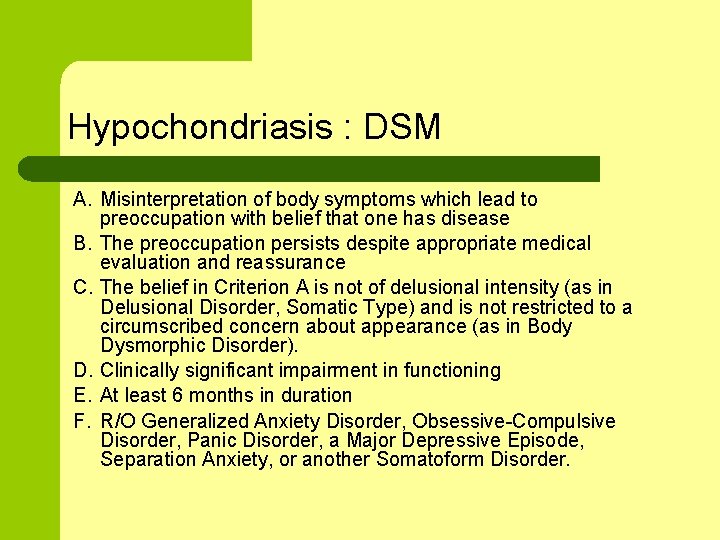
Hypochondriasis : DSM A. Misinterpretation of body symptoms which lead to preoccupation with belief that one has disease B. The preoccupation persists despite appropriate medical evaluation and reassurance C. The belief in Criterion A is not of delusional intensity (as in Delusional Disorder, Somatic Type) and is not restricted to a circumscribed concern about appearance (as in Body Dysmorphic Disorder). D. Clinically significant impairment in functioning E. At least 6 months in duration F. R/O Generalized Anxiety Disorder, Obsessive-Compulsive Disorder, Panic Disorder, a Major Depressive Episode, Separation Anxiety, or another Somatoform Disorder.
Hypochondriasis: Prevalence l l 1 – 5% of general pop 2 – 7% of primary care OPD
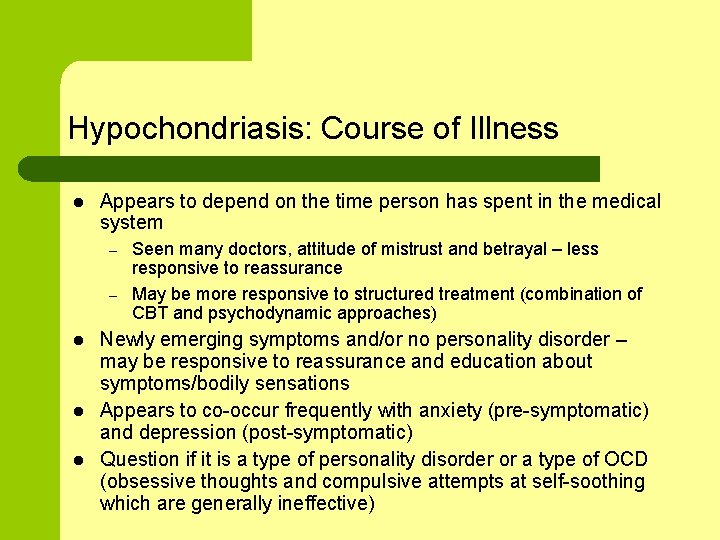
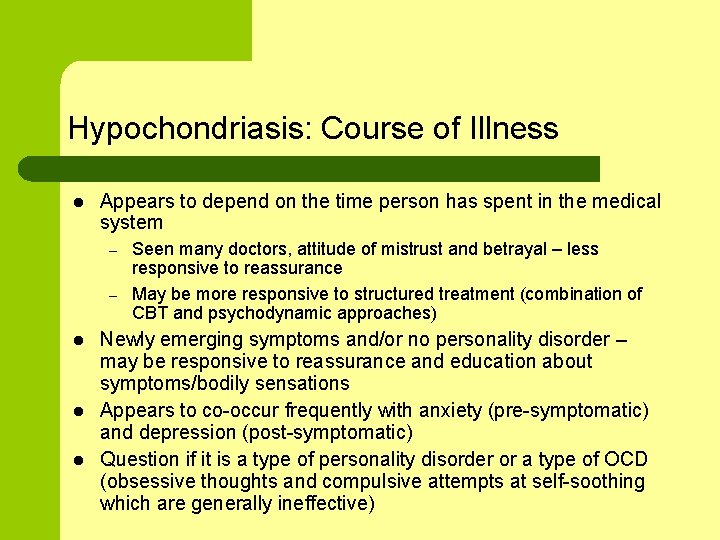
Hypochondriasis: Course of Illness l Appears to depend on the time person has spent in the medical system – – l l l Seen many doctors, attitude of mistrust and betrayal – less responsive to reassurance May be more responsive to structured treatment (combination of CBT and psychodynamic approaches) Newly emerging symptoms and/or no personality disorder – may be responsive to reassurance and education about symptoms/bodily sensations Appears to co-occur frequently with anxiety (pre-symptomatic) and depression (post-symptomatic) Question if it is a type of personality disorder or a type of OCD (obsessive thoughts and compulsive attempts at self-soothing which are generally ineffective)
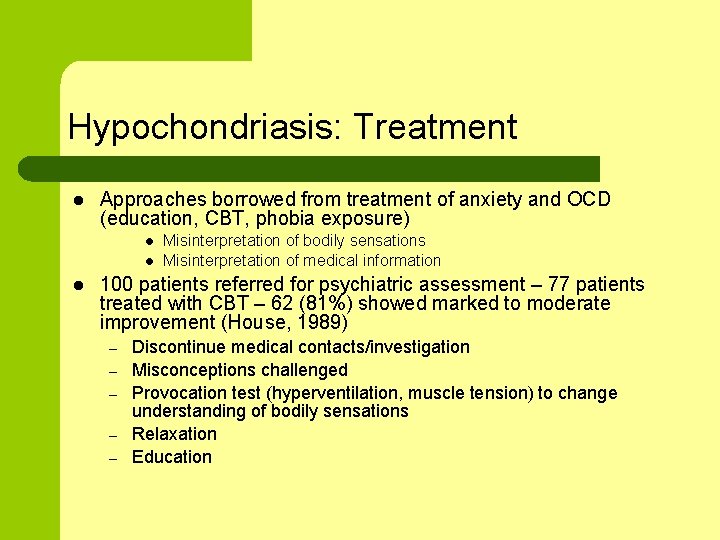
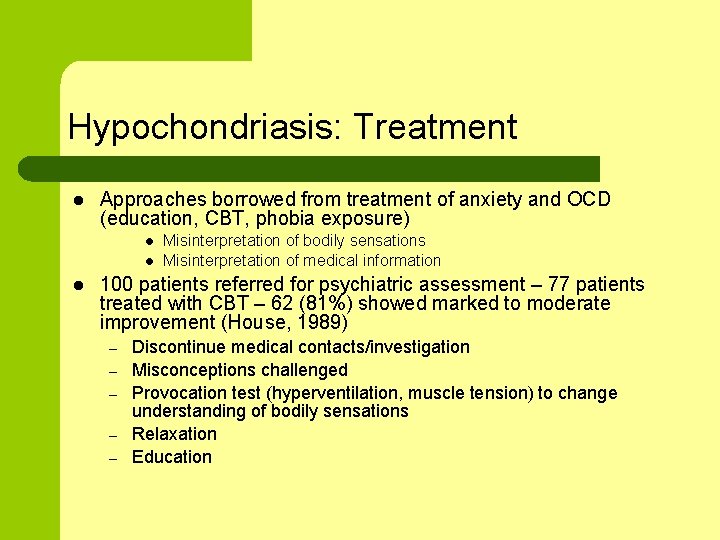
Hypochondriasis: Treatment l Approaches borrowed from treatment of anxiety and OCD (education, CBT, phobia exposure) l l l Misinterpretation of bodily sensations Misinterpretation of medical information 100 patients referred for psychiatric assessment – 77 patients treated with CBT – 62 (81%) showed marked to moderate improvement (House, 1989) – – – Discontinue medical contacts/investigation Misconceptions challenged Provocation test (hyperventilation, muscle tension) to change understanding of bodily sensations Relaxation Education
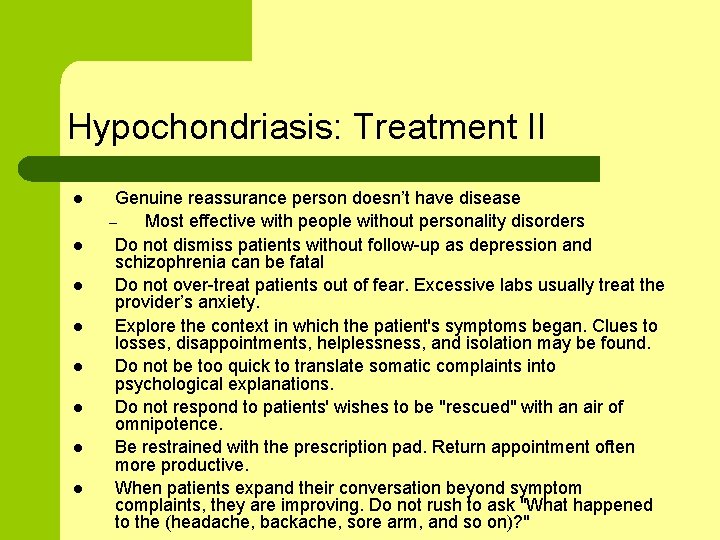
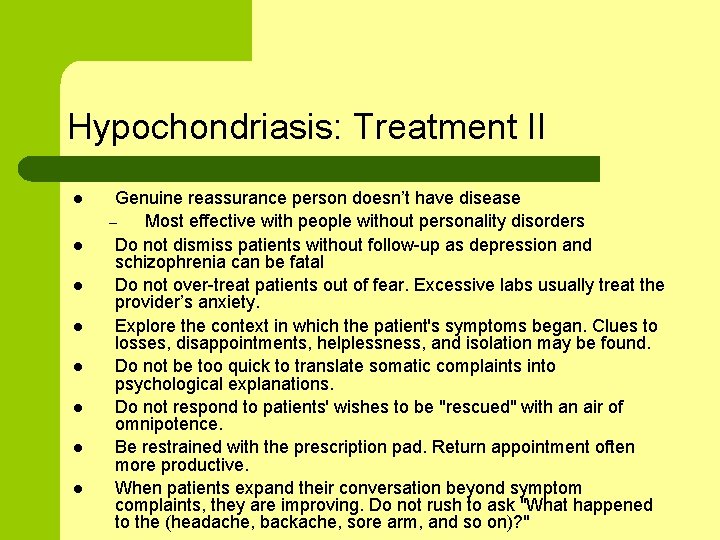
Hypochondriasis: Treatment II l l l l Genuine reassurance person doesn’t have disease – Most effective with people without personality disorders Do not dismiss patients without follow-up as depression and schizophrenia can be fatal Do not over-treat patients out of fear. Excessive labs usually treat the provider’s anxiety. Explore the context in which the patient's symptoms began. Clues to losses, disappointments, helplessness, and isolation may be found. Do not be too quick to translate somatic complaints into psychological explanations. Do not respond to patients' wishes to be "rescued" with an air of omnipotence. Be restrained with the prescription pad. Return appointment often more productive. When patients expand their conversation beyond symptom complaints, they are improving. Do not rush to ask "What happened to the (headache, backache, sore arm, and so on)? "
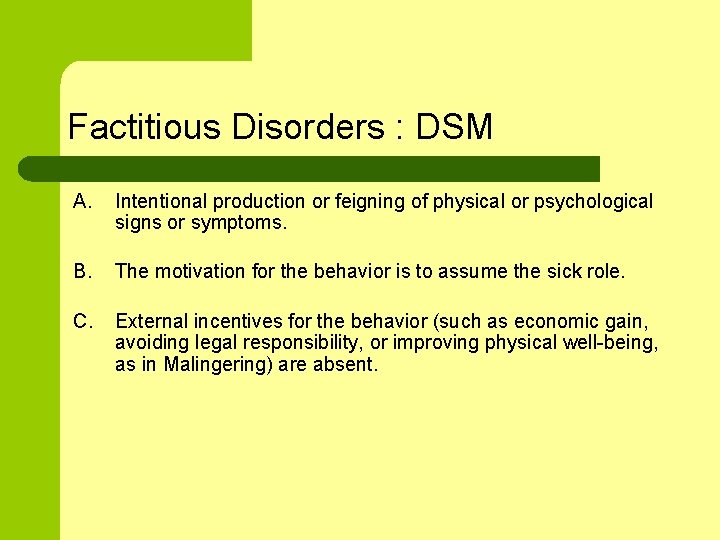
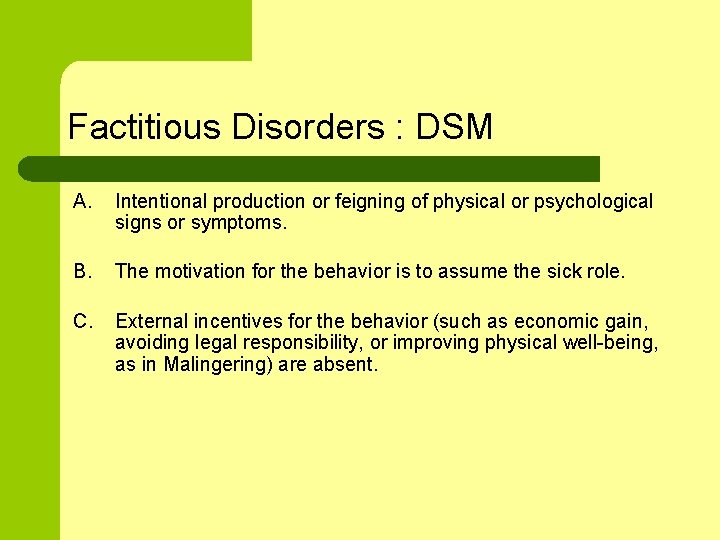
Factitious Disorders : DSM A. Intentional production or feigning of physical or psychological signs or symptoms. B. The motivation for the behavior is to assume the sick role. C. External incentives for the behavior (such as economic gain, avoiding legal responsibility, or improving physical well-being, as in Malingering) are absent.
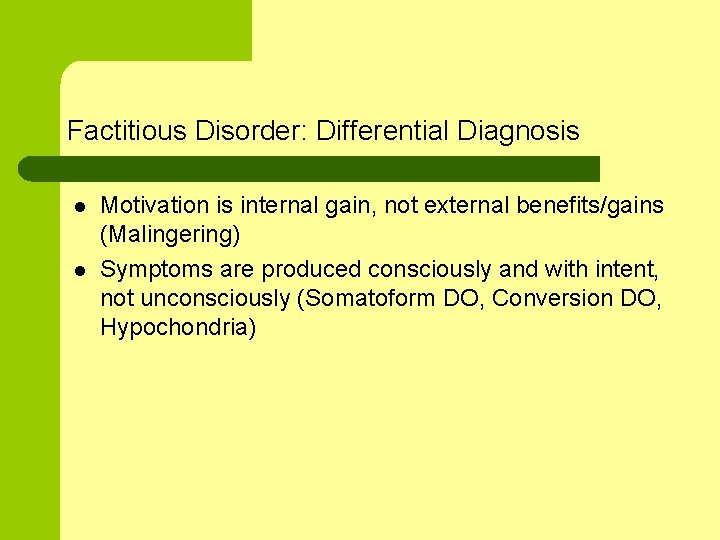
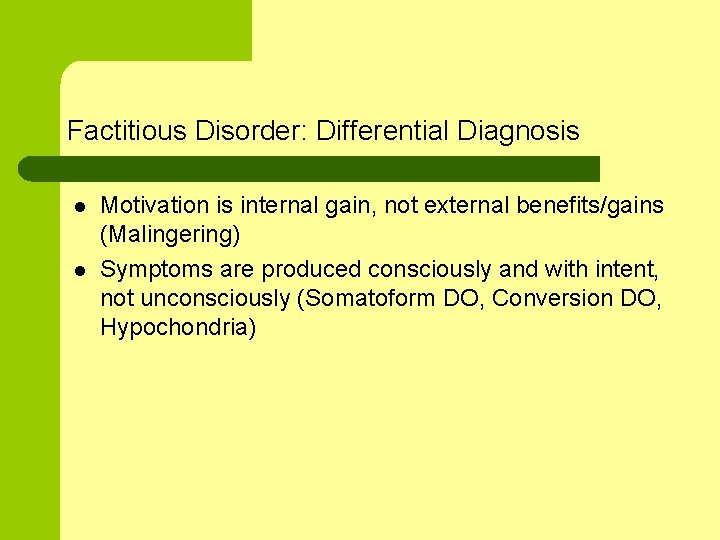
Factitious Disorder: Differential Diagnosis l l Motivation is internal gain, not external benefits/gains (Malingering) Symptoms are produced consciously and with intent, not unconsciously (Somatoform DO, Conversion DO, Hypochondria)
Factitious Disorders : Prevalence l l l Difficult to measure (disorder involves deception) 1% of mental health consults in large, general hospital 50% are male
Factitious Disorders : Course of Illness l l Typically has intermittent episodes Less common is one episode or chronic, ongoing episode
Factitious Disorder: Course of Illness l l Acute onset secondary to stress (easier to treat) – Associated with Axis I dx Munchausen syndrome is at extreme – typically male, often travels and cons people in order to be an patient endlessly. Can be very expensive. – Associated with personality disorder (antisocial and/or borderline)
Factitious Disorders: Assessment l Possible clues: – Hx of having worked in medical field or known others who worked in medical field – Failure to respond to medical treatment – Inconsistent medical findings – Collateral information is very important ‣ Request prior medical records – Appearance of being socially isolated ‣ Few visitors despite serious medical problem
Factitious Disorder: Etiology l l l Mastery/Masochism – Create illness to master having experienced illness as a child or being abused Dependency gratification – Dependency needs not adequately met during childhood Defense against loss
Factitious Disorders : Treatment l l Earlier, illegal strategy – List circulated to forbid admissions Confrontation in a non-punitive, validating way – This is a coping skill for dealing with stress, let’s see if we can help you develop some healthier coping skills. – May be experienced by pt as shameful and pt may flee to another provider/hospital.
Factitious Disorders : Case Study l Action Team Client – Factitious vs. Dissociative
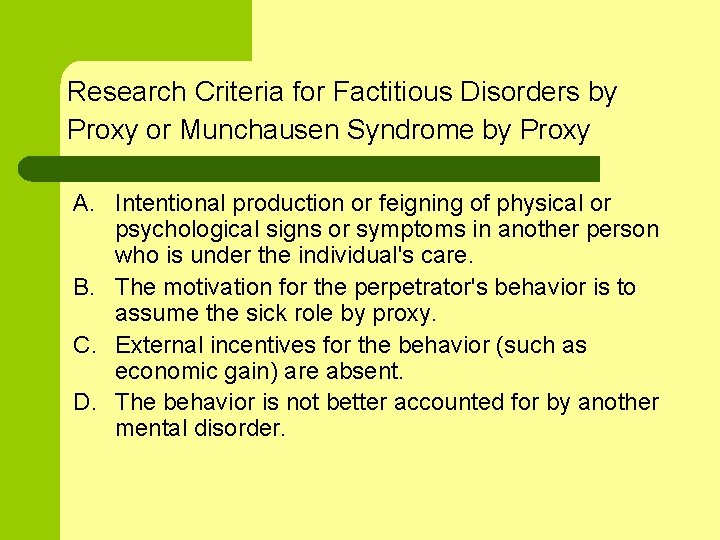
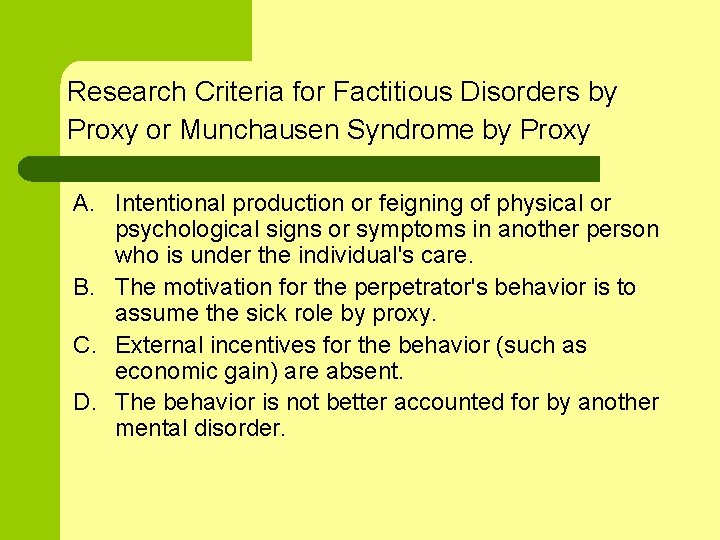
Research Criteria for Factitious Disorders by Proxy or Munchausen Syndrome by Proxy A. Intentional production or feigning of physical or psychological signs or symptoms in another person who is under the individual's care. B. The motivation for the perpetrator's behavior is to assume the sick role by proxy. C. External incentives for the behavior (such as economic gain) are absent. D. The behavior is not better accounted for by another mental disorder.
Malingering: DSM l l l False or grossly exaggerated medical or psychiatric symptoms are intentionally produced Motivation is some type of external gain – Avoid work, military service, criminal sentencing – Obtain drugs, financial gain May be adaptive in some situations (kidnapped, abuse)
Malingering: Treatment l l l Management, not treatment Be direct and discuss your assessment with patient – They may disclose at this point – Beware your own countertransference. You may feel angry at having been lied to and conned. Avoid shame-based retribution. Rare in people with chronic pain, those who seek disability
Case Examples l Woman moved here from another part of the state. Some confirmation of her story. Homeless. REPEATED use of ER and psych. hospital. Precipitous discharges. – l Gentleman recently DC’ed SHH, presents next day wanting hospitalization and medications. Providers disagree. – l Factitious vs. malingering vs. dissociative Factitious vs. malingering vs. psychotic Increase in late fall of presentation in ER of homeless folks – Malingering vs. depression secondary to environmental change
Sources/More Information l l l l Treatments of Psychiatric Disorders, 3 rd Ed. (2001), Editor Glen O. Gabbard, M. D. DSM-IV-TR The Anxiety & Phobia Workbook (2005) by Edmund J. Bourne Aaron T. Beck, Cognitive Therapy Inside Out and Outside In (2000) by Joan Berzoff, Laura Melano Flanagan, Patricia Hertz Freud and Beyond: A History of Modern Psychoanalytic Thought (1996) by Stephen A. Mitchell, Margaret J. Black Holloway, K. L. and K. J. Zerbe, Simplified approach to somatization disorder: When less may prove to be more. Postgraduate Medicine 2000; 108(6): 89 -95. Psychoanalytic Diagnosis: Understanding Personality Structure in the Clinical Process (1994) by Nancy Mc. Williams.